Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/21/52. The contractual start date was in November 2015. The final report began editorial review in September 2019 and was accepted for publication in March 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Janssens et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Context
Introduction
This report presents the results of a mixed-methods study conducted between 2015 and 2019 exploring the transition of young people with attention deficit hyperactivity disorder (ADHD) from child to adult health services. First, we provide a brief overview of the arrangement of health services for ADHD in the UK and the existing literature, before describing study objectives. Chapter 2 describes the methodology of this three-strand mixed-methods study (Figure 1). The following three chapters then focus on each of these strands. In Chapter 3, surveillance methods suited to the study of rare conditions/difficulties are used to estimate the national incidence of young people who are in need of a transition, and the incidence rate of successful transition. Chapter 4 maps service availability for adults with ADHD. In Chapter 5 we present the patient, carer and clinician perspectives and experiences of the transition process. The final chapter integrates the results of each of the strands before presenting our conclusions, recommendations for future research and examples of the impact of our work to date.
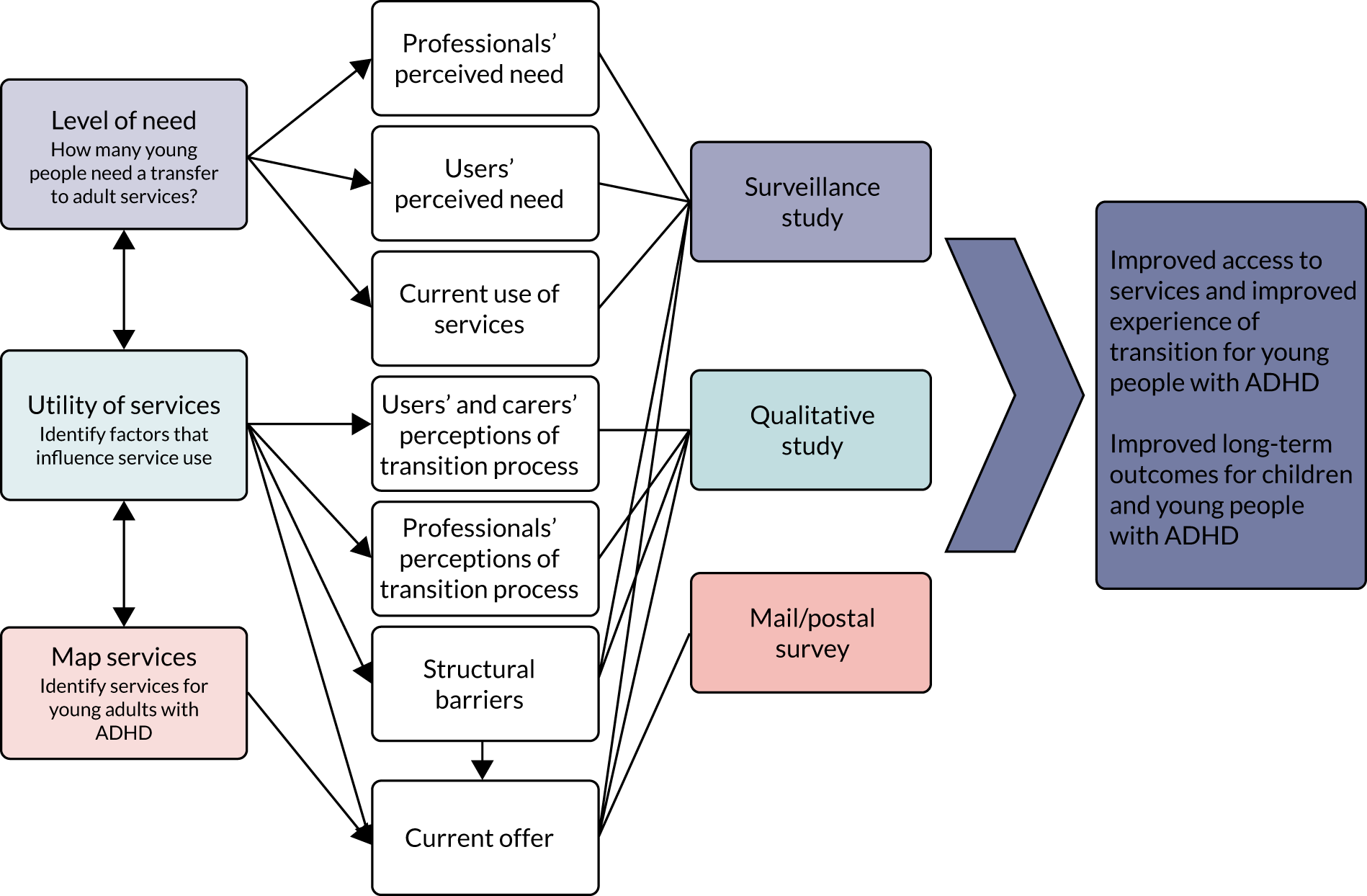
FIGURE 1.
Three strands of the CATCh-uS mixed-method study.
The relationship between a provider and a receiver of health care depends on how they address each other; it is one of the most important and sensitive relationships. The receiver has been historically referred to as a ‘patient’. In recent times, the use of terms such as ‘service user’ and ‘client’ has become commonplace. Some of these terms have their origins outside health care and may not encompass the sacred and sensitive relationship that is found between a patient and a clinician. We do not generally check with our patients how they would like to be referred to. Interestingly, research carried out in this area supports the long-held practice, as a large majority of patients (73–77%) prefer to be referred to as such, in a clinical setting. 1,2 The Royal College of Psychiatrists also explored this issue and concluded that ‘the term patient would be used in all College documents’. 1 For this reason, we will use the term ‘patient’ in this report.
Some of the results and study methodology have been discussed further in separate scientific papers. Where appropriate, these are referenced within the report and a list is provided in the Impact section of the report. Further papers based on this study will be added to the list on the project web page as and when they are published. For a list of further project documentation available, see Report Supplementary Material 1–28. For any further information, please contact catchus@exeter.ac.uk.
The Chief Medical Officer (CMO)’s 2012 report entitled Our Children Deserve Better: Prevention Pays3 acknowledged that we need to improve access for patients with ADHD in transition from child to adult services. The most recent UK data on transition revealed that one in two young people with ADHD and an ongoing clinical need do not transfer to or engage with adult mental health services (AMHS). 4 The CMO’s report identified that the annual short-term costs of emotional, conduct and hyperkinetic disorders among children aged 5–15 years in the UK are estimated to be £1.58B and the long-term costs £2.35B. Key themes emerged around the importance of data sharing, service provision and prevention, with the report concluding with a call for a programme of evaluative research that increases the knowledge base as the burden of disease continues to shift towards long-term conditions.
Attention deficit hyperactivity disorder as a long-term condition
Attention deficit hyperactivity disorder is classified as a childhood-onset neurodevelopmental disorder defined by the presence of a persistent pattern of inattention and/or hyperactivity–impulsivity that interferes with functioning or development. 5 People with ADHD often find organisation and time management challenging, with associated negative outcomes in education, employment and relationships. 6 They are at an increased risk of mortality, driving accidents and divorce, and have higher rates of criminal justice contact, particularly if left untreated. 6–9 ADHD is also commonly associated with comorbid anxiety, mood difficulties and substance abuse. 10–12 There are effective interventions,13–17 and there is a risk of potential and preventable adverse health outcomes if individuals disengage from treatment. 18–21 There is evidence that treatment with medication is associated with a significant reduction in drug and alcohol disorders,22 a reduction in the likelihood of road traffic accidents in males23 and a reduction in criminality rates of > 30% compared with periods of no treatment. 24
Originally conceptualised as a disorder of childhood, ADHD is now recognised as a long-term condition, with many experiencing ongoing difficulties into adulthood. Cross-sectional epidemiological surveys found that 5–6% of children and 3–4% of adults meet Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), criteria for ADHD. 25–28 Meta-analysis of follow-up studies of children with ADHD found that 15% retain the full diagnostic criteria by the age of 25 years, and a further 50% struggle with subthreshold symptoms and continued impairments. 29 Other studies report similar persistence of impairment into adulthood. 30–32 Since 2008, the National Institute for Health and Care Excellence (NICE) treatment guidelines have recognised and formalised ADHD’s status as a long-term condition, recommending lifelong, age-appropriate service provision. 33–36 NICE guidelines recommend that there should be continuity of care for people with ADHD, and that they should be treated by health-care professionals with training and expertise in diagnosing and managing ADHD. 36 The guidelines officially apply to England only, but are widely accepted as indicators of best practice across the UK.
Transition in health-care services
In the context of health care, transition extends beyond the simple transfer of clinical responsibility to supporting a young person towards and onto a new life stage. 37 Existing evidence indicates optimum transition is characterised by planning, information transfer across teams, joint working between teams and continuity of care during and following the transfer. 38 The importance of getting health-care transitions right for young people with long-term health conditions is increasingly recognised. 39,40 NICE has published a guideline for transition from children’s to adults’ services for young people using health or social care services;41 however, these are not condition specific and do not address barriers to the transition process. Rigorous evaluation of different models of transitional care is needed. 42
A recent longitudinal study of young people in the UK with a range of long-term conditions [i.e. diabetes, cerebral palsy and autism spectrum condition (ASC)] found three features of transitional health care that were strongly associated with better outcomes: appropriate parent involvement, promotion of health self-efficacy and meeting the adult team before transfer. 43 This observational study also found differences in transitional experiences between health conditions, indicating gaps that need to be addressed through service development. 43 A systematic review of barriers to transition from paediatric to adult care across chronic illness groups in the USA found that each chronic illness presented specific challenges. Certain barriers were universal, including difficulties with changing relationships, difficulties accessing or funding adult services, negative beliefs about adult care, lack of knowledge about the transition process and lack of self-management skills. 44
Several studies45–47 on transition for both physical and mental health conditions have found that young people, families and clinicians experience transition and the provision of support by health services differently. This underlines the importance of consulting with patients, their families and providers, to better understand key aspects of transition. Existing research suggests that a seamless transition process between child and adult services happens much less often than can be expected based on adult prevalence rates. 4 Poor transition may result in young people with ongoing needs disengaging from services48,49 and experiencing poorer health as a result. Transitions, even successful ones, are often stressful. Adolescence is a life stage that is characterised by major developmental changes and challenges. There is considerable development at the level of behaviour, cognition and the brain,50 and the timing of transition can coincide with other important changes in young people’s lives, such as leaving school, starting further education or employment, and leaving care. 51
The transition from Child and Adolescent Mental Health Services (CAMHS) to AMHS poses particular challenges, as the peak onset for severe and enduring mental illness falls in the late teens around the age boundary between services focused on children and those focused on adults. 52 This is further compounded by differences in thresholds and focus between CAMHS and AMHS, leaving a proportion of children without a clear pathway into adult services. 53,54 Several studies, government documents and policy guidelines highlight the difficulty faced by young people who require a transition from child to adult services. 39,53 Young people with neurodevelopmental disorders, such as ADHD, may be less likely to make the transfer from child to adult health care. 39,53 Studies of long-term conditions, such as ADHD, rarely follow participants across developmental transitions,55,56 and national empirical data on the number of young people who wish to access ongoing care for ADHD in adulthood or the number that successfully access follow-up care in early adulthood are sparse. To our knowledge, there has yet to be an in-depth study of this issue in the UK.
Two multimethod studies of transition and a case note review in mental health have demonstrated that transition is often poorly planned, lacks co-ordination and frequently results in discontinuity of care, particularly for children with neurodevelopmental disorders such as ADHD. 53,56,57 The limited qualitative research available also indicates that unsupported or non-existent transition for young people with ADHD, combined with inadequate adult service provision, leads to cessation of treatment and emotional distress for young people with ADHD and their families. 58,59 The lack of a national estimate of service leavers hampers commissioning and provision of services for this group. The latter is made even more difficult by a lack of national-level data on existing services for young adults with ADHD.
UK and Ireland mental health services configuration
Health service organisation varies widely across the world, as well as within countries over time. The focus on the UK and Ireland in this chapter provides the context for the programme of research that we will describe. The study had a UK focus, but the surveillance study was carried out in the UK and Ireland because Ireland reports to the Child and Adolescent Psychiatry Surveillance System (CAPSS) so its exclusion from the CATCh-uS study was logistically impossible; therefore, a brief discussion of Irish health-care models is included. Different models and the international context will be discussed in Chapter 6.
In the UK, taxation provides a health-care service via the NHS that is free to access at the point of delivery. Health care for children with ADHD may be provided by CAMHS teams or community paediatricians, often depending on whether or not there are other mental health or physical illnesses, or developmental delay. Children’s services are commissioned to provide care until a patient is 16–18 years old, sometimes with stipulations about remaining in education for older teenagers. Adult services for individuals with ADHD may be provided by community-based AMHS, shared care agreements between psychiatrists and general practitioners (GPs), the private sector or voluntary organisations.
Box 1 provides an overview of provider organisations across the UK and Ireland, with subtle differences between countries. The King’s Fund (London, UK) has produced a helpful summary of commissioning of government-funded health services in England, which it defines as ‘the process by which health and care services are planned, purchased and monitored’ (Reproduced with permission from The King’s Fund. 60 This is distributed in accordance with the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 licence. See: https://creativecommons.org/licenses/by-nc-nd/4.0/). 60 As they indicate, service configurations and commissioning processes change over time. During data collection for the CATCh-uS study there were geographical variations in provision depending on the local Clinical Commissioning Groups (CCGs), NHS England, local authorities or collaborative commissioning groups for specialised services. Other bodies, such as sustainability and transformation partnerships and devolved cities and local authorities, may also influence what is provided. 61 Commissioning in Scotland, Wales and Northern Ireland differs from that in England and between the three nations according to which health-related issues are devolved from the UK Parliament to the Scottish or Welsh Parliaments or Northern Ireland Assembly, as well as the constituent agencies and ‘arm’s length’ partner organisations involved. 62–64 In general, the devolved nations have largely avoided the market-based reforms that are increasingly adopted by the English health system.
In England, government-funded services may be delivered by:
-
NHS organisations (e.g. NHS trusts)
-
national or specialist services (directly commissioned by NHS England)
-
single private sector or third-sector organisations (i.e. non-governmental and non-profit-making organisations or associations, including charities)
-
conglomerates of NHS and/or private sector and/or third-sector organisations.
In Scotland [see Scotland’s Health; URL: www.scot.nhs.uk/organisations/ (accessed 19 September 2020)], such services are delivered by:
-
fourteen regional NHS boards
-
seven special NHS boards that provide a range of specialist and national services.
In Wales [see Health in Wales; URL: www.wales.nhs.uk/ourservices (accessed 19 September 2020)], such services are delivered through a variety of providers, including:
-
local health boards
-
NHS trusts.
In Northern Ireland [see Health and Social Care ONLiNE; URL: http://online.hscni.net/ (accessed 19 September 2020)], services are provided by:
-
six health trusts
-
the Health and Social Care (HSC) board
-
other HSC agencies.
In the Republic of Ireland, the Health Services Executive delivers mental health services [URL: www.hse.ie/eng/services/list/4/mental-health-services/services/ (accessed 19 September 2020)].
In Ireland, government-funded health care is managed by the Heath Service Executive (HSE). A person living in Ireland for at least 1 year is considered by the HSE to be ‘ordinarily resident’ and is entitled to either full eligibility (category 1) or limited eligibility (category 2) for health services. If an ordinary resident attends an outpatient department of a public hospital without being referred by a GP, he or she may be charged a standard fee. 65 All five nations have private health-care provision.
Health services change over time,60 and there is no ‘definitive’ way to ensure that health service workers, patients, carers and commissioners identify the same ‘unit of service’. For example, in England, a patient might report a locality base that they attend, which organisationally falls under a community mental health team (CMHT), which in turn might be one of a number of CMHTs forming an adult community mental health service, which in turn may be a directorate within an NHS trust that also provides learning disability (LD) liaison and inpatient mental health care. A clinician might report to the CMHT within which they work or to the directorate or the trust that employs them. A commissioner could report to NHS trusts or tender-winning conglomerates within their purview. To further complicate matters, some highly specialist services may be set up and commissioned as national or regional services. Clarity of definitions as well as the time and location at which data were collected are, therefore, key to thinking about health service provision. We defined services as ‘dedicated’ services where the service name indicated that it had dedicated staff to see adult patients with ADHD, and defined other AMHS where the name of the service did not communicate ADHD-specific dedicated time or resource as ‘generic’ services.
Need for the current study
Attention deficit hyperactivity disorder is one of the most common long-term conditions managed by child mental health and paediatric services,66 and an increasingly large cohort of young adults who have been diagnosed and managed within children’s services are growing out of the remit of these. Previous studies have reported the proportion of young people with ADHD who reach adulthood with an ongoing need for services for residual difficulties from general population surveys. 25–28 However, we have no national figure for young people in services who reach the end of child service’s provision and have an ongoing need for service input, nor do we have a national figure for successful transition.
As ADHD has been only recently recognised as a life-long condition, service configuration and workforce development have yet to respond to the growing ongoing treatment needs of adults with ADHD. 67,68 Adult community mental health services are often not configured to work with young adults with ADHD, who struggle with rather different issues to those of individuals with chronic psychosis, or personality, eating and affective disorders, who constitute the majority of AMHS attenders. Many adult mental health practitioners lack experience and/or training in the management of ADHD as training pathways diverge into specialisation early, and for many practitioners who have been in generic roles, such as nursing, occupational therapy and social work, it may be largely absent prior to qualification;69 some have negative or sceptical attitudes towards ADHD as a condition that warrants intervention. 70–73 Similarly, very few GPs have direct experience of child psychiatry and are unfamiliar with ADHD management without support from specialist services. 74 In the UK, at least, patchy service provision leaves young people with ADHD particularly vulnerable to poor transition or loss of service. Recent research reported that half of health trusts have prematurely discharged young people with ADHD from CAMHS because there were no suitable adult services. 75
In summary, there is perception of significant problems in the health-care transitions of young people with ADHD. However, we lack evidence to inform change in policy and practice: we do not know how many young people in the UK need to transition to adult services for ongoing management of their treatment, we do not know which services support young people with ADHD, and there is no evidence on the experiences of young people at all stages of the transition process (pre, post and no transition). This research aimed to address these gaps by exploring what happens to young adults with an ongoing need for management of their ADHD when they are too old for children’s services.
Research objectives
-
To assess the current need for adult services for young people with ADHD and describe young people with ADHD in need of a transfer to adult services.
-
To identify the range and type of services that are currently available for young people with ADHD in transition from childhood to adulthood.
-
To explore the quality of service delivery during transition and identify factors that (1) influence the experience of transition and could improve continuity of care and (2) contribute to disengagement and subsequent (dis)continuation of treatment.
Chapter 2 Study design
The study adopts a mixed-methods design incorporating three inter-related research strands to answer each of the study objectives: (1) a surveillance of young people diagnosed with ADHD who have ongoing service needs as they cross the upper age boundary of their service, (2) a mapping study to identify and describe services for adults with ADHD and (3) a qualitative study to explore the views and experiences of patients, parents and service providers of the transition process from children’s to adults’ health care. The study protocol is depicted in Figure 2. In this chapter, the reasoning for the mixed-methods approach is explained, followed by a description of the surveillance, mapping and qualitative methods and any changes to the protocol for each strand. Further details about each strand’s method can be found in later chapters. The governance and ethics approval for this project is also described in this chapter. Members of the public actively advised on each stage of this study and a description of this public involvement is also presented below.
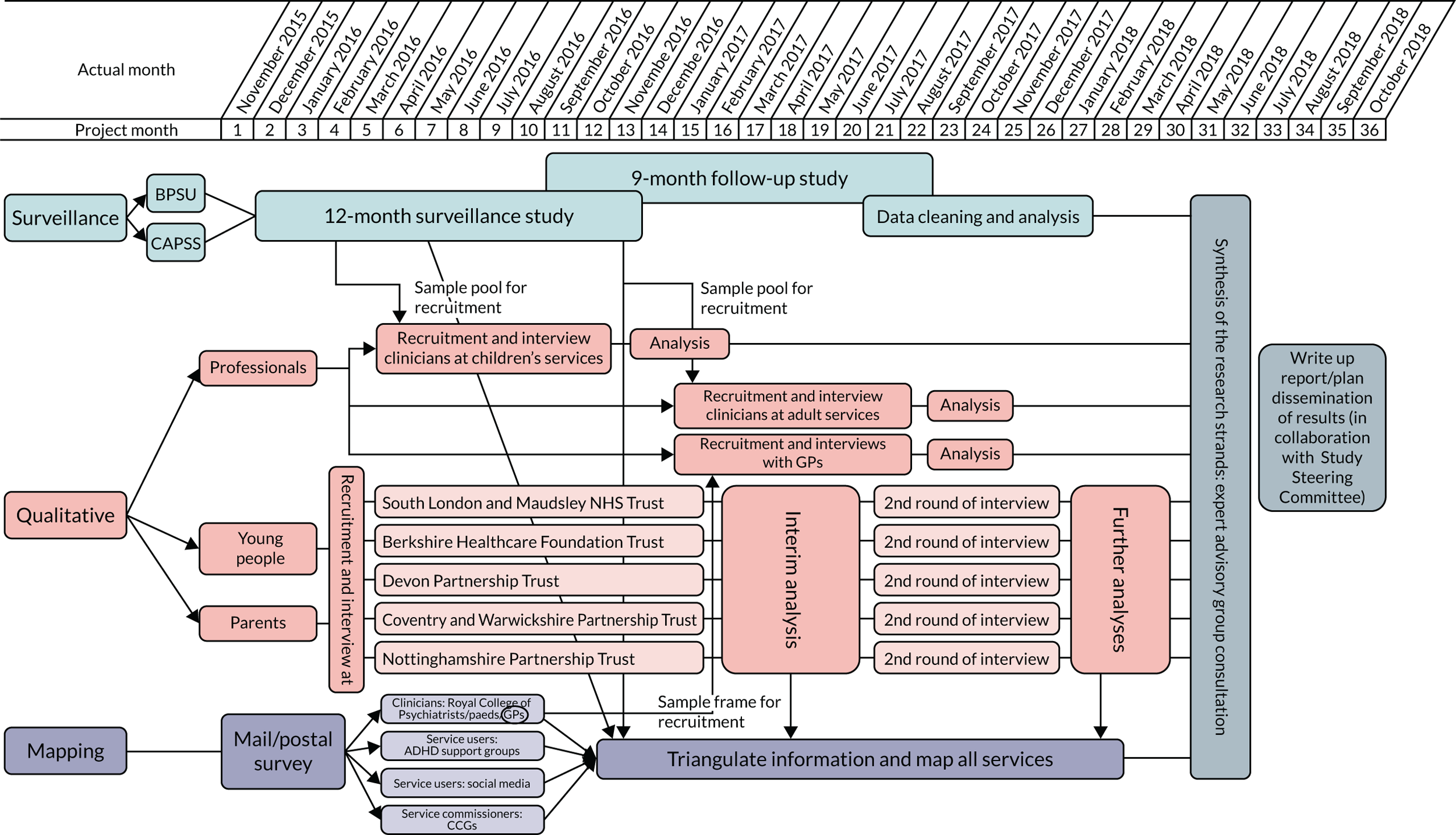
FIGURE 2.
Study protocol.
Mixed-methods approach
We took an interactive, systems-based approach to design the study76 to address our three research questions, as illustrated in Figure 1. The multistrand design allowed us to consider and integrate multiple components of research design to reflect the inter-related nature of the questions and choose methods to provide the best available data. Some strands were designed to be conducted sequentially, as the results of one strand fed into the design of another; other strands were designed to be completed concurrently (see Figure 2). The three strands were strongly interlinked and designed to complement each other; for example, the surveillance and qualitative strands both studied various elements of the transition process as well as its success. The data collected via the surveillance provided a national insight into the transition to adult services and how this was organised. The qualitative strand delivered context to the national data and contextual understanding; with in-depth interviews, we explored the reasons behind successful or failed transitions from participating trusts. The surveillance and mapping studies interacted in a similar way with the qualitative study: a database with services accessed by young people and young adults with ADHD served as a sample pool for interviews with clinicians and was checked against the services reported in the mapping study. We required mixed methods for several reasons; we needed the best methods to address the different research questions but, overall, the study was designed to facilitate data triangulation and provide greater validity for the findings. 77,78 Together, the three strands allowed us to provide detailed understanding of the transition of young adults with ADHD in the UK.
Strand 1: the surveillance study
This strand aimed to determine how many young people with ADHD need to transfer to adult services because of ongoing treatment needs. We used two existing methods to assess ongoing service need for young people with ADHD when they are too old for children’s services: a surveillance methodology triangulated with an electronic clinical case note search. The surveillance study ran from November 2015 to August 2017 in parallel through the CAPSS and the British Paediatric Surveillance Unit (BPSU). 79,80 These systems collect prospective reports of cases seen from all consultants registered with the Royal Colleges. Over a period of 13 months (November 2015 to December 2016), consultant paediatricians and child psychiatrists in the UK and Ireland were asked to report patients who were within 6 months of the age boundary of their service who had been diagnosed with ADHD, were on medication and required ongoing services for their medication management. After 9 months (between August 2016 and August 2017), a follow-up questionnaire was sent to the reporting clinician to establish if the young person had been successfully referred to adult services, and data were collected on aspects of optimal transition and the adult services to which they had been referred. This strand was restricted to transition for young people with ADHD who required medication because of the requirement for an unambiguous definition of service need that would be understood similarly by paediatricians and psychiatrists. This means that the estimates produced will necessarily reflect only a minimum level of the need for transition, as young people may change their minds about the role of medication. The qualitative and mapping strands covered transition to adult services for any reason, including medication.
Changes to the study protocol for strand 1
Our application to CAPSS and BPSU required estimates of the number of expected cases, which we based on the best available evidence to be three transition cases per provider trust over 12 months. These units are designed for rare conditions, or fewer than 300 notifications per year, although our estimates suggested a total of 573 cases. 4,56 To protect the participating clinicians from respondent fatigue, BPSU and CAPSS agreed to run the surveillance for 6 months, with the possibility to extend to the more usual period of 12 months should the number of reported cases be fewer than anticipated. We received 138 notifications from BPSU during the first 6 months, 58 of which were eligible for the study. Case notifications for CAPSS were very similar with 118 notifications, of which 38 were eligible for the study. These numbers presented a case for extension to both BPSU and CAPSS, which was approved.
The BPSU and CAPSS encourage the use of additional reporting sources to check for any cases that might have been missed by the original data source. South London and Maudsley NHS Foundation Trust (SLaM) has created an anonymised, regulated database of clinical records for research purposes: the Clinical Record Interactive Search (CRIS). SLaM was one of five trusts associated with this project and, after the submission of the initial protocol, we were granted access to the database to complete a complementary piece of research that provided data that supported the calculation of a national estimate for transition incidence. This allowed us to compare transition from CAMHS to AMHS in SLaM with reports from CAPSS. Unfortunately, there were no comparable data sets for transition from paediatric services to AMHS. Additionally, SLaM is a national centre of excellence for mental health, with national and specialist services for children and for adults with ADHD, as well as local teams for both age groups in each borough of London served. This level of provision is not representative of the UK.
There was also a minor change to the terminology used in the definition in the first month of the 13-month surveillance period as there was some misunderstanding among clinicians (see Chapter 3, Data validation).
Strand 2: the mapping study
Previous studies have investigated services for young people with ADHD; however, their findings could not be linked to a geographical location. The aim of this part of the study was to map the variation in NHS AMHS for young people with ADHD in the UK. To maximise the completeness of our map, we collected data using an online survey from different sources:
-
those receiving treatment/support (patients)
-
those providing services (clinicians, health-care professionals)
-
those funding services (commissioners).
The technique was piloted in 2016. After an iterative process of trialling and refining the methodology, the mapping survey was repeated in 2017. Service provision information collected via the surveillance and qualitative strands were included in the mapping study.
Changes to the study protocol for strand 2
At the project start-up meeting [with co-applicants and members of the Study Steering Committee (SSC) present] it became evident that seeking one informant per area to inform the national service provision map would fail to deliver a complete map. The clinicians and researchers who were present had conflicting information on service provision for some areas because of the idiosyncratic knowledge of individuals. The mapping study developed into a multistakeholder, multi-informant study that included a pilot phase to test the new methodology. We had not planned a pilot for this work, yet it proved essential to work out which stakeholders to include and the most efficient method of mapping services to produce a useful and accurate map.
Strand 3: the qualitative study
Qualitative research with individuals representing four key stakeholder groups was carried out. Semistructured interviews were used to gather data relevant to generating a detailed understanding of heath-care transitions in the UK for patients with ADHD. The four stakeholder groups were:
-
young people with ADHD at different stages in the transition (pre transition, post transition and those who disengage and do not transition but return to adult services later)
-
parents of young people with ADHD who identify themselves as a primary carer, again representing different stages in transition
-
clinicians in children’s services
-
clinicians in adult services.
Paediatricians and child psychiatrists who reported cases to the surveillance study were invited to take part in an in-depth interview on transition. Information collected regarding the reported cases included details of the ongoing referral; this information was used to identify and approach clinicians working in adult services. The initial design involved recruitment of patients and parents from five different NHS trusts purposefully chosen to represent different service provision models and geographical spread. Individual interviews were conducted face to face or by telephone. Data were analysed thematically using a framework analysis approach. NVivo (QSR International, Warrington, UK) version 10 software was used to facilitate systematic and transparent analysis.
Changes to the study protocol for strand 3
The adoption of the CATCh-uS study by the National Institute for Health Research (NIHR) portfolio created a lot of interest among health trusts, which then contributed to the study and requested to be added as recruitment sites. This offered an opportunity to diversify our sample geographically and increase the diversity of service models accessed by the recruited patients (with or without follow-up services within or outside the trusts).
In addition, preliminary analysis of our interviews with clinicians highlighted primary care as a potential ‘destination’ for patients with ADHD leaving children’s health care, particularly for young people dropping out of services or for whom no ongoing services were available. Representation of GPs was not originally included in the design of the qualitative study; however, given no existing studies could be identified that included this stakeholder group, the decision was taken, in consultation with the SCC and with approval from our programme manager at NIHR, to recruit a sample of GPs. It was possible to resource this work from the existing funding envelope.
Research governance and ethics
We started informal discussions with the University of Exeter Medical School (UEMS) Research Ethics Committee (REC) and the NHS REC/Health Research Authority (HRA) regarding which of these bodies we should apply for ethics approval shortly after the study was accepted for a stage 2 application of the NIHR Health Services and Delivery Research programme funding call for long-term conditions. As a result of a change in the ethics approval system (HRA replacing NHS REC for multisite studies), we had to go through all systems: HRA (17 June 2016) and NHS REC and research and development (R&D) governance processes for each individual trust participating in the study (the last trust was approved by the HRA on 20 January 2017). Ethics approval from the UEMS REC was sought to assure that some elements of the study, which did not require NHS REC approval, were approved to ensure a timely start.
The CATCh-uS study and subsequent amendments received ethics committee approval from the National Research Ethics Service (NRES) Committee Yorkshire and the Humber – South Yorkshire; the original protocol was approved in October 2015 (REC reference 15/YH/0426). Both surveillance units, CAPSS and BPSU, by virtue of their rigorous two-stage application processes, have HRA approval for access to case note information without patient/parent consent, provided that the study has Confidentiality Advisory Group (CAG) approval. CAG approval is a fast-track process occurring as a result of the established rigour of the application process to the surveillance units that prospective studies go through. This type of surveillance required HRA approval as cases may be reported from any NHS trust that works with children. In addition, a section 251 approval was required from and granted by the CAG to permit clinicians to report anonymous case note information without patient/parent consent provided there is no requirement or expectation for additional patient contact as a result of the study (CAG reference number 15/CAG/0184). The CRIS was approved as an anonymised data resource for secondary analysis by Oxfordshire REC (08/H0606/71+5). The searches that were run as part of this project were reviewed and approved by the CRIS patient-led oversight committee (CRIS reference: 961).
Research and development approval was sought and gained in all 12 hospital trusts that contributed to the qualitative strand of the study; letters of access were sought for the data collection in these sites. The researchers collecting data had enhanced Criminal Records Bureau clearance and current Good Clinical Practice training certificates and were issued with research passports to access the premises and conduct interviews with NHS patients on site. Gaining R&D approvals, however, was a complex and often lengthy process, differing logistically and administratively from site to site, and in some sites delayed patient recruitment for several weeks. The full CATCh-uS study and subsequent amendments obtained ethics approval from the UEMS Ethics Committee. The original protocol was approved in December 2015 (reference: PF/CB/15/07/070).
Obstacles in obtaining ethics approval
The need to approach several different local R&D committees in addition to a central REC (and despite central ethics approval already having been given) led to very significant delays in recruitment. Opinions vary across R&D committees about how to conduct research with children or adults with mental health problems, for example the appropriateness of seeking assent from minors. The absence of systematic patient databases often hindered case finding. The surveillance study was CAG approved; yet some trusts were reluctant for their clinicians to contribute to the BPSU and CAPSS surveillance study unless we also had R&D approval from their trust, despite HRA approval. They did not allow their clinicians to spend time completing the paperwork related to the study although participating in research is a central tenet of the NHS.
Patient and public involvement
The Peninsula Childhood Disability Research Unit (PenCRU) at UEMS involves families of children and young people with a disability in all their activities through a family faculty. We presented our idea of a research project on transition for young people with ADHD to a group of parents with children who had ADHD identified through PenCRU’s family faculty. We discussed the project proposal and explored further involvement by designing a patient and public involvement (PPI) plan. As a result, one parent with lived experience of ADHD in adults and young people was named as a co-applicant, which helped keep our focus on issues of importance to those in need of services during the study planning and communication with the parent advisory group. The proposed research was strongly endorsed by our parent advisors, who acknowledged that transition to adult services is a big challenge and a source of worry for them and their children. In response to parents’ concerns, interviews with young people who dropped out of services to understand why they chose not to continue mediation or treatment were added to the study design. Parents who were interested in the project became our parent advisory group (n = 21), which we consulted with throughout.
Over the years, our research group has developed good relationships with local secondary schools (including a special needs school), and pupils attending these schools demonstrated great interest in participating in new research projects. The project was introduced to year 9 students, who advised the team on how to conduct interviews with young people and helped design patient interview consent forms for the qualitative study. In addition, we were supported by Cerebra (Carmarthen, Wales), UK Adult ADHD Network (UKAAN) and Adult Attention Deficit Disorder-UK (AADD-UK), three third-sector organisations that work extensively with young people with ADHD and their families, or clinicians working with young adults with ADHD. These organisations supported communication throughout the project, notably sharing the map of services and helping to obtain feedback from patients with ADHD, which they now plan to host and update in perpetuity. PPI in this project contributed to the:
-
definition of case study for the surveillance strand
-
design of topic guides and information leaflets for the qualitative study
-
development of the recruitment strategy for the qualitative study
-
development of an online survey asking patients about service availability (mapping study)
-
analytical process, through preliminary discussions of the findings
-
dissemination of findings.
Chapter 3 Strand 1: the surveillance study
To plan services, commissioners and service providers need data about how many people may require that service. Although previous studies have reported on the proportion of young people still meeting diagnostic criteria in adulthood,29 few studies provide empirical data on the number of patients who wish to access ongoing care, or the number who successfully do so. Studies for common developmental disorders, such as ADHD, also rarely follow participants across developmental transitions. 55 Two previous studies have reviewed case notes to identify transition cases between CAMHS and AMHS for all children with all types of mental health conditions over a 12-month period. 53,56 The first study identified an average of 12 neurodevelopmental cases per CAMHS team who were eligible for transition in 1 year, of whom 40% were never referred to any adult service; in addition, only 67% of those referred actually made the transition. 39,53 This study was limited to health trusts in two geographical areas of England. The second study focused on ADHD cases in Ireland and identified 20 patients from four CAMHS teams who required transition. None of these patients were directly transitioned to AMHS; they were retained by CAMHS, referred to a private service or discharged to their GP. 56 The CATCh-uS surveillance study was the first national study that aimed to determine how many young people with ADHD, with an ongoing need for medication, need to transfer to an adult service, and to describe this population across the UK and Ireland.
Surveillance is the collection of reliable and timely information about health conditions in the population to improve health. 81 It is defined as the systematic ongoing collection of data, including analysis and interpretation, and, by its continuous nature, is more than just routine outcome monitoring. It is also separate from screening, because of the broader focus on factors that influence prevalence and management; screening, in contrast, is intended to detect individuals who need care. 82 Surveillance of a condition over time has the potential to provide national estimates of incidence and highlight needs or gaps in service provision that should be addressed at policy level to inform commissioning.
Monthly surveillance with reporting via questionnaires in paediatric services was developed in the 1980s to measure and monitor important infectious and rare diseases by the BPSU, which has been a prominent influence on child health policy and practice. 83 It studies the national incidence of rare conditions across the UK via monthly reports from consultant paediatricians. Much mental health surveillance has involved collection of data via morbidity surveys, such as the surveys of psychiatric morbidity,84 or enquiries, and data collection at mental health services, which still continues; however, since the 1990s, recognition of the impact of mental illness on the health of the population has led to more continuous surveillance being conducted. CAPSS was developed as a pilot in 2005 for a study of early onset eating disorders to maximise the identification of cases, and was fully established in 2009. 85 It applies the same methods as the BPSU, but obtains reports from consultant child and adolescent psychiatrists. The current study focused on surveying the incidence of a service need: the need for transition between child and adult services for young people with ADHD.
The objectives of the surveillance study were to:
-
estimate the range and mean age for transition to adult services and variation within this across the UK and Ireland for CAMHS and paediatric services
-
estimate the incidence rate of young people with ADHD requiring ongoing medication for ADHD after they pass the age boundary for the service that they attend, and variation within this across the UK and Ireland
-
describe the services offered to young people going through this age boundary
-
estimate the proportion of young people with ADHD judged in need of transition who successfully transfer to a specialist adult health service, defined as an accepted referral to a specialist adult service within the time frame of the current study.
Methods
This study used the BPSU and CAPSS to collect surveillance data on transition in health services that support young people with ADHD. As young people with ADHD (especially those who require medication) are most commonly seen by CAMHS or paediatric clinicians, the CAPSS and BPSU system offered access to the most appropriate clinicians and care pathways. This was one of only five studies to use the CAPSS and BPSU system simultaneously and was unique in that it focused on the incidence of transition as a process in ADHD as opposed to the incidence of ADHD as a condition. Additional work compared the relative strengths and weaknesses of surveillance and electronic case note review methods in quantifying the need for transition, which is summarised below and described in more detail in a separate paper. 86
Surveillance methodology design
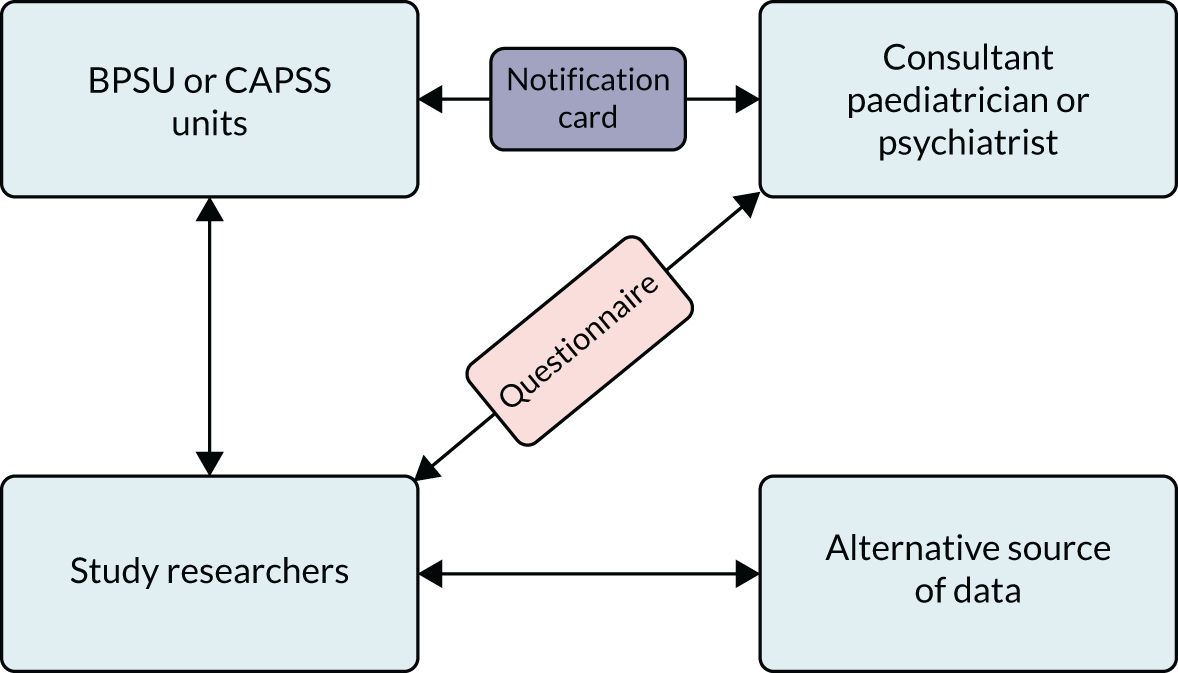
The BPSU and CAPSS methodology is well established and replicated in 14 countries; the study results influence management, planning and policy internationally. 87 Figure 3 illustrates how the system works. Over 3800 registered paediatricians from BPSU88 and 1000 psychiatrists from CAPSS89 are sent a surveillance orange/yellow ‘reporting card’ (now by e-mail) each month that lists the rare disorders or events currently under study. A limited number of research studies can be featured on the card at any one point in time, and the clinician returns the notification card indicating how many patients they have seen that meet the relevant study criteria. The research team then sends a questionnaire directly to the clinician. Usually BPSU and CAPSS studies run for 13 months; the first month is considered a pilot to identify any potential difficulties raised by clinicians, with the remaining 12 months’ data included as the full study.
FIGURE 3.
BPSU and CAPSS surveillance methodology. Reproduced with permission from Richard Lynn, British Paediatric Surveillance Unit, 2019, personal communication.
Governance and ethics
Both BPSU and CAPSS have a two-phase application process before granting approval to run a study. Phase I assesses the suitability of the research question to this type of surveillance methodology, whereas Phase II ensures that the surveillance definition and questionnaires cover only what clinicians would be expected to know or be able to access from clinical notes. Respondent burden is a prime consideration.
The approval granted by BPSU and CAPSS for this surveillance study was initially for 6 months with review thereafter. Both units were concerned that a large number of notifications would be received that would be beyond the capacity of each organisation and, thus, swamp the system. The plan was to review at 6 months and extend to 12 months, if warranted. At 6 months, 138 notification reports from BPSU and 118 from CAPSS had been received, which allayed the fears that both the clinicians and the surveillance organisations would be overburdened. The surveillance period was duly extended and, in total, ran from November 2015 to November 2016 with a 9-month follow-up post notification from August 2016 to August 2017. Responses were followed up for 3 months after the end of the surveillance and follow-up periods. Relevant ethics approval was sought and granted for this part of the study. Both BPSU and CAPSS have HRA approval for access to case note information without patient/parent consent, provided the study has CAG approval (Integrated Research Approval System registration number 159209, REC reference 15/YH/0426 and CAG reference 15/CAG/0184).
Case definition criteria
The surveillance unit asked consultants to report if they had seen any of the following in the previous month:
-
young people with a clinical diagnosis of ADHD under the care of CAMHS or paediatric services who were reviewed within 6 months of the service age boundary
-
young people considered to require continued drug treatment for their symptoms of ADHD after crossing the age boundary of the child service
-
young people with ADHD and comorbid diagnoses, including learning/developmental disabilities, but only if it was their ADHD that required ongoing drug treatment.
Young people were excluded if they:
-
had a diagnosis of ADHD but did not require medication or were unwilling to take it
-
required transition to an adult service only for a psychiatric comorbid condition
-
had already been notified to the study.
The definition was designed in close collaboration with members of both BPSU and CAPSS and had to be appropriate for both paediatricians and psychiatrists, to ensure that both sets of clinicians would identify young people to be reported in the study in as similar a manner as possible. The development of the definition required an iterative process of discussions and revisions. The final definition that was used unequivocally specified the need for ongoing support from specialist AMHS, as outlined in the NICE guidelines. 36 The aim of the definition was to provide a minimum estimate of the number of young people requiring a transfer from CAMHS and paediatric services to adult services during the surveillance period. Because not all children’s services extend to the age of 18 years, and some extend beyond this age, the age boundary was left unspecified to prevent the loss of cases in measuring when transition was occurring. The requirement for ongoing medication was chosen as a criterion to rule out subjectivity in the application of definitions of ‘ongoing care’. It would not capture those who did not need or want medication but did need ongoing psychological support.
Questionnaires
Baseline notification and follow-up questionnaires were developed using the corresponding systems templates, which comprised structured questions (30 at baseline and 19 at follow-up) with two open-text responses. All four surveillance study questionnaires are available (see Report Supplementary Materials 1–4). The baseline notification questionnaire was sent to all clinicians who reported a case to the study; questions confirmed eligibility and gathered semi-identifiable data on the patient (NHS number, gender, age in months and truncated postcode) to allow duplicate reports of patients seen by both general and specialist services, or by both CAMHS and paediatric services, to be identified. It also collected details of patient treatment and details of the planned transition to an adult service. Any professional with access to the patient notes could complete the baseline notification questionnaire on behalf of the lead clinician if necessary, although the reporting card was sent only to consultant paediatricians and child and adolescent psychiatrists.
