Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/156/10. The contractual start date was in October 2015. The final report began editorial review in February 2020 and was accepted for publication in May 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2021 Cornes et al. This work was produced by Cornes et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Cornes et al.
Chapter 1 Introduction
Background
This realist evaluation was commissioned in response to a call from the National Institute for Health Research (NIHR) Health Services and Delivery Research programme (reference 13/156/10). The call sought to provide evidence for commissioners and service leaders on ‘what works best’ with regard to the appropriateness, quality and cost-effectiveness of specialist integrated homeless health and care (SIHHC). Two studies were commissioned: one study,1 which explored specialist primary care services, and this present study, which explores hospital discharge. The call was made in response to an announcement in September 2013 that £10M funding was to be made available by the Department of Health [now the Department of Health and Social Care (DHSC)] to develop specialist homeless hospital discharge schemes (HHDSs), including ‘step-down’ intermediate care. Fifty-two schemes were funded across England as part of the Homeless Hospital Discharge Fund (HHDF). This evaluation of these and other specialist homeless hospital discharge arrangements commenced in September 2015 and was completed in December 2019. It was carried out by a consortium of researchers from different universities, led by King’s College London (London, UK). The reporting of this research adheres to the Realist And Meta-narrative Evidence Syntheses: Evolving Standards II (RAMESES II) for realist evaluation. 2,3 Ethics approval was obtained from the London and South East Research Ethics Committee in April 2016 (reference 16/EE/0018)
Research objectives
The overall aim of the study was to explore how SIHHC works, for whom, in what circumstances and why to deliver consistently safe, timely transfers of care. The study objectives were to:
-
situate what is already known about delayed transfers of care (DToCs) among people who are homeless in terms of the broader literature on hospital discharge and intermediate care
-
explore how different models of SIHHC are being developed and implemented across England to facilitate effective hospital discharge
-
explore the views and experiences of people who are homeless and if and, if so, how SIHHC works to improve experiences of hospital discharge and deliver improved health and well-being outcomes
-
explore how SIHHC has an impact on outcomes and different patterns of service use across the whole system (e.g. the use of unplanned care) and the associated cost implications of this
-
produce a ‘toolkit’ for commissioners on developing SIHHC if the findings support this.
Report structure
In the remainder of this chapter, we outline the broader policy context in which the HHDF was operationalised. This includes background information about homelessness in England, the impact of austerity on public services, including the NHS, and the development of intermediate care services as a means of maintaining ‘patient flow’ in the face of rising demand for acute care.
In Chapter 2, we outline why we used a realist evaluation approach and how we applied realist principles of generative causation to the evaluation of specialist homeless hospital discharge arrangements. First, we describe the findings of a realist synthesis of the literature that situates what is already known about DToCs among people who are homeless in terms of the broader literature on hospital discharge and intermediate care (objective 1). We then show how this evidence was used to inform the development of our initial (tentative) programme theories about what works to deliver consistently safe, timely transfers of care.
The results section comprises three chapters, each of which outline the findings of a separate work package (WP) designed to interogate programme theory. We consider the data collection methods used in each WP at the beginning of each chapter.
Chapter 3 reports the findings of WP1. This WP comprised qualitative observational case studies of seven study sites in England. This involved (non-participant) observation of discharge practices in sites with ‘specialist care’ (n = 5) and comparing these with sites with ‘standard care’ (n = 2), interviews with service users (n = 70) at baseline and the 3-month follow-up, and interviews with a wide range of stakeholders (n = 77). The overall purpose of this chapter is to explore how specialist care is being implemented and perceptions of the barriers to and facilitators of successful implementation from the perspective of a range of stakeholders, including service users (objectives 2 and 3).
Chapter 4 reports the findings of WP2. This comprised a ‘data linkage’, tracking outcomes for 3882 homeless patients by means of Hospital Episode Statistics (HES) and civil registration death data. WP3 provides quantitative evidence to enable the interrogation of our programme theories (e.g. that schemes with ‘step down’ will be more effective) by reporting a range of outcomes, such as hospital readmission rates and time from discharge to next accident and emergency (A&E) attendance. Chapters 4 and 5 address research objective 4.
Chapter 5 reports the findings of WP3. This is an economic evaluation that explores the effectiveness and cost-effectives of specialist compared with standard hospital discharge arrangements, and also the effectiveness and cost-effectiveness of different typologies of HHDS. WP3 also generates evidence that can be used to interrogate our programme theories (e.g. that schemes offering ‘step down’ will be more cost-effective than schemes that do not offer this).
In Chapter 6 we triangulate the evidence generated across the three individual WPs to further interrogate and refine our programme theories. We present the overall findings of this realist evaluation as an evidence-informed ‘checklist’ of the complex set of factors that decision-makers will need to consider to ensure consistently safe, timely transfers of care for people who are homeless (objective 5).
Definition of homelessness
Homelessness is a complex phenomenon that covers a wide range of circumstances. According to the Homeless Monitor,4 it encompasses people sleeping rough; single homeless people living in hostels, shelters and temporary supported accommodation; statutorily homeless households that are seeking housing assistance from local authorities on grounds of being currently or imminently without accommodation; and the hidden homeless (e.g. ‘sofa surfing’ in the homes of friends and relatives).
The primary focus of this study is on ‘multiple exclusion homelessness’ (MEH). This term is used to capture the overlap between homelessness and other domains of deep social exclusion, such as ‘institutional care’ (e.g. prison, local authority care, stays in mental health hospitals or wards), ‘substance misuse’ (e.g. drug problems, alcohol problems, abuse of solvents, glue or gas) and participation in street culture activities (e.g. begging, street drinking, ‘survival’ shoplifting or sex work). 5
We decided to focus on MEH because it was anticipated that people falling within this group may be more likely to be admitted to hospital and to have more complex discharge experiences. The excess morbidity and mortality associated with MEH and other forms of deep social exclusion are extreme. Aldridge et al. 6 studied four inclusion health populations (homeless populations, individuals with substance use disorders, sex workers and imprisoned individuals) and found all-cause mortality standard mortality ratios (SMRs) of 7.9 in male individuals and 11.9 in female individuals compared with those living in the least deprived areas of England and Wales.
National policy context
This study took place against the backdrop of the Coalition and Conservative governments’ policies of austerity that were implemented following the global financial crises of 2007/8, leading to heavy cuts to welfare services and benefits, an NHS funding freeze and extensive cuts to local government budgets. 7 From 2010, there were significant rises in the levels of homelessness in England, particularly rough sleeping. By the time this study was reporting in 2020, the situation has been characterised as a ‘national crisis’8 and a ‘public health disaster’. 9
In October 2018, the Homeless Reduction Act 2017 (HRA)10 came into force in England and widened access to assistance from housing authorities to all households at risk of homelessness (not just those in priority need). The Act also introduced a ‘duty to refer’, in which specified public services (including NHS trusts) now have a legal duty to refer patients they consider may be homeless or threatened with homelessness to a local housing authority. In August 2018, the HRA was complemented by a new rough sleeping strategy. 11 This strategy aims to end rough sleeping by 2027, focusing on three ‘core pillars’ of prevention, intervention and recovery. Both of these measures were implemented outside the data collection time frame of the study; however, we will return to discuss them later in the light of the study findings.
Poor hospital discharge arrangements
The research literature on hospital discharge goes back at least 50 years and there is remarkable consistency in its findings, which continue to report the frequent breakdown of routine discharge arrangements. 12 In a comprehensive review of the policy and research landscape, highlighting the often-neglected housing dimensions of hospital discharge, Glasby13 describes feeling left with an overwhelming sense of the intractable and persistent nature of many of the problems.
Older people and people with multiple and complex needs (e.g. long-term conditions), including people who are homeless, are particularly affected by poor discharge. 14 In 2012, the DHSC commissioned a report on how homeless patients were being treated in hospital. 15 This identified ‘countless examples’ of the mention of homelessness on admission, triggering prejudice among hospital staff. The report highlighted that premature and unsafe discharge tended to be more of a problem for homeless patients than delayed discharge. The review reported that > 70% of homeless patients were being discharged back onto the streets without having their care and support need assessed, further damaging their health and all but guaranteeing their readmission. According to the then Secretary of State, Paul Burstow, ‘We commissioned the report to expose poor practice . . . What it reveals is too many hospitals simply discharging homeless people back to the streets. Patching a person up and sending them out without a plan makes no sense’16 (contains public sector information licensed under the Open Government Licence v1.0).
Other concerns highlighted in the report included hospital staff not asking people about their housing situation on admission; failure to manage drug and alcohol withdrawal, leading to early self-discharge; hospital staff not alerting accommodation providers to the fact that a person is in hospital, leading to tenancies being terminated; hospital staff having a poor understanding of the services available to homeless people, including overestimating the level of care that can be provided in hostel settings, leading to unsafe discharges; a lack of practical support, such as no replacement of soiled clothing; uncertainty regarding where the involvement of one sector should start and end, including little agreement about how far hospital staff should be expected to proactively seek accommodation; and a lack of appropriate accommodation options, raising the question of whether of not ‘signposting’ is an adequate response if this potentially leads to discharge back onto the streets.
The Homeless Hospital Discharge Fund
In 2013, the DHSC announced that £10M funding would be made available to the voluntary and community sector to work with the NHS and local councils to develop specialist hospital discharge arrangements and intermediate care services for people who are homeless:
All too often, the homeless end up in a hostel that is an inappropriate environment for treatment plans and for their recovery. For those who are TB [tuberculosis] patients, homelessness is a major barrier to completing their treatment and recovery from infection. [The HHDF funding] will ensure adequate provision of intermediate care facilities to be available upon discharge from hospital.
DHSC. 17
What is intermediate care?
In the literature on hospital discharge, it has long been recognised that there is tension between two competing notions of ‘good practice’. On the one hand, a perspective that is narrowly concerned with the most cost-effective use of hospital resources (and hence rapid throughput). On the other hand, a perspective that emphasises the importance of needs-led assessments and choice for individuals. 13 Increasingly, intermediate care and discharge to assess (D2A) are being promoted as ways of addressing the need to ensure both ‘patient flow’ and safe discharge practice.
Intermediate or ‘step-up’ and ‘step-down’ care is an umbrella term for a wide range of admission avoidance and out-of-hospital care services, including Rapid Response, Crises Response, D2A, Home First, Reablement and Safely Home. It usually comprises:
Networks of local health, housing and social care services, which deliver targeted, short-term support to individual patients, in order to: prevent inappropriate admission to NHS acute inpatient or continuing care, or long-term residential care; facilitate timely discharge from hospital; and, most importantly, maximise people’s ability to live independently.
Cowpe18
Bolton19 summarises the thinking behind out-of-hospital care services as follows. First, there should be less focus on assessment for longer-term care and support at the point of discharge and more emphasis on recovery. Second, there is a specifically commissioned set of services to help people recover post hospital. He suggests that intermediate care will not work at its best if services are solely commissioned from existing services where they were not established for that purpose (e.g. using standard home care agencies that are not geared up to take a regular flow of new people).
Guidance is clear that ‘step-down’ care should not be used to warehouse people. That is, creating an additional transfer in a person’s care pathway to free up a hospital bed without adding value to their experience of care or meeting good outcomes for the person. 20
The National Institute for Health and Care Excellence (NICE)21 guideline for intermediate care recommends that commissioners should consider making home-based intermediate care, reablement, bed-based intermediate care and crises response all available locally. These services need to be delivered in an integrated way so that people can move seamlessly between them, depending on their changing needs.
Eligibility for intermediate care
Intermediate care entered the mainstream of health and care services delivery in England through the National Service Framework for Older People. 22 Here, it was recognised that although intermediate care services are likely to be of particular importance for older people, service planning and investment need to take account of the needs of all potential services users. Updated guidance23 defined intermediate care as support for anyone with a health-related need through periods of transition and made the point that no-one should be excluded on the basis of age or ethnic or cultural group. Specific reference was made in this guidance to the eligibility of homeless people and prisoners. 23 However, later guidance has tended to move away from this broader, more inclusive definition. One reason for this may be that investment in intermediate care services (particularly reablement) has not kept pace with rising demand. 24
Housing-led intermediate care
The £10M investment that underpinned the HHDF was restricted to voluntary and community sector providers. This targeting led to the development of a new tier of specialist ‘housing-led’ intermediate care services (i.e. services that are designed and delivered mainly by housing associations and homeless charities/voluntary sector organisations). Until this point, intermediate care had been delivered mainly as a health and social care service. 25 In total, 52 schemes were funded through the HHDF. Two principal models emerged:
-
a housing-led [Home First (floating support)] ‘step-down’ model (n = 37)
-
a housing-led (residential/bed-based) ‘step-down’ model (n = 7).
In the Home First ‘step-down’ model, HHDSs provide access to a ‘link worker’. Link workers aim to support the patient to find accommodation (i.e. somewhere safe to stay). They will also assist with other aspects of discharge planning using their knowledge of local homeless services and resources. Once the patient has been discharged from hospital, the link worker will stay in touch, providing (floating) ‘step-down’ support in the community for a time-limited period until longer-term care and support are in place.
In addition to Home First (floating support) schemes, HHDF capital funding was used to develop a number of residential (bed-based) intermediate care facilities. Two of the largest HHDF capital grants (totalling in excess of £1M) were allocated to charities to establish medical respite centres with 24-hour clinical staffing. The first HHDS failed to become operational because of difficulties finding a building. The second HHDS failed to secure revenue funding for clinical staffing once the refurbishments were complete and hence did not became operational. Five smaller residential ‘step-down’ (without 24-hour clinical staffing) schemes did become operational, but only one of these (a housing association-led scheme) is currently operational.
Clinically led teams
In addition to the ‘housing-led’ schemes, we consider, as part of this evaluation, a number of ‘clinically led’ schemes (some of which predate/or were not funded by the HHDF). These are often called Pathway Homeless Teams by virtue of their affiliation with the Pathway Charity [URL: www.pathway.org.uk (accessed 3 June 2021)]. The Pathway model is a multidisciplinary team (MDT) approach that employs general practitioners (GPs), nurses, housing workers, social workers, occupational therapists and peers (i.e. people with lived experience of homelessness). The Pathway homeless teams are usually led by the GP or senior nurse and focus on individual care co-ordination (including discharge planning). As the primary aim of the clinically led team is to maximise the window of opportunity afforded through a hospital stay, these schemes usually close cases at the point at which the patient leaves hospital (i.e. they do not routinely integrate ‘step-down’ care as part of the service model).
Summary
In this section, we have introduced the background to HHDF programme and some of the problems that it set out to address, namely ‘discharge to the street’ and a lack of appropriate ‘step-down’ intermediate care facilities for recuperation and recovery. We have also introduced the wider policy context in which the HHDF was implemented, charting the impact of austerity, including increased rates of homelessness; severe shortages of housing, care and support; and a consequent rising demand for acute hospital services and intermediate care. We now turn our attention to the evaluation of specialist HHDSs and their role in delivering consistently safe, timely transfers of care.
Chapter 2 Realist evaluation and literature synthesis: constructing an initial tentative programme theory
Parts of this chapter are reproduced or adapted from Cornes et al. 26
Overview of realist evaluation approach
Realist evaluation is a theory-driven approach based on a realist philosophy of science that addresses the question ‘what works, for whom, under what circumstances and how’. 27 Central to the realist method is the identification and refinement of propositions about how a programme is supposed to achieve its intended outcomes, known as ‘programme theories’. Programme theory is operationalised as ideas about (1) what works and why, (2) how to remedy any identified deficiency and (3) how the remedy itself may be undermined. 25
According to the RAMESES II quality standards for realist evaluation,2 the main ideas that go into the making of an intervention should be surfaced and made explicit at an early stage. An initial tentative programme theory should be constructed, setting out how and why an intervention is thought to ‘work’ to generate the outcome(s) of interest. This initial tentative theory (or theories) are then progressively refined (recast) over the course of the evaluation.
In this chapter we describe how we applied realist principles of generative causation to the evaluation of specialist HHDSs and show how we used the literature to arrive at an initial tentative programme theory about what works to deliver consistently safe, timely transfers of care. We start with an overview of the generic hospital discharge literature and then present a more a detailed synthesis of the specialist (homeless) intermediate care literature. First, we explain why we considered a realist approach to be the most appropriate methodology for this evaluation and how we anticipated the findings would be used.
Selecting the most appropriate research methodology
The HHDF is a complex service development initiative. This is because of the diversity of the projects funded (level of professional input, intensity and duration, etc.) and the wide range of geographical contexts in which they are situated. In designing the research, we drew on the methodological learning from earlier evaluations of similar policy developments that sought to pilot a range of intermediate care or ‘step-up’ and ‘step-down’ projects for older people. 22 In England, considerable variation in the design, definition and configuration of intermediate care services has been permitted at local levels. Consequently, the range of possible combinations/schemes made it difficult to establish any strong link between scheme features and effectiveness. 28 As a result, it has not been possible to arrive at definitive conclusions about particular service models being more effective than others (e.g. ‘nurse led’ vs. ‘therapy led’). This inconclusiveness led the DHSC to observe that ‘A thousand flowers have bloomed’. 18 This captured not only the diversity of intermediate care development in England, but also an unintended outcome, namely the benefits arising from the enthusiasm that had been unleashed through opportunities of piloting many new and innovative ways of working.
It has also been suggested that working towards a ‘standardised model’ of intermediate care is undesirable because different areas will have different levels of need and different resources. 29 As the DHSC23 pointed out, intermediate care should provide the function of linking and filling the gaps in the local network, leading to what Medcalf and Russell30 term ‘independent local pathways of care’. According to the DHSC, Association of Directors of Adult Social Services and NHS England,20 no one model can meet all the needs of all patients leaving hospital. The aim should be to develop a ‘complex adaptive system’ that involves simple rules to function rather than rigid, inflexible criteria.
We opted for a realist evaluation approach because we considered this research lens to be most suited to overcoming the challenges outlined above, namely the need to move beyond questions of effectiveness. Realist evaluation starts from the premise that ‘Nothing will work everywhere all of the time’. 31 The fundamental question that researchers working with a realist perspective ask is how do certain causal mechanisms (e.g. GP-led advocacy) operating in particular circumstances (e.g. a HHDS) create certain changes or outcomes (e.g. improved experiences of hospital discharge). In many respects, the purpose of a realist evaluation is to support decision-makers to implement successful schemes in contexts that may differ markedly from those in the original effectiveness studies. Pearson et al. 25 argue that using a realist synthesis to build a conceptual ‘road map’ that can guide future intervention development about ‘what works for whom and in what circumstances’ may be an important step in complementing more traditional evidenced-based approaches, which often leave these questions unaddressed.
Realist principles of generative causation
In a realist evaluation, ‘context + mechanism = outcome’ configurations are used as a heuristic device by the researcher to develop programme theories about how an intervention is supposed to function. The theories are then tested using empirical data. To illustrate the correct utilisation of these concepts, Dalkin et al. 32 use the example that programme evaluators do not suppose that closed circuit television (the intervention) simply causes a fall in crime rates (the outcome). It does so by persuading potential perpetrators of increased risks of detection where there is a camera (this is the mechanism). Within this view, it is acknowledged that programmes and interventions do not change people, rather it is how people interpret and use what the programme provides that changes things. 31 Within a realist evaluation a context describes the conditions in which programmes and interventions are introduced, acknowledging that mechanisms will be active only in particular circumstances. Context includes cultural norms, economic conditions, public policy, etc. Mechanism describes what it is about programmes and interventions that bring about any effects (i.e. changes in reasoning). The focus is on the ‘intervention resources’ and new practice approaches that programmes offer to enable them to work. The process of how subjects interpret and act on these ‘intervention resources’ is known as the mechanism. Here, impact is understood as the process through which these ‘intervention resources’ facilitate or ‘fires’ a change in reasoning and behaviour, leading to different outcomes and costs. Outcomes are the intended and unintended consequences of programmes resulting from the changes in reason.
It should be noted that in this study we adopt Dalkin et al. ’s32 slightly modified formula for realist evaluation. In the original framework proposed by Pawson and Tilley,27 the change process is conceptualised as ‘context + mechanism = outcome’. In Dalkin et al. ’s32 formula ‘intervention resources’ and ‘reasoning’ are seen as mutually constitutive of a mechanism, but are explicitly disaggregated to allow for the interplay of context. The revised formula is:
Applying realist principles to the research design
In this section, we describe how we incorporated realist principles in the overall design of the study. The specialist HHDS is the intervention or ‘black box’. The main outcome of interest is securing safe, timely transfers of care for people who are homeless or in housing need.
Step 1: literature synthesis
The first step in this realist evaluation (literature synthesis) sought to identify the many different ‘intervention resources’ [including ‘simple rules’ and key practice principles (KPPs)] that might be deployed in a HHDS to facilitate the outcome of interest. The literature was then used to develop programme theories by exploring the existing evidence for each of these ‘intervention resources’.
Step 2: mapping typological configurations
Once the research team was familiar with the full range of (possible) intervention resources, the next step was to explore HHDS documentation (project leaflets, evaluation reports, etc.) and to undertake a series of preliminary site visits and discussions with key HHDS stakeholders. The objective here was to map the ‘intervention resources’ that are actually being deployed across the 52 HHDSs and, importantly, to tease out the underpinning logic for their use (i.e. why the scheme has opted to utilise these resources and practices). This preliminary mapping also informed site selection, enabling subsequent testing of the initial tentative programme theories.
Step 3: testing and refining programme theories through empirical data collection
The third step was to test and refine programme theories through empirical data collection. This study employed a mixed-methods approach comprising three WPs, allowing for both qualitative and quantitative interrogation. We will return to discuss the design of each WP later in the report once we have specified the theories being tested. In the remainder of this chapter, we focus on how our initial tentative programme theories were generated through a realist synthesis of the intermediate care literature.
Towards an initial tentative programme theory
According to the RAMESES II quality standards for realist evaluation, initial ‘hunches’ about what works should be clearly described at the outset. 2 The starting point for this evaluation was to ascertain a broad overview of the generic literature on hospital discharge in terms of what is known to work for all patient groups. This evidence base is summarised for commissioners and service planners in High Impact Change Model. Managing Transfers of Care between Hospital and Home. 33 This guidance outlines eight key high-impact changes.
Change 1: early discharge planning
Underpinning logic
In emergency/unscheduled care, robust systems need to be in place to develop plans for management and discharge and to allow an expected date of discharge to be set within 48 hours.
Change 2: systems to monitor patient flow
Underpinning logic
Protocols enable teams to identify and manage problems (e.g. if capacity is not available to meet demand) and to plan services around the individual.
Change 3: discharge co-ordination underpinned by multidisciplinary team working, including the voluntary and community sector
Underpinning logic
Co-ordinated discharge planning based on joint assessment processes and protocols, and on shared and agreed responsibilities, promotes effective discharge and good outcomes for patients.
Change 4: Home First (intermediate care) and discharge to assess
Underpinning logic
Providing short-term care and reablement in people’s homes or using ‘step-down’ beds to bridge the gap between hospital and home means that people no longer need to wait unnecessarily for assessments in hospital. In turn, this reduces delayed discharges and improves patient flow.
Change 5: flexible working patterns
Underpinning logic
Successful, joint 24 hours a day, 7 days a week (24/7) working improves the flow of people through the system and across the interface between health and social care, and means that services are more responsive to people’s needs.
Change 6: trusted assessment
Underpinning logic
Using trusted assessors to carry out a holistic assessment of need avoids duplication and speeds up response times so that people can be discharged in a safe and timely way.
Change 7: focus on choice
Underpinning logic
Early engagement with patients, families and carers is vital. A robust protocol, underpinned by a fair and transparent escalation process, is essential so that people can consider their options and the voluntary sector can help patients consider their choices and reach decisions about their future care.
Change 8: improved discharge to care homes
Underpinning logic
Offering people joined-up, co-ordinated health and care services, for example aligning community nurse teams and general practices with care homes, can help reduce unnecessary admissions to hospital, as well as improve hospital discharge.
Initial hunch
Our initial hunch was that these eight high-impact changes [or mechanism intervention resources (MIRs)] might prove to be equally important in delivering consistently safe, timely transfers of care patients who are homeless. More specifically, we hypothesised that specialist HHDSs encompassing all of most of these changes would deliver better outcomes for service users than those schemes employing fewer or none.
Testing this programme theory empirically through new research was important because much of the evidence underpinning the high-impact change model (HICM) (version 2015) was based on research with older people. At the outset of the research, very little was known about if and how the HICM might work for patients who were homeless.
How we anticipated the research might be used
In terms of the potential to lever change and improve outcomes for patients who are homeless, the HICM is an important tool. Developing pathways out of hospital is a key objective of the government’s programme for ‘integration and better care funding’. 34 The Better Care Fund (BCF) is the main source of funding for intermediate care in England and places clear expectations on health and well-being boards to oversee health and social care, including (1) pooling budgets, (2) integrating services to ensure more people can leave hospital when they are ready and (3) following guidelines laid down by the HICM. Local progress to implement the HICM is actively monitored by NHS England and NHS Improvement (NHSE&I), meaning that any research that is embedded as part of this is potentially more likely to be implemented than other research that is not linked to government priorities.
In terms of how we envisaged the research would be used, we anticipated that the evaluation findings would either confirm the relevance of the HICM in its current format or make recommendations as to how it could be sensitised to better meet the needs of homeless patients.
Realist synthesis of the intermediate care literature
In testing and further refining our initial programme theory (prior to empirical data collection), the next step was to interrogate the literature more fully with regard to how each of the HICM changes might work for homeless patients and also to identify any other intervention resources that might support timely discharge. However, undertaking a literature synthesis for all eight changes was beyond the scope of the present study. As intermediate care is the key change recommended in the HHDF, we decided to concentrate the searches around change 4. We also thought it probable that the evidence for intermediate care would surface information on many of the other HICM changes, such as benefits of MDT working and promoting patient choice. Furthermore, of the different changes outlined in the HICM, intermediate care arguably has the greatest impact (transformational), especially with regard to outcomes linked to reducing the number of DToCs. 35 We also had the added advantage of being able to build on an already completed realist synthesis of the ‘generic’ intermediate care literature, as we discuss in the next section.
A conceptual platform for intermediate care
In 2013, a realist synthesis of the (generic) intermediate care literature was published. 25,27–36 This identified over 10,314 sources for potential inclusion and generated an extensive list of ‘programme theories’ for testing and refinement. An iterative Delphi-style technique was then used to arrive at a conceptual framework for intermediate care. This identified three programme theories as having the most ‘explanatory power’ when seeking understanding of how intermediate care works to improve outcomes for service users in a wide range of contexts. According to this conceptual framework, improved service user outcomes are achieved when:
-
the place of care and timing of transition to it are decided in consultation with service users based on the pre-arranged objectives of care and the location that is most likely to enable the service user to reach these objectives (programme theory 1)
-
health and social care professionals foster the self-care skills of service users and shape the environment so as to re-enable service users (programme theory 2)
-
health and social care professionals work in an integrated fashion with each other and carers (programme theory 3). 25
However, a limitation of this review was that it did not include literature on (specialist) intermediate care services for patients who are homeless.
To fill this knowledge gap and further develop our own initial programme theory, we applied the same methods and search strategy as outlined by Pearson et al. ,25 but extended the scope of the search to include ‘homelessness’. Although Pearson et al. ’s25 search strategy used, what they believed to be, a comprehensive list of phrases relating to intermediate care, we extended the scope of this search to encompass [‘medical respite’] and [‘homelessness AND ‘hospital discharge’ (schemes)] and [‘homelessness AND ‘delayed discharge’.] This is because the term intermediate care is not widely or consistently used in the homelessness sector. The search terms used are shown in Box 1.
Homelessness AND
‘hospital discharge’ (scheme)
‘delayed discharge’
‘Intermediate care’
‘Hospital at home’
‘Admission avoidance’ (scheme)
‘Early discharge’ (scheme)
‘Step-down’ (care)
‘Step-up’ (facilities)
‘Geriatric day hospital’ (day care)
‘Rapid response’ (team)
‘Intensive rehabilitation’ (service)
‘Recuperation facilities’ (residential or nursing home)
‘Integrated home care team’
‘One-stop primary care centre’
‘Nurse-led’/‘Consultant-led’/‘GP-led’/‘Physician-led’ (schemes/inpatient units)
‘Residential (care) rehabilitation’
‘Supported discharge’
‘Day (centre) rehabilitation’
(Acute care) ‘at home’
Hospital in the home
‘Rehabilitation at home’
‘Community Assessment and Rehabilitation Teams’ (CARTs)
‘Re-ablement’
‘Restorative care’
To this list we added the term ‘medical respite’, as it is often applied to residential-based intermediate care schemes for homeless people.
In terms of analysis, the overall aim of this exercise was to map how this additional evidence on specialist (homeless) intermediate care ‘speaks’ to the conceptual ‘road map’ already proposed for generic intermediate care by Pearson et al. 25 The literature synthesis is reported in accordance with the RAMESES II publication standards for realist reviews. 3
Methods used in literature synthesis
Searching processes
Electronic searches were carried out for peer-reviewed articles published in English from 2000 to June 2019 in the MEDLINE, MEDLINE In-Process & Other Non-Indexed, EMBASE, Social Policy & Practice, Health Management Information Consortium, British Nursing Index, The Cochrane Library, Cumulative Index to Nursing and Allied Health Literature and Applied Social Sciences Index and Abstracts. We searched the ‘grey’ literature through relevant websites [e.g. DHSC and Homeless Link (London, UK)], as well as through the internet using the Google search engine (Google Inc., Mountain View, CA, USA). We also contacted the 52 HHDF schemes seeking copies of any local evaluations and project reports.
It should be noted that an earlier version of this literature synthesis was published by the research team in 2018. 26 In preparing this present report, the original searches were updated to cover the period June 2017 to June 2019.
Selection and appraisal of documents
Intermediate care is a complex term that can encompass a wide range of different service configurations and functions. In selecting material for inclusion in the review, Pearson et al. 25 helpfully distinguish between conventional ‘hand-overs’ of care between providers and interventions that have been specifically designed to support service users’ transitions. The inclusion criteria for this present review was that articles and reports should describe specific interventions to support homeless service users in transition and that the intervention should encompass most of the key characteristics of intermediate care (Box 2). We included a small number of additional articles that considered homeless health or hospital discharge more generally, but only where they raised questions about the need for intermediate care. 26,30–37
Supports transition (e.g. hospital to home).
Occurs at a critical point (i.e. on the cusp of the shift from independence to dependence, at the point of acquisition of a chronic illness or disability, or at the intersection of illness and frailty).
FunctionsA bridge between (1) locations, (2) health or social care sectors (or within these sectors) and (3) health states. Views people holistically as individuals in a social setting.
Time limited (e.g. 72 hours, 2 weeks, 6 weeks).
StructureDesigns and embeds new routes through services (which enhance sensitivity to needs and wishes of service users).
ContentTreatment or therapy (to increase strength, confidence and/or functional abilities).
Psychological, practical and social support.
Support/training to develop skills and strategies.
Each source was read by at least two members of the research team. Papers were assessed based on the same realist ‘quality’ criteria utilised by Pearson et al. 25 This makes distinctions between those that are ‘conceptually rich’ (with well-grounded and clearly elucidated theories, ideas and concepts), ‘thick’ (a rich description of a programme, but without explicit reference to theory underpinning it) and ‘thin’ (weaker description of a programme, where discerning a programme theory would be problematic).
Data extraction, analysis and synthesis process
The literature was synthesised to discern how it addressed Pearson’s et al. ’s25 conceptual framework. When reviewing the literature, we sought to identify programme theories that were both explicitly argued and those that were tacit or implied, making it clear which was the case. A data extraction pro forma was designed to allow the evidence to be carefully mapped against each of the three programme theories. This included space for identification of any new programme theories. The final stage of the synthesis was to take the evidence as a whole and to reflect on the overall utility of Pearson et al. ’s25 conceptual framework, highlighting where any changes or refinements could be made.
Limitations
The limitations of a synthesis approach are that, although we have outlined our search strategy, we made judgments about the interpretations of the findings. Identifying programme theories and mechanisms from sources that are not explicitly theory driven, or do not provide adequate descriptions of the services, is also problematic and risks bias arising from the perspectives of the reviewers. Using multiple reviewers for each literature source helped address any uncertainty in the utility of the findings, challenging any bias.
Results of literature synthesis
The searches yielded 87 references, of which 48 met the inclusion criteria. Additional hand-searching revealed eight further articles. Internet-searching and direct contacts with intermediate care projects yielded 13 reports. These were mostly project reports and/or small-scale external evaluations. In total, 69 reports and articles were included in the synthesis.
Document characteristics
Appendix 1 summarises the articles and reports (n = 69) that were included in the review, the methods they used, their ‘richness rating’ and to which programme theories they aligned. Most of the literature fell into the ‘thick’ category, with few papers including a theoretical perspective. Most of the empirical evidence was from the USA and focused on medical respite. The UK evidence comprised mainly local grey literature reports and was focused mainly on the hospital discharge schemes that had been set-up with the HHDF funding.
Programme theory 1: the place of care and timing of transition to it are decided in consultation with the service user
The literature on homeless intermediate care confirms the central importance of consulting with service users about all aspects of their care and support. 38,39 In an early feasibility study, Lane40 noted that a particular advantage of intermediate care was its focus on person-centred care, rather than disease management, and that this could benefit people experiencing homelessness who are often familiar with and respond well to individually tailored care, as in supported housing. Poor outcomes, such as ‘self-discharge’ or a return to ‘rough sleeping’, are a significant problem where there is a failure to tailor care and support to the specific needs of people experiencing homelessness. 26,30–45
Tackling stigma and discrimination
Many people experiencing homelessness encounter stigma and discrimination in hospital. 37 Backer et al. 46 and Canham et al. 47 advise that this requires attention as part of good discharge planning. Indeed, although many of the HHDF schemes focus on ‘delayed discharge’ to meet their funders’ objectives,48 the more immediate concern of front-line practitioners is often preventing premature discharge. 49 Dorney-Smith et al. 50 describe how premature discharges can be linked to low thresholds being employed by ward staff for ‘bad’ behaviour (with no management techniques being tried or employed) and inexperienced staff affecting the overall quality of discharges.
Pearson et al. ’s25 review highlights the training of staff in the specific skills needed to deliver person-centred care as an important mechanism in the delivery of successful intermediate care. However, in homeless intermediate care, ‘cultural distance’ emerges as a complicating factor. Drury,51 for example, describes how the daily lives of health-care practitioners and homeless people are so different that they may become cultural strangers, fearfully avoiding contact with each other. Cultural distance often creates the ‘gaps’ that specialist intermediate care is then expected to fill. In their study of continuity post hospital discharge, Whiteford and Simpson52 found that some community nurses will not provide care inside hostels because they are perceived as ‘dangerous places’.
Many of the HHDSs funded as part of the HHDF perceived it as part of their role to offer mentorship and training to educate (mainstream) hospital staff about working with people experiencing homelessness. However, the grey literature suggests that this learning quickly evaporates without a ‘continuous and consistent presence’. 53,54
Engagement (patient in-reach) as a distinct mechanism
Compassionate kindness, dignity and respect are values that are seen to sit at the heart of psychological- or trauma-informed care and are aspired to by many specialist HHDSs. Halligan and Hewett55 observe how a visit from an empathetic team that is dedicated to the care of homeless patients in the hospital can improve patient experience and also prevent problems such as premature discharge.
Indeed, what also emerges from this literature is the importance of professionals first ‘engaging’ or building rapport with service users and how this may act as a distinct mechanism for underpinning more formal consultative or collaborative care planning processes. As Halligan and Hewett55 observe, it is only once a relationship is established that the hard work of planning community support and negotiating with housing, social care and health-care providers and the voluntary sector can begin.
Discussing a ‘nurse-led’ residential intermediate care scheme, Dorney-Smith56 describes how up to 1 month of engagement work may be needed to counter the suspicion and distrust patients may have of professional support. In the hospital setting, this work is often conceptualised as primary care or ‘patient in-reach’. This brings highly specialist clinical knowledge and understanding of homelessness onto the hospital ward, whereby specialist GPs and nurses are employed to work side by side with hospital consultants and ward staff to raise awareness about homelessness and tackle stigma and problems, such as the prevention of early self-discharge.
One of the key mechanisms for achieving patient in-reach is the ‘homeless ward round’, in which clinicians from the homeless team will identify and support homeless patients located across the hospital site. Identification of homeless patients at an early stage of admission is key to early discharge planning. Teams will use ‘concerned curiosity’ to understand a patient’s housing circumstances, mindful of the stigma of homelessness and that some patients will not want to reveal that they are homeless. They will then work with patients in psychologically informed ways to build relationships and support them to remain in hospital, have their voices heard and complete treatment.
As noted above, when working with patients who are homeless, the main challenge is not delayed discharge but more usually preventing ‘early self-discharge’. Often this can be a result of substance misuse and the patient wanting to discharge themselves against medical advice because of the onset of unpleasant withdrawal symptoms. Withdrawal can also be at the root of much challenging behaviour on the wards, for example where the patient feels that his or her withdrawal is not being appropriately managed and leaves the ward to use street drugs. Ward staff will then often address such absenteeism from the hospital bed, issuing behavioural contracts that can lead to conflict. In such circumstances, homeless team nurses and GPs can intervene to de-escalate the situation through more appropriate skilled clinical management (e.g. correct titration of opiate substitution medication such as methadone). The homeless team will also raise awareness among ward staff about many other forms of ‘silent stigma’ that lead people who are homeless to feel uncomfortable in hospital, such as being mindful that they may have no visitors to take home their washing and provide access to clean clothes and toiletries. Ultimately, the main goal of GP- or primary care-led ‘patient in-reach’ is to maximise the benefits of a hospital admission. However, Canham et al. 47 make the point that, in the absence of adequate aftercare resources, the benefits of trauma-informed care and patient in-reach can quickly evaporate.
Tomita and Herman57 undertook a randomised controlled trial (RCT) that evidenced reduced hospital readmission rates and other positive outcomes for 150 homeless psychiatric (mental health) patients receiving a care co-ordination intervention (vs. usual care). This suggested that the relationship with the social services’ worker may be as equally an important mechanism in delivering these positive results as securing housing tenure and stability.
Place of care
The strongest correlate of hospital readmission among homeless people is discharge location. 58 Kertesz et al. 59 showed that discharge to a medical respite facility was associated with significantly lower odds of readmission than discharge to ‘own care’ (including homeless shelters). Discharge to supportive housing has similar benefits. 60
Pearson et al. 25 reported that the characteristics of the local health and social care system could significantly limit care options for service users. This was evidenced in the homelessness literature, with people who are homeless having little opportunity to influence decisions about their place of care because few options might be available. 61
Doran et al. 58,62 reported that many US respite schemes will not admit homeless people who continue to drink and whose behaviour is identified as ‘challenging’. It might be argued that the lack of system capacity in the community, geared to the realities of persons’ needs, equates to acute care being a fall-back option. According to the Housing Learning and Information Network,29 having a specialist homeless hospital discharge worker does not eradicate delayed discharge if appropriate community care is not available. However, it can work to highlight where the gaps exist. The Housing Learning and Information Network caution that finding placements for people who continue to drink and have disabilities is often challenging. 29
The notion that intermediate care might itself fill some of these gaps raises questions about scope and remit and how far this should extend into the territory of longer-term care. According to van Laere et al. ,63 the high mortality rate among users of a Dutch medical respite scheme might be explained by the fact that the homeless population in Amsterdam most commonly comprises people with mental health challenges, long-term opiate users and people misusing alcohol who are not able to live independently and depend on fragmented services. In addition, many intermediate care schemes for people experiencing homelessness currently provide palliative care to compensate for the lack of provision elsewhere. 63–65
Generic or specialist?
Mainstream intermediate care facilities may not currently meet the needs of people who are homeless. 66 The argument for ‘specialist’ provision stems, in large, from the challenges of co-housing people with different challenges and vulnerabilities. 67 For example, Lane40 charts the advantages and disadvantages of admitting people who use substances and are experiencing homelessness to mainstream intermediate care. On the one hand, it is considered that when someone is in recovery they should not be exposed to hostel environments in which drug and alcohol use is commonplace. On the other hand, it is recognised that people who use substances may have ways of being that are problematised by health and care providers and other users of intermediate care services.
Rather than being understood in the context of patient choice and the need for person-centred care planning, debates around ‘place of care’ may be conflated with potentially discriminatory assumptions about the characteristics of different user groups. For example, Lane40 reports that some GPs and hostel managers he interviewed expressed concerns that ‘homeless people’ would not mix well with other users of intermediate care because they may be older and fragile both physically and emotionally. They were, therefore, overlooking the potential for challenging behaviours among older people related to conditions such as dementia.
Safe spaces for women
A study of early exit from medical respite reported that ‘respite structure’ (i.e. rules and regulations) could make some service users feel unsafe and may account for why up to one-third of people leave medical respite earlier than planned. 41 Women in this study were significantly more likely to leave respite before discharge completion than men. According to Bauer et al.,41 gender-specific treatment models or women-only spaces could enhance safety and consequently retention outcomes.
Programme theory 2: professionals foster the self-care skills of service users and shape the environment so as to re-enable them
One of the key objectives of intermediate care is that people should not be admitted straight from hospital to long-term care facilities without the opportunity for ‘reablement’, ‘recuperation’ and ‘rehabilitation’. 23 Importantly, although some local intermediate care services are integrated in England, physical rehabilitation tends to fall within the domain of the NHS, whereas recuperation (in a care home) and reablement fall under the banner of local authorities (councils) with social services responsibilities. Although health care is free in England, social care is means tested and potentially subject to a financial charge, as well as having eligibility thresholds. However, because recuperation and reablement are badged as intermediate care they are usually provided free of charge for a period of up to 6 weeks. The optimum time frame for intermediate care is considered to be between 2 and 8 weeks.
Reablement and physical rehabilitation needs
A feasibility study reviewed the caseload of a specialist homeless primary health-care team in Ireland to assess the need for a specialist homeless intermediate care centre. 68 It found that 15% of homeless people on the caseload had mobility and disability challenges attributable to health conditions, such as stroke, hip replacement, fracture or amputation.
In the literature on homeless intermediate care, ‘re-enablement’ or ‘reablement’ were not mentioned. Many studies reported difficulties collaborating with local authority adult social care, which may indicate that local authority reablement services are not easily accessible to people who are homeless. 42,45,65,69,70
Reports also suggest that the physical rehabilitation needs of people experiencing homelessness are not well catered for. 61–71 Whiteford and Simpson65 observed that many homeless people struggled to access rehabilitation not because they were homeless, but because of their age, with many services excluding people under the age of 55 years. Indeed, there is a recognised need for improved disability access in many UK hostels for homeless people. 45–73
‘Reablement’ environments
Mainstream residential intermediate care facilities in care homes or in hospitals often provide access to specially adapted environments, such as a ‘training kitchen’, in which people can practice the activities of daily living. A complaint arising from service users in one (specialist homeless) hostel-based intermediate care facility was boredom due to the lack of any kind of structured daily activity. 64 More recently, Pathway teams in London have employed occupational therapists to address this risk by promoting meaningful activity. 50
Recovery
There is emerging consensus in the intermediate care literature specific to people experiencing homelessness that to stop the ‘revolving door’ of hospital readmissions, support needs to extend beyond the discharge process itself and into the community, either by means of a residential ‘step-down’ facility or ‘floating support’ arrangement. 45,48,54 However, what is less clear is the ideal time frame for such arrangements, which may be termed intermediate care.
In the literature on specialist homelessness intermediate care, ‘recovery’ from drug and alcohol misuse and/or mental health problems emerges as the primary rehabilitative focus. O’Carroll et al. ’s68 feasibility study, for example, found that 48% of the caseload were experiencing problematic substance misuse, 33% had mental health challenges and 17% were dually diagnosed. However, the setting of goals around ‘recovery’ raises further questions about the accepted time frames for intermediate care. Dorney-Smith,56 for example, charts how service users’ health deteriorated when they were discharged from a nurse-led intermediate scheme that provided between 6 and 8 weeks of support. Dorney-Smith56 observes that recovery is a ‘long game’ for many homeless clients and time frames may be upwards of 24 months.
Resettlement
The 6- to 8-week time frame for intermediate care is further brought into question by the multiple overlapping natures of the transitions facing service users who are homeless (i.e. from ‘hospital to home’ and from ‘homelessness to housed’). Managing the transition from ‘homelessness to housed’ encompasses both the practical aspects of securing accommodation, as well as meeting what are termed ‘resettlement needs.’74 Indeed, there are many parallels to be drawn between ‘reablement’ and ‘resettlement’ work, with the latter being ‘housing’ rather than ‘social care’ led. Both share the aim of ‘doing things with rather than for people’ and have the overall aim of promoting independence. It might even be suggested that ‘resettlement’ work has a broader, more personalised focus than ‘reablement’, as it is often encompassing of both ‘citizenship goals’, such as securing employment, education and volunteering opportunities, as well as those linked to reablement and the promotion of ‘self-care’. Describing a specialist residential intermediate care facility for homeless people in northern England providing up to 3 months of resettlement support, Lowson and Hex75 describe the goal of the service as giving people the opportunity to make real life-changing decisions and to have a ‘real go’ at their lives, improving their life chances and quality of life, as well as improving independence with daily living tasks.
Pearson et al. ’s25 review noted that one drawback with (mainstream) intermediate care is that it has tended to prioritise a desire for service users to attain certain functional goals within a specified time period over service users’ self-knowledge and desire to reach a wider set of goals over longer, less clearly defined time periods.
Programme theory 3: health and social care professionals work together in an integrated fashion with each other and carers
Multidisciplinary team skill mix
Many hospitals in England now employ discharge co-ordinators to manage the most complex discharges. As recommended in the HICM,33 these roles are usually embedded in MDTs comprising senior nurses and social workers. The main focus of their work is usually on managing transfers of care for older people requiring continuing health care and/or moves into care homes. 76 Where there are large numbers of homeless patients (≥ 200 per year), it is recommended that hospital trusts develop specialist clinically led multidisciplinary ‘homeless teams’ to work alongside existing discharge teams. 77 As noted earlier, these are often called Pathway Homeless Teams by virtue of their affiliation with the Pathway charity, and these employ GPs, nurses, housing workers and a range of other staff. A RCT of the costs and benefits of two ‘clinically led’ services (vs. ‘standard care’) indicated that this clinically led approach does not alter length of stay, but improves the quality of life of homeless people (with fewer service users returning to the streets) at a cost deemed cost-effective under current guidelines. 78
An early evaluation of the HHDF similarly concluded that those schemes taking a specialist MDT approach were more effective in delivering improved health and housing outcomes than other models. 70 Without the benefit of a clinician, some of the (uniprofessional) housing link worker projects described difficulties in engaging with what they described as the ‘medical model’. 79 Wood et al. 80 suggest that the combination of nursing and social care is particularly effective for people who have complex problems or who have experienced long-term homelessness, given that the early stages of being housed can be immensely challenging, with poor physical and mental health adding to the concomitant stress of adjusting to a very different way of life. Case study evidence also highlights the important role of the GP in the MDT, particularly in advocating for homeless patients’ needs in a holistic way where there may be pressure from senior clinicians to discharge prematurely. 39–81
In the wider literature, discussions around ‘skill mix’ could reflect different ‘occupational lenses’ or types and levels of comprehensiveness around how homelessness might be addressed. Although the focus of the housing link worker schemes was often on housing and benefits advice, with ‘referrals on’ to primary care and other agencies, Hendry64 describes how staff in one medical respite scheme provided a full assessment under one roof, including a full screen blood test, screening for sexually transmitted diseases, medication compliance work, pre-detox work, smoking cessation, mental health, social services, occupational therapy referrals, benefits advice and chiropody. This comprehensiveness is a key feature of many residential step-down or medical respite schemes. 66
Involving carers and family members
In none of the material reviewed was there explicit reference to family member, carers and friends being involved in discharge and intermediate care support planning. However, there was an account of one discharge scheme that focused specifically on linking people who were experiencing homelessness back to their country of origin or their home town where they may have a ‘local connection’ and, therefore, a better chance of securing housing and social care support. 69
Mechanisms for integrating services
For many of the HHDF projects, integration into the hospital setting was described as challenging. 70 Formal protocols (e.g. developing a homeless hospital discharge protocol) were identified as important in most of the grey literature accounts, especially with regard to making sure ward staff asked about homeless and housing on admission. However, the main problem was sustaining them. 29 Successful ways of doing this and raising awareness about the schemes more generally included having the scheme championed by senior hospital staff and actively promoting the scheme through posters, leaflets and contact cards. 44 Co-location and being ‘a face’ on the ward were thought to help ensure the flow of referrals and ease of communication. 54–61,72 Participating in ward rounds, attendance at weekly hospital staff meetings to discuss patient discharge planning and running reflective practice and training sessions for hospital staff on the subject of homelessness were also considered helpful. Once the referral pathways were established in HHDF schemes, hospital staff seemed to appreciate being able to ‘hand over’ responsibility for the homeless people on their wards. 54 ‘Passing the baton’ could, however, potentially reduce opportunities for collaborative working.
Advocacy as an additional key mechanism
Although integration and co-ordination are foregrounded as key mechanisms for the successful delivery of intermediate care,25 the homeless-specific literature suggests that advocacy (‘arguing the case’) may be equally important. 44 Many grey literature accounts of the HHDF schemes alluded to the impact of austerity and depleted budgets, which meant reduced availability of housing and longer-term care and support. It was noted that housing authorities will often defend their budgets by rigidly restricting access to a defined ‘local’ population. This renders care co-ordination particularly challenging for homeless people who often have weak or no ties to any locality and lack documentary proof of any entitlements. 45
Integrating housing as the ‘third pillar’ of intermediate care
UK intermediate care has been delivered primarily as a health and social care service. 25 Canham et al. 47 recognise housing assessment as a key ‘health support’ for persons transitioning from hospital. The HHDF highlights the role of housing services in delivering improved health and well-being outcomes and, consequently, the importance of housing professionals working alongside health and social care professionals. Several grey literature accounts report that hospital staff appreciated this resource, especially in terms of its potential to free up their time. Charles et al. 54 observed that ward staff lacked the knowledge to find accommodation for homeless patients.
One report of a ‘housing link worker’ scheme describes extending its remit beyond ‘homeless people’ so that support could additionally be provided to older people who were being delayed in hospital because of ‘housing issues’. 82 This reflects the importance of integrating housing as the third pillar of health and well-being for all patient groups.
Discussion: framework utility
The additional evidence presented above broadly supports the validity or usefulness of Pearson et al. ’s25 conceptual framework for understanding ‘what works best’ in intermediate care. This is with regard to three key programme theories: (1) the importance of consulting with service users, (2) working in ways that are enabling and (3) ensuring integrated professional working. However, it might be suggested that these three ‘programme theories’ are likely to be implicated in the successful delivery of many other health and social care services. Herein lies a potential limitation of the current framework in that it may not answer some of the more complex or nuanced questions relating specifically to the development of intermediate care services.
The first challenging question to emerge from this review is how to maintain the integrity of intermediate care as a ‘time-limited’ intervention. This question arises where there is a need to encompass multiple and overlapping rehabilitative and resettlement goals, which may require housing solutions underpinned by much longer-term or continued health and social care support. Indeed, decisions around ‘time frame’ and scope are relevant to commissioners of intermediate care for both older people and people who are homeless (some of whom overlap). It is acknowledged that the rehabilitation of older people has sometimes fallen short because it has often prioritised short-term reablement goals linked to ‘physical functioning’ over and above those for inclusion and citizenship. Meanwhile, intermediate care for people who are homeless has reversed the ‘occupational lens’, prioritising longer-term resettlement and recovery outcomes over and above those for reablement. How to encompass these different needs and vulnerabilities under a single service banner is a significant additional challenge, with the danger that ‘specialist’ provision starts to confirm cultural distance (e.g. ‘elderly people’ are quiet and frail and ‘homeless people’ are challenging and disruptive).
These complexities are compounded in times of austerity, when the integrity of intermediate care is further compromised by the need not just to ‘fill the gaps’ in local provision but, on occasions to substitute for the widespread loss of longer-term support services. As Backer et al. 46 suggest, discharge planning and intermediate care will have little impact unless housing and other services are available. Interventions that were shown to work well in areas with well-resourced and efficient community support services were seen to have little or no impact where services are inadequate or lacking. 83
It is recognised that this poses perhaps the most serious threat to the viability of intermediate care as a service organisation and delivery construct. If the boundaries with longer-term care services start to blur, then intermediate care risks quickly becoming ‘blocked’. 66–71,73–84
In terms of a refined ‘conceptual framework’ that might address some of these issues, a US study57–71,73–85 is particularly insightful. It reports the findings of a RCT of a clinically led case management intervention called ‘critical time intervention’ (CTI). 57–71,73–85 CTI was designed to provide emotional and practical support over a 9-month period, with the primary objective of preventing homelessness among people being discharged from a psychiatric (mental health) hospital. In CTI, intermediate care is conceptualised as comprising the following three distinct phases:
-
Transition to the community focuses on engagement and relationship building, providing intensive support and assessing the resources that exist for the transition from in-patient care to community providers.
-
Try out is devoted to testing and adjusting the systems of support and assessing whether or not they are working as planned. By now, community providers are assumed to have adopted primary responsibility for delivering support.
-
Transfer of care focuses on completing the transfer of responsibility to community resources that deliver long-term support. 85
The findings of the RCT, which compared the outcomes of those receiving the CTI intervention with those receiving standard care, suggested that this brief, clearly focused intervention led to a reduction in the risk of homelessness that was evident 9 months after the intervention ended. In accounting for ‘what works and why’, consultation, enabling and ensuring integrated professional working are all implicated in CTI, but the cornerstone of the approach is a potential fourth programme theory. Namely, this is maintaining continuity of care during critical transition periods while responsibility gradually passes to existing community supports that will remain in place after the intervention ends. 85
In CTI, ‘scope’ is clearly defined as being about the management of transitions rather than specific kinds of ‘needs’ or ‘gaps’ in existing provision. It is, therefore, generic in that it can be applied to all client groups and can potentially be operationalised in any given local context, as the aim is to ‘weave together’ the resources and infrastructure that are already in existence. The ‘time frame’ for the intermediate care intervention is also determined not by any rigid ‘service-led’ criteria, but by the adaptive capacity of the local context to meet the person’s needs. It might be added that where CTI becomes ‘blocked’ (i.e. there are no appropriate services to take over responsibility), then this should ring alarm bells for commissioners that there are ‘cracks’ in local provision.
