Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 17/45/22. The contractual start date was in September 2018. The final report began editorial review in March 2020 and was accepted for publication in November 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2021 Law et al. This work was produced by Law et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Law et al.
Chapter 1 Context
Parts of this chapter have been reproduced from Law et al. 1,2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
In the 2011 census of England and Wales, nearly one in five people (17.9%) in England and Wales reported having a disability that limited their daily activities. 3 Furthermore, approximately 25% of people with one long-term condition reported having ‘problems walking about’ and ‘problems performing usual activities’; this figure rises to > 60% among people with three or more long-term conditions. 4 In 2016, 24% of men and 31% of women in England aged ≥ 65 years needed help with at least one ‘activity of daily living’ (ADL). 5 The global estimate of disability is approximately 15% of the world’s population, and this figure is rising due to population ageing and the increasing prevalence of chronic diseases. 6
Long-term conditions (also called chronic diseases) are the most common cause of disability in the UK. 4 A long-term condition has been defined as one that cannot currently be cured but can be controlled using medication and other therapies. 7 Examples of long-term conditions are hypertension, coronary heart disease, asthma, chronic obstructive pulmonary disease, diabetes, depression, chronic kidney disease and osteoarthritis. In 2019 in the UK, > 18 million adults (i.e. aged ≥ 18 years) had a long-term condition (i.e. 38% of the total adult population). 8 Long-term conditions constitute the biggest burden on the NHS, being the reason for more than half of all general practitioner (GP) consultations, 65% of outpatient visits and 70% of inpatient bed-days. 4 The prevalence of long-term conditions rises with age, affecting 50% of people aged > 50 years and 80% aged > 65 years. 8 In particular, older populations often have more than one condition (multimorbidity) and, as the population ages, the number of people with two or more conditions is projected to increase. 9 As older people accumulate more long-term conditions, they can also become increasingly frail. This is a consequence of accumulated age-related defects in different physiological systems,10 with frail older adults at the highest risk of adverse outcomes such as falls, disability, admission to hospital and the need for long-term care. 11,12 Treatment and care for people with long-term conditions is estimated to account for around £7 in every £10 of total health and social care expenditure. 4 This increasing prevalence of long-term conditions is one of the biggest challenges facing our health and social care systems. 4
Physical functioning
Physical capability, a concept also referred to as ‘physical functioning’, is a term used to describe an individual’s capacity to undertake the physical tasks of everyday living. 13 Poor physical functioning is associated with negative outcomes, including higher risk of 30-day hospital re-admission,14 increased morbidity and mortality15,16 and long-term disability. 12,17 Multimorbidity predicts future functional decline, which is more marked with increasing numbers of conditions and with condition severity. 18 Worsening physical function also affects older adults with long-term conditions in terms of health and independence, and may have an impact on how they perceive their overall health and symptom management. 19 Thus, physical function is one of the most important factors in quality of life among older adults,19,20 and optimising and preserving physical functioning should be a central goal for all people with long-term conditions. Increasing awareness about the important relationship between physical function and overall health status is likely to lead to improvement in care for people with long-term conditions. 21,22
Physical activity
A different, but related, concept is physical activity, defined as ‘any bodily movement produced by skeletal muscles that results in energy expenditure’. 23 ‘Physical activity’ refers to what one actually does (i.e. a behaviour), rather than just the capacity to do something. Habitual performance of at least minimal levels of recommended physical activity is important for preventing and managing long-term conditions, with positive effects comparable to those from optimal medication. 24 Previous studies of middle-aged and older adults show that more physically active people have better levels of physical functioning. 13,25–28 Indeed, physical inactivity, or sedentarism, is one of the strongest predictors of physical disability in older people. 29,30 The proposed process behind this association is that physical activity helps to maintain muscle and cardiac function, improves gait, balance and mood, and subsequently prevents functional decline. 31–34 Moreover, regular physical activity prevents or improves conditions that underlie disability in older adults, including falls,35 hip fracture,36 cardiovascular disease,37 diabetes,38 obesity39 and frailty,40 with longitudinal studies suggesting that regular physical activity is associated with reduced mortality. 41 Several studies have also demonstrated the benefits of physical activity for psychosocial functional outcomes in older adults. 42–44
There are known benefits of physical activity for the management of long-term conditions and particularly for improving physical function. 40,45–50 Despite this evidence, the proportion of the adult population in England and Wales reporting moderate levels of physical activity (i.e. participating in moderate physical activity for at least 30 minutes, five times per week) was 66% in 2017/18,51 22% were classified as inactive (i.e. participating in < 30 minutes of physical activity per week), and increasing age associated with less physical activity. However, individuals overestimate the amount of physical activity they do in self-reported surveys and so the true situation is likely to be worse. For example, objective measurements of physical activity collected using accelerometery have demonstrated that only 6% of men and 4% of women meet the recommended activity guidelines, suggesting considerably lower levels of participation. 52
Levels of physical activity in people with long-term conditions are even lower, and an inverse association has been found between physical activity and multimorbidity. 53,54 The worldwide economic burden of physical inactivity has been estimated to be at least £51.5B per year55 and the estimated annual direct cost of physical inactivity to the NHS across the UK is £1.06B. 56 This is not just a UK issue, as the World Health Organization has the target of achieving a 10% reduction in physical inactivity by 2025. 57
Public Health England launched ‘One You’, the first nationwide campaign to address preventable disease in adults. This aimed to encourage people, particularly adults in middle age, to take control of their health by ‘moving more’ to enjoy significant benefits now and in later life. 58 In addition, the importance of physical activity and physical function was emphasised in the ‘Start Active, Stay Active’ report from the four home countries’ Chief Medical Officers on physical activity for health. 59 The variation in physical function that exists among people as they age was acknowledged and the report gave recommendations for groups of older adults with different functional status and activity needs, including the following:
-
People who are already active, through daily walking, an active job or engaging in regular recreational or sporting activity. This group may benefit from sustaining their current activity levels and potentially by increasing their general activity or introducing an additional activity to improve specific aspects of fitness or function.
-
People whose function is declining owing to low levels of activity and excessive sedentary time, who may have lost muscle strength, or are overweight but otherwise remain reasonably healthy. This is the largest group with a great deal to gain from changing behaviour, restoring function and preventing disease.
-
People who are frail or have very low physical or cognitive function, perhaps as a result of old age or long-term conditions such as arthritis and dementia. This group requires a therapeutic approach (e.g. falls prevention programmes) and many will be in residential care.
In Wales, the Well-being of Future Generations (Wales) Act 201560 put in place seven well-being goals, including ‘a heathier Wales’. A strategic aim of this policy is ‘to encourage more adults to be more active, more often, throughout life’.
The important role of primary care
In total, 90% of patient interaction with the NHS occurs in primary care and people with long-term conditions are in regular contact with primary care services. 7 The management of these conditions has been strongly influenced by the Quality and Outcomes Framework,61 which emphasises disease-centred outcomes and the recording of risk factors, such as blood pressure and body weight, rather than the assessment of physical activity and physical function. Although managing disease remains important, placing more emphasis on functional limitations, such as whether or not people can perform ADLs, has the potential to improve care for people with long-term conditions. Organisational interventions targeted on patient-specific difficulties (e.g. functional ability) appear to be more effective than generic interventions,62 especially when the intervention is more comprehensive and integrated into routine care. 63
Physical activity could be promoted in primary care by making physical activity an explicit element of regular behavioural risk factor screening, patient education and referral, as well as developing and maintaining strong links between primary care settings and local community-based opportunities. Patients can be referred from primary care to exercise referral schemes. 64 However, the effectiveness of these schemes is limited by low rates of recruitment and retention. 65 There are several possible reasons for this. First, the benefits of physical activity and fitness are poorly taught in medical education. 66 Second, referral to these schemes is not routine in primary care management of long-term conditions. Third, these gym-based schemes may appear irrelevant to people’s day-to-day lives. A different approach is warranted. Interventions could also be widened to include community care, as primary and community care are increasingly integrated. Further examples of areas for integration include social care, leisure services and the third sector.
International examples of importance include the ‘Exercise is Medicine’67 movement in the USA and the Canadian Chronic Care model, which takes the perspective that function is the ‘sixth vital sign’. 22 A multicomponent rehabilitation intervention including function-based individual assessment and action planning, rehabilitation self-management workshops, online self-assessment of function, and organisational capacity-building has been explored in a Canadian primary health-care setting. 21 This functional approach is different from the medical model of illness that focuses on the diagnosis, categorisation and medication of disease. 68 Rather, it concentrates on functional limitations, such as whether or not people can perform ADLs. 69 In addition, to improve care for people with long-term conditions, it has been suggested that there is a need to shift away from a reactive, disease-focused, fragmented model of care towards one that is proactive, holistic and preventative. 63 Similarly, the chronic care model, which has influenced health policy around the world, also stresses the need to transform health care for people with long-term conditions from a system that is largely reactive in responding mainly when a person is sick to one that is much more proactive and focuses on supporting patients to self-manage. 70
Systematic reviews and guidelines
Previous systematic reviews and guidelines have explored the effects of physical activity interventions in sedentary adults and people with multimorbidity, osteoarthritis, obesity and chronic pain in the primary care setting. 45,71,72 They have also explored barriers to and facilitators of physical activity and the effectiveness of different intervention ‘deliverers’. 73,74 However, although the links between physical activity and physical function are evident and the benefits of physical activity are clear, the best way for primary care to help people with long-term conditions increase physical activity is unclear.
The National Institute for Health and Care Excellence (NICE) guidelines for the clinical assessment and management of multimorbidity recommend that functional assessments, such as objective measurement of gait speed and grip strength and subjective patient self-reported health status, should be used in primary care to assess frailty. 71 NICE has also issued guidelines for the prevention of frailty, disability and dementia in mid-life by increasing habitual physical activity. 75 NICE recommends that campaigns should promote the message that it is not inevitable for older people to experience sustained ill health, it is possible to reduce the risk and severity of dementia, disability and frailty, and, although it is better to make changes earlier in life, even changing behaviours in mid-life can bring about health gains. Moreover, NICE recommends that future research should focus on determining the most effective and cost-effective mid-life services and interventions, including how these can be delivered in a consistent and sustainable manner.
In summary, insufficient habitual physical activity levels are most apparent in those with long-term conditions. However, despite the benefits of physical activity for physical (and psychosocial) functioning and the regular contact with primary care for long-term condition management, primary care interventions to increase physical activity for people with long-term conditions are used in only a limited way in the UK NHS. Therefore, a better way for primary care to help reduce functional decline and promote physical activity is needed. 76 This includes a consideration of changes in the culture of primary care and an understanding that physical activity promotion is an important health promotion activity and long-term condition management, as well as having the tools available to assist the workforce and change behaviour.
Rationale for a realist approach
Optimising physical function and physical activity is likely to involve a complex intervention, drawing on a range of resources that activate different participant responses. 77 Therefore, a methodology that focuses on this complexity is required. A realist approach recognises how ‘patterning of social activities are brought about by the underlying mechanisms constituted by people’s reasoning, and the resources they are able to summon in a particular context’ (p. 220). 78
Realist methods examine the interplay between different contexts and mechanisms that underpin interventions in primary care to improve physical activity and physical function for people with long-term conditions, and how these different contexts and mechanisms lead to different outcomes.
The rationale for using realist synthesis, as opposed to a systematic non-realist review, is that through the identification of context, mechanism and outcome (CMO) configurations it provides a contextualised explanation of ‘what works, for whom, in what circumstances, in what respects and why’. 79 It has also been recommended that the research community should shift from designing and testing small-scale interventions to change individual behaviour towards expanding the evidence on strategies for translating, disseminating, implementing and scaling up effective policy and practice for physical activity promotion worldwide. 80 As increasing habitual physical activity plays an important role in maintaining and improving physical function, this synthesis considers these issues. It also explores the potential for a ‘culture shift’ in the focus of NHS general practice from a disease-centred approach, emphasising diagnosis, categorisation and medication, to one that promotes overall function and well-being.
A key part of realist synthesis is the interrogation of relevant theory-rich literature. However, realist evidence syntheses are also participatory in nature, drawing on the lived experiences of service users and professionals providing services to identify ‘nascent’ theories based on individual experiences. 78 To enable this, creative methods from the field of co-design were used to ensure that the views of all stakeholders were included and embedded in the review process. The co-produced theory and ideas from these stakeholders were fed back into the literature searches, refining the search criteria, adding an interpretative frame to interrogate the literature, and corroborating and refuting the evidence. The resulting theories then informed a co-design stage, during which they were refined and prioritised before being used to generate implications for service innovation and implementation. 1
Aims and objectives
-
To identify and produce a taxonomy of physical activity interventions that aim to reduce functional decline in people with long-term conditions managed in primary care.
-
To work with patients, health professionals and researchers to uncover the complexity associated with the range of physical activity interventions in primary care, and how they directly or indirectly affect the physical functioning of people with long-term conditions.
-
To identify the mechanisms through which interventions bring about functional improvements in people with long-term conditions, and the circumstances associated with the organisation and operation of the interventions in different primary care contexts.
-
To understand the potential impacts of these interventions across primary care and other settings, such as secondary health care and social care, paying attention to the conditions that influence how they operate.
-
To co-produce an evidence-based, theory-driven explanatory account in the form of refined programme theory to underpin and develop a new intervention through a co-design process with patients, health professionals and researchers. 1
Chapter 2 Methodology and theory-building stakeholder workshops
Parts of this chapter have been reproduced from Law et al. 1,2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
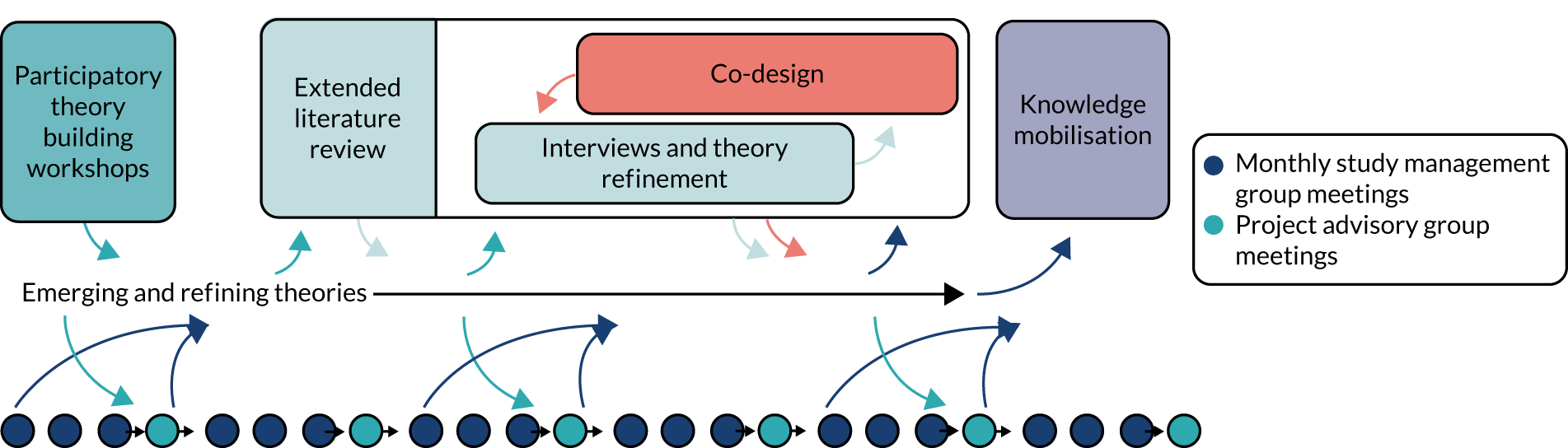
This project involved a realist synthesis of literature, with input from key stakeholders, public contributors and study management and advisory groups. Co-production was embedded throughout and included a co-design process where intervention ideas were developed. The process was iterative, with data sources informing each other as the synthesis progressed (Figure 1).
FIGURE 1.
Schematic showing the iterative, integrated flow of information throughout the synthesis. Arrows indicate how each element informed another. The Study Management Group and Project Advisory Group meetings continuously informed the synthesis throughout the life of the project, and both groups involved input from public members.
Co-production of the short title and acronym
Members of the study management group, including public research partners, worked together to develop the short title of the study ‘Function First’ and the strapline ‘Be Active, Stay Independent’. We first discussed project keywords and gathered suggestions to develop 11 options. The final version was chosen following a vote and subsequent discussion.
Summary of the overall methods
We used Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) methodological guidance and standards to inform our application of realist methods. 81
The first stage of the synthesis developed initial theories about how and why primary care interventions aiming to improve physical function and physical activity among patients with long-term conditions work (or may not work), for whom, and in which circumstances. These theories were developed through two theory-building stakeholder workshops and an early scoping search of published and grey literature. This phase informed theory development and literature searches by helping to develop a shared understanding of the key topic areas and stimulate initial ideas.
Following the theory-building workshops, a list of ‘if . . . then’ statements were created, and the search strategy and inclusion and exclusion criteria were developed and refined. The ‘if . . . then’ statements also formed part of the activities included in the first co-design workshop, where stakeholders took part in activities and games to familiarise themselves with the emerging ideas and match different statements.
After an initial sift of titles and abstracts, we refined our inclusion and exclusion criteria a second time and identified relevant systematic reviews. We created an evidence table to capture relevant realist critique from the systematic reviews. This evidence table and the ‘if . . . then’ statements were then used to develop eight emerging ‘theory areas’. To explore these theory areas, we then conducted 10 individual ‘theory-refining’ interviews with stakeholders. These theory areas were explored during the second co-design workshop, with stakeholders considering how particular intervention assets related to the theory areas.
Data were extracted from papers that were identified as rich and relevant to the eight theory areas, including individual qualitative and quantitative studies, guidelines and the grey literature. Through this process, and iterative discussion, we developed initial ‘candidate’ CMO statements. These were further refined and tested through the organisation of extracted information into evidence tables representing the different sources of evidence, including the individual stakeholder interviews. This enabled exploration of confirming or refuting evidence. We also developed a taxonomy of primary care physical activity interventions for people with long-term conditions.
The CMOs formed part of the final co-design and knowledge mobilisation workshops, where participants considered the emerging CMOs and how they were embodied within the co-designed resources. The ‘final’ five CMO statements were then defined, alongside the co-designed ‘Function First’ product.
As this was an iterative process, there were some changes to the original protocol, and these changes are outlined in more detail below.
Changes to the original proposal
Figure 2 shows the original schematic of project progression.
FIGURE 2.
The original schematic of project stages. See Figure 1 for the actual process of project progression.
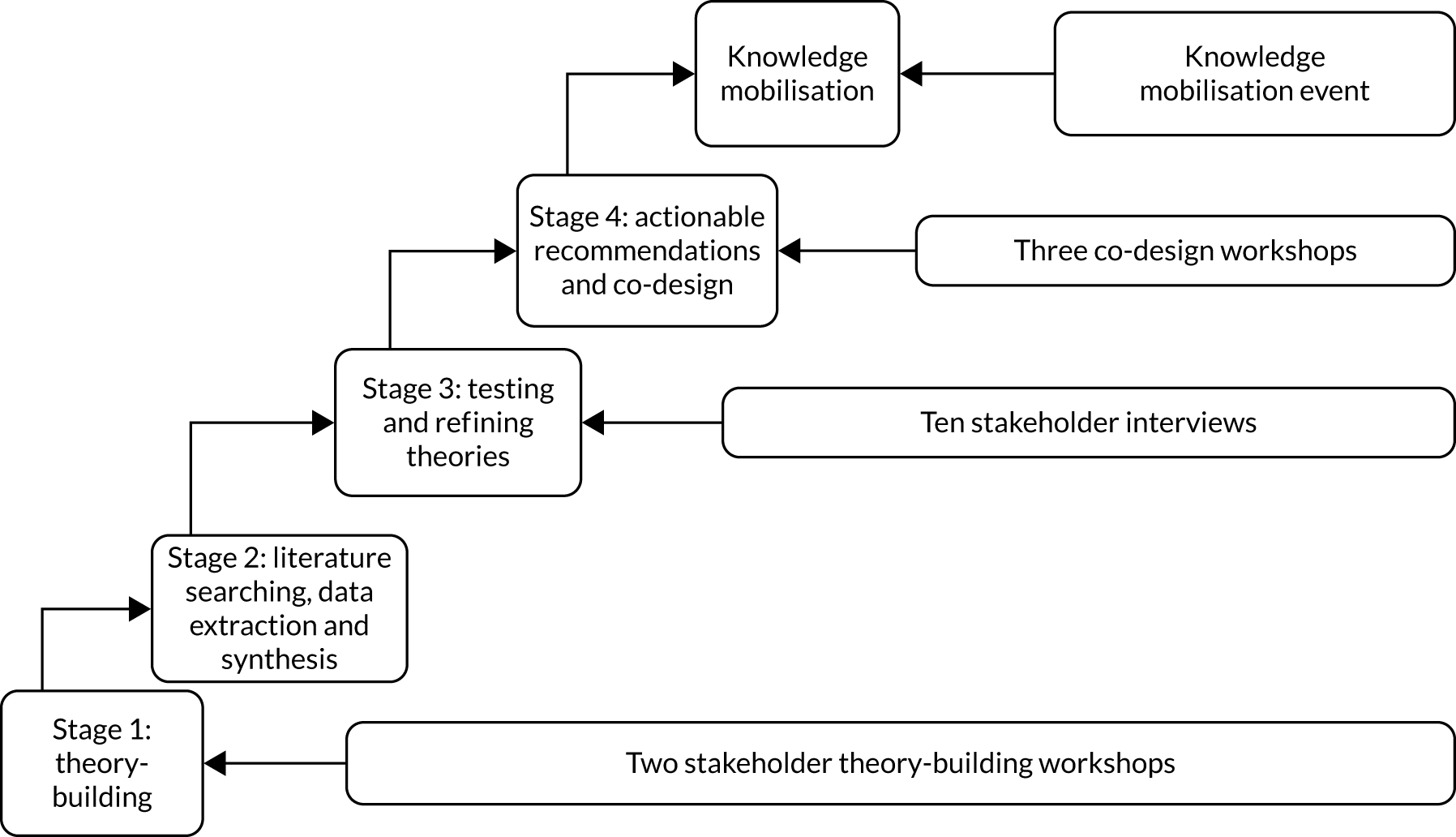
All elements of the protocol were completed as planned. However, there was more overlap in the stages than originally anticipated because of the large evidence base in the areas of physical activity, physical function and primary care for people with long-term conditions. This meant that:
-
We discussed emerging ‘theory areas’ with stakeholders in the theory-refining interviews, rather than conjectured CMO statements.
This was necessary to enable refinement of the key emerging theories and to avoid artificially ‘jumping ahead’ to CMO development. It allowed for a deeper understanding of the areas involved, strengthening the eventual theories developed.
-
The CMOs were not finalised before the first co-design workshops began and developed further as we progressed through the workshops.
The integration of CMO development with the co-design workshops was an unanticipated strength of the research process and meant that the refinement of the final CMOs benefited greatly from further stakeholder input, including suggestions for additional literature searches. In addition, the co-design process was not limited by a final set of CMO statements and was more authentic as a result. Chapter 6 discusses this further.
Data sources, analysis and synthesis
The data sources and how they were analysed and synthesised are described in the following sections. The realist synthesis of literature including stakeholder interviews, co-design workshops and knowledge mobilisation event are described in the Chapters 3 and 4.
Early scoping exercise of published and grey literature
To gain familiarity with the literature and aid with the identification of keywords, we carried out a preliminary scoping of the literature to retrieve reports, theses, key articles, systematic reviews and any relevant websites to help inform our formal search strategy. This scoping exercise was informed by previous work in this area,82–84 proposal work-up, early study management, and Project Advisory Group meetings and discussions with patient and public representatives.
Theoretical landscape
As part of the above scoping exercise and to stimulate early thinking about important areas, we identified the overarching theories and frameworks that we determined as likely to inform the realist synthesis. We drew from theories that address a wide social context including theories and models relating to physical function (e.g. International Classification of Functioning, Disability and Health69); environmental factors and individual compensation strategies;85 psychological theories of motivation, behaviour and behaviour change relevant to patients and health professionals (e.g. self-efficacy and self-determination theory,86,87 intention and behaviour,88 health beliefs, planned behaviour);89,90 interventions based around Capability, Opportunity, Motivation – Behaviour (COM-B) principles;91,92 and the self-regulation of illness,93,94 sociological theory (e.g. governmentality,95 habitus,96 social and peer support97,98); implementation theories (e.g. diffusion,99 knowledge to action100); and organisational theories relevant to how interventions fit into different ways of delivering services and pathways. 1,101,102
Stakeholder analysis
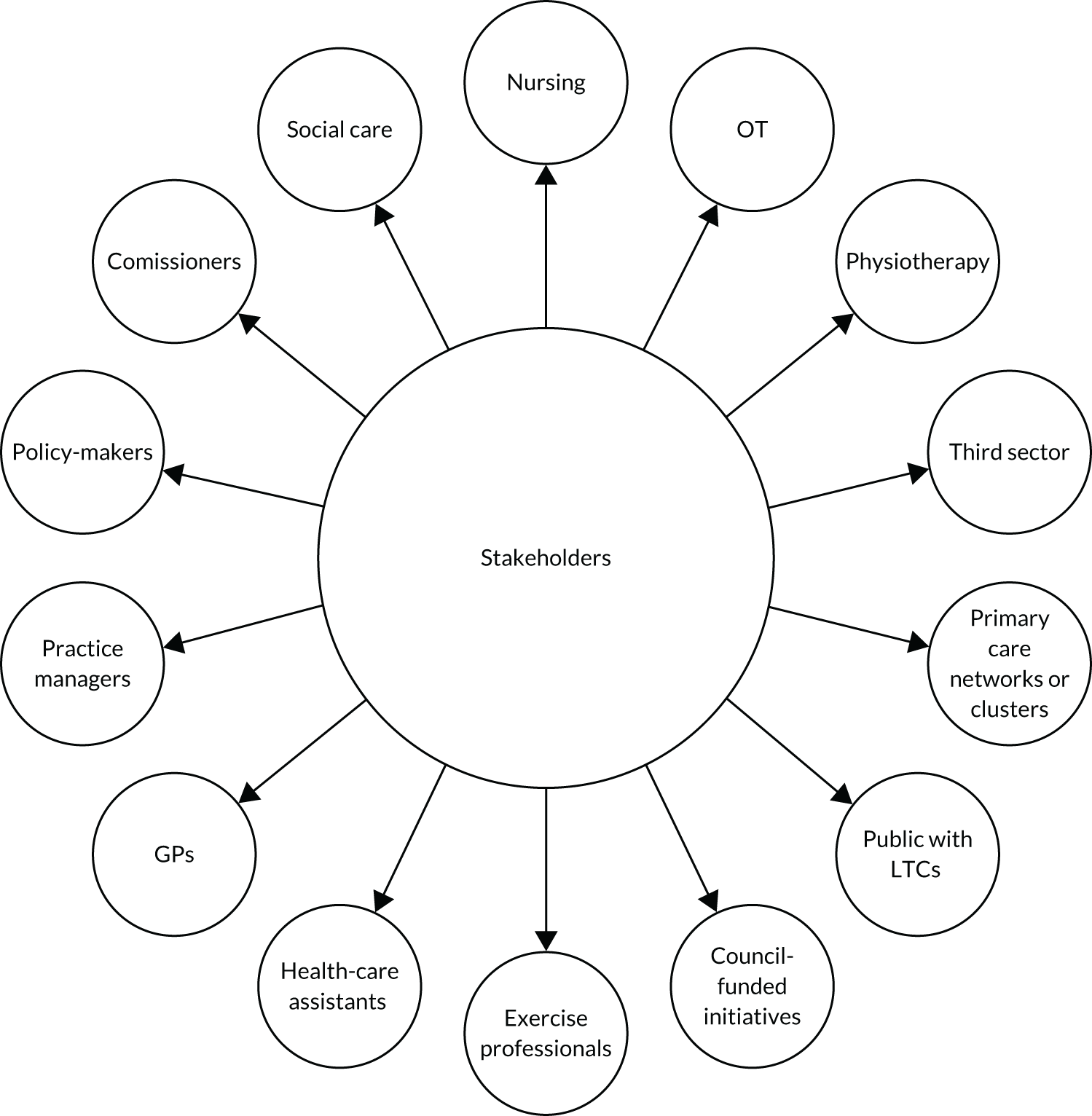
An initial stakeholder analysis helped us to identify and target the most relevant groups for the different stages of the synthesis. 103 It included representation from people with long-term conditions, primary care professionals working in general medical practices, allied health professionals, third-sector organisations, council-funded initiatives, social care, policy-makers and commissioners of services (Figure 3). The stakeholder analysis was used to ensure that no particularly important groups were missed. The stakeholder analysis took place across two or three study management meetings and one external Project Advisory Group meeting, and involved a process of feedback and iteration. This was consistently monitored, and care was taken to incorporate any missing perspectives. Researchers with knowledge and experience relevant to the syntheses were also identified as stakeholders as the project progressed.
FIGURE 3.
Summary of the stakeholder analysis. LTC, long-term condition; OT, occupational therapy.
Theory-building workshops
Data collection using LEGO® Serious Play®
Creative methods, borrowed from the field of co-design, were employed to structure the two theory-building workshops and elicit the views and experiences of all stakeholder representatives, including a facilitated session using LEGO® Serious Play® (LEGO, Billund, Denmark). This method has been used previously in service improvement work, training of health professionals, and research. 104–108 The specific choice to use LEGO Serious Play as opposed to other participatory approaches was because of the tangibility of working with LEGO. LEGO Serious Play enabled a move from ‘research’ activity into ‘co-design’ activity through making tangible outputs. By using these tangible forms, it set some expectations early on in the programme of work about the transition from intangible to tangible (i.e. from evidence to actionable tools). Participants who attended these two workshops are detailed in Report Supplementary Material 1.
Following a series of skills-building activities, each individual created and described LEGO models (physical metaphors) in response to the following questions: ‘What does physical function mean to you?’ and ‘What are your experiences of maintaining physical function?’.
Participants were encouraged to play with the LEGO as they considered the questions, connecting bricks while they thought. This gave the participants’ hands, and part of their mind, an occupation while they pondered the topic in question. What is built by the end of the reflective period then becomes a physical ‘tool’ that can be used to enhance the expression of those thoughts back to the wider group. We also asked participants to summarise their thoughts in three words written on a Post-it Note (Post-it® Brand; 3M, Cynthiana, KY, USA). As shown in Figure 4a, some participants chose to augment this communication further by using illustrations as well as their LEGO model. This demonstrates one of the core values behind the LEGO Serious Play methods; these media give people a greater opportunity for self-expression (using LEGO model plus verbal description) than the sole use of speech or writing.
FIGURE 4.
Example models built by participants in the theory-building workshops to reflect on and describe their interpretation of (a) what physical function meant to them; (b) how they maintained physical function; and (c) an example of a ‘shared landscape’.

This process helped to develop a shared understanding of the key topic areas and stimulate initial ideas and thoughts for theory development. It exposed researchers involved in the workshop to first-hand lived experiences of people with long-term conditions and professionals working in primary care. These LEGO models were then incorporated into a shared ‘landscape’ to explore which aspects of these experiences helped or hindered the maintenance of physical function (see Figure 4b).
As shown in Figure 4, photographics of the models were captured. Participant descriptions were audio-recorded and then transcribed for analysis and interpretation, and were used to shape emerging theories.
Data analysis workshop
The project team members convened for a face-to-face data analysis workshop to interpret the data gathered from the two LEGO Serious Play workshops. The data from the two workshops comprised anonymised transcripts from the audio-recordings of the workshop dialogue, images of the models, three-word text descriptors and images of the landscapes with annotations. The photograph of the LEGO model and the associated transcribed description were linked so that during the group analysis session it was possible to view the LEGO model and the description from each anonymised participant at the same time. This helped to bring the description in the transcript ‘to life’.
The models themselves served three functions:
-
Building these models aided reflection as people considered the question about their experiences.
-
The models were a tangible visual aid to assist people in their explanation of their reflections, or personal theories in their heads. Once their initial explanation was ‘out’, the explanation became refined through careful probing and ‘cross-examination’ by the facilitator until the explanation stood alone without the need of the model to ‘support’ it.
-
The models acted as a tangible representation for all participants in the workshop of each person’s theories.
The models were built in response to two specific questions; thus, the transcripts and images were divided into the relevant sections for each participant. This enabled consideration of the responses of each individual holistically and in depth. Researchers also returned to the transcription to understand the ‘full picture’ of the dialogue between participants, as it was the ‘connecting’ dialogue between participants’ responses that often illustrated how the threads of explanatory narratives were formed.
The transcripts and image models were divided between the project team members who identified any explanatory statements coming from the participants (see Report Supplementary Material 2). For example, statements that explained why they (or others they knew) had (or had not) done certain things, why some things had or had not happened, why health-care professionals had (or had not) done specific things. To gain familiarity with the process, the copies of the first two examples were shared among project team members who reviewed them together as ‘worked examples’. We discussed the statements that identified and moved towards a shared understanding of what we were all looking for.
In some instances, it was helpful to refer to the images of the individual models, the landscapes and annotations. However, there was common agreement that the annotations had often been stated ‘out loud’ and captured on the audio-recording, and the images of the models were limited in their usefulness. The images occasionally prompted a memory but were considered to be more useful in the moment of creation and immediate explanation (in the participatory theory-building workshops) rather than as a longitudinal record of the event for later analysis. We were seeking the theory in the heads of the stakeholders, and so we were reliant on their explanations. Therefore, the models could be defined as a data extraction tool (i.e. something to elicit the personal theories from stakeholders’ heads into forms that others could engage with). Once this was complete, the model no longer served a purpose as the recorded explanation formed the data. Moreover, the models themselves were not interpreted by the research team; it was the transcripts of participants’ explanations that were used to inform theory-building.
All explanatory statements were highlighted, discussed and compiled into a list of 28 ‘If . . . then . . .’ explanatory statements (see Report Supplementary Material 3). These nascent theories were used to identify early clues to possible ‘contexts’, ‘mechanisms’ and ‘outcomes’. The information from these workshops was then used to refine the literature searches and the inclusion and exclusion criteria. For example, these workshops raised our awareness of the importance of studies detailing the wide range of barriers to and facilitators of physical activity and the implementation of interventions, as well as the range of community-based physical activity opportunities.
Chapter 3 Methods for realist synthesis of the literature
Parts of this chapter have been reproduced from Law et al. 1,2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Literature searching
We reviewed the existing literature to look for evidence that suggested how and for whom physical activity interventions work to optimise physical function in the primary care setting. As interventions or services based in other areas of literature (e.g. secondary care, social services, the voluntary sector, exercise science) also hold relevant insight for the development of the initial programme theories, searches were not restricted. A systematic search strategy was developed and amended for use with the following databases: Cochrane Library, MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycInfo® (American Psychological Association, Washington, DC, USA), Sociological Abstracts, Web of Science™ (Clarivate Analytics, Philadelphia, PA, USA), Applied Social Sciences Index and Abstracts (ASSIA; ProQuest®, ProQuest LLC, Ann Arbor, MI, USA), Social Care Online and Social Care Institute for Excellence (see Report Supplementary Material 4). 1 Keywords were developed from the early scoping exercise and the key themes underpinning the initial programme theories were adapted for each information source as necessary. The searches were run in March 2019 and updated in 2020.