Only cases confirmed as eligible in the baseline questionnaire were sent a follow-up questionnaire 9 months later. The follow-up questionnaire was sent to the same clinician who reported the case at baseline, with questions to confirm the outcome and details of the transition. There were nine elements of transition listed at follow-up and only five at baseline. This was to reflect what was stated in the NICE guidelines,33–36 and it was anticipated that at follow-up the transition would have occurred and clinicians would therefore be able to report on factors such as continuity and consistency that would not have been possible at baseline.
E-mail and postal reminders for non-returned questionnaires were sent after 4 weeks and again after 6 weeks, and finally a follow-up telephone call was made if the questionnaire was still outstanding. Clinicians were offered certificates to represent time committed to research to acknowledge their participation.
Data validation
Most BPSU studies choose to triangulate their data with other sources to help improve completeness and accuracy. 90 To check the reliability and validity of the data collected in this surveillance study, additional data were collected using clinical case notes from the Maudsley Biomedical Research Centre CRIS at SLaM. These additional data had several limitations. First, SLaM provides only CAMHS and not paediatric services; only the total numbers of cases and descriptive data captured by both systems could be compared because neither CRIS nor CAPSS allows individuals to be identified. Second, the geographical boundary of SLaM could not directly map with CAPSS data as researchers are blind to patient data and the information provided on each case related to the reporting consultant and not the service or clinic; therefore, the comparison with CAPSS reports could not get closer than the wider boundary of ‘London’. This method enabled a real-time data comparison and provided an indication of the completeness of the CAPSS reporting systems at collecting data on the incidence of rare events and processes in mental health services. We expected that CRIS would reveal fewer cases, as SLaM encompasses four London boroughs and the CAPSS data encompassed the whole of London.
The case definition criteria were the same as those applied to the surveillance study; criteria were operationalised into a structured query language, which was used to identify eligible cases in CRIS. Manual review of the electronic records by two researchers extracted the individual, clinical and service-related characteristics of the case, including details of transition (Table 1). The aim, given the previously mentioned limitations, was to replicate the data collected by the surveillance study.
| CRIS identifier | Reason for appointment | Other medication 3 |
| Gender | Current CAMHS or AMHS | Other medication 4 |
| Ethnicity | Seen by clinician | CGAS score (1–100) |
| Date of birth (specified) | Comorbidity 1 | SDQ assessment date |
| Truncated postcode | Comorbidity 2 | SDQ total score |
| Indices of social deprivation (LSOA) | Comorbidity 3 | SDQ hyperactivity score |
| Date of diagnosis of ADHD | Comorbidity other | SDQ impact score |
| CAMHS directorate | ADHD medication 1 | Contact frequency |
| Last date seen | ADHD medication 2 | DNA rate |
The CRIS was approved as an anonymised data resource for secondary analysis by Oxfordshire REC (08/H0606/71+5). This project was reviewed and approved by the CRIS patient-led oversight committee (CRIS project reference: 961).
Challenges from case definition and questionnaires: British Paediatric Surveillance Unit and Child and Adolescent Psychiatry Surveillance System responses combined
It became clear from queries to the researchers and the surveillance units during the pilot month that some consultants misunderstood the term ‘first time’ used in the original surveillance definition. They were unclear if this meant the first time they had ever met the patient or the first time the patient was reviewed in the surveillance period. This was resolved by changing the terminology to ‘the first time the case is reported’ (Table 2).
| Original | Final |
|---|---|
|
|
Other detected errors from clinicians included reporting a whole caseload of ADHD patients rather than reporting only the patients who required a transition (n = 2), duplicate reports of the same case if seen more than once (n = 13), reporting a case but not remembering the patient details (n = 31), reporting a case that did not meet one or more of the case definition criteria (n = 90) and ‘reporting in error’ (e.g. ticking the wrong box on the card, misreading the card, no recollection of reporting) (n = 43). Queries were resolved by direct contact with the reporting clinician.
Analysis of surveillance data
Response rates at each stage of the study are described, as are sociodemographic details of the reported cases by each reporting surveillance unit, and overall. The response rate was generated from the number of notification cards returned to BPSU or CAPSS divided by the total sent. Incidence is defined as the number of new health-related events, in a defined population, in a set period of time. 91 Using the data collected in this surveillance study, the incidence rate was calculated by determining the number of confirmed cases of transition in patients with ADHD identified over the course of the study’s 12-month surveillance period. The population at risk (n = 116,651) was derived by applying the estimated prevalence of ADHD (approximately 5% in the child and adolescent population)92 to the total number of young people aged 17–19 years in the UK, as reported in 2016 (n = 2,333,035). 93 Our incidence rates were calculated by dividing the estimate obtained from the surveillance of cases aged 17–19 years by the population at risk and multiplied by 100,000 to provide the incidence rate of transition per 100,000 young people.
Two incidence rates were calculated: the incidence of young people who were eligible for transition and the incidence rate of successful transition in the obtained sample. The incidence rate was adjusted to take into account the non-returned or missing data from the surveillance study (via monthly reporting cards and surveillance questionnaires). The following corrections were made:
-
Correction for unreturned BPSU/CAPSS notification cards. To account for incidence among unreturned cards, a correction to the observed incidence rate was applied, using two assumptions as suggested by Petkova et al. 94 in a previous study:
-
Assumption 1 considers that the incidence observed in the study applies to half of the unreturned cards, assuming no incidence of transition among the remaining half of unobserved cases. The rationale for the assumption is that a larger proportion of missing notification cards are negative (i.e. those reporting no cases that month) given that it is more likely that people will fail to submit a nil return than a positive return. This assumption translates to a correction coefficient derived from the calculation (half of unreturned cards + percentage returned cards)/percentage of returned cards.
-
Assumption 2 considers that the incidence observed in the study applies to all unreturned cards, assuming that all unreturned notification cards follow the same pattern of yes/no responses as those notification cards already received. This assumption translates to a correction coefficient (100/percentage unreturned cards).
-
-
Correction for unreturned baseline questionnaires. To account for incidence among the unreturned baseline questionnaires, a correction coefficient calculated from the return rate for baseline questionnaires (100/percentage returned baseline questionnaires) was applied. The two correction coefficients described above were combined in the following adjusted rates:
-
Adjusted incidence rate 1 –
-
= observed incidence rate × correction for unreturned notification cards (assumption 1) × correction for unreturned baseline questionnaires
-
this estimate applied the study observed incidence rate to half of all missing cases owing to unreturned notification cards and to all unobserved data owing to unreturned baseline questionnaires.
-
-
Adjusted incidence rate 2 –
-
= observed incidence rate × correction for unreturned notification cards (assumption 2) × correction for unreturned baseline questionnaires
-
this estimate applied the study observed incidence rate to all missing cases due to unreturned notification cards and to all unobserved data due to unreturned baseline questionnaires.
-
The observed incidence rate and adjusted incidence rate 2 will provide a likely minimum to maximum range within which the actual rate is likely to fall.
Results
The results below are further described in a separate paper. 95 The mean response rate to the monthly cards was 94% in BPSU and 53% in CAPSS. In total, there were 614 notifications reported by clinicians, all of whom were sent a baseline questionnaire. Table 3 illustrates the data responses for each stage of the surveillance study.
| Data obtained | BPSU (%) | CAPSS (%) | Combined (%) |
|---|---|---|---|
| Baseline | n = 314 | n = 300 | n = 614 |
| Not returned (error/reason) | 9 | 9 | 9 |
| Not returned (no reason) | 13 | 42 | 27 |
| Returned baseline questionnaire | 76 | 46 | 61 |
| Duplicate cases | 2 | 2 | 2 |
| Ineligible cases | 11 | 9 | 10 |
| Eligible cases | 64 | 38 | 51 |
| Follow-up | n = 202 | n = 113 | n = 315 |
| Returned questionnaire | 80 | 76 | 78 |
| Not returned (error/reason) | 6 | 7 | 6 |
| Not returned (no reason) | 14 | 17 | 15 |
These response rates take into account any contact with clinicians resulting in an explanation for not returning the questionnaire, which included not remembering the patient, reporting the case in error or the clinician realising that the case did not meet the definition criteria. Some contact details provided by both surveillance organisations were out of date (n = 26), which prevented the research team being able to provide the clinician with the questionnaire. Questionnaires were returned blank (n = 7) or with missing data (n = 86), and anecdotally some clinicians reported that they struggled to find the time to complete the questionnaires (n = 17). Of the reported cases who were defined as ineligible for the study, 35% (BPSU) and 19% (CAPSS) became ineligible as they no longer took medication.
There was no overlap in cases reported through BPSU and CAPSS. The 13 duplicate cases identified were from clinicians who reported the same case more than once in the surveillance period. There were 17 questionnaires that could not be completed at follow-up, as the clinician either no longer had access to the medical records or no longer worked at the service. Some questionnaires at baseline and follow-up were returned blank or not completed in full (n = 86). The sections most frequently left blank at baseline were one or more of the plans regarding transition and, at follow-up, one or more of the elements of optimal transition (see questions 7.2, 7.3 and 7.1 of the questionnaires; see Report Supplementary Material 1–4).
Characteristics of eligible young people reported
The population of young people reported via surveillance was largely male (80% of BPSU cases and 74% of CAPSS cases) and white British (91%), which would be expected from what is known about the epidemiology of ADHD in children and young people96 (Figure 4).
FIGURE 4.
Ethnicity of the population. (a) CAPSS; and (b) BPSU.
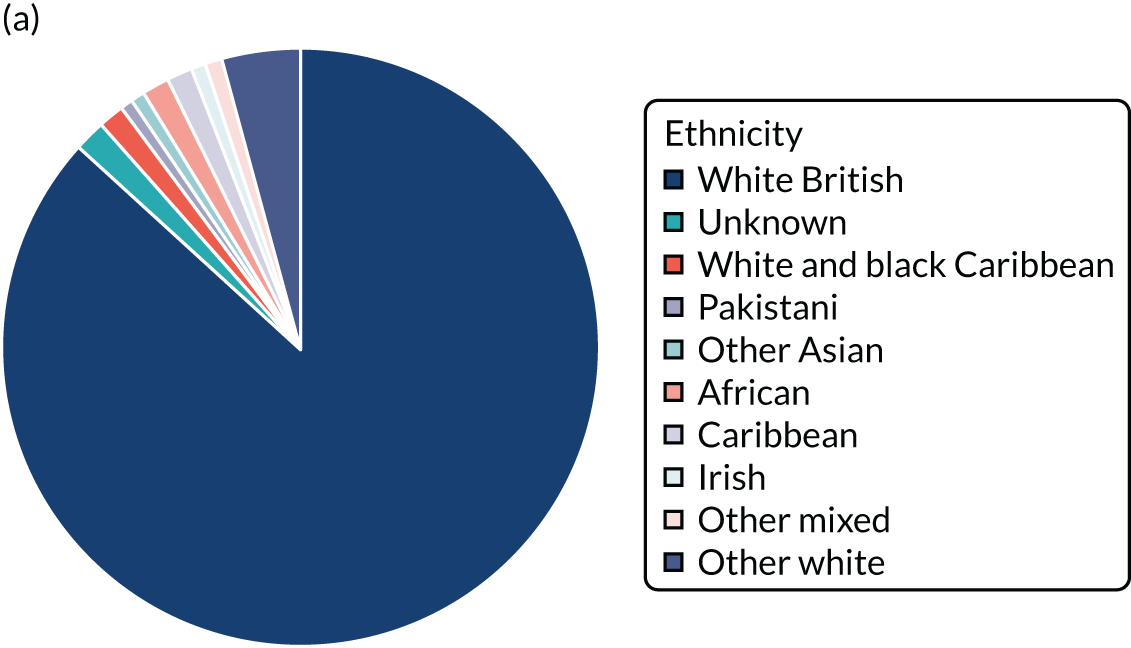

Cases were reported from across the UK, but, as would be expected, the majority (> 85%) were from England (Figure 5). All cases reported from Wales, Scotland or Ireland were identified as white British or white Irish.
FIGURE 5.
Geographical spread of cases in the UK. Owing to low numbers of reports, Northern Ireland and the Republic of Ireland cases are reported together.
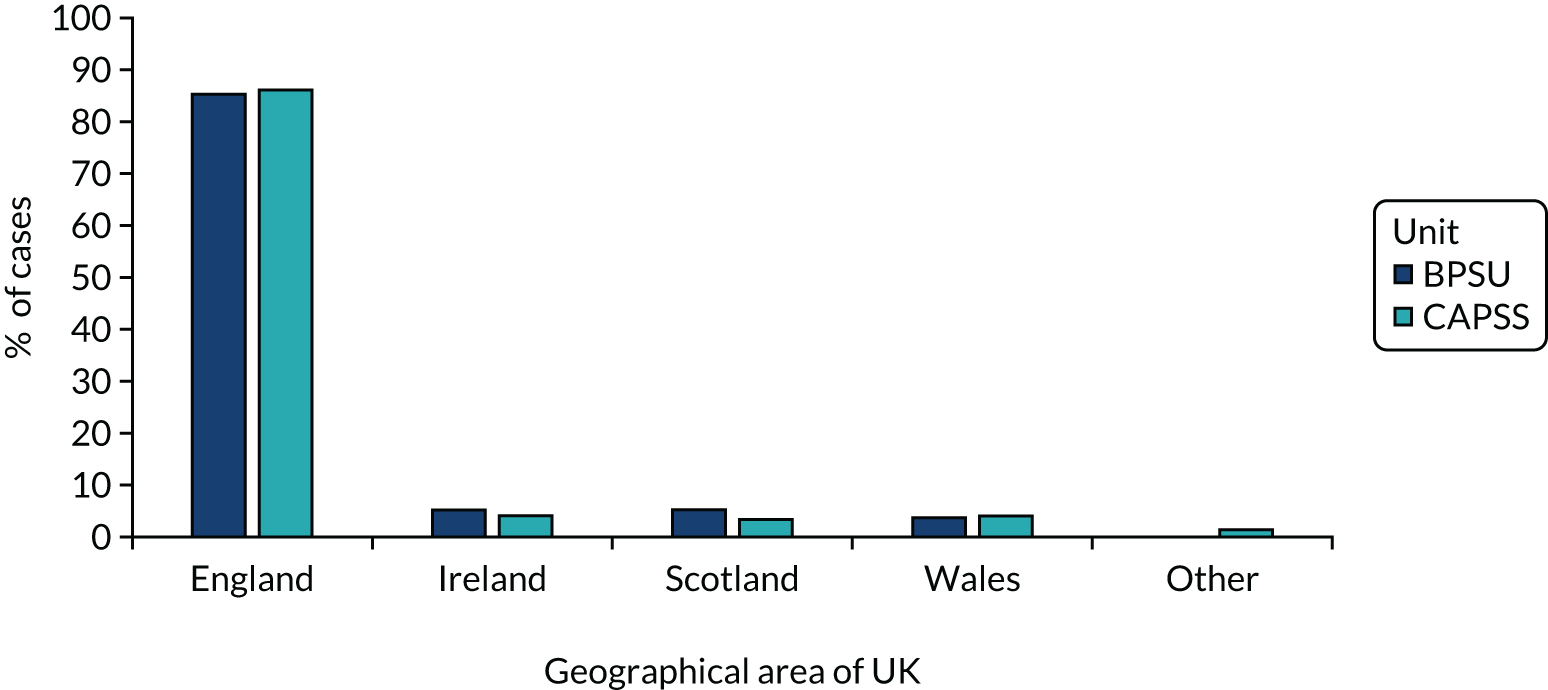
Table 4 shows the proportion of clinicians who reported the age boundary that their service works within, and Table 5 shows the range of the age boundary by country. Two cases originated from the USA, but were registered students who were seen in private practice in England. Over 80% of reported patients were aged 17 or 18 years at the point of referral for transition (mean age 17.4 years for BPSU, mean age 17.7 years for CAPSS), although the reported range extended from 14 to 20 years. A small percentage of clinicians (3%) stated that the age boundary for transition was variable. Paediatricians reported a more variable age boundary than child psychiatrists. Services in Wales, Scotland and Ireland appear to have more consistent age boundaries than services in England, perhaps as a result of the smaller administrative area covered.
| Age boundary | BPSU (%) | CAPSS (%) |
|---|---|---|
| 14 to 14 years 11 months | 0 | 1 |
| 15 to 15 years 11 months | 0.5 | 0 |
| 16 to 16 years 11 months | 12 | 0 |
| 17 to 17 years 11 months | 17 | 12 |
| 18 to 18 years 11 months | 63 | 83 |
| 19 to 19 years 11 months | 3 | 1 |
| Variable | 3 | 0 |
| Unknown | 2 | 3 |
| Country | BPSU | CAPSS | ||
|---|---|---|---|---|
| Service age boundary 18 years (%) | Age range (years) | Service age boundary 18 years (%) | Age range (years) | |
| England | 62 | 15–19 | 82 | 14–19 |
| Ireland | 75 | 17–18 | 100 | – |
| Wales | 75 | 16–18 | 67 | 17–18 |
| Scotland | 80 | 16–19 | 100 | – |
A large proportion of patients (56% of those reported by paediatricians, 68% of those reported by psychiatrists) had a comorbid condition, which in 25% of cases was ASC. Nearly one-quarter (23%) of patients reported by paediatricians and over one-third (41%) reported by psychiatrists were prescribed more than one medication.
Transition details reported
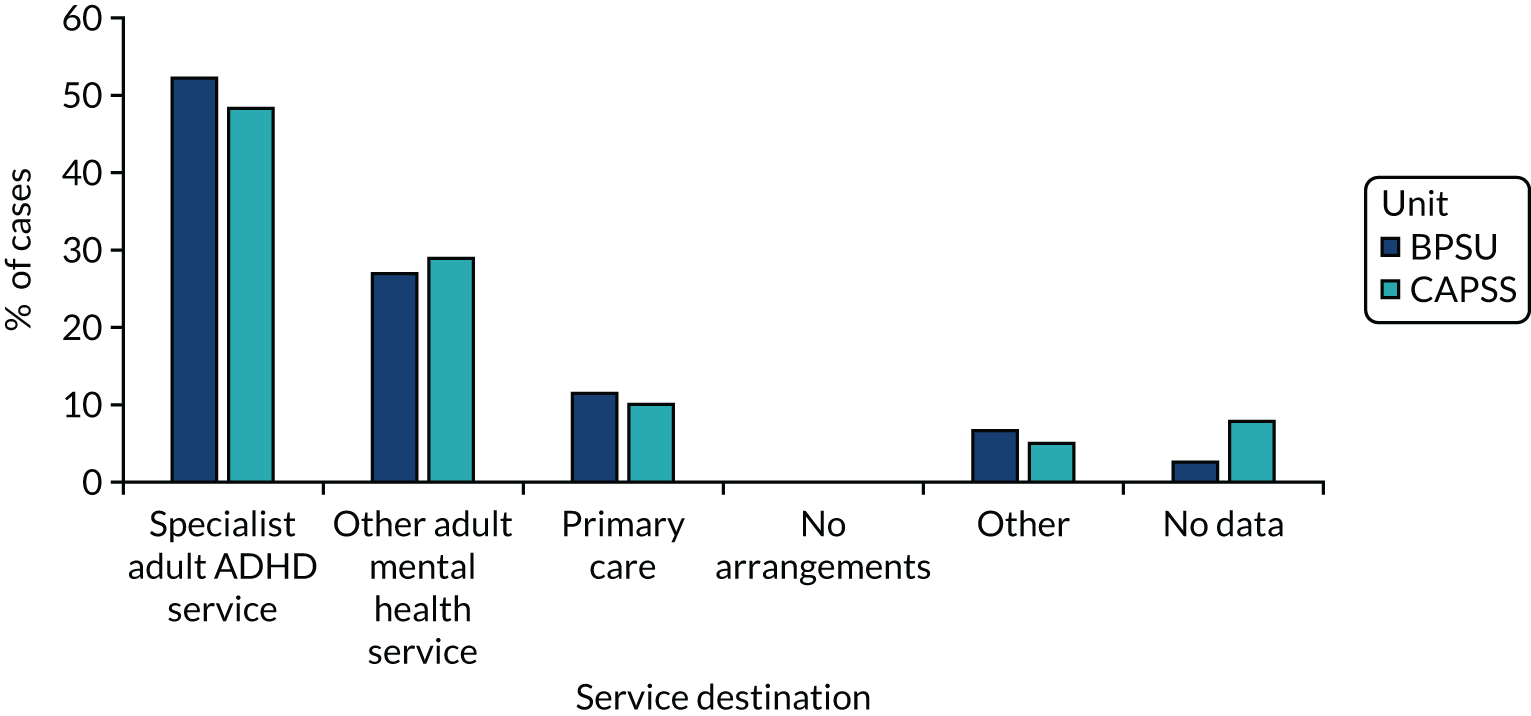
Figure 6 illustrates the range of services to which patients were referred half were referred to a specialist adult ADHD service, just over one-quarter were referred to general AMHS and 10% were referred to primary care. Referral destinations were similar regardless of whether the young person was reported by a paediatrician or a psychiatrist. In total, 64% of patients who were referred to an adult service were accepted (BPSU 52%, CAPSS 86%), but only 22% of those accepted were reported to have attended an appointment at AMHS (14% BPSU, 38% CAPSS). A number of clinicians provided extra free-text details about why transition failed, which included that the patient disengaged or did not want medication or referral, the patient did not meet service criteria, there was no funding available, and the adult service was closed to new referrals because of a lack of resources or long waiting lists.
FIGURE 6.
Transition referral destinations.
Nearly all clinicians reported that the patient had been involved in the planning of the transition process (93%), and > 80% reported that the parent or carer was also involved in the process. Access to and use of a transition protocol was reported more frequently by psychiatrists than paediatricians; psychiatrists reporting having access to a protocol in 81% of cases and using it in 66% of cases; the corresponding figures for paediatricians were 39% and 36%. There were nine elements of transition listed at follow-up, compared with five at baseline. At baseline notification, only 6% of paediatricians and 10% of psychiatrists indicated that all five listed criteria for optimal transition (as illustrated in Table 6) were apparent in the transition planning.
| Transition factor | BPSU (n = 202) | CAPSS (n = 113) | Combined (n = 315) | |||
|---|---|---|---|---|---|---|
| Total ‘Yes’ response | % | Total ‘Yes’ response | % | Total ‘Yes’ response | % | |
| Information sharing | 176 | 87.1 | 93 | 82.3 | 269 | 84.6 |
| Young person involvement | 162 | 80.2 | 97 | 85.8 | 259 | 81.4 |
| Planning meeting | 23 | 11.4 | 29 | 25.7 | 52 | 16.3 |
| Plan and agree care plan | 49 | 24.3 | 46 | 40.7 | 95 | 29.9 |
| Handover period | 56 | 27.7 | 25 | 22.1 | 81 | 25.5 |
At follow-up, only 2% of paediatricians and 6% of psychiatrists considered all nine criteria of optimal transition to have been adhered to (Table 7). At follow-up, some elements of optimal transition were reported to occur significantly less frequently than they were at baseline. This suggests that the element had not actually been adhered to, or that the clinician could not recall whether it had been in place. These included information sharing (84.6% at baseline vs. 68.8% at follow-up), young person involvement (81.4% vs. 69.6%) and joint working/handover (25.5% vs. 10.5%).
| Transition factor | BPSU (n = 161) | CAPSS (n = 86) | Combined (n = 247) | |||
|---|---|---|---|---|---|---|
| Total ‘Yes’ response | % | Total ‘Yes’ response | % | Total ‘Yes’ response | % | |
| User/carer involvement | 116 | 72 | 56 | 65.1 | 172 | 69.6 |
| Information sharing | 105 | 65.2 | 65 | 75.6 | 170 | 68.8 |
| Care plan agreed | 35 | 21.7 | 44 | 51.2 | 79 | 32.0 |
| Joint working before transfer | 12 | 7.5 | 14 | 16.3 | 26 | 10.5 |
| Alignment of assessment procedures | 9 | 5.6 | 12 | 14.1 | 21 | 8.5 |
| Continuity of care | 35 | 21.7 | 41 | 47.7 | 76 | 30.8 |
| Consistency of care | 13 | 8.1 | 36 | 41.9 | 49 | 19.8 |
| Consideration of appropriate service | 78 | 48.4 | 50 | 58.1 | 128 | 51.8 |
| Clarity of funding and eligibility | 66 | 41.1 | 51 | 59.3 | 117 | 47.4 |
Incidence of transition
A total of 315 reported patients were confirmed to be eligible for transition (202 BPSU, 113 CAPSS) during the surveillance period. A total of 55 transitions (22 BPSU, 33 CAPSS) were confirmed to be successful defined as a referral made, accepted and young person attended their first appointment in the adult service. The observed incidence rate and adjusted incidence rate 2 provide a likely minimum to maximum range within which the actual rate is likely to fall. Table 8 demonstrates the incidence calculations for all cases, and an adjusted version for those aged 17–19 years only [there were 46 eligible cases (32 BPSU, 14 CAPSS) who were not aged 17–19 years and, therefore, were not included in the adjusted incidence calculations].
| Description of incidence rate to be calculated | CAPSS | BPSU | Combined |
|---|---|---|---|
| Incidence: eligible for transition (all eligible patients identified in 12 months) per 100,000 per year | (113/116,651) × 100,000 = 96.9 | (202/116,651) × 100,000 = 173.2 | (315/116,651) × 100,000 = 270.0 |
| Incidence: successful transition (referral made, accepted and first appointment attended) per 100,000 per year | (33/116,651) × 100,000 = 28.3 | (22/116,651) × 100,000 = 18.9 | (55/116,651) × 100,000 = 47.1 |
| Observed incidence for people aged 17–19 years only | |||
| Incidence: eligible for transition aged 17–19 (all eligible patients aged 17–19 years identified in 12 months) per 100,000 per year | (99/116,651) × 100,000 = 84.9 | (170/116,651) × 100,000 = 145.7 | (269/116,651) × 100,000 = 230.6 |
| Incidence: successful transition aged 17–19 years (referral made, accepted and first appointment attended) per 100,000 per year | (31/116,651) × 100,000 = 26.6 | (20/116,651) × 100,000 = 17.1 | (51/116,651) × 100,000 = 43.7 |
| Correction for non-returned notification cards | |||
| Returned | 53.2% | 94.2% | 73.7% |
| No response | 46.8% | 5.8% | 26.3% |
| Assumption 1 (the same incidence applies to half non-returned) | (23.4 + 46.8)/53.2 = coefficient 1.32 | (2.9 + 5.8)/94.2 = coefficient 0.09 | (13.2 + 26.3)/73.7 = coefficient 0.54 |
| Assumption 2 (the same incidence applies to all non-returned) | 100/53.2 = coefficient 1.88 | 100/94.2 = coefficient 1.06 | 100/73.7 = 1.36 |
| Correction for non-returned baseline questionnaires | |||
| Returned | 139/300 = 46.3% 100/46.3 = coefficient 2.15 | 238/314 = 75.7% 100/75.7 = coefficient 1.32 | 377/614 = 61.4% 100/61.4 = coefficient 1.63 |
| Combined coefficients | |||
| Adjusted incidence rate 1 = incidence rate × correction for unreturned notification cards (assumption 1) × correction for unreturned baseline questionnaires |
Eligible for transition: 96.9 × 1.32 × 2.15 = 275.0 Successful transition: 28.3 × 1.32 × 2.15 = 80.3 |
Eligible for transition: 173.2 × 0.09 × 1.32 = 20.6 Successful transition: 18.9 × 0.09 × 1.32 = 2.2 |
Eligible for transition: 270.0 × 0.54 × 1.63 = 243.8 Successful transition: 47.1 × 0.54 × 1.63 = 41.5 |
| Adjusted incidence rate 2 = incidence rate × correction for unreturned notification cards (assumption 2) × correction for unreturned baseline questionnaires |
Eligible for transition: 96.9 × 1.88 × 2.15 = 391.7 Successful transition: 28.3 × 1.88 × 2.15 = 114.4 |
Eligible for transition: 173.2 × 1.06 × 1.32 = 242.3 Successful transition: 18.9 × 1.06 × 1.32 = 21.3 |
Eligible for transition: 270.0 × 1.36 × 1.63 = 598.5 Successful transition: 47.1 × 1.36 × 1.63 = 104.4 |
| Combined coefficients for people aged 17–19 years only | |||
| Adjusted incidence rate 1 = incidence rate × correction for unreturned notification cards (assumption 1) × correction for unreturned baseline questionnaires |
Eligible for transition: 84.9 × 1.32 × 2.15 = 240.9 Successful transition: 26.6 × 1.32 × 2.15 = 75.5 |
Eligible for transition: 145.7 × 0.09 × 1.32 = 17.3 Successful transition: 17.1 × 0.09 × 1.32 = 2.0 |
Eligible for transition: 230.6 × 0.54 × 1.63 = 202.9 Successful transition: 43.7 × 0.54 × 1.63 = 38.5 |
| Adjusted incidence rate 2 = incidence rate × correction for unreturned notification cards (assumption 2) × correction for unreturned baseline questionnaires |
Eligible for transition: 84.9 × 1.88 × 2.15 = 343.2 Successful transition: 26.6 × 1.88 × 2.15 = 107.5 |
Eligible for transition: 145.7 × 1.06 × 1.32 = 203.9 Successful transition: 17.1 × 1.06 × 1.32 = 23.9 |
Eligible for transition: 230.6 × 1.36 × 1.63 = 511.2 Successful transition: 43.7 × 1.36 × 1.63 = 96.9 |
Data validation results
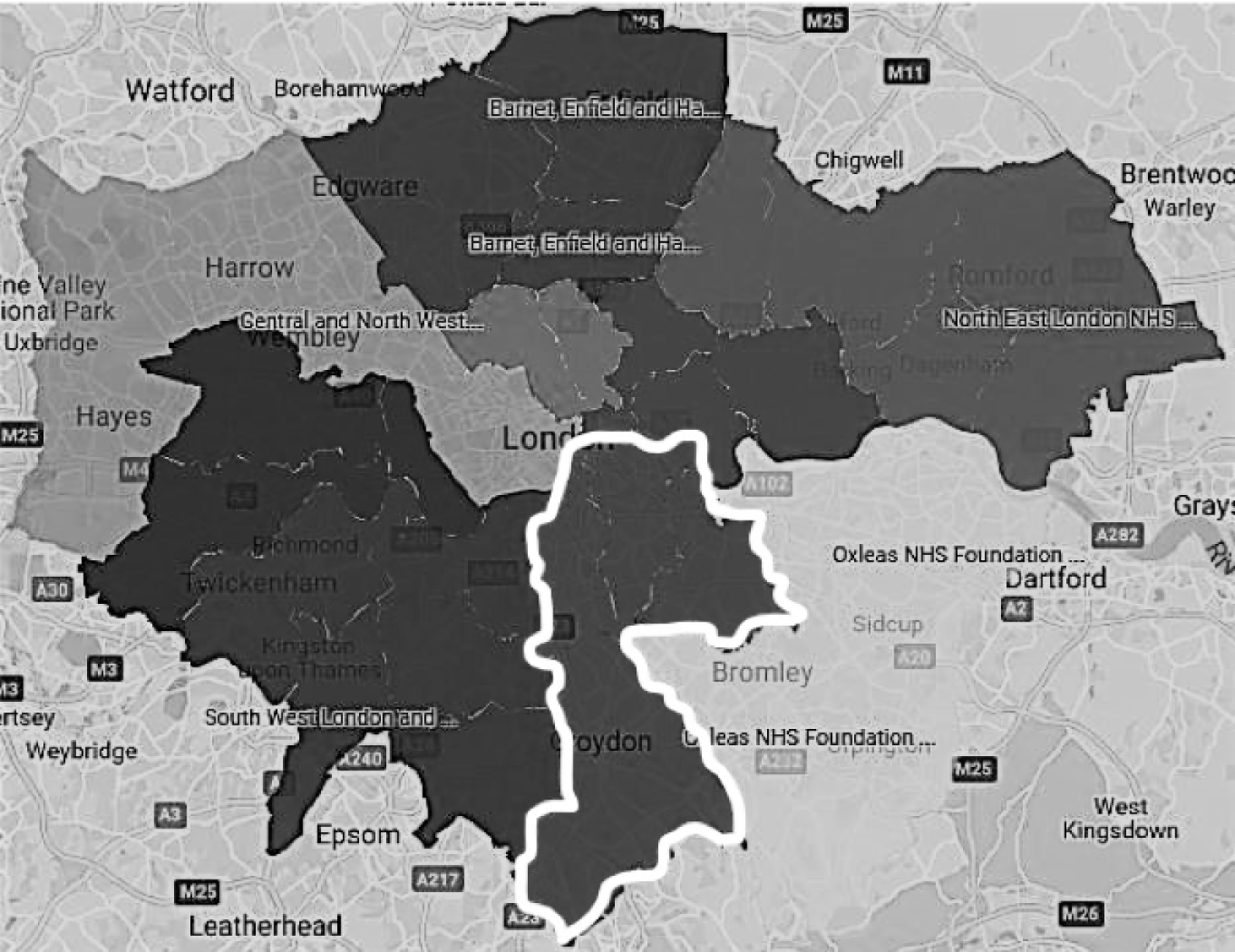
In total, 91 people with a clinical diagnosis of ADHD who were within 6 months of the service age boundary and, therefore, potentially eligible for transition were identified in the search of SLaM case notes. However, 15 people were discharged prior to transition or were no longer taking medication or requiring treatment, leaving 76 people eligible for transition according to our definition. The London CAPSS identified 45 notified cases, 18 of which were confirmed eligible cases. However SLaM, and thus CRIS, is only one of nine mental health trusts in London, which covers 7 out of 32 London boroughs. 97 CAPSS encompasses all of the London boroughs in this example. Figure 7 demonstrates the SLaM boundary in the rest of London. Table 9 shows a comparison between the CAPSS and CRIS data.
FIGURE 7.
London Mental Health NHS Trust boundaries (SLaM highlighted). Reproduced with permission from https://myhealth.london.nhs.uk98
The ratio of male to female was similar in both sets of data (83%: 17% surveillance; 84%: 16% CRIS); however, ethnic diversity was much greater in the CRIS sample (46% white British compared with 72% white British in CAPSS), which more closely reflects the ethnicity seen in the London boroughs served by SLaM. 99 Approximately half (54%) of the 76 eligible CRIS cases were seen by a consultant psychiatrist, which probably explains much of the disparity in reports of transition cases. The remaining young people were seen by a range of clinicians that included specialist ADHD nurses, junior doctors or clinical psychology trainees. Evidence in the case notes of a completed transition (referral made, accepted and first appointment attended in AMHS) could be found for only 37% (28) of cases in CRIS compared with 22% (4) of cases in CAPSS.
| Factor | CAPSS | CRIS |
|---|---|---|
| Notifications/identified cases (n) | 45 | 91 |
| Did not meet eligibility criteria (n) | 27 | 15 |
| Met all eligibility criteria (n) | 18 | 76 |
| Eligible cases only | ||
| Gender ratio (male % : female %) | 83 : 17 | 84 : 16 |
| Ethnicity (% white British) | 72 | 46 |
| Reported/reviewed by consultant (n) | 18 | 41 |
| Reported/reviewed by other health professional (n) | 0 | 35 |
| Transition referral made, accepted and first appointment offered in adult service (n) | 10 | 37 |
| First appointment confirmed attended (n) | 4 | 28 |
In total, 76 patients reported by CRIS were potentially eligible for transition, 28 of whom were confirmed to have been referred, accepted and attended the first appointment in the adult service. When compared with CAPSS (see Table 9), this validation exercise suggests that the surveillance study figures are likely to have been significantly under-reported; four times as many more eligible cases and seven times more successful transitions were identified via CRIS than CAPSS in the London area.
The same method of calculating incidence rate as used for the surveillance study data was applied to the CRIS data. The population at risk was calculated from the total number of young people aged 17–19 years in the area served by SLaM, as reported in 2016 (n = 40,382). 93 The same ADHD prevalence estimate of 5%29 was applied, resulting in a population at risk of 2019 young people. This results in an incidence rate for eligibility for transition of 3764.3 per 100,000 young people with ADHD; approximately one-third [36% or 1386.8 per 100,000; (28/2019) × 100,000] of transitions were successful. In contrast, the ratio of successful to eligible transitions from the surveillance data was only 17%.
Discussion
Our data suggest that the minimum annual need for young adults with ADHD to transition to adult services for ongoing medication would lie between 270.0 and 598.5 per 100,000 people aged 17–19 years. This amounts to 96.9–391.7 per 100,000 people aged 17–19 years among CAMHS attenders and 173.2–242.3 per 100,000 people aged 17–19 years from paediatric services. These data provide the current best estimate into early adulthood for commissioners and service providers to consider. It is important to note that even the upper estimate is likely to significantly underestimate the level of need according to our triangulation with the CRIS data, which suggested that the upper limit could be as many as 3764.3 per 100,000 young people. As a centre of excellence, SLaM have much more highly developed national and local ADHD services for both children and adults than most areas. We, therefore, consider the surveillance data to provide more reliable national estimates of current service-driven levels of need, but suspect that many more children and adults may remain undetected in the wider community. Moreover, these figures relate only to those who require and are willing to take medication for their ADHD, and thus excludes those who do not want or cannot tolerate medication but require ongoing care.
This study was the first to use rare disease and event surveillance methodology to address a process. ADHD is a common reason for attendance at community paediatric services and CAMHS;100 however, unfortunately, as our data confirm, successful transition to AMHS is uncommon. The study was, to our knowledge, also the first time additional data had been used to validate and compare the data collected using CAPSS, and suggests that, in relation to transition for ADHD at least, the involvement of non-consultant practitioners illustrated from the CRIS database in particular leads to significant under-reporting. The emphasis on complete ascertainment of cases in the study of rare outcomes supports the inclusion of the two overseas residents in our calculations. In small samples, missing individuals make a disproportionate impact on estimates, and given our concerns about case ascertainment we opted to include them as they represent the workload on mental health professionals dealing with ADHD in this age group.
The estimated annual incidence of successful transition is considerably lower than the estimated need. The higher proportion of successful transitions seen in the CRIS data may relate to the availability of ADHD services in SLaM, which include national and specialist teams for both children and adults with ADHD, but it is still notably low. A study in one locality found that only 15% of patients eligible for transition actually successfully transferred to the adult service. 101 These data suggest that less than one-fifth of those requiring transition for ongoing medication successfully make the transfer. Given that medication predicted transition in the TRACK study,72 it seems likely that transition is even less successful for young adults with ADHD needing psychosocial treatments alone.
The gender ratio and ethnic origin of the cases identified in both the surveillance study and the CRIS study were in line with published national averages for the UK and England; the 2011 census confirmed London as 45% and the UK as a whole as 79% white British,102 and previous research has shown the gender ratio for patients with ADHD to be between 3 : 1 in epidemiological studies and 9 : 1 in clinical samples. 103,104 This suggests that both methods yielded a sample that is representative of those with ADHD attending services. There is an underidentification and under diagnosis of girls with ADHD worldwide,105 and previous research has shown that children of black and minority ethnicity are less likely to be diagnosed with ADHD than white children. 106,107 There is a lack of epidemiological data to study transition in this age group and we, likewise, lacked power to explore transition in these subgroups. A recent report reviewing children and young people’s mental health care highlighted a lack of data availability and monitoring of transition. 108 Moreover, such reviews consider only young people up to the age of 18 years; therefore, knowledge of young adults is particularly poor.
Our findings suggest poor adherence to the recommendations for transition from NICE. NICE recommends that a smooth transition between child and adult services should be complete by age 18 years, and should involve a detailed care plan and a formal joint meeting between the child and the adult service, use the care programme approach and involve the young person and the parent or carer. 36 In contrast, we found that a joint planning meeting, a care plan and a joint handover period are conducted in < 30% of cases. Other studies have also highlighted the lack of planning for transition of young people with ADHD. 53,56,109,110 Although the reported high level of involvement of the young person and carer in the process is commendable, paediatricians, in particular, reported poor continuity and consistency of care, which may reflect poorer links between community paediatric services and AMHS than with CAMHS. A lack of planning is likely to undermine the potential for successful transition, and existing research has highlighted the need to adhere to recommendations to ensure effective transition. 67 It is further recommended that policies and guidelines are reviewed regularly so that they can be operationalised and effectively translated in to clinical practice. 49
Although the surveillance study allowed us to gather data across the UK and Ireland, it required a clearly defined definition that was easily operationalised for clinicians to report cases. The need for medication and the shared care recommended for the management of medication in the NICE guidance36 means that our definition provides a concrete, if restrictive, indication of access to adult ADHD services. The use of the BPSU and CAPSS systems presented a number of other methodological challenges that will have affected initial notifications and subsequent return of questionnaires. Registration to receive the monthly reporting cards is voluntary and restricted to those on the consultant grade; therefore, not all relevant clinicians may receive them. The comparison with CRIS data highlighted that surveillance can provide meaningful data only if consultants are sufficiently involved in the condition under study, which is more likely to be the case for severe, complex and rare conditions. Some specialist ADHD services, in discussion with the researchers, arranged for non-medical and non-consultant grades to assist with the reporting, but notification had to remain via the card system. Adults with ADHD may be reviewed in settings other than paediatric services and CAMHS, such as social care, education, primary care or forensic services. 111 However, the prescribing of medication will only be overseen only by a medical doctor or nurse prescriber within specialist services and, therefore, reviews of patients in non-health settings would not represent a gap in reporting. Health professionals in primary care and forensic settings should have access to specialist advice according to the NICE guidance, but our results suggest that other recommendations in relation to transition for ADHD are not being implemented, which would add another source of under-reporting to our estimates. A study of surveillance approaches has highlighted the relative absence of surveillance in the private sector despite its role in health-care provision,112 perhaps particularly for young people with ADHD, for whom there are extensive gaps in the provision of NHS services. 113
Incomplete data also presented a limitation, as non-response was experienced at each stage. Reporting with no obligation potentially prevents reporting consistency112 so, to encourage reporting and questionnaire response, the research team offered ‘participation in research’ certificates that could be used for appraisal. This incentive was generally well received. Research is enshrined in the NHS constitution as a core activity;114 however, clinicians complained that current workloads made it difficult or impossible to respond to questionnaires, despite efforts from the research team to keep the questionnaires as brief as possible (30 structured items at baseline and 19 at follow-up). Attrition through missing data can introduce bias115 and is one of the reasons that the surveillance units encourage triangulation to assess the completeness of case ascertaintment. 116 We adjusted for non-response when calculating incidence, but our calculations are inevitably based on assumptions that may be incorrect. Incomplete case ascertainment will risk our underestimating the incidence of young people requiring transition. According to a census conducted by the Royal College of Paediatrics and Child Health in 2013, there were 3718 registered consultant paediatricians whereas BPSU reports 3300 on the database, and a 2017 census by the Royal College of Psychiatrists reported there to be 5395 consultant psychiatrists (approximately one-quarter of whom are child psychiatrists), whereas CAPSS have around 1000 on the database. 117,118 Although the return rate of reporting cards by paediatricians via BPSU was excellent (perhaps as a result of the longevity of the system), the average return rate of the reporting cards was lower in CAPSS. As CAPSS started only 8 years ago, it perhaps has yet to become normal practice for child and adolescent psychiatrists.
Data validation with the CRIS database to assess the completeness of case ascertainment was a strength of this study, as it was important to attempt to quantify potential undercounting119 and verify findings. Governance systems prevented direct linkage between CAPSS and CRIS, which would have allowed more direct inference of the accuracy of CAPSS to be drawn. Interestingly, data protection rules may be more stringent than the attitudes of many patients and the public; a previous study has highlighted the benefits of linking data to provide information that is missing and reduce bias,120 and a study of attitudes towards linking concluded that it was perceived to be acceptable to share health data in a medical context. 121 In addition, the geographic location of SLaM clinics and hospitals could not be directly replicated in the surveillance data, as the address provided from the surveillance notifications was that of the clinician, which did not necessarily correspond to where the patient was seen. The broader term of ‘London’ was used, which gathered cases from a wider boundary than is included in SLaM. Although adjustments have been attempted, we acknowledge that all the adjustments are based on assumptions that will not be completely accurate.
Both methods of quantifying the incidence rate for transition have their strengths and their weaknesses. The data collected using BPSU and CAPSS surveillance were prespecified according to the research questions. These questions were not simple variables that would be easily extracted from CRIS, and answering them required a researcher to read and interpret data extracted from medical records. Although both methods require some interpretation, validity is likely to be higher when reported directly by the clinician who is working with the young person in a questionnaire tailored to specific questions than when a researcher is making assumptions from medical records that vary in their level of completeness and detail. The surveillance method has the advantage of gathering what the clinician remembers and knows, as well as what is recorded in the notes. It also covers the whole of the UK and Ireland rather than the usual constellation of services in a metropolitan region served by a centre of excellence. However, surveillance methodology is limited by the accuracy of the database of consultants, the exclusion of non-medical and non-consultant grades in reporting, and by response rate as a result of clinicians’ workloads. CRIS allowed us to estimate the extent to which the national surveillance underestimates incidence, but it offered poorer, less clear and less tailored information about the details of transition. Both the surveillance and the CRIS studies had stringent governance and required considerable researcher time for data collection and analysis, but used in combination, as opposed to in isolation, it offers a more complete and accurate picture of the need and success of transition to adult service among young people with ADHD.
Conclusion
National surveillance was combined with data extraction from CRIS to estimate the national incidence of young adults requiring ongoing medication for their ADHD, as well as those who successfully transitioned. The restriction of eligibility to those requiring and being willing to take medication, plus difficulties in case ascertainment, mean that the estimates provided represent the lower limit of the need for transition to AMHS for young people with ADHD. Attempts have been made to correct the data to account for incomplete ascertainment and provide a series of transparent estimates for policy, commissioning and service provision. Although certainly imperfect, these data are the best currently available. These findings also emphasise a relative lack of adherence to recommended guidelines for transition, and the low proportion of eligible patients who experience successful transition and continuity of care.
