Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number HSDR 17/49/42. The contractual start date was in January 2019. The final report began editorial review in August 2022 and was accepted for publication in April 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Long-Sutehall et al. This work was produced by Long-Sutehall et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Long-Sutehall et al.
Structure of the report
This report has 3 sections and 10 chapters. For this report, the WP (illustrated in Figure 1) and data arising from each stage (S) will not be presented in the order they are laid out in Figure 1. The layout in Figure 1 was established at the start of the study in order to facilitate project planning. Instead, the report will follow a narrative as follows:
-
Section 1 comprises three chapters. Chapter 1 provides the background and introduction to the study and the research questions and objectives guiding the study; Chapter 2 outlines the study methodology and study design, including details of partner research sites, participants, data management and analysis. Chapter 3 delivers a review of the extant literature specific to the context of the study.
-
Section 2 comprises four chapters which combine all findings from service providers and service users and includes the methods, findings and commentary of findings related to associated WP and stages (S). Each chapter is supported by tables, figures and quotes from participants. Chapter 4 presents the findings of the retrospective note review (WP1S1). Chapter 5 presents the findings from interviews with service providers, participant observation in research sites and investigation of existing clinical and policy information regarding ED (WP1S2). Chapter 6 reports findings from the national survey with service providers (WP1 and 2), and Chapter 7 presents findings from service users and recommendations for improving ED-related support for these groups. Recommendation for practice related to all service providers is outlined in the conclusion of Chapter 6, and service users’ findings (see Chapter 7).
-
Section 3 comprises three chapters. Chapter 8 presents the development and evaluation process for identifying priorities for intervention development through a TEC. Chapter 9 provides a description of the resulting complex service development intervention, the STEPS. Chapter 10 presents a detailed discussion of key findings, and their implications for future service development research, concluding with a review and reflection on PPI involvement, Equality and Diversity, study limitations, acknowledgements and statement of ethical approval.
Because of the mixed-methods nature of this project, involving multiple participant groups and addressing different aspects of health service development, we have structured each chapter so that it includes a discussion of findings and implications for practice. This is to ensure that specific points are summarised and made explicit prior to the overarching discussion in Chapter 10, which focuses on bringing together the broad scope of the project. Chapter 10 therefore draws on points introduced in preceding chapters, with a focus on more general themes that cut across different areas of the project.
Chapter 1 Background and introduction
The need for corneal tissue – global and UK national contexts
Globally, the estimated number of people who are visually impaired is reported [by World Health Organization (WHO) databases] to be 285 million, with 39 million individuals recorded as blind, and 246 million recorded as having low vision. 1 According to Pascolini and Mariotti,1 over 10 million of those people reported as blind have bilateral corneal blindness, which could be restored with a corneal transplant. However, these individuals do not have access to the benefits of sight-saving and sight-restoring transplantation surgery, due to a shortfall in the supply of tissue (cornea and sclera) that is only available via eye donation.
According to the Royal National Institute of Blind (RNIB), over 2 million people in the UK are living with sight loss2 caused by conditions such as keratoconus and Fuchs’ corneal dystrophy, which can be treated if eye tissue is available (e.g. by corneal transplantation and reconstructive surgery). Eye tissue is also needed for research into a wide variety of eye diseases, for example endothelial failure post cataract surgery. 1,3 The RNIB reports that approximately 5000 corneal transplants are required annually in the UK to address disease and injury resulting in sight loss, with annual costs to the UK economy (unpaid carer burden and reduced employment rates) reported as £4.34 billion. 2 Critically, the organisation predicts that by 2050, the number of people with sight loss will double to nearly 4 million, mainly due to the ageing population. 2 If the burden of disease is to be minimised, it is imperative that the tissue needed to intervene in these conditions via corneal transplantation, reconstructive surgery, glaucoma surgery and research into the causes and treatment of eye disease is available.