Indeed, CTI also seems to encapsulate the ‘how to’ of what Parker-Radford37 terms a ‘transition of care approach’. This has the additional advantage of shifting the focus of the ‘organisational lens’ from the acute sector to the management of a much wider range of transitions (e.g. ‘prison to community’ and ‘armed forces to civilian’). It is, therefore, potentially key to continuity and seamless care, as seen from the perspective of people who use or reject services.
Summary
Pearson et al. ’s25 conceptual framework proved a useful heuristic device for synthesising the literature on intermediate care for patients who are homeless. It worked as a ‘coat hanger’ on which a wide range of evidence could be hung and critically appraised. As we outline below, it also helped refine our initial programme theory for empirical testing.
First, the findings confirm our initial hunch about the broad utility of the HICM for delivering safe, timely transfers for patients who are homeless. In the specialist homeless literature, there is strong evidence for high-impact change [i.e. change 3 (discharge co-ordination underpinned by MDT working) and change 4 (intermediate care)]. Importantly, an early evaluation of the HHDF suggested that multidisciplinary HHDSs were more effective on some measures than housing-led (uniprofessional) schemes. In addition, there is some evidence that MDT working should encompass ‘clinical input’ (i.e. the inclusion of GPs and nurses) to enable effective advocacy for patients on medical- as well as housing-related matters, preventing problems such as early self-discharge. ‘Patient in-reach’ also emerges as an important additional high-impact change for challenging stigma and underpinning patient engagement and choice (change 7). There is evidence about the importance of specialist homeless hospital discharge protocols to facilitate patient flow (change 2) and specialist ward rounds to facilitate early discharge planning (change 1). Co-locating housing workers on the hospital site is important for keeping protocols live and ensuring that early discharge planning can commence, bringing in housing and homelessness services, home adaptations and equipment. The need to integrate housing (worker/expertise) as the third pillar of health and well-being (i.e. as an integral component of multidisciplinary working) can be conceptualised as an additional high-impact change, such is its importance for early, safe and effective discharge planning. There is less clear evidence for trusted assessment (change 6) and flexible working (change 5). Improving access to care homes was not raised directly (change 8); however, questions were raised about the accessibility (suitability) of residential intermediate care provided in care home settings. This is a potentially important change, which may not feature strongly in the current literature because of the different occupational lenses that may downplay physical frailty and early onset of ageing and cognitive problems in the homeless population. 73 The practice reported of using intermediate care as a palliative care service may be further symptomatic of this.
Second, turning our attention to Pearson et al. ’s25 conceptual framework for ‘generic’ intermediate care, it was hypothesised that good outcomes would be secured for patients on the basis of implementing three KPPs (tested as programme theories): (1) consulting with service users, (2) working in ways that are enabling and (3) ensuring integrated professional working. The additional evidence reviewed here suggests the need for some refinement of these generic principles if they are to support the needs of people who are homeless leaving hospital. These refinements are shown in italics in Box 3. Box 3 synthesises all the above evidence to specify the programme theory we took forward into the next stage of the research for empirical testing. It should be noted that Box 3 is also used as the ‘coat hanger’ (coding framework) for our subsequent qualitative data collection and analysis. The coding draws on Dalkin et al. ’s32 formula outlined earlier. The codes are as follows.
-
MIRs:
-
MIR1 [protocols for early discharge planning/patient flow (high-impact change model 1 and 2)]
-
MIR2 (patient in-reach)
-
MIR2mdt [patient in-reach (with clinical and housing advocacy/expertise combined)]
-
MIR2up [patient in-reach (housing advocacy/expertise only)]
-
MIR3 (discharge co-ordination)
-
MIR3mdt [discharge co-ordination (undertaken by multidisciplinary team)]
-
MIR3up [discharge co-ordination (undertaken by uniprofessional team)]
-
MIR4 (step-down intermediate care)
-
MIR4res (residential step down)
-
MIR4hf [community/home-based (floating support) step-down care]
-
MIR5 (trusted assessment/direct referral rights)
-
MIR6 (strong leadership)
-
MIR7 (strengthening safeguarding).
-
-
KPPs:
-
KPP1 (consultation with service users)
-
KPP2 (promoting reablement and resettlement)
-
KPP3 (integrated working between health, housing and social care)
-
KPP4 (continuity of care).
-
In the next three chapters, we explore how these are being implemented in different contexts, any changes in reasoning and the outcomes achieved:
Achieving consistently safe, timely transfers of care for patients who are homeless (improved outcomes) will depend on localities developing complex adaptive systems that are underpinned by clear protocols for patient flow and early discharge planning (MIR1), access to patient in-reach (MIR2), multidisciplinary discharge co-ordination (encompassing both clinical and housing support) (MIR3) and step-down intermediate care (MIR4). MIRs must be underpinned by the following ‘simple rules’ or KPPs.
KPP1The place of care and timing of transition to it are decided in consultation with service users based on the pre-arranged objectives of care and the location that is most likely to enable the service user to reach these objectives. ‘Engagement work’ [as part of patient in-reach] is recognised as a distinct mechanism for underpinning these more formal consultative or collaborative care planning processes.
KPP2Health, housing and social care professionals foster the self-care skills of service users and ensure that rehabilitation and recovery are encompassing of outcomes linked to both physical reablement and broader health and well-being objectives for inclusion and citizenship.
KPP3Health, housing and social care practitioners work in an integrated way with each other, ensuring that local advocacy support is available.
KPP4Continuity of care is maintained during critical transition periods while responsibility gradually passes to existing community supports that will remain in place after the intermediate care episode ends.
HHDSs with more of the ‘jigsaw pieces’ will be more effective and cost-effective. Any missing pieces will open up the potential for untimely or unsafe discharge and poorer outcomes for service users (Figure 1).
FIGURE 1.
Jigsaw pieces.
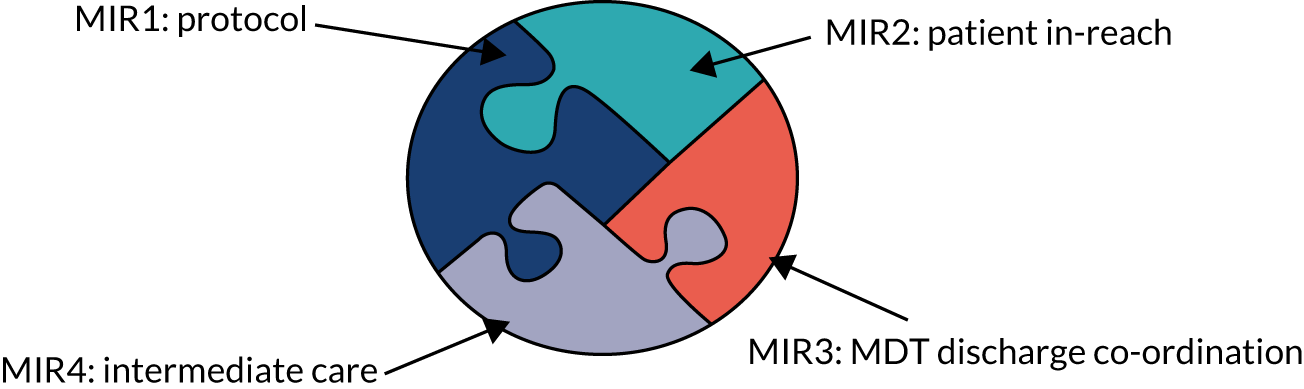
Refinements made to generic principles required to support the needs of people who are homeless leaving hospital are displayed in italics.
Chapter 3 Results: qualitative case studies
Overview
In this chapter, we interrogate and refine our initial tentative programme theory about what works to deliver consistently safe, timely transfers of care by means of a series of qualitative case studies carried out in seven hospital sites. We begin by outlining the methodology for the case studies and then report the results. The overall aim of the qualitative fieldwork was to map the typological configurations evidenced in the site (e.g. the different MIRs and KPPs employed) and explore a range of different service user and stakeholder perspectives on how these are working in practice to deliver consistently safely, timely transfers of care for homeless patients.
Methodology for qualitative case studies
In the original protocol, we planned to undertake in-depth qualitative fieldwork across six principal case study sites. However, mid-way through the research one of the HHDSs was threatened with closure and, therefore, an additional hospital site was recruited. Five hospital sites had HHDSs that represented ‘specialist care’ and two sites did not have a HHDS that represented ‘standard care’. Data collection involved several steps, as outlined below.
Documentary analysis
Having completed the literature synthesis to identify the full range of (possible) interventions/changes (i.e. MIRs), the next step was to explore how these were being implemented in the HHDS sites. To achieve this, we collected and studied HHDS documentation (e.g. project leaflets, evaluation reports), monitoring data held by NHSE&I (for DToCs) and undertook a series of preliminary discussions and site visits with key HHDS stakeholders.
In carrying out the mapping exercise, we were able to make use of a database held by Homeless Link (an umbrella organisation for the homeless sector). This held typological details for all 52 HHDF schemes gathered as part of an early implementation evaluation. 70 All projects on the database were contacted for information and informed about the study. In addition to the information provided by Homeless Link, we were also able to access a wealth of information from the Pathway charity, which acts as an umbrella organisation for the ‘clinically led’ schemes. Preliminary interviews were carried out with staff at Pathway and Homeless Link. We also held three regional focus groups to which HHDS practitioners and managers were invited. These groups invited participants to discuss early progress and gauge interest in taking part in the research. Information was collected for 62 HHDSs, including the 52 HHDF-funded schemes and additional information for nine ‘clinically led’ schemes and one intermediate care network that was not funded by HHDF.
The analysis underpinning the mapping exercise was framed by means of our realist hypothesis (outlined earlier in Box 3). Documentary information was analysed to explore the interventions/changes (i.e. MIRs) that were being implemented in each of the HHDSs (e.g. protocols, patient in-reach, discharge co-ordination and step-down intermediate care) and more general information on funding history, staffing, skill mix and any evidence of effectiveness, as reported in local evaluation reports. At this initial mapping stage, we did not document KPPs, as these were not easily discernible from documentary information. The information was then compiled as a database. This was regularly updated throughout the life of the study, enabling us to chart the history of the projects and whether or not they were sustained in the longer term.
Site selection: specialist sites
The five sites with HHDSs were purposefully selected to represent different geographical contexts and typological (MIR) configurations. Selection was guided by the findings of the initial mapping exercise. The working hypothesis was that sites with more of the jigsaw pieces (i.e. more MIRs) would deliver better outcomes for patients and so we purposefully selected sites to enable interrogation of this, including sites with no HHDS (i.e. no specialist MIRs). We briefly summarise the findings of the mapping exercise below to show why the sites shown in Table 1 were recruited. The mapping also enabled us to further refine our understanding of MIRs for analysis and coding purposes.
| Care | Specialist care | Standard care | ||||
|---|---|---|---|---|---|---|
| Site 1 | Site 2 | Site 3A and site 3B | Site 4 | Site 5 | Site 6 | |
| ‘Clinically led’ (multidisciplinary) | ✓ | ✓ | ||||
| ‘Housing led’ (uniprofessional) | ✓ | ✓ | ||||
| MIR1 homeless hospital discharge protocol | ✓ | ✓ | ✓ | |||
| MIR2mdt patient in-reach (with clinical and housing advocacy/expertise combined) | ✓ | ✓ | ||||
| MIR2up patient in-reach (housing advocacy/expertise only) | ✓ | |||||
| MIR3mdt discharge co-ordination (undertaken by a MDT) | ✓ | ✓ | ✓ | |||
| MIR3up discharge co-ordination (undertaken by a uniprofessional team/single housing worker) | ✓ | |||||
| MIR4res direct access to residential step-down care | ✓ | ✓ | ||||
| MIR4hf direct access to community-/home-based (time-limited) floating support step-down care | ✓ | |||||
| Description of specialist HHDS sites | ||||||
| Site 1: clinically led HHDS with no direct access into step-down intermediate care | ||||||
|
Here, the HHDS serves a large hospital in the capital city with large numbers of patients who sleep rough. The scheme is a co-located ‘clinically led’ (multidisciplinary) homeless team, comprising a GP, a nurse, an occupational therapist, four housing workers and a peer case worker. The team undertakes patient in-reach (MIR2mdt) and discharge co-ordination (MIR3mdt), but has no direct access or ‘referral rights’ into ‘step-down’ intermediate care. Some specialist intermediate care beds (n = 6) are available locally, but these are earmarked for ‘step up’ (prevention of admission) rather than ‘step down’ and so are not easily accessible to the HHDS Configuration = (MIR1 + MIR2mdt + MIR3mdt) |
||||||
| Site 2: clinically led scheme with ‘referral rights (direct access) to residential step-down intermediate care | ||||||
|
The hospital here is based in a small northern city that is part of a large urban conurbation. It is served by two HHDSs. Scheme A is a co-located ‘clinically led’ (multidisciplinary) homeless team, comprising a GP, two nurses, a care navigator and a housing worker. Scheme A undertakes patient in-reach (MIR2mdt) and discharge co-ordination (MIR3mdt), and has direct access (via trusted assessment MIR6) into scheme B. Scheme B is a dedicated 14-bed residential intermediate care (MIR4res) facility. This is staffed 24 hours a day with four housing support workers and a manager. Clinical staff from scheme A ‘boundary span’ (i.e. continue to work with patients once they enter scheme B) Configuration = [MIR1 + MIR2mdt + MIR3mdt + MIR4res + (MIR6)] |
||||||
| Site 3a/b: housing-led schemes with community/Home First (floating support) step down | ||||||
|
Site 3a: the hospital here is based in a small city in the south of England that serves a large rural area. It has smaller numbers of homeless patients compared with sites 1 and 2. The HHDS here is a uniprofessional ‘housing-led’ scheme that has one worker who provides patient in-reach (MIR2up), discharge coordination (MIR3up) and ‘step down’ (MIR4hf) (time-limited floating support in the community) for a time-limited period. As this scheme was threatened with closure during the fieldwork, we recruited an additional site with a similar typological configuration Site 3b: this hospital is based in a large city in the north of England with larger numbers of homeless people than site 3a, but offering a similar ‘housing-led’ single worker service (MIR2/3up + MIR4 hf). A novel feature here was the attachment of the HHDS worker to the safeguarding adults’ team based at the hospital Configuration = (MIR1 + MIR2up + MIR3up + MIR4hf) |
||||||
| Site 4: housing-led scheme offering residential step-down intermediate care | ||||||
|
The hospital here was based in a large town in the north of England. The HHDS was a residential three-bed intermediate care (MIR4res) facility (occupying a separate wing of a hostel). The scheme was staffed by one hostel worker and had no significant resource for patient in-reach or discharge co-ordination beyond the assessment of potential referrals Configuration = MIR4res |
||||||
| Description of usual/standard-care sites (with no HHDSs) | ||||||
|
Site 5: the hospital here was based in a medium-sized city in the south of England. A HHDS had once operated in the hospital, but had lost its funding and ceased to operate prior to the start of the HHDF Site 6: the hospital here was a mental health facility based in the north of England, serving a large mainly rural population. This site had no specialist homeless discharge provision and no generic complex discharge co-ordination team (i.e. ward staff have full responsibility for all aspects of discharge planning for all patients regardless of complexity) |
||||||
The mapping exercise confirmed the important typological distinction between HHDSs that were ‘clinically led’, employing a (specialist) MDT to deliver patient in-reach (MIR2) and multidisciplinary discharge co-ordination (MIR3), and those that were ‘housing led’ (uniprofessional). Housing-led schemes also delivered patient in-reach (i.e. supporting and building relationships with patients prior to discharge) (MIR2) and undertook discharge co-ordination (MIR3). However, this was not necessarily multidisciplinary if, for example, the housing link worker from a uniprofessional scheme worked in isolation from other professionals and agencies. Therefore, for analysis (coding) purposes, we distinguish between MIR2 (patient in-reach) and MIR3 (discharge coordination) that is embedded in a MDT working (MIR2/3mdt) and that which is uniprofessional (MIR2/3up).
Another key typological feature to emerge from the mapping was that intermediate care (MIR4) was nearly always delivered as an integrated component of the ‘housing-led’ HHDSs (as time-limited floating support post discharge), whereas most of the ‘clinically led’ services closed cases when the patient exited the acute sector. For analysis (coding) purposes, we distinguish between intermediate care that is Home First (community-based floating support) (MIR4hf) and that which is residential/bed based (MIR4res) (i.e. where people move straight from hospital into a dedicated residential step-down unit).
The mapping exercise also demonstrated many other ways in which HHDSs were configured locally using different MIRs. For example, some localities had used HHDF funding to set up or refurbish an intermediate care facility (MIR4res), but did not then have resource to ‘in-reach’ into the hospital (MIR2-missing) and to assist ward staff with discharge co-ordination (MIR3-missing). Furthermore, in only one site could we find evidence of what might be termed sustained and purposeful engineering of a ‘complex adaptive system’. In this site, there were two HHDSs in operation. These were integrated by means of protocols (MIR1) for flexible working and ‘trusted assessment’ (MIR5) in which staff from the clinically led homeless team had direct referral rights into a housing-led residential intermediate care facility. This created an out-of-hospital care pathway that encompassed most of the jigsaw pieces:
On the basis of the mapping exercise, we hypothesised that this configuration (i.e. site 2) would deliver the best outcomes for homeless patients.
Standard care site selection
Two standard care sites were selected. The first did not have a HHDS. This site was selected opportunistically on the basis that the researcher knew one of the hospital managers and of her concerns around the need to improve hospital discharge for patients who were homeless. There was, therefore, interest on the part of the hospital trust in being part of the research. The site was also considered a good fit in terms of the wider portfolio of sites, as it was a mental health hospital (whereas trusts in other sites were acute) and also a hospital site serving a large rural area (whereas the other sites were mainly inner city). It was also recognised that this site could reflect the challenges of setting up specialist services in areas where there are few homeless patients. Another unusual feature of the site, in terms of poverty of MIRs (including non-specialist), was that it did not have a ‘generic’ complex discharge team. Here, ward staff were expected to take responsibility for all aspects of discharge planning.
The second standard care site was selected on the basis that it was a hospital site that had once had a specialist HHDS, but that scheme had recently been decommissioned. It was thought that this could shed light on the issue of sustainability and the ‘evaporation effect’. 86 Here, we were interested to explore what Dalkin et al. 32 term the ‘dimmer switch’ effect. In Pawson and Tilly’s27 seminal work, realist causation is explained by means of a gunpowder analogy in which a spark is introduced to the chemicals in gunpowder (mechanism), resulting in an explosion (outcome). However, if the conditions (context) are not right, for example if the gunpowder is damp, then there is no explosion. Here, mechanisms are seen as ‘triggering’ or ‘firing’ in context to achieve an outcome. However, Dalkin et al. 32 argue that where human volition is intertwined with an intervention, reasoning is rarely activated via a firing akin to an ‘on/off’ switch. Instead, they see activation as operating along a continuum similar to a light created by a dimmer switch where intensity varies in line with ever evolving context. Given the current austerity context, we recognised that this could be a particularly helpful heuristic for exploring the overall impact of the HHDF. We wanted to know if the different schemes were able to achieve a sustained ‘linear’ effect toward ‘good practice’ (safe discharge) or if ‘poor practice’ (unsafe discharge) crept back in once the MIRs were reduced or cut. Our hunch was that the latter may be the case, given that nationally delayed discharge figures could be seen to rise again once policy focus and resourcing shifted to other priorities.
Fieldwork
The fieldwork comprised non-participant observation in the everyday life of the HHDS (and/or hospital setting) and semistructured interviews with a range of stakeholders. Approximately 3 months was spent with each site, with the researcher spending 2 or 3 days on site each week. Non-participant observation encompassed shadowing workers and observations of assessments, case conferences, team meetings and other activities. Extensive fieldnotes were taken to record observational data.
Semistructured interviews with practitioners, managers and commissioners
In total, 77 semistructured interviews were carried out with a wide range of (non-service user) stakeholders (a minimum of 10 interviews per site) (see Appendix 2). Sampling was mainly purposeful (guided by the need to collect data to interrogate and refine programme theories), but ensured coverage of key staff groups in each site (e.g. HHDS managers and practitioners, discharge co-ordinators, ward staff, staff working on other local services and agencies, and service commissioners). Informed consent was ascertained for all participants. A topic guide (see Appendix 3) was used to gather information on a range of matters, including the history and current conceptualisation of the ‘problem’ of homeless people’s discharge from hospital in that particular site, understanding what changes/mechanisms (i.e. MIRs and KPPs) are being implemented, and perceptions about how they are working (i.e. leading to any changes in reasoning) and the associated outcomes. Key stakeholders (e.g. HHDS staff and managers) took part in a formal interview, but were then re-interviewed informally on many occasions as our programme theories evolved. Interviewing/recruitment stopped when it was felt that enough data were ascertained to have a comprehensive (rich) understanding of the programme theory under scrutiny. Interviews were digitally recorded and transcribed.
Interviews with homeless patients
Interviews were carried out with homeless patients (n = 70) at two time points, shortly after discharge and then again after 3 months. The timing of the second interview at 3 months gave sufficient time to reveal outcomes linked to continuity (e.g. what happened after step down ended), but not so far into the future as the connections with the initial hospital and discharge planning episode would be lost to memory.
Inclusion criteria (homeless patients)
In each site, we purposively recruited (≥ 10) homeless patients referred to either a HHDS or, in standard-care sites, to discharge co-ordinators/ward managers. Homeless patients (including HHDS service users) were recruited on the basis that they were ‘key informants’ with regard to different experiences of MEH. People experience MEH if they are ‘homeless’ (broadly defined to include temporary/unsuitable accommodation, as well as sleeping rough) and have also experienced one or more of the following domains of deep social exclusion: ‘institutional care’ (e.g. prison, local authority care, stays in mental health hospitals or wards), ‘substance misuse’ (e.g. drug problems, alcohol problems, abuse of solvents, glue or gas) or participation in street culture activities (e.g. begging, street drinking, ‘survival’ shop lifting or sex work). 5 Recruitment also aimed to monitor inclusion of the following groups/demographics and, whenever possible, we approached people in the order to which they referred to the service to avoid any selection bias:
-
young homeless people (aged 18–24 years)
-
people in the middle age range (aged 25–49 years)
-
older homeless people (aged ≥ 50 years).
Recruitment/ascertaining informed consent/incentivisation
Sensitive strategies were employed to successfully recruit respondents from this ‘hard-to-reach’ group. Prior to the researcher making contact, we asked the HHDS worker/discharge co-ordinator to give the prospective participant an invite letter and study information sheet and to seek their permission to tell the interviewers if they were interested in taking part. When the interviewers subsequently visited the hospital, patients who had expressed an interest were contacted. The researcher explained that (1) participation was voluntary and they could withdraw at any time or refuse to answer any question, (2) that they would be seen twice by a researcher over the following 3 months, (3) that their consent was needed to collect information from HHDS staff and from their medical records and (4) if they said something that indicated that they or someone else was at risk of harm, the interviewer would be obliged to take appropriate action. Written consent was obtained prior to the first interview, with verbal consent obtained prior to subsequent interview. Only participants who gave informed and written consent were recruited. Participants’ capacity to give informed consent was determined before each subsequent interview. It was planned that should a participant lose capacity during the following 3 months then they would be kept in the study and, in accordance with the Mental Capacity Act 2005,87 a nominated consultee would be involved. To build trust and rapport before the first interview, the researchers visited patients on the ward on several occasions in the run up to their discharge. Participants also received a £10 voucher (per interview) for sharing their expertise and giving-up their time.
In total, 70 patients were recruited at time point 1 (T1) and 35 patients at time point 2 (T2). Finding participants at T2 was time-consuming and challenging for many reasons (e.g. people moving between areas with no fixed abode and regularly changing mobile telephone numbers):
-
young homeless people (age 18–24 years) – T1 n = 5 male/n = 2 female; T2 n = 1 male
-
people in the middle age range (aged 25–49 years) – T1 n = 27 male/n = 2 female; T2 n = 13 male/ n = 7 female
-
older homeless people (aged ≥ 50 years) – T1 n = 20 male/n = 5 female; T2 n = 11 male/n = 3 female.
Topic guide
Interviews employed a semistructured topic guide (see Appendix 3) to unearth participants’ experiences of being admitted to hospital (i.e. the events leading up to the admission) and discharged from hospital and whether or not the HHDS (and the MIRs and KPPs therein) had the intended impact. The main focus of the second follow-up interview was on the following:
-
Patterns of service use in the intervening 3-month period, including any readmission to hospital. What support was received? Did the support materialise as planned? Did the support meet self-perceived needs?
-
What was liked and disliked about the support?
-
How was the support perceived to have helped? What outcomes were achieved? What outcomes were still aspired to and what additional support might have helped?
Interviews were digitally recorded and transcribed. We also gained participants’ written consent to access support plans and personal information held by a range of providers.
Patient and public involvement and engagement
Two ‘peer researchers’ (researchers with live experience of homelessness) accompanied us on some site visits and undertook a small number of interviews alongside the university researcher (e.g. one of the peer researchers was an ex-army veteran and so accompanied us on interviews where the patient was an ex-army veteran). Having peer researchers alongside helped establish trust and rapport with research participants and led to more targeted probing because of greater understanding (lived shared experiences) of the topics covered.
Some of the original study participants also became ‘peer researchers’ themselves (after the fieldwork had concluded), joining a special advisory group and contributing mainly to the dissemination stages (e.g. producing cases studies and attending high-level meetings and conferences to share first-hand experiences about issues such as discharge to the street). This was acknowledged by policy stakeholders as being very effective in bringing the academic findings to life and supporting a greater commitment to change.
Analysis
In realist evaluations, the analysis is retroductive. It involves ‘to-ing and fro-ing’ between theories and data to tease out what works, for whom, in what circumstances and why. More specifically, qualitative analysis moves beyond thematic categorisation to identify and explain the relationship between context, mechanism and outcome. Here, the aim is to describe the interaction between MIRs and context, and the change (if any) in reasoning this generates. To facilitate this, data from fieldnotes and interview transcripts were entered into a software package (NVivo 2, QSR International, Warrington, UK) and then coded and organised using the formula:
Mechanism intervention resources were subcoded by means of the tentative programme theory framework (protocol MIR1, patient in-reach MIR2, etc.) (see Box 3). Comprehensive context–mechanism–outcome descriptions were built for each of the seven fieldwork sites and comparative analysis undertaken across the full data set. Analysis was conducted specifically to ‘test’ linkages (e.g. changes in reasoning produce greater outcomes when MIR X in place/MIR X missing). Analysis was further disaggregated by subgroup (e.g. outcomes for practitioners/outcomes for service users). Finally, data were reviewed with regard to the overall utility of the programme theory, looking across the cases for confirmation, rebuttal and ‘silence’. Emerging findings about ‘what works and why’ were fed back to sites for scrutiny and further analysis by means of local meetings and/or feedback events (n = 7). This was intended to guard against ascertainment bias where evaluators focus on outcomes of which they have knowledge and will investigate these outcomes more thoroughly. The final stage of the analysis was iterative, showing how the qualitative data led to refinements in the initial tentative programme theory (see Box 3), before moving on to quantitative testing stages (see Chapters 4 and 5).
Results
Overview
The qualitative findings support our initial tentative programme theory about the importance of having all the ‘jigsaw pieces’ in place to deliver consistently safe, timely transfers of care. Our observations (based on 10 patient journeys per site) confirmed that consistently safer, timelier transfers of care were more likely to occur in site 2 compared with the other sites. Site 2 was purposefully selected on the basis that it came closest to NHSE&I’s description of a ‘complex adaptive system’. 20 This site had a fully integrated out-of-hospital care pathway that encompassed protocols (including those for early discharge planning) (MIR1), multidisciplinary patient in-reach (MIR2mdt), discharge co-ordination (MIR3mdt) and a residential step-down intermediate care facility (MIR4res). Patients (accepted for the ‘step-down’ service) were collected by taxi and taken straight to the facility. Here, hospital discharge was a ‘non-event’ and there were no reports of poor or unsafe discharge. Furthermore, the out-of-hospital care pathway itself was embedded as part of a wider whole system of care. This matched the description for the highest level of integration as defined by the DHSC’s Office of the Chief Analyst:
Fully coordinated primary and secondary care that provides an integrated service, including specialist primary care, outreach services, intermediate care beds, and in-reach service to acute beds.
p. 18. 88
In the remainder of this section, we describe in more detail how MIRs and KPPs are integrated into the specialist out-of-hospital care pathway in site 2 and how this works to deliver good outcomes for (some) patients. We then draw on observational and interview data from the other fieldwork sites to pinpoint how ‘gaps’ (i.e. missing jigsaw pieces) lead to poorer outcomes. We also consider, across all the sites, the factors that dampen effects, leading MIRs and KPPs to fail to deliver their intended outcomes. In Chapters 4 and 5 we then interrogate these qualitative findings by means of a quantitative lens, mindful of the limitations inherent in a case study approach.
Specialist care: ‘all the jigsaw pieces’
Site 2 contained two specialist HHDSs that work in partnership to create an out-of-hospital care pathway for patients who are homeless and who have a physical health need. A multidisciplinary (clinically led) homeless team was based at the hospital with a 14-bed (housing-led) residential step-down respite and intermediate care facility in the community.
Clinically led multidisciplinary hospital-based homeless team
In site 2, the homeless team was clinically led, comprising a manager (a band 7 nurse), a nurse, a housing worker and a care navigator, with sessional support provided by a GP and a mental health nurse. The homeless team manager was employed by the acute trust and the other clinical staff by a specialist primary care practice (holding overall management responsibility for the team). The housing workers were seconded to the team from a housing association that also managed and ran the step-down facility. The homeless team was originally co-located in the same offices as the (generic) complex discharge team, but at the time of data collection occupied its own office space. The two discharge teams complemented each other, with the homeless team taking on full responsibility for the discharge of patients who are homeless and other patients with housing problems. The manager of the generic discharge team had performance oversight of the homeless team with regard to monitoring and addressing any DToCs. The homeless team operated extended working hours on some evenings, but there was pressure for more flexible working and for the service to operate 24/7 should funding allow.
In site 2, the homeless team acted as the named point of contact for patients who were homeless, usually taking on responsibility for all aspects of their discharge planning (MIR3). Just as social workers provided detailed specialist knowledge of the Care Act 201489 and other legislation and the local care market, the homeless team provided expertise on housing legislation and local homeless service provision. The housing workers in the homeless health team also took responsibility for the considerable administrative burden that can be associated with making an approach to housing or maximising income (e.g. sorting out access to benefits or helping people ascertain identification proof or to establish a local connection). As the homeless team was co-located at the hospital (avoiding the need for ward staff to make external referrals and wait for a response), they were highly appreciated by ward staff and credited by hospital managers with playing a vital role in maintaining patient flow and reducing delays. This point was mirrored across nearly all the research sites that had HHDS:
Before we had a homeless team, homeless patients were referred to the social work team, but the social work team would say its housing not care and signpost them to outside . . . Now that we have a [homeless worker based at the hospital] it’s a massive bonus for the trust, someone we can turn to, specialising in homelessness and who knows the processes, policies, laws, benefits and everything that comes with that than an everyday nurse wouldn’t be able to deal with . . . It’s a massive bonus.
Ward manager, S3b
In addition to discharge co-ordination, clinically led homeless teams also undertook patient in-reach (MIR2mdt), with the overall aim of building relationships with patients and maximising the benefits of a hospital stay. This included preventing early self-discharge and increasing access to planned health care:
We see ourselves more as a homeless health team rather than just a discharge team . . . We work with homeless patients at the level they’re at – optimising their stay – making sure that they’ve had their jabs, that they been seen by the substance misuse services even though they’ve come in for a broken arm; that they have a sexual health screening if the need that; that they get the things done that the homeless nurses in the community have been trying to get them have done for ages, for example, a particular set of bloods. This might not be indicated in terms of why they’ve come in with, but it’s about maximising the stay and following this up with outpatient appointments.
Homeless health care team nurse, S1
Residential step-down intermediate care (MIR4res)
In site 2, HHDF capital funding had been secured to refurbish a former student hall of residence into a 14-bed dedicated residential intermediate care step-down facility. The Respite and Intermediate Care Support Service (RICSS) was ‘housing led’ and managed by a housing association. It was staffed 24/7, with housing/resettlement workers during the daytime and security staff at night. Revenue funding was mainly sourced in the same way as for other hostels in the district (e.g. from housing benefit), but the facility is only accessible to people who are homeless and assessed as needing intermediate care on the basis of physical health need. Additional funding for RICSS was also provided through the BCF and used to pay the support staff and manager who are on duty every day of the week. Without this additional funding, the service was not thought to be viable.
Seen from the perspective of the patient, the journey into RICSS starts in the hospital and is facilitated by the homeless team. The homeless team start to assess and work with patients while they are in hospital and will continue to work with them (‘boundary span’) when they move into RICSS. Importantly, the homeless team has direct referral rights into RICSS and the team’s nurse and GP are ‘trusted assessors’ (MIR5), meaning that RICSS staff will accept their assessments and judgements about a patient’s suitability for the service. Therefore, when medically optimised, people move seamlessly from hospital into RICSS, such that hospital discharge is an ‘uneventful’ event (a short taxi ride). The homeless team’s GP and nurse undertake a weekly ‘ward round’ at RICSS (reviewing the care of each resident) and work flexibly to be on hand to provide housing staff with advice and back-up on health matters. For patients, trusted assessment (MIR5) facilitates integration (KPP3), leading to a high degree of continuity (KPP4), in which ‘I only have to tell my story once’.
Once settled into RICSS, a fully integrated assessment commences of the patient’s health, housing and social care needs. Importantly, admission to RICSS enables clinical staff from the homeless team and RICSS housing staff to work together to observe needs over time and ascertain a fuller picture, rather than relying on a verbal snapshot at the point of discharge. These ‘snapshots’ can be unreliable given that people are ‘never themselves’ when in hospital and in crises or unwell. This opportunity for comprehensiveness is at the heart of intermediate care based on a D2A model. Below we describe how KPPs are embedded in intermediate care in site 2.
Key practice principle 1: location – convalescent atmosphere
Staff at RICSS work hard to ensure a quiet convalescent atmosphere at all times. One resident captured the success of this approach as follows:
Prior to going into hospital, I was living in a homeless hostel. It was noisy, doors slamming all night long and there were stairs I couldn’t manage . . . This place is completely quieter, nicer, there’s medical care and it’s just lovely.
Tom, aged 64 years, RICCS resident
Key practice principle 2: reablement
Key practice principle 2, reablement, is a time-limited person-centred intervention that aims to restore self-care and daily living skills, and to support access to, or reconnection with, the local community and social and leisure activities. Support for physical reablement (e.g. helping people re-establish ‘activities of daily living’ such as washing and dressing) is, however, perceived to fall outside the skill set of the RICSS housing support worker role and as requiring referral into the support provided by (adult social care) reablement teams. Accessing adult social care was particularly challenging for workers across all the HHDSs involved in the study, and often required strong and persistent advocacy with good legal literacy. This boundary was successfully negotiated for some RICSS residents who received a Care Act 201489 assessment and, subsequently, 6 weeks of ‘free’ reablement, with reablement workers visiting the RICSS facility each day (KPP3). If longer-term care and support are needed, this will be assessed at 6 weeks, with plans put in place for a move to sheltered housing or a care home. Patients with palliative care needs can remain at RICSS if that is their wish (KPP1).
Key practice principle 2: self-management
Time in RICSS enables staff to support people towards improved ‘self-management’ (e.g. to better manage conditions such as diabetes through healthier diet and understanding of medication regimes). This can also encompass support for managing addictions, for example encouragement for residents to reduce their alcohol consumption.
Mechanism intervention resource 1: early discharge planning (with/without key practice principle 2: resettlement)
Plans for ‘move on’ (rehousing) commence at the point of entry to RICSS. Its staff are ‘housing workers’ employed by a Housing Association and are skilled resettlement workers. Resettlement involves supporting people to find and establish a home, maximise their income, maintain a habitable home environment and to (re-)establish independent living skills. Resettlement is a close cousin of reablement, but tends to focus more on inclusion outcomes, such as preventing social isolation and supporting people to take part in education, employment and other community activities.
Key practice principle 4: continuity – link work
An important aspect of the inclusion work undertaken by RICSS housing staff is to support people to register with a GP and to manage any outpatient appointments. Workers keep a central database of all appointments and will accompany people to them. In effect, this further maximises the benefits of the hospital stay by providing the practical ‘link work’ needed to ensure continuity of access to health care in the community.
Key practice principle 1: engagement and choice (person-centred care)
Enabling people to have some ‘breathing space’ between hospital and (finding a new) home is key to opening up opportunities for person-centred care and increased choice and control. At RICSS, people have time to build trusting relationships with staff and are fully involved in all decisions, including those about where they want to live. Staff accompany residents to view properties and will help them set up a home.
Key practice principle 4: continuity
People will not be discharged from RICSS until they are happy about where they will be living and about their ongoing care arrangements. Once a patient leaves the RICSS facility, continuity is maintained through monthly multidisciplinary meetings convened by the homeless team. This brings together the ‘multiple and complex needs community’ (i.e. practitioners from across health, homelessness and criminal justice services). According to staff in the homeless team, this affords an opportunity to review cases of concern and prevent any subsequent crises, potentially reducing subsequent hospital admissions and A&E usage.
Key practice principle 3: integration
For RICSS residents, the integration of these different elements meant that the ‘holy grail’ of a single integrated care plan was often achieved, with health, housing and social care professionals all co-ordinating their work toward the achievement of a common set of outcomes (see Appendix 4 for a case study).
What binds a complex adaptive system?
Strategic factors
Importantly, both these specialist HHDSs were connected not only to each other but also to a much wider housing, care and support network. It is this wider network that seemed key to ensuring ‘patient flow’ both through the hospital and the intermediate care facility. Protocols (MIR1) and, more importantly, their active nurturing appeared to be the scaffolding of these networks and wider systems. In England, the HRA10 (implemented from April 2018) placed a new statutory ‘duty to refer’ on hospitals (including A&E departments) and other public bodies to notify the local housing authority where a patient is homeless or threatened with homelessness.
Under the HRA, the duty to refer can be discharged by sending an e-mail notification. There is no set timescale for the housing authority to complete its assessment on receipt of a referral notice and nothing to prevent hospitals from discharging a patient before an assessment is complete. In site 2, prior to the implementation of the HRA, local system partners had already put in place a set of protocols for joint working as part of a locally agreed ‘homeless hospital discharge protocol’. In this site, it was agreed that the housing authority would undertake an assessment within 72 hours of receiving a referral (a so-called ‘bed-blocking’ form) from the hospital. If problems arose, these were actively addressed by housing/hospital managers and great effort went into keeping the protocol live. As a result, it was rare for patients to be discharged to the housing authority unannounced. Appointment times and workflow challenges within this housing authority were respected, as were those in the hospital. In other sites, without well-nurtured protocols, we found that appointments for a housing assessment could be fixed 3 or 4 weeks ahead, with the consequence that ward staff would ignore them and ‘signpost’ the person to the housing authority unannounced. Discharging patients to the housing authority in an unplanned way, rather than delaying the discharge, had the knock-on effect of rendering any ‘pinch points’ invisible and, therefore, perpetuating underlying ‘patient flow’ issues and poorer outcomes for patients who were being discharged unsafely.
Relational factors
As noted above, a specialist primary care practice held management responsibility for the hospital-based homeless team in site 2. Staff from the homeless team worked flexibly and provided sessional input into other local inclusion health services provided by the specialist primary care practice (e.g. the mobile outreach service for sex workers). This made for a strong community of practice, in that workers got to know patients over time and other workers, including what was going on in related services across the city. This detailed knowledge of ‘other’ services and strong relationships with staff therein (e.g. in terms of negotiating any access criteria) is also recognised as assisting patient flow. In site 2, it was acknowledged by stakeholders that the practice manager of the specialist primary care practice had been central to engineering this complex adaptive system along with progressive leadership of the commissioners at the local authority who held BCF and other responsibilities. This suggests that strong and progressive leadership (MIR6) that nurtures both the strategic and relational dimensions of a complex adaptive system may be a key additional mechanism in embedding high-impact change.
Seen from the perspective of the patient, Box 4 illustrates how the out-of-hospital care pathway in site 2 worked to deliver a range of positive outcomes that were linked to the safe, timely transfer of care from both the acute and intermediate care sectors.
RICSS is a hostel. I did have some initial concerns about staying in a hostel, but staff worked hard to maintain a peaceful environment and reminded residents constantly that this a place for convalescence and for people who were not well. I had my own room, bathroom and cooking facilities with the use of a laundry. I was provided with bedding, towels, toiletries and cooking utensils and a microwave. I felt that my stay there, apart from very possibly saving my life, was an extremely beneficial halfway house to helping me begin to re-construct my life [outcome = improvement in overall health and well-being]. During my stay, I had access to a nurse and a GP who were attached to the hospital. They visited every Thursday to undertake a ‘ward round’ (or visited whenever anyone needed medical attention). On their advice, I had a further 6 nights in hospital due to pseudo-gout in one of my knees which was excruciatingly painful and required aspirating [outcome = improved access to planned health care]. I was on bed rest for 6 days . . . I often wonder what would have happened to me if I had not been able to stay at RICSS. The staff gave me social support, helped me to apply for Personal Independent Payment and took me shopping for a bed and a chair for my new flat. I couldn’t have done that on my own [outcome = successful resettlement]. A member of staff also physically helped me move into my flat once it became available. They gave me all the bedding and kitchen utensils from my room at RICSS. This was marvellous as I had very little income and was worried as to how I would pay my bills for the flat with enough left over for food. On the same day that I moved into my new flat, the RICSS worker took me to register at the local doctor’s surgery [outcome = access to preventative health care]. My feet continued to be gangrenous and I continued to need the service of the district nurses. This was arranged without problem.
Jenny, aged 59 years, RICSS former resident
Does this out-of-hospital care pathway work for everyone?
As noted above, RICSS staff worked hard to create a peaceful convalescent atmosphere. However, one consequence of this is that people with active addictions or loud, disruptive and challenging behaviour were perceived to be less suitable for the service. Rather than actively exclude this group, the aim was to have a balance of residents with different needs. Even so, having a ‘physical health need’ (as a determinant of eligibility) seemed to align more closely with physical disabilities and non-addiction-related conditions. For example, a man whose primary need was considered to be related to his heroin addiction was considered unsuitable for RICSS, despite being homeless and having a physical health need arising from a groin abscess. He returned to rough sleeping on discharge. A limitation of our case study approach is that in this site we focused on the RICSS pathway and not on hospital discharge more generally.
What dampens the effect of the mechanism intervention resources embedded in this out-of-hospital care pathway?
In site 2, although there had been budget cuts, the perception of the homeless team and RICSS staff was that there was still a good range of accommodation and support services. As compared with the other fieldwork sites, we observed that there appeared to be much more scope for specialist discharge co-ordination (MIR3mdt) and D2A to function as intended. Patients also seemed to have much more scope to exercise choice and control (KPP1). Indeed, for RICSS staff, a particular challenge was how to manage choice (KPP1) where people may have reached their goals as regards their physical health, but where they are waiting solely for the right property or post code (locality) to become available. It is anticipated that the usual length of stay at RICSS should be around 3 months. However, it was often the case that people stayed much longer (sometimes for up to a year), leading to ‘bed blocking’. It was recognised by RICSS senior managers that it was important to strengthen protocols for patient flow (MIR1) by placing reasonable limits on how choice was exercised.
In addition to ‘patient exercising choice’, the other main cause of delayed discharge from RICSS was the shortage of suitable long-term care and support services, especially for people aged < 55 years who needed adult social care or sheltered housing. Again, this could cause long delays and there was awareness of the danger that that intermediate care could start to substitute for long-term care. Indeed, in sites without intermediate care, commissioners often expressed the view that the main reason why they had not commissioned this service was because of fears that it would become quickly ‘silted up’.
There was also a recognised unmet need for some RICSS residents to have a further period of Home First ‘step-down’ care in the form of floating support in the community (MIR4hf) once they had moved into a new home of their own. To compensate for this, RICSS workers kept hold of some patients for perhaps longer than necessary and then held ‘secret caseloads’ of former residents whom they kept an eye on until they knew longer-term community services and (relationships) were in place and working well (KPP4).
Learning from site 2 for programme theory refinement
In the literature review, we found less clear evidence for MIRs linked to trusted assessment (MIR5). However, in site 2, there was strong evidence that this mechanism is crucial to the delivery of good outcomes and patient experience. The importance of MIR5 becomes even more apparent when evidence is considered from site 1 where it was missing. Site 1 had a ‘clinically led’ homeless team but no direct access to step-down intermediate care (MIR4-missing). Although a small number of residential intermediate care beds were available locally, these were earmarked for ‘step-up’ care (preventing admission to hospital and rarely available for step-down care). Furthermore, there is no protocol (MIR1) in place for trusted assessment (MIR5). As a result, patients referred to the intermediate care service were discharged from the acute sector and reassessed by the intermediate care team on presentation. In site 1, patients had to tell their story more than once. In addition, if the intermediate care bed was not available on the day of discharge as planned then this could leave them in limbo, having been discharged from hospital without an agreed discharge/support plan in place (Box 5).
Mark (anonymised) is aged 42 years and a ‘verified rough sleeper’ who is well known to the street outreach team. He was severely alcohol dependent and admitted to hospital following a suicide attempt, where he spent 10 days on the A&E admissions ward. Mark described feeling very low and depressed and how he knew he was going to die on the streets unless he got help. He underwent a detox while in hospital and was very impressed by the amount of support that was offered. He had several visits from the homeless team whom he described as very good. At the point of discharge, he described feeling really positive about the future for the first time in a long time. The plan was for discharge to an intermediate care bed. On the day of discharge, Mark was sent by taxi to a specialist primary care practice where the assessment for the intermediate care bed would take place. However, the bed that had been allocated for Mark was no longer available because the previous occupant had trashed the room. Mark could not return to hospital (as his bed was closed) and was found emergency accommodation in a wet hostel [i.e. a hostel permitting alcohol, which he had previous experience of and which he thought was totally unsuitable for him (KPP1-missing)]. He was evicted that evening because of his starting to drink again and assaulting a member of staff. (Outcome = Mark returned to rough sleeping within 24 hours of discharge.) The following day, Mark was found by one of the researchers lying unconscious on the pavement. He had returned to heavy drinking and was very angry that the discharge plan had not materialised and that no one had come to find him. He had telephoned the HHDS multiple times that day and had verbally abused his worker on the telephone. He felt that he had been abandoned by the hospital, despite all the promises that had been made.
Standard care: ‘no jigsaw pieces’
Without access to a HHDS, discharge co-ordinators and ward staff in standard care sites stated that they found it challenging to deliver consistently safe, timely transfers of care for their homeless patients. The most commonly reported difficulties were navigating complex rules and systems and understanding what resources and services were available for homeless people locally. They felt that there was too little time to complete the administrative work associated with supporting a housing application (e.g. helping someone to ascertain proof of identity or local connection) and also too much pressure on beds, which meant that people could not wait in hospital while housing was arranged.
In site 6 (standard care), it was not uncommon for patients to be given very short notice to leave the ward, hours in some cases, before being ‘signposted’ to the local council homeless office. This was highly distressing for patients and often led to angry and open confrontations on the ward. In one case, the patient had not disclosed domestic violence and was too afraid to go into the city centre. In this site, the relationship between the hospital and the local council housing/homeless department was underdeveloped. A consultant from the hospital was a member of the local homeless strategy group, but had been too busy to attend meetings. Meanwhile, the local housing officers were frustrated that patients were presenting as homeless with no prior warning, but did not know whom to approach inside the hospital to address this. A homeless hospital discharge protocol (MIR1) had been developed by the local council, but had been stuck somewhere in the hospital governance system for over 2 years.
Following a research interview with the homeless officer in site 6 (standard care), the details of the ward manager were passed on and a meeting was set-up. Once this meeting occurred, discharges were quickly transformed. The housing officer agreed to spend time on the ward each week to assist with discharge planning, along with a worker from a local voluntary agency who helped patients fill out forms to access support services. In this city, serving a large rural area, there was good availability of hostel places and temporary accommodation (for those not wanting to go into a hostel) plus intensive support for 6 weeks to organise benefits and move on. Therefore, this standard care site was able to start delivering safe and timely transfers of care without a specialist HHDS. However, having an informal arrangement [without a dedicated resource or protocol (MIR1-missing)] led to a lack of consistency. Should the housing officer be off sick or go on holiday, for example, the outcome was often a DToC or unsafe discharge. Therefore, the perception of ward staff in this site (as was the case in all case study sites) was that having a dedicated specialist resource to in-reach into the hospital and co-ordinate housing and homelessness arrangements (MIR2 + MIR3) was essential to more efficient and consistent patient flow.
This qualitative finding is supported by evidence gathered as part of the documentary analysis. NHSE&I statistics show that the two standard-care sites that did not have access to a HHDS had a higher rate of DToC linked to housing (category I) than the other fieldwork sites (Figure 2).
FIGURE 2.
Number of patients with a DToC due to housing (category I). The data are taken from NHS England monthly situation reports90 (2012 to March 2017). It reports the number of patients delayed on the last Thursday of the month. These data were no longer collected after April 2017. From April 2017, the reported data were the total delayed days during the month for all patients delayed throughout the month. Data are shown at provider organisation level from NHS trusts, NHS foundation trusts and primary care trusts. The six trusts with HHDS include an additional pilot site not included in the main fieldwork. The way in which DToCs are counted and recorded in England was changed again in 2020,91 with the introduction of a new category ‘Homeless/no right of recourse to public funds/no place to discharge to.’ Contains information licensed under the Open Government Licence v3.0.
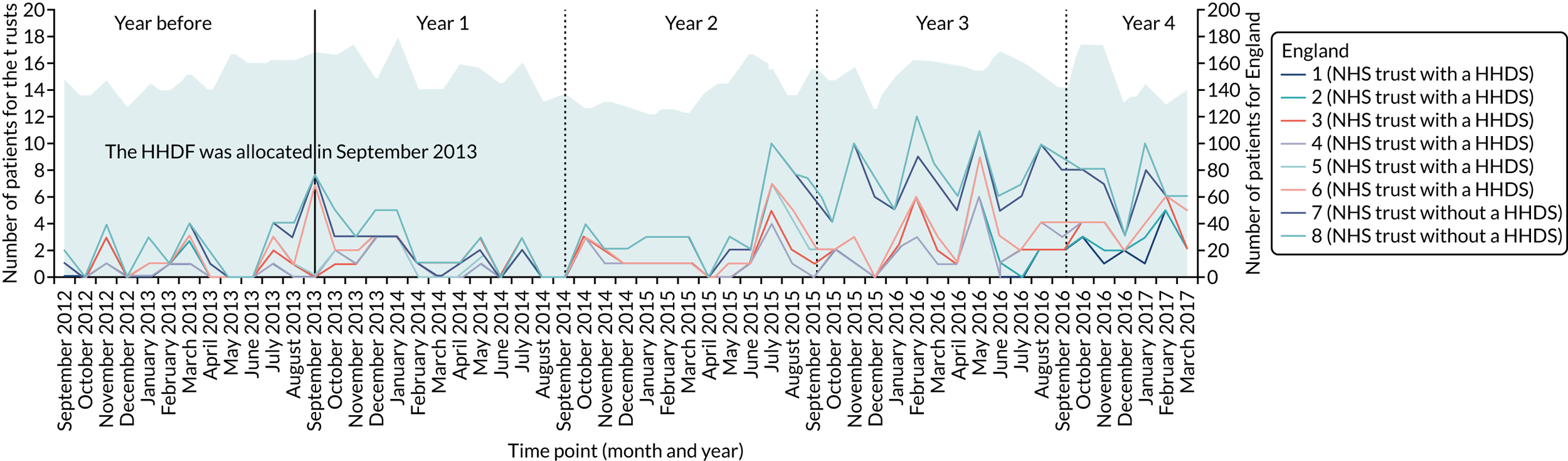
Evaporation effect
In site 5, a standard-care site that had lost its specialist HHDS because of funding cuts, it was reported that the relationships that had been built up between voluntary workers and hospital staff sustained benefits for a time, but gradually suffered the dimmer switch effect, as voluntary workers were pulled onto new contracts. In this site, it is interesting that, once the specialist HHDS had ceased to operate, the management of discharges for patients who were homeless increasingly fell to the alcohol liaison team. This can be seen as a reflection of not only the level of specialist expertise within the alcohol liaison team around housing and homelessness, but also the extent to which the alcohol liaison service was able to link more directly (and easily) into community services and resources. Concerns were expressed, however, that the ‘specialist’ alcohol service might not be able to continue to bridge this gap without undermining its own effectiveness and long-term sustainability.
In several sites, the underpinning programme logic was that HHDSs would be time-limited interventions designed to educate and up-skill hospital staff about working with homelessness patients. However, the consensus among stakeholders was that because of high staff turnover in hospitals, the impact of the HHDS is rarely sustained once a scheme has ended.
Missing jigsaw pieces
In this section, we provide more illustrative examples to demonstrate how missing ‘jigsaw pieces’ limit the effectiveness of HHDS to deliver intended outcomes.
Example 1: out-of-hospital care pathway with Home First (MIR4hf) but no residential step-down acre (MIR4res-missing)
In England, Home First (MIR4hf) is the default pathway for all patients leaving hospital and is based on the belief that people will recover best in their own home (KPP1). However, if patients are homeless and they do not have a home or somewhere safe to stay, then the Home First model is compromised. This was evident from our observations in site 3a. This site had a ‘housing-led’ HHDS (with a single member of staff) offering patient in-reach and discharge co-ordination (MIR2/3up) with time-limited floating support post discharge (MIR4hf). This scheme had no direct access to a specialist residential step-down unit (MIR4-res missing) or any other units of specially earmarked accommodation. As illustrated in Box 6, where patients are being discharged to bed and breakfasts or other unsuitable accommodation, this makes for poorer patient experience and almost certainly has a negative impact on the health outcomes that are achieved (e.g. speed of recovery after surgery). Nevertheless, a caveat here is that having a HHDS link worker to help advocate and negotiate the hardship of unsafe discharge is hugely appreciated by the patient and may go some way to negating some of the impacts of this.