Chapter 4 Strand 2: the mapping study
Service provision for adults with ADHD remains relatively scarce and difficult to access in the UK because service configuration and workforce development is lagging behind recent medical recognition that ADHD is a long-term condition that typically persists beyond adolescence into adult life. 71,122,123 Previous studies revealed patchy transitional care provision124 and identified reasons for poor or failed transition, such as a lack of clarity on service availability and the operation of different eligibility criteria between child and AMHS, with variable service provision for young people with ADHD. 125 In many areas, this is compounded by a lack of services for onward referral, and limited information about what is available. 126 Previous research either is restricted to a certain region of England or explores specific aspects of provision, rather than systematically mapping available services for those with ADHD in AMHS. 68,75,127–129 Hall et al. 127 concluded their work by stating that ‘the next step is to map the provision of ADHD services nationally’. 127
The UK NICE guidelines state that the following services should be available for adults with ADHD: transitional care, assessment and diagnostic services, drug titration, monitoring and review, and psychoeducation. 33,36 Treatment should be holistic, addressing psychological, behavioural, occupational and educational needs, and services should be provided by multidisciplinary teams with expertise in ADHD. 36 Medication should be offered as the first line of treatment after environmental modifications have been implemented and reviewed. After titration and dose stabilisation, care may be carried out under shared care protocol arrangements with primary care;36 however, controversy remains over organisation of services for managing ADHD in adults,130 with wide variation in treatment approaches across the UK. In addition, research indicates that, partly because of existing gaps in services, adults with ADHD may either cease to access treatment or seek help at an extended range of services, including those not commissioned to treat adult ADHD. 131 Even after the NICE guidance in 2008 stressed the need for adults who required medication to be able to access it, there remained a much more rapid decline in prescriptions for ADHD medication than the epidemiology would lead us to anticipate. 132 As nearly 8% resumed their prescriptions of ADHD medication after the age of 20 years, this suggests that some young people are stopping treatment prematurely. 133
To date, studies that have mapped services for adults with ADHD have tended to draw on the perspectives of one stakeholder group, such as senior service managers75 or practitioners. 127 A recent systematic review of qualitative research about transition into adult ADHD services found that a lack of available information about adult ADHD services created difficulties in accessing treatment. 58 Patients are unsure where to access treatment,70 and some clinicians reported difficulties in finding an adult service to which they could refer their patients. 131 This implies that, even if commissioners hold knowledge about an appropriate service, patients and practitioners may not. The inclusion of a range of stakeholders minimises the risk of incomplete knowledge and may reveal previously hidden discrepancies in awareness.
As discussed in Chapter 1, health service provision in the UK is highly complex and there is no clear definition of the ‘unit’ of ‘service’, which can lead to variation in respondent-defined adult ADHD clinical care provision ‘services’.
The mapping study reported in this chapter aimed to identify service provision for adults with ADHD across the UK. By surveying multiple stakeholders, the study aimed to include services relevant to all groups and to analyse differences in the perspectives of commissioners, health workers and patients on service availability. This study was designed to provide national-level data on existing services that could be used to identify gaps in provision and knowledge as well as to optimise transition and service provision for this vulnerable group.
This mapping stream aimed to provide:
-
a geographical overview of services for young adults with ADHD
-
details of support/treatment provided (transition, diagnosis, medication or psychological) by dedicated NHS adult ADHD services
-
an exploration of the awareness of services by different stakeholder groups (commissioners, health workers and patients).
Methods
The mapping methodology was piloted and refined in 2016. A copy of the pilot survey is available (see Report Supplementary Material 5). An iterative process of trial and review led to the development of the protocol used in the definitive study, which ran between 8 and 11 February 2018. An overview of the methodology is presented below, while a more detailed description of the development process and a detailed description of the different steps is published elsewhere. 134
We collected information on UK services for adults with ADHD from the following essential stakeholders in the transition process:
-
those receiving treatment/support (patients)
-
those providing services (clinicians, health-care practitioners)
-
those funding services (commissioners).
This wide range of stakeholders from across the UK were approached to gather local knowledge and ensure that as many relevant services were identified as possible. To collect information on service provision from these different sources, we used several different techniques to optimise data capture:
-
Online survey – an online survey distributed using different techniques to a wide range of stakeholders.
-
Freedom of information (FOI) requests – (based on the same survey questions) sent to UK health service commissioners.
-
Surveillance study – information on services was extracted from questionnaires completed by consultant psychiatrists and paediatricians. 95
We particularly targeted child and adolescent psychiatrists, adult psychiatrists, paediatricians, GPs, nurses, practice managers and administrators, as well as young adults and their parents/carers. Commissioning bodies within the NHS were identified as they hold a key role in service provision. They differ slightly across the UK, with CCGs in England, health boards in Scotland and Wales, and health and social care trusts in Northern Ireland. The resulting service list was cross-checked against services described in the CATCh-uS qualitative study interviews with young adults and parents. 135 Services not already included on the list were added, with the interviewee listed as the informant.
Definition of services
In the light of the complex nature of the provision being mapped, we asked stakeholders to respond to an inclusive service definition of ‘any mental health service for people with ADHD aged 18 years and above’. The categorisation of responses is described in Data analysis.
The online survey
The survey was designed using SurveyMonkey® (Palo Alto, CA, USA) and in collaboration with the Parent Advisory Group and local clinicians. We used lay terms accessible to all informants and limited the length of the survey to include between five and nine questions (see Report Supplementary Material 6). The same version was used for all respondents. Basic demographic information was collected, including region (from a predefined list) and postcode. Respondents were provided with a checklist of services identified in a 2016 pilot survey and given the opportunity to indicate which of these services they knew, and were asked to provide details of any other services that were not already listed. After identifying a service, informants were asked to indicate if they, or anyone they knew, had experience of using that service for treatment/support of adult ADHD.
Respondents were also asked to indicate their primary role, with the opportunity to identify up to seven non-primary roles; for example, ‘Parent of child with ADHD’ as their primary role, but also a ‘Psychiatrist’ or an ‘Adult with ADHD’. The categories applied and their definitions are available in Report Supplementary Material 7.
Freedom of information
All commissioning bodies within the NHS were sent FOI requests, which give individuals the right to access recorded information held by public sector organisations. 136 The survey was sent via FOI e-mail addresses that were published online. In total, 209 English CCGs, 21 health boards (14 in Scotland, seven in Wales) and seven Northern Ireland health and social care trusts were contacted. These FOI requests asked the same five core questions as the online survey (e.g. template e-mail sent; see Report Supplementary Material 8). In addition, details were requested about the service type (adult, specialist, child and adolescent mental health or other) and interventions available (transitional care, medication, shared care, psychological, diagnosis or other). Respondents were automatically identified as commissioners and were not given the opportunity to indicate additional roles.
Surveillance study
Responses to two questions about service provision were included in mapping data analysis. The first question, included in the baseline questionnaire, asked for the young person’s intended destination (specialist adult ADHD, other AMHS, primary care or other), with identifying details, such as service name. The second, at follow-up 9 months later, asked for confirmation of the service to which the young person had been referred.
Qualitative study
Identified services were checked against services described in the CATCh-uS study qualitative interviews with patients and parents. Any other services mentioned in these interviews were added to the list of services, with the interviewee listed as the informant.
Online survey data collection
Survey links were distributed to potential informants via multiple methods, with the aim of maximising the responses:
-
direct e-mails via the mailing lists of AADD-UK, ADHD Foundation and the Royal College of Psychiatrists (Faculty of Child and Adolescent Psychiatry as well as the Faculty of General Adult Psychiatry) (see Report Supplementary Material 9).
-
e-mails via all regional Clinical Research Networks, with a request to target nurses, GPs, managers and clinical psychologists, as these groups had not been targeted via their professional organisation mailing lists
-
Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) – sharing the survey link via accounts of the various team members, tagging appropriate organisations
-
publication of the link and an explanation in the British Association of Community Child Health, the Royal College of General Practitioners and the George Still Forum.
In addition, awareness of the research was raised through university press releases, organisational newsletters, conference presentations and social media. The survey was open for 34 days from 8 January 2018. An interim analysis of responses was conducted to identify under-represented locations or informant groups. Subsequently, ADHD and clinical organisations in those locations and working with those groups were targeted, with the aim of improving the balance of responses.
Data handling
Data were uploaded to Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and analysed using Stata® SE15 (StataCorp LP, College Station, TX, USA). Response data were validated against online information, using free-text responses as key search terms and searching for details of the named services online to create a list of identified and verified services. This process allowed researchers to index all identified services and link services with the relevant organisational provider.
Services were categorised into four groups according to how ADHD specific the provision was (Figure 8). As online information was often quite dated or did not specify whether or not adult ADHD could be treated at that service, FOI requests were sent to check service provision of the dedicated ADHD services (see Report Supplementary Material 10). This generated a nested model of service specificity, with four layers of service provision for adults with ADHD in which layers also relate to the degree of certainty about the data. Layer 1 included the greatest degree of certainty as well as specificity.
FIGURE 8.
Stacked Venn diagram showing layers of service identification, decreasing in specificity of service type and reliability of information.
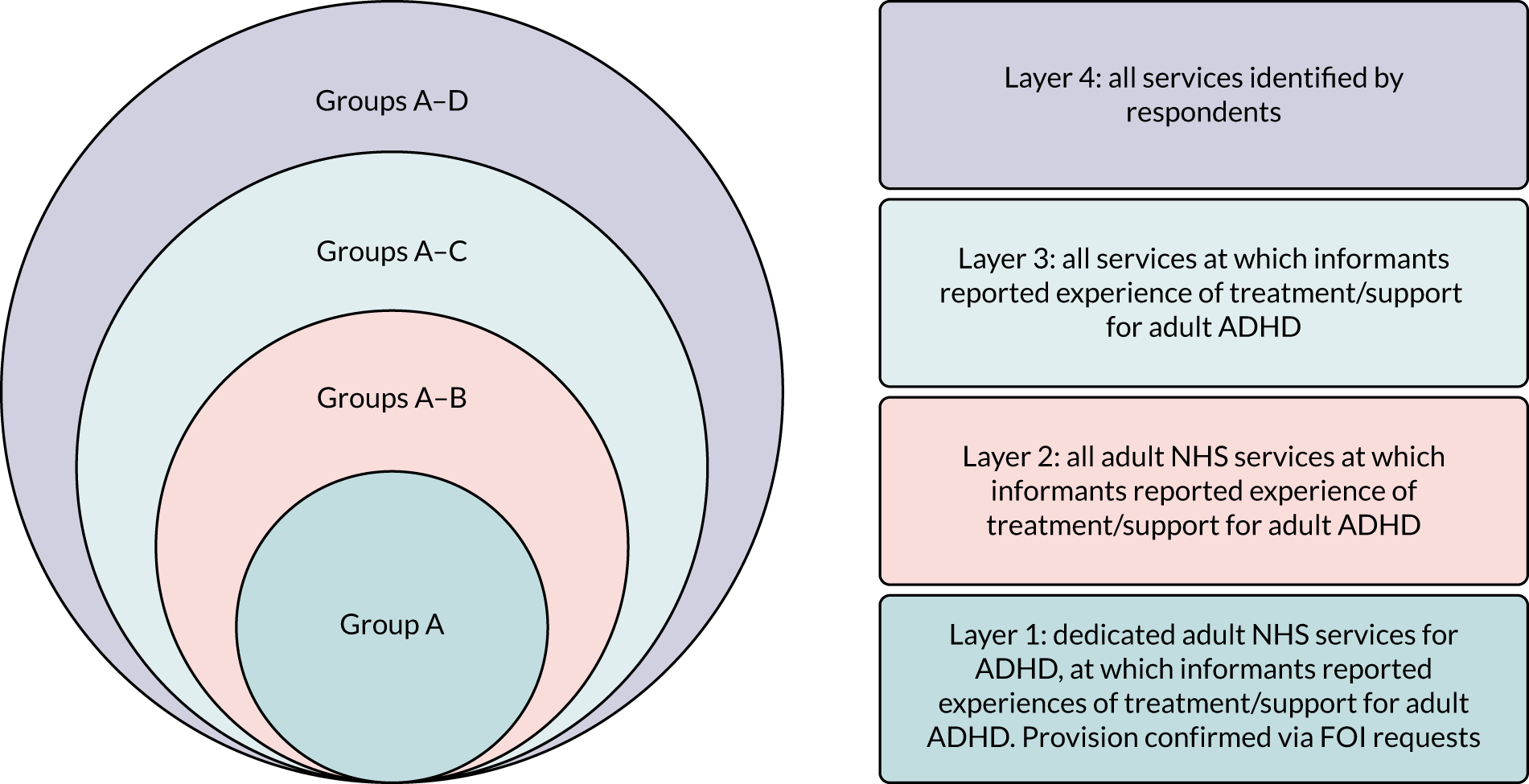
Service groupings
Services are organised in four nested layers of service (1–4), comprising differing combinations of four discrete groups of services (groups A–D) as described below and illustrated in Figure 8:
-
Layer 1 (group A) was made up of services that dedicated provision for adult ADHD within NHS services, verified by FOI request.
-
Layer 2 (groups A and B) was made up of all other NHS services for adults experienced by respondents as providing treatment/support. Group B comprised generic NHS services for adults. Learning disability services were also categorised as group B; however, as a result of the large number identified, providers of these services were also contacted to verify details of provision.
-
Layer 3 (groups A, B and C) comprised all services experienced by respondents as providing treatment/support for adult ADHD. Group C included services at which stakeholders reported experience of receiving treatment/support for adult ADHD that were either not NHS services or not commissioned to provide services for adults. Examples include NHS services for those < 18 years as well as private and third-sector services.
-
Layer 4 (groups A, B, C and D) comprised all services identified by respondents, including those reported but without any confirmed experience of access for adults (group D).
Counting the number of services
For every service identified in group A (dedicated services), every uniquely named service was counted separately; for example, Oxleas NHS Foundation Trust had a ‘Bromley adult ADHD service’ and a ‘Bexley adult ADHD service’, which were counted as two services. For all other services (groups B–D), owing to constraints on study resources, each service type was treated as a single service for each area; for example, all the CMHTs provided by Somerset Partnership NHS Foundation Trust were listed as one service, although these are delivered at multiple locations across the county. In the same way, private or voluntary/charity providers, such as AADD-UK, with multiple locations or national reach, were listed as a single service.
Data analysis
Descriptive statistics
Responses were presented by informant group (patient, health worker or commissioner) and location (UK NHS region) using a geographic information system, QGIS version 2.18, to analyse and display the data. Shapefiles for UK counties and regions were imported. 137–139
Services identified
Descriptive summaries were created of identified services. These were sorted into the above groups and layers, and by NHS region. Owing to difficulties in differentiating specialist services from specialist clinics operating within a generic adult mental health service, services were described as ‘dedicated’ if they had ‘ADHD’ or ‘neurodevelopmental’ in the service name. Findings were presented using maps, to explore geographic variation in service availability.
Stakeholder perspectives
Differences in service identification were explored by creating descriptive summaries of the numbers of services identified by each informant group. Venn diagrams were used to display group differences and overlap in service identification. The percentages of services identified by each respondent type (commissioner, health worker and patient) and for each service group where there was direct experience of care (A to C) were summarised and tabulated, with Pearson’s chi-squared tests used to investigate statistically significant differences in stakeholder reporting. Categories ranged from ‘all stakeholders’ to a single stakeholder group. Group D was not included in this analysis, as these were services at which no stakeholder had reported experiences of treatment/support.
Results
Descriptive statistics, by data source
In total, 2686 different reports were included in the study, with most data (80%) coming from the online survey; 12% of reports came from the clinicians in the surveillance study and 8% from commissioners in response to FOI requests (Figure 9).
FIGURE 9.
Graphic showing mapping study data sources.
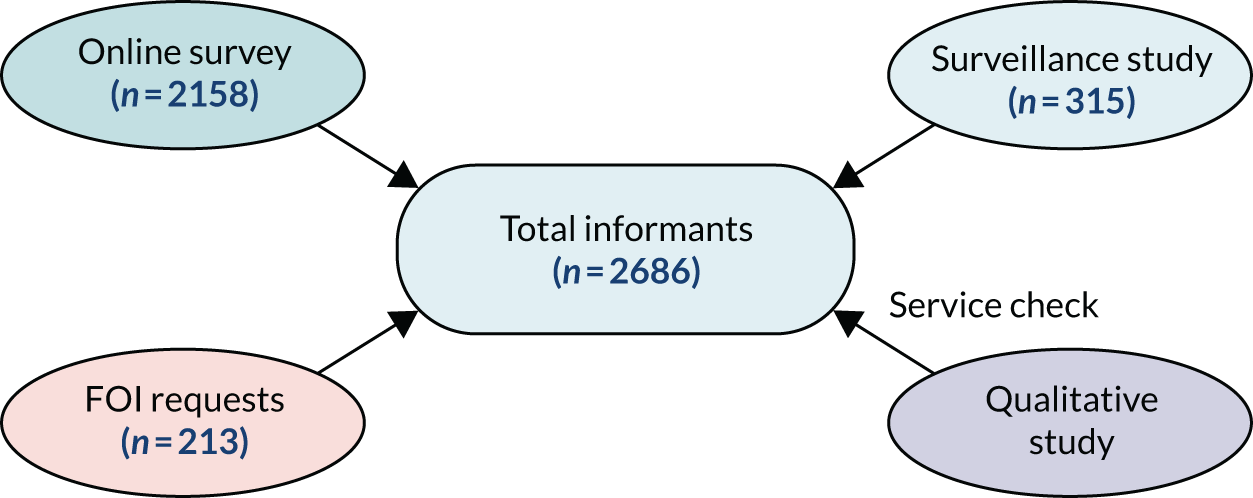
Table 10 describes how informants varied in their method of reporting. Health workers contributed the most responses in the online survey, with a further contribution via the surveillance study, but we were pleased that 17% of the responses overall were from patients.
| Responses | Data source | All | |||||
|---|---|---|---|---|---|---|---|
| Online survey | Surveillance study | FOI requests | |||||
| Patients | Health workers | Commissioners | Other | Health workers | Commissioners | ||
| Number of responses | 461 | 1631 | 3 | 63 | 315 | 213 | 2686 |
| Percentage of reports (%) | 17 | 61 | 0 | 2 | 12 | 8 | 100 |
No new services were identified through checking qualitative study interviews; therefore, the qualitative study is not mentioned any further in this chapter.
Online survey
In total, online survey respondents identified with between one and four roles [median 1.3, standard deviation (SD) 49]; 23% identified with at least one additional role. Table 11 summarises online survey contributors by informant groups and primary role identified. It also summarises the overlap between primary and non-primary roles and indicates an overlap between being a patient and parent and/or carer and being a health worker in primary care and a commissioner.
| Informant group | Primary role identifieda | Total (n) | Per cent of all roles | Code | Non-primary role (n)b | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S1 | S2 | S3 | H1 | H2 | H3 | H4 | H5 | H6 | H7 | H8 | H9 | C1 | O1 | O2 | O3 | |||||
| Patient | Adult with ADHD; aged ≥ 18 years | 262 | 12 | S1 | – | 45 | < 6 | < 6 | < 6 | 0 | 0 | 25 | < 6 | 7 | 0 | < 6 | 0 | 16 | < 6 | 9 |
| Parent/carer of someone with ADHD | 193 | 9 | S2 | 18 | – | < 6 | < 6 | 7 | 0 | 0 | 15 | 7 | 8 | 0 | < 6 | 0 | 18 | 0 | < 6 | |
| Young person with ADHD; aged < 18 years | 6 | 0 | S3 | < 6 | < 6 | – | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Health worker | Administrator | 93 | 4 | H1 | < 6 | < 6 | < 6 | – | 0 | 0 | 0 | 0 | < 6 | < 6 | 0 | 0 | < 6 | < 6 | 0 | < 6 |
| Allied health professional | 101 | 5 | H2 | < 6 | < 6 | < 6 | 0 | – | 0 | 0 | < 6 | < 6 | < 6 | 0 | 0 | 0 | < 6 | < 6 | < 6 | |
| Clinical psychologist | 84 | 4 | H3 | < 6 | < 6 | 0 | < 6 | < 6 | – | 0 | 0 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | < 6 | |
| GP | 387 | 18 | H4 | 0 | 10 | 0 | 0 | 0 | 0 | – | 0 | < 6 | 0 | < 6 | < 6 | 18 | < 6 | < 6 | 25 | |
| In an ADHD support rolec | 29 | 1 | H5 | < 6 | 12 | 0 | < 6 | 0 | 0 | 0 | – | < 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Manager | 116 | 5 | H6 | 0 | 0 | < 6 | 7 | 6 | 0 | 0 | < 6 | – | 10 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Nurse | 217 | 10 | H7 | < 6 | 8 | < 6 | < 6 | < 6 | 0 | 0 | < 6 | 17 | – | 0 | 0 | 0 | < 6 | 0 | 17 | |
| Paediatrician | 75 | 3 | H8 | < 6 | < 6 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | – | < 6 | 0 | 0 | < 6 | < 6 | |
| Psychiatrist | 529 | 25 | H9 | < 6 | 21 | < 6 | 0 | 0 | 0 | < 6 | 7 | 20 | 0 | 0 | – | 0 | < 6 | < 6 | 29 | |
| Commissioner | Clinical commissioner | 3 | 0 | C1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | < 6 | 0 | 0 | – | 0 | 0 | 0 |
| Other | Educational practitionerd | 16 | 1 | O1 | < 6 | 0 | < 6 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | – | 0 | < 6 |
| Researcher or academic | 43 | 2 | O3 | < 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | < 6 | – | 0 | |
| Other (please specify) | 4 | 0 | O2 | 0 | < 6 | 0 | < 6 | < 6 | 0 | < 6 | 0 | < 6 | < 6 | 0 | < 6 | 0 | 0 | 0 | – | |
| Total | 2158 | 100 | 39 | 111 | 21 | 17 | 26 | 0 | 5 | 54 | 74 | 36 | 1 | 7 | 19 | 42 | 9 | 97 | ||
There were some interesting overlaps between stakeholder groupings in terms of their identified roles. Of the 461 respondents primarily identifying as patients, 84 (18%) also identified as health workers. Of the 1631 respondents primarily identifying themselves as health workers, 92 (6%) also identified as patients. In total, 176 survey respondents (8% of those identifying as health workers or patients) identified with both roles.
Surveillance study
Of the baseline surveillance study questionnaires, 315 contained information potentially relevant for the mapping study;95 203 were from paediatricians and 112 from psychiatrists. Some clinicians listed multiple services on the questionnaires for cases reported to the study; they either listed the same referral service for all reported cases or reported different services for different cases.
Freedom of information requests
All 236 organisations responsible for commissioning/providing NHS mental health services in the UK140–143 were contacted via FOI requests as part of the mapping study, and 213 (90%) responded (Table 12). Although this method contributed a relatively small proportion of the overall information, the data were nearly complete.
| Country | Organisation typea | Numberb | Responses (n) | Response rate (%) |
|---|---|---|---|---|
| England | CCGs | 209 | 190 | 91 |
| Northern Ireland | Health and social care trusts | 6 | 5 | 83 |
| Scotland | Health boards | 14 | 12 | 86 |
| Wales | Local health boards | 7 | 6 | 86 |
Descriptive statistics, all data sources
Respondent type
For a summary of the roles of contributors from all sources informing the mapping study, see Figure 10. The online survey is reported from the primary role identified and surveillance study respondents were categorised as health workers, but no additional roles could be attributed as this was not queried in the surveillance questionnaires.
FIGURE 10.
The balance of roles from all sources. Dark blue, patients; light blue, health and educational practitioners; orange, commissioners, academics and other.
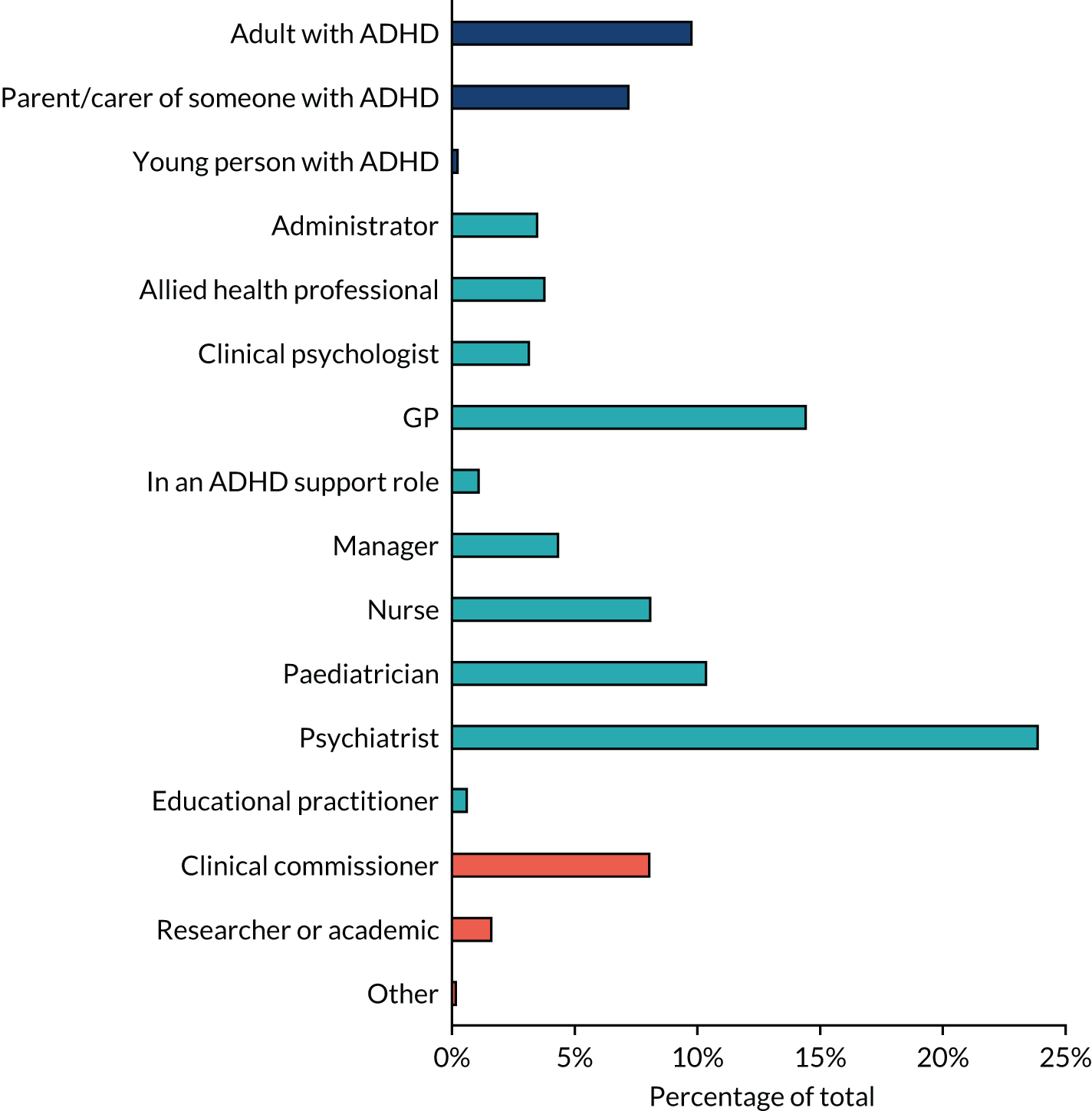
Psychiatrists were the most represented group and provided nearly one-quarter of the responses (24%, n = 641), followed by GPs (14%, n = 387) and paediatricians (10%, n = 278). Large numbers of responses from medical doctors are not surprising given the central role of medication in the management of ADHD and the direct e-mails that the Royal College of Psychiatrists was willing to send to its members. The least represented respondents were young people with ADHD aged < 18 years (six respondents), who accounted for < 1% of all respondents.
Location of contributors
Contributors to all data sources indicated the region of the UK in which they lived or, if a health worker, the location of their workplace. These locations were plotted onto a regional map of the UK, providing an overview of the geographic spread of contributions (Figure 11).
FIGURE 11.
Number of contributions by UK NHS region. Map produced using the free and open source QGIS application available at http://qgis.org144 in accordance with the terms of the Creative Commons Attribution-ShareAlike 3.0. See: https://creativecommons.org/licenses/by-sa/3.0/.
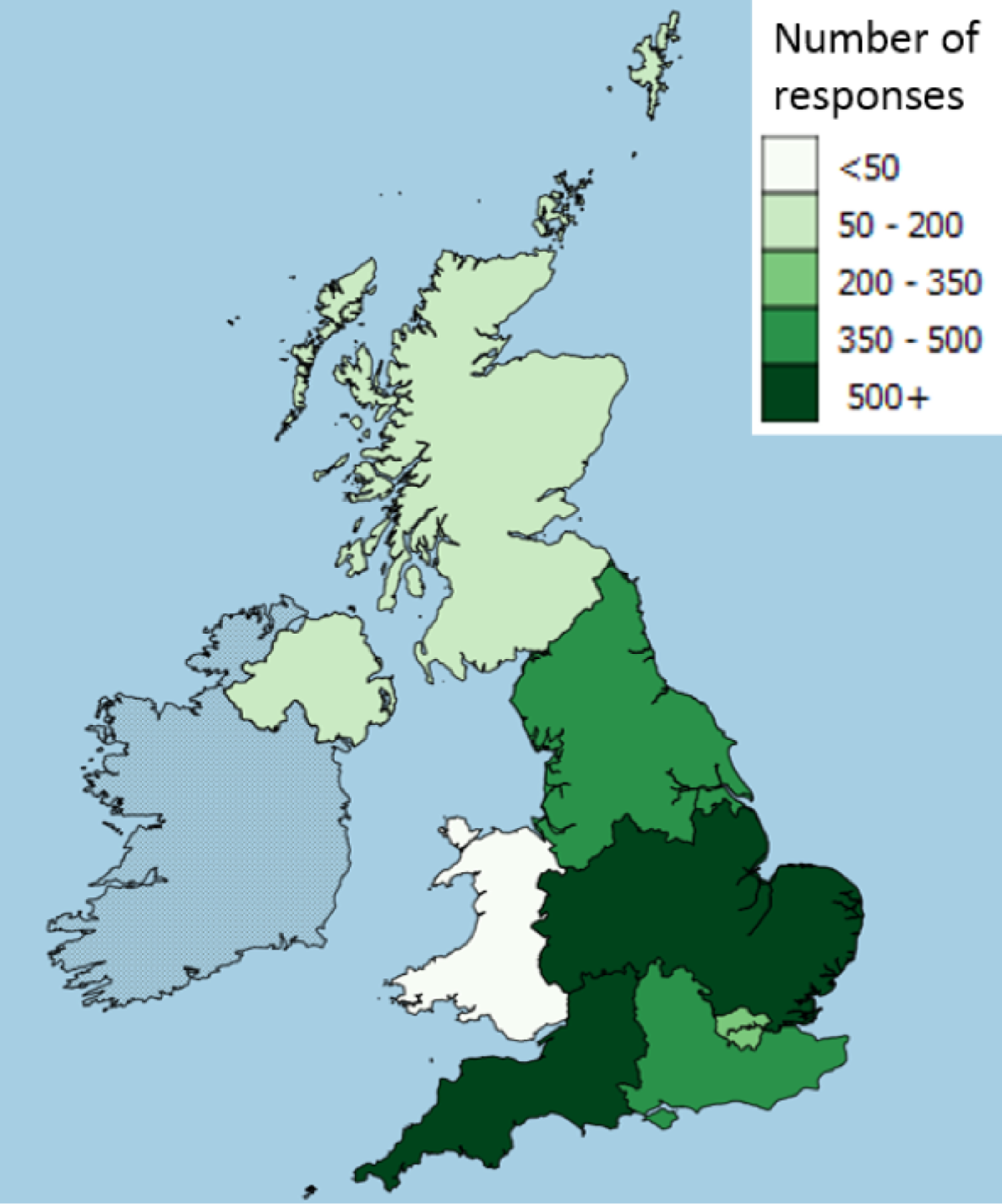
A minimum of 50 contributors were reached for every NHS region of the UK, except in Wales, where 40 contributions were received. Table 13 displays a more detailed summary of unique contributions by NHS region, data source and informant group, against the percentage of the UK population resident in that region.
| NHS region | Data source and informant group (n) | All sources (n) | Per cent of all contributions | Per cent of UK population located in this regiona | |||||
|---|---|---|---|---|---|---|---|---|---|
| Online survey | Surveillance study | FOI requests | |||||||
| Patients | Health workers | Commissioners | Other | Health workers | Commissioners | ||||
| London | 40 | 163 | 0 | 8 | 20 | 31 | 262 | 10 | 13 |
| Midlands and East of England | 70 | 362 | 0 | 8 | 107 | 54 | 601 | 22 | 26 |
| North of England | 127 | 166 | 1 | 15 | 76 | 57 | 442 | 16 | 20 |
| South East England | 64 | 306 | 0 | 11 | 36 | 36 | 453 | 17 | 14 |
| South West England | 34 | 425 | 1 | 10 | 42 | 12 | 524 | 20 | 9 |
| Northern Ireland | 32 | 23 | 0 | 1 | 12 | 5 | 73 | 3 | 3 |
| Scotland | 37 | 53 | 0 | 2 | 15 | 12 | 119 | 4 | 9 |
| Wales | 11 | 16 | 0 | 0 | 7 | 6 | 40 | 1 | 5 |
| Missingb | 46 | 117 | 1 | 8 | 0 | 0 | 172 | 6 | – |
| Total | 461 | 1631 | 3 | 63 | 315 | 213 | 2686 | 100 | 100 |
As can be seen from the data displayed in Table 13, the informant response approximated to the distribution of the UK population by NHS region, except in South West England (study location), which had relatively higher numbers of reports, and in Scotland and Wales, which had relatively lower numbers.
Service identification
Table 14 summarises the number of respondents from each data source identifying at least one service; there were 3829 unique instances of service identification from across all sources. Just over half of the informants (57%) identified one or more services. The large numbers of services identified by some respondents reflect the online survey methodology, which provided a pre-populated list of possible services derived from pilot data as well as asking respondents to identify other new services. Respondents to the surveillance study could report only one service, whereas commissioners could report between zero and four services. In the online survey, health workers (44%) were significantly more likely than patients (32%) to identify at least one service in which they had experience of someone accessing support for adult ADHD [χ2 (1, N = 2092) = 8.65; p = 0.003]. A similar proportion of psychiatrists and paediatricians (61%) mentioned at least one service in the surveillance study. Over 90% of commissioners, who were responding to FOIs and, therefore, legally bound to provide information, formally identified at least one service. Respondents to the online survey each identified experiences of treatment/support at between zero and 10 services, which left 32 services identified as known (with or without experience) by a single respondent.
| Source | Informant group | Total (n) | Type of service identification | Respondents identifying services | Number of times any service was identified (n) | Number of services identified by any single respondent | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| ≥ 1 (n) | None (n) | Percentage of ≥ 1 | Range | Mean | SD | |||||
| Online survey | Patients | 461 | Knowna | 188 | 273 | 41% | 555 | 0–32 | 1.20 | 2.61 |
| Experiencedb | 149 | 312 | 32% | 254 | 0–9 | 0.55 | 1.10 | |||
| Health workers | 1631 | Knowna | 929 | 702 | 57% | 2720 | 0–28 | 1.67 | 2.89 | |
| Experiencedb | 716 | 915 | 44% | 1139 | 0–10 | 0.70 | 1.06 | |||
| Commissioners | 3 | Knowna | 2 | 1 | 67% | 2 | 0–2 | 0.67 | 0.58 | |
| Experiencedb | 2 | 1 | 67% | 2 | 0–2 | 0.67 | 0.58 | |||
| Other | 63 | Knowna | 28 | 35 | 44% | 132 | 0–15 | 2.10 | 3.59 | |
| Experiencedb | 11 | 52 | 17% | 23 | 0–15 | 0.37 | 0.97 | |||
| Surveillance study | Health workers | 315 | Baselinea | 191 | 124 | 61% | 191 | 0–1 | – | – |
| Follow-upb | 152 | 163 | 48% | 152 | 0–1 | – | – | |||
| FOI requests | Commissioners | 213 | Formally identifiedc | 197 | 16 | 92% | 229 | 0–4 | 1.08 | 0.53 |
| All sourcesd | All | Knowna | 1537 | 1149 | 57% | 3829 | 0–32 | – | – | |
| Experiencedb | 1030 | 1656 | 38% | 1570 | 0–10 | – | – | |||
Respondents identified 294 unique services, with relatively few dedicated to adults with ADHD (group A, n = 44). There were approximately equal numbers of reports of service provision in generic NHS AMHS (group B, n = 99) and non-NHS or NHS services that were not for adults (group C, n = 111). Relatively few were identified that were not supported by respondent experience (group D, n = 40). For a summary of numbers of services at each layer and by group, see Figure 12.
FIGURE 12.
Stacked bar chart showing the number of identified services by layer of service specificity. Layer 1 = dedicated NHS services for adults with ADHD (group A); layer 2 = all NHS adult services experience by informants (groups A + B); layer 3 = all services experienced by informants (groups A + B + C); layer 4 = all identified services.
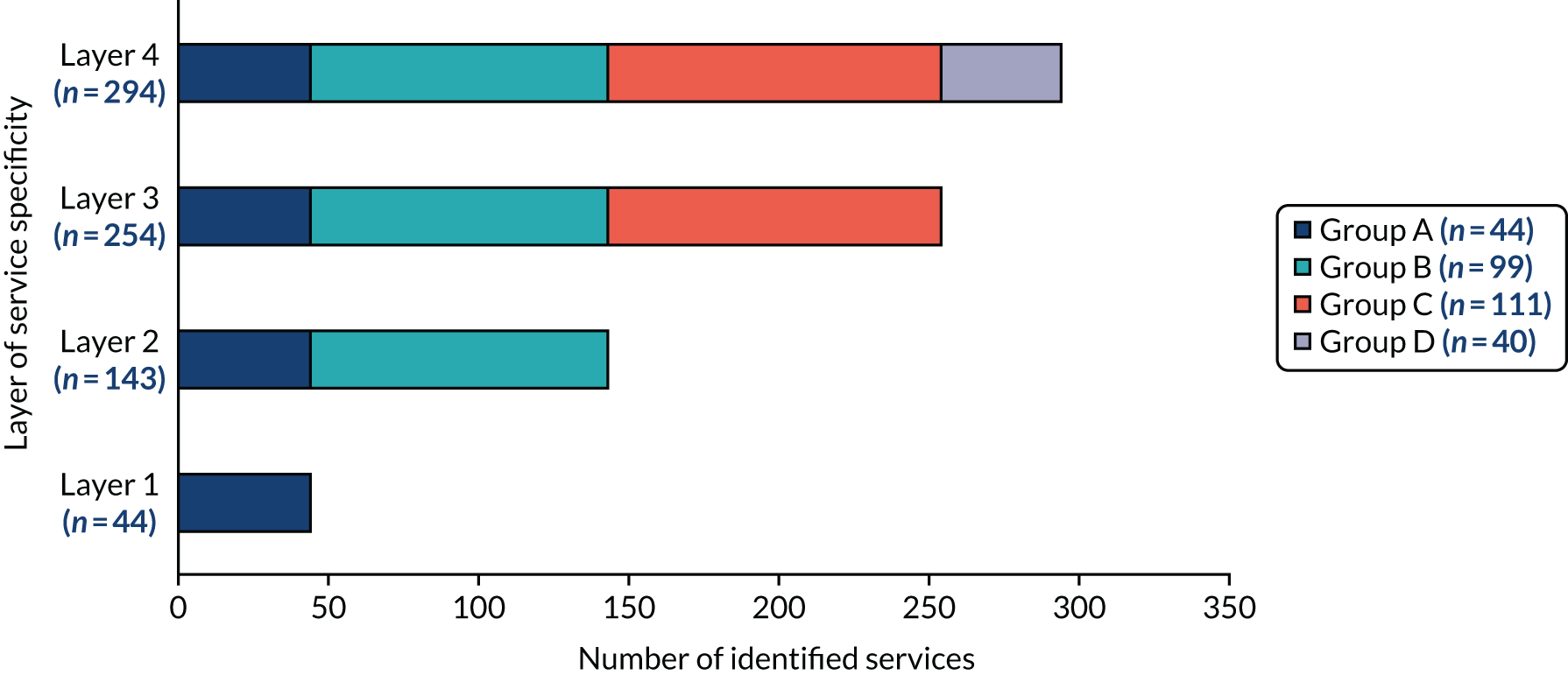
Table 15 provides further details of the different types of services reported for each layer and illustrates the huge range of service models in which adults with ADHD may access support. Although dedicated services and, arguably, those for autism spectrum disorder and LD, which are common comorbidities, would be expected to provide services for this group, other types of service may also provide services. In some areas, CMHTs may be commissioned to provide care, whereas other services may relate to comorbidities (drug and alcohol services) or be pragmatic responses (prison and primary care services).
| Layers | Service type | Number of services | Cumulative total (N) |
|---|---|---|---|
| 1. Dedicated NHS service for adults with ADHD (group A) | NHS adult ADHD | 29 | |
| NHS adult ADHD and ASD | 7 | ||
| NHS adult neurodevelopmental | 8 | 44 | |
| 2. All NHS adult services experienceda by informants (groups A + B) | Group A (see above) | 44 | |
| NHS 0–25 years’ service | 2 | ||
| NHS adult ASD | 2 | ||
| NHS adult drug and alcohol | 1 | ||
| NHS adult mental health CMHT | 70 | ||
| NHS health and social care | 1 | ||
| NHS adult LD | 17 | ||
| NHS adult mental health and LD | 2 | ||
| NHS adult mental health primary care | 2 | ||
| NHS adult mental health prison and custody | 2 | 143 | |
| 3. All services experienceda by informants (groups A + B + C) | Groups A and B (see above) | 143 | |
| Charity/voluntary | 15 | ||
| Charity/voluntary (support group) | 24 | ||
| NHS child ADHD specialist | 3 | ||
| NHS child neurodevelopmental | 3 | ||
| NHS generic child | 26 | ||
| Private | 36 | ||
| Private (social enterprise) | 4 | 254 | |
| 4. All identifiedb services (groups A + B + C + D) | Groups A–C (see above) | 254 | |
| Charity/voluntary | 6 | ||
| Charity/voluntary (support group) | 2 | ||
| NHS child neurodevelopmental | 2 | ||
| NHS generic child | 7 | ||
| NHS generic adult mental health | 6 | ||
| NHS adult LD | 6 | ||
| Private | 10 | ||
| Private (social enterprise) | 1 | 294 |
Layer 1 (group A): dedicated adult ADHD services (see Tables 15 and 16)
Group A comprised 44 dedicated services for adults with ADHD provided by 35 organisations. As implied by the service name, services were dedicated to working either with adults with ADHD (n = 29), ADHD and ASD (n = 7) or with adults with neurodevelopmental disorders (n = 8). Five provider organisations provided more than one service. The most extensive geographic spread of services was offered by SLaM, with one national service and four satellite clinics that offered treatment in several locations and across several counties.
| Location | Service details | FOI responses from NHS trust/organisation confirming the treatment/support available for adults with ADHD | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NHS region | NHS trust/organisation name | Number of services | Main service name | Service type | Location(s) | Number of services provided (n) | Lower/upper age (years) limit | Transition (n) | Diagnosis (n) | Medication management (n) | Ongoing prescribing (n) | Shared care (n) | Psychological (n) | Other (n)a | Funding access (n)b | |
| London | Barnet, Enfield and Haringey Mental Health NHS Trust | 1 | Adult ADHD Service | ADHD | Single | 1 | ||||||||||
| London | Central and North West London NHS Foundation Trust | 1 | Central and North West London ADHD Service | ADHD | Multiple | 1 | 18 | N/A | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 |
| London | Camden and Islington NHS Foundation Trust | 1 | Adult ADHD Clinic | ADHD | Single | |||||||||||
| London | East London NHS Foundation Trust | 1 | City & Hackney Adult ADHD Service | ADHD | Single | 1 | 18 | N/A | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 |
| London | Oxleas NHS Foundation Trust | 3 | Bexley, Oxleas and Greenwich Adult ADHD Service | ADHD | Multiple | 3 | 18 | N/A | 0 | 3 | 3 | 0 | 3 | 3 | 0 | 2 |
| London | SLaM | 5 | National and satellite adult ADHD and ASD Services | ADHD and ASD | Multiple | 5 | 18 | N/A | 3 | 5 | 5 | 1 | 4 | 2 | 0 | 2 |
| London | SW London and St George’s Mental Health NHS Trust | 1 | Richmond ADHD Services | ADHD | Single | 1 | 18 | N/A | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| Midlands and East of England | Birmingham and Solihull Mental Health NHS Foundation Trust | 1 | 25 + Adult ADHD Service | Neurodevelopmental | Multiple | 1 | 25 | N/A | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 |
| Midlands and East of England | Cambridgeshire and Peterborough NHS Foundation Trust | 1 | Adult ADHD Clinic | ADHD | Multiple | |||||||||||
| Midlands and East of England | Coventry and Warwickshire Partnership NHS Trust | 2 | Adult Neurodevelopmental and Transitions Service | Neurodevelopmental | Multiple | 2 | 17 | N/A | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 0 |
| Midlands and East of England | Dudley and Walsall Mental Health Partnership NHS Trust | 1 | Adult Neurodevelopmental Service | Neurodevelopmental | Multiple | |||||||||||
| Midlands and East of England | Leicestershire Partnership NHS Trust | 1 | Adult ADHD Service | ADHD | Single | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| Midlands and East of England | Norfolk and Suffolk NHS Foundation Trust | 1 | Norfolk & Waveney Adult ADHD Service | ADHD | Single | 1 | 18 | 65 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 |
| Midlands and East of England | Northamptonshire Healthcare NHS Foundation Trust | 1 | Adult ADHD & Asperger’s Team | ADHD and ASD | Multiple | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Midlands and East of England | Nottinghamshire Healthcare NHS Foundation Trust | 1 | Adult ADHD Clinic | ADHD | Single | 1 | 18 | N/A | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 |
| North of England | Blackpool Teaching Hospitals NHS Foundation Trust | 1 | Adult ADHD Clinic | ADHD | Single | 1 | 16 | N/A | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| North of England | Cheshire and Wirral Partnership NHS Foundation Trust | 1 | Wirral Adult ADHD Service | ADHD | Multiple | 1 | 16 | N/A | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| North of England | Greater Manchester West Mental Health NHS Foundation Trust | 1 | Trafford Extended Service | ADHD and ASD | Single | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| North of England | Lancashire Care NHS Foundation Trust | 1 | Adult ADHD Assessment Team | ADHD | Multiple | 1 | 16 | N/A | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| North of England | Leeds and York Partnership NHS Foundation Trust | 1 | Adult ADHD Service | ADHD | Single | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| North of England | Mersey Care NHS Foundation Trust | 1 | Adult ADHD Service | ADHD | Multiple | 1 | 16 | 65 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| North of England | North West Boroughs Healthcare NHS Foundation Trust | 1 | Adult ADHD Service | ADHD | Multiple | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| North of England | Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust | 1 | Adult ADHD Service | ADHD | Multiple | 1 | 18 | N/A | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 |
| North of England | Rotherham Doncaster and South Humber NHS Foundation Trust | 1 | Doncaster ADHD clinic | ADHD | Single | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | |||
| North of England | Sheffield Health and Social Care NHS Foundation Trust | 1 | Sheffield Adult Autism and Neurodevelopmental Service | Neurodevelopmental | Single | |||||||||||
| North of England | South West Yorkshire Partnership NHS Foundation Trust | 1 | Service for Adults with ADHD and Autism | ADHD and ASD | Multiple | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| North of England | Tees, Esk and Wear Valleys NHS Foundation Trust | 1 | Tees, Esk and Wear Valleys Adult ADHD Service | ADHD | Single | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 |
| South East England | Berkshire Healthcare NHS Foundation Trust | 1 | Neuropsychology Service | Neurodevelopmental | Single | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| South East England | Isle of Wight NHS Trust | 1 | ADHD Assessment and Treatment Service | ADHD | Multiple | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| South East England | Surrey and Borders Partnership NHS Foundation Trust | 2 | Hampshire, Surrey and Borders Autism and ADHD Services | ADHD and ASD | Multiple | 2 | 18 | N/A | 0 | 2 | 2 | 2 | 2 | 2 | 0 | 1 |
| South East England | Sussex Partnership NHS Foundation Trust | 2 | East Sussex, Brighton & Hove Neurobehavioural Services | Neurodevelopmental | Multiple | 2 | 18 | N/A | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 |
| South West England | Avon and Wiltshire Mental Health Partnership NHS Trust | 1 | Adult ADHD Service | ADHD | Multiple | 1 | 18 | N/A | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| South West England | Devon Partnership NHS Trust | 1 | Devon Autism and ADHD service | ADHD and ASD | Single | 1 | 17.5 | N/A | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| Scotland | NHS Lothian | 1 | Adult ADHD Resource Team | ADHD | Multiple | 1 | 18 | N/A | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 |
| Wales | Hywel Dda University Health Board | 1 | Adult ADHD Assessment Service | ADHD | Single | 1 | 18 | N/A | 0 | 0 | 0 | 0 | 1 | 0 | 0 | NA |
| Total | 35 trusts/boards | 44 | 39 | 26 | 36 | 38 | 27 | 35 | 22 | 13 | 13 | |||||
In England, a total of 42 dedicated ADHD services for adults were identified, provided by 33 trusts. Wales and Scotland each had one identified service. No dedicated services were identified for Northern Ireland; however, FOI responses from some health board/trusts (particularly in Scotland, Wales and Northern Ireland) implied that generic services (see group B) were more likely to be configured to treat adult ADHD in these countries.
