Notes
Article history
The research reported here is the product of an HSDR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HSDR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HSDR journal.
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR132679. The contractual start date was in August 2020. The final report began editorial review in October 2021 and was accepted for publication in December 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Ramsay et al. This work was produced by Ramsay et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Ramsay et al.
Chapter 1 Background
Parts of this chapter have been adapted with permission from the evaluation protocol (Version 1.3). 1
Context and rationale for this evaluation
Optimising access to organised stroke care in the NHS in England
Stroke is a major cause of death and disability in the UK and internationally. 2 Evidence from urban settings suggests that ‘system optimisation’ of stroke services, whereby they are centralised into a small number of hyper-acute stroke units (HASUs), is linked with better care delivery and outcomes. 3–6 HASUs (which in future will be termed acute stroke centres, or comprehensive stroke centres if they deliver mechanical thrombectomy) offer rapid access to stroke specialist assessment and treatment, including intravenously administered ‘clot-busting’ therapies, if appropriate.
Such centralised services rely on effective collaboration between multiple stakeholders, including hospital stroke services and ambulance services, to ensure the appropriate conveyance of patients to a HASU. 7–9
In recent years, the NHS in England has sought to improve patient access to organised stroke care in several ways. The NHS Long Term Plan reinforces the role of networked stroke systems at a regional level to improve care delivery and clinical outcomes. 10 Integrated Stroke Delivery Networks (ISDNs) are made up of multiple health agencies, including ambulance trusts, and aim to ensure that NHS stroke services comply with 7-day quality standards for stroke care and National Clinical Guidelines for Stroke. In addition, there is support to scale up technologies that improve the quality of stroke services, such as the potential use of artificial intelligence to interpret computerised tomography (CT) and magnetic resonance imaging (MRI) scans and the implementation of telehealth. 10
Minimising unnecessary conveyance to specialist stroke units using telemedicine
Because of the limited specificity of screening tools for stroke [e.g. the Facial drooping, Arm weakness, Speech difficulties and Time (FAST) tool, or variations, which is used by most ambulance clinicians and has been heavily promoted in the national press], acute stroke services commonly manage large numbers of patients who, although suspected to be having a stroke (e.g. because they are ‘FAST positive’), turn out to have non-stroke conditions (so-called ‘mimics’). 11 Remote specialist stroke assessment via telemedicine has been found to support accurate triage of patients12 and has the potential to identify patients who do not need urgent treatment in a specialist unit. However, to date, the piloting and implementation of such technologies has been limited in England. Reported obstacles to adoption include technical issues (e.g. reliable video-call signal quality) and cultural barriers (e.g. ambulance clinicians’ concern regarding the benefits of potentially increasing on-scene time to seek specialist secondary care stroke expertise).
International evidence for ‘telestroke’ and mobile stroke units
Elsewhere, there has been movement towards the uptake of telemedicine in stroke care, particularly in the USA and Germany (see Chapter 3). 16 There is emerging evidence about telemedicine’s safety and cost-effectiveness,13,14 indicating that the uptake of telemedicine in stroke care can provide neurological expertise in real time effectively and within the tight time window necessary for hyper-acute stroke treatment. 12
However, from clinicians’ perspectives, there may be issues with the usability of new telestroke systems or mobile facilities that rely on visual cues. Reviews of the evidence on implementing telestroke describe several obstacles to and enablers of adoption. Major barriers include unfamiliarity with the technology and how it conflicts with cultural norms; technical issues with audio-visual quality; lack of staff confidence in systems; lack of information technology (IT) support; and poor communication between clinicians. 15,16 Reviews also note the potential impact of prehospital video triage on decision-making, for example through the addition of stroke specialist expertise. 15
A recent scoping review16 describes a small but growing evidence base on how remote technologies may support ambulance clinicians in triaging potential stroke patients, including the use of prehospital biomarkers and imaging and mobile telemedicine. The review16 reports no UK-based research on ambulance telemedicine systems to support remote assessment by stroke clinicians. However, the international research reported indicates that such systems are viewed positively by staff and can result in reduced time to care interventions, and that prehospital remote diagnosis can be as accurate as hospital-based diagnosis. 16 The review also noted relatively few data to suggest that such systems result in more appropriate conveyance of patients, or about their impact on outcomes such as patient safety. 16
Understanding implementation of digital innovations in health-care systems
There is increasing interest in how innovative digital technologies come to be adopted by and used in health-care systems and may shape clinical practices and workflows. For example, recent World Health Organization guidance17 suggests that digital health should be understood in terms of an ongoing process of development, whereby digital interventions evolve from early piloting and prototyping to digital maturity, requiring ‘real-time’ monitoring of both technical functionality and stability in addition to health outcomes.
NHS service context for the pilot services
As outlined above, there are many areas (including implementation, impact and experience) where knowledge is limited in relation to prehospital digital triage services.
In this evaluation, we studied two pilot schemes that introduced prehospital video triage for suspected stroke patients in North Central (NC) London and East Kent. These pilots were introduced in response to the COVID-19 pandemic. Below, we provide contextual information on these two areas and summarise briefly the local responses to COVID-19.
The NC London pilot took place in the North Central sector of London, covering a population of 1.2 million people. 18 The area is served by a single HASU, hosted by University College London Hospitals NHS Foundation Trust (UCLH) and the London Ambulance Service NHS Trust (LAS). This sector is part of the wider London ‘hub-and-spoke’ acute stroke service model, implemented in 2010, whereby all suspected stroke patients are eligible for initial treatment in a HASU (hub) and, if required, ongoing acute care in stroke units (SUs), which act as ‘spokes’, offering specialist acute rehabilitation services nearer home. 8 In response to the pandemic, the UCLH HASU was relocated from the main UCLH hospital site [where it had been co-located with an emergency department (ED)] to the nearby National Hospital for Neurology and Neurosurgery (NHNN), a dedicated neurological and neurosurgical hospital (which did not have an ED).
The East Kent pilot covered the area served by East Kent Hospitals University NHS Foundation Trust (EKHUFT) and the South East Coast Ambulance Service NHS Trust (SECAmb). EKHUFT serves a population of just under 700,000 people. Pre pandemic, this area was served by two stroke units, at the William Harvey Hospital and Queen Elizabeth the Queen Mother Hospital (QEQM). However, in response to the pandemic, hyper-acute stroke services were moved from these sites to a single routinely-admitting service at Kent and Canterbury Hospital (Canterbury, UK). As with the revised model in UCLH, this reorganisation moved the HASUs away from co-location with the trust’s ED and to a new location that did not have immediate ED support.
Pre-hospital video triage services implemented in North Central London and East Kent
In 2020, NHS services in NC London and East Kent introduced prehospital video triage services in response to the developing COVID-19 pandemic. These were ‘on-scene’ digitally supported systems that let ambulance clinicians contact acute stroke clinicians for remote clinical assessment using digital communication platforms [i.e. FaceTime (Apple Inc. Cupertino, CA, USA)] using communications devices [i.e. smartphones and iPads (Apple Inc.)]. The aim of the video assessments was to establish whether or not a patient was suitable for conveyance to a HASU or if they should be on a different care pathway, thus minimising unnecessary conveyance or delays. The anticipated benefits of this system were to:
-
Support appropriate referrals to HASUs or other pathways [e.g. local ED, General Practitioner (GP) or transient ischaemic attack (TIA) clinic] during the COVID-19 pandemic. This would contribute to streamlining of care for different patient groups and protect vulnerable older patients from unnecessary conveyance to hospital, where there was a risk of exposure to COVID-19.
-
Ensure the timeliness of treatment for optimal patient outcomes, in accordance with best practice guidelines.
-
Help services to run as efficiently as possible (e.g. by providing decision support to ambulance clinicians and reducing the number of unstable non-stroke patients being brought to a HASU without co-located ED support).
Table 1 provides an overview of the key events in the development and early implementation of prehospital video triage in NC London and East Kent.
| NC London | East Kent |
|---|---|
| Pre-pandemic context | |
|
2017/18: stroke lead and LAS leads had agreed in principle that a model could be useful but nothing further was done across teams 2019: UCLH Stroke Team obtained funding for a fellow to take this forward |
2010: first discussions of telemedicine using video cameras in ambulances 2013: received grant from NHS Improvement Agency for regional prehospital tele-medicine pilot. This was not conducted owing to safety concerns about video equipment in the ambulance November 2018: ‘proof of concept’ pilot introduced in Thanet area. Ran 14 nights, small number of cases |
| Implementation | |
| March 2020: NHSE London CAG set up to act as the governance group to scrutinise and approve any changes to London care pathways | March–April 2020: COVID-19 pandemic reinvigorates discussion of the pilot in the context of the reconfiguration of local stroke services |
|
March 2020: in response to pandemic, UCLH HASU moved to NHNN, at Queen Square. Move discussed with East Kent to confirm strategy UCLH connect with LAS, to discuss clinical safety and options given move to Queen Square, as well as strains on ambulance crews – could unnecessary journeys be avoided? |
1 April 2020: Invicta HASU (Kent and Canterbury Hospital) opened in response to pandemic, receiving all stroke patients in East Kent area. William Harvey and QEQM stroke services no longer to receive stroke patients |
|
17 May 2020: pilot goes live, with consultants providing assessments 24/7 All suspected strokes eligible for prehospital video triage service |
6 April 2020: pilot goes live, consultant-led, with neurology trainees providing assessments out-of-hours. Patients where there is uncertainty about stroke diagnosis are eligible for remote triage |
|
May–August 2020: training of LAS ambulance clinicians commenced in the northern stations and NC London and progressed south Ongoing collaboration between UCLH and LAS to develop triage algorithm and process, and training video |
Summer 2020: implementation issues with stroke consultants – could not provide weekend or night cover to respond to ambulance clinicians |
| June 2020: clinical fellow commences work to support pilot. The role includes training doctors and conducting events at other hospital EDs to raise awareness about the model | July 2020: junior doctors provide weekend cover, with stroke nurses fielding calls |
| August 2020: service shifted to Specialist Registrar-led 24/7 service with consultant support |
September 2020: video calls go directly to junior doctors and stroke consultants (not nurses) Eight consultants take it in turns to cover Monday to Friday, 09.00–17.00. Junior doctors cover out of hours |
| September 2020: following approval from NC London CAG prehospital video triage rolled out fully across NC London and agreed as standard of care | October 2020: all suspected stroke patients eligible for prehospital video triage |
| Wider roll-out | |
| London-wide roll-out remains under consideration, pending pan-London discussions and evidence of the safety and effectiveness of the pilot services | January 2021: pan-Kent and Medway roll-out commenced |
The evaluation of these services represented an important opportunity to build an understanding of the acceptability and safety of prehospital video triage for suspected stroke patients. Key examples of potential learning were establishing the acceptability of the services to their users (i.e. ambulance and stroke clinicians); factors influencing usability (e.g. signal quality and environment); the impact of the service on patient destination, travel times and the delivery of clinical interventions; and factors influencing the implementation of these services (e.g. governance and training).
In 2020 and 2021, the authors engaged with ambulance and stroke services across the UK, establishing that, at the time, no equivalent prehospital video triage services were active. Since our evaluation commenced in July 2020, two other areas of Kent have launched their own prehospital video triage services and a number of other areas of the NHS in England have indicated that they are interested in potentially implementing a service of this kind.
Aim and evaluation questions
We aimed to conduct a rapid, mixed-methods service evaluation19,20 of how prehospital triage to support appropriate HASU attendance was facilitated by new service models using digital technologies that enable remote clinical input. Our service evaluation questions (EQs), agreed with clinician and patient stakeholders, were the following:
-
EQ1 – what evidence exists on prehospital video triage for suspected stroke patients, in terms of implementation, usability, safety and outcomes?
-
EQ2 – are the prehospital video triage services piloted in NC London and East Kent acceptable to their users (stroke clinicians and ambulance clinicians)?
-
EQ3 – are the services effective in terms of usability and image/sound quality?
-
EQ4 – do the services support the appropriate, safe and timely conveyance and treatment of suspected stroke patients?
-
EQ5 – which factors influence the uptake and impact of these services?
-
EQ6 – which aspects of these services should be retained post COVID-19 and which adaptations (if any) are required to support their implementation?
Overview of the project
This service evaluation was conducted through the Rapid Service Evaluation Team (RSET) programme. RSET, funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research (HSDR) programme, is a 5-year research programme that aims to rapidly evaluate health and care service innovations to produce timely findings of national relevance and immediate use to decision-makers. The topic of this evaluation was identified through discussions between RSET staff and leaders of the local pilots. A proposal to evaluate an earlier East Kent pilot of prehospital video triage was explored by RSET in 2018/19, but initial scoping indicated that it was at insufficient scale for study. Further discussions commenced in spring 2020 with clinical representatives of stroke and ambulance services who were leading the NC London and East Kent pilots. Working with these clinical leaders, RSET staff developed an evaluation protocol which underwent local review by RSET colleagues outside the core team, review by a panel of two patient experts and independent peer review by Professor Henry Potts [University College London (UCL)] and Professor Helen Snooks (Swansea University). The final version of the revised protocol (v1.3) was approved by the NIHR HSDR programme in August 2021.
Our protocol underwent a number of revisions over the course of the service evaluation. The key revision in terms of evaluation design was the addition in March 2021 of a staff survey conducted with ambulance clinicians. The other revisions related to extending the evaluation timeline. Although the project was initially scheduled to conclude on 31 March 2021, it was extended to 30 June 2021 to permit the completion of qualitative data collection (which had been severely disrupted by the winter wave of the COVID-19 pandemic); it was then extended to 30 September to permit write-up and the incorporation of clinician and patient feedback in report drafts.
Structure of the report
-
Chapter 1, Background presents the research and policy context for prehospital video triage for stroke and an overview of the pilot video triage services that we evaluated.
-
Chapter 2, Evaluation methods presents the methods employed in our evaluation, including an overview of our approach to patient and public involvement (PPI).
-
Chapters 3–6 present the findings of our evaluation, in terms of:
-
Chapter 3 – literature review of the evidence on prehospital triage for suspected stroke patients (addressing EQ 1)
-
Chapter 4 – qualitative analysis of staff perceptions of the implementation, impact, safety and further development of these services (EQs 2, 3, 5, 6)
-
Chapter 5 – survey of ambulance clinician experiences of these services (EQs 2, 3, 6)
-
Chapter 6 – quantitative analysis of the impact of prehospital video triage on safety and effectiveness of patient conveyance and delivery of stroke clinical interventions (EQ 4).
-
-
Chapter 7, Discussion and conclusions presents our findings linked to our evaluation questions and discusses the implications of our findings for health services and future research.
-
Appendix 1 includes supplementary information on our empirical findings.
Chapter 2 Evaluation methods
Overview
Parts of this chapter have been adapted with permission from the evaluation protocol (version 1.3). 1
This chapter describes our service evaluation, in terms of its mixed-methods, formative design and the qualitative and quantitative methods employed. We present the data sampled and analysed and report how we approached collecting and requesting these data. We then describe our overall approaches to analysing these data. Where appropriate, greater methodological detail is provided in the relevant chapters. Finally, we provide details of research governance approvals and an overview of our approach to PPI.
Further details of methods may be found in the relevant sections in Chapters 3, 4, 5, and 6.
Design
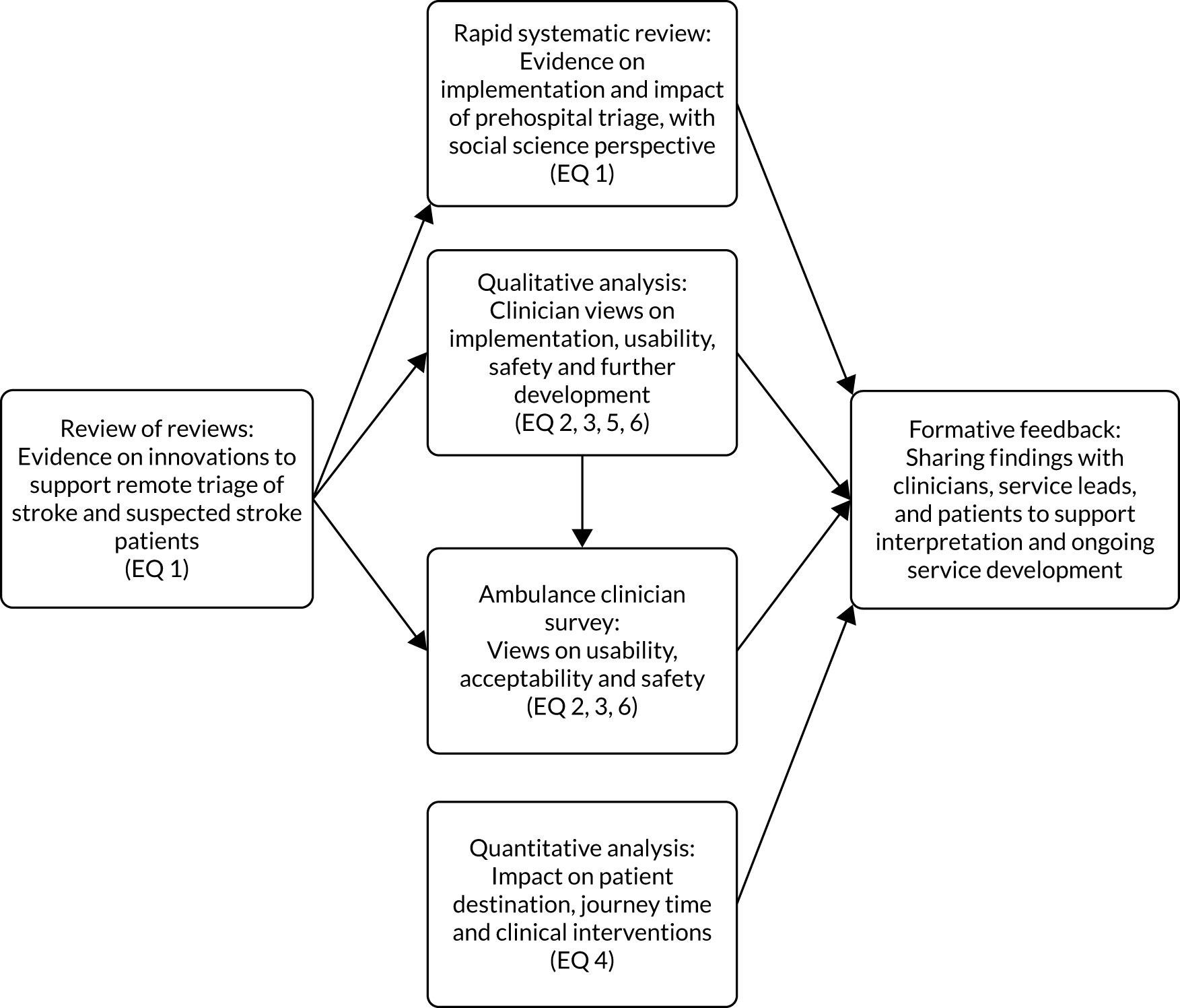
This was a rapid, formative, mixed-methods service evaluation, reflecting recent recommendations for such approaches. 20,21 The overall evaluation design is summarised in Figure 1 and contained the following workstreams:
-
Workstream 1 – a rapid review of the literature (incorporating a scoping review of reviews and systematic review) to establish the existing evidence on remote triage of stroke and suspected stroke patients and to inform the development of other evaluation components (e.g. interview topic guides and analysis approach).
-
Workstream 2 – a qualitative analysis of clinician views on the implementation, usability, safety, and further development of the prehospital video triage services implemented in NC London and East Kent. This analysis was guided by a conceptual framework describing factors that influence implementation of digital innovations. 17 Note that given the rapid nature of this project, it was designed as a service evaluation; one implication of this was that we were unable to seek Health Research Authority (HRA) ethical permission to interview patients and carers about their experiences of prehospital video triage.
-
Workstream 3 – a survey of ambulance clinicians to learn more about their experiences of prehospital video triage, in terms of usability, safety and implementation.
-
Workstream 4 – a quantitative analysis of ambulance data on patient destination and journey times, and national stroke audit data on delivery of key clinical interventions. This analysis helped assess whether or not prehospital video triage was associated with any changes in effectiveness or safety of services, for example in terms of timely patient conveyance to the hospital/HASU or the delivery of key clinical interventions.
-
Formative feedback – this evaluation was co-designed with ambulance clinicians, stroke clinicians, and patient collaborators. Throughout the project we engaged regularly with our collaborators, for example sharing progress and developing findings, in part to strengthen our interpretation and focus of the evaluation, but also to ensure that local collaborators could draw on our findings to support service development.
FIGURE 1.
Overview of evaluation design.
Rapid reviews of the literature
We undertook a rapid literature review22,23 of evidence on digital and telemedicine/telestroke interventions used to triage potential stroke patients at the prehospital stage. The review was conducted in two phases, and its objectives were to:
-
define relevant concepts and key terms, and summarise what is currently known about digital interventions used in the triage of potential stroke patients (through a rapid appraisal of existing reviews and primary studies)
-
identify any conceptual frameworks or theories used to understand the implementation of digital interventions in this context
-
identify any gaps in research or evaluation knowledge
-
determine how our evaluation and future research might address these gaps.
Further details of this analysis can be found in Chapter 3.
Phase 1: review of existing reviews
First, we identified existing systematic, scoping, or rapid reviews on this topic published in the last five years using key words (e.g. telemedicine, telestroke, stroke, ambulance/paramedic, triage and review). The search was limited to peer-reviewed outputs published in English. We searched a range of databases and resources [e.g. The Cochrane Library, Association for Computing Machinery (ACM) Digital Library, Web of Science, Epistemonikos and PROSPERO]. This search was conducted in June–July 2020.
The findings from this phase are summarised in Chapter 3 and were shared with clinical collaborators in an umbrella ‘review of reviews’ paper. In addition, this review informed the design of the rapid systematic review conducted in phase 2 (thus helping to avoid any unnecessary duplication of existing reviews) and helped shape interview topic guides for the qualitative workstream.
Phase 2: rapid systematic review
The rapid systematic review built on the results of phase 1 and followed recent guidance and recommendations on conducting systematic reviews. 24 We aimed to identify conceptual frameworks and social science perspectives on the implementation of digital and communication technologies used for remote assessment and triage and assisting two-way communication between ambulance and stroke clinicians. In addition, we aimed to identify any knowledge and evaluation gaps, such as whether or not any economic impact analyses had been conducted about similar service innovations. We searched for an inclusive range of empirical studies [including randomised controlled trials (RCTs), feasibility studies, pilots, and service evaluations], using several relevant databases [including MEDLINE, Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), EMBASE and Web of Science]. Our search terms were developed in collaboration with clinical co-authors and a librarian who specialises in literature searches. Search results were screened for duplicates and relevance against inclusion/exclusion criteria at title and abstract stages. The papers included in the review were then assessed for quality using the Mixed Methods Appraisal Tool (MMAT)25 and relevant Critical Appraisals Skills Programme (CASP)26 tools.
Data extracted from the included papers were then summarised in a table detailing the study type and methodology, population, outcomes and findings, and then written up using narrative synthesis27 and reported following Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) recommendations. 24 Data extraction was completed in July–August 2021.
Further details of this review can be found in Chapter 3 and the PROSPERO protocol for this review [URL: www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021254209 (accessed 15 July 2022)].
Qualitative analyses: insights on usability, acceptability and safety
We used qualitative methods (i.e. interviews, non-participant observations of meetings and documentary analysis) to analyse the implementation of the pilot video triage systems, including the analysis of users’ perspectives on usability, acceptability, cognitive load and patient safety (e.g. potential delays in care and appropriateness of patient conveyance). Further details of this analysis can be found in Chapter 4.
We aimed to:
-
provide rapid evidence about the perceived impact and effectiveness of the triage systems being piloted, for example evidence on any immediate issues with implementation (including technical issues that have been addressed and modified, or could be in future) and users’ early and later impressions
-
capture learning about the service innovation and staff experiences of the remote assessment process.
First, we conducted remote interviews (using telephone or video calls) with consultant stroke physicians and ambulance clinicians in NC London and East Kent (n = 27). Interviews were guided by semistructured topic guides. This focused on experiences of using the service, including acceptability, usability (e.g. reported cognitive load), patient safety and training, and implications for future developments. We interviewed a mix of ambulance clinicians and hospital-based stroke consultant physicians involved in the pilots, including service leads (interview topic guides are presented in Report Supplementary Material 1).
Second, we conducted non-participant observations of activities (n = 9) related to the prehospital video triage services (e.g. local governance meetings and training events). The focus of the observations was (1) to understand local development of the pilot services, for instance in terms of which stakeholders were involved in decision-making; and (2) to analyse oversight, governance, and management of the pilots, for example how service leaders responded to technical or safety issues and planned further development of the services.
Third, we analysed relevant documents (n = 23) (e.g. meeting minutes, service pathways and protocols, and training materials) to provide ongoing insights about the triage systems as they developed. For example, documents were an important source of detail on when important decisions were made (for our timelines) and how services were progressing (e.g. in terms of the numbers of patients processed and the numbers of safety issues).
Recruitment/consent
Participation in qualitative aspects of this service evaluation took place only with fully informed consent. Potential interviewees were sent an information sheet and had at least 48 hours to consider participation and ask any questions about the project. Interviews were conducted and recorded only with informed consent. Interviewees were free to withdraw at any time, up to and including during the interview. Participant details were anonymised for analysis and write-up.
For observations, meeting members were sent an information sheet in advance, alongside other meeting papers. The chairperson announced the evaluation team’s presence at the beginning of the meeting and confirmed that no names would be used in the final report. Although the situation did not arise, the evaluation team agreed that they would ‘dial out’ if issues were being discussed that those present at the meeting preferred not to be observed.
Data collection and analysis
Non-participant observations were conducted between August 2020 and May 2021. Interviews were conducted between October 2020 and May 2021.
Interviews were recorded using digital audio recorders and transcribed by a professional transcription service. Observations were recorded as handwritten or electronic field notes. Interview transcripts and observation field notes were imported into NVivo version 12.0.0.71 (QSR International, Warrington, UK) and analysed using framework analysis.
Emerging data (including from interviews, observations and documents) were captured using Rapid Assessment Procedures (RAP) sheets (see Report Supplementary Material 2). 21 These sheets supported the iterative nature of the evaluation by facilitating parallel data collection and analysis. The RAP sheet was structured to reflect the interview and observation guides and was refined over the course of the evaluation in response to the data. Team members involved in data collection met weekly to discuss progress and ensure consistency in data collection and analysis. The RAP sheets were updated regularly over the course of the study to facilitate quick and ongoing analysis and feedback with stakeholders. 28
Ambulance clinicians survey: usability, safety and experiences
A survey for ambulance clinicians was co-designed with ambulance collaborators and distributed to clinicians at LAS and SECAmb. The survey explored such issues as pilot feasibility, technical stability, usability and perceptions of safety. For each survey item, a chi-squared test of independence was performed to compare the patterns of responses from ambulance clinicians from NC London with those from East Kent. Further details of this analysis can be found in Chapter 5.
Quantitative analyses: impact on safety and delivery of services
We analysed the pilot triage systems quantitatively in terms of (1) patient conveyance by ambulance and (2) delivery of key clinical interventions within stroke services. Given the data available, our analysis of safety related to whether or not stroke patients were being conveyed to a HASU within recommended time thresholds and our analysis of service delivery related to the timely delivery of clinical interventions. Further details of these analyses can be found in Chapter 6.
Ambulance conveyance data
We analysed routinely collected ambulance journey data for NC London and East Kent, as provided by our partner organisations. These patient-level data were anonymised. They covered journey destination (e.g. which HASY or non-HASU the patient was conveyed to) and the timings of different stages of the ambulance job cycle (i.e. time from first call to dispatch, time from dispatch to scene, time at scene and time from scene to hospital). As outlined in Chapter 6, these data covered only the areas in which prehospital video triage was implemented during the period April–September 2020, that is, the months following the initial implementation of prehospital video triage. Therefore, a limitation of these data was that we had no comparators (either geographic or historic) against which to analyse performance.
National stroke clinical audit data
We analysed national stroke clinical audit data via the Sentinel Stroke National Audit Programme (SSNAP). We accessed publicly available data, aggregated at a team-level. We collected data covering teams in the participating areas (NC London and East Kent), and compared with figures for the rest of England (RoE) as a cross-sectional control. SSNAP aggregate data are reported quarterly and, at the time of analysis, only two quarters of post-implementation data were available: July–September 2020 and October–December 2020. Therefore, to permit understanding of whether performance changed over time, we analysed July–December quarterly data for 2018 and 2019 as historical controls.
Quantitative analysis
These data were analysed to assess the following outcomes.
Patient destination
We analysed local ambulance data descriptively to assess the proportion of all patients undergoing prehospital video triage who were conveyed to local HASUs or other services. We also analysed SSNAP data on the proportion of stroke patients being treated by HASUs and non-routinely-admitting teams. According to SSNAP, routinely-admitting teams ‘directly admit the majority of their stroke patients’ (in the context of this evaluation, these teams would be local HASUs); non-routinely admitting teams ‘provide acute care but [. . .] are typically transferred the majority of their stroke patients from other teams’ (e.g. specialist acute stroke rehabilitation units – in the context of the London system, these units are called SUs). 29 In addition, to analyse whether or not the proportions of patients admitted to HASUs and non-routinely-admitting teams changed over time in NC London and East Kent relative to RoE, we also analysed the SSNAP data using a between-region difference-in-differences (DiD) regression analysis (see Difference-in-differences regression).
Stroke patient conveyance
We analysed local ambulance data on time from departing scene to arrival at hospital. We analysed the proportion of patients whose conveyance from scene to hospital reflected recommended journey times as set out in national recommendations. 30 We also analysed SSNAP data on time from symptom onset to arrival at hospital and the HASU. We analysed descriptively median times from stroke symptom onset to arrival at hospital and the HASU. This was in order to analyse whether or not the additional time devoted to prehospital video triage in NC London and East Kent resulted in patients reaching stroke services more slowly than they did before the introduction of prehospital triage, and whether or not patterns of change were equivalent to those observed in RoE during the same time period.
Numbers of stroke patients treated by stroke teams
We analysed whether the number of patients treated in these services changed during the period in which prehospital video triage was introduced, including the number of patients admitted by routinely admitting and non-routinely admitting teams. We analysed these data descriptively over time to identify any changes following the introduction of (although not necessarily as a result of) prehospital video triage.
Delivery of key clinical interventions
We analysed delivery of ‘front door’ clinical interventions, including time from arrival at hospital to brain scan, swallow assessment, and thrombolysis, where appropriate, to analyse whether stroke care delivery in HASUs had changed (for better or worse) following the introduction of prehospital video triage (e.g. whether or not stroke teams were better prepared for patients thanks to the remote assessment). We analysed these data using a controlled DiD design (explained under Difference-in-differences regression). 31 This let us assess whether or not changes in delivery of clinical interventions following the introduction of prehospital video triage in NC London and East Kent reflected wider patterns of change observed in RoE (as noted in Chapter 1, several other important changes to stroke service organisation took place in the same period, which may also have contributed to any changes observed).
Difference-in-differences regression
To understand changes in patient destination and delivery of clinical interventions, we analysed SSNAP data using between-region DiD regression analyses. Our approach was consistent with the Medical Research Council guidelines for using natural experiments to evaluate population health interventions32 and previous research investigating regional service changes. 8,33,34 Our DiD regression analyses compared changes in delivery of stroke clinical interventions over time in NC London and East Kent with the change over time in RoE. Equation 1 shows how outcome variables in the DiD estimator were measured at the trust level (i.e. NC London and East Kent) in each time period (before and after the implementation of prehospital video triage) and were regressed against covariates, with particular interest in the interaction showing the impact of the area following the introduction of the prehospital video triage:
where Y is each outcome of interest (i.e. whether the patient was transferred to a routinely-admitting or non-routinely admitting unit; and whether or not stroke patients received clinical interventions, including timely admission to a stroke unit, brain scan, thrombolysis and assessment by specialists). i indicates the particular trust, t indicates the period, A indicates the area (1 = NC London or East Kent, 0 = RoE), P is the period (before or after) and R is an indicator variable taking the value of 1 if ambulance services in trust i in area A in period t have introduced the prehospital triage (1 = yes, 0 otherwise). X is a vector representing patients’ characteristics [sex proportions of admitted patients, number of comorbidities, median National Institutes of Health Stroke Scale (NIHSS) score, type of infarction, and arrival by ambulance]. α indicates coefficients to be estimated, and ε is an error term. The analysis was carried out at a team level focusing on HASUs and we included binary indicators for the three quarters (time fixed effects).
Data requests
We requested local data via participating NHS organisations. We submitted a request for team-level aggregate SSNAP audit data, but the data were put in the public domain in sufficient time to permit our analyses.
Synthesis of findings
We drew together findings from the literature review and the quantitative, qualitative and survey analyses to provide insights on the relationships between the pilot triage systems’ design, implementation, usability and safety.
For each pilot area (NC London and East Kent), we drew on qualitative interviews and survey data to identify context-specific factors that helped explain patterns observed in the quantitative data. We also analysed across the two areas, for example to identify common lessons for implementation. Finally, we organised our findings around themes emerging from the rapid literature review to identify how they contribute to the existing literature.
Information governance/data storage
All evaluation data were collected and stored for analysis in compliance with the UCL Records Retention Schedule and data protection regulations. 35,36
Qualitative data
Stakeholder interviews were conducted only with fully informed consent. All interviews were recorded using encrypted digital audio recorders. They were transcribed by a professional transcription service, and data were transferred to and from this service via a secure File Transfer Protocol (FTP) system. Interview transcripts were pseudo-anonymised and stored on a secure drive to which only the evaluation team had access, located on the password-protected UCL system. All non-participant observations were recorded as handwritten or electronic fieldnotes and stored in the same secure UCL system.
Quantitative data
Ambulance and SSNAP data were stored as Microsoft Excel® (version 2204, Microsoft Corporation, Redmond, WA, USA) spreadsheets on a secure drive to which only the evaluation team had access, located in the password-protected UCL system.
Survey
Survey data were collected via the secure UCL Opinio platform [version 7.18, UCL Information Services Division, London, UK; URL: www.ucl.ac.uk/isd/services/learning-teaching/e-learning-services-for-staff/e-learning-core-tools/opinio (accessed 27 July 2021)]. 37 Survey results were extracted from the software platform and stored on a secure drive to which only the evaluation team had access, located in the password-protected UCL system.
Patient and public involvement
We involved patients and the public in this evaluation in the following ways. During project scoping and development, we engaged with Raj Mehta and Fola Tayo, who are patient representatives on the wider RSET programme. We held several online meetings to discuss the pilot services and proposed evaluation. Both patient representatives conducted an expert review of our developing evaluation protocol and approved the version submitted to the funder. Over the course of the evaluation, we recruited a stroke survivor (Simon Payne) based in the East Kent area, via the local evaluation team. Our project update meetings (discussed in Dissemination and sharing learning) included both our clinical and our patient collaborators. Our patient representatives were invited to attend all of these meetings and, in the event that they could not attend, we arranged separate meetings to cover the same issues. While writing up this report, we shared developing drafts with all our collaborators – including our patient representatives – for their contributions; in addition, we worked with our patient representatives to ensure that the Plain English summary was clear and accessible. In line with the RSET PPI strategy, our patient representatives were paid for all these activities to support development and write-up of this project.
Dissemination and sharing learning
This was a rapid formative evaluation, where we sought to share our findings as they developed. As discussed above, our approach to analysis (facilitated through regular team and subgroup meetings) allowed us to develop lessons in parallel with data collection. Because of this it was possible for us to share developing lessons at several points over the course of the evaluation. In particular we worked to share progress and lessons with our clinical collaborators, who were leading the prehospital video triage services in NC London and East Kent, and our patient representatives, who had played an important role in developing our evaluation protocol. Key examples of sharing learning included:
-
written updates on the progress of evaluation and interim results, shared with all collaborators via e-mail (December 2020, May 2021 and June 2021)
-
virtual meetings to share the progress of evaluation and interim findings with all collaborators, and a small number of non-collaborators (i.e. representatives of participating stroke and ambulance services) (January 2021 and June 2021)
-
verbal updates on the progress of evaluation and emerging headline findings at local governance meetings (four in NC London, three in East Kent)
-
catch-up meetings with local collaborators to discuss the progress of evaluation in NC London and East Kent separately (approximately every 6 weeks).
As outlined in our protocol, we will share findings from this evaluation more widely via an online stakeholder workshop following the completion of our final report. We will present our findings to wider academic and professional audiences through publication in high-impact research journals (supported by accessible summaries of findings) and present findings at relevant academic and professional conferences.
Chapter 3 Literature review
Overview
What was already known?
-
There is a well-established evidence base on telestroke networks (which link stroke centres to rural or community hospitals using telemedicine) and mobile stroke units (MSUs) (highly equipped vehicles with CT scanners, laboratory equipment and telemedicine equipment, as well as stroke staff).
-
Less is known about prehospital ‘mobile’ stroke telemedicine, which connects emergency clinicians/paramedics to hospital-based stroke clinicians.
What this chapter adds
-
We conducted a systematic review into ‘mobile telestroke’ or ‘in-ambulance telemedicine’, a process that enables communication between ambulance crews and hospital-based doctors in cases of suspected stroke.