Fred (anonymised) was in hospital for nearly 3 months and had nine operations linked to a heart condition. He had recently lost his home because of tenancy problems. While in hospital, Fred described how once his legs started to get better, social workers, housing officials and the ward manager all started ‘kicking in’. He was also referred to the HHDS in the hospital, which was a ‘housing-led’ (floating support) step-down scheme (with no attached accommodation).
When it came to discharge planning, Fred described himself as:
Getting stuck in a big battle . . . I nearly got evicted [from the hospital to the street]. They said ‘right you’re medically ready to be discharged’. [My HHDS worker] was there [arguing my case] . . . He got onto the Council and the Council sorted me out for that night in the Premier Inn of all places.
Having spent 2 nights in the Premier Inn, Fred was then sent to another B&B in a seaside resort. The second B&B was up a big hill and a way out of town. This caused numerous problems for the management of his health conditions (outcome = negative impact on health and well-being). Fred was told by his consultant that he must rest and ‘do very little for the next 6 weeks’. However, to get his leg dressings changed he had to walk (in his slippers) down the hill to the local NHS walk-in centre:
I did so much walking, I’m surprised my heart didn’t give out and that I didn’t have another heart attack.
Although the B&B provided breakfast, Fred also struggled to eat at other meal times because of the distance to the town centre and lack of cooking facilities. Fred was placed in the seaside B&B for the weekend before being moved into a hostel and then back into B&B accommodation (outcome = failure to meet basic care needs, e.g. nutrition).
It was over 1 year before Fred was provided with somewhere he could call home. During this time, he had a succession of different key workers as he moved between hostels and B&B accommodation (outcome = fragmented care). During this time, he relied heavily on his HHDS worker to chase things up, for example if a housing application was started but not followed up. Although the HHDS worker could not ‘magic-up’ a solution to Fred’s housing crises, his continuous support and kindness made an enormous difference to him:
He’s done a lot for me . . . I’ve had really bad days and he’s seen me when I’ve been in complete agony crying my eyes out because I haven’t got anywhere [with the housing] and I can’t do anything with my legs . . . It’s just having somebody I can banter with, I know it sounds stupid, because sometimes we don’t talk about the housing, we talk about everything else.
B&B, bed and breakfast.
In site 3b, which had a similar housing-led scheme to site 3a, the Clinical Commissioning Group commissioned a number of ‘health beds’ in a local homeless hostel that were then earmarked for use by people leaving hospital. However, the ‘health beds’ did not come with any additional support other than that usually provided in the hostel, which meant that this could place an extra burden on staff in terms of having to manage the more complex health and care needs of residents who had recently left hospital. Furthermore, the ‘health beds’ were not always occupied by people recently discharged from hospital, which resulted in knock-on effects for patient flow out of the hospital.
Example 2: uniprofessional homeless hospital discharge scheme with no clinically led patient in-reach (MIR2mdt-missing)
Link workers in ‘housing-led’ HHDSs play a vital role in supporting homeless patients while they are in hospital. This support is concerned with engagement and relationship building and also ensuring that patients have toiletries and other essentials, especially clean clothes, and, therefore, addresses factors that can lead to stigmatisation. However, in site 3b, a housing-led scheme with no primary care in-reach (MIR2mdt), early self-discharge due to poor methadone prescribing was recognised as a significant problem at the hospital. Hostel staff in this site also spoke of their difficulty of getting residents to go into hospital (site 3b) and to stay there. This was because they could not guarantee that the hospital would prescribe methadone. Hostel staff described the consequences of this as being left with very ‘poorly residents’ who were at risk of worsening health conditions, which was distressing for staff.
Example 3: multidisciplinary homeless hospital discharge scheme with no access to step-down care – Home First (floating support) (MIR4hf-missing and KPP4-missing)
It is common practice for (generic) hospital discharge teams and discharge co-ordinators to close cases at the point at which the patient leaves the acute sector. Most of the clinically led HHDSs also managed their caseload in this way, with some limited outpatient follow-up (i.e. where a housing application has been started). However, for many homeless patients this unsupported transition out of hospital can be problematic (Box 7). Indeed, although charities such as the British Red Cross (London, UK) provide a vital service for older patients (e.g. turning their heating on and putting milk in the fridge), a much enhanced logistical and intensive support service may be required for patients who are homeless. For example, in addition to the logistical challenges that go with trying to ‘move house’ from a hospital bed (often by means of patient transport), patients may also need to organise a methadone prescription on the day of discharge and may be given a strict time slot when they can present for this. If this element of the discharge plan goes wrong, then the huge health and well-being benefits of a hospital stay (i.e. rest, care, kindness, treatment, emotional support, good food, detox for alcohol and getting off heroin and onto methadone) can evaporate in an instant. Similarly, sending someone to a cold, empty, depressing flat, alone, late in the evening and with no belongings (because of patient transport rules or lack of money) is a recipe for disaster that can quickly lead back to rough sleeping. These problems were much less likely to occur where the patient had a link worker to accompany them on the day of discharge and to help with all aspects of resettlement, including making sure community services were in place and working well (KPP4).
Dave spent 12 weeks in hospital for a serious infection. On discharge, Dave was to be relocated to a supported housing project many miles from the hospital. He was taken by patient transport to the town where he was moving to. With all his worldly possessions in tow, his first task was to collect a methadone prescription, as instructed by the homeless team. On arrival at the drug service, he was told that they had not been expecting him. Had he not been able to advocate for himself that this would have jeopardised the huge steps toward recovery that he had made while in hospital, as the only alternative would have been to use street heroin to avoid experiencing highly unpleasant withdrawal symptoms. The ‘move-in’ day was further complicated, as the supported housing provider assumed that patient transport would wait for Dave while he was at the drug service, transporting him and his belongings to the new property. As this was not the case, Dave was left stranded in town. Having made his way to the new property, Dave was then upset by the fact that the project worker was unfriendly and seemingly only interested in extracting money from him for the upfront payment of his service charge. This would have left him without any money for basic necessities. In the weeks that followed, very little practical support materialised from the supported housing provider. There was no support to get registered with a GP and no attempt to put in place a ‘recovery care plan’. Was it not for Dave’s own resilience and very high levels of motivation, the benefits gained through the hospital stay could easily have been lost.
Example 4: residential intermediate care facility with no resource for patient in-reach and multidisciplinary discharge co-ordination (MIR2/3-missing)
Site 4 contained a three-bed respite/intermediate care facility housed within a self-contained wing of a hostel. The scheme did not include any resource for the worker to ‘in-reach’ (MIR2/3-missing) into the hospital other than when a referral was received to undertake an assessment. After a few months, the scheme closed because of lack of referrals, reflecting the importance of HHDSs maintaining networks and a high-profile ‘face-to-face’ presence in the hospital to ensure that ward staff know what services are available ‘out’ in the community. In summary, although residential intermediate care (MIR4res) is key to safe, timely transfers for patients who have nowhere safe to stay on discharge, it will not work effectively or be sustainable if it is not linked to other MIRs.
What dampens the effects of specialist care?
There are three key contextual factors that can dampen the effect of the MIRs and KPPs in out-of-hospital care: (1) a lack of adequate funding for the HHDS itself; (2) situations where housing and wider community support services are poorly resourced, inadequate or lacking; and (3) circumstances where stigma and cultural distance persist. Where these factors have an impact on a HHDS, the outcome can be ‘poor practice’ (e.g. discharge to the street).
Lack of adequate funding for the homeless hospital discharge scheme
Over the lifetime of the study, we tracked the funding history of the 52 HHDF schemes. Once the HHDF ‘pilot funding’ ended, most (if not all) of the 52 schemes struggled to secure recurrent funding, regardless of any consideration of evidence for effectiveness or cost-effectiveness. Of the 52 schemes funded through the HHDF, 25 had ceased to operate by 2017. Where schemes have continued to operate, the trend has been toward a gradual shrinkage in capacity and geographical reach over time. In some areas, this has had a significant impact on ‘intervention fidelity’, meaning that schemes cannot put into practice what is known to be warranted and effective.
In site 1, the HHDS was a clinically led homeless team with no direct access to step-down care. Within the team, there was a significant gap between workforce capacity and demand. In sites 1 and 2, the HHDSs had similar staffing levels, but site 1 had twice the caseload of site 2 and, arguably, a much more complex caseload, comprising mainly of people who were rough sleeping and often with no clear local connection. This mismatch led to a range of problems, including recruitment and retention difficulties (low team morale) and, ultimately, poor scheme fidelity. High and complex caseloads and insufficient staff led to an increasing focus on ‘patient flow’ (discharge co-ordination) at the expense of other aspects of the service, such as engagement and relationship building (patient in-reach). Here, patients described themselves as having only brief contact with the homeless team. User feedback was generally much less positive than for the other sites. Seen from the perspective of a member of the homeless team:
At times our caseload feels really, really high and difficult to manage and at that point we do have to prioritise people who are going to be leaving within the next couple of days. When things feel a bit more settled we’re able to do more of the inclusive, holistic work.
Homeless team nurse, S1
Lack of housing and community services
In site 1, there was an acute shortage of housing and care and support services. Hostel places were in short supply and some hostels had no support attached, only concierge services. Outreach and floating support services were also in short supply. Where patients were identified has having no ‘local connection’ to an area or no recourse to public funds, they were perceived by the homeless team and ward staff to have few options other than discharge to the street. Wendy (anonymised) had been homeless in the city for 4 years and attended the hospital frequently to get some respite from the street:
I used to go to hospital, I won’t lie to you just to get my head down . . . I wasn’t used to being on the street, sleeping rough it was hard for me . . . When the nurses knew I was homeless they’d throw me out at 3 or 4 [o’clock] in the morning. I used to feel terrible having to go back to the street again . . . It’s only in the past year [the homeless team] started getting me into hostels . . . I’ve been here 4 years. Before that they couldn’t help me.
Wendy, patient, S1
Staff in the homeless team described how the local authority’s housing options team would often make patients identified as being in priority need a ‘single-service offer’ and would then discharge their duty if the patient refused that offer. As a result of very few options being available, there was much reduced scope for discharge co-ordination centred on supporting patients to exercise choice and control over the place of care and the timing of transition to it (MIR2 and KPP1-missing). This lack of choice and control led some patients to return to the street quite quickly after discharge. This happened most commonly where, for example, patients who wanted to ‘get dry’ were offered a place in a ‘wet hostel’ or where patients were offered accommodation many miles from the areas with which they are familiar.
Being discharged to the street is a highly distressing experience. This is especially the case for patients who have been in hospital for a sufficiently lengthy period of time to have undergone a ‘detox’ and to have perceived themselves to have ‘turned the corner’ with regard to substance misuse. Returning to the street at this point was associated with much anger and frustration, and often a sense of despair and loss of hope that things could ever change.
For primary care staff, having to deal with patients presenting in crises due to an unsafe discharge is exceptionally frustrating and highly disruptive to their day-to-day practices. ‘Passing the buck’ in this way was perceived to add more pressures to an already overstretched specialist primary care service and was not conducive to collaborative working between community and hospital staff (KPP3-missing).
Stigma and cultural distance
Where it was perceived that the patient is ‘clinically optimised’ and that all options had been exhausted, then it remained (tacitly) accepted practice across all the sites to discharge patients who are homeless to the street. How hospitals and HHDSs mediate the right to remain in a hospital bed as a DToC varied from site to site. In site 3a, for example, one patient described how his HHDS worker was ‘right up in the face of the ward manager arguing my case that I shouldn’t be discharged to the street’. In site 1, there was resigned acceptance from staff that, for some patients, the lack of appropriate accommodation and community services means that discharge to the street was unavoidable. Here, the homeless team were fearful of taking on too many ‘battles’ because certain wards and consultants were known to be less tolerant of housing-/homeless-related delays. The concern was that if the HHDS started to delay discharges then they would stop receiving referrals and possibly lose their funding. In one case, for example, the patient was told that he must leave the hospital because ‘acute beds are not for detox’. He explained that he was sleeping rough and that his choice was to wait in hospital until a detox bed became available. He was pressurised into leaving and subsequently readmitted 24 hours later for a period of 14 days. In relation to this case, we observed ward staff advocating for the patient against the homeless team, with the homeless team recommending discharge to the street to be the best option. Central access criteria for homeless services locally meant that this patient’s best hope of accessing any support was to be picked up by an outreach team whose role was to prevent a ‘second night out’ on the streets. However, to be eligible, potential service users must be seen to be bedded down on the street (rough sleeping). Here, a lack of trusted assessment (MIR5-missing) meant that people had to be put at risk to secure help (e.g. the outreach team was not permitted to in-reach into the hospital and assess the person while they were still occupying their hospital bed).
As a result of the homeless team’s need to ‘pick their battles’, some homeless patients received more leeway to remain in hospital than others (i.e. to have their transfer delayed). Across all the sites, we observed how much professional discretion was used to decide whether or not a homeless patient might avoid unsafe discharge and stay in a hospital bed as a DToC:
We would rather have someone in an extra night or two while they are waiting for a placement as opposed to, ‘Let’s discharge them now’. If they are going onto the street they are only going to come back to A&E 2 hours later. What’s the point? Everybody wins [this way] especially the patient.
Staff nurse S3a
[The doctor] is totally ignorant and it was on the Wednesday I saw [the nurse] and I said ‘Look, I’m disabled, I can’t handle [being discharged homeless]’. The nurse says, ‘Look don’t worry’, and he put his hand on my shoulder and he said, ‘You will not be homeless, we will not kick you out onto the street’, which is what the doctor wanted – he wanted me out. Well, I didn’t want to be in hospital. I was taking up a bed that someone desperately needed. All I wanted was a roof over my head.
Homeless patient S3a
Our observations pointed to those with drug and alcohol issues and those whose behaviour was perceived to be challenging as being more likely to be discharged unsafely. This may reflect that substance use is a highly stigmatised condition and when resources are stretched there is less tolerance of the challenging behaviour that can be associated with this:
[Discussing homeless patients] Some of them feel judged and that the whole aim of their admission is to get them out because they are difficult to manage on the ward. If you have got a drug-dependent patient who’s constantly leaving the ward to score that’s really difficult to manage from a practical point of view.
Staff nurse S3b
Some of the nurses are brilliant, but there’s hell of a lot of nurses that talk down to you as soon as they find out you are on the gear [illicit drug using] . . . It’s not as bad if they see you are in a hostel but if they know that you are actually living on the street and you’re on the gear or on the ale [alcohol] and that’s when they change they really do look on it as like, ‘Well they put themselves out there’.
Homeless patient, S3
Discussion
The qualitative evidence reported in this chapter supports our programme theory about the utility of the HICM and the importance of sites having all the ‘jigsaw pieces’ to deliver consistently safe, timely transfers of care. Where pieces of the jigsaw were missing, particularly residential intermediate care (MIR4res), patients consistently reported a range of poorer outcomes and experiences. These could be seen to have an impact on recovery and health and well-being more broadly.
Some minor programme theory refinements are indicated. This is with regard to incorporating additional MIRs for trusted assessment (MIR5) and strong and progressive leadership (MIR6). Trusted assessment (MIR5) is key to integrated care (i.e. patients having to tell their story only once) and leadership (MIR6) is important for nurturing the complex adaptive system. This is especially the case where protocols (MIR1) lack statutory ‘bite’ (i.e. where there is a need to implement system-wide adherence to local arrangements, such as carrying out housing assessments within 72 hours of receiving a ‘duty to refer’ notice).
In the standard-care site, with no specialist MIRs, we observed that safe, timely transfers were still possible. This was dependent on active nurturing of local partnership arrangements and a good supply of housing, care and support. However, across all the sites, there was strong consensus about the added value and benefit of having a dedicated specialist resource in terms of achieving more consistent patient flow and reducing DToCs. An important finding of the documentary analysis is that the sites with specialist care have fewer DToCs than those with standard care.
Interplay between mechanisms and context
As outlined in Chapter 1, the HHDF introduced additional ‘resources’ into contexts that were heavily affected by austerity. Indeed, there is a strong case to be made that this additional resource per se has improved outcomes (without necessarily firing any change in reasoning as is anticipated in realist theory). For example, HHDSs bring a significant additional staffing resource into the hospital, which allows ward staff to free-up their time by handing over responsibility for complex homeless patients. Without this extra resource, ward staff acknowledge that they would not have the time to undertake the work needed to secure safe discharge beyond ‘signposting’ to relevant agencies. In sites that had lost their HHDSs or where schemes were reduced in scale (i.e. where resourcing was not sustained), then the benefits of the HHDF were seen to evaporate.
Our observations also chart the dampening effects of a wider lack of resources across the whole system. We observed, for example, that discharge to the street was commonplace in sites where HHDS staff felt that the patient had no options left open to them (i.e. where there was a lack of housing, care and support). These findings mirror those of the earlier national evaluations of intermediate care for older people that we reported earlier. Here, it was concluded that the effectiveness of interventions to improve the speed and quality of discharge will depend, to a large extent, on the broader service context in which they take place. Interventions that are shown to work well in areas with well-resourced and efficient community support services may have little or no impact where services are inadequate or lacking. 83
Changes in reasoning
Although HHDSs ‘work’ effectively (in certain contexts) to deliver outcomes linked to patient flow (e.g. reducing DToCs), there is little evidence to suggest that they have ‘fired’ a change in reasoning with regard to discharge to the street. Eradicating the ‘poor practice’ that led to discharge to the street was a key objective of the HHDF and other government guidance at the time:
Too often discharge is seen as freeing-up a hospital bed rather than acting in the patient’s best interest to move them . . . To a safer environment that will encourage supported self-management, speed . . . recovery and have them feel better. We must make every effort to shift understanding to this reality.
p. 2092
Prior to the introduction of new COVID-19 hospital discharge guidance in 2020,91 situation reports for DToCs were indicative of large numbers of older adults being permitted to remain in an acute hospital bed once they were clinically optimised. This was for a variety of reasons, including ‘awaiting a care package’ or ‘patient and family exercising choice’ (i.e. waiting for a specific care home place to become available). For the research team undertaking the fieldwork, this raised the question as to why patients who were homeless were not accorded the same leeway to remain in a hospital bed while they waited for the housing, care and support of their choice to be arranged. Our observations suggested that this difference lay in the perpetuation of stigma and cultural distance that positioned ‘homeless patients’ as somehow less vulnerable and/or deserving than other groups of patients.
We observed that patients who were homeless and using substances were particularly affected by unsafe discharge, especially when their behaviour was perceived to be challenging. NHS incident reports suggest that the demographic most likely to be involved in aggressive incidents in the acute sector is men aged between 75 and 95 years (with their female peers not far behind) and that dementia and delirium lie behind much of this distress. 93 However, it would be unusual for this group of older patients to be discharged unsafely on ‘behavioural grounds’, alerting us as to how different conditions and vulnerabilities garner more or less sympathy.
Viewed through the lenses of professional ethics and adult safeguarding, it is difficult to see how discharging a patient to the street can be justified within the parameters of ‘safe to transfer’. 94 Local safeguarding adult reviews have increasingly drawn attention to instances where poor discharge arrangements have contributed to the deaths of people who are homeless. In particular, they have highlighted the poor practice associated with seeing each hospital admission in isolation, the failure to provide appropriate multidisciplinary responses and the failure to initiate safeguarding where unsafe discharge occurs. In one case, a man was signposted to a homeless resource centre, shortly before his death, with known risks that he was unlikely to receive any support there because of his incontinence. 95 There is a specific category of abuse defined in the Care Act 201489 under ‘Neglect – Acts of Omission’ to describe circumstances where there is a ‘failure to provide access to appropriate health, care and support; a neglect of medical, emotional and physical needs; and withholding necessities of life, such as adequate nutrition and heating’ (contains information licensed under the Open Government Licence v3.0). 89 This suggests that MIRs for adult safeguarding (MIR7) are currently the missing piece of the jigsaw and may be a necessary driver for changes in reason.
Indeed, there is a case to be made that this change in reason is necessary to secure adequate provision of specialist intermediate care. When DToCs reach crisis point, the government will usually intervene to create extra capacity in the system. In the winter of 2016/17, DToCs hit an all-time high when, on average, 6660 people were delayed every day in NHS beds. In March 2017, the government introduced a new target to reduce the level of bed-days ‘lost’ to 3.5% and announced an extra £2B of funding for social care services. It might be argued that because people who are homeless are more likely to be discharged prematurely, out-of-hospital care for this group remains underdeveloped and under-resourced, further exacerbating the drivers to discharge people unsafely.
Chapter 4 Results: data linkage
Parts of this chapter are reproduced or adapted with permission from a protocol paper published by the research team in BMJ Open. 96 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Overview
The overall aim of WP2 was to provide quantitative evidence to enable further testing of our programme theory about what works to deliver consistently safe, timely transfers of care. The underpinning logic of the HHDF was that safe, timely transfers of care will have an impact on a range of outcomes, including those for improved health and well-being of patients and the wider health and social care economy. In this chapter, we use data linkage findings to explore HHDSs’ impact on outcomes and different patterns of service use (objective 5). The primary outcomes are (1) time from discharge to next hospital inpatient admission, (2) time from discharge to next A&E attendance and (3) 28-day emergency readmission. We also consider a range of secondary outcomes.
In WP2, we broaden the focus of study, collecting data for 17 HHDSs. To test our programme theory about the importance of systems having all the ‘jigsaw pieces’ (including access to a clinically led multidisciplinary homeless team), we analyse and report the data linkage findings, comparatively exploring differences in the following:
-
Standard care compared with specialist care.
-
HHDSs that are clinically led (multidisciplinary) compared with those that are housing led (uniprofessional).
-
HHDSs with ‘step-down’ (intermediate) care compared with those without ‘step-down’ care. We focus on all types of intermediate care as the key mechanism of interest because of its relative importance, as evidenced in the previous chapter, and also because time and resources precluded any further deeper analysis of different typological configurations. This third comparator for step-down care was not outlined in the original protocol; however, reflecting good practice for realist quality standards, we have made allowances in the overall design of the study to collect additional data for further refinement of programme theories as the evaluation unfolds.
The main advantages of employing the data linkage as part of the wider realist mixed-method approach were twofold. First, it enabled us to gather data on outcomes that would be more geographically representative than previous analyses. For example, Hewett et al. ’s78 RCT of the Pathway schemes was limited to two hospital sites, whereas this present analysis focuses on 17 hospital sites and a broader range of scheme typologies. Second, the use of administrative records may offer a complimentary and/or more realistic evaluation of the benefits of the intervention than measurements taken in an interventional study setting, especially as there is the risk of bias when HHDS staff are involved in data collection.
Methods
Comparator groups
Three groups of individuals admitted to hospital were included in the analysis. The first group comprised homeless individuals admitted to hospital at any one of 17 sites with a HHDS between 1 November 2013 and 30 November 2016. An initial audit of HHDSs established the date on which they were implemented.
The second group comprised individuals seen by a community homeless service in London, UK [Find & Treat (F&T)] and subsequently admitted to a hospital that did not have a HHDS. This group was, therefore, selected to provide a comparison group of people experiencing homelessness, admitted to hospital, but not seen by a HHDS. F&T is a specialist outreach team that works alongside over 200 NHS and third-sector front-line services to prevent or treat tuberculosis among homeless people. It is primarily based in London. We looked for hospital admissions during the study period for all individuals seen by F&T between 1 November 2013 and 30 November 2016.
The third group was a random sample of individuals equal in size to the F&T group and living in lower-layer super output areas in England in the most deprived quintile, as measured by the Index of Multiple Deprivation (IMD), who were recorded as having a fixed address. These individuals came from hospitals offering HHDSs with an admission during the study period but without being seen by the HHDS. This group was used to confirm or refute our hypothesis that the homeless people included in the study have worse outcomes than non-homeless people living in deprived areas. This group is subsequently referred to as IMD5 (Index of Multiple Deprivation quintile 5).
Data linkage
Data were linked in respect of each group from HES, which includes dates, causes and length of admission, and the Office for National Statistics (ONS) mortality database, which includes dates and causes of death.
Data collection, processing and linkage
Data flows used in this analysis are described in Figure 3. We obtained demographic-identifying variables under our legal and ethics approvals. Where available, NHS numbers were collected from the 17 HHDS sites. NHS Digital (formally the Health and Social Care Information Centre) used the personal demographics service to identify and add NHS numbers to as many individual records as possible.
FIGURE 3.
Study data flows. PDS, personal demographics service; UCL, University College London.
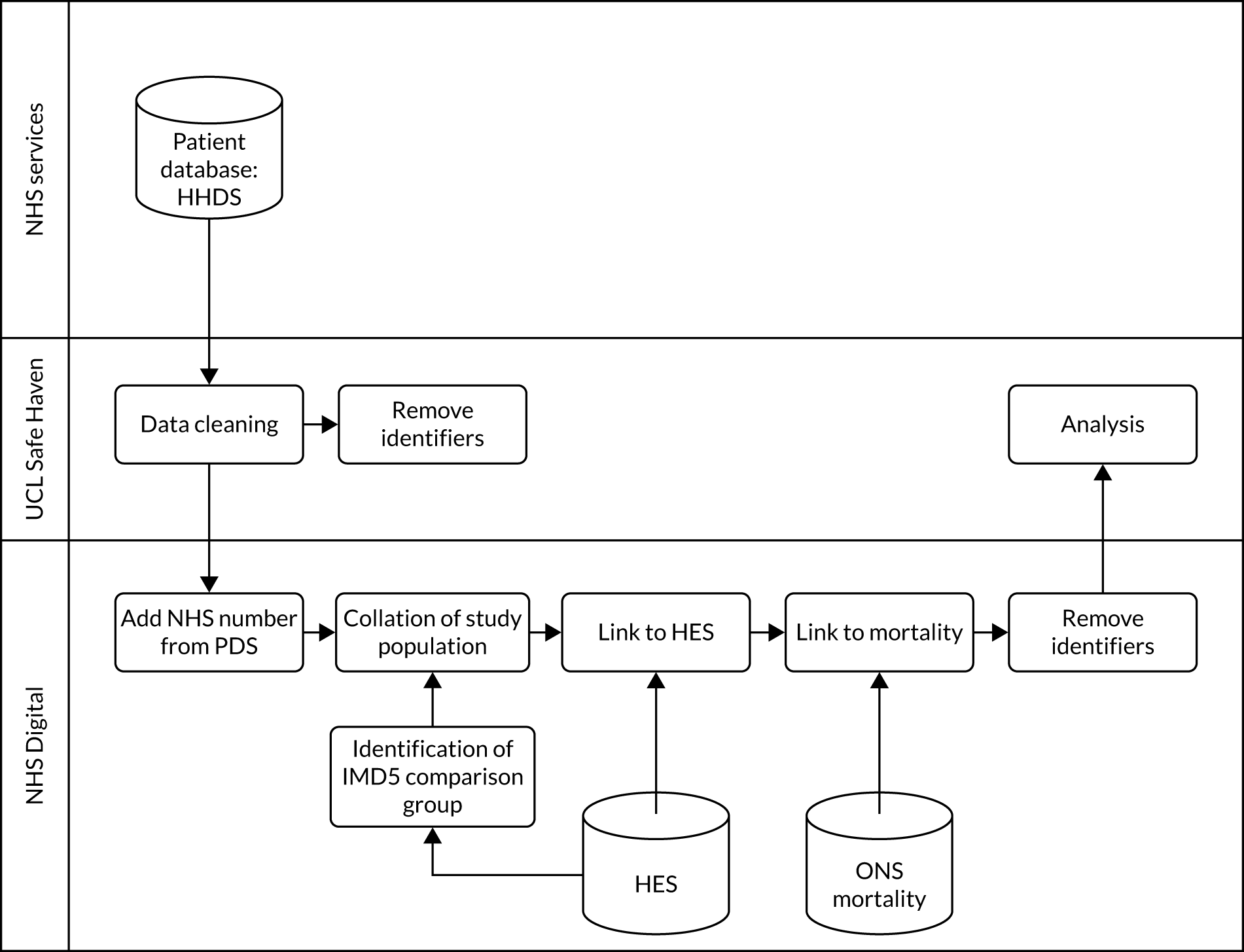
NHS Digital undertook all data linkage to HES data using patient identifiers obtained (in combination with personal demographics service tracing) and we securely uploaded a de-identified copy of the data to the University College London (London, UK) Institute of Health Informatics’ Data Safe Haven, which is a robust infrastructure certified for processing and analysing identifiable data in accordance with international and national information security standards (ISO/IEC 27001:2013 and NHS Information Governance Toolkit). The deterministic linkage process was undertaken in three steps to ensure that the three groups were mutually exclusive:
-
HES linkage to data collected at the HHDS sites
-
HES linkage to data collected from F&T services, with admissions stratified into those sites with and without HHDSs
-
identification of people in the most deprived IMD quintile from HES at the HHDS sites who were admitted after the implementation date at a given HHDS site.
In the main analysis, individuals identified in more than one of the steps described above were classified using the hierarchy 1 > 2 > 3, such that data on homeless patients who were admitted multiple times to a combination of hospitals with, and without, HHDSs were analysed according to admission to the HHDS site only. Patients identified as both homeless (i.e. HHDS or F&T) as well as those in the non-homeless (IMD5) group were assigned to the homeless HHDS category. In addition to collecting data on admissions after being seen by an HHDS, we obtained data on all individuals from HES in respect of admissions to any hospital in England from 1 January 2008 to 31 October 2013 to create a profile of their existing health conditions.
Sample size
Our sample size calculation was based on historical data from the two types of HHDS, suggesting an average of 92 patients per month across the 17 sites. We estimated that each type would have data from approximately 2208 patients for the duration of the study.
From previous health service evaluations, we expected 0.7 hospital episodes per person-year for homeless individuals. A clinically important reduction in readmission rates would be 10%. To undertake a sample size calculation to determine the study size required to detect such a reduction in readmission rates, the following variables were defined:
-
µ_0 – mean readmission rate in the baseline (F&T) group = 0.7 episodes per person-year.
-
µ_1 – mean readmission rate in the HHDS group = 0.6 episodes per person-year.
-
v = 1.96 – percentage point of the normal distribution corresponding to a 5% two-sided significance level.
-
u = 0.84 – one-sided percentage point of the normal distribution corresponding to {100% – type II error [false negative/(true positive + false negative)]} at 80% power.
Using the following equation, we estimated minimum sample size (per group) required for comparison of two rates (readmissions per person-year):
Adjustment for confounders (i.e. age, sex, ethnicity, calendar quarter of admission and existing comorbidities), as far as is possible within the analysis, resulted in a required doubling of sample size (additional 10% per confounder) required. Therefore, 2038 person-years were required per group. Assuming that the HHDS sites see, on average, 90 patients each month during the study period (which, for the purposes of the initial calculation we assumed to be November 2013 to November 2015, as many schemes may have been shut down before this time period and in some data may have been collected at an earlier point), we estimated that this translated to a total of 2160 individuals at each of the two types of scheme (e.g. housing led and clinically led). Given that the average follow-up period was likely to exceed 1 year, we anticipated that the study would be powered to detect a 10% difference in readmission rates between HHDS sites and non-HHDS sites for both the clinically- and the housing-led HHDSs.
Outcomes
A series of primary and secondary outcomes were included to ensure that our analysis was both consistent with outcomes used in previous published analyses and included outcomes that previous studies were not powered to collect. We chose several secondary outcomes that collectively reflect the priorities of health policy-makers and individuals attending patient engagement workshops. Full definitions of primary and secondary outcomes are provided in Tables 2 and 3.
| Primary outcome | Definition |
|---|---|
| Time from discharge to next hospital inpatient admission (any cause) | Binary indicator for readmission (yes/no). Time to event defined as index admission discharge date until the earliest of:
|
| Time from discharge to next A&E attendance | Binary indicator for subsequent A&E attendance (yes/no). Time to event defined as index admission discharge date until the earliest of:
|
| 28-day emergency readmission | Binary indicator for emergency readmission (yes/no) recorded within 28 days of the index admission discharge date. Emergency admissions are defined as those where the admission method is HES code 11, 12 or 13 |
| Secondary outcome | Definition |
|---|---|
| Time from discharge to ACS condition admission | Binary indicator for admission with ACS (yes/no). Time to event defined as index discharge date until the earliest of:
|
| Time from discharge to next elective admission | Binary indicator for elective readmission (yes/no). Time to event defined as index discharge date until the earliest of:
|
| Overall readmission rates | Number of readmissions divided by the total time under follow-up between admissions (i.e. where the patient was not already hospitalised). Calculated as the number of admissions occurring in the time from index discharge date to the earliest of death or November 2016 divided by the number of days from index discharge date to the earliest of death or November 2016 minus the number of days in the same time period where the individual was admitted to hospital |
| Unscheduled readmission rates | As for overall readmission rates (above), but excluding (from the numerator only) admissions where the admission method was elective (i.e. methods 11–13) |
| Time from admission to death | Binary indicator for death (yes/no). Time to event defined as index admission date until the earliest of:
|
| Time from admission to avoidable deaths | Binary indicator for avoidable death (yes/no). Time to event defined as index admission date until the earliest of:
|
| All-cause mortality expressed as a SMR | Deaths will primarily be identified through linkage to ONS deaths registration data, but also through HES [where the method of discharge field is coded as ‘dead’ (4)], as the latter method may better ascertain information on recent deaths where there is a delay in death registration (e.g. because a coroner’s report is required) |
| ICD-10 chapter-specific SMR | As for all-cause mortality (above), but examining deaths by ICD-10 chapter for primary cause of death |
Throughout the report we refer to three terms, avoidable,96 preventable and amenable, for which we use the following definitions and their associated ICD-10 (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision) codes:
-
Avoidable mortality – avoidable deaths are all those defined as preventable, amenable or both, where each death is counted only once. Where a cause of death falls within both the preventable and amenable definition, all deaths from that cause are counted in both categories when they are presented separately.
-
Amenable mortality – a death is amenable if, in the light of medical knowledge and technology at the time of death, all or most deaths from that cause (subject to age limits, if appropriate) could be avoided through good quality health care.
-
Preventable mortality – a death is preventable if, in the light of understanding of the determinants of health at the time of death, all or most deaths from that cause (subject to age limits, if appropriate) could be avoided by public health interventions in the broadest sense.
Analysis plan
We undertook the analysis in two phases. In the first phase, we analysed baseline characteristics (Table 4) of all participants to describe the characteristics of each of the study groups at or before the index admission (Figure 4). With the exception of ethnicity, all baseline characteristics were anticipated to be fully observed (chronic disease is presumed to be absent unless recorded). Missing values of ethnicity were analysed grouped as ‘not recorded’.
| Variable | Description |
|---|---|
| Age | (In years) at a given time point will be estimated as [(date of admission – month and year of birth)/365.25] for the index admission |
| Sex | As recorded at the index admissiona |
| Ethnicity | As recorded at the index admissiona |
| ICD-10 chronic disease conditions | Obtained from all admissions at or before the index admission and subdivided into categories of:
|
| Admitting diagnosis | Reason for index hospital admission classified according to Healthcare Resource Group, which describes case mix according to the chapter and subchapter of the reason for admission and associated procedures |
FIGURE 4.
Schematic outlining hypothetical patients. Data on the characteristics of patients before their index admission were collated from admissions occurring before the implementation of HHDSs at a given site (or for comparator groups a randomly selected date within the range of implementation dates for HHDS sites).
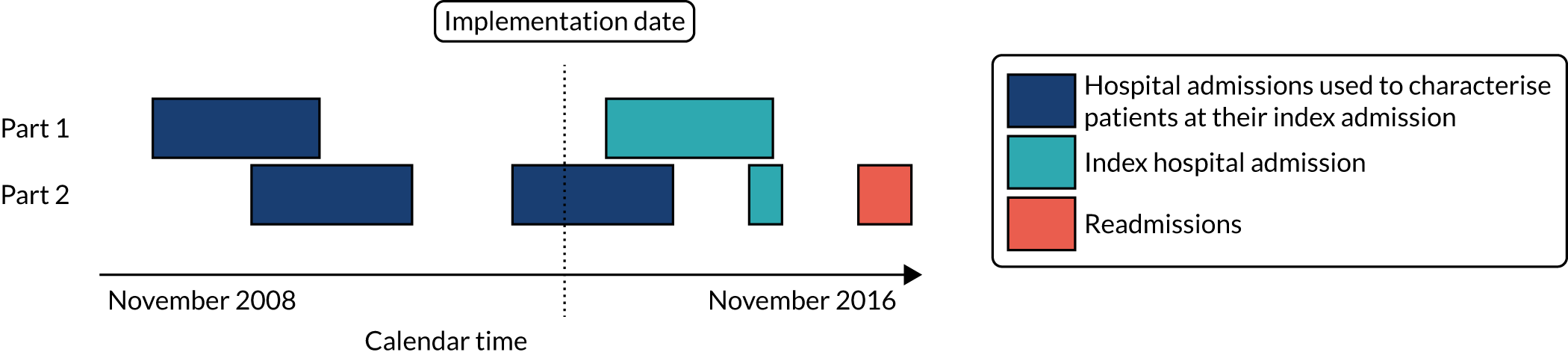
We then summarised each of the primary and secondary outcomes by comparison group and explored the geographical spread of our 17 sites to explore their representativeness. This work enabled us to confirm the suitability of the proposed statistical methods and analysis protocol proposed. Where applicable, we compared our baseline mortality data with those in the recent analysis of homeless deaths by the ONS (see Blackburn et al. ,96 table S1, supplementary file, for definitions and full ICD-10 code lists used).
In the second phase, we identified evidence of differences in the baseline characteristics, including age, sex, chronic disease and reason for hospital admission at the time of their index admission. We estimated the crude association between each of the primary and secondary outcomes and the study population groups. The baseline comparator group was IMD5. We then re-estimated the association between each of the outcomes and the study population group after adjusting for the following characteristics at the time of admission: age, sex, chronic disease and reason for hospital admission. We undertook supplementary subgroup analyses to evaluate evidence of a difference in the outcomes of people (1) admitted to clinically- compared with housing-led schemes and (2) schemes with step-down care compared with schemes without access to step-down care.
Crude models were fitted prior to adjustment for ‘baseline’ measurements at or before the index admission. We then wrote-up the analysis in accordance with the RECORD (REporting of studies Conducted using Observational Routinely collected Data) statement.
Protocol deviations
The data linkage study was significantly delayed at commencement because of the launch of the Health Research Authority and changes to the procedures for securing ethics approvals. It was further delayed by NHS Digital in relation to approving and returning the linked data set and then, finally, because of NHS Digital initially returning a data set without an IMD5 comparison group or linked death data. As a result, we did not have time to complete the analyses for the following secondary outcomes:
-
time from discharge to next elective admission
-
all-cause mortality expressed as a SMR
-
ICD-10 chapter-specific SMR.
Having completed the main literature synthesis (some 6 months after the study began), we developed our original realist hypothesis to capture new evidence about the importance of HHDSs having direct access to ‘step-down’ intermediate care. To enable us to interrogate this revised theory, we introduced a further comparative element across the evaluation to establish the effectiveness and cost-effectiveness of HHDSs with access to ‘step-down’ care (MIR4) compared with those with no direct access to ‘step-down’ care.
Results
Parts of this section are reproduced or adapted with permission from Aldridge et al. 97 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
To create an analysis data set, we joined the HHDS data (12,931 records) with F&T comparator group data (47,569 records). The combined data set (60,500 records) was cleaned, assigned gender and underwent validation of NHS numbers. We then applied age and date exclusions, and expanded the data set on names. We then validated NHS numbers within the data set. This was then split into an identifiable linkage data set with 73,432 records. Identifiable records were destroyed prior to receiving HES data from NHS Digital. The second retained unidentifiable data set was kept within the Data Safe Haven. This data set was linked to HES data from NHS Digital and underwent cleaning after linkage. After the cleaning process, we created three separate cohorts of patients. First was the HHDS group for whom we had 3894 unique patients, 6985 admission records and a record level linkage rate of 54% (6985/12,931). Second was the F&T–HES group with 7226 unique patients, 20,206 hospital admission records and a linkage rate of 42.5% (20,206/47,569). Third was the IMD5 group with 34,450 unique patients. Linkage rates were, therefore, higher in the HHDS group [54.0%, 95% confidence interval (CI) 53.2 to 54.9] than in the F&T group (42.5%, 95% CI 42.0 to 42.9).
To examine possible biases introduced into the linkage, we undertook several descriptive analyses. We also compared the age and sex characteristics of each cohort before and after linkage (Table 5). This analysis revealed that after linkage the data sets contained slightly more women and older patients, on an admission record basis, than the data sets prior to linkage. The HHDS sites from which data were collected covered seven out of nine statistical regions in England (Figure 5), with London having the largest number of participants. We examined comorbidities across comparator groups and, with few exceptions, we found these to be markedly high in those seen by HHDS sites (Table 6). HHDS patients had the highest levels of comorbidities across all ICD-10 chapters, except for endocrine and maternal disorders.
| Variable | F&T | HHDS | Housing led | Clinically led | Step-down scheme | No step-down scheme | IMD5, % | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unlinked, % | Linked, % | Unlinked, % | Linked, % | Unlinked, % | Linked, % | Unlinked, % | Linked, % | Unlinked, % | Linked, % | Unlinked, % | Linked, % | ||
| Male | 82 | 76 | 77 | 73 | 76 | 72 | 78 | 73 | 75 | 71 | 78 | 73 | 43 |
| Age (years) | |||||||||||||
| 18–24 | 5 | 5 | 6 | 9 | 10 | 7 | 6 | 9 | 10 | 8 | 5 | 9 | 8 |
| 25–34 | 20 | 17 | 20 | 19 | 22 | 23 | 20 | 18 | 22 | 22 | 20 | 18 | 15 |
| 35–44 | 25 | 25 | 26 | 27 | 26 | 26 | 26 | 27 | 27 | 28 | 26 | 26 | 13 |
| 45–54 | 27 | 29 | 26 | 26 | 21 | 24 | 27 | 27 | 21 | 23 | 27 | 28 | 16 |
| 55–64 | 15 | 15 | 13 | 13 | 11 | 12 | 14 | 13 | 12 | 11 | 14 | 13 | 16 |
| ≥ 65 | 8 | 8 | 8 | 7 | 9 | 8 | 7 | 6 | 8 | 8 | 8 | 7 | 33 |
FIGURE 5.
Map of number of individuals seen by HHDSs by ONS statistical region. There were no HHDS data linkage sites in the greyed areas.
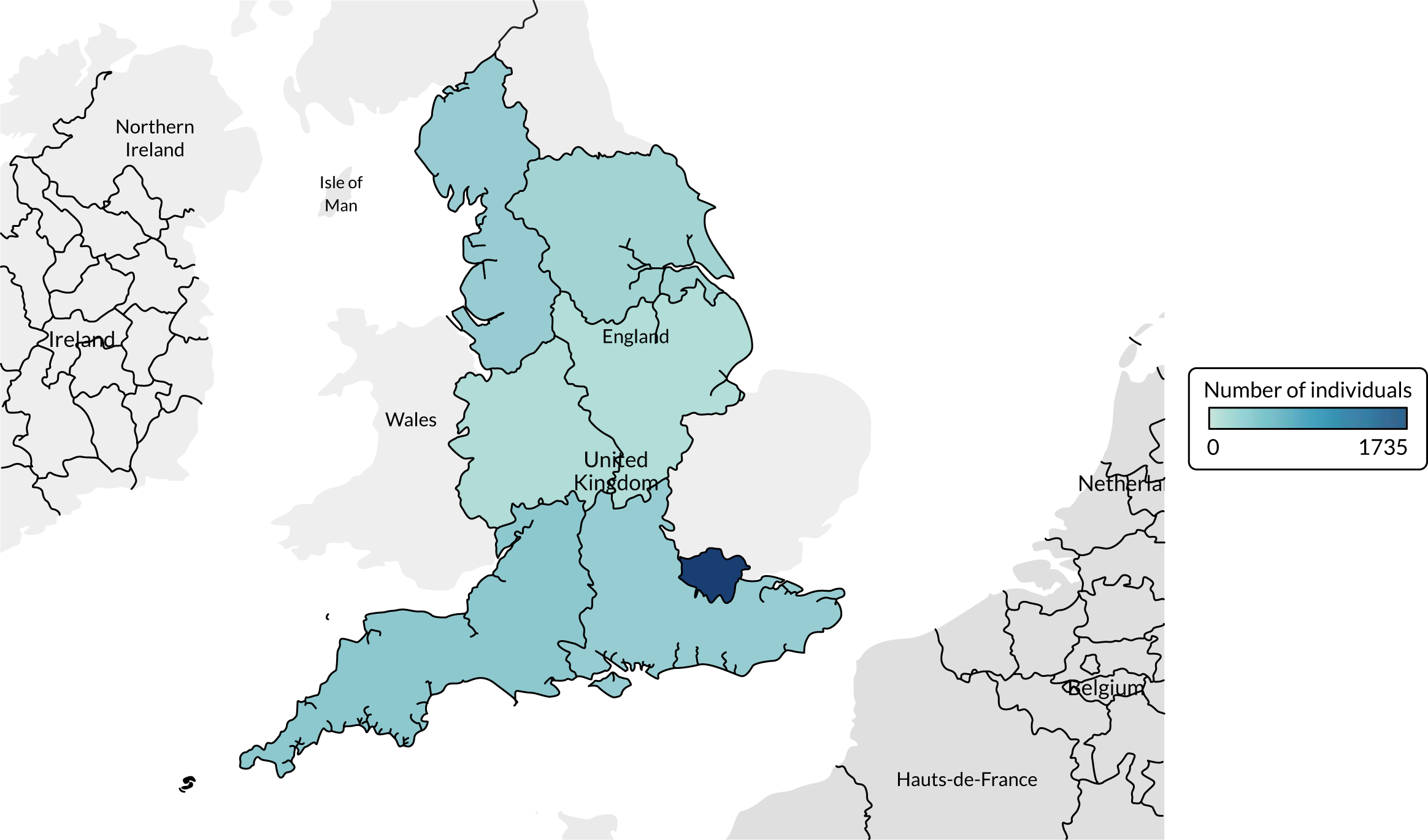
| ICD-10 chapter | HHDS, % | F&T, % | IMD5, % | Housing led, % | Clinically led, % | Step-down scheme, % | No step-down scheme, % |
|---|---|---|---|---|---|---|---|
| 1 | 29 | 21 | 12 | 26 | 30 | 27 | 30 |
| 2 | 7 | 6 | 14 | 6 | 7 | 6 | 7 |
| 3 | 13 | 9 | 11 | 13 | 14 | 13 | 14 |
| 4 | 27 | 21 | 29 | 26 | 27 | 27 | 27 |
| 5 | 79 | 67 | 31 | 85 | 77 | 86 | 76 |
| 6 | 19 | 13 | 13 | 18 | 20 | 19 | 20 |
| 7 | 8 | 7 | 11 | 9 | 8 | 9 | 7 |
| 8 | 2 | 2 | 3 | 3 | 2 | 2 | 2 |
| 9 | 35 | 28 | 35 | 36 | 35 | 36 | 35 |
| 10 | 37 | 29 | 25 | 38 | 37 | 39 | 36 |
| 11 | 42 | 38 | 40 | 44 | 41 | 45 | 40 |
| 12 | 23 | 14 | 10 | 19 | 24 | 20 | 24 |
| 13 | 28 | 22 | 27 | 27 | 28 | 27 | 28 |
| 14 | 20 | 16 | 25 | 20 | 20 | 20 | 20 |
| 15 | 7 | 11 | 19 | 7 | 7 | 8 | 7 |
| 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 17 | 2 | 1 | 2 | 2 | 1 | 2 | 2 |
| 18 | 65 | 51 | 44 | 68 | 64 | 69 | 63 |
| 19 | 54 | 40 | 20 | 61 | 52 | 61 | 51 |
| 20 | 56 | 40 | 21 | 62 | 53 | 63 | 52 |
| 21 | 78 | 63 | 60 | 78 | 77 | 77 | 78 |
These preliminary descriptive analyses showed that the F&T group had lower linkage rates and levels of comorbidity than the HHDS groups. These differences in linkage rates and comorbidity between the F&T and the HHDS groups, and lack of data on timing of homelessness exposure in the F&T data set, provided cause for concern about the validity of our assumption that this group was still homeless during their hospital admission during the study time period. For this reason, we took the decision not to include the F&T population as a comparison group in analyses of the primary and secondary outcomes.
Causes of death
In addition to understanding the geographical spread of the data, the demographic differences in each group after linkage and the levels of comorbidities, we also examined causes of death before undertaking a full analysis of the primary and secondary outcomes. Table 7 shows the demographic characteristics of decedents in each group. Males made up 77.7% (466/600) of deaths in the HHDS group and 56.4% (1416/2512) of deaths in the IMD5 group. The median age of death was 51.6 [interquartile range (IQR) 42.7–60.2] years for the HHDS group and 71.5 (IQR 60.67–79.0) years for the IMD5 group. Ethnicity was broadly similar across comparison groups, but 12.9% (403/3,112) of ethnicities were either not known or not stated. The top three underlying causes of death by ICD-10 chapter in the HHDS group were external causes of death (21.7%, 130/600), cancer (19.0%, 114/600) and digestive disease (19.0%, 114/600) in the unweighted analysis.
| Characteristic | All, n (%a) | IMD5, n (%a) | HHDS, n (%a) |
|---|---|---|---|
| Total | 3112 (100.0) | 2512 (100.0) | 600 (100.0) |
| Sex | |||
| Male | 1882 (60.5) | 1416 (56.4) | 466 (77.7) |
| Female | 1230 (39.5) | 1096 (43.6) | 134 (22.3) |
| Age (years) | |||
| 20–34 | 269 (8.6) | 171 (6.8) | 98 (16.3) |
| 35–44 | 199 (6.4) | 84 (3.3) | 115 (19.2) |
| 45–54 | 370 (11.9) | 205 (8.2) | 165 (27.5) |
| 55–64 | 483 (15.5) | 356 (14.2) | 127 (21.2) |
| ≥ 65 | 1791 (57.6) | 1696 (67.5) | 95 (15.8) |
| Ethnicity | |||
| British, Irish (white) and any other white | 2234 (71.8) | 1792 (71.3) | 442 (73.7) |
| African, Caribbean, Indian, Pakistani, Bangladeshi, Chinese and Mixed | 475 (15.3) | 389 (15.5) | 86 (14.3) |
| Not stated or not known | 403 (12.9) | 331 (13.2) | 72 (12.0) |
In an age- and sex-weighted analysis (Table 8 and Figure 6), the top three underlying causes of death in the HHDS group were cardiovascular disease (30.1%, 180/600), cancer (21.8%, 131/600) and respiratory disease (16.7%, 100/600). In this weighted analysis, the underlying causes of death for each cohort by ICD-10 chapter showed a greater proportion of deaths with an underlying cause in ‘External Causes of Morbidity and Mortality’ chapter in the homeless group (7.4%, 44/600) than in the IMD5 group (3.9%, 99/2,512). This chapter covers a range of causes, including accidents, intentional self-harm, assault and events of undetermined intent (e.g. poisoning). Weighted alcohol- and drug-related causes were higher in the HHDS group (9.8%, 59/600 and 3.6%, 22/600, respectively) than in the IMD5 group (2.7%, 67/2512 and 0.9%, 23/2512, respectively). The percentage of deaths with an amenable cause of mortality was higher in the HHDS group (30.2%, 181/600) than in the IMD5 group (23.0%, 578/2512). This means that after weighting for age and sex, nearly one in three deaths of people in our homeless hospital discharge cohort were due to conditions, many of which are common in the general population (e.g. heart disease), that are amenable to timely health care.
| Cause of death | Homeless, n (%) | Homeless weighted, n (%)a | IMD5, n (%) |
|---|---|---|---|
| Total | 600 (100.0) | 600 (100.0) | 2512 (100.0) |
| ICD-10 chapters | |||
| I: infections | 18 (3.0) | 7 (1.1) | 36 (1.4) |
| II: cancers | 114 (19.0) | 131 (21.8) | 926 (36.9) |
| Other | 48 (8.0) | 76 (12.6) | 355 (14.1) |
| Digestive | 28 (4.7) | 25 (4.1) | 242 (9.6) |
| Lung | 22 (3.7) | 17 (2.9) | 247 (9.8) |
| Lymph/blood | 16 (2.7) | 13 (2.2) | 82 (3.3) |
| IV: endocrine, nutritional and metabolic | 17 (2.8) | 13 (2.2) | 61 (2.4) |
| V: mental and behavioural | 14 (2.3) | 21 (3.5) | 82 (3.3) |
| VI: nervous system | 11 (1.8) | 9 (1.6) | 94 (3.7) |
| IX: CVD | 96 (16.0) | 180 (30.1) | 571 (22.7) |
| Stroke | 17 (2.8) | 63 (10.6) | 145 (5.8) |
| Ischaemic heart disease | 39 (6.5) | 60 (10.1) | 251 (10.0) |
| Other | 18 (3.0) | 26 (4.3) | 89 (3.5) |
| Other heart disease | 22 (3.7) | 31 (5.2) | 86 (3.4) |
| X: respiratory | 60 (10.0) | 100 (16.7) | 339 (13.5) |
| COPD | 36 (6.0) | 52 (8.7) | 213 (8.5) |
| Other | 24 (4.0) | 48 (8.0) | 126 (5.0) |
| XI: digestive | 114 (19.0) | 77 (12.8) | 227 (9.0) |
| Liver | 83 (13.8) | 51 (8.6) | 69 (2.7) |
| Other | 31 (5.2) | 25 (4.2) | 158 (6.3) |
| XX: external | 130 (21.7) | 44 (7.4) | 99 (3.9) |
| Accidents | 105 (17.5) | 35 (5.8) | 66 (2.6) |
| Self-harm | 15 (2.5) | 6 (1.0) | 14 (0.6) |
| Other | 10 (1.7) | 3 (0.6) | 19 (0.8) |
| Other | 26 (4.3) | 17 (2.8) | 77 (3.1) |
| Deaths related to alcohol, drugs or suicideb | |||
| Alcohol | 97 (16.2) | 59 (9.8) | 67 (2.7) |
| Drugs | 79 (13.2) | 22 (3.6) | 23 (0.9) |
| Suicide | 24 (4.0) | 9 (1.5) | 22 (0.9) |
| Other | 400 (66.7) | 510 (85.1) | 2400 (95.5) |
| Amenable to health carec | |||
| Amenable | 166 (27.7) | 181 (30.2) | 578 (23.0) |
| Not amenable | 434 (72.3) | 419 (69.8) | 1934 (77.0) |
FIGURE 6.