As Table 16 indicates, only 12 (27%) of these dedicated adult ADHD services offered the range of interventions specified by NICE. 36 They were most likely to provide medication management, ongoing prescribing or shared care (89%) and diagnosis (82%). But transitional care (59%) and psychological treatment (50%) were less frequently offered. Two reported an upper age limit of 65 years, which may present problems in the future as increasing numbers of adults with persistent ADHD reach the boundary for psychiatry services for older adults. Nearly one-third (30%) indicated that patients from outside their commissioned/funded location might be able to access treatments. As Figure 13 illustrates, the provision of NHS-dedicated adult ADHD services are not evenly distributed across the country.
FIGURE 13.
Map showing locations of dedicated NHS services for adults with ADHD in the UK, and the number of residents per square kilometre. Population density displayed by lower layer super output area for England and Wales, HSC Board for Northern Ireland and Health Board for Scotland. 137,146–149 Map produced using the free and open source QGIS application available at http://qgis.org144 in accordance with the terms of the Creative Commons Attribution-ShareAlike 3.0. See: https://creativecommons.org/licenses/by-sa/3.0/.

Layer 2 (groups A and B): adult NHS services
Group B comprised 99 adult NHS services provided by 71 organisations. Layer 2 (n = 143) was made up of:
-
111 English services provided by 58 organisations (57 mental health NHS trusts and one London Council)
-
six Northern Irish services provided by each of the five NHS health and social care trusts
-
17 Scottish services provided by each of the 14 NHS health boards
-
nine Welsh services provided by each of the seven local health boards.
Table 17 summarises the types of adult NHS adult services identified in layer 2, by region.
| NHS service type | Number of services by UK NHS region | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Primary | Detailed | London | Midlands and East of England | North of England | South East England | South West England | Northern Ireland | Scotland | Wales |
| Dedicated ADHD services for adults | ADHD | 9 | 5 | 10 | 2 | 1 | 0 | 1 | 1 |
| ADHD and ASD | 2 | 1 | 1 | 2 | 1 | 0 | 0 | 0 | |
| Neurodevelopmental | 0 | 3 | 1 | 4 | 0 | 0 | 0 | 0 | |
| Total group A | 44 | 11 | 9 | 12 | 8 | 2 | 0 | 1 | 1 |
| Percentage group A | 100% | 25% | 20% | 27% | 18% | 5% | 0% | 2% | 2% |
| Services for adults | ASD | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| Drug and alcohol | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | |
| Generic adult mental health | 8 | 14 | 11 | 5 | 8 | 5 | 13 | 6 | |
| Health and social care | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Mental health and LD | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | |
| Primary care mental health | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | |
| Prison and custody mental health | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | |
| 0–25 service | 0–25 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Adult LD services | LD | 1 | 5 | 3 | 3 | 2 | 0 | 2 | 1 |
| Total group B | 99 | 11 | 23 | 14 | 9 | 12 | 6 | 16 | 8 |
| Percentage group B | 100% | 11% | 23% | 14% | 9% | 12% | 6% | 16% | 8% |
| Per cent of UK NHS region populationa | 100% | 13% | 26% | 24% | 8% | 13% | 3% | 8% | 5% |
Learning disability services
The most commonly identified type of service unique to layer 2, after generic AMHS, were LD services. These were sent FOI requests about the nature of their provision; of 17 providers contacted, 13 (76%) responded. One provider, NHS Fife in Scotland, confirmed that its LD service provided treatment for adults with ADHD. The remainder were unclear (n = 3), confirmed they did not provide adult ADHD treatment within LD services (n = 5) or mentioned other services in their trust at which treatment was provided (n = 4).
Figure 14 illustrates the geographic locations of services at layer 2, which suggests that some gaps in dedicated service provision may be explained by access to services within generic mental health services.
FIGURE 14.
Map showing adult NHS services at which respondents reported experience of treatment for adult ADHD, and the number of residents per square kilometre (population density). Map produced using the free and open source QGIS application available at https://qgis.org144 in accordance with the terms of the Creative Commons Attribution-ShareAlike 3.0. See: https://creativecommons.org/licenses/by-sa/3.0/.
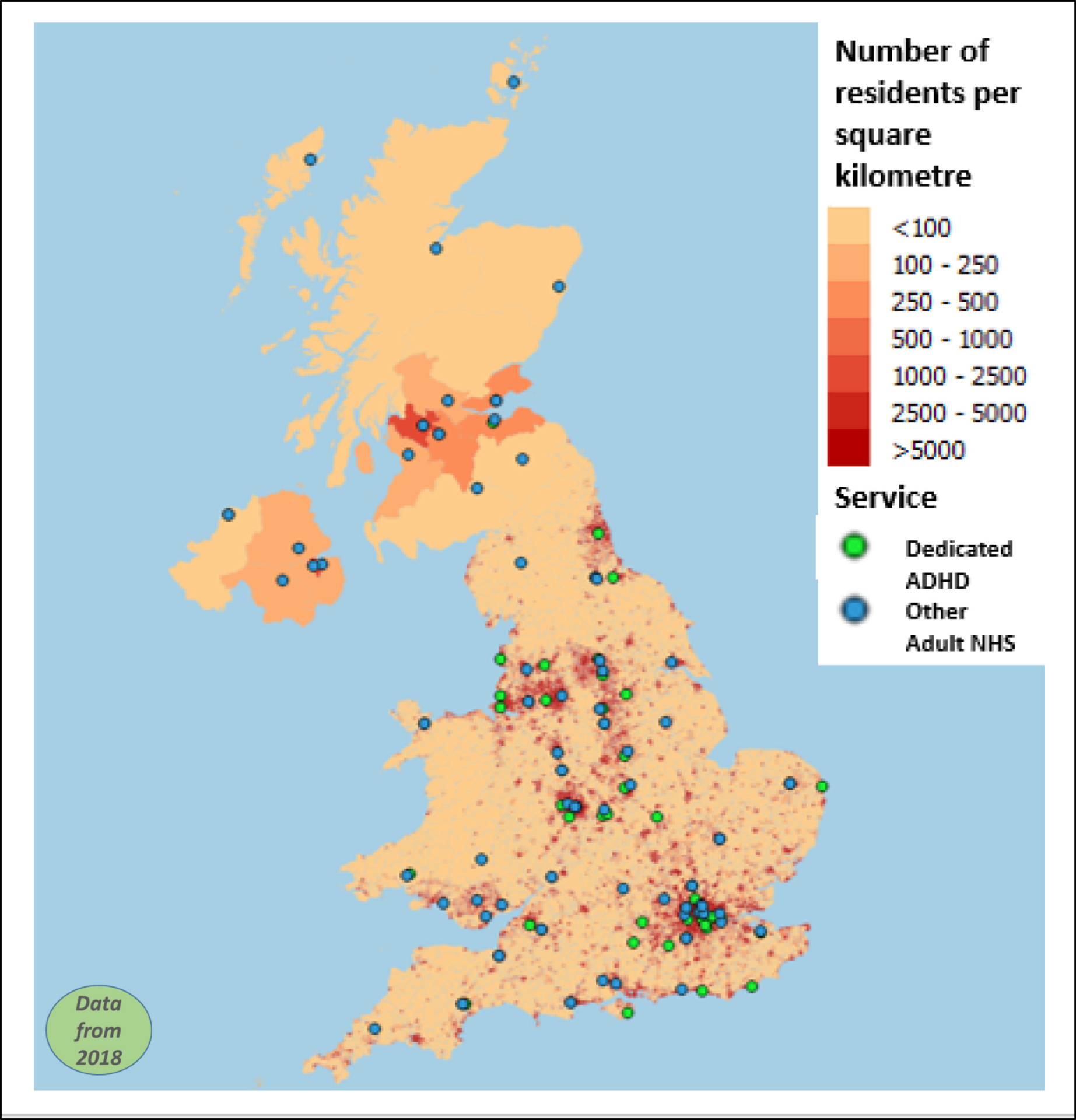
Layer 3 (groups A, B and C): all services at which support experienced
Group C comprised 32 NHS children’s services (which officially treat patients only up to age 18 years, but at which respondents reported experiences of post-18 years support), as well as 40 private organisations and 39 voluntary services/charities (111 services in total). Layer 3 (n = 254) was made up of all services experienced as providing treatment/support for adults with ADHD. This included NHS services for children and adults as well as private and charity/voluntary services.
Layer 4 (groups A, B, C and D): all services
Group D comprised an additional 40 services (9 NHS children’s services, 12 NHS adult services, 11 private organisations and 8 charity/voluntary services) that were reported but without confirmation of experience. Layer 4 (n = 294) was made up of all the unique services identified by contributors to the study.
Sharing service
Services in groups A, B and C were uploaded to an interactive Google My Maps (Google Inc., Mountain View, CA, USA) and posted onto the project website (Figure 15) (see URL: http://bit.ly/AdultADHD2018; accessed 19 September 2020). The map included a disclaimer stating it was ‘a work in progress and not definitive’. 150 Partner organisations embedded links to the map on their websites. Findings were also shared via social media.
FIGURE 15.
Illustration of the interactive Google My Map of NHS-dedicated adult services. Map data © 2019 GeoBasis-DE/BKG (© 2009), Google.
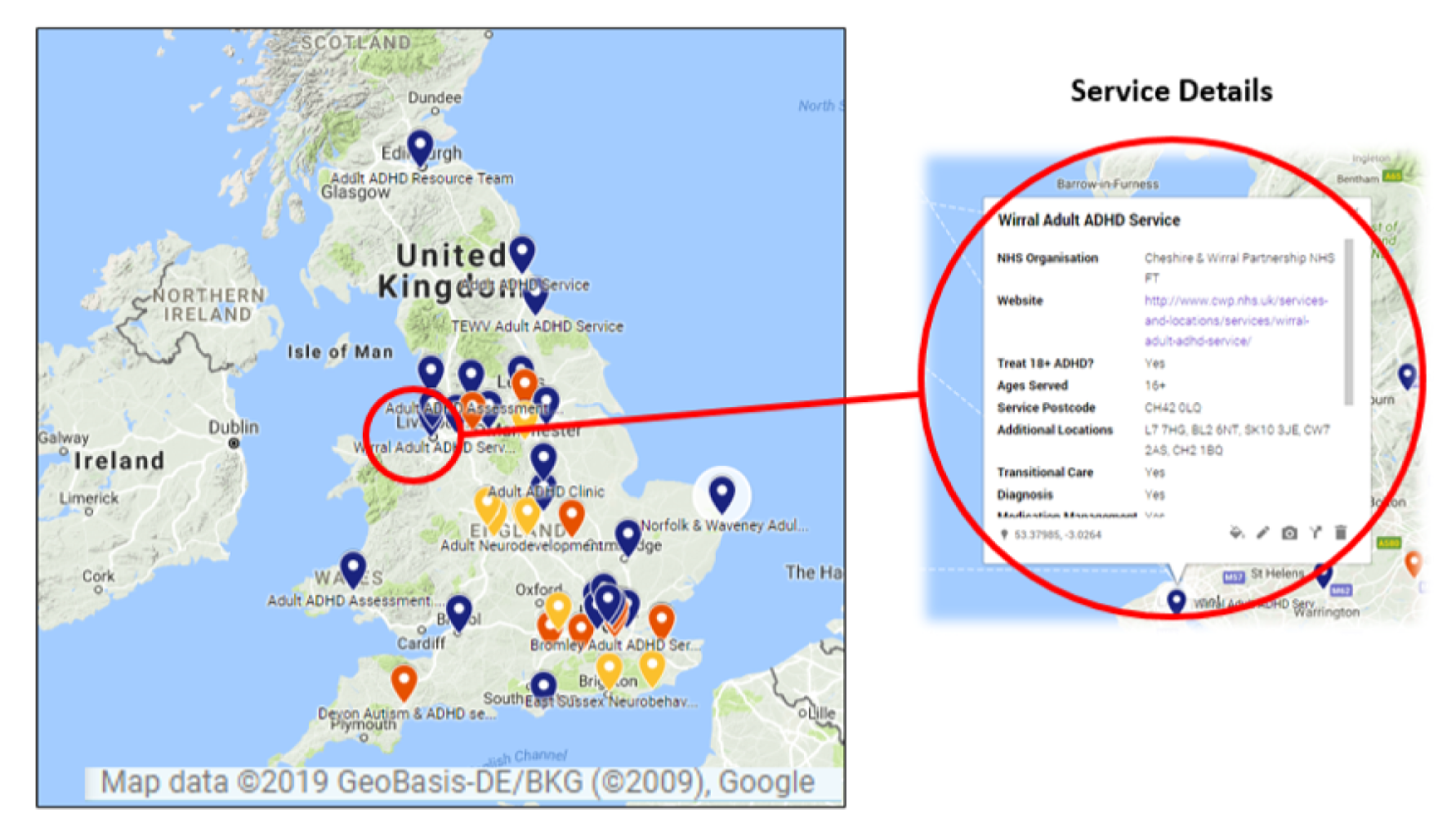
Stakeholder perspectives
Informants reporting types of service experienced
The figures displayed in Table 18 should be viewed in the context of the distribution of survey responses: 73% of respondents identified themselves primarily as health workers, 17% as patients, 8% as commissioners and 2% as other.
| Service layer | Number of services | Experienced by patients | Experienced by health workers | Identified via FOI by commissioners | |||
|---|---|---|---|---|---|---|---|
| Number of services | Per cent of services in that layer | Number of services | Per cent of services in that layer | Number of services | Per cent of services in that layer | ||
| Group A | 44 | 25 | 57 | 38 | 86 | 41 | 93 |
| Layer 1 | 44 | 25 | 57 | 38 | 86 | 41 | 93 |
| Group B | 99 | 23 | 23 | 89 | 90 | 34 | 34 |
| Layer 2 | 143 | 48 | 34 | 127 | 89 | 75 | 52 |
| Group C | 111 | 42 | 38 | 90 | 81 | 17 | 15 |
| Layer 3 | 254 | 90 | 35 | 217 | 85 | 92 | 36 |
There were significant differences between informants (commissioners, patients and health workers) in the proportion of services reported in groups A, B and C [χ2 (4, n = 399) = 34.29; p < 0.001]. Commissioners were more likely to report dedicated NHS adult services [χ2 (2, n = 346) = 32.09; p < 0.001] than other NHS adult services or NHS children’s services, or private or voluntary/charity services. Patients were marginally more likely to report dedicated NHS adult or child NHS, private or voluntary/charity services, [χ2 (2, n = 344) = 7.13; p = 0.028], and less likely to report other NHS adult services. In contrast, health workers reported similar proportions of all services, [χ2 (2, n = 471) = 0.26; p = 0.88].
Combinations of informants reporting service experience
Every service was categorised by the combination of informant groups for which at least one contributor had reported experience of treatment/support for adult ADHD at that service. Categories were all three informant groups (commissioners, health workers and patients), a combination of two or only one informant group. Table 19 provides a descriptive summary.
| Service grouping | Total | Combination of informant groups identifying service experiencea | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Co, HW + P | Co + HW | Co + P | HW + P | Co | HW | P | Other | ||
| Group A (n) | 44 | 24 | 11 | 0 | 1 | 6 | 2 | 0 | 0 |
| 100% | 55% | 24% | 0% | 2% | 14% | 5% | 0% | 0% | |
| Group B (n) | 99 | 7 | 18 | 0 | 15 | 9 | 49 | 1 | 0 |
| 100% | 7% | 18% | 0% | 15% | 9% | 50% | 1% | 0% | |
| Group C (n) | 111 | 7 | 4 | 0 | 22 | 6 | 57 | 13 | 2 |
| 100% | 6% | 4% | 0% | 20% | 5% | 51% | 12% | 2% | |
The overlap between informants of reporting services is interesting in terms of what it may indicate about information needs and flows. The majority of dedicated NHS adult services (group A) were reported by all stakeholder groups, whereas the majority of other NHS adult and child NHS, private and voluntary/charity services (groups B and C) were reported by health workers alone. There was a statistically significant difference in the proportion of group A (55%) services experienced by all informant groups, compared with group B (7%) and group C (6%) services (p < 0.001, Fisher’s exact test) (Figure 16). The implication from these data is that dedicated NHS adult services were generally known about by all three informant groups, whereas there were differences in respondents’ knowledge about the other services experienced.
FIGURE 16.
Venn diagrams illustrating overlap of service identification for groups A, B and C. Two services identified by ‘other’ are excluded, so the total number of services is not equal to the sum of services in each group.
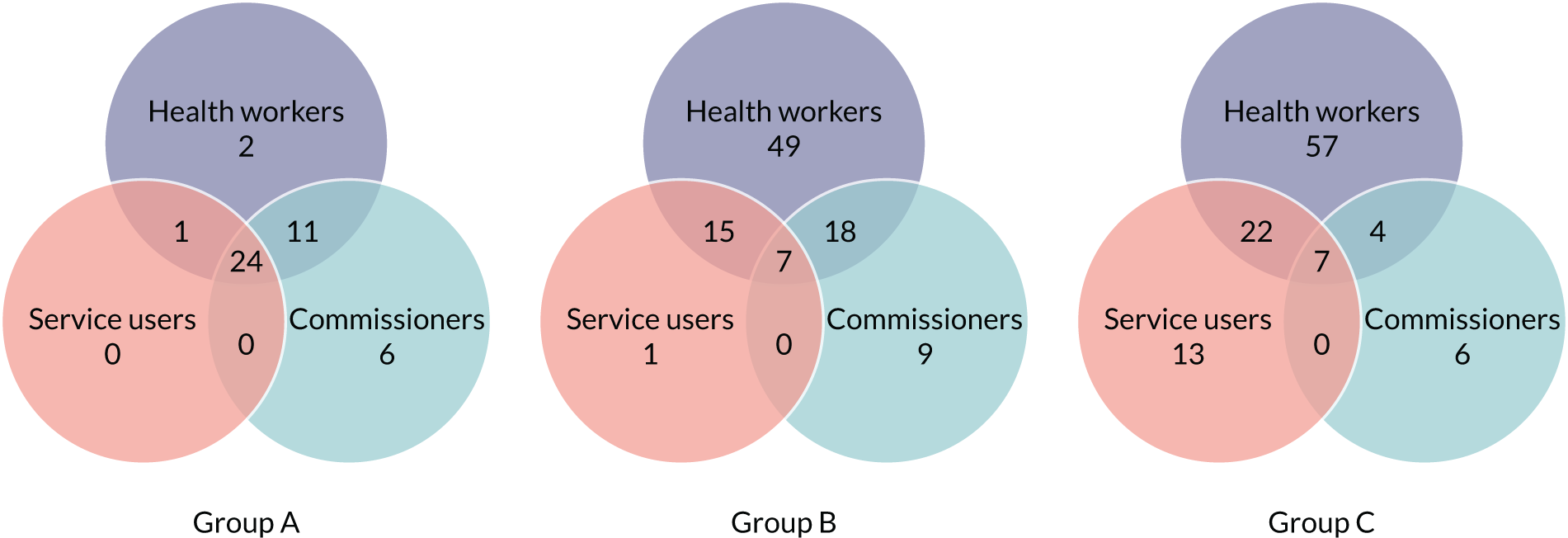
Learning disability services
The reporting of adult NHS LD services is of interest, as they constituted the largest proportion of group B service type identified (Figure 17).
FIGURE 17.
Venn diagram illustrating identification of LD services, by informant group.
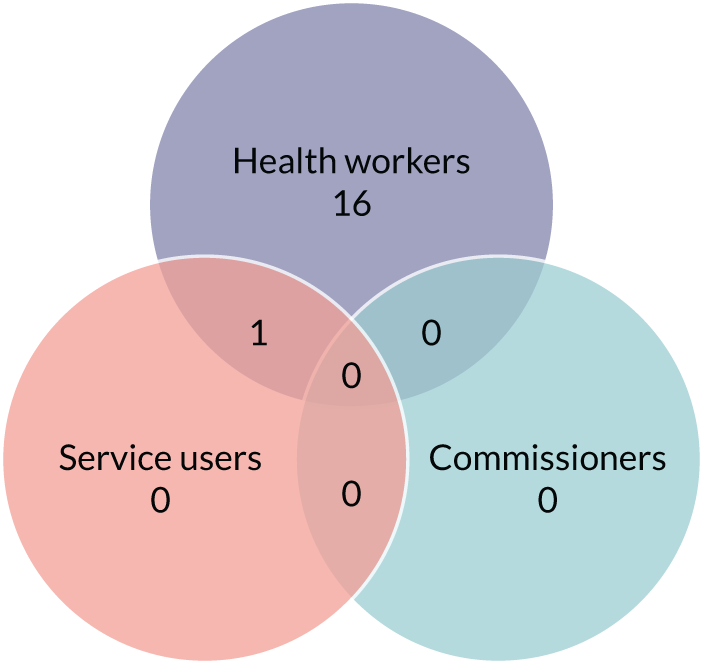
Of the LD services identified, all were named by health workers, only one was named by a patient and none was named by commissioners as providing treatment/support for adult ADHD. Although 17 LD services were identified in group B, in responses to FOI requests only one provider confirmed that its LD service worked with adult patients with ADHD.
Discussion
Gathering data on service provision from a range of stakeholder perspectives is an important part of improving health care and identifying barriers to transition. 45,151 Mapping services is particularly relevant for conditions such as adult ADHD, for which gaps in care have been identified. 74,127 Therefore, in line with recommendations from Implementing the Five Year Forward View for Mental Health,152 our findings may meet multiple needs, including those of patients in need of more accessible and better-quality information, health workers wanting to know where to refer to, and commissioners and service providers making decisions about future service design, co-ordination and delivery.
This study was designed to provide national-level data on existing services for young adults with ADHD, which could be used to optimise transition and service provision. 127,152 The methods used build on existing surveys of adult ADHD service provision, which have focused on indexing and describing services in specific UK regions or surveying a single stakeholder group, by seeking multiple informants on a national scale. 68,127,131 The significantly different pictures of service availability provided by different stakeholder groups emphasise the importance of combining information from multiple informants and raise questions about the validity of mapping methodologies that rely on input from a single source. The methodology used was relatively quick and focused, which suggests that it may be appropriate for ongoing updating and for indexing health service provision for other health conditions.
Defining dedicated services
The complexity of health service provision and commissioning in the UK means that there was no way to ensure that health service workers, patients and commissioners identified the same ‘unit’ of ‘service’ when responding to the survey. In addition, like many specialist services in the NHS, such as specialist services for older people and eating disorder services,153,154 specialist adult ADHD services are not clearly defined, which made categorising services in a way that reflected experiences of multiple stakeholders challenging.
Within UK health care, a ‘team’ of clinicians may identify themselves (or be identified by patients) as a ‘service’ when they work across the whole or parts of provider organisations or their constituent units and localities. A ‘specialist service’ may be labelled through the individual perspective of a patient, a clinician, a manager or a commissioner without it necessarily being perceived as such by a provider or commissioner. Highly specialist services may be regional or even national in terms of the ‘catchment area’ from which they are willing to accept referrals; but, equally, as commissioning arrangements are complex and varied, local areas may commission their own specialist teams, which may include dedicated time for practitioners working in generic services to focus on adults with ADHD. This complex picture, paired with the aim of including multiple stakeholder perspectives, made the task of categorising adult ADHD services challenging. The label ‘dedicated’ will cover a range of services, from the highly specialist national and regional to the ADHD consultant who has 1 or 2 days per month within an AMHS.
Service types
Identified adult NHS services (groups A and B) were of most interest as they had scope to provide the range of treatments recommended by NICE via a ‘multidisciplinary specialist team/clinic with expertise in ADHD’;36 however, findings showed that many dedicated services (group A) do not offer the full range of recommended provision. It is possible that other adult NHS services (group B) offer treatments in line with UK clinical guidelines, but we lacked the resources to check these details. There seemed to be an interesting disagreement between health workers’ reports of adults accessing adult LD services for ADHD, perhaps for comorbid LD, and FOI request responses that stated that few of them provided services to adults with ADHD. The range of group C services identified (NHS services for those < 18 years, private and charity/voluntary services) provided a snapshot of ‘alternative’ ways that stakeholders currently access treatment or support for adult ADHD, and such services were surprisingly commonly reported, particularly by health workers.
Geographic variations in provision
Although our maps suggest that services are generally clustered in areas of higher population density (e.g. as illustrated in Figure 13), they also clearly illustrate geographic inequalities in dedicated provision, with areas where services appear to be currently lacking and where young people may need to travel long distances. However, it is possible that treatment is being provided through non-dedicated (group B) services in some of these areas, for example in Scotland, Wales and Northern Ireland, as indicated by FOI responses. The findings tie in with existing evidence of variable specialist service provision for adults with ADHD in the UK, with high levels of geographic variation and identified gaps in care. 75,125,129,155–157 Health-care services in Scotland and Northern Ireland have identified an urgent need to develop capacity and capability for treatment of adult ADHD. 155,156 The current study, with data collected in 2018, identified one dedicated service in Scotland and none in Northern Ireland, but some generic provision.
Various service models are currently employed in the treatment of adult ADHD. 130 One region that initially integrated ADHD services into CMHTs158 now has a dedicated service, implying a move towards specialist provision. By contrast, in one Scottish region where work was carried out to treat ADHD within generic children’s services,159 an adult CMHT was identified by patients and health workers, implying that support for adult ADHD may be being successfully accessed within this generic service. If there was sufficient expertise in generic services, the need for specialist provision would lessen.
Changes in service provision over time
In 2012, Zaman et al. 129 described seven UK services for adults with ADHD, which, if an exhaustive list, indicates that the numbers of dedicated services have increased rapidly over the last decade. The 33 English organisations identified here as providing dedicated services, when compared with 16 mental health trusts identified by Hall et al. ,75 also suggests an increase. However, owing to changing NHS structures, the number of English NHS trusts responsible for providing mental health services has almost doubled since 2013. 160 Examined with proportionality in mind, the 55% of English NHS mental health trusts found to provide dedicated adult ADHD services in 2018 represents only a marginal increase on the 44% found in 2014. 75
Organisation of services
Some controversy remains over how to organise adult ADHD services,159 and there is, as yet, no established, evidence-based service model. Some NHS organisations may treat adult ADHD within non-dedicated AMHS. NICE guidelines specify that services should include a team of clinicians with expertise in the diagnosis and treatment of adult ADHD. 36 Generic adult NHS services’ capacity and availability for treating adults with ADHD represent a grey area that needs urgent further investigation. 130 It is worrying that less than 30% of identified dedicated services provided the full range of NICE-recommended treatments, but, equally, it can be difficult to provide transitional or psychological care to those who live a considerable distance away. Some recommended treatments, particularly transitional care and psychological treatment, could be provided by other services.
Stakeholder perspectives
Analysis of stakeholder perspectives showed that a significantly lower proportion of other adult NHS services (group B) were identified by all stakeholders than the proportion of dedicated NHS adult ADHD services (group A) that were identified. This raises questions over which generic adult NHS services provide accessible treatment for adult ADHD in practice and in line with guidelines. 36,158 The significant differences in stakeholder identification of other NHS adult (group B) services, the majority of which were identified by health workers alone, implies that patients may not be accessing these services. This could be because patients do not know about them, those that attend them did not respond to the survey or only a ‘lucky’ few patients received care from clinicians going beyond the remit of their service to meet patients’ needs. It could also mean that, although health workers believe that general adult NHS services offer treatment to adults with ADHD, in practice referrals to that service are not accepted. This barrier to transition was identified in the surveillance study, which found that only two-thirds of ADHD referrals to adult services were accepted. The fact that large numbers of patients referred were not accepted into adult services is particularly concerning as this can cause significant emotional distress. 58,125,131,161
Non-NHS services and child NHS services
Of the services identified by respondents at group C (child NHS, private and voluntary/charity), the large number of NHS services for those < 18 years replicates research findings that when transition fails or adult ADHD services are not available, child services may keep young people beyond the age boundary of their service. 58,131,155,162 This represents a pragmatic short-term solution to gaps in adult ADHD provision, but one which may lead to suboptimal care,163 and reduce the capacity of CAMHS to work with other younger people. The large number of private and charity/voluntary services indicates their significant role in adult ADHD treatment and support. The large number of private providers raises the question of whether patients are being pushed into paying for care because of the lack of NHS services, although this is an issue not necessarily confined to ADHD.
Methodological issues
To our knowledge, this study was the first national ADHD service survey in the UK to triangulate perspectives from a wide range of patients, health workers and commissioners, and apply multiple methods to optimise responses. Checking provision offered by generic adult NHS services was challenging because of a lack of up-to-date information available online, so we had to rely on informant reports, which could lack detail about what is provided. Study resource limitations meant that we were able to send FOIs to verify provision to LD and dedicated services. Of LD services, only 6% were confirmed by their providers as treating adult ADHD, which implies that, for this subsection of group B at least, not all identified services provided treatment as part of their official remit.
Although large response numbers and a reasonable balance of responses were attained, the majority of responses came from the online survey, which necessarily accessed a sample of interested and computer-literate responders. As it was not obtained via a known sample frame, this approach potentially introduced information bias, but we would argue that our findings still contribute significantly towards knowledge of and reporting of services. For this reason, analysis of service identification by stakeholder group should be treated with caution, as those who may be struggling to access services may be particularly likely to be in contact with the support organisations that supported us to disseminate the survey. Despite efforts to target young people with ADHD, very few responded to the online survey and, thus, their views are under-represented. In addition, we had differential access to stakeholders, with direct e-mail contact from the Royal College of Psychiatrists and ADHD support organisations, which, clearly, are likely to be more concerned than other health disciplines.
Service capacity of dedicated services, in terms of staffing levels, size of service and catchment area, was not evaluated and we lacked resources to confirm the status of other adult NHS (group B) services. The pragmatic definition of ‘dedicated’ ADHD services, adopted when grouping services, was in line with the study aims. A more robust definition of ‘dedicated’ or ‘specialist’ ADHD adult NHS services could enhance the clarity of the service map but would take considerable additional resources to complete with a high level of accuracy. Alternative approaches to mapping provision, such as contacting all providing NHS organisations and asking them to confirm which ADHD treatments are provided and by which type of service, could potentially help clarify complexities in service organisation. However, reporting by health providers alone would not capture patient experience of access to services. UK adult ADHD services continue to change and evolve, and these data provide only a snapshot in time of provision. Thus, any map will need to be regularly updated if it is to provide accurate information.
Future work
Developing optimum and economic service models for treating adults with ADHD remains an urgent priority. The Department of Health and Social Care NHS mandate164 highlighted areas for NHS improvement, with one focus being on providing better care for long-term conditions through improved integration of primary and secondary care services. There is a need to better understand barriers to management of ADHD within primary care and explore ways of supporting this integration. As discussed in the next chapter, a key problem for adults with ADHD is registration with a GP who is willing to prescribe medication if they require it. Future research could map availability of primary care practices to support adults with ADHD either through a shared care model or as standalone practices. Future research should also focus on differentiating between services provided by generic AMHS and those provided by dedicated services for adults with ADHD, so that apparent geographic gaps in provision can be more clearly understood.
Findings reported from the qualitative study also indicate that having a dedicated service and confirmation from a provider of treatments offered does not necessarily mean that the services are provided in practice. Therefore, research is needed to assess the capacity of dedicated services for ADHD, providing an overview of staff numbers and backgrounds, and the time and resources available for them to support their work with adults who have ADHD, as well as waiting lists.
Conclusion
Ensuring adequate provision of adult services, both across geographic locations and in line with NICE guidelines, is an important factor in removing structural barriers to successful transition for young people with long-term conditions. 44,72 This applies for young people with ADHD, whose associated difficulties with organisation and managing change can make health-care transitions especially challenging. 53,72,127 Mapping the availability of adult ADHD services is an important step towards increasing the transparency of current services and structures,125,165 with the aim of providing information to help optimise service design, and preventing premature disengagement from treatment and the associated negative life outcomes for this vulnerable group. Given that services change with time, we are delighted that the work we have started will be continued and developed by the UKAAN.
Chapter 5 Strand 3: the qualitative study
Understanding stakeholders’ views and experiences provides ‘insight into why an intervention fails unexpectedly or has unanticipated consequences, or why a successful intervention works and how it can be optimised’. 166 It is, therefore, an important component of service evaluation and development.
The NICE guidelines for optimal transition35 promote person-centred care whereby the patient is involved in planning their transition service, design, delivery and evaluation. Specifically, guidelines recommend that clinicians start planning for care in adulthood from age 13–14 years; transition should involve parents and carers, ensuring that the patient has communicated how they would like their parent/carer to be involved; the patient should be able to name the clinician taking on a co-ordinating role during transition; support should be provided before transfer, with a worker from adult services meeting the patient prior to their first appointment; and transition should be managed to facilitate the building of independence, with the patient informed of the support they can access both during transition and going forward. 35
Existing literature on transition from child to adult mental health care services suggests that the success of transition is influenced by different philosophies of care in child and adult services (e.g. family-centred vs. individual focus), lack of understanding of different service structures between child and adult services, accessibility of adult services, paucity of information about the services, stigma attached to mental illness and the fragmented nature of adult services. 73,124,167,168 This research suggests that the main reason transition fails is lack of adult service provision; thus, referrals from children’s services are either not made or not accepted. Those who are more likely to transition are patients who are on medication or have a history of severe mental illness, including in-patient mental health unit admittance. 72,124
Research about transition for young people with ADHD, specifically, suggests that there are many similarities with the general mental health transition research, but what exists is relatively sparse. 58 A national survey of mental health trusts in England in 2014 suggested that a lack of specialist services, staff training in adult ADHD and defined care and transition protocols acted as significant barriers. 75 The small qualitative literature suggests that lack of adult service provision, different eligibility thresholds between child and adult services, poor preparation for transition, poor patient information transfer and accessibility of adult services can undermine transition, whereas continued parent involvement may facilitate it. 58 UK studies of primary care prescribing have previously reported a steep fall in prescribing prevalence of ADHD medication over the transition period, with the reduction being most marked between the ages of 16 and 17 years. 131,169 A recent study suggests a continuing disparity between the expected age-related decrease in symptoms and continuation of medication, implying that premature cessation may still be taking place while young people are still experiencing impairment. 132,168
The aims of the qualitative study were to:
-
explore how stakeholders experience transition
-
identify factors that influence the quality and experience of the process of transition from children’s services to AMHS
-
identify factors or processes that underlie continuing or discontinuing treatment when approaching the service age boundary.
Methods
Sample and recruitment
Semistructured interviews were carried out to gather data from seven sample groups comprising three groups of patients at different stages of transition (pre transition, recent post transition and re-engaged patients who re-entered adult services but did not directly transition), parents of children with ADHD who were similarly at different stages of transition, and clinicians from child and adult specialist services and GPs.
To seek diversity of transition experiences, a purposive sampling approach was adopted,170 with individualised recruitment strategies for each sample group. The sampling frames included different NHS regions, ADHD service models, patient comorbidities, age, years of professional experience and gender. We focused recruitment to ensure that we included some girls or young women, who are under-represented among ADHD service attenders given the higher prevalence of ADHD among males. 171 The inclusion and exclusion criteria for each group is available (see Report Supplementary Material 11).
Decisions about sample size were informed by requirements of the sampling frame, our experiences of previous studies on transition and wider methodological writings regarding the anticipated stage in data collection when ‘data saturation’ is likely to occur. 172–175 As advised by the NHS REC, we stopped recruitment once data saturation was reached.
Young people: identifying the population for study
As NHS ethics restricted sampling to currently registered patients, we could not recruit young people who had dropped out of treatment. The pre-transition group (group 1) were aged 14–16 years and attending CAMHS. The post-transition group (group 2) were aged ≥ 18 years and transitioned straight from children’s services without a break in service, whereas the group who re-entered services (group 3) had ceased service contact for at least 1 year (Figure 18).
FIGURE 18.
Three groups of young people representing different stages in the transition process.
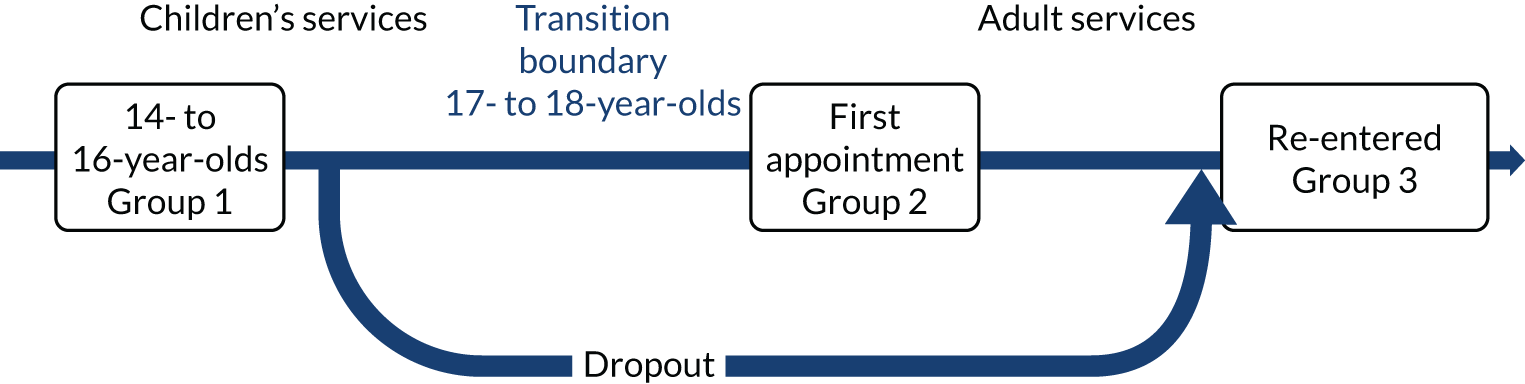
Selection and recruitment of young people and parents
We aimed to recruit 20–25 young people for each transition stage subsample from across participating sites. We similarly aimed to recruit 25 parents who would be approximately evenly distributed across the three subsamples of young people. Recruitment of young people and parents was continuously monitored to ensure that it proceeded as planned and that the sampling frame was being evenly populated as we proceeded.
Location of recruitment
Five NHS trusts (listed below in bold type) were initially purposefully selected as recruitment sites to capture both geographical variation and different models of adult ADHD service provision. During the project, we were contacted by other trusts that wanted to support recruitment and we obtained R&D approval for 12 additional trusts:
-
SLaM.
-
Berkshire Healthcare NHS Foundation Trust.
-
Devon Partnership NHS Trust.
-
Coventry and Warwickshire Partnership Trust.
-
Nottinghamshire Healthcare NHS Foundation Trust.
-
South West Yorkshire Partnership NHS Foundation Trust (HRA approved 29 March 2017).
-
Dudley and Walsall Mental Health Partnership NHS Trust (HRA approved 20 January 2017).
-
South Staffordshire and Shropshire Healthcare Foundation Trust (HRA approved 13 January 2017).
-
Torbay and South Devon NHS Foundation Trust as a Primary Integrated Community for Devon Partnership NHS Trust (HRA approved 14 October 2016).
-
Leicestershire Partnership NHS Trust (HRA approved 11 July 2016).
-
Lincolnshire Partnership NHS Foundation Trust (LPFT) (HRA approved 11 July 2016).
-
Somerset Partnership NHS Foundation Trust (HRA approved 11 July 2016).
-
Sussex Community NHS Foundation Trust (HRA approved 11 July 2016).
-
Black Country Partnership NHS Foundation Trust (HRA approved 11 July 2016).
-
Leeds Community Healthcare NHS Trust (HRA approved 11 July 2016).
-
Leeds and York Partnership NHS Foundation Trust (HRA approved 11 July 2016).
-
Sheffield Children’s NHS Foundation Trust (HRA approved 11 July 2016).
On-site recruitment procedure
Each of the five original recruitment sites had an allocated research nurse to facilitate recruitment, while additional sites were similarly supported by their local Clinical Research Network. The recruitment strategy varied slightly for each site as we adapted it to the needs of each of the three groups of young people, parents, and the local context; however, to comply with NHS R&D governance processes, NRES and data protection requirements, the basic procedure followed the five steps described below:
-
Identification of eligible young people by treating clinicians.
-
Clinicians advised the research nurse on how best to approach the young person/parent.
-
Research nurse approached the young person and handed over the information sheet and offered to discuss the study and answer any questions. The young person was encouraged to discuss the study with their parents/carer before making a decision. Participants were informed that they could have a companion to accompany them during the interview.
-
Twenty-four hours after the first contact, the research nurse approached potential participants to seek consent to pass their details to the research team. Potential participants were given as much time as they needed to make this decision. If the patient or parent agreed, the research nurse provided the research team with the completed participant notification sheet comprising details about eligibility.
-
Potential participants were contacted by telephone, text message or e-mail by a researcher to arrange a suitable time and location to conduct the interview. This also allowed the researcher to attend the interview being familiar with the interviewee and aware of any safety issues.
Incentives
Incentives (£10 shopping vouchers) were used to support recruitment of young people. Drawing on evidence that respondents’ sense of choice and control affects study take-up,176 participants could choose how [face to face, telephone, Skype™ (Microsoft Corporation, Richmond, WA, USA)] and where they were interviewed. Bearing in mind the impact of ADHD on individuals’ organisational abilities, we tried to conduct interviews as soon as possible after recruitment and used text messaging to remind participants about their forthcoming interview.
Clinicians working in children’s services
Child and adolescent psychiatrists and paediatricians who took part in the surveillance study and indicated that they were willing to take part in an interview about transition formed the sampling pool. Purposive sampling was used to ensure a spread of geographical locations and types of service provision in the area (adult ADHD mental health services availability, specialised vs. generic). We aimed to recruit 15 clinicians.