-
Mobile telemedicine systems in stroke care have been piloted and found to be technically feasible. These systems enable two-way audio and video communication between emergency personnel and stroke clinicians, provided that there is good network coverage [e.g. fourth-generation broadband cellular network technology (4G)]. Indeed, reliable two-way audio and video communication is deemed especially important for remote clinical assessment of stroke.
-
Several factors support successful implementation. These include staff training, compatibility with existing systems, clear communication, reliable network coverage, co-design with staff, high-performing microphones and a stable audio connection (especially to avoid clinicians having to repeat information or misunderstandings).
-
Barriers to implementation include background noise, poor usability and weak or inconsistent network coverage.
-
Few process evaluations or RCTs have been conducted on in-ambulance telemedicine for stroke compared with studies of telestroke networks and MSUs, especially with regard to the impact on destinations (including patients remaining at home in the case of mimics) and treatment times.
-
Little is known about cost-effectiveness, patient privacy and patient experience in mobile telestroke in prehospital settings.
Background
This chapter presents a two-phase review of published literature about digital and communication systems that enable stroke specialists to assess potential stroke patients remotely while patients are attended to by emergency services personnel. The focus was on the prehospital pathway, prior to patient admission to a general hospital or specialist stroke centre.
‘Telestroke’ has been defined as ‘the process by which electronic, visual and audio communications (including the telephone) are used to provide diagnostic and consultation support to practitioners at distant sites, assist in or directly deliver medical care to patients at distant sites, and enhance the skills and knowledge of distant medical care providers’. 38 By comparison, MSUs are highly equipped ambulances, which usually incorporate a ‘CT scanner, point-of-care laboratory and a device for teleconsultation with the hospital neuroradiologist’,39 along with highly trained staff. MSUs therefore represent a high-tech (and often high-cost) solution, one deemed particularly useful where access to hyper-acute services is limited. However, although much research has focused on MSUs or hospital-based telestroke networks that leverage telemedicine to provide remote neurological cover in rural areas, there is growing recognition of innovations within the prehospital care pathway and ambulances that provide an alternative to MSUs and may improve time to treatment over standard care. The literature, therefore, suggests that prehospital telemedicine may be one way to reduce travel times as it can (1) connect emergency medical services (EMS) clinicians to hospital-based stroke teams and (2) alert hospitals to an incoming patient and direct patients to the most appropriate point of care (e.g. a specialist stroke team). ‘Prehospital telestroke’/‘mobile telemedicine’ is therefore identified as a promising, novel development to support clinical examination in the field by EMS clinicians, with remote support provided from hospital-based staff and stroke experts. 16,39–41 This topic was the focus of a two-phase literature review, which we outline below. Phase 1 of the review was used to inform the design of research materials in our rapid evaluation.
Methods
We sought to understand the nature of the published evidence base on digital interventions used in the triage of potential stroke patients. Owing to a rapid evaluation timeframe, the literature search was split into two distinct phases: one conducted early in the project and one that could report towards the end once we had empirical findings.
Phase 1: umbrella ‘review of reviews’ – a rapid, exploratory search
To guide this rapid evaluation and quickly identify key terms and relevant topics, a rapid search for existing reviews was undertaken from June–July 2020. According to the Joanna Briggs Institute (JBI) Manual for Evidence Synthesis, umbrella review permits consideration of multiple wide-ranging aspects of a given issue. 42 We deliberately broadened the search to quickly identify existing systematic, scoping, narrative or rapid reviews on the use of innovative technologies to support remote triage of stroke and suspected stroke patients by ambulance and paramedic crews on site.
The aims of the rapid umbrella review were to:
-
identify relevant reviews on the topic (systematic and other types, e.g. scoping reviews)
-
identify conceptual frameworks or theories used to understand the implementation of digital interventions in this context
-
identify gaps in research or evaluation knowledge
-
determine how our rapid evaluation and future research might address these gaps (and avoid duplication).
The following headings were used to guide the search:
-
population – patients suspected of stroke, ‘stroke mimic’ or TIA
-
phenomenon of interest – paramedic and ambulance crews (i.e. EMS clinicians) using technologies to triage and treat stroke (or suspected stroke) patients at the prehospital stage
-
context – ambulance clinicians triaging patients in ambulances or in patients’ homes or care settings (i.e. non-hospital or hyper-acute clinical settings)
-
outcomes – for example efficiency, safety and outcomes compared with usual practice and stroke management pathways.
Inclusion criteria
Using a select number of key word strings, the following databases were accessed and searched from 1 to 4 July 2020: Cochrane Library, ACM Digital Library, Web of Science Core Collection, Epistemonikos and PROSPERO. Searches were by title/abstract and topic. The search was limited to outputs published in English between 2010 and 2020 (Table 2). One member of the team (JL) executed the search. The following parameters were used to identify existing reviews:
-
eligible for inclusion – systematic/rapid/scoping/literature reviews (including published protocols) and evidence syntheses on the topic
-
not eligible for inclusion – pilot and feasibility studies, primary research studies, reviews on stroke rehabilitation, reviews of patient behaviour or person-generated health data, diagnostic test reviews (e.g. FAST) and reviews of thrombolysis (without reference to telestroke or ambulance/paramedics).
| Search terms | Database | Searched by (e.g. title/abstract/topic) | Records found within parameters (n) |
|---|---|---|---|
|
‘stroke’ AND ‘ambulance’ OR ‘triage OR ‘digital’ ‘telestroke’ |
Epistemonikos | Title/abstract | 22 |
|
‘stroke’ AND ‘ambulance’ OR ‘triage OR ‘digital’ ‘telestroke’ |
PROSPERO | Title/abstract | 14 |
|
‘stroke’ AND ‘ambulance’ OR ‘paramedic’ ‘stroke’ AND ‘triage’ |
ACM Digital Library | Title/abstract | 0 |
| ‘stroke’ AND ‘ambulance’ AND ‘review’ | Web of Science Core Collection | Title and topic, refined by type (review) | 6 |
| Total eligible for full-text review (once duplicates removed) | 31 | ||
| Eligible for inclusion (met search and inclusion parameters) | 15 |
As this was a rapid ‘review of reviews’, we excluded empirical studies that could later be identified in phase 2, as well as reviews on less relevant topics such as stroke rehabilitation and patient behaviour change to prevent stroke. Key terms to drive the search were ‘stroke’, ‘ambulance’, ‘paramedic’, ‘triage’, ‘digital’, ‘telestroke’ and ‘review’.
Sharing lessons from umbrella review
The findings from this phase were summarised in a ‘review of reviews’ paper that was circulated to the wider team and clinical collaborators for comment. Feedback was provided through team communications and meetings with the evaluation team and clinical collaborators on the study. The findings were used to inform the design of research materials (e.g. topic guides) and the design of the literature search in phase 2.
Phase 2: systematic review
In addition to placing this evaluation and its conclusions in the context of a wider literature, it was decided to conduct a systematic review for four reasons. First, the most recent and relevant review identified in phase 1, Lumley et al. ,16 focused on a variety of prehospital interventions in the stroke pathway (e.g. biomarkers), whereas we were interested primarily in a very specific intervention covered in that scoping review: ‘mobile telemedicine’. This meant that we needed to focus specifically on technologies that enabled communication between ambulance clinicians and stroke clinicians and centres. Second, following discussion of the phase 1 search results and new guiding questions with an information specialist at UCL, the published search strategy used in Lumley et al. 16 was discussed and it was noted that there were some medical subject index headings (MeSH) and key words that had not been included but which would be important in the context of this particular evaluation (e.g. we added terms such as ‘bidirectional communication’, ‘iPad’, ‘clinical informatics’ and ‘HASU’). In addition, Lumley et al. 16 had framed part of their review on process outcomes (e.g. ‘detect’ and ‘diagnosis’) and the information specialist advised that this may have missed some literature of relevance to this review. We therefore wished to employ a fine-grained search strategy focused on mobile telemedicine, the prehospital emergency context and communication between health professionals, requiring a modified design. We also wanted to identify any social science or human–computer interaction literature associated with this topic to provide an interdisciplinary focus, requiring new terms to be added (see Report Supplementary Material 3 for the detailed MEDLINE search we developed). Third, the phase 1 search revealed a relatively large literature on MSUs. Because we were interested in evidence about potentially lower-cost digital technologies that support two-way communication in the field, we required a different strategy from that for other reviews, and to go beyond the literature on MSUs. Finally, as the two pilots evaluated here were implemented in the context of COVID-19, it was important to capture any more recent studies that had been implemented and written up during the last year (2020–21), although it was noted that, owing to publication time delays, more recent empirical studies and reports might be small in number.
The final systematic review search strategy involved close working between a researcher (JL) and a UCL information specialist (Debora Marletta, UCL librarian) and extensive trialling of key terms and Boolean operators across multiple databases. The review was guided by PRISMA 2020 recommendations24 to ensure that the approach taken was both transparent and explicit, and a final protocol was published on PROSPERO following team discussion and review. 43 Collaboration between the researcher and the information specialist was essential to maximise the sensitivity of the search and to sense-check returns, helping ensure that the final records included insights about the implementation of digital and communication technologies within prehospital acute stroke pathways. The information specialist checked all final search strategies that had been refined until consensus was reached. In addition, a ‘test list’ of potentially eligible papers was used drawing on phase 1 in order that JL could confirm that the final search strategy was picking up relevant papers.
We developed a specific title and research questions for the systematic review in autumn 2020, which were discussed and agreed on as a team. The phase 2 review aimed to identify implementation factors associated with digital and communication technologies that could impact on health-care service quality and health outcomes, and any conceptual frameworks and social science perspectives that could help explain these relationships. The search strategy was framed around the participants, intervention, and health context and setting, but not limited by outcomes in order to capture the wider literature. Instead, we were interested in a variety of outcomes of interest, such as implementation factors, safety and security of digital and communication systems, usability, user experience, acceptability (staff and patients), cost-effectiveness, overall clinical effectiveness, and ambulance destination outcomes (e.g. faster treatment times, but also issues of usability, staff experience, enhanced communication and safety). We also wanted to confirm any evaluation gaps, such as whether or not economic analyses had been conducted.
The final review title was ‘The implementation of digital interventions and communication technologies in emergency care pathways to support the remote assessment and triage of patients suspected of stroke: a systematic review’.
The review questions were as follows:
-
Which human, technological, and usability factors are associated with the implementation of digital and communication technologies in ambulance settings (e.g. mobile telemedicine) that enable two-way communication between paramedics and hospital physicians in the care of stroke and potential stroke patients?
-
Which system and local contextual factors are important for the implementation of these kind of technologies in the care of stroke and potential stroke patients?
-
What service-level outcomes (e.g. clinical, financial and resource impacts) are associated with the use of these kind of technologies in the care of stroke and potential stroke patients?
-
What evidence exists about the safety and security of these kind of technologies and systems when used at the prehospital admission stage? Relatedly, are any adverse effects reported in the literature?
-
What (if any) conceptual frameworks have been used to understand the implementation of these kind of technologies and systems?
Database search strategies and specific operators were developed and piloted by a researcher and information specialist during the first part of 2021. Six databases were used for the systematic review:
-
the Cochrane Systematic Reviews Database
-
The University of York Centre for Reviews and Dissemination [covering the Database of Abstracts of Reviews of Effects (DARE), the NHS Economic Evaluation Database (NHS EED) and Health Technology Assessment (HTA) database]
-
MEDLINE (via Ovid)
-
CINAHL
-
EMBASE (1980–present)
-
Web of Science Core Collection.
The final searches were run across the databases from July to August 2021. Searches were saved so that the main reviewer received automatic alerts about new records. Report Supplementary Material 3 provides details of the search strategies executed across a selection of these databases.
Eligibility criteria
The review was limited to including articles published in English from 2010 onwards. The population eligible for inclusion comprised patients of any age suspected of having acute stroke, ‘stroke mimic’ or TIA and assessed remotely by paramedics/ambulance clinicians and stroke doctors using digital and communication technologies. The exclusion criteria for the review were as follows:
-
diagnostic instruments used by ambulance clinicians/paramedics only (e.g. FAST+ test) without the input of a hospital-based stroke doctor
-
processes and interventions not facilitated by digital and communication technologies
-
patients treated in MSUs equipped with specialist diagnostic equipment (e.g. scanners)
-
patients treated for stroke, ‘stroke mimic’ or TIA in hospital accident and emergency (A&E), EDs or clinical settings only without prior triage by ambulance or EMS
-
commentaries/editorials, grey literature, conference proceedings or opinion pieces
-
non-peer-reviewed studies.
There was no restriction based on study type. RCTs, feasibility studies, pilots, service evaluations, implementation studies (qualitative), health economic studies, and so on, were all deemed relevant.
Data extraction and screening
A total of 4577 records were downloaded from the databases into EndNote [version 20, Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA], which was used to identify duplicate entries (Figure 2). The process used for deduplication was recommended by the information specialist. 45 Duplicates were automatically identified by EndNote and manually checked by one researcher (JL) using this method. Records were next uploaded to the software Rayyan.ai for screening of titles and abstracts, a package that also facilitates team collaboration. To ensure reliability in the screening of titles and abstracts, a screening tool was developed (see Report Supplementary Material 4) and piloted on the first 200 records, and the results were discussed with a second reviewer (AIGR). This led to a validated final screening protocol for searching all titles and abstracts, which was led by one reviewer (JL). If any papers were identified in which eligibility was unclear, the title and abstract were discussed by two reviewers and an agreement was reached. This process was important for screening a large number of papers that addressed telestroke ‘hub-and-spoke’ configurations, but excluded discussion about emergency care pathways and ambulance/paramedic teams.
FIGURE 2.
Systematic review: PRISMA flow diagram. Based on PRISMA 2020 – flow diagram for systematic reviews which include searches of databases and registers only). 44 CRD, Cochrane Systematic Reviews Database; WOS, Web of Science Core Collection.

One reviewer (JL) identified the 288 records for review against the inclusion criteria and validated screening tool. This resulted in the identification of around 60 relevant reports for inclusion. A second reviewer (AIGR) was involved in screening this final group, using Rayyan.ai. 46 Any reports where it was uncertain whether or not they should be included were discussed until consensus was reached. For example, a number of studies incorporated a prenotification telephone call from emergency clinicians to stroke clinicians or units; these were excluded following discussion because they did not involve the explicitly use of video or two-way communication to support remote triage and diagnosis. Two reviewers (JL and AIGR) approved the final group of 47 included reports.
Data extraction
The full texts were reviewed, and the thematic findings are summarised below (for detailed study characteristics, see Appendix 1, Table 11). We extracted and recorded information in Microsoft Excel about (1) study details (e.g. title, year, publication, authors, study type, the intervention, setting and population); (2) details of the study design and methods (e.g. trial, economic evaluation, feasibility, pilot or observational study); (3) results, including any implementation factors associated with implementation of the intervention; and (4) researcher observations regarding relevance.
Findings
Phase 1 identified 15 relevant reviews within the search parameters (Table 3). The findings are summarised as follows:
-
Types of research –
-
The most recent review on the topic,16 having identified published protocols and studies up until June 2019, was highly relevant to our review.
-
-
Defining terms –
-
The terms ‘telestroke’ and ‘telemedicine’, when used in reference to prehospital stroke care/emergency diagnosis, identify pilots, primary research, RCTs and protocols on the topic.
-
There are varied service innovations in prehospital stroke care, including diagnostic algorithms for dispatch teams, MSUs and remote deployment of treatment on scene, and new handover protocols and templates.
-
MSUs are highly equipped specialised ambulances, originally piloted in Germany, and form part of a prehospital stroke management response. They are a high-tech solution and potentially useful where access to hyper-acute services is limited. They require specialist teams and training. Stroke specialists may be onboard or accessed via telemedicine facilities within MSUs.
-
-
Aims/focus of reviews –
-
Reviews focused strongly on the impact of prehospital triage using communication technologies on time taken to reach hospital, time taken to deliver clinical treatment, mortality and clinical outcomes.
-
In contrast, there was little focus on the impact of prehospital triage using communication technologies on the following key outcomes: appropriate patient destination, ambulance and stroke clinicians’ shared decision-making, patient safety, patient satisfaction, cost-effectiveness, and communication between stroke and ambulance clinicians.
-
However, we recognised that such detail may be present in the underpinning primary studies.
-
-
Quality of reviews –
-
Mixed quality: systematic and systematic scoping reviews identified alongside descriptive reviews based on a limited number of databases.
-
A lack of social science concepts and theory is apparent in the literature. There is more focus on treatment and journey times and outcomes (e.g. there is a lack of insight reported from science and technology studies, although concepts may have been applied in the original studies). One exception by French et al. 15 applied normalisation process theory to telestroke.
-
-
4G may be more effective for mobile telemedicine in stroke care (e.g. in supporting video communication).
-
The telemedicine and telestroke literatures discuss general barriers to implementation, for example technical issues such as poor transmission or network speeds (especially for earlier systems), low usability, level of compatibility with systems already in use and the costs of equipping ‘high-tech’ ambulances; however, there was a lack of cost information about mobile telemedicine compared with MSUs overall.
| Review focus | Authors | Examples of outcomes and themes discussed (drawing on underpinning studies) |
|---|---|---|
| Prehospital stroke pathway and management, including new technologies/telemedicine | aAude Bert, 201347 | ‘Onset-to-door’ times, ‘onset-to-needle’ times, implementation factors (e.g. technical issues) |
| aLumley et al. 202016 | ||
| aRogers et al. 201748 | ||
| MSUs | Calderon et al. 201849 | Treatment times |
| Ehntholt et al. 202050 | ||
| Telestroke and telemedicine and telehealth in stroke management (largely hospital focused) |
Baratloo et al. 201851 Totten et al. 201952 Hubert et al. 201453 Rubin et al. 201354 Demaerschalk et al. 201055 Johansson and Wild 201038 |
Thrombolysis times/time to treatment, comparisons with face-to-face ‘bedside’ care (e.g. in-hospital mortality), 90-day mortality, administration of tissue plasminogen activator, implementation factors, costs |
| Enhanced ambulance/paramedic role | Flynn 201756 | Impact of handovers and paramedic on health outcomes |
| ‘Stroke mimics’ | Jones et al. 202157 | Increased thrombolysis within this population (risk) |
| Digital health intervention in cardiovascular disease – economic evidence | Jiang et al. 201858 | Cost-effectiveness, co-utility, cost–benefit, cost–consequences analyses |
Key words that were frequently identified across the papers and therefore informed the design of the phase 2 systematic review, were ‘telemedicine’ OR ‘telestroke’, ‘Stroke’ OR ‘Acute Ischaemic Stroke’, ‘emergency medical services’ (EMS), ‘Mobile Stroke Unit’ (MSU), ‘Prehospital’, ‘Paramedics’, ‘Emergency medical technicians’, ‘ambulances’.
Phase 2: systematic review
The systematic review identified 47 papers that met the inclusion criteria (32 primary studies39,41,59–88 and 15 reviews16,39,40,47,48,53,89–97; for details, see Appendix 1, Table 11). One record was a trial registration;98 this led to the identification of a research paper,80 which was included in place of the trial registry record. The publication date ranges suggested a fairly slow research trajectory, with signs of growth from 2019 onwards. The majority of studies originated in the USA and Germany, with a small number of studies found from across Scandinavia, Asia and mainland Europe. The UK studies were based in Scotland and no studies were based in the NHS in England. Below we provide a summary of the findings. We included other reviews to ensure that no underlying studies were missed, to provide continuity with phase 1 and to confirm any evidence and knowledge gaps.
Insights from available reviews
In a systematic review into prehospital EMS telehealth, Winburn et al. 40 identified 68 studies, the majority of which focused on stroke and acute cardiovascular care, suggesting a broader trend in this area. Amadi-Obi et al. 89 also found that the literature on prehospital telemedicine largely focused on stroke. Generally, existing reviews described how technological innovations in prehospital stroke management may improve acute care management and workflows (e.g. timely assessment) and potentially lead to faster access to intravenous (i.v.) thrombolysis treatment. This followed the ‘time is brain’ rationale and importance of improvement interventions in the hyper-acute time window (e.g. Aude Bert et al. 2013). 47
Interventions to reduce delays to treatment included ‘advanced notification’ by EMS, alerting hospital stroke teams of an incoming patient, as well as the administration of therapies within ambulances. However, within-ambulance treatment was not the primary focus of our review. We found limited information in the literature about the impact of ambulance telemedicine on destinations or pathway determination in stroke care. This included leveraging digital technology to allow patients to remain at home and be referred to an outpatient TIA clinic rather than be taken to hospital following a remote diagnosis.
Previous reviews identified the concept of ‘video examination of stroke patients in ambulances for earlier stroke recognition’,47 and there was a wider interest in ‘adjunctive technology’ at the prehospital stage to support the stratification of patients by ambulance crews. 16 For example, a systematic review about ‘advances in TeleStroke’53 identified a number of issues in the prehospital ‘stroke rescue chain’, viewing telemedicine as a potential solution to ‘cut down prehospital times’ and improve prehospital stroke recognition and ‘prenotification’ to hospital stroke teams. However, the review concluded that, although prehospital video triage could enhance stroke identification and facilitate advance knowledge of incoming patients, there remained gaps in understanding about 4G coverage, impact on outcomes and cost-effectiveness. 53
Reviews published in 2020–21 confirmed these observations, reporting a small but growing evidence base about mobile telestroke technology based on primary studies, but with few employing a randomised design. In their scoping review, Lumley et al. 16 found only 15 studies that reported mobile telemedicine using video and audio technology. Most of these (11 of the 15) had limited information on costs, safety and outcomes. While Lumley et al. 16 note the relative maturity of telemedicine for stroke, they report:
little robust evidence of impact on patient outcomes . . . Telestroke may expedite time-to-treatment by attenuating hospital-based assessment, but studies to date have shown little evidence of more efficient patient redirection to stroke-specific centres and no impact on health outcomes for specific population groups.
Lumley et al. 16
More recently, Guzik et al. 93 hypothesised that there may be additional advantages of mobile telestroke in prehospital assessment, particularly in the context of COVID-19, in terms of reducing the need for ‘multiple re-evaluations’ of the patient and directing them to the most appropriate hospital.
Regarding implementation factors, which were also a focus of our systematic review, Rogers et al. 48 provided helpful insights into ‘prehospital telehealth utilization’. They identified a variety of health studies, including six studies specific to stroke. Issues concerned bandwidth and download speeds, with an ethnographic study noteworthy for highlighting usability problems. The authors recommended greater input from patients, doctors, and staff in the design of telemedicine systems to support implementation, noting the potential for telemedicine to support remote triage in emergency care. However, they observed ‘a paucity of published studies describing scientifically valid and reproducible evaluations at various stages of telemedicine implementation in ambulances.’48 Although this general observation was confirmed by our up-to-date systematic review, we also identified additional new primary studies on this topic, some of which reported positive outcomes (see Service outcomes).
Intervention characteristics
Information on the types of interventions found in the primary studies included in this systematic review is provided in Appendix 1, Table 11. There has been a gradual evolution in the approaches and technologies adopted over time, and a range of studies conducted, including feasibility pilots and prospective studies. We saw a shift to studying prehospital ‘mobile telestroke’ or ‘mobile telemedicine’. A term found in earlier literature was ‘online medical control’, defined by Verma et al. as instances where ‘paramedics contact the medical control physician before a Code Stroke triage is assigned’:87 a prehospital stroke protocol was implemented to identify patients eligible for tissue plasminogen activator treatment and to expedite transfer to a specialist stroke centre.
Although this study did not include the use of sophisticated videoconferencing technology, the authors did highlight an opportunity to improve diagnostic accuracy and triage by implementing an online approach as such a system would enable paramedics to contact a doctor remotely and seek advice before a final decision is made to triage a patient to a stroke centre. This approach was contrasted with ‘offline’ medical control, whereby paramedics make decisions independently from a hospital doctor, following guidance and stroke protocols. 87
More recent studies demonstrated a shift from pre-alerting stroke teams in hospitals to using videoconferencing technology in an ambulance to support two-way communication, alongside the use of recommended stroke protocols and diagnostic tools. However, it became evident during this review (especially when screening titles and abstracts and 288 full texts) that it was not always straightforward to determine the precise nature of communication between ambulance and EMS personnel and hospital doctors. For example, a receiving clinician could be a neurologist, a teleconsultation physician, or an emergency or ‘EMS’ physician. This appeared to result from differing terminology used in published research, and differing acute stroke service configurations employed internationally. In the USA, first emergency responders may be paramedics or firefighters, and therefore there is some mention of firefighting personnel in the EMS response. We included papers discussing ‘EMS physicians’ as well as stroke doctors to avoid missing any important insights about within-ambulance telemedicine systems and communication between EMS teams to external experts who used stroke diagnostic tools to support remote triage and diagnosis, although this did push the limits of our inclusion criteria.
In terms of technological capabilities, although MSUs are highly equipped vehicles and thus excluded from this review, there was evidence that standard ambulances can be equipped with more advanced digital and communication technologies. High-definition cameras and audio equipment were used to support EMS-hospital communication, accurate triage and real-time sharing of patient data [e.g. heart rate and blood pressure (BP)] via stroke teleconsultations. Prehospital ambulance systems showed signs of greater digital maturity over time, including data integration with hospital information systems, as well as more portable elements with the move to 4G and as new technologies come on board (e.g. iPads, handheld devices and computers). The majority of pilots and feasibility studies identified in this systematic review typically involved building telemedicine or ‘mobile telestroke’ systems in ambulances and testing their functionality (e.g. via simulations) before use in the field and on actual cohorts of patients. Noteworthy studies of this kind were undertaken in Germany and the USA. Our systematic review also found several newer studies, including an important prospective and observational study from Germany that suggested that the evidence base on these systems is indeed evolving over time. Eder et al. 81 described the ‘Stroke Angel’ programme, an ‘interdisciplinary project, which aims to improve acute stroke management using mobile technologies (handheld computer) for decision-making, documentation, and communication support between EMS and in-hospital stroke staff’. 81 This was an example of a well-developed prenotification and acute stroke management system in the prehospital pathway, integrating stroke diagnostic protocols, a handheld device, time stamping, image capture and integration with the receiving hospital’s own information system. Another example, from China, was Wu et al. ’s77 study of ‘Green’, which was a prehospital notification ‘real-time communication’ system for the management of acute stroke. This approach used a smartphone application, which underscores the use of more portable and advanced digital approaches over time that support data integration with hospital records and information systems.
Although we found a small number of recent examples of within-ambulance telemedicine in acute stroke care that are particularly relevant to the rapid evaluation, our review generally highlighted a gap around mobile systems used outside the ambulance by emergency clinicians, specifically the use of videoconferencing to bring the neurologist on site, for example in a patient’s home or at a residential care facility. Moreover, some studies (e.g. Mazya et al. 84) focused on more traditional hospital pre-notification systems rather than prehospital mobile telemedicine that enables video and audio data transmission in real-time, either in or outside an ambulance. By contrast, recent research has provided examples of more digitally advanced systems. 66,77,81 This review therefore confirmed the relative newness of EMS clinicians using videoconferencing and digital technologies in the field to diagnose and triage stroke patients with the support of a remote stroke doctor, alongside the use of established stroke protocols (e.g. the FAST test).
Technological, human and usability factors
Many studies focused on feasibility analyses and piloting prior to their use in the field, owing to the newness of the intervention and a need to ensure technological stability and usability. Such studies also explored interactive elements, such as communication between health professionals, and task and workflow features.
The first ambulance telemedicine system dates to the early 2000s. 62 However, a research group from Germany reported ‘the first study that evaluated prehospital teleconsultation including real-time video transmission from an ambulance in real stroke patients’ in 2010. 79 In this prospective study, the researchers tested a within-ambulance telemedicine system (the intervention) on patients and compared it against patients treated in the standard way (the control group). The researchers were interested in testing the feasibility of the emergency telemedicine system and its technical functions. 79 They found that the telemedicine system worked well in the majority of cases and that ‘neurological co-evaluation’ was feasible. Video streaming was found to be helpful, although there were some cases of loss of audio or video transfer. This represented one of the earliest studies on this topic involving patients and which concluded that the concept of telemedicine system for stroke care was feasible, while noting that technical issues would require resolution. In another paper, the authors suggested that lack of mobile network coverage was a limiting factor. 60
Other pilot and feasibility studies confirmed that video image quality and audio transmission was good enough to support remote neurological assessment, with ambulance telemedicine for stroke care performing well technically in feasibility and usability testing with clinicians, including in rural areas, provided there was reliable network or broadband coverage. 62,64,67,75 Although it should be noted that these telemedicine set-ups were typically within an ambulance and reliant on mounted ceiling cameras and audio units, the suggestion was that technical failure may be less common than human error. Chapman Smith et al. ,62 for example, found in their study of a telestroke platform that ‘91% of the prehospital mobile evaluations were completed without any major technical failure’.
An important human factor is communication; that is, both verbal and non-verbal signalling within consultations. Joseph et al. 66 were interested in staff interactions when using an ambulance telemedicine system and applied cognition theory to understand this phenomenon. The research team looked at communication between nurses, paramedics, and neurologists through simulated teleconsultations and structured analysis. They found ‘significant back and forth verbal interactions between the neurologist and the paramedic and the neurologist and the patient, with the paramedic frequently serving as the intermediator between the other two’. 66 The researchers also noted potential risks to teleconsultation, including ‘loud background noise from sirens and traffic and poor audio signals’, all of which can make communication problematic. They therefore suggested telemedicine systems should be designed with consideration for ‘nonverbal team communication’. 66
Elsewhere, the same US-based research group (Rogers et al. )69 analysed task structure and flow in a remote ambulance telemedicine system for stroke to provide greater understanding of the usability issues and human factors that might influence implementation, again using simulations. They found that not being able to fully understand or clearly hear the paramedic or neurologist was an issue, leading the researchers to observe that better technical equipment (e.g. microphones, camera) in an ambulance can help reduce instances of miscommunication and ensure that the remote neurologist can see the patient and pick up on non-verbal cues. 69
It is also important to note the added value of bidirectional video data transmission. In Germany, for example, emergency physicians have often been dispatched on site. However, owing to a shortage of staff, there has been an interest in remote EMS-physician telemedicine, including for diagnosing cases of suspected stroke and other neurological events. 85 Although at the boundaries of inclusion for this review owing to use of ‘EMS physicians’ rather than neurologists, the study from Aachen, Germany, was an interesting case of an evolving emergency telemedicine system used for prehospital stroke clinical assessment because the system was modified for neurological conditions to ensure that video became mandatory. Our review thus suggested that two-way audio and video communication may be especially important for clinical assessment of stroke. 65
Staff training
It has already been established in the literature that training of emergency medical services personnel can improve stroke screening. 90 Several studies have reported training for emergency staff before going live with telemedicine systems, such as by using simulations, protocols and scripts. 59,65,79 Chapman et al. 62 have noted that doctors needed to be trained about ‘best positioning of tablet and lighting’ in their study of a mobile telestroke platform (the iTreat study), and Bergrath et al. 79 have observed that new equipment and workflow processes required doctors to be trained. In one analysis, for example, the researchers discuss an 8-hour staff training programme designed for a prehospital telemedicine system and undertaken prior to implementation. 60 The training was for both paramedics and emergency care physicians to ensure that they were familiar with workflow, technical equipment in the ambulance, communication and miscommunication, and processes for emergencies (e.g. via simulated activity).
Service outcomes
Recent studies included in this review indicated that prehospital ambulance telemedicine, which includes prenotification to a hospital, can reduce transfer and treatment times. Studies reported an array of impacts [e.g. feasibility and door-to-needle (DTN) times] depending on their study design, purpose and the development or maturity stage of the specific system under investigation. We did not limit our review to searching for particular outcomes in order to capture this diversity.
Wu et al. 78 examined the impact of the ‘Green’ system on DTN times, reporting that, in 2 years of using the system in Beijing, ‘DTN time was significantly reduced from 50 minutes in 2018 to 42 minutes in 2019’. 78 The authors concluded that the Green system was impactful in terms of DTN time and highlighted additional time-saving opportunities, such as patients consenting to treatment earlier at the prehospital stage.
Eder et al. 81 reported findings from the Stroke Angel initiative, which involved two study cohorts. Cohort II, which followed ‘workflow modification’ after Cohort I, found an impact on door-to-scan times and DTN times compared with standard care, and a higher rate of thrombolysis. Although the study was not a RCT and the authors acknowledge a number of limitations (e.g. use of the system being at EMS clinician discretion), they concluded that ‘Stroke Angel improves the odds of systemic thrombolytic therapy use as compared with a conventional prenotification workflow protocol’. 81
Drenck et al. ,80 reported a cross-sectional study of an intervention implemented in Denmark, where emergency staff assessed the patient for symptoms and signs of stroke in the field and communicated with a neurologist in a stroke centre to assess eligibility for scanning and potential thrombolysis. Ambulance on-scene time (OST) was a primary outcome, with the authors finding that ‘the median on scene time was 21 min[utes]’ and that ‘neither relatives nor ambulance trainees present on-scene or in the ambulance were found to affect OST when compared to no relatives or ambulance trainees, respectively’. 80
Economic and resource outcomes
Our systematic review identified one cost-effectiveness analysis on this topic. Valenzuela Espinoza et al. 41 attempted the ‘first cost effectiveness model for in-ambulance telemedicine’, defining in-ambulance telemedicine as ‘live bidirectional audio-video between a patient and a neurologist in a moving ambulance and the automated transfer of vital parameters’. 41 The authors compared standard stroke care with in-ambulance telemedicine, applying a decision tree and Markov model. Several cost advantages were identified at the hospital end (e.g. staff) as well as the fact that ambulances can be straightforwardly equipped with telemedicine systems. Therefore, there was overall added value, even when factoring in staff training as an implementation cost. The authors also predicted lower costs as mobile telemedicine is more widely implemented in ambulances. Although the authors acknowledged that their analysis was not based on RCT data, they concluded that ‘in-ambulance telestroke is highly cost-effective from a health-care perspective, resulting in more QALYs and less costs starting from a realized time gain of 12 minutes’. 41
Discussion
Principal findings
Our review confirmed a limited, yet growing evidence base about telemedicine use within ambulances for the diagnosis of stroke. This can be viewed as a growing field of research compared with a traditional focus on MSUs, telestroke networks and other hospital-to-hospital telemedicine systems, which are common in the USA and Europe where rural areas require access to neurological expertise that is otherwise unavailable.
This systematic review provided an important update on a scoping review by Lumley et al. 16 identified in phase 1. We conducted a systematic review containing more key terms and medical subject headings to hone in on the emerging topic of within-ambulance mobile telemedicine (Lumley et al. 16 included a number of other innovations in their scoping review, such as biomarkers, which was not the focus of our study). Despite not including conference proceedings, we were able to identify new studies as our search was highly sensitive and extended beyond 2019 to 2021. As with Lumley et al. ,16 a meta-analysis was not attempted owing to the diversity of studies found. We also included existing literature reviews to get a wider overview of the topic and growth in the field and to ensure that we captured all relevant studies.
Our systematic review found limited data on the impact on outcomes, although these, including data showing the impact on treatment and destination times, are emerging. However, there was generally limited information about other service outcomes of importance to understanding prehospital video triage, such as the impact on decision-making, patient destination and avoidance of unnecessary hospital admissions (thus helping reduce demands on hospital services).
It has already been observed that ‘ambulance-to-hospital teleconsultation may result in markedly reduced delivery times for thrombectomy without delaying intravenous thrombolysis’;84 further research and evaluation is required to support this assessment, although there are early indications of positive impacts on thrombolysis and destination times from a small number of observational and cohort studies. Yet, clearly, more insights are needed about not just transfer and treatment times, but destination end points within the stroke care pathway. With regard to the technical specifications and usability of these systems, there was a gap concerning the influence of different professional roles, such as whether there are advantages of ‘paramedic–neurologist’ communication over ‘paramedic–nurse’ communication. Joseph et al. 66 provided an especially helpful study into communication between different professional groups, taking a human factors and task-based approach and highlighting teamwork and a number of practical considerations (e.g. background noise).
There was a lack of insight about the overall safety of these systems (although clinical safety is covered by reference to the use of diagnostic scales and stroke protocols, e.g. FAST and NIHSS). We found one study on overall cost-effectiveness that confirmed what some authors have noted elsewhere: that mobile telemedicine in ambulances is a lower-cost option than introducing MSUs. Notably, there were few RCTs, although a number of studies attempted comparisons with standard acute stroke care and emergency pathways. Finally, more needs to be understood about the impact of different health system models and stroke service configurations on implementation. For example, in some cases designated telestroke centres may field all calls from paramedics/EMS clinicians; in other cases, it may be neurologists based within specific hospitals. The impact of different service models, therefore, requires further investigation.
Observations regarding quality and characteristics of evidence
Both of our reviews identified a large number of pilot and feasibility studies, as opposed to mixed-methods service evaluations (i.e. studies including qualitative, quantitative and economic analyses) or comparative study designs (e.g. of standard pathways versus prehospital triage). We found many literature reviews, of variable quality, indicating ongoing interest in the topic of prehospital triage in stroke pathways and its impact on consultation, journey and treatment times. We also noted a smaller number of prospective and retrospective study designs using cohorts of stroke patients. Yet overall, there was a limited amount of empirical evidence drawn from implementation and prospective studies of emergency care and stroke pathways, especially studies reporting national findings as opposed to results from interventions within specific regions or urban geographies. The novelty of the intervention and approach is likely to explain these findings and the tendency in the literature towards ‘proof of concept’ and pilot studies focused on issues of technical feasibility, user satisfaction, system performance and stability. A common example was simulations conducted by researchers and developers concerned with user acceptance and issues of signal quality and data transmission to test whether prehospital triage technology can be used safely in clinical care to support remote diagnostic assessment. Therefore, evidence on prehospital triage systems for suspected stroke that use low-cost telemedicine technologies – specifically, real-time, audio-visual data transmission outside highly equipped ambulances – remains at a relatively early stage of maturity.