Our searches included adults of all ages and socioeconomic backgrounds. We translated non-English-language papers where relevant and practical. We did not limit our searches by publication date and there was no restriction on the type of publication or study type. We examined published and unpublished literature including research articles, systematic reviews and documents detailing policy and local and national initiatives. We did not search for, or include, studies that had limited transferability to NHS primary care, such as interventions involving pharmacological agents or very technical, high-cost equipment.
Literature initially was screened for relevance to the initial programme theories and cross-checked by two members of the research team. To assist with this, articles were uploaded to Covidence (Melbourne, VIC, Australia) to complete the initial sift. This software enabled multiple members of the team to participate in the sifting out of irrelevant articles.
The review team then followed predefined inclusion and exclusion criteria to remove irrelevant articles (see Report Supplementary Material 5). Thirty per cent of articles were reviewed by two members of the review team, with conflicts resolved through discussion between the two main reviewers and other members of the review team as necessary. As part of these discussions, study team meetings and following the initial theory-building workshops, we iteratively refined the inclusion and exclusion criteria. After this initial phase of double reviewing, the criteria were deemed sufficiently robust, and the remaining articles were reviewed by a single member of the review team. This resulted in a library of 2083 relevant papers. From that library, a purposive sample of 170 papers were selected for data extraction, chosen on the basis that they were the most relevant to the developing theory areas and gave the clearest and richest examples of evidence of interventions aimed at functional improvements in people with long-term conditions, and evidence of how these interventions are organised and operate with different primary care contexts. We supplemented the systematic search with forwards and backwards citation tracking of key articles. We also drew on the expertise of the project team, external Project Advisory Group, patient and public representatives, and other key researchers (nationally and internationally) and organisations to ensure that we did not miss any relevant evidence that may not have been retrieved by our traditional systematic searching methods.
We also carried out a grey literature search by targeting relevant organisations and programmes:
-
organisational websites of professional bodies (i.e. Royal College of General Practitioners, Royal College of Physicians, Royal College of Nursing, Chartered Society of Physiotherapy, Royal College of Occupational Therapists, Academy of Medical Royal Colleges, Royal College of Surgeons, British Association of Sport and Exercise Sciences and Royal College of Psychiatrists)
-
government departments and national centres (i.e. Public Health Wales, Public Health England, National Centre for Sport and Exercise Medicine, UK Faculty of Sport and Exercise Medicine, Sport England, Sport Wales and The King’s Fund)
-
specific organisations and charities for people with long-term conditions
-
Natural Resources Wales and National Parks England.
We also searched the Evidence for Policy and Practice Information and Co-ordinating Centre, NHS Evidence, Social Care Online and OpenGrey. In addition, we conducted an open web search for any grey literature (including from commercial leisure services). We used the grey literature sources to ensure that we had captured information about specific campaigns around physical activity for people with long-term conditions.
As previously described,109 unlike a traditional systematic review, a realist synthesis requires an iterative process for identifying literature. In addition to the systematic review of the literature, we also performed additional purposive searches enabling the initial programme theories developed in stage 1 to be expanded. The purposive searches were as follows:
-
Guidelines: MEDLINE was searched using specific physical function keywords (physical function* OR physical activity OR physical fitness or exercise) with guideline keywords (exp guideline/ OR Guideline$.ti OR (guideline or practice guideline).pt. We also manually checked the websites of major guideline producers: NICE, Centre for Reviews and Dissemination, professional organisations, World Health Organization, Scottish Intercollegiate Guidelines Network and the National Guideline Clearinghouse.
-
Social prescribing: we carried out a MEDLINE search using the phrase ‘social prescribing’ and filtered for recent reviews. We followed up with forwards and backwards citation searching on those reviews and consulted with the project team for additional references.
-
Physical literacy: we carried out a MEDLINE search using the phrase ‘physical literacy’ and filtering for adults only. We also followed up with forwards and backwards citation searching on the papers identified and consulted with the project team.
Data extraction
Consistent with the realist synthesis approach,110 the test for inclusion was whether or not the evidence was ‘good and relevant enough’ to be included. 79 Relevance was defined as the ability of the data to contribute to the programme theory. 81 Assessment of relevance involved seeking any ‘trustworthy nuggets of information to contribute to the overall synthesis’ (p. 90). 111 For example, evidence-rich papers included detailed and reflective descriptions of what it was about interventions that worked (or not) (e.g. papers including qualitative or service evaluation elements), whereas less-rich papers provided limited in-depth description of the intervention and the factors influencing whether or not it worked (e.g. randomised controlled trials with mainly objective outcomes). Rigour or whether or not the quality of the evidence is ‘good enough’ was the research team’s judgement of the credibility of the data, including fidelity, trustworthiness and value. 82
Owing to the large data set, we adopted the following approach to data extraction:
-
We identified all of the systematic reviews and conducted a ‘realist critique’ of all those which were relevant to gather an overview of the evidence available. The realist critique consisted of brief notes describing what information the paper provided about what was working or what was not working to improve physical activity or physical function and why, for whom and in what settings. It enabled us to identify the rich systematic reviews and also increased our awareness of broader patterns in the emerging contexts, mechanisms and outcomes.
-
Using the information from this process and from the stakeholder work, we then developed eight theory areas.
-
To facilitate data extraction, we designed a bespoke data extraction form to ensure that we captured data informing the developing theory areas, including intervention details and any differences in implementation.
-
We then identified literature that was specific to primary care and used the bespoke data extraction form to capture relevant data (see Report Supplementary Material 6).
When discrepancies were encountered, the project team discussed whether or not the evidence provided met the criteria to be included.
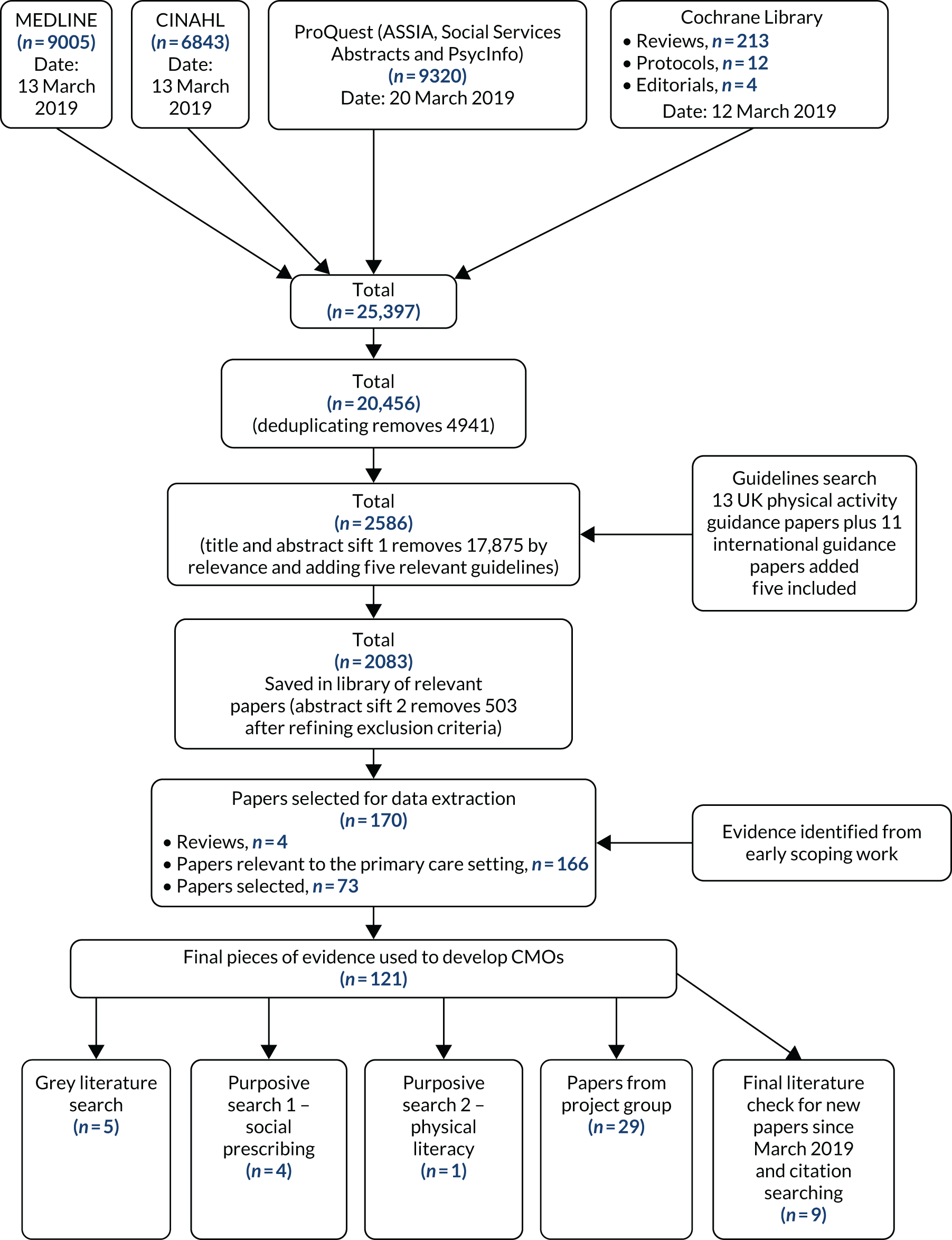
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram depicts the flow of information through the different phases of the synthesis, and details the number and type of papers identified, included and excluded (Figure 5). The list of final included papers is included in Report Supplementary Material 7.
FIGURE 5.
The PRISMA flow diagram detailing the flow of information through the different phases of the review and the purposive searches.
Theory-refining interviews
As part of the iterative process of refining final programme theories, we explored the developing theory areas with stakeholders through 10 qualitative telephone interviews. Purposive sampling of the stakeholders was informed by the stakeholder analysis to provide a range of perspectives, which included three people with long-term conditions, three GPs, two practice nurses, one health-care assistant and one researcher with a background in pedagogy. One of the people with a long-term condition and one of the GPs were also participants in a theory-building workshop. The researcher with a background in pedagogy also participated in a later co-design and knowledge mobilisation workshop.
A semistructured interview topic guide was used to elicit the views of stakeholders on their resonance with the developing theory areas. The approach used in the interviews was a ‘teacher–learner cycle’ whereby the researcher presented the developing theory areas to the stakeholder (‘teaching’) and then verified with the stakeholder where they needed adjusting (‘learning’) to create an improved, refined version and a ‘mutual understanding’ of the developing theories. 1,112
With permission, the telephone interviews were audio-recorded and transcribed verbatim for descriptive analysis of the key themes, which contributed to refinement of the theories. 1 NVivo version 12 (QSR International, Warrington, UK) was used to organise the data. Coding linked the themes with the developing theories.
Synthesis of evidence from literature and interviews
This analytical stage involved synthesising the evidence to elicit relationships between the contexts, mechanisms and outcomes. Through the research team’s experience of conducting realist syntheses,82,108,113 suggestions from Pawson and Tilley,78 and underpinned by the principles of realist enquiry, we used the following approach:
-
organisation of extracted information into evidence tables representing the different bodies of evidence
-
developing themes across evidence tables in relation to emerging patterns among the developing programme theories to seek confirming or refuting evidence
-
linking patterns to develop hypotheses that support or refute the developing programme theories. 1
Three very early ‘conjectured’ CMO configurations focused primarily on early themes of primary care culture, providing advice adapted to individual circumstances, and the confidence and behaviour of primary care health professionals. We then developed two overarching CMOs with further explanatory subthemes based on the theory areas, covering organisational and system-wide influences, as well as influences affecting people with long-term conditions at an individual level. However, to clearly acknowledge the interactions between systemic and individual factors, and after incorporating additional evidence and discussion, we settled on five ‘final’ CMOs. These provided further nuance and depth to the initial CMOs and expanded on the area around credibility.
Following this process, a set of synthesised statements were written together with a narrative summarising the nature of the links between context, mechanism and outcome (i.e. what works, for whom and in what circumstances). This also summarised the evidence underpinning the statements (see Chapter 5). This process involved ongoing, iterative discussion among the project team members and the Project Advisory Group, which included public contributors.
Taxonomy
Alongside the evidence synthesis process, we developed a taxonomy of primary care physical activity interventions for people with long-term conditions, which categorised and provided examples of interventions in the following categories:
-
brief interventions
-
telephone interventions
-
online/‘eHealth’ interventions
-
exercise referral schemes
-
community navigators
-
referral to exercise specialists
-
intervention delivery by existing primary care staff
-
physical activity pathways
-
practice-wide initiatives
-
community initiatives
-
whole-system approaches to embed physical activity promotion in clinical practice
-
multifaceted interventions.
Chapter 4 Methods for co-design and knowledge mobilisation workshops
Parts of this chapter have been reproduced from Law et al. 1,2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
A team of design researchers facilitated three consecutive co-design workshops, involving purposively sampled stakeholders, which included people with long-term conditions; primary care clinicians such as GPs, nurses and therapists; practice managers; service delivery managers; commissioners; and researchers. As much as possible, the three co-design workshops included the same group of participants in each, so that ongoing ideas could be developed and expanded during each workshop. There were key ‘deliverables’ from each workshop and, between workshops, designers worked to develop ideas and provocations for the next workshop, termed ‘design activities’. Although described separately here, the content of these workshops was informed by the developing theory areas, facilitated development of the CMO configurations and eventually helped to refine the ‘final’ programme theories.
Participants
The participants at each workshop were key ‘data sources’ (see Report Supplementary Material 1). Public contributors had a range of long-term conditions including hypertension, previous stroke, cancer and chronic obstructive pulmonary disease. Some professional contributors also described their own experiences of living with a long-term condition as well as providing care for someone with a long-term condition.
Workshop 1 (immersion)
The first activities in this workshop were card games designed to enable participants (in three small mixed groups) to immerse themselves in the evidence and apply it to the context of their own experiences and beliefs, and those of their group peers. This was about developing a nascent, shared understanding based on the evidence available to the whole co-design group both from the literature review and from their own experience.
The two components of the ‘If . . . then’ statements were divided into two decks of cards. The three components of emergent CMOs were also divided into three decks of cards and the eight emergent theory areas were added as a separate deck of cards. The participants were divided into three groups, each containing a mix of project team members, people with long-term conditions, health-care professionals, service providers, managers and other researchers. The cards were shuffled and the participants in each group were challenged to find matching pairs or trios, and to critically reflect on the theory areas in the context of their own experiences. The format of this activity as a card game created an informal and equal environment. People took turns to draw cards, discuss them and then move on to the next ‘player’. This engaged everyone in the group without requiring reference to rules or formal facilitation by a leader. The cards themselves and the notion of this as a card game facilitated this process and supported the agency of all the participants, removing any perceived hierarchy in the group. The groups made their own notes, edited cards if they wished and added cards as they felt necessary (Figure 6).
FIGURE 6.
Illustration of the ‘If . . . then’ card game (a) and sample images of the cards edited by participants (b, c).
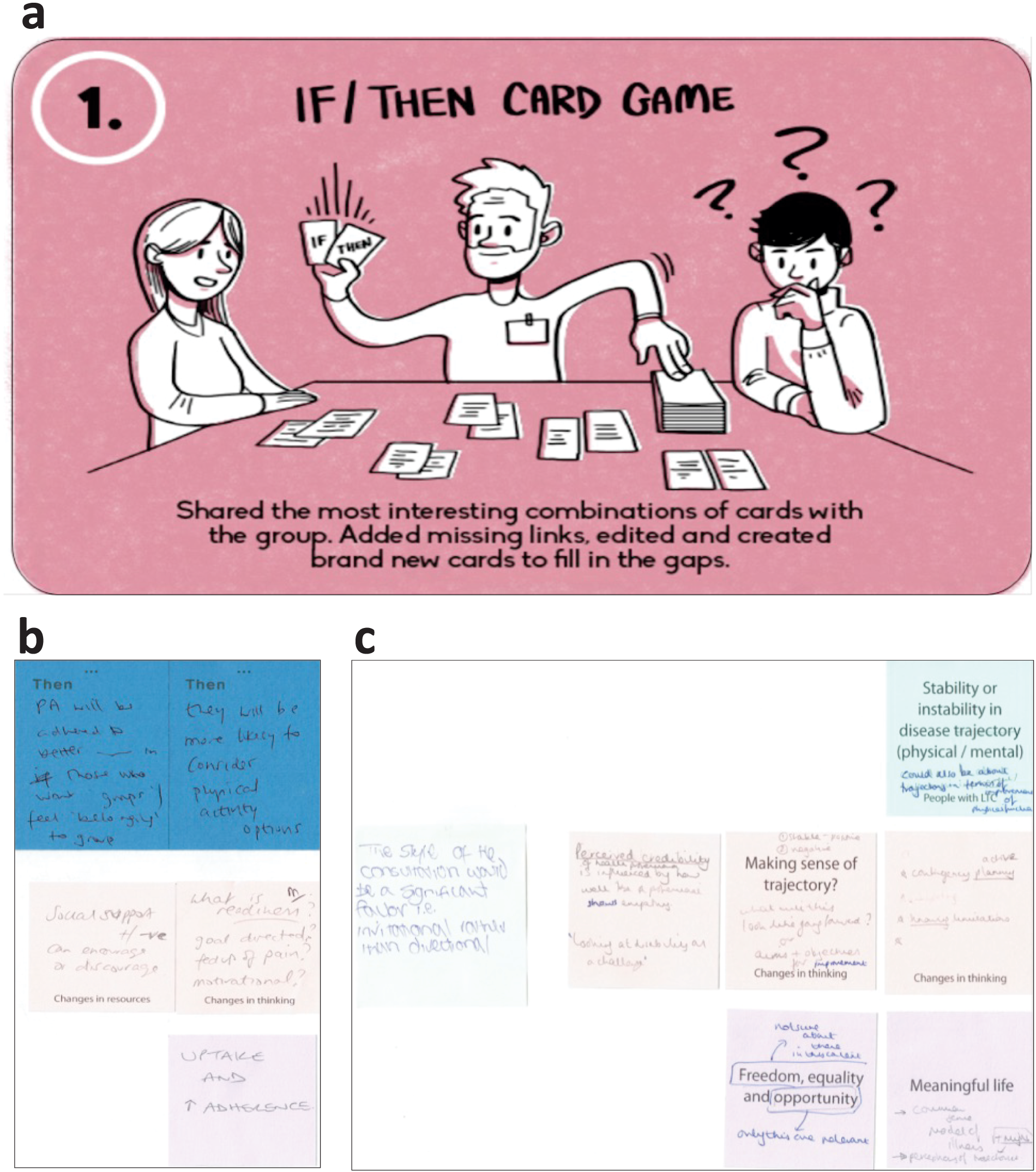
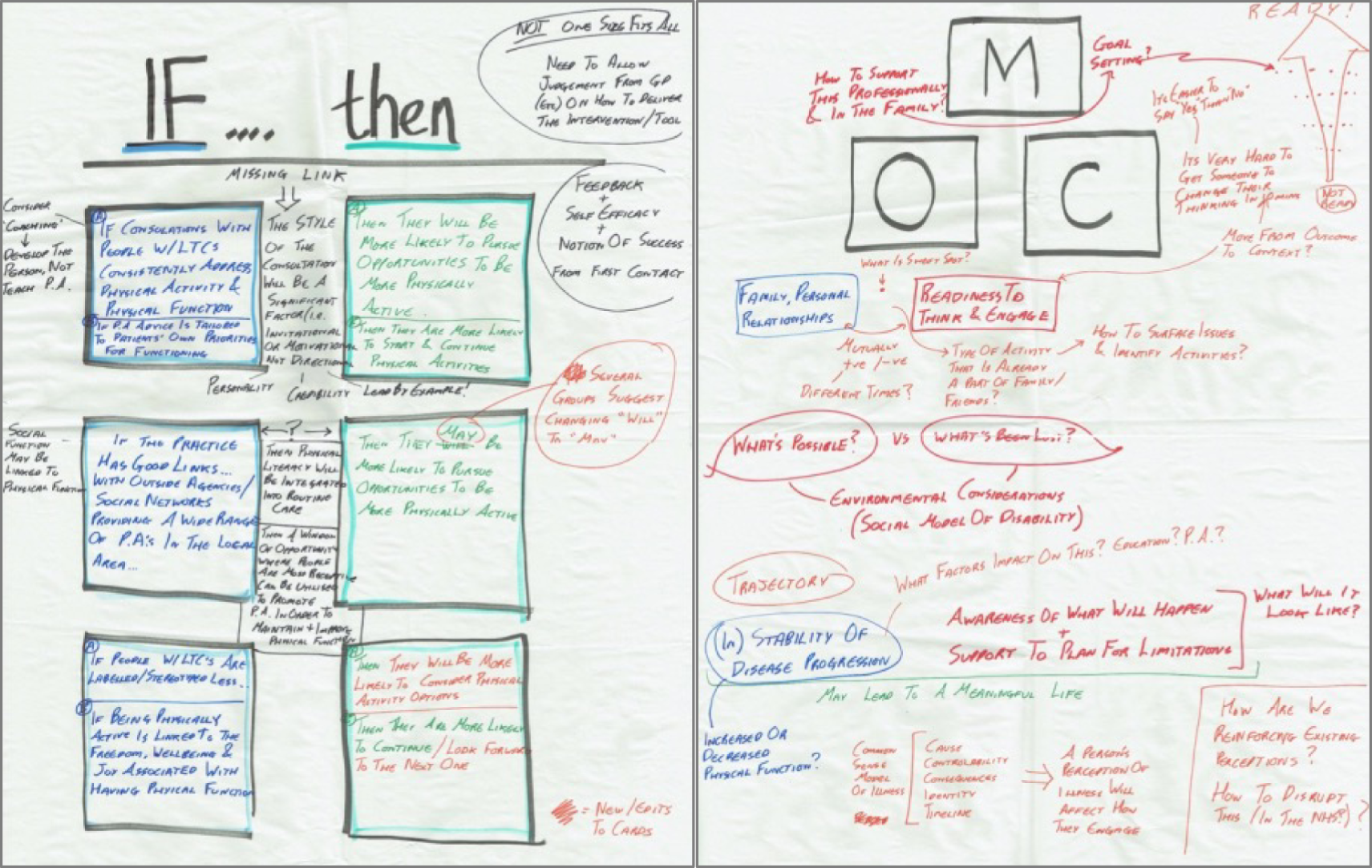
The important thing with these card games was that they represented the wider evidence base and playing the game elicited critical discussion among the smaller groups about the evidence, enabling participants to make sense of it in the context of their own experiences and those of the other group members. The groups then shared their discussions with all the participants by selecting one issue arising from the ‘If . . . then’ card game that had created the most discussion in their group, followed by a general point about the discussion emerging from the CMO card game. These discussions were ‘captured’ by the facilitators on paper using flip charts (Figure 7).
FIGURE 7.
Summary notes of the whole-group discussion about the evidence emerging from the literature, following the ‘If . . . then’ and CMO card games.
The next activity in this workshop was designed to get participants thinking about themselves and their individual experiences. They had to identify which CMOs would most support them to engage with physical activities, and which would discourage them. Figures 8a and 8b are examples of some of the personal profiles created by the participants. The ‘data’ from this activity was not essential for developing an intervention but helped the co-design participants to think about the practical application of this evidence to a wider variety of people and the challenges associated with this.
FIGURE 8.
Examples of the personal profiles created by the participants (a, b), an example of one of the personas (c) and suggested relevant CMOs for this ‘case’; and (d) a final group discussion presented the personas and the CMO combinations defined for each case.
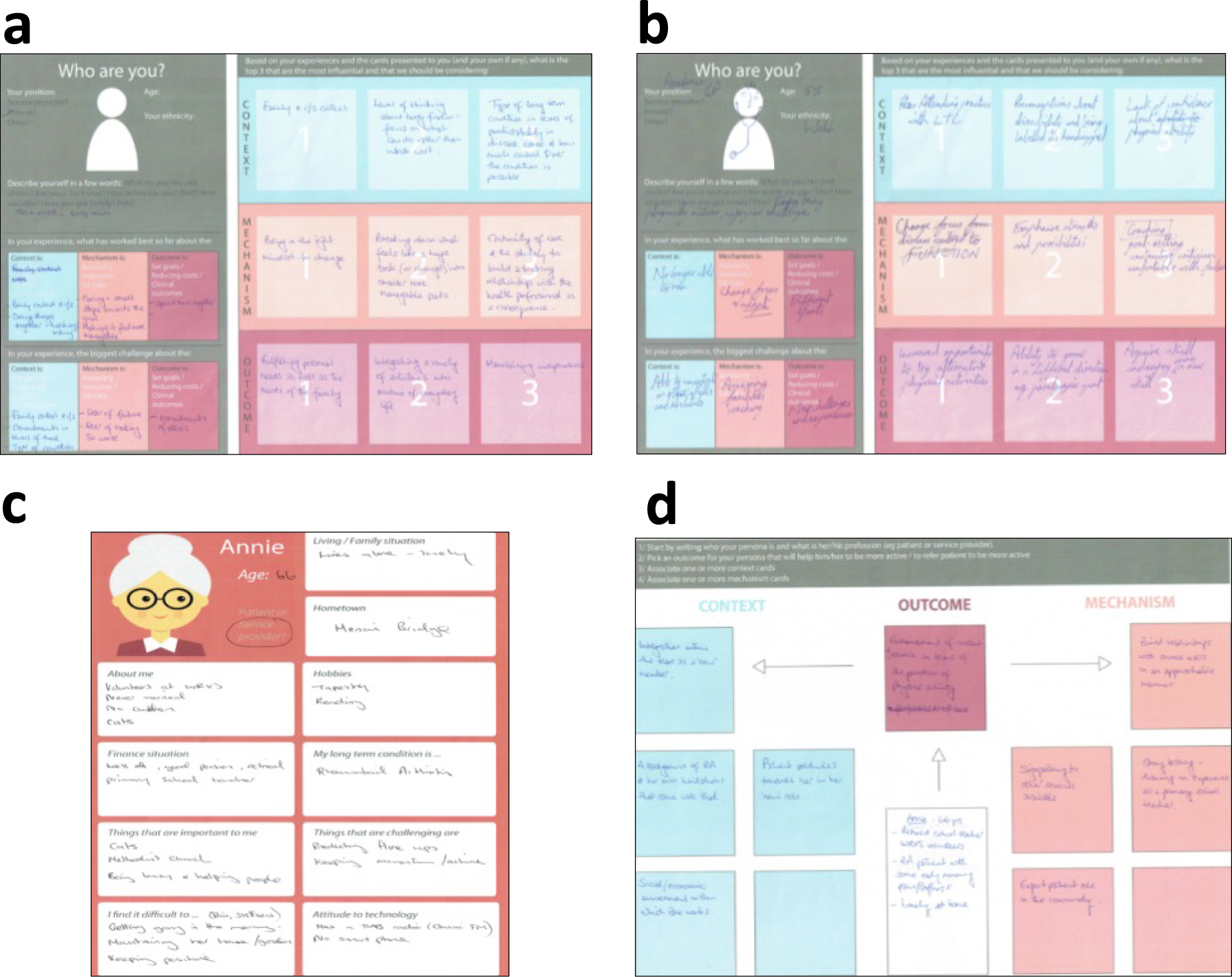
To encourage participants to think about the practical application of this evidence to other people, they created archetype personas (two per subgroup). They constructed comprehensive, holistic ‘pictures’ of these people and then considered what might work, and what might not work (in terms of CMOs) for each individual to encourage them to maintain or improve their physical function. To do this, they created personas that were culturally, socially and geographically diverse (in urban and rural settings); built up comprehensive ‘pictures’ of the whole life of each persona; and considered what CMOs would be most relevant in enabling primary care services to support each persona to be active and maintain physical function. Figures 8c and 8d illustrate one persona and the suggested relevant CMOs for this ‘case’.
This was followed by a broad discussion reflecting on everything that had been considered in this first workshop. These discussions were captured on paper on wall and flip charts.
This final discussion opened up some important topics:
-
Ubiquitous or positive pervasive messaging – it is the responsibility of every health-care professional to have an understanding of the importance of physical activity, which should be discussed with patients in a consistent manner.
-
The stages or states of ‘readiness for change’ on the part of the patient. Different strategies or interventions may be required at different stages of readiness, which raised further points –
-
There was a need to think creatively about how to enable people to move from ‘not being ready to engage’ to ‘being ready to engage’.
-
How to identify that ‘key moment’ when someone is ready to change and receptive to help.
-
There was a pragmatic argument to invest more time, effort and resources into that moment.
-
There was a need to think very differently about how to sustain long-term engagement in any activity.
-
The need to personalise or tailor the intervention at a practice level for staff and also for patients.
-
It was acknowledged that the context varied for different workshop participants, so this workshop provided an opportunity for sense-checking as well as further refinement of the emerging theories. Giving everyone the same time and space to do this at the start respected and valued their history and personal narrative, enabling everyone to move towards the main purpose of the co-design process. The activities in these workshops did not contribute directly to the design and development of ‘an intervention’ per se, but were vital building blocks, creating a shared understanding of each other, and of the evidence, as well as raising awareness of potential challenges and opportunities for developing a practical set of resources.
Design activity 1
Between workshops 1 and 2 the designers created a visual summary of workshop 1 to add to the growing visual narrative of the whole research process (Figure 9). This visual summary was brought back to every workshop as a way of enabling participants to continually position the co-design activity in the context of the process and evidence of the research project to that point.
FIGURE 9.
Visual ‘storyboard’ of the function first co-design process. (See also Report Supplementary Material 8 for a larger version.)
The design researchers reflected on and categorised the data produced by the co-design partners in workshop 1, using this to refine and adapt the plan for the next workshop. They then designed and produced the templates, resources and visual wall displays for the next workshop. Some of these activities included an exploration of previous co-design work strategies for engaging co-design partners and a breadth of existing interventions and analogous practices for presentation at workshop 2 as provocations for new ideas. We also invited participants to bring examples of existing interventions or resources relating to existing interventions that they had experienced or had knowledge of.
Workshop 2 (ideation)
The ultimate goal of this workshop was to generate ideas of tangible things that might help primary care professionals enable people with long-term conditions to sustain and improve their function. Before being able to generate ideas, it was important to enable participants to consider the kinds of ‘assets’ that individuals, communities and primary care services might utilise to support this kind of work (e.g. people, places, services, media, knowledge or technology).
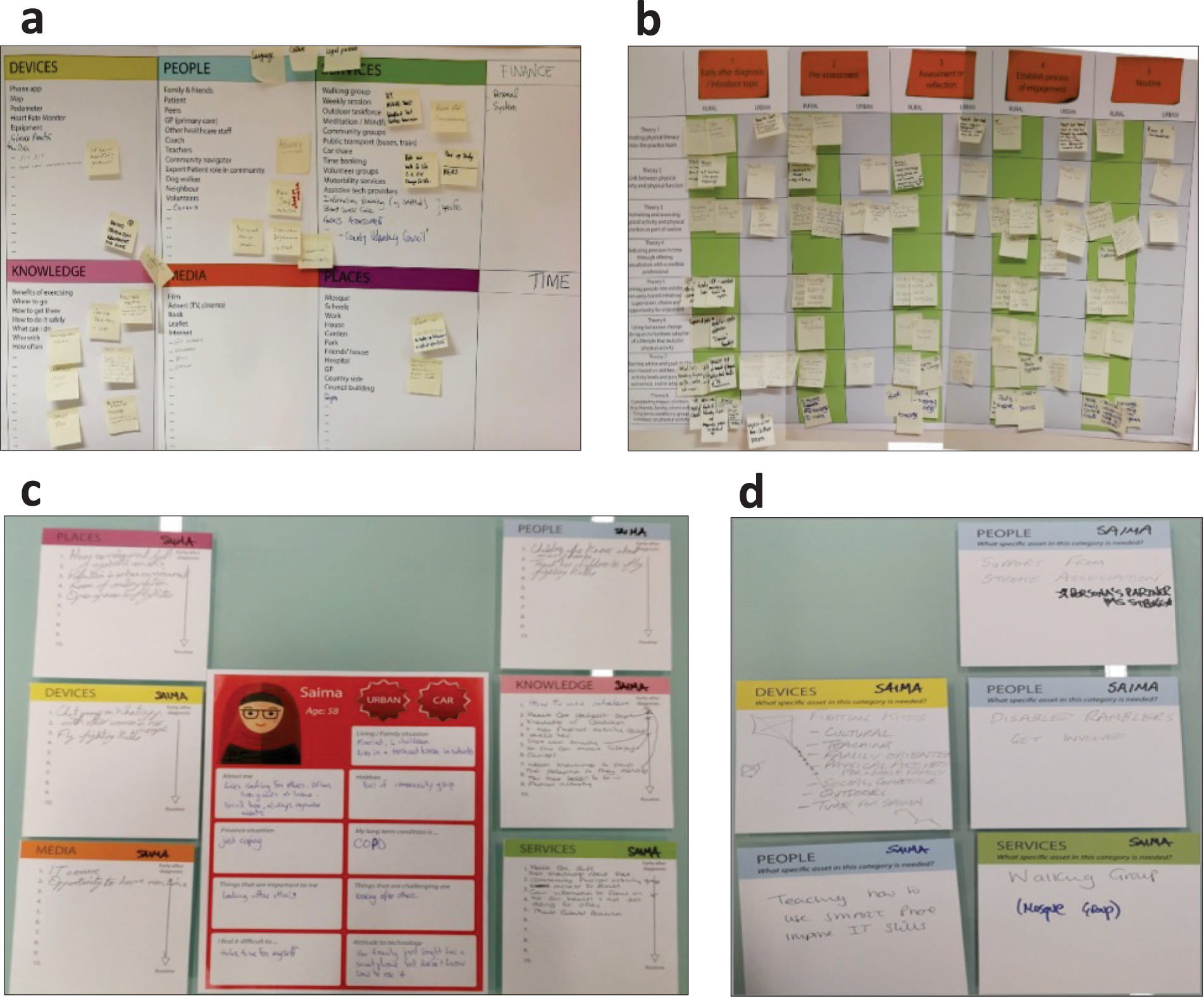
This began by drawing up a working list of potential assets that might be available to people (Figure 10a) and then thinking about how these assets might relate to the eight theory areas. The groups also considered how these assets may have greater (or lesser) utility at different stages of ‘readiness’ to engage in activities related to sustaining physical function (Figure 10b). The participants then returned to the personas that they had created in workshop 1 and listed all of the possible assets that may be relevant to each persona (Figure 10c), before developing a specific ‘package’ of assets that could be used for the persona over a period of time (Figure 10d).
FIGURE 10.
Images showing lists of (a) potential assets; (b) the potential utility of these assets at different stages of ‘readiness’; (c) application to different personas; and (d) development of a specific package of assets.