Underlying cause of death by ICD-10 group and subgroup, comparing homeless weighted and IMD5 groups. COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; IHD, ischaemic heart disease. Adapted with permission from Aldridge et al. 97 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
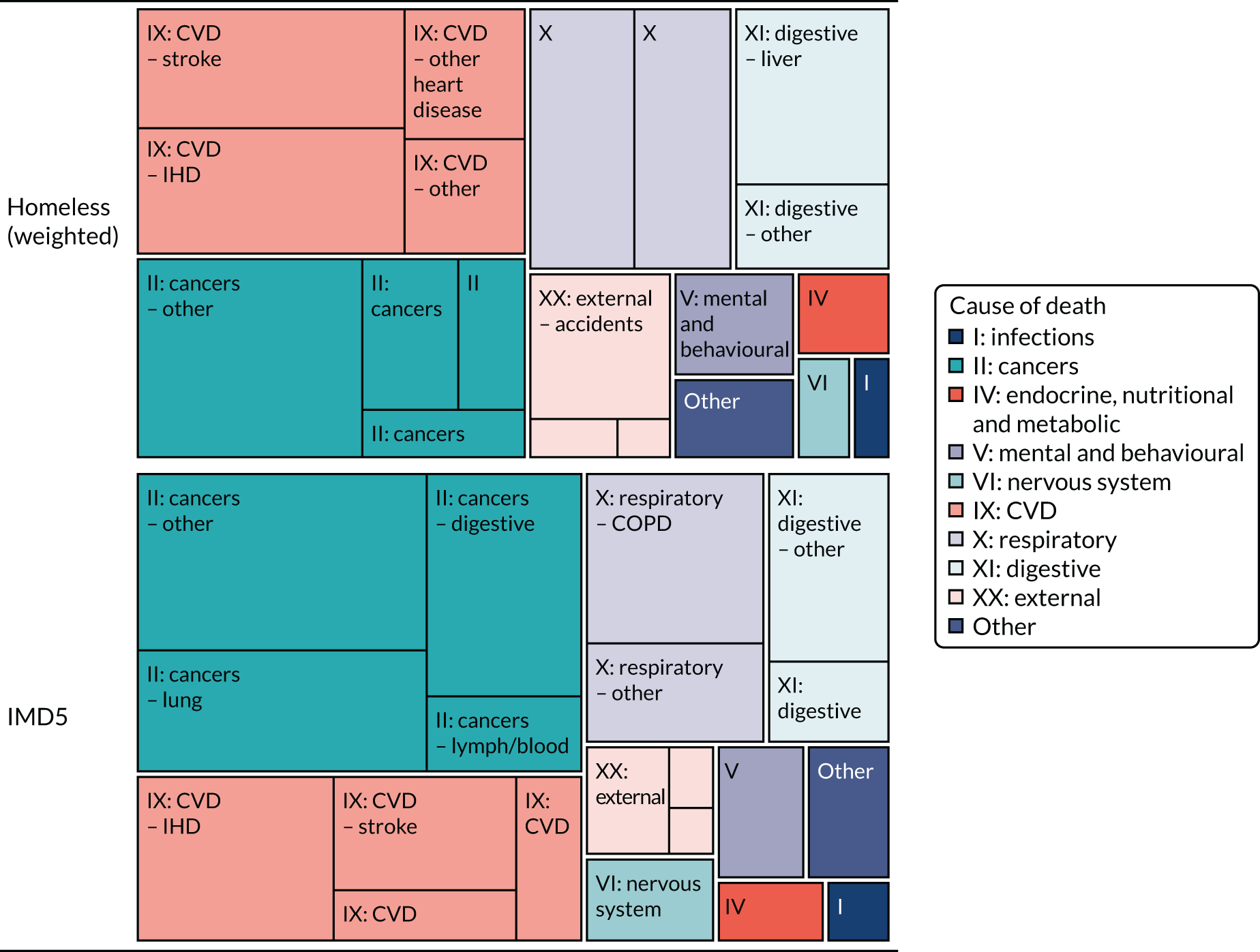
In an unweighted analysis that compared the HHDS group with the ONS homeless causes of death analysis, accidents and suicides contributed to a smaller percentage of all underlying causes of death in the HHDS homeless group (19.5%, 117/600) than in the ONS homeless group (54.9%, 319/581) (Figure 7). Conversely, we observed a larger number of deaths due to cancer (18.2%, 109/600 vs. 4.6%, 27/581), diseases of the liver (13.8%, 83/600 vs. 9.0%, 52/581) and chronic lower respiratory disease (6.0%, 36/600 vs. 2.2%, 13/581) in the HHDS group than in the ONS analysis.
FIGURE 7.
Underlying cause of death across the three comparator groups. Adapted with permission from Aldridge et al. 97 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
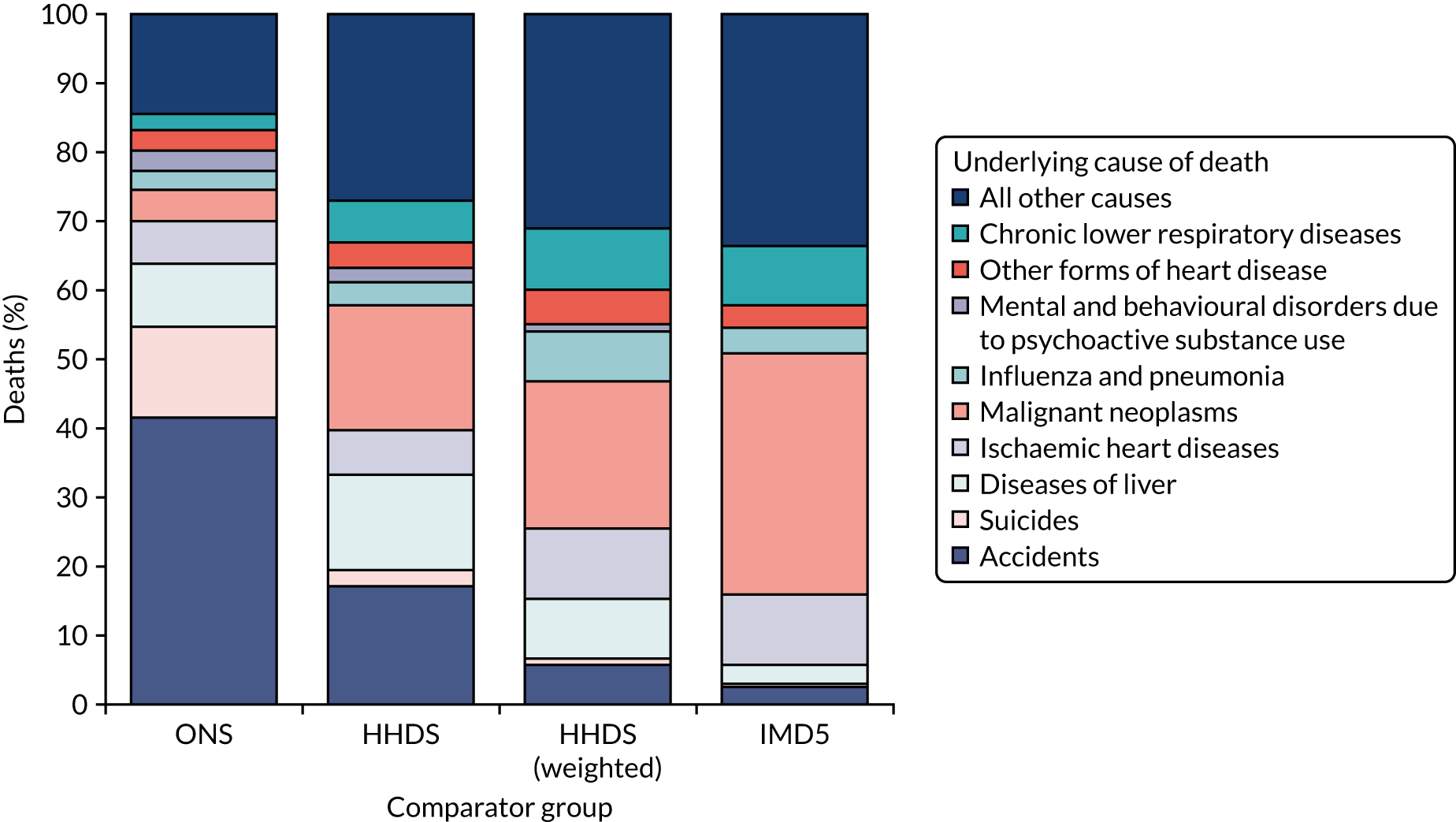
Primary outcomes
Time from discharge to next hospital inpatient readmission (any cause)
In the unadjusted analysis comparing clinically led schemes with housing-led schemes for time from discharge to next hospital inpatient readmission (any cause), male sex, older age group, larger number of comorbidities and larger number of admissions in the 1 year before index admission were all associated with an increase in readmissions (Table 9). In the multivariable analyses, there remained an association between older age, larger numbers of comorbidities, larger numbers of numbers of admissions in the 1 year before the index admission and an increase in readmissions. We found no evidence in either the unadjusted or adjusted analyses for a difference between the housing- or clinically led services for readmissions [hazard ratio (HR) 1.07, 95% CI 0.88 to 1.30; p = 0.4827]. When grouping the HHDS sites into those with step-down care and those without step-down care, in a multivariable analysis, we found no evidence for a difference in readmission rates between the two groups (HR 1.10, 95% CI 0.92 to 1.33; p = 0.2863) (see Table 12). In an adjusted analysis, hazard of readmission was higher in the combined HHDS group than in the IMD5 group (HR 3.14, 95% CI 2.81 to 3.51; p < 0.0001) (see Table 12).
| Baseline characteristic | Number of events | Median follow-up (days) (IQR) | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |||
| Cohort group | ||||||
| Housing led | 145 | 123 (34–417.75) | 1 | 1 | ||
| Clinically led | 426 | 104 (26–359.75) | 1.10 (0.91 to 1.33) | p = 0.3167 | 1.07 (0.88 to 1.30) | 0.4827 |
| Sex | ||||||
| Male | 439 | 113 (28–388.75) | 1 | 1 | ||
| Female | 132 | 104 (29–349) | 0.82 (0.68 to 1.00) | p = 0.0480 | 0.95 (0.78 to 1.16) | 0.6227 |
| Age group (years) | ||||||
| < 25 | <10 | 131.25 (29–396.625) | 1 | 1 | ||
| 25–34 | 60–70 | 106 (28–331.6875) | 5.05 (2.18 to 11.68) | 4.44 (1.92 to 10.25) | ||
| 35–44 | 128 | 120 (29–353) | 8.41 (3.70 to 19.13) | 6.78 (2.98 to 15.40) | ||
| 45–54 | 165 | 108 (29.375–354) | 11.73 (5.18 to 26.56) | 9.13 (4.03 to 20.68) | ||
| 55–64 | 120 | 88.125 (24–344) | 16.96 (7.45 to 38.59) | 13.42 (5.87 to 30.65) | ||
| 65–74 | 56 | 141 (40.75–410.6875) | 17.93 (7.73 to 41.61) | 14.06 (5.99 to 33.01) | ||
| ≥ 75 | 33 | 133 (34–513) | 23.58 (9.86 to 56.39) | p < 0.0001 | 19.90 (8.31 to 47.61) | < 0.0001 |
| Number of comorbid chapters | ||||||
| 1 or 2 | 31 | 166 (43–515) | 1 | 1 | ||
| 3–5 | 72 | 157 (39–529) | 1.12 (0.74 to 1.71) | 1.06 (0.70 to 1.61) | ||
| 6–9 | 272 | 107 (28.25–354) | 2.38 (1.64 to 3.45) | 1.79 (1.23 to 2.61) | ||
| 10–15 | 184 | 60 (16–187.5) | 5.98 (4.08 to 8.76) | 3.14 (2.09to 4.71) | ||
| > 15 | 12 | 29 (11–60) | 11.21 (5.89 to 21.34) | p < 0.0001 | 2.74 (1.23 to 6.13) | < 0.0001 |
| Number of admissions 1 year before index | ||||||
| 0 | 343 | 149 (37–461) | 1 | 1 | ||
| 1 | 62 | 94 (23–247.75) | 1.85 (1.42 to 2.42) | 1.46 (1.09 to 1.95) | ||
| 2 | 56 | 51 (19.5–157) | 3.65 (2.75 to 4.84) | 2.60 (1.93 to 3.52) | ||
| 3 | 21 | 79 (25–182) | 2.18 (1.41to 3.34) | 1.66 (1.08 to 2.57) | ||
| 4 or 5 | 31 | 38 (12–151) | 3.19 (2.21 to 4.61) | 2.43 (1.65 to 3.58) | ||
| 6 or 7 | 18 | 28 (11–93) | 4.84 (3.02 to 7.75) | 2.97 (1.79 to 4.92) | ||
| 8 or 9 | < 10 | 22 (10–52.5) | 4.63 (2.28 to 9.41) | 2.76 (1.35 to 5.61) | ||
| ≥ 10 | 30–40 | 13 (5–36.75) | 8.55 (5.63 to 12.98) | p < 0.0001 | 4.98 (3.04 to 8.16) | < 0.0001 |
Time from discharge to next accident and emergency attendance
In the unadjusted analysis comparing clinically led services with housing-led services for time from discharge to next A&E attendance, sex, age group, number of comorbidities and number of admissions in the year before index admission were all associated with an increase in emergency attendance (Table 10). In the multivariable analyses, older age, larger numbers of comorbidities and larger numbers of admissions in the 1 year before the index admission were all associated with an increase in emergency attendance. We found no evidence in either the unadjusted or adjusted analyses for a difference between the housing- or clinically led services for emergency attendance (HR 1.05, 95% CI 0.83 to 1.32; p = 0.6835) (Table 11). We grouped HHDS sites into those with step-down care and those without step-down care and found no evidence for a difference in emergency attendance between the two groups in a multivariable analysis (HR 1.01, 95% CI 0.82 to 1.26; p = 0.9063) (Table 12). In a multivariate analysis, the hazard of emergency attendance was higher in the combined HHDS group than in the IMD5 group (HR 7.34, 95% CI 6.31 to 8.54; p < 0.0001) (see Table 12).
| Baseline characteristic | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Cohort group | ||||
| Housing led | 1 | 1 | ||
| Clinically led | 1.02 (0.82 to 1.27) | 0.8489 | 1.05 (0.83 to 1.32) | 0.6835 |
| Sex | ||||
| Male | 1 | 1 | ||
| Female | 0.64 (0.50 to 0.81) | 0.0003 | 0.67 (0.52 to 0.86) | 0.0015 |
| Age group (years) | ||||
| < 25 | 1 | 1 | ||
| 25–34 | 3.72 (1.59 to 8.71) | 3.21 (1.37 to 7.53) | ||
| 35–44 | 6.60 (2.89 to 15.07) | 5.09 (2.22 to 11.66) | ||
| 45–54 | 7.16 (3.15 to 16.30) | 4.99 (2.18 to 11.43) | ||
| 55–64 | 8.09 (3.52 to 18.62) | 5.90 (2.54 to 13.69) | ||
| 65–74 | 8.98 (3.76 to 21.46) | 6.12 (2.51 to 14.90) | ||
| ≥ 75 | 13.73 (5.65 to 33.35) | 0.0001 | 10.91 (4.38 to 27.15) | 0.0001 |
| Number of comorbid chapters | ||||
| 1 or 2 | 1 | 1 | ||
| 3–5 | 1.17 (0.66 to 2.06) | 1.07 (0.60 to 1.89) | ||
| 6–9 | 3.11 (1.90 to 5.10) | 2.41 (1.46 to 3.97) | ||
| 10–15 | 7.87 (4.77 to 12.98) | 4.68 (2.77 to 7.90) | ||
| > 15 | 15.69 (7.63 to 32.29) | 0.0001 | 6.78 (2.98 to 15.44) | 0.0001 |
| Number of admissions 1 year before index | ||||
| 0 | 1 | 1 | ||
| 1 | 1.87 (1.37 to 2.55) | 1.41 (1.02 to 1.94) | ||
| 2 | 3.73 (2.69 to 5.17) | 2.48 (1.76 to 3.51) | ||
| 3 | 2.16 (1.31 to 3.57) | 1.45 (0.88 to 2.41) | ||
| 4 or 5 | 3.16 (2.03 to 4.92) | 2.20 (1.40 to 3.46) | ||
| 6 or 7 | 6.71 (4.10 to 10.99) | 3.69 (2.16 to 6.30) | ||
| 8 or 9 | 4.13 (1.84 to 9.30) | 2.46 (1.11 to 5.43) | ||
| ≥ 10 | 4.45 (2.66 to 7.46) | 0.0001 | 1.97 (1.08 to 3.60) | 0.0001 |
| Baseline characteristic | Patients admitted, % (n/N) | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| Cohort group | |||||
| Housing led | 19.48 (196/1006) | 1 | 1 | ||
| Clinically led | 21.23 (613/2888) | 1.11 (0.93 to 1.33) | 0.2408 | 1.08 (0.89 to 1.29) | 0.4420 |
| Sex | |||||
| Male | 21.13 (600/2840) | 1 | 1 | ||
| Female | 19.83 (209/1054) | 0.92 (0.77 to 1.10) | 0.3753 | 0.89 (0.74 to 1.07) | 0.2128 |
| Age group (years) | |||||
| < 25 | 17.10 (46/269) | 1 | 1 | ||
| 25–34 | 22.74 (171/752) | 1.43 (1.00 to 2.05) | 1.31 (0.91 to 1.90) | ||
| 35–44 | 19.27 (186/965) | 1.16 (0.81 to 1.65) | 1.01 (0.70 to 1.46) | ||
| 45–54 | 21.87 (215/983) | 1.36 (0.95 to 1.93) | 1.10 (0.76 to 1.59) | ||
| 55–64 | 22.37 (134/599) | 1.40 (0.96 to 2.02) | 1.14 (0.78 to 1.68) | ||
| 65–74 | 17.26 (39/226) | 1.01 (0.63 to 1.62) | 0.85 (0.52 to 1.39) | ||
| ≥ 75 | 18.00 (18/100) | 1.06 (0.58 to 1.94) | 0.1698 | 1.02 (0.55 to 1.89) | 0.2995 |
| Number of comorbid chapters | |||||
| 1 or 2 | 15.55 (67/431) | 1 | 1 | ||
| 3–5 | 14.19 (127/895) | 0.90 (0.65 t 1.24) | 0.89 (0.65 to 1.23) | ||
| 6–9 | 20.98 (391/1864) | 1.44 (1.09 to 1.91) | 1.24 (0.93 to 1.66) | ||
| 10–15 | 31.28 (208/665) | 2.47 (1.82 to 3.36) | 1.53 (1.09 to 2.15) | ||
| > 15 | 41.03 (16/39) | 3.78 (1.90 to 7.53) | 0.0001 | 1.49 (0.70 to 3.18) | 0.0036 |
| Number of admissions 1 year before index | |||||
| 0 | 16.52 (473/2863) | 1 | 1 | ||
| 1 | 22.16 (78/352) | 1.44 (1.10 to 1.88) | 1.29 (0.98 to 1.70) | ||
| 2 | 29.95 (59/197) | 2.16 (1.57 to 2.98) | 1.88 (1.35 to 2.61) | ||
| 3 | 28.57 (34/119) | 2.02 (1.34 to 3.04) | 1.69 (1.11 to 2.57) | ||
| 4 or 5 | 39.07 (59/151) | 3.24 (2.30 to 4.56) | 2.71 (1.90 to 3.86) | ||
| 6 or 7 | 46.48 (33/71) | 4.39 (2.72 to 7.07) | 3.55 (2.17 to 5.82) | ||
| 8 or 9 | 56.10 (23/41) | 6.46 (3.46 to 12.06) | 5.12 (2.70 to 9.68) | ||
| ≥ 10 | 50.00 (50/100) | 5.05 (3.37 to 7.57) | 0.0001 | 3.84 (2.46 to 5.98) | 0.0001 |
| Outcomea | Housing led vs. clinically led, HR (95% CI); p-value | Step-down care vs. no step-down care, HR (95% CI); p-value | HHDS vs. IMD5, HR (95% CI); p-value |
|---|---|---|---|
| Time from discharge to next hospital inpatient readmission (any cause) | 1.07 (0.88 to 1.30); 0.4827 | 1.10 (0.92 to 1.33); 0.2863 | 3.14 (2.81 to 3.51); < 0.0001 |
| Time from discharge to next A&E attendance | 1.05 (0.83 to 1.32); 0.6835 | 1.01 (0.82 to 1.26); 0.9063 | 7.34 (6.31 to 8.54); < 0.0001 |
| 28-day emergency readmission | 1.08 (0.89 to 1.29); 0.4420 | 1.05 (0.88 to 1.25); 0.5821 | 3.60 (3.24 to 3.99); < 0.0001 |
| Time from admission to death due to any cause | 1.01 (0.84 to 1.21); 0.9285 | 1.05 (0.88 to 1.24); 0.6103 | 2.20 (1.98 to 2.44); < 0.0001 |
| Time from admission to avoidable deaths | 1.02 (0.69 to 1.49); 0.9383 | 0.99 (0.69 to 1.42); 0.9583 | 1.78 (1.43 to 2.22); < 0.0001 |
| Time from discharge to ACS condition admission | 1.11 (0.86 to 1.44); 0.4159 | 1.27 (0.99 to 1.62); 0.0551 | 3.52 (3.06 to 4.06); 0.0001 |
28-day emergency readmission
The overall percentage of patients with a 28-day emergency readmission in the housing-led group (19.5%, 196/1006) was slightly lower than in the clinically led group (21.2%, 613/2888) (see Table 11). Male patients (21.1%, 600/2840) had slightly higher readmission rates than female patients (19.8%, 209/1054) and readmission rates were highest in the 55- to 64-years age group (22.4%, 134/599). In both the unadjusted and the adjusted analyses, only number of comorbidities and number of admissions in the year before index admissions were associated with 28-day emergency readmissions. In an adjusted analysis, no evidence was found for a difference in readmission rates between housing- and clinically led services [odds ratio (OR) 1.08, 95% CI 0.89 to 1.29; p = 0.4420]. In an adjusted analysis, we found that the HHDS group had higher odds of 28-day emergency readmissions than the IMD5 group (OR 3.60, 95% CI 3.24 to 3.99; p < 0.0001) (see Table 12). When comparing services with step-down care with those without step-down care, the percentage of patients with 28-day emergency readmissions was similar across both groups (20.2% for step-down care vs. 21.1% for no step-down care). There was no evidence in either the unadjusted or adjusted multivariate analysis for a difference between these groups in terms of 28-day emergency readmission (OR 1.05, 95% CI 0.88 to 1.25; p = 0.5821) (see Table 12).
Secondary outcomes
Time from discharge to admission with ambulatory care sensitive conditions
Being of female sex appeared to be somewhat slightly protective against readmission with ambulatory care sensitive conditions (Table 13) in the unadjusted figures (HR 0.82, 95% CI 0.68 to 1.0; p = 0.0480); however, this was not true of the adjusted HR 0.95 (95% CI 0.78 to 1.16; p = 0.6227). There was no overall difference in likelihood of readmission when comparing the housing-led group with the clinically led group, with the unadjusted HR being 1.11 (95% CI 0.86 to 1.42; p = 0.4174) and adjusted HR being 1.11 (95% CI 0.86 to 1.44; p = 0.4159).
| Baseline characteristic | Number of events | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | ||
| Cohort group | |||||
| Housing led (n = 1006) | 82 | 1 | |||
| Clinically led (n = 2888) | 253 | 1.11 (0.86 to 1.42) | 0.4174 | 1.11 (0.86 to 1.44) | 0.4159 |
| Sex | |||||
| Male | 261 | 1 | |||
| Female | 74 | 0.72 (0.55 to 0.93) | 0.0109 | 0.84 (0.65 to 1.10) | 0.2019 |
| Age group (years) | |||||
| < 25 | < 10 | 1 | |||
| 25–34 | 30–40 | 4.17 (1.27 to 13.67) | 3.61 (1.10 to 11.84) | ||
| 35–44 | 68 | 8.37 (2.63 to 26.63) | 6.46 (2.02 to 20.68) | ||
| 45–54 | 112 | 14.52 (4.61 to 45.76) | 10.45 (3.29 to 33.15) | ||
| 55–64 | 63 | 15.84 (4.97 to 50.49) | 11.61 (3.62 to 37.20) | ||
| 65–74 | 37 | 24.49 (7.54 to 79.47) | 17.10 (5.21 to 56.14) | ||
| ≥ 75 | 22 | 32.21 (9.61 to 107.97) | 0 | 27.15 (8.07 to 91.36) | 0 |
| Number of comorbid chapters | |||||
| 1 or 2 | 11 | 1 | |||
| 3–5 | 30 | 1.33 (0.67 to 2.65) | 1.27 (0.64 to 2.54) | ||
| 6–9 | 153 | 3.35 (1.82 to 6.17) | 2.75 (1.48 to 5.10) | ||
| 10–15 | 130 | 10.11 (5.47 to 18.68) | 6.55 (3.43 to 12.50) | ||
| > 15 | 11 | 17.12 (7.15 to 40.99) | 0 | 6.72 (2.49 to 18.10) | 0 |
| Number of admissions 1 year before index | |||||
| 0 | 183 | 1 | |||
| 1 | 42 | 1.84 (1.32 to 2.57) | 1.27 (0.89 to 1.83) | ||
| 2 | 37 | 2.97 (2.09 to 4.22) | 1.82 (1.25 to 2.65) | ||
| 3 | 12 | 1.69 (0.94 to 3.01) | 1.18 (0.66 to 2.11) | ||
| 4 or 5 | 19 | 2.17 (1.35 to 3.48) | 1.34 (0.81 to 2.21) | ||
| 6 or 7 | 14 | 3.90 (2.22 to 6.85) | 2.00 (1.12 to 3.57) | ||
| 8 or 9 | < 10 | 3.18 (1.28 to 7.86) | 1.31 (0.49 to 3.51) | ||
| ≥ 10 | 20–40 | 4.35 (2.80 to 6.76) | 0 | 2.09 (1.26 to 3.48) | 0.0131 |
Overall and unscheduled readmission rates
We looked at the 12-month risk of readmission by ICD-10 chapter of index admission (Figure 8). The 12-month risk of unscheduled readmission (often referred to as emergency readmission) was 59% (95% CI 57% to 61%) for homeless patients and 20% (95% CI 19% to 21%) for housed patients, for planned readmission it was 18% (95% CI 17% to 20%) for homeless patients and 28% (95% CI 26% to 29%) for housed patients and for A&E visits it was 92% (95% CI 91% to 93%) for homeless patients and 57% (95% CI 55% to 59%) for housed patients.
FIGURE 8.
Twelve-month risk of readmission, stratified by the ICD-10 chapter of index admission: (a) emergency readmission; (b) planned readmission; and (c) A&E.
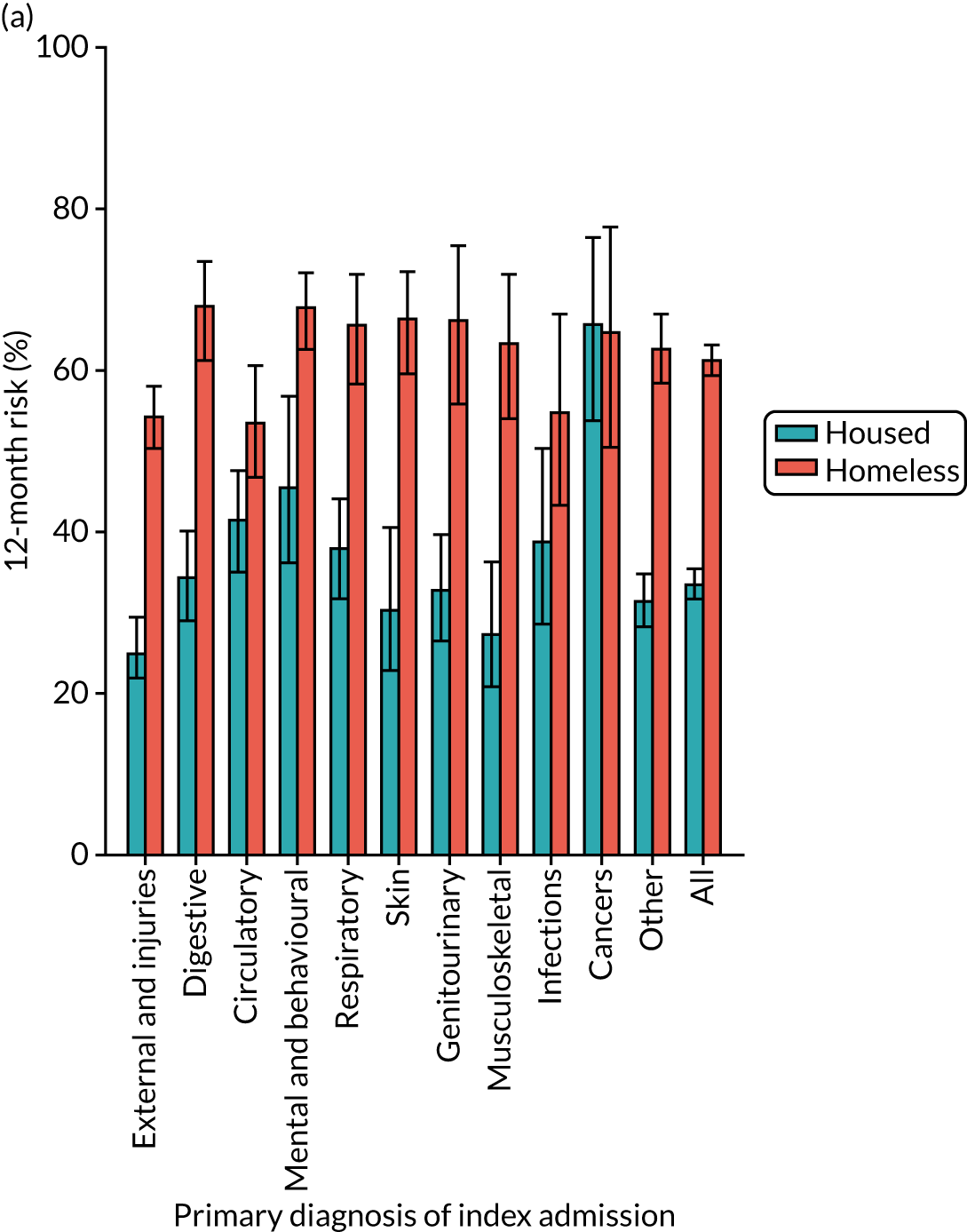

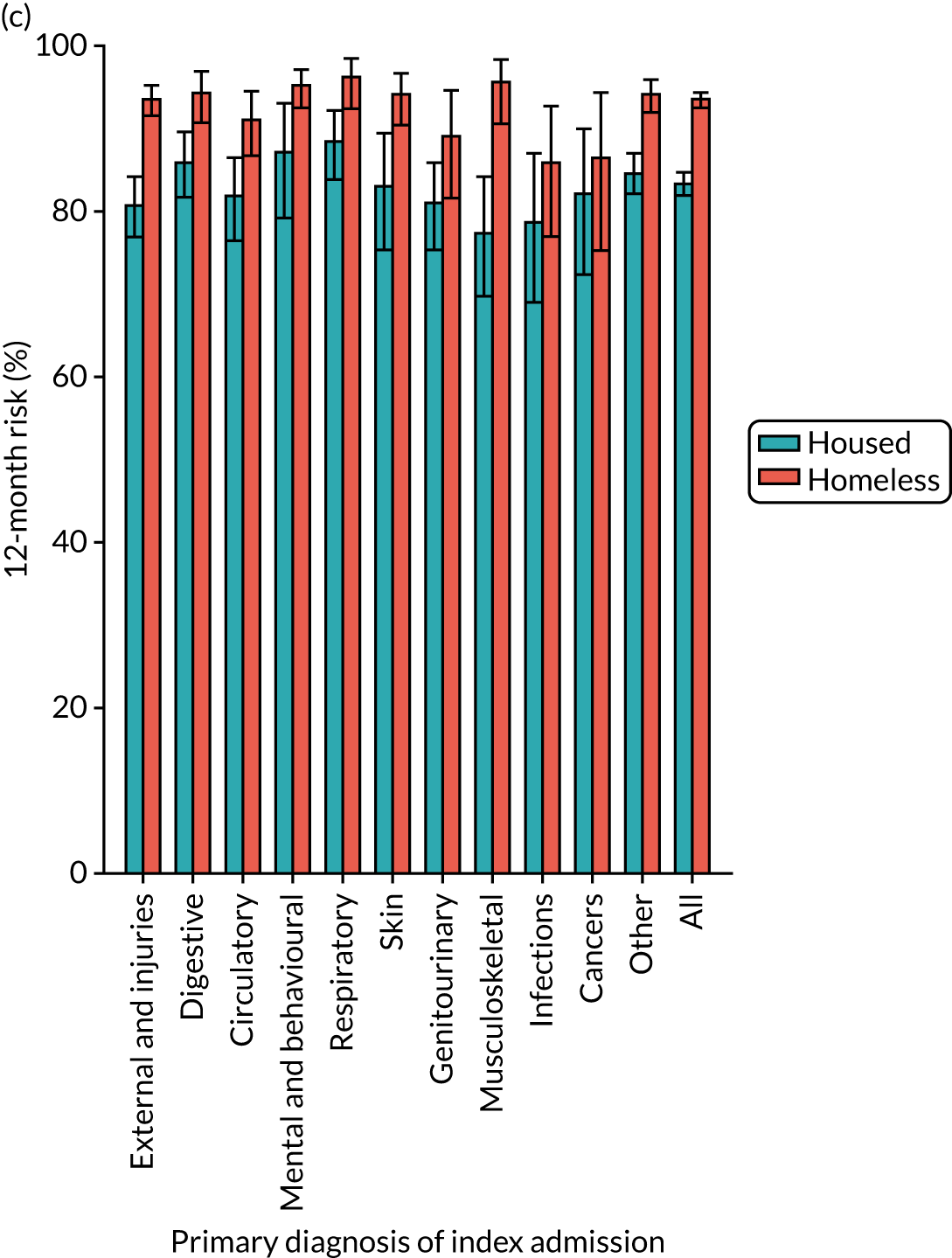
Unplanned and A&E readmissions were extremely high for the HHDS group, and these unplanned readmissions are high regardless of the type of index admission. This is in contrast to the IMD5 group, where the readmission risk was lower than in the HHDS group and varied according to the type of index admission. In addition, the readmission risk was particularly high for those admitted for ‘mental and behavioural’ causes. Planned readmissions were generally lower in the HHDS group than in the IMD5 group.
Unadjusted incident rate ratios from a negative binomial model that examined the risk of readmission showed that homeless patients had 5.14 (95% CI 4.71 to 5.62) times the rate of unscheduled readmission, 1.08 (95% CI 0.95 to 1.23) times the rate of planned readmission and 5.38 (95% CI 5.04 to 5.72) times the rate of A&E visits (Table 14). Adjusting for comorbidities and the ICD-10 chapter of the index admission partially attenuated these values, with adjusted rate ratios of 3.77 (95% CI 3.46 to 4.10), 0.71 (95% CI 0.63 to 0.81) and 3.76 (95% CI 3.53 to 4.01), respectively. As an exploratory sensitivity analysis (not prespecified), we fit the model for planned readmissions, excluding ‘series’ of admission (defined above, mainly for renal failure and dialysis), which gave an unadjusted rate ratio of 0.69 (95% CI 0.62 to 0.78) and an adjusted ratio of 0.62 (95% CI 0.55 to 0.69).
| Outcome | Unadjusted (matched on age, sex, year and hospital), rate ratio (95% CI); p-value | Adjusted for comorbidities and ICD-10 chapter of admissions, rate ratio (95% CI); p-value |
|---|---|---|
| Unscheduled admissions | 5.14 (4.71 to 5.62); < 0.001 | 3.77 (3.46 to 4.10); < 0.001 |
| Planned admissions | 1.08 (0.95 to 1.23); 0.236 | 0.71 (0.63 to 0.81); < 0.001 |
| A&E visits | 5.38 (5.04 to 5.72); < 0.001 | 3.76 (3.53 to 4.01); < 0.001 |
We then constructed negative binomial regressions models to examine the risks of readmission, comparing homeless patients at sites with an associated step-down service with homeless patients at sites without a step-down service (baseline group). Among homeless patients, the rate of unscheduled admissions was similar when comparing those discharged at a site with or without a step-down service, but the rate of planned admissions was 56% lower (incident rate ratio 0.44, 95% CI 0.35 to 0.55; p < 0.001) and the rate of A&E visits was 21% lower (incident rate ratio 0.79, 95% CI 0.71 to 0.87; p < 0.001) (Table 15). These results were partially attenuated when adjusting for comorbidities and the ICD-10 chapter of the index admission. After adjustment, there was evidence that A&E visits were 18% lower among homeless patients discharged at a site with a step-down service than among those without a step-down service (incident rate ratio 0.82, 95% CI 0.75 to 0.91; p < 0.001).
| Outcome | Adjusted for age, sex and year of admission, rate ratio (95% CI); p-value | Further adjusted for comorbidities and ICD-10 chapter of admissions, rate ratio (95% CI); p-value |
|---|---|---|
| Unscheduled admissions | 1.02 (0.92 to 1.13); 0.742 | 1.08 (0.98 to 1.18); 0.102 |
| Planned admissions | 0.44 (0.35 to 0.55); < 0.001 | 0.88 (0.73 to 1.06); 0.140 |
| A&E visits | 0.79 (0.71 to 0.87); < 0.001 | 0.82 (0.75 to 0.91); < 0.001 |
Time from admission to death
In the unadjusted analysis for this outcome, male sex, older age group, larger number of comorbidities and larger number of admissions in the year before index admission were all associated with an increase in likelihood of death (Table 16). In the multivariable analyses, there remained an association only between older age and higher comorbidities. We found no evidence in either the unadjusted or adjusted analyses for a difference between the housing- or clinically led services for death (adjusted HR 1.01, 95% CI 0.84 to 1.21; p = 0.9285). In another adjusted analysis, hazard of death was also higher in the combined HHDS group than in the IMD5 group (HR 2.20, 95% CI 1.98 to 2.44; p < 0.0001) (see Table 12). When comparing schemes with and without step-down care, we found no evidence for a difference in likelihood of death between the two groups (adjusted HR 1.05, 95% CI 0.88 to 1.24; p = 0.6103) (see Table 12).
| Baseline characteristic | Number of events | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | ||
| Cohort group | |||||
| Housing led (n = 1006) | 154 | 1 | 1 | ||
| Clinically led (n = 2888) | 446 | 1.00 (0.83 to 1.20) | 0.9934 | 1.01 (0.84 to 1.21) | 0.9285 |
| Gender | |||||
| Male | 461 | 1 | 1 | ||
| Female | 139 | 0.78 (0.65 to 0.95) | 0.0119 | 0.93 (0.77 to 1.13) | 0.4783 |
| Age group (years) | |||||
| < 25 | <10 | 1 | 1 | ||
| 25–34 | 40–50 | 2.25 (1.02 to 4.98) | |||
| 35–44 | 128 | 5.37 (2.50 to 11.50) | 4.64 (2.16 to 9.98) | ||
| 45–54 | 180 | 7.61 (3.57 to 16.20) | 6.33 (2.96 to 13.55) | ||
| 55–64 | 138 | 11.00 (5.14 to 23.57) | 9.12 (4.24 to 19.65) | ||
| 65–74 | 60 | 12.31 (5.63 to 26.95) | 10.03 (4.54 to 22.14) | ||
| ≥ 75 | 39 | 20.97 (9.39 to 46.82) | < 0.0001 | 19.19 (8.61 to 42.79) | < 0.0001 |
| Number of comorbid chapters | |||||
| 1 or 2 | 35 | 1 | 1 | ||
| 3–5 | 82 | 1.15 (0.78 to 1.72) | 1.13 (0.76 to 1.69) | ||
| 6–9 | 285 | 1.75 (1.23 to 2.49) | 1.61 (1.12 to 2.31) | ||
| 10–15 | 186 | 3.00 (2.09 to 4.31) | 2.58 (1.75 to 3.82) | ||
| > 15 | 12 | 2.89 (1.48 to 5.64) | < 0.0001 | 1.84 (0.85 to 3.95) | < 0.0001 |
| Number of admissions 1 year before index | |||||
| 0 | 369 | 1 | 1 | ||
| 1 | 64 | 1.01 (0.77 to 1.32) | 0.86 (0.65 to 1.13) | ||
| 2 | 56 | 1.62 (1.23 to 2.14) | 1.23 (0.92 to 1.63) | ||
| 3 | 21 | 0.96 (0.61 to 1.49) | 0.81 (0.52 to 1.28) | ||
| 4 or 5 | 31 | 1.11 (0.76 to 1.62) | 0.88 (0.59 to 1.31) | ||
| 6 or 7 | 18 | 1.42 (0.86 to 2.33) | 0.99 (0.59 to 1.64) | ||
| 8 or 9 | < 10 | 0.76 (0.38 to 1.51) | |||
| ≥ 10 | 30–40 | 0.0088 | 1.14 (0.75 to 1.73) | 0.4945 | |
Time from admission to mortality from causes amenable to health care
Male sex, older age group and larger number of comorbidities were all associated with an increase in likelihood of death from causes amenable to health care (Table 17) in the analysis before and after adjusting. We found no evidence in either the unadjusted or adjusted analyses for a difference between the housing- and clinically led services for readmissions (HR 1.02, 95% CI 0.69 to 1.49; p = 0.9383). The HHDS group had a higher hazard of death from amenable causes than the IMD5 group in the adjusted analysis (HR 1.78, 95% CI 1.43 to 2.22; p < 0.0001) (see Table 12). We found no evidence for a difference in likelihood of death between the step-down care group and the no step-down care group (adjusted HR 0.99, 95% CI 0.69 to 1.42; p = 0.9583) (see Table 12).
| Baseline characteristic | Number of events | Median follow-up (days) (IQR) | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |||
| Cohort group | ||||||
| Housing led (n = 1003) | 48 | 1135 (826–1388) | 1 | |||
| Clinically led (n = 2879) | 152 | 1148 (787–1390) | 1.06 (0.73 to 1.56) | 0.7478 | 1.02 (0.69 to 1.49) | 0.9383 |
| Sex | ||||||
| Male | 167 | 1135 (778–1387) | 1 | |||
| Female | 33 | 1170 (862.5–1399) | 0.51 (0.33 to 0.78) | 0.0019 | 0.62 (0.40 to 0.96) | 0.0335 |
| Age group (years) | ||||||
| < 25 | < 10 | 1 | ||||
| 25–34 | 10–20 | 1218 (915.25–1424.5) | 5.69 (0.75 to 43.04) | 5.06 (0.67 to 38.23) | ||
| 35–44 | 39 | 1201 (885–1417.25) | 12.15 (1.67 to 88.48) | 9.93 (1.36 to 72.56) | ||
| 45–54 | 63 | 1178 (840.5–1408.5) | 20.47 (2.84 to 147.52) | 15.70 (2.17 to 113.81) | ||
| 55–64 | 54 | 1110.5 (741–1374) | 33.03 (4.57 to 238.62) | 24.32 (3.35 to 176.74) | ||
| 65–74 | 28 | 1155 (705–1382) | 45.91 (6.25 to 337.22) | 31.70 (4.27 to 235.53) | ||
| ≥ 75 | < 10 | 0 | < 0.0001 | |||
| Number of comorbid chapters | ||||||
| 1 or 2 | < 10 | 1062 (762.75–1314.75) | 1 | |||
| 3–5 | 30–40 | 1029 (736–1307) | 1.93 (0.91 to 4.12) | 1.90 (0.89 to 4.06) | ||
| 6–9 | 82 | 1173 (825–1404) | 1.88 (0.93 to 3.80) | 1.80 (0.88 to 3.68) | ||
| 10–15 | 63 | 1295.5 (867.75–1459.75) | 3.68 (1.80 to 7.53) | 3.51 (1.61 to 7.63) | ||
| > 15 | 12 | 1453.5 (1083.75–1517.5) | 9.72 (3.62 to 26.14) | 0 | 7.94 (2.10 to 30.09) | 0.0029 |
| Number of admissions 1 year before index | ||||||
| 0 | 117 | 1025 (730.25–1275) | 1 | |||
| 1 | 23 | 1399 (1285–1471) | 0.98 (0.58 to 1.65) | 0.84 (0.48 to 1.47) | ||
| 2 | 22 | 1393 (1233.5–1480.5) | 1.66 (0.94 to 2.94) | 1.22 (0.67 to 2.21) | ||
| 3 | < 10 | 0.74 (0.27 to 2.03) | ||||
| 4 or 5 | < 10 | 0.49 (0.20 to 1.22) | ||||
| 6 or 7 | < 10 | 0.45 (0.15 to 1.30) | ||||
| 8 or 9 | < 10 | 0.16 (0.02 to 1.26) | ||||
| ≥ 10 | 18 | 1486 (1287.75–1523.75) | 2.15 (1.21 to 3.82) | 0.0766 | 0.91 (0.37 to 2.24) | 0.2891 |
Summary
Overall, the data linkage results show that HHDSs were engaging with a population with high levels of unmet health-care needs that were often linked to common long-term conditions, such as heart disease, as well as conditions more usually associated with homelessness, such as drug and alcohol misuse. There is some evidence in support of our programme theory about the MIRs that enable HHDSs to deliver their intended outcomes; however, this is not supportive of all elements.
-
We found no evidence of a difference for our primary outcomes between HHDSs that were clinically led and those that were housing led.
-
We found no evidence of a difference for our primary outcomes between HHDSs that did and did not encompass ‘step-down’ intermediate care.
-
In a secondary outcome analysis, we found evidence that A&E visits were 18% lower among homeless patients discharged at a site with step-down service than among those discharged at a site without a step-down service.
-
In the HHDS cohort, regardless of scheme typology, readmission rates increased across the board with increasing comorbidities.
-
After weighting our analyses for age and sex, nearly one-third of deaths in the HHDS cohort were from conditions amenable to health care, suggesting a service shortfall in the HHDS and/or the wider complex adaptive system.
-
When making comparisons between the HHDS group (as a whole) and the IMD5 groups, the HHDS group consistently fared worse. We expected this finding, as we did not expect the HHDSs to improve the health outcomes to that of a deprived housed population. Instead, these results are helpful in terms of providing evidence on the extent of the remaining health gap between those experiencing homelessness and housed populations. Of note is the finding that the HHDS group were more likely than others to be readmitted in an emergency, with five times the rate of unplanned hospital readmission and five times the rate of A&E visits than housed people from deprived neighbourhoods. This was not explained by morbidity, although there is likely to be some residual confounding in which differences in health at the index admission are not captured by long-term conditions identified from previous hospital records (our measure of morbidity). The predominance of emergency rather than planned health care suggests that access to planned care and community support is poor, despite high levels of need.
In the next chapter, we begin to tease out the implications of these quantitative findings for our programme theory by situating them as part of the wider picture ascertained through both the qualitative and economic WPs. In the remainder of this section, we reflect on some of the limitations of the data linkage and how this may have an impact on these results.
Limitations
As described above, when designing the study, we chose the F&T comparator group (for standard care), as we hoped that this would provide a control group of people initially identified as homeless in the community and subsequently admitted to hospitals without HHDSs (i.e. a standard-care comparator). However, with the benefit of hindsight, and our initial descriptive analysis of the data once we received it, we do not feel this to be a fair comparison. For this reason, we do not present results for our primary and secondary outcomes for the F&T comparator group. We were, therefore, not able to undertake a comparative effectiveness analysis that examined the outcomes for people experiencing homelessness admitted to hospitals with a HHDS and those admitted to a hospital without a HHDS.
As noted above, we found no evidence for a difference in our primary outcomes when comparing housing- and clinically led services, or those with step-down service or no step-down service. These findings may be correct, but there remain several important alternative explanations that mean there could still be a difference between these types of service that we were unable to detect. First, we gained data from the sites we planned to and were only slightly under the total number of patients required by our sample size calculation. However, there were more than twice the number of patients in the clinically led sites than in the housing-led sites. Our study is, therefore, underpowered to detect the clinically significant 10% difference in the primary outcomes that we set out to achieve. Taking one of our primary outcomes as an example – readmission owing to any cause – the CI in our final adjusted comparison between housing- and clinically led services (HR 1.07, 95% CI 0.88 to 1.30) is statistically consistent with housing-led services being up to 30% better or up to 12% worse than clinically led services. Our secondary outcome analysis of multiple readmission rates between different types of HHDSs had greater power because of the larger number of events included and it is, therefore, not surprising that this was the one analysis where we found statistical evidence of a difference between different typologies of HHDS for a reduction in A&E admissions. Second, the data we collected were for routine records and, therefore, there may be problems in the recording of outcomes and exposures, which may introduce random measurement error into our analyses, reducing power of the study to detect a difference between the groups further. Third, we were limited in the number of variables we could collect in our analysis on each group and there may be residual confounding in our comparisons. Fourth, there was substantial geographical differences in the way sites were run and the number of patients they saw, with capital city sites seeing larger numbers of patients and being mainly clinically led. This may introduce biases to our analyses in both directions. Finally, we were not always able to identify the date of index admission, therefore limiting our ability identify the exact intervention for each participant, which would further reduce our study power.
Despite these limitations, in being able to compare the effectiveness of different HHDSs, our linkage study had many strengths. The linkage between hospital and death records enabled us to determine long-term outcomes in our groups, which is evidence that has been sorely lacking from this population in England. We present some of the first analysis of the long-term morbidity and mortality outcomes in this socially excluded population and we also describe, in great detail, their health trajectory on admission to hospital and when subsequently admitted or at death.
A further strength of our study is the certainty with which the homeless groups were identified, as these individuals had been seen by services that provide support specifically for people with experience of homelessness. Although ‘no fixed abode’ can be entered as a patient’s address in NHS systems, the use of this coding is inconsistent and, as a result, has limitations as marker of homelessness within HES records. 88
The deaths in this study for the HHDS and IMD5 groups relate to people who have had a hospital admission at centres providing a HHDS service. We were not able to identify patients accessing primary care services, which would be likely to provide an insight into deaths of patients with fewer acute health conditions, but may also include unexpected deaths that occur without prior hospitalisation. The IMD5 comparison group was older and included more women, and we stratified and adjusted our analyses to account for these differences.
The higher levels of deaths owing to alcohol-related causes and drug poisoning in the recent ONS data compared with our study may be as a result of the large number of death records in this study identified from coroners’ reports. Our study is not subject to this potential bias, but we recognise that deaths arising from those admitted under care of HHDSs may also not be representative of all deaths. We have data on deaths for people with experience of homelessness who were admitted to hospital only and, therefore, our results will exclude those people who died having never accessed health care, many of whom may be individuals who die because of external causes. Our results will likely over-represent people with chronic diseases admitted to hospital treatment, compared with the ONS analysis. All methods employed to measure the homeless population have limitations and it is difficult to envisage a method that would provide a fully generalisable population-level estimate for this excluded population. Data linkage for further services that work with homeless people is likely to offer the best opportunities for future research.
Chapter 5 Results: economic evaluation
Background
The primary goal of the economic evaluation (WP3) was to generate evidence to enable further testing of the realist hypothesis outlined earlier in Box 3. The objectives were as follows:
-
to evaluate the effect of specialist HHDSs on access to resources and individual well-being as compared with sites relying on standard provision only (i.e. sites that do not have access to a specialist HHDS)
-
to evaluate the effect of different HHDS typologies and configurations on access to resources and on individual well-being, their attached costs (i.e. health care and mental health services, drug and alcohol services, criminal justice, social care services, housing situation and social benefits) and how effect may vary across schemes in different sites
-
to evaluate any variation in the effect of HHDSs across time.
The economic evaluation comprised three parts. Each part addressed the evaluation objectives through a different data source, employing a range of economic modelling techniques.
Part 1: economic literature review
Part 1 reviewed the economic evidence contained in the individual audit and evaluation reports for the 52 HHDF schemes.
Part 2: evidence for key mechanism resources across 17 homeless hospital discharge schemes
This primary economic evaluation linked HES data to explore the effectiveness and cost-effectiveness of 17 specialist HHDSs (vs. a standard-care control group). The analysis included a comparative focus on HHDSs with different mechanism resources, focusing on two key typologies: (1) clinically led services (i.e. MDTs) compared with housing-led services (i.e. uniprofessional teams) and (2) those with direct access to ‘step-down’ care compared with those without direct access to ‘step-down’ care.
Part 3: focus on three out-of-hospital care configurations
This primary economic evaluation explored the effectiveness and cost-effectiveness of three different ‘out-of-hospital care’ configurations, using three data sources [i.e. published evidence, a survey (see Appendices 7 and 8) and local audit data] in addition to HES data. This considered cost-effectiveness from both NHS and wider public perspectives.
Before introducing the findings linked to each part of the economic evaluation, we outline the methods used for economic modelling. There were some significant protocol changes in the economic evaluation. The main change was linked to the work outlined for part 3 (study of three out-of-hospital care configurations). Although we had planned to collect primary survey data in the seven sites, only one site (site 2) collected sufficient data. In standard-care sites, it was not possible to collect survey data because hospitals without homeless teams did not keep lists of homelessness patients (making their identification for recruitment across the hospital sites difficult). To overcome this problem, we re-recruited the site that had taken part in the pilot for the study. In addition, we drew on primary data from a RCT78 that had studied two HHDSs. We discuss these changes further in Appendices 9 and 10.
Methods
In this section, we outline the economic models used in the evaluation. In part 1, the literature synthesis is followed by an outline of the methods. Table 18 gives an overview of how the economic models were applied across different sections of this present report.
| Part | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Part 2: comparative study of 17 HHDSs – (1) clinically led vs. housing led and (2) schemes with and without step-down care | What is the cost-effectiveness of SIHHC schemes for the NHS? | N/A | N/A |
| Part 3: comparative study of three out-of-hospital care configurations | What is the cost-effectiveness of SIHHC for the NHS? | What is the cost–utility of SIHHC for the NHS? | What is the cost–utility of SIHHC for the broader public perspective? (Limited to evaluation of two configurations) |
Model 1: what is the cost-effectiveness of homeless hospital discharge schemes for the NHS?