Strengths and weaknesses
Strengths of the review included a transparent and explicit search strategy, specifically following PRISMA for Scoping Reviews (PRISMA-ScR) 2020 guidelines in phase 2 where multiple databases were searched by an experienced researcher with expert information specialist input. Collaboration was used to design and execute a systematic search strategy (i.e. with tailoring to the different databases). We developed and validated a screening tool to operationalise the inclusion and exclusion criteria with a second reviewer sense-checking findings and final inclusion decisions through a process of using software (Rayyan.ai’s collaboration function) and meeting to discuss interpretations. The wider team and co-investigators also provided ongoing advice and feedback into the design and findings.
Owing to the timeframes of this rapid evaluation, no risk-of-bias assessment or detailed critical appraisal was performed, although this will take place prior to publication of the systematic review in a peer-reviewed journal, following PRISMA-ScR 2020 recommendations. 24 Given the limited evidence on this topic, the review could be further strengthened by undertaking additional steps that were not feasible within the timeframe of a rapid evaluation (e.g. additional citation searching and checking pre-print servers and recent conference proceedings). In this chapter, we have summarised the main findings with a focus on the issues most relevant to the empirical findings and conclusions of this report, and the most recent empirical evidence found.
Implications
There were several implications from this search of the literature, especially from the findings from the systematic review. First, mobile telemedicine was found to involve some examples of well-equipped ambulances with high-definition cameras and audio equipment, and there are suggestions in the literature that these may mitigate background noise and capture non-verbal cues, which are important in stroke teleconsultations. Given a small but growing evidence base in this area, there is need for further evaluations and clinical trials of these systems that take into consideration the specific equipment used, its functionality, its costs and the implementation factors that shape usage, for example understanding which contexts are optimal for performing remote triage and assessment and which are not, and why. Second, only one cost-effectiveness analysis was identified in the systematic review, suggesting a need for more economic studies, especially given the variations found between health systems internationally and regionally and different system set-up costs. Finally, there was a lack of detailed exploration about the patient experience, with most studies focusing instead on the perspectives of health-care professionals and advantages for health providers.
Overall, we found that less is known about stroke teleconsultations that are on scene (such as in a person’s home), away from a more highly equipped ambulance, and involve emergency clinicians and remote stroke neurologists. In particular, more knowledge is needed about how prehospital telemedicine systems affect stroke destination decisions (including the identification of non-stroke patients or ‘stroke mimics’), and this may help to ensure that patients are directed to the most appropriate point of care or service. This is also necessary given the potential of mobile telemedicine to help with managing high levels of demand on stroke and emergency services, and the possibility of costs savings (e.g. by reducing unnecessary ambulance journeys and diagnostic scans). Very few studies discussed in any detail bypassing certain hospitals as a result of remote triage decision-making between ambulance and stroke clinicians.
More understanding is also required about the contribution of mobile telemedicine over prehospital stroke notification systems that involve a stroke alert to the hospital and data transmission (e.g. vital signs). Future studies may also wish to consider which types of service outcomes are most appropriate for measurement when evaluating pilot services. For example, there may be only marginal gains of using mobile telemedicine for prehospital triage if onset-to-treatment times are already excellent and occur within a well-specified destination pathway. As one paper80 noted, there has been much attention on studying and improving onset-to-treatment times for decades, yet only in recent years has there been a focus on prehospital stroke care, including how much time is spent on scene by emergency clinicians.
Chapter 4 Qualitative analysis of perceived usability, acceptability and safety of prehospital video triage, and influential factors
Overview
What was already known?
-
Prehospital video triage for suspected stroke patients was introduced in early 2020 in NC London and East Kent.
-
Gaps exist in the evidence related to patient outcomes, experience and satisfaction, communication between professionals, and impact on decision-making.
-
Little use has been made of social science concepts to understand such services.
What this chapter adds
-
There were contrasts in aspects of the triage services and how they were implemented in both areas. However, stroke and ambulance clinicians in both areas saw the interventions as highly usable and acceptable. A barrier to acceptability and sustainability was that acute stroke physicians delivered triage assessments alongside their other professional duties, placing pressure on them and potentially limiting the quality of communication.
-
Leaders of the triage services were conscious of risks to patient safety and set processes in place to monitor and manage potential adverse incidents. Local data collected through these processes indicated few reported safety incidents, and there was a broader perception among ambulance and stroke clinicians that these services are providing safe care.
-
Several factors relating to theory about implementation and sustainability of innovations (including contextual factors, innovation characteristics, and implementation approaches) helped explain what drove change rapidly, how widespread ownership of the services was achieved, and which further actions might facilitate sustainability of these services.
-
In terms of context, the COVID-19 pandemic created a ‘burning platform’ for change, which interacted with long-established challenges around appropriate conveyance of suspected stroke patients. These factors combined to encourage more facilitative governance processes at local system and service levels.
-
In terms of innovation characteristics, stroke and ambulance clinicians found prehospital video triage straightforward to use, suggesting it offered important advantages over conventional approaches to assessing and conveying suspected stroke patients.
-
In terms of implementation approaches, service leaders worked across organisational and professional boundaries to ensure rapid and effective development of the services, approval by local organisations and systems, and uptake by frontline clinicians. Training (in terms of its availability and intensity) was seen as an important influence on clinicians’ awareness of and confidence in using prehospital video triage.
Background
As discussed in Chapters 1 and 3, there is limited evidence on how prehospital video triage for suspected stroke patients is implemented and delivered, with particular knowledge gaps related to usability, acceptability and safety of such services. 15,16,99 In addition, social science concepts have seldom been used to understand implementation and delivery of prehospital video triage for stroke. The introduction of prehospital video triage in NC London and East Kent represented an opportunity to study two such services implemented under similar circumstances but with differences in the intervention itself, how it was implemented, the contexts into which they were introduced and their perceived usability, acceptability, and safety. In this analysis, we therefore sought to address the following three questions:
-
What was the usability, acceptability, and safety of prehospital video triage implemented in NC London and East Kent, as perceived by the ambulance and stroke clinicians who used them?
-
Which factors influenced uptake and impact of these systems?
-
Which aspects of these systems should be retained post COVID-19 and what adaptations (if any) are required to support their implementation?
Method
To address these questions, we conducted a cross-case analysis (where each pilot prehospital video triage service was a case), drawing on a range of qualitative data sources. These included stakeholder interviews, non-participant observations and relevant documentation. Data collection took place from August 2020 to May 2021; our overall approach to recruitment, data collection, and analysis can be found in Chapter 2.
To analyse the factors influencing delivery and experience of prehospital video triage – alongside exploring our evaluation questions – we used a framework developed through a review of factors influencing health service innovation, with a particular focus on digital innovations (Figure 3). 17 Key factors included the nature of the innovation, ways in which it was implemented, the settings into which it was introduced and the wider context for change, reflecting broader literature on diffusion of innovations. 99
FIGURE 3.
Factors influencing adoption and sustainability of innovations in health-care. Purple segments relate to contextual factors, orange segments relate to how interventions were implemented, and the green segment relates to the intervention itself. Adapted from Nolte E, How Do We Ensure that Innovation in Health Service Delivery and Organization is Implemented, Sustained and Spread?, Box 2, Page 11, Copyright (2018) WHO Regional Office for Europe. URL: https://apps.who.int/iris/bitstream/handle/10665/331980/Policy-brief-3-1997-8073-2018-eng.pdf?sequence=5&isAllowed=y (accessed 1 September 2022). 17
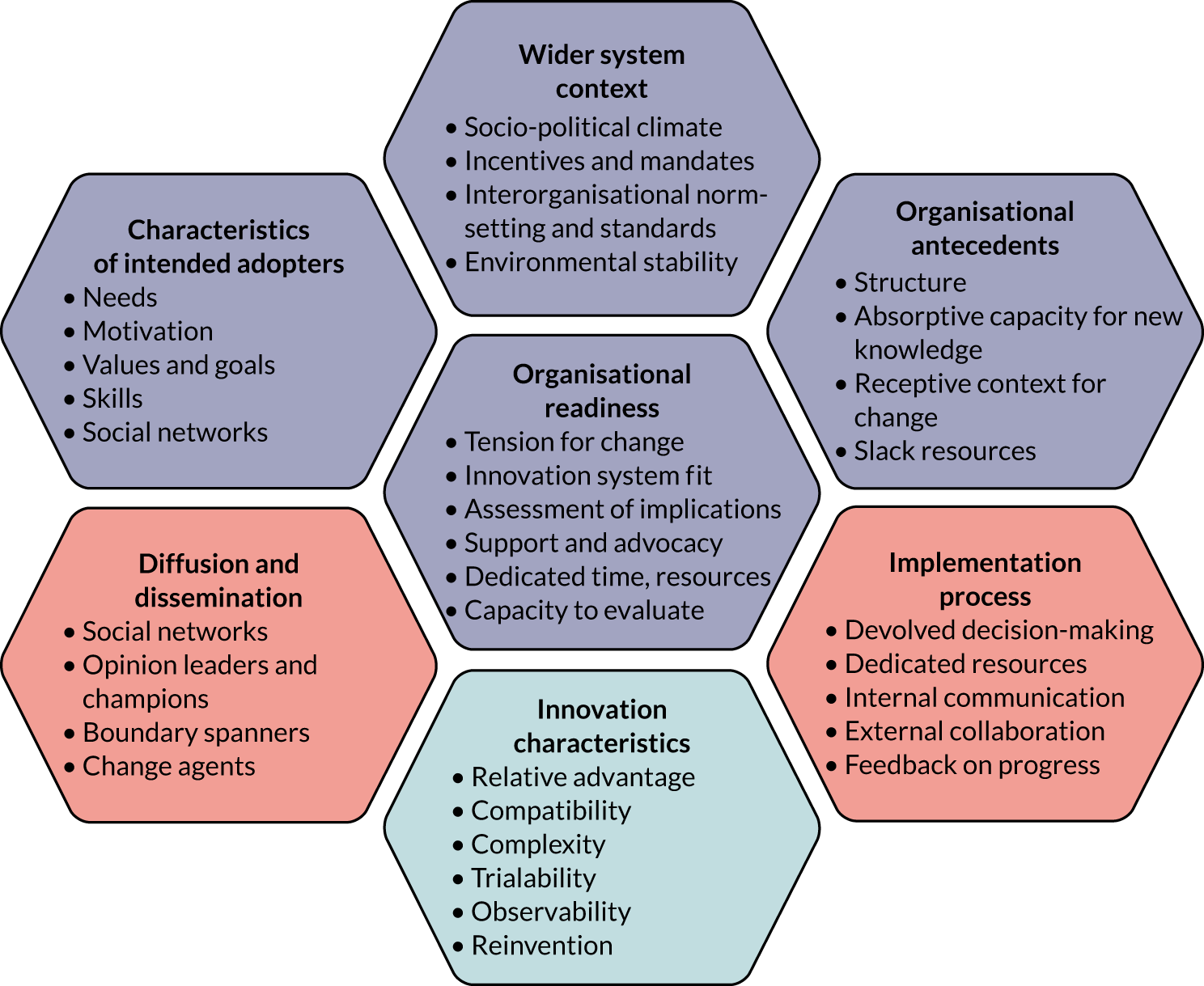
Results
Overview of findings
Our results are organised as follows. First, we present the data collected and analysed in this analysis. Second, to address important gaps identified in the literature, we present the analysis of ambulance clinician and stroke clinician perspectives on the usability, acceptability, and safety of prehospital video triage. Third, we describe some factors related to implementation of these services, guided by the Nolte framework17 for understanding implementation of digital innovations in health-care settings (see Figure 3). Throughout, we discuss issues that appeared specific to clinician groups and areas, but also draw out common themes.
Data analysed
We analysed interviews conducted remotely with 27 local stakeholders in NC London and East Kent (Table 4). Interviewees included stroke consultant physicians and ambulance clinicians who had experience of using prehospital video triage, and local clinical leads of the prehospital video triage services based in ambulance and stroke services in both areas. We analysed observation data on 9 events, including governance meetings, training sessions and engagement events (which we attended remotely). Finally, we analysed 23 documents, including meeting minutes, service pathways and protocols, and training documentation.
| Data type | Source | Area | Total | |
|---|---|---|---|---|
| NC London | East Kent | |||
| Interviews, n | Stroke consultant physicians | 7a | 2a | 9 |
| Ambulance clinicians | 11a | 7a | 18 | |
| Total interviews | 18 | 9 | 27 | |
| Observations, n | Governance meetings | 4 | 3 | 7 |
| Training/engagement events | 2 | 0 | 2 | |
| Total observations | 6 | 3 | 9 | |
| Documents, n | Meeting documents | 12 | 5 | 17 |
| Training/support documentation | 2 | 2 | 4 | |
| Service pathways | 1 | 1 | 2 | |
| Total documents | 15 | 8 | 23 | |
Clinician perspectives on usability
Ambulance and stroke team clinicians in both areas reported overall that they found prehospital video triage usable, in terms of the platform used (FaceTime), reliability of connection, and sound and image quality.
Ambulance clinician perspectives
Ambulance clinicians were broadly positive about sound and image quality, with clinicians frequently suggesting that it was very much in line with what one might expect from any video call:
The call quality has been as good as it can be on a screen. So I haven’t, it hasn’t been blurred or anything, it’s been as good as FaceTime can be.
ST008, ambulance clinician, NC London
I can’t really fault it at all. I think FaceTime is very, very easy to use. You can call a number, we’ve all got the number in our phones now and the FaceTime number logged in our iPads and you’ll get an answer straightaway from one of the doctors or the nurses.
ST013, ambulance clinician, East Kent
Although clinicians emphasised that the overwhelming majority of calls had clear image and sound, some clinicians noted occasional connection issues, which had implications for image quality. For example, in NC London, ambulance clinicians highlighted ‘black holes’ in certain built-up areas:
It just depends whether you’re in a building, what part of London you’re in. There’s areas which are black holes really for signal.
ST018, ambulance clinician, NC London
Reflecting their more rural setting, East Kent ambulance clinicians described gaps in coverage in the countryside:
In Kent especially, sometimes the patients that you go to it’s really hard to get any sort of signal, because they live in the middle of nowhere. So, occasionally that can be a problem, but for the most part it was fine.
ST014, ambulance clinician, East Kent
In describing difficulties in making a connection, ambulance clinicians emphasised the urgent, time-limited nature of the situation [‘they’re time critical, you can’t wait until you’ve got a signal (ST014, ambulance clinician, East Kent)]. In response, interviewees described using other available connections to improve signal quality:
It’s all done through mobile data networks, but if you’re in an area where there’s very poor data networks or poor signal, we’ve been known to talk to the patient relatives and use their home Wi-Fi and get a better signal through that way.
ST017, ambulance clinician, East Kent
To avoid delays and support safety, if a signal could not be obtained clinicians indicated that they would revert to protocols employed before the introduction of prehospital video triage. For instance, this would involve making a telephone call to pre-alert the hospital and convey the suspected stroke patient to the nearest routinely-admitting stroke unit.
Stroke clinician perspectives
Stroke consultant physicians in both areas suggested that image quality and connection was broadly sufficient for conducting the remote triage process. For example, a stroke physician in East Kent who was a frequent user of the service reported that only a small proportion of calls faced issues that prevented an assessment being conducted:
You’re talking about four, four-and-a-half months now, there were less than 10 calls where we could not do FaceTime, the reception is so poor we couldn’t. Maybe I would even say half a dozen times. So, yes there were moments where we couldn’t continue the call and we need to come out of it and speak to them over the phone.
ST016, stroke consultant physician, East Kent
In NC London, clinicians reported that there had been initial problems with accessing the Wi-Fi services in the host hospital, which meant that many calls suffered from poor signal initially. However, once this issue had been identified it was resolved quickly by team leaders:
We had a few cases where the Wi-Fi coverage or the quality of the picture and the audio seemed to be cutting out. And we investigated this. When I say investigated, we spoke about this. And what we found was that the device that was being used in Queen Square [NHNN] wasn’t connected to the Wi-Fi in the hospital. And therefore, it was using 4G or 3G. So, the immediate solution we made sure that all devices were connected to Queen Square Wi-Fi. And that was quite a quick solution to a problem that was reported from the frontline.
ST021, service lead, NC London
Another technical challenge described by stroke physicians in NC London related to pass-codes and the ‘baton phone’, which was passed between members of the stroke team, depending on who was on duty. Particular challenges emerged for stroke clinicians who were not working onsite:
There was one technical problem actually which was quite a big deal. That happened Friday I think when I did it last. I’m using it from home and not from the office, which I think is something to touch on later, and I thought I’d signed in and I got all the signing details, but I hadn’t. So, I was sitting there constantly thinking I’m plugged in, unfortunately the person who has passed the baton on to me still had the phone with them, and just messaged me going, ‘[Name removed] are you picking up?’ And I was like, ‘What do you mean?’ Not realising that I actually hadn’t fully logged in. Fortunately, because he gave me the alert, I then logged in again but if he hadn’t done so I could have been blissfully unaware.
ST005, stroke consultant physician, NC London
NC London service leads referred to ongoing discussions of the possibility of moving the service to the GoodSAM platform. This was seen as a way to address some of the challenges faced by offsite stroke physicians in accessing the service. However, at the time of data collection discussions were ongoing to address local IT obstacles preventing use of the platform:
[Host organisation] created a firewall that stopped GoodSAM running properly on any of its devices and it took us months to realise . . . So it’s a marker of somehow, some of the difficulties with big hospital trusts in trying to do things that are new, are relatively untested and with relatively short time frames.
ST019, service lead, NC London
Clinician perspectives on acceptability
Ambulance clinician perspectives
A question raised during the design phase of this evaluation was whether ambulance clinicians would find this service acceptable. This derived from concerns that, by introducing stroke physician perspectives earlier in the patient pathway, ambulance clinicians might perceive these new services as reducing their agency in clinical decision-making. However, in practice, ambulance clinicians were highly supportive of prehospital video triage, citing increased confidence/reassurance about their decisions on patient conveyance:
When we hand over we get reactions that suggest that they think we’ve been a bit silly. So, when we use this system we can feel comfortable in the knowledge that someone above us made that decision. So, even it ends up being the wrong decision, we don’t feel silly.
ST006, ambulance clinician, NC London
It is good to be able to have a phone conversation with a specialist and for them to say, yes bring them here or no take them to Margate or take them to Ashford. So, it definitely does relieve some of the pressure, which I find a benefit anyway, especially being newly qualified.
ST014, ambulance clinician, East Kent
Stroke clinician perspectives
For the stroke clinicians, the prehospital video triage process itself was not seen to represent a major change to what they would do when assessing a suspected stroke patient under ‘traditional’ circumstances, the only difference being that they were doing it earlier in the care pathway:
[O]nce I’d done a few, it was actually very straightforward and not a huge amount different to coming and seeing a patient in A&E.
ST002, stroke consultant physician, NC London
An important issue that was likely to affect acceptability to stroke physicians and the long-term sustainability of prehospital video triage was that assessments were being conducted in addition to – and alongside – their existing duties. Therefore, several clinicians described having to take a triage call while conducting another aspect of their role, such as conducting a ward round or assessing a TIA patient:
It’s quite disruptive: you are assessing a TIA patient, the phone rings, and you have to stop the clinic. It’s not good: you have a good feedback experience from the patients on the LAS, but the ones that are in the hospital will not give you a good feedback.
ST001, stroke consultant physician, NC London
Because of the threat to sustainability this issue represents to these services, local leads have discussed the potential for alternative models whereby clinicians are given dedicated time to deliver assessments as part of a rota (as recorded in our field notes at the NC London stroke triage oversight meeting, February 2021).
Clinician perspectives on patient safety
Interviewees reported relatively few concerns about patient safety. The main (and interrelated) considerations identified related to whether conducting the prehospital video triage assessment contributed to unwarranted delays in patients receiving care and whether patients were conveyed to the appropriate service.
Appropriate patient conveyance and timely delivery of care
There was a general recognition from all clinicians that conducting the remote triage consultations could potentially add time to reaching a decision on where a patient should be taken, which may in turn increase overall journey time. However, ambulance clinicians recognised the additional value of reaching the appropriate services:
Your journey time from Dover to Canterbury is 10 minutes, but your journey time from the Sussex border to Canterbury, you’re looking at 30–35 minutes, whereas the nearest A&E is a shorter distance – but through the triage system we find out, ‘is it right for the patient?’.
ST017, ambulance clinician, East Kent
Ambulance clinicians in East Kent felt the requirement to call a stroke nurse before commencing the prehospital video triage process with a stroke physician was unnecessary, and viewed the removal of this process (see timeline, Table 1) positively, as it reduced unwarranted delays:
The main one was the delays with phoning the stroke nurse first, but now that’s all been taken care of, that’s obviously a positive thing.
ST014, ambulance clinician, East Kent
In addition, several stroke physicians described the value of conducting initial assessments of patients in advance of their arrival at hospital, whereby the stroke teams felt primed to deliver appropriate care as soon as the patient arrived:
If we purely stick to the diagnostic element of it, (a) you have seen the patient already, which meant that when the patient comes to the hospital certain pre-admission events we could tick, so that when the patient comes to the hospital we can put them through the appropriate channel of investigation and the diagnosis. We arrive at the right diagnosis much faster, much faster. Since time literally is brain, that shorter time of investigations time allows us to treat the patients much quicker.
ST016, stroke consultant physician, East Kent
One stroke physician raised an important patient safety issue that reflected a potential downside of introducing stroke specialist assessment. Specifically, they asked whether or not stroke specialists, through their expertise in and prioritisation of stroke, might on occasion miss more urgent conditions:
There have been a few patients who I think if I’d have assessed them on the video call I would have said, this person is really sick and needs to be in an A&E immediately . . . I think a lot of people are, probably just how the human brain works and especially a lot of doctors, are very focused on their specialty, and so when things come where there might be symptoms outside their specialties – so, for example, cardiology emergencies, they may be just unaware of what those are, so, that was a slight issue.
ST011, stroke consultant physician, NC London
Governing patient safety
Given the significant changes to patient pathways, patient safety was a central consideration for service leads and their colleagues:
We were petrified that the project could fail with an early problem, this thing if we had made a mistake with any of the early cases and something terrible had happened, it felt as if it could stop quite quickly.
ST019, service lead, NC London
In response to this natural concern, teams in both areas set up governance processes to monitor potential patient safety issues, primarily in relation to decisions resulting from the triage process, but also in terms of changes in how the services were to be delivered:
We wanted to make sure that any of the revocations didn’t result in a mistreatment. And as far as I’m aware we’ve only had one case out of 1000 where that may have happened. But even that’s debatable. So those meetings were set up with the Stroke Networks, so I think we probably had – it would be interesting to know how many we’ve had and the minutes. But they were key points of, you know, ‘Is this working? Is it safe? And are we good to proceed?’
ST021, service lead, NC London
We have put in a more formal governance process, where we review any clinical incidents, misdiagnoses, complaints – you know, sometimes you get dissatisfied paramedics with the service they’ve received. So, there’s now a formal process that we didn’t have before we started in the autumn. Yeah, before the second wave, while we caught our breath in the summer, we put in a monthly prehospital governance set-up where we’d discuss any instance. We’d discuss problems with the pathway and try and improve things.
ST027, service lead, East Kent
Examples of these processes in action included analysing missed calls and cases where patients had a second conveyance from a non-stroke service to a HASU or where patients treated in a non-stroke service had a stroke. Root cause analyses were conducted routinely on such cases to establish contributing factors and to ensure that issues with the system were identified and addressed (as recorded in our field notes at the NC London stroke triage planning group meeting, February 2021).
Communications and decisions
Communication was central to prehospital video triage. This reflected the fact that (without access to brain scanners in the ambulance) both ambulance and stroke clinicians had limited tools available to aid diagnosis:
I think the FAST test was quite basic and that’s all the kind of . . . We don’t have any other tools to kind of establish what’s going on.
ST008, ambulance clinician, NC London
The key interactions were between stroke and ambulance clinicians, and between clinicians and patients.
Interactions between clinicians: shared decision-making
Analysis of the interactions between ambulance and stroke clinicians revealed both parallels and contrasts. One contrast was in relation to who made the final decision on patient destination. In NC London, the position was that, although stroke physicians made a recommendation, ambulance clinicians could still over-ride this if they had concerns:
We made it clear that if at any stage, again, because of this hierarchy component between doctors and paramedics, we wanted the onus – although the responsibility might go to the doctor in terms of taking on a patient, we wanted the paramedic to be able to over-ride any decision that was deemed to be dangerous or that the paramedic significantly disagreed with. We really wanted to empower the paramedic to say, ‘Thank you doctor for that advice. I’m a bit worried about this, so I’m going to revert to my normal pathway which we know is safe.’ It might not be the most – it may end up with a patient being overtriaged. But it won’t end up with someone being undertriaged.
ST021, service lead, NC London
Ambulance teams reported valuing the process of working with stroke specialists, as it enhanced decision-making:
Speaking with the stroke consultant then was amazing because you could then kind of go into a deeper assessment, whether it was the right eye that was affected or his kind of right visual field, which was really helpful because otherwise it wasn’t triggering the FAST test. So we kind of mutually came to agreement about where to take that patient which was really helpful.
ST008, ambulance clinician, NC London
In contrast, in East Kent there was the expectation that the stroke physician’s recommendation would be followed and that responsibility for that decision would sit with the stroke physician:
We’ve said on the flowchart, you know, you get the name of the doctor and you document the name of the doctor. And in terms of governance then the responsibility, the clinical responsibility for that decision sits with the doctor not with the ambulance service.
ST025, service lead, East Kent
One interviewee indicated some discomfort with this principle, stating that they would prefer to trust their own instincts and describing their concern that other ambulance clinicians might reduce their investment in clinical decision-making around suspected stroke:
I myself would take the initiative going, no you know, I still think from my clinical experience that this could still be, so I’m going to treat as is. But I would worry that other clinical staff would potentially, would take that for gospel, and say, OK fine, we don’t need to worry then. Let’s just pootle along, half an hour journey to the local. And then actually it was a full-blown stroke and now the patient is like even worse off because of that.
ST023, ambulance clinician, East Kent
Interactions between clinicians and patients and carers
Another important aspect of communication was between clinicians and patients and carers. Frequently, interviewees reported how positively patients and carers perceived prehospital video triage:
They’re already quite reassured that we’re there, but then when you have a consultant in their home they found it amazing. You could see that they were so impressed and they felt like they were getting gold-standard care from the outset.
ST006, ambulance clinician, NC London
At the same time, many suspected stroke patients tend to be older, and sometimes unfamiliar with videoconferencing (though some clinicians noted that many older people are now used to such technology, especially following the pandemic). Interviewees related that patients were sometimes confused by the video consultation, which in turn, required a degree of support from the onsite ambulance clinicians:
I’ve never had a problem with any patient kind of during the iPad conversation or anything like that, everything has been quite straightforward especially when it’s been explained properly and therefore they’ve been quite for it.
ST013, ambulance clinician, East Kent
However, some stroke team interviewees raised concerns about the impact that their environment might have on the quality of their communication. Many interviewees noted that stroke physicians did not have a dedicated space in which to conduct these assessments; furthermore, calls could come at any time of the day or night. By extension, some stroke clinicians described how unusual or noisy spaces might negatively impact the quality of their communication, even suggesting that their professionalism might be questioned:
I’ve taken calls when I’ve been outside Pret; it’s really not ideal for my patient, confidentiality and professionalism as well. Your doctor to not have the wind blowing and there to be traffic noise and stuff.
ST011, stroke consultant physician, NC London
Some of these work setting issues were addressed with a straightforward technical fix:
The immediate solution that came up is that the doctors in Queen’s Square have a headset that’s connected to their device so that it reduces background noise and makes the consultation easier to understand.
ST021, service lead, NC London
However, as discussed in Clinician perceptions of acceptability, the wider pressures associated with clinicians conducting this role on top of other aspects of their lives (professional and otherwise) remained a challenge to both delivery and sustainability of this service.
Factors perceived as influencing implementation of prehospital video triage
In this section, we discuss factors that emerged as important to the implementation and delivery of prehospital video triage in NC London and East Kent. This is arranged around the factors identified by Nolte (Figure 4). 17 In each case, we consider how aspects of these factors (e.g. relative advantage in relation to ‘innovation characteristics’) might help explain the implementation and impact of prehospital video triage.
FIGURE 4.
Overview of factors perceived as influencing implementation. Italic text covers obstacles to implementation; roman text covers facilitators. Adapted from Nolte E, How Do We Ensure that Innovation in Health Service Delivery and Organization is Implemented, Sustained and Spread?, Box 2, Page 11, Copyright (2018) WHO Regional Office for Europe. URL: https://apps.who.int/iris/bitstream/handle/10665/331980/Policy-brief-3-1997-8073-2018-eng.pdf?sequence=5&isAllowed=y (accessed 1 September 2022). 17
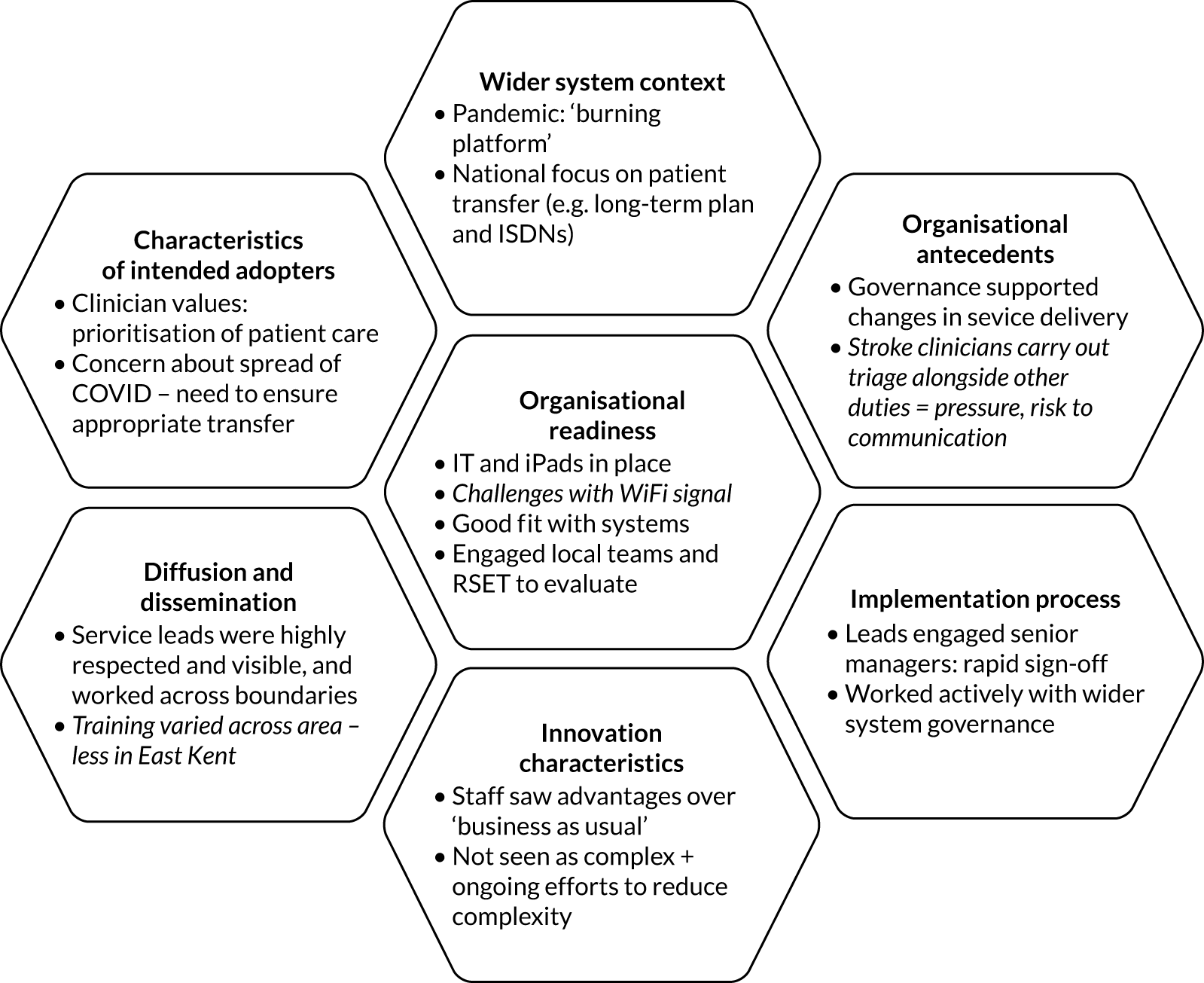
Innovation characteristics
In terms of relative advantage, clinicians felt the new services offered clear potential benefits as compared with ‘business as usual’, in terms of both service delivery and patient care. This was central to building a sense of ownership among local clinicians (all of whom were taking on additional work and changing practice in order to deliver this service):
I think it’s got benefits for patients, in terms of they can potentially be managed differently to go to a specialist hospital. But also, it can be better for stroke units as well, so that we’re not taking patients there unnecessarily if they don’t need to go. So, I think there’s benefits for both really.
ST018, ambulance clinician, NC London
In terms of complexity, clinicians commonly described delivering prehospital video triage as straightforward, as the majority of the assessment processes were those that ambulance and stroke clinicians would conduct under any circumstance. Ambulance clinicians frequently referred to how straightforward it was to initiate contact with stroke teams. However, they also noted the value of (1) an introduction to using prehospital video triage; and (2) reminders about how to use it, noting that strokes represent a small proportion of patients treated by ambulance clinicians overall.
Wider system context
There were concerns within stroke services about prehospital patient conveyance long before these services were introduced. Much has been written over the years (including research by several of the co-authors) about low specificity of prehospital triage instruments (e.g. FAST): this leads to unnecessary conveyance of many ‘stroke mimic’ patients to stroke units, which has implications for both quality of care for stroke and non-stroke patients and the efficiency and sustainability of stroke services. Therefore, much national guidance (e.g. the Long Term Plan and associated plans for delivery of ISDNs)10 already acknowledged the need for more effective prehospital triage.
However, COVID-19 introduced greater urgency to this discourse. As outlined throughout this report, the COVID-19 pandemic was central to many aspects of the story of the prehospital services in NC London and East Kent. The pandemic represented a ‘burning platform’, transforming the established concerns about prehospital conveyance of suspected stroke patients by adding a significant threat to patient safety, made more urgent by the fact that the HASUs in both areas had been moved and thus were no longer co-located with ED services:
There was a catalyst. And the catalyst was COVID-19 and the fact that COVID-19 created the need for a radical expansion of critical care beds at UCLH . . . When the hyper-acute stroke unit was at UCLH it had the fortunate position of being co-located with an ED . . . When it moved to Queen’s Square then it obviously doesn’t have that versatility. So, there was a concern that lots of patients would suddenly turn up at Queen’s Square and then have to be rediverted to different EDs, which would cause a massive backlog and a bottleneck in the system.
ST021, service lead, NC London
Therefore, the wider service changes implemented to help manage the pandemic may have acted as an important lever to increase uptake of prehospital video triage. These wider contextual factors interacted with more local contextual factors, as outlined in the sections below.
Characteristics of intended adopters
In our interviews it emerged strongly, and perhaps unsurprisingly, that one of the key priorities of both ambulance and stroke clinicians was ensuring safe, high-quality patient care. Another shared priority inherent to these professions was the importance of patients receiving care at the right place, first time. Some interviewees stated explicitly how firmly the new services aligned with their professional values:
My initial impression is probably, number one, was that’s it way over time, like we’ve been wanting to do this for ages.
ST002, stroke consultant physician, NC London
However, as discussed in Chapter 1, there were some concerns at the outset that this shared overarching priority might have conflicting implications for stroke and ambulance clinicians. An example of this was the concern that ambulance clinicians might perceive the potential benefits of accessing specialist secondary care stroke expertise as being outweighed by a delay in patient conveyance to hospital.
As outlined below (see Diffusion and dissemination), an important task in implementing prehospital video triage related to ensuring that the intervention fitted with these clinicians’ priorities, and that the case was made sufficiently for the benefits of the triage process.
Organisational antecedents
Interviewees described a receptive context for prehospital video triage. This was reflected in local systems (1) encouraging innovative thinking and (2) being open to doing things differently. It was felt that COVID-19 (see Wider system context) acted to shape these local organisational antecedents. In both areas, in terms of internal processes, the pandemic prompted an increased focus on responding quickly to the unfolding crisis. This was in turn facilitated by an increased willingness of organisational and system leadership to enable new ways of working through timely sign-off of innovations:
Everything went into top gear in terms of getting different processes through governance. Certainly, within SECAmb anyway, it did. So there was a huge focus on how can we support the entire system and make sure that everything doesn’t fall over because of COVID.