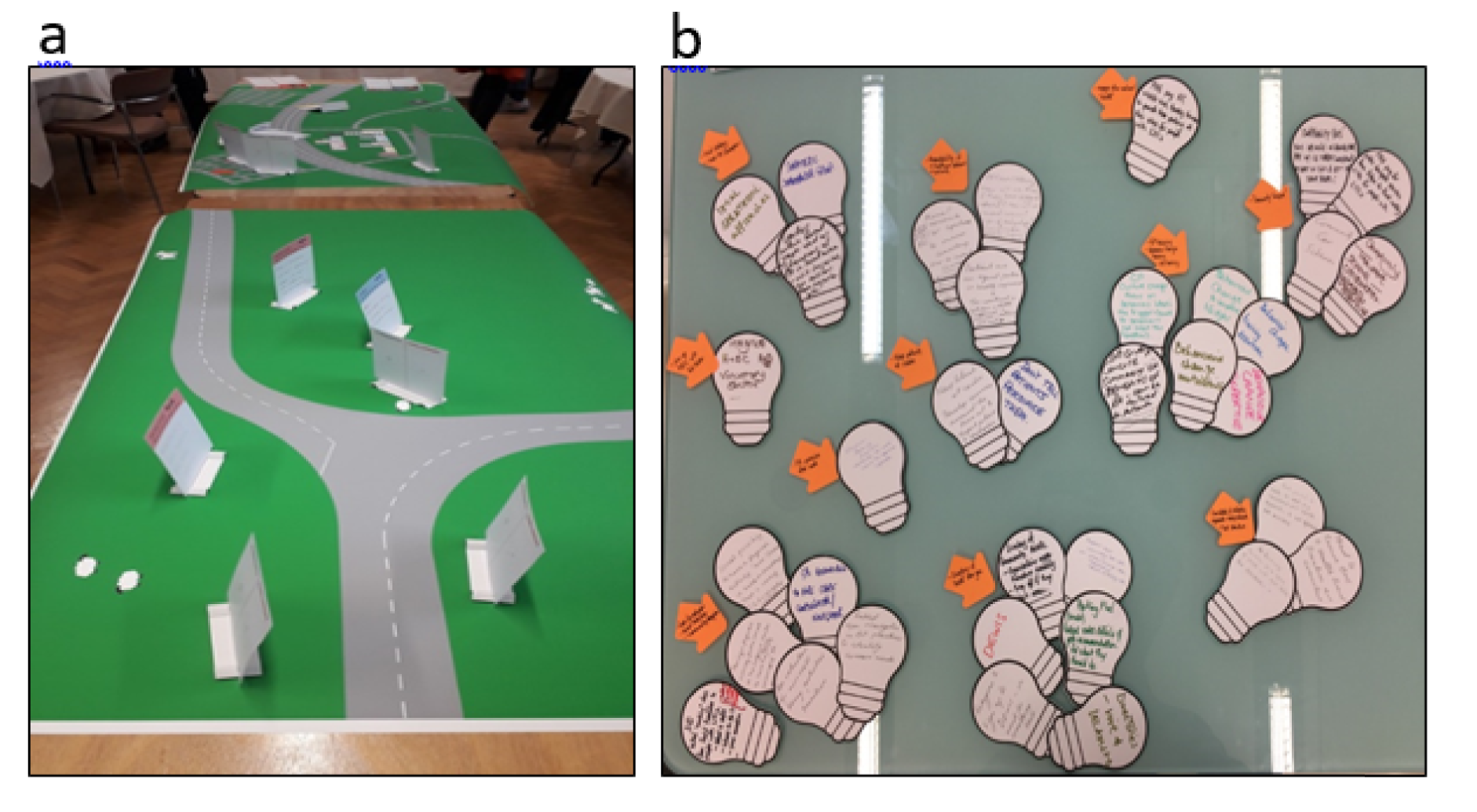
Following this, the participants physically mapped these persona-specific packages of assets onto geographic representations of rural and urban areas (Figure 11a) before considering ‘spanners’ (i.e. disruptions to people’s routines that made it challenging to sustain behaviours). Considering these possible disruptions was an important step to heighten awareness and consider ideas that might overcome these issues. The group also considered what might affect the scaling up of these assets from individual to group, local, regional and then national levels. Finally, the group were challenged to generate novel ideas (new assets, ways of connecting assets or new combinations of assets) that might augment or add value to the existing maps (Figure 11b).
FIGURE 11.
(a) The beginning of the mapping activity; and (b) novel ideas written onto ‘light bulbs’.
Design activity 2
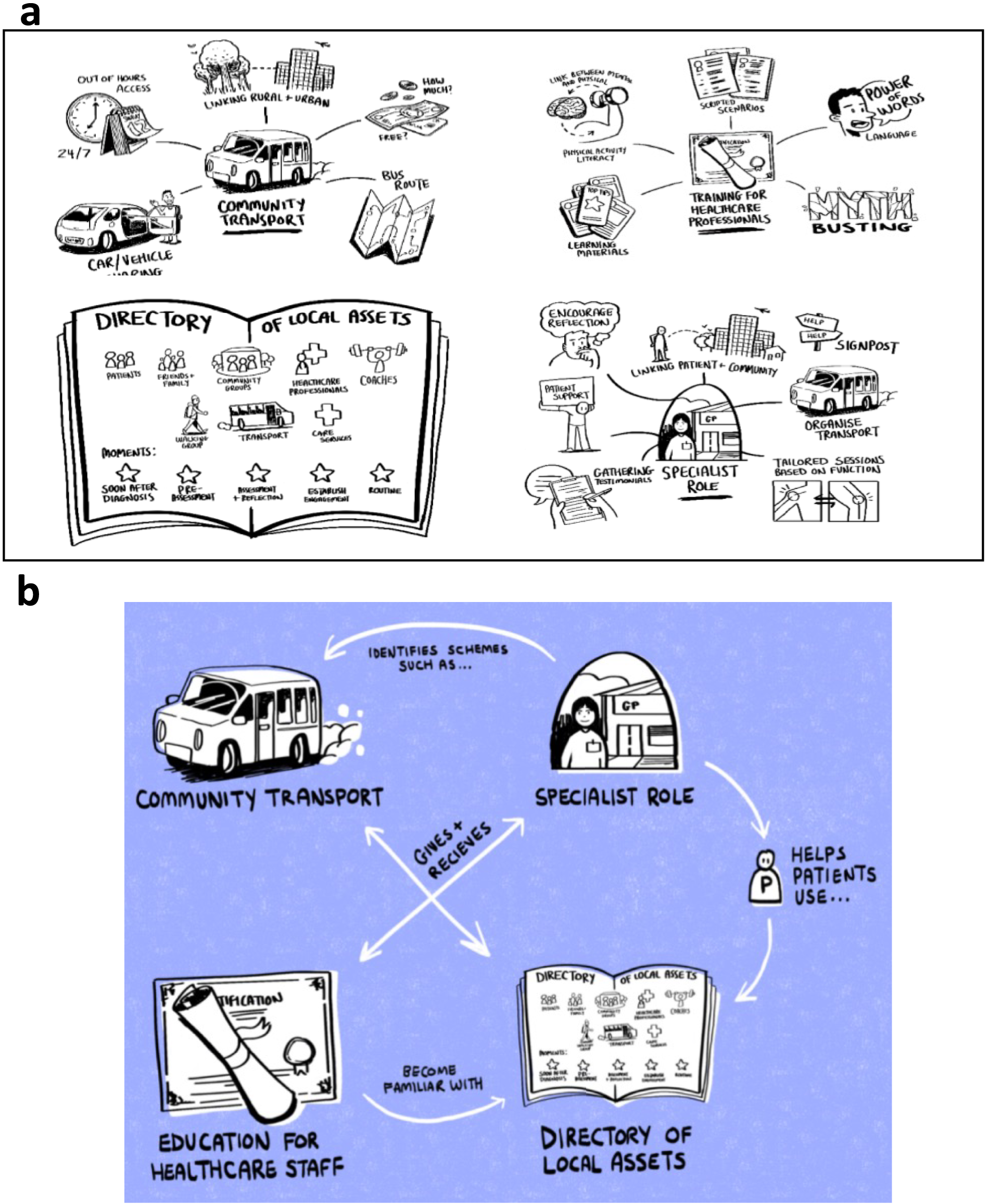
Between workshops 2 and 3, the design researchers visually documented the previous work and updated the storyboard of the research process ready for workshop 3. They grouped the ideas generated by participants into 11 broad categories (see Figure 11b) and made illustrations to represent and challenge these ideas and how they might (or might not) work in practice.
These categories were:
-
credible professional, social prescriber, community navigator
-
directory of ‘assets’ near you
-
community transport
-
consistent and reliable approach
-
primary care staff training, physical literacy, physical activity literacy, behaviour change literacy
-
joining up primary care with health and social care and voluntary sector
-
physical activity provision after work
-
keeping patients at the centre
-
local strategy, local physical activity champions, credible professionals with local knowledge
-
engaging other national assets
-
accountability of health-care professionals and of patients.
Plans for workshop 3 were adapted to reflect these categories and templates and resources for co-design activities in workshop 3 were designed and produced.
Workshop 3 (co-design)
In this workshop, the prototypes were refined and selected. This involved all participants testing and refining the ideas and models further and employing a shared prioritisation process to select the top four ideas. This involved a ‘Dragon’s Den’-style activity, where participants were split into groups. Each group took responsibility for one of the top four concepts (Figure 12a). The participants developed these concepts to a point where they could be shared with a panel of external people; people with expertise and experience in this area who had not been involved in the project to date (see Report Supplementary Material 1). This process provided useful critical feedback that helped the participants develop the four ideas further and begin to make stronger connections between them. The ideas began to coalesce into a cohesive single intervention with four different elements that embodied the evidence and refined CMO statements (Figure 12b).
FIGURE 12.
(a) The four top concepts for the intervention idea; and (b) how they connect together.
Design activity 3
Between workshop 3 and the knowledge mobilisation event the designers extended the visual summary to include workshop 2, adding to the growing visual narrative of the whole research process.
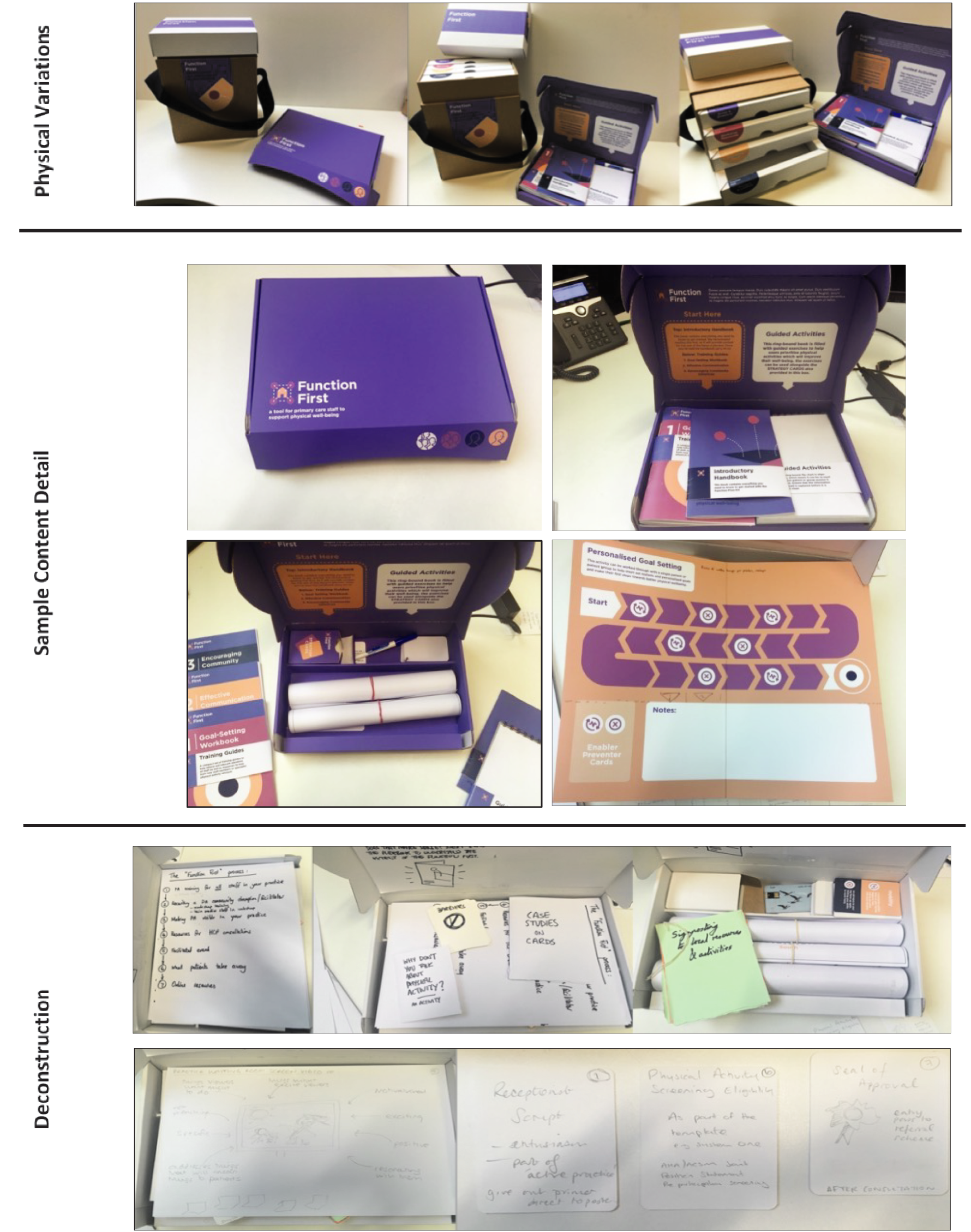
The design researchers reflected on and categorised the data produced by the co-design partners in workshop 3, using this to refine and adapt the plan for the next knowledge mobilisation workshop. They then designed and produced the templates, resources and visual wall displays for the next workshop along with early, rough prototypes based on the ideas and content generated in workshop 2. This conversion of ideas into material form was a key step in setting up workshop 3. These early forms had to be sufficiently vague and roughly finished to encourage participants to critique, change and deconstruct them. Yet they had to have sufficient form to bring the ideas to life and give people a strong sense of what this might or might not be, and how it might or might not work. Part of this process involved presenting a range of possibilities to avoid leading people down a specific route (Figure 13). The design team then made further adjustments based on feedback and developments from the co-design workshop.
FIGURE 13.
Physical variations, sample content detail and an image showing how the content was deconstructed and refined as part of the workshop.
Knowledge mobilisation
The design researchers presented a physical example and embodiment of the top four concepts generated in the co-design phase. Although detailed content was missing, the demonstration was able to illustrate how each physical element related to the refined CMO statements and theory areas, creating an evidence-informed design solution.
The group were asked to consider these physical elements and add or amend features to ensure that all aspects of the conjectured CMOs were represented in a tangible tool or resource that could be used in primary care settings. The images in Figure 13 show some of the additions that were made to purposefully represent or amplify the representation of elements the evidence indicated were important for this intervention.
The group then presented this to an invited group of representatives from key organisations who were already actively working in this field (see Report Supplementary Material 1). The idea behind this was to gather further feedback, and also to bring the prototype intervention to their attention at an early stage as an invitation to engage in the future use of this set of tools. This raised several useful issues such as ‘branding’ and barriers that might emerge regarding ‘competition’ with other initiatives. The groups worked on possible mechanisms to address these issues.
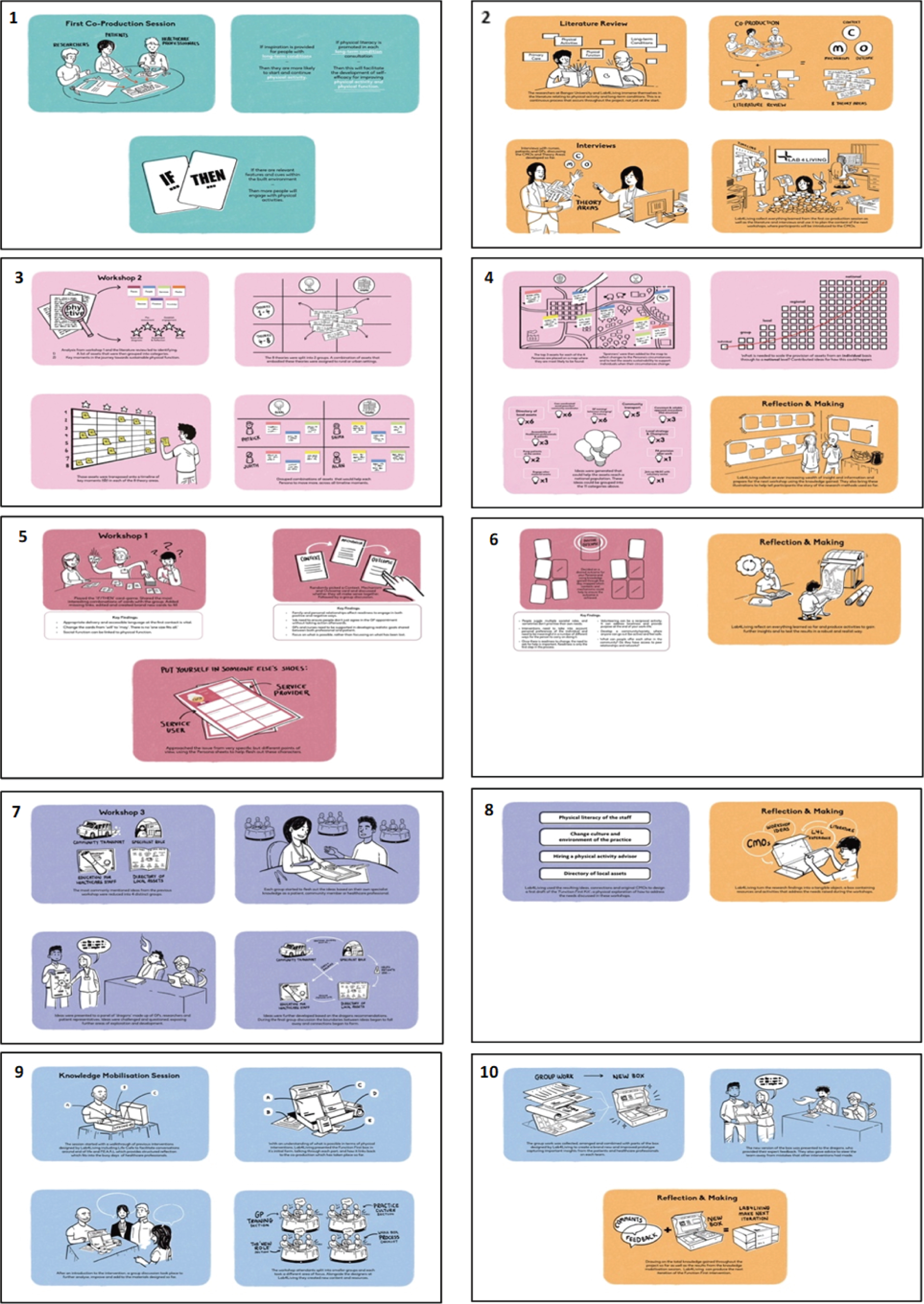
Summary and storyboard
Evidence from the realist synthesis phases was integrated into the co-design process in an iterative way. Figure 9 shows a storyboard of the overall process (see also Report Supplementary Material 8 for the larger version). This was displayed at each workshop and added to as the process progressed.
The co-designed resources are discussed in full in Chapter 3.
The series of images are a visual representation of the whole research and co-design process. The storyboard was essential in the participatory work, being used as a visual update at each participatory event of the work done to date and as a way of ensuring that participants in the co-design process were continually mindful of the wider evidence and context. This helped to make the co-design work evidence-informed co-design; informed by the wider academic literature as well as personal experiences of those delivering and receiving health-care services or living with a long-term condition.
Patient and public involvement
Use of the UK Standards for Patient and Public Involvement in Research
Understanding what matters to patients is crucial in designing interventions that are acceptable and rooted in the reality of patients’ lives. 114 Our aim was to involve members of the public throughout the project to ensure that our work continued to consider the issues and perspectives that are directly relevant to people who engage with primary care services, and who have long-term conditions. The UK Standards for Patient and Public Involvement in Research115 are based on initial work on the values and principles of public involvement undertaken by NIHR INVOLVE and Health and Care Research Wales. 115 We used the standards and associated audit tool (see Report Supplementary Material 9) to facilitate reflection and learning, and as a framework for what ‘good’ public involvement looks like. In summary, and in response to the six standards, we:
-
Endeavoured to provide ‘inclusive opportunities’ by involving members of the public at the earliest stage; identifying barriers (e.g. we offered remote methods of contributing at times convenient to the individual and offered travel expenses and honoraria); using the Involving People network as a fair, transparent process to identify members of the public; and offering choice and flexibility in involvement. The Involving People network has now been replaced by new infrastructure delivered through Health and Care Research Wales. 116
-
Encouraged ‘working together’ by keeping in regular communication through Study Management Group meetings, discussing roles and responsibilities on a one-to-one basis as needed, and recognising contributions to build and sustain mutually respectful and productive relationships.
-
Promoted ‘support and learning’ through the identification of a named point of contact for public contributors (RL). Public contributors were members of the Involving People network through which training, resources and support was available to them. The study co-chief investigators also attended workshops on public involvement to supplement their own learning.
-
Made our ‘communications’ more relevant with the help of the public contributors, enabling us to decide how we can most effectively share our public involvement activities through local and national dissemination activities.
-
Identified and shared the ‘impact’ of public involvement activities through our use of the national standards. Through our project oversight groups, we considered how well we were using suggestions from public contributors to influence our work, including how to proactively enhance our work by considering possible barriers to public involvement, such as time and work commitments, as well as facilitators.
-
Fully engaged members of the public in the ‘governance’ of this project through inclusion as members of the co-applicant team in regular Study Management Group meetings, participation in Project Advisory Group activities and regular e-mail correspondence about project progress. A named member of the study (RL) was responsible for ensuring that all necessary resources were allocated and monitored to support this.
We have also used the Guidance for Reporting Involvement of Patients and the Public 2 (GRIPP2, short form)117 to ensure appropriate reporting of public involvement our final report (see Report Supplementary Material 10).
How members of the public were involved and at what stages
Public involvement in this study began at proposal stage and involved a series of meetings with the project team and two public research partners, both of whom had experience of using primary care services, being involved in research projects and experience relevant to living with a long-term condition. Both became co-applicants, and then members of the Study Management Group once the project was funded. Another public research partner joined the study when one of the two original public research partners stepped down.
As part of the Study Management Group, meetings took place approximately monthly, to which the study public research partners were invited and contributed regularly in person, remotely and via e-mail correspondence. We also involved two members of the public in our external Project Advisory Group, which met four times over the course of the project.
This project also had a strong participatory element and included people with long-term conditions as participant stakeholders throughout the process. For the final co-design workshop, we involved two further members of the public as active partners in the research process. These contributors acted as ‘Dragons’ in the co-design workshop to help provide critical insight and refine the intervention resources that had been co-designed by participants.
The impact of public involvement and how it was useful
At the proposal stage, the two study co-applicants helped to refine the research question, proposed methods, lay summary and public involvement sections, ensuring that they were both relevant and appropriate. This included consideration of ‘who’ the target group would be, the potential for participant burden in workshops, use of language in the lay summary, and consideration of appropriate public involvement activities and reimbursement. They also contributed directly to the co-production of the project short title and tagline: Function First – Stay Active, Be Independent.
Once the project had started, the two public research team members were involved on a regular basis as part of the Study Management Group, and particularly in the following activities, with the following impact:
-
When preparing public-facing materials and responding to comments from the ethics review, changes were made to –
-
the wording of information sheets and consent forms to reduce formality and provide reassurance of processes in place to deal with distress
-
the plans for the workshops by clarifying content and focus of activities, considering time burden and specific issues that may arise for people with long-term conditions (e.g. the use of LEGO bricks by someone with arthritis and the need for rest breaks)
-
the telephone interview topic guides to ensure clarity in explanations of methods, coverage of important issues (e.g. additional prompts to facilitate further information and procedures for if a person discloses information of concern to the interviewer).
-
-
During ‘group analysis’ of the data from the theory-building workshops, the study team public contributors ensured that we considered the patient perspective, including those from varying socioeconomic and ethnic groups.
-
Review of a selection of titles, abstracts and full papers for the literature searching and contributed to ongoing discussions among the project team about our methods (e.g. refinement of inclusion/exclusion criteria).
-
Commenting on abstracts submitted for presentation at conference proceedings, presentations and posters, with changes made to improve clarity of wording and explanations.
-
Writing of ‘Function First’ protocol paper as authors, the study team public contributors reviewed and made comments that helped to improve clarity, particularly for the public involvement section.
-
Participation in co-design and knowledge mobilisation workshops as public members of the research team, enabling influence on intervention development from both a project and public perspective.
-
Help in considering use of resources available to facilitate public involvement. Following discussion, we decided to use the UK Standards for Patient and Public Involvement in Research as a tool to reflect on our ongoing public involvement and keep a record of examples to supplement, and use the GRIPP2 to ensure appropriate reporting in the final report.
-
Help in considering appropriate methods of reimbursement for public contributors and participants. For example, preference for payment to workshop participants using vouchers, consideration of tax and benefit issues, and discussion of updates to guidance from INVOLVE.
-
Writing of this section of the report, ensuring that it was accurate, clear and comprehensive.
As part of the independent Project Advisory Group, two public contributors were actively involved in the following specific activities:
-
providing independent feedback on ‘If . . . then’ statements and emerging theory areas from a public perspective, thus helping to refine and improve their relevance
-
suggesting the inclusion of particular groups as stakeholders
-
discussing options for reporting of public involvement
-
providing independent, reflective feedback during and following meetings on overall project progress, emerging findings and next steps
-
writing this section of the report, ensuring that it was accurate, clear and comprehensive.
Reflections and critical perspective
What went well:
-
continuity in involvement from proposal through to write-up stage
-
regular attendance and contribution to Study Management Group and Project Advisory Group meetings and activities, including the addition of ‘public involvement’ as a regular agenda item
-
ability to enable public contribution using various methods to improve accessibility (e.g. videoconference, telephone, face to face, e-mail correspondence)
-
mutual respect between public contributors and researchers as members of the project team
-
a named point of contact for public contributors
-
implementation of suggestions made by public contributors, including in response to comments from the ethics review panel
-
involvement of public contributors in aspects of the study methods (e.g. literature reviewing, co-design), decision-making (e.g. contribution to project oversight groups) and dissemination (e.g. co-authoring abstracts and papers).
What could have been improved:
-
Better clarity from study outset about arrangements for paying honoraria and reimbursing public contributors for travel and subsistence. Importantly, arrangements and clarity around this have improved as a result.
-
Support for public contributors to attend relevant training and development events (e.g. costing in expenses and further direct encouragement).
Project oversight
The day-to-day running of the project was overseen by a Study Management Group that met monthly. This group had a management role, but meetings also included a strong element of co-production, with the expertise and experience of the different members infiltrating the development of programme theory and co-designed products and processes.
Our study also benefited greatly from an independent Project Advisory Group that met on four occasions. This group included two public representatives and professional expertise from Australia, Canada, the Netherlands and across the UK (see Report Supplementary Material 11) in the areas of physiotherapy, exercise science, realist synthesis, public health and geriatric medicine. In addition, this group provided critical oversight and scrutiny, as well as advice from a methods and practice perspective. The group was particularly involved in helping us to refine the CMOs and supplementing our evidence searches with additional literature.
Chapter 5 Results
Parts of this chapter have been reproduced with permission from Law et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Chapters 2 and 3, described the overall methodology, theory-building workshops and realist synthesis of the literature. Chapter 4 explained the co-design approach, the knowledge mobilisation workshops and public involvement used to develop the intervention. It was through the combination, interplay and synthesis of these methods that the study results were produced. This chapter describes those results in detail, outlining the taxonomy, the CMO configurations, and the co-designed prototype intervention.
Taxonomy
Table 1 describes the categories of interventions included in this review, with an accompanying example of each.
| Type of intervention | Description | Example papers |
|---|---|---|
| Brief interventions | Brief verbal advice, discussion, negotiation or encouragement, with or without written or other support or follow-up. It can vary from basic advice to a more extended, individually focused discussion | Lamming et al.118 – systematic review of reviews. Brief interventions can increase self-reported physical activity in the short term, but there is insufficient evidence about their long-term impact, the impact that they have on objectively measured physical activity, and about the factors that influence their effectiveness, feasibility and acceptability |
| Telephone interventions | Physical activity interventions delivered predominantly over the telephone | Goode et al.119 – systematic review. Findings provide continuing strong evidence supporting the efficacy of telephone-delivered interventions to promote physical activity |
| Online/‘eHealth’ interventions | The use of information and communication technologies for health120 | Muellmann et al.121 – systematic review. ‘eHealth’ interventions can effectively promote physical activity in older adults aged ≥ 55 years in the short term, whereas evidence regarding long-term effects and the added benefit of eHealth compared with non-eHealth intervention components is still lacking |
| Exercise referral schemes | The practice of referring a person from primary care to a qualified exercise professional who uses relevant medical information about the person to develop a tailored programme of physical activity usually lasting from 10 to 12 weeks | Campbell et al.122 – systematic review. Compared with usual care, exercise referral schemes had a small effect in increasing the proportion of individuals achieving 90–150 minutes of at least moderate-intensity activity per week |
| Community ‘navigators’ | Appropriately trained individuals who can guide patients towards local physical activity opportunities | Leenaars et al.123 – CSCs. Introduced in 2012 in the Netherlands, CSCs seem to hold the promise of improving collaboration between the primary care and the physical activity sector, especially because the roles that CSCs perceive themselves as having seem to be directed at eliminating barriers in this connection |
| Referral to exercise specialists (e.g. exercise physiologists) | Referral to a qualified exercise physiologist from primary care (implemented in Australia) | Ewald et al.124 – RCT to establish cost-effectiveness. Referral to an exercise physiologist increased physical activity, which persisted at the 9-month follow-up. Coaching achieved a modest increase in activity equivalent to 10 minutes walking per day, at a cost of AU$245 (approximately £150) per person. Face-to-face and telephone counselling were both effective. Note that a change in quality of life was not observed so could not estimate utility |
| Intervention delivery by existing primary care staff | When primary care professionals (e.g. practice nurses, health-care assistants) deliver physical activity interventions | Williams et al.125 – a mixed-methods treatment fidelity assessment. Two practice nurses and six health-care assistants delivered a theory-based walking intervention to 63 patients in their own practices. High levels of fidelity of delivery were demonstrated. However, patient-, provider- and component-level factors had an impact on treatment delivery and receipt |
| Physical activity ‘pathways’ | ‘Let’s Get Moving’; a UK-based attempt at embedding physical activity promotion into routine primary care, recommended by Public Health England for commissioning at a local level by primary care trusts within NHS England | Bull et al.126,127 – feasibility pilot study and process evaluation
|
| Boehler et al.128 – ‘the costs of changing physical activity behaviour’. Disease register screening is more costly than opportunistic patient recruitment (£53 vs. £191). However, additional costs come with a higher completion rate and better outcomes in terms of behavioural change in patients completing the care pathway | ||
| Department of Health and Social Care commissioning guidance129 – includes resources and protocols for implementation | ||
Loughren et al.130 – ‘Let’s Get Moving’ Physical Activity Care Pathway (Gloucestershire). Factors determining implementation success:
|
||
| Barrett et al.131 – feasibility in primary care physiotherapy. Concluded to be a clinically feasible resource to primary care physiotherapists with some modifications and with the support of additional resources (i.e. professional training and integration with existing schemes) | ||
| Practice-wide initiatives | Active Practice Charter promoted by the Royal College of General Practitioners | Active Practice Charter.132 The Royal College of General Practitioners and Sport England have launched the Active Practice Charter to inspire and celebrate GP practices that are taking steps to increase activity and reduce sedentary behaviour in their patients and staff |
| Community initiatives adopted by primary care | parkrun practice | Quirk and Haake133 – parkrun launched a project called PROVE in 2016 to engage people living with long-term health conditions in England. Over the 3-year project, parkrun appointed volunteer outreach ambassadors with a specialist interest in the health condition they represented whose role was to ensure parkrun was welcoming, supportive and inclusive. A qualitative evaluation showed that PROVE was regarded by the ambassadors (patients, carers, professionals) as important for ensuring that people with long-term health conditions can engage in physical activity and volunteering in a safe and supportive environment |
| A whole-system approach to embed physical activity in clinical practice | Moving Healthcare Professionals Programme (MHPP) | Brannan et al.134 – the MHPP model is a partnership between Public Health England and Sport England. It has delivered face-to-face training to 17,105 health-care professionals, embedded materials in almost three-quarters of medical schools in England and overseen > 95,000 e-learning modules over 2.5 years. The programme aims to bring about improvements in knowledge, skills and practice. Individual elements of the model are being evaluated and further evaluation is planned to assess patient impact |
| Moving Medicine | ‘Moving Medicine’135 was created to aid health-care workers in integrating conversations about physical activity during routine clinical care. Moving Medicine offers this online support for all patients of all ages and conditions. It also offers advice depending on the amount of time available with a patient and adjusts the conversations to these needs. Moving Medicine has the option of completing an ‘online physical activity training course’, which is accredited with 16 CPD points from the Faculty of Sport and Exercise Medicine (UK) | |
| Multifaceted interventions | Interventions involving a combination of approaches | Avery et al.136 – ‘Movement as Medicine for type 2 diabetes’ is a multifaceted intervention informed by the theory of planned behaviour and social cognitive theory and consisted of 15 behaviour change techniques. It includes an accredited online training programme for health-care professionals who deliver a behavioural intervention for adults with type 2 diabetes. This intervention intensity and duration were informed by a systematic review and stakeholder work. Usability testing resolved technical problems with using the online training intervention on practice information technology (IT) systems. An open pilot study of the intervention identified mechanisms to enhance intervention implementation during routine diabetes consultations |
| Campaigns | Age UK Resources – ‘We Are Undefeatable’ | The ‘We Are Undefeatable’137 campaign was developed by 15 leading health and social care charities. Its main aim is to support and encourage ways for individuals with a wide range of health conditions, to remain active even during times when this can be challenging |
Programme theories
The theory development and refinement process, outlined in Chapters 2 and 3, led to the development of five CMO configurations that, collectively, provide an evidence-based theoretical account of what it is about physical activity interventions in primary care that work (or do not work) for people with long-term conditions, and in what circumstances. In this section, each CMO configuration is reviewed, including the evidence underpinning physical activity interventions in primary care and explaining how the contexts and mechanisms identified lead to outcomes relevant to improving physical activity in people with long-term conditions. Examples of evidence from the literature review and from the stakeholder interviews (see Chapter 3) are included in the explanatory account to highlight meaning and illustrate salient points. We also group all of the interventions that contributed evidence for each CMO (see Boxes 1–5).
The CMO configurations were developed and refined by a range of stakeholders, who considered all sources of evidence, and provided regular purposeful input into the co-design process. When considered together, they offer a programme theory about ‘what works, for whom, under what circumstance’.