Clinicians working in adult services or primary care
A sampling pool of adults’ clinicians was created using data from the surveillance and mapping studies. The surveillance study questionnaire asked for the intended destination of patients following transfer from their service. This information was used to identify and approach clinicians working in adult services. Similarly, participants working in adult services or primary care in the mapping study were asked to indicate if they were willing to take part in an interview. We aimed to recruit 15 adult mental health clinicians and 15 GPs. We also recruited GPs by advertising on Twitter, involving the NIHR Clinical Research Network and through the snowball method, whereby participants were asked to recommend other potential participants to approach.
Data collection
Semistructured interviews were conducted with all participants. Using the principles of the constant comparative method,177 data collection was split into three distinct phases so that interim analysis could inform subsequent recruitment and adjustments to topic guides. It also allowed us to stop the recruitment if data saturation was reached. The first phase ran from April 2016 to November 2016. There was a second phase from March 2017 to May 2017 and a third phase, which focused on GPs, and ran from October 2017 to December 2018. We reached our target number of interviewed parents in November 2016; therefore, no more notifications were accepted after this date. The exception to stopping recruitment during the interim analysis was for group 2 participants. Most sites found that the required follow-up of patients transferring to adult services to check that the young person had attended at least one appointment was more challenging than anticipated. Pausing group 2 recruitment may have risked negatively affecting this longitudinal element of the recruitment process, so group 2 notifications were accepted and these patients approached from April 2016 to May 2017. Following the first phase of data collection, topic guides were revised with some questions added to reflect learning from the interviews conducted and to focus on emerging themes; for example, questions were added to patient topic guides asking patients when they first realised that they might need support as an adult, and about the role of their GP. The third phase with GPs was introduced because of the prominence of reports about the role of primary care in the initial qualitative data collection from all groups.
Consent and confidentiality
Before the interview, the researcher discussed the study with the participant, who was then given the opportunity to ask any questions. Once the participant had agreed to continue with the interview, they were asked to sign the consent form. Copies of the study information sheets and consent forms for all sample groups are available (see Report Supplementary Material 12–17). Parents of young people aged ≤ 15 years were asked to consent to the participation of their child, and we also sought assent from the young person. Interview transcripts were stored on a university server. Digital recorders and any hand-written notes were stored in a locked cabinet until files were uploaded or notes scanned. Any potentially identifying information was deleted.
Content of the interviews
The semistructured interviews were conducted using a topic guide informed by the research questions, existing research and guidelines on transition, and discussions with our PPI group members and the SSC. All interviews were audio-taped and transcribed verbatim. The interviews with young people and parents covered the following topics:
-
current and future medication use (e.g. reason for taking, what might make patient want to continue or stop medication in the future)
-
current and future contact with services
-
experiences of the transition process
-
views on key elements of optimal transition (e.g. having a named contact, continuity of care).
The interviews with clinicians included the following themes:
-
practicalities related to transition process (e.g. age boundary of the service, existence and use of transition protocol)
-
pre-transition dropout
-
key elements of optimal transition – continuity of care, parallel care, a transition planning meeting and information transfer
-
involvement of young person, parents and/or other services in the process of transition
-
personal experiences with good and difficult transitions
-
re-entry (clinicians working with adults including GPs)
-
management of young people in transition in primary care (GPs).
The topic guides for all sample groups are available (see Report Supplementary Material 18–24).
Analysis
Data were managed using QSR International (Warrington, UK) NVivo 11 qualitative data analysis software. Data analysis followed a framework analysis approach, an approach to thematic qualitative analysis that has been explicitly developed in the context of applied social science research. 178 This method facilitates systematic and transparent data analysis, allowing the researcher to move between levels of abstraction while maintaining clear links to the original data. 179 Figure 19 provides an overview. The approach allows the researcher to identify patterns or commonalities, as well as contradictions in and between participants’ accounts, and to explore and test explanations for those patterns. It is also open to external scrutiny, and the systematic nature of the process means that it can be replicated, which facilitates analysis by different researchers. Data from each of the six samples were analysed separately. In a later stage, findings were compared and integrated to seek consensus and differences in views and perspectives between the stakeholder groups. More detail regarding the analytical approach is available (see Report Supplementary Material 25).
FIGURE 19.
Overview of the different steps in framework analysis, illustrating researcher contributions.
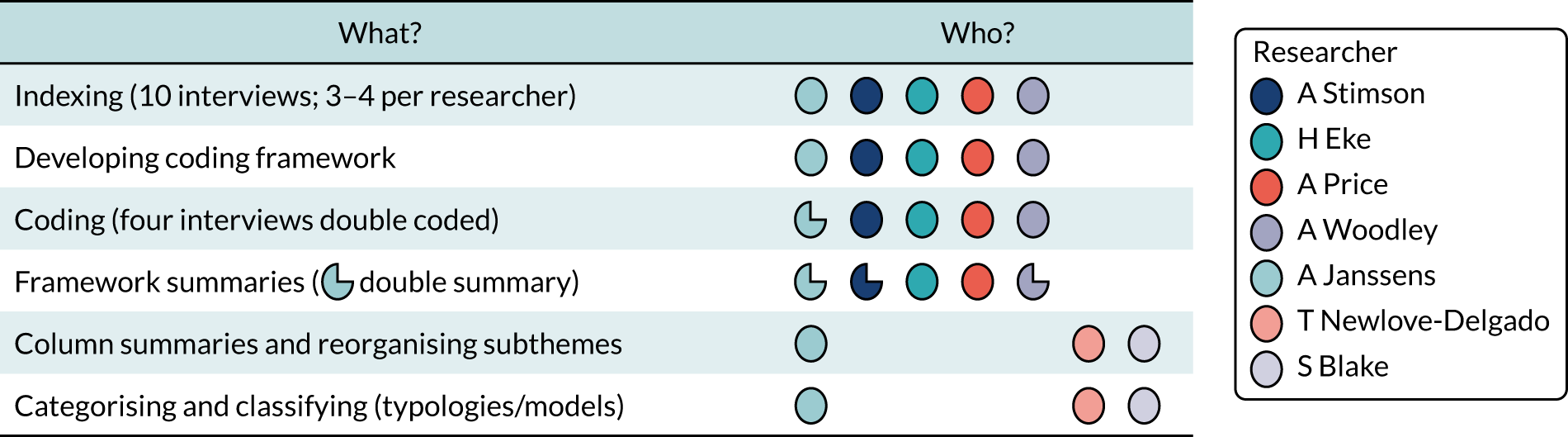
Results
Interviews were carried out with 144 individuals from across all regions of the UK (Table 20). Patients and parents were recruited from 10 of the 17 participating health trusts.
| Region of UK | Total number of participants | Patients group 1 pre transition | Patients group 2 post transition | Patients group 3 re-entry (no transition) | Parents | Clinicians in children’s services | Clinicians in adults’ services | GPs |
|---|---|---|---|---|---|---|---|---|
| East of England | 8 | 0 | 0 | 0 | 0 | 4 | 4 | 0 |
| East Midlands | 26 | 5 | 6 | 6 | 6 | 1 | 1 | 1 |
| London | 26 | 3 | 7 | 7 | 5 | 3 | 1 | 0 |
| North East | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 |
| North West | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
| Northern Ireland | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Scotland | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| South East | 21 | 5 | 2 | 0 | 6 | 2 | 4 | 2 |
| South West | 33 | 0 | 5 | 7 | 5 | 4 | 3 | 9 |
| Wales | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| West Midlands | 17 | 5 | 2 | 1 | 6 | 1 | 1 | 1 |
| Yorkshire and the Humber | 5 | 3 | 0 | 0 | 0 | 2 | 0 | 0 |
| Total | 144 | 21 | 22 | 21 | 28 | 22 | 16 | 14 |
We interviewed 64 patients (see Table 20). In group 1 (pre transition), we were notified of interest from 26 patients and interviewed 21. These patients had a mean age of 15 years (SD 0.921 years, range 14–17 years) and comprised five females and 16 males. For group 2 (post transition), we were notified of interest from 38 patients and interviewed 22. These patients had a mean age of 18 years (SD 0.963 years, range 17–21 years) and comprised nine females and 13 males. In group 3 (re-entered services), we were notified of interest from 27 patients and interviewed 21. These patients had a mean age of 23 years (SD 3.109 years, range 19–29 years) and comprised six females and 15 males. Of the total patients interviewed, 27 were in education, 11 were employed, two were in vocational training and 11 were not in education, employment or training; the occupational status of 13 patients was unknown. Forty-five patients were living with parents, 17 were living independently and one attended a residential special school; the living situation of one young person was unknown. A total of 16 of the 64 patients interviewed reported contact with the criminal justice system, which included over half of those who re-entered services (12/21 patients). Reported comorbidities of patients interviewed included autism, anxiety, depression, dyslexia, dyspraxia, anger issues, LD, cerebral palsy, obsessive–compulsive disorder, Tourette syndrome, insomnia and oppositional defiant disorder (Table 21).
| Pre transition < 18 years | Post transition ≥ 18 years | Male | Female | Comorbidities | No comorbidity disclosed | Comorbidity unknown |
|---|---|---|---|---|---|---|
| 42 | 50 | 67 | 25 | 53 | 32 | 7 |
We were notified of interest from 33 parents and interviewed 28 (27 mothers and three fathers – two of whom contributed to interviews held with the mother). The mean age of the child of the parent interviewed was 18 years (SD 4.029 years, range 14–28 years) and the gender of their child with ADHD included five females and 23 males.
We contacted 130 clinicians who expressed interest in the study from the surveillance or mapping studies, or social media/snowball sampling methods, and interviewed 52, which comprised 22 clinicians from children’s services (15 paediatricians and seven psychiatrists); 16 adult mental health clinicians (seven psychiatrists, two psychologists, one nurse prescriber, one mental health nurse, five unknown) from specialist adult ADHD services and general mental health practice; and 14 GPs (including two working in university practices, two who had a mental health lead role or special interest, and one with an additional commissioning role).
Two overarching and inter-related themes were identified as affecting transition experience and outcomes: (1) how invested stakeholders are in continuing ADHD treatment and (2) the architecture of services (how services are commissioned, configured and function) in local areas (Figure 20). We identified a number of factors, within and across these themes, which appeared to influence transition, as well as a default role for GPs.
These findings are set out next, with direct quotations from the interviews in italic. The code attached to the quotation indicates the stakeholder group and interview number. Parts of the quotations that refer to interviewer speech are indicated. The term parent includes carers or significant others who may take a caring role.
FIGURE 20.
The ADHD transition process as perceived by key stakeholders.
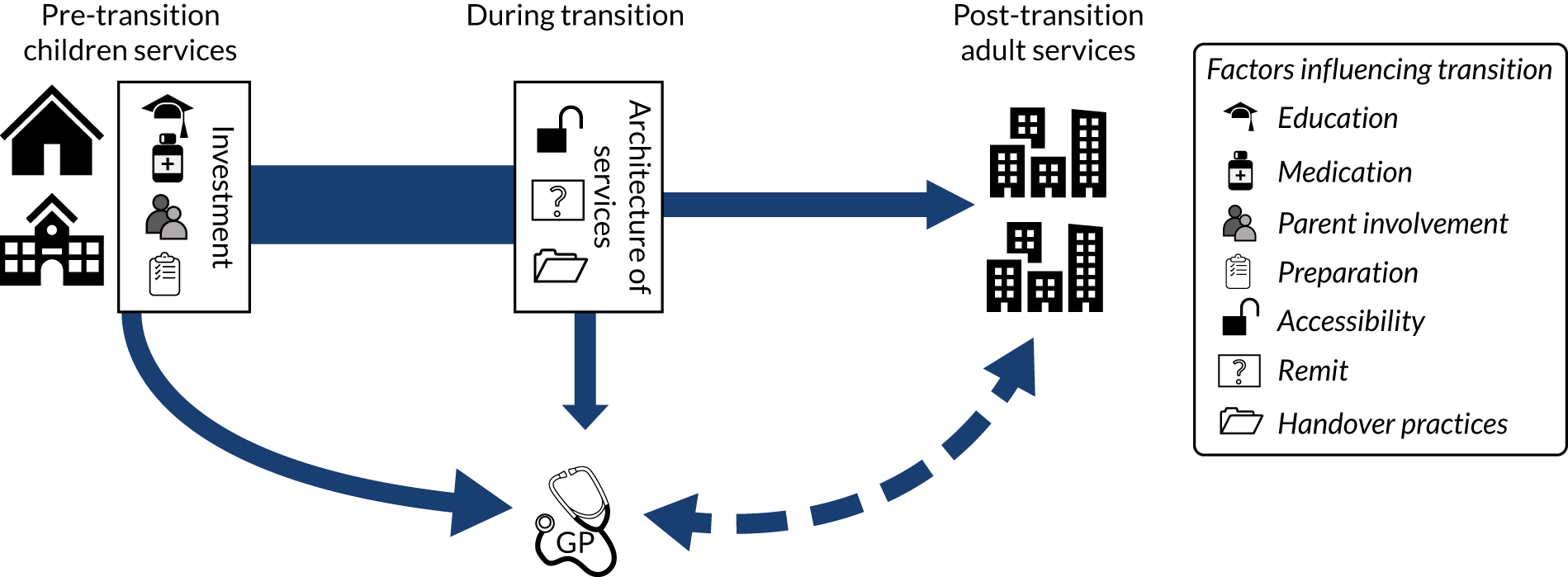
Being invested
The interviews suggested that the degree of investment in continuing ADHD treatment influenced transition. Those who transitioned or returned to services as a young adult accepted ongoing medication as beneficial, or demonstrated a recognition of ADHD as a long-term condition:
I think I’ve got to the stage where I kind of just stopped caring. It is part of me now, I can hate it and I can love it sometimes and sometimes it’s lovely and sometimes it’s the most annoying thing in the world but it’s part of me.
Transitioned patient 01
So that sort of tricky age of adolescents where they feel, ‘Oh maybe I don’t need medication, I’m not in school’ or ‘I’m in charge of my own mind now, I’ll do what I want’ and that transition within their own perception of who they are and taking control of their lives now they are an adult, that’s the barrier, I suppose, in some respects, but once they are into the service then we can work with them.
Adults’ clinician 05
Four inter-related factors were identified as influencing investment in continuing treatment into adulthood and, thus, could act as barriers to, or facilitators of, transition: (1) an association made between ADHD and education, (2) a view of medication as beneficial, (3) parent involvement and (4) feeling prepared for transition and adult life with ADHD.
Education
The interviews revealed a strong association between ADHD and its management, and the school environment and academic attainment. School was commonly the place where symptoms were first flagged as problematic and the rationale for medication was often understood as improving academic performance or behaviour in school, with medication breaks reserved for outside term time or weekends:
To help me get qualifications, get the grades I need, help me concentrate. Because I don’t take them at weekends.
Pre-transition patient 13
They’ve actually said that they don’t want him in the college if he’s not medicated . . . So we are caught between a rock and a hard place really. Because he wants to stop taking his medication. He hates being on the medication . . . if he’s not on the medication we can see it straightaway.
Parent 09
I mean we do obviously give drug holidays for weekends and children that are doing well during half-term and things, let them run a bit wild when it doesn’t matter, they’re not learning anything. Some of them can cope, some of them can’t.
Paediatrician 15
Like I say, for the sake of school, that’s what I was taking them for really. So, I was kind of excited, well not excited, but waiting to finish school so I wouldn’t have to take them.
Re-engaged young adult patient 07
Some clinicians in children’s services reported advising patients that medication was to be taken when needed and not necessarily related to education; however, the association with education meant that patients often assumed that treatment would end when school finished. This assumption appears to be reinforced by the timing of trials off medication. In line with NICE guidelines,36 clinicians in children’s services described trialling a medication ‘holiday’ to see if a patient can cope without medication, or if there is an ongoing need requiring transition to adult services. Although clinicians reported that this process was flexible depending on the complexities of patients’ needs, it typically occurred at the end of mandatory education. These clinicians reflected that the timing matched a desire expressed by patients to come off medication once school exams were completed; however, it could mean that if after trialling a period off medication patients wanted to restart their prescription, they may have become too old to return to children’s services:
Particularly once they are past GCSEs [General Certificates of Secondary Education] and they have done their exams, then we would try to wean the medication down and see how they manage without it, but over a long period of time.
Paediatrician 19
It depends on your young person, there are some who are 16 who you start talking about [adult services and transition] . . . You estimate what their trajectory is going to be partly depending on their functioning and all their other needs and their academic engagement, family engagement, their history, their responsibility . . . They tend to disengage from wanting to take medication . . . around 17ish . . . when they finish mainstream education, so if our ADHD kids are moving into more the college based or the apprenticeship based, that’s when they might say ‘I don’t want “meds” anymore’ and if they come off their meds then we would probably discharge them, if they haven’t got any other needs.
Child and adolescent psychiatrist 08
Those who were continuing on to higher education were typically more invested in continuing treatment and, therefore, were more likely to transition:
Some of them will be going to college. Those are probably the ones that are most likely to want to carry on medication . . . because they are more aware that they are not concentrating as well.
Paediatrician 11
If they’re not going to university, if they’re going into employment then it’s [referral to] GP.
Child and adolescent psychiatrist 08
However, young people who had recently transitioned reported seeing a future in which symptoms would improve once formal education was completed, a view also expressed by some clinicians in children’s services:
I can imagine it still [being an issue] because it’s just me, but it’s not going to be that bad if I’m in a job that I like and I’m not having to be forced to do something I hate. It probably won’t be as bad. But having to sit, that’s just what has been really difficult at college and school. So, I think it will get easier.
Transitioned patient 05
I think there’s a small proportion where the ADHD symptoms have genuinely stopped being an issue because they are in a situation where they are doing more of what they want to do . . . they have either left school or are leaving school, they are going on to something they are actively interested in, rather than something they are being forced into doing in the context of school, so they are not having problems in the same way.
Paediatrician 11
Many of the young adults who returned to services regretted their decision to stop treatment because they mistakenly thought they had ‘outgrown’ ADHD, or treatment was no longer necessary as they had left school. They reflected on the timing of transition decisions when they lose the structure of school and gain more responsibilities, including greater consequences if things go wrong:
The bottom line was you are 16, this is it, you’ve got through school. I think they targeted school as that was the battlefield that I need to get beyond to give me a step in later life and once that was achieved it was, yes, you can do it on your own, you don’t need us anymore. There was never any discussion about if you do need post-16 care, this is where to go, this is how to apply, nothing like that.
Re-engaged young adult patient 02
ADHD is different as an adult, and risks and all that . . . Being impulsive can have a bigger impact on you as an adult. So, when you’re a child there’s a bit more safeguards around you, parents, school . . . you’ve got these people round you. And also, you have less responsibility. But then when you’re older, and if you do something impulsive or don’t think it through, as with me, it can have a massive detrimental impact.
Re-engaged young adult patient 13
Parents and young adult patients with ADHD advised that part of accepting ADHD and being invested in continuing support and treatment was identifying strengths and finding a niche, such as a sport or looking after animals, regardless of continuing education:
That was the thing that saved me, is finding something that focuses my brain. Really enjoying something that focuses me makes everything else I do bearable.
Re-engaged young adult patient 21
Because she’s who she is and she’s sort of quirky and loud, she’s started getting into the music photography scene, so she’s been off and she’s been shooting bands . . . I think actually that would probably fit in with who she is. She probably wouldn’t quite fit into an office environment [laughs].
Parent 01
Child and adolescent psychiatrists and paediatricians described how education could play a significant role in transition, particularly if the patient had learning disabilities and/or attended a special school:
A lot of the handover I end up doing is actually to the further education colleges.
Paediatrician 22
I guess if they are in a special school the story is very different, and some of my kids are at special schools, then the process is usually led by education . . . From 14 plus I think people start talking about transition, there’s a transition team and the process is clear.
Paediatrician 02
Clinicians in children’s services described how patients moving area to start university or moving to new supported living arrangements could add a layer of complexity to transition; notably a lack of clarity over funding arrangements and clinical responsibility, including who was going to prescribe ADHD medication. The response to those moving area around the time of transition varied. In some cases, patients were transferred to waiting lists for adult services in their existing local area, some discharged patients to their GP and recommended help from university student health services, whereas others held onto their patients until they were settled in their new area:
It took me about a year and a half to transfer this 17-and-a-half-year-old . . . who was going to uni [university] . . . we weren’t clear what the funding arrangements were . . . I referred this one about 6 months ago and they still haven’t received the confirmation of funding from our CCG . . . it’s just paperwork and bureaucracy that tends to get in the way.
Paediatrician 05
Obviously, the GP won’t prescribe unless the psychiatrists are going to see him, so it landed up with a teenager going to college very much on medication . . . and nobody prepared to prescribe it. Well I can do it for so long, but you can’t start prescribing as a paediatrician for a 20-year-old that’s not in your care anymore. So, we did sort it, but it was very difficult. I think that group of children probably are the ones that land up in limbo because nobody is taking responsibility.
Paediatrician 12
So, what seems to happen is they leave our service, they go on the queue for the adults but don’t get seen by them and when they do, the appointment comes up when they’re off at college anyway.
Paediatrician 18
Medication
Whether a patient was being prescribed ADHD medication at the time of transition appeared to influence whether or not they were referred to adult services, with transition typically reserved for those continuing to use medication. Clinicians in children’s services explained that, although not a decision made in haste, in order to manage resources, patients off medication and without any other significant issues would usually be discharged to GPs:
Ideally if they weren’t on medication you should carry on seeing them, but it’s not going to happen in the real world . . . we don’t have the clinic space, so after they have chosen to go off medication, so you have maybe given them one or two appointments, after that you are going to have to discharge them.
Paediatrician 11
So, at 17 they’re going to have a view whether they’re going to be continuing medication or not in adulthood. So, if it looks like they are likely to want to continue medication then a referral is made at that point . . . If you don’t want medication the adult services won’t see you anyway so on you go with your family doctor . . . If you want to continue with medication there’s a psychiatrist who will see you. If you don’t want to continue with medication, you know, carry on. You’re on your own.
Paediatrician 18
The perception of clinicians in children’s services that medication was an eligibility requirement for adult services was reflected in other stakeholders’ experience of adult services as being medication focused. Adults’ clinicians typically reported that they are commissioned to provide only pharmacological services:
I think they just think that you are druggies and you want drugs. But that was not the case. I wanted to try and get some help.
Parent 14
All they [adults’ clinician have] done really is just met me twice, started me on the medication, seen how I’m going and then tell me they’ll see me in 6 months or a year to see if the medication is still working.
Re-engaged young adult patient 02
It’s the medication that gets you the access to the [adult] service. And if you have ADHD and autism or if you have ADHD and you’re not on medication and you’ve got autism and perhaps I don’t know Tourette’s . . . as well then you wouldn’t access services just because you have more than one thing. But if you had relatively mild ADHD perhaps on medication which you wanted to continue with then you would access services so there’s a bit of inequity there.
Paediatrician 14
The medication focus of services meant that a patient’s choice to stop medication also meant processes to transfer to adult services were not initiated; however, our data suggests that these may not always be thoughtful and future-orientated decisions. Treatment decisions were often described by patients as led by the clinician and parents who ‘know best’ or made to support short-term goals, such as to pass exams:
I just kind of say to do what’s best because really, I don’t know as much as she does about it. Even though it’s me who has it, they know a lot more than I do. So, I just think just let them just try.
Pre-transition patient 08
Do you think you’re going to continue to need support for it once you’re in your 20s?
I’m really hoping not . . . I mean to be fair the only reason I came for medication was to get me through college . . . I’m just about to finish. I mean possibly if I’d have found the right medication, I would be, but I’ve given up on that idea.
Transitioned patient 01
Numerous reasons were given for medication cessation. Some stopped medication as they finished education and ‘slid’ out of services without a conscious decision or action. Others stopped taking medication because of pregnancy or a desire to establish a career where ADHD medication is not permitted, such as in the military services. Medication was also stopped because of a struggle with side effects, such as insomnia, migraines, weight loss and dry mouth. For those who struggled, once short-term goals had been achieved, the ‘bad’ outweighed the ‘good’:
So, can you remember much about why you stopped going to the service when you were younger?
The side effects . . . I just stopped taking it all and then I just didn’t go anymore. Three years I was off [medication]. Because it affects your appetite and affects your sleeping and I was on sleeping tablets, but they weren’t even helping.
Re-engaged young adult patient 03
Yes, we get lots and lots of people who have dropped out of treatment for all sorts of reasons, sometimes because they’ve disengaged, sometimes because they’ve wanted a period without medication. Quite a lot of people seem to want to go into the forces . . . [they] try to white-knuckle life a bit without medication.
Adults’ clinician 06
The experience of patients in group 3 who were discharged after stopping medication but returned to services a few years later was reflected in the adults’ clinician interviews. The re-engagement with services very often followed a profoundly negative experience in their lives, which prompted them to question the influence of ongoing ADHD symptoms on their functioning and seek support:
There’s lots of people who decide they don’t want to continue with the medication. It often is the case and people will be referred back a year or two down the line saying, ‘Actually, things have got really difficult now and I need to rethink about medication’. That’s not uncommon at all.
Adults’ clinician 10
I just went to jail and even when I was sitting in jail I was sitting there thinking, ‘I’m here over something stupid. If I was on my medication I wouldn’t even be here’.
Re-engaged young adult patient 20
I did the stupid thing that all teenagers who know better do, especially when they’re on medication and they see that they are coping and don’t actually tie it back to the fact that it’s the medication that’s meaning that they can cope. I took myself off the medication. I lasted a good couple of years before anything went sideways but then it went sideways in a big way.
Re-engaged young adult patient 08
Clinicians and parents recognised the challenge of discussing treatment options during adolescence when young people were seeking greater autonomy. Both groups spoke of the difficulty of encouraging continuation of treatment when patients were struggling with side effects and views were expressed that it can take time and distance from services for patients to accept a need for external support to manage ADHD:
‘I don’t want to take this medication and it doesn’t make me feel alright, I don’t feel great on it, I don’t feel myself on it, I feel dulled down on it’ is often a comment – ‘and I just don’t want to take it and you can’t make me. I’m 16, I’m 15. I’m a whacking great 6-foot kid, what are you going to do about it?
Paediatrician 11
When you are thinking about young people, there is a tendency to (a) just want to be normal like everyone else and (b) to think well it will all be OK, I’m older now . . . I’ve come out the other side and now I’m going to go out to work and I don’t have to do all that school work anymore . . . it takes a little while before the person finally realises and then is prepared to acknowledge that actually, you know what, I’m not OK and I’m not managing . . . and by then people can be in really serious difficulties.
Adults’ clinician 14
However, patients who had not transitioned but re-engaged with services as young adults expressed a great deal of regret about their involvement in decisions. They reflected that, at the time, they thought they knew best, but wished that their consultant and/or parent had pushed harder for continuation of treatment and service engagement:
The clinician didn’t ask me why I stopped. If I knew what I knew today then I would never have stopped . . . I did not cope at all. I really struggled. And then obviously now with all the trouble that I’ve got now it would have been so much easier if I’d just moved naturally over to the adult ADHD. But I knew best.
Re-engaged young adult patient 14
It’s just that I didn’t feel that they were pressuring me enough to stay with them. After I said I don’t want to be with them they were like, ‘All right, fine. We can’t really force you’. They didn’t really force or, say ‘It will be beneficial for you to stay’. My mum was chatting but I wasn’t really listening. I was 16, 17 . . . Well, I assumed I was a big person. I know what’s right from wrong but I didn’t realise that I actually did need that service as I need help and now I realise that this is what I need.
Re-engaged young adult patient 20
All stakeholders expressed a frustration over the medication focus of commissioned ADHD services. Clinicians recognised the need to provide psychosocial support (e.g. life skills, coaching and psychological therapy) and include those who are unhappy to take or are refusing medication, but typically this was not available:
Unfortunately, medication has been at the moment the only reliable patch, for want of a better phrase, because I’ve not been able to get anywhere with any form of counselling.
Re-engaged young adult patient 08
I think we can offer support as far as medication goes. There’s nothing else. And I think that’s really poor . . . If they don’t want the medication, they can be passed back to their GP and then it would be up to the GP to refer them into adult mental health because any kind of talking therapies or any of that would have to come from them . . . Things like parent education and teacher education, which is so desperately needed, doesn’t exist here. ADHD equals Ritalin [Ritalin®; Novartis Pharmaceuticals UK Ltd, London, UK].
Adults’ clinician 12
I mean to be fair with ADHD normally the hyperactivity has settled down by [transition], the impulsivity is there to a certain extent, it’s the disorganisation that’s a big problem and the emotional dys-regulation and also the emotional consequence of going through school having to take medication because of behaviour and struggling with social relationships, some of these guys feel quite isolated, quite angry, they’ve got very difficult family circumstances often as well. And so actually that becomes the bigger problem which medication doesn’t normally deal with anyway.
Paediatrician 05
Many of the young adults interviewed had actively sought out interventions such as cognitive–behavioural therapy, group or individual counselling, animal therapy, restricted diets (i.e. avoiding certain foods), exercise or meditation, or had tried cannabis as an addition or alternative to medicinal treatment with varying degrees of success. They discussed how the medication focus of services had meant that they had not known what other non-pharmacological options might have been helpful to have sought them out earlier. On re-engagement with services, they wanted a flexible approach to medication in which they could experiment with being off medication without losing support. They strongly expressed views that medication and mental health support were separate, and that psychological support should be available for adults with ADHD who are off medication:
So, it’s only from getting the help that you realise that you needed it, in a way. So loads of things changed for me: my behaviours and relationships, everything. It had a huge impact on me, having that CBT [cognitive–behavioural therapy], but I wouldn’t have known how much impact that had before doing it, if you know what I mean? And it would’ve been nicer, it would’ve been better to have that CBT or something a few years ago.
Re-engaged young adult patient 13
But some people who don’t like to take the pills I reckon they should at least get some . . . psychological help. Like going to a therapist. Getting trained how to not to go to those urges, like fidget or think before you speak.
Re-engaged young adult patient 05
I said I still want help. I don’t want this to end. All because there’s no medication, I don’t want this help and support to end because it is good.
Re-engaged young adult patient 16
Parents wanted services to help their child learn appropriate strategies for managing ADHD as an adult. A need recognised by some adults’ clinicians, who described undertaking specialist training or joint working outside their limited commissioned services to provide a service to better meet patients’ needs:
I want him to have some help to understand how he can sort himself out and how he can control it himself. There’s only so much I can tell him or he can find out himself . . . driving, going into the workplace and getting some more qualifications is our next stage. So yes, consistency and someone to actually help us manage his ADHD in the next few years.
Parent 05
I’ve been working with somebody that’s got a diagnosis that didn’t want to take medication . . . I worked with her just to do some awareness with her and her mum round the symptoms regarding ADHD . . . she didn’t want to take the medication because it didn’t agree with her and she felt it made her worse so we just worked on how she could manage her symptoms. Me and my colleague . . . went on some CBT [cognitive–behavioural therapy] therapy for ADHD . . . and through that we’ve been doing informal CBT stuff.
Adults’ clinician 07
Ours is more medication and if we can, we use other services . . . The CPN [community psychiatric nurse] has got CBT [cognitive–behavioural therapy] expertise so she will give that . . . probation can offer life skills . . . The OTs [occupational therapists] will do the normal OT [occupational therapy] . . . Accommodation issues will be the social worker will deal with that . . . we’ll just filter them to whoever can help. Generally, we’ve found it’s worked but sometimes we get stuck with very difficult cases, how to handle.
Adults’ clinician 08
Parent involvement
There was a shared belief across different samples that parent involvement supported transfer to adult services. Reflecting difficulties associated with ADHD symptoms, parents (typically mothers) continued to take an active role in adolescent and young adult patients’ engagement with services and treatment. They arranged, transported and accompanied patients to appointments, explained information provided by clinicians and advocated on behalf of patients, ensured that they ate and washed, as well as helping them to learn and implement coping strategies:
I’m there when they make the appointments, but my parents will make the appointments, my parents will do the prescriptions.
Pre-transition patient 09
I usually sort everything out for him.
If he’s got appointments one of us goes with him . . .
Yeah his memory is so poor he don’t remember nothing. So that has to be done for him because he just wouldn’t . . . And spending an hour or so in a car with [son], is a complete nightmare I’ve got to say. It doesn’t matter who takes him, whether it’s a taxi, whether it’s you. He will just flip at the slightest thing.
Parent 20
Because often these kids with ADHD . . . actually still need quite a lot of guidance and with their organisation by their parents so that their parents are more actively involved than routinely.
Child and adolescent psychiatrist 07
Medication management was particularly highlighted as a role parents adopted: sorting prescriptions, observing effects of medication trials and ensuring adherence. Although, as already described, patients were considering short-term goals, the parents that were interviewed perceived an ongoing need for support, with most viewing medication as beneficial to support their child and the wider family:
I have to keep a track of whatever she is taking, the medication. She’s not very good at taking medication . . . because she’s now a young person who is busy out with friends and staying out, she’s not very good, so I need to keep track of her from that perspective.
Parent 03
Do you think her symptoms or the effect that has on her, do you think that will change as she becomes an adult?
No.
You think it’s always going to be there?
Yeah. The thing is when she first got it, I got told ‘Oh she’ll grow out of it’ and I know adults with ADHD so that didn’t make much sense . . . I think in a way it’s learning to live with it. And some things I think she’s doing very, very well in and other things I think we’re going to have to keep an extra eye on that.
Parent 17
I don’t think there’ll ever be a time when he’ll be able to control it to that level. That’s what it is. It’s like an Incredible Hulk . . . That’s all I can explain to you. Until you’ve been through it and experienced it, and seen somebody kick off, and think that’s your child and he can be that nasty, and that angry, and that vicious . . . the main thing in his life that he needs is that little white tablet. It sounds pathetic, I know, but he needs that, and we need him to have that, for our sanity as much as his own.
Parent 07
Parents felt that an emotional immaturity associated with ADHD meant that there was a greater need for continued parental guidance into adulthood. They also suggested that, because of the ‘fight’ required to access and retain health-care support, parents’ drive to overcome obstacles was required during and after transition to see their child fulfil their potential:
[Child psychiatrist] wanted [son] to take kind of ownership of it and responsibility for it. But because of the nature of his condition even when he wants to take responsibility for things they don’t get taken responsibility for . . . he doesn’t see that he needs to take medication almost daily to just get on with tasks that other people don’t even think about . . . I think at some point they kind of need to acknowledge the limitations of the condition to access the service independently like an adult.
Parent 15
Do you know what you would do if you couldn’t get the help you needed for [son] once he’s turned 18?
I would make a big . . . I would just go and sit there, because I’m not willing to get to the stage where he’s not allright. But then you do feel bad doing that and you do feel like you are sort of overstepping the mark. I think we learned quite early on that sometimes thinking that everything is being dealt with and they are busy and you are waiting your turn and they’ll get in touch, it’s not always the case.
Parent 14
This ongoing active role of parents was also recognised as essential by young people who transitioned:
I’m at that stage in life where I’m perfectly capable of looking after myself, I can cook for myself, I can cook, I can clean, I can do all my washing up. But because my brain works at 50,000 miles an hour, I find myself so mentally exhausted from existing that I wouldn’t manage without her looking after me. It’s not that I’m not capable, it’s just that I don’t have the energy in my brain to even consider starting to do that sort of stuff. My mum has always been very involved.
Transitioned patient 01
I wouldn’t have [moved to adult services] myself because no matter how much research I do, I’m not good at confrontation and that is all that tends to happen with my experiences with mental health care. I normally just give up at the second hurdle because I know from my experience it never works properly.
Transitioned patient 21
Parents and clinicians in children’s services expressed concern over differences in care models between child and adult services, notably, a lower tolerance of missed appointments and loss of direct communication with parents in adult services:
I think the issues of transition for our kids would involve the concept of sort of family-based support which would be different from adult psychiatry . . . I think we see quite a lot of problems when individuals are seen just as individuals not in the context of those who have been supporting them up to then.
Paediatrician 16
So, I’m sending him in to see this person. I’m waiting in the waiting room, because he doesn’t like going anywhere on his own . . . he’s in there and I’m going, ‘What have you talked about?’ And to be fair, he didn’t really want to talk about it. Basically, nothing . . . My son has gone off the rails a bit and once this 18 months is up, I’ve got no control . . . no one gets it. Unless you are bringing up a kid with this problem, no one gets it and all they think is they are an adult, it’s up to them and they [adult services] won’t speak to me anymore.
Parent 23
In CAMHS we will tolerate a level of disengagement . . . still prescribing and seeing them when we can . . . but not having a massively engaged discussion with them . . . we tend to do that via parents or carers. Whereas in adult services that isn’t tolerated . . .
Child and adolescent psychiatrist 08
However, the adults’ clinicians interviewed recognised the importance of working with families and described welcoming parent input (e.g. arranging and attending appointments to support patients), as long as the patient assented. Attaining assent for continued parental involvement prior to the first appointment was acknowledged as a challenge, as was negotiating with families and communicating with patients who were used to parents taking the lead:
When they come to us, we welcome families but it’s entirely up to the young person to make a decision about this . . . We would not automatically send the clinic letters to parents; we send them to young people. This is all-round difficult.
Adult clinician 04
My experience is if the parents are still involved, the transition is often better, smoother, because the parents remind them to take their medication and if they’re ‘good’ parents I think that they learn to take themselves back . . . give more remote support . . . But then there are . . . parents . . . who are really overprotective and don’t let their children go, or can’t let them go, and this then creates problems for those who just pull out because they have enough.
Adult clinician 16
As I say, it depends if they are invested or not, because that’s the hardest thing. When you get them come in and they’ve got their hoodies on and they’ve got their earphones in, or they’re on their phone and they grunt at you, it’s really hard to get them to engage with you . . . I think paediatrics and CAMHS service are very much led by the parents, so all of a sudden, they’re an adult . . . and I’m directing my questions to them. They really struggle with that sometimes . . . it’s trying to get the parents to loosen those reins a bit as well. You have to be very diplomatic . . . especially around medication, really difficult. The young person possibly doesn’t want to be on meds anymore and the parents say, ‘If you are not on your medication you can’t live with me’.
Adults’ clinician 15
Clinicians and parents noted that some parents may be better resourced than others to advocate for their child’s need for ongoing support. A number of parents expressed a view that they would be prepared to ‘go private’ to ensure continued access to support:
There’s a group of kids for whom they have challenging amounts of dopamine transition, but they have a fantastic family, a fantastic neighbourhood and a really dynamic school and actually it comes out as all positive. Whilst if you put that same kid into a dysfunctional family, in a dysfunctional area, in a dysfunctional school it would be all negatives.
Paediatrician 21
Because I work with special needs kids I understand a little bit of the educational side of the system. A lot of people don’t. Some of the parents that I’ve worked with, they haven’t got a hope because they don’t understand the system, they don’t understand what their rights are or where they need to go for help or what to do and haven’t got it in them to be pushing.
Parent 18
Preparation for transition and adult life with attention deficit hyperactivity disorder
Patients reported different levels of readiness for the transfer to adult services. Some felt ready for and welcomed the change in care model and environment, others were overwhelmed by it and saw adult services as less caring, and others were ambivalent. For those who felt ready, they reported being pleased to be more involved in their ADHD management, feeling listened to and taken seriously:
In the child ones I feel like they’re more accommodating to your needs a little bit more. A little bit more like ‘How are you going to cope with your exams? Have you spoken to your school to get extra time?’ But I feel like in the adult one it’s a little bit less, it’s like you need to just find out for yourself kind of thing.
Transitioned patient 05
When I was in CAMHS, that was more them telling me what to do rather than listening to me, so I felt more understood in that appointment with the doctor there in adult services and I felt like I was in a bit more control which to me was good.
Transitioned patient 21
The importance of patient familiarity with adult services before transition was described by a number of interviewees across sample groups; however, the experience of preparation for transition and for adult life with ADHD was varied:
I describe ADHD as trying to pay attention to everything at the same time. And if you’re doing that in a completely new place where you don’t know anything, that’s exceptionally overwhelming, I completely shut down, I feel incapable . . . Just getting to go in there and just seeing it, even if I didn’t have an appointment with someone, even though I just spent 10 minutes sat in the room that would be such a massive help.
Transitioned patient 01
I know from the adult services that some of our people we do refer just don’t attend. That’s why we hope to get this new thing going where we meet . . . a sort of joint appointment . . . because they’ve been very used to us, often for very, very many years and it’s a big jump to meet someone new.
Child and adolescent psychiatrist 01
It’s still a bit hit and miss . . . 60% feel well prepared and that they’re adequately experienced, 40% of people say that they didn’t know about what they’re supposed to know . . . what’s supposed to happen, which is not happening, is that our CAMHS colleagues or paediatrician colleagues start preparing people for that transition process and explain about how adult services work in a different way and, potentially, start that graded reduction of input. So, we are probably not doing that very well . . .
Adults’ clinician 02
Patients in group 1 (pre transition) knew little about transition; they may have been informed about a potential future change of service provision but could not recall it. Experiences of group 2 (post transition) were mixed. Some described feeling unprepared for using adult services, whereas others described feeling informed about the transition process and had attended a joint meeting with their new adults’ clinician. Some interviewees reported that clinicians in children’s services described their own reservations about the limits of adult services to patients. Patients who felt informed about what was going to happen reported that their transition went well:
I didn’t get told about anything; I didn’t know there was any support for adults. And all I heard about support for adults is no doctor really wants to do it, because there’s no money in it.
Re-engaged young adult patient 05
We had a bit of a bad experience with one who was expecting the same service as they were getting from us . . . And they were quite irritated that they didn’t and now I’m making it clear to patients that these guys will not look at your ASD, they won’t manage that side of things . . .
Paediatrician 05
How did you feel about changing?
Alright. Because they prepared me before. It’s not like I came one day . . . ‘Where’s everything gone?’ At least I knew what I was going on, instead of walking in, not knowing what’s going on.
Transitioned patient 17
Parents of pre-transition patients typically did not know at what age transition would occur. One parent had assumed child services would continue to provide support until the end of full-time education. Another assumed CAMHS went on indefinitely and reflected that discussion of transition and remit of services needs to be repeated and reinforced with patients and their families over time. Other parents reflected on their inability to help prepare their child for the move to adult services when they are not themselves informed:
It didn’t really dawn on me that they’d get passed onto just the mental health team. And or I suppose maybe it goes back to his GP . . . they probably have gone through everything that you’re asking, if I knew what they’d said to me, if it had made sense when they first told me, I may have retained it but you just don’t retain it because you’re at the beginning of all this other stuff that you’re thinking ‘Oh right, so what I’ve got to do, I’ve got to get an appointment and then there’s this type of medication, that type of medication’ and you forget that they say ‘He will only be with this team until he’s 18 and then we’ll whatever’.
Parent 15
What do you think the best or the worst things will be about her leaving CAMHS and going on to another service?
Well, the fact that we don’t know what that other service is. It’s this thing called adult services. What is it? It’s like something out of an Orwell novel. What is it? We’ve had no information, we’ve had no contact. In the meantime, she’s going through a really vulnerable time of change. She’s potentially going off to university in a month or so. Where’s the support? What happens if it becomes too much for her? Who does she turn to? There’s just nothing. I’ve said to her, ‘We’ll just have to go private’.
Parent 01
The interviews with patients who had re-entered adult services without transition (group 3) highlighted a need for clearer information for discharged patients about what to do if symptoms deteriorate and support is required. Those who dropped out and re-entered services and those who had been on waiting lists for adult services described information about how to make an appointment and where to get medication, in case difficulties develop, as essential:
So, what might have helped before we decided to drop out, [is] if they gave us some information for later on in life . . . because obviously no one can predict the future, so you don’t know what’s going to happen around the corner. So, it might have been just nice to give a heads up of what we could do if we really found an issue.
Re-engaged young adult patient 06
If I was saying to a 16-year-old, ‘You need to find out. Don’t stop child services until you’ve got the next step forward’. That would be my big thing.
Re-engaged young adult patient 18
Although some clinicians in children’s services described providing this information, others acknowledged that it could be limited, with patients simply directed towards their GP if support is needed in the future. The limited nature of this information was also the experience of parents:
Do you talk to them about what happens kind of later on in life or a few years down the line in their mid-20s if they decide they need more support? I probably would, but it probably wouldn’t be a lot more than saying ‘You’re off your treatment now, I hope everything goes well, you need to go back to your doctor if you wanted to talk about this again’.
Paediatrician 14
They said ‘He’ll be fine and he’s managing’ and at that time I didn’t even think that if we need to come back, where do we go? I thought maybe because he’d seen the group, he will automatically [get] transferred to that route if ever needed . . . So I just assumed that OK fine, maybe he’s got the gist of it how to handle himself.
Parent 25
The accounts of patients, parents and adults’ clinicians consistently indicated that children’s services had provided limited or no information in relation to ADHD as a long-term condition. Some adults’ clinicians reported being surprised by patients’ (and parents’) rudimentary knowledge of ADHD when they first attended adult services appointments. They also reported that young adult ADHD patients are often troubled by a negative perception of themselves as stupid or lazy:
Did anyone ever talk to you when you were 15/16/17 about what to expect with your ADHD over time? No . . . It was all about the now. It was all about what’s happening on this day, that day.
Re-engaged young adult patient 16
What I find most shocking is that when you ask them what is ADHD and what does that mean to you they have no idea . . . And they say, ‘I’m just bad, aren’t I?’ or ‘I’m worthless, I’m useless,’ . . . they don’t actually understand what ADHD is . . . what we’ve tried to do with all our service users with ADHD is for them to become their own experts in ADHD. So if they have a better understanding of what ADHD is and how ADHD affects them then they are more likely to be able to feel they have more control and put stuff into place. But a lot of the youngsters that come have no idea.