SE025, service lead, East Kent
Another important aspect of organisational antecedents was the resources available to deliver the services. Although the technology and IT infrastructure was broadly available (discussed further under Organisational readiness), perhaps the resource most keenly required was stroke clinicians available to conduct the remote assessments. In practice, the prehospital services were delivered by stroke clinicians alongside their existing workload. Delivering these services could only be achieved through a degree of sacrifice, which was in part encouraged and justified by staff in terms of the unprecedented crisis services were facing. Furthermore, it placed substantial pressure on the individuals concerned, with implications for the delivery and sustainability of both their new and established duties:
It [delivering prehospital triage assessment] is quite disruptive in terms of other activities you are doing at the same time. There is no clear plan how to change this, is this going to continue a triage system and every time I go to do my TIA weekend clinic have to do this at the same time? It’s quite disruptive you are assessing a TIA patient, the phone rings and you have to stop the clinic.
ST001, stroke consultant physician, NC London
Organisational readiness
Challenges identified around capacity to deliver the services suggest that the organisations were not entirely ‘ready’ to deliver these new services without a degree of sacrifice. However, many conditions for change were supportive. One example of this was in terms of technical resources: ambulance services in both areas had already distributed iPads throughout their services (i.e. all ambulance clinicians had one), and initial issues with connectivity in NC London were addressed by establishing access to the local Wi–Fi network. Another example of technological resources being available was the provision of communication headsets to reduce environmental distraction during remote consultations.
As discussed under Wider system context, the pandemic prompted a sudden tension for change: as the crisis grew, many staff described a clear impetus for this change to happen as quickly as possible.
We found evidence of good innovation-system fit, in that prehospital video triage did not require substantial changes to what staff did in assessing patients, but instead a shift in the stage and the setting in which certain decisions were made. Yet, at the same time, staff felt strongly that this shift in stage had an effect on the contribution they were making:
I can’t say that it was a massive change for me as such, it wasn’t, I think everyone around my area took to the change quite well and have been using the system fairly easily.
ST013, ambulance clinician, East Kent
The first time, I thought, ‘Wow, this is amazing’. It was great for me as a physician seeing things first-hand and felt as if you were making a difference . . . You know, lots of symptoms can be mimics of neurology as well and helping the triage appropriately it’s self-efficient whilst doing it, and a really worthwhile service . . . I thought it was really impressive and innovative and it felt as if you were making an impact instantly.
ST005, stroke consultant physician, NC London
In terms of capacity for evaluation, both areas drew effectively on local resources (e.g. local clinical fellows) to support internal evaluation. For example, the evaluation team attended several meetings in NC London where the local clinical fellow took the central role in describing progress of prehospital video triage and presenting in-depth analysis of local service-level data. Furthermore, the service evaluation presented in this report reflects the clinical leaders drawing on locally available sources of independent evaluation support.
Implementation processes
As discussed in Organisational antecedents, local governance systems were adapted in the early stages of the pandemic to facilitate rapid innovation. In both areas, prehospital video triage service leads engaged actively with local and wider governance to drive rapid implementation of change. For example, a service lead in NC London described the processes by which they engaged with internal leaders to build organisational support for the pilot prehospital video triage service:
I think it was pulling, using certain people, so using [senior manager] and using our chief clinical information officer, [senior manager]. And you know, posing it to them that it’s not progressing this. Do we think it’s a good idea or not? And if not then that’s fine we just need to know, yes or no. And I think I did sit down with our chief medical officer and gave them a 5-minute elevator pitch. And I had a PowerPoint® [Microsoft Corporation] slide and we worked through it. And told her about the concerns raised by that particular individual and they weren’t, those concerns weren’t seen as relevant. So it was quite, I think that was quite a useful mountain to get over there.
ST021, service lead, NC London
Similarly active responses were seen in terms of wider external governance. In both NC London and East Kent, service leads engaged actively with external systems, for example the NC London and Pan-London Clinical Advisory Groups (CAGs). Service leads indicated that governance was predominantly facilitative of change and ‘red tape’ was less pronounced than under pre-pandemic circumstances:
These Clinical Advisory Groups, [. . .] they were either set up during this first phase or they sort of came to full life during this first phase and they were set up entirely to help with the rapid process of evaluation and decision making in the context of the crisis and COVID. So this proposal [for prehospital triage] went to these CAGs because the CAGs were there to try and judge whether this change or that change was necessary or appropriate, specifically to get through COVID.
ST019, service lead, NC London
In East Kent, service leaders worked with local hospital and ambulance services senior management during the initial development of the prehospital video triage services, and described a view from wider system governance that going through established committee processes would have slowed progress of change unnecessarily given the circumstances:
There was an edict saying all bets are off with regard to governance, just do the right thing. This is a pandemic. Don’t waste your time going through committees, just do the right thing. We quickly locked up the SOP [standard operating procedure], did a very limited bit of training and comms, and just went live with it.
So, do you think without COVID you would have been able to implement that quickly?
No. Absolutely. We probably would still be at the drawing board, because (a) we wouldn’t have moved the stroke service, so we wouldn’t have had this possible imperative to do something to look after the patients that were travelling further, so we wouldn’t have moved the stroke service. And also, (b) we wouldn’t have got the change of governance.
In both areas, service leaders shared progress on the new prehospital video triage services with the wider system, for example the CAGs in NC London and the Kent and Medway Stroke Board in East Kent. The focus of these updates included impact on patient destination and safety within increasingly tight governance processes. This ensured wider transparency around the new services and was seen as an important aspect of quality assurance, with potential to facilitate further roll-out of the services if shown to be effective.
Diffusion and dissemination
An important component of implementation was how and by whom clinicians were engaged with the new services. In terms of opinion leaders and boundary spanners, service leads in both stroke and ambulance services were well-respected both as clinicians and as innovators in their localities (and beyond in several cases). An important example of how service leads worked across organisational boundaries was the efforts in NC London to ensure that ambulance clinicians’ knowledge of the patient was suitably valued by stroke clinicians:
So there are two things there really. One that you might miss on really key information that the paramedic had. But also you might alienate one of your key stakeholders. So what we did, we agreed that the primary vignette, I think they refer to it as, would always be asked of the paramedic, you know what, or the initial person on the scene. ‘What’s been happening? Can you tell me the story?’ And then just be quiet and let them talk. And then it would be, ‘Right please introduce me to the patient’. And that really helped, I think it really helped build this professional trust and respect.
ST021, service lead, NC London
As noted in Intervention characteristics, training was seen as a potentially important way to ensure that ambulance clinicians remained confident and aware of prehospital video triage (given that stroke patients represent a small proportion of cases treated by ambulance clinicians). Interviewees reported that NC London did more in the way of training, in terms of having online and in-person run-throughs. Ambulance clinicians seemed positive about this training, suggesting that the process could be enhanced by involving stroke clinicians, ambulance clinicians and patient perspectives, citing potential to bridge professional/organisational boundaries:
One thing that would be useful, not necessarily using the system, but in terms of educational perspective would be to have some case studies presented by ambulance crews and with maybe some patients’ perspectives. But with the consultants to actually go through some of the decisions that are being made, just to try and share some of their knowledge.
ST018, ambulance clinician, NC London
East Kent clinicians reported receiving less in the way of active training, but many indicated that they would find this useful:
I mean it’s not difficult for me to go and ask, ‘How do you use this?’ But I think a lot of the time they just assume that an email is enough and then they say, any queries contact your own CL (Clinical Lead). But yes, training could be done a lot more for a lot of things, for sure.
ST014, ambulance clinician, East Kent
I don’t think there was any formal training, certainly no face-to-face classroom type training from the trust. We had plenty of e-mails and written information about it and how to do procedures, how to go through it. They all made sure that we had the FaceTime on our devices, but anything further than that, you know, anything technical I’ve got a teenage son to be honest, so he does technology.
ST006, ambulance clinician, East Kent
These contrasting approaches (and related experiences of ambulance clinicians) suggest a need for future, training-based adaptations to the implementation or roll-out of services.
Discussion
Principal findings
There were several contrasts in the prehospital video triage implemented in NC London and East Kent, and in how they were put into action. However, there were many common findings on usability, acceptability and safety. The first of these concerned the usability of prehospital video triage, in terms of the platform used, reliability of connection, and sound and image quality: stroke and ambulance clinicians in both areas saw the services as highly usable. Clinicians reported that the processes concerned did not represent a significant change to how patients were assessed, and the technology used was perceived as familiar and straightforward. Ongoing governance processes permitted rapid adaptation to address obstacles to usability, for example by enabling access to local Wi-Fi or providing headphones to reduce environmental distractions.
In terms of acceptability to users (i.e. ambulance and stroke clinicians), both clinician groups found the services acceptable (despite concerns that ambulance clinicians may have been reluctant to lose decision-making agency, we only found pockets of this in East Kent, where responsibility shifted more firmly to stroke physicians). A potential obstacle to clinician acceptability was that stroke physicians found delivering assessments alongside their other professional duties a significant challenge. In terms of safety (as perceived by ambulance and stroke clinicians), the new services represented an important change to the patient pathway in both areas. Therefore, service leads were highly conscious of risks to patient safety and set processes in place to monitor and manage any incidents. Observations of local governance meetings suggested these reviews identified very few safety incidents, and each incident was analysed to support further development of the service.
Several factors related to theory about implementation of innovations (innovation characteristics, contextual factors and implementation approaches) helped explain what drove the decision to change, how development progressed so rapidly, how widespread professional ownership of the services was achieved and which further actions might facilitate greater sustainability of these services. Key among these were national and local contextual factors, characteristics of the innovation itself, and the implementation and dissemination approaches employed.
Contextual factors (at system and local levels) played an important and interrelated role in implementation and delivery of prehospital video triage. The ‘burning platform’ of the pandemic and longstanding challenges of appropriate conveyance of suspected stroke patients combined to form a highly receptive local context for change. This was reflected in more facilitative governance processes and high local buy-in for change. In addition, other service changes implemented locally to manage the pandemic (specifically, moving stroke units so that they were no longer co-located with ED services) may have been important levers to increase the uptake of prehospital video triage. There was a strong influence of adopter characteristics: clinicians’ and local systems’ prioritisation of quality and safety of care facilitated rapid uptake by frontline clinicians. It also ensured that processes to monitor and address potential adverse incidents or other issues were central to governance of the pilots. Organisational antecedents also played a role: limited resources in the form of stroke team capacity represented a significant source of clinician stress; this may have important implications for the sustainability of prehospital video triage services.
The innovation characteristics of prehospital video triage were viewed positively by their intended users. Stroke and ambulance clinicians found prehospital video triage straightforward to use and reported that it offered important advantages over conventional approaches for assessing and conveying suspected stroke patients.
Implementation and dissemination were pivotal to the development and delivery of prehospital video triage. Clinical leaders took active and collaborative approaches to negotiate and drive change: they worked across several boundaries, including organisational (working beyond local acute and ambulance trusts to engage the wider system) and professional (with close collaboration between stroke and ambulance clinicians in both areas). This supported rapid development, approval and implementation of the prehospital video triage services. Regular governance meetings played a key role in monitoring delivery of prehospital video triage and providing important assurance and learning opportunities about patient conveyance and patient safety. Contrasts in training approaches employed in NC London and East Kent suggest that more active approaches were preferred by staff and may act to form stronger interprofessional collaboration in future.
Strengths and weaknesses
A strength of this analysis was that we were able to study two similar innovations implemented at the same time in two regions of the NHS in England . However, there were also several contrasts, including patient eligibility, decision-making processes and training approaches. Therefore, this evaluation represented a ‘natural experiment’, and was thus a valuable learning opportunity. Several features of the cases evaluated may make them relevant to other parts of the NHS in England. The innovation itself relied on established technology (i.e. iPads and FaceTime) that are increasingly common in NHS ambulance services. In terms of contexts, we were able to study implementation of prehospital video triage in NHS settings during the COVID-19 pandemic in contrasting urban and rural settings. Another important strength of this analysis was that it was coproduced with stroke and ambulance leads in both pilot areas but also informed by an up-to-date review of the evidence, meaning that the focus of the evaluation reflected both local expertise and the wider evidence base. Using remote data collection methods [i.e. Microsoft Teams® (Microsoft Corporation) videoconferencing for interviews] increased the evaluation team’s flexibility, meaning that interviews could be conducted or reorganised to accommodate the requirements of extremely busy clinicians.
There were several limitations, chiefly related to data collection. We were unable to recruit similarly large numbers of clinicians in both areas; this meant that our sample from East Kent might not reflect the same range of clinician perspectives as in NC London. Furthermore, we only interviewed stroke consultant physicians, and future research would benefit from capturing the perspectives of less senior doctors who also delivered prehospital video triage. There were several other clinical groups we were unable to interview for this evaluation. Towards the end of the project, we approached a number of nursing and ward management staff in the hope of obtaining a broader perspective on the impact of prehospital video triage on stroke teams. However, given wider pressures and the limited time available, we were unable to conduct any of these interviews, and therefore to gain their insights we shared our interim findings with these individuals for their feedback. To mitigate the gaps in our clinical stakeholders, we shared interim findings with a wider range of clinical stakeholders in NC London and East Kent, all of whom felt that the themes presented rang true. Finally, we were unable to interview patients and carers about their experiences of these services; this was due to our project’s status as a rapid service evaluation. We prioritised obtaining clinicians’ views of patient experience, but recognise this as a key limitation that flows from the nature of projects of this kind.
Comparison with other studies
As outlined at the beginning of this chapter (and in Chapter 3), there is a small but growing evidence base related to the implementation and outcomes of prehospital video triage for suspected stroke. We believe that our analysis both complements and extends this evidence base.
Previous research on acceptability of prehospital video triage for stroke has described staff being satisfied in terms of the quality, safety and reliability of services. 16 Our analysis confirmed broad satisfaction with services while also noting some important underlying benefits. Examples of benefits reported by ambulance clinicians were educational (i.e. learning more about the nature of stroke) and improved experience of delivering this care pathway (i.e. feeling more confident that hospital services would not query the patient conveyance decision).
Our findings on usability aligned with previous research in this context. For example, our analysis confirmed the previously-identified importance of signal stability and audio-visual quality to ensuring a clear assessment process. 16 However, whereas previous simulation-based research has focused recommendations on improving audio-visual technology,69 some of the interventions identified in our analysis (e.g. the value of an audio headset or a separate office to reduce ambient distraction) may reflect the advantages of studying service delivery in the (frequently overcrowded and noisy) real world.
Our evidence on interprofessional communication contrasts somewhat with previous research on prehospital video triage for stroke. Whereas past work has presented the role of the paramedic as ‘the ears and eyes of the neurologist’,66 in our analysis we found a strength in a more balanced dynamic. Placing ambulance clinicians’ evaluations at the heart of the overall patient assessment was felt to increase buy-in from these clinicians; furthermore, it gave stroke clinicians an increased appreciation of ambulance clinicians’ expertise.
Previous research has commonly noted the importance of training ambulance clinicians to ensure effective use of prehospital video triage. 16 Our analysis confirmed the contribution training made to clinicians’ confidence in using the system. In addition, some participating ambulance clinicians also described the potential for joint training to bridge interprofessional boundaries between stroke and ambulance clinicians. This issue, related to engendering shared ownership of such services, aligns with findings from previous reviews on implementing telestroke networks. 15
Our analysis demonstrated the value of applying social science theory to the analysis of implementation factors, which our systematic review (see Chapter 3) found to be a gap in the literature. Nolte’s framework17 helped us identify several important factors related to contextual factors (at national, regional and service levels), implementation approaches (e.g. collaborative leadership, governance of change and training approaches), and the innovation itself (i.e. its perceived straightforwardness and advantage over ‘business as usual’).
Implications
Prehospital video triage as implemented in NC London and East Kent was seen as usable and acceptable by clinicians. However, greater capacity (i.e. more stroke clinicians available to conduct assessments) may increase the acceptability, experience and sustainability of these services. Rapid implementation of change was enabled by the global pandemic (its effects were also likely to have been strengthened by increased facilitation of change by local governance processes at system and service level). Clinical leadership in both stroke and ambulance services was key to implementation. The collaborative approaches taken by these leaders to work across organisational boundaries and to engage frontline clinicians (e.g. by designing processes that reflected professional expertise and where training ensured clear understanding of the new services) was important in ensuring uptake of the new services.
Chapter 5 Survey of ambulance clinician perceptions of prehospital video triage
Overview
What was already known?
-
Prehospital identification of stroke can be challenging. Prehospital video triage may improve identification of stroke, thus supporting more appropriate patient conveyance decisions, better-informed stroke teams in receiving hospitals and by extension improved time to treatment and better patient outcomes.
-
There is little published evidence on how ambulance clinicians experience prehospital video triage and what influences their decision-making; furthermore, the majority of such research has been conducted in simulation (as opposed to ‘real-world’) settings.
-
Our qualitative analysis (see Chapter 4) included a limited number of ambulance clinician perspectives, but identified several key themes related to prehospital video triage, including its usability, influence on conveyance decisions and patient safety, and implementation.
What this chapter adds
This chapter presents a survey of 233 ambulance clinicians who had experience of using prehospital video triage in NC London and East Kent. Responses identified several factors related to major themes of this evaluation, including usability, impact on conveyance decisions and patient safety, and implementation (specifically training); ambulance clinicians also provided views on the future use and development of prehospital video triage:
-
Usability – although ambulance clinicians in both areas found prehospital video triage usable, a higher proportion of NC London clinicians were of this view. This pattern was mirrored in clinician views of audio-visual signal, where again NC London clinicians were more likely to agree that signal was of sufficient quality. Underlying these patterns may be differing likelihood of experiencing difficulties with internet/Wi-Fi coverage in the studied areas.
-
Conveyance decisions – ambulance clinicians in both areas felt that prehospital video triage influenced conveyance decisions occasionally.
-
Patient safety – NC London clinicians were more confident about the safety of prehospital video triage than clinicians in East Kent. Safety concerns included potential for misdiagnosis and delayed or inappropriate conveyance.
-
Training – ambulance clinicians in NC London were much more likely to feel that they had received sufficient training. This is likely to reflect the different training approaches employed in NC London and East Kent.
-
Future use and development – ambulance clinicians overall saw prehospital video triage as an improvement on previous prehospital approaches and wanted it to continue. Again, this was felt more strongly in NC London than in East Kent.
Background
Research suggests that prehospital diagnosis of stroke is important but potentially challenging. 15,16,100 Our review of the literature on prehospital video triage (see Chapter 3) indicated that most research conducted in this domain has related to technical usability, such as audio-visual signal and reliability of internet/Wi-Fi. 13,16,48,93 The bulk of this research has been conducted in simulated (as opposed to ‘real-world’) settings, which may partly limit applicability of findings to real-world implementation. To date, little research has been conducted on several important factors related to the impact of prehospital video triage, including patient conveyance decision, patient safety and implementation (e.g. in terms of how it is supported and disseminated through leadership and training). 16
Our qualitative analysis (see Chapter 4) was able to access only a limited number of ambulance clinician perspectives. However, it identified several potentially important themes related to prehospital video triage, including its usability and acceptability (including quality of audio-visual signals and communication with stroke teams), its influence on decision-making and patient safety, and factors influencing its implementation (e.g. training).
This chapter presents a staff experience survey that was distributed to ambulance clinicians in NC London and East Kent. The survey was co-designed with ambulance and stroke clinicians, and in part guided by human factors thinking on human interaction with technological systems. Human factors approaches bring together engineering and design perspectives to improve and optimise information systems and technologies, making them more user-friendly. 101
The survey aimed to capture ambulance clinician perceptions of the new prehospital video triage services, and in doing so complement and extend understanding of several themes raised in Chapter 4. These included acceptability of prehospital video triage (EQ2); usability (e.g. audio-visual quality) (EQ3); perceived influence on conveyance and patient safety (EQ4); and whether or not, and how, prehospital video triage might be sustained and developed in the future (EQ6). In addition, by addressing training, the survey addressed one of the central implementation themes that emerged in Chapter 4.
Methods
Survey tool development
The survey was developed by members of the evaluation team (led by JL) alongside clinical collaborators in NC London and East Kent. It was designed to be short and as easy as possible to complete, to reduce burden on participating clinicians (who were at the time dealing with substantial service pressures during the COVID-19 pandemic) and thus maximise survey completion.
Examples of collaborator feedback included clarifying items on conveyance decision-making and training. The final version of the survey was tested and signed off by clinical collaborators and built using the software package Opinio (which is hosted on the UCL information services infrastructure and meets UCL information governance standards).
The survey consisted of 18 questions, including consent, and was designed to take approximately 10 minutes to complete (see Report Supplementary Material 5 for the final survey questions). Most questions were multiple choice, with a ‘free text’ option for some questions, for example those covering patient safety, training and recommendations for future development.
Sampling
Our sample was ambulance clinicians who had experience of using prehospital video triage for stroke, piloted in NC London and East Kent. To ensure that respondents had some experience of using prehospital video triage, we asked about frequency of use of the system. Beyond this, our survey used a convenience sample of ambulance clinicians based in the NC London and East Kent areas. As a result, the extent to which our findings can be generalised to other ambulance clinicians and services piloting such services in other clinical or geographic contexts is limited.
Distribution of survey and data collection
The survey link was distributed to 550 ambulance clinicians who had used prehospital video triage in NC London, and to 424 ambulance clinicians in East Kent. Our clinical collaborators sent potential participants a survey invitation by e-mail; the e-mail included a participant information sheet and a link to the survey. Reminders were sent out at regular intervals to promote survey participation. In East Kent, the survey was also promoted to staff on a private Facebook (Facebook, Inc., Menlo Park, CA, USA) page.
Informed consent was taken at the beginning of the survey. The survey invitation made it clear that the survey should only be completed by ambulance clinicians who had used the prehospital video triage services (e.g. specifying FaceTime on iPads). To ensure confidentiality, no names, e-mail addresses or other personal data were collected. Respondents were therefore able to complete the survey completely anonymously using the link provided. Participation was on a completely voluntary basis.
The survey was left open for just over 5 weeks, from 21 April to 30 May 2021.
Data analysis
The raw survey data were downloaded to Microsoft Excel for analysis; we used the ‘pivot table’ function to collate overall scores and percentages for the overall sample and disaggregated by participating areas (i.e. NC London and East Kent). For each survey item, a chi-squared test of independence was performed on the raw data to compare the patterns of responses from NC London and East Kent ambulance clinicians.
Results
Response rates
A total of 309 staff accessed the survey, but 76 responses were found to be incomplete and therefore removed from the sample. There were 233 total respondents across both regions, with 159 fully completed responses in NC London (representing a response rate of 159/550, 28.9%) and 74 in East Kent (representing a response rate of 74/424, 17.5%).
Overview of findings
Detailed survey responses are presented in Appendix 1, Table 12. In the sections that follow, we report in-depth survey responses, covering ambulance clinicians’ perspectives on the following topics:
-
clinician experience and usage of prehospital video triage
-
usability of prehospital video triage
-
technical performance of prehospital video triage
-
responsiveness of stroke teams
-
influence on conveyance decisions
-
impact on patient safety
-
sufficiency of training
-
future use and development of prehospital video triage.
Clinician experience and frequency of use
As noted in Appendix 1, Table 12, the majority of respondents across both regions had ≥ 3 years’ experience of working as ambulance clinicians (76%, n = 177) and there was no significant difference between the levels of experience reported in the two areas [χ2(3, N = 233) = 3.40; p > 0.05]. Usage patterns were broadly similar across both regions at an aggregate level, with the majority (93.1%) of all respondents having used the system three or more times. However, there was a significant difference in the pattern of responses from NC London and East Kent ambulance clinicians [χ2(3, N = 233) = 12.97; p < 0.01]: Figure 5 shows that a higher proportion of respondents in East Kent (49%) reported using the triage system 10 times or more than in NC London (26%).
FIGURE 5.
Frequency with which respondents reported using prehospital video triage. Baseline, N = 233 (LAS, n = 159; SECAmb, n = 74).
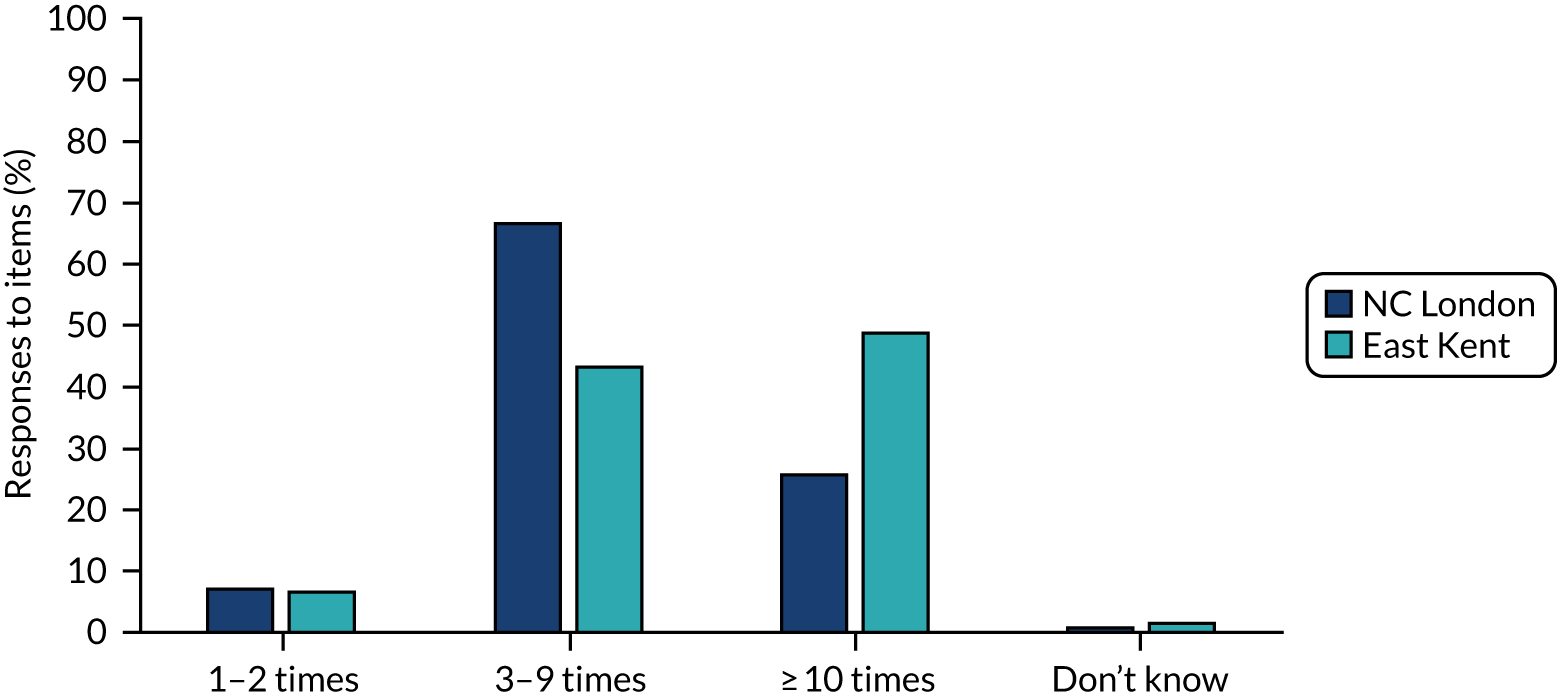
Usability of prehospital video triage
The majority (89%) of respondents in both areas reported that they were satisfied with ease of use of prehospital video triage. However, the pattern of responses in NC London and East Kent differed significantly [χ2(3, N = 233) = 35.33; p < 0.01]: Figure 6 shows that although most respondents in both areas agreed, strong agreement was higher in NC London (94%) than in East Kent (78%, with 16% either disagreeing or strongly disagreeing). It is possible that a number of factors (discussed in Chapter 4) may have contributed to this, including signal strength and coverage, image/sound quality, responsiveness of stroke clinicians, and training. In the following sections, we present ambulance clinicians’ views on all these potential contributing factors.
FIGURE 6.
Proportion of respondents who felt prehospital triage was easy to use. Baseline, N = 233 (LAS, n = 159; SECAmb, n = 74).
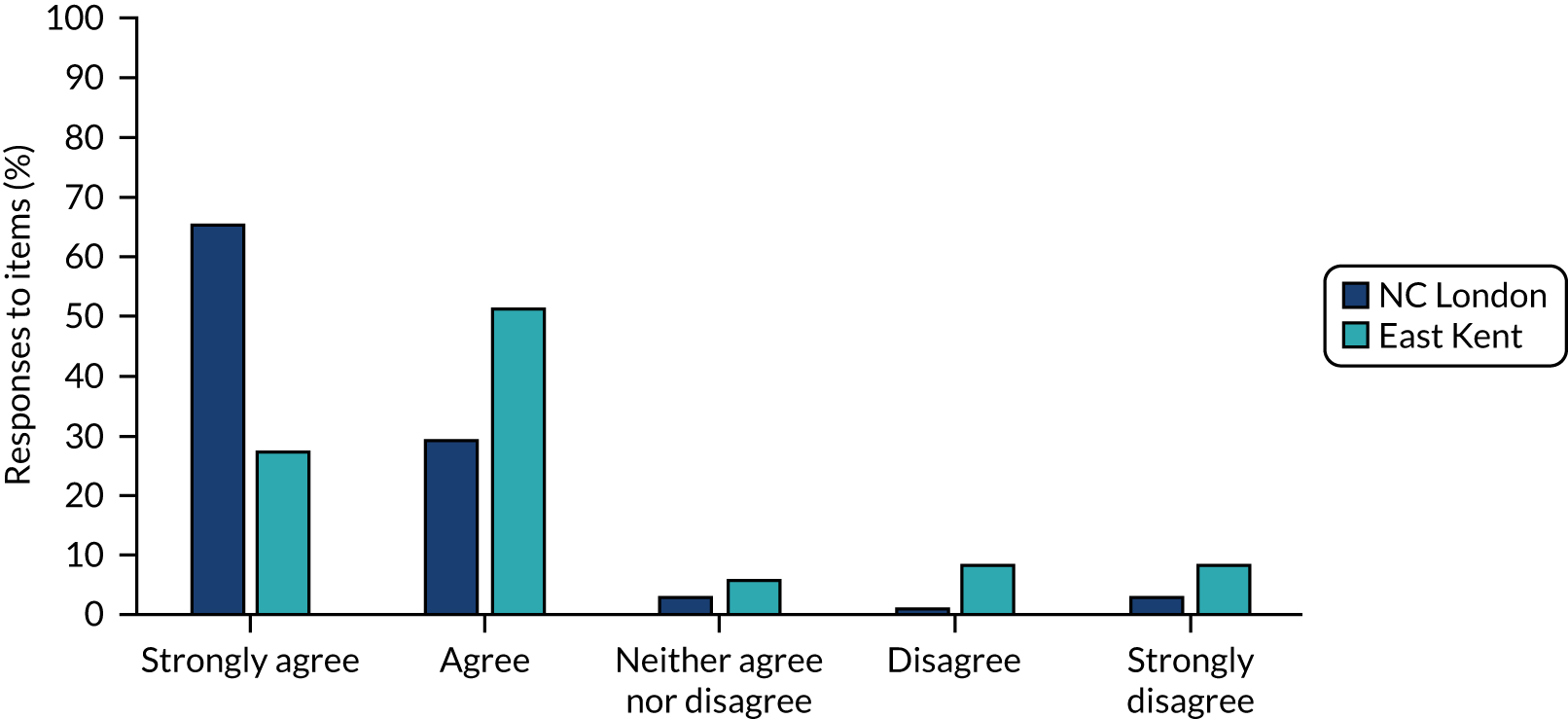
Technical performance of prehospital video triage
The majority of respondents across both regions (77%) found the sound and video quality sufficient for the task of remote triaging suspected stroke patients. The pattern of responses in NC London and East Kent differed significantly [χ2(3, N = 233) = 17.48; p < 0.01]: the level of agreement was higher in NC London (84%) than in East Kent (62%). Where technical problems had been encountered (see Appendix 1, Table 12), the most common issue reported among all respondents was poor sound quality, followed by calls not being answered. In NC London, 37.7% of respondents reported no issues with the system, while in East Kent 18.9% reported no issues.
Thematic analysis of 22 ‘other’ text comments indicated system performance issues centred around three main areas:
-
lack of signal/connectivity (e.g. unable to connect to FaceTime application and poor video and sound)
-
background noise (at the HASU end)
-
iPad device tricky for some older patients to engage with (e.g. those with dementia).
Responsiveness of stroke teams
The majority of all respondents (91%) reported that their call was answered by a stroke clinician after one or two attempts. However, the pattern of responses in NC London and East Kent differed significantly [χ2(3, N = 233) = 33.02; p < 0.01], with 98% of NC London respondents requiring one or two attempts, while 77% of East Kent respondents required one or two attempts, and 23% of East Kent respondents required more attempts (Figure 7). When asked what they did in instances where they did not receive an immediate response from a stroke doctor, the majority of respondents in both areas (overall 54%) suggested that they would attempt contact up to two times, then revert to the standard patient conveyance procedure. A minority in both areas (6.9% in NC London and 18.9% in East Kent) reported that they would keep trying until the call was picked up.
FIGURE 7.
Number of attempts to have call answered by a hospital stroke team. Baseline, N = 233 (LAS, n = 159; SECAmb, n = 74).
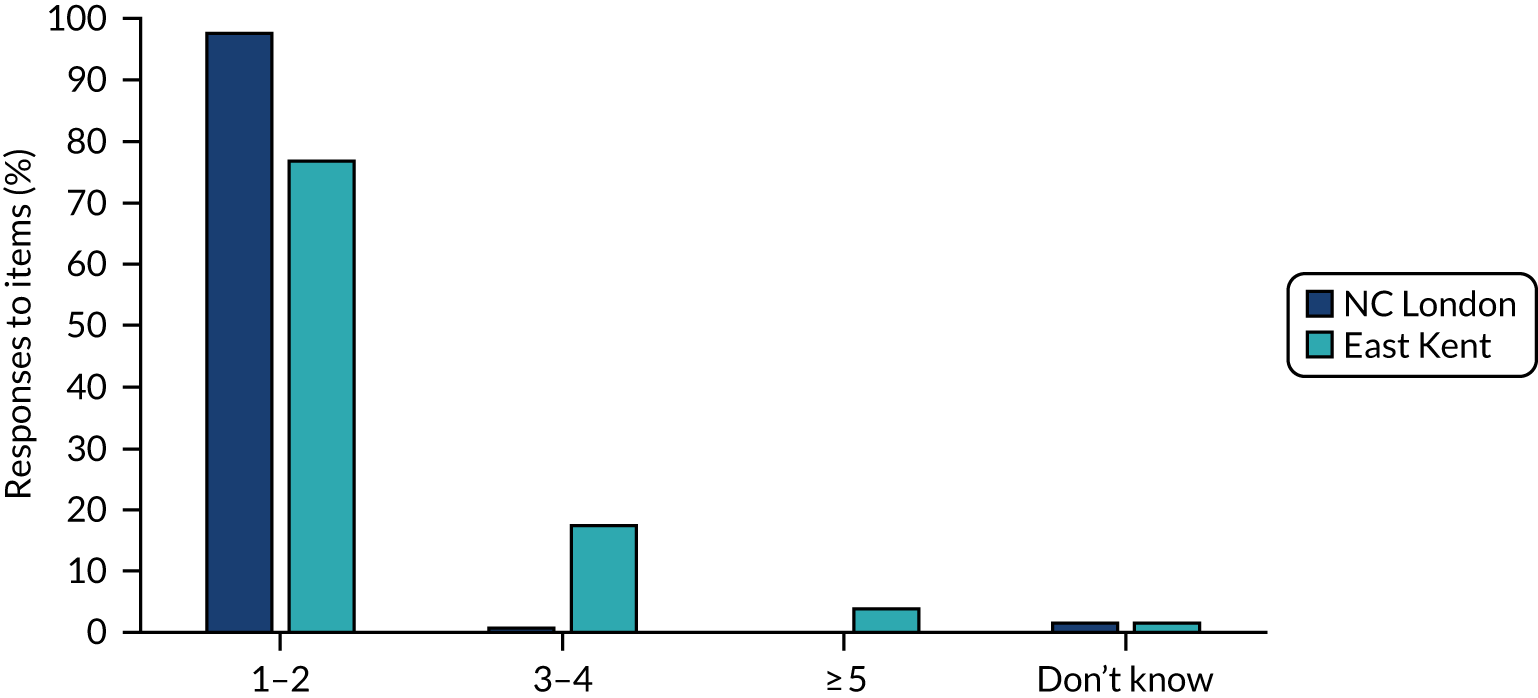
Free text responses were provided by the 24% who responded ‘other’. Many used this to report that calls were picked up straight way or that respondents had not encountered any issues (e.g. ‘Always had response’ and ‘We have been rung back almost immediately’). Others described reverting to the usual conveyance process, for example if the patient was FAST positive (e.g. ‘Depending on how critical or how obvious the stroke is I will only try a maximum of twice before conveying’).
Influence on conveyance decisions
A majority of respondents reported that triage influenced decisions about where to convey patients (e.g. convey to HASU or local ED, referral to TIA service, or remain at home) infrequently: this suggests that prehospital video triage tends to confirm initial stroke-related assessments by ambulance clinicians based on FAST. However, the pattern of responses in NC London and East Kent differed significantly [χ2(3, N = 233) = 8.72; p < 0.05]: Figure 8 suggests that a larger proportion of NC London respondents reported that prehospital video triage influenced decisions frequently, while a larger proportion of East Kent respondents felt prehospital video triage never influenced their decisions.
FIGURE 8.
Frequency that respondents felt prehospital video triage influenced conveyance decisions. Baseline, N = 233 (LAS, n = 159; SECAmb, n = 74).