The five configurations are summarised here and described in further detail in the following sections:
-
changing practice culture through alignment
-
providing resources
-
individual advice
-
improving capability of practice workforce
-
programme credibility.
Rather than presenting the CMO configuration as an addition equation (i.e. C + M = O), we have chosen to present outcomes (O) as a function (f) of the interactions between the context (C) and mechanism (M), because this better reflects the nature of the relationships observed in this synthesis. Therefore, in Figure 14 we present the visual representations of the CMO configurations by applying the following formula:
FIGURE 14.
Visual representation of the five CMO statements. From top to bottom: CMO 1 – ‘changing practice culture through alignment’; CMO 2 – ‘providing resources’; CMO 3 – ‘individual advice’; CMO 4 – ‘improving capability of practice workforce’; CMO 5 – ‘programme credibility’. C, context; M, mechanism; O, outcome; PA, physical activity.
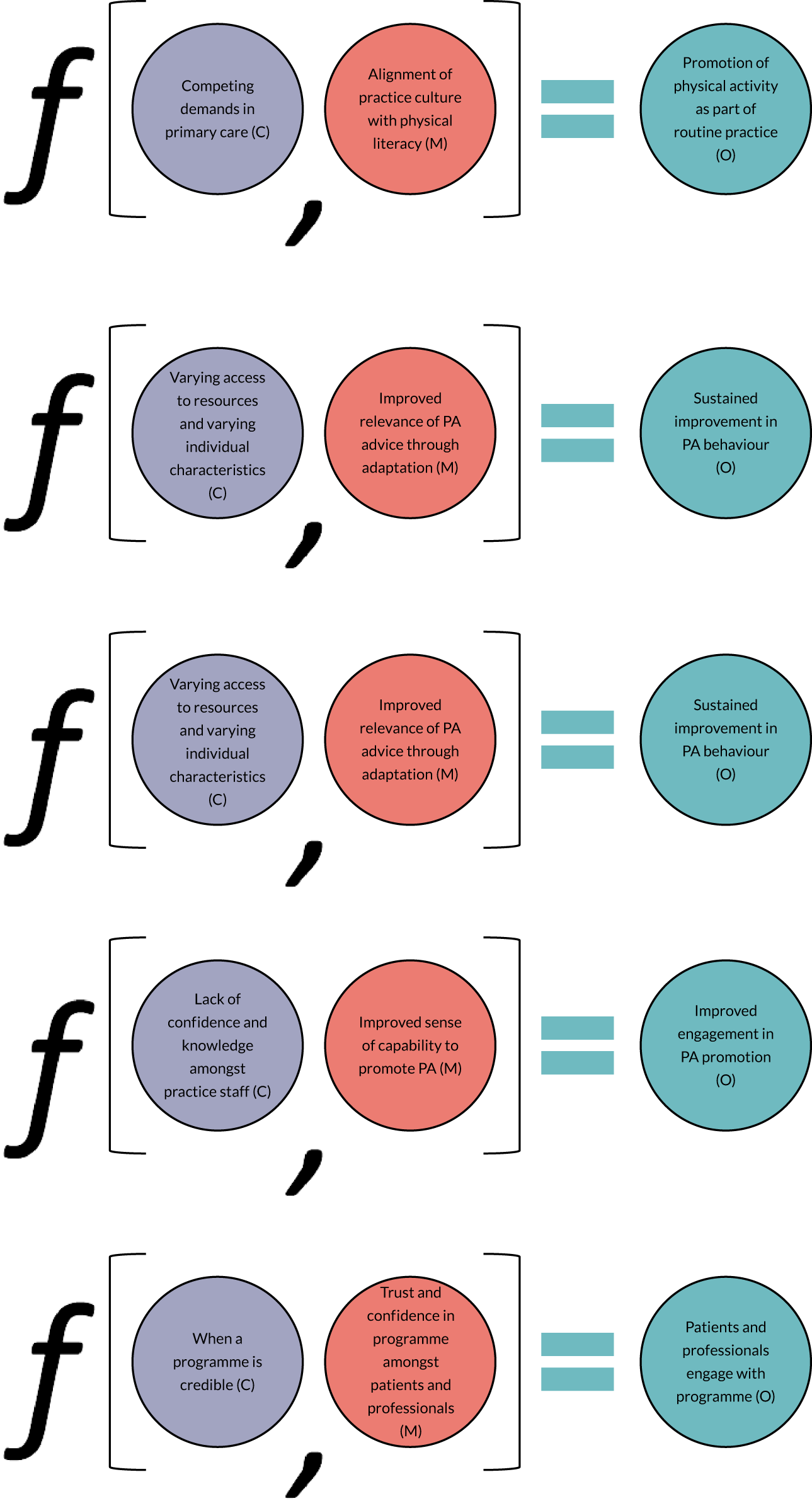
Context–mechanism–outcome statement 1: changing practice culture through alignment
Summary of context, mechanism and outcome
Primary care settings are characterised by competing demands and improving physical activity, and physical function is often not prioritised in a busy practice (context). If the practice team culture can be aligned to promote and support the elements of physical literacy (mechanism), then physical activity promotion will become more routine and embedded in usual care (outcome).
The types of interventions that contributed evidence to CMO statement 1 are shown in Box 1.
Competing demands in primary care (context)
Barriers to promoting physical activity among UK general practitioners include a lack of time, competing clinical priorities, and limitations in resources and relevant education. For example, in a survey of 166 GPs, 65 GP registrars and 71 practice nurses, 91.2% of respondents described time as a factor limiting them in discussing physical activity with their patients. 138 Similarly, a survey of all 1228 GPs in Perth, Australia, WA, indicated that a lack of time was the most frequently cited barrier to the promotion of physical activity. 139 A qualitative focus group study in the USA explored perceptions of nurse practitioners regarding their role in physical activity and its promotion for older adults and concluded that nurse practitioners felt unable to give systematic attention to physical activity for older adults:
All of the nurse practitioner (NP) participants were clear that only a small percentage of a primary care healthcare visit for any adult client can be devoted to counselling regarding physical activity and exercise . . . NPs described other important issues that of necessity take priority in the primary healthcare visit . . .
Melillo et al. 140
Data from interview participants in our study provided further explanation about competing priorities:
When we have 10 minutes, we don’t have time to even do what we’re meant to be doing.
GP, interview participant 004
I think physical activity unfortunately does take a bit of a back step because it’s probably not seen as so important as referring somebody who is expected cancer or sorting somebody’s medications out.
GP, interview participant 001
It’s a recurring theme that there’s just not enough hours in the day to do everything, so you have to pick and choose what you think that patient is going to change.
Practice nurse, interview participant 003
Our work suggested that competing priorities in primary care also include different models of care. The primary care management of long-term conditions typically focuses on the diagnosis and categorisation of disease according to the International Classification of Diseases and Related Health Problems, Tenth Revision. 68 It emphasises the management of mediators such as blood pressure and glycaemic control in diabetes. 141 The International Classification of Functioning, Disability and Health69 provides an alternative perspective, which places more emphasis on functional limitations within a biopsychosocial context. It emphasises activity limitations and participation restrictions that include contextual, personal and environmental factors. In the context of the International Classification of Functioning, Disability and Health,69 physical activity has the potential to promote more proactive, ‘whole-person’ and preventative care approaches, benefiting the patient and targeting health-care resources more effectively. 21,22 Primary care nurse practitioners have also expressed concerns that there is a focus on diagnosis as opposed to health promotion. 140 Data from interviews supported this view that health professional culture should focus more on preventative actions:
People can do a lot for themselves but there needs to be a change in the culture for health professionals. The medical model needs to become an upstream public health model and a rehabilitation and a social model.
Public contributor, long-term condition, interview participant 005
However, evidence suggests that this approach has time and resource implications for GPs, nurses and other primary care professionals, which can act as barriers to its implementation. For example, in a paper reporting a rehabilitation programme combining cognitive behavioural therapy principles and therapeutic exercise for the self-management of low back pain, professionals found it difficult to challenge the beliefs of patients, such as preferences for medication,139 which led towards application of a biomedical approach, rather than a broader biopsychosocial approach. 142 On the other hand, the American College of Sports Medicine established the ‘Exercise is Medicine’ campaign in 2007, which aims to facilitate improved health and well-being through regular exercise prescription from primary care health professionals. They promote the idea that physical activity and exercise are ‘medicine’ and that health-care providers should and will ask about, and recommend, physical activity and exercise. 67
Aligning practice culture with physical literacy (mechanism)
Physical literacy is defined as ‘the motivation, confidence, physical competence, knowledge and understanding to value and take responsibility for engagement in physical activities for life’. 143 (Reproduced with permission from the International Physical Literacy Association, May 2021.) Thus, if practice culture is aligned with the elements of physical literacy, then this could stimulate and augment physical activity promotion. Aligning a practice culture with the elements of physical literacy would involve influencing the beliefs, attitudes, values and behavioural norms within a practice (i.e. ‘how things get done). 144
The promotion of physical literacy is emerging as a promising strategy to increase lifelong physical activity participation in younger age groups of the population, but there is less evidence for physical literacy in the context of supporting older adults with long-term conditions to achieve physical activity guidelines. However, an iterative, mixed-methods, consensus development process in Canada produced a model of physical literacy for adults aged ≥ 65 years. 145 This model proposes the promotion of physical literacy to facilitate successful and sustained increase in physical activity participation by older adults. 145
In one of our theory-refining stakeholder interviews, the teaching and learning of physical literacy was discussed, alongside how a culture of physical literacy might be promoted:
The only thing that we can aspire to is actually create a culture in which the environment and the educator has such knowledge and practice that physical literacy becomes nurtured, over a considerable period of time.
Researcher, pedagogy, interview participant 007
An important initiative aiming to enhance physical activity promotion across the primary care setting is the Active Practice Charter from the Royal College of General Practitioners. The vision behind this initiative is that, despite having a crucial role, GPs and their teams have not felt empowered, and lack the skills, to encourage physical activity in their practice or the local community (see also Context–mechanism–outcome statement 4: improving capability of practice workforce). The criteria for becoming an ‘active practice’ have been left intentionally broad and undefined, and emphasise that the practice team and their patients will have the best idea of what will work for them. Practices are encouraged to consider changes that will reduce sedentary behaviour, encourage partnership with local physical activity providers, and increase physical activity in staff as well as patients. Indeed, evidence shows that health professionals who are more physically active are more likely to encourage their patients to be physically active and provide better counselling and motivation of their patients to adopt such health advice. 146,147 The initiative also provides some ideas for implementation, including walking to the waiting room to call patients in, providing standing space in the waiting room with information for patients explaining why, improving cycle facilities, signposting to local fitness opportunities and signing up to be a parkrun practice. The practice ‘lead’ could be a GP, a practice nurse, a social prescriber or the patient participation group. The initiative is designed to celebrate and inspire GP surgeries to take steps to increase physical activity and reduce sedentary behaviour in their patients and staff. 148 This initiative promotes the elements of physical literacy by enhancing motivation through celebration of a new ‘Active Practice’ status, confidence by offering achievable, realistic suggestions of ways to develop an ‘Active Practice’, and physical competence, knowledge and understanding through the provision of information and resources to facilitate ‘Active Practice’ activities.
The ‘Moving Healthcare Professionals Programme’134 and ‘Moving Medicine’135 are two further examples of initiatives designed to support health professionals working in primary care to promote physical activity. These programmes have not yet been evaluated.
Consistent messaging that aligns with the principles of physical literacy is also evident in relevant guidelines. For example, NICE guidance emphasises the lifelong value of physical activity, recommending that campaigns should provide messages that sustained ill health in old age is not inevitable,75 thus contributing to increased alignment across the practice and more widely.
Promoting physical activity as part of routine practice (outcome)
Evidence indicates that interventions promoting physical activity are more likely to be effective when integrated into routine care. 63,149 NICE recommends that all health-care practitioners and policy-makers view the encouragement of physical activity as a part of routine practice, to take place at every opportunity. 75,150,151 This integration into routine practice is more likely to happen if practice culture is aligned with the elements of physical literacy. For example, the ‘Let’s Get Moving’ (LGM) physical activity pathway is a UK-based attempt at embedding physical activity promotion into routine primary care and was recommended by Public Health England for commissioning at a local level by primary care trusts within NHS England. 129 It combines several methods of supporting behavioural change including brief interventions, motivational interviewing, goal-setting, providing written resources and follow-up support. A feasibility study conducted in 14 London surgeries showed that 75% of the patients who attended the follow-up consultation had increased their physical activity level, and almost all patients (97%) participated in one of the physical activity options. Of note, patients were identified either opportunistically or through electronic disease registers. Opportunistic intervention reached only 6% of patients, whereas recruitment using disease registers ranged from 9% to 59%, indicating that this method of embedding routine physical activity promotion may be more effective. Moreover, although disease register screening was more costly (£191 per patient) than opportunistic recruitment (£53 per patient), these additional costs also came with a higher completion rate and better outcomes in terms of self-reported behavioural change in patients completing the care pathway. 127,128 Practices that recruited via disease registers were also able to book longer consultations to accommodate the care pathway steps and components. 126 This suggests that increased alignment with physical literacy (e.g. the practice taking specific steps to take responsibility for physical activity by adopting a disease register approach) could have increased the promotion of physical activity as routine.
Although encouraging, it is important to note that only a small number of practices who were supportive and motivated towards physical activity took part126 and the evaluation relied on self-reported physical activity, which is prone to recall and response bias. 152 The LGM programme was also less successful when rolled out to other locations. In Gloucestershire, it did not work well alongside existing established local exercise referral schemes. The programme flow chart was viewed as too complicated and lacked the simplicity needed to align it with other programmes. There needed to be more investment in improving the visibility of LGM to ensure understanding of its role and purpose and for it to become successfully embedded over time into local routine health services. Recommendations for improvement included establishing a steering group to assist with co-ordination, wider consultation, improved alignment with current programmes, and streamlining paperwork to alleviate the challenge of delivering the intervention in a time- and resource-constrained setting. 130 Similarly, although the LGM pathway was accepted as a clinically feasible resource for primary care physiotherapists, it did require modifications and the support of additional resources. 131 Therefore, taking steps to align a practice with the elements of physical literacy may only work to increase routine physical activity promotion if the programme itself is aligned with existing systems.
When improving alignment of the practice with physical literacy, our work suggests that care also needs to be taken so that routine, embedded physical activity promotion does not become burdensome. For example, one participant explained the benefits of electronic systems designed to facilitate conversations about physical activity:
Templates are quite useful because they do prompt you to ask the question.
Practice nurse, interview participant 006
In contrast, one of the GPs interviewed explained how such tasks could be unhelpful:
But, would I want any more forms to fill in or boxes to tick or guidance that says, ‘If you can touch your toes and tie up your shoelaces without getting breathless you score a 1’ . . . it wouldn’t help me at all.
GP, interview participant 004
Similarly, NICE has acknowledged the competing demands on primary care practitioners’ time during patient appointments. NICE recommends that practitioners deliver very brief informal advice repeatedly, if this fits better with the time available. 150 Although brief interventions can increase self-reported physical activity in the short-term, there is insufficient evidence of their long-term impact, the impact that they have on objectively measured physical activity and factors influencing effectiveness, feasibility and acceptability. 118
Overall, the evidence suggests that in order to encourage the promotion of physical activity ‘as routine’, protocols, pathways and procedures are insufficient; an inherent belief in the value of physical activity or ‘physical literacy’ needs nurturing across the practice team. Some strategies appear to promote increased alignment of people, settings and systems to create an environment that promotes physical literacy. However, there also needs to be sufficient scope in a practice context for people to work in a biopsychosocial way, adopt a functional approach and promote physical activity to people with long-term conditions.
Context–mechanism–outcome statement 2: providing resources
Summary of context, mechanism and outcome
Physical activity promotion in primary care is inconsistent and unco-ordinated (context). If specific resources are allocated to physical activity promotion (in combination with a practice culture that is supportive) (mechanism), then this will improve opportunities to change behaviour (outcome).
The types of interventions that contributed evidence to CMO statement 2 are shown in Box 2.
Interventions providing additional resources such as:
-
dedicated time
-
financial resource
-
trained staff (including ‘social prescribers’)
-
electronic/remote interventions (e.g. online web applications)
-
resources to facilitate behaviour change (e.g. goal-setting diaries, printed booklets).
Inconsistent and unco-ordinated physical activity promotion (context)
Despite a rise in primary care physical activity initiatives and research,153 physical activity promotion in primary care remains inconsistent. For example, an online survey of 1013 self-selecting UK GPs found that the conditions for which GPs indicated that they would discuss and recommend physical activity varied from 78% for people who were overweight to 43% for asthma and 15% for cancer. There was a lack of skills, knowledge and confidence relating to the guidelines with only 20% of responders expressing that they were ‘broadly’ or ‘very familiar’ with the national physical activity guidelines, with over half reporting not having had any form of training. 154 Similarly, a cross-sectional study of 1937 patients in Germany were asked whether or not their GP had advised them about regular physical activity in the preceding 12 months. Only 33% stated that they had been advised to be more physically active, and those more likely to receive GP advice on physical activity were men; those suffering from specific long-term conditions such as pain, coronary heart disease, diabetes mellitus or arthritis; those taking more than five medications; and younger age groups. 155 In Australia, only 18% of patients (n = 1799) reported receiving a physical activity recommendation from their GP in the past 12 months, although other developed countries had higher percentages such as the USA (32%) and Canada (42%). 156 From a GP’s perspective, 95.5% (127/223) of GP survey respondents in Denmark reported giving advice on physical activity at least weekly,157 and over half of GPs in the USA reported discussing physical activity with most of their at-risk patients. 158 In a scoping review determining the extent to which GPs record information about physical activity in medical records, there was a large variation in the recording of advice on physical activity, ranging from 1% to 78.8%. 159
In the UK, primary care health professionals can refer patients with long-term conditions to exercise referral schemes, consisting of an initial assessment, a tailored programme of exercise and professional supervision. 160 Compared with usual care, they have shown a small effect in increasing the proportion of individuals achieving 90–150 minutes of at least moderate-intensity exercise per week. 122 However, these are often not implemented as intended, with low referral rates, and poor rates of attendance and completion. 65,161 Barriers to referral include geographic isolation, uncertainty about patient selection criteria, medicolegal responsibilities and a lack of feedback about patients’ progress. 162 In another focus group study, participants reported that it was not easy to access the scheme as it was poorly advertised by primary care staff. Very few participants had been referred to the scheme as a result of a GP or nurse making a recommendation and were more likely to have been informed about the scheme from others and then have requested a referral from staff themselves. 163
One participant in our theory-building workshops talked about her experiences of the exercise referral scheme, also highlighting a lack of co-ordination:
There’s the exercise referral scheme but we don’t refer a huge number to it because it is there and then it disappears due to short-term funding, or the criteria change and then you have to get a new form, with a paper pad that has to be signed by different people, everything else is online so it’s a bit of a palaver and puts barriers in place whereas it should be quite easy to do.
GP, interview participant 004
Awareness of alternative community initiatives can also be inconsistent and unco-ordinated. Out of a representative random sample of 800 Dutch general practitioners, less than one-fifth were involved in any kind of formal collaboration network with other health-care professionals and physical activity providers. 164 However, GPs who did participate in a formal alliance more often referred patients from their practice to a local fitness centre or sports facility. Furthermore, these GPs were more positive about the physical activity facilities in their area, indicating that this kind of co-ordination is valuable.
Finally, it is suggested that in order to develop and sustain consistency and co-ordination of physical activity promotion, synergy of all the relevant stakeholders is needed (e.g. government, civil society, private sector, non-governmental organisations and sport bodies) and should be implemented at all levels of physical activity promotion, including international, national, local and within the primary care teams. 153
Allocation of resources (mechanism)
To reduce the burden on GPs, many studies have identified alternative professionals to deliver physical activity advice. For example, interventions have involved practice nurses;165–170 health-care assistants;171 expert patients;172 physical activity ‘coaches’, ‘counsellors’ or ‘facilitators’;173–176 exercise professionals;177 physiotherapists;178,179 accredited exercise physiologists;180 or combinations of allied health professionals. 21,181 The idea is that these professionals are trained to deliver relevant physical activity advice and work with patients on specific goals, meaning that GPs can concentrate on other tasks and, consequently, enabling physical activity promotion to be delivered more consistently because specific resources (i.e. time, money and expertise) have been allocated for this purpose. To be effective, these professionals should be appropriately trained, appropriately resourced and the physical activity intervention should be aligned to condition management pathways. 153 However, there is a risk that delegating this task to other health professionals would mean that GPs do not feel responsible for this activity.
A randomised controlled trial of such an intervention has provided evidence of effectiveness and cost-effectiveness. In total, 203 Australian primary care patients were referred from general practice to exercise physiologists who provided face-to-face coaching and telephone coaching over 12 weeks. The primary outcome was step count, recorded for 7 days on a pedometer. Coaching achieved a modest increase in activity equivalent to 10 minutes of walking per day, at a cost of AU$245 (< £150) per person. The authors concluded that the persistence of increased activity at 9 months after the end of coaching suggests that this is a good value health intervention. 124 Australia is already in a unique position as the only country that provides some federal government sponsored reimbursement for exercise physiology consultations. Therefore, advice and referral to accredited exercise professionals can assist in promoting physical activity and exercise, reducing physical inactivity and, hence, potentially, alleviating some of the burden of chronic disease. 67 Although an increase from 0.38 to 1.44 referrals per 1000 encounters was shown over a 7-year study period, 2009–16, GP referral rate to exercise physiologists was low, suggesting that education about the role of exercise physiologists is needed. 185
An emerging type of intervention, involving ‘Care Sport Connectors’ (health-care or community-based exercise professionals) who connect primary care to the sport and recreation sector, is being tested in the Netherlands. 123 Patients are referred to these ‘connectors’ who help them be more physically active, by explaining the benefits and normalising physical activity as a behaviour rather than as a therapy. They guide patients towards local physical activity opportunities in the patients’ locality, at a time suited to them, thus reducing the burden on pressurised health services. 153 It is important to acknowledge, however, that surgeries staffed largely by GPs without much role substitution from nurses and other allied health professionals may have less flexibility to accommodate physical activity counselling. 128 As previously described, the LGM pilot study demonstrated that allocating resources to the identification of patients through electronic disease registers can improve the reach and effectiveness of physical activity interventions compared with opportunistic recruitment because this method enabled longer appointments to be made in advance and may have reduced selection bias on behalf of professionals. 128 The Exercise as a Vital Sign programme also enabled rapid, structured data collection by medical assistants through an electronic medical record system. Prior to the physician entering the room, medical assistants asked patients two questions: (1) ‘How many days a week do you engage in moderate to strenuous exercise (like a brisk walk)?’ (2) ‘On average, how many minutes per day do you exercise at this level?’. 186 The idea is that collecting this ‘vital sign’ data acts to increase physician and patient awareness of inadequate physical activity, thus acting as a ‘red flag’ helping to trigger a broad range of health-related, preventative actions, such as lifestyle counselling and referrals. These actions would then bring about increased physical activity, weight loss and improved glycaemic control among patients with inadequately controlled diabetes. 186
Finally, NHS general medical practices between 2014 and 2015 were provided with financial incentives to assess physical activity levels in people with hypertension using the General Practice Physical Activity Questionnaire (GPPAQ). However, it is not known whether or not this approach resulted in an increase in physical activity levels in this group as it was discontinued after 1 year. 154
Improved opportunities to change behaviour (outcome)
If physical activity promotion becomes more consistently co-ordinated in primary care through the allocation of resources, then evidence suggests that there will be improved opportunities for people with long-term conditions to change their behaviour.
The Exercise as a Vital Sign programme was designed to increase consistency and co-ordination of physical activity promotion through ascertainment and recording of patients’ self-reported physical activity by a medical assistant as part of an initial visit to primary care. The programme improved exercise-related clinical care processes (increased progress note documentation, exercise counselling and lifestyle-related referrals) and provided clinical benefit (e.g. weight loss among overweight/obese patients and improved glycaemic control among patients with diabetes), thus improving opportunities for behaviour change. This supports a model in which the identification and initial discussion of exercise can be increased by the systematic collection of patient-reported exercise data as part of usual clinical workflow. However, it is important to note that the clinical improvement was relatively small, suggesting that this approach needs to be linked to more intensive and effective tools to help patients increase their physical activity. Indeed, information-only interventions seldom have a clinically significant impact if not linked to effective means for patients or providers to act on the information provided. 186
The LGM evaluation128 found that identifying patients using electronic records was more effective than opportunistic identification, with the completer rate being 27% compared with 16%, respectively. This method of patient identification has been used previously in primary care-based health behaviour interventions. This is probably because the method removes the potential for selection bias that might be introduced when GPs or practice staff make subjective decisions about which people to promote physical activity to, and also does not rely on busy GPs or practice staff to remember to recruit patients. 187
In a systematic review,188 barriers to and facilitators of social prescribing were related to the implementation approach, legal agreements, leadership, management and organisation, staff turnover, staff engagement, relationships and communication between partners and stakeholders, characteristics of general practices, and the local infrastructure.
Despite limited evidence for the success or value for money, the use of non-medical referral, community referral or ‘social prescribing’ interventions have been proposed as a cost-effective alternative to help those with long-term conditions manage their illness and improve health and well-being. 182,183 Social prescribing includes but is not specific to physical activity promotion; however, the associated evidence is relevant because it involves a specific professional making referrals to community-based initiatives. 184
Other means of providing physical activity advice include online121,189,190 or telephone counselling,119,191,192 to improve opportunities for physical activity promotion. In one study, telephone counsellors with degrees in public health, health promotion or allied health sciences were trained to provide a patient-centred, motivational interviewing intervention. Maintenance outcomes for the 12-month telephone-delivered intervention for physical activity and dietary behaviour change demonstrated that the intervention was effective in promoting sustained behaviour change following a 6-month period of no intervention contact. 193,194 However, in 201 people with back pain, acceptance of face-to-face contact has been shown to be higher than with online or web-based coaching, indicating that integrating some element of actual contact is important to consider. 195
In conclusion, our work suggests that if primary care can consistently identify and advise patients about insufficient physical activity during their primary care consultations and link them to a robust referral system of physical activity opportunities, then this could improve opportunities for physical activity promotion.
Context–mechanism–outcome statement 3: individual advice
Summary of context, mechanism and outcome
People with long-term conditions have varying levels of physical function and physical activity, varying attitudes to physical activity and differing access to local resources that enable physical activity (context). If physical activity promotion is adapted to individual needs, priorities and preferences, and considers local resource availability (mechanism), then this will facilitate a sustained improvement in physical activity (outcome).
The types of interventions that contributed evidence to CMO statement 3 are shown in Box 3.
Interventions including behaviour change techniques such as:
-
goal-setting
-
personalised advice
-
motivational interviewing
-
social support
-
improving self-efficacy
-
considering local resources (e.g. social prescribing)
-
self-management.
Varying access to resources and varying individual characteristics (context)
Evidence suggests that individuals are on a spectrum of physical functioning and this can affect how people access or receive physical activity promotion. At one end of the spectrum are those who are healthy, active and mobile and who can organise their everyday lives independently, pursue their interests and are integrated into social networks. This group most often receives physical activity promotion through public health or through group interventions in fitness or community centres and would benefit from sustaining physical activity. At the other end of the spectrum is a group of chronically ill, immobile or frail older individuals who have already lost their independence and live in special residences or nursing homes. This group would most likely be approached by going into their residences and recruiting them for on-site exercise (group) interventions and therapy. Older people between those two extremes are often sedentary, with one or more long-term conditions and mobility restrictions, but still live in their own homes. This group are at high risk of losing their independence and have a lot to gain from increasing physical activity, but are difficult to reach for physical activity interventions. 59,155,196,197 This varying context of people living with long-term conditions is important to consider when designing ways of delivering physical activity promotion through primary care. For example, some patients may require one-to-one support and supervision to start and continue physical activity, whereas some patients require less direct input and would be able to self-select and self-monitor appropriate activities if given the opportunity. Similarly, in a survey of GPs, the most important barrier to referring patients to local exercise activities was their patients limited financial possibilities (46%) and restricted knowledge of local exercise or sport facilities (19%). 164
People with long-term conditions can also be at varying stages in the behaviour change process. According to the transtheoretical model (stages of change theory), a specific health behaviour develops and progresses, ideally but not inevitably, through five stages. These stages can be used to describe readiness to become and stay physically active and include (1) precontemplation, (2) contemplation, (3) preparation, (4) action and (5) maintenance. 198,199 For example, the Physician-based Assessment and Counselling for Exercise (PACE) intervention for people with type 2 diabetes aimed to change physical activity behaviour by applying this theory. However, a possible reason for the lack of effectiveness of the PACE intervention was that most intervention providers did not tailor their counselling to individual stages of change but instead discussed the same topics with all patients. 200,201
One participant interviewed as part of the current study corroborated this idea, stating that interventions would be less likely to succeed with ‘precontemplators’ as they are not yet considering change:
There’s no point in people starting to dictate to people if they’re not on board with it.
Public contributor, long-term condition, interview participant 005
The NICE guidance also highlights the importance of recognising times when people may be more open to change, such as when recovering from a related condition (e.g. following diagnosis of cardiovascular disease), as well as recognising when offering a behaviour change intervention may not be appropriate owing to personal circumstances. 202
Improving relevance of advice through adaptation (mechanism)
All relevant guidelines emphasise how physical activity interventions should be tailored for individuals and relevant in terms of an individual’s motivations and goals; current level of activity and ability; circumstances, preferences and barriers to being physically active; and health status (e.g. whether they have a medical condition or a disability). In particular, NICE guidance for exercise referral schemes recommend that policy-makers and commissioners should fund exercise referral schemes only if the scheme incorporates the core techniques of behaviour change, recognises when people are open to change, agrees goals and develops action plans, advises on and arranges social support, tailors behaviour change techniques to the individual, monitors progress, develops coping plans to prevent relapse, and collects data on the programme and participants. Furthermore, NICE recommends that when delivering brief advice, it is important to tailor it for people with a range of abilities, preferences and needs. 64,150 Advice should also be tailored to the availability of local resources and possibilities.
In addition, GPs have expressed dissatisfaction that patients do not act on advice about increasing physical activity levels and feel that a different approach is needed to effectively communicate information that is more amenable to patients’ personal situations. 136
This was further explained by one of the GPs interviewed:
It’s about taking a patient and establishing what they can do currently and then building from that . . . giving realistic scenarios of what they can do which is tailored to their ability and uses what is in community already.
GP, interview participant 001
Many studies and interventions have done this by linking into existing programmes or community initiatives,168,192,203–206 thus making physical activity opportunities more relevant and accessible in an individual’s local environment. The LGM initiative involved signposting patients to local physical activity opportunities including local authority leisure services, private clubs, sports and dance, pedometer schemes, outdoor activities and exercise referral schemes. 128 Furthermore, a 12-week primary care physical activity programme in Spain linked people with long-term conditions to local resources, encouraged social support and also included a visit with all participants to the nearest community resources (e.g. sport facilities). This was a place where regular physical activity could be continued and participants were offered a special monthly rate, thus reducing barriers associated with cost and resource availability. Increases in self-reported physical activity were sustainable over a 15-month period. 207 In a realist review of social prescribing, it suggested that patients are also more likely to engage if the activity is accessible and transit to the first session is supported. 184
A survey of 340 Dutch GPs found that 49% felt that giving a specific and directed recommendation was more effective in stimulating patients to start physical activity than giving open-ended advice. 164 Furthermore, people with chronic obstructive pulmonary disease have described pursuing physical activity because of personal interests, values and pleasure. 208
When asked about how best to adapt physical activity advice, one participant interviewed as part the current study said:
Asking them what they would like to do, rather than telling them to do something. What would you like to be able to do in your life that you are not able to do at the moment, and do you think you might be able to do it if you worked at it?
Public contributor, long-term condition, interview participant 002
Similarly, a practice nurse interviewed as part of the current study explained that they focused discussions on meaningful, personalised and achievable goals:
I try to set achievable goals . . . you have to know your patient well to set goals.
Practice nurse, interview participant 003
Research indicates that it is also important that physical activity interventions are adapted in terms of the amount of challenge given to participants. For example, in a qualitative study of older adults with and without cognitive impairment, healthy control participants placed more importance on interesting, challenging, and enjoyable physical activities whereas people with cognitive impairment emphasised the theme of ‘simple/light/safe exercise’. 209 Moreover, falls prevention programmes that are considered too demanding by the participants can have a negative impact on quality of life,210 with other researchers observing patterns in study attrition where participants with the worst function withdrew from the rehabilitation group (perhaps because it was too difficult) and those with better function withdrew from the control group (perhaps because it was too easy). 211 This suggests that a lack of tailoring can negatively affect the effectiveness of physical activity interventions, whereas incorporating individualised, relevant and tailored advice has the potential to maximise the relevance and effectiveness of advice.
Self-management and educational programmes, where there is increased patient involvement in long-term condition management, have a key role. 212,213 For example, a behaviour change counselling protocol was delivered by practice nurses, named the Self-management Support Programme, and involved consultations based on the ‘five As’ cycle counselling technique (assess–advise–agree–assist –arrange). The trial showed improvements in physical activity in people with long-term conditions, but also that the intervention was more effective with an accompanying, personalised monitoring and feedback tool suggesting that techniques to enable monitoring and feedback is an important element in promoting sustained behaviour change. 167,170
Finally, considering the impact of support networks that can act as barriers to or facilitators of physical activity is also shown to be an important part of promoting physical activity and physical function for people with long-term conditions. In many studies, participants were encouraged to use a variety of supports including family and friends, their health-care team and community supports (e.g. walking groups) identified from a community reference guide compiled at study outset. 187,193,194 Guidance from the USA214 also explains how participation in physical activity in a community setting with others, such as friends and family, can increase physical activity levels. Buddy systems, contracts with others to complete specified levels of physical activity, and walking groups are recommended ways to provide individuals with friendship and support for physical activity. 214 Furthermore, one-to-one sessions can be helpful to enable initial tailoring and review, whereas group-based activities can offer another source of immediate motivation, other than anticipated health benefits. As discussed by Fife-Schaw et al. :177 ‘The challenge is to associate exercise with other affective responses such as those resulting from success or socialising – hence an interest in linking activity to sport rather than repetitive activity on gym equipment’. 177 Group consultations for people with long-term conditions have shown positive effects on lifestyle, indicating significant potential for delivering system-wide benefits when resources are limited,215 and have started to gain traction in Australia and America, with examples also in the UK for diabetes care. 216
Barriers to physical activity that are relevant to support networks include an overprotective family member or the need to care for a family member. 208 One of the people with a long-term condition interviewed as part of this study also explained the different ways in which family support systems can work:
Some families may not be good for increasing PA [physical activity] as have a restricted view of the world, but walking with a friend and talking, you don’t notice the extreme pain. Some families are very supportive and can be very important for changing attitude but sometimes you need to go outside to find a support system for your activities.