Model 1 used HES data to estimate the differential cost and effectiveness of different types and configurations of ‘specialist care’ for the NHS. Incremental cost-effectiveness was calculated in terms of cost per bed-day avoided. Variation in effect was compared with a control group (‘standard care’) and over time. Aggregate estimates98 are reported for the following key performance indicators:
-
number of elective readmissions per homeless patient
-
number of emergency readmissions per homeless patient
-
other readmissions.
Intervention groups (specialist care)
In part 1, 17 HHDSs were recruited and divided into the following intervention groups:
-
clinically led (multidisciplinary) schemes (n = 12)/housing-led (uniprofessional) schemes (n = 5) (vs. standard care)
-
schemes with access to step-down care (n = 9)/schemes with no direct access to step-down care (n = 8) (vs. standard care).
In part 2, the intervention groups were three different out-of-hospital care configurations:
-
A multidisciplinary clinically led (homeless health-care) team that offers patient in-reach and specialist discharge co-ordination, with no direct access to intermediate care. Two examples of this configuration are considered, one situated in a capital city and one in a seaside resort in the south of England.
-
A multidisciplinary clinically led (homeless health-care) team that offers patient in-reach and specialist discharge co-ordination, with direct access to a 14-bed residential step-down unit. Based in an old industrial city in the north of England (described as site 2 in previous chapters). (Note that here, two separate HHDSs are working together in an integrated way in the same locality.)
-
A uniprofessional housing-led scheme that offers (non-clinically focused) patient in-reach and specialist discharge co-ordination, with housing workers providing floating support in the community for a time-limited period (i.e. community step-down care). Based in an old industrial city in the Midlands. (This was an original pilot site for the study and it did not take part in the qualitative case studies.)
Control group (standard care)
In the study protocol, ‘standard care’ was conceptualised by means of two ‘control groups’. These were the same controls as for the data linkage process, described previously:
-
The first proposed control group comprised individuals who were known to be homeless and were admitted to hospital between 1 November 2013 and 30 November 2016 at any one of the 17 participating research sites, but who were not seen by the HHDS operating in that site.
-
The second proposed control group was a sample of individuals who accessed the F&T service. As noted earlier, F&T is a specialist outreach team that works alongside over 200 NHS and third-sector front-line services to respond to the risk and presence of, among homeless people, drug or alcohol users, vulnerable migrants and people who have been in prison. The F&T database included individuals screened for active pulmonary tuberculosis and patients with tuberculosis managed by the service with record dates between September 2007 and July 2010.
Following analysis of the (homeless) patient characteristics data for control groups 1 and 2, it emerged that the homeless individuals who were not seen by a HHDS were generally healthier and, therefore, they did not constitute a comparator group suitable for analysis. To compensate for this, we considered a third control group that was not originally specified in the protocol.
-
This control group comprised patient-level data that were extracted from the RCT conducted by Hewett et al. 78 The RCT had been conducted by a co-applicant of this study, enabling access to the data. The trial compared ‘standard care’ with ‘specialist care’ across two hospital sites in England (London and Brighton). The primary end point was the reduction in length of stay. Predefined secondary end points included the impact on the quality of life, post-discharge accommodation and cost-effectiveness. Homeless people admitted to hospital were randomised to either standard care or the HHDS (a clinically led HHDS with no access to step-down care). Homeless patients assigned to standard care were visited once by a homelessness health nurse and provided with an information leaflet that described local services. The hospital data system provided health-care usage information and questionnaires were used to assess the quality of life using the EuroQol 5 Dimensions (EQ-5D). EQ-5D is a generic measure used primarily by economists to calculate quality-adjusted life-years (QALYs) (see Appendices 7 and 8). In total, 206 homeless people were allocated to specialist care and 204 to standard care. It was estimated that the service delivery or operating costs were £154,228 per year, with salary costs being added to training costs (£11,120). The impact of the intervention on inpatient activity was assessed by comparing the average cost per inpatient spell or period using all spells for which data were available. The trial found no impact on inpatient costs and it compared operating costs of the intervention with the effect on homeless individuals’ health gain, measured in QALYs. At baseline, health-related quality of life was similar across the arms.
Analysis of the (homeless) patient characteristics data (i.e. age, gender and utility in terms of QALYs) for control group 3 found comparable results with what was reported by the groups of homeless users assigned to the present study interventions. Therefore, control group 378 was considered a suitable ‘standard-care’ comparator.
Data sources for the interventions
Part 1
For the 17 HHDSs recruited to the study, unconsented information was ascertained on 3882 patients and this was linked to HES data. Eligible participants were adults aged ≥ 18 years with one or more hospital admissions between 1 November 2013 and 30 November 2016.
Part 2
In configuration 2, there were two HHDSs working together in the same locality, whereas in configuration 1 a single HHDS was in operation. All three of these HHDSs were included in the sample of the 17 schemes above (therefore, conferring access to HES data, as detailed above). Configuration 1 used data for two HHDSs that had previously been ascertained for Hewett et al. ’s78 RCT. This used hospital administrative data rather than HES data.
Methodology for model 1
The primary outcome chosen for the cost-effectiveness analyses was the cumulative duration of hospital stay (i.e. number of bed-days after the index admission). This followed published literature. 78 As noted above, owing to limitations with the originally proposed comparator groups, data from the control group of the RCT study published by Hewett et al. 78 were used as a proxy for ‘standard care’. Unfortunately, standard-care group data did not present any baseline estimates for either the primary outcome or cost data. For this reason, only annual patient-level estimates for bed-days and readmission costs (relating to the follow-up period) were compared between intervention and control groups. The statistical analyses were consistent with the regression approach used by Hewett et al. 78 A regression model was used to analyse the difference in length of stay between groups at follow-up, adjusting for age and sex. We applied bootstrapping to allow for non-normality in the outcome data. The perspective adopted was that of the NHS. The time frame was 1 year (primary analyses) or 3 years,99 based on the assumption that the individual remains homeless and yearly cost and benefit are constant across time.
Cost data were derived from the use of health-care resources (i.e. number of readmissions) and estimates for the intervention group were extracted from HES data (Table 19). The quantities were then multiplied by a set of national average unit costs (Table 20). The total costs of health services were then summarised at an aggregated level (e.g. according to the type of readmission costs) for the corresponding periods. Economic outcomes used for this analysis included (1) elective readmissions per homeless patient, (2) emergency readmissions per homeless patient, (3) other readmissions per patient and (4) all readmissions. Costs were updated to 2017 figures. A regression model (similar to the one adopted for length of stay) was used to analyse any difference in NHS costs between groups at follow-up and was adjusted according to patient characteristics.
| Patient group | Source of data | Number of elective readmissions per patient, mean (SD) | Number of emergency readmissions per patient, mean (SD) | Number of other readmissions per patient, mean (SD) | Number of bed-days per patient, mean (SD) | Number of QALYs per patient, mean (SD) | Number of patients at index discharge, mean (SD) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |||
| Patients discharged without a HHDS (control group) | ||||||||||||
| Homeless patients receiving standard care at discharge | Hewett et al.78 | N/A | 0.16 (1.25) | N/A | 1.25 (2.61) | N/A | 0.13 (0.56) | N/A | 20.8 (2.8) | 0.48 (0.33) | 0.47 (0.2) | 204 |
| Patients discharged with a HHDS | ||||||||||||
| Schemes combined | HES data | N/A | 0.82 (6.83) | N/A | 2.52 (4.68) | N/A | 0.1 (0.48) | N/A | 18.98 (48.38) | N/A | N/A | 3998 |
| Clinically led | HES data | N/A | 0.92 (7.06) | N/A | 2.62 (4.98) | N/A | 0.1 (0.48) | N/A | 18.88 (52.04) | N/A | N/A | 2958 |
| Housing led | HES data | N/A | 0.55 (6.11) | N/A | 2.24 (3.71) | N/A | 0.12 (0.48) | N/A | 19.25 (35.98) | N/A | N/A | 1040 |
| Schemes (n = 17) with and without step-down care | ||||||||||||
| Intervention group 1 schemes offering patient in-reach and discharge co-ordination (with no ‘step-down’ care) | HES data | N/A | 0.98 (7.40) | N/A | 2.55 (4.88) | N/A | 0.1 (0.45) | N/A | 19.23 (53.73) | N/A | N/A | 2688 |
| Intervention groups 2 and 3 schemes offering patient in-reach and discharge co-ordination (with step-down care, either community based or residential) | HES data | N/A | 0.5 (5.45) | N/A | 2.45 (5.26) | N/A | 0.12 (0.53) | N/A | 18.46 (34.93) | N/A | N/A | 1310 |
| Interventions/sites (n = 3) with audit or survey data | ||||||||||||
| Configuration 1 (clinically-led scheme offering patient in-reach and discharge co-ordination with no ‘step-down’ care) | HES data | N/A | 1.62 (12.13) | N/A | 2.47 (4.5) | N/A | 0.12 (0.63) | N/A | 18.24 (34.48) | N/A | [0.56 (0.3) Hewett et al.78] | 703 [269] |
| Configuration 2 (clinically-led scheme offering patient in-reach and discharge co-ordination with residential step-down care) | HES data | N/A | 0.31 (0.81) | N/A | 2.99 (5.38) | N/A | 0.13 (0.8) | N/A | 15.90 (32.34) | N/A | [0.64 (0.22) project survey data] | 340 [50] |
| Configuration 3 (clinically-led scheme offering patient in-reach and discharge co-ordination with community-based step-down care) | HES data | N/A | 0.23 (1.23) | N/A | 2.21 (3.9) | N/A | 0.15 (0.47) | N/A | 0.9 (1.7) | N/A | [0.75 (0.11) project audit data] | 188 [70] |
| Type of cost | Intervention group 1 (configuration 1)/intervention group 2 (configuration 2) | Intervention group 3 (configuration 3) | Unit cost (£) (2017) | Source of unit costs |
|---|---|---|---|---|
| Health-care costs | Hospital admissions (average) | Hospital admissions (average) | 1783 | PSSRU 2017100 |
| Elective inpatient stays | Elective inpatient stays | 3903 | PSSRU 2017100 | |
| Emergency admissiona | Emergency admission | 1074 | PSSRU 2017100 | |
| Visits to A&E | Visits to A&E | 157 | PSSRU 2017100 | |
| Hospital outpatient attendances | Hospital outpatient attendances | 137 | PSSRU 2017100 | |
| GP visits (GP contact per patient contact lasting 9.22 minutes) | GP visits (GP contact per patient contact lasting 9.22 minutes) | 38 | PSSRU 2017100 | |
| N/A | 999 ambulance (average of all callouts) | |||
| Mental health-care costs | Admission to a mental health hospital (mental health-care clusters per day) | N/A | 404 | PSSRU 2017100 |
| Contact with mental health community provision [mental health specialist teams (per care contact)] | N/A | 172 | PSSRU 2017100 | |
| Stay in a local authority care home for people with mental health problems (average duration 4 × 12 weeks) | N/A | 786 | PSSRU 2017100 | |
| Access to local authority social services day care for people with mental health problems | N/A | 35 per client attendance | PSSRU 2017100 | |
| N/A | Mental health services for the 1 year (average based on Derby data) | 2670 | PSSRU 2017100 | |
| Drug and alcohol treatment costs | Substitute prescriptions (methadone) | N/A | 55 a week | Gossop et al.101 |
| Detox and rehab centre stay | N/A | Average 417 | PSSRU 2017100 | |
| One-to-one contacts with a drug/alcohol treatment team | N/A | Average 125 | PSSRU 2017100 | |
| Group session contacts with a drug/alcohol treatment team | N/A | Average 16 | PSSRU 2017100 | |
| N/A | Drug and alcohol treatment services for 1 year (average based on Derby data) | 1061 | PSSRU 2017100 | |
| Housing costs | Rough sleeping | Rough sleeping | 7900 | Ashton and Hempenstall102 |
| Direct access hostel (night) | N/A | 48 | Ashton and Hempenstall102 | |
| Second-stage supported accommodation (semi-independent accommodation) | N/A | 27 per night | Battrick et al.103 | |
| Own social tenancy | N/A | 69 per week | Average from MEAM103 | |
| Own private rented sector tenancy | N/A | 100 per week | Average from MEAM103 | |
| Room in shared private rented sector property | N/A | 65 per week | Average from MEAM103 | |
| N/A | Homelessness investigation and decision | 6639 | Shelter104 | |
| Criminal justice costs | Arrest by police | N/A | 2130 | Cabinet Office Social Exclusion Task Force105 |
| Other police contact | N/A | 17 | Home Office106 | |
| Magistrate court attendance | N/A | 995 | Average from MEAM103 | |
| Crown court attendance | N/A | 11,245 | Average from MEAM103 | |
| Nights in prison/nights in police custody | N/A | 75 | Average from MEAM103 | |
| Social care costs | Comprehensive clinical assessment | N/A | 55 | PSSRU 2017100 |
| N/A | Occupational therapy assessment | 35 | PSSRU 2017100 | |
| Visit with social worker | Visit with a social worker | 55 | PSSRU 2017100 | |
| Night in residential care | Night in residential care | 543 per week | PSSRU 2017100 | |
| Social benefits | Employment and Support Allowance | N/A | 73.10 per week | Benefits entitlement |
| GOV.UK | ||||
| Personal Independence Payment | N/A | 57.30 per week | Benefits entitlement | |
| Daily living standard rate | GOV.UK | |||
| Disability Living Allowance for adults | N/A | 57.30 per week | Benefits entitlement | |
| Frequent help or constant supervision during the day, supervision at night or someone to help you while on dialysis | GOV.UK | |||
| Universal credit | N/A | 317.82 per month | Benefits entitlement | |
| GOV.UK | ||||
| State pension | N/A | N/A | 125.95 per week for those reaching state pension age before April 2016 | Benefits entitlement |
| GOV.UK | ||||
| Service delivery costs | Configuration 2 site delivery costs were calculated using costing information collected from the site | Service delivery costs were calculated using costing information collected from the site | See Table 5 | Hewett et al.78 Local site data |
A cost-effectiveness analysis enumerated the additional resources consumed for an improvement in the effects (i.e. avoided bed-days) associated with the intervention groups, compared with standard care. The difference in mean 12-month costs and outcomes were estimated based on the model. Incremental cost-effectiveness ratios (ICERs) were calculated by dividing the difference in mean cost by the difference in mean health outcome.
One-way sensitivity analyses were conducted to assess the impact on the base-case results. With the first sensitivity analysis, the service delivery costs were taken into consideration (along with all readmissions costs). In addition, to test the impact of the intervention when shifting costs from non-elective to elective readmissions, we added a second sensitivity analysis where we separately explored elective readmissions costs (together with the service delivery costs) and non-elective readmissions costs (together with the service delivery costs). Additional scenario analyses for the economic model included the following: bed-days avoided for the comparator were increased to the upper-limit 95% CI and the total costs of the comparator were equal to the lower-limit 95% CI. To investigate the effect of the HHDSs across time, a follow-up period of 3 years was considered. (Three years was used to represent the medium-term follow-up period as reported by Crisis. 99) For the latter, the recommended discount rate of 3.5% was applied to both costs and benefits. A probabilistic sensitivity analysis was performed to assess the uncertainty in the economic model outputs associated with the uncertainty in parameter inputs. A non-parametric bootstrap technique was employed to explore the uncertainty of point estimates of the difference in mean 12-month costs and outcomes from primary analyses. The results from bootstrap resampling were used to construct 95% CIs for incremental costs and incremental bed-days avoided and to plot the cost-effectiveness plane and cost-effectiveness acceptability curve to show the uncertainty surrounding the primary results.
Data derived from the cost-effectiveness analysis were used to estimate the budget impact of replacing usual care when adopting the various interventions. For each intervention, we calculated the rate of return for the investment made:
Model 2: what is the cost–utility of homeless hospital discharge schemes for the NHS?
Model 2 considers the cost–utility of HHDSs for the NHS. This economic model is similar to economic model 1, but the measure of benefit used was represented by QALY gains (instead of bed-days avoided). The analyses followed a controlled comparative approach and allowed us to estimate the comparative cost-effectiveness of three different specialist configurations compared with standard care. QALY gain from morbidity and mortality averted was also examined.
Intervention groups (specialist care)
The need for both HES and EQ-5D data to facilitate this analysis meant that we could not include all 17 HHDSs, but instead had to focus opportunistically on those schemes for which EQ-5D data were available. This led us to focus on the three out-of-hospital care configurations, as outlined above.
Control group (standard care)
The control group used is the same as for model 1 (i.e. control group 3).
Data sources
In addition to HES data and hospital data (as outlined for model 1), the following additional data sources were employed in model 2:
-
Configuration 1 – a member of our research team had recently completed a RCT of two homeless health-care teams employing EQ-5D at two time points. We were able to draw on this EQ-5D data, which conferred access to 206 T1 completions and 56 T2 completions (at 6 weeks post discharge).
-
Configuration 2 – in this fieldwork site we were able to meet the target for EQ-5D questionnaire completions. Here we accessed 64 completions at T1 and 54 at T2 (at 3 months post discharge).
-
Configuration 3 – this site worked with us in the pilot phase of this present study and was collecting EQ-5D data as part of its own internal monitoring and review procedures. From this site, we accessed 84 completions at T1 and 84 at T2 (at 12 months post discharge).
In total, drawing on these different data sources, we accessed 354 EQ-5D completions at T1 and 248 at T2.
Methodology for model 2
Although Hewett et al. 78 did not collect any (retrospective) baseline data for the length of stay and use of health-care resources (i.e. emergency, elective and other types of admissions), they reported both baseline and 12-month follow-up data for EQ-5D scores. A regression model was used to enable differences in EQ-5D score at follow-up to be adjusted for patient characteristics (i.e. age and sex) and for differences in outcome at baseline (see Hewett et al. 78). The tariff for each combination of the EQ-5D levels for the UK population was applied to calculate utility values. 107 QALYs were then calculated over the duration of the economic model using the area under the curve of utility values from the three time points. 108 For the primary analyses, costs and QALYs were not discounted because the assessing period was 12 months. For the 3-year economic model, a discount rate of 3.5% was applied.
Cost outcomes were the same as reported for economic model 1. Costs were updated to 2017 figures. Cost and effectiveness estimates were calculated for a 1-year follow-up period and a 3-year follow-up period (with costs discounted at 3.5% per annum).
The ICER was calculated by dividing the incremental costs (mean intervention minus mean control) by the incremental QALY (mean intervention minus mean control). 109 The intervention is considered cost-effective if the ICER falls below the NICE threshold of £20,000–30,000 per QALY. The cost-effectiveness acceptability curve presented the impact of uncertainty on the result of an economic evaluation. It was produced by resampling the data 1000 times to generate a mean cost and life-year or QALY gain from each group, using a non-parametric bootstrap approach. 110 The proportion of resampled data sets for which the calculated ICER lies below a given threshold is interpreted as the probability that the ICER of the intervention is below that threshold. Cost of the service delivery was not included in the main analyses, but was included in the sensitivity analyses (and this followed the same approach considered for economic model 1). Both the one-way sensitivity analysis and the probabilistic sensitivity analysis were similar to the above (see economic model 1).
This economic model allowed us to measure the cost-effectiveness of two different out-of-hospital care configurations ‘before and after’ their introduction. Observed differences in performance are assumed to be because of the intervention. This economic model also took a wider public sector perspective (e.g. exploring costs for use of health care, mental health care, drug and alcohol treatment, housing, criminal justice, social care, social benefits and state pension). It replicated the approach used in the Making Every Adult Matter (MEAM) evaluation. 111 In the UK, the MEAM pilot programmes aimed to understand the economic impact of specialist provision targeted at a similar multiple needs cohort where homelessness was the most significant issue. Therefore, the MEAM pilot study provided an already tested methodology for understanding the economic impact of the specialist provision on service use across the whole system.
Intervention groups (specialist care)
The configurations that could be evaluated were limited to two because these were the only sites where it was possible to collect service delivery costs:
-
Configuration 2 – multidisciplinary clinically led (homeless health-care team) scheme that offers patient in-reach and specialist discharge co-ordination, with direct access to a 14-bed residential step-down unit. Based in an old industrial city in the north of England. (Note that here, two separate HHDSs are working together in an integrated way in the same locality.)
-
MIR1 + MIR2mdt + MIR3mdt + MIR4res + MIR5.
-
-
Configuration 3 – uniprofessional housing-led scheme that offers (non-clinically focused) patient in-reach and specialist discharge co-ordination, with housing workers providing floating support in the community for a time-limited period (i.e. community step-down care). Based in an old industrial city in the Midlands.
-
MIR1 + MIR2up + MIR3up + MIR4hf.
-
Control group (standard care)
No control group was used in this model. This economic model allowed us to measure the cost-effectiveness of the HHDS ‘before and after’ the introduction of the intervention in the same study site(s).
Data sources
-
Configuration 2: in this fieldwork site we were able to meet the target for EQ-5D questionnaire completions. Here, we accessed 64 completions at T1 and 54 at T2 (at 3 months post discharge).
-
Configuration 3: this site worked with us in the pilot phase of the study and was collecting EQ-5D data as part of its own internal monitoring and review procedures. From this site, we accessed 84 completions at T1 and 84 at T2 (at 12 months post discharge).
Methodology for model 3
The measure of utility was gain in QALYs. Annual cost estimates were reported from health-care and larger public provider perspectives. Outcomes included use/cost of health-care and utility data (QALYs). Costing data included hospitalisation and A&E visits. Costs were updated to 2017 figures. Unit costs are reported in Table 20. For each configuration, effectiveness was expressed as QALYs gained (compared with the care available prior to the project starting). Cost-effectiveness was reported as costs to be invested per QALY gained (ICERs). The time frame was 1 year. Service delivery costs were calculated using costing information collected from the site.
The robustness of the economic model was tested using one-way deterministic sensitivity analyses looking at the following alternative scenarios: no service delivery, service delivery costs increased by 10%, service delivery costs increased by 20%, mean hospitalisation cost at follow-up equal to the upper-limit 95% CI, mean housing costs at follow-up equal to the upper-limit 95% CI and mean QALY at follow-up equal to the lower-limit 95% CI.
In addition, probabilistic sensitivity analyses were undertaken and CIs for the cost per QALY gained were estimated using the non-parametric percentile bootstrap method. The data were resampled 1000 times to generate a mean cost and life-year or QALY gain from each point of interest, and the resulting ICERs were calculated and plotted into the cost–utility plane. A cost–utility acceptability curve was also plotted. The economic model was tested using data from a subgroup of patients of the HHDS in configuration 3 as part of piloting in preparation for the main study modelling (see Report Supplementary Material 1). Summary information providing an overview of the different models is presented in Report Supplementary Material 2.
Part 1: economic literature review
Overview
In this section, we report the findings of a review of the economic data that were contained in the audits and evaluation reports that had already been published for the 52 HHDSs. Papers for the economic review were identified through the main literature synthesis (reported in Chapter 2). Overall, 39 (57.35%) studies from the main synthesis were relevant for this focused review. Inclusion criteria were that studies had reported on socioeconomic impact and quality-of-life data. Table 21 presents a summary of the papers and considers (1) the quality of the evidence, (2) the economic outcomes measured and (3) the main findings for the cost-effectiveness of different HHDSs. Reports were available for 31 different HHDSs (some schemes were evaluated more than once), representing the following typological configurations:
-
discharge co-ordination with no step-down care/limited community follow-up (11 services)
-
discharge co-ordination with residential (bed-based) step-down care (three services)
-
discharge co-ordination with community (floating support) step-down care (eight services)
-
discharge co-ordination with residential and community step-down care (nine services).
| Hospital discharge scheme | Papers reviewed | Sources used | Type of economic evaluation and key economic outcomes | Key results (compared with before/standard care) | Quality of the economic evidence | |
|---|---|---|---|---|---|---|
| Discharge co-ordination with no step-down care/limited community follow-up | ||||||
| 1 |
HHDS – Julian House, Bath Study scheme reference: [D111] |
4 | Julian House, Bath, UK, 2015, personal communication | Cost comparison analysis, NHS secondary care costs | Cost saving | Satisfactory |
| 2 |
Time to Heal – Elim Housing, Gloucester Study scheme reference: [HHDF/D056] |
2 | ||||
| 3 |
King’s Health Partners Pathway Homeless Team, London Study scheme reference: [D108] |
4 | Dorney-Smith et al.;50 Hewett and Dorney-Smith112 and Dorney-Smith113 | Cost comparison analysis, use/cost of secondary care resources | The service was able to make cost savings for the commissioning CCG by reallocating the charging of clients who are registered on the hospital system as having no fixed abode or GP | Satisfactory |
| 4 |
Pathway Discharge Schemes based at Royal London [D103] and Brighton Hospitals Study scheme reference: [D104] |
2 | Hewett et al.78 | Cost-effectiveness analysis, use/cost of secondary care resources, EQ-5D (utility estimates) | Pathway approach improves the quality of life of homeless people and reduces street homelessness. The increased quality of life cost per QALY was £26,000 | Satisfactory |
| 5 |
North Middlesex University Hospital (Pathway) Homeless Discharge Team Study scheme reference: [D113] |
1 | Burnett and Doherty114 | Service delivery cost evaluation, service delivery costs | The service provision costed £48,000 for 6 months (North Middlesex University Hospital Pathway Pilot July to December 2014) | Not satisfactory (methods not reported/partially reported) |
| 6 |
Pathway, Manchester (mpath) Study scheme reference: [D105] |
3 | mpath115 | Use of comparison analysis in health-care resources, use of secondary care resources |
Change in costs not estimated Housing outcomes were improved |
Not satisfactory (methods not reported/partially reported) |
| 7 |
Homeless Patient Pathway Trident Reach, Birmingham Study scheme reference: [HHDF/D093] |
1 | Trident Reach116 | Use of comparison analysis in health-care resources, use of secondary care resources, social value (ROI) estimates | Reduced length of stay in hospital, best use of resources and cost savings, avoided readmissions | Not satisfactory (methods not reported/partially reported) |
| 8 |
Hospital to Housing Support Service Bournemouth Study scheme reference: [HHDF/D078] |
1 | Housing Learning and Information Network61 | Use/cost comparison analysis, readmission rate, readmission costs | Cost savings due to readmission rates | Not satisfactory (methods not reported/partially reported) |
| 9 |
Hospital to House, Wigan Brick Study scheme reference: [D095a] |
2 | ||||
| 10 |
Homeless Accommodation Leeds Pathway HALP, CRI Study scheme reference: [HHDF/D052A] |
1 | ||||
| 11 |
Integrated Hospital Discharge Service, Framework, Nottingham Study scheme reference: [HHDF/D011] |
1 | Framework Housing Association, Nottingham, UK, 2014, personal communication | Use of comparison analysis in health-care resources, hospital admission rates only | Change in use of resources not estimated | Not satisfactory (methods not reported/partially reported) |
| Discharge co-ordination with residential step-down care | ||||||
| 12 |
Breathing Space, Two Saints Ltd., Southampton Study scheme reference: [HHDF/D005] |
2 | ||||
| 13 |
Homeless Intermediate Care Pilot Project, Cedars Road Hostel, Clapham Study scheme reference: [D112] |
3 | Hendry64 | Cost comparison, consequences analysis, use of secondary care resources, NHS secondary care costs, EQ-5D (utility estimates) | Cost saving | Satisfactory |
| 14 |
BRICSS, Horton Housing Study scheme reference: [HHDF/D007] integrated with Bradford Pathway [D102] Bevan Health |
3 | Lowson and Hex;117 Hewett and Dorney-Smith112 and Trident Reach;116 Julian House, 2015, personal communication; Framework Housing Association, 2014, personal communication, and Pathway Team, Bradford, UK, 2017, personal communication | Use/effectiveness comparison analysis in health-care resources, use of secondary care resources, secondary care costs (A&E, admission, bed-days), discharge outcomes, social value (ROI) estimates |
Comparison of NHS costs before and after: cost saving ROI: even under the most conservative assumptions, every £1 invested in each of these services generates at least £1.50 worth of benefit and under less conservative (but entirely realistic) assumptions as much as £8 worth of benefit |
Satisfactory |
| Discharge co-ordination with community step-down care | ||||||
| 15 |
Homeless Hospital Discharge Project Coventry and Cyrenians Midland Heart Study scheme reference: [HHDF/D023/D048] |
1 | Danahay118 | Use analysis in health-care resources, cost analysis pre scheme | Reduced A&E visits, reduced hospital admissions | Not satisfactory (methods not reported/partially reported) |
| 16 |
From Hospital to Community – Thames Reach Housing, Croydon Study scheme reference: [HHDF/D042] |
2 | Thames Reach119,120 | Use of analysis in health-care resources |
No comparator Change in costs not estimated |
Not satisfactory (methods not reported/partially reported) |
| 17 |
Hospital to Home, Hammersmith and Fulham, Broadway St Mungo’s, London Study scheme reference: [HHDF/D039] |
1 | ||||
| 18 |
Hospital Community Link, Brighter Futures, North Staffordshire Study scheme reference: ran two schemes, one in Stoke [HHDF/D019] and one in Tamworth [HHDF/D021] |
3 | Brighter Futures (Stoke)121 and Tamworth Borough Council and South East Staffordshire and Seisdon Peninsular Clinical Commissioning Group (Tamworth)122 | Use of analysis in health-care resources, use of secondary care resources, figures not presented |
Reduced readmissions Reduced presentations at A&E Figures not presented |
Not satisfactory (methods not reported/partially reported) |
| 19 |
H4 Hospital, H3 Stockpot Study scheme reference: [HHDF/D034] |
2 | H3, Stockport, UK, 2014 and 2017, personal communication | Use of analysis in health-care resources, use of secondary care resources, public sector costs (case study analysis) | Change in costs not estimated | Not satisfactory (methods not reported/partially reported) |
| 20 |
Derby Healthy Futures, Derventio Housing Trust, Derby Study scheme reference: [HHDF/D060] |
8 | Gillespie48 and Derventio Housing Trust, Derby, UK, 2014 and 2015, personal communication | Use/effectiveness comparison analysis in health-care resources, use of secondary care resources, secondary care costs, social value (ROI) estimates, EQ-5D (utility estimates) | Reduced avoidable admissions, improved quality of life, reduced A&E presentations, reduced length of stay, increased social value | Not satisfactory (methods partially reported) |
| 21 |
Bay 6, Community Housing Aid, Exeter Study scheme reference: [HHDF/D054] |
2 | Charles et al.54 | Use/cost comparison analysis, use of secondary care resources, secondary care costs | Saving in secondary care costs | Satisfactory (methods reported) |
| 22 |
Homeless Hospital Discharge Project, Wirral Study scheme reference: [D109] |
1 | White82 | Cost comparison analysis, bed-days, admission rates, emergency rates, secondary care costs | Reduced bed-days, numbers of admission and emergency readmission, saving in total secondary care costs | Not satisfactory (methods partially reported) |
| Discharge co-ordination with residential and community step-down care | ||||||
| 23 |
Aftercare Set-up Project Trinity, Winchester Study scheme reference: [HHDF/D010] |
1 | Trinity Winchester123 | Financial activity analysis | ||
| 24 |
Hospital Discharge Project and Cornwall Intermediate Care and Recovery Facility, St Petrocs, Cornwall Study scheme reference: [HHDF/D020a/b] |
1 | Shelter and Coastline Housing124 | Use of analysis in health-care resources | No comparator, change in costs not estimated | Not satisfactory (methods not reported/partially reported) |
| 25 |
Navigation and Respite Project Newcastle, Changing Lives/Cyrenians Study scheme reference: [HHDF/D057] |
1 | Aitchison125 | Use analysis in health-care resources, use of secondary care resources | Change in use/costs not estimated | Not satisfactory (methods not reported/partially reported) |
| 26 |
Navigation and Respite Project Sunderland, Changing Lives/Cyrenians Study scheme reference: [HHDF/D062] |
1 | Aitchison125 | Comparison before and after, use analysis in health-care resources, use of secondary care resources, public sector costs (case study analysis) | Costs before and after: costs to the public providers in the 6 months previous to users accessing the service and in the last 6 months where the user is engaged. Results not clearly reported | Not satisfactory (methods not reported/partially reported) |
| 27 |
Basis Beds, Aquila Way, Gateshead Study scheme reference: [HHDF/D090] |
1 | ||||
| 28 |
Discharge Initiative, First Stop, Darlington Study scheme reference: [HHDF/D092] |
1 | ||||
| 29 |
The Hospital to Housing Support Service, Plymouth Study scheme reference: [HHDF/D037a] |
3 | Housing Learning and Information Network;61 SERI Insight79 and Copeman et al.126 | Use of comparison analysis in health-care resources, hospital readmission rates only | The data available do not provide sufficient information to quantify the savings in bed-stays and readmissions | Not satisfactory (methods not reported/partially reported) |
| 30 |
Liverpool City Region Hospital Discharge Project, The Whitechapel Centre, Liverpool Study scheme reference: [HHDF/D025] |
8 | Ubido et al.127 | Use of health-care resources, use of secondary care resources | Change in use/costs not estimated | Not satisfactory (methods not reported) |
| 31 | Evaluation of 52 discharge schemes funded through HHDF | 1 | Homeless Link70 | Cost–consequences analysis |
69% of patients were discharged into suitable accommodation out of total discharges 55% of patients received health support on discharge 58% of patients received housing support on discharge Of those patients admitted into the hospital, only 28% were readmitted within 30 days of a prior admission |
Satisfactory (methods reported) |
| Total | 68 (100%) | 39 (57.35%) | ||||
One additional paper (reporting the findings of early evaluation of the HHDF) reported on the service delivery costs for all HHDSs. 70 This reported that the average cost per client across all projects that returned expenditure and outcomes data was £2543. This did not consider effectiveness and cost-effectiveness.
Results
The findings from the economic literature review are presented in Figure 9:
-
Twenty-one of 39 papers (53.84%) were rated as having good-quality data.
-
Nineteen of 39 papers (48.72%) demonstrated economic benefit in terms of decreases in the use of health-care services and NHS economic savings, and societal benefit in terms of return in social value, and three papers demonstrated improved health and well-being of individuals (EQ-5D data).
-
In this review, the most methodologically robust evidence is for HHDSs with access to residential ‘step-down’ care. These schemes are shown to be both cost-effective and cost saving:
-
The Economic Evaluation of Homeless Intermediate Care Pilot Project reported that the intervention delivered by Cedars Road Hostel (Clapham) was cost saving. 64 This service is clinically led.
-
One configuration, encompassing the integration of a clinically led HHDS with a residential step-down unit, was able to show that under the most conservative assumptions every £1 invested in each of these services generates at least £1.50 worth of benefit (wider public perspective) and under less conservative (but realistic) assumptions as much as £8 worth of benefit was generated (again, wider public perspective). 117
-
FIGURE 9.
Economic evidence from the literature: per cent of papers reporting information on the economic evaluation conducted, the data sourced and the economic results. ROI, return on investment.
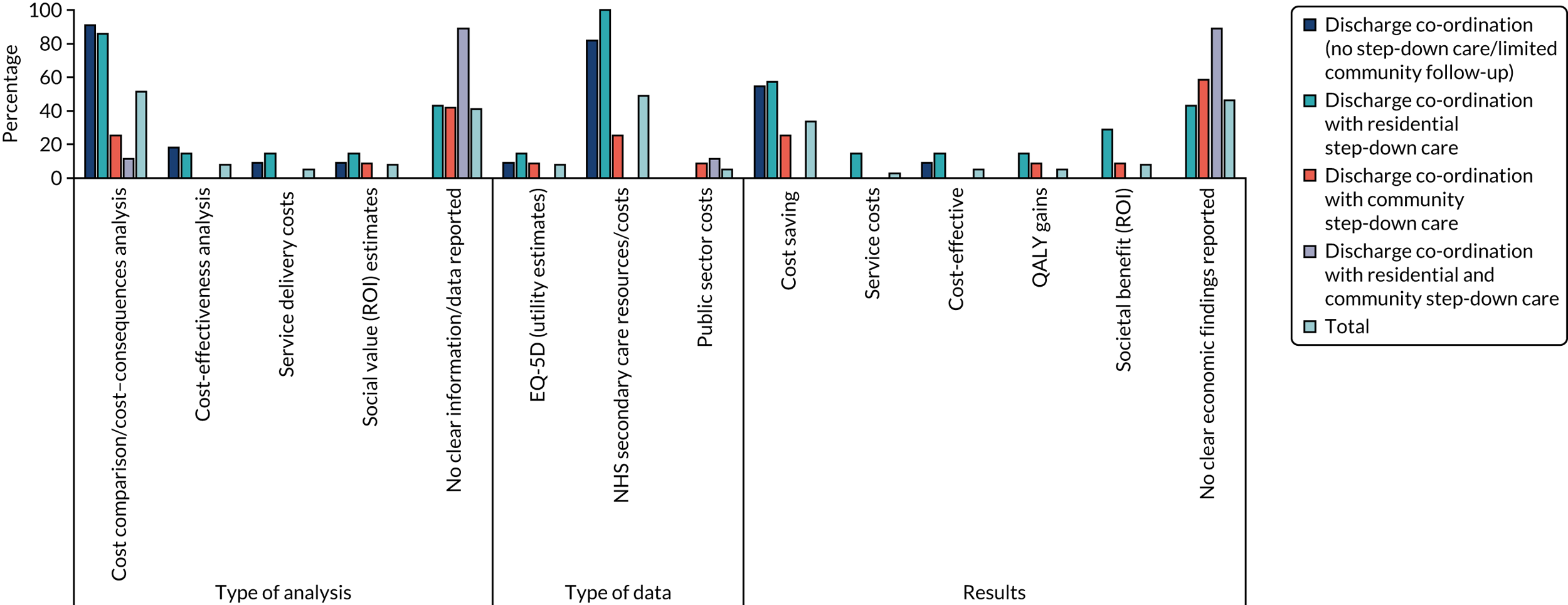
Implications for realist hypothesis testing
-
The review of the published literature alerted us to an emerging evidence base that ‘step-down’ intermediate care is both cost-effective and cost saving. However, there is also strong evidence to suggest that schemes without this component can be cost-effective and cost saving. These findings might, therefore, be taken as a broad indication of the likely benefits of specialist care per se.
-
Our theory does not currently distinguish between different types of step-down [residential and home-based (floating support)] care and our findings suggest that this may be an important consideration.
-
Clinically led MDT working is a key component in examples of (residential) step-down intermediate care that are cost-effective and cost saving.
Limitations of economic literature review
The main limitation of this preliminary analysis (drawing on grey literature and evaluations of individual schemes) is that many HHDSs and their evaluations are not reporting robust economic outcome data. There is a notable lack of economic evidence for schemes offering community (housing-led) step-down care and schemes with access to both community and residential step-down care. As a result, this may bias the result towards certain schemes.
Part 2: evidence for key mechanism-resources across 17 homeless hospital discharge schemes
Overview
This section reports the findings of a primary economic evaluation using linked HES data to explore the effectiveness and cost-effectiveness of 17 specialist HHDSs (vs. a standard-care control group). The analysis includes a comparative focus on HHDSs with different mechanism resources, focusing on two key typologies: (1) clinically led services (i.e. MDTs) compared with housing-led services (i.e. uniprofessional teams) and (2) those with direct access to ‘step-down’ care compared with those without direct access to ‘step-down’ care.
Results
The effect of homeless hospital discharge schemes on health-care resources and costs
Table 19 gives an overview of the number of patients (at index discharge), completed admissions and bed-days in the 1 year after discharge, by HHDS intervention type and for the control group.
Costs per patient for each readmission
The difference in annual NHS costs per patient for a range of readmission types (e.g. elective readmissions, emergency readmissions, other readmissions and costs for all admissions) is shown in Figure 13. Considering all readmissions, homeless patients in the specialist HHDS intervention group used more resources. These patients had higher rates of readmissions and increased hospital costs.
The difference in annual NHS costs per patient (vs. standard care) were greater for clinically led schemes than for ‘housing-led’ schemes (£3112.02 vs. £1295.45; p < 0.01) and for schemes with no ‘step-down’ care than for schemes with ‘step-down’ care (£3271.02 vs. £1325.84; p < 0.01) (Figure 10).
FIGURE 10.
Economic model 1: difference in annual NHS costs per patient (vs. standard care from Hewett et al. 78). All readmissions [i.e. readmitted for the same problem (e.g. within 28 days)] included the sum of elective, emergency and other readmissions. Comparison 1: clinically-/housing-led schemes (vs. standard care) (based on data for 17 schemes). Comparison 2: schemes with/without ‘step-down’ care (vs. standard care) (based on data for 17 schemes).
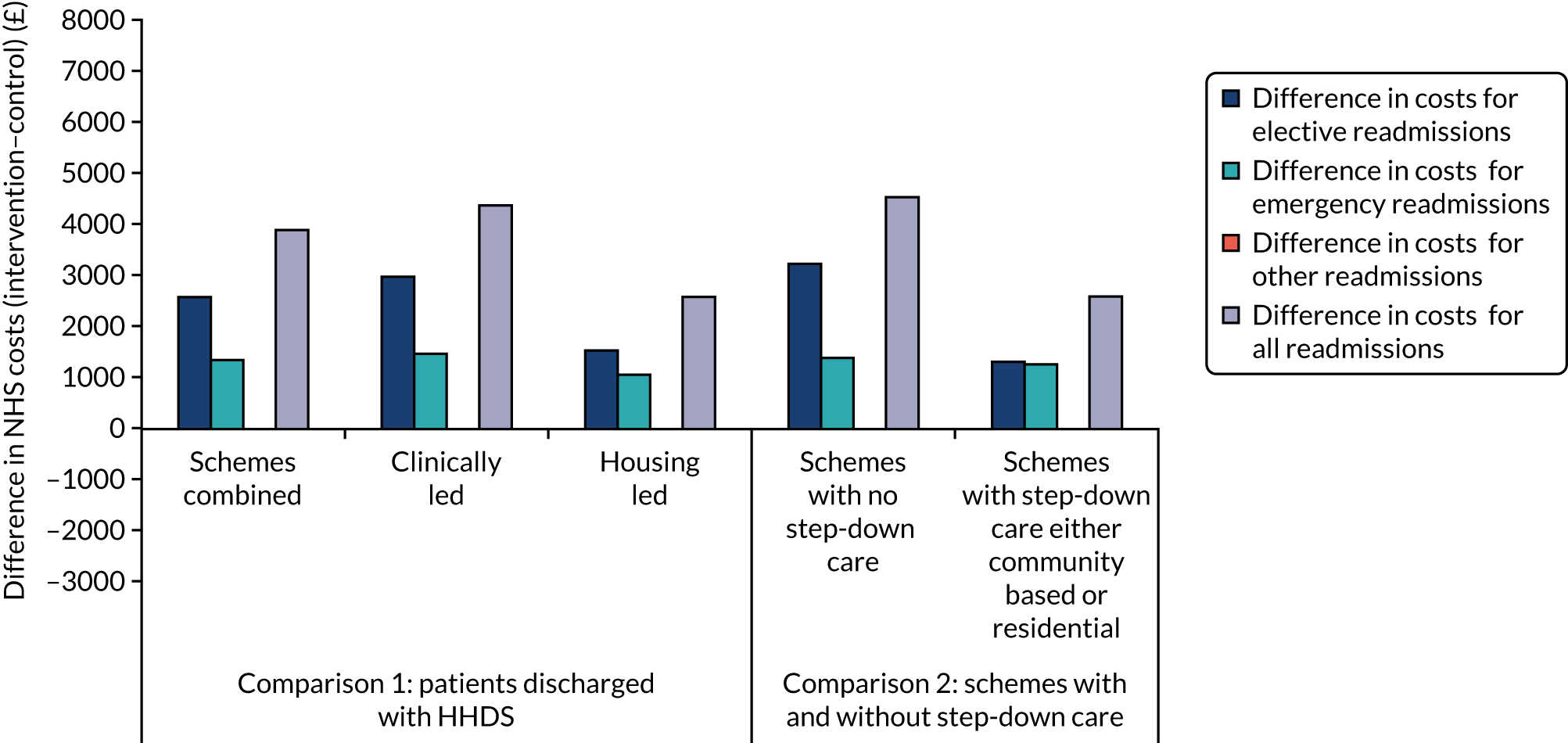
Clinically led schemes reported higher costs for elective readmissions than housing-led schemes (for which there was a cost saving).
Schemes with no ‘step-down’ care reported higher costs for elective readmissions than schemes with ‘step-down’ care (for which there was a cost saving).
Access to step-down care (vs. no step-down care) results in slightly lower costs associated with emergency readmissions. Clinically led services have higher costs associated with emergency readmissions than ‘housing-led’ schemes.
Bed-days avoided per patient
Table 19 shows that patients using a HHDS used slightly fewer bed-days than homeless people discharged from the hospital without the support of a HHDS.
Figure 11 shows the difference in annual bed-days per patient. The number of bed-days avoided per patient (vs. control group) was comparable for clinically- and housing-led schemes (1.92 vs. 1.55, respectively) and sites with no ‘step-down’ care and with ‘step-down’ care (1.57 vs. 2.34, respectively).
FIGURE 11.
Economic model 1: difference in annual bed-days per patient (vs. standard care from Hewett et al. 78). Comparison 1: clinically-/housing-led schemes (vs. standard care) (based on data for 17 schemes). Comparison 2: schemes with and without ‘step-down’ care (vs. standard care) (based on data for 17 schemes).
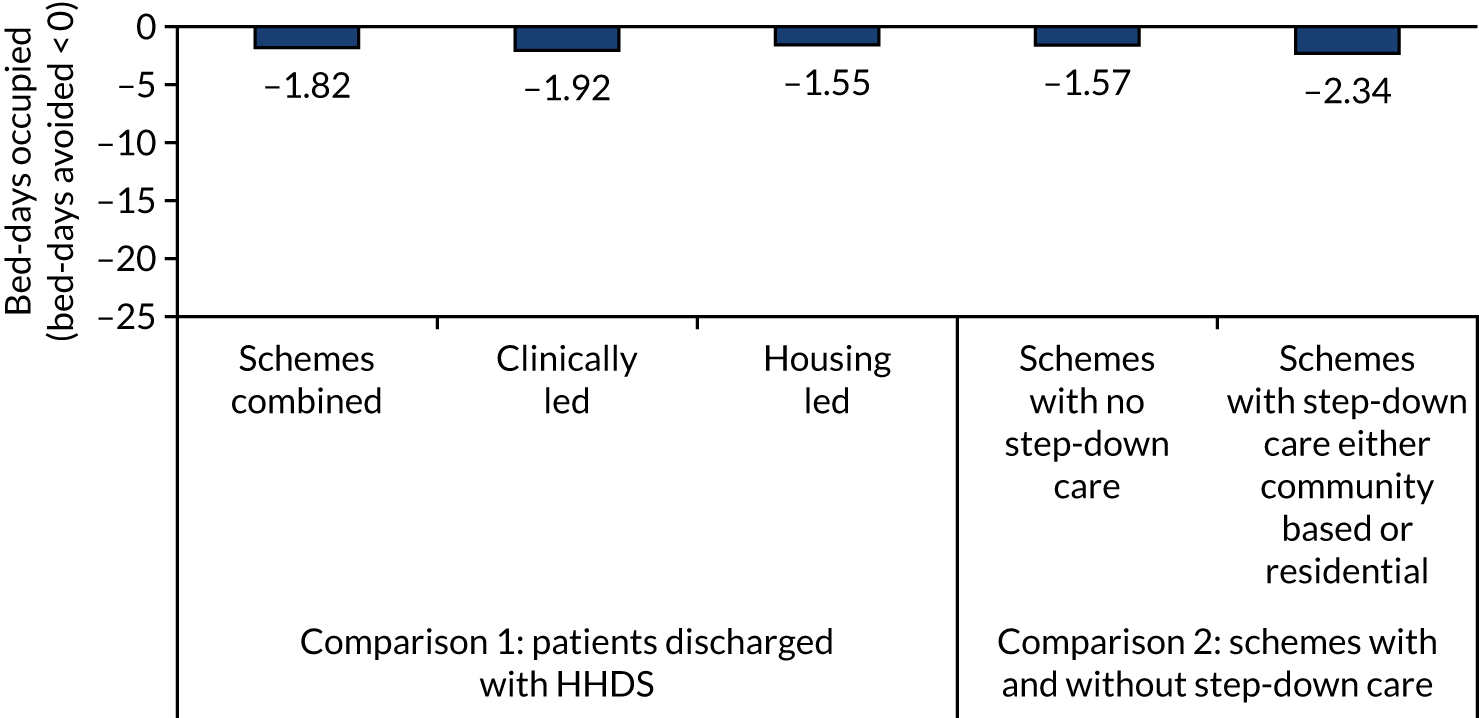
Cost-effectiveness (resources to be invested per bed-day avoided)
Figure 12 shows the NHS resources to be invested per bed-day avoided. The analysis includes only the economic consequences on the NHS (readmissions), as service delivery costs were not made available for the 17 HHDSs.
FIGURE 12.
Economic model 1: NHS resources to be invested per bed-day avoided (control group = standard care from Hewett et al. 78). Comparison 1: clinically-/housing-led schemes (vs. standard care). Comparison 2: schemes with and without ‘step-down’ care (vs. standard care). Main analysis: NHS resources included costs for all readmissions (without service delivery costs). Sensitivity analysis 2: NHS resources covered costs for non-elective (emergency) readmissions without service delivery costs.
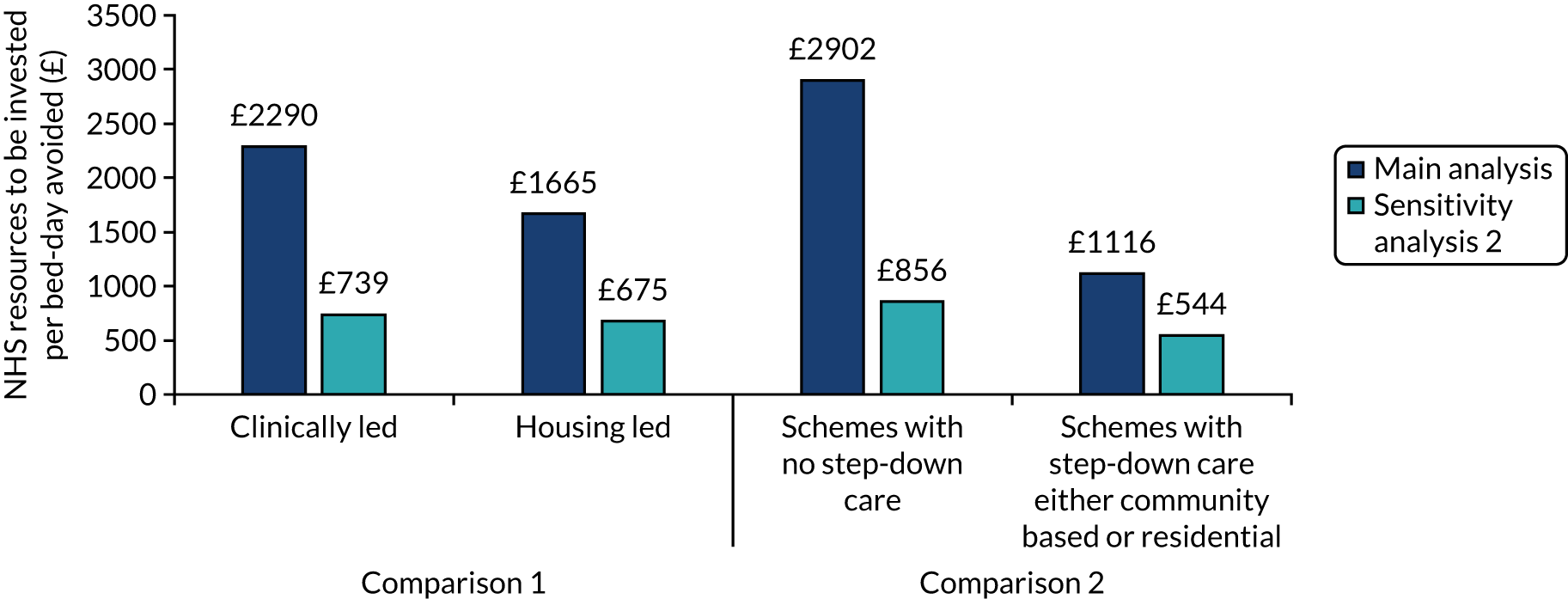
Bed-days avoided is one measure commonly used to assess the effectiveness of NHS services for homeless people and was adopted here as the primary outcome measure (following Hewett et al. 78). In the main analysis, the NHS resources to be invested included costs for all readmissions (without service delivery costs). In the sensitivity analysis, NHS resources covered costs for non-elective (emergency) readmissions (without service delivery costs). This sensitivity is important because not all costs associated with readmissions are negative. Increasing the number of elective (planned) readmissions is, for example, a positive outcome that can be linked to improved access to health care and potentially better longer-term outcomes.
The cost-effectiveness analysis considered the additional resources to be invested for an improvement in the effects (i.e. avoided bed-days) associated with clinically- or housing-led schemes (comparison 1) and schemes with or without ‘step-down’ care (comparison 2), compared with standard care. The difference in mean 12-month costs and outcomes was estimated based on the model presented earlier. ICERs were calculated by dividing the difference in mean cost by the difference in mean length of stay per patients. ICERs indicated positive costs (NHS costs to be invested) and positive effects (saving in bed-days) (see Figure 12). Given that the number of hospital admissions per homeless person is four times higher than for the general public,128 reduction in homeless-related hospitalisation is a key priority for the NHS in England.
Main analysis
In the main analysis, NHS resources included costs for all readmissions (without service delivery costs).
The hospital costs to be invested by the NHS to save 1 bed-day were greater for clinically led schemes than for housing-led schemes (£2290.36 vs. £1665.10 per bed-day avoided), indicating that housing-led schemes are more cost-effective. If we assume that the NHS cost savings associated with a reduction of 1 bed-day are equal to £447 [we take an average cost per day of stay = £2323/6.86 = £339 (2007 value129 ≈ £447, using Bank of England rates130)] and we consider the NHS money invested by the NHS for readmissions within 1 year, the rate of return for the investment made [i.e. (net profit)/(total investment) × 100] is negative for both groups, meaning a lack of returns within the 1 year on the investment made.