Impact on patient safety
A clear majority of respondents had no concerns about the safety of prehospital video triage. However, the pattern of responses in NC London and East Kent differed significantly [χ2(3, N = 233) = 30.48; p < 0.01]: Figure 9 shows that 91% of NC London respondents reported no concerns about safety, compared with 62% in East Kent. This suggests that more ambulance clinicians in East Kent than in NC London had concerns about the safety of prehospital video triage.
Thematic analysis of 35 free-text responses submitted alongside this question highlighted four overlapping safety concerns. Below, we provide quotations to illustrate each theme.
FIGURE 9.
Proportion of respondents who had concerns about patient safety. Baseline, N = 233 (LAS, n = 159; SECAmb, n = 74).
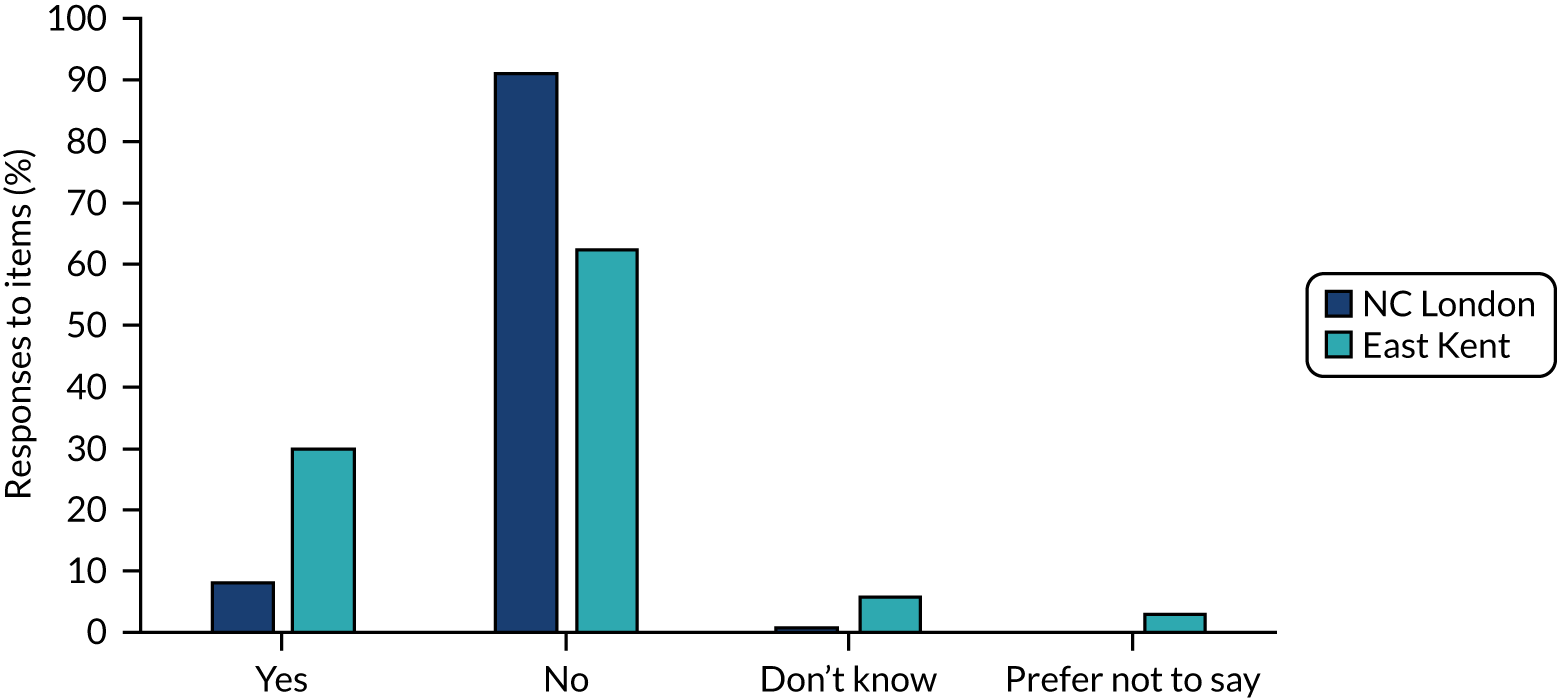
First, ambulance clinicians noted concerns about delays to treatment, either through time spent on scene or through inappropriate decisions:
Occasionally the person who answers will not listen to a handover or look at the pt [sic – ‘patient’] and will make a decision that is not suitable. This leads to pts [sic] being conveyed to inappropriate hospitals and then delaying treatment.
Ambulance clinician, East Kent
My concern is that conveyance is delayed in order to make the call therefore shortening the window for treatment.
Ambulance clinician, East Kent
I feel sometimes this could delay patient care, time is brain after all.
Ambulance clinician, NC London
The process hinders efficient conveyance, the line is hard to hear, it questions our judgement as clinicians.
Ambulance clinician, East Kent
Second, ambulance clinicians raised concerns about misdiagnosis or suboptimal clinical assessment (especially where a paramedic and neurologist may disagree):
Sometimes it can be very hard to handover the patient via FaceTime, and I feel on only a couple of occasions doctors have disregarded a patient I have felt has clearly been a stroke positive.
Ambulance clinician, East Kent
Missed diagnosis of stroke. Dismissive attitude of consultants towards paramedics. Dangerous practice of some doctors saying it is a TIA with ongoing stroke symptoms.
Ambulance clinician, East Kent
Third, a small number of comments were made about stroke clinicians having a ‘dismissive’ or ‘unfriendly’ response on calls with ambulance clinicians:
Some doctors do not trust clinicians or are quick to dismiss symptoms such as grip strength imbalance.
Ambulance clinician, East Kent
Very occasional but I have had occasions where I thought the team were dismissive of the possibility of a stroke and told us to convey to the nearest [hospital].
Ambulance clinician, NC London
Respondents also provided some reflections on how ambulance clinicians could revert to standard approaches if prehospital video triage did not work, and that positive interactions with stroke clinicians also took place:
This system only adds to our options. If for some reason the call is not successful, we can still continue as we did prior to the systems [sic] introduction.
Ambulance clinician, NC London
The HASU team have been able to speak and see the patient and any concerns are discussed in handover.
Ambulance clinician, NC London
Sufficiency of training
As noted in Chapters 3 and 4, training is a potentially important component of implementing and disseminating a new way of working. However, the pattern of responses suggests significantly different perceptions of training in NC London and East Kent [χ2(3, N = 233) = 66.54; p < 0.01]: Figure 10 shows that 91% of NC London respondents reported that they felt they had received enough training, whereas in East Kent only 42% reported that they had received enough training and 47% of ambulance clinicians in East Kent felt that they had not received enough training.
FIGURE 10.
Proportion of respondents who felt they had received sufficient training. Baseline, N = 233 (LAS, n = 159; SECAmb, n = 74).
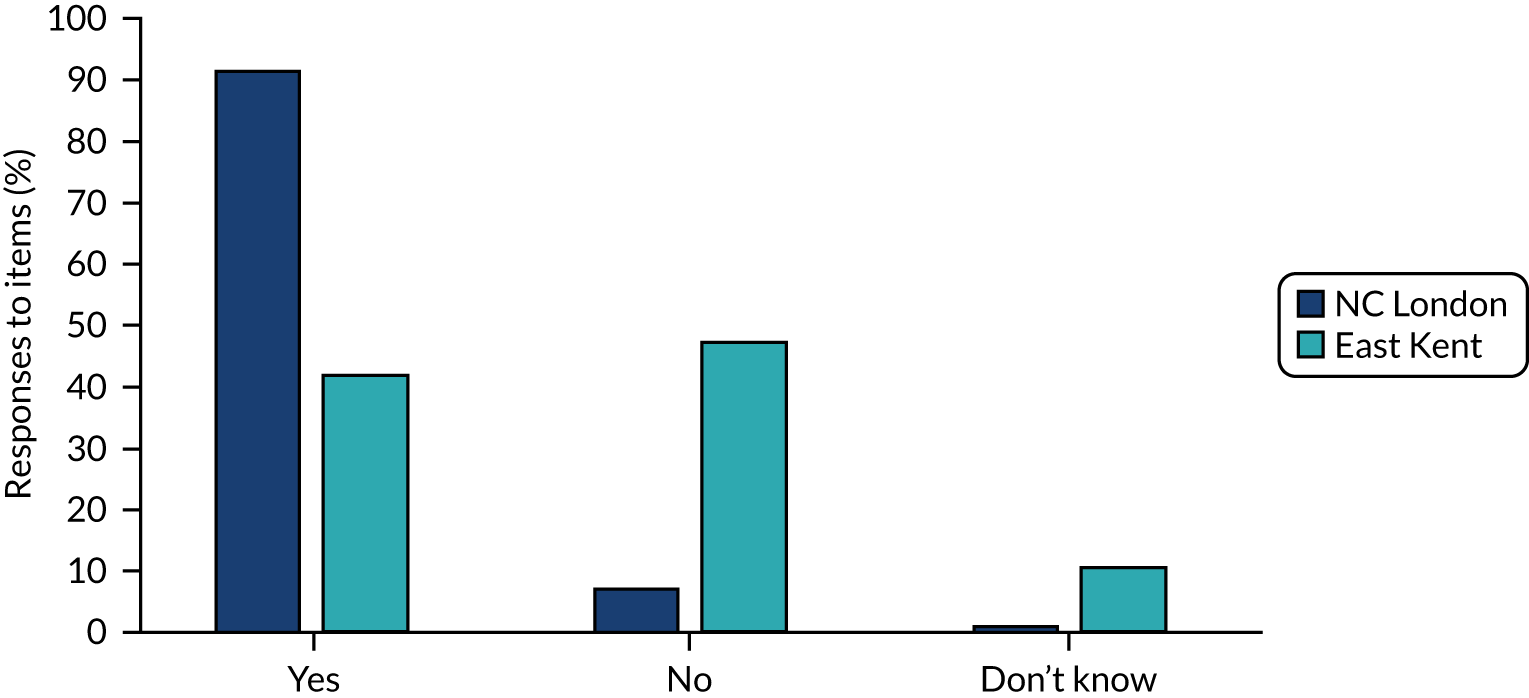
Free-text responses provided by ambulance clinicians who indicated that they had not received training suggested that, although some staff found the system intuitive to use (thus perhaps not feeling a need for training), not all did. Respondents identified several topics for training, which included finding and accessing FaceTime and what to do when calls are not answered. They also wanted greater clarity on the handover process and decision-making, including stroke clinician expectations and decisions to leave a patient at home or convey to a local ED (as opposed to a HASU) when a patient appears to be FAST-positive. Respondents also noted that stroke clinicians might benefit from training to increase their awareness of ambulance clinicians’ knowledge and skills.
As noted above, most concerns about training were raised by ambulance clinicians in East Kent. Many of the topics identified above are in fact covered in the flow charts on SECAmb’s NHS Service Finder portal, which is provided through NHS Digital and offers ambulance clinicians access to key decision-making and service provision information. That many clinicians remained unaware of this information suggests that more active approaches to dissemination and training on prehospital video triage would be valued by clinicians. For example, further free-text responses indicated clinician preferences for in-person or online delivery of training, whereas others indicated that a team leader should deliver the training.
Future use and development of prehospital video triage
The majority of all respondents (86%) agreed or strongly agreed with the statement that overall, the new telemedicine triage system was an improvement on the previous triage process for suspected stroke patients. However, the pattern of responses in NC London and East Kent differed significantly [χ2(3, N = 233) = 40.49; p < 0.01], with 94% of NC London respondents stating the new system was an improvement but only 68% of East Kent respondents doing so (see Appendix 1, Table 12).
Similarly, the majority of respondents thought that prehospital video triage should continue. However, the pattern of responses in NC London and East Kent differed significantly [χ2(3, N = 233) = 32.86; p < 0.01]: Figure 11 suggests that support for continuation was felt more strongly by ambulance clinicians in NC London (96%) than in East Kent (70%), with 13.5% of East Kent respondents indicating that the service would require improvements if it were to continue.
FIGURE 11.
Proportion of respondents who felt prehospital video triage should continue. Baseline, N = 233 (LAS, n = 159; SECAmb, n = 74).
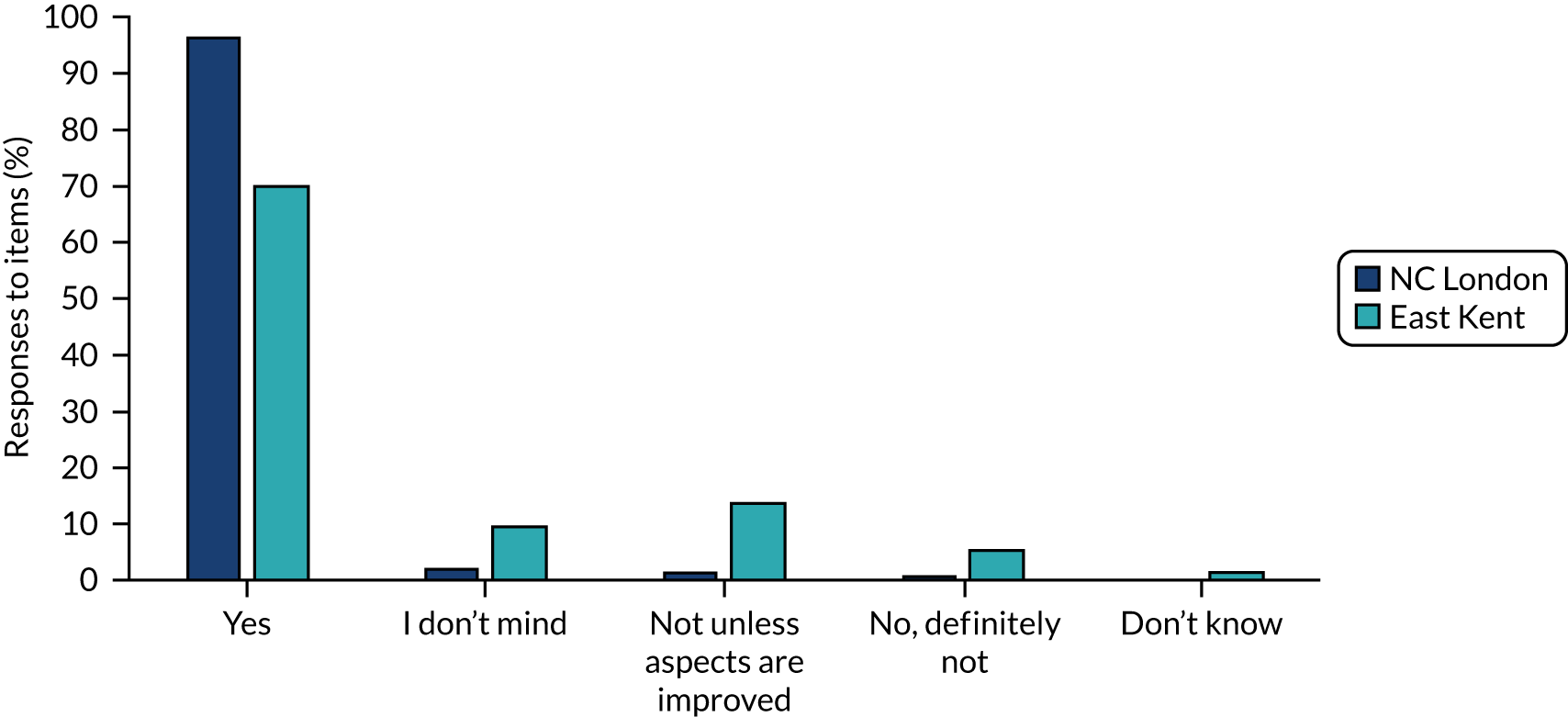
In relation to prehospital video triage’s potential use in other areas [e.g. myocardial infarction triage and sharing electrocardiogram (ECG) readings], there was a significantly different pattern of responses in NC London and East Kent [χ2(3, N = 233) = 41.15; p < 0.01]: while 79.9% of NC London respondents supported its use in other clinical contexts, only 39.2% of East Kent respondents were supportive (see Appendix 1, Table 12).
Below we provide a sample of free-text comments from respondents when asked if they would like prehospital video triage to continue in their region. Their tone reflects the generally positive view presented in the survey responses:
This is a very safe system, with highly experienced specialist neurologists directly impacting and improving patient care and outcomes, not only with strokes but with some more complex neurological cases.
Ambulance clinician, NC London
I think that this is a valuable tool to assist clinicians in their decision making. It is less stressful knowing that when in doubt we do have a specialised line that we can call for a second opinion.
Ambulance clinician, NC London
Used it yesterday, managed to leave a severely frail patient at an appropriate rehab facility following a likely TIA with the help of the consultant on the call. Really in-depth assessment.
Ambulance clinician, East Kent
I think it is helping our patients drastically.
Ambulance clinician, NC London
My concern, is that less subtle signs of CVA [cerebrovascular accident] are being missed e.g. for posterior CVA. And therefore, the pt [sic] is not being treated in a timely manner.
Ambulance clinician, East Kent
When it works it works well. I believe it would be better to have the stroke teams at all A&E to avoid misdiagnosis and delayed management.
Ambulance clinician, East Kent
Discussion
Principal findings
Our survey of ambulance clinicians in NC London and East Kent found broad acceptance and good usability for the new triage system overall. However, a common pattern throughout survey responses was that although both areas were broadly supportive, ambulance clinicians in NC London were more positive about prehospital video triage than ambulance clinicians in East Kent.
Considering usability and acceptability of prehospital video triage, a higher proportion of ambulance clinicians in NC London found prehospital video triage to be usable than in East Kent. This was paralleled – and perhaps partly explained – by NC London clinicians being more likely to report reliable technical performance, including audio and visual signals. Underlying this may be stronger and more reliable internet/Wi-Fi connections in NC London than in East Kent.
Ambulance clinicians reported differing impacts of prehospital video triage in NC London and East Kent. Respondents in both areas reported mainly that prehospital video triage influenced conveyance decisions infrequently. This potentially reflects our qualitative analysis (see Chapter 4) which suggested that triage often confirms ambulance clinicians’ initial stroke-related assessments and provides clinicians with a degree of reassurance and confidence about their decisions. In contrast, ambulance clinicians in NC London and East Kent diverged in their views of prehospital video triage’s impact on patient safety, with NC London clinicians clearly more confident about its safety than those in East Kent. Particular concerns raised included delays owing to the time taken to conduct the remote triage assessment and the potential for misdiagnosis and thus inappropriate conveyance.
In terms of implementation and dissemination of prehospital video triage, we found that ambulance clinicians in NC London were clearly more satisfied that they had received sufficient training. This may reflect our qualitative findings (Chapter 4), which indicated that NC London took a more active approach to training, employing in-person and online approaches, whereas East Kent’s approach was more passive, sharing information through e-mail and established online resources.
Turning to future use and development of the services, most ambulance clinicians in both areas felt prehospital video triage was an improvement on what had gone before it, and were supportive of its continued use in future. However, perhaps reflecting the previously mentioned points on usability and safety, these views were more pronounced among ambulance clinicians in NC London than in East Kent.
Strengths and weaknesses
This survey was a valuable opportunity to collect individual perspectives from ambulance clinicians across NC London and East Kent at scale, using a survey tool codesigned with stroke and ambulance clinicians. In addition, this analysis complemented our qualitative analysis (see Chapter 4) by providing further ambulance clinician perspectives on such central issues as usability, acceptability and training.
There were several limitations. First, our analysis was based on a convenience sample (although we asked respondents to confirm that they had used prehospital video triage). Second, to promote ease of use and rapid distribution, the survey was not distributed with a unique invitation link or password; therefore, it is possible that people submitted more than one completed response. This means that there are limits to the extent to which findings can be generalised to other ambulance clinicians and services piloting such systems nationally. There were also variable response rates across the two regions, resulting in a higher level of representation from LAS than SECAmb.
Comparison with other studies
To our knowledge (see Chapter 3), research on prehospital video triage for stroke (and associated interventions) has predominantly focused on single approaches to delivering such services; furthermore, the bulk of past research has relied on simulation methods. By surveying a large number of ambulance clinicians in two areas that have implemented prehospital video triage in different ways, we provide a substantial data set reflecting clinicians’ experiences of ‘real-world’ implementation and delivery of these services.
Given that research suggests that diagnosing stroke is important but potentially challenging in the prehospital environment,15,16,100 this may explain why many staff responded so positively overall to the introduction of the new triage system. In connection with this, our survey demonstrated that ambulance clinicians overall value the contribution of prehospital video triage in the context of the COVID-19 pandemic. 93
Our survey confirmed findings in the literature on telemedicine in ambulances concerning technical issues with bandwidth, audio and video quality. 13,16,48,93 Furthermore, it confirmed recent simulation research suggesting background noise in stroke clinicians’ environment might be influential. 66
As noted in Chapter 3, very little research has been conducted on the safety of prehospital video triage. 16 Our findings suggest that the perceived safety of similar prehospital video triage services may vary as a result of other factors that have been analysed heavily (for example audio-visual quality).
Previous research on prehospital video triage (and associated interventions) has noted that training may be required to support delivery of such services. 59,62,65,79 Our findings on ambulance clinician perceptions of the training they received suggested that more active approaches to training may make a difference, with more active approaches (as used in NC London) preferred by clinicians.
Implications
Ambulance clinicians overall found prehospital video triage usable and acceptable; furthermore, they considered it an improvement on previous arrangements for prehospital assessment of stroke and wanted it to continue to be used in future. However, NC London clinicians reported these positive views more strongly than East Kent ambulance clinicians. A number of contrasts between the areas might help explain these differences in views. In particular, ambulance clinicians in NC London were more likely to report stable audio-visual signals and high responsiveness of stroke clinicians; furthermore, they were much more likely to report feeling that they had received sufficient training. Finally, NC London ambulance clinicians were less likely to report feeling concerned about the safety of prehospital video triage. Throughout, survey responses identified issues that planners and service leaders might think about if they plan to implement prehospital video triage sustainably in these and other contexts. Key considerations include stable internet/Wi-Fi coverage to support a suitable audio-visual signal, high responsiveness from stroke clinicians in addressing triage calls and sufficient training to ensure that ambulance clinicians are confident in using the services.
Chapter 6 Impact of prehospital video triage on ambulance conveyance and clinical interventions
Overview
What was already known?
-
There is a small but growing evidence base on the impact of prehospital video triage for stroke on delivery of care.
-
Some evidence suggests that prehospital video triage may improve access to key interventions (e.g. a timely brain scan and thrombolysis).
-
There is little evidence on the safety of prehospital video triage for suspected stroke.
What this chapter adds
-
We analysed locally collected ambulance conveyance data for ambulance journeys over the period April–September 2020 (n = 1400). Our analysis demonstrated that, of the patients who underwent prehospital video triage, 39.1% in NC London and 51% in East Kent were transferred to the local HASU. Over 95% of stroke patients conveyed to a HASU arrived within recommended time thresholds in both NC London and East Kent.
-
National stroke data reporting time from symptom onset to arrival at hospital and stroke services suggested that, despite additional time spent on scene, prehospital video triage was delivered while supporting timely patient conveyance.
-
We analysed data for stroke patients submitted to the national stroke audit for the July–December periods of 2018, 2019 and 2020 (n = 137,650). Our DiD analysis suggested that, in both areas, delivery of important stroke clinical interventions (time to brain scan, stroke unit, thrombolysis and swallow screen) either improved significantly or did not change following introduction of prehospital video triage (relative to changes in RoE). These effects may be explained in part by other stroke service changes that took place concurrently in the studied areas.
-
Our findings suggest that prehospital and acute stroke care in NC London and East Kent, supported by prehospital video triage, either improved or was sustained during a time of extreme system stress.
Background
Timely access to specialist stroke care and treatments such as thrombolysis is associated with better stroke patient outcomes and may be more cost-effective. 4,102–105 Therefore, timely conveyance to an appropriate service and timely delivery of clinical interventions are critical components of care.
The prehospital video triage services introduced in NC London and East Kent aimed to establish whether a patient is suitable for conveyance to stroke services or should be on a different care pathway. Prehospital video triage has the potential to ensure that stroke patients are conveyed appropriately to a specialist stroke unit and that stroke teams are prepared to deliver clinical interventions associated with improved outcomes upon arrival. However, alongside these potential benefits there was the risk of increasing patient journey times, which may be seen as a risk to patient safety.
This chapter aims to address the question ‘Did the digital prehospital video triage services in NC London and East Kent support appropriate, safe conveyance and treatment of suspected stroke patients?’. The analysis addressed the following questions:
-
What proportion of patients in NC London and East Kent who underwent prehospital video triage were conveyed to stroke and other services, or discharged at home?
-
Did suspected stroke patients in NC London and East Kent reach stroke services within recommended timings?
-
Did stroke patients in NC London and East Kent receive clinical interventions within recommended timings?
Method
Setting
As outlined in Chapter 1, during the early stages of the COVID-19 pandemic, alongside the introduction of prehospital video triage there were other changes to how services were organised in NC London and East Kent. Notably, the location(s) of stroke services operating as HASUs changed: in NC London, the HASU relocated from the UCLH main hospital site to Queen Square. In East Kent, stroke services at William Harvey Hospital and QEQM hospital stopped admitting stroke patients routinely and the new Kent and Canterbury Hospital (K&CH) HASU opened.
Data
We analysed two data sources, summarised in Table 5:
-
Ambulance conveyance data: patient-level data routinely collected by ambulance services for suspected stroke patients in NC London and East Kent, for the period April–September 2020.
-
Stroke national audit data: publicly available, team-level clinical audit data from SSNAP for the period July 2018–December 2020.
| Data source | Regions | Time periods | Measures |
|---|---|---|---|
| Local ambulance |
NC London East Kent |
April–September 2020 |
|
| SSNAP |
NC London East Kent RoE |
July–September 2018a October–December 2018a July–September 2019a October–December 2019a July–September 2020 October–December 2020 |
Time from symptom onset to:
|
The ambulance journey data recorded patient destination and conveyance time. These patient-level data were provided by our collaborating ambulance services, and covered the period April–September 2020, that is, the period immediately following introduction of prehospital video triage. The absence of data covering pre-implementation in NC London and East Kent and conveyance in areas that had not introduced prehospital video triage limited the extent to which we could analyse the impact of prehospital video triage on ambulance journeys.
The SSNAP data were analysed separately from the ambulance data and used to analyse delivery of key clinical interventions for stroke patients before and after the introduction of prehospital video triage. These data were available in the form of quarterly reports. At the time of analysis, two ‘quarters’ covering the period following implementation of prehospital video triage were available: July–September 2020 and October–December 2020. As a pre-implementation comparator, we analysed the July–September and October–December quarters for 2018 and 2019 (these quarters were selected to minimise the influence of seasonal variations). We used RoE as a regional comparator.
Analysis: patient destination
To understand effects on patient destination, we analysed the proportion of patients undergoing prehospital video triage who were then conveyed to HASUs (which admit stroke patients routinely) and other services in NC London and East Kent.
First, we analysed local ambulance data descriptively, calculating the proportion of patients conveyed to HASUs and other services in NC London and East Kent. We also analysed SSNAP data on the proportion of stroke patients being treated by HASUs and non-routinely-admitting teams (which generally provide ongoing hospital-based stroke rehabilitation stroke care for patients, following transfer from the local HASU, but may also provide care to late-presenting stroke patients who are no longer eligible for HASU care).
In addition, we analysed SSNAP data using a between-region DiD regression analysis to analyse whether the proportions of patients admitted to HASU and non-routinely-admitting teams changed over time in NC London and East Kent relative to the changes over time in RoE (see explanation in Chapter 2, Difference-in-differences regression).
Analysis: timely transfer of stroke patients to stroke services
To understand whether stroke patients were transferred to HASUs in a timely fashion, we analysed local ambulance data to assess whether patients who were conveyed to HASUs arrived within recommended time thresholds. The National Stroke Configuration Guidance recommends that journey times in urban areas should be ideally 30 minutes but no more than 60 minutes. 30 In the absence of regional or historic comparators, we present only descriptive results for this period of time, comparing journey times against these thresholds.
In addition, we examined SSNAP data reporting median time from symptom onset to arrival at hospital and arrival at a HASU, in NC London, East Kent, and RoE, before and after the introduction of prehospital video triage. Because these public data only presented median times, we were unable to combine quarterly data or conduct any formal data analysis.
Analysis: timely delivery of clinical interventions
National guidance for stroke recommends that stroke patients should undergo a range of interventions upon arrival at hospital, including brain imaging, swallow screening, and assessment by stroke specialists. 106 We analysed SSNAP data to examine whether or not delivery of such interventions changed in the period following the introduction of prehospital video triage services in NC London and East Kent relative to RoE.
To understand changes in delivery of clinical intervention over time, we used a between-region DiD regression analysis, comparing the changes over time in NC London and East Kent with the change over time in RoE (see explanation in Chapter 2, Difference-in-differences regression). Patient characteristics were included separately in the estimations (as the small number of hospitals did not permit inclusion of more predictors than cases): these are reported as a robustness check in Appendix 1, Table 15. A statistically significant DiD estimator in this case would confirm the difference in effect over time between the compared regions. Delivery of interventions analysed was timed relative to ‘clock start’, which refers to the point when patients arrived at hospital services, and were as follows:107
-
proportion of stroke patients directly admitted to a stroke unit within 4 hours of clock start
-
proportion of stroke patients scanned within 1 hour of clock start
-
proportion of stroke patients given thrombolysis
-
proportion of stroke patients assessed by a stroke specialist.
Results
We organised our data analysis in two main parts. First, we present our analysis of ambulance conveyance data, to assess (1) the proportion of patients taken to HASUs or non-routinely admitting teams, or discharged at home; and (2) the proportion of suspected stroke patients who reached HASUs within recommended time thresholds following introduction of prehospital video triage. Second, we present our analysis of SSNAP data, assessing delivery of stroke clinical interventions before and after the introduction of prehospital video triage.
Destinations of patients who underwent prehospital video triage
This section presents our analysis of ambulance patient destination data for NC London and East Kent. We found that, following introduction of prehospital video triage, a substantial proportion of suspected stroke patients who may traditionally have been conveyed to a HASU were instead (following specialist assessment) referred to alternative acute services (e.g. a local ED) or recommended to stay home.
Table 6 presents local ambulance data for the period April–September 2020, covering 929 patients in NC London and 471 patients in East Kent who underwent prehospital video triage. From these patients, 181 (19.5%) in NC London and 61 (13.0%) in East Kent were not conveyed. It is important to note that the data included all calls for patients who underwent prehospital video triage – that is, including patients who were initially suspected of having stroke, but many of whom were assessed and found likely not to be having stroke.
| Hospital name | HASU/non-HASU | Time from 999 call to arrival at hospital (minutes), median (IQR) | Time from scene to arrival at hospital (minutes), median (IQR) | Number of patients | Proportion of the total (%) |
|---|---|---|---|---|---|
| NC London | |||||
| National, Queen Square HASU | HASU | 87.3 (35.4) | 29.7 (17.3) | 338 | 36.4 |
| Northwick Park HASU | HASUa | 73.1 (43.3) | 16.3 (17.0) | 11 | 1.2 |
| Royal London (Whitechapel) HASU | HASUa | 74.2 (22.2) | 23.3 (14.8) | 11 | 1.2 |
| Other HASU | HASUa | 65.9 (12.3) | 14.5 (3.8) | 3 | 0.3 |
| North Middlesex | Non-HASU | 84.2 (33.2) | 13.3 (8.2) | 125 | 13.5 |
| Barnet | Non-HASU | 78.7 (30.9) | 14.6 (6.9) | 62 | 6.7 |
| Whittington | Non-HASU | 86.8 (46.1) | 13.8 (7.9) | 46 | 5.0 |
| University College Hospital ED | Non-HASU | 91.1 (34.4) | 17.6 (13.9) | 41 | 4.4 |
| Royal Free | Non-HASU | 89.0 (32.4) | 14.7 (11.4) | 40 | 4.3 |
| Northwick Park | Non-HASU | 73.8 (21.8) | 17.6 (8.1) | 11 | 1.2 |
| Whipps Cross | Non-HASU | 79.5 (31.1) | 13.4 (9.0) | 10 | 1.1 |
| Other hospital – non-HASU | Non-HASU | 78.9 (38.2) | 14.7 (12.1) | 50 | 5.4 |
| Not conveyed | – | – (–) | – (–) | 181 | 19.5 |
| Total | – | 84.6 (34.8) | 20.2 (17.6) | 929 | |
| East Kent | |||||
| Kent and Canterbury HASU | HASU | 58.8 (31.3) | 24.3 (10.8) | 239 | 50.7 |
| Darent Valley Hospital | HASUa | 55.5 (–) | 15.1 (–) | 1 | 0.2 |
| Maidstone Hospital | HASUa | 73.3 (–) | 64.1 (–) | 1 | 0.2 |
| QEQM | Non-HASU | 64.2 (33.5) | 24.2 (22.6) | 85 | 18.0 |
| William Harvey Hospital | Non-HASU | 81.1 (34.3) | 24.6 (11.5) | 82 | 17.4 |
| Tunbridge Wells Hospital | Non-HASU | 53.8 (–) | 17.5 (–) | 1 | 0.2 |
| Medway Maritime Hospital | Non-HASU | 257.9 (–) | 20.1 (–) | 1 | 0.2 |
| Not conveyed | – | – (–) | – (–) | 61 | 13.0 |
| Total | – | 63.3 (34.7) | 24.3 (13.3) | 471 | |
Our analysis shows that in NC London during the observed period the National Queen Square HASU was a major destination, with 338 patients (36.4% of the total) conveyed there. A small proportion of patients was conveyed to neighbouring HASUs (with Northwick Park HASU and Royal London HASU each admitting 1.2%). The median time from the 999/111 call to the ambulance reaching the hospital for all patients was 84.6 minutes [interquartile range (IQR) 34.8] and the median time from scene to patient arriving at the hospital was 20.2 minutes (IQR 17.6).
In East Kent, most patients were conveyed to K&CH HASU (50.7%), while a smaller proportion was conveyed to QEQM (85 patients, 18%) and William Harvey Hospital (82 patients, 17.4%). The median time from the 999/111 call until the ambulance reached hospital for all cases was 63.3 minutes (IQR 34.7) and the median time from leaving scene to patient arriving at the hospital was 24.3 minutes (IQR 13.3).
Overall, our data show that a large proportion of the triaged patients in both NC London and East Kent was sent to non-HASU services. As noted in Chapter 4, there were very few cases where patients who were transferred to non-HASU services turned out to have had a stroke.
Proportion of stroke patients directly admitted to a hyper-acute stroke unit
An aim of prehospital video triage was to ensure appropriate patient destination. This section presents our analysis of SSNAP data (covering 137,650 stroke patients) to examine the proportion of stroke patients directly admitted to HASUs and non-HASUs before and after the introduction of prehospital video triage.
Table 7 suggests that in NC London the number of stroke patients admitted to a HASU was smaller in 2020 than in 2019, but comparable to 2018. For comparative purposes, the numbers of routinely admitted patients at a national level did not vary substantially during the same periods (see Table 7). The proportion of admissions to non-HASUs in NC London was higher in 2020 (10.6%) than in 2019 (7%), but again similar to 2018 (9.2%); in 2020, non-HASU admissions were highly localised around one SU (Barnet).
| Teams | Admitting team | Patients admitted in 2018 (n) | Patients admitted in 2019 (n) | Patients admitted in 2020 (n) |
|---|---|---|---|---|
| NC London | ||||
| UCLH HASU | HASU | 681 | 753 | 667 |
| North Midd SUa | Non-HASU | 23 | 0 | 5 |
| Barnet SUa | Non-HASU | 19 | 26 | 52 |
| Royal Free Hospital SUa | Non-HASU | 26 | 30 | 22 |
| UCLH SUa | Non-HASU | 1 | 0 | 0 |
| Total | 750 | 809 | 746 | |
| East Kent | ||||
| QEQM Hospital | HASU then non-HASUb | 179 | 208 | 71 |
| William Harvey Hospital | HASU then non-HASUb | 234 | 282 | 100 |
| K&C HASU | HASU | – | – | 319 |
| K&CH | Non-HASU | 3 | 0 | 1 |
| Total | 416 | 490 | 491 | |
| RoE | ||||
| National routinely admitted teams | 43,666 | 44,579 | 44,003 | |
| National non-routinely admitted teams | 375 | 455 | 870 | |
In East Kent, the majority of patients were conveyed to the new K&CH HASU (65%). Despite stopping as routinely-admitting units, a proportion of stroke patients were still conveyed directly to QEQM (14.5%) and William Harvey (20%) following this change (Table 8). The changes in stroke patients directly admitted to a HASU before and after the pandemic were less clear in East Kent and this was possibly confounded by the fact that K&CH started as a HASU and replaced QEQM and William Harvey at the start of the pandemic.
| Measure | Median time to HASU (IQR) | Patients (n) | Proportion of patients |
|---|---|---|---|
| NC London | |||
| Leave scene-to-hospital less than 30 minutes | 22.1 (9.7) | 192 | 52.9% |
| Leave scene-to-hospital 30–45 minutes | 35.1 (6.8) | 108 | 29.8% |
| Leave scene-to-hospital 45–60 minutes | 51.2 (6.3) | 45 | 12.4% |
| Leave scene-to-hospital more than 60 minutes | 68.0 (18.3) | 18 | 5.0% |
| Total leave scene-to-hospital – NC London HASU | 29.2 (17.6) | 363 | |
| East Kent | |||
| Leave scene-to-hospital less than 30 minutes | 21.7 (7.9) | 177 | 74.1% |
| Leave scene-to-hospital 30–45 minutes | 34.2 (4.8) | 54 | 22.6% |
| Leave scene-to-hospital more than 45 minutes | 49.6 (4.1) | 8 | 3.3% |
| Total leave scene-to-hospital – East Kent HASU | 24.3 (10.8) | 239 | |
We used DiD regression analysis to compare trends in the numbers of patients admitted to HASUs and non-HASUs in NC London and East Kent relative to RoE before and after the introduction of prehospital video triage. Results showed that the number of patients admitted to non-routinely admitting teams decreased (p < 0.05) in these regions relative to RoE for the period July–December 2020 (see Appendix 1, Table 14).