Adults’ clinician 15
Reflecting the discussion in Education, interviews with patients and parents suggested that, instead of discussions of possible long-term needs, they are commonly told that ADHD is a condition one grows out of:
Well I rang up CAMHS and they said ‘Well he’s 18’ well I never knew nothing about that because you weren’t really given any information . . . I saw a lady at CAMHS first and she said ‘Well he’s 18 so there’s nothing really we can do’ and told him basically to grow up, it’s time he grew up.
Parent 20
The way it’s put across is basically you’ve got this condition that means you act in a way that is unacceptable by society, therefore you need to take this drug that is going to change who you are to make you fit in to the way that we think you should be. Every kid that I’ve spoken to with ADHD does not know what it is.
Re-engaged young adult patient 02
Parents felt that it would have been helpful if clinicians had explained the restrictions that ADHD medication might have on specific employment. A particular concern across all interviews was unanswered questions about the effects of long-term use of ADHD medication:
One thing that I wasn’t aware of until just after the medication started though was perhaps possible effects of employment, like police and joining the military . . . it would have been useful to have known that.
Parent 22
Not knowing what the long-term effects are. That still bothers me now. It’s an issue that I’ve got now. I’m on a very low dosage at the moment and I try my hardest not to take it when I don’t have to.
Re-engaged young adult patient 02
This expensive drug, it’s a drug of abuse, is this something people are going to take lifelong? It seems like some kind of guidance is needed, otherwise it just sits on our record and they carry on the medication. It seems a bit open-ended.
GP 11
Many of the young adults in group 3 believed that a better understanding of ADHD might have prevented them from dropping out of services. Some described the shock they felt when they found out ADHD was a long-term condition:
So I do feel I just need to be generally more informed about ADHD, about the services that are on offer and that would be much more useful to me, because now . . . well I do accept, with some resentment, that this is something that I will have to deal with for the rest of my life, so if that’s the case then I want to be as prepared as I can be.
Re-engaged young adult patient 07
I explained to [consultant] I didn’t really understand why I was having these issues . . . I kept saying to him, ‘I know I’ve got ADHD, but I’ve grown out of it. I did really well at college’, and all this. He just said, ‘ADHD is actually a lifelong condition but people tend to grow out of the hyperactivity side of it, or it fades away a bit, but there are actually other things that you will struggle with as a result of attention deficit disorder’. That was horrible. I got really upset. I started crying in his office because to me I felt like I’d overcome a massive barrier in my life and then to be hit with the fact that, oh actually, no, this is something that you are going to have to deal with for your whole life.
Re-engaged young adult patient 02
Clinicians in children’s services reported presenting ADHD as a long-term condition, but many acknowledged that their practice could be improved. A few referred to uncertainties about ADHD diagnosis, which may make clinicians cautious in presenting ADHD as a long-term condition:
I was seeing cases that were 17 and a half where there had been no discussion about what was going to happen to them in adulthood . . . But now I’m having those sorts of conversations from a very young age and I find it interesting for those that are on medication when they’re 13, they start wondering are they going to be on it for a long time? And they start “kicking off a little bit and saying ‘I don’t want to take it’”. So then I use the opportunity to have a discussion about ‘Okay why are you on this medication? Are you going to be on it for a long time? And if not, what are the alternatives?’ . . . I take the opportunity to talk about the long-term consequences of ADHD.
Paediatrician 05
I suppose what I’m trying to say is that for something like ADHD where the diagnosis has a whole lot of subjective socially bits coming into it . . . We can have this conversation, it’s not like me saying ‘You must carry on with this insulin for the rest of your life, you might benefit from this now, but you might not we don’t know’.
Paediatrician 14
A lack of dedicated appointment time for preparation for transition was highlighted as a barrier to transition. One clinician described how their current information technology system does not flag when a patient is approaching transition, which affected their preparation:
Some of these families are just moving from crisis to crisis and the appointment is spent more trying to support them through the crisis or specific difficulty, meaning that there’s less time to talk about transition or plan the transition. I think my personal practice at present is that it’s been quite late.
Paediatrician 20
In your opinion do you feel like transition is working quite well in your trust in your area?
I don’t think so because I think a lot of people aren’t thinking about it. And I can understand that. You’ve got long waiting lists, you’ve got more patients really in theory than you can handle . . . It’s not going to be sitting in your mind all the time to look at their date of birth and work out exactly how old they are . . . With our clinical commitments at the moment, we’re two and a half consultants down and that’s probably the same with everybody. The clinical workload is huge and you keep thinking ‘Right I’ll do that next month and I’ll do that at the weekend’ and then something else comes up.
Paediatrician 12
Adults’ clinicians typically placed responsibility for preparation for transition on clinicians in children’s services and speculated that a lack of preparation reflected a lack of knowledge of adult services; however, some felt that familiarity with adult services could happen after transition rather than before. Some clinicians in children’s services thought that adults’ clinicians were better placed to discuss ADHD in adulthood:
To be able to do transitions of children’s ADHD cases into our service [would] have basically been a different clinic each day just doing transition clinics, not doing the actual work of people who are waiting for a year anyway. So, we need to sort of focus. We can manage that expectation at the first appointment, say, ‘This is what our service provides, this is what we are going to do’.
Adults’ clinician 05
The people from adult services who know what more of the challenges are in adult life, because we tend to forget about some of those. We do ask about drugs and alcohol and whatever else you are doing but we probably tend to forget a bit about . . . actually really possibly working as a steeplejack isn’t the best idea in the universe if you have got ADHD, that sort of thing.
Paediatrician 11
Clinicians and parents described a need for better information to be provided about adult services and ADHD in adulthood. The need for this information to be in an accessible format for young people with ADHD was emphasised:
A psycho-educational process where they are prepared to either look at some information, material, or attend educational sessions around the ADHD . . . that would be useful in terms of preparing them for adult life and what ADHD could mean in adult life.
Adults’ clinician 13
We don’t have a website, adults don’t have a website. Our young people . . . they look a bit horrified when you hand them booklets these days. [Laughs.] They all want to go online and Google [Google Inc., Mountain View, CA, USA] it and stuff like that . . . They generally do want to just look at a picture and go, ‘OK, that’s Doctor So-and-so, that’s who I am going to see for my ADHD meds’. . . . We would love there to be better written information for the young people as well, for them to kind of take away and digest and look at.
Child and adolescent psychiatrist 13
I don’t think [son] would look at anything. I don’t think he’d care enough to read about it. He’d watch a video. If there was a little YouTube video [YouTube, LLC, San Bruno, CA, USA], or if somebody came to talk to him that had been through it, again a mentor system, so somebody could say, ‘Right, this is what happened to me. It might not necessarily happen for you but it might be similar’. I don’t think he’d bother to read anything.
Parent 26
Architecture of services
The interviews showed that, even if invested in continuing ADHD treatment, transition outcomes depended on whether or not a patient’s needs ‘fitted’ with how local adult services were structured. As discussed in the Mapping Study, a wide variety in configuration of adult services was reported by interviewees in this qualitative study. A few areas had specialised ADHD services but, even with specialist services, gaps existed in what was provided and who could access it. Clinicians largely described transition protocols as being recently introduced or a work in progress. Existing transition protocols had varied elements, including ring-fenced budgets, fast-tracked triage assessments, joint clinics or a named individual responsible for transition:
I mean, you hear things on the news about postcode lottery and other little key phrases that are bandied about but somehow you don’t actually think it’s true . . . I was a little bit horrified that there aren’t any adult mental health services in [local area].
Parent 11
You said the transition protocol at your service is in progress. Is that specific to ADHD or is that just a transition in general? Transition in general. There is now a newly appointment lead for transition within the children’s unit or the trust, as it were . . . So yes, it’s very much in progress at the moment.
Paediatrician 02
For transitions, I’m glad to report that they are usually seen within 4 to 6 weeks in all areas because there is a budget allocated specifically for transitions which we ring fence . . .
Adults’ clinician 13
However, having a protocol did not always make transition a smooth process. How accessible a service is, the remit of services provided and handover practices were identified as interlinked factors influencing transition. Although some clinicians reported having clear shared care protocols with primary care, the interviews revealed that GPs can end up in a care co-ordination role by default during transition and their role is discussed further below.
Accessibility
The lack of equivalent adult service to which ADHD patients could be transitioned was highlighted as a barrier to transition. Many interviewees reported a lack of adult ADHD service provision in their local area, with one clinician in children’s services describing it as:
. . . almost like winning a lottery if you’re actually seen and something was done about it.
Paediatrician 15
Well we have a transition protocol that involves a structured interview through the clinical nurse specialist service and then of course is the issue of what do you transfer to? We have a process of addressing specific issues that are relevant to a certain stage of life, but we don’t have a transition process to a specific adult service.
Paediatrician 16
There’s not really a lot out there for adults with ADHD . . . because a lot of things with ADHD you can grow out of with age. So, I don’t know if a lot of people just have that perception of when you turn 18 everything goes away.
Re-engaged young adult patient 07
Finding who could support him in terms of the life skills stuff that he needed to know . . . was quite hard . . . I again, haven’t got anyone medically, apart from the GP that I can transition him over to . . . You can do transition, you can try and empower the young people and their carers but if you haven’t got people engaged within adult services or services commissioned within adult services to be the other side of the transition then I think that is more of a challenge.
Paediatrician 09
Both clinicians from children’s services and GPs reported that it could be challenging to find the appropriate service(s) to which to refer patients with ADHD. No local provision could mean no transition, or long delays while funding was sought for services outside the CCG region:
OK, have you encountered any real difficulties with transitioning them?
Only the practicalities of knowing who it is . . . every single time somebody was too old to come back to see me, there would a question of asking the GP who the right person locally is and they would normally suggest somebody who would turn out to say ‘No it’s not me because I don’t cover that area’ or ‘that’s not me because this young person doesn’t have a learning disability’.
Paediatrician 14
Generally, with ADHD we just get stuck to know where to go next . . . I have done a little bit of phoning today actually to try and get hold of the mental health teams for adult services to find out if there has been any development but I have just been passed around between four different people this morning and didn’t get any answers and there’s nothing on the websites for our local services about any ADHD clinics . . . I think we all find it difficult to really know what’s out there even within the children’s services let alone the adult services. So, I’d say no we probably don’t do that very well because we don’t actually have much information about what is available.
Paediatrician 19
We cover a massive area. And we also have lots of people from out of areas . . . [One neighbouring area] doesn’t have any adult services and every time anybody from [there] is actually referred to us and is declined, which makes me wonder what on earth happens to all the children in transition, where do they go?
Adults’ clinician 15
Lack of local provision also meant further to travel for appointments and for medication. Travel was highlighted as a challenge for ADHD patients, with young people reporting that without their parent’s involvement they would struggle to attend appointments. Complicated or time-consuming travel requirements to access services could, therefore, affect engagement with services:
I’m hoping to get transferred to ‘Place Y’ because ‘Place A’ [where the young adult is currently registered] is quite a lot to get to monthly for me while I’ve got a full-time job.
But they didn’t do an adult service then?
No. It stops at 18. He’s now referred to ‘Place A’. [Patient] Oh it’s too far. [Mother] We went once and the journey was just horrendous. We are going again but we’ve got someone taking us . . . But we will then have to go to ‘Place M’ to get his medication. Well that’s another journey.
How long is that to get to M?
That’s over an hour.
Transitioned patient 21
I was in college. I had just started college and I thought I was doing really well . . . I don’t need it, I hate the constant appointments, because I used to have to travel to [place] for my appointments. It was getting a bit too much and I was like, do you know what . . . I’ll be absolutely fine and just stopped the medication. Rung them up and said, ‘Look, I don’t want any appointments anymore, I’m going to do it by myself’.
Re-engaged young adult patient 14
I think the fact that our service is less able to go out, to as many sort of geographical locations, so people are having to travel further, and I think we do quite a lot of people at that stage because yes, having been to quite a local clinic to see someone they know and then realising they are going to have to travel quite a distance to see somebody new.
Adults’ clinician 06
In some interviews, clinicians in children’s services also described a reluctance from young people to be referred to AMHS and having to tackle stigma associated with mental illness with their patients. A few parents also questioned the fit of ADHD with mental health services:
The kids would obviously say, ‘I’m not going to go to where all the nutters go’ . . . I would spend hours trying to persuade this healthy, normal, mentally healthy young person with ADHD or autism that they had to turn up to a transition clinic in the loony bin. It may have been grossly untrue but . . .
Paediatrician 21
It’s a bit daunting . . . like someone had obviously graffiti or something on the wall. It was a bit like . . . and then there was people walking by, staring at you that were being walked about by guards.
Transitioned patient 13
You can see that apart from getting stuff done there’s nothing wrong with [son], he’s very popular. He’s got loads of mates. He’s really polite and patient. So, he’s got loads of good qualities that I think everybody wants their child to have. So then to see him going under mental health where my sister goes, she’s got horrific mental health, it’s really, really bad . . . And so to think [son] is using that same service is a bit odd really.
Parent 15
Typically, patients and parents viewed the accessibility of adult services in a negative light compared with their experience of child services, with concerns reported that adult services were less easy to contact and less flexible with appointments:
I have tried with adults; I rang them obviously the other day and told them to ring me back and they never did.
Transitioned patient 10
What do you think the best or worst things might be about that change into adult service?
If we were to lose what we’ve got now, if we were to lose the communication . . . I think certainly the knowing that [clinician] will always say, ‘If there’s anything between meets and you want to pick up the phone, I’m on the end of the phone’. She makes that quite clear. And I think if we were to lose that, just knowing that they’re there. There’s been the odd occasion where I’ve had to ring for something and they’ll always come back within 24, 48 hours. If they don’t know the answer straight away, somebody will come back, and . . . they’ll offer an extra appointment.
Parent 19
Adults’ clinicians explained that limited time and high workloads meant there were often strict policies in place for appointment non-attendance. Some clinicians recognised the impact of these policies on young people with limited organisational skills, describing how they were adapting practices to respond to patient needs:
The reality is we just cannot have DNAs [did not attends]. We have so little resources to deal with the demand, so if people want to be seen they really need to make an effort . . . if people don’t turn up, we send them an opt-in letter, saying ‘Sorry you couldn’t come but please let us know within 14 days that you wish to be seen again or continue’. . . A lot of people, because by definition we are dealing with disorganised, forgetful population, they would give us a ring and say, ‘Oh yes, I know, I completely forgot about this’ . . . so we would give them another appointment.
Adult clinician 04
If I reduce someone’s medication down, then I contact them by phone about a month later just to see how they are getting on with the reduced dose and then whether we need to adjust it anymore. And that can go on for around four or five appointments and then they come back in for a face to face . . . It just saves them having to keep coming in . . . and we get less DNAs [do not attends] that way because people are more engaging with us and they don’t think they have to give a day up for college or whatever . . . They also know that . . . if they have any concerns then they can always contact me and then I can contact them on the phone.
Adult clinician 15
Remit
Adult clinicians described the fragmented design of adult services in comparison with their perceptions of child services. Interventions provided were often restricted by limited remit of commissioned adult services. For example, a number of clinicians mentioned that their adult ADHD service could not prescribe medication for coexisting sleep or affective disorders:
They don’t have the one umbrella of a service like CAMHS . . . [they] do the ADHD, do the anxiety, do the family therapy or whatever, they come to us and . . . I think that might be a difficulty, that they want to talk about their anxiety as a comorbidity or they want to talk about their low mood, which is fine, we need to pick up on that, but I can’t treat it, they’d need to go back to primary care for that or IAPT [Improving Access to Psychological Therapies] . . . The other thing is melatonin is an issue. A lot of young people come in with melatonin then once they are out of children’s services GPs have stopped it. But we are not commissioned to treat sleep disorders, we are commissioned to treat ADHD, so we’ve been told we can’t prescribe it.
Adult clinician 05
Some people are referred to us with a diagnosis of ADHD but the medication they are currently on isn’t ADHD medication, so somebody coming to us on an antidepressant. And risperidone for aggressive behaviour as well . . . if what they need to do is stay on this medication then unfortunately it’s not a referral that we can accept, because we can’t take anybody, we can’t have people on the caseload that aren’t on medication for ADHD because that’s all we are paid to do.
Adults’ clinician 06
Clinicians described the limited remit of adult services as a shock for patients used to the broader focus of child services. Some expressed views that the lack of joined-up working made it very challenging for patients with ADHD to navigate services. These views were supported by interviews with patients, who found the limited remit difficult to understand:
They are kind of used to just having the one therapist with us and so it is a bit more hard to organise the transition when you are sort of saying you need to go here for that bit and here for that bit.
Child and adolescent psychiatrist 13
A lot of the other aspects of my health are completely separate, well in the NHS are completely separate even though they are not. So, I didn’t really have a chance to talk about much apart from the ADHD and the Asperger’s. [Young person has had anorexia and has self-harmed].
Transitioned patient 21
I did think it was odd that an organisation that’s there for adults with ADHD can’t prescribe my medication. I don’t really think that’s acceptable, because the GP didn’t want to know . . . It’s probably to do with money because it’s quite expensive.
Transitioned patient 09
When trying to find the appropriate service to transition patients to, a common experience for GPs and clinicians in children’s services was the response ‘we are not commissioned to do it’:
We try and refer when they’re adults and then they say there’s no service . . . If there’s mention of learning disability, we’ll give that a go, or if there’s mention of mental health, we’ll give CMHT a go. We’ll see how we can plug these people into a service, but generally that doesn’t really work.
GP 13
Adult psychiatrists . . . are saying they are not commissioned to provide a service for ADHD . . . They are stretching all the services and having to make savings. You don’t have the luxury if you are not specifically commissioned to do something but it’s just not fair on the patients.
Child and adolescent psychiatrist 03
In addition to ongoing medication use, the interviews suggest that eligibility for adult services was based on complexity of need and presence of comorbidities. Higher thresholds for adult services than for child services meant that ‘stable’ or ‘straightforward’ cases were likely to be discharged to GPs rather than transferred to an adult service:
Because we are not urgent because it’s not severe, it affects his life. I understand they see children that are an awful lot more urgent than him, but I think it’s people like [son] that will fall through the net and be left to cope on their own.
Parent 05
He was below the level of illness at the point that he needed transition that would be accepted through secondary services, so then I ended up coming up with a transition plan with his general practitioner.
Child and adolescent psychiatrist 10
Clinicians in children’s services also described getting adult services to accept highly complex cases as challenging. Sometimes the tight remit of adult services could leave those with the more severe and complex problems without a service:
It landed up with me having to write some quite rude letters. I don’t mind that being quoted to say that ‘you can’t leave this child in limbo’. Nobody would prescribe, the GP wouldn’t prescribe, the consultant wasn’t overseeing it. Psychiatry wouldn’t take it on because of the learning disability, social services said his IQ [intelligence quotient ] wasn’t low enough for them to take it on . . . by 19 I managed to sort it out, but it took a lot of hard work.
Paediatrician 12
[Describing a loked-after child with complex emotional needs and conduct disorder] she is one of those that doesn’t fit in anything, any kind of box, but she is massively needy . . . I’ve no idea when I am going to be able to discharge her because I have no way of knowing where she can go, who is going to have the remotest capacity to look after her.
Paediatrician 22
Care Programme Approach (CPA) processes, which include the appointment of a care co-ordinator, were described by some clinicians as administratively burdensome but a need for someone to liaise with other agencies and co-ordinate support for ADHD patients was posited:
CPA is probably underused in children’s services across our trust largely because . . . people don’t feel it adds anything. The young people would get the same number of reviews which are normally held multiagency anyway. So, putting them on CPA is a bit of an admin [administrative] task rather than a clinical task. It doesn’t make any difference to the care they receive.
Child and adolescent psychiatrist 08
We do a lot of screening of those referrals to really make sure that we get this segment of this adult ADHD population that we are commissioned to look after . . . There’s limited funding . . . The idea really is to not provide care co-ordination, so patients who are too complex or too risky . . . who would need a care co-ordinator or involvement of other HSEs. So, we are not staffed to provide the service for these patients . . . So, they then have to go to the community mental health teams and the community mental health teams say ‘No, no, we don’t have a pathway for complex adult ADHD patients’, so they go in circles.
Adults’ clinician 16
The cut-off point for access to adult LD teams was particularly highlighted by clinicians as being difficult for patients, families and services. Although clinicians reported that transferring patients with ADHD and coexisting LD to adult services was typically easier because of established LD services, patients whose LD was borderline fell into gaps between services. Many clinicians in children’s services reported transition for patients with ADHD and autism as similarly challenging, as they would not meet eligibility criteria for adult services:
There’s a subgroup of those with ADHD who have borderline learning needs who have quite a lot of social deprivation . . . We were clear that they needed adult services input because there were ongoing needs for post 18, but we’ve struggled to get them accepted by adult services . . . so their IQ [intelligence quotient] is hovering around 70, so 71 or 72, so they’ve got significant learning needs . . . [but] adult learning disability services won’t take them because their level of functioning is too high . . . but our general adult effective team really struggle to take these young people in, because they’re well below their normal client functioning. So, these kids really fit in a bit of a between the two.
Child and adolescent psychiatrist 08
Sometimes it’s not appropriately sent to us because sometimes they’ve got a lot of LD as well and it may be more appropriate for them to be actually referred to a community adult LD service, but I’m also very aware that there’s a really hard criteria for them to get through and that can be problematic for parents as well, especially if you’ve got someone with LD who has got ADHD and is also extremely aggressive.
Adults’ clinician 15
So that would be a big, big, a big issue, is that we have a few who are ADHD and ASD and, yes, like I say, they probably need a wee bit more support but don’t quite meet the threshold.
Child and adolescent psychiatrist 13
As with learning disabilities, interviewees reported that a psychiatric comorbidity could potentially make it easier to have a service to transition to. However, they noted that adult mental health teams may be configured to manage episodic illness rather than long-term conditions, such as ADHD:
It depends what their other needs are. If they’re hitting 18 and they’ve only got ADHD and they’re off their medicine, then that’s probably them done. But if they’ve got secondary mental health needs then they’d stay in the service for those needs . . . But there’s no one to hand them on to if they don’t have very clear defined mental health needs.
Child and adolescent psychiatrist 08
Adult services are very much moving towards episodes of illness and whilst you are poorly you are seen by psychiatry and then you will be discharged, whereas there’s still a fair bit of monitoring of well people that happens in CAMHS and that can be tricky.
Child and adolescent psychiatrist 10
Clinicians reported that ‘pure’ ADHD without any comorbidities is not that common in routine clinical practice. Many expressed a view that highly specified teams create gaps in provision for patients with complex needs. The varied needs of patients with ADHD led some to suggest that a specific ADHD transition protocol would not work as there would be no adult service that would suit all:
I have been around in the NHS for a long time and my experience is that when . . . someone is looking after one arm, another person is looking after another arm, left ear, right ear . . . it creates gaps and this is what is happening . . . I think locally mental health services are restructuring again, constantly restructuring . . . What happens when people have comorbidities, its mind blowing, and I think it’s actually a problem with then creating more gaps.
Adults’ clinician 04
I am dreading him . . . changing over services, because I know what mental health services in [local area] are and I know how awful they are at the moment . . . I work in the field. I have to battle to get my service users mental health services . . . I have had to sit at A&E [accident and emergency] for 7 hours . . . waiting for a psychiatrist because we haven’t been able to take him to an appointment because they won’t take him onto their books because he doesn’t fit into any of their boxes. He doesn’t fit in the memory clinic, he doesn’t fit this clinic, he doesn’t fit that . . . and they just kept on shunting him over until he became so acutely unwell, and I am not looking forward to that for [son].
Parent 28
In some ways it’s positive that an ADHD service was set up and commissioned but in other ways it’s actually unhelpful because people would have been seen in general services . . . but now because they all get signposted in the ADHD service and everything gets attributed to ADHD they sometimes get less response in this service because our service is so overwhelmed and such a wait.
Adults’ clinician 10
However, this did not mean that access to specialist ADHD staff was not welcomed. Across the interviews, specialist training and increased competence in working holistically with presenting difficulties was deemed important:
It’s absolutely vital to have support that comes from a knowledge of what ADHD is really, because lots of people think they know what ADHD is and astoundingly in some cases know either almost nothing or have an entirely erroneous view of what it’s all about and that really can cause a lot of problems. So, it’s really important for people to be properly trained and have knowledge of what ADHD really is and what ADHD isn’t.
Adults’ clinician 14
He’s got social, emotional problems and behavioural and learning difficulties . . . I think it all comes into one circle really. I mean, you could find something that would help them out for one thing but then another thing would come in and you’d have to find another way to work with that as well.
Parent 09
I think that’s a problem with mental health nursing across the board, because although we’re expected to work with people with dual diagnosis, we don’t, really . . . we really don’t work with many people with ADHD and mental health. Sometimes we do a few with Asperger’s, and autistic spectrum disorders, but . . . I think that’s a competency issue across the board for mental health nurses, that actually, we don’t do it enough to be good at it and recognise it, and then what we do is we try and shoehorn a set of symptoms or presentation into a mental health diagnosis that feels comfortable, which is why we get the emotionally unstable personality disorders, and why we get the conduct disorders.
Adults’ clinician 01
Handover practices
Adults’ clinicians reported that their experience of handover of patient information from child services varied. Although detailed patient information could be provided, handovers could also be very limited:
Some clinicians are really good, they would phone us and we’d say, ‘OK, send us all the relevant information, documents, reports, whatever, from your clinic’ and they would do it, but very often it’s requesting some information, not getting it.
Adults’ clinician 04
So, the paediatricians write us a letter, at usually [age] 17.5, which will say ‘this person has got ADHD and they’re on ritalin’. It’s always the same. There is no indication of how that was diagnosed or when. Well we try and get hold of their notes but sometimes they’ve either been archived or they’re on a different site and they’re medical, they are not mental health, so we can’t access it which is really unhelpful . . . What we end up doing is set out in the NICE guidelines, the architecture is we have to kind of reassess them really, do a full history.
Adults’ clinician 12
Having access to the same case files and using the same paperwork as child services was a reported facilitator to transition. Access to up-to-date patient information was challenging if referrals were from different health trusts or there was a lack of patient engagement prior to transition:
We’ve got the same electronic health records, so we can access that. We don’t access the paediatrician stuff because they are in a different organisation . . . it helps especially with transition . . . I get a bigger picture before seeing a person of what’s been presenting, so that’s helpful, whereas . . . liaising with CAMHS or whatever or phoning them up . . . I wouldn’t have time to do that for every person, so I just wouldn’t do it.
Adults’ clinician 05
For people that are not exactly from our area, to get any information it’s close to impossible . . . it’s kind of very brief, or there is absolutely nothing apart from ADHD being mentioned in a letter, sort of random letter. So, information is not very easily obtainable, and this is what adds to the pressure because we would have to really assess someone to know what is happening and what is the impact on someone. It’s not easy.
Adults’ clinician 04
I think the faces of the people that have had a child in the service from the age of five, when they come in and I say, ‘I’m going to be honest with you, I’ve got this one piece of paper’, they are really quite shocked by that . . . I think, ideally, we would like the last appointment with the previous service to have . . . [provided] an explanation about the service that they are going on to and also to have a final assessment . . . some people get referred having not attended their last planned appointment . . . And that’s really difficult.
Adults’ clinician 06
Limited or out-of-date clinical information could lead to reassessment. Although some adults’ clinicians reported not having a reason to doubt existing diagnoses of ADHD, others felt that it was important to reassess to understand how symptoms are presenting as an adult and the degree of severity. Some adults’ clinicians and GPs reported a mistrust of diagnoses, because of a lack of access to initial diagnostic records and a current care plan. For GPs, this mistrust confounded concerns about prescribing controlled medication for adults with ADHD:
Sometimes . . . we look in their notes and we think well, actually, I don’t know on what basis you ever really were prescribed these drugs, it’s not clear from your notes that you ever had a proper assessment.
GP 14
None of the ones who had the ADHD diagnosed as a child have any ongoing follow-up or any plan that I’ve ever seen. You do end up questioning the diagnosis, whether that diagnosis just becomes a non-diagnosis at 18, if there is no plan and no follow-up and no management plan.
GP 11
This mistrust could be picked up by patients and have an impact on engagement with services. Patients and parents questioned the handover of patient information and valued not having to retell their history. There was a sense from some patients that the ‘reassessment’ in a new service might not recognise the impact of persisting impairment from their ADHD, focusing instead on severity of symptoms:
She [consultant in adult services] just . . . kept saying things like, ‘Well your ADHD is not that severe’. It’s never been measured on severity . . . I feel like it has got a huge impact on my life and she just said, ‘Oh well, it doesn’t really do anything’. It’s like, ‘I just won’t give you medication’. I was like, right, OK. So, I’ve been given this diagnosis and you can’t do anything to help me, so what was the point of having that?
Transitioned patient 10
I don’t know how much my doctor from the child’s place told the one from the adult’s place, it didn’t seem like he knew everything . . . So, it doesn’t seem like they’re working together that well.
Transitioned patient 5
When we went last week [to AMHS], it was so refreshing and so nice . . . the most refreshing thing was, ‘I’ve read your notes, mate’. Because every time you see anybody, you have to start right from the beginning and go through everything.
Parent 21
Joint appointments with both services present or telephone case conferences were viewed as helpful handover practices, whether on a formal or on an ad hoc basis. However, because of demands on time because of high workloads in both child and adult services, clinicians reported that typically these processes were reserved for complex cases:
We have started to hold joint transitional clinics . . . And that seems to have worked really well, there’s a visible and a tangible handing over . . . witnessed by the patient and their parents . . . We’re also able to ask a lot more specific and detailed questions to which we are much more likely to get answers than doing that over the phone or in writing. So, it’s a very worthwhile process and we aspire to rolling that out in other areas.
Adults’ clinician 13
If it’s a consultant who knows me or I know this consultant, gives me a ring, gives me a heads-up or is asking . . . this informal contact sometimes, it’s actually sufficient . . . I think this transition concept, transition process, should be a bridge, slight overlap between children and adult services.
Adults’ clinician 04
The current protocol is that if you felt a joint handover was really needed, a kind of complex case, then you can do that but it’s not routine. So initially when the [transition] panel was set up, the hope was that it would be routine that everyone would have a joint appointment with their CAMHS worker and their adult worker as a kind of handover but that just hasn’t worked out resources . . .
Child and adolescent psychiatrist 13
Clinicians in children’s services also reported not knowing what happens to patients after transition, with few data, if any, passed on to them or collected to monitor transition outcomes:
I’m not sure that I would know if they’ve dropped out after transition . . . I know that nobody has rung me up to say . . . and I wouldn’t always check that they had been seen, honestly.
Paediatrician 09
I don’t think anybody keeps a record of whether the ones that transition stay with the service. We have talked about that a lot, how we would love to know, are they still with them 6 months later, are they still with them a year later? As far as I am aware, nobody collects that data.
Child and adolescent psychiatrist 13
Default role of the GP
Across the interviews, there were numerous examples of child services discharging patients to GPs rather than transitioning to adult secondary services, and adults’ clinicians explained that the bulk of their ADHD patient referrals came from GPs and not child services. Some clinicians in children’s services felt that they had no choice but to discharge to GPs, as there was no-one else who could co-ordinate the transfers to the relevant appropriate fragmented adult services and that it was important to highlight gaps in services:
So, he turned 18, she’d got rid of him.
When you said she got rid of him, do you remember the last appointment?
Literally we just had a letter saying, ‘Now he’s 18 he’s referred back to his GP’.
Parent 23
[Child services] will send a letter saying the age is now out of their hands. But they never actually transfer care to adult ADHD services.
GP 04
So, the overall co-ordination that you’re used to with kids, the GP becomes the overall co-ordinator . . . So, these young people do have a problem in that they’re so used to us co-ordinating care and overall managing them and then suddenly they get to 18 and it’s back to the GP who hasn’t got the time or the expertise to take on our role.
Paediatrician 12
I think previously we would try and do what we could to refer on to another service and persuade adult mental health services to take them, we are now just passing those back to the GP because I think it needs to be really highlighted back to the commissioners in terms of what service is needed.
Paediatrician 19
GPs were also reported as assuming responsibility for care when patients were in ‘limbo’ between child and adult services. This could be the result of long waiting lists for adult services’ appointments and/or gaps in local provision where, for example, the remit of child services finished at 16 years and adult services started at 18 years, or there was no appropriate adult service to transfer to:
You get that sort of situation where you are too late to get something from CAMHS but too early to get something from the adult services and then you’re left in a limbo situation and if you have really significant issues with your ADHD . . . it’s easy to see how a young person might end up in the criminal justice system before anybody in the health-care system gets a chance to actually formally diagnose and really get to grips with it.
Adults’ clinician 14
Until services are properly commissioned, I think there’s going to be an unmet need there. It’s a real problem for primary care because they feel like they’re having to manage things that they don’t necessarily feel comfortable . . . or feel like they’re giving as good as a service as the patient should be getting . . . I think it’s the picking up the patients that’s probably the issue, rather than CAMHS dumping them. I think it’s just that there’s a lack of service in the adult age range, but that’s just my perception.
GP 12
Some parents described how families ‘fell into a black hole’ after child services finished, often with no idea of what was meant to happen or without anyone other than their GP to contact during transition. They questioned the timing of transition at a time of change in a young person’s life and explained that being in limbo could mean symptoms worsened. Some clinicians in children’s services described how they held onto patients with complex needs or offered ongoing ad hoc support to the patient, family or GP when needed to ensure that they were not left in limbo:
The GP’s been amazing, bless her. She doesn’t know what to do. She’s referred him and they just did an assessment and then, ‘We’ll try and find some help’, and then you hear nothing for 6 months and in the meantime my son is smoking dope until it’s coming out of his ears, which he knows makes it worse.
Parent 21
I do have a few who are a little bit more complex or maybe they have got other social issues or safeguarding issues that I’ve tended to hang on to, so I’ve been looking after them for several years.
Paediatrician 19
I’ll put on the letter to the GP that I’m quite happy to supervise, provide the specialist support whilst they’re in the interim so that the whole thing doesn’t crash.
Paediatrician 18
How long did you have to wait as well to get an appointment?
Probably 6 months but I was still seeing CAMHS in the interval, I wasn’t left, because CAMHS didn’t allow that. But I should have been, if you put it that way . . . She refused to shut my case. My case still isn’t shut. They won’t shut it until they know that they are going do the right thing. They just haven’t yet.
Transitioned patient 10
The time between the last child service’s appointment and the first adult service’s appointment varied from a few months to 2 years. Adult services took different approaches to patients trying to re-access secondary care support; some fast tracked patients with a history of ADHD and child service use, whereas others treated all as new referrals, which then meant longer waiting times:
So, there’s a backlog. There’s like 220 people on the waiting list . . . and this is where the problem is, because he’s going to be well into 18 and a half before his name comes up . . . As I said, with his sister we were still waiting 5 months after she was 18 and I’d ring up CAMHS saying, ‘Well, could you please chase the people who you’ve written to? Can I chase them?’.
Transitioned patient 03 [mum]
We see them often coming back when they start studying at university and realise that actually they struggle . . . and ask if the GP can restart their ADHD medication, which the GP can’t because the patient’s now an adult and needs to be seen first by the ADHD service. And then they end up on a waiting list which is again quite unfortunate. We still have quite long waiting lists for assessments in the adult ADHD service.
Adults’ clinician 16
Some GPs took a pragmatic approach to treating patients in limbo between secondary care services. Others felt strongly that prescribing and monitoring ADHD medication was outside their role, even with additional training. For some GPs, this was linked to concerns over the risks of prescribing without specialist oversight. Although some accessed specialist advice through virtual systems or informal relationships with colleagues in secondary services, for others it was accessible only via lengthy referral processes:
You’ve got a family and patient that are suffering, so it was just weighing the risks and benefits really and whether they can afford to wait or actually they did want something to happen . . . [so I] used the dosing that was safe as per BNF [British National Formulary] guidelines . . . and then just closely following up with the patient.
GP 12
I think the role of the GP should be managing their primary health needs and not their mental health needs . . . My personal view is that this is not my job. This should be done by somebody else who knows about it – because they’re proper drugs, not something that I would like to prescribe.
GP 13
Letter from secondary care says, ‘please prescribe this – re-refer back if there is a problem’. No recognition of the fact that there’s months and months worth of waiting lists if you do actually want to refer them back because it’s not all going swimmingly well . . . [it would] be really useful to have fairly quick access to advice . . . on what we could do if things were unstable . . . some support to tweak things which I don’t think we should be doing ourselves.
GP 01
Childrens’ and adults’ clinicians, patients and parents reported variable experiences of primary care. Some families had found their GP’s help invaluable. There were also reports of clinicians supporting GP prescribing while the patient was waiting to be seen in a secondary care service; however, shared care protocols between primary and secondary care were not always implemented, causing concerns about continued access to medication. Stakeholders discussed a number of perceived barriers to shared care and primary care prescribing, including GP workload, funding of prescriptions, responsibility for medication monitoring, different ADHD medication licences for children and adults, and beliefs and knowledge around ADHD. The issue of licensing was also alluded to by parents, who reported that pharmacists had advised them that they could not keep fulfilling ADHD medication prescriptions into adulthood:
We’ve come to a working agreement that we will support GPs in prescribing medication for ADHD if they can demonstrate to us that the [patient] was under a reputable service or an NHS service before, that there is a history of a sound diagnosis follow-up and a stable medication. We would then support GPs in prescribing until we are able to see the young person.
Adults’ clinician 13
The much-vaunted shared care agreement with the GPs has never actually been done. GPs had not signed up to it . . . of 17 GP practices, I think two or maybe three will prescribe, the rest don’t. And they will happily have prescribed for them when they were under 18, happily, because it came from paediatricians, that’s a whole other story. But with us, no they won’t do it.
Adults’ clinician 12
Our own GP, he flatly refused to prescribe stims [stimulant medication], he just said, ‘I’m not doing it’, and it kept going back to the paediatrician . . . he doesn’t really agree with ADHD meds. And I do see why, I think he’s sort of doing it from a dad point of view, but he’s got three daughters but he’s also a GP and, from a patient perspective, that didn’t help me because it started me thinking, well why, what does he know that I don’t, what should he be telling me and why should I not be giving them to him? Then you are stuck.
Parent 14
Secondary care clinicians largely reported that continued specialist oversight was important. In particular, individually tailored medication plans and support of underlying impulsive behaviour was considered to be a specialist role:
I give them much more options in planning their medication, like we could do a combination of long acting and short acting . . . that works really well. People do come back and do see me, and we talk about it and we change the meds and see how they go . . . with the GP they couldn’t do that.
Adults’ clinician 12
Stimulant medication is amber, meaning it has to be specialist overseeing, so GPs cannot take on prescribing responsibility. So, it’s structurally built into the system locally. Which is yet another reason why it’s critical that the adult services have sufficient capacity.
Paediatrician 18
In relation to the issue of limited capacity within specialist services, however, some adults’ clinicians and GPs believed that GPs could manage cases where patients were stable and there was no comorbid mental illness:
I’ve got a couple of people that are really stable, and I’ve just said that I’m going to see them again and then . . . we are going to pass the care on to the GP . . . Not everybody that we get from that transition period needs that ongoing service for a year, otherwise we’d never be able to discharge people and take new referrals.
Adults’ clinician 07
I think with a bit of experience, I’m sure we could manage . . . because you’d just basically titrate it against the behaviour . . . It’s not actually a toxic drug as such.
GP 08
Discussion
The interviews provided a wealth of data about ADHD and health-care services for patients with ADHD. The overall finding is that the experience of transition from child to adult services for young people with ADHD is highly varied. For some it is straightforward, for others challenging. The qualitative strand of this study suggests that transition between child and adult services for ADHD patients depends on how invested stakeholders are in the process and the architecture of services.
Being invested
The stakeholders interviewed for this study suggest that there are gaps in the understanding of ADHD as a long-term condition, particularly in respect of ongoing impairment and how it may affect people in different ways at different stages of life. Across the stakeholder groups, concerns were expressed as to the long-term use of ADHD medication, and clinicians reported a lack of clarity around the licensing for adult ADHD medication. Patients associated taking ADHD medication with managing behaviour in school and academic achievement, with pre-transition and post-transition patients both envisaging a time in the future when their schooling would finish and their medication would stop. These findings echo the ADHD VOICES study180 with children aged between 9 and 14 years, who also viewed ADHD as a disorder of academic performance or aggression. Only the patients in this study who did not transition but re-entered adult services as a young adult reported an understanding of ADHD as a long-term condition that impacts their life outside education. Although it is recommended that clinicians start planning for care in adulthood from age 13–14 years, this is not consistent with the experiences of many stakeholders. Some described clear communication from an early age regarding transition to adult services, but others experienced no communication or limited communication regarding transition or ADHD as a long-term condition.
As found previously, engagement with services and transition was often focused on medication continuation rather than on the condition itself, with reports of some patients being discharged before transition as a result of a voluntary discontinuation of medication or non-attendance around school leaving age. 70,74,101 A pattern was found in the transition experiences explored in this study that suggests that both the medication focus of services and the association with education meant that transition was more likely for patients going on to higher education, who perceived ADHD medication as beneficial in the short term to help with educational goals. The timing of trials off medication before transition age, when schooling may be finishing, perpetuates misconceptions between ADHD and education. As it can take time for effects of impairment to show, or for symptoms to worsen, and as patients typically lack understanding of ADHD in adulthood, this timing can mean that patients with ongoing needs are off medication and, therefore, do not transition.
Many stakeholders were frustrated with the medication focus of ADHD services and expressed recognition of the importance of a holistic approach, including psychoeducation, pharmacotherapy and access to systemic interventions. 67,70 In line with a prior qualitative study of adult ADHD experiences,70 patients who had had trouble in accessing care reported being reluctant to disclose if, or how, medication was working, or even if they were taking it, in fear of support being withdrawn. As most of the patients who did not transition but re-entered adult services did so after a profoundly negative life experience, this suggests that their discharge may have been premature and that patients are losing their connection with services at a vital point. This finding is reflected in prescribing studies, which suggest that a higher than expected proportion of adolescents stop their medication, with only a small proportion of those that stop resuming their prescriptions in early adulthood. 133 Although access to adult services is likely to have improved since the ‘re-entry’ group left child services, the results suggest a need to better identify patients who might continue to have clinically significant impairment in adulthood, and to develop standardised re-entry processes for patients with a pre-existing clinical diagnosis of ADHD so that support can be easily accessed to avoid crisis.
In line with NICE guidelines35 and a recent transition research programme,181 there was a shared belief across stakeholder groups that parent involvement supported transition. In contrast to adolescent patients, parents anticipated a continuing need for support in adulthood and their investment facilitated transition. In addition to supporting their child’s heath care, parents considered that their ongoing role was necessary because of the ‘fight’ required to access and retain support from health-care services, particularly given ADHD’s status as a ‘contested illness’. 182,183 Parents and patients described a need for persistence and advocacy skills to gain support – skills that their children did not have, or were yet to acquire. Parents reasoned that owing to limited resources in the NHS, a perceived ongoing scepticism about ADHD diagnosis and a lack of ‘fit’ of ADHD within adult services that their ‘fight’ would continue to be needed during and after transition. In line with the large number of private ADHD services found in the mapping study, many parents reported that they would ‘go private’ to ensure that support was accessed.
Interestingly, although clinicians in children’s services and parents perceived that parent involvement might not be welcome at adult services, adults’ clinicians were happy to work with families, as long as the patient consented. However, attaining consent for continued parental involvement prior to first appointment was acknowledged as a challenge. Parents also reflected that a lack of information about transition had an impact on their ability to help prepare their child for transition. Patients, parents and clinicians in children’s services reported that realistic expectations of what adult services can offer were often emphasised prior to transition as part of a preparation for expected changes in care philosophy and a more restricted remit. It is possible that limited or negative expectations can affect engagement. There was an acknowledgement from adults’ clinicians that adult services were less flexible and required patients to have certain levels of organisational skill that young people with ADHD might find difficult. There were also examples of adult services adapting their practice to better suit newly transferred patients. These findings suggest a need for greater understanding of the working practices of child and adult services, in addition to adjustments that can be made to deliver developmentally appropriate care. The data suggest a family-centred approach to transition that recognises how autonomy can be relational when patients have long-term health conditions. 184 However, in line with other studies, the interviews with clinicians described the challenge of both respecting increasing needs for autonomy and negotiating with ADHD patients and their families, particularly in relation to medication decisions. 67,73,161 Parents may have ADHD themselves and can have higher levels of parenting stress than other parents,185 and young people with ADHD may have general and disorder-specific needs in relation to both joint decision-making and non-health-care issues that impinge on independence in health settings.
NICE guidelines35 recommend that transition should be managed to facilitate the building of independence. Colver et al. 181 found that that young people adopt different interaction styles when approaching transition, including ‘laid-back’, ‘anxious’, ‘autonomy-seeking’ and ‘socially-orientated’, which our findings support. Further research is needed to explore ADHD patients’ understanding and desire for independence and parent involvement, including whether or not it would be acceptable to young people to acquire their consent and parent contact details before discharge from child services to allow communications from adult services to be directed to both patients and parents to facilitate transition. Future research could also explore models of care that may best facilitate negotiation between clinicians, ADHD patients and parents, continuity of care and increased understanding of ADHD as a long-term condition. This could include the use of digital technologies for communication between clinicians and ADHD patients, such as FaceTime (Apple Inc., Cupertino, CA, USA), Skype, WhatsApp (WhatsApp Inc., Menlo Park, CA, USA) or text messaging, which may support independence and accessibility of services, and may have particular benefits in rural areas where there is a decreased rate of service use. 186–188 The findings from this sample, that going on to higher education and having parents who are able to advocate can positively influence transition, indicate a possible association between transition and social capital (resources that increase the ability to advance individual interests). 189 Other studies have suggested that low socioeconomic status can increase the odds of an ADHD patient not receiving services,190 and that social networks of white and higher socioeconomic status families contain higher proportions of health-care workers to help access support. 191 Future research could further explore the characteristics of those who do successfully transition to see whether or not current processes reproduce societal inequalities.