Public contributor, long-term condition, interview participant 005
Sustained improvement in physical activity (outcome)
Many studies have described ‘tailoring’ of an intervention but have in fact chosen from a range of standardised protocols. However, in a randomised controlled trial of primary pare patients with musculoskeletal pain, tailoring an exercise intervention to patients’ highest-valued daily activity goals (e.g. ability to walk to the shop) resulted in improvements in pain, functioning and physical performance. 217,218 Furthermore, in a study of behaviour change counselling by Australian Accredited Exercise Physiologists (AEPs),180 flexible behaviour change counselling, based on the professional judgement of the AEP, and the preferences of the participant, resulted in improved physical activity levels in participants.
As living with a long-term condition can be unpredictable in nature, the ability to provide adaptable physical activity advice is important to promote sustained improvements in physical activity. Incorporating the ability to make adjustments to changes in individual needs over time means that interventions are more effective when compared with treatment solely tailored to predefined characteristics of a particular long-term condition. 217,218 Moreover, in the interviews conducted by Holden et al. ,219 the complexity of exercise behaviour was highlighted, showing that physical activity can fluctuate over time in response to numerous barriers and facilitators. In the light of this, several studies have incorporated relapse prevention elements. 168,169,171,220–222
Another important strategy highlighted by patients as way of increasing physical activity is establishing a habitual behaviour. 208 An example of this is ‘Join2move’, which is a successful web-based self-paced physical activity programme in which the patient’s favourite recreational activity was gradually increased in a time-contingent way. The programme sought to align with the day-to-day activities of people by including common activities (e.g. walking, cycling) that are easy to integrate into their daily routine. 223 Being able to retain independence and take part in activities that a person enjoys doing, has been shown to be important. For example, canine-based interventions and community-based football schemes appear to be effective in helping to initiate and sustain physical activity for people with long-term conditions. 224,225 Therefore, linking improvements in physical activity with personally relevant improvements in physical function may influence reasoning for being more physically active across the lifespan. A qualitative study including primary care patients with chronic obstructive pulmonary disease identified that believing that physical activity can positively affect chronic obstructive pulmonary disease can be a motivational factor. 208 Similarly, as part of a randomised controlled trial involving a physical therapist-guided aerobic exercise intervention for people with depression, 13 trial participants took part in semistructured interviews. In this group, movement could be categorised into four aspects: (1) movement as an absolute value, (2) movement as a personal value, (3) movement as a means and (4) movement as a sensation in body and mind. They connected their emerging categories ‘struggling toward your healthy self’ and ‘challenging the resistance’ to the aspect ‘movement as a means’ and ‘movement as a personal value,’ in terms of feeling proud and more like oneself again and by enhancing participation and ability. 226 Finally, in a mixed-methods review of exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis, it was concluded that people exercised regularly if they perceived exercise to be important, fun and enjoyable. However, if the benefits derived from exercise were not considered a ‘good return’ for the time and effort people invested, exercise was not sustained. 227
Taken together, our work suggests that physical activity promotion needs to consider the characteristics of the individual and their personal priorities, as well as the resources they have (or do not have) available to them and how these might change. Furthermore, doing so means that advice would be more personally relevant and improving physical activity is more likely to be sustainable.
Context–mechanism–outcome statement 4: improving capability of practice workforce
Summary of context, mechanism and outcome
Many primary care practice staff have a lack of knowledge and confidence to promote physical activity (context). If staff develop an improved sense of capability through education and training (mechanism), then they will increase their engagement in physical activity promotion (outcome).
The types of interventions that contributed evidence to CMO statement 4 are shown in Box 4.
Interventions such as:
-
training for primary care staff (e.g. Moving Medicine, the RCGP’s Physical Activity and Lifestyle Toolkit, Movement as Medicine, Motivate 2 Move, BMJ Learning)
-
education for health professionals as part of professional training curricula (e.g. Moving Healthcare Professionals Programme).
Lack of confidence and knowledge among practice staff (context)
Primary care is an ideal setting for physical activity promotion for people with long-term conditions because of its familiarity to patients who are used to attending for appointments, established trust and rapport, and the ability to assess eligibility. 196,228 Although the general medical practice venue has many advantages, the effectiveness of GP, nurse and other primary care staff counselling on physical activity is hindered by barriers, including a lack of educational resources for primary care professionals, a lack of formal clinician training for physical activity counselling and time constraints. 131 As previously mentioned, in an online questionnaire-based survey of self-selecting GPs in England, only 20% of responders were broadly or very familiar with the national physical activity guidelines, 26% were not familiar with any physical activity assessment tools and 55% reported that they had not undertaken any training with respect to encouraging physical activity. 154 Furthermore, in a qualitative study 12 in-depth semistructured interviews of nurses in Dutch general practices involved in diabetes care reported a deficiency in their lifestyle counselling skills. The nurses explained that they did not know how to develop a structured action plan in co-operation with the patient and the difficulties in adapting their counselling to the patient’s stage of change. The nurses expressed the wish to develop skills to overcome this barrier; for example, ‘Sometimes I supply information too fast. The patients are in an earlier stage of change’. 229
In a study examining the knowledge and practice of GPs (n = 342) and primary care physiotherapists (n = 89), more physiotherapists (50.5%) than GPs (28%) correctly reported the minimal physical activity guidelines. However, with the exception of overweight patients, GPs were more likely than physiotherapists to promote physical activity to patients with known cardiovascular risk factors, such as hypertension, suggesting that there is scope to improve knowledge. 230 In a recent study, two practice nurses and six health-care assistants delivered a theory-based walking intervention to 63 patients in their primary care practices. Although the intervention was mostly delivered as planned, motivational components aimed at improving self-efficacy were not. 125
Prescribing medication is considered a more attractive and effective option than promoting physical activity, with lifestyle behaviour change considered to be the most difficult part of diabetes management, with advice limited to providing specific, standardised suggestions such as walking for 30 minutes three times per week. 136,142
There also appears to be a lack of confidence, knowledge and understanding in the perceived roles and responsibilities associated with physical activity promotion. For example, in a qualitative systematic review of the barriers to effective management of type 2 diabetes in primary care, it emerged that, despite continuing policy drives to promote self-management, clinicians often find it hard to share responsibility effectively with patients to support behaviour change. Changing role boundaries, between primary and secondary care, and also between physicians and nurses within primary care, have generated uncertainty and unease about where clinical responsibility resides. 231 Similarly, in a survey exploring views about collaboration between GPs and exercise providers in the promotion of physical activity, half of the GPs thought that they had an important role in stimulating physical activity, while the other half considered their role present but ‘limited’. 164 On the other hand, in a process evaluation exploring the adoption and implementation of physical activity and dietary counselling by community health centre professionals (GPs, nurses and nurse practitioners, physician assistants), lifestyle counselling was rated as an important activity that they ‘should do’. This suggests that health professionals may be responsive to providing lifestyle counselling if it is brief, easy to implement (CMO statements 1 and 2), and if they can be trained at their convenience. 165
Improving sense of capability (mechanism)
When there is a lack of knowledge, skills or confidence, training, evidence suggests that it is important to encourage a sense of capability (or ‘self-efficacy’) among health professionals to promote physical activity. Indeed, patient behaviour change is probably related to GPs’ ‘professional self-efficacy’ to deliver an intervention. 232 However, recent surveys have highlighted the very limited medical curriculum time dedicated to physical activity and health, leaving professionals feeling insufficiently equipped to provide support or information to their patients. 233–236 In response, studies have developed interventions to address this need and improve capability among a variety of primary care professionals.
‘Movement as Medicine’ for type 2 diabetes represents an evidence-informed multifaceted behavioural intervention targeting physical activity for the management of type 2 diabetes. 136 It was co-developed for delivery in primary care. The exploratory work highlighted a need to focus on training provision for health-care professionals to equip them with the knowledge and skills to target the physical activity behaviour of their patients. Barriers to the acceptability and feasibility of the intervention were associated with six theoretical domains from the theoretical domains framework (TDF). These barriers and elements identified as having a positive influence are shown in Box 5.
-
Memory, attention and decision processes (i.e. difficulties recalling specific components of the intervention).
-
Optimism (i.e. that the intervention is unlikely to help change physical activity behaviour of patients).
-
Environmental context and resources (i.e. lack of time to complete training and practice intervention delivery).
-
Social influences (i.e. improving diabetes care is considered to be a practice norm and something healthcare professionals are already doing).
-
Professional role and identity (i.e. the belief that nurses and not GPs should be delivering the intervention).
-
Beliefs about consequences (i.e. the intervention will work only with a minority of patients).
-
Knowledge (i.e. completing the online training programme has improved knowledge of diabetes and the value of physical activity for glycaemic control).
-
Skills (i.e. the training programme has facilitated acquisition of behaviour change skills).
-
Beliefs about capabilities (i.e. practice delivering the intervention to patients will make it easier to use).
-
Intentions (i.e. completing the training programme has increased the likelihood that physical activity will be targeted in future consultations).
-
Optimism (i.e. practice will improve delivery of the intervention during routine consultations and lead to beneficial changes in patient behaviour).
Reproduced with permission from Avery et al. 136 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The box includes minor additions and formatting changes to the original box.
An online, modular training programme has been developed in accordance with GPs’ stated preference for flexibility in completion and is currently undergoing evaluation in a pilot randomised controlled trial. 136
The ‘Moving Healthcare Professionals Programme’ model is a partnership between Public Health England and Sport England which provides educational resources about physical activity promotion. The interventions are designed to ‘spiral through’ existing educational approaches rather than be additional special study modules or ‘bolt-on’ courses, thus reducing self-selection bias in completion. The programme has delivered face-to-face training to 17,105 health-care professionals, embedded materials in almost three-quarters of English medical schools and overseen > 95,000 e-learning modules completed over 2.5 years. Evaluation of individual elements of the model is ongoing and aims to focus on the impact it has on the confidence and capability to provide brief advice. The model is designed to take a whole educational system approach to embed physical activity into clinical practice, including integration in undergraduate education as well as develop the capability of qualified health-care practitioners. This programme is supported by a consistent public health awareness campaign reiterating the importance of physical activity advice from clinicians. The model is designed to eventually become redundant as a result of taking a ‘whole educational life’ approach, and as the clinical social norm shifts towards the routine integration of brief physical activity advice into daily clinical practice134 (see also Context–mechanism–outcome statement 1: changing practice culture through alignment).
One of the GPs interviewed as part of our study explained how knowledge and confidence might be influencing health professionals when talking to people with different long-term conditions about the benefits of physical activity:
It comes probably down to the knowledge and the confidence of the practitioner sat in front of the patient about how comfortable they feel about advising patients about physical activity with their conditions.
GP, interview participant 001
The ‘Exercise Is Medicine’ campaign established by the American College of Sports Medicine also aims to embed more information regarding the benefits of exercise through health professional training and continuing education programmes for primary care doctors and nurses. 67
Improved engagement of staff in physical activity promotion (outcome)
Effective physical activity promotion in health-care settings relies on professionals having the appropriate level of knowledge and skills to assess, counsel and support their patients. 153 Evidence suggests that an improved sense of capability helps improve engagement with physical activity promotion among primary care health professionals. For example, in comparison to GPs, who felt that their knowledge was inadequate, those who felt that they had adequate exercise knowledge were more likely to ask (72% vs. 49%) and counsel about exercise (48% vs. 29%). 237 Other health-care professionals, such as physiotherapists, nurses or pharmacists, are also able to counsel patients to be more active; however, they too are in need of training in physical activity-related counselling. 153
A Canadian study promoting the importance of physical function as a ‘vital sign’ developed professional skills in functional goal-setting through (1) workshops, (2) a problem-based learning module, (3) case reviews of selected patients participating in the study and (4) development of a flow sheet for monitoring changes in physical functioning to be used within a patient’s electronic medical record. Although there was no significant change in the amount or type of information relating to physical functioning that were documented in patients’ medical records, primary care professionals reported an increase in the level of patients’ physical activity, improved goal-setting and problem-solving, and greater focus in their interactions. However, professionals felt that their own efforts at integrating the self-management aspects of care could be improved, with the main barrier being a lack of time to address the multiple concerns that patients with chronic conditions face, meaning that self-management goals were often given a lower priority21 (see also Context–mechanism–outcome statement 1: changing practice culture through alignment).
It is suggested that a lack of education on this topic will limit health-care professionals from encouraging physical activity, reducing their personal confidence to deliver advice, lowering their perceptions of benefit, and adversely affecting public health and commissioning decisions. 238 Training health professionals to improve their knowledge about physical activity for people with long-term conditions, alongside how to apply effective behaviour change techniques, should improve their confidence and help them engage with physical activity promotion activities. However, evaluations of the current initiatives that are designed to enhance education and training for primary care health professionals and thus evidence to support this is currently limited.
Context–mechanism–outcome statement 5: programme credibility
Summary of context, mechanism and outcome
If a programme is credible (context), then trust and confidence in the programme will develop (mechanism) and more patients and professionals engage with the programme (outcome).
The types of interventions that contributed evidence to CMO statement 5 are shown in Box 6.
‘Accredited’ interventions, such as:
-
parkrun or ‘Couch to 5k’
-
Active Practice Charter from the Royal College of General Practitioners
-
Exercise referral schemes run by exercise professionals.
Interventions run by specially qualified professionals:
-
Exercise referral schemes
-
Falls prevention schemes
-
Cardiac/pulmonary rehabilitation.
Credible programmes (context)
Established programmes that take place in hospitals or leisure centres, and are delivered by qualified personnel (e.g. cardiac rehabilitation or exercise referral schemes), often have a high degree of inherent credibility due to their association with the health service, relevant regulatory bodies (e.g. the Register of Exercise Professionals) and inclusion as part of NICE guidance. 64 Furthermore, GPs often have established long-lasting, trusting relationships with their patients. 196,239 In Australian primary care, patients have been referred from general practice to receive physical activity coaching by exercise physiologists. The strategy is chosen because it is felt that a recommendation from a known and trusted GP would increase the uptake of coaching. 124
One of the patients in the current study also explained the credibility associated with recommendation from a GP:
Not everyone will want to take part but often they’ll listen to a doctor whereas they wouldn’t listen to anyone else.
Public contributor, long-term condition, interview participant 002
Similar views were captured in a qualitative exploration of facilitators of and barriers to active lifestyles among adults with osteoarthritis: ‘If my doctor tells me to [exercise], then I will’. 240
However, as discussed previously, it is likely to be unfeasible for a GP to deliver and follow-up more complex physical activity advice and, therefore, further elements of credibility are drawn upon. For example, a mixed-methods review reflected how information about exercise for people with osteoarthritis is viewed as valuable if it comes from someone who is considered to be a knowledgeable health-care professional, who can explain why a person should do something, tailors the advice, clearly specifies what (or what not) to do and explains the benefits of adhering to the advice. 227 Credibility can also be achieved by including peer-led elements. In line with Bandura’s social cognitive theory,241 if a person with a long-term condition sees someone similar to them following treatment and lifestyle advice (e.g. improved physical activity), their own self-efficacy to change their lifestyle can increase. 172 Moreover, leaders who are themselves patients with long-term conditions, or have close personal experience of a long-term condition, show greater empathy and tend to suggest more appropriate and realistic options than health professionals. Gamboa Moreno et al. 212,213 studied the impact of a self-care education programme on patients with type 2 diabetes in primary care. The programme was led by two leaders, one of whom either had a long-term condition or was a carer for someone who had. The other leader, who was a doctor or nurse, introduced themselves as a programme leader, rather than as a health professional, with the aim of strengthening the idea of peer education and support. Although this intervention did not show significant improvements in clinical outcomes for type 2 diabetes, self-efficacy improved significantly.
Intervention safety and effectiveness is also an important element of credibility for professionals and patients. In a home-based exercise intervention that was supported by primary care for older adults with long-term conditions and limited mobility (the HOMEfit randomised controlled trial), the authors concluded that it may have been ineffective due to the limited degree of supervision and less social interaction associated with a home-based intervention. There were also a high number of adverse events meaning that there were periods of restricted or suspended participation. 242 Similarly, one participant interviewed as part of this study described the need to know that a programme is safe:
They have to have their safeguards in place because the last thing they want is to push somebody to do something and then something happens.
Practice nurse, interview participant 003
When allocating physical activity promotion to other professionals, studies have ensured appropriate levels of training to improve credibility. For example, telephone counsellors in the study by Eakin et al. 194 had at least bachelor’s-level training in nutrition and dietetics, received intensive training in study protocols and motivational interviewing using a detailed training manual. This intervention led to modest but significant improvements in physical activity at 24 months for people with type 2 diabetes.
Increased trust and confidence in the programme (mechanism) leads to greater engagement (outcome)
Our work suggests that both professionals and patients need to develop trust and confidence in the programme to engage. An example of where a programme has not worked because of a lack of credibility among professionals is ‘Physical Activity on Prescription (PAP)’. The intervention was designed to increase physical activity among patients with a sedentary lifestyle but was used only occasionally by GPs in Sweden. In a qualitative study designed to explore and understand GPs’ perspectives of the scheme, it emerged that, whereas pharmaceutical treatment is used in the first instance and has good support, the PAP has low status and is regarded with distrust as some doctors feel the method lacks credibility and significance for the patient. Even though the GPs interviewed were convinced that physical activity was an important factor in preventing and treating illness, many were doubtful that a prescription can make a difference and were sceptical about the existing evidence for PAP and had doubts about the long-term effect. 243 The method was viewed as an attempt at a simple solution to a complex lifestyle problem, or as one GP stated in a focus group as part of Persson et al. ’s243 qualitative study:
We know that physical activity is good but I’m not sure that a slip of paper is enough.
Persson et al. 243
Similar findings have been shown in a UK pilot trial of the Physical Activity Clinical Advice Pad, where use of the pads reduced over time, with data suggesting that the decline could be explained by health professionals not seeing its value. 244 Therefore, it appears that professional acceptance and widespread implementation is more likely if an intervention is accompanied by an evaluation that determines its effectiveness and benefit. 153
In order to engage, evidence suggests that it is also important for professionals to feel that the intervention is reliable. For example, when exploring professional views of the National Exercise Referral Scheme it was concluded that a ‘lack of information about patient’s eligibility criteria or the nature of the intervention; long delays by the leisure centres in contacting, assessing and accepting the participants into the scheme; cumbersome paper work; and lack of feedback about patients’ progress as major factors that negatively affected their engagement with the scheme’. 162 One of the practice nurses interviewed in this study stated: ‘I do not know what happened to the patients once we referred . . . I just tend not to refer any more . . .’. 162
Finally, credibility has been shown to be an important factor in increasing patient engagement. In a mixed-methods review of exercise interventions and patients’ beliefs for people with hip, knee or hip and knee osteoarthritis, health-care professionals were viewed as an important source of information, advice, reassurance and motivation. Clear instructions and advice from a trusted health-care professional were important in allaying people’s fears and anxieties about exercise, and convincing them that exercise is safe and beneficial, with the provision of good advice and information having a positive influence on people’s attitudes and behaviours towards exercise and its benefits. 227 Feedback from professional focus groups about the physical activity advice pads suggested that tailoring advice to local opportunities added value for patients (see also Context–mechanism–outcome statement 2: providing resources); however, this was not built into the design of the intervention, which perhaps discouraged use by health professionals. 244 Evidence from the social prescribing literature184 suggests that adherence to activity programmes can be affected by having an activity leader who is skilled and knowledgeable, or through changes in the patient’s conditions or symptoms. Moreover, in a realist review exploring what is known about whether different methods of social prescribing referral do (or do not) work, it was suggested that people with long-term conditions are more likely to engage if they believe that the social prescription will be of benefit, the referral is presented in an acceptable way that matches their needs and expectations, and concerns are elicited and addressed appropriately by the referrer. 184
Further qualities and communication skills that people appreciate and derive value from include understanding, tolerance, taking a genuine interest, encouragement and support. 227 Furthermore, research suggests that active health professionals are more likely to provide better, more credible, and motivating advice to their patients. 146
The characteristics needed to develop trust and confidence were also highlighted by people with long-term conditions interviewed as part of this study:
They’d need to be welcoming. They’d need the right attitude. Happy disposition, I think . . . somebody who is friendly towards you and listens to what you’ve got to say and doesn’t disregard what you’ve said.
Public contributor, long-term condition, interview participant 002
Someone who is really qualified, got a good track record. They do assessments . . . part of the assessment is talking to people for a while, not just 5 minutes and that’s it.
Public contributor, long-term condition, interview participant 005
In summary, our work suggests that programme credibility is important to encourage both patient and professional engagement in a physical activity intervention. The right professional with the appropriate skills and resources, delivering an intervention proven to be successful, and endorsed by patient groups and a GP, seems to be the most effective.
Summary of final programme theory
Throughout the synthesis, five CMO configurations were developed and then refined to explain how physical activity could be promoted to enhance physical functioning (and also psychosocial functioning) in people with long-term conditions whose care is managed in primary care. Together, the configurations represent a final programme theory of what works, for whom, how and under which conditions. We suggest that this programme theory offers a more specific level of abstraction,245 which reflects the nature of the focus of this particular synthesis, and which could better guide the prototype intervention development. Ultimately, the aim in realist approaches is to generate mid-range (testable) theories by subjecting the programme theory to different contexts over time. For this study, our programme theory has resulted in an explanatory account which shows that:
-
Primary care settings are characterised by competing demands, and improving physical activity and physical function are not prioritised in a busy practice (context). If the practice team culture is aligned to promote and support the elements of physical literacy (mechanism), then physical activity promotion will become routine and embedded in usual care (outcome).
-
Physical activity promotion in primary care is inconsistent and unco-ordinated (context). If specific resources are allocated to physical activity promotion (in combination with an aligned practice culture) (mechanism), then this will improve opportunities to change behaviour (outcome).
-
People with long-term conditions have varying levels of physical function and physical activity, varying attitudes to physical activity and differing access to local resources that enable physical activity (context). If physical activity promotion is adapted to individual needs, priorities and preferences, and considers local resource availability (mechanism), then this will facilitate a sustained improvement in physical activity (outcome).
-
Many primary care practice staff have a lack of knowledge and confidence to promote physical activity (context). If staff develop an improved sense of capability through education and training (mechanism), then they will increase their engagement in physical activity promotion (outcome).
-
If a programme is credible to patients and professionals (context), trust and confidence in the programme will develop (mechanism) and more patients and professionals engage with the programme (outcome).
Revisiting the theoretical landscape
At the start of the project, we considered the theoretical foundations relevant to promoting physical activity and physical function (see Chapter 2). Table 2 provides a summary of where and how we found resonance between the final programme theory and the theoretical landscape.
| Overview of CMO | Commentary |
|---|---|
| CMO statement 1 | |
| Primary care settings are characterised by competing demands, and improving physical activity and physical function are not prioritised in a busy practice (C). If the practice team culture is aligned to promote and support the elements of physical literacy (M), then physical activity promotion will become routine and embedded in usual care (O) | This CMO is focused at practice level, uncovering the importance of paying attention to physical literacy. Organisational theories may also be informative, showing how interventions fit into different ways of delivering services and pathways |
| CMO statement 2 | |
| Physical activity promotion in primary care is inconsistent and unco-ordinated (C). If specific resources are allocated to physical activity promotion (in combination with an aligned practice culture) (M), then this will improve opportunities to change behaviour (O) | The contingency between resources, culture and behaviour is apparent in this CMO. Behaviour change theories were considered as part of the initial theoretical landscape. We suggest that this CMO may be underpinned by professional behaviours and organisational theories as well as behaviour theories (e.g. self-efficacy and self-determination theory) |
| CMO statement 3 | |
| People with long-term conditions have varying levels of physical function and physical activity, varying attitudes to physical activity and differing access to local resources that enable physical activity (C). If physical activity promotion is adapted to individual needs, priorities and preferences, and considers local resource availability (M), then this will facilitate a sustained improvement in physical activity (O) | This CMO recognises the individual at the core of intervention success or failure. Self-regulation, psychological theories of motivation, behaviour and behaviour change, health belief, planned behaviour, self-regulation of illness and sociological theories, habitus, social and peer support can all illuminate this CMO |
| CMO statement 4 | |
| Many primary care practice staff have a lack of knowledge and confidence to promote physical activity (C). If staff develop an improved sense of capability through education and training (M), then they will increase their engagement in physical activity promotion (O) | In the theoretical landscape we postulated that knowledge deficit may pose a barrier to intervention success in physical functioning. We suggest that further explanation is sought through examining this CMO through the lens of adult learning theory, self-efficacy and theories of motivation |
| CMO statement 5 | |
| If a programme is credible to patients and professionals (C), trust and confidence in the programme will develop (M) and more patients and professionals engage with the programme (O) | The importance of trust and credibility on the part of professionals and people with long-term conditions is illuminated by this CMO. Attention should be paid in intervention development to credibility enhancing solutions |
Co-designed prototype intervention
The Function First kit: a tool for primary care staff to support physical activity promotion
The design illustrated on the next few pages is not a ‘final’ design. It is a prototype or a concept that has been made into physical components using the methods described in Chapter 4. These would require far more detailed content if they were to be taken forward and subsequent co-design work may still add to, or change, some of these components. The participants involved in this co-design process felt that what is presented here embodies the features of the CMOs and represented their collective thinking about how best to realise this in a physical form.
The following pages illustrate the overall design concept, the various components are labelled to illustrate which of the five CMOs they represent and embody. This labelling is only for the purposes of this report and indicates how the research evidence manifests in a physical form. It is not proposed that these labels would be included in any end-product delivered to primary care.
The prototype is illustrated in the following way, using a combination of design images and written narrative:
-
general presentation of the kit and its packaging (Figure 15)
-
how box presentation could be branded to work with existing schemes (Figure 16)
-
components of box 1 and their relation to the CMOs (Figure 17)
-
components of box 2 and their relation to the CMOs (Figure 18)
-
detailed descriptions of each component in the kit
-
how a proposed web-based resource would complement the boxes.
The full design presentation file for the intervention, that could be used as part of the non-academic dissemination strategy for further development and potential future use, is shown in Report Supplementary Material 12.
FIGURE 15.
Design images showing the initial presentation of the Function First kit and its packaging, including how the CMOs are referenced.
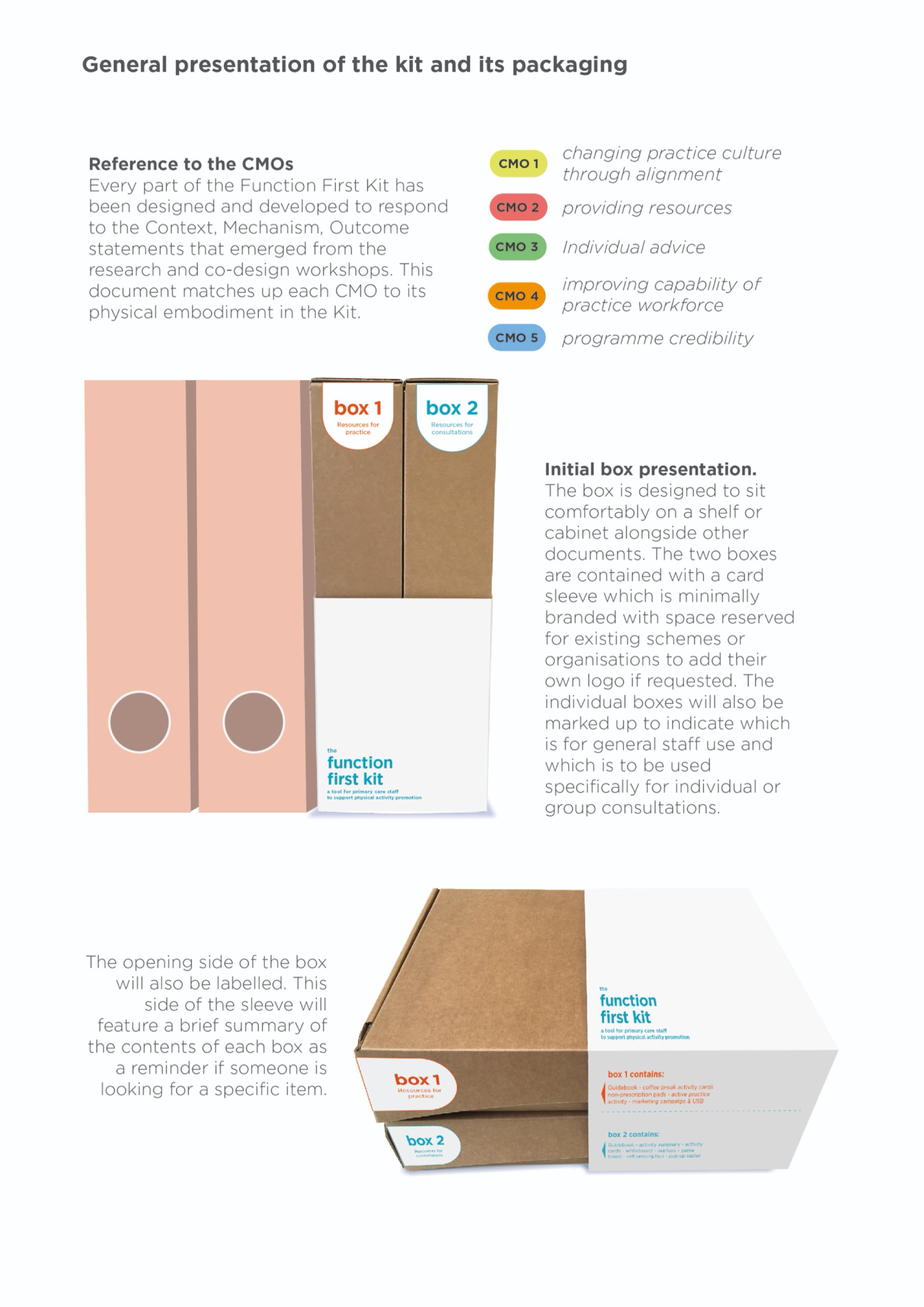
FIGURE 16.
Design images showing how box presentation could be branded to work with existing schemes. ‘Move More’ logo reproduced with the permission of Sheffield Hallam University (March 2020) on behalf of the National Centre for Sport and Exercise Medicine in Sheffield.

FIGURE 17.
Design image showing the components of box 1 and their relation to the CMOs.
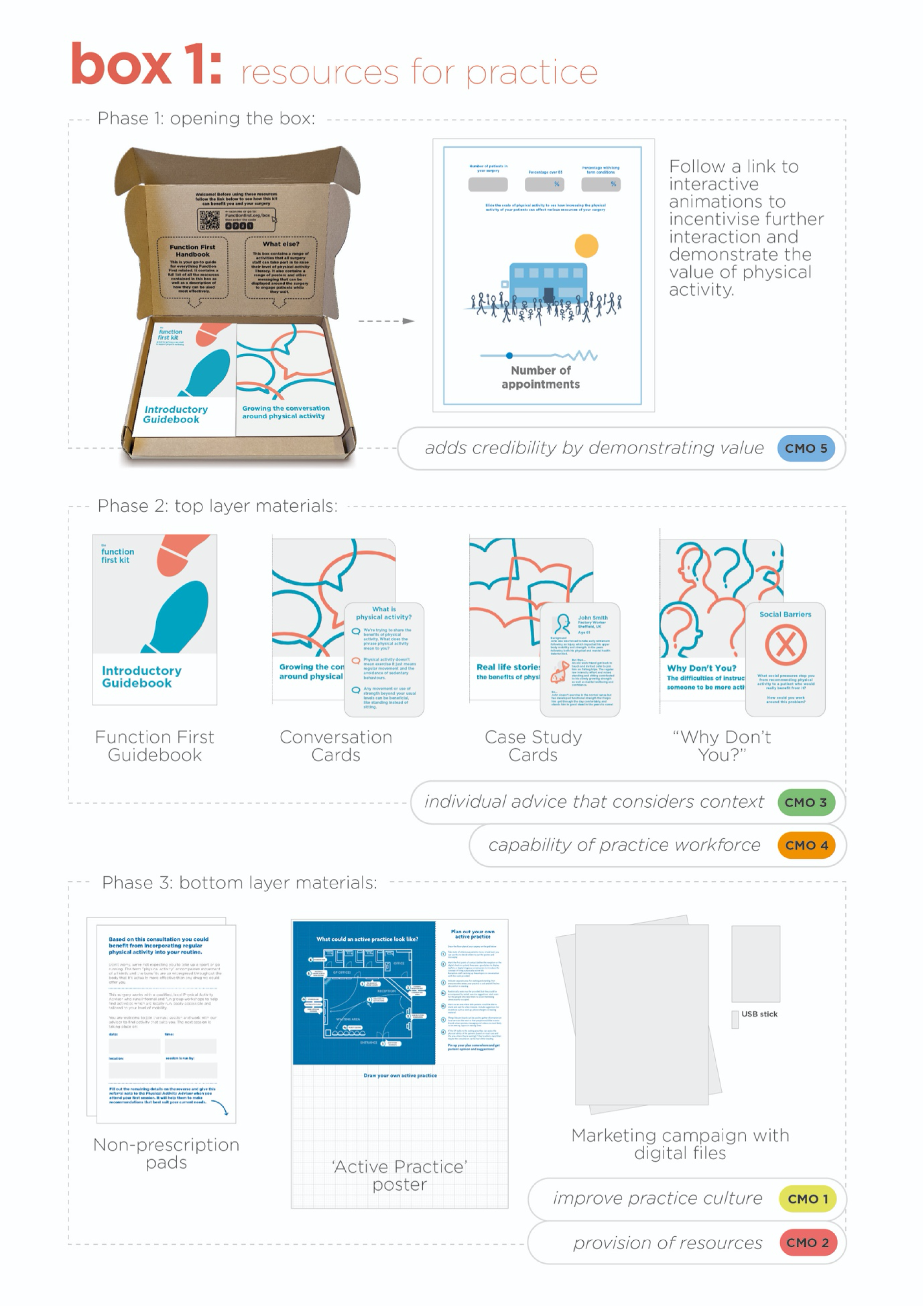
FIGURE 18.
Design image showing the components of box 2 and their relation to the CMOs.

Components of the Function First kit
The following sections provides a detailed description of each of the components of the kit.
The prototype itself is divided into two main parts, one aimed at the health-care service and the other at individuals, thus addressing two different sets of needs. However, both parts provide resources that enable people (primary care staff or people with long-term conditions) to ‘work out’ an optimal intervention for themselves rather than simply giving people a defined answer or a one-size fits all intervention. This addresses two fundamental and interlinked points emerging from the realist evidence: (1) tailored, individual solutions are more likely to be sustained and (2) involving people in working out a solution for themselves facilitates ‘buy in’ and gives people the tools and capabilities to make adaptations as needed. These are both important principles when considering the sustainability of an intervention.
For the health service users of this intervention, buy-in is essential; it must be worth their time and effort to engage with it. Therefore, the first thing they need to see as part of an intervention is the potential value to them and their practice. The remainder of the resources for the health professionals focuses on physical literacy, promoting dialogue between staff, promoting informed dialogue for all staff-patient interactions, and promoting visibility of the initiative within the practice.