Stroke patient conveyance times from scene of stroke to hospital
The majority of patients conveyed to a HASU had journeys that fell within nationally recommended time thresholds (see Table 7). In NC London, the median time from leaving scene to arrival at hospital was 29.2 minutes (IQR 17.6); 47.1% of the patients fell beyond the 30-minutes threshold and 5.0% of them fell beyond the 60-minutes threshold (see Table 7). In East Kent, the median time from leaving scene to arrival at hospital was 24.3 minutes (IQR 10.8); 25.9% of the patients fell beyond the 30-minutes threshold and only 3.3% of them fell beyond the 45-minutes threshold, with no patients arriving beyond the 60-minutes threshold. Locations of patients whose conveyance times exceeded thresholds are reported in Appendix 1, Table 13.
Time from stroke symptom onset to arrival at hospital and arrival at stroke unit
To examine whether prehospital video triage contributed to increased patient transfer times, we looked at SSNAP data on median time from stroke symptom onset to stroke patients’ arrival at hospital (Figure 12) and median time from stroke symptom onset to stroke patients’ arrival at a routinely admitting stroke unit or HASU (Figure 13). These data suggest that prehospital video triage in NC London and East Kent did not result in an increase in overall time from symptom onset to arrival at hospital or a HASU. In NC London, median times from symptom onset to arrival at hospital appeared slightly lower in July–December 2020 than they were in July–December 2018 and 2019; median times from symptom onset to arrival at a HASU were clearly lower in July–December 2020 than they were in July–December of 2018 and 2019. In East Kent, median times from symptom onset to arrival at hospital and arrival at a HASU in July–December 2020 appeared broadly consistent with median times in July–December of 2018 and 2019. Times for RoE for both measures appeared consistent over 2018, 2019 and 2020.
FIGURE 12.
Median time from stroke symptom onset to arrival at hospital in NC London, East Kent and RoE, July–December, 2018, 2019 and 2020.

FIGURE 13.
Median time from stroke symptom onset to arrival at stroke unit in NC London, East Kent and RoE, July–December, 2018, 2019 and 2020.
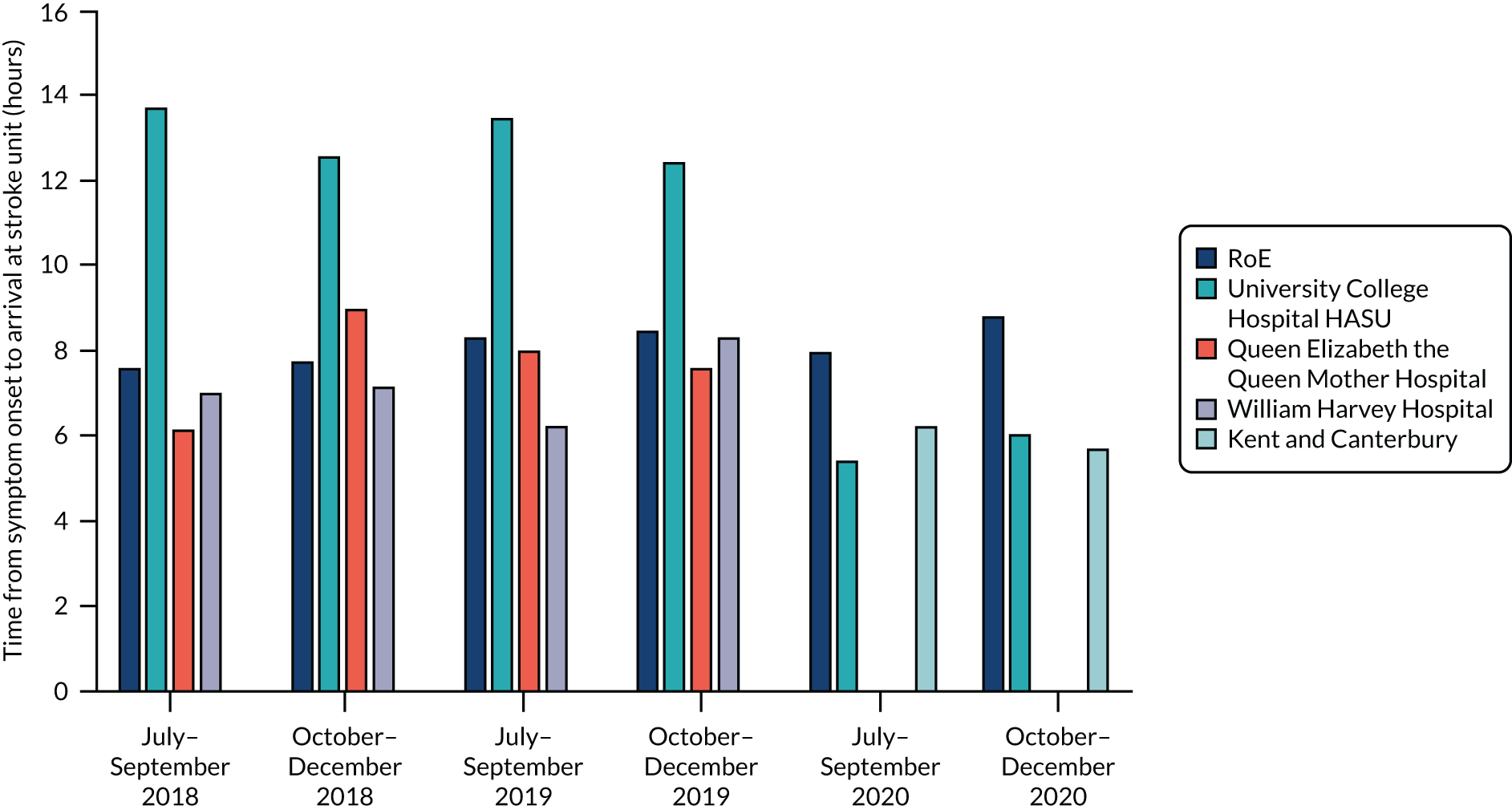
The numbers and characteristics of stroke patients treated by hyper acute stroke units
Table 9 presents our analysis of SSNAP data on the numbers and characteristics of patients treated by HASUs in NC London, East Kent and RoE for the period July–December from 2018 to 2020. These data help explain whether or not the characteristics of patients treated changed during the pandemic (e.g. whether or not only more severe strokes were being conveyed to a HASU). In addition, we used these characteristics as risk adjustments to assess whether or not these characteristics made any difference to the likelihood of receiving clinical intervention.
| Patient characteristic | Year 2018 (July–December) | Year 2019 (July–December) | Year 2020 (July–December) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| National (RoE) | NC London | East Kent | National (RoE) | NC London | East Kent | National (RoE) | NC London | East Kent | |
| Number of stroke patients | 43,211 | 663 | 411 | 44,772 | 747 | 486 | 43,822 | 615 | 315 |
| Female patients (%) | 47.9 | 45.2 | 52.5 | 47.9 | 42.5 | 48.1 | 46.9 | 41.0 | 47.8 |
| Age (median) | 76.5 | 74.0 | 78.0 | 76.5 | 74.0 | 76.6 | 76.0 | 72.5 | 77.0 |
| Type of stroke (%) | |||||||||
| Infarction | 87.4 | 97.9 | 91.1 | 87.3 | 86.1 | 90.1 | 87.5 | 87.4 | 93.7 |
| Primary intracerebral haemorrhage | 12.2 | 1.8 | 8.7 | 12.3 | 13.5 | 9.3 | 12.2 | 10.7 | 5.7 |
| NIHSS at arrival (median) | 4.6 | 4.5 | 5.6 | 4.6 | 4.5 | 5.8 | 4.4 | 4.0 | 5.5 |
| Comorbidities (%) | |||||||||
| 0 comorbidities | 26.2 | 23.2 | 26.5 | 25.9 | 23.4 | 29.4 | 26.7 | 25.7 | 37.3 |
| 1 comorbidity | 35.3 | 30.5 | 34.8 | 35.1 | 37.5 | 37.4 | 34.7 | 36.9 | 34.1 |
| 2 comorbidities | 26.3 | 30.1 | 26.2 | 26.5 | 26.7 | 24.6 | 25.9 | 26.1 | 20.0 |
| 3 comorbidities | 10.1 | 13.8 | 8.2 | 10.4 | 10.7 | 7.6 | 10.4 | 9.4 | 8.7 |
| 4 comorbidities | 1.9 | 2.5 | 4.4 | 1.9 | 1.8 | 0.7 | 2.0 | 1.9 | 0.0 |
| 5 comorbidities | 0.2 | 0.0 | 0.0 | 0.2 | 0.2 | 0.3 | 0.2 | 0.2 | 0.0 |
| Arrival by ambulance (%) | 79.4 | 91.5 | 85.1 | 77.3 | 94.4 | 83.9 | 79.9 | 95.8 | 89.1 |
Table 9 shows that the median age of stroke patients treated by HASU teams was higher for East Kent than NC London. This may be because East Kent’s population has a higher population age than NC London overall. 108 The demographic structure of the population may also explain why the proportion of female stroke patients in East Kent is higher (as, on average, female individuals live longer) than NC London. There were no clear trends in stroke type over time for NC London and East Kent, although both regions generally admitted a lower proportion of ischaemic stroke patients with infarction than RoE.
The NIHSS quantifies impairment caused by stroke. NIHSS status varied on average between four and six (the only exception being QEQM hospital in July–September 2018, which had an average of 7.5). The proportion of HASU-treated stroke patients with two or more comorbidities was higher for NC London than for East Kent and more comparable with RoE for all three compared years. The proportion of patients who were conveyed to a HASU by ambulance was generally higher for NC London than for East Kent.
Delivery of clinical interventions before and after the introduction of prehospital video triage
Using SSNAP, we analysed whether there were any changes in delivery of key stroke clinical interventions in NC London and East Kent HASUs relative to RoE before (July–December 2018 and 2019) and after (July–December 2020) the introduction of prehospital video triage. The changes before and after DiD estimators are presented in Table 10. As a robustness check we also included patient characteristics (including stroke type, sex, age, NIHSS and number of covariates) as covariates in our analyses; we report these separately in Appendix 1, Table 15.
| Measure | Region | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| RoE | NC London | East Kent | DiD | ||||||||
| Beforea | After | Difference | Beforea | After | Difference | Beforea | After | Difference | NC London minus RoE (SE) | East Kent minus RoE (SE) | |
| Number of stroke patients | 43,992 | 43,822 | –170 | 705 | 615 | –90 | 449 | 315 | –134 | – | – |
| Unadjusted outcomes,b % | |||||||||||
| Admitted to stroke unit (within 4 hours) | 57.45 | 53.80 | –3.65 | 58.35 | 97.80 | 39.45 | 43.30 | 80.60 | 37.30 | 43.10 (10.96) | 40.95* (5.58) |
| Brain scan (within 1 hour) | 54.60 | 54.80 | 0.20 | 57.90 | 60.80 | 2.90 | 59.25 | 82.60 | 23.35 | 2.70 (5.91) | 23.15* (5.65) |
| Thrombolysis, % | |||||||||||
| Given thrombolysis (all stroke types) | 11.65 | 10.50 | –1.15 | 14.60 | 9.20 | –5.40 | 14.15 | 16.50 | 2.35 | –4.25 (2.77) | 3.50 (2.17) |
| Eligible patients for thrombolysis | 11.30 | 10.30 | –1.00 | 14.05 | 8.90 | –5.15 | 14.20 | 19.00 | 4.80 | –4.15 (1.85) | 5.80 (3.31) |
| Eligible patients given thrombolysis | 88.80 | 87.10 | –1.70 | 89.55 | 88.50 | –1.05 | 73.25 | 64.30 | –8.95 | 0.65 (0.58) | –7.25* (1.56) |
| Thrombolysis (within 1 hour) | 61.60 | 59.60 | –2.00 | 85.40 | 81.60 | –3.80 | 40.95 | 60.70 | 19.75 | –1.80 (3.36) | 21.75 (2.77) |
| Assessed by a specialist, % | |||||||||||
| Assessed by stroke consultant (within 24 hours) | 84.35 | 84.70 | 0.35 | 87.45 | 95.20 | 7.75 | 67.25 | 100.00 | 32.75 | 7.4* (0.96) | 32.4** (1.48) |
| Assessed by stroke nurse (within 24 hours) | 91.15 | 90.70 | –0.45 | 94.85 | 98.10 | 3.25 | 84.20 | 100.00 | 15.80 | 3.7** (0.37) | 16.25** (1.58) |
| Given swallow screen (within 4 hours) | 75.45 | 74.60 | –0.85 | 78.55 | 98.00 | 19.45 | 67.20 | 97.90 | 30.70 | 20.30* (4.62) | 31.55** (2.51) |
The proportion of stroke patients admitted to a HASU within 4 hours (see Table 10) increased significantly relative to RoE in East Kent following introduction of prehospital video triage (40.95%, p < 0.05).
The proportion of patients receiving a brain scan within 1 hour (see Table 10) did not change significantly in NC London relative to RoE following introduction of prehospital video triage, but increased significantly in East Kent (23.15%, p < 0.05).
In terms of thrombolysis, we found no significant changes following implementation of prehospital video triage in NC London and East Kent relative to RoE for the proportion of stroke patients thrombolysed, stroke patients eligible for thrombolysis or patients thrombolysed within 1 hour (see Table 10). However, we found a significant reduction in the proportion of patients eligible for thrombolysis in East Kent following introduction of prehospital video triage (–7.25%, p < 0.05).
The proportion of patients assessed by a stroke physician within 24 hours of clock start (see Table 10) increased significantly relative to RoE in both NC London (7.4%, p < 0.05) and East Kent (32.4%, p < 0.001) following introduction of the prehospital video triage.
The proportion of patients assessed by a stroke nurse within 24 hours of clock start (see Table 10) increased significantly relative to RoE following introduction of prehospital video triage in both NC London (3.7%, p < 0.001) and East Kent (16.25%, p < 0.001).
The proportion of eligible patients who underwent a swallow screen within 4 hours (see Table 10) increased significantly relative to the rest of England in both NC London (20.30%, p < 0.05) and East Kent (31.55%, p < 0.001).
Robustness check
In addition, we analysed the effect of the different risk factors (age, sex, NIHSS, stroke type, having two or more comorbidities and arriving by ambulance) in a series of DiD regression analyses. The small number of teams did not permit inclusion of more predictors than cases, so we analysed the effect of the risk factors separately (see Appendix 1, Table 15). Only the DiD results are provided for each risk factor. The results showed that some DiD estimators became statistically significant when these risk factors were included. However, it is important to highlight that the direction of the effect remained the same and effect sizes remained similar.
Discussion
Principal findings
In this chapter, we aimed to analyse whether prehospital video triage supported appropriate and safe conveyance and treatment of suspected stroke patients. Our analysis of ambulance and SSNAP data on patient destinations found that (1) relatively few patients were being conveyed to HASUs outside the studied areas of NC London and East Kent; and (2) the number of stroke patients being treated in a HASU in NC London reduced somewhat in the early stages of the pandemic (results were unclear for East Kent because of the restructuring of the HASU services in this region). Although this suggests that the overwhelming majority of stroke patients were being conveyed to a HASU rather than their local ED, it reflects an observational analysis indicating a reduction in the number of milder stroke admissions from March through May 2020. 109 Likely contributing factors may include general reluctance of patients to attend hospital and clinical concerns about the safety of conveying patients between hospitals during the early stages of the COVID-19 pandemic.
The proportion of patients who arrived at a HASU by ambulance was higher for NC London than East Kent. In addition, a higher proportion of stroke patients was admitted to non-routinely admitting stroke units during the implementation period (i.e. 2020 data) in NC London, in East Kent, and at national level. Possible reasons for non-conveyance of strokes to the HASU need to be better explored but there may be several factors associated with this. First, during the time of analysis there were changes to stroke numbers reported nationally and locally because of the COVID-19 pandemic. These changes were mainly driven by the conservative management in local hospitals and nursing homes, patients presenting later or not at all, and the impact that the lockdowns and the pandemic had on the mobility of people in large metropolitan areas like London. 110 Second, some patients may have been conveyed to hospital by ambulance clinicians who were unaware of prehospital video triage service (e.g. private ambulance services). Third, some patients may have preferred to go to the nearest point of care (for example their local EDs). Finally, there may have been fewer interhospital ED to HASU transfers, primarily owing to factors associated with the COVID-19 pandemic, including clinician concerns about COVID-19 infection, ambulance capacity and availability of HASU beds.
Our analysis of ambulance conveyance times from scene of stroke to hospital found that the overwhelming majority of stroke patients reached stroke services within the recommended time thresholds. In addition, publicly reported median times from stroke symptom onset to stroke patients’ arrival at hospital and a HASU suggested that prehospital video triage did not result in increases in overall stroke patient conveyance times. These data suggest that prehospital video triage can be delivered while still supporting timely patient conveyance to stroke services. However, these patterns may in part have been facilitated by the relocation of HASUs in NC London and East Kent and reduced traffic during the pandemic.
Our analysis of clinical interventions over 2018–2020 found no evidence of significant reductions in delivery of key stroke clinical interventions (e.g. brain scan, admission to HASU and specialist assessments) in NC London and East Kent (relative to RoE). Rather, in several cases we found that the proportion of patients receiving timely interventions increased significantly (particularly in East Kent). This was despite the context of COVID-19, which placed unprecedented pressure on emergency services. However, it is likely that improvements may also be attributed to wider service changes conducted by the stroke teams in NC London and East Kent, for example, the introduction of new ‘front door’ processes or factors related to the COVID-19 context (e.g. there was less pressure on the system overall, leaving greater capacity in HASUs to attend to stroke patients).
Strengths and weaknesses
The main strength of the analyses was the unique regional data set we used, which contained detailed information on ambulance destination and conveyance times. We were also able to analyse a substantial (aggregate) data set covering delivery of stroke care for over 80,000 stroke patients over a 30-month period. The robust quasi-experimental framework we used is another strength of the study, permitting useful and informative comparison over time with RoE and ruling out other factors that could affect outcomes across the country during the same period. Having control over the trends over two different quarters also allowed us to account for seasonality in the trends.
Our study had several limitations that caution against interpreting our findings as purely causal effects. First, the local routinely collected ambulance conveyance data for stroke patients were only available for the period April–September 2020. This covered only the period after implementation of prehospital video triage, which continued to develop during this period. Furthermore, these data covered only the areas in which prehospital video triage had been introduced. Therefore, our analyses of these data lacked both historic and geographic controls, and we could not account for the impact of COVID-19 on patient behaviour and on the system (i.e. lower overall activity during this period, etc.). Second, we were unable to assess the impact of the new system on patient outcomes, such as long-term quality of life, disability or functional independence, as these measures are not collected with sufficient reliability in SSNAP clinical audit 6-month follow-up. Third, SSNAP data include only patients admitted to hospital; we were therefore unable to analyse impact on patients pronounced dead at home or while being conveyed to hospital. Fourth, the SSNAP data we analysed were aggregated at the team level: analyses of patient-level data would have permitted assessment of the relationship between patient characteristics and care delivery, especially in terms of analysing time to intervention. Fifth, in the SSNAP data we were not able to distinguish between the video and non-video assisted cases, meaning we could not assess any differential effect on delivery of HASU care. Sixth, we could not account for a series of factors that could influence the indicators analysed here, such as the number of ambulances, organisation of primary care, accessibility of nearer general hospital EDs and potentially public awareness of the FAST test in NC London or East Kent. Seventh, several system changes, including major system optimisation of stroke services, occurred during the analysed period in both NC London and East Kent and this made it difficult to attribute changes in, for example, care delivery to prehospital video triage.
Comparison with other studies
The evidence on prehospital video triage is small but growing, although with several important gaps. We believe that our analysis builds on or confirms some of the existing evidence base, but also begins to fill some of these gaps. As outlined in Chapter 3, research on prehospital video triage tends not to address the impact of such services on patient destination, in particular the potential for the avoidance of unnecessary conveyance to a HASU. In our analysis, prehospital video triage resulted in a substantial proportion of suspected stroke patients being conveyed to alternative destinations, such as the local ED, or remaining home. Taken alongside our qualitative findings (e.g. governance meetings investigating inappropriate patient conveyance), this suggests that specialist stroke assessment may have resulted in a substantial reduction in unnecessary patient conveyance to a HASU. Previous reviews in this area (see Chapter 3) indicate that the potential impact of prehospital video triage on patient safety is largely unstudied. 16 Our analysis of ambulance conveyance showed overwhelmingly that prehospital video triage did not result in conveyance times that went beyond recommended time thresholds. Our findings on improvements to delivery of clinical interventions reflect recent studies suggesting the potential of such interventions to support significant improvement of acute care for stroke patients, including administration of thrombolytic therapies. 41,111,112
Implications
Our analysis showed that a substantial proportion of suspected stroke patients who would traditionally be conveyed to a HASU were, following prehospital video triage assessment, conveyed to alternative destinations, thus avoiding unnecessary conveyance to a HASU. There was a slight reduction in the proportion of stroke patients being treated in a HASU during the early stages of the pandemic, reflecting wider evidence of obstacles to HASU conveyance nationally. Our analysis of the times from symptom onset to arrival at hospital and the HASU suggested that prehospital video triage can be conducted while also permitting timely conveyance of stroke patients to a HASU. We found several significant increases in the proportion of patients receiving timely stroke clinical interventions, and no examples of significant decreases. However, it is likely that these changes may be attributed at least in part to other service changes and COVID-19, in addition to prehospital video triage.
Chapter 7 Discussion and conclusions
Overview
We aimed to conduct a rapid, mixed-methods evaluation of prehospital video triage for suspected stroke patients, as implemented in NC London and East Kent. In order to understand the implementation, experience and impact of these services, our EQs were the following:
-
EQ1: what evidence exists on prehospital video triage for suspected stroke patients, in terms of implementation, usability, safety and outcomes?
-
EQ2: are the prehospital video triage services piloted in NC London and East Kent acceptable to their users (i.e. stroke clinicians and ambulance clinicians)?
-
EQ3: are the services effective in terms of usability and image/sound quality?
-
EQ4: do the services support the appropriate, safe conveyance and treatment of suspected stroke patients?
-
EQ5: which factors influence uptake and impact of these services?
-
EQ6: which aspects of these services should be retained post COVID-19 and which adaptations (if any) are required to support their implementation?
In this chapter, we first present our principal findings organised by these evaluation questions. Second, we discuss the implications of our evaluation, referring to key themes that emerged from our literature review and empirical work. Third, we present the main strengths and weaknesses of the evaluation, including the evaluation design and data used. Finally, we set out our main conclusions and recommendations for future research, formed in agreement with our clinical and patient collaborators.
Principal findings
In this section, we set out our principal findings, where we draw together the key lessons from our analyses and organise them around our EQs.
What evidence exists on prehospital triage services for suspected stroke patients, in terms of implementation, usability, safety and outcomes?
-
There is a limited, but growing evidence base on remote prehospital video triage for stroke, which sits alongside more established and substantial literatures covering other aspects of telemedicine for stroke (e.g. systems permitting hospital-to-hospital communication and mobile stroke ambulance units). Much of this evidence was based on pilot or feasibility research, using both simulated and ‘real-world’ settings.
-
In terms of usability, research suggested that stable network coverage and clear audio-visual signals were important to successful patient assessment. Communication between ambulance and stroke clinicians was also important in ensuring that stroke clinicians could access appropriate patient information.
-
Training of both ambulance and stroke clinicians was identified as an important facilitator of effective prehospital video triage, for example using simulations to enable a clear understanding of new protocols and effective use of communications technology.
-
Importantly, both reviews and primary studies on outcomes of prehospital video triage tended to focus on delivery of stroke clinical interventions, for example time from arrival at hospital to brain scan or thrombolysis. They presented little evidence on the impact of prehospital video triage on such key factors as appropriate patient destination, patient safety, and cost-effectiveness.
Were the prehospital video triage services piloted in North Central London and East Kent acceptable to their users (stroke clinicians and ambulance clinicians)?
-
Our qualitative analysis suggested that in NC London and East Kent, some ambulance clinicians reported ongoing concerns about whether the potential benefits of accessing specialist secondary care stroke expertise might be outweighed by a delay in patient conveyance. However, most ambulance and stroke clinicians interviewed were supportive and accepting of the prehospital video triage services; for example, both groups cited perceived improvements in appropriate patient conveyance and potential reductions in pressure on services (e.g. unnecessary ambulance journeys and fewer ‘stroke mimics’ to manage in HASUs).
-
Ambulance clinicians cited increased confidence and reassurance about their decisions on patient conveyance, and the view that they were learning more about stroke through their communications with stroke clinicians.
-
Stroke clinicians noted that the service did not involve a significant change in practice, beyond having the opportunity to conduct assessments earlier in the pathway and gain advance knowledge of patients. However, they also described a barrier to acceptability in the common requirement to conduct triage assessments alongside their other professional duties, placing pressure on clinicians and potentially limiting the quality of communication.
-
Our survey of over 200 ambulance clinicians in NC London and East Kent confirmed that a substantial majority of respondents (86%) found the prehospital video triage services an improvement on ‘business as usual’ and a similarly high proportion (88%) wanted the new services to continue to operate. However, these positive views were significantly stronger among NC London ambulance clinicians.
Were the services effective in terms of usability and image/sound quality?
-
In our interviews with ambulance and stroke clinicians, image and sound quality were seen as sufficient to conduct prehospital video triage assessments. Ambulance clinicians noted that connections could be disrupted, as both built-up areas and highly open spaces had potential for limited Wi-Fi coverage. Under such circumstances, ambulance clinicians reverted to conveyance protocols that operated before the introduction of prehospital video triage. Issues with connectivity and ambient noise in hospital settings were addressed through connection to hospital Wi-Fi and by giving stroke clinicians audio headsets. Our survey confirmed that ambulance clinicians (77%) agreed that the prehospital video triage services were usable in terms of audio-visual quality.
-
Ambulance and stroke clinicians reported that using the FaceTime communication platform was straightforward to use, although some ambulance clinicians suggested that training and ‘refresher’ courses could be beneficial. NC London’s approach to training was more active, with both face-to-face training and distribution of video information, whereas in East Kent protocols were distributed via e-mail and an online portal. In line with this, our survey found that a majority of respondents (89%) saw the services as easy to use. However, a higher proportion of NC London respondents (94%) rated the service as usable than in East Kent (78%): this may reflect the more active approach to training taken in NC London, where 91% of ambulance clinicians reported having received sufficient training, in contrast to East Kent, where 42% of ambulance clinicians reported having received sufficient training.
Did the services support the appropriate, safe conveyance and treatment of suspected stroke patients?
-
Our analysis of ambulance journey data showed that only a small percentage of stroke patients did not reach hospital within 60 minutes of leaving the scene of stroke. Publicly reported national stroke audit data on times from symptom onset to stroke patients’ arrival at hospital and HASUs found that prehospital video triage did not result in increased median stroke patient conveyance times. This suggests that, despite the additional time spent on prehospital video triage consultations, prehospital video triage can be delivered while still supporting timely patient conveyance to stroke services.
-
Our analysis of national stroke audit data found several significant increases and no significant reductions in delivery of stroke clinical interventions in NC London and East Kent following introduction of prehospital video triage (i.e. relative to changes observed in RoE over the same time period). However, it is possible that other factors, such as relocation of the hospitals’ hyper-acute stroke services in both areas, were significant contributors to these improvements.
-
Our qualitative research suggested that leaders of the triage services were conscious of risks to patient safety and put processes in place to monitor and manage any incidents. Observations of meetings where these data were discussed suggested that there were few reported safety incidents, each of which was explored to identify potential improvements. Our interviews suggested that there was a broader perception among ambulance and stroke clinicians that these services were providing safe care.
-
Our survey of ambulance clinicians confirmed that prehospital video triage influenced patient destination at least once for most (86%) respondents, while 82% of respondents had no concerns about the safety of the services. However, there was again a significant difference between responses in NC London, where 91% had no concerns about safety, and East Kent, where 62% had no concerns.
Which factors influenced uptake and impact of these services?
-
Our qualitative research suggested that several factors helped enable the rapid development, implementation and uptake of prehospital video triage. These factors related to (1) the local and wider contexts into which prehospital video triage was introduced; (2) the interventions themselves; and (3) how they were put into action.
-
Two national/international contextual factors helped drive these changes. First, there existed a longstanding challenge related to the limited specificity of screening instruments such as FAST, which led to the conveyance of a substantial proportion of non-stroke patients to stroke units. Second, the COVID-19 pandemic, by adding a significant patient safety risk to the issue of inappropriate patient conveyance, acted as a ‘burning platform’ for change.
-
These drivers interacted with more local contextual factors. For example, they encouraged adoption of governance processes that were more facilitative of change at system and service levels. The pandemic also raised issues that played on values important to the ambulance and stroke clinicians who were to deliver prehospital video triage, specifically the desire to provide high-quality, safe care to stroke and non-stroke patients.
-
In terms of the interventions themselves, the prehospital video triage services were attractive to many ambulance and stroke clinicians. They saw the process and interface as straightforward to use. Furthermore, reflecting their professional values (cited above), they indicated that it offered advantages over ‘business as usual’, in terms of getting the patient to the most appropriate service for the best possible care.
-
Collaborative leadership was key to implementation: ambulance and stroke clinical leads worked in multiple directions to develop the new services. Within their organisations, clinical leads engaged with senior management to gain local endorsement for the services and worked actively with frontline clinicians (e.g. to encourage uptake, provide training and monitor progress of services). They also reached beyond their local organisations; for example, ambulance and stroke clinical leads worked together across organisational boundaries to develop services that would work for ambulance and stroke clinicians alike. They also engaged with wider system governance to obtain support for these changes and aid ongoing preparations for wider roll-out of the services, if successful.
Which aspects of these services should be retained post COVID-19 and which adaptations (if any) are required to support their implementation?
-
The ambulance and stroke clinicians we interviewed were emphatic that the new prehospital systems represented should be retained. Many suggested that they should be implemented more widely, both in other parts of the country and other health-care specialties. This support for continuation was reflected in our ambulance clinician survey, where 88% of respondents indicated that they would like to see the service continue, and 67% suggested that similar services should be considered for other clinical settings.
-
Broadly, interviewees suggested that relatively few changes were required to the services. A potential risk to sustainability of these services likely to require adaptation was ensuring sufficient capacity among stroke clinicians to deliver the assessments. The current arrangement, where stroke clinicians conduct assessments alongside their other duties, was felt to be disruptive and placed undue pressure on clinicians (which may have important implications for sustainability of prehospital video triage). Our findings on training suggest that more active approaches are preferred by staff: such approaches, if extended, may have potential to encourage increased collaboration between ambulance and stroke clinicians.
Implications
Our literature review confirmed the findings from other reviews that the evidence base on prehospital video triage for suspected stroke patients is small but growing. 15,16 Reflecting a general appreciation of the increasing stability and power of mobile technology, we found recent cases (i.e. published in 2021) of localised activity (in the form of pilots and feasibility studies) in different parts of the world, but little from UK settings. We identified important gaps in relation to the impact of prehospital video triage on appropriate patient destination and patient outcomes, including patient experience, patient safety and cost-effectiveness; we address several of these gaps in our evaluation.
In terms of usability, our qualitative findings confirmed the importance of having a stable Wi–Fi network and clear audio-visual signals, as reported in previous research and reviews. 16,66,69 In addition, our qualitative analysis identified the value of back-up processes for situations where clear audio-visual communication is not possible. In line with previous research, we found that training was seen by clinicians as essential to their becoming confident users of the new service. 59,61,65 However, in addition, our qualitative analysis suggested the value of ‘refresher’ courses, given ambulance clinicians’ view that they treat suspected stroke patients relatively infrequently. Clinicians also suggested the potential for joint training events that bring together ambulance and stroke clinicians to enable a stronger sense of shared culture across these professions.
Our qualitative and survey findings on acceptability suggested that the stroke and ambulance clinicians using prehospital video triage found it acceptable, with the overwhelming majority wanting the services to continue or even expand. This was in line with previous research, which has suggested high user acceptability of prehospital video triage. 16,39,48,65,67 In addition, we were able to identify factors contributing to acceptability. These included increasing ambulance clinicians’ confidence in decisions about patient destination and their understanding of stroke as a condition. An important obstacle to acceptability – and by extension sustainability – of prehospital video triage services was that many stroke clinicians were required to conduct these assessments alongside their standard duties. This was felt to place significant pressure on stroke clinicians.
Our real-world evaluation confirmed findings from recent simulation studies,66,69 which have indicated the importance of clinician communication. However, our qualitative analysis also extended this evidence by providing insights on the distractions that might result from the settings in which ambulance and stroke clinicians conduct the assessment (e.g. ambient noise and competing tasks) and some simple solutions applied (e.g. providing stroke clinicians with communication headsets).
Our systematic review found little published evidence on the impact of prehospital video triage for stroke on patient safety. 16,66,69 Our analysis of ambulance journey times suggested that an overwhelming majority of patients who underwent prehospital video triage assessment were conveyed to a HASU within recommended journey time thresholds. Publicly available national stroke audit data on times from symptom onset to stroke patients’ arrival at hospital and a HASU indicated that prehospital video triage did not result in increased median stroke patient conveyance times. This suggests that, despite additional time potentially spent on scene, prehospital video triage can be delivered while still supporting timely patient conveyance to hospital and stroke services. In addition, our qualitative analysis captured examples of how clinical leaders monitored and managed potential patient safety issues (e.g. reviewing potentially inappropriate patient conveyance in terms of both contributing factors and outcomes).
We found no evidence of reductions in delivery of key stroke clinical interventions, and several examples of significant increases in delivery of interventions (although these may be attributed to other service changes that took place concurrently). These patterns were broadly in line with previous research indicating potential to improve delivery of key interventions, such as time to brain scan and time to thrombolysis. 78,80,81
Strengths and limitations
This rapid evaluation represented an important opportunity to develop timely lessons on a potentially important change in organising prehospital care for suspected stroke patients, implemented during a highly innovative period for the NHS in England. Our evaluation had several strengths:
-
We were able to study ‘real-world’ implementation of two prehospital video triage services. These were implemented in parallel, but differed in several important ways, including the ways in which the service was delivered and supported, and the rurality of the area served by the participating ambulance and stroke services; this hopefully allowed our findings to be relevant to a range of contexts.
-
Our mixed-methods design allowed us to draw on multiple sources of quantitative and qualitative data, letting us address our research questions from several different perspectives.
-
We were able to access a range of high-quality data in a relatively short time: thanks to our strong collaboration with local clinical leads, we were able to interview many ambulance and stroke clinicians and observe a range of governance meetings, and we also obtained over 200 responses to our ambulance clinician survey. In addition, we received high-quality case-level data on ambulance destinations and were able to analyse publicly available national audit data (to which stroke teams broadly continued to submit data throughout the pandemic).
-
Using a social science perspective (in particular, Nolte’s conceptual framework for understanding implementation of digital innovations)17 permitted a rich understanding of the factors contributing to the development, implementation and sustainability of prehospital triage.
There were also several limitations:
-
Although the services we studied contrasted in some important ways, there were some contextual issues that we could not explore. For example, the services we studied were both based in the south-east of England (because none had been implemented elsewhere at that time), and local stroke services had been reorganised so that the local HASU was not co-located with an ED (a separation that may have increased pressure to use the triage service). Similarly, the services studied were introduced during an unprecedented period of change and adaptation in the NHS in England prompted by the COVID-19 pandemic. We were also unable to study alternative prehospital triage systems, for example using telephone discussion of cases. This may limit the extent to which lessons on the implementation and impact of the studied services might be translated to other contexts.
-
We were unable to interview several stakeholder groups for this evaluation. Key among these groups were patients and carers. This project was highly time-sensitive and obtaining HRA ethics approval would have caused a substantial delay to commencing work: we therefore designed this project as a service evaluation so that it could commence in a timely fashion. However, this meant that we could not include interviews with patients and carers in our evaluation design and we recognise this as an important limitation to our work. In addition, we interviewed only ambulance clinicians and stroke consultant physicians, and were able to interview only two stroke consultant physicians (including the service lead) in East Kent. This limited the extent to which we could draw conclusions about clinician views of these services. To address some of these gaps, we shared interim findings with patient representatives and members of stroke teams and ambulance services.
-
Our ambulance conveyance data covered only the areas where prehospital video triage had been introduced and only the time period following the introduction of the triage services; therefore, our analyses had no historical or regional comparators, which limited the nature of analyses we could conduct.
-
Again as a result of project timelines, we were unable to request national stroke audit data at patient level, meaning we were limited in the types of analysis we could conduct (for instance, we could not apply patient-level risk-adjustment or develop matched controls for our studied areas, and we could not examine the effects of shifting from consultant-led to registrar-led prehospital video triage services).