Housing-led schemes were ‘less worse off’ than clinically led schemes (–73% vs. –80%, respectively). The NHS cost invested (per bed-day saved) would need to be lower than £447 to have a positive return on investment.
The ICER was greater for schemes with no ‘step-down’ care than for schemes with ‘step-down’ care (£2902.22 vs. £1115.94), indicating that step-down care is more cost-effective. Similar considerations (to those stated above on lack of returns within the 1 year on the investment) may apply here. Overall, the models suggest that the intervention groups (vs. usual care) are cost-effective. In particular, they can be resource saving (e.g. secure fewer bed-days in the hospital and, therefore, reduce their associated costs). However, from the budget impact analyses, we understand that within the first year the investment costs are greater than the gains.
Sensitivity analysis 2
In sensitivity analysis 2, NHS resources covered costs for non-elective (emergency) readmissions without service delivery costs.
The hospital costs for non-elective (emergency) readmissions to be invested by the NHS to save 1 bed-day were greater for clinically led schemes than for housing-led schemes (£739 vs. £675 per bed-day avoided), indicating that housing-led schemes are more cost-effective. If we consider a threshold of £477, the return on investment is still negative for both groups, with housing-led schemes less worse off than clinically led schemes (–34% vs. –40%, respectively).
The ICER was greater for schemes with no ‘step-down’ care than for schemes with ‘step-down’ care (£856 vs. £544), indicating that step-down care is still more cost-effective. The step-down schemes reported a smaller loss in investment in the first year than schemes with no ‘step-down’ care (i.e. negative return on investment of 18% vs. 48%, respectively).
Other sensitivity analyses (variations in overall costs or effectiveness for the comparator as well as longer follow-up)
More analyses are reported in Report Supplementary Material 3. The analyses looked at alternative scenarios where we varied the overall costs or effectiveness for the comparator. In addition, we looked at longer follow-up. The findings emerging from these alternative sensitivity analyses confirmed those in the main analyses above.
Report Supplementary Material 4 and 5 show the degree of uncertainty around the differences in costs and bed-days avoided between the intervention and control groups. The cost-effectiveness acceptability curves (see Report Supplementary Material 5) show that ‘housing-led’ schemes are more cost-effective than clinically led schemes, and schemes with step-down care are more cost-effective than schemes with no step-down care.
Implications for realist hypothesis testing
Specialist care will be more cost-effective than standard care
-
Based on model 1 (resources to be invested per bed-day avoided), specialist care is more cost-effective than standard care.
-
Patients using HHDSs have more readmissions to the hospital and use more NHS resources than those who use standard care. We interpret this as a positive outcome, indicating that HHDSs are working more effectively than standard care to improve access to health care among a marginalised group for whom one in three deaths are due to conditions amenable to timely health care.
-
Patients using HHDSs use fewer bed-days per year. We take this as an indication that HHDSs may be working more effectively than standard care to improve patient flow and prevent delayed discharges.
The case for clinically led multidisciplinary team working as a key mechanism resource
-
Based on model 1 (resources to be invested per bed-day avoided), housing-led (uniprofessional) teams are more cost-effective than those that are clinically led (multidisciplinary). Uniprofessional housing-led teams also perform comparatively as well as clinically led MDTs on measures such as bed-days avoided. This challenges the theory about the assumed benefits of clinically led MDT working. However, across model 1, we were unable to control for different levels of patient need. It may be that the clinically led schemes are working with a different cohort of patients with more complex and/or severe needs. This could potentially make such schemes appear less effective and cost-effective when subjected to the same economic parameters as the housing-led schemes (in effect comparing ‘apples and pears’). Similarly, model 1 cannot control for context and the extent to which the results are being affected by differential access to housing and other community services. As clinically led teams tend to be located in larger cities (because they need to see ≥ 200 homeless patients per year to be viable), it may be that they are working in difficult conditions, making good outcomes harder to achieve.
-
Clinically led teams report higher costs for elective readmissions than housing-led teams (for which there is a cost saving). We interpret this higher cost to be a positive outcome in terms of conferring greater access to planned follow-up care. We assume increased access to planned follow-up care to be a result of clinically led advocacy (patient in-reach), whereby clinicians (GPs) based in the hospital may have easier access to outpatient and other clinical services than would a housing worker. An anomaly here is that ‘step-down’ services are also cost saving when it comes to elective readmissions when it might have been anticipated that providing continuity of support after leaving hospital would increase access to (elective) health care. An explanatory factor here may be that the majority of HHDSs with ‘step-down’ care are housing led and so may not confer access to clinically led advocacy (patient in-reach).
-
Taking the above assumptions into account and sensitising the data for emergency readmissions only, there is little difference in cost-effectiveness between clinically led and housing-led schemes. We interpret this to be the more accurate measure of effectiveness.
The case for ‘step-down’ intermediate care as a key mechanism resource
-
Based on model 1 (resources to be invested per bed-day avoided), HHDSs with direct access to ‘step-down’ care are more cost-effective than schemes with no access to step-down care.
-
Access to step-down care results in slightly lower costs associated with emergency readmissions than schemes without step-down care.
-
Clinically led teams, because of their primary focus on improving the quality of in-patient care (i.e. patient in-reach and discharge co-ordination), do not provide the same level of access to ‘step-down’ care as housing-led schemes. A distinctive feature of nearly all the housing-led schemes is that workers ‘in-reach’ into the hospital and will then provide floating support for a time-limited period until community services are in place and working well. This association with intermediate care (i.e. continuity of support post exit from the acute sector) may be the more significant factor in accounting for the better performance of housing-led schemes (i.e. clouding our understanding of any distinctions to be drawn between multidisciplinary and uniprofessional working).
Part 3: focus on three out-of-hospital care configurations
Overview
This section reports on the cost-effectiveness of three specialist ‘out-of-hospital’ care configurations using three different modelling techniques. We begin by briefly recapping on the different configurations, their geographical contexts and the data sources used in the modelling.
Configuration 1
A multidisciplinary ‘clinically led’ (homeless health-care) team that offers patient in-reach and specialist discharge co-ordination, with no direct access to ‘step-down’ intermediate care. Substantive support for the patient usually ends at the point of exit from the acute sector. Two examples of this configuration are considered, one situated in a city and one in a seaside resort in the south of England. The regions in which these places are situated have the highest percentages of people sleeping rough in England (27% and 20%, respectively). 131 Qualitative reports suggest severe shortages of housing and support services. Many patients will not have local connections to the area.
Data source
Hospital data and EQ-5D data are from Hewett et al. 78
Configuration 2
In this site, two HHDSs work together in an integrated way. This configuration comprises a clinically led (homeless health-care) team that offers patient in-reach and discharge co-ordination. This site also has access to a 14-bed residential facility, offering step-down intermediate care and providing support to patients for up to12 weeks post discharge. The hospital-based homeless health-care team provides ‘clinical in-reach’ into the residential intermediate care facility, ensuring continuity of multidisciplinary support for patients. The HHDSs are based in an old industrial city in the north of England (Yorkshire). This region has 5% of the people sleeping rough in England. 131 Qualitative reports suggest a good supply of housing and housing-related support services.
Data source
Hospital Episode Statistics data and EQ-5D data were collected by homeless health-care team as part of their routine monitoring.
Configuration 3
In this site, there is a single housing-led HHDS in which a small team of housing support workers visit the hospital to provide patient-in reach and discharge co-ordination. The housing workers then continue to support the patient in the community (offering floating support) until longer-term services are in place and working well (i.e. community ‘step-down’ intermediate care). This is usually for around 12 weeks post discharge. The scheme is uniprofessional and does not have access to a multidisciplinary clinically led homeless health-care team based at the hospital. The HHDS is based in an old industrial city in the Midlands. This region contains 8% of the people sleeping rough in England. 131 This HHDS is run by a housing association with direct access to a good supply of accommodation. The city has, however, experienced severe cuts to housing-related support services.
Data source
Hospital Episode Statistics data and EQ-5D data from audit data.
It should be emphasised that the unit of analysis here is not the individual HHDS per se, but what NHS England terms the ‘complex adaptive system’. If our realist hypothesis is correct, then configuration 2 should be the most effective and cost-effective because it integrates specialist services to deliver a clinically led MDT response, encompassing all key ingredients for safe, timely transfers of care (i.e. ‘patient in-reach’, ‘discharge co-ordination’ and ‘step-down’ intermediate care). Configurations 1 and 2 each lack what we hypothesise to be a key MIR. Configuration 1 has no direct access to step-down intermediate care and configuration 2 is housing led (uniprofessional) and does not have the benefit of access to a clinically led MDT based in the hospital.
Results: primary analysis using linked Hospital Episode Statistics data (model 1)
Effect on health-care resources and costs
Table 19 gives an overview of the number of patients (at index discharge), completed admissions and bed-days in the 1 year after discharge for each of the three configurations and for the control (control group 3).
Costs per patient for each readmission
Figure 13 shows the difference in annual NHS costs per patient for a range of readmission types (i.e. elective readmissions, emergency readmissions, other readmissions and costs for all admissions). Considering all readmissions, configuration 1 (clinically led/no step-down care) and configuration 2 (clinically led/residential step-down care) reported considerably greater costs than configuration 3 (housing led/community step-down care) (£7004 vs. £2468 vs. £1353; p < 0.01).
FIGURE 13.
Economic model 1: difference in annual NHS costs per patient across three out-of-hospital care configurations (control group = standard care from Hewett et al. 78).
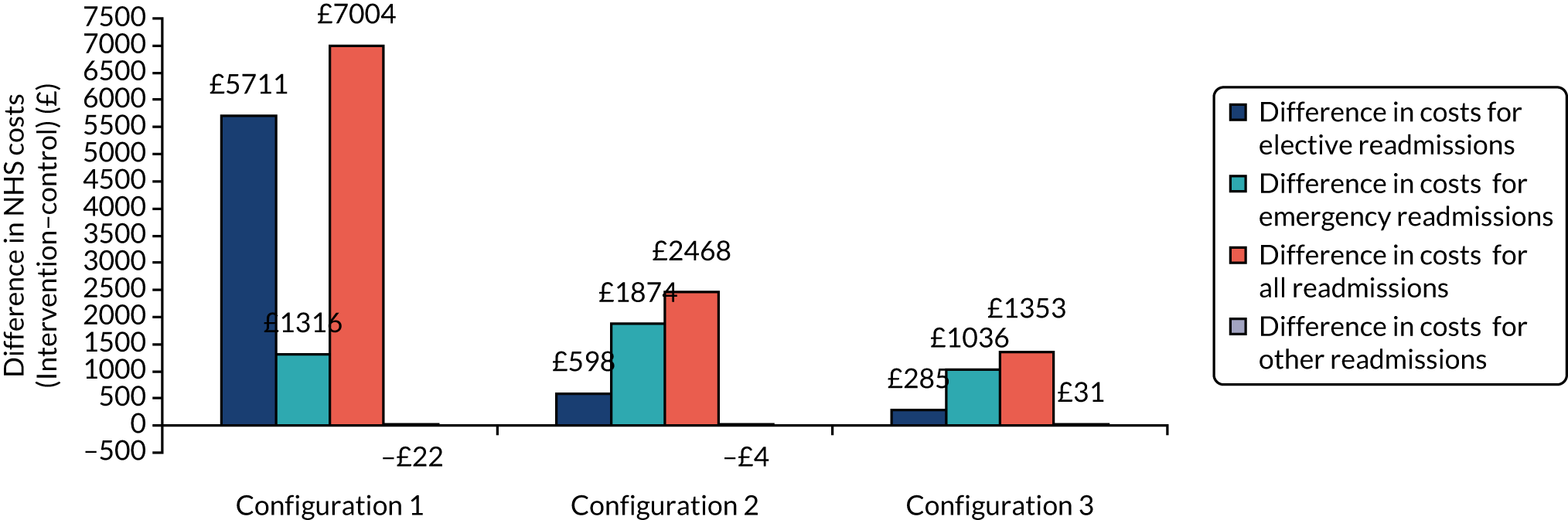
Configuration 1 has the highest costs for elective readmissions, followed by configurations 2 and 3 (£5711 vs. £598 vs. £285; p < 0.01).
Configuration 2 has highest costs for emergency readmissions, followed by configurations 1 and 3 (£1874 vs. £1316 vs. £1036; p < 0.01).
Bed-days avoided per patient
Figure 14 shows the difference in annual bed-days per patient. Configuration 1 (clinically led/no step-down care) and configuration 2 (clinically led/residential step-down care) reported fewer bed-days avoided than configuration 3 (housing led/community step-down care). It should be noted that configuration 3 performs significantly better than the other two configurations on this measure in terms of the number of bed-days that it is saving (2.56 vs. 4.9 vs. 19.9 days per year per patient; p < 0.01).
FIGURE 14.
Economic model 1: difference in annual bed-days per patient across three out-of-hospital care configurations (control group = standard care from Hewett et al. 78).
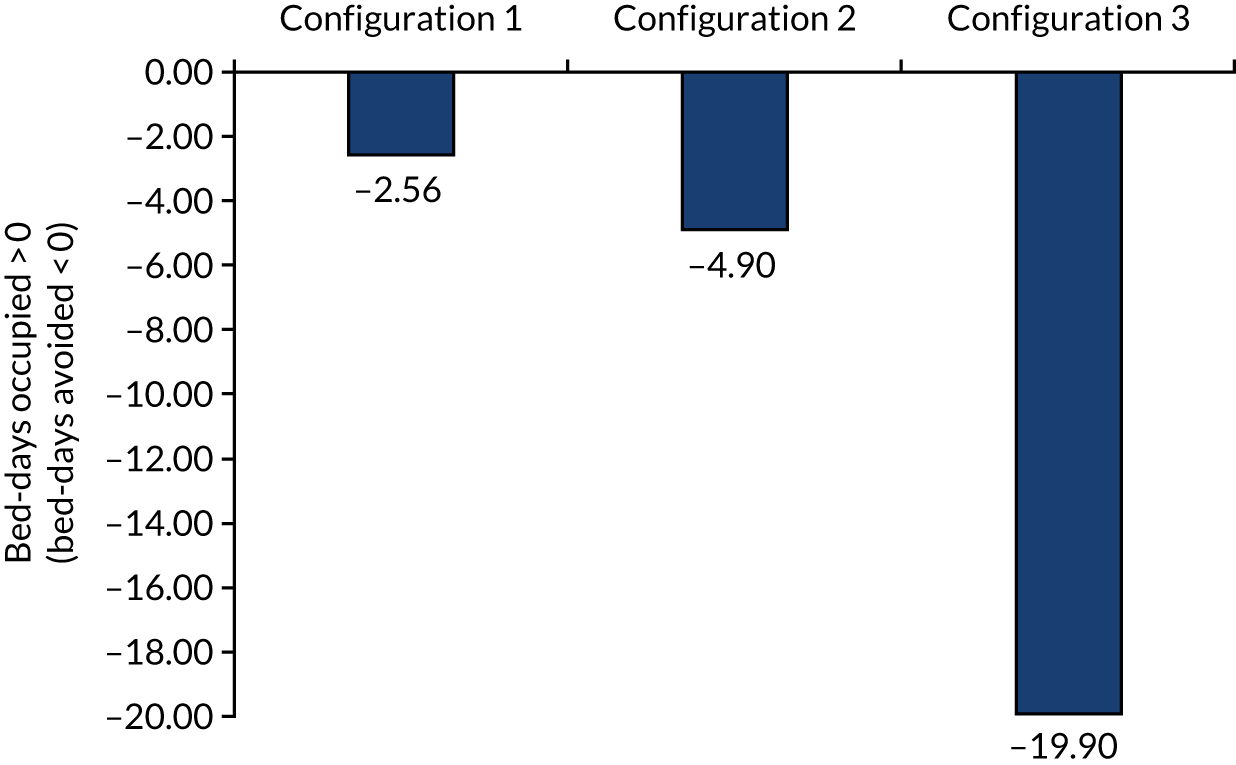
Cost-effectiveness (resources to be invested per bed-day avoided)
This section explores the NHS costs that need to be invested per bed-day avoided.
Overall, we see that for all three out-of-hospital care configurations, the ICERs present positive costs and positive effects (Figure 15). Details on the cost-effectiveness and budget impact analyses for the following three separate models are discussed below:
-
main analysis – NHS resources included costs for all readmissions (without service delivery costs)
-
sensitivity analysis 1 – NHS resources included costs for all readmissions (with service delivery costs)
-
sensitivity analysis 2 – NHS resources included costs for non-elective (emergency) readmissions (with service delivery costs).
FIGURE 15.
Economic model 1: NHS resources to be invested per bed-day avoided (control group = standard care from Hewett et al. 78). Main analysis: NHS resources included costs for all readmissions (without service delivery costs). Sensitivity analysis 1: NHS resources include costs for all readmissions (with service delivery costs). Sensitivity analysis 2: NHS resources include costs for non-elective (emergency) readmissions (with service delivery costs).
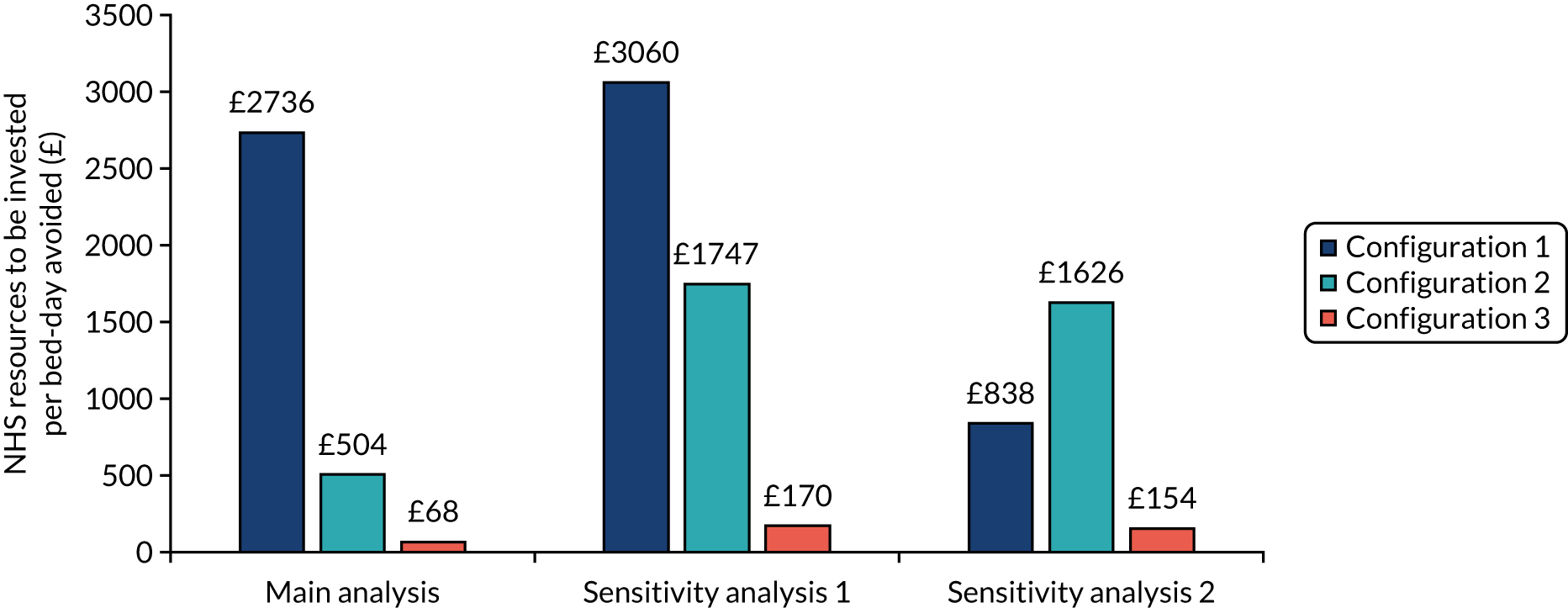
Service delivery costs
Service delivery cost estimates are shown in Table 22. According to the public provider perspective, the average costs per homeless patient was £6092.62 [configuration 2 (clinically led/residential step-down care)] and £2036.62 [configuration 3 (housing led/community step-down care)]. When looking at the staff-related costs (NHS perspective), the average costs per homeless patient dropped for both groups, but more dramatically for configuration 2 than for configuration 3 (see Table 22). Service delivery costs for configuration 1 were covered by the NHS budget only (£830) and were well below the average costs per homeless patient reported for the other configurations.
| Service delivery cost | Configuration 1 (£) | Configuration 2 (£) | Configuration 3 (£) |
|---|---|---|---|
| 1. Paid staff: total | 123,481.00 | 264,152.60 | 122,470.90 |
| 2. Staff training, travel and subsistence expenses (e.g. for outreach activities) | 12,328.00 | 3477.00 | 9947.98 |
| 3. Overhead costs: non staff | 22,352.00 | 105,185.33 | 7728.00 |
| 4. Overhead costs: staff | 10,262.00 | 1508.00 | 3164.00 |
| 5. Capital overheads | 2556.00 | 58,873.33 | 29,333.33 |
| 6. Hotel costs (e.g. food, cleaning) | 0 | 13,424.00 | 0 |
| 7. Advertising of the service | 0 | 0 | 252.00 |
| 8. Other indirect central infrastructure costs | N/A | 40,789.33 | 6326.67 |
| Provision for 206 users from the RCT78 | Provision for 80 users | Provision for 88 users | |
| NHS perspective (1–5 only) | |||
| Total yearly costs (2017) | 170,979.00 | 433,196 | 172,644 |
| The average cost per homeless user | 830 | 5415 | 1962 |
| Public sector perspective (1–8) | |||
| Total yearly costs (2017) | N/A | 487,409.60 | 179,222.90 |
| Average cost per homeless user | N/A | 6092.62 | 2036.62 |
Main analysis
This shows NHS costs for all readmissions (without service delivery costs).
The hospital costs to be invested by the NHS to save 1 bed-day were higher for configuration 1 followed by a significant drop in investment for configuration 2 and an even bigger drop for configuration 3 (£2736 vs. £504 vs. £68 per bed-day avoided). Our analyses indicated that configuration 3 (housing led/community step-down care) is the most cost-effective.
If we assume that the NHS cost saving associated with a reduction of 1 bed-day is equal to £447 (see above) and we consider the NHS money invested by the NHS for readmissions within 1 year, the rate of return for the investment made is as follows:
-
negative for configurations 1 (–84%) and 2 (–11%), meaning a lack of returns of 84% and 11% within the 1 year on the investment made, where the loss was much smaller for configuration 2 than for configuration 1
-
positive for configuration 3 (557%), meaning a positive return of 557% within the 1 year on the investment made.
Please note that (return on investment) = (net profit)/(total investment) × 100. In addition, the NHS investment [i.e. NHS cost (per bed-day saved)] would need to be lower than £447 per bed-day to have a positive return on investment.
Housing-led schemes were ‘less worse off’ than clinically led schemes (–73% vs. –80%, respectively). The NHS cost (per bed-day saved) would need to be lower than £447 to have a positive return on investment.
Model 1 (i.e. NHS resources included costs for all readmissions without service delivery costs) suggests that the intervention groups (vs. usual care) are cost-effective. In particular, they can be resource saving (e.g. secure fewer bed-days in the hospital and, therefore, reduce their associated costs). Following that, from the budget impact analyses, we understand that within the first year for configuration 1 (and to a smaller extent for configuration 2) the investment costs are greater than the gains, whereas for configuration 1 the economic gains are much greater than the investment costs.
Sensitivity analysis 1
NHS resources include costs for all readmissions with service delivery costs. When the service delivery costs were taken into consideration (along all readmissions costs), the incremental costs per bed-day avoided varied, with £3060 for configuration 1 (clinically led/no step-down care), £1609 for configuration 2 (clinically led/residential step-down care) and £167 for configuration 3 (housing led/community step-down care).
The rate of return for the investment reports bigger losses for configurations 1 and 2 (compared with the main analysis).
Sensitivity analysis 2
As noted above, not all costs associated with readmissions are negative, in the sense that increasing access to planned health care (i.e. elective readmissions) is a desirable outcome. To account for this, sensitivity 2 compared the difference in non-elective readmission costs (together with the service delivery costs). The ICERs decreased to £506 for configuration 1 (clinically led/no step-down care), to £382 for configuration 2 (clinically led/residential step-down care) and to £54 for configuration 3 (housing led/community step-down care) per bed-day avoided (see Figure 15). Note how the costs for configuration 1 are dramatically reduced.
Other sensitivity analyses
This considers variations in overall costs or effectiveness for the control group (as well as longer follow-up).
Deterministic scenario analyses are reported in Report Supplementary Material 4. The analyses reported comparable results to the main analyses reported in Figure 15.
Report Supplementary Material 4 and 5 show the degree of uncertainty around the differences in costs and bed-days avoided between the different configurations and control groups. Configuration 1 (clinically led/no step-down care) reported a lower percentage of dots than configuration 2 (clinically led/residential step-down care) and configuration 3 (housing led/community step-down care) (53% vs. 99% vs. 100%). The cost-effectiveness acceptability curves (see Report Supplementary Material 5) show that configuration 1 (clinically led/no step-down care) reported less probability of being cost-effective than configuration 2 (clinically led/residential step-down care) and configuration 3 (housing led/community step-down care). Configurations 2 and 3 have a high probability of being cost-effective (see Report Supplementary Material 5).
Results: cost–utility for the NHS (model 2)
In this section, we report on additional analyses using linked HES data and EQ-5D data to establish the cost–utility of three different ‘out-of-hospital’ care configurations for the NHS.
The effect of different out-of-hospital care configurations on health-care resources, costs and health utility
Figures 13 and 16 report the difference in annual NHS costs and QALY outcomes per patient compared with standard care (control group 3: Hewett et al. 78). Costs were commented on above (see Model 1: what is the cost-effectiveness of homeless hospital discharge schemes for the NHS?). All three configurations confer better QALY outcomes than standard care (Figure 16).
FIGURE 16.
Economic model 2: difference in QALY outcomes per patient vs. standard care (Hewett et al. 78). Intervention: QALY data for configuration 1 were extracted from Hewett et al. ,78 whereas local data were used for configurations 2 and 3. QALY data for the control group (standard care) were extracted from Hewett et al. 78 The graph reports on the gains in QALY between intervention and control groups.
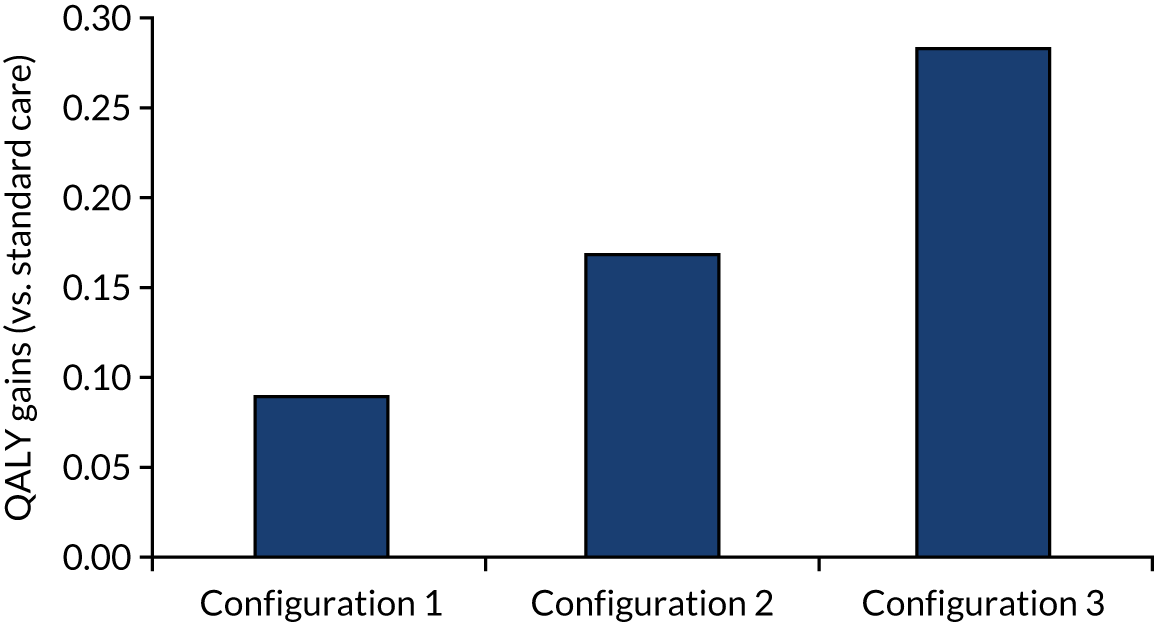
Configuration 3 (housing led/community step-down care) achieved the largest number of QALY gains (vs. standard care) followed by configuration 2 (clinically led/residential step-down care) and then configuration 1 (clinically led/no step-down care) (0.29 vs. 0.17 vs. 0.09).
Configuration 1 (clinically led/no step-down care) and configuration 2 (clinically led/residential step-down care) reported greater costs per QALY gain than configuration 3 (housing led/community step-down care) (£7004.14 vs. £2467.52 vs. £1353.22; p < 0.01).
Cost-effectiveness
Configuration 1 (clinically led/no step-down care) and configuration 2 (clinically led/residential step-down care) reported greater ICERs than configuration 3 (housing led/community step-down care) (£55,602 vs. £14,515 vs. £4743) (Figure 17). If a threshold of £30,000 is applied, then configuration 1 may not be cost-effective, whereas configurations 2 and 3 are cost-effective well within the NICE recommendations. It should be noted that when the multidisciplinary ‘clinically led’ homeless health-care team is working in a busy city with higher workload and dealing more frequently with people with more complex needs (and this may apply to configuration 1), it is likely to be costlier to achieve a QALY gain than when sites placed in smaller old industrial cities, dealing with fewer cases and less frequently with complex ones (see configurations 2 and 3).
FIGURE 17.
Economic model 2: additional costs to be invested per QALY gained. Main analysis: NHS resources include costs for all readmissions (without service delivery costs – this is aligned with the analyses in part 2 of this present report). Sensitivity analysis 1: NHS resources include costs for all readmissions (with service delivery costs). Sensitivity analysis 2: NHS resources include costs for non-elective (emergency) readmissions (with service delivery costs). Utility data used here are reported in Figure 16. The cost-effectiveness analyses reported positive costs and positive effects, and trade-offs between costs and effects were considered. This represents the situation where the intervention may be cost-effective compared with the control group, and the value at which the ICER is considered good value for money is provided by NICE (under the threshold of £20,000–30,000 per QALY).
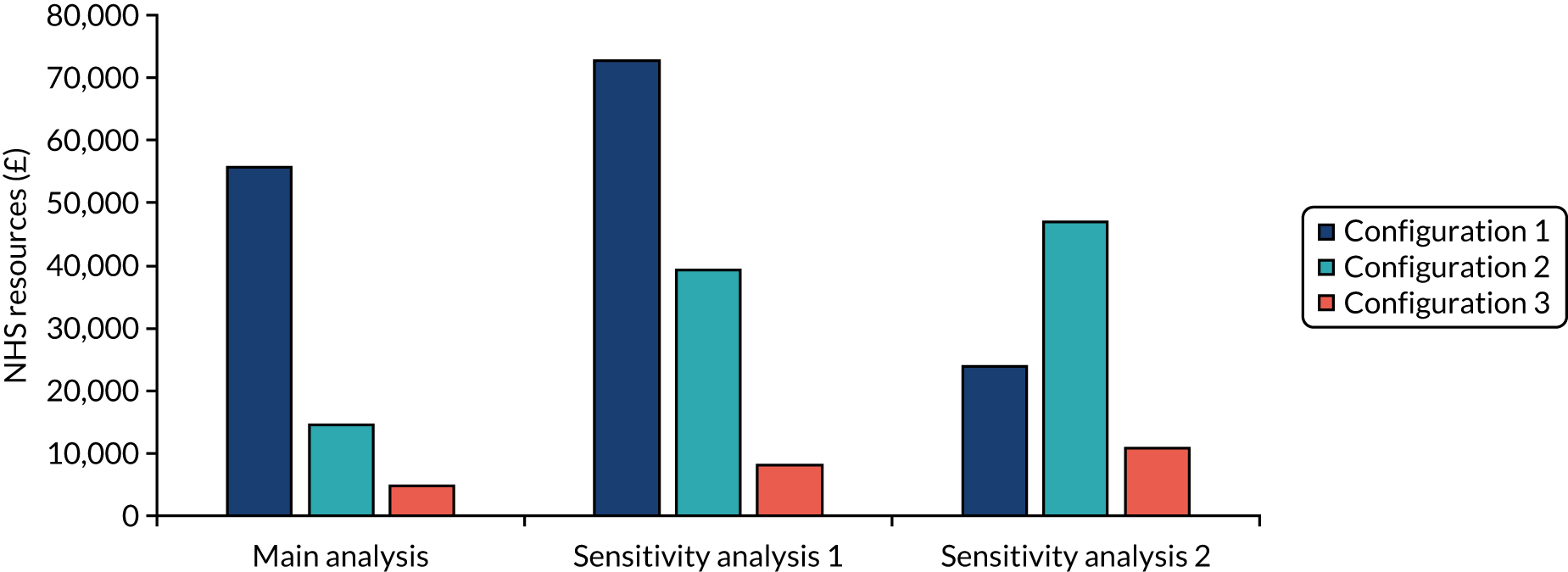
Sensitivity analyses
Including both the NHS-related economic outcomes (readmissions) and also service delivery costs (NHS-related costs only)
When service delivery costs were taken into consideration (along with all readmissions costs), the incremental costs per QALY gain varied, with £72,674 for configuration 1, £43,792 for configuration 2 and £11,620 for configuration 3. To test the impact of the intervention when shifting costs from non-elective (emergency) to elective readmissions (as an indicator of appropriate care pathway treatment), we added an additional sensitivity analysis (sensitivity analysis 2) where we explored difference in non-elective (emergency) readmission costs (together with the service delivery costs). From this analysis, all interventions were cost-effective according to NICE thresholds (see Figure 15, sensitivity 2). The incremental cost–utility ratios decreased to £23,839 (configuration 1), £10,388 (configuration 2) and £3743 (configuration 3) (see Figure 17).
Other sensitivity analyses
Deterministic scenario analyses are reported in Report Supplementary Material 6. They show comparable results to the primary analyses reported in Figure 17.
Report Supplementary Material 7 and 8 show the degree of uncertainty around the differences in costs and QALYs between the interventions and control groups. Configuration 1 (clinically led/no step-down care) reported 0% probability of being cost-effective, whereas configuration 2 (clinically led/residential step-down care) and configuration 3 (housing led/community step-down care) presented some probability of being cost-effective (80% at a threshold of £30,000 and 100% at a threshold of £8000, respectively) (see Report Supplementary Material 9).
Results: cost–utility for the NHS and broader public perspective (model 3)
In this section, we report on additional analyses using linked HES data and EQ-5D data to establish the cost–utility of different ‘out-of-hospital’ care configurations for the NHS and the wider public perspective. As noted above, this analysis is limited to configurations 2 and 3 because service delivery costs could not be ascertained for configuration 1.
The difference in annual costs for health-care resources (A&E and hospitalisation) showed that there is an annual patient saving in NHS costs [between £856 for configuration 2 (clinically led/residential step-down care) and £2466 for configuration 3 (housing led/community step-down care)] (see Figure 17). For both configurations, the cost saving was greater when considering the broader public provider perspective (£5758 and £4454, respectively). When considering total health-care costs (A&E and hospitalisation plus service delivery costs), there was a cost saving of £2318 for configuration 3, whereas for configuration 2 there was an increase in NHS costs to be invested, equal to £334. QALY gains increased to 0.16 for configuration 2 and 0.23 for configuration 3 (see Figure 17). More information on the sample, patient characteristics, use of resources, costs and health utility is reported in Report Supplementary Material 10.
The cost-effectiveness analyses (i.e. the total costs for the broader public sector perspective with service delivery costs) for configuration 3 (housing led/community step-down care) presented negative costs and positive effects (costs < 0 and effects > 0) (see Figure 18). For configuration 2 (clinically led/residential step-down care), we found positive costs and positive effects (costs > 0 and effects > 0; £2029 cost per QALY) (Figures 18 and 19). Both configurations were cost-effective according to NICE recommendations.
FIGURE 18.
Economic model 3: difference in total annual total costs (broader public perspective) and QALY outcomes per patient.

FIGURE 19.
Economic model 3: ICER and cost per QALY gained (project local survey sites, comparison before and after). NHS costs data covered hospitalisation, outpatient visits and A&E visits and are comparable across sites. ICER estimates based on public sector and total cost estimates are not comparable as the type of data available on the use of resources was inconsistent across sites.
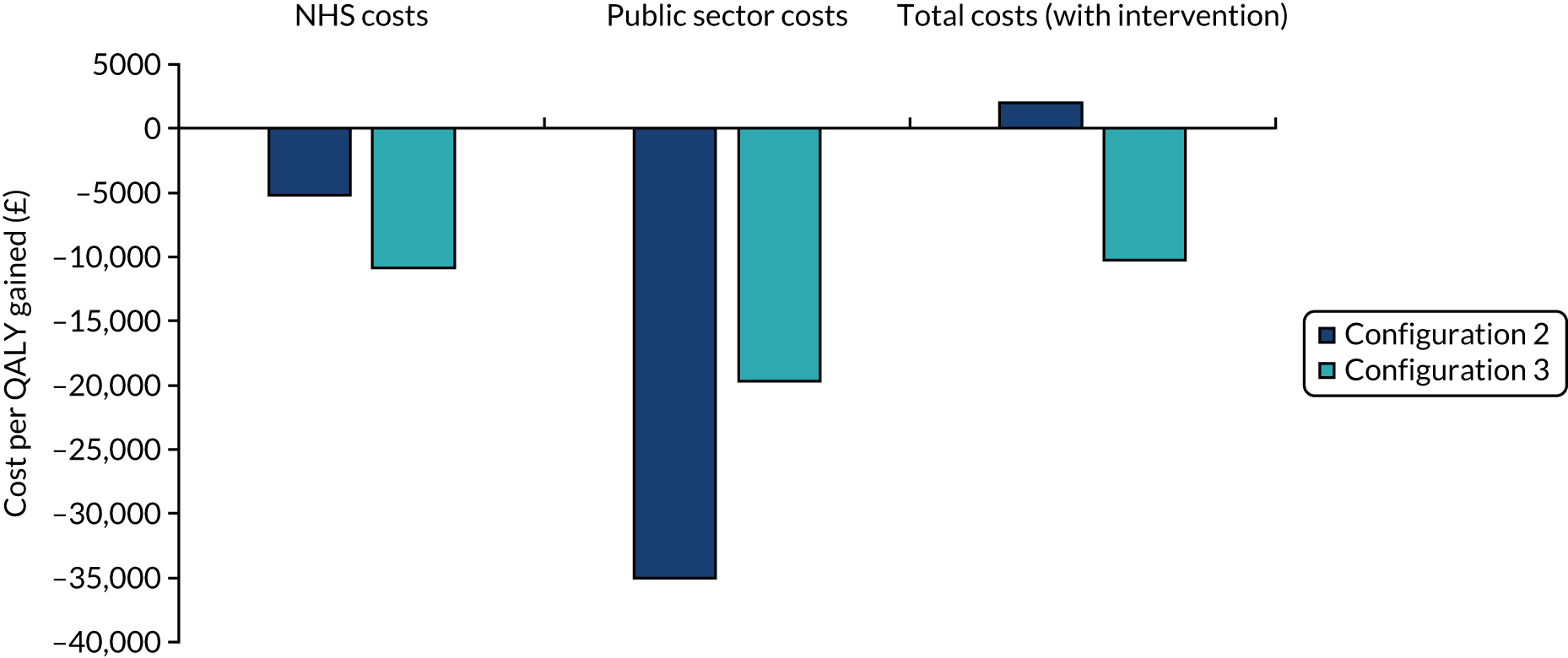
Sensitivity analyses
Deterministic scenario analyses are reported in Report Supplementary Material 11. Configurations 2 and 3 were cost-effective for all sensitivity scenarios (ICERs based on total costs for the broader public sector perspective with service delivery costs). Details on alternative scenarios (and ICER calculations using NHS costs or public sector costs with no service delivery costs) are presented in Report Supplementary Material 9. Report Supplementary Material 10 and 12 show the degree of uncertainty around the differences in costs and QALYs between ‘after the intervention’ and ‘before the intervention’ groups. The percentages of dots for the primary analysis (i.e. total costs for the broader public sector perspective with service delivery costs) in the south-east quadrant (costs < 0 and effects > 0) were 100% for configuration 3 and 44% for configuration 2 (vs. 56% in the north-east quadrant costs > 0 and effects > 0). Both configurations had a 100% probability of being cost-effective according to NICE recommendations.
Implications for realist hypothesis testing
Specialist care is more effective and cost-effective than standard care
-
Access to out-of-hospital care that encompasses HHDSs is more cost-effective than standard care.
-
From a NHS perspective, all three configurations are cost-effective with regard to NICE thresholds for QALY gains (based on sensitivity for elective readmissions). This finding is supported in the wider literature.
-
From a wider public perspective, configurations 2 and 3 reported 100% probability of being cost-effective according to NICE recommendations (configuration 1 was excluded from this analysis because of lack of service cost data).
The case for ‘step-down’ intermediate care
-
The two configurations that encompass ‘step-down’ care consistently outperform, in economic terms, the configuration that does not have any direct access to ‘step-down’ care.
The case for clinically led multidisciplinary team working
-
On the basis of our realist hypothesis, we anticipated that configuration 2 would be the most effective and cost-effective because it contained more of the ‘jigsaw pieces’ than the other two configurations. However, on nearly every measure, configuration 3 was better performing. This is the uniprofessional housing-led site with a single HHDS in operation, with no access to specialist clinically led support. Again, this challenges the theory about the benefits of clinically led MDT working. In these modelling exercises, we have, to some extent, been able to control for the context in that both configurations 2 and 3 have similar levels of rough sleeping and are geographically similar areas. However, we have not been able to control for case mix and the possibility that configuration 2 is able to treat more ‘complex patients’ because it has access to both clinical support and residential step-down beds (with associated increased costs for these beds, e.g. ‘hotel’ costs). If this is the case, then this may explain why configuration 2 looks comparatively less cost-effective than the housing-led service in configuration 3. A good indication that this may be the case is that configuration 3 has much lower costs associated with elective readmissions, potentially indicating a healthier cohort of patients. It is also worth noting that the housing-led HHDS in configuration 3 was planning to open a residential ‘step-down’ facility to cater for people leaving the hospital with high levels of need that could not be safely catered for via floating support in the community.
In terms of what this finding may mean for our commissioning ‘road map’, the NICE guideline for intermediate care132 is clear in that to cater for different levels of need localities should have access to both residential (bed-based) and community (home-based) step-down care. In terms of developing a complex adaptive system (rather than a single service delivery model), these economic findings awaken us to the enormous gains that can be achieved through the integration of housing-led support in the wider out-of-hospital care system. In other words, housing-led support should not be substituted for clinically led support (on the grounds that is cheaper/more cost-effective), but should be considered as a mechanism resource of equal significance in the delivery of effective and cost-effective out-of-hospital care. This is an important point, as housing- and community- (voluntary-) led services are often assumed by commissioners to be the ‘icing on the cake’ and, therefore, the most easily dispensable part of the out-of-hospital care system. 86 This economic evaluation establishes that they are far more important than has hitherto been assumed.
Summary of economic evaluation findings
In terms of developing a conceptual road map for commissioners, the economic evaluation supports the development of HHDSs to ensure consistently safe, timely transfers of care for patients who are homeless. Table 23 provides a summary of the cost-effectiveness findings. Indeed, these findings provide much stronger evidence for HHDSs as compared with the previous chapter and it is important to note that the economic analysis has used a different control group. Across the different modelling exercises, the findings confirm the following:
-
Specialist care is more effective and cost-effective than standard care.
-
Clinically led advocacy (patient in-reach) increases costs for the NHS, but improves access to elective (planned follow-up) care. We interpret this as a positive outcome, indicating that SIHHC is working more effectively than standard care to improve access to health care among a marginalised group for whom one in three deaths are due to conditions amenable to timely health care.
-
HHDSs with direct access to step-down intermediate care are more cost-effective than those without.
-
When developing complex adaptive systems for out-of-hospital care, it is important not to underestimate the value of housing-led support. This is shown to be as effective and cost-effective as clinically led schemes on a wide range of measures.
-
Overall, the evidence points to the potential of well-integrated HHDSs providing continuity of both clinical- and housing-related support, in the hospital and in ‘step-down’ intermediate care.
| Outcome | Part 2: comparative study of 17 HHDSs | Part 3: comparative study of 3 out of hospital care configurations | |||||
|---|---|---|---|---|---|---|---|
| Clinically-/housing-led schemes (vs. standard care) | Schemes with and without ‘step-down’ care (vs. standard care) | Configuration 1 (clinically led only), configuration 2 (clinically led/residential step-down care) and configuration 3 (housing led/community step-down care) | |||||
| Clinically led | Housing led | No step-down care | With step-down care | Configuration 1 | Configuration 2 | Configuration 3 | |
| Economic model 1: what is the cost-effectiveness of SIHHC for the NHS? | |||||||
| Economic outcome: all readmission costs | Both services are cost-effective | Both services are cost-effective | All three services were cost-effective | ||||
| Economic outcome, non-elective readmission costs | Both services are cost-effective | Both services are cost-effective | All three services were cost-effective | ||||
| Housing led > clinically led | With step-down care > no step-down care | Configuration 3 best-performing site > configuration 2 > configuration 1 | |||||
| No change in 3 years for all | No change in 3 years for all | No change in 3 years for all | |||||
| Economic model 2: what is the cost–utility of SIHHC for the NHS? | |||||||
| Economic outcome, all readmission costs | Not cost-effective | Cost-effective | Cost-effective | ||||
| Economic outcome, non-elective readmission costs | Cost-effective | Cost-effective | Cost-effective | ||||
| Configuration 3 > configuration 2 > configuration 1 (all readmissions) | |||||||
| Configuration 3 > configuration 1 > configuration 2 (non-elective readmission) | |||||||
| No change in 3 years for all | |||||||
| Economic model 3: what is the cost–utility of SIHHC for the broader public perspective? (Limited to evaluation of two configurations) | |||||||
| Cost-effective | Cost-effective and cost saving | ||||||
| Configuration 3 > configuration 2 | |||||||
| No change in 3 years for all | |||||||
Strengths and limitations
The main strength of the analysis is that, to the best of our knowledge, the study is the largest evaluation of HHDSs ever conducted in England (and, to our knowledge, internationally). The study involved 17 different schemes (31 in the literature review), covering all England. To the best of our knowledge, no other study in this field has adopted the same multiple data linkage and multioutcome measures approach to assess the impact of hospital discharge service delivery on different aspects of cost-effectiveness and cost–utility for the NHS, as well as for the broader public perspective.
There were, however, several limitations and weaknesses inherent in the study and we summarise these in Table 24. The most significant of these is the lack of primary questionnaire data from the target research sites and the consequent need to use proxy data from an earlier RCT. 78 Proxy data from this RCT were used for both the standard-care control group and for specialist care in configuration 1. The most important learning here is about the importance of not overestimating the capacity of front-line services to support research through their routine monitoring and data collection. This point is also reinforced in a recent study of reablement services in which similar data collection problems were encountered. 133
| Analysis | Weaknesses and suggestions for future research |
|---|---|
| NHS perspective for the main data linkage analyses |
There are challenges when using NHS perspectives when talking about homelessness (e.g. the impact of the discharge schemes is not limited to health but also to other public services). Our analyses considered different public sector perspectives (beyond NHS), although we experienced numerous challenges in collecting data Future research Diversion of costs to another public sector should be better considered with data linkage with relevant databases |
| Broader public perspective |
It is important to note that when wider perspective is included in cost-effectiveness that this markedly increases cost-effectiveness. This is likely to also apply to the clinically led models, although we were not able to assess this through lack of data In addition, desirable costs, such as outpatient department appointments, planned admissions and drug and alcohol treatment, should be analysed in an opposite group to avoidable costs, such as A&E and unplanned admissions (and these subgroup analyses were not considered for economic model 3, as information on non-elective/elective readmissions was not available). Otherwise, a service that prevents/denies planned treatment may appear more cost-effective Future research Future research should allow researchers to collect a broader spectrum of data and extend the analyses for the broader public perspective Additional analyses should investigate the impact of services for the broader public perspective on different typologies of costs (e.g. not avoidable costs vs. avoidable costs) |
| Comparison across sites | Although the service models compared in the analyses tend to be applied at the hospital level, the case mix of the patients utilising these models may differ across them. Findings can also be biased through local variations in availability of housing, care and support. This greatly limits the extent to which we can compare effectiveness and cost-effectiveness across service models and configuration. The cost saving for configuration 3 may, for example, arise from the proportion of homeless patients subsequently housed, rather than arising from the mechanism resource typological configuration itself |
| Selection of control group (Hewett et al.78) |
Control group referred to standard care provided in Hewett et al. ’s78 trial rather than the standard care provided across the study sites. Outcomes among patients enrolled in the control arm of a trial may be better than real-world outcomes of untreated groups. This may underestimate the effect of interventions. Therefore, the results of this analysis should not be seen to outweigh the original trial results In addition, this trial was a London/Southern-based study where the housing options are most challenging and hospital readmission rates were only to the original admitting hospital and did not measure admissions to other hospitals, as is the case with data linkage to HES. These factors mean that comparisons between service models need to be treated with caution Future research Control group data should be collected to make sure that an appropriate comparator is used. For example, recognising the implications and potential biases associated with comparator selection is necessary to ensure the validity of study results. Confounding by severity and selection bias (e.g. healthy user bias) is particularly challenging, especially with comparators of different service modalities. Confounding by indication can be minimised by choosing a comparator with models that have similar treatment modality and engage with a similar group of users (when possible) |
| Access to data |
The numerous delays in accessing HES data put a strain on the team and on the programme of analyses. Adjustments were to be made to the analyses of the HES data for the economic model. Use of resource data for the intervention groups were extracted from HES data as aggregate-level estimates instead of individual homeless user-level analyses. According to reasonable practice, the unit (e.g. hospitalisation type) was bundled at a level that matched the price weight In addition, the low response rate from participating users compromised the analyses to be undertaken and may not support the generalisability of the results |
| Outcome indicators and monitoring performance |
The primary outcome chosen for the cost-effectiveness analyses was the cumulative duration of hospital stay. It may be worth highlighting that there is some concern that, although this is an important economic indicator, improving patient outcomes may require increasing hospital stay duration and preventing people from being discharged before they are fit and have somewhere to go. Alternative outcomes looked at QALYs, although we recognised the challenges of collecting QALY data and the lack of collection of standardised QALY data across sites limited the economic results produced. More robust evidence is needed to better monitor and compare the performance of the hospital discharge services available in England in terms of standardised economic, quality-of-life and social value indicators. The analysis proposed here is to be understood as a rather conservative test of the model. Specifically, data limitations severely limit the application of the model to disaggregated or microeconomic data, and they constrain the time span for which even aggregate data can meaningfully be used Future research Future research should consider the opportunity to change current monitoring systems and collect standardise outcomes across sites, including different parameters of interest (e.g. effectiveness, quality of care, economic outcomes and user experience) |
| QALY |
Lack of QALY data across sites did not allow the research team in this present study to compare data across the study sites and their different typologies. Our analyses tried to overcome such imitations by drawing on published data (Hewett et al. 78) (see economic model 2, King’s Health Partners Pathway Homeless Team), but we need to be cautious when applying the trial data to local setting In addition, it may be easier to follow up patients and obtain QALY data for those who have continuing health problems leading to admission and re-engagement with services. Therefore, the QALY data may be biased towards those with worse outcomes, potentially underestimating the impact of the interventions. The analyses were limited to a subgroup of sites from where QALY data were available (either collected using surveys or extracted from the literature). As QALY data were difficult to collect and were incomplete, it may be biased towards those with ongoing health needs who, therefore, re-engage with services. It may, therefore, systematically underestimate the impact on QALYs For the ‘drill-down’ analyses, we were fortunate to be able to access local audit data from Derby Health Futures (Derventio Housing Trust, Derby) (and overcome the limited availability of data from other sites). This scheme was routinely collecting EQ-5D and other audit information prior to the present research commencing and, in many respects, we did not realise at the outset that this site was atypical in that it had such robust procedures and systems in place. In nearly all the other HHDSs, monitoring and auditing systems were underdeveloped when compared with this scheme Future research More research is needed to allow a better exchange of good practices and experiences and to educate local sites towards the benefit of adopting a more robust data monitoring systems across the territory. The framework of performance measurement developed and tested with this study could be used to reshape local monitoring systems |
| Timeline |
Longer time should be included and modelled using longer-term data that were not available for the purposes of this project Future research A more robust data collection and performance monitoring system for the audit data, routinely collected in the field, would assist long-term prediction performance |
| Service delivery |
Service delivery costs were excluded from the main modelling, as relevant data were not made available across the different study sites. Sensitivity analyses included service delivery costs alongside all readmissions or non-elective readmissions only (a subgroup of three sites) Future research Future research should involve the measurement of service delivery costs and their variation across sites and time |
| Model assumption on the effects of the intervention | Readmission rates may vary according to local community resources, secondary care resources, bed pressures and hospital willingness to admit homeless patients and, therefore, the assumption that the observed differences in performance were due to the intervention needs to be taken with caution |
As we were limited to a subgroup of sites from where QALY data were available (either collected using surveys or extracted from local audit data), this limited the configurations that could be studied. For example, we did not study sites that had access to intermediate care, but no resource for patient in-reach and discharge co-ordination. These standalone services had closed down (before evaluation could be completed), arguably lending some utility to the theory about the need for multiple and integrated mechanism resources.
As QALY data were difficult to collect and were incomplete, it may be biased towards those with ongoing health needs who re-engage with services and it may, therefore, systematically underestimate the impact on QALYs. In addition, the QALY data for the control group were linked to patients seen (randomised) by a clinically led service that may see more complex patients, potentially exaggerating the impact of the non-clinically led models.