For individuals, this buy-in is also important and so the resources aim to support a facilitated dialogue about personal circumstances, goals, resources and preferences, before following with the development of a personal plan, including addressing practical issues such as transport, access and scheduling to fit with other commitments. This holistic approach was deemed essential as it was often wider life issues that became ‘barriers’ to the uptake or sustainability of physical activity.
Box 1: resources for practice
Phase 1: opening the box
What is this box for? This box contains resources to help improve the practice culture around physical activity, by encouraging conversation and demonstrating the value of physical activity to staff and patients. There are four suggested steps:
-
Step 1 – ordering the Function First Kit.
When the kit is ordered a private profile would be created online for the practice.
-
Step 2 – opening for the first time.
From the moment the first box is opened, it needs to prove its value to the practice staff. The first thing staff would be prompted to do is to see how using the kit would benefit the surgery.
-
Step 3 – personalised interactive animations.
Following the link would take the individual to an online profile where they can interact with a series of animated scenes. Using practice-specific data, either preloaded or entered by staff, these animations would visually demonstrate the effect of physical activity on variables such as number of appointments, cost to the practice, time saved, etc. This should be a quick and effective way of demonstrating the value of physical activity to encourage further engagement with the materials in the box.
-
Step 4 – introduction to the materials.
The inside lid details the contents of the box as well as a recommended reading order. Initially the reader is presented with two documents: an introductory guidebook and a stack of card-based activities.
Phase 2: top-layer materials
This booklet summarises the goals and methods that would be used in the Function First kit, taking the reader step-by-step through each resource and explaining how it should be used. This would include a detailed strategy to find and recruit a ‘Physical Activity Advisor’ to be a part of the practice, delivering sessions to generate personalised recommendations for physical activity.
Phase 3: bottom-layer materials
These demonstrate a series of activities suggested by the participants in the co-design workshops. In this iteration they are represented as card-based resources. These could be used in a variety of settings, such as coffee breaks and team meetings, and include:
-
Conversation cards
These cue cards are designed to help reception staff initiate conversations with patients. This is to act as a kind of primer before the GP starts to raise these questions in the consultations.
-
Case study cards
A selection of real-life stories from patients and health-care professionals of the whole-body benefits of physical activity. To be read, shared and discussed as a group during a coffee break or team meeting.
-
‘Why don’t you?’ cards
A reflective activity where staff can address why they may not currently recommend physical activity to patients and as a group acknowledge and resolve the reasons behind these decisions.
Non-prescription pads are tools that help to communicate why a person has not received treatment in the form of medication, as might be expected. This method could be employed in this case, where physical activity would be recommended but not necessarily ‘prescribed’ in the traditional sense. An existing example is the non-prescription for ‘get well soon – without antibiotics’ that can be seen at www.wales.nhs.uk/sitesplus/866/page/75953 (accessed 13 March 2020). Figure 19 shows a prototype ‘non-prescription’ pad for physical activity.
FIGURE 19.
Design image of a ‘non-prescription’ pad for physical activity.

Evidence from the literature and from health professionals who have used physical activity prescriptions suggest that they have not worked in the past because a slip of paper is not seen as credible. However, it is proposed that this element would not be seen (or used) in isolation and would fit into the whole range of changes of culture, practice and behaviour for both patients and primary care professionals, giving it greater credibility.
This poster captures suggestions from co-design participants to make the GP practice more ‘activity friendly’ (Figure 20). Presented in the form of a blueprint, it provides inspiration and practical advice for creating more awareness and opportunity to engage in physical activity. The bottom half of the poster provides space to map out how a practice’s own space could be improved. Stationery would be provided to facilitate this.
FIGURE 20.
Design image detailing resources to facilitate the development of an ‘activity friendly’ practice.
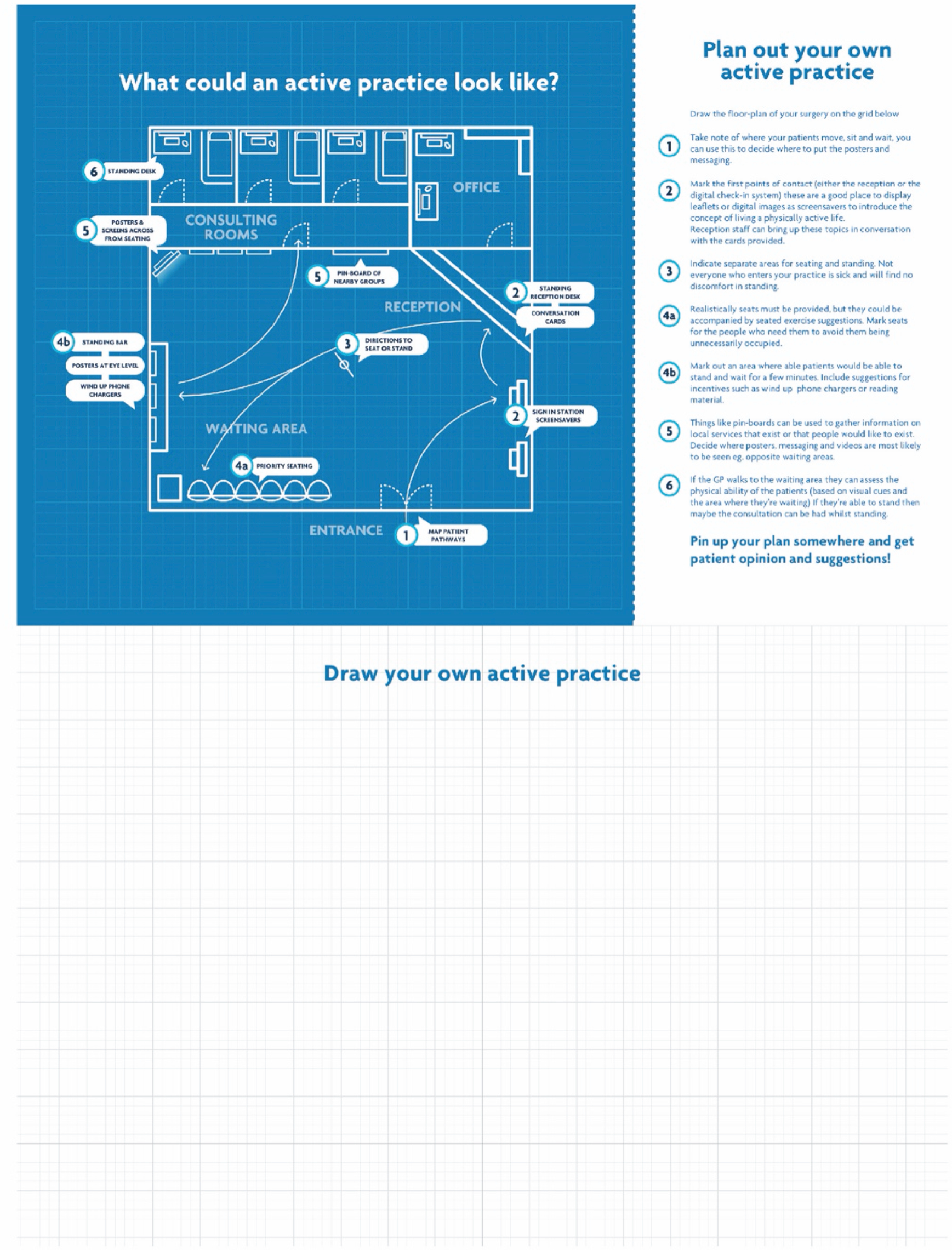
To help communicate a clear and consistent message across all GP surgeries, as well as more widely, our co-design work suggests a marketing campaign relevant to the benefits of physical activity. We have not developed the content for this yet but would take inspiration from the bold and creative campaign recently launched called ‘HELP US HELP YOU’ (www.adsoftheworld.com/media/print/nhs_take_the_drama_out_of_minor_illnesses; accessed 12 March 2020). Working with a marketing company alongside designers and artists, provocative and eye-catching posters and films have been created, encouraging people to change their behaviour and see a pharmacist rather than their GP. These posters cut through the traditional formality of marketing material found in GP surgeries and it would be worth considering the value of these in terms of effectiveness. The digital files for this campaign would be included in the box on a Universal Serial Bus (USB) or available to download through the online portal described in Function First online. These could then be displayed on screens or monitors already installed in waiting rooms.
Box 2: resources for one-to-one/group consultations
Phase 1: opening the box
What is this box for? One of the evidence-informed implications arising from the co-design work was the potential for a ‘credible professional’ to run consultations where participants can explore a range of physical activity options, work to solve potential problems or barriers and set attainable goals that take into account their life situation. This box contains resources to help someone run such a consultation.
As this box is designed for more social situations, the inside lid acts as a session summary and list of guidelines that can be referred to throughout the session. The box could remain open and visible to patients as the consultation progresses.
Phase 2: top-layer materials
The guidebook would be a reference document for whoever is running the consultation. It would contain methods and materials needed to run a range of activities as well as offering advice and useful strategies on initiating behaviour change. This would not be a patient-facing book but should be the first thing that the credible professional reads when receiving the kit for the first time.
This flip chart would be a patient-facing document summarising the goals and methods of each of the activities. It is constructed to be free-standing so could be placed on a table as a constant visible reminder of the activity in progress.
Phase 3: bottom-layer materials
These materials include:
-
Multipurpose game boards
A supporting feature to help facilitate different activities with the same set of cards. The actual content of these could be refined and developed during future co-production sessions (Figure 21).
-
Adding more utility/dimension to the cards
It could be useful to arrange cards on a tabletop or gameboard. The cards could be given even more utility if there was a way to elevate or prioritise cards. Conversely, it may also be desirable to hide or discard cards from view (Figure 22).
-
Self-prescription
This ‘self-prescription’ could be the take-away result of the card-game. Reflections and goals can be distilled into this simple folding card. This would act as a visual reminder of the goals set during the workshop and could be referred to during follow-up consultations (Figure 22).
FIGURE 21.
Design image showing details of guided card games.
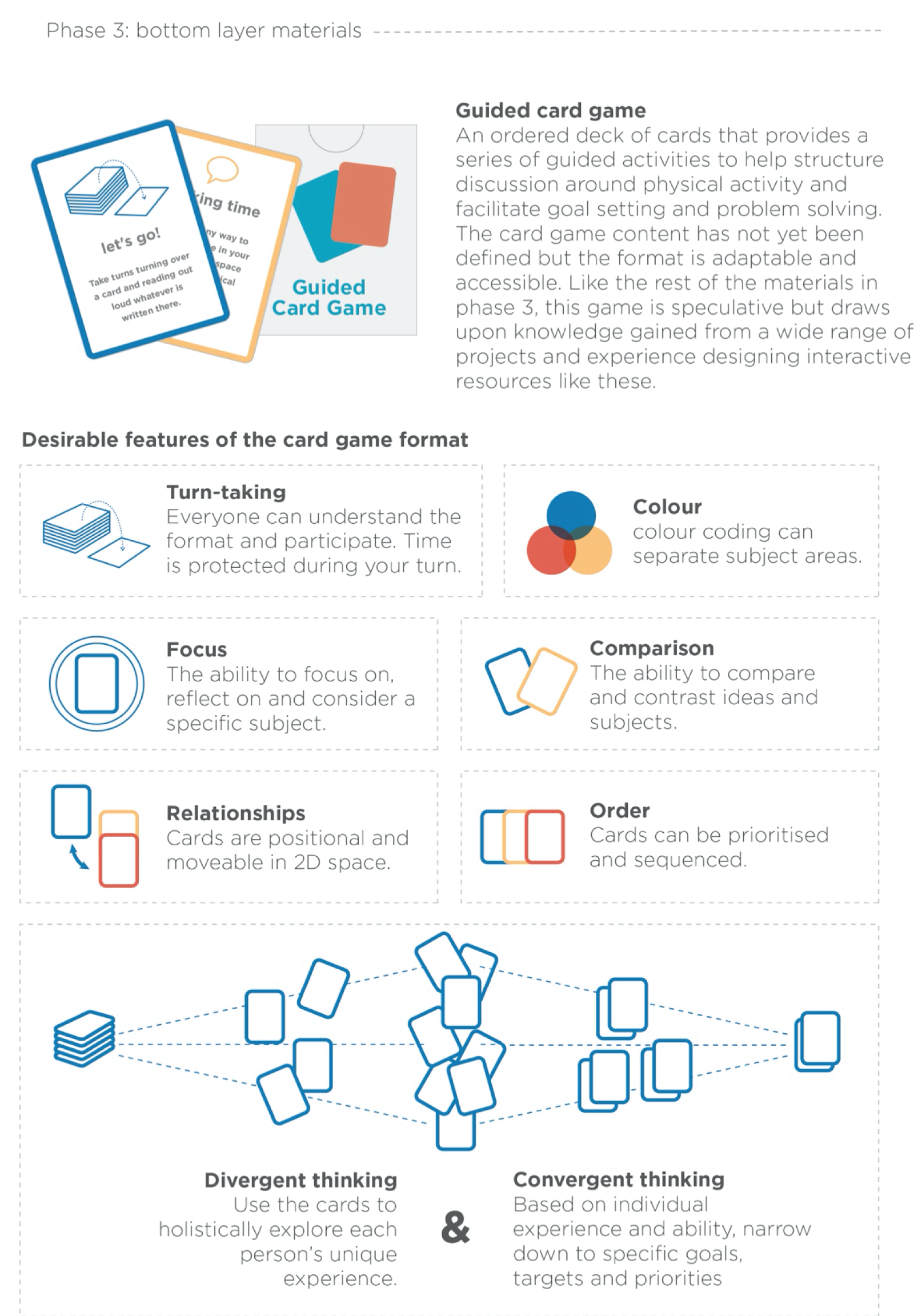
FIGURE 22.
Design image showing the multipurpose gameboards, methods of displaying cards and the resulting self-prescription.
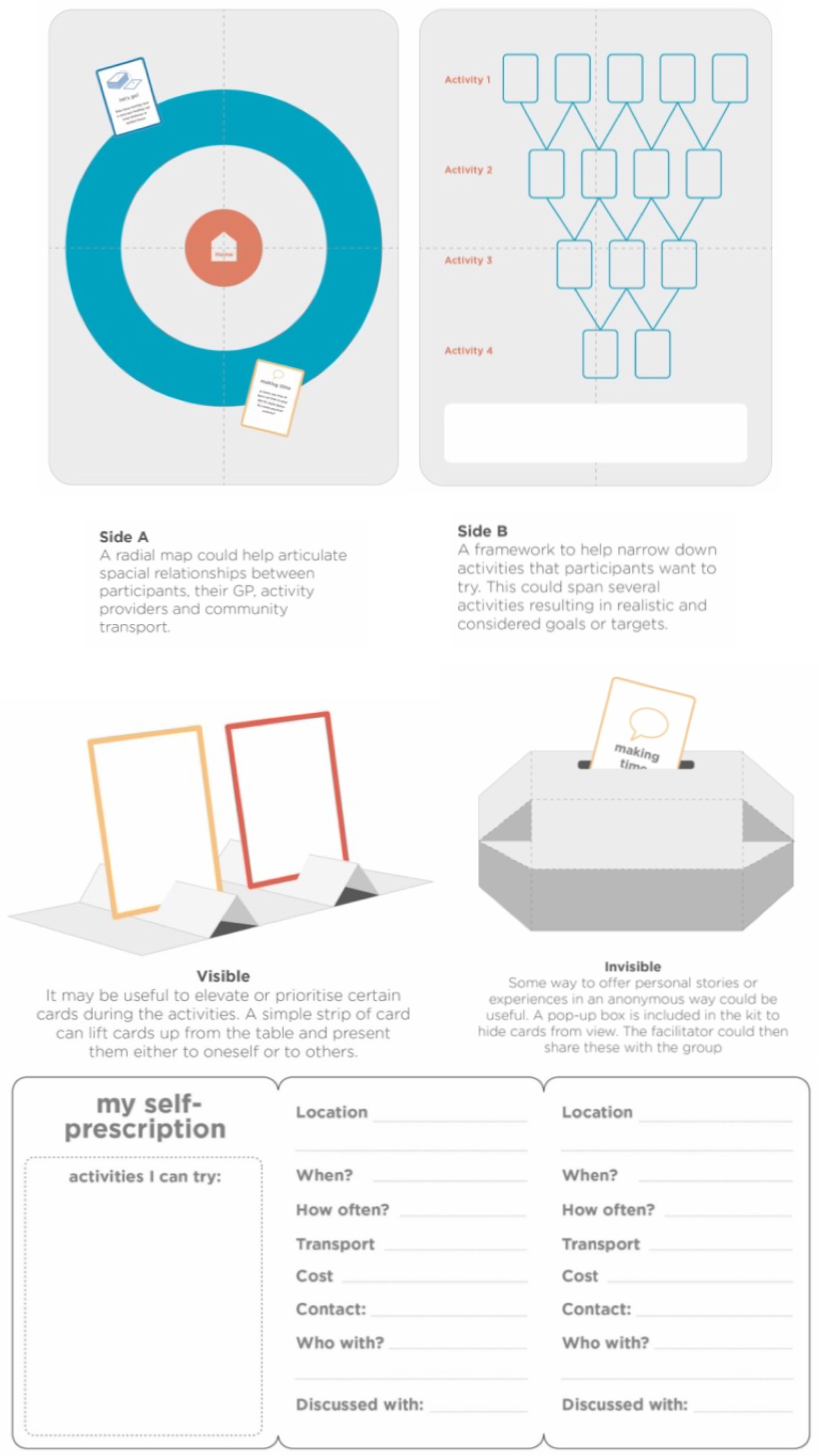
Function First online
A key evidence-informed implication that emerged was the need for an online directory of community assets that would benefit different stakeholders. In the interest of clear communication, what we present here is a conceptual online resource. We envisage an account system ensuring that individuals or groups would see only the information that is relevant to them. Report Supplementary Material 13 shows some initial examples of what each account would allow access to.
Directory of local assets
As shown in Figure 23, from here users could view a range of activities, groups, events and transport options in their local area. Activities could be filtered based on personal preference, ability, location and other variables. The Physical Activity Advisor would help people navigate the site during consultations.
FIGURE 23.
Design image illustrating screenshots of a website showing a publicly accessible portal to search and filter physical and social activities within a specific filter.

Personalised interactive animations from Box 1
The online profile could be the space where health-care staff are directed to see the personalised animations.
Patient goals and activity record
General practice staff and the Physical Activity Advisor can access simple patient information such as goals and agreed activities during consultation (Figure 24).
FIGURE 24.
Design image illustrating screenshots of web pages showing (left) a possible way of visualising local value to a primary care practice and (right) enrolled patients, their goals and current activities.
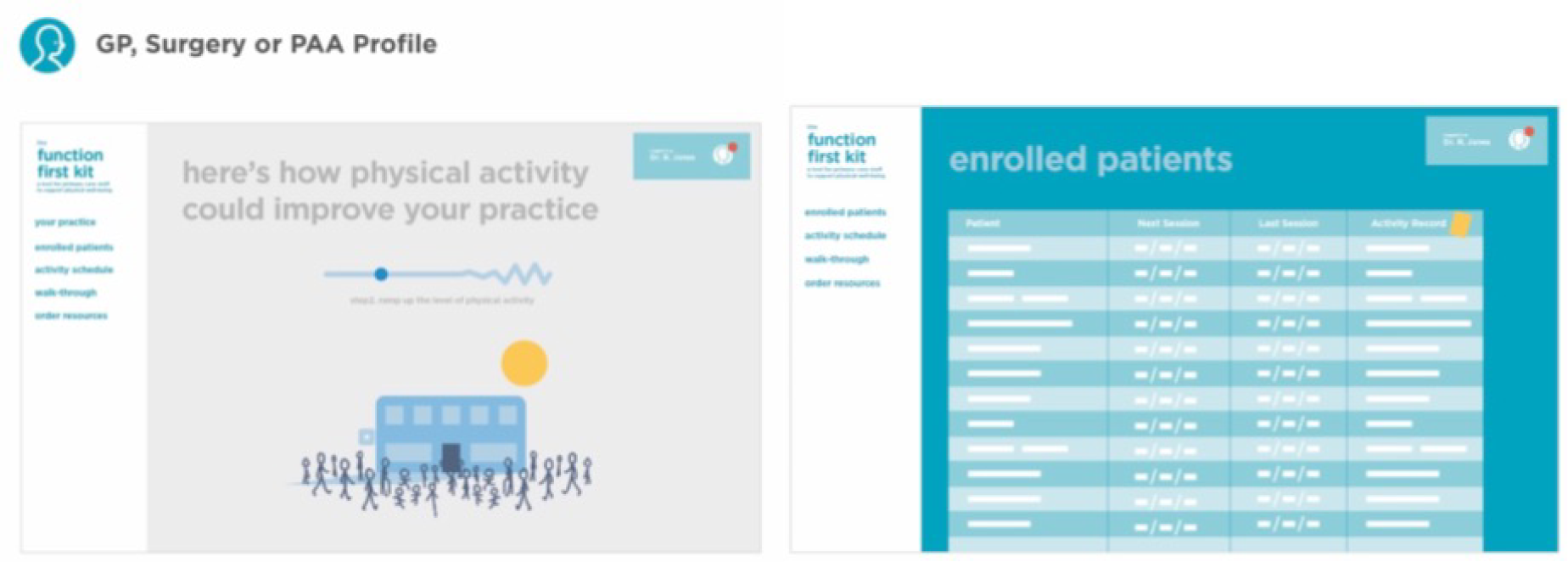
Community transport description and contact
Each transport scheme could have its own page populated by the team with a brief description of the service, who it is aimed at and a map of the operating area. If the user has added specific Community Transport scheme to their ‘favourites’, then they could see at a glance if it would be available to transport them to the activities on screen. This would enable reference throughout the rest of the directory.
Community activity description and contact
Each community activity scheme can have its own page populated by the team with a brief description of the service, photos of recent events, directions and contact information (Figure 25).
FIGURE 25.
Design image illustrating screenshots of web pages showing possible community transport links and ways that community activities could register on the directory to welcome new participants with long-term conditions.

Summary of co-designed prototype intervention
This section has presented the prototype Function First intervention; a whole system intervention aimed at addressing the individual needs of people with long-term conditions to maintain physical function, and the needs of the primary care practices supporting those individuals. Features of the intervention system that embody the CMOs defined by the evidence synthesis have been highlighted.
Individual elements of this intervention could work on their own and have some beneficial impact. Yet the basis and strength of this design, supported by the evidence from the realist synthesis, is that the sum of the parts is far greater than the individual elements; the impact of the whole will be greater than picking individual elements.
Throughout the co-design process, it was vital to provide continuous, accessible updates of the evolving CMOs to the co-design partners, highlighting how their input contributed to the evolution of the CMOs and ensuring that the CMOs were being directly addressed within specific features of the design concepts. This continuous attention to the flow of information between the realist synthesis and the co-design partners ensured a balance between research evidence and evidence from co-design partners in the creation of the prototype intervention, balancing the ideals of controlled academic studies with the lived realities of service providers and patients. Both realist syntheses and co-design are iterative approaches, and the natural synchronicity between iterations of both approaches in this project facilitated this two-way flow of information; it was a natural methodological fit.
For the wider research community, in the context of co-produced research, the approach we adopted can be used to overcome perceptions of tokenism in which non-academic contributors may feel undervalued or unable to contribute meaningfully.
Chapter 6 Discussion
Parts of this chapter have been reproduced with permission from Law et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Summary of findings
‘Function First’ aimed to determine the role of primary care in promoting physical activity and physical function for people with long-term conditions and developed programme theories, which describe what works, for whom and in what circumstances. This study is the first realist synthesis in this area, offering a theory-based consideration of the current literature, views and perspectives of the role of primary care in promoting physical activity and physical function for people with long-term conditions.
This realist evidence synthesis with embedded co-design has resulted in five CMO statements and a co-designed set of resources that embody these CMOs and are designed to facilitate improvements in physical activity and physical function for people with long-term conditions in primary care.
The five CMO statements are as follows:
-
Primary care settings are characterised by competing demands, and improving physical activity and physical function are not prioritised in a busy practice (context). If the practice team culture can be aligned to promote and support the elements of physical literacy (mechanism), then physical activity promotion will become routine and embedded in usual care (outcome).
-
Physical activity promotion in primary care is inconsistent and unco-ordinated (context). If specific resources are allocated to physical activity promotion (in combination with a practice culture that is supportive) (mechanism), then this will improve opportunities to change behaviour (outcome).
-
People with long-term conditions have varying levels of physical function and physical activity, varying attitudes to physical activity and differing access to local resources that enable physical activity (context). If physical activity promotion is adapted to individual needs, priorities and preferences, and considers local resource availability (mechanism), then this will facilitate a sustained improvement in physical activity (outcome).
-
Many primary care practice staff have a lack of knowledge and confidence to promote physical activity (context). If staff develop an improved sense of capability through education and training (mechanism), then they will increase their engagement in physical activity promotion (outcome).
-
If a programme is credible to patients and professionals (context), then trust and confidence in the programme will develop (mechanism) and more patients and professionals will engage with the programme (outcome).
We also co-designed a prototype multicomponent intervention with a range of stakeholders, embodying the emerging programme theories and developing resources to promote physical activity and physical function for people with long-term conditions. These consisted of resources designed to help nurture physical literacy among practice staff and complement existing schemes promoting physical activity. Suggestions for changing the layout of the practice and other promotional materials are included and would aim to create an environment encouraging physical activity. Although it is important that all members of staff promote physical activity during routine consultations, resources have been developed for a credible professional who can concentrate on physical activity behaviour change with individual people with long-term conditions. We developed prototype materials to facilitate this behaviour change, as well as resources to signpost to local community assets and to address barriers to the uptake of physical activity, such as community transport schemes. People would be directed to local exercise opportunities, clubs and groups following the adaptation of existing electronic social prescribing directories. These resources would need further development and refinement before being ready for use in practice (see Chapter 7).
Findings in the context of previous research and guidance
This realist synthesis of evidence has drawn from a wide variety of evidence sources and has identified many interventions designed for use by primary care professionals to promote physical activity to people with long-term conditions (e.g. LGM; Movement as Medicine for Type 2 diabetes). These have had varying levels of success in implementation. There are also a growing number of initiatives that provide additional education and resources for GPs and primary care staff on physical activity promotion for different long-term conditions (e.g. Motivate2Move, Moving Healthcare Professionals Programme, Moving Medicine). There is also the ‘Active Practice Charter’ developed by the Royal College of General Practitioners, which is designed to encourage practices to become ‘Active Practices’ by adopting ways of working to encourage physical activity in both patients and professionals. As described as part of this synthesis, research within the area of physical activity promotion interventions in primary care is rapidly developing; for example, the number of PubMed-referenced articles about physical activity within primary care has doubled between 2012 and 2014. 153
Recent Public Health England guidance246 on the prevention and management of long-term conditions summarises health and social benefits of physical activity, discusses the scale of physical inactivity and the barriers that people with long-term conditions experience. It then sets out available physical activity resources, programmes and campaigns for the public, physical activity training for health-care professionals, digital toolkits for clinicians, and initiatives in general medical practices such as the ‘Active Practice Charter’ and the parkrun practice initiative. There is a call for action for health-care professionals, local authorities and NHS organisations. What ‘Function First’ adds is:
-
a set of evidence-based theoretical statements of what works, for whom and in what circumstances when promoting physical activity and physical function for people with long-term conditions, and how this could be embedded in routine practice
-
a prototype multicomponent intervention of how this could be implemented, which involves practice alignment, a set of resources that sit alongside existing interventions and initiatives and makes a credible intervention for people with long-term conditions and their treating clinicians.
To our knowledge, this realist synthesis is the first to explore the role of primary care in promoting physical activity and physical function for people with long-term conditions. There are a limited number of existing realist evidence syntheses in the area of physical activity promotion for people with long-term conditions. In the primary care setting, a realist review has explored what works, and why, in the identification and referral of adults with comorbid obesity to weight management services. Similar mechanisms to the current study emerged including those operating at an individual level, such as having the confidence to talk about weight management and recognition of the importance and value of weight management. At an interpersonal level, mechanisms included discussing weight management at the right time and without blame. However, most mechanisms were operating at primary care practice level, requiring changes to systems or culture, such as developing consensus around working to promote weight management, not assuming ‘one size fits all’ and improving communication between practices and weight management services. Importantly, this review also identified contextual factors including varying patient and practitioner characteristics and competing priorities. 247
In an evidence synthesis, which included a realist approach, different versions of a health-related lifestyle advisor role in improving health were explored. Levels of acceptability were high, with advisors helping to remove barriers to prescribed behaviour and creating facilitative social environments. However, there was only limited evidence suggesting that lifestyle advisors have a positive impact on health knowledge, behaviours and outcomes, and there was some ambiguity about the role and the impact of the lay and peer characteristics of the interventions,248 thus indicating that further development of this role and subsequent research is required. Finally, similar evidence in a realist review found potential benefits of promoting physical activity when health care was located in leisure settings including theories relevant to the creation of a physical environment that re-enforces a physical activity culture and supports behaviour change, improvement of staff and patient experience, increased collaboration and co-ordination between health professionals, and increased awareness of facilities. Theories explaining the challenges of embedding physical activity in the NHS concerned the logistics of service delivery and inconsistency of clinical schedules. 249 One example of a strategy designed to create a culture of physical activity across a larger population is ‘Move More’ in Sheffield, which has been commissioned in three locations where medical intervention and physical activity are combined. 250
As far as we are aware, this study is the first to co-design intervention resources that embody realist programme theories, particularly in the area of physical activity promotion for the primary care management of people with long-term conditions. There are limited examples of the application of realist methods to facilitate intervention development. One such example is a study developing a complex intervention for improving outcomes in elderly patients following hip fracture. Three programme theories were developed and used to inform intervention development: improving patient engagement by tailoring the intervention to individual needs, reducing fear of falling and improving self-efficacy to exercise and perform activities of daily living, and co-ordination of rehabilitation delivery. 251 Studies have also used participatory methods to co-create new ways of working. For example, ‘Movement as Medicine’ included stakeholder work to develop a prototype intervention136 and the Choose to Move programme in Canada has been shown to enhance physical activity, mobility and social connectedness in older adults. 252 This study also highlighted the central role of community-based partner organisations when scaling up complex interventions in diverse settings, alongside the need to interact with stakeholders to develop collaborations and engage at multiple levels, in multiple sectors. 252
Strengths of this work
This project had a strong and embedded co-production element. People with long-term conditions, primary care health professionals, researchers with relevant expertise and experience and other relevant stakeholders were involved regularly at all stages, both as research participants and as members of the study oversight groups. The Study Management Group and independent Project Advisory Group provided scrutiny and advice, but also academic input into the development of the programme theories and co-design processes. Research participants were involved in co-creation activities designed to facilitate input into the development of programme theories and associated Function First resources. An initial stakeholder analysis strengthened this co-production element by ensuring that we captured insight from relevant groups.
We carried out systematic, comprehensive and transparent literature searches to identify a wide range of evidence that could be used to identify underlying programme theories. We used Covidence software to enable a team of reviewers to contribute to all aspects of the review process involving a large data set of publications. The theory-building work informed the inclusion and exclusion criteria, which were refined in an iterative manner. Implementation of the ‘good and relevant enough’ criteria at the data extraction stage allowed a more inclusive approach within the synthesis. Discussion among review team members, and iteration as the review progressed and programme theories were developed, was essential to ensure rigour. Discussion about the nature and quality of the evidence also helped to inform thinking about the emerging programme theory as the synthesis developed.
We co-designed a set of tangible resources that embodied the programme theories. These resources were designed to be flexible and to augment existing initiatives that are working successfully. They need further development and refinement before they can be used in primary care consultations.
A strength of co-design is that it involves giving new ideas tangible form and testing how these will work in the real world. It is ‘solution’ focused, looking to introduce something into the world that will create change. It considers the ‘solution’ at various scales, from the specific to the general, from the individual to the mass market. It considers technical as well as aesthetic matters. Co-design is democratic and pragmatic, ensuring that the issues relating to desirability, feasibility and viability have been considered by the involved stakeholders both throughout the generation of ideas and the embodiment of those ideas into tangible forms. It provides a solution within constraints; for example, if cost is the limiting factor, then the solution will be tailored to fit the budget.
The use of material culture such as LEGO Serious Play and the physical prototypes to share ideas and knowledge in co-design processes is a vital component for democratising the process by removing the exclusivity of technical language. It is also a ‘designerly’ skill and inherent to ‘designerly’ ways of thinking. This makes it a notable feature that distinguishes ‘designerly’ co-design (led by and facilitated by designers such as in this study) from ‘design-like’ co-design (led by and facilitated by non-designers). 253 The visual and physical objects made become boundary objects for sharing ideas and knowledge. We hypothesise that this relationship with material culture has implications between the final physical manifestation (the intervention) and knowledge mobilisation or use of the intervention. Material objects can mediate and afford people agency, guide a person through a series of actions or words, and give them a tool with which to perform a specific action. For example, when a person unpacks a new mobile telephone, the package, its contents and the way it is packed should lead the consumer through a series of intuitive steps. This agency that the consumer is afforded is mediated by the design of the box, its contents and the way that it is arranged.
The use of qualitative interviews to help refine the programme theories is an established part of realist method and was extremely valuable in this study. As described by Mukumbang et al. ,254 these interviews helped to ‘reinforce and maintain theoretical awareness and contribute to trustworthiness’. They were also helpful in other ways: guiding further literature reviewing, enabling more in-depth exploration with stakeholders we had not yet been able to hear from, contributing to a greater understanding of context and acting as a sense-checking point for the developing ideas.
Overall, the realist approach offers a theory-driven explanation that considers theoretical depth, breadth and transferability. Guided by realist principles, it is based on the assumption that reality is dynamic. Theorising was not purely deductive (theory-testing) or inductive (theory-building), thus providing more scope for deeper theorising and greater ontological depth, and potentially wider applicability of the resulting theories. 255 The key methodological strength of a realist approach is the requirement to pay attention to context. The analytical stance assumes that individuals, including patients and primary care staff, and the systems in which they live and work, bring different perspectives to the promotion of physical activity and physical function. Consequently, different patterns of outcomes may be observed, which can be specific to time and place, and, in this sense, the successful promotion of physical activity in primary care can be described as emergent. Any structured attempts to improve activity therefore meet the definition of a complex intervention and require particular methods for development and evaluation. Although the purpose of some systematic review approaches is to manage and control for context in the specification of an overall effect size, a realist approach has enabled us to focus our analysis on the interactions between context and physical activity interventions. We have done this by specifying conjectured, contingent hypotheses about what might work and how physical activity programmes generate engagement and success.