Architecture of services
In line with other studies, a number of factors were acknowledged as barriers to transition, including limited clinician time to prepare patients for transition, lack of information provided about transition and standardised approaches to patient information handovers, distance to travel and stigma of accessing AMHS. 73,124,125 Indeed, although stakeholders largely agreed with the transition recommendations set out in the relevant NICE guidelines, the architecture of services often limited the extent to which they could be delivered. Adult services designed to support episodic and acute rather than chronic conditions, and restrictive eligibility criteria, also had an impact on transition, in relation to both actual and presumed thresholds for access. In accordance with other studies, clinicians working in child services reported not referring patients to adult services because of their assumption that patients would not meet adult services thresholds,72,161 particularly in relation to patients off medication or those whose symptoms are well managed at the time of transition. This is also relevant as young people may still require support because of persisting impairment even if their symptoms subside to become ‘subthreshold’ to the diagnostic criteria. 29
As described in previous research, in this study, stakeholders questioned the ‘fit’ of neurodevelopmental disorders such as ADHD with adult services. 49,124 There were reports of patients with ADHD who did not meet acceptance thresholds for any suitable adult service. Patients with comorbid autism and those with LD just above the threshold for support by adult LD teams were particularly highlighted as falling into gaps between services. However, only one LD team in the mapping study confirmed that they would treat adult ADHD, suggesting a need for future research to explore the support provided to patients with ADHD and LD, both those above and those below the intelligence quotient threshold.
Rather than supporting the use of dedicated ADHD services, a number of clinicians suggested that their limited remit (no treatment of comorbidities, diagnosis or medication services only) can create further gaps in services. The usefulness of a specific ADHD transition pathway was similarly questioned owing to the varied needs and comorbidities of ADHD patients. Instead, views were expressed that specialist training across services, including knowledge and skills in ADHD diagnosis and treatment125 and competence in working holistically with patients with comorbidities, would better support transition. These views, and the lack of adult ADHD services, perhaps explain why transition protocols were largely described as being recently introduced or a work in progress despite being recommended in NICE guidelines years ago. 33
In accordance with NICE guidelines,36 the importance of patient familiarity with adult services before transition was acknowledged by all stakeholder groups; however, because of demands on time as a result of high workloads, transition processes, such as joint appointments between children’s and adults’ clinicians, were reported as reserved for those with complex needs. Care co-ordination was highlighted as a challenge for transitioning ADHD patients, where multiple transitions were often required across multiple agencies. This is in line with a consensus of ADHD professionals in the UK, who considered that a care co-ordination role for adult patients with complex health and social needs would facilitate multiagency service input. 192 In most community and inpatient AMHS, there is a specific role of care co-ordinator under the CPA, but some clinicians in this sample described CPA processes as administratively burdensome. A care co-ordination function for young people with ADHD could present a valuable focus for development and research to help facilitate transition for ADHD patients with comorbidities and those with complex needs, as well as access to non-pharmacological support.
National Institute for Health and Care Excellence guidance36 recommends that primary care should be involved in the transition process, and that ADHD medication for children and adults should be provided and monitored under shared care protocols between primary and secondary care. Although there were examples in this study of shared care and good communication between primary and secondary care, the experience of some interviewees suggested that primary care was sometimes involved by default. Participant reports suggested that this might happen where patients were left ‘in limbo’, where no onward referral was made by child services, where there were waiting lists for adult services, where there was no appropriate local adult service to transfer to, or when patients were too young to move to adult services but too old to continue attending their local child service. These findings are in line with a survey of paediatricians,74 which found that half of the paediatricians referred ADHD patients to their GPs when ongoing care was needed into adulthood, despite GPs’ concerns that they were not appropriately trained to take on this role. In this study, some interviewees, including GPs themselves, expressed reservations about GPs’ skills, knowledge and appropriateness to manage the care of young adults with ADHD, particularly in the perceived absence of specialist support and agreements to share risk and responsibility. There were also reports from interviews where GPs’ concerns had led to refusal to prescribe, or even to sign up to shared care protocols, which echo findings from other studies. 131,193,194 Although the CATCh-uS project did not map the existence of shared care protocols, previous research75 found that only one-third of English mental health trusts had such protocols in place for ADHD medication in adults. Although it is likely that the adoption of shared care agreements has increased since 2014, the findings of this study suggest that further work may be needed to improve communication and shared care between primary and secondary care for patients with ADHD in transition. Future research could explore and evaluate different models of shared care and examine how best to support GPs in their role in caring for this patient group.
Strengths and limitations
The purposive wide sampling gathered a broad understanding of a range of transition experiences from patients, parents and clinicians involved in the process. Although the study design was not longitudinal in nature (did not follow one cohort through transition), the three groups of patients interviewed (and their parents) followed the whole transition process. Recruiting clinicians from the surveillance study allowed us to explore underlying reasons behind identified variations. The addition of GP interviews meant that we were able to include their perspective, which was indicated to be important from early interviews.
Coding frames were developed from an initial analysis of interviews and discussion with the study project management group before the remaining interviews were coded. This meant that the interpretation of the themes identified reflect a wealth of experience (clinical, methodological, lay). The framework analysis approach produced an overview of factors that influence transition and continuation of treatment when approaching a service age boundary. The data presented here reflect this overview. More in-depth presentations of the rich data collected, such as reasons for medication cessation, are being prepared. Please see the list of academic publications (Report Supplementary Material 26) for more information.
Reflecting the findings of poor information flow between child and adult services, we needed to extend the time to recruit patients for the post-transition group, as it proved difficult to know which patients had attended their first appointment at adult services. The aim of this study was to compare themes across groups (patients, parents, clinicians) rather than characteristics, such as gender or ethnicity. Future studies could employ smaller sampling to probe experiences in relation to individual-level cases.
Conclusion
The qualitative study found that a number of factors influence transition of ADHD patients from child to adult services. The varied needs of ADHD patients make transition to an equivalent service for adults difficult, and there is currently a lack of patient understanding of ADHD as a long-term condition. Reflecting the results of the surveillance study, the findings of the qualitative study suggest that further exploration is needed about why only some patients with an ongoing need make the transfer to adult services, alongside any attempts to improve the quality of transition processes. Although the recommendations set out in the NICE guidelines were largely agreed upon by stakeholders, the experiences collected confirm that further work is needed to ensure that these recommendations are delivered in practice. Future research could explore models of practice where NICE recommendations are being delivered successfully.
Chapter 6 Discussion
Attention deficit hyperactivity disorder is a common reason for attendance at CAMHS or community paediatric clinics. 100,195 Historically, AMHS did not treat people with ADHD, which was initially conceptualised as a disorder of childhood. Training for adult and child mental health practitioners diverges early, so, until recently, very few practitioners working in AMHS had any experience of ADHD; however, at least 15% of those diagnosed with ADHD in childhood continue to meet the full diagnostic criteria for ADHD into their mid-20s, and a further 50% experience subclinical symptoms. 29 There has been a steady increase in clinical diagnosis and prescriptions for stimulant medication in childhood over the last few decades in many parts of the world, resulting from better recognition and improved service provision. 130
Improved access to treatment for children has generated an expanding cohort of young adults with ADHD who need ongoing support. The need for adult ADHD service provision was first formally recognised in the UK by NICE in 2008. 33 The CATCh-uS study was developed in response to evidence that suggests that young people with ADHD are particularly unlikely to transition from CAMHS to adult mental services. 56,72,196 We applied mixed methods to explore what happens to young adults with ADHD attending children’s services as they cross the age boundary of those services. Using surveillance methodology, electronic case note review, semistructured interviews and a novel approach to mapping services, we addressed the following objectives to:
-
provide prospectively gathered national estimates of how many young people need ongoing medication and how many of these young people had continuity of care over the age boundary for their child service
-
identify the level of current service provision in the UK for adults with ADHD
-
describe the quality of transition and factors that might improve continuity of care or contribute to drop out.
The work involved the three separate but interlinked studies described in the preceding chapters; each includes a brief discussion focused on the implications arising from that particular work. This final chapter explores where the findings from all three component studies converge or diverge, and, having integrated the results, explores their implications for practice, policy and research, as well as their methodological robustness.
Key findings and their implications for policy and practice
How many young people with attention deficit hyperactivity disorder need and access adult services?
The surveillance study (see Chapter 3) and the triangulation with the electronic case note review addressed this question. After adjusting for non-response and case ascertainment, our estimate suggests that between 270 and 599 per 100,000 young people aged 17–19 years will need continued medication for ADHD in the UK. The association of ADHD with certain population characteristics, such as deprivation, male gender, age and ethnicity,197,198 implies that commissioners and service providers should consider how these estimates may need adjusting to their context.
It is essential that these estimates are regarded as a minimum level of the need for transitional provision for several reasons. First, surveillance requires an easily operationalised and unambiguous definition of need that applies similarly to CAMHS and community paediatric services. Given the NICE guidance for specialist oversight of medication for ADHD,36 we followed only those who needed and wanted to continue their medication. This group constituted only a small proportion of those with ongoing need for support. Data from UK primary care suggest that the majority of young people prescribed ADHD medication when aged 16 years stopped receiving prescriptions by the age of 18 years. 132 Of those who stopped their prescriptions, 7.6% had resumed them after the age of 20 years, and resumption was associated with referral to AMHS. 133 Indeed, the CATCh-uS qualitative study (see Chapter 5) suggests that many young people do not fully understand the potential of ADHD to be a long-term condition or perceive medication as being necessary only in relation to school. These commonly cited reasons for dropping out of services imply a need to support young people to develop greater awareness of the impact of ADHD on their lives and strategies to manage it. 43,196 Indeed, current guidelines would recommend reassessment at the point of transition as part of transition planning, which could prompt such discussions. 67,122 A recent systematic review of transition for long-term conditions in paediatric services suggests that effective preparation should start in the mid-teens, with transition completed by the age of 18 years. 199 Our qualitative work suggests that this recommendation is rarely followed, despite its inclusion in the NICE guidelines.
Second, our qualitative work replicates other studies in indicating a consensus about the need for non-pharmacological approaches as well as medication. 130,196,200 Our estimates obviously do not include those with ongoing problems who wish to access psychosocial interventions only. Finally, as a minority of children with ADHD are treated by specialist health services, some young people are likely to present in adulthood for the first time as their social situation or life experience undermines their ability to cope. For example, only one-third of children with ADHD in the first British Child and Adolescent Mental Health Survey accessed CAMHS over a 3-year period; the equivalent figure for paediatric services was 15%. 100 Although the severity of difficulties predicted access to services in childhood,171 the implication for commissioners and service providers is that some childhood ADHD is missed, therefore, adult ADHD services need to be able to diagnose as well as manage ADHD to support those who present in adulthood for the first time; this group are also not included in our estimates.
Reports from paediatricians and child and adolescent psychiatrists indicated service age boundaries that were most commonly around the age of 18–19 years; the optimum age for transition to be completed. 199 The reported age boundaries in CATCh-uS ranged from 14 to 20 years or more, with greater variability reported by paediatricians than by psychiatrists. Access required attendance in full-time education for some 16 and 17 year olds, which implies a service gap for some of this age group. Our qualitative data echo others in suggesting that, as a result of their difficulties in school, young people with ADHD are more likely than their peers to be out of education at this age, particularly those who are living in disadvantaged circumstances. 67 This is one of several factors that emerge from CATCh-uS and which implies that current service structures may amplify disadvantage; private health care was most often accessed to continue with further and higher education, but would not be affordable to all. Moreover, these data were collected during a period of austerity within the UK, which affected mental health services and support for those with special educational needs disproportionately.
Paediatricians and child psychiatrists reported low rates of continuity of care via the surveillance study. 95 This may represent a failure by the clinicians involved in sharing and retrieving this information or delays in offering first appointments, but our follow-up period extended from 3 to 6 months beyond the age boundary. Arguably, longer gaps represent discontinuity of care. Referral (75% referred, 63% accepted) and first attendance (only 22% were known to have attended their first appointment at AMHS) were key points of drop-out, and, by implication, potential targets for intervention. 95 These findings echo the reluctance of CAMHS clinicians to refer, as reported in the TRACK study,39 as well as the CATCh-uS qualitative study and an allied systematic review. 58 Clinicians fear that cases would not be accepted, were concerned about raising false expectations or did not know where to refer. 58,72 Our qualitative work also suggests that familiarity and clear information about adult services might encourage attendance, in line with recent evidence, as well as the strong wish by those who had dropped out of services that they had received better information about ADHD as a long-term condition and more encouragement to remain engaged with services. 43 Models that have been reported but, to our knowledge, have not been evaluated, include joint clinics where practitioners from adult and child services work together with the young people approaching transition, or a transition team or officer work between services to support young people across the gap. 72,201
Current level of service provision
As we anticipated, our multi-informant mapping process (see Chapter 4) indicated an uneven distribution of services of all kinds for adults with ADHD, which implies that at least some discontinuity of care is explained by lack of provision. Furthermore, our qualitative study indicated that the process for re-entry into health care for those who needed it was often protracted and difficult. A wide range of services were reported, which spanned dedicated or specialist services, generic AMHS, prolonged access to CAMHS or community paediatric services, private health care and the voluntary sector. One implication of continued attendance at children’s services beyond the age boundary is reduced capacity for younger children to be seen, and potentially suboptimal care for young adults still being seen in child services. The recent NHS plan recommends selectively moving to services that support young people from 0 to 25 years, and neurodevelopmental disorders with their impact on maturation might be such an example. 202
The relative merits of the provision of care for adults with ADHD within generic AMHS or dedicated specialist services are a current issue for debate within the field, largely unsupported by empirical evidence. 203 The training, experience and availability of professionals who understand ADHD is arguably more important than their qualifications or the setting in which they work. 130 Our findings also indicate the practical obstacles that can impede engagement with services, for example where adult services are at a distance from home. This problem is more likely with highly specialist tertiary services, which are necessarily provided at regional level.
Service users and carers were more likely to report alternatives to both dedicated and generic AMHS, particularly private health care and the voluntary sector. In contrast, generic mental health services were mostly identified by clinicians alone, which raises the question of whether services users were able to identify and access them or whether or not commissioners were aware that support for ADHD was being offered. If not formally commissioned, adult ADHD services might be particularly vulnerable to decommissioning, particularly in the context of service pressures arising from austerity and the current psychiatric workforce crisis. That our finding that LD services were reported to treat adults with ADHD was not confirmed by our direct contact with trusts is confusing. This may be explained by comorbidities, which were high in our study, which may provide a ‘ticket of entry’ to such services, which then provide support for ADHD in an adult that they have accepted for other reasons. 95,130 These interesting differences emphasise the importance of seeking multiple perspectives when mapping service provision and suggest a lack of clear information. The latter was identified as a barrier to transition in a recent review,58 as well as an important theme arising from our qualitative work.
Clinical guidelines state that the following provision should be available for adults with ADHD: transitional care, assessment and diagnostic services, drug titration, monitoring and review, and psychoeducation. 33,36,41 Both the mapping study and our qualitative work suggest an overwhelming focus of services on the provision of medication for both children and adults, whereas our qualitative work replicates the consensus that psychoeducational treatment options are essential. 36,130,196 Furthermore, our qualitative findings imply that the medication focus of services meant that a decision to stop medication often resulted in the loss of all support, which was compounded by the view that the purpose of medication was to support access to education. Importantly, even among dedicated adult ADHD services, very few services provided the full range of services recommended by NICE. 36
The CATCh-uS qualitative work clearly indicates that GPs are involved in the care of young adults with ADHD in transition by default, without being included in planned transition processes. This may be influenced by the patchy distribution of services reported in the mapping study. Although training and improved access to relevant information might support GPs in this task, some would argue that the variable and complex presentations of ADHD may mean that unsupported GPs may miss important comorbidities, even in ‘uncomplicated cases’. 130
Quality of transition and influences on continuity of care
Transition in health care is conceptualised to extend beyond the simple transfer of clinical responsibility, namely to support a young person into a new life stage in a way that optimises their health and function. 37 As our findings emphasise, transition often coincides with other major life changes, such as leaving or changing type of education, starting work or moving out of the parental home. Young adults are often deprived of familiar support networks while facing increasing demands in several domains simultaneously. 72,204 The difficulties of ADHD may render transition especially challenging, while impaired function during adolescence is particularly detrimental to subsequent health, educational, occupational and social outcomes. 67,196 At its simplest, optimum transition has been characterised by planning, the transfer of information between the child and adult service, joint working and continuity of care. 35,38 Despite setting such a low level of expectation, both our surveillance and our qualitative findings suggest that few young adults with ADHD experience optimal transitional care.
Studies of transition across different long-term conditions suggest that some generic issues undermine smooth transition, all of which emerged in our qualitative work to some extent. These include accessing adult practitioners, negative beliefs about adult care, lack of knowledge about the transition process and lack of self-management skills. 43,44,58 The difficulties of ADHD reduce the ability to organise and regulate the self, which means that developmental capacity may be out of step with chronological age, and provide particular barriers to young adults trying to negotiate adult-focused services. 95,130 As the qualitative work indicates, the cultural gap between child-centred services, which expect parental involvement, and adult-oriented services, in which patient autonomy is assumed and prioritised, can be problematic for young people in transition and their carers. 58,72 Our findings indicated the critical role of parents as advocates, with obvious implications for those who lack such support, such as care-leavers. The balance between parental control and a young person’s autonomy needs to shift over time. The management of this process is arguably more familiar to those working in children’s services, as are the inevitable tensions between the needs and wishes of the young adult and those of their carers,43,72 Young people’s participation in treatment decisions needs to be balanced with the duty to protect their interests according to their developmental capacity. 43 This implies that there are two potential therapeutic targets: how prepared the young person is for transition, and their ability to manage their ADHD themselves.
Methodological issues
The CATCh-uS study benefited from a robust mixed-methods approach, including the application of surveillance to a process (transition) rather than a disorder or event, and the development of a novel multi-informant mapping study. The resultant data set is rich and novel. The findings from our three studies are highly convergent with each other as well as with the limited extant literature, which engenders confidence. Both the mapping study and the qualitative studies successfully recruited a large and varied samples of stakeholders, which is important given the research demonstrating large differences between clinicians’ reports of what they provide and service users’ descriptions of what they experience. 43 The interim analysis of qualitative data helped us to ensure that as broad a range of experiences were reflected as possible. The estimates from the surveillance study were based on prospectively collected data that were triangulated against electronic case records to check case ascertainment and were adjusted for non-response. The fact that we needed to extend the surveillance period for an additional 6 months, although partly reflective of non-response, emphasises the high level of drop-out of young people from services prior to the transition period.
Unfortunately, information governance requirements for the surveillance and CRIS systems meant that we could not triangulate reports at an individual level, and the geographical regions covered did not perfectly match and included a highly atypical NHS trust serving an area of unusual population density and ethnic diversity. To our knowledge, our study is the only mental health study to attempt such a sensitivity analysis to date, and it contributed important data that allowed us to adjust our estimates for non-response. The need for an unambiguous definition of ongoing need involved medication use; therefore, we can provide only minimum estimates that ignore those who drop out prior to transition, those who present for the first time in adulthood and those who need non-pharmacological support. It is essential to understand that as prescriptions for ADHD medications increase, it is likely that the cohort of graduates from child services will also increase and, therefore, our estimates will rapidly become out of date. Although it would be expensive and time-consuming to repeat the surveillance too frequently, the more widespread use of electronic case records might facilitate follow-up studies. However, the case note data extraction is also time-consuming, relies on the completeness of the notes and is constrained by what is likely to be recorded. 86
Young people, particularly those with ADHD, are a difficult group to recruit into research, and we included a number of methods to ensure that we met targets. In fact, the only group that we failed to recruit to the initial set target were GPs. Reassuringly, data saturation had been reached prior to discontinuing recruitment. In line with some of the consultants involved in the surveillance, GPs reported huge time pressures that vastly constrained their ability to participate in research. Research is enshrined as part of the NHS constitution, so these reports should be troubling and imply a need to engage people at every level about the importance of research. Studies such as these would not be possible without the contribution of clinicians. Owing to resource and ethics constraints, we lacked evidence of the experiences of young people with ADHD who attended services in childhood and did not seek further support in adulthood; future research should seek to systematically follow a sample of this group.
The mapping methodology applied different techniques to gather multiple informants’ experiences of services, but inevitably the use of social media to maximise participation means that we are unaware of our response rate and cannot assess if selection bias has influenced our findings. It seems intuitively plausible that those people with ADHD who are struggling to access services might have more incentive to respond, for example. However, the experiences reported in the qualitative and mapping studies were not universally negative and the similarity of findings from all three strands provides confidence in these results. We are particularly concerned about the lack of response from adolescents with ADHD, but this chimed with their lack of awareness of how ADHD might continue to affect their lives, which we elicited in the qualitative strand of CATCh-uS. Our chosen methods involved engagement only with those in services, as current ethics guidance will not allow contact with ex-patients. Registries for involvement in research would solve this problem and could be explored. As a result, the majority population of ADHD service attendees, who are from England, white and male, dominate our surveillance findings, and this study can tell us little about other groups, such as females and those from ethnic minorities. We endeavoured to ensure that such groups were represented in the qualitative work, but further focused studies are needed to establish the particular needs and experiences of these groups.
The classification of services into dedicated and generic was purely descriptive and not intended to imply that one model should take precedence over the other. It is harder than might first be imagined to define what constitutes a specialist service. A Delphi study94 conducted about this issue in relation to eating disorders concluded that specialist services providing evidence-based interventions must be multi disciplinary, and staff working within the service must have a clear focus on, and expertise in, the focus condition. The number of cases managed was also considered important, but consensus was not achieved on how many were required to signify specialist expertise. It is unclear how many dedicated services identified would meet this definition from our mapping study or what this might mean in relation to ADHD. A combination of regional highly specialist services to provide training, consultation and direct work with those with complex difficulties might complement more widespread support in generic adult mental health teams, but evaluation is desperately needed.
Recommendations for future research
There are three important avenues for future research to improve transition for young people with ADHD, as discussed below. These are evaluation of models of transition, the role of primary care and economic modelling of the costs of failed transition. Additionally, CATCh-uS highlighted the desire for psychosocial approaches. 196 Although there is little evidence of their effectiveness among children, they have yet to be evaluated for adolescents and adults. 205 Motivational interviewing, cognitive–behavioural approaches focusing on emotional regulation, organisational skills and problem-solving, as well as mindfulness, are obvious candidates for evaluation. 206,207 Personalised programmes that include education, occupation and social issues may be more successful than medication provision alone,130,200 and could be highly cost-effective given the large numbers of young adults with ADHD among the prison population. 67
Role of primary care
Our qualitative findings suggested that primary care plays a pivotal role in the care of young people with ADHD in transition and beyond, whether in a planned fashion or ‘by default’. The rising number of ADHD ‘graduates’ leaving children’s services will place increased demands on primary care provision, with implications for future patient care. We need to better understand GPs’ knowledge and training needs, and to develop and evaluate models of shared care. This work would benefit from a mixed-methods approach involving a similar combination of national surveys and case studies as in the current study.
Although training and support tools for GPs may improve primary care management of ADHD, and are sometimes presented as a possible solution to a lack of specialist services, the options and evidence base for such interventions are not well established. 205 These research gaps can hinder efforts to develop and evaluate services, and to optimise outcomes, and could be addressed in various ways, including the mapping of primary care prescribing practice and shared care arrangements for adults with ADHD; case studies of service models; a systematic review of training and interventions; linked data set analysis to gather more information on pathways between primary and secondary care; and a Delphi study aimed at developing consensus on options for better supporting GPs.
Evaluation of transition models
There is similar lack of evaluation of different ways to support transitions. 201 Although some suggest that continuity of care for young people with ADHD could be supported via technology, the benefits have yet to be empirically demonstrated. 196 Similarly, psychoeducational techniques that have been suggested as vehicles that might improve self-awareness, or organisational, problem-solving and decision-making skills, need evaluation for effectiveness and cost-effectiveness. 196 Our findings suggest that the extent to which young people are prepared for transition and their ability to manage their ADHD themselves are key areas for development in transitional services. 43,44 These studies would involve intervention development and evaluation along the lines of the Medical Research Council complex intervention guidance, whereas service models would require mixed-methods evaluation. 166
Economic evaluations
These could provide a compelling business case for adult ADHD service provision. Scandinavian patient registries suggest that continued ADHD medication into early adulthood is associated with substantially reduced levels of suicidal behaviour,208 depression,209 substance misuse,210 road traffic accidents,211 convictions and violent reoffending. 24 If these findings were replicated and modelled in a cost–benefit analysis, adult ADHD service provision would potentially reduce costs to health and social care, particularly given the recent research showing high levels of ADHD, both diagnosed and undiagnosed, among the prison population. 67
Conclusion
In summary, CATCh-uS applied integrated mixed methods to collect a rich and novel data set and our findings replicate and significantly extend previous research on transition for those with ADHD. Our results suggest that few of those who need ongoing medication for their ADHD successfully transfer to adult services, and only a small proportion of those who transfer experience anything that approaches optimal transitional care. 95,130,204 Furthermore, our estimates of need do not include those who do not want or need medication, those who present in adulthood for the first time and those who seek re-referral following discontinuation of support in adolescence. All stakeholders perceive psychosocial approaches as essential, although there is a lack of evidence-based approaches for non-pharmacological interventions with this age group, and a real need to evaluate various models of transitional care and adult ADHD provision. Our participants reported a range of experiences, including smooth transition. This seemed more likely with parental investment and procedures that supported parental involvement in attendance: familiarity with or support to meet the adult team, the promotion of understanding and self-awareness of ADHD as a long-term condition and solid information transfer. Most of these could be implemented without huge investment of resources.
Impact
Throughout this programme of research, we disseminated and discussed our findings, which included the development of a project website (http://medicine.exeter.ac.uk/catchus/). The project website includes summaries of each strand of research and a series of videos by an adult with ADHD about his experience, and by one of the researchers about the project. Anecdotally, we have heard that awareness of the study encouraged clinicians and managers to examine their transition systems. As shown in Figure 21, there was also a great deal of enthusiasm for the project from adults with ADHD and their families and the organisations that support them, who were delighted that research was addressing an issue of great importance to them. One of our most impactful outputs is the map of mental health services for adults with ADHD; lack of information about services was a major issue for all stakeholders. There were high levels of interest, with over 30,000 views of the map on our website in 12 months and 44,000 impressions on Twitter in 2018. The map was also used by the Exploring Diagnosis research project to send information leaflets to relevant services. UKAAN has agreed to host and keep the map updated and so, as a legacy of the research, it will be available on its website (www.ukaan.org/adult-adhd-service-map).
FIGURE 21.
Example of interest in CATCh-uS on Twitter. Reproduced with permission (2019, personal communication).
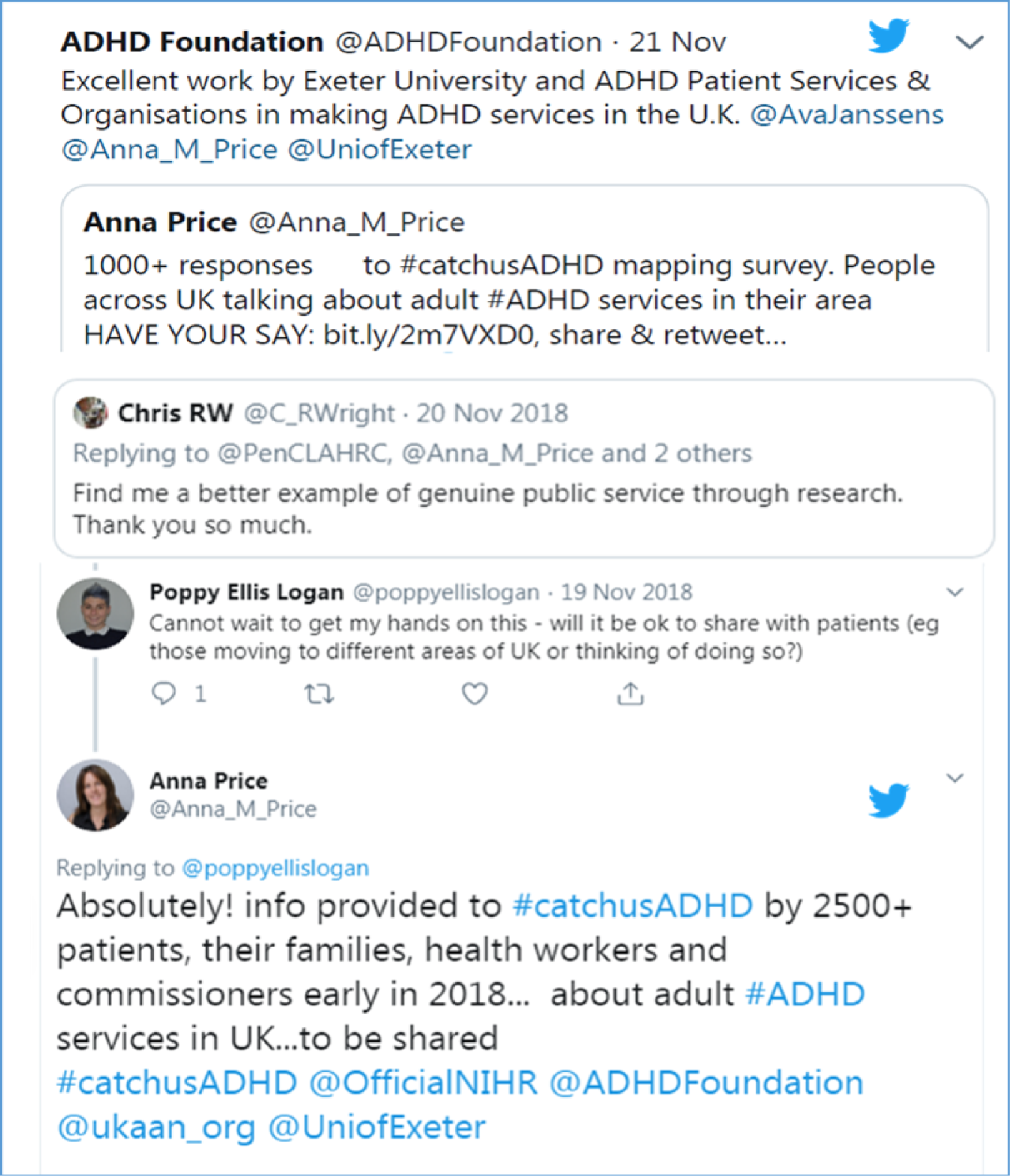
During the course of the project we contributed emerging findings to ongoing work in relation to transition or ADHD services. In 2016, we advised the Royal College of Psychiatrists on its input into the NICE guidance on transition. 41 In 2019, we contributed findings to UKAAN consensus meetings and worked with the NICE working party on ADHD services in relation to transition. We provided a summary of our findings for commissioners at the UKAAN and the NICE working party at national meetings, as well as at the east of England NHS England Mental Health Commissioners Event. The summary for commissioners is available (see Report Supplementary Material 27). In January 2020 we presented the findings in a webinar hosted by the Royal College of Paediatrics and Child Health, with more than 200 registered delegates, while Dr Eke’s review of guidelines for transition was summarised in the Bridge, an evidence-based digest e-mailed to all members of the Association of Child and Adolescent Mental Health (ACAMH) and freely available to all via the ACAMH web page. We have also submitted an application to further explore and support the role of GPs in transitional care for young adults with ADHD.
Project updates were disseminated by our research partners, PenCRU, BPSU, CAPSS and UKAAN, via their newsletters and/or annual reports throughout the project; for example, see the BPSU Annual Report 2017–18 (http://medicine.exeter.ac.uk/catchus/). Two press releases about the project went out during the course of the research and we also posted podcasts and briefings about articles on the ACAMH website:
-
12 January 2018, NIHR press release: National research extended to stop young adults with ADHD slipping through the net
-
10 May 2018, ACAMH: In conversation, Professor Tamsin Ford
-
22 November 2018, University of Exeter press release: Online ADHD service map aims to stop young people slipping through net
-
27 November 2018, ACAMH: Online ADHD service map aims to stop young people slipping through net
-
4 June 2019, ACAMH: The experiences of healthcare transitions between child and adult services for young people with attention deficit hyperactivity disorder: a review of evidence.
Capacity building
During the programme we endeavoured to develop capacity and are pleased to report the following:
-
Dr Astrid Janssens was promoted to Associate Professor in Public Health at the University of Southern Denmark.
-
Dr Tamsin Newlove-Delgado is now a Senior Clinical Lecturer at the University of Exeter after being awarded an NIHR Clinician Scientist Fellowship.
-
Dr Helen Eke and Dr Anna Price were awarded PhDs based on the theses they completed during the CATCh-uS project.
-
Ms Abigail Woodley, a psychology undergraduate student who was placed with us for 1 year, has now completed a masters course in health psychology and is working as a Psychology Assistant, with aspirations to train as a clinical psychologist.
-
Ms Molly Beaulah, an advanced-level (A-level) student, assisted with the dissemination of the qualitative findings as a Nuffield Research Placement; Nuffield is using her experience, which convinced her to apply for a place at university, as an example of the impact of this scheme for next year’s advertisements.
-
Two psychiatric trainees, Dr Daniel Titheridge, ST5 general adult psychiatry, and Dr Joanna Godfrey ST4 child and adolescent psychiatry, carried out an additional analysis of the qualitative data on reasons for stopping ADHD medication. This will be submitted for publication and has been taken as a poster to the International Congress and the South West Divisional meeting of the Royal College of Psychiatrists in spring 2019 (at which the work was awarded a prize for best poster). Dr Daniel Titheridge was selected to give an oral presentation at the Annual Royal College Child and Adolescent Psychiatry Faculty Conference in September 2019 (Belfast), for which he was awarded the Margaret Davenport Prize for best trainee presentation. He has also been awarded a Medical Research Council Clinical Training Fellowship.
-
Parents who were involved in the Parent Advisory Group reported enjoying their experience of being involved in the research: ‘Being heard. Being respected. Feeling part of the team. Feeling I have been valued and contributed in some small way’ (parent adviser).
Oral conference presentations
For a full list including posters presented at conferences, please see Report Supplementary Material 28.
-
27 April 2016: The British Paediatric Surveillance Unit: Celebrating 30 Years of Improvement in Public Health for Children (Royal College of Paediatrics and Child Health, London). Playing With Psychiatrists – CAPSS and its Interface With BPSU.
-
28 April 2016: Cerebra Annual Conference: Improving Mental Health and Wellbeing for Young People with Autism, ADHD and Learning Disabilities (Royal Society of Medicine, London). Transition from CAMHS to Adult Services for Young People With ADHD.
-
6–7 October 2016: The Royal College of Psychiatrists – Joint Conference – Faculties of Child and Adolescent Psychiatry, and General Adult Psychiatry Annual Scientific Meeting (International Convention Centre, Birmingham). Young People With Attention Deficit Hyperactivity Disorder (ADHD) in Transition From Children’s Services to Adult Services (CATCh-uS): A Mixed Methods Study.
-
14 June 2017: Bridging Transitions: Youth Mental Health – Risk and Resilience Conference (Queen Elizabeth Teaching and Learning Centre, Glasgow). Using a Surveillance Study Methodology to Estimate the Incidence of Transition.
-
9 July 2017: European Society for Child & Adolescent Psychiatry: Transition – Child and Adolescent Psychiatry in a World of Change (Geneva). Children and Adolescents With Attention Deficit Hyperactivity Disorder (ADHD) in Transition Between Children’s Services and Adult Services.
-
14 September 2017: The Royal College of Psychiatrists Faculty of Child and Adolescent Psychiatry Annual Scientific Conference (East Midlands Conference Centre, Nottingham). National Survey Mapping Adult ADHD Services: Developing Methods for Mapping Clinical Service Provision.
-
12–13 March 2018: The International Network of Paediatric Surveillance Units Conference (Glasgow). ADHD – The Issue of Transition.
-
28–31 May 2018: 30th European Academy of Childhood Disability Conference. Developmental Medicine and Child Neurology (Georgia). Using a Surveillance Methodology to Estimate the Incidence of Transition for Young People With ADHD Requiring Ongoing Support.
-
23–27 July 2018: Symposium at the World Congress of the International Association for Child and Adolescent Psychiatry and Allied Professions (Prague). In Transition from Children’s Services to Adult Services: The Case of ADHD.
-
26 September 2019: Faculty of Child and Adolescent Psychiatry Annual Residential Meeting (Belfast). Medication Discontinuation in Young People With ADHD.
-
30 January 2020: The Royal College of Paediatrics and Child Health webinar series. CATCh-uS Before We Fall; Transition in Young People With ADHD.
Academic publications
The list of academic publications published prior to the completion of this report are in Acknowledgements, Publications. Please see Report Supplementary Material 26 for other publications published since or in submission.
Acknowledgements
We would like to thank the following people for their contribution to the study: the participants who kindly gave their time and their experiences of transition and the members of our parent advisory group whose guidance was invaluable throughout the project. We are grateful to a number of organisations (Cerebra, Royal College of Psychiatrists, UKAAN, the ADHD Foundation, AADD-UK and Clinical Research Network South West) for their helpful advice and support throughout the project. We are delighted that UKAAN will be hosting, improving and updating the map of services that we created during this project, and are very grateful for their willingness to do so.
Particular thanks go to Professor Edmund Sonuga Barke for chairing our SSC and Dr Tony Lloyd, Ms Susan Dunn Morua, Dr Anita Pearson, Mr Tim Francis, Dr Barbara Jones, Professor Eric Taylor, Dr Kristin Liabo and Dr Muhammad Arif for their guidance and challenge as committee members; the motivated clinical research nurses and trust staff who assisted with recruitment of participants for the qualitative and mapping streams, including Ms Alice Garrood, Ms Heather Cogger-Ward, Dr Barbara Keogh, Ms Carinna Vickers, Dr Jessica Baskerville, Ms Amy Duffield, Mr Tom Pringle, Ms Leigh Franks and Dr Rubina Anjum. Particular thanks also go to Ms Rachel Califano and Dr Kate Powell who gave time to help check services; Ms Anna Stimson for her administrative support of the first two-thirds of the project; Ms Sue Curtis for support with developing the map of services; Dr Johnny Downs who facilitated our access to the CRIS database; Dr Abigail Woodley and Mr Andi Stanescu for data cleaning; Ms Kerry Pearn and Dr Sean Manzi from the PenChord team for support with QGIS mapping software; Dr Siobhan Mitchell, Mr Simon Benham-Clarke and Ms Molly Beaulah for assisting in dissemination; and Mr Kalyan Mitra and Dr Michael Zervos for proofreading.
Contributions of authors
Associate Professor Astrid Janssens (https://orcid.org/0000-0001-8419-0937) (Child Health and Public Involvement) developed the study design with Tamsin Ford and was the project manager for all three study streams. She also led the public involvement, contributed to CRIS data gathering, analysed the qualitative data and co-ordinated the drafting of this report.
Dr Helen Eke (https://orcid.org/0000-0003-4781-6683) (Research Fellow, Child Health) conducted the data gathering and led the analysis of the surveillance and CRIS studies, conducted interviews with young people, parents and clinicians for qualitative study, analysed the qualitative data and drafted Chapter 3 of this report.
Dr Anna Price (https://orcid.org/0000-0001-9147-1876) (Associate Research Fellow, Child Health) conducted the data gathering and led the analysis of the mapping study, conducted interviews with young people, parents and clinicians for qualitative study, analysed the qualitative data and drafted the Chapter 4 of this report.
Dr Tamsin Newlove-Delgado (https://orcid.org/0000-0002-5192-3724) (Senior Clinical Lecturer, Child Public Mental Health) led the qualitative study with GPs, guided recruitment of young people with ADHD and was involved in the analysis of qualitative data.
Ms Sharon Blake (https://orcid.org/0000-0003-0683-9424) (Associate Research Fellow, Child Health) was involved in the analysis of all the qualitative data, drafted Chapter 5 of this report and prepared the full report for publication.
Dr Cornelius Ani (https://orcid.org/0000-0003-0050-7939) (Consultant Child and Adolescent Psychiatrist and Honorary Clinical Senior Lecturer) contributed to the overall study as a co-investigator, advised the surveillance study, including the applications to the surveillance units, the development of questionnaires and the presentation of the results. He recruited patients and parents for the qualitative study and contributed to this report.
Professor Philip Asherson (https://orcid.org/0000-0003-2667-2254) (Neurodevelopmental Psychiatry) helped design the overall study, was an active member of the wider project management group and contributed to this report.
Professor Bryony Beresford (https://orcid.org/0000-0003-0716-2902) (Health and Care Services Research) advised on the qualitative study and contributed to this report.
Tobit Emmens (https://orcid.org/0000-0002-0654-9198) (Managing Partner Research and Development, research management and governance) supported the collection of the surveillance questionnaires and linked us to the Devon ADHD team.
Professor Chris Hollis (https://orcid.org/0000-0003-1083-6744) (Child and Adolescent Psychiatry) guided recruitment of young people with ADHD, was an active member of the wider project management group and contributed to this report.
Professor Stuart Logan (https://orcid.org/0000-0002-9279-261X) (Paediatric Epidemiology) helped design the overall study, was an active member of the wider project management group and contributed to this report.
Dr Moli Paul (https://orcid.org/0000-0003-2398-4308) (Child and Adolescent Psychiatry) advised on the design and conduct of the qualitative aspects of the study, was an active member of the wider project management group and contributed to this report.
Professor Kapil Sayal (https://orcid.org/0000-0002-2050-4316) (Child and Adolescent Psychiatry) helped design the overall study, was an active member of the wider project management group, guided recruitment of young people with ADHD and contributed to this report.
Dr Susan Young (Registered Clinical and Forensic Psychologist, Child and Adolescent and Adult Clinical Services) helped design the overall study, was an active member of the wider project management group and contributed to this report.
Professor Tamsin Ford (https://orcid.org/0000-0001-5295-4904) (Child and Adolescent Psychiatry) was the principal investigator on the proposal. She developed the study design with Astrid Janssens, supervised data collection, analysis and writing up, and drafted Chapter 6 of this report.
Publications
Eke H, Ford T, Newlove-Delgado T, Price A, Young S, Ani C, et al. Transition between child and adult services for young people with attention-deficit hyperactivity disorder (ADHD): findings from a British national surveillance study. Br J Psychiatry 2019:1–7.
Eke H, Janssens A, Downs J, Lynn RM, Ani C, Ford T. How to measure the need for transition to adult services among young people with Attention Deficit Hyperactivity Disorder (ADHD): a comparison of surveillance versus case note review methods. BMC Med Res Methodol 2019;19:179.
Eke H, Janssens A, Ford T. Transition from children’s to adult services: a review of guidelines and protocols for young people with attention deficit hyperactivity disorder in England. Child Adolesc Ment Health 2019;24:123–32.
Newlove-Delgado T, Blake S, Ford T, Janssens A. Young people with attention deficit hyperactivity disorder in transition: a qualitative study of the experiences of general practitioners in the UK. BMC Fam Pract 2019;20:159.
Price A, Janssens A, Dunn-Morua S, Eke H, Asherson P, Lloyd T, Ford T. Seven steps to mapping health service provision: lessons learned from mapping services for adults with Attention-Deficit/Hyperactivity Disorder (ADHD) in the UK. BMC Health Serv Res 2019;19:468.
Price A, Janssens A, Woodley AL, Allwood M, Ford T. Review: experiences of healthcare transitions for young people with attention deficit hyperactivity disorder: a systematic review of qualitative research. Child Adolesc Ment Health 2019;24:113–22.
Price A, Newlove-Delgado T, Eke H, Paul M, Young S, Ford T, Janssens A. In transition with ADHD: the role of information, in facilitating or impeding young people’s transition into adult services. BMC Psychiatry 2019;19:404.
Eke H, Janssens A, Newlove-Delgado T, Paul M, Price A, Young S, Ford T. Clinician perspectives on the use of NICE guidelines for the process of transition in attention deficit hyperactivity disorder (ADHD). Child Care Health Dev 2020;46:111–20.
Ford T. Transitional care for young adults with ADHD: transforming potential upheaval into smooth progression Epidemiol Psychiatr Sci 2020;29:e87.
Price A, Ford T, Janssens A, Williams AJ, Newlove-Delgado T. Regional analysis of UK primary care prescribing and adult service referrals for young people with attention-deficit hyperactivity disorder. BJPsych Open 2020;6:e7.
Price A, Janssens A, Newlove-Delgado T, Eke H, Paul M, Sayal K, et al. Mapping UK mental health services for adults with attention-deficit/hyperactivity disorder: national survey findings, with an analysis of differences in reporting between stakeholder groups [published online ahead of print June 2020]. BJPsych Open 2020.
Data-sharing statement
All requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Simmons P, Hawley C, Gale T, Sivakumaran T. Service user, patient, client, user or survivor: describing recipients of mental health services. Psychiatrist 2010;34:20-3. https://doi.org/10.1192/pb.bp.109.025247.
- Ritchie C, Hayes D, Ames D. Patient or client? The opinions of people attending a psychiatric clinic. Psychiatr Bull 2000;24:447-50. https://doi.org/10.1192/pb.24.12.447.
- Chief Medical Officer . Annual Report of the Chief Medical Officer 2012: Our Children Deserve Better: Prevention Pays 2013. www.gov.uk/government/publications/chief-medical-officers-annual-report-2012-our-children-deserve-better-prevention-pays.