-
The national stroke audit data did not cover several potential patient safety issues, such as appropriateness of patient destination (e.g. patients initially identified as non-stroke who then required inter-hospital transfer to a HASU, and non-stroke patients who were conveyed to a HASU unnecessarily). However, we observed meetings where these data were discussed, which indicated that such incidents were rare and analysed actively.
-
Our ambulance clinician survey recruited a convenience sample and although we obtained over 200 responses, these numbers were too small to permit further disaggregation of responses, for example by frequency of use of prehospital video triage.
Conclusions
Our evaluation sought to contribute lessons about prehospital video triage for suspected stroke patients, particularly in relation to implementation, acceptability and usability, and impact on safety.
Implementation
We found that prehospital video triage can be developed and implemented rapidly. By drawing on a relevant theory of implementation and sustainability of innovations, we were able to establish that influential factors included context, implementation approaches and the characteristics of the prehospital video triage services themselves. These factors were interrelated; for example, the COVID-19 pandemic acted as a ‘burning platform’, encouraging more facilitative governance processes and local professional and organisational receptivity to new ways of working. The wider service reorganisations – whereby local stroke units were no longer co-located with ED services – may have encouraged staff to engage more with prehospital video triage. Ambulance clinicians saw training as an important means of becoming confident users of the new service; more active approaches to training are more likely to be viewed positively by clinicians. Collaborative leadership was key to implementation: ambulance and stroke clinical leads engaged with local senior management, frontline clinicians and beyond their local organisations to develop services that would work for ambulance and stroke clinicians alike and to gain ongoing support across the system.
Acceptability and usability
Ambulance and stroke clinicians overall found prehospital video triage acceptable and usable. The technology was seen as straightforward to use and generally reliable. A potentially important factor was the nature of training offered in the two areas, with more active approaches (as employed in NC London) preferred by ambulance clinicians. Stroke clinicians reported concerns about delivering prehospital video triage alongside their other duties, suggesting that addressing this issue would be important to ensuring sustainability of services.
Impact on safety and quality
Almost all stroke patients’ ambulance journeys to HASUs remained within recommended conveyance time thresholds. Publicly reported national stroke audit data on times from symptom onset to stroke patients’ arrival at hospital and a HASU suggested that, despite additional time potentially spent on scene, prehospital video triage can be delivered while still supporting timely patient conveyance to hospital and stroke services. In terms of stroke care delivery, we found several significant increases in delivery of key clinical interventions following the introduction of prehospital video triage (above and beyond what was seen elsewhere in England), although other concurrent changes to service organisation may have played influential roles. Our qualitative data – in terms of both interviews and observations of meetings where safety issues were analysed – suggested that safety was a key priority of the clinicians delivering these services; governance processes gave assurance that the services were indeed delivering safe care as well as wider service and system benefits.
Future research agenda
Although we believe that our evaluation has made several important contributions to the understanding of prehospital video triage for suspected stroke patients, there were several important issues that we could not address. Taken alongside the gaps in evidence identified in our literature reviews, we propose that the following issues should be prioritised in future research:
-
Qualitative research on patient and carer experience of prehospital video triage is an important gap in current understanding. There would be value in analysing the perspectives of stroke and non-stroke patients and their carers (including people from different ethnic, cultural and socioeconomic backgrounds, and from remote, rural areas), and understanding factors that might influence how people experience prehospital video triage (e.g. immediate symptoms such as dysphagia or loss of ability to communicate verbally). This would provide important learning on how these services work and how they might be improved, for example on how to be accessible to all communities who might require these services.
-
Qualitative research on the views and experiences of the wider health-care system would provide a clearer understanding of implementation, delivery and sustainability of these services. Such stakeholders would include clinicians and managers (at varied levels of seniority) in ambulance, stroke and other acute teams, senior organisational managers, commissioners, patient representative groups, and wider system governance (e.g. NHS England/Improvement and ISDNs).
-
Quantitative research using national data sets at patient-level would permit more detailed analyses of the impact on prehospital and acute care delivery, conveyance, and patient outcomes for both stroke and non-stroke patients. In particular, such data would permit longitudinal designs using historical (i.e. pre-/post-implementation) and regional comparators, with patient-level risk-adjustment.
-
Research on cost-effectiveness remains an important gap in knowledge about these services. Quantitative research of the kind described above, integrated with qualitative data on implementation activities, would permit large scale cost-effectiveness evaluation of these services.
-
Mixed-method research on the issues outlined above may be conducted to address sustainability of established prehospital video triage services and roll-out elsewhere. Research on sustainability would permit understanding of how established services develop over time, in accommodating contextual changes and other issues identified here (e.g. stroke clinicians delivering prehospital video triage alongside other duties). Research on roll-out (for instance, to services that have a co-located ED) would illustrate how prehospital video triage might be adapted to different contexts. Such research would thus increase the likelihood of lessons being engaged with by a wide range of patient, professional and managerial stakeholders based in different settings.
To address many of these issues, the authors recently commenced a new research project, funded by the NIHR HSDR programme. PHOTONIC (PreHOspital Triage for potential stroke patients: lessONs from systems Implemented in response to COVID19) will run from September 2021 to August 2023 inclusive, with the aim of understanding the implementation, experience and impact of prehospital video triage for suspected stroke. It will employ a mixed-methods approach, using qualitative methods to study implementation and experience from a wide range of stakeholders, including (stroke and non-stroke) patients and carers; it will also analyse patient-level data from national and local data sets to understand the impact of prehospital video triage on patient conveyance, care delivery, patient outcomes and cost-effectiveness, relative to national and regional comparators. For further information, please see https://fundingawards.nihr.ac.uk/award/NIHR133779.
Acknowledgements
We thank the following individuals for their contributions (ordered alphabetically):
-
all of the people who took part in this evaluation and our contacts who helped to co-ordinate our interactions with the ambulance and stroke services
-
Professor Rachael Fothergill (LAS) for constructive comments on our evaluation protocol and our draft final report
-
Dr Salman Haider (UCLH) for insights provided at formative feedback meetings and for contributions to the development of the ambulance clinician survey tool
-
Mr James Kear (LAS) for contributions to the development of the ambulance clinician survey tool
-
Ms Debora Marletta (UCL) for providing expertise in the design of the systematic review search strategy and protocol
-
Professor Steven Morris (University of Cambridge) for reviewing and advising on statistical aspects of our ambulance survey analysis (Chapter 5) and our quantitative analysis (Chapter 6)
-
Ms Pei Li Ng (UCL) for project management expertise and support during key stages of development and completion of this project, including drafting of the final report
-
Professor Henry Potts (UCL) for peer reviewing our evaluation protocol
-
Ms Joanna Shaw (LAS) for constructive comments on our draft final report
-
Professor Helen Snooks (University of Swansea) for peer reviewing our evaluation protocol
-
Dr Cecilia Vindrola-Padros (UCL) for contributing to the planning of the evaluation and protocol, providing expertise in rapid methodologies for the literature review and qualitative analysis
-
Ms Louise Ward (East Kent University Hospitals NHS Foundation Trust) for insights provided at formative feedback meetings.
Contributions of authors
Angus IG Ramsay (https://orcid.org/0000-0002-4446-6916) (Senior Research Fellow) was the principal investigator and led the overall evaluation. He contributed to the design and analysis of all aspects of the study. He is lead author of this report and led authorship of Chapters 1, 2, 4 and 7, and co-led Chapter 5.
Jean Ledger (https://orcid.org/0000-0003-2523-7971) (Senior Research Fellow) led the literature review and ambulance clinician survey analysis (including development of the survey tool); she supported the qualitative analysis (including development of data collection tools, data collection and interpretation). She contributed to the design and interpretation of all other aspects of the study, and made important contributions to drafting the final report. She led authorship of Chapter 3 and co-led Chapter 5.
Sonila M Tomini (https://orcid.org/0000-0002-4241-2121) (Research Fellow) led the quantitative analysis of ambulance conveyance and stroke clinical interventions data. She contributed to the design and interpretation of all aspects of the study, and made important contributions to drafting the final report. She led authorship of Chapter 6.
Claire Hall (https://orcid.org/0000-0003-1248-0999) (Special Paramedic for Urgent and Emergency Care; Clinical Pathways Lead) contributed clinical and organisational knowledge on ambulance services and prehospital video triage in East Kent. She supported development of the evaluation protocol, provided valuable insights at formative feedback meetings, supported data collection (providing access to interviewees, governance meetings, local documents and ambulance conveyance data, and supporting the development and distribution of the ambulance clinician survey), and made important contributions to the interpretation of findings and drafting of the final report.
David Hargroves (https://orcid.org/0000-0003-0127-3011) (Clinical Lead for Stroke) contributed clinical and organisational knowledge on stroke services and prehospital video triage in East Kent, and insights on the national context for stroke care. He supported development of the evaluation protocol, provided valuable insights at formative feedback meetings, supported data collection (providing access to interviewees, governance meetings, and local documents), and made important contributions to the interpretation of findings and drafting of the final report.
Patrick Hunter (https://orcid.org/0000-0002-4553-3594) (Sector Senior Clinical Lead) contributed clinical and organisational knowledge on ambulance services and prehospital video triage in NC London. He supported development of the evaluation protocol, provided valuable insights at formative feedback meetings, supported data collection (providing access to interviewees, governance meetings, local documents and ambulance conveyance data, and supporting the development and distribution of the ambulance clinician survey), and made important contributions to the interpretation of findings and drafting of the final report.
Simon Payne (patient representative) provided insights from the perspective of a stroke survivor based in the Kent area, advising on the interpretation and communication of our findings over the course of the evaluation, including reviewing our final report and commenting on our plain English summary.
Raj Mehta (https://orcid.org/0000-0002-4003-530X) (patient representative) peer-reviewed our evaluation protocol before agreeing to support the evaluation as a patient representative, then provided insights on the interpretation and communication of our findings over the course of the evaluation, including commenting on our final report and plain English summary.
Robert Simister (https://orcid.org/0000-0003-0578-6711) (Consultant Stroke Neurologist; Clinical Lead for Stroke) contributed clinical and organisational knowledge on stroke services and prehospital video triage in NC London. He supported the development of the evaluation protocol, provided valuable insights at formative feedback meetings, supported data collection (providing access to interviewees, governance meetings and local documents), and made important contributions to the interpretation of findings and drafting of the final report.
Fola Tayo (https://orcid.org/0000-0002-4977-8564) (patient representative) peer-reviewed our evaluation protocol before agreeing to support the evaluation as a patient representative, then provided insights on the interpretation and communication of our findings over the course of the evaluation, including commenting on our final report and plain English summary.
Naomi J Fulop (https://orcid.org/0000-0001-5306-6140) (Professor of Health Care Organisation and Management) oversaw the evaluation and contributed to the design and analysis of all aspects of the evaluation, and made important contributions to the drafting of the final report.
Data-sharing statement
The ambulance conveyance data were shared securely and anonymously by local clinical collaborators for the purposes of this evaluation only. The team-level SSNAP clinical audit data are in the public domain and available from www.strokeaudit.org/results/Clinical-audit/National-Results.aspx. All qualitative data and ambulance clinician survey data that can be shared are contained within the report. The nature of the data means that nothing else can be provided. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data are vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Ramsay AIG, Ledger J, Vindrola-Padros C, Tomini SM, Hargroves D, Simister R, et al. Pre-Hospital Specialist Triage of Potential Stroke Patients Using Digital Technology: A Rapid Service Evaluation to Capture Learning and Impact of Innovations Prompted by the COVID19 Pandemic; Protocol v1.3 2021 n.d. https://fundingawards.nihr.ac.uk/award/NIHR132679 (accessed 24 November 2021).
- Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol 2016;15:913-24. https://doi.org/10.1016/S1474-4422(16)30073-4.
- Morris S, Hunter RM, Ramsay AI, Boaden R, McKevitt C, Perry C, et al. Impact of centralising acute stroke services in English metropolitan areas on mortality and length of hospital stay: difference-in-differences analysis. BMJ 2014;349. https://doi.org/10.1136/bmj.g4757.
- Morris S, Ramsay AIG, Boaden RJ, Hunter RM, McKevitt C, Paley L, et al. Impact and sustainability of centralising acute stroke services in English metropolitan areas: retrospective analysis of hospital episode statistics and stroke national audit data. BMJ 2019;364. https://doi.org/10.1136/bmj.l1.
- Ramsay AI, Morris S, Hoffman A, Hunter RM, Boaden R, McKevitt C, et al. Effects of centralizing acute stroke services on stroke care provision in two large metropolitan areas in England. Stroke 2015;46:2244-51. https://doi.org/10.1161/STROKEAHA.115.009723.
- Elameer M, Price C, Flynn D, Rodgers H. The impact of acute stroke service centralisation: a time series evaluation. Future Healthc J 2018;5:181-7. https://doi.org/10.7861/futurehosp.5-3-181.
- Fulop NJ, Ramsay AI, Perry C, Boaden RJ, McKevitt C, Rudd AG, et al. Explaining outcomes in major system change: a qualitative study of implementing centralised acute stroke services in two large metropolitan regions in England. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0445-z.
- Fulop NJ, Ramsay AIG, Hunter RM, McKevitt C, Perry C, Turner SJ, et al. Evaluation of reconfigurations of acute stroke services in different regions of England and lessons for implementation: a mixed-methods study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07070.
- Turner S, Goulding L, Denis J-L, McDonald R, Fulop NJ, Raine R, et al. Challenges, Solutions and Future Directions in the Evaluation of Service Innovations in Health Care and Public Health. Health Serv Deliv Res. 2016.
- NHS England . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 18 June 2022).
- Rudd M, Buck D, Ford GA, Price CI. A systematic review of stroke recognition instruments in hospital and prehospital settings. Emerg Med J 2016;33:818-22. https://doi.org/10.1136/emermed-2015-205197.
- Demaerschalk BM, Levine SR. Telestroke: solid support for virtual acute stroke care. Neurology 2016;87:1314-15. https://doi.org/10.1212/WNL.0000000000003166.
- Fassbender K, Grotta JC, Walter S, Grunwald IQ, Ragoschke-Schumm A, Saver JL. Mobile stroke units for prehospital thrombolysis, triage, and beyond: benefits and challenges. Lancet Neurol 2017;16:227-37. https://doi.org/10.1016/S1474-4422(17)30008-X.
- Kepplinger J, Barlinn K, Deckert S, Scheibe M, Bodechtel U, Schmitt J. Safety and efficacy of thrombolysis in telestroke: a systematic review and meta-analysis. Neurology 2016;87:1344-51. https://doi.org/10.1212/WNL.0000000000003148.
- French B, Day E, Watkins C, McLoughlin A, Fitzgerald J, Leathley M, et al. The challenges of implementing a telestroke network: a systematic review and case study. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-125.
- Lumley HA, Flynn D, Shaw L, McClelland G, Ford GA, White PM, et al. A scoping review of pre-hospital technology to assist ambulance personnel with patient diagnosis or stratification during the emergency assessment of suspected stroke. BMC Emerg Med 2020;20. https://doi.org/10.1186/s12873-020-00323-0.
- Nolte E. How Do We Ensure That Innovation in Health Service Delivery and Organization is Implemented, Sustained and Spread?. Copenhagen: WHO Regional Office for Europe; 2018.
- University College London Hospitals NHS Foundation Trust . How the Stroke Team Transformed the Service at UCLH 2021. www.uclh.nhs.uk/news/how-stroke-team-transformed-service-uclh (accessed 3 September 2021).
- Shrank W. The Center For Medicare and Medicaid Innovation’s blueprint for rapid-cycle evaluation of new care and payment models. Health Aff 2013;32:807-12. https://doi.org/10.1377/hlthaff.2013.0216.
- Skillman M, Cross-Barnet C, Friedman Singer R, Rotondo C, Ruiz S, Moiduddin A. A framework for rigorous qualitative research as a component of mixed method rapid-cycle evaluation. Qual Health Res 2019;29:279-89. https://doi.org/10.1177/1049732318795675.
- Beebe J. Rapid Qualitative Inquiry: A Field Guide to Team-based Assessment. Lanham, MD: Rowman & Littlefield; 2014.
- Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141-6. https://doi.org/10.1097/XEB.0000000000000050.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372. https://doi.org/10.1136/bmj.n71.
- Hong Q, Pluye P, Fábregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT), Version 2018. Montreal, QC: McGill University; 2018.
- Critical Assessment Skills Programme (CASP) . CASP Checklists n.d. https://casp-uk.net/casp-tools-checklists/ (accessed 27 July 2021).
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product of the ESRC Methods Programme. Lancaster: University of Lancaster; 2006.
- Fulop N, Barbosa EC, Hill M, Ledger J, Sherlaw-Johnson C, Spencer J, et al. Special measures for quality and challenged providers: study protocol for evaluating the impact of improvement interventions in NHS trusts. Int J Health Policy Manag 2020;9:143-51. https://doi.org/10.15171/ijhpm.2019.100.
- Sentinel Stroke National Audit Programme . Data Analysis Methodology. 2021. www.strokeaudit.org/About-SSNAP/SSNAP-Clinical-Audit/Data-Analysis-Methodology.aspx (accessed 18 July 2022).
- NHS England . Stroke Services: Configuration Decision Support Guide 2015. www.england.nhs.uk/mids-east/wp-content/uploads/sites/7/2018/03/stroke-services-configuration-decision-support-guide.pdf (accessed 9 September 2021).
- Ashenfelter O, Card D. Using the longitudinal structure of earnings to estimate the effect of training programs. Rev Econ Stat 1985;67:648-60. https://doi.org/10.3386/w1489.
- Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health 2012;66:1182-6. https://doi.org/10.1136/jech-2011-200375.
- McDonald R, Boaden R, Roland M, Kristensen SR, Meacock R, Lau YS, et al. A qualitative and quantitative evaluation of the Advancing Quality pay-for-performance programme in the NHS North West. Health Serv Deliv Res 2014;3. https://doi.org/10.3310/hsdr03230.
- Sutton M, Nikolova S, Boaden R, Lester H, McDonald R, Roland M. Reduced mortality with hospital pay for performance in England. N Engl J Med 2012;367:1821-8. https://doi.org/10.1056/NEJMsa1114951.
- University College London – Library Services . UCL Records Management Policy 2022. www.ucl.ac.uk/library/collections/records-office/ucl-records-management-policy (accessed 25 August 2022).
- University College London – Data Protection . Understanding Data Protection at UCL n.d. www.ucl.ac.uk/data-protection/data-protection-overview/understanding-data-protection-ucl (accessed 25 August 2022).
- UCL Information Services Division . Learning and Teaching: Opinio n.d. www.ucl.ac.uk/isd/services/learning-teaching/e-learning-services-for-staff/e-learning-core-tools/opinio (accessed 27 July 2021).
- Johansson T, Wild C. Telemedicine in acute stroke management: systematic review. Int J Technol Assess Health Care 2010;26:149-55. https://doi.org/10.1017/S0266462310000139.
- Yperzeele L, Van Hooff RJ, De Smedt A, Valenzuela Espinoza A, Van de Casseye R, Hubloue I, et al. Prehospital stroke care: limitations of current interventions and focus on new developments. Cerebrovasc Dis 2014;38:1-9. https://doi.org/10.1159/000363617.
- Winburn AS, Brixey JJ, Langabeer J, Champagne-Langabeer T. A systematic review of prehospital telehealth utilization. J Telemed Telecare 2018;24:473-81. https://doi.org/10.1177/1357633X17713140.
- Valenzuela Espinoza A, Devos S, van Hooff RJ, Fobelets M, Dupont A, Moens M, et al. Time gain needed for in-ambulance telemedicine: cost-utility model. JMIR Mhealth Uhealth 2017;5. https://doi.org/10.2196/mhealth.8288.
- Aromataris E, Fernandez RS, Godfrey C, Holly C, Khalil H, Tungpunkom P. Joanna Briggs Institute Reviewer’s Manual. Adelaide, SA: Joanna Briggs Institute; 2020.
- Ledger J, Ramsay A, Marletta D, Tomini S, Fulop N. The Implementation of Digital Interventions and Communication Technologies in Emergency Care Pathways to Support the Remote Assessment and Triage of Patients Suspected of Stroke: A Systematic Review n.d. www.crd.york.ac.uk/prospero/display_record.php?RecordID=254209 (accessed 25 August 2022).
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) . PRISMA Flow Diagram n.d. http://prisma-statement.org/prismastatement/flowdiagram.aspx (accessed 16 September 2021).
- Falconer J. Removing Duplicates from an EndNote Library n.d. https://blogs.lshtm.ac.uk/library/2018/12/07/removing-duplicates-from-an-endnote-library/ (accessed 15 July 2022).
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan – a web and mobile app for systematic reviews. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0384-4.
- Aude Bert HJ, Saver JL, Starman S, Lees KR, Endres M. Prehospital stroke care: new prospects for treatment and clinical research. Neurology 2013;81:501-8. https://doi.org/10.1212/WNL.0b013e31829e0fdd.
- Rogers H, Madathil KC, Anasarca S, Narasimha S, Ashok A, Nair A, et al. A systematic review of the implementation challenges of telemedicine systems in ambulances. Telemid J E Health 2017;23:707-17. https://doi.org/10.1089/tmj.2016.0248.
- Calderon VJ, Kasturiarachi BM, Lin E, Bansal V, Zaidat OO. Review of the mobile stroke unit experience worldwide. Interv Neurol 2018;7:347-58. https://doi.org/10.1159/000487334.
- Ehntholt MS, Parasram M, Mir SA, Lerario MP. Mobile stroke units: bringing treatment to the patient. Curr Treat Options Neurol 2020;22. https://doi.org/10.1007/s11940-020-0611-0.
- Baratloo A, Rahimpour L, Boshoku AI, Safari S, Lee CW, Abdala A. Effects of telestroke on thrombolysis times and outcomes: a meta-analysis. Perhaps Emerg Care 2018;22:472-84. https://doi.org/10.1080/10903127.2017.1408728.
- Totten AM, Hansen RN, Wagner J, Stillman L, Vile I, Davis-O’Reilly C, et al. Telehealth for Acute and Chronic Care Consultations. Rockville, MD: Agency for Healthcare Research and Quality; 2019.
- Hubert GJ, Müller-Baran P, Audebert HJ. Recent advances in TeleStroke: a systematic review on applications in prehospital management and Stroke Unit treatment or TeleStroke networking in developing countries. Int J Stroke 2014;9:968-73. https://doi.org/10.1111/ijs.12394.
- Rubin MN, Wellik KE, Channer DD, Demaerschalk BM. A systematic review of telestroke. Postgrad Med 2013;125:45-50. https://doi.org/10.3810/pgm.2013.01.2623.
- Demaerschalk BM, Hwang HM, Leung G. Cost analysis review of stroke centers, telestroke, and rt-PA. Am J Manag Care 2010;16:537-44.
- Flynn D, Francis R, Robalino S, Lally J, Snooks H, Rodgers H, et al. A review of enhanced paramedic roles during and after hospital handover of stroke, myocardial infarction and trauma patients. BMC Emerg Med 2017;17. https://doi.org/10.1186/s12873-017-0118-5.
- Jones SP, Bray JE, Gibson JME, McClelland G, Miller C, Price CI, et al. Characteristics of patients who had a stroke not initially identified during emergency prehospital assessment: a systematic review. Emerg Med J 2021;38. https://doi.org/10.1136/emermed-2020-209607.
- Jiang X, Ming WK, You JH. The cost-effectiveness of digital health interventions on the management of cardiovascular diseases: systematic review. J Med Internet Res 2019;21. https://doi.org/10.2196/13166.
- Barrett KM, Pizzi MA, Kesari V, TerKonda SP, Mauricio EA, Silvers SM, et al. Ambulance-based assessment of NIH Stroke Scale with telemedicine: a feasibility pilot study. J Telemed Telecare 2017;23:476-83. https://doi.org/10.1177/1357633X16648490.
- Bergrath S, Czaplik M, Rossaint R, Hirsch F, Beckers SK, Valentin B, et al. Implementation phase of a multicentre prehospital telemedicine system to support paramedics: feasibility and possible limitations. Scand J Trauma Resusc Emerg Med 2013;21. https://doi.org/10.1186/1757-7241-21-54.
- Bergrath S, Rörtgen D, Rossaint R, Beckers SK, Fischermann H, Brokmann JC, et al. Technical and organisational feasibility of a multifunctional telemedicine system in an emergency medical service – an observational study. J Telemed Telecare 2011;17:371-7. https://doi.org/10.1258/jtt.2011.110203.
- Chapman Smith SN, Brown PC, Waits KH, Wong JS, Bhatti MS, Toqeer Q, et al. Development and evaluation of a user-centered mobile telestroke platform. Telemed J E Health 2019;25:638-48. https://doi.org/10.1089/tmj.2018.0044.
- Chapman Smith SN, Govindarajan P, Padrick MM, Lippman JM, McMurry TL, Resler BL, et al. A low-cost, tablet-based option for prehospital neurologic assessment: the iTREAT study. Neurology 2016;87:19-26. https://doi.org/10.1212/WNL.0000000000002799.
- Eadie L, Regan L, Mort A, Shannon H, Walker J, MacAden A, et al. Telestroke assessment on the move: prehospital streamlining of patient pathways. Stroke 2015;46:e38-40. https://doi.org/10.1161/STROKEAHA.114.007475.
- Felzen M, Brokmann JC, Beckers SK, Czaplik M, Hirsch F, Tamm M, et al. Improved technical performance of a multifunctional prehospital telemedicine system between the research phase and the routine use phase – an observational study. J Telemed Telecare 2017;23:402-9. https://doi.org/10.1177/1357633X16644115.
- Joseph A, Chalil Madathil K, Jafarifiroozabadi R, Rogers H, Mihandoust S, Khasawneh A, et al. Communication and teamwork during telemedicine-enabled stroke care in an ambulance. Hum Factors 2022;64:21-4. https://doi.org/10.1177/0018720821995687.
- Lippman JM, Smith SN, McMurry TL, Sutton ZG, Gunnell BS, Cote J, et al. Mobile telestroke during ambulance transport is feasible in a rural EMS setting: the iTREAT study. Telemed J E Health 2016;22:507-13. https://doi.org/10.1089/tmj.2015.0155.
- Mort A, Eadie L, Regan L, Macaden A, Heaney D, Bouamrane MM, et al. Combining transcranial ultrasound with intelligent communication methods to enhance the remote assessment and management of stroke patients: framework for a technology demonstrator. Health Informatics J 2016;22:691-70. https://doi.org/10.1177/1460458215580353.
- Rogers H, Chalil Madathil K, Joseph A, McNeese N, Holmstedt C, Holden R, et al. Task, usability, and error analyses of ambulance-based telemedicine for stroke care. IISE Trans Healthc Syst Eng 2021;11:192-208. https://doi.org/10.1080/24725579.2021.1883775.
- Torres Zenteno AH, Fernández F, Palomino-García A, Moniche F, Escudero I, Jiménez-Hernández MD, et al. Mobile platform for treatment of stroke: a case study of tele-assistance. Health Informatics J 2016;22:676-90. https://doi.org/10.1177/1460458215572925.
- Valenzuela Espinoza A, Van Hooff R-J, De Smedt A, Moens M, Yperzeele L, Nieboer K, et al. Development and pilot testing of 24/7 in-ambulance telemedicine for acute stroke: prehospital stroke study at the Universitair Ziekenhuis Brussel-Project. Cerebrovasc Dis 2016;42:15-22. https://doi.org/10.1159/000444175.
- Van Hooff R-J, Cambron M, Van Dyck R, De Smedt A, Moens M, Espinoza AV, et al. Prehospital unassisted assessment of stroke severity using telemedicine: a feasibility study. Stroke 2013;44:2907-9. https://doi.org/10.1161/STROKEAHA.113.002079.
- Al Kasab S, Almallouhi E, Grant C, Hewitt D, Hewitt J, Baki M, et al. Telestroke consultation in the emergency medical services unit: a novel approach to improve thrombolysis times. J Stroke Cerebrovasc Dis 2021;30. https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.105710.
- Belt GH, Felberg RA, Rubin J, Halperin JJ. In-transit telemedicine speeds ischemic stroke treatment: preliminary results. Stroke 2016;47:2413-15. https://doi.org/10.1161/STROKEAHA.116.014270.
- Johansson A, Esbjörnsson M, Nordqvist P, Wiinberg S, Andersson R, Ivarsson B, et al. Technical feasibility and ambulance nurses’ view of a digital telemedicine system in pre-hospital stroke care – a pilot study. Int Emerg Nurs 2019;44:35-40. https://doi.org/10.1016/j.ienj.2019.03.008.
- Liman TG, Winter B, Waldschmidt C, Zerbe N, Hufnagl P, Audebert HJ, et al. Telestroke ambulances in prehospital stroke management: concept and pilot feasibility study. Stroke 2012;43:2086-90. https://doi.org/10.1161/STROKEAHA.112.657270.
- Wu T-C, Nguyen C, Ankrom C, Vahidy F, Grotta J, Savitz S, et al. Pre-hospital utility of rapid stroke evaluation using in-ambulance telemedicine: a pilot feasibility study. Stroke 2014;45:2342-7. https://doi.org/10.1161/STROKEAHA.114.005193.
- Wu Y, Chen F, Song H, Feng W, Sun J, Liu R, et al. Use of a smartphone platform to help with emergency management of acute ischemic stroke: observational study. JMIR Mhealth Uhealth 2021;9. https://doi.org/10.2196/25488.
- Bergrath S, Reich A, Rossaint R, Rörtgen D, Gerber J, Fischermann H, et al. Feasibility of prehospital teleconsultation in acute stroke – a pilot study in clinical routine. PLOS One 2012;7. https://doi.org/10.1371/journal.pone.0036796.
- Drenck N, Viereck S, Bækgaard JS, Christensen KB, Lippert F, Folke F. Pre-hospital management of acute stroke patients eligible for thrombolysis – an evaluation of ambulance on-scene time. Scand J Trauma Resusc Emerg Med 2019;27. https://doi.org/10.1186/s13049-018-0580-4.
- Eder PA, Laux G, Rashid A, Kniess T, Haeusler KG, Shammas L, et al. Stroke Angel: effect of telemedical prenotification on in-hospital delays and systemic thrombolysis in acute stroke patients. Cerebrovasc Dis 2021;50:420-8. https://doi.org/10.1159/000514563.
- Felzen M, Beckers SK, Kork F, Hirsch F, Bergrath S, Sommer A, et al. Utilization, safety, and technical performance of a telemedicine system for prehospital emergency care: observational study. J Med Internet Res 2019;21. https://doi.org/10.2196/14907.
- Hölscher T, Dunford JV, Schlachetzki F, Boy S, Hemmen T, Meyer BC, et al. Prehospital stroke diagnosis and treatment in ambulances and helicopters – a concept paper. Am J Emerg Med 2013;31:743-7. https://doi.org/10.1016/j.ajem.2012.12.030.
- Mazya MV, Berglund A, Ahmed N, von Euler M, Holmin S, Laska AC, et al. Implementation of a prehospital stroke triage system using symptom severity and teleconsultation in the Stockholm Stroke Triage Study. JAMA Neurol 2020;77:691-9. https://doi.org/10.1001/jamaneurol.2020.0319.
- Quadflieg LTM, Beckers SK, Bergrath S, Brockert AK, Schröder H, Sommer A, et al. Comparing the diagnostic concordance of tele-EMS and on-site-EMS physicians in emergency medical services: a retrospective cohort study. Sci Rep 2020;10. https://doi.org/10.1038/s41598-020-75149-8.
- Schröder H, Beckers SK, Ogrodzki K, Borgs C, Ziemann S, Follmann A, et al. Tele-EMS physicians improve life-threatening conditions during prehospital emergency missions. Sci Rep 2021;11. https://doi.org/10.1038/s41598-021-93287-5.
- Verma A, Gladstone DJ, Fang J, Chenkin J, Black SE, Verbeek PR. Effect of online medical control on prehospital Code Stroke triage. CJEM 2010;12:103-10. https://doi.org/10.1017/S1481803500012124.
- Seah HM, Burney M, Phan M, Shell D, Wu J, Zhou K, et al. Code Stroke Alert – concept and development of a novel open-source platform to streamline acute stroke management. Front Neurol 2019;10. https://doi.org/10.3389/fneur.2019.00725.
- Amadi-Obi A, Gilligan P, Owens N, O’Donnell C. Telemedicine in pre-hospital care: a review of telemedicine applications in the pre-hospital environment. Int J Emerg Med 2014;7. https://doi.org/10.1186/s12245-014-0029-0.
- Chowdhury SZ, Baskar PS, Bhaskar S. Effect of prehospital workflow optimization on treatment delays and clinical outcomes in acute ischemic stroke: a systematic review and meta-analysis. Acad Emerg Med 2021;28:781-80. https://doi.org/10.1111/acem.14204.
- Fassbender K, Balucani C, Walter S, Levine SR, Haass A, Grotta J. Streamlining of prehospital stroke management: the golden hour. Lancet Neurol 2013;12:585-96. https://doi.org/10.1016/S1474-4422(13)70100-5.
- Fassbender K, Walter S, Grunwald IQ, Merzou F, Mathur S, Lesmeister M, et al. Prehospital stroke management in the thrombectomy era. Lancet Neurol 2020;19:601-10. https://doi.org/10.1016/S1474-4422(20)30102-2.
- Guzik AK, Martin-Schild S, Tadi P, Chapman SN, Al Kasab S, Martini SR, et al. Telestroke across the continuum of care: lessons from the COVID-19 pandemic. J Stroke Cerebrovasc Dis 2021;30. https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.105802.
- Martinez-Gutierrez JC, Chandra RV, Hirsch JA, Leslie-Mazwi T. Technological innovation for prehospital stroke triage: ripe for disruption. J Neurointerv Surg 2019;11:1085-90. https://doi.org/10.1136/neurintsurg-2019-014902.
- Mazighi M, Derex L, Amarenco P. Prehospital stroke care: potential, pitfalls, and future. Curr Opin Neurol 2010;23:31-5. https://doi.org/10.1097/WCO.0b013e328334dafb.
- van Gaal S, Demchuk A. Clinical and technological approaches to the prehospital diagnosis of large vessel occlusion. Stroke 2018;49:1036-43. https://doi.org/10.1161/STROKEAHA.117.017947.
- Weber J, Ebinger M, Audebert HJ. Prehospital stroke care: telemedicine, thrombolysis and neuroprotection. Expert Rev Neurother 2015;15:753-61. https://doi.org/10.1586/14737175.2015.1051967.
- NCT . Prehospital Management of Stroke Patients by Emergency Medical Services 2014. www.cochranelibrary.com/central/doi/10.1002/central/CN-02030514/full (accessed 16 September 2021).
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Brown CW, Macleod MJ. The positive predictive value of an ambulance prealert for stroke and transient ischaemic attack. Eur J Emerg Med 2018;25:411-15. https://doi.org/10.1097/MEJ.0000000000000475.
- Proctor RW, Van Zandt T. Human Factors in Simple and Complex Systems. Boca Raton, FL: CRC Press; 2018.
- Stroke Unit Trialists’ Collaboration . Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2013;9. https://doi.org/10.1002/14651858.CD000197.pub3.
- Bray BD, Ayis S, Campbell J, Hoffman A, Roughton M, Tyrrell PJ, et al. Associations between the organisation of stroke services, process of care, and mortality in England: prospective cohort study. BMJ 2013;346. https://doi.org/10.1136/bmj.f2827.
- Langhorne P, Fearon P, Ronning OM, Kaste M, Palomaki H, Vemmos K, et al. Stroke unit care benefits patients with intracerebral hemorrhage: systematic review and meta-analysis. Stroke 2013;44:3044-9. https://doi.org/10.1161/STROKEAHA.113.001564.
- Hunter RM, Davie C, Rudd A, Thompson A, Walker H, Thomson N, et al. Impact on clinical and cost outcomes of a centralized approach to acute stroke care in London: a comparative effectiveness before and after model. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0070420.
- Intercollegiate Stroke Working Party . National Clinical Guideline for Stroke 2016. www.strokeaudit.org/Guideline/Full-Guideline.aspx (accessed 24 November 2021).
- Sentinel Stroke National Audit Programme . Simplified Technical Information for Key Indicators 2015. www.strokeaudit.org/SupportFiles/Documents/Clinical-Audit-Resources/Simplified-Technical-Info-version-3-(September-201.aspx (accessed 27 November 2021).
- Office for National Statistics . Population Projections for Local Authorities: Table 2 2018. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/datasets/localauthoritiesinenglandtable2 (accessed 8 September 2021).
- Perry R, Banaras A, Werring DJ, Simister R. What has caused the fall in stroke admissions during the COVID-19 pandemic?. J Neurol 2020;267:3457-8. https://doi.org/10.1007/s00415-020-10030-2.
- Douiri A, Muruet W, Bhalla A, James M, Paley L, Stanley K, et al. Stroke care in the United Kingdom during the COVID-19 pandemic. Stroke 2021;52:2125-33. https://doi.org/10.1161/STROKEAHA.120.032253.
- Audebert HJ, Schenkel J, Heuschmann PU, Bogdahn U, Haberl RL. Telemedic Pilot Project for Integrative Stroke Care Group . Effects of the implementation of a telemedical stroke network: the Telemedic Pilot Project for Integrative Stroke Care (TEMPiS) in Bavaria, Germany. Lancet Neurol 2006;5:742-8. https://doi.org/10.1016/S1474-4422(06)70527-0.