Finally, this study was conducted in a highly iterative, at times almost cyclical manner. Originally intended as a largely linear and sequential process, it emerged during the process of conducting the study that the iterative nature of the interaction between elements of the study added unanticipated strength and richness. It facilitated a greater integration of the different sources of data and enhanced the depth and breadth of the findings. This demonstrated that it is possible to deliberately overlap stages in a realist synthesis with embedded co-design, enabling the process to be more emergent. This became a much more natural evolvement of knowledge and helped to improve our collective understanding of the evidence into a shared body of knowledge, which was then embodied into the ‘product’. In fact, the striking ease with which the two methodological approaches (realist review and co-design) related to each other led us to reflect on their similarities and differences. ‘What works, for whom in specific circumstances’ connects the two as a fundamental way of expressing realist synthesis, yet also an important aspect of design. Although similar, realist is more cognitive and theoretical, whereas design is more practical, tangible, based on making tools, artefacts or materials. However, employing a design–evaluation cycle is hypothesised to improve the design and implementation of complex innovation by using programme theories to develop design propositions, which are evaluated through realistic evaluation, resulting in further refinement of programme theories. 256
Challenges, limitations and alternative approaches
A realist approach generates evidence-based hypothetical ‘recommendations’ that are developed at a specific time and place, by specific stakeholders. They are context specific and, as with all methods based on qualitative findings, they may not apply in a different set of circumstances.
The literature searching identified a large volume of literature due to the broad research area. The aim was to be comprehensive to capture a diverse range of evidence. This meant that we had to manage large numbers of publications and had to adapt our reviewing methods to deal with this large volume. The Covidence software was helpful in managing the data and for screening abstracts. Screening guidelines and inclusion/exclusion criteria went through multiple stages of refinement by the project group who all understood and agreed on the final criteria. This meant that all members of the project group could take part in the screening of abstracts.
To identify programme theories as soon as possible at the start of the review, we carried out a broad literature search early in the project. This search aimed to capture descriptions of all interventions that had been designed to improve physical function in primary care for people with long-term conditions. This gave us a large library of relevant papers that we could select from but presented a large number of data to sift. An alternative option would have been to build up the initial programme theory areas based on preliminary scoping and a review of reviews, and then to design a purposive search designed for each of the identified theory areas.
The grey literature search included a review of websites and publications of relevant UK organisations. However, only a small number (five items of grey literature and five guidelines) were included in the final data set. We recognise the importance of these other sources of evidence for avoiding publication bias, to provide useful contextual information and to understand interventions and programmes that are already used in practice. We faced a challenge in capturing undocumented knowledge. Although we did not extensively survey social media communication channels, the review benefited from the strength of the stakeholder group and attendees at the workshops who were able to identify additional unpublished evidence.
Despite having identified a large number of published data on physical activity interventions for people with long-term conditions, we found that in most of these publications there was a lack of detailed description (thick description) of the organisational context, delivery planning, patient characteristics and the circumstances that led to the success of the intervention. We also found fewer published reports of negative results, or descriptions of complications that had led to interventions not being as successful as planned. However, we aimed to identify, and present in this report, the clearest evidence describing what lies beneath the success of an intervention.
As a result, coverage of what ‘does not work’ may appear to be less well covered than ‘what works’. Some of this is due to framing (i.e. we tended to frame our statements and programme theories more positively than negatively). However, it is important to note that although more difficult to find, we did make a point of exploring ‘what does not work’ in the literature. For example, ‘one size fits all’ approaches, and interventions introduced without consideration of existing schemes and pathways, appeared to work less well.
The LEGO Serious Play method, facilitated by experienced researchers, successfully enabled all participants to reflect and build models to help them explain their thoughts regarding the questions posed in the ‘theory-building’ workshops. However, the following two challenges are standard to the practice of co-design. First, there were some challenges associated with instilling confidence in participants to build models on an abstract topic. However, facilitators led participants through a series of skills-building ‘warm-up’ type activities that helped participants feel comfortable using the methods. Second, one participant explained how the activity was an emotional process because the activity and questions posed were reflective in nature and likened it to ‘therapy’. This was not a new finding and is common to many methods that encourage reflection, deeper thought and explanation. We reiterated at future workshops that although there would be scheduled breaks, it was also completely acceptable for anyone, to take a break at any time if they felt that they needed a physical or emotional break. There were two ‘new’ challenges that arose during the LEGO workshops. First, one of the workshop participants was partially sighted but was able to contribute fully to the workshops; we spent more time with them, explaining what was in front of them and using larger LEGO blocks. Second, it proved more challenging to encourage professional participants to reflect on their professional experiences of working with people with long-term conditions, rather than their own personal experiences of physical activity and physical function.
Co-design is often criticised for being too specific, focusing on the needs of the participants in the process, resulting in personal rather than generalisable solutions. Design strategies, such as the use of personas, is a mechanism for addressing this as it asks co-design participants to design for other people (the personas) that are more widely representative. This weakness was mitigated further by introducing the evidence through the medium of card games at the start of the co-design process. This shared the wider, generalisable evidence with the co-design participants. Thereafter, the visual story of the whole project and the list of evolving CMOs was displayed on the wall for every co-design workshop, ensuring that the participants maintained this wider context and understanding of the evidence throughout the co-design activities.
There are many initiatives promoting physical activity. There are challenges when introducing yet another physical activity programme in a saturated environment. From the outset, we aimed to complement and not compete with these campaigns. We acknowledged and addressed this by involving representation from relevant bodies in our activities and including a specific search for existing initiatives and campaigns. We believe that many of these initiatives could address some of our programme theories, for example the promotion of physical literacy among all practice staff, and facilitating behaviour change within the consultation. However, these initiatives do not address all of our five programme theories and are individually insufficient to promote physical activity and preserve physical function in all of the people with long-term conditions managed in primary care. We have designed a multicomponent intervention, in which several of the components could be interchanged with materials that have already been developed.
We also acknowledge that despite using a stakeholder analysis, our range of stakeholders included people with similar socioeconomic status, ethnicity and attitudes and, therefore, the findings may be limited in their application. However, although indirect, these varying considerations were represented in the literature and in workshop activities that involved considering issues from the perspective of a range of different people.
Chapter 7 Conclusions
The challenge of improving and sustaining physical function through physical activity for people with long-term conditions is complex and multifaceted. It requires a mixed-mode complex intervention whereby any one component in isolation is likely to have limited results. However, when combined, these components augment each other. An intervention also needs to reach deeply into the health-care organisation, nurturing health-care professionals’ personal and professional capacity and capability and developing the capacity and capability of each person with a long-term condition.
The use of participatory design and realist synthesis methods, from the theory-building workshops through to the knowledge mobilisation workshop, has demonstrated a process with interdisciplinary strength, active participation and engagement throughout the project. It has enabled a strong synthesis of patients’ and professionals’ lived experience with literature and wider academic sources.
Implications for primary care
If general medical practice in the UK is to address the low levels of physical activity, and poor physical functioning of people with long-term conditions then current practice needs to change. Involving the whole practice, nurturing physical literacy and developing a commitment that it is everyone’s role to promote physical activity at every appropriate opportunity is important and would need a change in the emphasis of the practice team and additional resources to support behaviour change. Initiatives already exist for this, for example Public Health England and Sport England have developed the Moving Healthcare Professionals Programme. 134 However, this training needs to include all the practice staff, and not only the enthusiastic clinicians. There are also many initiatives that have been developed to promote physical activity behaviour change during consultations, for example the Faculty of Sport and Exercise Medicine UK initiative ‘Moving Medicine’. 135 However, time constraints and competing priorities are significant barriers to using these materials in all consultations for people with long-term conditions. Our work suggested that a new role could be developed for a credible professional who has protected time for this activity. This physical activity advisor could be a nurse, a physiotherapist, a physician associate, or one of the new roles in health care such as social prescribing navigators or exercise scientists. The job description for this role and the funding model needs further development. Our work also suggests that it is important to engage with local providers of physical activity opportunities and fully utilise electronic directories that are being developed for social prescribing. It is acknowledged that these resources and new roles need to be flexible enough to apply in the differing contexts of different general medical practices. The development of primary care networks, or clusters of practices, provides the opportunity for a common approach with the sharing of resources. This would have cost implications but may also have direct benefits to the NHS in terms of reduced consultations and demand for services. Developing all these components into a combined ‘Function First’ intervention, which addresses the CMOs is more likely to be acceptable in practices that are already committed to increasing physical activity in their populations. However, partial adoption of these components would enable some changes to be made in practices where physical activity promotion is less part of the practice culture.
Recommendations for research
The prototype multicomponent ‘Function First’ intervention is not yet ready to be implemented in primary care. In line with the Medical Research Council framework for complex interventions, a further research programme could be developed. 257 The first phase would develop and refine the intervention components. Several of the programme components have already been developed in other initiatives (e.g. Moving Healthcare Professionals Programme and Moving Medicine); however, other components, such as the physical activity advisor, need further development. The job description would need to be agreed across a range of stakeholders, using methods to gain a consensus. A range of potential professionals who could perform this role, including nurses, physiotherapists, occupational therapists, health psychologists, physician associates, exercise physiologists and behaviour change experts, would need to be discussed. Existing electronic diaries of local social prescribing opportunities would need to be adapted for use in this group. The different components could be combined into a single multicomponent intervention and then piloted in one or two general medical practices to obtain feedback about acceptability among patients and staff. This would also provide information about feasibility in busy NHS settings and alongside existing physical activity promotion schemes.
The second phase would involve a feasibility study to test trial methods in a group of practices. This would include recruitment and retention rates, acceptability of randomisation and outcome measurement. The feasibility study would help choose the most appropriate primary outcome, as well as advise on the objective measurement of physical activity and the testing of physical function.
This feasibility study would inform the methods and the sample size for a third-phase, definitive randomised controlled trial in a large sample of practices, of different types and locations throughout the UK, to assess effectiveness. The trial would include a concurrent economic evaluation to assess cost-effectiveness and a concurrent process evaluation to determine whether or not what was delivered in the trial was as intended in the programme theory.
Finally, further research would benefit from increased representation of different socioeconomic and ethnic groups.
Acknowledgements
We are extremely grateful to all who contributed and supported this study as stakeholders and participants through engagement in workshops, interviews and meetings across the life of the project.
We would also like to acknowledge the contribution and support of the Lab4Living research team at Sheffield Hallam University:
-
Chris Redford, who created the illustrations, storyboard and the graphics for the co-designed intervention resources, all of which were imperative to the progress and outcome of this project.
-
Rebecca Partridge, who was involved in developing and facilitating the overarching creative participatory processes, including the theory-building stage and the co-design stage.
-
Remi Bec, who developed and facilitated the games and participatory activities for the co-design and knowledge mobilisation workshops, and Gemma Wheeler, who also facilitated a co-design workshop.
We would like to thank the following members of the study external Project Advisory Group for their ongoing support, oversight and perspectives: Adrian Edwards (chairperson), Robert Van Deursen, Julie Richardson, Asan Akpan, Jeanette Thom, Malcolm Ward, Louise Williams, Freya Davies, Andrea Hughes and Alan D Pryce.
The authors would like to thank Philip Bell, who was a co-applicant and gave valuable insight from a public and patient perspective during the early stages of this project.
For support with research delivery, we would like to thank Health and Care Research Wales and the North West Coast Clinical Research Network.
From the North Wales Centre for Primary Care Research, School of Health Sciences at Bangor University, we would like to acknowledge and thank:
-
Annie Hendry and Matthew Jones for their help preparing the final report.
-
Natasha Hulley, Nicola Nikolic and Richard Evans for their ongoing administrative support throughout the project.
Finally, we are grateful to the anonymous reviewers whose critical reading and constructive comments have helped to strengthen and clarify this report.
Ethics approval
Ethics approval was received from the Healthcare and Medical Sciences Academic Ethics Committee (reference 2018–16308) and from the NHS Wales Research Ethics Committee 5 (references 256729 and 262726).
Contributions of authors
Rebecca-Jane Law (https://orcid.org/0000-0002-1435-5086) (Co-chief Investigator, Research Officer) was principal author and original co-applicant, overall study lead and researcher, responsible for drafting and revising content critically for important intellectual content, led the collection and interpretation of data, and provided final approval of the version to be published.
Joseph Langley (https://orcid.org/0000-0002-9770-8720) (Co-investigator, Senior Research Fellow in Healthcare Innovation) was an original co-applicant and responsible for the co-design elements of the study (Chapters 2 and 3, in particular), provided substantial contribution to the collection and interpretation of data, was responsible for drafting and revising content critically for important intellectual content, and provided final approval of the version to be published.
Beth Hall (https://orcid.org/0000-0003-4980-3720) (Co-investigator, Academic Support Librarian) was an original co-applicant and conducted systematic and purposive literature searches, gave methodological advice on evidence synthesis, provided substantial contribution to the collection and interpretation of data, was responsible for drafting and revising content critically for important intellectual content (Chapter 2, in particular), and provided final approval of the version to be published.
Christopher Burton (https://orcid.org/0000-0003-1159-1494) (Co-investigator, Professor of Health Services Research) was an original co-applicant and gave advice on realist methods, implementation and rehabilitation, provided substantial contribution to the interpretation of data, was responsible for drafting and revising content critically for important intellectual content (Chapter 3, in particular), and provided final approval of the version to be published.
Julia Hiscock (https://orcid.org/0000-0002-8963-2981) (Co-investigator, Research Fellow and Medical Sociologist) was an original co-applicant and gave a sociological perspective and advice on qualitative methods, provided substantial contribution to the collection and interpretation of data, was responsible for drafting and revising content critically for important intellectual content, and provided final approval of the version to be published.
Lynne Williams (https://orcid.org/0000-0003-2575-9710) (Co-investigator, Reader) was an original co-applicant and gave a nursing perspective and advice on realist methods, contributed to the interpretation of data, was responsible for drafting and revising content critically for important intellectual content, and provided final approval of the version to be published.
Val Morrison (https://orcid.org/0000-0002-4308-8976) (Co-investigator, Professor of Psychology) was an original co-applicant, provided advice from a health psychology perspective on physical activity for people with long-term conditions, contributed to the collection and interpretation of data, was responsible for drafting and revising content critically for important intellectual content, and provided final approval of the version to be published.
Andrew B Lemmey (https://orcid.org/0000-0003-1667-4539) (Co-investigator, Professor of Clinical Exercise Physiology) was an original co-applicant, provided advice on physical activity for people with long-term conditions, contributed to the collection and interpretation of data, was responsible for drafting and revising content critically for important intellectual content, and provided final approval of the version to be published.
Candida Lovell-Smith (Co-investigator, public research partner) was an original co-applicant, provided advice from a public perspective on physical activity for people with long-term conditions, contributed to the development of public-facing materials and the collection and interpretation of data, helped draft and revise content critically for important intellectual content, and provided final approval of the version to be published.
John Gallanders (Co-investigator, public research partner) advised from a public perspective on physical activity for people with long-term conditions, contributed substantially to analysis workshops and the collection and interpretation of data, was responsible for drafting and revising content critically for important intellectual content, and provided final approval of the version to be published.
Jennifer Cooney (https://orcid.org/0000-0002-9828-8000) (Lecturer in Sports Physiology) advised from a sports physiology perspective, contributed substantially to the collection and interpretation of data, was responsible for drafting and revising content critically for important intellectual content, and provided final approval of the version to be published.
Nefyn H Williams (https://orcid.org/0000-0002-8078-409X) (Co-Chief Investigator, Professor in Primary Care) advised from a general practice perspective, provided support for the new Co-chief Investigator, contributed substantially to the collection and interpretation of data, was responsible for drafting and revising content critically for important intellectual content, and provided final approval of the version to be published.
Publications
Law RJ, Williams L, Langley J, Burton C, Hall B, Hiscock J, et al. ‘Function First-Be Active, Stay Independent’ – promoting physical activity and physical function in people with long-term conditions by primary care: a protocol for a realist synthesis with embedded co-production and co-design. BMJ Open 2020;10:e035686.
Law RJ, Langley J, Hall B, Burton C, Hiscock J, Williams L, et al. ‘Function First’: how to promote physical activity and physical function in people with long-term conditions managed in primary care? A study combining realist and co-design methods. BMJ Open 2021;11:e046751.
Data-sharing statement
This is an evidence synthesis involving qualitative data collection and, therefore, the data generated is not suitable for sharing beyond that contained within the report. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Law RJ, Williams L, Langley J, Burton C, Hall B, Hiscock J, et al. ‘Function First—Be Active, Stay Independent’—promoting physical activity and physical function in people with long-term conditions by primary care: a protocol for a realist synthesis with embedded co-production and co-design. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-035686.
- Law RJ, Langley J, Hall B, Burton C, Hiscock J, Williams L, et al. ‘Function First’: how to promote physical activity and physical function in people with long-term conditions managed in primary care? A study combining realist and co-design methods. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-046751.
- Office for National Statistics . Nearly One in Five People Had Some Form of Disability in England and Wales 2015. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/disability/articles/nearlnearlyoneinfivepeoplehadsomeformofdisabilityinenglandand/2015-07-13 (accessed 19 July 2020).
- Department of Health and Social Care . Long Term Conditions Compendium of Information: Third Edition 2012. www.gov.uk/government/publications/long-term-conditions-compendium-of-information-third-edition (accessed 5 April 2020).
- NHS Digital . Health Survey for England, 2016 2017. https://digital.nhs.uk/catalogue/PUB30169 (accessed 5 April 2020).
- World Health Organization . World Report on Disability 2011. www.who.int/teams/noncommunicable-diseases/sensory-functions-disability-and-rehabilitation/world-report-on-disability (accessed 21 May 2021).
- Royal College of General Practitioners . Health Select Committee Inquiry on Management of Long-Term Conditions 2013. www.rcgp.org.uk/policy/rcgp-policy-areas/long-term-conditions.aspx (accessed October 2019).
- Office for National Statistics . People With Long-Term Health Conditions, UK: January to December 2019 2020. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/adhocs/11478peoplewithlongtermhealthconditionsukjanuarytodecember2019 (accessed 14 July 2020).
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37-43. https://doi.org/10.1016/S0140-6736(12)60240-2.
- Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med 2011;27:1-15. https://doi.org/10.1016/j.cger.2010.08.009.
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146-56. https://doi.org/10.1093/gerona/56.3.m146.
- Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Biol Sci Med Sci 2000;55:M43-52. https://doi.org/10.1093/gerona/55.1.m43.
- Cooper R, Mishra GD, Kuh D. Physical activity across adulthood and physical performance in midlife: findings from a British birth cohort. Am J Prev Med 2011;41:376-84. https://doi.org/10.1016/j.amepre.2011.06.035.
- Greysen SR, Stijacic Cenzer I, Auerbach AD, Covinsky KE. Functional impairment and hospital readmission in Medicare seniors. JAMA Intern Med 2015;175:559-65. https://doi.org/10.1001/jamainternmed.2014.7756.
- Matzen LE, Jepsen DB, Ryg J, Masud T. Functional level at admission is a predictor of survival in older patients admitted to an acute geriatric unit. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-32.
- Ostir GV, Berges IM, Kuo YF, Goodwin JS, Fisher SR, Guralnik JM. Mobility activity and its value as a prognostic indicator of survival in hospitalized older adults. J Am Geriatr Soc 2013;61:551-7. https://doi.org/10.1111/jgs.12170.
- Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc 2011;59:266-73. https://doi.org/10.1111/j.1532-5415.2010.03276.x.
- Ryan A, Wallace E, O’Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes 2015;13. https://doi.org/10.1186/s12955-015-0355-9.
- Zubritsky C, Abbott KM, Hirschman KB, Bowles KH, Foust JB, Naylor MD. Health-related quality of life: expanding a conceptual framework to include older adults who receive long-term services and supports. Gerontologist 2013;53:205-10. https://doi.org/10.1093/geront/gns093.
- Fried TR, McGraw S, Agostini JV, Tinetti ME. Views of older persons with multiple morbidities on competing outcomes and clinical decision-making. J Am Geriatr Soc 2008;56:1839-44. https://doi.org/10.1111/j.1532-5415.2008.01923.x.
- Richardson J, Letts L, Chan D, Officer A, Wojkowski S, Oliver D, et al. Monitoring physical functioning as the sixth vital sign: evaluating patient and practice engagement in chronic illness care in a primary care setting – a quasi-experimental design. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-29.
- Bierman AS. Functional status: the sixth vital sign. J Gen Intern Med 2001;16:785-6. https://doi.org/10.1111/j.1525-1497.2001.10918.x.
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 1985;100:126-31.
- Naci H, Ioannidis JP. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ 2013;347. https://doi.org/10.1136/bmj.f5577.
- Blair SN, Wei M. Sedentary habits, health, and function in older women and men. Am J Health Promot 2000;15:1-8. https://doi.org/10.4278/0890-1171-15.1.1.
- Balboa-Castillo T, León-Muñoz LM, Graciani A, Rodríguez-Artalejo F, Guallar-Castillón P. Longitudinal association of physical activity and sedentary behavior during leisure time with health-related quality of life in community-dwelling older adults. Health Qual Life Outcomes 2011;9. https://doi.org/10.1186/1477-7525-9-47.
- Visser M, Pluijm SM, Stel VS, Bosscher RJ, Deeg DJ. Longitudinal Aging Study Amsterdam . Physical activity as a determinant of change in mobility performance: the Longitudinal Aging Study Amsterdam. J Am Geriatr Soc 2002;50:1774-81.
- van Oostrom SH, Picavet HS, de Bruin SR, Stirbu I, Korevaar JC, Schellevis FG, et al. Multimorbidity of chronic diseases and health care utilization in general practice. BMC Fam Pract 2014;15. https://doi.org/10.1186/1471-2296-15-61.
- Miller ME, Rejeski WJ, Reboussin BA, Ten Have TR, Ettinger WH. Physical activity, functional limitations, and disability in older adults. J Am Geriatr Soc 2000;48:1264-72. https://doi.org/10.1111/j.1532-5415.2000.tb02600.x.
- Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med 1999;48:445-69. https://doi.org/10.1016/S0277-9536(98)00370-0.
- Rantanen T, Guralnik JM, Sakari-Rantala R, Leveille S, Simonsick EM, Ling S, et al. Disability, physical activity, and muscle strength in older women: the Women’s Health and Aging Study. Arch Phys Med Rehabil 1999;80:130-5. https://doi.org/10.1016/S0003-9993(99)90109-0.
- Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of the scientific evidence. Am J Prev Med 2003;25:129-36. https://doi.org/10.1016/S0749-3797(03)00176-4.
- Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane Database Syst Rev 2011;11. https://doi.org/10.1002/14651858.CD004963.pub3.
- Kumar A, Delbaere K, Zijlstra GA, Carpenter H, Iliffe S, Masud T, et al. Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing 2016;45:345-52. https://doi.org/10.1093/ageing/afw036.
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9. https://doi.org/10.1002/14651858.CD007146.pub3.
- Feskanich D, Willett W, Colditz G. Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA 2002;288:2300-6. https://doi.org/10.1016/S0749-3797(03)00176-4.
- Rodriguez BL, Curb JD, Burchfiel CM, Abbott RD, Petrovitch H, Masaki K, et al. Physical activity and 23-year incidence of coronary heart disease morbidity and mortality among middle-aged men. The Honolulu Heart Program. Circulation 1994;89:2540-4. https://doi.org/10.1161/01.cir.89.6.2540.
- Hu FB, Sigal RJ, Rich-Edwards JW, Colditz GA, Solomon CG, Willett WC, et al. Walking compared with vigorous physical activity and risk of type 2 diabetes in women: a prospective study. JAMA 1999;282:1433-9. https://doi.org/10.1001/jama.282.15.1433.
- Shaw K, Gennat H, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev 2006;4. https://doi.org/10.1002/14651858.CD003817.pub3.
- Puts MTE, Toubasi S, Andrew MK, Ashe MC, Ploeg J, Atkinson E, et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: a scoping review of the literature and international policies. Age Ageing 2017;46:383-92. https://doi.org/10.1093/ageing/afw247.
- Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet 2011;378:1244-53. https://doi.org/10.1016/S0140-6736(11)60749-6.
- Park SH, Han KS, Kang CB. Effects of exercise programs on depressive symptoms, quality of life, and self-esteem in older people: a systematic review of randomized controlled trials. Appl Nurs Res 2014;27:219-26. https://doi.org/10.1016/j.apnr.2014.01.004.
- Zubala A, MacGillivray S, Frost H, Kroll T, Skelton DA, Gavine A, et al. Promotion of physical activity interventions for community dwelling older adults: a systematic review of reviews. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0180902.
- Windle G, Hughes D, Linck P, Russell I, Woods B. Is exercise effective in promoting mental well-being in older age? A systematic review. Aging Ment Health 2010;14:652-69. https://doi.org/10.1080/13607861003713232.
- Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev 2017;1. https://doi.org/10.1002/14651858.CD011279.pub2.
- Larun L, Brurberg KG, Odgaard-Jensen J, Price JR. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev 2015;2. https://doi.org/10.1002/14651858.CD003200.pub3.
- Fransen M, McConnell S, Hernandez-Molina G, Reichenbach S. Exercise for osteoarthritis of the hip. Cochrane Database Syst Rev 2014;4. https://doi.org/10.1002/14651858.CD007912.pub2.
- Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med 2015;49:1554-7. https://doi.org/10.1136/bjsports-2015-095424.
- Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC. Home versus center based physical activity programs in older adults. Cochrane Database Syst Rev 2005;1. https://doi.org/10.1002/14651858.CD004017.pub2.
- Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev 2011;10. https://doi.org/10.1002/14651858.CD003236.pub2.
- NHS Digital . Statistics on Obesity, Physical Activity and Diet, England, 2019 2019. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/statistics-on-obesity-physical-activity-and-diet-england-2019 (accessed 5 April 2020).
- NHS Information Centre . Health Survey for England 2008 2009. https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/health-survey-for-england-2008-physical-activity-and-fitness (accessed 5 April 2020).
- Cimarras-Otal C, Calderón-Larrañaga A, Poblador-Plou B, González-Rubio F, Gimeno-Feliu LA, Arjol-Serrano JL, et al. Association between physical activity, multimorbidity, self-rated health and functional limitation in the Spanish population. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-1170.
- Autenrieth CS, Kirchberger I, Heier M, Zimmermann AK, Peters A, Döring A, et al. Physical activity is inversely associated with multimorbidity in elderly men: results from the KORA-Age Augsburg Study. Prev Med 2013;57:17-9. https://doi.org/10.1016/j.ypmed.2013.02.014.
- Ding D, Lawson KD, Kolbe-Alexander TL, Finkelstein EA, Katzmarzyk PT, van Mechelen W, et al. Lancet Physical Activity Series 2 Executive Committee . The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet 2016;388:1311-24. https://doi.org/10.1016/S0140-6736(16)30383-X.
- Allender S, Foster C, Scarborough P, Rayner M. The burden of physical activity-related ill health in the UK. J Epidemiol Community Health 2007;61:344-8. https://doi.org/10.1136/jech.2006.050807.
- World Health Organization . World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020 2013. www.who.int/nmh/publications/ncd-action-plan/en/ (accessed 21 May 2021).
- Public Health England . PHE Launches One You: Living Healthily in Midlife Can Double Your Chances of Being Healthy at 70 and Beyond 2016. www.gov.uk/government/news/phe-launches-one-you (accessed June 2019).
- Health Improvement and Protection . Start Active, Stay Active: A Report on Physical Activity from the Four Home Countries’ Chief Medical Officers 2011. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/830943/withdrawn_dh_128210.pdf (accessed 21 May 2021).
- Welsh Government . Well-Being of Future Generations (Wales) Act 2015 n.d. www.futuregenerations.wales/about-us/future-generations-act/ (accessed 8 June 2021).
- NHS Digital . Quality and Outcomes Framework (QOF), Enhanced Services and Core Contract Extraction Specifications (Business Rules) 2016. http://content.digital.nhs.uk/qof (accessed 21 May 2021).
- Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Interventions for improving outcomes in patients with multi-morbidity in primary care and community settings. Cochrane Database Syst Rev 2012;4. https://doi.org/10.1002/14651858.CD006560.pub2.
- Coulter A, Entwistle VA, Eccles A, Ryan S, Shepperd S, Perera R. Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database Syst Rev 2015;3. https://doi.org/10.1002/14651858.CD010523.pub2.
- National Institute for Health and Care Excellence (NICE) . Physical Activity: Exercise Referral Schemes 2014.
- Murphy S, Moore G, Williams A, Moore L. An exploratory cluster randomised trial of a university halls of residence based social norms intervention in Wales, UK. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-186.
- Radenkovic D, Aswani R, Ahmad I, Kreindler J, Robinson R. Lifestyle medicine and physical activity knowledge of final year UK medical students. BMJ Open Sport Exerc Med 2019;5. https://doi.org/10.1136/bmjsem-2019-000518.
- Coombes JS, Law J, Lancashire B, Fassett RG. ‘Exercise is Medicine’: curbing the burden of chronic disease and physical inactivity. Asia Pac J Public Health 2015;27:NP600-5. https://doi.org/10.1177/1010539513481492.
- World Health Organization . ICD-10: International Statistical Classification of Diseases and Related Health Problems, Tenth Revision 2004.
- World Health Organization . International Classification of Functioning, Disability and Health 2001.
- Wagner EH. Chronic Disease Management: What Will It Take to Improve Care for Chronic Illness? Eff Clin Pract 1998;1:2-4.
- National Institute for Health and Care Excellence (NICE) . Multimorbidity: Clinical Assessment and Management. NICE Guideline [NG56] 2016. www.nice.org.uk/guidance/ng56 (accessed 21 May 2021).
- Sanchez A, Bully P, Martinez C, Grandes G. Effectiveness of physical activity promotion interventions in primary care: a review of reviews. Prev Med 2015;76:S56-67. https://doi.org/10.1016/j.ypmed.2014.09.012.
- Drennan VM, Halter M, Brearley S, Carneiro W, Gabe J, Gage H, et al. Investigating the contribution of physician assistants to primary care in England: a mixed-methods study. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02160.
- Tulloch H, Fortier M, Hogg W. Physical activity counselling in primary care: who has and who should be counselling?. Patient Educ Couns 2006;64:6-20. https://doi.org/10.1016/j.pec.2005.10.010.
- National Institute for Health and Care Excellence . Dementia, Disability and Frailty in Later Life – Mid-Life Approaches to Delay or Prevent Onset. NICE Guideline [NG16] 2015.
- Williams NH, Law RJ. Putting function first: redesigning the primary care management of long-term conditions. Br J Gen Pract 2018;68:388-9. https://doi.org/10.3399/bjgp18X698249.
- Hewitt G, Sims S, Harris R. The realist approach to evaluation research: an introduction. Int J Ther Rehab 2012;19:250-9. https://doi.org/10.12968/ijtr.2012.19.5.250.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 1997.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-33.
- Reis RS, Salvo D, Ogilvie D, Lambert EV, Goenka S, Brownson RC. Lancet Physical Activity Series 2 Executive Committee . Scaling up physical activity interventions worldwide: stepping up to larger and smarter approaches to get people moving. Lancet 2016;388:1337-48. https://doi.org/10.1016/S0140-6736(16)30728-0.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Rycroft-Malone J, Burton CR, Williams L, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04120.
- Williams NH, Roberts JL, Din NU, Charles JM, Totton N, Williams M, et al. Developing a multidisciplinary rehabilitation package following hip fracture and testing in a randomised feasibility study: Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR). Health Technol Assess 2017;21. https://doi.org/10.3310/hta21440.
- Law RJ, Nafees S, Hiscock J, Wynne C, Williams NH. A lifestyle management programme focused on exercise, diet and physiotherapy support for patients with hip or knee osteoarthritis and a body mass index over 35: a qualitative study. Musculoskeletal Care 2019;17:145-51. https://doi.org/10.1002/msc.1382.
- Tomey KM, Sowers MR. Assessment of physical functioning: a conceptual model encompassing environmental factors and individual compensation strategies. Phys Ther 2009;89:705-14. https://doi.org/10.2522/ptj.20080213.
- Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: WH Freeman; 1997.
- Deci EL, Ryan RM. Intrinsic Motivation and Self-Determination in Human Behaviour. New York, NY: Plenum Press; 1985.
- Eccles MP, Hrisos S, Francis J, Kaner EF, Dickinson HO, Beyer F, et al. Do self-reported intentions predict clinicians’ behaviour: a systematic review. Implement Sci 2006;1. https://doi.org/10.1186/1748-5908-1-28.
- Ajzen I, Fishbein MT. The prediction of behaviour from attitudinal and normative beliefs. J Exp Soc Psychol 1970;6:466-87. https://doi.org/10.1016/0022-1031(70)90057-0.
- Ajzen I. The theory of planned behaviour. Organ Behav Hum Decis Process 1991;50:79-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011;26:1479-98. https://doi.org/10.1080/08870446.2010.540664.
- Leventhal H, Nerenz DR, Steele DJ, Baum A, Taylor SE, Singer JE. Handbook of Psychology and Health: Social Psychological Aspects of Health, Volume 4. Hillsdale, NJ: Lawrence Erlbaum; 1984.
- Cameron LD, Leventhal H. The Self-regulation of Health and Illness Behaviour. New York, NY: Routledge; 2003.
- Foucalt M. On Governmentality. Ideol Conscious 1979;6:5-21.
- Bourdieu P. Outline of a Theory of Practice. Cambridge: Cambridge University Press; 1977.
- Orsega-Smith EM, Payne LL, Mowen AJ, Ho CH, Godbey GC. The role of social support and self-efficacy in shaping the leisure time physical activity of older adults. J Leis Res 2007;39:705-27. https://doi.org/10.1080/00222216.2007.11950129.
- Lindsay Smith G, Banting L, Eime R, O’Sullivan G, van Uffelen JGZ. The association between social support and physical activity in older adults: a systematic review. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966-017-0509-8.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Wilson KM, Brady TJ, Lesesne C. NCCDPHP Work Group on Translation . An organizing framework for translation in public health: the Knowledge to Action Framework. Prev Chronic Dis 2011;8.
- Easterby-Smith M. Disciplines of organizational learning: contributions and critiques. Hum Relat 1997;50:1085-113. https://doi.org/10.1177/001872679705000903.
- Dewing J, Manley K, McCormack B, Wilson V. International Practice Development in Nursing and Healthcare. Oxford: Blackwell Publishing; 2008.
- Spitters HP, Lau CJ, Sandu P, Quanjel M, Dulf D, Glümer C, et al. Unravelling networks in local public health policymaking in three European countries – a systems analysis. Health Res Policy Syst 2017;15. https://doi.org/10.1186/s12961-016-0168-2.
- Langley J, Partridge R, Ankeny U, Wheeler G, Carroll C, Durate Rosa. Developments in Design Research and Practice – Best Papers from 10th Senses and Sensibility 2019: Lost in (G)localization, Springer Series in Design and Innovation. 2021.
- Langley J, Wheeler G, Partridge R, Bec R, Wolstenholme D, Sproson L, et al. Design of Assistive Technology for Ageing Populations. Springer International Publishing; 2020.
- Wolstenholme D, Snellgrove-Clarke E, Langley J, Matheson L. How Lego Serious Play Supports Team Building through the Creative Coproduction n.d.
- Sheard L, Marsh C, Mills T, Peacock R, Langley J, Partridge R, et al. Using patient experience data to develop a patient experience toolkit to improve hospital care: a mixed-methods study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07360.
- Burton C, Rycroft-Malone J, Williams L, Davies S, McBride A, Hall B, et al. Managers’ use of nursing workforce planning and deployment technologies: protocol for a realist synthesis of implementation and impact. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-013645.