- Paul M, Ford T, Kramer T, Islam Z, Harley K, Singh SP. Transfers and transitions between child and adult mental health services. Br J Psychiatry Suppl 2013;54:s36-40. https://doi.org/10.1192/bjp.bp.112.119198.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Wilens TE, Faraone SV, Biederman J. Attention-deficit/hyperactivity disorder in adults. JAMA 2004;292:619-23. https://doi.org/10.1001/jama.292.5.619.
- Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta-analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psychol Med 2015;45:247-58. https://doi.org/10.1017/S0033291714000762.
- Fletcher J, Wolfe B. Long-term consequences of childhood ADHD on criminal activities. J Ment Health Policy Econ 2009;12:119-38. https://doi.org/10.2139/ssrn.1489147.
- Gjervan B, Torgersen T, Nordahl HM, Rasmussen K. Functional impairment and occupational outcome in adults with ADHD. J Atten Disord 2012;16:544-52. https://doi.org/10.1177/1087054711413074.
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. an 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry 1990;29:546-57. https://doi.org/10.1097/00004583-199007000-00007.
- Taylor E, Chadwick O, Heptinstall E, Danckaerts M. Hyperactivity and conduct problems as risk factors for adolescent development. J Am Acad Child Adolesc Psychiatry 1996;35:1213-26. https://doi.org/10.1097/00004583-199609000-00019.
- Biederman J, Petty CR, Monuteaux MC, Fried R, Byrne D, Mirto T, et al. Adult psychiatric outcomes of girls with attention deficit hyperactivity disorder: 11-year follow-up in a longitudinal case-control study. Am J Psychiatry 2010;167:409-17. https://doi.org/10.1176/appi.ajp.2009.09050736.
- Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry 2018;5:727-38. https://doi.org/10.1016/S2215-0366(18)30269-4.
- Fredericks EM, Dore-Stites D, Lopez MJ, Well A, Shieck V, Freed GL, et al. Transition of pediatric liver transplant recipients to adult care: patient and parent perspectives. Pediatr Transplant 2011;15:414-24. https://doi.org/10.1111/j.1399-3046.2011.01499.x.
- Lopez PL, Torrente FM, Ciapponi A, Lischinsky AG, Cetkovich-Bakmas M, Rojas JI, et al. Cognitive-behavioural interventions for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev 2018;3. https://doi.org/10.1002/14651858.CD010840.pub2.
- Punja S, Shamseer L, Hartling L, Urichuk L, Vandermeer B, Nikles J, et al. Amphetamines for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Cochrane Database Syst Rev 2016;2. https://doi.org/10.1002/14651858.CD009996.pub2.
- Chan E, Fogler JM, Hammerness PG. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA 2016;315:1997-2008. https://doi.org/10.1001/jama.2016.5453.
- Turgay A, Goodman DW, Asherson P, Lasser RA, Babcock TF, Pucci ML, et al. ADHD Transition Phase Model Working Group . Lifespan persistence of ADHD: the life transition model and its application. J Clin Psychiatry 2012;73:192-201. https://doi.org/10.4088/JCP.10m06628.
- Patton GC, Olsson CA, Skirbekk V, Saffery R, Wlodek ME, Azzopardi PS, et al. Adolescence and the next generation. Nature 2018;554:458-66. https://doi.org/10.1038/nature25759.
- Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet 2012;379:1630-40. https://doi.org/10.1016/S0140-6736(12)60072-5.
- Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet 2016;387:2423-78. https://doi.org/10.1016/S0140-6736(16)00579-1.
- Wilens TE, Faraone SV, Biederman J, Gunawardene S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics 2003;111:179-85. https://doi.org/10.1542/peds.111.1.179.
- Chang Z, Lichtenstein P, D’Onofrio BM, Sjölander A, Larsson H. Serious transport accidents in adults with attention-deficit/hyperactivity disorder and the effect of medication: a population-based study. JAMA Psychiatry 2014;71:319-25. https://doi.org/10.1001/jamapsychiatry.2013.4174.
- Lichtenstein P, Halldner L, Zetterqvist J, Sjölander A, Serlachius E, Fazel S, et al. Medication for attention deficit-hyperactivity disorder and criminality. N Engl J Med 2012;367:2006-14. https://doi.org/10.1056/NEJMoa1203241.
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007;164:942-8. https://doi.org/10.1176/ajp.2007.164.6.942.
- Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics 2012;9:490-9. https://doi.org/10.1007/s13311-012-0135-8.
- Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry 2007;190:402-9. https://doi.org/10.1192/bjp.bp.106.034389.
- Simon V, Czobor P, Bálint S, Mészáros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry 2009;194:204-11. https://doi.org/10.1192/bjp.bp.107.048827.
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med 2006;36:159-65. https://doi.org/10.1017/S003329170500471X.
- Lara C, Fayyad J, de Graaf R, Kessler RC, Aguilar-Gaxiola S, Angermeyer M, et al. Childhood predictors of adult attention-deficit/hyperactivity disorder: results from the World Health Organization World Mental Health Survey Initiative. Biol Psychiatry 2009;65:46-54. https://doi.org/10.1016/j.biopsych.2008.10.005.
- Cheung CH, Rijdijk F, McLoughlin G, Faraone SV, Asherson P, Kuntsi J. Childhood predictors of adolescent and young adult outcome in ADHD. J Psychiatr Res 2015;62:92-100. https://doi.org/10.1016/j.jpsychires.2015.01.011.
- Van Lieshout M, Luman M, Twisk JWR, Groenman AP, Thissen AJ, Faraone SV, et al. A six-year follow up study of a large European cohort of children with attentiondeficit/hyperactivity disorder combined subtype: outcomes in late adolescence and young adulthood. Eur Child Adolesc Psychiatry 2016;25:1007-17. https://doi.org/10.1007/s00787-016-0820-y.
- NICE . Attention Deficit Hyperactivity Disorder: Diagnosis and Management of ADHD in Children, Young People and Adults (CG72) 2008. www.nice.org.uk/guidance/cg72 (accessed September 2019).
- NICE . Service for the Diagnosis and Management of ADHD in Children and Young People. Commissioning Guide: Implementing NICE Guidance 2009.
- NICE . Attention Deficit Hyperactivity Disorder. Quality Standard (QS39) 2013. www.nice.org.uk/guidance/qs39 (accessed September 2019).
- NICE . Attention Deficit Hyperactivity Disorder: Diagnosis and Management (NG87) 2018. www.nice.org.uk/guidance/ng87/chapter/Recommendations (accessed September 2019).
- Beresford B. On the road to nowhere? Young disabled people and transition. Child Care Health Dev 2004;30:581-7. https://doi.org/10.1111/j.1365-2214.2004.00469.x.
- Royal College of Paediatrics and Child Health . Bridging the Gap: Health Care for Adolescents 2003.
- Islam Z, Ford T, Kramer T, Paul M, Parsons H, Harley K, et al. Mind how you cross the gap! Outcomes for young people who failed to make the transition from child to adult services: the TRACK study. B J Psych Bull 2016;40:142-8. https://doi.org/10.1192/pb.bp.115.050690.
- Lotstein DS, McPherson M, Strickland B, Newacheck PW. Transition planning for youth with special health care needs: results from the National Survey of Children with Special Health Care Needs. Pediatrics 2005;115:1562-8. https://doi.org/10.1542/peds.2004-1262.
- NICE . Transition from Children’s to Adults’ Services for Young People Using Health or Social Care Services (NG43) 2016. www.nice.org.uk/guidance/ng43 (accessed September 2019).
- Campbell F, Biggs K, Aldiss SK, O’Neill PM, Clowes M, McDonagh J, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev 2016;4. https://doi.org/10.1002/14651858.CD009794.pub2.
- Colver A, McConachie H, Le Couteur A, Dovey-Pearce G, Mann KD, McDonagh JE, et al. A longitudinal, observational study of the features of transitional healthcare associated with better outcomes for young people with long-term conditions. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1102-y.
- Gray WN, Schaefer MR, Resmini-Rawlinson A, Wagoner ST. Barriers to transition from pediatric to adult care: a systematic review. J Pediatr Psychol 2018;43:488-502. https://doi.org/10.1093/jpepsy/jsx142.
- Colver A, Pearse R, Watson RM, Fay M, Rapley T, Mann KD, et al. How well do services for young people with long term conditions deliver features proposed to improve transition?. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3168-9.
- Gray WN, Reed-Knight B, Morgan PJ, Holbrook E, Kugathasan S, Saeed SA, et al. Multi-site comparison of patient, parent, and pediatric provider perspectives on transition to adult care in IBD. J Pediatr Nurs 2018;39:49-54. https://doi.org/10.1016/j.pedn.2018.01.008.
- Tilton AH. Transition of children with neurological disorders. Curr Neurol Neurosci Rep 2018;18. https://doi.org/10.1007/s11910-018-0822-x.
- Harpaz-Rotem I, Leslie D, Rosenheck RA. Treatment retention among children entering a new episode of mental health care. Psychiatr Serv 2004;55:1022-8. https://doi.org/10.1176/appi.ps.55.9.1022.
- Young S, Murphy CM, Coghill D. Avoiding the ‘twilight zone’: recommendations for the transition of services from adolescence to adulthood for young people with ADHD. BMC Psychiatry 2011;11. https://doi.org/10.1186/1471-244X-11-174.
- Blakemore SJ, Choudhury S. Development of the adolescent brain: implications for executive function and social cognition. J Child Psychol Psychiatry 2006;47:296-312. https://doi.org/10.1111/j.1469-7610.2006.01611.x.
- Singh SP, Paul M, Islam Z, Weaver T, Kramer T, McLaren S, et al. Transition from CAMHS to Adult Mental Health Services (TRACK): A Study of Service Organisation, Policies, Process and User and Carer Perspectives. Report for the National Institute for Health Research Service Delivery and Organisation Programme 2010.
- McGorry PD. The specialist youth mental health model: strengthening the weakest link in the public mental health system. Med J Aust 2007;187:S53-6. https://doi.org/10.5694/j.1326-5377.2007.tb01338.x.
- Singh SP, Paul M, Ford T, Kramer T, Weaver T. Transitions of care from Child and Adolescent Mental Health Services to Adult Mental Health Services (TRACK Study): a study of protocols in Greater London. BMC Health Serv Res 2008;8. https://doi.org/10.1186/1472-6963-8-135.
- Tuomainen H, Schulze U, Warwick J, Paul M, Dieleman GC, Franić T, et al. Managing the link and strengthening transition from child to adult mental health Care in Europe (MILESTONE): background, rationale and methodology. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1758-z.
- Glantz MD, Anthony JC, Berglund PA, Degenhardt L, Dierker L, Kalaydjian A, et al. Mental disorders as risk factors for later substance dependence: estimates of optimal prevention and treatment benefits. Psychol Med 2009;39:1365-77. https://doi.org/10.1017/S0033291708004510.
- Tatlow-Golden M, Gavin B, McNamara N, Singh S, Ford T, Paul M, et al. Transitioning from child and adolescent mental health services with attention-deficit hyperactivity disorder in Ireland: Case note review. Early Interv Psychiatry 2018;12:505-12. https://doi.org/10.1111/eip.12408.
- McNamara N, McNicholas F, Ford T, Paul M, Gavin B, Coyne I, et al. Transition from child and adolescent to adult mental health services in the Republic of Ireland: an investigation of process and operational practice. Early Interv Psychiatry 2014;8:291-7. https://doi.org/10.1111/eip.12073.
- Price A, Janssens A, Woodley AL, Allwood M, Ford T. Review: experiences of healthcare transitions for young people with attention deficit hyperactivity disorder: a systematic review of qualitative research. Child Adolesc Ment Health 2019;24:113-22. https://doi.org/10.1111/camh.12297.
- Newlove-Delgado T, Ford TJ, Stein K, Garside R. ‘You’re 18 now, goodbye’: the experiences of young people with attention deficit hyperactivity disorder of the transition from child to adult services. Emot Behav Diff 2018;23:1-14. https://doi.org/10.1080/13632752.2018.1461476.
- The King’s Fund . What Is Commissioning and How Is It Changing? 2017. www.kingsfund.org.uk/publications/what-commissioning-and-how-it-changing (accessed August 2019).
- Sandford M. Devolution to Local Government in England. House of Commons Library Briefing Paper Number 07029. London: House of Commons Library; 2019.
- Robson K. The National Health Service in Scotland. SPICe Briefing. Scottish Parliament Information Centre; 2016.
- Health and Social Care Board . Commissioning 2019. www.hscboard.hscni.net/our-work/commissioning/ (accessed September 2019).
- Simpson M. How Is Healthcare in Wales Structured? BMA Briefing Note 2016 n.d. www.bma.org.uk/-/media/files/pdfs/working%20for%20change/doctors%20in%20nhs/brief%20how%20is%20healthcare%20in%20wales%20structured.pdf?la=en (accessed September 2019).
- Health Service Executive . Hospital Charges n.d. www.hse.ie/eng/about/who/acute-hospitals-division/patient-care/hospital-charges/ (accessed September 2019).
- Williams J, Klinepeter K, Palmes G, Pulley A, Foy JM. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics 2004;114:601-6. https://doi.org/10.1542/peds.2004-0090.
- Young S, Adamou M, Asherson P, Coghill D, Colley B, Gudjonsson G, et al. Recommendations for the transition of patients with ADHD from child to adult healthcare services: a consensus statement from the UK adult ADHD network. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1013-4.
- Edwin F, McDonald J. Services for adults with attention-deficit hyperactivity disorder: national survey. Psychiatr Bull 2018;31:286-8. https://doi.org/10.1192/pb.bp.106.012237.
- Martin AM, Fishman R, Baxter L, Ford T. Practitioners’ attitudes towards the use of standardized diagnostic assessment in routine practice: a qualitative study in two child and adolescent mental health services. Clin Child Psychol Psychiatry 2011;16:407-20. https://doi.org/10.1177/1359104510366284.
- Matheson L, Asherson P, Wong IC, Hodgkins P, Setyawan J, Sasane R, et al. Adult ADHD patient experiences of impairment, service provision and clinical management in England: a qualitative study. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-184.
- McCarthy S, Asherson P, Coghill D, Hollis C, Murray M, Potts L, et al. Attention-deficit hyperactivity disorder: treatment discontinuation in adolescents and young adults. Br J Psychiatry 2009;194:273-7. https://doi.org/10.1192/bjp.bp.107.045245.
- Singh SP, Paul M, Ford T, Kramer T, Weaver T, McLaren S, et al. Process, outcome and experience of transition from child to adult mental healthcare: multiperspective study. Br J Psychiatry 2010;197:305-12. https://doi.org/10.1192/bjp.bp.109.075135.
- McLaren S, Belling R, Paul M, Ford T, Kramer T, Weaver T, et al. ‘Talking a different language’: an exploration of the influence of organizational cultures and working practices on transition from child to adult mental health services. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-254.
- Marcer H, Finlay F, Baverstock A. ADHD and transition to adult services – the experience of community paediatricians. Child Care Health Dev 2008;34:564-6. https://doi.org/10.1111/j.1365-2214.2008.00857.x.
- Hall CL, Newell K, Taylor J, Sayal K, Hollis C. Services for young people with attention deficit/hyperactivity disorder transitioning from child to adult mental health services: a national survey of mental health trusts in England. J Psychopharmacol 2015;29:39-42. https://doi.org/10.1177/0269881114550353.
- Creswell JW, Plano Clark VL, Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. London: SAGE Publications Ltd; 2011.
- Bryman A. Integrating quantitative and qualitative research: how is it done?. Qual Res 2006;6:97-113. https://doi.org/10.1177/1468794106058877.
- Greene JC, Caracelli VJ, Graham WF. Toward a conceptual framework for mixed-method evaluation designs. Educ Eval Policy Anal 1989;11:255-74. https://doi.org/10.3102/01623737011003255.
- Royal College of Paediatrics and Child Health . British Paediatric Surveillance Unit n.d. www.rcpch.ac.uk/what-we-do/bpsu/british-paediatric-surveillance-unit (accessed September 2019).
- Royal College of Psychiatrists . Welcome to the Child and Adolescent Psychiatry Surveillance System (CAPSS) n.d. www.rcpsych.ac.uk/improving-care/ccqi/research-and-evaluation/current-research/studies-relating-to-capss (accessed September 2019).
- Knowles RL, Smith A, Lynn R, Rahi JS. British Paediatric Surveillance Unit. Using multiple sources to improve and measure case ascertainment in surveillance studies: 20 years of the British Paediatric Surveillance Unit. J Public Health 2006;28:157-65. https://doi.org/10.1093/pubmed/fdl005.
- Ford T, Stewart R, Downs J, Prince M, Stewart R, Ford T, et al. Practical Psychiatric Epidemiology. Oxford: Oxford University Press; 2019.
- Lynn R, Avis J, Reading R. The British Paediatric Surveillance Unit 30th Anniversary Report: Facilitating Childhood Rare Disease Research for Over 30 Years 2016.
- Jenkins R, Bebbington P, Brugha T, Farrell M, Gill B, Lewis G, et al. The National Psychiatric Morbidity surveys of Great Britain – strategy and methods. Psychol Med 1997;27:765-74. https://doi.org/10.1017/s003329179700531x.
- Gupta J, Hodgins P, McWilliams A. The Child and Adolescent Psychiatry Surveillance System (CAPSS). The Seven Year Report: 2016 2016.
- Eke H, Janssens A, Downs J, Lynn RM, Ani C, Ford T. How to measure the need for transition to adult services among young people with Attention Deficit Hyperactivity Disorder (ADHD): a comparison of surveillance versus case note review methods. BMC Med Res Methodol 2019;19. https://doi.org/10.1186/s12874-019-0820-y.
- Grenier D, Elliott EJ, Zurynski Y, Rodrigues Pereira R, Preece M, Lynn R, et al. Beyond counting cases: public health impacts of national Paediatric Surveillance Units. Arch Dis Child 2007;92:527-33. https://doi.org/10.1136/adc.2006.097451.
- Royal College of Paediatrics and Child Health . Applying to the BPSU to Run a Study on the ‘Orange Card’ Reporting Scheme n.d. www.rcpch.ac.uk/resources/applying-bpsu-run-study-orange-card-reporting-scheme (accessed August 2019).
- Royal College of Psychiatrists . Welcome to the Child and Adolescent Psychiatry Surveillance System (CAPSS) 2018. www.rcpsych.ac.uk/workinpsychiatry/qualityimprovement/researchandevaluation/capss.aspx (accessed May 2019).
- Nicoll A, Lynn R, Rahi JS, Verity C, Haines L. Public health outputs from the British Paediatric Surveillance Unit and similar clinician based systems. J R Soc Med 2000;93:580-5. https://doi.org/10.1177/014107680009301107.
- Porta M. A Dictionary of Epidemiology. Oxford: Oxford University Press; 2016.
- Faraone, Asherson P, Banaschewski T, Biederman J, Buitelaar JK, Ramos-Quiroga JA, et al. ADHD. Nat Rev Dis Prim 2015;1. https://doi.org/10.1038/nrdp.2015.27.
- Office for National Statistics . Estimates of the Population for the UK, England and Wales, Scotland and Northern Ireland n.d. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed September 2019).
- Byford S, Petkova H, Stuart R, Nicholls D, Simic M, Ford T, et al. Alternative community-based models of care for young people with anorexia nervosa: the CostED national surveillance study. Health Serv Deliv Res 2019;9. https://doi.org/10.3310/hsdr07370.
- Eke H, Ford T, Newlove-Delgado T, Price A, Young S, Ani C, et al. Transition between child and adult services for young people with attention-deficit hyperactivity disorder (ADHD): findings from a British national surveillance study. Br J Psychiatry 2019:1-7. https://doi.org/10.1192/bjp.2019.131.
- Sadler K, Vizard T, Ford T, Goodman A, Goodman R, McManus S. The Mental Health of Children and Young People in England 2017: Trends and Characteristics. Leeds: NHS Digital; 2018.
- South London and Maudsley NHS Foundation Trust . About Us: Who We Are 2018. www.slam.nhs.uk/about-us/who-we-are (accessed August 2018).
- NHS . My Health London n.d. https://myhealth.london.nhs.uk (accessed September 2020).
- Office for National Statistics . Ethnicity n.d. www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity (accessed August 2019).
- Ford T, Hamilton H, Meltzer H, Goodman R. Child mental health is everybody’s business: the prevalence of contact with public sector services by type of disorder among British school children in a three-year period. Child Adolesc Ment Health 2007;12:13-20. https://doi.org/10.1111/j.1475-3588.2006.00414.x.
- Ogundele MO. Transitional care to adult ADHD services in a North West England district. Clin Gov 2013;18:210-9. https://doi.org/10.1108/cgij-01-2013-0001.
- Office for National Statistics . 2011 Census Data n.d. www.ons.gov.uk/census/2011census/2011censusdata (accessed August 2019).
- Health Service Executive . Fifth Annual Child and Adolescent Mental Health Service Report 2012–2013 n.d. www.hse.ie/eng/services/publications/mentalhealth/camhs12,13.pdf (accessed September 2019).
- Gershon J. A meta-analytic review of gender differences in ADHD. J Atten Disord 2002;5:143-54. https://doi.org/10.1177/108705470200500302.
- Skogli EW, Teicher MH, Andersen PN, Hovik KT, Øie M. ADHD in girls and boys – gender differences in co-existing symptoms and executive function measures. BMC Psychiatry 2013;13. https://doi.org/10.1186/1471-244X-13-298.
- McManus S, Bebbington P, Jenkins R, Brugha T. Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014. Leeds: NHS Digital; 2016.
- Morgan PL, Staff J, Hillemeier MM, Farkas G, Maczuga S. Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics 2013;132:85-93. https://doi.org/10.1542/peds.2012-2390.
- Care Quality Commission . Are We Listening? Review of Children and Young People’s Mental Health Services 2018. www.cqc.org.uk/sites/default/files/20180308b_arewelistening_report.pdf (accessed September 2019).
- Appleton S PK. Planning Mental Health Services for Young Adults – Improving Transition. A Resource for Health and Social Care Commissioners. London: National Mental Health Development Unit; 2011.
- Swift KD, Sayal K, Hollis C. ADHD and transitions to adult mental health services: a scoping review. Child Care Health Dev 2014;40:775-86. https://doi.org/10.1111/cch.12107.
- NICE . Attention Deficit Hyperactivity Disorder Overview: NICE Pathway 2017. https://pathways.nice.org.uk/pathways/attention-deficit-hyperactivity-disorder (accessed September 2019).
- Kroll M, Phalkey RK, Kraas F. Challenges to the surveillance of non-communicable diseases – a review of selected approaches. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2570-z.
- Ford T, Janssens A, Asherson P, Beresford B, Paul M, Ani C, et al. CATCh-US: Children With ADHD in Transition From Children’s Services to Adult Services n.d. www.hra.nhs.uk/planning-and-improving-research/application-summaries/research-summaries/catch-us-children-with-adhd-in-transition-to-adult-services/ (accessed September 2019).
- NHS . The NHS Constitution n.d. www.gov.uk/government/publications/the-nhs-constitution-for-england (accessed September 2019).
- Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Increasing response rates to postal questionnaires: systematic review. BMJ 2002;324. https://doi.org/10.1136/bmj.324.7347.1183.
- Lynn RM, Viner RM, Nicholls DE. Ascertainment of early onset eating disorders: a pilot for developing a national child psychiatric surveillance system. Child Adolesc Ment Health 2012;17:109-12. https://doi.org/10.1111/j.1475-3588.2011.00613.x.
- Royal College of Paediatrics and Child Health . RCPCH Medical Workforce Census 2013 n.d. www.rcpch.ac.uk/sites/default/files/RCPCH_medical_workforce_census_2013_-_main_findings.pdf (accessed September 2019).
- Royal College of Psychiatrists . Census 2017: Workforce Figures for Consultant and Specialty Doctor Psychiatrists n.d. www.rcpsych.ac.uk/docs/default-source/improving-care/workforce/workforce-census-report-2017.pdf (accessed September 2019).
- Rahi JS, Dezateux C. Capture-recapture analysis of ascertainment by active surveillance in the British Congenital Cataract Study. Invest Ophthalmol Vis Sci 1999;40:236-9.
- Audrey S, Brown L, Campbell R, Boyd A, Macleod J. Young people’s views about consenting to data linkage: findings from the PEARL qualitative study. BMC Med Res Methodol 2016;16. https://doi.org/10.1186/s12874-016-0132-4.
- Wellcome Trust . Summary Report of Qualitative Research into Public Attitudes to Personal Data and Linking Personal Data 2013.
- Kooij JJS, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, et al. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur Psychiatry 2019;56:14-3. https://doi.org/10.1016/j.eurpsy.2018.11.001.
- Asherson P, Chen W, Craddock B, Taylor E. Adult attention-deficit hyperactivity disorder: recognition and treatment in general adult psychiatry. Br J Psychiatry 2007;190:4-5. https://doi.org/10.1192/bjp.bp.106.026484.
- Paul M, Street C, Wheeler N, Singh SP. Transition to adult services for young people with mental health needs: a systematic review. Clin Child Psychol Psychiatry 2015;20:436-57. https://doi.org/10.1177/1359104514526603.
- Belling R, McLaren S, Paul M, Ford T, Kramer T, Weaver T, et al. The effect of organisational resources and eligibility issues on transition from child and adolescent to adult mental health services. J Health Serv Res Policy 2014;19:169-76. https://doi.org/10.1177/1355819614527439.
- Singh SP. Transition of care from child to adult mental health services: the great divide. Curr Opin Psychiatry 2009;22:386-90. https://doi.org/10.1097/YCO.0b013e32832c9221.
- Hall CL, Newell K, Taylor J, Sayal K, Swift KD, Hollis C. ‘Mind the gap’ – mapping services for young people with ADHD transitioning from child to adult mental health services. BMC Psychiatry 2013;13. https://doi.org/10.1186/1471-244X-13-186.
- Taylor N, Fauset A, Harpin V. Young adults with ADHD: an analysis of their service needs on transfer to adult services. Arch Dis Child 2010;95:513-17. https://doi.org/10.1136/adc.2009.164384.
- Zaman R, Arif M, Vaze A, Müller U. Setting up adult ADHD service in the United Kingdom. Cutting Edge Psychiatry Pract 2012;1:170-5. https://doi.org/CEPiP.
- Coghill DR. Organisation of services for managing ADHD. Epidemiol Psychiatr Sci 2017;26:453-8. https://doi.org/10.1017/S2045796016000937.
- Wong IC, Asherson P, Bilbow A, Clifford S, Coghill D, DeSoysa R, et al. Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study. Health Technol Assess 2009;13. https://doi.org/10.3310/hta13490.
- Newlove-Delgado T, Ford TJ, Hamilton W, Stein K, Ukoumunne OC. Prescribing of medication for attention deficit hyperactivity disorder among young people in the Clinical Practice Research Datalink 2005-2013: analysis of time to cessation. Eur Child Adolesc Psychiatry 2018;27:29-35. https://doi.org/10.1007/s00787-017-1011-1.
- Newlove-Delgado T, Ford TJ, Hamilton W, Janssens A, Stein K, Ukoumunne OC. Resumption of attention-deficit hyperactivity disorder medication in early adulthood: findings from a UK primary care prescribing study. Eur Child Adolesc Psychiatry 2019;28:1589-96. https://doi.org/10.1007/s00787-019-01325-5.
- Price A, Janssens A, Dunn-Morua S, Eke H, Asherson P, Lloyd T, et al. Seven steps to mapping health service provision: lessons learned from mapping services for adults with Attention-Deficit/Hyperactivity Disorder (ADHD) in the UK. BMC Health Serv Res 2019;19. https://doi.org/10.1186/s12913-019-4287-7.
- Price A, Newlove-Delgado T, Eke H, Paul M, Young S, Ford T, et al. In transition with ADHD: the role of information, in facilitating or impeding young people’s transition into adult services. BMC Psychiatry 2019;19. https://doi.org/10.1186/s12888-019-2284-3.
- Information Commissioners Office . The Guide to Freedom of Information n.d. www.legislation.gov.uk/ukpga/2000/36/contents (accessed September 2019).
- Office for National Statistics . Output Areas (OA) Boundaries 2016. https://data.gov.uk/dataset/0bf536b7-466f-4e6b-a515-751903972dcf/output-areas-oa-boundaries (accessed September 2019).
- McGarva G. English Government Office Network Regions (GOR) 2017. https://datashare.is.ed.ac.uk/handle/10283/2404 (accessed September 2019).
- QGIS Development Team . QGIS Geographic Information System, Version 2.18 n.d. http://qgis.osgeo.org (accessed September 2019).
- Office for National Statistics . Clinical Commissioning Groups (April 2017) Names and Codes in England (Version 3) 2017. https://data.gov.uk/dataset/6abdac39-adc0-44d0-85ea-30b7d0851ee8/clinical-commissioning-groups-april-2017-names-and-codes-in-england-version-3 (accessed September 2019).
- NHS Scotland . Organisations 2018. www.scot.nhs.uk/organisations/ (accessed September 2019).
- NHS Wales . Structure 2018. www.wales.nhs.uk/nhswalesaboutus/structure (accessed September 2019).
- HSC Northern Ireland . HSC Organisations 2018. http://online.hscni.net/other-hsc-organisations/ (accessed September 2019).
- QGIS . A Free and Open Source Geographic Information System n.d. https://qgis.org (accessed August 2020).
- Office for National Statistics . 2011 Census: Population and Household Estimates for the United Kingdom, March 2011 2013. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/populationandhouseholdestimatesfortheunitedkingdom/2011-03-21 (accessed September 2019).
- UK Data Service . 2011 Census Geography Boundaries 2017. www.statistics.digitalresources.jisc.ac.uk/dataset/2011-census-geography-boundaries-lower-layer-super-output-areas-and-data-zones (accessed September 2019).
- OpenDataNI . Department of Health Trust Boundaries 2016. www.opendatani.gov.uk/dataset/department-of-health-trust-boundaries (accessed September 2019).
- National Records of Scotland . Mid-2005 Population Estimates Scotland 2018. www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/population/population-estimates/mid-year-population-estimates/archive/mid-2005-population-estimates-scotland/list-of-tables#table9 (accessed July 2019).
- Office for National Statistics . Estimates of the Population for the UK, England and Wales, Scotland and Northern Ireland, Mid-2015 2018. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed September 2019).
- University of Exeter . CATCh-US Mapping Study – Map of Services 2018. http://medicine.exeter.ac.uk/catchus/mapping/adhdservices/ (accessed March 2019).
- Love TE, Ehrenberg N, Group SR. Addressing Unwarranted Variation: Literature Review on Methods for Influencing Practice. Wellington: Health Quality & Safety Commission New Zealand; 2014.
- NHS England . Implementing the Five Year Forward View for Mental Health 2016. www.england.nhs.uk/wp-content/uploads/2016/07/fyfv-mh.pdf (accessed March 2019).
- Petrovici DA, Ritson C. Factors influencing consumer dietary health preventative behaviours. BMC Public Health 2006;6. https://doi.org/10.1186/1471-2458-6-222.
- Reed JAN, Cook M, Cook G, Inglis P, Clarke C. Specialist services for older people: issues of negative and positive ageism. Ageing Soc 2006;26:849-65. https://doi.org/10.1017/S0144686X06004855.
- Leavey G, McGrellis S, Forbes T, Fullerton D, Davidson G, Hughes L, et al. Improving Mental Health Pathways And Care for Adolescents in Transition to Adult Services in Northern Ireland (IMPACT) 2018. https://research.hscni.net/sites/default/files/Impact%20report%20final%2016%20April%202018.pdf (accessed April 2019).
- Healthcare Improvement Scotland . Attention Deficit and Hyperkinetic Disorders: Services Over Scotland (Final Report) 2012. www.healthcareimprovementscotland.org/our_work/mental_health/adhd_services_over_scotland/stage_3_adhd_final_report.aspx (accessed March 2019).
- Coghill D. Services for adults with ADHD: work in progress: commentary on . . . specialist adult ADHD clinics in East Anglia. BJPsych Bull 2015;39:140-3. https://doi.org/10.1192/pb.bp.114.048850.
- Crimlisk H. Developing integrated mental health services for adults with ADHD. Adv Psychiatr Treat 2011;17:461-9. https://doi.org/10.1192/apt.bp.109.006924.
- Coghill D, Seth S. Effective management of attention-deficit/hyperactivity disorder (ADHD) through structured re-assessment: the Dundee ADHD Clinical Care Pathway. Child Adolesc Psychiatry Ment Health 2015;9. https://doi.org/10.1186/s13034-015-0083-2.
- NHS England . Atlases 2018. www.england.nhs.uk/rightcare/products/atlas/ (accessed June 2018).
- Swift KD, Hall CL, Marimuttu V, Redstone L, Sayal K, Hollis C. Transition to adult mental health services for young people with attention deficit/hyperactivity disorder (ADHD): a qualitative analysis of their experiences. BMC Psychiatry 2013;13. https://doi.org/10.1186/1471-244X-13-74.
- Cheung KK, Wong IC, Ip P, Chan PK, Lin CH, Wong LY, et al. Experiences of adolescents and young adults with ADHD in Hong Kong: treatment services and clinical management. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0478-x.
- Bailey S, O’Connell B, Pearce J. The transition from paediatric to adult health care services for young adults with a disability: an ethical perspective. Aust Health Rev 2003;26:64-9. https://doi.org/10.1071/AH030064.
- Department of Health and Social Care . The Mandate: A Mandate From the Government to the NHS Commissioning Board: April 2013 to March 2015 2012. www.gov.uk/government/publications/the-nhs-mandate (accessed April 2019).
- NHS England . Implementing the Five Year Forward View For Mental Health 2016.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud 2013;50:587-92. https://doi.org/10.1016/j.ijnurstu.2012.09.010.
- Mulvale G, Nguyen T, Miatello A, Embrett M, Wakefield P, Randall G. Lost in Translation? Care philosophies and transitions between child and youth and adult mental health services: a systematic review. J Ment Health 2016. https://doi.org/10.3109/09638237.2015.1124389.
- Appleton R, Connell C, Fairclough E, Tuomainen H, Singh SP. Outcomes of young people who reach the transition boundary of child and adolescent mental health services: a systematic review. Eur Child Adolesc Psychiatry 2019;28:1431-46. https://doi.org/10.1007/s00787-019-01307-7.
- McCarthy S, Wilton L, Murray M, Hodgkins P, Asherson P, Wong IC. Management of adult attention deficit hyperactivity disorder in UK primary care: a survey of general practitioners. Health Qual Life Outcomes 2013;11. https://doi.org/10.1186/1477-7525-11-22.
- Emmel N. Sampling and Choosing Cases in Qualitative Research: A Realist Approach. London: SAGE Publications Ltd; 2013.
- Ford T, Fowler T, Langley K, Whittinger N, Thapar A. Five years on: Public sector service use related to mental health in young people with ADHD or hyperkinetic disorder five years after diagnosis. Child Adolesc Ment Health 2008;13:122-9. https://doi.org/10.1111/j.1475-3588.2007.00466.x.
- Beresford B, Stuttard L. Young adults as users of adult healthcare: experiences of young adults with complex or life-limiting conditions. Clin Med 2014;14:404-8. https://doi.org/10.7861/clinmedicine.14-4-404.
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006;18:59-82. https://doi.org/10.1177/1525822X05279903.
- Mitchell WS, Beresford BH. Young people with high-functioing autism and Asperger’s syndrome planning for and anticipating the move to college: what supports a positive transition?. Br J Spec Educ 2014;41:151-71. https://doi.org/10.1111/1467-8578.12064.
- Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018;52:1893-907. https://doi.org/10.1007/s11135-017-0574-8.
- Catania JA, Binson D, Canchola J, Pollack LM, Hauck W, Coates TJ. Effects of interviewer gender, interviewer choice, and item wording on responses to questions concerning sexual behavior. Public Opin Q 1996;60:345-75. https://doi.org/10.1086/297758.
- Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks, CA: SAGE Publications Ltd; 2006.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analyzing Qualitative Data. New York, NY: Routledge; 1994.
- Singh I. VOICES Study: Final Report. London; 2012.
- Colver A, Rapley T, Parr JR, McConachie H, Dovey-Pearce G, Le Couteur A, et al. Facilitating the transition of young people with long-term conditions through health services from childhood to adulthood: the Transition research programme. Programme Grants Appl Res 2019;7. https://doi.org/10.3310/pgfar07040.
- Conrad P, Barker KK. The social construction of illness: key insights and policy implications. J Health Soc Behav 2010;51:S67-79. https://doi.org/10.1177/0022146510383495.
- Dumit J. Illnesses you have to fight to get: facts as forces in uncertain, emergent illnesses. Soc Sci Med 2006;62:577-90. https://doi.org/10.1016/j.socscimed.2005.06.018.
- Racine E, Larivière-Bastien D, Bell E, Majnemer A, Shevell M. Respect for autonomy in the healthcare context: observations from a qualitative study of young adults with cerebral palsy. Child Care Health Dev 2013;39:873-9. https://doi.org/10.1111/cch.12018.
- Theule J, Wiener R, Tannock R, Jenkins J. Parenting stress in families of children with ADHD: a meta-analysis. J Emot Behav Disor 2013;21:3-17. https://doi.org/10.1177/1063426610387433.
- Local Government Association . Health and Wellbeing in Rural Areas n.d. www.local.gov.uk/health-and-wellbeing-rural-areas (accessed September 2019).
- Griffiths FE, Armoiry X, Atherton H, Bryce C, Buckle A, Cave J, et al. The role of digital communication in patient-clinician communication for NHS providers of specialist clinical services for young people [the Long-term conditions Young people Networked Communication (LYNC) study]: a mixed-methods study. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06090.
- Wilkins C, Kelly-Dean O, Kail A. Charities, Young People and Digital Mental Health Services 2019. www.thinknpc.org/resource-hub/charities-young-people-and-digital-mental-health-services/ (accessed September 2019).
- Bourdieu P, Richardson JG. Handbook of Theory and Research for the Sociology of Education. New York, NY: Greenwood Press; 1986.
- Bussing R, Zima BT, Belin TR. Differential access to care for children with ADHD in special education programs. Psychiatr Serv 1998;49:1226-9. https://doi.org/10.1176/ps.49.9.1226.
- Bussing R, Zima, B, Gary, F, Mason D, Leon C, Sinha K, et al. Social networks, caregiver strains and utilisation of mental health services among elementary school students at risk for ADHD. J Am Acad Child Adolesc Psychiatry 2003;42:842-50. https://doi.org/10.1097/01.CHI.0000046876.27264.BF.
- Ayyash A, Sankar S, Merriman C, Vogt T, Earl T, Shah S, et al. Multidisciplinary consensus for the development of ADHD services: the way forward. Clin Gov 2013;18:30-8. https://doi.org/10.1108/14777271311297939.
- Ferrin M, Taylor E. Child and caregiver issues in the treatment of attention deficit hyperactivity disorder: education, adherence and treatment choice. Future Neurol 2011;6:399-413. https://doi.org/10.2217/fnl.11.5.
- Carrington IM, McAloon J. Why shared-care arrangements for prescribing in attention deficit hyperactivity disorder may not be accepted. Eur J Hosp Pharm 2018;25:222-4. https://doi.org/10.1136/ejhpharm-2015-000743.
- Mandalia D, Ford T, Hill S, Sadler K, Vizard T, Goodman A, et al. Mental Health of Children and Young People in England, 2017; Professional Services, Informal Support, and Education. Leeds: NHS Digital; 2018.
- Buitelaar JK. Optimising treatment strategies for ADHD in adolescence to minimise ‘lost in transition’ to adulthood. Epidemiol Psychiatr Sci 2017;26:448-52. https://doi.org/10.1017/S2045796017000154.
- Russell AE, Ford T, Williams R, Russell G. The association between socioeconomic disadvantage and attention deficit/hyperactivity disorder (ADHD): a systematic review. Child Psychiatry Hum Dev 2016;47:440-58. https://doi.org/10.1007/s10578-015-0578-3.
- Forbes N, Pearce N, Vizard T, Sadler K, Ford T, Goodman A. The Mental Health of Children and Young People in England 2017: Hyperactivity Disorders. Leeds: NHS Digital; 2018.
- Yassaee A, Hale D, Armitage A, Viner R. The impact of age of transfer on outcomes in the transition from pediatric to adult health systems: a systematic review of reviews. J Adolesc Health 2019;64:709-20. https://doi.org/10.1016/j.jadohealth.2018.11.023.
- Embrett MG, Randall GE, Longo CJ, Nguyen T, Mulvale G. Effectiveness of health system services and programs for youth to adult transitions in mental health care: a systematic review of academic literature. Adm Policy Ment Health 2016;43:259-69. https://doi.org/10.1007/s10488-015-0638-9.
- Crowley R, Wolfe I, Wolfe I, McKee M. European Child Health Systems and Services; Lessons Without Borders. 113: Berkshire: Open University Press; 2013.
- NHS . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/ (accessed 22 January 2020).
- Cortese S, Barbui C. Attention-deficit/hyperactivity disorder (ADHD): from randomised controlled trials to evidence-based clinical services. Epidemiol Psychiatr Sci 2017;26:445-7. https://doi.org/10.1017/S2045796016001177.
- Signorini G, Singh SP, Marsanic VB, Dieleman G, Dodig-Ćurković K, Franic T, et al. The interface between child/adolescent and adult mental health services: results from a European 28-country survey. Eur Child Adolesc Psychiatry 2018;27:501-11. https://doi.org/10.1007/s00787-018-1112-5.
- Buitelaar JK. Optimising treatment strategies for ADHD in adolescence to minimise ‘lost in transition’ to adulthood. Epidemiol Psychiatr Sci 2017;26:448-52. https://doi.org/10.1017/S2045796017000154.
- Ford TJ. Transitional care for young adults with ADHD: transforming potential upheaval into smooth progression. Epidemiol Psychiatr Serv 2020;29. https://doi.org/10.1017/S2045796019000817.
- Young S, Gonzales RA, Fridman M, Hodgkins P, Kim K, Gudjonsson GH. (2018) The economic consequences of attention-deficit hyperactivity disorder in the Scottish prison system. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1792-x.
- Chen Q, Sjölander A, Runeson B, D’Onofrio BM, Lichtenstein P, Larsson H. Drug treatment for attention-deficit/hyperactivity disorder and suicidal behaviour: register based study. BMJ 2014;348. https://doi.org/10.1136/bmj.g3769.
- Chang Z, D’Onofrio BM, Quinn PD, Lichtenstein P, Larsson H. Medication for attention-deficit/hyperactivity disorder and risk for depression: a nationwide longitudinal cohort study. Biol Psychiatry 2016;80:916-22. https://doi.org/10.1016/j.biopsych.2016.02.018.
- Chang Z, Lichtenstein P, Halldner L, D’Onofrio B, Serlachius E, Fazel S, et al. Stimulant ADHD medication and risk for substance abuse. J Child Psychol Psychiatry 2014;55:878-85. https://doi.org/10.1111/jcpp.12164.
- Chang Z, Quinn PD, Hur K, Gibbons RD, Sjölander A, Larsson H, et al. Association between medication use for attention-deficit/hyperactivity disorder and risk of motor vehicle crashes. JAMA Psychiatry 2017;74:597-603. https://doi.org/10.1001/jamapsychiatry.2017.0659.
List of abbreviations
- AADD-UK
- Adult Attention Deficit Disorder-UK
- ACAMH
- Association for Child and Adolescent Mental Health
- ADHD
- attention deficit hyperactivity disorder
- AMHS
- adult mental health services
- ASC
- autism spectrum condition
- BPSU
- British Paediatric Surveillance Unit
- CAG
- Confidentiality Advisory Group
- CAMHS
- Child and Adolescent Mental Health Services
- CAPSS
- Child and Adolescent Psychiatry Surveillance System
- CCG
- Clinical Commissioning Group
- CMHT
- community mental health team
- CMO
- Chief Medical Officer
- CPA
- Care Programme Approach
- CRIS
- Clinical Record Interactive Search
- FOI
- freedom of information
- GP
- general practitioner
- HRA
- Health Research Authority
- HSC
- Health and Social Care
- HSE
- Health Services Executive
- LD
- learning disability
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NRES
- National Research Ethics Service
- PenCRU
- Peninsula Childhood Disability Research Unit
- PPI
- patient and public involvement
- R&D
- research and development
- REC
- Research Ethics Committee
- SD
- standard deviation
- SLaM
- South London and Maudsley NHS Foundation Trust
- SSC
- Study Steering Committee
- UEMS
- University of Exeter Medical School
- UKAAN
- UK Adult ADHD Network
Notes
-
Surveillance study: BPSU baseline notification questionnaire
-
Surveillance study: CAPSS baseline notification questionnaire
-
Mapping study: categorisation of informants by stakeholder group and role (respondent definitions)
-
Mapping study: freedom of information request sent to UK commissioners
-
Mapping study: freedom of information request sent to providing organisations
-
Qualitative study: participant inclusion and exclusion criteria
-
Qualitative study: study information sheet and consent form for pre-transition patients
-
Qualitative study: study information sheet and consent form for post-transition patients
-
Qualitative study: study information sheet and consent form for re-engaged adult patients
-
Qualitative study: study information sheet and consent form for parents
-
Qualitative study: study information sheet and consent form for clinicians
-
Qualitative study: study information sheet and consent form for GPs
-
Qualitative study: topic guide for re-engaged adult patients
-
Full list of academic publications relating to CATCh-uS (including papers being prepared or in submission)
-
Full list of conferences where CATCh-uS findings and methodology was presented (including posters)
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08420).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