- Schwamm LH, Rosenthal ES, Hirshberg A, Schaefer PW, Little EA, Kvedar JC, et al. Virtual TeleStroke support for the emergency department evaluation of acute stroke. Acad Emerg Med 2004;11:1193-7. https://doi.org/10.1197/j.aem.2004.08.014.
Appendix 1 Supplementary information for analyses
| First author and year | Location | Study type | Intervention | Population/review scope | Outcomes | Findings |
|---|---|---|---|---|---|---|
| Barrett et al., 201759 | USA |
Feasibility study1 Simulation and ‘live’ phase |
Audio-visual communication (iPad) EMS clinician supporting ambulance clinician assessment of patient |
Stroke patients (live phase) |
Completion of NIHSS assessment Time to conduct NIHSS assessment Staff satisfaction |
NIHSS completed in 13/14 cases Video signal dropped periodically NIHSS assessment completed in average of 7.6 minutes Both neurologists and ambulance clinicians reported high satisfaction with prehospital video triage |
| Bergrath et al., 201161 | Germany | Feasibility study |
Transmission of vital signs and 12-lead ECG data Audio-visual communication EMS physician in teleconsultation centre supporting assessment of patient in ambulance |
157 emergency ambulance calls |
Completion of assessments Clinicians assessed technical performance of system (quality of audio and visual signal, background noise, etc.) Degree of cooperation between ambulance and hospital EMC physicians |
97% of video calls completed successfully Quality of video signal rated highly EMS clinician contributed to decisions on several occasions |
| Bergrath et al., 201360 | Germany | Prospective, observational study |
Transmission of blood pressure, 3-lead ECG, 12-lead ECG data EMS physician in teleconsultation centre supporting assessment of patient in ambulance (either by ambulance clinician or EMS physician) |
35 emergency ambulance calls (i.e. many not stroke), used audio-visual consultation |
Duration of consultation Patient conditions addressed Stage at which consultation commenced (e.g. without onsite EMS physician, while awaiting one, or once one arrived) |
Mean duration of consultations 24.9 minutes 3/35 calls involved a diagnosis of neurological emergency 26/35 calls commenced without or while awaiting on-scene EMS clinician Conclusion that this approach is feasible for a range of emergency conditions |
| Chapman Smith et al., 201663 | USA |
Feasibility study Simulation |
Audio-visual communication (using iPad) between trained NIHSS assessors and either prehospital clinicians or study investigators | Actors performing scripted stroke scenarios |
Signal reliability Completion of NIHSS assessment Reliability of NIHSS scoring (ambulance vs. bedside) |
All 27 calls and NIHSS assessments completed without significant interruption High correlation of ambulance and bedside NIHSS ratings (0.96) |
| Chapman Smith et al., 201962 | USA |
Feasibility study Simulation |
Audio-visual communication between neurologists using tablets and ambulance fitted with dedicated audio-visual system | Actors performing scripted stroke scenarios |
Interruptions of signal Clinician ratings of audio-visual quality and acceptability of service Obtaining clinical data and NIHSS score (compared with bedside/script-based NIHSS assessments) |
91% of calls were completed Variable assessment of signal quality stability, and safety Moderate agreement between remote vs. script-based NIHSS scores |
| Eadie et al., 201564 | Scotland | Feasibility study | Audio-visual communication to support stroke clinicians conduct remote assessments in different parts of the rural highlands, with a focus on mobile vs. static calls | Healthy volunteers performing scripted stroke scenarios |
Reliability of signal Accuracy of decision about eligibility thrombolysis Time to decision about thrombolysis |
Drops in signal in 47% of calls, but resumed in all cases, with delays of 2–3 minutes in assessment No difference in accuracy or time taken in completing remote assessments in mobile and static calls |
| Felzen et al., 201765 | Germany | Feasibility study |
Transmission of vital signs and 12-lead ECG data Consultation report printout in ambulance Audio-visual communication and still images to allow EMS physician in teleconsultation centre supporting assessment of patient in ambulance (either by ambulance clinician or EMS physician) |
539 ambulance emergency calls (33 stroke cases) |
Reliability of different transmissions (e.g. malfunctions, impact on quality of communication) Clinical value of communication sources, quality of audio-visual signals, background noise |
Transmissions of all information types successful in > 90% of cases Clinicians rated images and videos as being of significant clinical value |
| Joseph et al., 202166 | USA |
Feasibility study Simulation |
Audio-visual communication (via laptops at each end) to let a neurologist and nurse support ambulance clinician in simulated assessment | 13 simulated stroke consultations |
Communication (verbal/non-verbal) between ambulance clinician, neurologist, nurse and patient Types of interaction (requests for information/confirmation, giving instruction, repetition, camera movement, hand or facial gestures) Responses to disruptions in communication |
82% communication verbal Neurologist, ambulance clinician and patient equally involved in discussion Disruption in 8% of all interactions, with 44% of these being communication-related |
| Lippman et al., 201667 | USA |
Feasibility study Simulation |
Audio-visual communication (via iPad) with portable Wi-Fi. Permitting communication between hospital and ambulance to permit NIHSS assessment | 30 simulation sessions |
Sustained audio-visual signal Audio-visual signal quality |
Signal was sustained and audio-visual signal was of sufficient quality to permit NIHSS assessment |
| Mort et al., 201668 | Scotland |
Feasibility study Simulation; preliminary findings |
Ambulance technology to send live transcranial ultrasound images and audio-visual stream to stroke unit (to assess potential for prehospital thrombolysis) | 23 simulation sessions | Feasibility of transmission of ultrasound and audio-visual signals | Variable data transfer rate, but suggesting transmission feasible |
| Rogers et al., 202169 | USA |
Feasibility study Simulation |
Audio-visual communication to let neurologist, nurse and ambulance clinician conduct full neurological assessment in ambulance | 13 simulation sessions | Observation by three human factors experts assessing usability and performance of system from human factors perspective, including error types |
Issues with usability of interface (e.g. incorrect data entry, clicking the wrong buttons, inappropriate menu selections); errors most commonly made by nurses, then neurologists Recommendations for clearer system design, including clear labelling, highlighting errors, interface layout, system automation |
| Torres Zenteno et al., 201670 | Spain |
Feasibility study Simulation |
System to let ambulance clinicians alert stroke team, including videoconferencing to let neurologist perform NIHSS assessment | 3 simulation sessions | Capturing times taken for each stage of information-sharing | System seems feasible; technical issues include mobile network coverage |
| Valenzuela Espinoza et al., 201671 | Belgium | Feasibility study | Audio-visual communication letting stroke specialists provide 24/7 remote assessment of suspected stroke patients in the ambulance | 187 emergency calls (16 with suspected stroke) |
Completion of calls Consultation time Information transfer Diagnosis |
94% of calls completed successfully Median consultation lasted 9 minutes (IQR 8–13 minutes) 12 patients identified as having stroke or TIA; 10 confirmed by in-hospital diagnosis Information was transferred safely and reliably from ambulance to hospital |
| Van Hooff et al., 201372 | Belgium |
Feasibility study Simulation |
Audio-visual communication using laptops and cameras to let stroke clinician perform remote assessment of suspected stroke using UTSS | 41 simulated calls from ambulance exhibiting different symptoms |
Audio-visual and network signal reliability Examination times Consistency of scoring of stroke symptoms |
Signal mostly reliable (5 video freezes, but nothing preventing the assessment) Mean examination using UTSS was 3.1 minutes High inter-rater reliability |
| Yperzeele et al., 201439 | Belgium | Feasibility study | Audio-visual communication between ambulance and hospital using laptops, plus transmission of patient vital signs | 41 emergency calls of which 5 were suspected stroke (3 confirmed stroke) |
Data transfer of patient characteristics Patient diagnosis (prehospital and in-hospital) |
Prehospital diagnosis reached in 37/41 cases High agreement between prehospital and hospital diagnosis No adverse incidents or safety issues reported |
| Wu et al., 202178 | China | Observational study | Smartphone platform ‘Green’ to enable prehospital notification and communication between prehospital and ED clinicians | 8457 acute ischaemic stroke patients who underwent thrombolysis | Time from arrival at hospital to administration of thrombolysis | Significant reductions in time to administration of thrombolysis observed in patients transferred using Green system vs. patients who arrived by themselves (i.e. without prehospital notification) |
| Al Kasab et al., 202173 | USA | Pilot study | Audio-visual communication to let stroke clinicians assess suspected stroke patient remotely, including medical history, demographics, and NIHSS | 67 stroke patients who received thrombolysis: 15 patients who underwent prehospital video triage compared with 52 patients who underwent standard transfer processes (which included telephone consultation) |
Stroke onset to hospital Time from arrival at hospital to thrombolysis decision Time from arrival at hospital to thrombolysis administration |
Patients who underwent prehospital video triage had no significant difference in time to hospital, but had significantly shorter time to thrombolysis decision and administration of thrombolysis |
| Belt et al., 201674 | USA | Pilot study | Audio-visual communication, using high-definition camera, microphone and screen to let stroke clinicians work with ambulance clinicians to assess suspected stroke patients and coordinate care with acute setting | 89 suspected stroke patients |
Reliability of connection Length of remote consultation Time from when patient was last well to thrombolysis administration Time from arrival at hospital to thrombolysis administration |
Connection adequate for all but two cases Remote consultations lasted around 7 minutes for thrombolysis cases and around 4 minutes for non-thrombolysis cases Patients who underwent prehospital video triage had shorter times to thrombolysis |
| Johansson et al., 201975 | Sweden | Pilot study | Audio-visual communication to let neurologist and prehospital emergency nurses work together to support assessment of suspected stroke patients, e.g. using NIHSS | 11 suspected stroke cases |
Clinician perceptions of image and sound quality, and consistency of assessment Qualitative research with nurses |
Clinicians felt images were good or very good and were confident in uniformity of assessments Nurses split on whether to develop service further owing to operational interference and unclear efficacy |
| Liman et al., 201276 | Germany |
Pilot study Simulation |
Audio-visual communication system built into ambulance (including head and body camera) to permit remote assessment by stroke physician | Actors displaying different stroke symptoms |
Completion of NIHSS Reliability of remote NIHSS assessment vs. stroke physician assessment of video recorded in-ambulance |
NIHSS completed in 12 of 30 calls Moderate reliability of remote NIHSS assessment in remaining 12 calls |
| Wu et al., 201477 | USA |
Pilot study Simulation |
Audio-visual communication to let vascular neurologists conduct assessment (e.g. using NIHSS) of suspected stroke patients while being conveyed by fire department | 40 simulated scenarios performed by actors in ambulance |
Reliability of technology (i.e. to permit completion of assessment) Reliability of assessment (i.e. agreement between remote assessments vs. independent neurologist assessment of scripted scenarios) |
85% of assessments completed without major technological interruption 90% agreement between remote assessment and independent assessment of scripts |
| Bergrath et al., 201279 | Germany | Prospective study | Audio-visual communication, plus transmission of still pictures and vital data, letting emergency physician support assessment of patient in ambulance | 18 stroke patients undergoing prehospital video triage; 46 control stroke patients attended by a prehospital emergency car and ambulance |
Timings of assessments Technical assessment of system Diagnosis |
No significant difference between patients undergoing prehospital triage and control group in terms of time onsite, time to hospital and time to scan |
| Drenck et al., 201980 | Denmark | Prospective study | Prehospital assessment of suspected stroke patients, including onsite ECG, consultation with neurologist in hospital | 520 suspected stroke cases | Factors contributing to increased/decreased on-scene time | On-scene time lower when ECG conducted in hospital, other processes conducted in transit rather than onsite and when communication with hospital neurologists was rated as good |
| Eder et al., 202181 | Germany | Prospective study | Audio-visual communication (using hand held and desktop PCs) to support communication between stroke clinicians and ambulance clinicians in assessing suspected stroke patients | 845 acute ischaemic stroke patients |
Time from arrival at hospital to brain scan Time from arrival at hospital to thrombolysis administration |
Arrival to brain scan was significantly lower in people who underwent prehospital video triage No significant difference in arrival to thrombolysis times |
| Mazya et al., 202084 | Sweden | Prospective study | Telephone-only consultation between ambulance and stroke clinicians, to support diagnosis of potential for mechanical thrombectomy and decision-making on patient destination (i.e. to primary stroke centre or comprehensive stroke centre) | 2905 suspected stroke patients |
Accuracy of diagnosis of large-artery occlusion (i.e. suitable for mechanical thrombectomy) Delivery of mechanical thrombectomy (time from onset) Delivery of thrombolysis (time from onset) |
87% accuracy of diagnosis of large-artery occlusion Prehospital telephone triage associated with significantly lower time from onset to thrombectomy, no significant change in onset to thrombolysis |
| Felzen et al., 201982 | Germany | Retrospective study | 24/7 service, including transmission of vital signs and 12-lead ECG data. Audio-visual communication and still images to allow EMS physician in teleconsultation centre supporting assessment of patient in ambulance (either by ambulance clinician or EMS physician) | 6265 emergency calls (of which 1049 neurological conditions; stroke unspecified) |
Number of teleconsultations Number of complications Number of transmission malfunctions |
Use of prehospital triage increased over time Only 6 adverse events reported Transmission malfunctions were uncommon, with the highest occurring in audio communication (1.9%) |
| Quadflieg et al., 202085 | Germany | Retrospective study | 24/7 service, including transmission of vital signs and 12-lead ECG data. Audio-visual communication and still images to allow emergency physician in teleconsultation centre supporting assessment of patient in ambulance (either by ambulance clinician or EMS physician) | 1218 emergency calls (including 584 patients who underwent prehospital video triage and 634 patients treated by onsite emergency physician) | Concordance of prehospital diagnosis with diagnosis at end of hospital stay | No significant difference between concordance of diagnoses provided by onsite emergency physician and remote emergency physician |
| Schröder et al., 202186 | Germany | Retrospective study | 24/7 service, including transmission of vital signs and 12-lead ECG data. Audio-visual communication and still images to allow emergency physician in teleconsultation centre to support assessment of patient in ambulance (either by ambulance clinician or EMS physician) |
10,362 emergency calls using prehospital video triage Of these, 2007 life-threatening calls (of which 890 involved stroke) |
Change in vital signs, pre and post prehospital video triage consultation |
Significant improvements in vital signs overall 96% of 890 stroke cases could be managed by the remote emergency physician |
| Verma et al., 201087 | Canada | Retrospective study | ‘Patching’ to let stroke clinicians support ambulance clinicians in decision-making about ‘false positives’, including stroke patients who are not eligible for thrombolysis | 2966 stroke patients conveyed by ambulance | Proportion of ‘false positive’ stroke patients, comparing patients where there was prehospital patch with stroke clinician and where ambulance clinicians applied assessment alone | Proportion of false positives was significantly higher when ambulance clinicians did not receive prehospital input from stroke clinicians |
| Valenzuela Espinoza et al., 201741 | Belgium | Cost-effectiveness model | Prehospital video triage allowing prenotification of stroke clinicians and a range of patient data from the ambulance | 2282 stroke patients from Brussels stroke registry | Cost-utility model measuring costs and quality-adjusted life-years, driven by assumptions about reduced time to key interventions and resultant improvements in patient outcomes | If time gains are greater than 6 minutes, the model estimates that prehospital video triage is cost-effective. If time gains exceed 12 minutes, it becomes dominant (i.e. saving cost and improving outcomes) |
| Hölscher et al., 201383 | – | Concept paper |
Discussion of potential of prehospital transcranial ultrasound scans Brief discussion of evidence related to prehospital video triage |
– | – | Proposal that prehospital ultrasound may be less costly than mobile stroke units and less technologically challenging than prehospital video triage |
| Seah et al., 201988 | – | Concept paper | Description of development of online platform to allow all clinicians associated with stroke pathway to communicate | – | – |
Outline of communication, principally involving instant text-messaging, but with function of sharing images or videos Summary of key roles across stroke pathway |
| Amadi-Obi et al., 201489 | – | Review | Telemedicine (not just prehospital video triage) related to trauma, myocardial infarction, and stroke | Studies from 1970–2014 | Outcomes of interest included cost-effectiveness, feasibility and clinical outcome |
5 studies covered communication between ambulance and hospital Review found limited conclusive evidence for effectiveness of telemedicine for emergency generally |
| Aude Bert et al., 201347 | – | Review | Prehospital management of stroke patients (not just video triage) | Review process unclear | Current approaches to prehospital stroke management, noting risks and potential benefits | Alongside other interventions, prehospital video triage discussed as feasible, but noting the limitations of 3G networks and the potential of 4G to carry a stable signal between ambulance and stroke clinicians |
| Chowdhury et al., 202190 | – | Review |
Improved triage for thrombolysis Identification of patients with large arterial occlusion (i.e. eligible for diversion to centre that provides thrombectomy) Mobile stroke units |
Systematic review and meta-analysis of papers from 2005 | Analysed impact on time to key interventions, including thrombolysis (time from onset; time from arrival at hospital) and patient outcomes (function; mortality) |
27 articles included in analysis Improved triage for thrombolysis associated with increased thrombolysis rates, reduced time to thrombolysis No impact of interventions on functional outcome or mortality |
| Fassbender et al., 201391 | – | Review | Approaches to improve timely access to acute stroke care, principally thrombolysis | Review process unclear | Role of patients/public, ambulance services (e.g. ambulance clinician triage, prenotification), future directions (including prehospital video triage) | Prehospital video triage is seen as of potential value, but mobile transmission from ambulance is identified as a significant obstacle |
| Fassbender et al., 202092 | – | Review | Approaches to improve timely delivery of mechanical thrombectomy | Review process unclear | Role of different stakeholders in timely pathway to thrombectomy, including patients/public, ambulance services and acute hospitals | Prehospital video triage discussed in relation to prenotification, noting potential for two-way communication between ambulance and stroke clinicians. The technology is described as reliable, although impact on outcomes yet to be established |
| Guzik et al., 202193 | – | Review | Use of telemedicine in different parts of the stroke pathway during the COVID-19 pandemic | Review process unclear | Use of telemedicine from prehospital through to long-term rehabilitation | Prehospital triage by remote stroke clinician has potential to support screening process, permit ambulance clinicians to focus more on COVID-19 control (e.g. PPE), and help ensure appropriate patient destination. However, evidence is required on how best to deliver these services |
| Hubert et al., 201453 | – | Review | Prehospital management of stroke in developing countries. Interventions include mobile stroke units and remote prehospital triage | Systematic review of papers from 2014 onward | In the context of prehospital video triage, main outcome was reliability of signal |
25 articles included in analysis Studies reported variable stability of signal, but noted potential of 4G networks |
| Lumley et al., 202016 | – | Review |
Technology to support ambulance clinicians in assessing suspected stroke Interventions included blood biomarkers, prehospital imaging and ‘mobile telestroke’ (including prehospital video triage) |
Scoping review of papers between 2000 and 2019 | In terms of prehospital video triage, accuracy of diagnosis, acceptability of technology, impact on delivery of interventions and patient outcomes |
19 articles included in analysis Most studied found good agreement between prehospital and final assessments Most studies reported high satisfaction with technology and a view that it was reliable No robust evidence on patient acceptance reported Some evidence suggested that time to interventions either improved through, or was not affected by, prehospital triage Little evidence reported on outcomes |
| Martinez-Gutierrez et al., 201994 | – | Review | Approaches to improve time to thrombectomy, focusing on detection, evaluation, triage and transport of patients | Review process unclear | In terms of prehospital video triage, reliability of signal and quality of communication between ambulance and stroke services |
Signal reliability reported as poor in earlier years, but indications of improvement with advances in technology Describes importance of appropriate transfer to thrombectomy-capable centres, and the potential of prehospital triage to support this |
| Mazighi et al., 201095 | – | Review |
Approaches to improve timely access to acute stroke care, principally thrombolysis Main focus on inter-hospital communication and prenotification of stroke services from ambulance Limited focus on prehospital triage |
Review process unclear | In terms of prehospital video triage, there is a brief focus on feasibility | Purely identified as a future development, dependent on improvements in image quality and signal reliability |
| Rogers et al., 201748 | – | Review | Telemedicine to support prehospital emergency care, including stroke | Systematic review of articles between 2000 and 2016 | Feasibility, diagnostic accuracy, and impact on treatment timings (time to thrombolysis) |
23 articles were selected, of which 6 focused on stroke Generally positive views of usability and quality of images High accuracy of remotely conducted NIHSS ratings Prehospital assessments associated with shorter time to thrombolysis |
| van Gaal et al., 201896 | – | Review |
Discusses approaches to improve access to thrombectomy, importantly noting that diagnosis is ‘primarily a means to support transport decision-making, not an end’ Range of interventions discussed, including real-time involvement of stroke clinicians |
Review process unclear | Potential impact on appropriate diagnosis (via NIHSS), wider eligibility for thrombectomy and destination decision-making |
Describes no evidence conducted on thrombectomy settings Draws on previous research on thrombolysis to suggest prehospital triage services are likely to be reliable and support accurate decision-making Makes a general point for implementation, relating to local requirements for sensitivity and specificity of processes, and the need to consider under- and over-triage Notes that prehospital triage is likely to disrupt ambulance and stroke clinicians’ other duties |
| Weber et al., 201597 | – | Review | Prehospital stroke care, focusing on telemedicine, thrombolysis and outcomes | Systematic review covering 2004–2015 | In terms of prehospital video triage, focus on reliability of signal to permit assessment (e.g. via NIHSS) | Reported many issues with 3G-based systems, but greater reliability of assessment via 4G systems |
| Winburn et al., 201840 | – | Review | Prehospital telemedicine, focusing on different types of care. Interventions include audio communication, transmission of data (images, patient vital data), videoconferencing, and remote monitoring | Systematic review covering 2000–2017 | Covers the trends, scope and type of telemedicine used in prehospital emergency medicine. Outcomes were not discussed | 68 papers included, of which 19 related to stroke and 12 related to prehospital video triage (i.e. videoconferencing more common in stroke than other conditions) |
| Yperzeele et al., 201439 | – | Review | Approaches to prehospital care to improve access to stroke care. Interventions include education of different stakeholders and prehospital triage | Review process unclear | In terms of prehospital video triage, accuracy of decision-making, reliability of connection, journey times and time to clinical intervention |
Reports limited evidence on prehospital video triage, with most studies simulations with healthy volunteers and relatively few ‘real-world’ studies Video consultations more accurate than telephone alone Improvements in technology suggest it is likely that prehospital triage may be delivered reliably Notes clear potential of prehospital video triage, but that data security, privacy and regulatory issues remain to be addressed |
| Item/option | NC London, n (%) | East Kent, n (%) | Total, n (%) |
|---|---|---|---|
| Q2: How long have you been an ambulance clinician for? | |||
| Less than 1 year | 8 (5.0) | 3 (4.1) | 11 (4.7) |
| 1–2 years | 33 (20.8) | 12 (16.2) | 45 (19.3) |
| 3–4 years | 44 (27.7) | 15 (20.3) | 59 (25.3) |
| 5 years or more | 74 (46.5) | 44 (59.5) | 118 (50.6) |
| Q4: How often have you used prehospital video triage? | |||
| 1–2 times | 11 (6.9) | 5 (6.8) | 16 (6.9) |
| 3–9 times | 106 (66.7) | 32 (43.2) | 138 (59.2) |
| 10 times or more | 41 (25.8) | 36 (48.6) | 77 (33.0) |
| Don’t know | 1 (0.6) | 1 (1.4) | 2 (0.9) |
| Q5: Were you satisfied with ease of use? | |||
| Strongly agree | 104 (65.4) | 20 (27) | 124 (53.2) |
| Agree | 46 (28.9) | 38 (51.4) | 84 (36.1) |
| Neither agree or disagree | 4 (2.5) | 4 (5.4) | 8 (3.4) |
| Disagree | 1 (0.6) | 6 (8.1) | 7 (3.0) |
| Strongly disagree | 4 (2.5) | 6 (8.1) | 10 (4.3) |
| Q6: Were sound and vision of sufficient quality? | |||
| Strongly agree | 54 (34.0) | 19 (25.7) | 73 (31.3) |
| Agree | 79 (49.7) | 27 (36.5) | 106 (45.5) |
| Neither agree or disagree | 14 (8.8) | 12 (16.2) | 26 (11.2) |
| Disagree | 10 (6.3) | 9 (12.2) | 19 (8.2) |
| Strongly disagree | 2 (1.3) | 4 (5.4) | 6 (2.6) |
| Don’t know | 0 (0.0) | 3 (4.1) | 3 (1.3) |
| Q7: Which problems have you experienced? | |||
| No issues | 60 (37.7) | 14 (18.9) | 74 (31.8) |
| Poor video | 26 (16.4) | 13 (17.6) | 39 (16.7) |
| Poor sound | 57 (35.8) | 26 (35.1) | 83 (35.6) |
| Poor sound and video | 14 (8.8) | 13 (17.6) | 27 (11.6) |
| Wi-Fi issues | 23 (14.5) | 13 (17.6) | 36 (15.5) |
| Other | 15 (9.4) | 8 (10.8) | 23 (9.9) |
| No answer | 18 (11.3) | 49 (66.2) | 67 (28.8) |
| Q8: Has it influenced conveyance decisions? | |||
| Yes, frequently | 50 (31.4) | 17 (23.0) | 67 (28.8) |
| Yes, infrequently | 93 (58.5) | 41 (55.4) | 134 (57.5) |
| No, never | 15 (9.4) | 12 (16.2) | 27 (11.6) |
| Not sure | 1 (0.6) | 4 (5.4) | 5 (2.1) |
| Q9: How many attempts needed to contact stroke team? | |||
| 1– 2 | 156 (98.1) | 57 (77.0) | 213 (91.4) |
| 3– 4 | 1 (0.6) | 13 (17.6) | 14 (6.0) |
| 5 or more | 0 (0.0) | 3 (4.1) | 3 (1.3) |
| Don’t know | 2 (1.3) | 1 (1.4) | 3 (1.3) |
| Q10: What if there is no immediate response? | |||
| Keep trying until call picked up | 11 (6.9) | 14 (18.9) | 25 (10.7) |
| Try up to 2 times, then revert to standard patient conveyance | 87 (54.7) | 39 (52.7) | 126 (54.1) |
| Other | 39 (24.5) | 18 (24.3) | 57 (24.5) |
| Don’t know | 22 (13.8) | 3 (4.1) | 25 (10.7) |
| Q11: Any safety concerns about prehospital video triage? | |||
| Yes | 13 (8.2) | 22 (29.7) | 35 (15.0) |
| No | 145 (91.2) | 46 (62.2) | 191 (82.0) |
| Don’t know | 1 (0.6) | 4 (5.4) | 5 (2.1) |
| Prefer not to say | 0 (0.0) | 2 (2.7) | 2 (0.9) |
| Q12: Is it an improvement on what went before? | |||
| Strongly agree | 99 (62.3) | 24 (32.4) | 123 (52.8) |
| Agree | 51 (32.1) | 26 (35.1) | 77 (33.0) |
| Neither agree or disagree | 4 (2.5) | 10 (13.5) | 14 (6.0) |
| Disagree | 1 (0.6) | 9 (12.2) | 10 (4.3) |
| Strongly disagree | 2 (1.3) | 5 (6.8) | 7 (3.0) |
| Don’t know | 2 (1.3) | 0 (0.0) | 2 (0.9) |
| Q13: Would you like prehospital triage to continue? | |||
| Yes | 153 (96.2) | 52 (70.3) | 205 (88.0) |
| I don’t mind | 3 (1.9) | 7 (9.5) | 10 (4.3) |
| Not unless aspects are improved | 2 (1.3) | 10 (13.5) | 12 (5.2) |
| No, definitely not | 1 (0.6) | 4 (5.4) | 5 (2.1) |
| Don’t know | 0 (0.0) | 1 (1.4) | 1 (0.4) |
| Q14: Should it be considered for other conditions? | |||
| Yes | 127 (79.9) | 29 (39.2) | 156 (67.0) |
| No | 10 (6.3) | 23 (31.1) | 33 (14.2) |
| Not sure | 22 (13.8) | 22 (29.7) | 44 (18.9) |
| Q15: Did you receive sufficient training? | |||
| Yes | 145 (91.2) | 31 (41.9) | 176 (75.5) |
| No | 12 (7.5) | 35 (47.3) | 47 (20.2) |
| Don’t know | 2 (1.3) | 8 (10.8) | 10 (4.3) |
| Total (all items were completed by all respondents) | 159 (100.0) | 74 (100.0) | 233 (100.0) |
| Postcode | NC London, n | East Kent, n | ||||
|---|---|---|---|---|---|---|
| 30–45 minutes | 45–60 minutes | > 60 minutes | Postcode | 30–45 minutes | 45–60 minutes | |
| E17 | 2 | CT10 | 10 | 1 | ||
| E4 | 1 | 2 | 2 | CT11 | 3 | |
| E5 | 1 | CT12 | 1 | |||
| EN1 | 8 | 3 | 3 | CT14 | 3 | |
| EN2 | 8 | 2 | 4 | CT16 | 1 | |
| EN3 | 16 | 3 | 2 | CT21 | 4 | |
| EN4 | 7 | 2 | 3 | CT5 | 1 | |
| EN5 | 9 | 1 | CT7 | 1 | ||
| EN9 | 1 | CT9 | 6 | |||
| HA8 | 1 | 2 | 1 | TN23 | 4 | |
| N10 | 1 | TN24 | 2 | |||
| N11 | 1 | TN25 | 1 | |||
| N12 | 2 | 1 | TN26 | 3 | ||
| N13 | 1 | 1 | 1 | TN27 | 3 | |
| N14 | 3 | 2 | TN28 | 3 | 2 | |
| N15 | 3 | 1 | TN29 | 7 | 1 | |
| N16 | 2 | TN30 | 1 | 3 | ||
| N17 | 4 | 4 | TN31 | 1 | ||
| N18 | 1 | 2 | CT10 | 10 | 1 | |
| N19 | 3 | CT11 | 3 | |||
| N2 | 2 | CT12 | 1 | |||
| N20 | 4 | 1 | CT14 | 3 | ||
| N21 | 2 | 1 | CT16 | 1 | ||
| N22 | 3 | 2 | CT21 | 4 | ||
| N3 | 1 | CT5 | 1 | |||
| N5 | 1 | CT7 | 1 | |||
| N6 | 2 | 1 | CT9 | 6 | ||
| N8 | 4 | TN23 | 4 | |||
| N9 | 4 | 5 | 1 | TN24 | 2 | |
| NW1 | 1 | TN25 | 1 | |||
| NW11 | 1 | TN26 | 3 | |||
| NW2 | 2 | TN27 | 3 | |||
| NW3 | 4 | 1 | TN28 | 3 | 2 | |
| NW4 | 2 | TN29 | 7 | 1 | ||
| NW6 | 2 | TN30 | 1 | 3 | ||
| NW7 | 1 | 1 | TN31 | 1 | ||
| W10 | 1 | |||||
| W8 | 1 | |||||
| W9 | 2 | 1 | ||||
| Characteristic | Region | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| RoE | NC London | East Kent | DiD | ||||||||
| Beforea | After | Difference | Beforea | After | Difference | Beforea | After | Difference | NC London minus RoE (SE) | East Kent minus RoE (SE) | |
| Number of patients admitted to HASU, n | 44,122.00 | 43,336.00 | –786 | 717.00 | 667.00 | –50 | 451.00 | 319.00 | –132 | 69.50 (793.16) | –13.00 (793.48) |
| Number of patients admitted to non-HASU, n | 415.00 | 870.00 | 455 | 62.50 | 79.00 | 17 | 1.50 | 172.00 | 171 | –438.50* (7.91) | –284.50* (–69.33) |
| Clinical interventions | DiD, % (SE) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted outcomes for age | Adjusted outcomes for sex (female) | Adjusted outcomes for NIHSS | Adjusted outcomes for type of stroke (infarction) | Adjusted outcomes for number of comorbidities (2 or more) | Adjusted outcomes for arriving by ambulance | |||||||
| NC London minus RoE | East Kent minus RoE | NC London minus RoE | East Kent minus RoE | NC London minus RoE | East Kent minus RoE | NC London minus RoE | East Kent minus RoE | NC London minus RoE | East Kent minus RoE | NC London minus RoE | East Kent minus RoE | |
| Admitted to stroke unit within 4 hours | 42.74 (12.59) | 40.29 (5.30) | 51.348 (6.38) | 42.611 (5.55) | 43.10 (10.96) | 40.95* (5.27) | 47.91 (5.41) | 24.68 (12.63) | 51.42 (7.30) | 46.47 (8.26) | 45.68 (13.37) | 33.24 (3.58) |
| Brain scan within 1 hour | 1.38 (6.79) | 24.03* (0.74) | 7.453 (0.67) | 20.88* (0.86) | 2.7 (5.91) | 23.15* (0.74) | 5.44 (0.85) | 43.48** (0.28) | 7.61* (0.16) | 15.10 (2.06) | 4.83 (4.47) | 27.87 (9.40) |
| Thrombolysis | ||||||||||||
| Given thrombolysis (all stroke types) | –5.43 (3.19) | 3.16* (0.12) | –2.018 (0.23) | 4.374* (0.16) | –4.25 (2.77) | 3.50* (0.12) | –2.96* (0.09) | –4.28 (0.54) | –1.96 (0.47) | 6.61 (0.56) | –3.33 (2.50) | 1.83 (3.73) |
| Eligible patients for thrombolysis | –5.25 (2.13) | 5.28 (0.49) | –2.69 (0.62) | 7.13 (0.57) | –4.15 (1.85) | 5.80 (0.49) | –3.30 (0.49) | –6.10** (0.01) | –2.66 (0.78) | 10.50 (1.29) | –3.62 (1.99) | 2.99 (5.45) |
| Eligible patients given thrombolysis | 0.35 (0.67) | –7.48 (0.74) | 0.45 (0.85) | –6.65 (0.74) | 0.65 (0.58) | –7.25 (0.74) | 0.53 (0.77) | –12.32 (2.59) | 0.47 (0.88) | –5.06 (0.78) | 0.69 (0.85) | –7.66 (3.12) |
| Thrombolysis (1 hour) | –11.32 (3.86) | 22.17* (0.99) | 0.84 (1.23) | 20.66* (0.97) | –1.80 (3.36) | 21.75* (0.98) | –0.27 (0.99) | 31.09 (3.75) | 0.89 (1.52) | 17.79* (0.91) | –0.85 (3.68) | 22.81 (5.43) |
| Assessed by a specialist | ||||||||||||
| Assessed by stroke physician (24 hours) | 6.16* (1.10) | 32.16** (0.12) | 8.17* (0.17) | 32.99** (0.15) | 7.4* (0.96) | 32.40** (0.12) | 7.84** (0.12) | 27.10** (0.26) | 8.18* (0.25) | 34.51** (0.44) | 7.70 (0.93) | 31.23 (2.51) |
| Assessed by a stroke nurse within 24 hours | 2.22* (16.01) | 16.01* (0.37) | 3.91 (0.42) | 16.88* (0.36) | 3.7** (0.37) | 16.25* (0.37) | 3.82 (0.39) | 10.77 (1.63) | 3.93 (0.40) | 18.53** (0.24) | 3.85* (0.09) | 15.45 (3.01) |
| Swallow screen within 4 hours | 19.06 (5.30) | 31.27 (2.59) | 23.69 (3.09) | 32.24 (2.70) | 20.30* (4.62) | 31.55 (2.57) | 22.28 (2.65) | 24.67 (6.29) | 23.71 (3.47) | 33.81 (3.98) | 21.29 (5.84) | 27.99* (1.22) |
List of abbreviations
- 4G
- fourth-generation broadband cellular network technology
- A&E
- accident and emergency
- ACM
- Association for Computing Machinery
- CAG
- Clinical Advisory Group
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CT
- computerised tomography
- DiD
- difference-in-differences
- DTN
- door-to-needle
- ECG
- electrocardiogram
- ED
- emergency department
- EKHUFT
- East Kent Hospitals University NHS Foundation Trust
- EMS
- emergency medical services
- EQ
- evaluation question
- FAST
- Facial drooping, Arm weakness, Speech difficulties and Time
- GP
- general practitioner
- HASU
- hyper-acute stroke unit
- HRA
- Health Research Authority
- HSDR
- Health and Social Care Delivery Research
- IQR
- inter-quartile range
- ISDN
- Integrated Stroke Delivery Network
- IT
- information technology
- K&CH
- Kent and Canterbury Hospital
- LAS
- London Ambulance Service NHS Trust
- MMAT
- Mixed Methods Appraisal Tool
- MSU
- mobile stroke unit
- NC
- North Central
- NHNN
- National Hospital for Neurology and Neurosurgery
- NIHR
- National Institute for Health and Care Research
- NIHSS
- National Institutes of Health Stroke Scale
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- PRISMA-ScR
- PRISMA for Scoping Reviews
- QEQM
- Queen Elizabeth the Queen Mother Hospital
- RAP
- Rapid Assessment Procedures
- RCT
- randomised controlled trial
- RoE
- the rest of England
- RSET
- Rapid Service Evaluation Team
- SECAmb
- South East Coast Ambulance Service NHS Trust
- SSNAP
- Sentinel Stroke National Audit Programme
- TIA
- transient ischaemic attack
- UCL
- University College London
- UCLH
- University College London Hospitals NHS Foundation Trust
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/IQZN1725).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