- McCormack B, Dewar B, Wright J, Harvey G, Ballantine K. A Realist Synthesis of Evidence Relating to Practice Development. Edinburgh: NHS Quality Improvement Scotland; 2006.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Pawson R. Evidence-Based Policy. A Realist Perspective. London: SAGE Publications Ltd; 2006.
- Westhorp G, Prins E, Kusters CSL, Hultink M, Guijt IM, Brouwers JHAM. Realist Evaluation: An Overview. Wageningen: Wageningen UR Centre for Development Innovation; 2011.
- Williams NH, Roberts JL, Din NU, Totton N, Charles JM, Hawkes CA, et al. Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR): a phase II randomised feasibility study of a multidisciplinary rehabilitation package following hip fracture. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012422.
- Locock L, Kirkpatrick S, Brading L, Sturmey G, Cornwell J, Churchill N, et al. Involving service users in the qualitative analysis of patient narratives to support healthcare quality improvement. Res Involv Engagem 2019;5. https://doi.org/10.1186/s40900-018-0133-z.
- NIHR INVOLVE . National Standards for Public Involvement 2019. www.invo.org.uk/posttypepublication/national-standards-for-public-involvement/ (accessed 21 May 2021).
- Health and Care Research Wales . Help With Research n.d. https://healthandcareresearchwales.org/public/help-research (accessed 8 June 2021).
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- Lamming L, Pears S, Mason D, Morton K, Bijker M, Sutton S, et al. VBI Programme Team . What do we know about brief interventions for physical activity that could be delivered in primary care consultations? A systematic review of reviews. Prev Med 2017;99:152-63. https://doi.org/10.1016/j.ypmed.2017.02.017.
- Goode AD, Reeves MM, Eakin EG. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am J Prev Med 2012;42:81-8. https://doi.org/10.1016/j.amepre.2011.08.025.
- World Health Organization . EHealth n.d. www.who.int/ehealth/about/en/ (accessed 8 June 2021).
- Muellmann S, Forberger S, Möllers T, Bröring E, Zeeb H, Pischke CR. Effectiveness of eHealth interventions for the promotion of physical activity in older adults: a systematic review. Prev Med 2018;108:93-110. https://doi.org/10.1016/j.ypmed.2017.12.026.
- Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, et al. A systematic review and economic evaluation of exercise referral schemes in primary care: a short report. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19600.
- Leenaars KE, Smit E, Wagemakers A, Molleman GR, Koelen MA. The role of the care sport connector in the Netherlands. Health Promot Int 2018;33:422-35. https://doi.org/10.1093/heapro/daw097.
- Ewald B, Stacey F, Johnson N, Plotnikoff RC, Holliday E, Brown W, et al. Physical activity coaching by Australian exercise physiologists is cost effective for patients referred from general practice. Aust N Z J Public Health 2018;42:12-5. https://doi.org/10.1111/1753-6405.12733.
- Williams SL, McSharry J, Taylor C, Dale J, Michie S, French DP. Translating a walking intervention for health professional delivery within primary care: a mixed-methods treatment fidelity assessment. Br J Health Psychol 2020;25:17-38. https://doi.org/10.1111/bjhp.12392.
- Bull F, Milton K, Boehler C. Evaluation of the Physical Activity Care Pathway London Feasibility Pilot–Final Technical Report 2008. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/192041/Evaluation_of_the_Physical_Activity_Care_Pathway_London_Feasibility_Pilot_-_Report.pdf (accessed 21 May 2021).
- Bull FC, Milton KE. A process evaluation of a ‘physical activity pathway’ in the primary care setting. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-463.
- Boehler CE, Milton KE, Bull FC, Fox-Rushby JA. The cost of changing physical activity behaviour: evidence from a ‘physical activity pathway’ in the primary care setting. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-370.
- Department of Health and Social Care . Resources for Commissioning Let’s Get Moving Interventions 2012. www.gov.uk/government/publications/let-s-get-moving-revised-commissioning-guidance (accessed 5 April 2020).
- Loughren EA, Baker C, Crone D. ‘Let’s Get Moving’ Physical Activity Care Pathway (Gloucestershire) Post-Programme Evaluation Report 2014. http://eprints.glos.ac.uk/2378/ (accessed 21 May 2021).
- Barrett EM, Hussey J, Darker CD. Feasibility of a physical activity pathway for Irish primary care physiotherapy services. Physiotherapy 2017;103:106-12. https://doi.org/10.1016/j.physio.2016.02.001.
- Royal College of General Practitioners . RCGP Active Practice Charter 2019. https://r1.dotdigital-pages.com/p/49LX-5IR/active-practice-charter (accessed 21 May 2021).
- Quirk H, Haake S. How can we get more people with long-term health conditions involved in parkrun? A qualitative study evaluating parkrun’s PROVE project. BMC Sports Sci Med Rehabil 2019;11. https://doi.org/10.1186/s13102-019-0136-6.
- Brannan M, Bernardotto M, Clarke N, Varney J. Moving healthcare professionals – a whole system approach to embed physical activity in clinical practice. BMC Med Educ 2019;19. https://doi.org/10.1186/s12909-019-1517-y.
- Moving Medicine . Moving Medicine 2018. https://movingmedicine.ac.uk/ (accessed 21 May 2021).
- Avery L, Charman SJ, Taylor L, Flynn D, Mosely K, Speight J, et al. Systematic development of a theory-informed multifaceted behavioural intervention to increase physical activity of adults with type 2 diabetes in routine primary care: Movement as Medicine for Type 2 Diabetes. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0459-6.
- We Are Undefeatable . We Are Undefeatable: About the Campaign 2019. https://weareundefeatable.co.uk/ (accessed 17 July 2020).
- Wheeler PC, Mitchell R, Ghaly M, Buxton K. Primary care knowledge and beliefs about physical activity and health: a survey of primary healthcare team members. BJGP Open 2017;1. https://doi.org/10.3399/bjgpopen17X100809.
- Bull FC, Schipper EC, Jamrozik K, Blanksby BA. Beliefs and behaviour of general practitioners regarding promotion of physical activity. Aust J Public Health 1995;19:300-4. https://doi.org/10.1111/j.1753-6405.1995.tb00448.x.
- Melillo KD, Houde SC, Williamson E, Futrell M. Perceptions of nurse practitioners regarding their role in physical activity and exercise prescription for older adults. Clin Excell Nurse Pract 2000;4:108-16.
- Forbes LJ, Marchand C, Doran T, Peckham S. The role of the Quality and Outcomes Framework in the care of long-term conditions: a systematic review. Br J Gen Pract 2017;67:e775-e784. https://doi.org/10.3399/bjgp17X693077.
- Arden K, Fatoye F, Yeowell G. Evaluation of a rolling rehabilitation programme for patients with non-specific low back pain in primary care: an observational cohort study. J Eval Clin Pract 2017;23:272-8. https://doi.org/10.1111/jep.12595.
- International Physical Literacy Association . Physical Literacy Can Be Described As the Motivation, Confidence, Physical Competence, Knowledge and Understanding to Value and Take Responsibility for Engagement in Physical Activities for Life 2017. www.physical-literacy.org.uk/ (accessed 21 May 2021).
- Stevenson K, Baker R. Investigating organisational culture in primary care. Qual Prim Care 2005;13:191-200.
- Jones GR, Stathokostas L, Young BW, Wister AV, Chau S, Clark P, et al. Development of a physical literacy model for older adults – a consensus process by the collaborative working group on physical literacy for older Canadians. BMC Geriatr 2018;18. https://doi.org/10.1186/s12877-017-0687-x.
- Lobelo F, Duperly J, Frank E. Physical activity habits of doctors and medical students influence their counselling practices. Br J Sports Med 2009;43:89-92. https://doi.org/10.1136/bjsm.2008.055426.
- Morishita Y, Numata A, Miki A, Okada M, Ishibashi K, Takemoto F, et al. Primary care physicians’ own exercise habits influence exercise counseling for patients with chronic kidney disease: a cross-sectional study. BMC Nephrol 2014;15. https://doi.org/10.1186/1471-2369-15-48.
- Royal College of General Practitioners . GP Practices Supported to Recommend Active Lifestyles to Patients and Staff With Launch of New UK-Wide Active Practice Charter 2019. www.rcgp.org.uk/about-us/news/2019/august/gp-practices-supported-to-recommend-active-lifestyles-to-patients-and-staff.aspx (accessed 21 May 2021).
- Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 2016;3. https://doi.org/10.1002/14651858.CD006560.pub3.
- National Institute for Health and Care Excellence (NICE) . Physical Activity: Brief Advice for Adults in Primary Care 2013.
- National Institute for Health and Care Excellence (NICE) . Making Every Contact Count: How NICE Resources Can Support Local Priorities n.d. https://stpsupport.nice.org.uk/mecc/index.html (accessed 21 May 2021).
- Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act 2008;5. https://doi.org/10.1186/1479-5868-5-56.
- Lion A, Vuillemin A, Thornton JS, Theisen D, Stranges S, Ward M. Physical activity promotion in primary care: a Utopian quest?. Health Promot Int 2019;34:877-86. https://doi.org/10.1093/heapro/day038.
- Chatterjee R, Chapman T, Brannan MG, Varney J. GPs’ knowledge, use, and confidence in national physical activity and health guidelines and tools: a questionnaire-based survey of general practice in England. Br J Gen Pract 2017;67:e668-e675. https://doi.org/10.3399/bjgp17X692513.
- Hinrichs T, Moschny A, Klaassen-Mielke R, Trampisch U, Thiem U, Platen P. General practitioner advice on physical activity: analyses in a cohort of older primary health care patients (getABI). BMC Fam Pract 2011;12. https://doi.org/10.1186/1471-2296-12-26.
- Short CE, Hayman M, Rebar AL, Gunn KM, De Cocker K, Duncan MJ, et al. Physical activity recommendations from general practitioners in Australia. Results from a national survey. Aust N Z J Public Health 2016;40:83-90. https://doi.org/10.1111/1753-6405.12455.
- Jorgensen TK, Nordentoft M, Krogh J. How do general practitioners in Denmark promote physical activity?. Scand J Prim Health Care 2012;30:141-6. https://doi.org/10.3109/02813432.2012.688710.
- Omura JD, Bellissimo MP, Watson KB, Loustalot F, Fulton JE, Carlson SA. Primary care providers’ physical activity counseling and referral practices and barriers for cardiovascular disease prevention. Prev Med 2018;108:115-22. https://doi.org/10.1016/j.ypmed.2017.12.030.
- Lindeman C, McCurdy A, Lamboglia CG, Wohlers B, Pham ANQ, Sivak A, et al. The extent to which family physicians record their patients’ exercise in medical records: a scoping review. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-034542.
- Pavey TG, Anokye N, Taylor AH, Trueman P, Moxham T, Fox KR, et al. The clinical effectiveness and cost-effectiveness of exercise referral schemes: a systematic review and economic evaluation. Health Technol Assess 2011;15. https://doi.org/10.3310/hta15440.
- Moore GF, Raisanen L, Moore L, Din NU, Murphy S. Mixed-method process evaluation of the welsh national exercise referral scheme. Health Educ 2013;113:476-501. https://doi.org/10.1108/HE-08-2012-0046.
- Din NU, Moore GF, Murphy S, Wilkinson C, Williams NH. Health professionals’ perspectives on exercise referral and physical activity promotion in primary care: findings from a process evaluation of the National Exercise Referral Scheme in Wales. Health Educ J 2015;74:743-57. https://doi.org/10.1177/0017896914559785.
- Wormald H, Ingle L. GP exercise referral schemes: improving the patient’s experience. Educ J 2004;63:362-73. https://doi.org/10.1177/001789690406300407.
- Leemrijse CJ, de Bakker DH, Ooms L, Veenhof C. Collaboration of general practitioners and exercise providers in promotion of physical activity a written survey among general practitioners. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0316-8.
- Wilcox S, Parra-Medina D, Felton GM, Poston MB, McClain A. Adoption and implementation of physical activity and dietary counseling by community health center providers and nurses. J Phys Act Health 2010;7:602-12. https://doi.org/10.1123/jpah.7.5.602.
- Croteau K, Schofield G, McLean G. Physical activity advice in the primary care setting: results of a population study in New Zealand. Aust N Z J Public Health 2006;30:262-7. https://doi.org/10.1111/j.1467-842x.2006.tb00868.x.
- Verwey R, van der Weegen S, Spreeuwenberg M, Tange H, van der Weijden T, de Witte L. Upgrading physical activity counselling in primary care in the Netherlands. Health Promot Int 2016;31:344-54. https://doi.org/10.1093/heapro/dau107.
- Verwey R, van der Weegen S, Spreeuwenberg M, Tange H, van der Weijden T, de Witte L. A pilot study of a tool to stimulate physical activity in patients with COPD or type 2 diabetes in primary care. J Telemed Telecare 2014;20:29-34. https://doi.org/10.1177/1357633X13519057.
- Verwey R, van der Weegen S, Spreeuwenberg M, Tange H, van der Weijden T, de Witte L. A monitoring and feedback tool embedded in a counselling protocol to increase physical activity of patients with COPD or type 2 diabetes in primary care: study protocol of a three-arm cluster randomised controlled trial. BMC Fam Pract 2014;15. https://doi.org/10.1186/1471-2296-15-93.
- Verwey R, van der Weegen S, Spreeuwenberg M, Tange H, van der Weijden T, de Witte L. Process evaluation of physical activity counselling with and without the use of mobile technology: a mixed methods study. Int J Nurs Stud 2016;53:3-16. https://doi.org/10.1016/j.ijnurstu.2015.10.008.
- Healey EL, Jinks C, Foster NE, Chew-Graham CA, Pincus T, Hartshorne L, et al. The feasibility and acceptability of a physical activity intervention for older people with chronic musculoskeletal pain: the iPOPP pilot trial protocol. Musculoskeletal Care 2018;16:118-32. https://doi.org/10.1002/msc.1222.
- van der Wulp I, de Leeuw JR, Gorter KJ, Rutten GE. Effectiveness of peer-led self-management coaching for patients recently diagnosed with type 2 diabetes mellitus in primary care: a randomized controlled trial. Diabet Med 2012;29:e390-7. https://doi.org/10.1111/j.1464-5491.2012.03629.x.
- Morgan GS, Haase AM, Campbell R, Ben-Shlomo Y. Physical ACtivity facilitation for Elders (PACE): study protocol for a randomised controlled trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0610-8.
- Shaw R, Gillies M, Barber J, MacIntyre K, Harkins C, Findlay IN, et al. Pre-exercise screening and health coaching in CHD secondary prevention: a qualitative study of the patient experience. Health Educ Res 2012;27:424-36. https://doi.org/10.1093/her/cys005.
- Vanroy J, Seghers J, Bogaerts A, Devloo K, De Cock S, Boen F. Short- and long-term effects of a need-supportive physical activity intervention among patients with type 2 diabetes mellitus: a randomized controlled pilot trial. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0174805.
- Rena Parish T. Examination of the Constructs of the Transtheoretical Model in Patients With Heart Failure: A Focus on Physical Activity Readiness 2006.
- Fife-Schaw C, de Lusignan S, Wainwright J, Sprake H, Laver S, Heald V, et al. Comparing exercise interventions to increase persistence with physical exercise and sporting activity among people with hypertension or high normal blood pressure: study protocol for a randomised controlled trial. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-336.
- McDonough SM, Tully MA, Boyd A, O’Connor SR, Kerr DP, O’Neill SM, et al. Pedometer-driven walking for chronic low back pain: a feasibility randomized controlled trial. Clin J Pain 2013;29:972-81. https://doi.org/10.1097/AJP.0b013e31827f9d81.
- Comer C, Redmond AC, Bird HA, Hensor EM, Conaghan PG. A home exercise programme is no more beneficial than advice and education for people with neurogenic claudication: results from a randomised controlled trial. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0072878.
- James EL, Ewald BD, Johnson NA, Stacey FG, Brown WJ, Holliday EG, et al. Referral for expert physical activity counseling: a pragmatic RCT. Am J Prev Med 2017;53:490-9. https://doi.org/10.1016/j.amepre.2017.06.016.
- Andryukhin A, Frolova E, Vaes B, Degryse J. The impact of a nurse-led care programme on events and physical and psychosocial parameters in patients with heart failure with preserved ejection fraction: a randomized clinical trial in primary care in Russia. Eur J Gen Pract 2010;16:205-14. https://doi.org/10.3109/13814788.2010.527938.
- Smith TO, Jimoh OF, Cross J, Allan L, Corbett A, Sadler E, et al. Social prescribing programmes to prevent or delay frailty in community-dwelling older adults. Geriatrics 2019;4. https://doi.org/10.3390/geriatrics4040065.
- Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013384.
- Husk K, Blockley K, Lovell R, Bethel A, Lang I, Byng R, et al. What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health Soc Care Community 2020;28:309-24. https://doi.org/10.1111/hsc.12839.
- Craike M, Britt H, Parker A, Harrison C. General practitioner referrals to exercise physiologists during routine practice: a prospective study. J Sci Med Sport 2019;22:478-83. https://doi.org/10.1016/j.jsams.2018.10.005.
- Grant RW, Schmittdiel JA, Neugebauer RS, Uratsu CS, Sternfeld B. Exercise as a vital sign: a quasi-experimental analysis of a health system intervention to collect patient-reported exercise levels. J Gen Intern Med 2014;29:341-8. https://doi.org/10.1007/s11606-013-2693-9.
- Eakin EG, Reeves MM, Lawler SP, Oldenburg B, Del Mar C, Wilkie K, et al. The Logan Healthy Living Program: a cluster randomized trial of a telephone-delivered physical activity and dietary behavior intervention for primary care patients with type 2 diabetes or hypertension from a socially disadvantaged community – rationale, design and recruitment. Contemp Clin Trials 2008;29:439-54. https://doi.org/10.1016/j.cct.2007.10.005.
- Pescheny JV, Pappas Y, Randhawa G. Facilitators and barriers of implementing and delivering social prescribing services: a systematic review. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-2893-4.
- Chaplin E, Hewitt S, Apps L, Edwards K, Brough C, Glab A, et al. The evaluation of an interactive web-based Pulmonary Rehabilitation programme: protocol for the WEB SPACE for COPD feasibility study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008055.
- Devi R, Powell J, Singh S. A web-based program improves physical activity outcomes in a primary care angina population: randomized controlled trial. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3340.
- Weinstock RS, Brooks G, Palmas W, Morin PC, Teresi JA, Eimicke JP, et al. Lessened decline in physical activity and impairment of older adults with diabetes with telemedicine and pedometer use: results from the IDEATel study. Age Ageing 2011;40:98-105. https://doi.org/10.1093/ageing/afq147.
- Allen KD, Bosworth HB, Brock DS, Chapman JG, Chatterjee R, Coffman CJ, et al. Patient and provider interventions for managing osteoarthritis in primary care: protocols for two randomized controlled trials. BMC Musculoskelet Disord 2012;13. https://doi.org/10.1186/1471-2474-13-60.
- Eakin E, Reeves M, Winkler E, Lawler S, Owen N. Maintenance of physical activity and dietary change following a telephone-delivered intervention. Health Psychol 2010;29:566-73. https://doi.org/10.1037/a0021359.
- Eakin EG, Reeves MM, Marshall AL, Dunstan DW, Graves N, Healy GN, et al. Living Well with Diabetes: a randomized controlled trial of a telephone-delivered intervention for maintenance of weight loss, physical activity and glycaemic control in adults with type 2 diabetes. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-452.
- Dejonghe LAL, Rudolf K, Becker J, Stassen G, Froboese I, Schaller A. Health coaching for promoting physical activity in low back pain patients: a secondary analysis on the usage and acceptance. BMC Sports Sci Med Rehabil 2020;12. https://doi.org/10.1186/s13102-019-0154-4.
- Hinrichs T, Moschny A, Brach M, Wilm S, Klaaßen-Mielke R, Trampisch M, et al. Effects of an exercise programme for chronically ill and mobility-restricted elderly with structured support by the general practitioner’s practice (HOMEfit) – study protocol of a randomised controlled trial. Trials 2011;12. https://doi.org/10.1186/1745-6215-12-263.
- Department of Health and Social Care . Physical Activity Guidelines: UK Chief Medical Officers’ Report 2019. www.gov.uk/government/publications/physical-activity-guidelines-uk-chief-medical-officers-report (accessed 21 May 2021).
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol 1992;47:1102-14. https://doi.org/10.1037//0003-066x.47.9.1102.
- Marcus BH, Simkin LR. The transtheoretical model: applications to exercise behavior. Med Sci Sports Exerc 1994;26:1400-4. https://doi.org/10.1249/00005768-199411000-00016.
- Van Sluijs EM, Van Poppel MN, Twisk JW, Brug J, Van Mechelen W. The positive effect on determinants of physical activity of a tailored, general practice-based physical activity intervention. Health Educ Res 2005;20:345-56. https://doi.org/10.1093/her/cyg129.
- van Sluijs EM, van Poppel MN, Twisk JW, Chin A, Paw MJ, Calfas KJ, et al. Effect of a tailored physical activity intervention delivered in general practice settings: results of a randomized controlled trial. Am J Public Health 2005;95:1825-31. https://doi.org/10.2105/AJPH.2004.044537.
- National Institute for Health and Care Excellence (NICE) . Behaviour Change: Individual Approaches 2014.
- Allen KD, Oddone EZ, Coffman CJ, Jeffreys AS, Bosworth HB, Chatterjee R, et al. Patient, provider, and combined interventions for managing osteoarthritis in primary care: a cluster randomized trial. Ann Intern Med 2017;166:401-11. https://doi.org/10.7326/M16-1245.
- McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The Diabetes Network Internet-Based Physical Activity Intervention: a randomized pilot study. Diabetes Care 2001;24:1382-34. https://doi.org/10.2337/diacare.24.8.1328.
- Royal College of General Practitioners (RCGP) . Parkrun UK Teams up With RCGP to ‘Prescribe’ Active Lifestyles to Patients and Practice Staff. 2018. www.rcgp.org.uk/about-us/news/2018/june/parkrun-uk-teams-up-with-rcgp-to-prescribe-active-lifestyles-to-patients-and-practice-staff.aspx (accessed 21 May 2021).
- Bird EL, Biddle MSY, Powell JE. General practice referral of ‘at risk’ populations to community leisure services: applying the RE-AIM framework to evaluate the impact of a community-based physical activity programme for inactive adults with long-term conditions. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-7701-5.
- Martín-Borràs C, Giné-Garriga M, Puig-Ribera A, Martín C, Solà M, Cuesta-Vargas AI. PPAF Group . A new model of exercise referral scheme in primary care: is the effect on adherence to physical activity sustainable in the long term? A 15-month randomised controlled trial. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-017211.
- Kosteli MC, Heneghan NR, Roskell C, Williams SE, Adab P, Dickens AP, et al. Barriers and enablers of physical activity engagement for patients with COPD in primary care. Int J Chron Obstruct Pulmon Dis 2017;12:1019-31. https://doi.org/10.2147/COPD.S119806.
- Chong TW, Doyle CJ, Cyarto EV, Cox KL, Ellis KA, Ames D, et al. AIBL Research Group . Physical activity program preferences and perspectives of older adults with and without cognitive impairment. Asia Pac Psychiatry 2014;6:179-90. https://doi.org/10.1111/appy.12015.
- Bjerk M, Brovold T, Skelton DA, Bergland A. A falls prevention programme to improve quality of life, physical function and falls efficacy in older people receiving home help services: study protocol for a randomised controlled trial. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2516-5.
- Bearne LM, Walsh NE, Jessep S, Hurley MV. Feasibility of an exercise-based rehabilitation programme for chronic hip pain. Musculoskeletal Care 2011;9:160-8. https://doi.org/10.1002/msc.209.
- Gamboa Moreno E, Sánchez Perez Á, Vrotsou K, Arbonies Ortiz JC, Del Campo Pena E, Ochoa de Retana Garcia L, et al. Impact of a self-care education programme on patients with type 2 diabetes in primary care in the Basque Country. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-521.
- Gamboa Moreno E, Ochoa de Retana Garcia L, Del Campo Pena ME, Sánchez Perez Á, Martinez Carazo C, Arbonies Ortiz JC, et al. A pilot study to assess the feasibility of the Spanish diabetes self-management program in the Basque Country. J Diabetes Res 2016;2016. https://doi.org/10.1155/2016/9145673.
- US Department of Health and Human Services . Physical Activity Guidelines for Americans 2018.
- Jones T, Darzi A, Egger G, Ickovics J, Noffsinger E, Ramdas K, et al. Process and systems: a systems approach to embedding group consultations in the NHS. Future Healthc J 2019;6:8-16. https://doi.org/10.7861/futurehosp.6-1-8.
- NHS Leading Change Adding Value Team . Introducing Group Consultations for Adults With Type 2 Diabetes 2019. www.england.nhs.uk/atlas_case_study/introducing-group-consultations-for-adults-with-type-2-diabetes/ (accessed 21 May 2021).
- Asenlöf P, Denison E, Lindberg P. Individually tailored treatment targeting activity, motor behavior, and cognition reduces pain-related disability: a randomized controlled trial in patients with musculoskeletal pain. J Pain 2005;6:588-603. https://doi.org/10.1016/j.jpain.2005.03.008.
- Asenlöf P, Denison E, Lindberg P. Long-term follow-up of tailored behavioural treatment and exercise based physical therapy in persistent musculoskeletal pain: a randomized controlled trial in primary care. Eur J Pain 2009;13:1080-8. https://doi.org/10.1016/j.ejpain.2009.01.010.
- Holden MA, Nicholls EE, Young J, Hay EM, Foster NE. Role of exercise for knee pain: what do older adults in the community think?. Arthrit Care Res 2012;64:1554-64. https://doi.org/10.1002/acr.21700.
- Leijon ME, Bendtsen P, Nilsen P, Ekberg K, Ståhle A. Physical activity referrals in Swedish primary health care – prescriber and patient characteristics, reasons for prescriptions, and prescribed activities. BMC Health Serv Res 2008;8. https://doi.org/10.1186/1472-6963-8-201.
- Lohmann H, Siersma V, Olivarius NF. Fitness consultations in routine care of patients with type 2 diabetes in general practice: an 18-month non-randomised intervention study. BMC Fam Pract 2010;11. https://doi.org/10.1186/1471-2296-11-83.
- Prochaska JJ, Zabinski MF, Calfas KJ, Sallis JF, Patrick K. PACE+: interactive communication technology for behavior change in clinical settings. Am J Prev Med 2000;19:127-31. https://doi.org/10.1016/S0749-3797(00)00187-2.
- Bossen D, Veenhof C, Van Beek KE, Spreeuwenberg PM, Dekker J, De Bakker DH. Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: randomized controlled trial. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2662.
- Rhodes RE, Baranova M, Christian H, Westgarth C. Increasing physical activity by four legs rather than two: systematic review of dog-facilitated physical activity interventions. Br J Sports Med 2020;54:1202-7. https://doi.org/10.1136/bjsports-2019-101156.
- Bjerre ED, Petersen TH, Jørgensen AB, Johansen C, Krustrup P, Langdahl B, et al. Community-based football in men with prostate cancer: 1-year follow-up on a pragmatic, multicentre randomised controlled trial. PLOS Med 2019;16. https://doi.org/10.1371/journal.pmed.1002936.
- Danielsson L, Kihlbom B, Rosberg S. ‘Crawling out of the cocoon’: patients’ experiences of a physical therapy exercise intervention in the treatment of major depression. Phys Ther 2016;96:1241-50. https://doi.org/10.2522/ptj.20150076.
- Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev 2018;4. https://doi.org/10.1002/14651858.CD010842.pub2.
- Forsyth A, Deane FP, Williams P. Dietitians and exercise physiologists in primary care: lifestyle interventions for patients with depression and/or anxiety. J Allied Health 2009;38:e63-8.
- Jansink R, Braspenning J, van der Weijden T, Elwyn G, Grol R. Primary care nurses struggle with lifestyle counseling in diabetes care: a qualitative analysis. BMC Fam Pract 2010;11. https://doi.org/10.1186/1471-2296-11-41.
- Barrett EM, Darker CD, Hussey J. Promotion of physical activity in primary care: knowledge and practice of general practitioners and physiotherapists. J Public Health 2013;21:63-9. https://doi.org/10.1007/s10389-012-0512-0.
- Rushforth B, McCrorie C, Glidewell L, Midgley E, Foy R. Barriers to effective management of type 2 diabetes in primary care: qualitative systematic review. Br J Gen Pract 2016;66:e114-27. https://doi.org/10.3399/bjgp16X683509.
- Sturgiss E, Haesler E, Elmitt N, Van Weel C, Douglas K. Increasing general practitioners’ confidence and self-efficacy in managing obesity: a mixed methods study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014314.
- Ward M. A Survey of Physical Activity in Medical Curricula: A Report of the HEPA in Health Care Settings 2015. https://ihcc.publichealthnetwork.cymru/files/6214/8527/7823/Final_Report_Jan_2016.pdf (accessed 21 May 2021).
- Dacey ML, Kennedy MA, Polak R, Phillips EM. Physical activity counseling in medical school education: a systematic review. Med Educ Online 2014;19. https://doi.org/10.3402/meo.v19.24325.
- Dunlop M, Murray AD. Major limitations in knowledge of physical activity guidelines among UK medical students revealed: implications for the undergraduate medical curriculum. Br J Sports Med 2013;47:718-20. https://doi.org/10.1136/bjsports-2012-091891.
- Weiler R, Chew S, Coombs N, Hamer M, Stamatakis E. Physical activity education in the undergraduate curricula of all UK medical schools. Are tomorrow’s doctors equipped to follow clinical guidelines?. Br J Sport Med 2012;46:1024-6. https://doi.org/10.1136/bjsports-2012-091380.
- Walsh JME, Swangard DM, Davis T, McPhee SJ. Exercise counseling by primary care physicians in the era of managed care. Am J Prev Med 1999;16:307-13. https://doi.org/10.1016/S0749-3797(99)00021-5.
- Savill B, Murray A, Weiler R. Is general practice engaged with physical activity promotion?. Br J Gen Pract 2015;65:484-5. https://doi.org/10.3399/bjgp15X686677.
- Schofield G, Croteau K, McLean G. Trust levels of physical activity information sources: a population study. Health Promot J Austr 2005;16:221-4. https://doi.org/10.1071/he05221.
- Stone RC, Baker J. Painful choices: a qualitative exploration of facilitators and barriers to active lifestyles among adults with osteoarthritis. J Appl Gerontol 2017;36:1091-116. https://doi.org/10.1177/0733464815602114.
- Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol 2001;52:1-26. https://doi.org/10.1146/annurev.psych.52.1.1.
- Hinrichs T, Bücker B, Klaaßen-Mielke R, Brach M, Wilm S, Platen P, et al. Home-based exercise supported by general practitioner practices: ineffective in a sample of chronically ill, mobility-limited older adults (the HOMEfit randomized controlled trial). J Am Geriatr Soc 2016;64:2270-9. https://doi.org/10.1111/jgs.14392.
- Persson G, Brorsson A, Ekvall Hansson E, Troein M, Strandberg EL. Physical activity on prescription (PAP) from the general practitioner’s perspective – a qualitative study. BMC Fam Pract 2013;14. https://doi.org/10.1186/1471-2296-14-128.
- Copeland R, Myers A, Quirk H, Crank H, Broom D, Goldsmith S. Evaluation of the Public Health England and Sport England Funded Physical Activity Clinical Advice Pad Pilot. Sheffield: National Centre for Sport and Exercise Medicine; 2019.
- Marchal B, Van Belle S, Van Olmen J, Hoerée T, Kegels G. Is realist evaluation keeping its promise? A review of published empirical studies in the field of health systems research. Evaluation 2012;18:192-21. https://doi.org/10.1177/1356389012442444.
- Public Health England . Health Matters: Physical Activity – Prevention and Management of Long-Term Conditions 2020. www.gov.uk/government/publications/health-matters-physical-activity/health-matters-physical-activity-prevention-and-management-of-long-term-conditions#physical-activity-initiatives-and-training-for-healthcare-professionals (accessed 21 May 2021).
- Blane DN, Macdonald S, O’Donnell CA. What works and why in the identification and referral of adults with comorbid obesity in primary care: a realist review. Obes Rev 2020;21. https://doi.org/10.1111/obr.12979.
- Carr SM, Lhussier M, Forster N, Geddes L, Deane K, Pennington M, et al. An evidence synthesis of qualitative and quantitative research on component intervention techniques, effectiveness, cost-effectiveness, equity and acceptability of different versions of health-related lifestyle advisor role in improving health. Health Technol Assess 2011;15. https://doi.org/10.3310/hta15090.
- Grinvalds N, Shearn K, Copeland RJ, Speake H. What works to facilitate the promotion of physical activity in co-located healthcare and leisure settings: a realist review. SportRxiv 2019. https://doi.org/10.31236/osf.io/h9r8w.
- Move More . Move More Challenge: We Are World Record Breakers 2019. www.movemoresheffield.com/#workplacechallenge (accessed 13 March 2020).
- Roberts JL, Din NU, Williams M, Hawkes CA, Charles JM, Hoare Z, et al. Development of an evidence-based complex intervention for community rehabilitation of patients with hip fracture using realist review, survey and focus groups. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014362.
- McKay H, Nettlefold L, Bauman A, Hoy C, Gray SM, Lau E, et al. Implementation of a co-designed physical activity program for older adults: positive impact when delivered at scale. BMC Public Health 2018;18. https://doi.org/10.1186/s12889-018-6210-2.
- Robert GB, Macdonald A, Sangiorgi D, Prendiville A. Designing for Service: Key Issues and New Directions. London: Bloomsbury Academic; 2017.
- Mukumbang FC, Marchal B, Van Belle S, van Wyk B. Using the realist interview approach to maintain theoretical awareness in realist studies. Qual Res 2019;20:485-51. https://doi.org/10.1177/1468794119881985.
- Jagosh J. Retroductive theorizing in Pawson and Tilley’s applied scientific realism. J Crit Realism 2020;19:121-30. https://doi.org/10.1080/14767430.2020.1723301.
- Keller C, Gare K, Edenius M, Lindblad S. Innovations in health care: design theory and realist evaluation combined. Innovations 2009;11. https://doi.org/10.1145/1555619.1555623.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
List of abbreviations
- ADL
- activity of daily living
- CMO
- context, mechanism and outcome
- GP
- general practitioner
- GRIPP2
- Guidance for Reporting Involvement of Patients and the Public 2
- LGM
- Let’s Get Moving
- NICE
- National Institute for Health and Care Excellence
- PACE
- Physician-based Assessment and Counselling for Exercise
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Notes
-
Stakeholder contribution to the theory-building workshops and telephone interviews, and cumulative contribution of individual stakeholders to the co-design and knowledge mobilisation workshops
-
Example extracts from analysis of the data from the theory-building workshops
-
Guidance for Reporting Involvement of Patients and the Public (GRIPP) 2 checklist
-
Design presentation file for the intervention; a document that could be used as part of a non-academic dissemination strategy for further development, and potential future use
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr09160).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