Finally, delays in securing initial ethics approvals for the study, and in receiving data from NHS Digital, meant that the research team was able to start preparatory work on the HES data sets only 3 months prior to the scheduled completion date of the project. This left insufficient time to complete all the work that was planned. The project was granted a 12-month unpaid extension to cover the economic analyses. Unfortunately, after completion of the evaluation, further issues with the quality of the data received from NHS Digital put the project on hold for longer while the team was waiting for new data to arrive. In addition, more time was needed to check the new batch of data and make sure that the data received were suitable for analysis. The numerous delays put a strain on the team and also on the programme of analyses. Adjustments were to be made to the analyses of the HES data for the economic model. Use of resource data for the intervention groups were extracted from HES data as aggregate-level estimates instead of individual homeless user-level analyses. According to reasonable practice, the units (i.e. visit to A&E, hospitalisation type) were bundled at a level that matched the price weight. 134
Chapter 6 Discussion
Overview
In this chapter we discuss the study’s main findings. We present the overall conclusions by means of an evidence-informed ‘road map’. This is an overview of the complex set of factors that decision-makers should consider to ensure consistently safe, timely transfers of care for patients who are homeless. We note the limitations and strengths of the study and outline the implications for commissioners and managers. We also make recommendations for future research.
We started our study in the context of 70% of homeless patients being discharged back to the street without having their care and support needs assessed, and the DHSC award of £10M funding to the voluntary and community sector to address this shortfall. This funding was intended to be used to improve hospital discharge arrangements and to secure adequate provision of ‘step-down’ intermediate care. From 2013 onwards, 52 HHDSs were funded through the HHDF. The overall aim of this evaluation was to provide evidence for commissioners and service leaders on ‘what works best’ with regard to the appropriateness, quality and cost-effectiveness of these specialist HHDSs.
The study adopted a realist evaluation methodology on the basis that the heterogeneity of intermediate care warrants a mixed-method approach, incorporating theories that relate context to outcomes. The first objective was to situate what is already known about DToCs among people who are homeless in terms of the broader literature on hospital discharge and intermediate care. It was hypothesised that no single service model (‘silver bullet’) would work everywhere all of the time and that understanding the wider complex adaptive system was key. Our hunch was that the good practice principles embodied in the (generic) ‘High Impact Change Model (HICM) for Improving Transfers Between Hospital and Home’ (LGA, 201533) might also work to improve discharge experiences among homeless patients. Empirical testing of this generic model was important because much of the evidence underpinning it related to research with older people with homes to return to and families to support them.
The HICM encompassed eight changes. These were (1) early discharge planning, (2) the introduction of protocols for managing patient flow, (3) multidisciplinary discharge co-ordination, (4) ‘step-down’ intermediate care (i.e. support for anyone with a health-related need through a period of transition), (5) flexible working, (6) trusted assessment, (7) engagement and choice and (8) improved discharge to care homes. We drew on the literature for specialist homeless hospital discharge and intermediate care schemes to assess the relative importance of each these, with some changes appearing to have more of an impact than others. We distinguished between changes that were interventions (MIRs) and more general KPPs, such as patient engagement and choice.
Early programme theory refinements
The specialist homeless hospital discharge literature also alerted us to a number of additional changes and sensitivities that we hypothesised to be important in the delivery of safe, timely transfers of care. Much of the HICM, and the hospital discharge literature more broadly, is predicated on addressing the problem of DToCs. However, the review (and the research study more broadly) highlighted that delayed discharge was rare for patients who were homeless and that the main issue was early self-discharge (a much less researched topic). We found that it was common practice for homeless patients to self-discharge before treatment was completed, mainly because of poor methadone prescribing or poor management of alcohol dependence on the ward. Hostel staff in the community also reported difficulties in getting residents (with substance use issues) to go into hospital and to stay there, as there was no guarantee the hospital would prescribe methadone. This reflects the need for every hospital to have a clinical protocol pertaining to urgent stabilisation of drug withdrawal through access to the prescriptions of NICE-recommended medications for the management of drug dependence. In the absence of such a protocol (at the time of the fieldwork), we found that clinically led homeless teams bringing specialist GPs and nurses on to the ward could help prevent early self-discharge (i.e. improve outcomes) by advocating for patients to secure the medication and support they needed. We, therefore, identified multidisciplinary patient in-reach as an additional MIR (MIR2mdt). Relatedly, a drawback of uniprofessional in-reach (a housing worker visiting the ward) (MIR2up) was that they did not always feel confident or have the prescribing know-how to address this issue with doctors on the ward.
After completing the literature synthesis, we were able to begin putting in place the building blocks of our programme theory or ‘road map’. We hypothesised that HHDSs that had access to all the ‘jigsaw pieces’ would deliver better outcomes linked to safe, timely transfers of care (Figure 20).
FIGURE 20.
Road map building blocks.
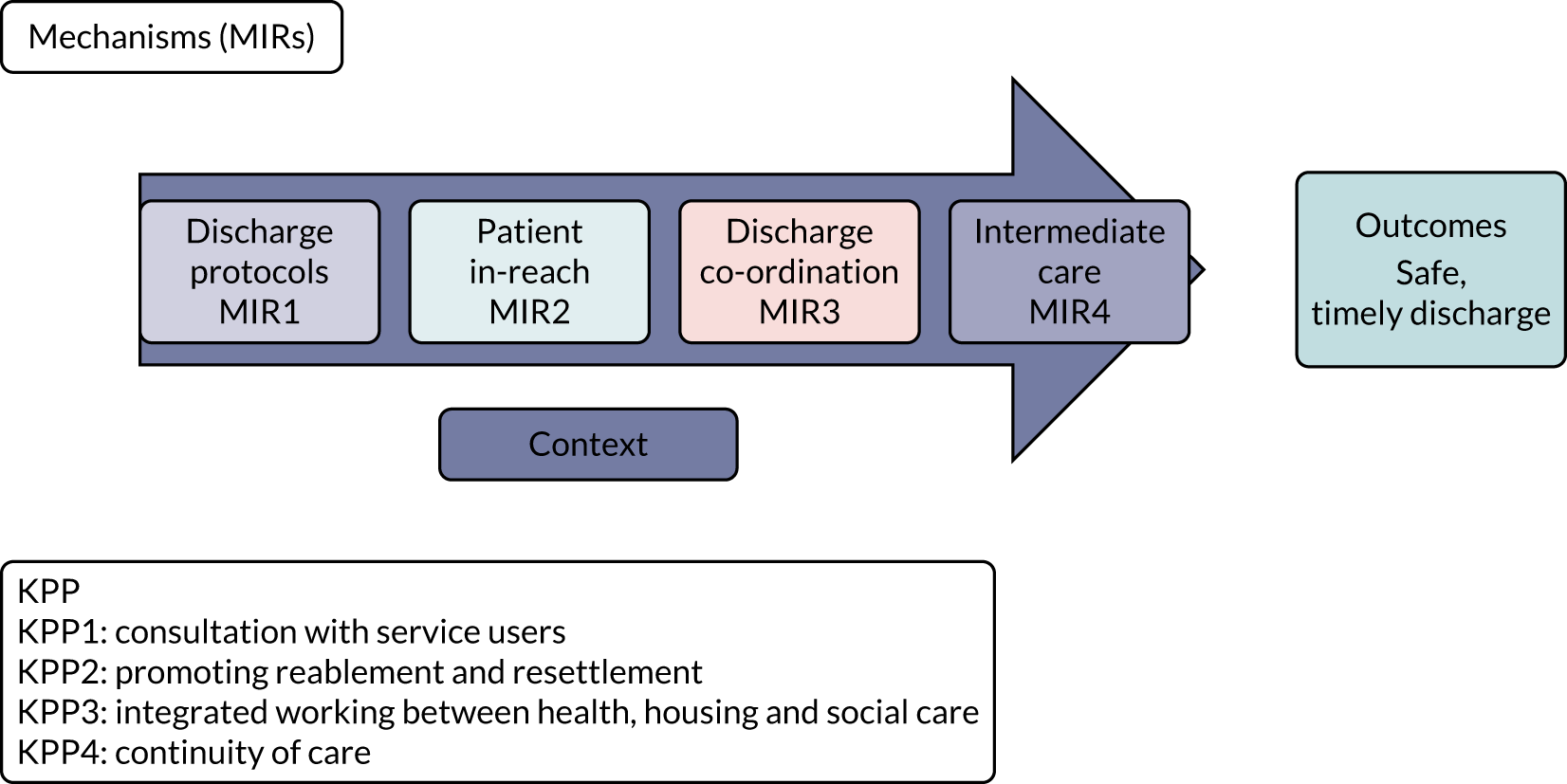
Implementation
The second objective of the study was explore how HHDSs were being developed and implemented across England. A documentary analysis and series of preliminary interviews revealed that the HHDSs were employing mechanisms in different ways and in different combinations. Some offered a specialist discharge co-ordination service (MIR3) (ending support when the patient left the acute sector/hospital), whereas others combined discharge co-ordination with a period of ‘step-down’ intermediate care (MIR4). Specialisation or sensitisation was mainly at the level of skills and staffing (e.g. employing clinicians and other professional and non-professional workers who had developed a ‘special interest’ in homelessness, especially legal literacy pertaining to housing law). The integration of housing alongside health and social care was another defining feature of the HHDSs, for example using ‘step-down’ accommodation provided through a housing association as an alternative pathway out of hospital.
-
The most common model was for a housing worker to ‘in-reach’ into the hospital (MIR2up), including building relationships with patients on the ward, assisting with discharge co-ordination [MIR3up] and then offering short-term ‘step-down’ peripatetic (floating) support until housing and longer-term community services were in place and working well (MIR4hf). These teams were found to be usually housing led (uniprofessional) rather than multidisciplinary.
-
In hospitals with large numbers of homeless patients (i.e. ≥ 200 per year), housing and resettlement support was often embedded as part of a specialist ‘clinically led’ MDT, comprising GPs, nurses, therapy and social work staff. Homeless health-care teams undertake multidisciplinary discharge co-ordination (MIR3mdt), but also offer ‘clinical advocacy’ (or primary care or patient in-reach) (MIR2mdt) to address common problems, such as early self-discharge. These teams usually close cases at the point of discharge and do not routinely provide step-down care (MIR4-missing).
-
A smaller number of sites developed dedicated residential step-down facilities exclusively for patients who were homeless (MIR4res). Other sites allocated ‘step-down’ beds in homeless hostels or earmarked accommodation that was dispersed in the community. These sites did not always encompass resources for workers to in-reach into the hospital to support discharge co-ordination (MIR2/3 missing).
-
One of the sites had access to both a clinically led multidisciplinary homeless health-care team and also a 14-bed dedicated residential step-down facility. This site was employing additional HICM principles to create a fully joined-up or integrated pathway out of hospital. For example, the site was using ‘trusted assessors’ (MIR5) so that homeless patients had to tell their story only once (i.e. staff at the hospital had direct referral rights into the intermediate care facility and, therefore, preventing the duplication of assessments) and ‘flexible working’ with staff from the hospital-based homeless care team provided clinical support into the step-down unit to ensure continuity of health care. Our hunch was that this would be the most effective and cost-effective site because it had all the ‘jigsaw pieces’ with lots of examples of implementing KPPs, such as ensuring that patients had choice and control (MIR1/2/3/4/5 + KPP1/2/3/4).
Importantly, the documentary analysis allowed for further programme theory refinements with regard to recognition of different typologies within mechanisms (Figure 21).
FIGURE 21.
Different typologies within principle mechanism resources.
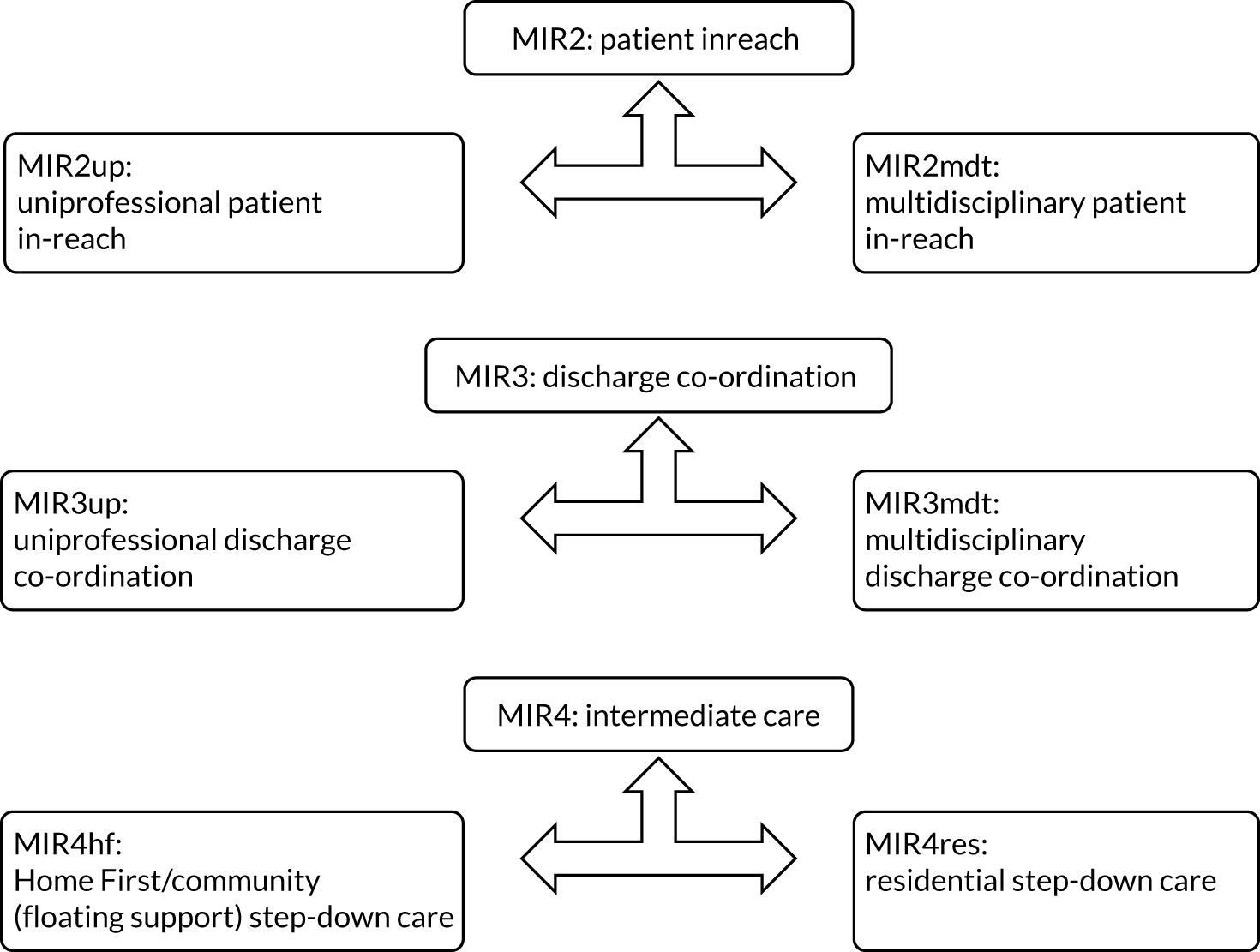
Testing programme theory
To test our programme theory about ‘what works best’, three WPs generated qualitative and quantitative evidence that was then triangulated to reach an overall conclusion. WP1 generated seven case studies of different HHDS configurations. Sites were selected purposively to enable study of HHDSs with (1) all the ‘jigsaw pieces’, (2) different pieces of the jigsaw missing (e.g. no step-down care) and (3) standard care (i.e. sites that had no specialist MIRs in place). WP1 (objective 3) explored these different configurations comparatively from the perspective of people who were homeless (following their out-of-hospital care journeys) over a 3-month period (T1, n = 70 + T2, n = 34). WP1 also interviewed a wide range of other stakeholders (e.g. scheme managers and practitioners n = 77). WPs 2 and 3 (objective 4) explored how HHDSs have an impact on outcomes and different patterns of service use across the whole system (e.g. use of unplanned care) and the associated cost implications of this.
Results
Table 25 presents a summary table of the findings. It sets out the initial tentative programme theory that was tested and then brings together the empirical evidence from across the three WPs with regard to evidence that supports the hypothesis, evidence that is silent or unclear and evidence that refutes/does not support the programme theory.
| Evidence | Summary |
|---|---|
| Programme theory tested | Achieving consistently safe and timely transfers of care for patients who are homeless (improved outcomes) will depend on localities developing complex adaptive systems that are underpinned by the HICM: clear protocols for patient flow and early discharge planning (MIR1), access to clinical patient in-reach (MIR2mdt), multidisciplinary discharge co-ordination (encompassing both clinical and housing support) (MIR3mdt) and step-down intermediate care (MIR4), MIRs must be underpinned by four ‘simple rules’ or ‘KPPs’ for engagement and consultative care planning (KPP1), fostering self-care (KPP2), integrated and collaborative working (KPP3), and continuity of care until longer-term services are in place and working well (KPP4) |
| Specialist care is more effective than standard care | |
| + | Specialist care is more effective and cost-effective than standard care (WP3) |
| + | Specialist care ensures more consistent patient flow and reduces DToCs (WP1) |
| +/– | The HHDS group is more likely than others to be readmitted in an emergency, with five times the rate of unplanned hospital readmission and five times the rate of A&E visits than housed people from deprived neighbourhoods |
| Clinically led MDT working/discharge co-ordination (MIR3mdt) is more effective than uniprofessional ‘housing-led’ approaches (MIR3up) | |
| + | Clinical advocacy [patient in-reach (MIR2mdt)] is key to preventing early self-discharge (WP1) |
| + | Clinically led MDT working (MIR3mdt) is a key component in examples of (residential) step-down intermediate care that are cost-effective and cost saving (WP3 literature review) |
| + | Clinically led advocacy [patient in-reach (MIR2mdt)] increases costs for the NHS, but improves access to elective (planned follow-up) care. We interpret this as a positive outcome, indicating that SIHHC is working more effectively than standard care to improve access to health care among a marginalised group for whom one in three deaths are due to conditions amenable to timely health care (WP3) |
| +/– | Uniprofessional housing-led support is shown to be as effective and cost-effective as clinically-led schemes on a wide range of measures (WP3) |
| – | We found no evidence of a difference for our primary outcomes between HHDSs that were clinically led and HHDSs that were housing led (WP2) |
| – | In the HHDS cohort, regardless of scheme typology, readmission rates increased across the board with increasing comorbidities (WP2) |
| Step-down care (MIR4) is more effective than without | |
| + | Poorer outcomes and patient experiences are reported where MIR4 is missing, particularly the absence of residential intermediate care (MIR4res) (WP1) |
| + | HHDSs with direct access to step-down intermediate care (MIR4res) are more cost-effective than those without (WP3) |
| + | In a secondary outcome analysis, we found evidence that A&E visits were 18% lower among homeless patients discharged at a site with a step-down service than in those without a step-down service (WP2) |
| +/– | The review of the published literature alerted us to an emerging evidence base that ‘step-down’ intermediate care is both cost-effective and cost saving. However, there is also strong evidence to suggest that schemes without this component can be cost-effective and cost saving. These findings might, therefore, be taken as a broad indication of the likely benefits of SIHHC per se (WP3 literature review) |
| – | We found no evidence of a difference for our primary outcomes between HHDSs that did and did not encompass ‘step-down’ intermediate care (WP2) |
| – | In the HHDS cohort, regardless of scheme typology, readmission rates increased across the board with increasing comorbidities (WP2) |
Evidence in support of programme theory
Overall, there was good evidence from across the three WPs to support our programme theory about ‘what works best’ to deliver consistently safe, timely transfers of care:
-
Employing a range of different economic modelling techniques, specialist HHDSs were consistently more effective and cost-effective than standard care (WP3).
-
NHS trusts with specialist HHDSs had lower rates of DToCs linked to ‘housing’ than standard care (WP1).
-
Employing a range of different economic modelling techniques, HHDSs with direct access to specialist intermediate care (step down) were more effective and cost-effective than HHDSs that had no direct access to intermediate care (WP3).
-
The data linkage showed that HHDSs with a step-down service were associated with a reduction in subsequent hospital use, with an 18% reduction in A&E visits compared with HHDSs without a step-down service (WP2).
-
Clinical advocacy (patient in-reach) provided by hospital-based homeless health-care teams increased access to planned (elective) follow-up care. This is an especially important outcome, as one in three deaths of people in our homeless hospital discharge cohort were due to common conditions (e.g. heart disease) that are amenable to timely health care.
Evidence that troubles programme theory
The data linkage shows that the HHDS cohort were more likely to be readmitted in an emergency, with five times the rate of unplanned hospital readmissions and five times the rate of A&E visits than housed people from deprived neighbourhoods. The data linkage also shows that one in three deaths of those in the hospital discharge cohort are from conditions that are amenable to timely health care. Although these outcome data introduce concerns regarding our programme theory (i.e. raise uncertainties about the efficacy of the HICM to deliver its intended outcomes), they are, we suggest, more indicative of a need to find ways to ensure that HHDSs have more of an impact. Using the metaphor of the lighthouse, we would argue that since the end of the HHDF, the lack of sustained recurrent funding has progressively dimmed their effects.
Need for increased investment in intermediate care
National audits of intermediate care135–137 (carried out in England until 2018) acknowledge a significant lack of investment and suggest that the capacity for intermediate care for all patient groups remains stubbornly stuck at a level below the threshold for whole-system impact. In one study, it is suggested that reablement provision needs to be increased by 200%. 24 One consequence of a lack of funding for intermediate care has been to tighten eligibility for the service. Although earlier guidance confirmed that this service should be accessible to homeless patients, later guidance has been silent on this matter, meaning that there has been little imperative to ‘mainstream’ the services piloted under the HHDF banner.
In Chapter 3, we described how the lack of investment in HHDSs is having an impact on scheme fidelity and the ability to achieve intended outcomes (i.e. the dimmer switch effect). Some HHDSs ceased to operate, whereas others have progressively reduced in reach and scale, sometimes reducing the number of hospitals that they are able to work with or reducing the size of the team (workforce). In one site, the increasing gap between workforce capacity and demand led to a range of problems, including recruitment and retention difficulties (resulting low team morale) and an increased focus on freeing-up hospital beds rather than other aspects of the service (such as patient advocacy). This was associated with poorer outcomes, including discharge to the street.
Need to increase delayed transfers of care (i.e. end discharge to the street)
As touched on above, where services were inadequate or lacking, it remained (tacitly) accepted practice (across both standard and specialist care sites) to discharge homeless patients to the streets rather than delay their transfer of care. Eradicating the ‘poor practice’ that led to discharge to the street was a key objective of the HHDF. However, we found little evidence to suggest that HHDSs had ‘fired’ a change in reasoning with regard to the stigma and cultural distance that positions ‘homeless patients’ as somehow less vulnerable and/or deserving than other groups of patients. We observed that patients who were homeless and using substances were particularly affected by unsafe discharge, especially when their behaviour was perceived to be challenging. Viewed through the lens of adult safeguarding, unsafe discharge may be viewed as neglect (acts of omission and a failure to provide access to appropriate health, care and support). 138 Strengthening adult safeguarding to challenge unsafe discharge is, therefore, an additional MIR necessary to improve outcomes. Certainly, we found no evidence that HHDSs could be deployed as short-term interventions to upskill hospital staff on homelessness issues. Once schemes ended, the high turnover of hospital staff meant that any benefits soon evaporated.
As homeless patients are discharged to the street (unsafely) rather than ‘delayed’ and counted as a DToC, this means that capacity issues linked to housing (i.e. ‘no place to discharge to’) are rendered largely invisible. When DToCs reach crisis point, the government will usually intervene to create extra capacity in adult social care provision. In the winter of 2016/17, DToCs hit an all-time high when, on average, 6660 people were being ‘delayed’ every day in NHS beds. In March 2017, the government introduced a new target to reduce the level of bed-days ‘lost’ to 3.5% and announced an extra £2B of funding for social care services. DToC metrics are, therefore, an important lever for system transformation in that they enable partners to work together to address pinch points in the system. Without this intelligence, the true impact of specialist HHDSs is likely to remain unknown and, as a consequence, appropriate levels of investment in their future unlikely to be forthcoming. From August 2020, new hospital discharge guidance was introduced by NHSE&I,91 including new arrangements for recording delays. The new system measures the number of people who have a length of stay over 14 and 21 days who have been judged as ready to discharge but who continue to reside in a hospital bed. Category xiii covers people who ‘continue to reside’ because of ‘homelessness/no right of recourse to public funds/no place to discharge to’91 (contains public sector information licensed under the Open Government Licence v3.0).
Need for increased investment in housing, care and support
The second dampening effect was shown to be the wider context in which some HHDSs were situated (i.e. where there was a shortage of housing, care and support). The findings of this study strongly support those reported in the national evaluations of intermediate care for older people, where it is reported that interventions that are shown to work well in areas with well-resourced and efficient community support services will have much reduced impact in areas where services are inadequate or lacking. 83 In Chapter 3, we observed how HHDSs could become blocked, as these ‘time-limited’ interventions started to substitute for permanent supportive housing.
Need for investment in chronic care management
Compared with the comparator group (matched housed patients), patients in the HHDS cohort had much higher levels of multimorbidity or combinations of long-term conditions or illnesses, with 8% of patients having five or more conditions (vs. 3% in the comparator group).
The data linkage confirms previous findings that external causes of death are considerably more common in homeless groups than in those from socially deprived areas. However, this investigation also highlights the importance of causes such as coronary heart disease, respiratory disease and cancer in homeless people. Compared with the recent ONS analysis of deaths of homeless people in England and Wales, we found that the proportion of deaths due to cancers and chronic lower respiratory disease was higher, and the proportion of alcohol- and drug-related deaths and suicide deaths was lower. In the comparator group, women and men were nearly two times more likely to die than the general population. In the homeless hospital discharge group, women were nine times, and men seven times, more likely to die than the general population. In the homeless hospital discharge group, 600 patients died between 1 November 2013 and 30 November 2016. Males made up 78% of deaths. The median age of death was 52 years for the homeless hospital discharge group and 72 years for the comparator group.
These findings alert us to the strong possibility that, regardless of scheme typology, the benefits of any type of short-term (time-limited) intervention targeted at this specific population group will quickly evaporate if they are not embedded as part of a fully integrated complex adaptive system that encompasses adequate provision for longer-term chronic care management and, indeed, palliative care. It surely goes without saying that more preventive working is needed to reduce homelessness and prevent these conditions from arising in the first place.
Mixed evidence for multidisciplinary team working
The economic evaluation (WP2) provides robust evidence that ‘clinically led’ (multidisciplinary) HHDSs increase the number of elective readmissions (i.e. access to planned follow-up care). Therefore, there is a strong case to be made that increasing investment (scaling-up) these HHDSs could work to reduce the numbers of deaths due to conditions that are amendable to timely health care.
However, the economic evaluation also finds that (cheaper) uniprofessional (housing-led) schemes are as effective and cost-effective as multidisciplinary (clinically led) schemes on a wide range of other measures (WP2). In this present study, we observed that clinically led teams, because of their primary focus on improving the quality of inpatient care [i.e. patient in-reach and discharge co-ordination (MIR2/3)], do not provide the same level of access to ‘step-down’ care as housing-led schemes (MIR4). A distinctive feature of nearly all the housing-led schemes is that workers ‘in-reach’ into the hospital and will then provide floating support for a time-limited period until community services are in place and working well (MIR4hf). This association with intermediate care (continuity of support post exit from the acute sector) may be the more significant factor in accounting for the comparable performance of housing-led schemes on some key measures (i.e. clouding our understanding of any distinctions to be drawn between multidisciplinary and uniprofessional working). A key finding of the qualitative phase of the study was how quickly the benefits of a hospital stay could evaporate where there was a lack of practical support immediately after discharge. In other words, a lack of intermediate care (MIR4) may dampen the effects of specialist MDT working and discharge co-ordination (MIR3mdt).
Indeed, it is important to acknowledge the value of uniprofessional housing-led HHDSs. Most likely, these positive results are reflecting the value of good-quality ‘floating support’ in bridging the gap between the hospital and the community. This is an important point because housing- and community- (voluntary-) led services are often assumed by commissioners to be the ‘icing on the cake’ and, therefore, the most easily dispensable part of the out-of-hospital care system. 86 Arguably, this evaluation establishes that they are far more important than has hitherto been assumed in terms of adding value for both the NHS and the wider public sector.
Summary of findings and road map
In summary, the empirical data from across the three WPs strongly support our original programme theory that achieving outcomes linked to consistently safe and timely transfers of care for patients who are homeless will depend on localities developing complex adaptive systems that are underpinned by the HICM. This encompasses clear protocols for patient flow and early discharge planning (MIR1), access to clinical patient in-reach (MIR2mdt), multidisciplinary discharge co-ordination (encompassing both clinical and housing support) (MIR3mdt) and step-down intermediate care (MIR4). MIRs must be underpinned by four KPPs for engagement and consultative care planning (KPP1), fostering self-care (KPP2), integrated and collaborative working (KPP3), and continuity of care until longer-term services are in place and working well (KPP4). In addition, our field data highlights the importance of strong leadership (MIR6) to nurture the complex adaptive system, putting in place additional mechanisms that glue the different pieces of the jigsaw together [e.g. flexible working and trusted assessment (MIR5)]. All these mechanisms and KPPs are vital to the creation of a seamless ‘out-of-hospital’ care pathway. Finally, strengthening adult safeguarding (MIR7) is a key mechanism needed to mitigate dampening effects (e.g. underfunded discharge schemes and shortages of permanent supportive housing, care and support) that can increase the likelihood of unsafe discharge. Figure 22 summarises these findings by means of a ‘road map’ of the complex set of factors that commissioners need to consider to deliver consistently safe, timely transfers of care for patients who are homeless. We include a set of audit questions that capture the key function of each mechanism.
FIGURE 22.
Road map and quick audit questions.
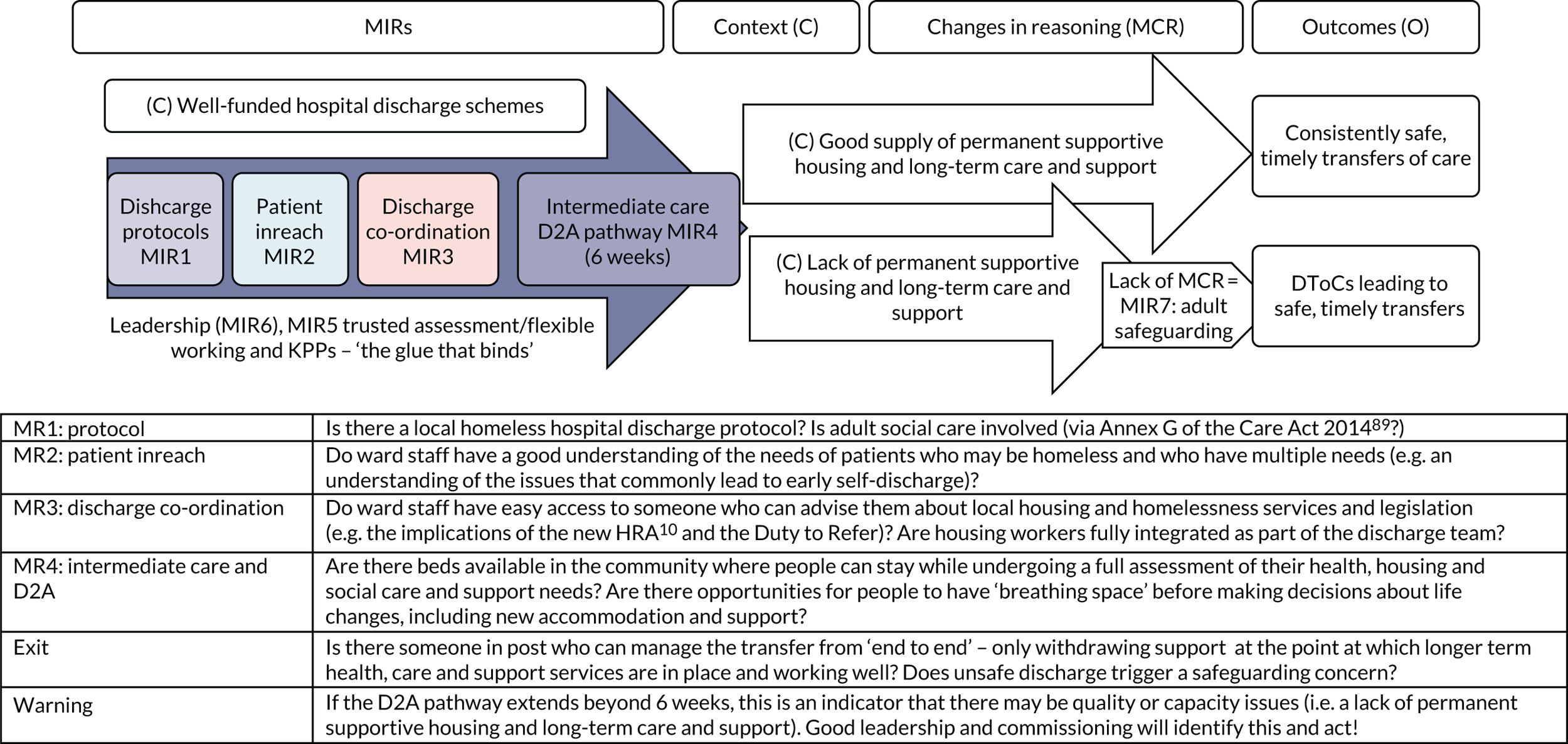
Implications for managers and impact of COVID-19
Earlier, we touched on the issue of sustainability and how once the initial HHDF pilot funding ended many of the hospital discharge schemes were reduced in scale or closed down. One reason for this may have been that HHDSs were developed as ‘homeless services’ and were not linked to other work going on inside hospitals and in the community to improve patient flow and tackle DToCs. As a result, we would conclude that the most important implication of this research for managers is that any future work to address homelessness at the point of discharge must be integrated as part of these wider local strategic frameworks for developing pathways out of hospital.
Much of the work to develop out-of-hospital care is linked to the government’s programme for ‘Integration and Better Care Funding’ (BCF). 34 This is the main source of funding for intermediate care (Home First). The BCF places clear expectations on health and well-being boards to oversee health and social care, including (1) pooling budgets, (2) integrating services to ensure that more people can leave hospital when they are ready and (3) following guidelines laid down by the HICM.
The HICM has been at the centre of this research because of its centrality to driving improvements in out-of-hospital care. In addition to the road map above, we have produced a ‘tool kit’139 to guide managers on how each of these various changes can be sensitised and implemented (in a wide range of contexts) to meet the needs of homeless patients. The ‘tool kit’ covers small-scale practice changes, such as showing ‘concerned curiosity’ about patients’ housing circumstances on admission to hospital (change 1: early discharge planning). It also includes guidance on commissioning and developing new specialist (housing-led) ‘step-down’ services, which will require significant investment to create alternative pathways out of hospital for people who cannot go straight home (change 4: Home First). The research here has clearly demonstrated that specialist ‘step down’ services can contribute to meeting targets linked to the BCF (such as reducing A&E attendances) and will hopefully lever the financial investment that specialist care needs to be sustainable into the future.
COVID-19 has also reinforced the value and importance of out-of-hospital care. As noted above, to free-up beds in the acute sector to accommodate COVID-19 patients, new hospital discharge guidance was issued in 2020,91 along with a refreshed and updated HICM. The overall objective of this new guidance was to speed-up the delivery of the long-held transformational goal of vastly increasing capacity in D2A. Under the old guidance for DToCs, the decision to transfer was based on a MDT decision that the person was clinically optimised and safe to transfer. Under the new guidance, patients are to be discharged on the same day they are clinically optimised. They are to be moved out of hospital on to one of four ‘D2A pathways’, with the multidisciplinary processes (including continuing health care and Care Act 201489 assessments) taking place after discharge. Without sufficient investment in specialist step-down services and alternative pathways for people who cannot go straight home, there is a real danger that these new arrangements will spin the carousel even faster for homeless patients, with more unsafe discharges to the street.
Although realist evaluation is designed to understand how mechanisms fire changes in reasoning, much of the positive change we identified in this study flowed from the additional resource itself, for example having housing workers on hand to take pressure of ward staff and to support people immediately after discharge. The stigma and cultural distance that underpins ‘poor practice’ (e.g. discharge to the street) was not strongly affected by HHDSs. The more HHDSs became assimilated into the hospital to sustain their own funding (and, therefore, less able to advocate for homeless patients), then the more they became hostages to the wider culture of ‘patient flow’ and freeing-up beds at all costs. It is good news that the latest hospital discharge guidance91 gives a clear statement that homeless patients should not be discharged to the street. However, strong leadership (MIR6) from national safeguarding leads will be necessary to police this.
Implications for future research
New hospital discharge guidance has been introduced since the time of the fieldwork. 91 This strongly supports the recommendations of this study with regard to the importance of developing intermediate care and alternative pathways out of hospital.
-
The impact of these new arrangements should be evaluated, taking forward the methodological learning from this study, namely to understand effectiveness across the chain of preventative, intermediate and long-term care management in any given locality. A danger with the evaluative gaze that we have employed in this research (particularly the data linkage) is that HHDS may be identified as an ineffective intervention rather than a key component in a wider chain that needs of strengthening.
Shining a spotlight on the whole system will, however, require significant methodological development, especially in the areas of quantitative and economic evaluation. The analysis presented here should be seen as a rather conservative test that relies on traditional gold-standard measures, such as EQ-5D, which, although captures health outcomes, does not illuminate the benefits beyond the NHS. The challenge is to develop more robust evidence to better monitor and compare the performance of HHDSs in terms of standardised economic, quality-of-life and social value indicators for the broader public sector.
-
We see considerable value in testing tools such as ‘discreet choice experiment’,140 which would illuminate value from a much broader perspective, including that of service users.
Only one of the research sites we visited during the research had developed a robust system for collecting local performance management (audit) data.
-
Any proposed future research should seek to work in partnership with local projects to improve these systems.
-
There is much scope to develop a ‘dashboard’ of indicators (i.e. a set of standardised measures) and to provide support to HHDSs to use them routinely. This should also encompass different parameters of interest (e.g. effectiveness, quality of care, economic outcomes and user experience).
Strengthening these internal monitoring procedures could potentially make the task of undertaking longer-term quantitative research much easier, perhaps overcoming some of the challenges (costs) associated with trying to follow-up large numbers of people identified as ‘hard to reach’ (e.g. because they have no fixed address).
-
A dashboard (developed with associated technology such as a mobile application) that could feedback meaningful results easily and cost-effectively could provide commissioners with more usable information (e.g. average cost of a step-down bed) and, ultimately, more confidence to commission and sustain specialist services.
Acknowledgements
We are grateful to all those who gave up their time to take part in the study and to share their expertise and experiences. Special thanks to all the projects that hosted the research and shared their valuable data and learning with us. Thanks also to members of our Study Steering Committee and colleagues at NIHR, Ministry for Housing, Communities and Local Government, DHSC, NHS England, the Local Government Association, Homeless Link, Pathway and Queen’s Nursing Institute who supported the research and its dissemination. We are especially grateful to Ann Rennie for all her hard work in transcribing the interview data, Dee Menezes, Dan Lewer, Ruth Blackburn and Hannah Evans who worked extensively on the data linkage, and Stan Burridge, Daren O’Shea and Joanne Coombes (members of our lived experience group) who brought the research to life at many conferences and events and have played a key role in ensuring that the project has some real impact among commissioners and policy-makers.
Contributions of authors
Michelle Cornes (https://orcid.org/0000-0001-5445-8592) was responsible for the overall design and delivery of the project, contributed to primary data collection (WP1), wrote the Abstract and Plain English summary, led the analysis for WP1 and co-authored the Scientific summary and Chapters 1–3 and 6.
Robert W Aldridge (https://orcid.org/0000-0003-0542-0816) contributed to the design of the study, led WP2 (data linkage) and wrote Chapter 4. He co-authored the Scientific summary and Chapters 1 and 6.
Elizabeth Biswell (https://orcid.org/0000-0003-1104-3535) undertook primary data collection across one of the main fieldwork sites, contributed to the writing of Chapter 2 (engaging with hard-to-reach populations) and reviewed sections of the report for clarity and content.
Richard Byng (https://orcid.org/0000-0001-7411-9467) contributed to the design of study, provided expertise on realist evaluation and reviewed sections of the report for clarity and content.
Michael Clark (https://orcid.org/0000-0003-4964-5005) contributed to the design of study, provided expertise on integrated care and reviewed sections of the report for clarity and content.
Graham Foster (https://orcid.org/0000-0002-3704-386X) contributed to the design of study, provided expertise on statistical issues and reviewed sections of the report for clarity and content.
James Fuller (https://orcid.org/0000-0003-0095-2338) contributed to the design and delivery of the study as an ‘expert by experience’ and reviewed sections of the report for clarity and content.
Andrew Hayward (https://orcid.org/0000-0002-3549-6232) contributed to the design of the study, provided methodological expertise on data linkage and reviewed sections of the report for clarity and content.
Nigel Hewett (https://orcid.org/0000-0002-7049-9252) contributed to the design of the study, facilitated access to fieldwork sites, provided clinical expertise and reviewed sections of the report for clarity and content.
Alan Kilmister contributed to the design and delivery of the study as an ‘expert by experience’ and reviewed sections of the report for clarity and content.
Jill Manthorpe (https://orcid.org/0000-0001-9006-1410) contributed to the design of study and edited and reviewed drafts of the final report.
Joanne Neale (https://orcid.org/0000-0003-1502-5983) contributed to the design of the study, provided expertise on undertaking mixed-methods research and reviewed sections of the report for clarity and content.
Michela Tinelli (https://orcid.org/0000-0002-8816-4389) contributed to the design of the study, led WP3 (economic evaluation), wrote Chapter 5 and co-authored the Scientific summary and Chapters 1, 2 and 6.
Martin Whiteford (https://orcid.org/0000-0002-1182-0309) contributed to the design of the study, secured ethics approval, led the literature synthesis, undertook primary data collection (WP1) and analysis, co-authored Chapter 3 and reviewed other sections of the report for clarity and content.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Crane M, Cetrano G, Joly L, Coward S, Daly B, Ford C, et al. Mapping of Specialist Primary Health Care Services in England for People Who are Homeless. London: Social Care Workforce Research Unit, King’s College London; 2018.
- Wong G, Westhorp G, Greenhalgh J, Manzano A, Jagosh J, Greenhalgh T. Quality and reporting standards, resources, training materials and information for realist evaluation: the RAMESES II project. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05280.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Crisis . The Homeless Monitor: England 2018 2018.
- Fitzpatrick S, Johnsen S, White M. Multiple exclusion homelessness in the UK: key patterns and intersections. Soc Policy Soc 2011;10:501-2. https://doi.org/10.1017/S147474641100025X.
- Aldridge R, Story A, Hwang S, Nordentoft M, Luchenski SA, Hartwell G, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet 2017;391:241-50. https://doi.org/10.1016/S0140-6736(17)31869-X.
- Mattheys K, Warren J, Bambra C. Treading sand: a qualitative study of the impact of austerity on inequalities in mental health. Soc Policy Adm 2017;52:1275-85. https://doi.org/10.1111/spol.12348.
- House of Commons Committee of Public Accounts . Homeless Households. Eleventh Report of Session 2017–2019 2017. https://publications.parliament.uk/pa/cm201719/cmselect/cmpubacc/462/462.pdf (accessed 23 March 2019).
- British Medical Association . Streets of Shame 2019. www.bma.org.uk/features/streetsofshame/ (accessed 4 June 2021).
- Great Britain . Homelessness Reduction Act 2017 2017.
- Ministry of Housing, Communities and Local Government . Rough Sleeping Strategy 2018.
- Department of Health and Social Care (DHSC) . Hospital Discharge Handbook 2003.
- Glasby J. Hospital Discharge. Oxford: Radcliffe Medical Press; 2003.
- Tansley K, Gray J. Ensuring safe and appropriate discharge for people who are homeless or in housing need. Nurs Times 2009;105:14-7.
- St Mungo’s and Homeless Link . Improving Hospital Admission and Discharge for People Who Are Homeless 2012. www.homeless.org.uk/sites/default/files/site-attachments/HOSPITAL_ADMISSION_AND_DISCHARGE._REPORTdoc.pdf (accessed 10 October 2019).
- Burstow P. Homeless Link and St Mungo’s Publish Report on Hospitals and the Homeless 2012. www.gov.uk/government/news/homeless-link-and-st-mungo-s-publish-report-on-hospitals-and-the-homeless (accessed March 2019).
- Department of Health and Social Care (DHSC) . Homeless Hospital Discharge Fund 2013–2014: Eligibility Criteria 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/198037/Eligibility_Document_FINAL.pdf (accessed 10 October 2019).
- Cowpe J, Rowe B, Beech R. Intermediate and Continuing Care Policy and Practice. London: Blackwell Publishing; 2005.
- Bolton J. Reducing Delays in Hospital Transfers of Care for Older People: Key Messages in Planning and Commissioning 2018. https://ipc.brookes.ac.uk/publications/pdf/Some_key_messages_around_hospital_transfers_of_care.pdf (accessed 10 October 2019).
- Department of Health and Social Care, Association of Directors of Adult Social Services and NHS England . Quick Guide: Discharge to Assess. Transforming Urgent and Emergency Care Services in England n.d. www.nhs.uk/NHSEngland/keogh-review/Documents/quick-guides/Quick-Guide-discharge-to-access.pdf (accessed 26 May 2019).
- National Institute for Health and Care Excellence (NICE) . Intermediate Care Including Reablement. NICE Guideline [NG74] 2017. www.nice.org.uk/guidance/ng74 (accessed 10 October 2019).
- Department of Health and Social Care . National Service Framework for Older People 2001. www.gov.uk/government/publications/quality-standards-for-care-services-for-older-people (accessed 10 October 2019).
- Department of Health and Social Care . Intermediate Care – Halfway Home. Updated Guidance for the NHS and Local Authorities 2009. https://webarchive.nationalarchives.gov.uk/20130124050747/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@pg/documents/digitalasset/dh_103154.pdf (accessed 10 October 2019).
- Newton Europe . People First, Manage What Matters 2019. https://reducingdtoc.com (accessed 10 October 2019).
- Pearson M, Hunt H, Cooper C, Shepperd S, Pawson R, Anderson R. Providing effective and preferred care closer to home: a realist review of intermediate care. Health Soc Care Community 2015;23:577-93. https://doi.org/10.1111/hsc.12183.
- Cornes M, Whiteford M, Manthorpe J, Neale J, Byng R, Hewett N, et al. Improving hospital discharge arrangements for people who are homeless: a realist synthesis of the intermediate care literature. Health Soc Care Community 2018;26:e345-59. https://doi.org/10.1111/hsc.12474.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 2008.
- Kaambwa B, Bryan S, Barton P, Parker H, Martin G, Hewitt G, et al. Costs and health outcomes of intermediate care: results from five UK case study sites. Health Soc Care Community 2008;16:573-81. https://doi.org/10.1111/j.1365-2524.2008.00780.x.
- Housing Learning and Information Network . Homelessness Prevention and Hospital Discharge: Three Case Studies. Case Study 46 (June) 2009.
- Medcalf P, Russell G. Homeless healthcare: raising the standards. Clin Med 2014;128:1033-5. https://doi.org/10.7861/clinmedicine.14-4-349.
- Douthwaite B, Mayne J, McDougall C, Paz-Ybarnegaray Y. Evaluating complex interventions: a theory-drive realist informed approach. Evaluation 2017;23:294-311. https://doi.org/10.1177/1356389017714382.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Local Government Association, Department of Health and Social Care, Association of Directors of Adult Social Care, NHS England and NHS Improvement . High Impact Change Model. Managing Transfers of Care Between Hospital and Home. A Self-Assessment Tool for Local Health and Care Systems n.d. www.local.gov.uk/our-support/our-improvement-offer/care-and-health-improvement/systems-resilience/high-impact-change-model (accessed 10 October 2019).
- GOV.UK . Better Care Fund: How It Will Work in 2019 to 2020 2019. www.gov.uk/government/publications/better-care-fund-how-it-will-work-in-2019-to-2020 (accessed 10 October 2019).
- Godfrey M, Townsend J, Cornes M, Donaghy E, Hubbard G, Manthorpe J. Reimbursement in Practice: The Last Piece of the Jigsaw. A Comparative Study of Delayed Discharge in England and Scotland. Leeds: University of Leeds; 2008.
- Pearson M, Hunt, H, Cooper C, Shepperd S, Pawson R, Anderson R. Intermediate Care: A Realist Review and Conceptual Framework. Final Report 2013. www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwiTwuSWr_nxAhXQesAKHZkiDtIQFjAAegQICBAD&url=https%3A%2F%2Fwww.bl.uk%2Fbritishlibrary%2F~%2Fmedia%2Fbl%2Fglobal%2Fsocial-welfare%2Fpdfs%2Fnon-secure%2Fi%2Fn%2Ft%2Fintermediate-care-a-realist-review-and-conceptual-framework.pdf&usg=AOvVaw32eZIjWCsvsz5Of4yqdUzn (accessed 4 June 2021).
- Parker-Radford D. Identifying standards to ensure seamless discharge to primary care for homeless people. Prim Health Care 2015;25:28-31. https://doi.org/10.7748/phc.25.3.28.e1015.
- Glennerster R, Sales K. Establishing a hospital healthcare team in a district general hospital – transforming a model into a reality. Hous Care Support 2019;22:65-76. https://doi.org/10.1108/HCS-09-2018-0022.
- Zana K, Haine P, Dorney-Smith S. The GP role in improving outcomes for homeless inpatients. Hous Care Support 2019;22:15-26. https://doi.org/10.1108/HCS-07-2018-0017.
- Lane R. The Road to Recovery. A Feasibility Study into Homeless Intermediate Care 2005. www.housinglin.org.uk/_assets/Resources/Housing/Housing_advice/The_Road_to_Recovery_-_A_feasibility_study_into_homelessness_and_intermediate_care_December_2005.pdf (accessed 10 October 2019).
- Bauer J, Moughamian A, Viloria J, Schneidermann M. Leaving before discharge from a homeless medical respite program: predisposing factors and impact on selected outcomes. J Health Care Poor Underserved 2012;23:1092-105. https://doi.org/10.1353/hpu.2012.0118.
- Hewett N, Halligan A, Boyce T. A general practitioner and nurse led approach to improving hospital care for homeless people. BMJ 2012;345. https://doi.org/10.1136/bmj.e5999.
- Cornes M, Aldridge R, Byng R, Clark M, Foster G, Fuller J, et al. Improving hospital discharge arrangements for people who are homeless: the role of specialist integrated care. Int J Integr Care 2018;18:1-8. https://doi.org/10.5334/ijic.s2018.
- Albanese F, Hurcome R, Mathie H. Towards an integrated approach to homeless hospital discharge: an evaluation of different typologies across England. J Integr Care 2016;24:4-44. https://doi.org/10.1108/JICA-11-2015-0043.
- Dorney-Smith S, Hewett N. Options for Delivery of Homeless ‘Medical Respite’ Services. London: Pathway; 2016.
- Backer TE, Howard EA, Moran GE. The role of effective discharge planning in preventing homelessness. J Prim Prev 2007;28:229-43. https://doi.org/10.1007/s10935-007-0095-7.
- Canham SL, Davidson S, Custodio K, Mauboules C, Good C, Wister AV, et al. Health supports needed for homeless persons transitioning from hospitals. Health Soc Care Community 2019;27:531-45. https://doi.org/10.1111/hsc.12599.
- Gillespie K. Beyond the Ward: An Evaluation of a Homeless Hospital Discharge Project 2016. https://issuu.com/derventio/docs/healthy_futures_two-year_evaluation (accessed 1 September 2017).
- Wade J. Hospital Discharge Fund: External Project Evaluation. Gateshead: Oasis Aquila Housing; 2014.
- Dorney-Smith S, Hewett N, Khan Z, Smith R. Integrating health care for homeless people: experiences of the KHP Pathway Homeless Team. Br J Healthc Manage 2016;22:215-24. https://doi.org/10.12968/bjhc.2016.22.4.215.
- Drury LJ. From homeless to housed: caring for people in transition. J Community Health Nurs 2008;25:91-105. https://doi.org/10.1080/07370010802017109.
- Whiteford M, Simpson G. A codex of care: assessing the Liverpool hospital admission and discharge protocol for homeless people. Int J Care Coord 2015;18:65-70. https://doi.org/10.1177/2053434515603734.
- Hochron J, Brown E. Ensuring appropriate discharge practices for hospitalized homeless patients. World Med Health Policy 2013;5:175-81. https://doi.org/10.1002/wmh3.37.
- Charles N, Hobson G, Hardwick R, Anderson R. Evaluation of the Bay6 Service for Homeless Patients in Three Devon Hospitals 2015. http://clahrc-peninsula.nihr.ac.uk/uploads/attachments/Projects/Bay6_Final%20evaluation%20report_July%202015.pdf (accessed 1 September 2017).
- Halligan A, Hewett N. Perspectives on the Homeless Patient. London: Pathway; 2011.
- Dorney-Smith S. Nurse-led homeless intermediate care: an economic evaluation. Br J Nurs 2011;20:1193-7. https://doi.org/10.12968/bjon.2011.20.18.1193.
- Tomita A, Herman D. The impact of critical time intervention in reducing psychiatric rehospitalisation after hospital discharge. Psychiatr Serv 2012;63:935-7. https://doi.org/10.1176/appi.ps.201100468.
- Doran KM, Ragins KT, Iacomacci AL, Cunningham A, Jubanyik KJ, Jenq GY. The revolving hospital door: hospital readmissions among patients who are homeless. Med Care 2013;51:767-73. https://doi.org/10.1097/MLR.0b013e31829fafbb.
- Kertesz S, Posner M, O’Connell J, Swain S, Mullins A, Schwartz M, et al. Post-hospital medical respite care and hospital readmissions of homeless persons. J Prev Interv Community 2009;37:129-42. https://doi.org/10.1080/10852350902735734.
- Sadowski L, Kee R, Vanderweele T, Buchanan D. Effects of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA 2009;301:1771-8. https://doi.org/10.1001/jama.2009.561.
- Housing Learning and Information Network . Providing Support to Homeless People When Leaving Hospital: Proving the Case 2014. www.housinglin.org.uk/_assets/Resources/Housing/Practice_examples/Housing_LIN_case_studies/HLIN_CaseStudy94_BCHA.pdf (accessed 9 June 2021).
- Doran KM, Greysen SR, Cunningham A, Tynan-McKiernan K, Lucas GI, Rosenthal MS. Improving post-hospital care for people who are homeless: community-based participatory research to community-based action. Healthc 2015;3:238-44. https://doi.org/10.1016/j.hjdsi.2015.07.006.
- van Laere I, de Wit M, Klazinga N. Shelter-based convalescence for homeless adults in Amsterdam: a descriptive study. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-208.
- Hendry C. Economic Evaluation of the Homeless Intermediate Care Pilot Project 2009. http://s3.amazonaws.com/zanran_storage/www.lambethpct.nhs.uk/ContentPages/1168320145.pdf (accessed 1 January 2018).
- Whiteford M, Simpson G. Who is left standing when the tide retreats? Negotiating hospital discharge and pathways of care for homeless people. Hous Care Support 2015;8:125-35. https://doi.org/10.1108/HCS-08-2015-0014.
- Dorney-Smith S, Hewett N, Burridge S. Homeless medical respite in the UK: a needs assessment for South London. Br J Healthc Manag 2016;22:405-13. https://doi.org/10.12968/bjhc.2016.22.8.405.
- Lephard A. Bradford Respite & Intermediate Care Support Service. Bradford: Bevan Healthcare; 2015.
- O’Carroll A, O’Reilly F, Corbett M, Quinn L. Homelessness, Health and the Case for an Intermediate Care Centre. Dublin: Mountjoy Street Family Practice; 2006.
- Lewis H. St Mungo’s Broadway Hospital to Home Pilot Evaluation. London: Crunch Consulting; 2014.
- Homeless Link . Evaluation of the Hospital Discharge Fund 2015. www.homeless.org.uk/sites/default/files/site-attachments/Evaluation%20of%20the%20Homeless%20Hospital%20Discharge%20Fund%20FINAL.pdf (accessed 10 October 2019).
- St John Ambulance . Hastings Homeless Service: Conquest Hospital Partnership Development Pilot Project July 2008–August 2009 2009.
- Burdett Trust for Nursing . Towards System Leadership – Defining the Role and Potential of Nurses Working in Homeless Hospital Discharge 2019. www.pathway.org.uk/wp-content/uploads/Burdett-Trust-for-Nurses-project-summary-edit-21st-June.pdf (accessed 1 October 2020).
- Manthorpe J, Samsi K, Joly L, Crane M, Gage H, Bowling A, et al. Service provision for older homeless people with memory problems: a mixed-methods study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07090.
- Crane M, Joly L, Manthorpe J. Rebuilding Lives: Formerly Homeless People’s Experiences of Independent Living and their Longer Term Outcomes. London: The Policy Institute at King’s/Social Care Workforce Research Unit; 2016.
- Lowson K, Hex N. Evaluation of the Bradford Respite and Integrated Care and Support Services (BRICSS). York: York Health Economics Consortium; 2014.
- Moriarty J, Steils N, Manthorpe J. Mapping Hospital Social Work. London: King’s College London; 2019.
- Pathway and Faculty for Homeless and Inclusion Health . Homeless and Inclusion Health Standards for Commissioners and Service Providers Version 3.1 2018.
- Hewett N, Buchman P, Musariri J, Sargeant C, Johnson P, Abeysekera K, et al. Randomised controlled trial of GP-led in-hospital management of homeless people (‘Pathway’). Clin Med 2016;16:223-9. https://doi.org/10.7861/clinmedicine.16-3-223.
- SERI Insight . Evaluation of Plymouth Hospital to Housing Support Service 2014. www.housinglin.org.uk/_assets/Resources/Housing/OtherOrganisation/BCHAPlymouthFinal.pdf (accessed September 2017).
- Wood L, Wood N, Vallesi S, Stafford A, Davies A, Cumming C. Hospital collaboration with a Housing First program to improve health outcomes for people experiencing homelessness. Hous Care Support 2019;22:27-39. https://doi.org/10.1108/HCS-09-2018-0023.
- Khan Z, Koehne S, Haine P, Dorney-Smith S. Improving outcomes for homeless inpatients in mental health. Hous Care Support 2019;22:77-90. https://doi.org/10.1108/HCS-07-2018-0016.
- White J. Homelessness and Hospital Discharge in the Wirral: An Investigation into the Hospital Discharge Project. Oxford: Centre for Health Service Economics and Organisation; 2011.
- Barton P, Bryan S, Glasby J, Heweitt G, Jagger C, Kaambwa B, et al. A National Evaluation of the Costs and Outcomes of Intermediate Care for Older People 2006. www.birmingham.ac.uk/Documents/college-social-sciences/social-policy/HSMC/research/intermediate-care-older-people.pdf (accessed 10 October 2019).
- Podymow T, Turnball J, Tadic V, Muckle W. Shelter-based convalescence for homeless adults. Can J Public Health 2006;97:379-83. https://doi.org/10.1007/BF03405346.
- Herman DB, Conover S, Gorroochurn P, Hinterland K, Hoepner L, Susser ES. Randomized trial of critical time intervention to prevent homelessness after hospital discharge. Psychiatr Serv 2011;62:713-19. https://doi.org/10.1176/ps.62.7.pss6207_0713.
- Cornes M, Weinstein P, Manthorpe J. The Evaporation Effect: Final Evaluation of the Help the Aged Intermediate Care Programme for Older People. London: Help the Aged; 2006.
- Great Britain . Mental Capacity Act 2005 2005.
- Department of Health and Social Care (DHSC) . Healthcare for Single Homeless People 2010.
- Great Britain . Care Act 2014 2014.
- NHS . Delayed Transfers of Care n.d. www.england.nhs.uk/statistics/statistical-work-areas/delayed-transfers-of-care/ (accessed 7 June 2021).
- HM Government . Hospital Discharge Service: Policy and Operating Model 2020.
- NHS England . Monthly Delayed Transfers of Care Situation Reports: Definitions and Guidance 2015.
- Harwood RH. How to deal with violent and aggressive patients in acute medical settings. J R Coll Physicians Edinb 2017;47:94-101. https://doi.org/10.4997/JRCPE.2017.218.
- Hodson N, Glennerster R. Discharge policies for homeless people and immigrants: compromising professional ethics. Nurs Ethics 2020;27:1355-63. https://doi.org/10.1177/0969733020912518.
- Martineau SJ, Cornes M, Manthorpe J, Ornelas B, Fuller J. Safeguarding, Homelessness and Rough Sleeping: An Analysis of Safeguarding Adults Reviews. London: NIHR Policy Research Unit in Health and Social Care Workforce; 2019.
- Blackburn RM, Hayward A, Cornes M, McKee M, Lewer D, Whiteford M, et al. Outcomes of specialist discharge coordination and intermediate care schemes for patients who are homeless: analysis protocol for a population-based historical cohort. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-019282.
- Aldridge RW, Menezes D, Lewer D, Cornes M, Evans H, Blackburn RM, et al. Causes of death among homeless people: a population-based cross-sectional study of linked hospitalisation and mortality data in England. Wellcome Open Res 2019;4. https://doi.org/10.12688/wellcomeopenres.15151.1.
- Wyatt L. Positive outcomes for homeless patients in UCLH Pathway programme. Br J Healthc Manag 2017;23:367-71. https://doi.org/10.12968/bjhc.2017.23.8.367.
- Crisis . The Homeless Monitor: England 2017 2017.
- Curtis L. Unit Costs of Health and Social Care 2017. Canterbury: PSSRU, University of Kent; 2017.
- Gossop M. The National Treatment Outcomes Research Study (NTORS) and its influence on addiction treatment policy in the United Kingdom. Addiction 2015;110:50-3. https://doi.org/10.1111/add.12906.
- Ashton T, Hempenstall C. Research into the Financial Benefits of the Supporting People Programme, 2009 2009. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/16136/1274439.pdf (accessed 23 May 2019).
- Battrick T, Cook L, Edwards K, Moselle B. Evaluation of the MEAM Pilots – Update on our Findings. London: FTI Consulting; 2014.
- Shelter . Value for Money in Housing Options and Homelessness Services 2010. https://england.shelter.org.uk/__data/assets/pdf_file/0008/297224/VFM_in_housing_options_and_homelessness_services_full_report_Oct_2010.pdf (accessed 23 January 2021).
- Cabinet Office Social Exclusion Task Force . Think Family: Improving the Life Chances of Families at Risk 2010. http://data.parliament.uk/DepositedPapers/Files/DEP2008-0058/DEP2008-0058.pdf (accessed 10 June 2021).
- Home Office . Police Pay: Winsor Review 2011. www.gov.uk/police-pay-winsor-review (accessed 20 February 2021).
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: Centre for Health Economics, University of York; 1999.
- Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ 2004;13:1203-10. https://doi.org/10.1002/hec.901.
- Fenwick E, Marshall DA, Levy AR, Nichol G. Using and interpreting cost-effectiveness acceptability curves: an example using data from a trial of management strategies for atrial fibrillation. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-52.
- Manfrin A, Tinelli M, Thomas T, Krska J. A cluster randomised control trial to evaluate the effectiveness and cost-effectiveness of the Italian medicines use review (I-MYUR) for asthma patients. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2245-9.
- Flatau P, Zaretzky K. The economic evaluation of homelessness programmes. Eur J Homelessness 2008;2:305-20.
- Hewett N, Dorney-Smith S. King’s Health Partners and the Impact of Homelessness 2013. www.pathway.org.uk/wp-content/uploads/2014/10/NEEDS-ASSESSMENT-KHP-EMAIL.pdf (accessed 10 June 2021).
- Dorney-Smith S. Kings Health Partners Pathway Homeless Team. First Year Project Report 2014 2014. www.pathway.org.uk/wp-content/uploads/2015/06/2014-first-year-report-KHP-Pathway-Homeless-Team-final-draft.pdf (accessed 10 June 2021).
- Burnett H, Doherty M. North Middlesex University Hospital Homeless Discharge Team; Summary of Activity and Needs Assessment 2014. www.pathway.org.uk/wp-content/uploads/2014/11/nmuh-summary-2.pdf (accessed 10 June 2021).
- mpath . Manchester’s Homeless Health Inclusion Pathway. A Review of the First 6 Months of the Pilot Service 2013. www.pathway.org.uk/wp-content/uploads/2013/05/MPAT-6-month-service-review.pdf (accessed 10 June 2021).
- Trident Reach . Homeless Patient Pathway 2013. www.healthylondon.org/sites/default/files/45.%20Homeless%20Patient%20Pathway%2C%20Sandwell%20and%20West_0.pdf (accessed 10 June 2021).
- Lowson K, Hex N. Evaluating Bradford Respite and Integrated Support Service, Bevan Pathway and the Street Medicine Team. York: University of York; 2014.
- Danahay A. Homeless hospital discharge programme: improving service delivery and reducing A&E readmission among homeless people in Coventry and Warwickshire. Commissioning 2014;1:52-6.
- Thames Reach . Learning Briefing: The Croydon Hospital Discharge Project 2016.
- Thames Reach . The Croydon Hospital Discharge Report Project Briefing (April 2016–January 2017) 2017.
- Brighter Futures . Brighter Futures and Staffordshire &Amp; Stoke on Trent Partnership Trust Hospital Discharge Pilot 2014. www.brighter-futures.org.uk/images/uploads/Hospital_discharge_pilot_report.pdf (accessed September 2017).
- Tamworth Borough Council and South East Staffordshire and Seisdon Peninsular Clinical Commissioning Group . Hospital to Home Project: 6 Month Project Review 2014.
- Trinity Winchester . Making a Real Impact. Changing Lives, Trinity Winchester Annual Review 2014–15 2015. http://trinitywinchester.org.uk/wp-content/uploads/2014/12/Trinity-Annual-Review-2015-web.pdf (accessed 1 January 2018).
- Shelter and Coastline Housing . Cornwall Homeless Patient Discharge Service Evaluation Report 2016.
- Aitchison H. Changing Lives Homeless Hospital Prevention Service, Second Year Progress Report (April 2016–March 2017) 2017.
- Copeman I, Edwards M, Porteus J. Home From Hospital. How Housing Services are Relieving Pressure on the NHS. London: Housing Learning and Information Network & National Housing Federation; 2017.
- Ubido J, Holmes L, Scott-Samuel A. Homelessness in Liverpool City Region. A Health Needs Assessment 2014. http://info.wirral.nhs.uk/document_uploads/Needs-Assessments/Homelessness%20HNA%20Final%20Report.pdf (accessed 1 January 2018).
- Homeless Link . The Unhealthy State of Homelessness. Health Audit Results 2014 2014. www.homeless.org.uk/sites/default/files/site-attachments/The%20unhealthy%20state%20of%20homelessness%20FINAL.pdf (accessed 10 June 2021).
- McCormick B, White J. Hospital care and costs for homeless people. J Clin Med 2016;6:506-10. https://doi.org/10.7861/clinmedicine.16-6-506.
- Bank of England . Inflation Calculator n.d. www.bankofengland.co.uk/monetary-policy/inflation/inflation-calculator (accessed 8 June 2021).
- Ministry of Housing, Communities and Local Government . Rough Sleeping Statistics Autumn England (Housing Statistical Release) 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/781567/Rough_Sleeping_Statistics_2018_release.pdf (accessed 10 June 2021).
- National Institute for Health and Care Excellence . Intermediate Care Including Reablement n.d. www.nice.org.uk/guidance/ng74 (accessed 10 September 2019).
- Beresford B, Mayhew E, Duarte A, Faria R, Weatherby H, Mann R, et al. Outcomes of reablement and their measurement: findings form an evaluation of English reablement services. Health Soc Care Community 2019;27:1438-50. https://doi.org/10.1111/hsc.12814.
- Polsky D, Glick H. Costing and cost analysis in randomized controlled trials: caveat emptor. PharmacoEconomics 2009;27:179-88. https://doi.org/10.2165/00019053-200927030-00001.
- NHS Benchmarking . National Audit of Intermediate Care: Summary Report 2015 2015. https://s3.eu-west-2.amazonaws.com/nhsbn-static/NAIC%20(Providers)/2018/NAIC%202018%20England%20-%20infographic%20-%20brochure%20v3.pdf (accessed 10 September 2019).
- NHS Benchmarking . National Audit of Intermediate Care: Summary Report 2017 2017. https://s3.eu-west-2.amazonaws.com/nhsbn-static/NAIC%20(Providers)/2017/NAIC%20England%20Summary%20Report%20-%20upload%202.pdf (accessed 10 September 2019).
- NHS Benchmarking . National Audit of Intermediate Care: Highlights 2018 2018. https://static1.squarespace.com/static/58d8d0ffe4fcb5ad94cde63e/t/58f08efae3df28353c5563f3/1492160300426/naic-report-2015.pdf (accessed 10 September 2019).
- Department of Health and Social Care . Care and Support Statutory Guidance 2021. www.gov.uk/government/publications/care-act-statutory-guidance/care-and-support-statutory-guidance (accessed 10 October 2019).
- Cornes M, Aldridge R, Tinelli M, Whiteford M, Hewett N, Clark M, et al. Transforming Out-of-Hospital Care for Patients who are Homeless. Support Tool & Briefing Notes: complementing the High Impact Change Model for Transfers Between Hospital and Home. London: King’s College London; 2019.
- Tinelli M. Applying Discreet Choice Experiments in Social Care Research 2016. http://eprints.lse.ac.uk/73723/1/Tinelli_Applying%20discrete%20social%20experiments%20in%20social%20care%20research_published_2016%20LSERO.pdf (accessed 10 June 2021).
- Biederman DJ, Gamble J, Wilson S, Douglas C, Feigal J. Health care utilization following a homeless medical respite pilot program. Public Health Nurs 2019;36:296-302. https://doi.org/10.1111/phn.12589.
- Gazey A, Vallesi S, Cumming C, Wood L. Royal Perth Hospital Homeless Team. A Report on the First 18 Months of Operation 2018. https://doi.org/10.13140/RG.2.2.26289.68960.
- Gazey A, Vallesi S, Martin K, Cumming C, Wood L. The cottage: providing medical respite care in a home-like environment for people experiencing homelessness. Hous Care Support 2019;22:4-64. https://doi.org/10.1108/HCS-08-2018-0020.
- Lamanna D, Stergiopoulos V, Durbin J, O’Campo P, Poremski D, Tepper J. Promoting continuity of care for homeless adults with unmet health needs: the role of brief interventions. Health Soc Care Community 2018;26:56-64. https://doi.org/10.1111/hsc.12461.
- Park B, Beckman E, Glatz C, Pisansky A, Song J. A place to heal: a qualitative focus group study of respite care preferences among individuals experiencing homelessness. J Soc Distress Homeless 2017;26:104-15. https://doi.org/10.1080/10530789.2017.1341462.
- Stafford A, Wood L. Tackling health disparities for people who are homeless. Int J Environ Res Public Health 2017;14. https://doi.org/10.3390/ijerph14121535.
- Stergiopoulos V, Gozdzik A, Nisenbaum R, Durbin J, Hwang S, O’Campo P, et al. Bridging hospital and community care for homeless adults with mental health needs: outcomes of a brief interdisciplinary intervention. Can J Psychiatry 2018;63:774-84. https://doi.org/10.1177/0706743718772539.
- Buccieri K, Oudshoorn, A, Frederick T. Hospital discharge planning for Canadians experiencing homelessness. Hous Care Support 2019;22:4-14. https://doi.org/10.1108/HCS-07-2018-0015.
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health 2006;96:1278-81. https://doi.org/10.2105/AJPH.2005.067850.
- Doran KM, Ragins KT, Gross CP, Zerger S. Medical respite programs for homeless patients: a systematic review. J Health Care Poor Undeserved 2013;24:499-524. https://doi.org/10.1353/hpu.2013.0053.
- Dorney-Smith S, Thomson E, Hewett N, Burridge S, Khan Z. Homeless medical respite service provision in the UK. Hous Care Support 2019:22-53. https://doi.org/10.1108/HCS-08-2018-0021.
- Forchuk C, MacClure S, Van Beers M, Smith C, Csiernik R, Hoch J, et al. Developing and testing an intervention to prevent homelessness among individuals discharged from psychiatric wards to shelters and ‘no fixed address’. J Psychiatr Ment Health Nurs 2008;15:569-75. https://doi.org/10.1111/j.1365-2850.2008.01266.x.
- Grech E, Raeburn T. Experiences of hospitalised homeless adults and their health care providers in OECD nations: a literature review. Collegian 2019;26:204-11. https://doi.org/10.1016/j.colegn.2018.04.004.
- Gundlapalli A, Hanks M, Stevens SM, Geroso AM, Viavant CR, McCall Y, et al. It takes a village: a multidisciplinary model for the acute illness aftercare of individuals experiencing homelessness. J Health Care Poor Underserved 2005;16:257-72. https://doi.org/10.1353/hpu.2005.0033.
- Lamb V, Joels C. Improving access to health care for homeless people. Nurs Stand 2014;29:45-51. https://doi.org/10.7748/ns.29.6.45.e9140.
- Murphy P, Cope R. Evaluation of Phase 2 of the Early Discharge Project of the ‘ASSIST’ Team at Mansfield District Council. Nottingham: Nottingham University; 2018.
- Pathway . A Needs Assessment for Homeless Medical Respite Provision in North Central London 2019.
- Pedersen M, Bring C, Andersen O, Petersen J, Jarden M. Homeless people’s experiences of medical respite care following acute hospitalisation in Denmark. Health Soc Care Community 2018;26:538-46. https://doi.org/10.1111/hsc.12550.
- Read C. Supporting homeless and vulnerably housed patients: Royal Brisbane and Women’s Hospital service model. Parity 2017;30:122-3.
- Rae B, Rees S. The perception of homeless people regarding their healthcare needs and experiences of receiving health care. J Adv Nurs 2015;71:2096-107. https://doi.org/10.1111/jan.12675.
- Redman Z. Hastings Homeless Service: Conquest Hospital Partnership Development Pilot Project. Hastings: St John Ambulance; 2010.
- Shelter D, Shepard D. Medical Respite for people experiencing homelessness: financial impacts with alternative levels of Medicaid coverage. J Health Care Poor Undeserved 2018;2:801-13. https://doi.org/10.1353/hpu.2018.0059.
- Wadhera RK, Choi E, Shen C, Yeh RW, Joynt Maddox KE. Trends, causes, and outcomes of hospitalizations for homeless individuals: a retrospective cohort study. Med Care 2019;57:21-7. https://doi.org/10.1097/MLR.0000000000001015.
- Office for National Statistics . Deaths of Homeless People in England and Wales: 2013 to 2017 2018. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsofhomelesspeopleinenglandandwales/2013to2017 (accessed 10 June 2021).
Appendix 1 Included studies (n = 69) and their use in the review
| Study | Data collection | Type | Number of participants | PT1 | PT2 | PT3 | Notes (e.g. significantly refines or surfaces new programme theory) |
|---|---|---|---|---|---|---|---|
| Conceptually rich | |||||||
|
Herman et al. 85 (USA) Tomita and Herman57 (USA) |
RCT | CL | 150 | ✓ | ✓ | ✓ | New PT4: health, housing and social care professionals proactively manage continuity |
| Medcalf and Russell30 (UK) | Review of homeless health initiatives | CL | N/A | ✓ | Note on PT3: conceptualises IC integration within broader homeless health pathways | ||
| Whiteford and Simpson52 (UK) | Exploratory case analysis | CL | 18 | ✓ | Refine PT3: knot-working identified as useful theoretical concept for understanding process of integration | ||
| Thick | |||||||
| Bauer et al.41 (USA) | Retrospective study | MR | 860 | ✓ | ✓ | Refines PT1: draws attention to need for women-only spaces | |
| Biederman et al.141 (USA) | Quantitative descriptive pre-/post-programme evaluation | MR | 29 | ✓ | Notes on PT2: provides evidence of the way in which exposure and engagement with a medical respite facility for homeless people facilitates access to community-based forms of support, which, in turn, lead to reduced hospital admissions and fewer inpatient days | ||
| Canham et al.47 (Canada) | Scoping review plus consultation cafe | All | 23 | ✓ | ✓ | Notes on PT1 and PT3: highlights particular – and pervasive – gaps in care co-ordination. These gaps are seen to present challenges to quality of care, co-ordination of care and aftercare for homeless patients | |
| Charles et al.54 (UK) | External evaluation | HL | 104 | ✓ | ✓ | ||
| Doran et al.62 (USA) | Systematic review | MR | 13 (articles) | See notes | ✓ | Note on PT2: only one scheme listed access to physiotherapy | |
| Dorney-Smith56 (UK) | Economic evaluation | CL | 34 | ✓ | ✓ |
Refines PT1: work is needed to establish engagement before consultation Refines PT3: advocacy is key where no agency wants to take responsibility |
|
|
Dorney-Smith and Hewett45 (UK) Dorney-Smith et al. 66 (UK) |
Feasibility study | MR | 53 | ✓ | See notes | ✓ |
Note on PT2: highlights long-term care needs often not being met Refine PT1: highlights potential of psychologically informed environments |
| Dorney-Smith et al.50 (UK) | Project report | CL | N/A | ✓ | See notes | ✓ | Note on PT2: a recent development within Pathway teams is to include access to occupational therapy |
| Drury51 (USA) | Participant observation | HL | 60 | ✓ | ✓ | Refines PT3: advocacy is key where no agency wants to take responsibility | |
| Gazey et al.142 (Australia) | Technical report | CL | 634 (patients) | ✓ | ✓ | Refines PT3 by demonstrating the need for specialist in-reach services to work in collaboration with community-based health, housing and social care, so as to ensure timely transfer of care, better patient outcomes and more effective clinical/professional practice | |
| Gazey et al.143 (Australia) | Qualitative interviews plus administrative data | MR | ✓ | ✓ | Notes on PT1 and PT3: suggests that medical respite facilities for homeless people represent a safe and nurturing environment in which to recuperate. Medical respite also contributes to reductions in unplanned inpatient days in the 12 months post support | ||
| Gillespie48 (UK) | Project report | HL | N/A | ✓ | ✓ | ||
| Glennerster and Sales38 (UK) | Narrative/autoethnographic account | CL/HW | ✓ | ✓ | ✓ | Notes on PT1, PT2 and PT3: provides a rich account of the processes leading to the re-establishment of a dedicated HHDS at a major acute hospital | |
| Hendry64 (UK) | Economic evaluation | MR | 34 | ✓ | ✓ | Refines PT1: work is needed to establish engagement before consultation with service users can take place | |
|
Hewett et al. 42 (UK) Halligan and Hewett55 (UK) |
Descriptive case study | CL | N/A | ✓ | See notes | ✓ |
Refine PT3: advocacy is key where no agency wants to take responsibility Note on PT2: highlights difficulties in engaging adult social care, potentially accounting for why reablement is overlooked |
| Hochron, and Brown53 (USA) | Exploratory case analysis | CL | N/A | ✓ | |||
|
Pathway and Faculty for Homeless and Inclusion Health77 Albanese et al. 44 (UK) |
External evaluation of HHDF programme | All | 52 | ✓ | See notes | ✓ | Note on PT2: highlights difficulties in engaging adult social care, potentially accounting for why reablement is overlooked |
| Housing Learning and Information Network29 (UK) | Three case studies | HL/CL | ✓ | ✓ | |||
| Lamanna et al.144 (Canada) | Qualitative study | CL | 52 | ✓ | ✓ | ✓ | Notes on PT1, PT2 and PT3: provides clear evidence of the importance of working in an integrated and person-centred fashion to overcome barriers to care comprehensiveness and continuity |
| Lane40 (UK) | Feasibility study and literature review | MR | ✓ | See notes | ✓ | Note on PT2 raises issues around accessibility to physical rehabilitation. | |
| Lewis69 (UK) | External evaluation | HL | 10 | ✓ | See notes | ✓ | Note on PT2: highlights difficulties in engaging adult social care, potentially accounting for why reablement is overlooked |
|
Lowson and Hex75 (UK) Lephard67 (UK) |
External economic evaluation and project report | CL/MR | ≥ 39 | ✓ | See notes | ✓ | Note on PT2: highlights how resettlement can encompasses aspects of reablement |
| O’Carroll et al.68 (Republic of Ireland) | Feasibility study | MR | N/A | ✓ | See notes | ✓ | Note PT2: notes that many hostels exclude people with mobility issues |
| Park et al.145 (USA) | Qualitative study | MR | 25 | ✓ | Notes on PT1: suggests that medical respite can decrease hospital length of stay and readmission rates; however, to be effective, service commissioners and service providers must give parity of esteem to four domains: physical, relational, facilitation and amenities | ||
| Parker-Radford37 (UK) | Policy review and survey | 184 | ✓ | ✓ | ✓ | Advocates transition of care approach | |
| Sadowski et al.60 (USA) | RCT | SW/MR | 407 | ✓ | See notes | ✓ | Note on PT2: records an improvement in physical functioning from baseline for both intervention and control groups |
| Stafford and Wood146 (Australia) | Mixed methods | CL/HL | 3 | ✓ | ✓ | ✓ | Notes on PT1, PT2 and PT3: provides a combination of data that would seem to suggest that integrated medical and social care coupled with a Housing First approach can led to better outcomes for homeless patients |
| Stergiopoulous et al.147 (Canada) | Mixed methods | MR | 223 | ✓ | Notes on PT3: suggests that the enrolment in a post-discharge interdisciplinary intervention can lead to improvements in the health of homeless and vulnerably housed patients | ||
| van Laere et al.63 (the Netherlands) | Statistical case study | MR | 629 | See notes | ✓ | Note PT2: notes that MR provides palliative care | |
| Whiteford and Simpson65 (UK) | Exploratory case analysis | CL | 18 | ✓ | See notes | ✓ | Note on PT2: describes lack of access to physical rehabilitation/reablement services |
| Thin | |||||||
| Buccieri et al.148 (Canada) | Mixed-methods survey | CL/SW | 660 | ✓ | Notes on PT3: identifies the existence of service gaps in the delivering of effective and co-ordinated care to patients affected by homelessness | ||
| Buchanan et al.149 (USA) | Cohort study | MR | 225 | See notes | Note PT3: skilled nursing not provided, highlights role of ‘volunteer health providers’ | ||
| Danahay118 (UK) | Project report | HL | N/A | ✓ | |||
| Doran et al.150 (USA) | Chart review | MR | 113 | ✓ | |||
| Doran et al.62 (USA) | Action research | MR | ✓ | ||||
| Dorney-Smith et al.151 (UK) | Literature review | MR | ✓ | ✓ | Notes on PT1: provides an overview of the development of specialist medical respite care for homeless people in the UK, with a particular argument being made for both the effectiveness and ethicality of post-discharge health and housing support | ||
| Forchuk et al.152 (Canada) | RCT | HL | 14 | See notes | Refine PT3: housing advocacy plus fast-track income support seen as main mechanism | ||
| Grech and Raeburn153 (Australia) | Literature review | CL | 10 (articles) | ✓ | Notes on PT2: highlights, albeit superficially, the role of nurses in empowering homeless patients to address homelessness and ill-health through the delivery of flexible, non-stigmatising nursing | ||
| Gundlapalli et al.154 (USA) | Descriptive case analysis | MR | N/A | o | Note PT1: describes eligibility criteria linked to a range of MR provision in one county; consulting with service users not mentioned | ||
| Hewett et al.78 (UK) | RCT | CL | 414 | Effectiveness and cost-effectiveness study | |||
| H3, Stockport, UK, 2014 (UK) | Project report | HL | N/A | ✓ | |||
| Khan et al.81 (UK) | Narrative review | CL | ✓ | ✓ | Notes on PT1 and PT3: argues for the utility of GP-led approach to the admission and discharge needs of patients who are homeless or at the risk of homelessness | ||
| Khan et al.39 (UK) | Narrative account | CL | ✓ | ✓ | Notes on PT1 and PT2: describes how the mental health support needs of homeless patients are managed by a multidisciplinary care team | ||
| Kertesz et al.59 (USA) | Retrospective cohort study | MR | 743 | ✓ | |||
| Lamb and Joels155 (UK) | Case study | CL | N/A | ✓ | ✓ | ||
| Murphy and Cope156 (UK) | Mixed methods (e.g. cost–benefit analysis and interviews/focus groups) | HW | 28 | ✓ | ✓ | ✓ | Notes on PT1, PT2 and PT3: provides clear evidence of the effectiveness and cost-effectiveness of the ASSIST hospital discharge scheme in Mansfield. Particular emphasis is given to the importance of co-ordinating health, housing and social care |
| Pathway157 (UK) | Needs assessment | MR | ✓ | Notes on PT1: documents on the need for intermediate care provision for people who are homeless in north-central London | |||
| Pedersen et al.158 (Denmark) | Case study | MR | 12 | ✓ | Notes on PT2: argues strongly for the role of medical respite for homeless people as a vehicle for self-actualisation and improved health and well-being | ||
| Podymow et al.84 (Canada) | Cohort study | MR | 140 | ✓ | Note on PT2: one of the few studies to list availability of physiotherapy on consultation | ||
| Read159 (Australia) | Project report | HL | N/A | ✓ | ✓ | Notes on PT1 and PT3: social work practice is underpinned by Housing First principles and collaborative engagement with clinician and community organisations, so as to ensure safe and timely discharge co-ordination | |
| Rae and Rees160 (UK) | Phenomenological | 14 | See notes | See notes | Makes case for IC, focusing on importance of engagement and need for improved co-ordination | ||
| Redman161 (UK) | Project report | CL | N/A | ✓ | See notes | ✓ | Note on PT2: highlights difficulties in meeting ‘physical needs’ |
|
Blackburn et al. 96 (UK) SERI Insight79 (UK) |
External evaluation | HL | Not given | ✓ | |||
| Shelter and Coastline Housing124 (UK) | Project report | HL | N/A | ✓ | ✓ | ||
| Shelter and Shepard162 (USA) | Economic evaluation | MR | N/A | ✓ | Notes on PT1: demonstrates the cost-effectiveness of medical respite for homeless patients by reducing length of hospital stay, subsequent emergency department visits and inpatient admissions in states with varying Medicaid coverage | ||
| Wade49 (UK) | External evaluation | HL | 8 | ✓ | ✓ | ||
| Wadhera et al.163 (USA) | Retrospective study of hospitalisation records | SW | ✓ | Notes on PT2: argues for the need to make better use of ambulatory services and specialist behaviour services to help reduce acute care use and improve the long-term health of homeless individuals | |||
| White82 (UK) | External economic evaluation | HL | N/A | Provides evidence on cost-effectiveness using HES data | |||
| Wood et al.80 (Australia) | Mixed methods (e.g. administrative data and case studies) | CL/HW | 5 | ✓ | ✓ | ✓ | Notes on PT1, PT2 and PT3: argues for the value of closer collaboration between primary and secondary care providers and Housing First models |
| Wyatt98 (UK) | Review | CL | 400 (patients) | ✓ | ✓ | Notes on PT2 and PT3: reaffirms the efficacy and cost-effectiveness of the Pathway model of homeless health care, although acknowledges the limits of its ability to ensure post-discharge/continuity of care | |
Appendix 2 Completed stakeholder interviews
| Staff | n |
|---|---|
| HHDS staff | |
| Scheme manager | 7 |
| Housing link worker | 7 |
| GP | 5 |
| Nurse | 4 |
| Occupational therapist | 1 |
| Peer navigator | 1 |
| Non-HHDS staff | |
| Health commissioner/senior manager | 10 |
| Patient flow/bed manager | 3 |
| Discharge liaison nurse | 2 |
| Emergency department consultant | 3 |
| Alcohol liaison worker | 1 |
| Public health manager | 2 |
| Consultant psychiatrist | 1 |
| Specialist homeless nurse | 4 |
| Social care commissioner | 2 |
| Social worker (safeguarding) | 5 |
| Occupational therapist | 1 |
| Independent mental health advocate | 1 |
| Housing/hostel manager | 9 |
| Housing/hostel worker | 8 |
Appendix 3 Topic guides
Appendix 4 Bradford Respite and Intermediate Care Support Service case study: discharge to assess
Needs (at point of discharge)
Jason (name has been changed) is aged 49 years and has had a 10-week hospital admission as a result of a seizure requiring intensive care and intubation. Jason was ‘self-neglecting’ prior to his admission. He could not return home because his rented property was in an unfit state and an eviction notice had been served. At the point of discharge, Jason’s needs were as follows.
Health
-
Had suffered a hypoxic brain injury. There is a query regarding his decision-making capacity (because of his age he does not meet the criteria for memory clinic assessment).
-
Has diabetes and is forgetful and unable to manage own medications, including insulin. He often refuses to eat. He is having frequent hypoglycaemic episodes and also some high blood glucose levels. He is unaware of the symptoms of hypoglycaemia and is unable to look after himself in this situation. This can be life-threatening.
-
He has a mild learning disability.
Co-existing mental health and substance misuse
-
Has a complex mental health history, including past episodes of psychosis. Hears voices episodically and these are usually telling him to harm himself.
-
Has a history of drug and alcohol misuse. There have been numerous occasions where he has had periods of being heavily intoxicated. This has then had a significant impact on his ability to self-care, including taking vital medication such as insulin. He has also been associated with antisocial behaviour and disturbances to other residents of accommodation services such as hostels.
Care and support needs
-
Safeguarding concerns. Neighbours were financially abusing Jason.
-
Self-neglect of personal care. Occasional urinary and bowel incontinence.
-
Cannot maintain a habitable home environment without support.
-
Has difficulties reading and writing and engaging in work, employment and education.
-
Is unable to use public transport (make use of community facilities, including GP access) because of being unable to read numbers and letters and has no sense of direction unless he is accompanied by staff.
Housing problem
-
Is homeless.
Outcomes
Care planning outcomes to be achieved through Bradford Respite and Intermediate Care Support Service stay
-
Improve self-management of diabetes (including medication).
-
Maintain personal hygiene/address self-neglect.
-
Make use of necessary facilities (e.g. attend hospital appointments).
-
Address co-existing mental health/substance misuse.
-
Develop family relationships (with children).
-
Maintain habitable home environment (including benefits and money management).
Multidisciplinary working co-ordinated through Bradford Respite and Intermediate Care Support Service
Pre discharge
-
Pathway nurse issues assessment notice to adult social care.
-
Initial Care Act 201489 and occupational therapy assessment carried out.
Weeks 1–6 post discharge
-
Ongoing day-to-day assessments by a Pathway nurse and Bradford Respite and Intermediate Care Support Service (BRICSS) staff plus a weekly review/ward round at BRICSS led by a Pathway GP.
-
Insulin administered and blood sugars monitored twice per day by district nurses.
-
BRICSS staff prompt Jason to take his other medication four times per day. BRICSS have organised for this to be put into a dosset box and for repeat prescriptions to be automatically ordered and delivered to scheme. Medication is kept locked in a medication safe to prevent accidental overdose.
-
Following discharge from hospital, Jason was provided with 6 weeks’ free reablement support (with care workers visiting the BRICSS facility twice per day).
-
BRICSS staff complement the reablement package by providing support with shopping, paying bills, attending appointments, medication, opening and reading post, and encouraging Jason to undertake activities and engage in community/social life.
Weeks 7+ (total length of stay at Bradford Respite and Intermediate Care Support Service = 8 months)
-
Reablement care workers struggle to work with Jason who continues to refuse care. Addressing self-neglect remains a challenge for staff.
-
Allocation of a community social worker and new Care Act 201489 assessment completed. Social worker considers extra care housing the most suitable option because of Jason’s care and support needs.
-
Reablement team withdraw/transition to private domiciliary care provider until a place in an extra care facility can be found. As these facilities are often restricted to those aged > 55 years, Jason effectively becomes delayed in BRICSS for > 6 months until a place can be sourced.
-
Before the move takes place, Jason suffers a stroke and is admitted to hospital.
-
On leaving hospital, he spends a short time in another intermediate care facility (because of his need for 24-hour nursing care) before moving in to an extra care flat with 24-hour care on site. Jason loves his new home and enjoys the company of the older people who live there. He does not mind being the youngest resident!
Appendix 5 ICD-10 codes used to define underlying causes of death due to alcohol, drugs or suicide
This appendix contains material reproduced with permission from ONS,164 which contains public sector information licensed under the Open Government Licence v3.0.
The codes used in this section are based on this recent ONS analysis. 164
ICD-10 codes
| Description | ICD-10 code97 |
|---|---|
| Intentional self-harm | X60–X84 |
| Injury/poisoning of undetermined intent | Y10–Y34 |
| Sequelae of intentional self-harm/event of undetermined intent | Y87.0/Y87.2 |
| Description | ICD-10 code |
|---|---|
| Mental and behavioural disorders due to drug use (excluding alcohol and tobacco) | F11–F16, F18–F19 |
| Accidental poisoning by drugs, medicaments and biological substances | X40–X44 |
| Intentional self-poisoning by drugs, medicaments and biological substances | X60–X64 |
| Assault by drugs, medicaments and biological substances | X85 |
| Poisoning by drugs, medicaments and biological substances, undetermined intent | Y10–Y14 |
| Description of condition | ICD-10 code |
|---|---|
| Alcohol-induced pseudo-Cushing’s syndrome | E24.4 |
| Mental and behavioural disorders due to use of alcohol | F10 |
| Degeneration of nervous system due to alcohol | G31.2 |
| Alcoholic polyneuropathy | G62.1 |
| Alcoholic myopathy | G72.1 |
| Alcoholic cardiomyopathy | I42.6 |
| Alcoholic gastritis | K29.2 |
| Alcoholic liver disease | K70 |
| Alcohol-induced acute pancreatitis | K85.2 |
| Alcohol induced chronic pancreatitis | K86.0 |
| Fetal induced alcohol syndrome (dysmorphic) | Q86.0 |
| Excess alcohol blood levels | R78.0 |
| Accidental poisoning by and exposure to alcohol | X45 |
| Intentional self-poisoning by and exposure to alcohol | X65 |
| Poisoning by and exposure to alcohol, undetermined intent | Y15 |
Appendix 6 ICD-10 codes used to classify underlying causes of death groups in Figure 7
This appendix contains material reproduced with permission from ONS,164 which contains public sector information licensed under the Open Government Licence v3.0.
The codes used in this section are based on this recent ONS analysis. 164
| ICD-10 code | ICD-10 subchapter grouping | ICD-10 subchapter97 |
|---|---|---|
| V01–X59 | Accidents | Accidents |
| X60–X84 | Suicides | Intentional self-harm |
| Y09–Y34 | Event of undetermined intent | |
| K70–K77 | Diseases of liver | Diseases of liver |
| I20–I25 | Ischaemic heart diseases | Ischaemic heart diseases |
| C00–C97 | Malignant neoplasms | Malignant neoplasms |
| J09–J18 | Influenza and pneumonia | Influenza and pneumonia |
| I30–I52 | Other forms of heart disease | Other forms of heart disease |
| R95–R99 | Unknown | Ill-defined and unknown causes of mortality |
| U50–U50 | Deaths from unknown and unspecified causes | |
| F10–F19 | Mental and behavioural disorders due to psychoactive substance use | Mental and behavioural disorders due to psychoactive substance use |
| J40–J47 | Chronic lower respiratory diseases | Chronic lower respiratory diseases |
Appendix 7 Questionnaire baseline (time point 1)
Appendix 8 Questionnaire follow-up (time point 2)
Appendix 9 Economic evaluation: significant protocol changes
The economic evaluation departed significantly from that outlined in the original protocol. In this section, we explain what necessitated this change.
Delays due to waiting for Health Research Authority approval
The economic literature review was not planned in the original protocol. However, this study, and many others, experienced significant delays at commencement due to the launch of the Health Research Authority and changes to the procedures for securing ethics approvals. It was agreed with NIHR that to make good use of this time we would undertake a review of the published economic evidence for the effectiveness and cost-effectiveness of the 52 HHDSs (and other schemes). As noted earlier, there was an extensive ‘grey literature’, comprising many local evaluations, some of which included economic evidence.
Enabling interrogation of an additional mechanism resource
In the original protocol, we set out to compare the effectiveness and cost-effectiveness of:
-
standard compared with specialist care
-
HHDSs that were clinically led (multidisciplinary) compared with those that were housing led (uniprofessional).
Having completed the main literature synthesis (some 6 months after the study began), we developed our original realist hypothesis to capture new evidence about the importance of HHDSs having direct access to ‘step-down’ intermediate care. To enable us to interrogate this revised theory, we introduced a further comparative element across the evaluation to establish the effectiveness and cost-effectiveness of:
-
HHDSs with access to ‘step-down’ care compared with those with no direct access to ‘step-down’ care.
Compensating for the lack of EQ-5D completions
In the original protocol, we planned to collect (unconsented) information on patients from 20 HHDSs and to link this to HES data. As described in Chapter 4, this data linkage worked well. Although only 17 HHDSs were recruited, the overall sample size was large enough to compensate for this. We used these data to feed into the economic evaluation, employing a single modelling technique, as planned in the original protocol. The findings from the economic analysis of linked HES data for 17 HHDSs were described in Chapter 5.
However, in addition to collecting the linked HES data from 17 HHDSs, we also planned more in-depth economic analysis in four of the HHDS case study sites recruited for the qualitative fieldwork. The plan was that staff in the HHDSs in these sites would complete a questionnaire (encompassing EQ-5D data) with every patient at the point of discharge from hospital (T1) and then again at the 3-month follow-up (T2) (copies of the T1 and T2 questionnaires are provided in Appendix 7). However, the HHDSs did not have the capacity to incorporate this research work as part of their routine monitoring (as we had anticipated), with the consequence that only one HHDS delivered sufficient questionnaires at T1 and T2. This left us significantly short of the target (n = 372) that was needed for statistical significance. To compensate for this, we introduced a new focus for economic study (part 3).
In part 3, we shifted the ‘lens’ or ‘evaluative gaze’ from scheme typology to the study of three ‘out-of-hospital’ care configurations. That is, moving beyond a binary comparative analysis (e.g. clinically led vs. housing led) to explore the interplay between different mechanism–resource combinations in different local (geographical) contexts, each with differential access to housing and services.
Configuration 1
A multidisciplinary ‘clinically led’ (homeless health-care team) scheme that offers patient in-reach and specialist discharge co-ordination, with no direct access to ‘step-down’ intermediate care. Here, support for the patient usually ends at the point of exit from the acute sector (hospital). Two examples of this configuration were considered, one situated in a city and one in a seaside resort in the south of England.
Data source
A research team member had recently completed a RCT of two homeless health-care teams, employing EQ-5D data at two time points. We were able to draw on these EQ-5D data, which conferred access to 206 T1 completions and 56 T2 completions (at 6 weeks post discharge).
Configuration 2
In this site, two HHDSs work together in an integrated way. The configuration studied here comprised a clinically led (homeless health-care) team that offered patient in-reach and discharge co-ordination. This site had access to a 14-bed residential facility that offered step-down intermediate care. The hospital-based homeless health-care team provided ‘clinical in-reach’ into the residential intermediate care facility, ensuring continuity of multidisciplinary support for patients. The HHDSs are based in an old industrial city in the north of England.
Data source
In this fieldwork site, we were able to meet the target for EQ-5D questionnaire completions. Here, we were able to access 64 completions at T1 and 54 at T2 (at 3 months post discharge).
Configuration 3
This site contained a single housing-led HHDS in which a small team of housing support workers visited the hospital to provide patient in-reach and discharge co-ordination. The housing workers then continued to support patients in the community (offering floating support) until longer-term services were in place and working well (i.e. community ‘step-down’ intermediate care). Although a uniprofessional scheme, it had access to a multidisciplinary clinically led homeless health-care team based at the hospital. The HHDS is based in an old industrial city in the Midlands.
Data source
This site worked with the research team in the pilot phase of the study and was collecting EQ-5Ds as part of its own routine monitoring and review procedures. From this site, we were able to access 84 completions at T1 and 84 at T2 (at 3 months post discharge).
In total, drawing on these different data sources, we were able to access a total of 354 EQ-5D completions at T1 and 248 at T2. This was sufficient to enable us to carry out a range of modelling techniques.
We acknowledge, however, that it was by chance (rather than purposeful selection) that the HHDSs conferring access to the EQ-5D data were such that they enabled the comparative study of three very different out-of-hospital care systems. On the one hand, by moving beyond binary comparisons (clinically led vs. housing led) to consider the interplay between multiple resource mechanisms in different contexts, this pragmatic approach afforded, what we believe to be, a more in-depth and nuanced interrogation of the realist hypothesis than was originally planned. On the other hand, there are limitations in making comparisons where the data source is not uniform across all sites and where (geographical) contexts are very different and cannot be controlled for.
More details of the protocol changes are presented in Appendix 10.
Appendix 10 Economic analysis plan for the study: original and revised analyses
| Economic analysis plan | Original plan | Main challenges | Revised plan | Source of data |
|---|---|---|---|---|
| Primary analyses using linked HES data | The original plan took a NHS perspective, with use of resources based on the linked HES data analysis and outcomes based on morbidity and mortality data. Service user outcomes of clinically- and housing-led HHDSs were to be compared, along with standard vs. specialist. Cost estimates were calculated using national NHS tariff data, and included length of hospital stay, emergency admissions, and fixed and variable costs estimates for each of the HHDS services | Delays in securing ethics approvals and data from NHS Digital |
Economic model 1 The revised model allowed for an estimate of the comparative cost-effectiveness of different types of HHDS vs. standard care (Hewett et al. 78). This model was based on aggregate estimates derived from HES data. It allowed us to compare the cost-effectiveness of different types of HHDS and introduced further comparisons to feed into the realist evaluation (i.e. HHDSs with and without step-down care). Evidence was sourced from 17 rather than 20 study sites. Measure of effectiveness is bed-days |
Plan was to use HES data, additional data used was from the literature review |
| Additional analyses using linked HES data | The original model included a NHS perspective and costs based on HES data, as for the cost-effectiveness model, but also uses outcomes based on QALY data (i.e. primary EQ-5D data collected through the field work in a subgroup of HHDS users at baseline and at the 3-month follow-up). Data from the two types of service were compared with each other and homeless controls from a wider London-based survey of 455 homeless individuals accessing F&T screening service for tuberculosis. QALY loss from morbidity and mortality averted are examined. Cost estimates were based on HES data. Outcome data (QALYs) are calculated from EQ-5D data. Cost and effectiveness estimates were calculated for a 1-year follow-up period after entering the study, with simulations to 20 years (costs discounted at 3.5% per annum). A sensitivity analysis was planned to examine uncertainties within the cost-effectiveness and utility model to examine the uncertainty within the parameters used | See above |
Economic model 2 The revised model allowed us to estimate the comparative cost–utility of different types of HHDS vs. standard care (Hewett et al. 78). Use of resource data for the intervention groups were extracted from HES data (aggregate estimates instead of individual homeless user analyses). Utility data were extracted from survey data collected from local sites The perspective adopted was NHS. Measure of effectiveness was gain in utility QALY. Time frame included 1- and 3-year sensitivity analysis |
Intervention groups Intervention groups were limited to the individual sites considered for the surveys for which we could access QALY data Use of resources For each group of interest, the analyses of the HES data provided annual aggregate estimates for the following variables: number of elective readmissions per homeless user and number of emergency readmissions per homeless user Utility data (QALYs) When data were collected from the case study sites, annual estimates were derived that analysed the project survey (configuration 2) or audit data (configuration 3). In case of the pathway sites, data were sourced from the literature (Hewett et al. 78) Control group Homeless users receiving standard care from Hewett et al. 78 |
| Additional analyses using data collected from case study sites | An additional cost–utility analysis was to be performed using costs and health outcome (consented) data collected from the four in-depth HHDS case study sites. This model had a NHS and also a wider public sector perspective (e.g. exploring costs for use of social care, prison, supported housing). The added value of this additional economic analysis was to estimate the cost–utility of HHDSs from a larger public sector perspective while incorporating contextual information from the realist evaluation into the economic evaluation | Questionnaires not completed/or insufficient T2 questionnaires in three out of four case study sites |
Economic model 3 An additional model considered a before-and-after analysis and allowed to measure the cost-effectiveness of discharge service delivery before and after the introduction of the intervention in the same study site(s). Observed differences in performance were assumed to be due to the intervention It was based on audit and survey data collected as part of this project. It allowed to compare the cost-effectiveness of a selection of sites and capture the larger public provider perspective for the two sites. Measure of utility was gain in QALY |
Groups were limited to configurations 2 and 3 as only two sites were able to provide data on the larger public provider perspective Data on use of resources (i.e. health care, mental health care, drug and alcohol treatment, housing, criminal justice, social care, social benefits and state pension) and utility (QALY) were sourced from local survey and audit data Service delivery costs were collected from the local sites |
List of abbreviations
- 24/7
- 24 hours a day, 7 days a week
- A&E
- accident and emergency
- BCF
- Better Care Fund
- BRICSS
- Bradford Respite and Intermediate Care Support Service
- CI
- confidence interval
- CTI
- critical time intervention
- D2A
- discharge to assess
- DHSC
- Department of Health and Social Care
- DToC
- delayed transfer of care
- EQ-5D
- EuroQol 5 Dimensions
- F&T
- Find & Treat
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- HHDF
- Homeless Hospital Discharge Fund
- HHDS
- homeless hospital discharge scheme
- HICM
- high-impact change model
- HR
- hazard ratio
- HRA
- Homeless Reduction Act 2017
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- ICER
- incremental cost-effectiveness ratio
- IMD
- Index of Multiple Deprivation
- IMD5
- Index of Multiple Deprivation quintile 5
- IQR
- interquartile range
- KPP
- key practice principle
- KPP1
- consultation with service users
- KPP2
- promoting reablement and resettlement
- KPP3
- integrated working between health, housing and social care
- KPP4
- continuity of care
- MDT
- multidisciplinary team
- MEAM
- Making Every Adult Matter
- MEH
- multiple exclusion homelessness
- MIR
- mechanism intervention resource
- MIR1
- protocols for early discharge planning/patient flow (high-impact change model 1 and 2)
- MIR2
- patient in-reach
- MIR2mdt
- patient in-reach (with clinical and housing advocacy/expertise combined)
- MIR2up
- patient in-reach (housing advocacy/expertise only)
- MIR3
- discharge co-ordination
- MIR3mdt
- discharge co-ordination (undertaken by multidisciplinary team)
- MIR3up
- discharge co-ordination (undertaken by uniprofessional team)
- MIR4
- step-down intermediate care
- MIR4hf
- community/home-based (floating support) step-down care
- MIR4res
- residential step down
- MIR5
- trusted assessment/direct referral rights
- MIR6
- strong leadership
- MIR7
- strengthening safeguarding
- NHSE&I
- NHS England and NHS Improvement
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- ONS
- Office for National Statistics
- OR
- odds ratio
- QALY
- quality-adjusted life-year
- RAMESES II
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards II
- RCT
- randomised controlled trial
- RICSS
- Respite and Intermediate Care Support Service
- SIHHC
- specialist integrated homeless health and care
- SMR
- standard mortality ratio
- T1
- time point 1
- T2
- time point 2
- WP
- work package
Notes
-
Piloting in preparation to economic modelling: Conf.3 case study
-
Economic model 1: project data and deterministic sensitivity analyses
-
Economic model 1: project data (probabilistic sensitivity analysis) – per cent of replicates in each quadrant
-
Economic model 1: project data (probabilistic sensitivity analysis) – bootstrap scatterplot and cost-effectiveness acceptability curve (control = standard care)
-
Economic model 2: project data and deterministic sensitivity analyses
-
Economic model 2: project data (probabilistic sensitivity analysis, control = standard care) – per cent of replicates in each quadrant
-
Economic model 2: project data (probabilistic sensitivity analysis) – bootstrap scatterplot and cost-effectiveness acceptability curve (control = standard care)
-
Economic model 3: sample, patient characteristics, use of resources, costs and health utility
-
Economic model 3: project local site data (before and after, probabilistic sensitivity analysis) – per cent of replicates in each quadrant
-
Economic model 3: project local site data (before and after, deterministic sensitivity analysis) and one-way sensitivity analyses
-
Economic model 3: project local site data (before and after, probabilistic sensitivity analysis) – bootstrap scatterplot and cost-effectiveness acceptability curve
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr09170).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