The unique and specific case of eye donation
Addressing barriers to eye donation (ED) requires attention to the unique and specific challenges that are associated with this form of donation; for example, why do family members of organ donors frequently reject ED despite agreeing to other organs (and tissues)? Data from UK-based studies indicate that personal views of potential donors and family decision-makers are influential in triggering a decline to donate when ED is proposed. 4 Prominent concerns include potential for disfigurement,5 beliefs compatible with eyes being needed in the afterlife and/or that eyes as ‘windows to the soul’ are an essential aspect of a person even after death. 5,6 ED is also known to elicit specific disgust-type responses in some patients and family members, characterised as an ‘ick factor’ attended by feelings of squeamishness in respondents7 that is not observed in other forms of donation.
Compounding the problem of low supply is the historic lack of attention that this form of donation has received from key policy-generating organisations. For example, eye and tissue donation was not mentioned in the 2008 UK Department of Health Organ Donation Taskforce Organs for Transplants national report,8 and therefore has not featured in ongoing planning initiatives and research agendas. This lack of attention to factors acting as barriers and facilitators to ED may contribute to explaining the continuing low levels of eye tissue supply via donation.
Optimising the supply of eye tissue for use in sight-saving and sight-restoring surgery and medical research
The National Health Services Blood and Transplant (NHSBT) Tissue and Eye Services (TES) Bank (based in Speke, Liverpool) supplies most eyes for surgical purposes in the UK and aims to achieve a weekly stock of 350 so that they can provide 70 eyes every working day for use in surgery or research. From April 2021 to March 2022, donation of eyes from all sources (solid organ donation, tissue donation) generated 4555 from 2286 donors, equating to only 88 eyes per week (13 eyes per day). These levels are not supplying sufficient tissue necessary for the roughly 5000 corneal transplants required each year for conditions such as keratoconus, Fuchs’ corneal dystrophy and endothelial failure post cataract surgery. 9 The actual number of people waiting for a corneal transplant is difficult to confirm as there is no centralised waiting list for patients who need a corneal transplant (unlike in solid organ donation where there is a centralised waiting list, and the actual need may therefore be greater). The Keratoconus Society, writing in support of the current project, has reported contact with patients who often face extended waiting periods for corneal tissue to become available for transplant. A further pressure on the nationally reported donation rate of 4555 eyes (NHSBT statistics and clinical studies, November 2022, personal communication) is that approximately 30% will be discarded due to infection/viruses, with supply further compromised by a 28-day limit to storage requiring disposal of tissue thereafter.
Current UK routes of eye tissue supply
There are currently two potential routes of supply for eye tissue in the UK:
-
Route 1: Eye donation from solid organ donors – Eye donation from solid organ donors (EPSOD) continues to prove problematic, with slow progress in increasing supply from this specific cohort of donors. For example, EPSOD generated 446 eyes between 1 April 2019 and 31 March 2020. 10
-
Route 2: Eye donation from deaths outside of ICU/ED environments – Unlike tissues such as heart valves, bone, tendons and skin, eye tissue can be considered for donation even if the donor has a diagnosis of cancer, because of the avascular status of the cornea and sclera. Current data indicate that approximately 258,900 deaths in hospital11 and 25,498 annual deaths in hospices12 could potentially result in donation of eye tissue. However, from April 2021 to March 2022, NHSBT-TES only received 443 referrals from 63 hospice locations with 293 of those referrals resulting in the donation of eyes. Therefore, on average, these 63 hospices referred 7 donors each to NHSBT-TES in that year. As there are 208 hospices across the UK, there appears to be significant potential for donation within these settings that is currently unrealised.
Increasing supply is a key strategic aim for the NHSBT-TES division13 with other professional bodies including the Royal College of Ophthalmology (RCO),14 and NHSBT-TES OtAG (Ocular tissue Advisory Group)15 expressing the need for research into the barriers to eye donation and new supply routes. Therefore, in view of the low referral rates generated by palliative care services in the UK and with the aim of identifying current barriers and facilitators to ED in palliative care settings, the ED from palliative and hospice care contexts: investigating potential, practice, preference and perceptions (EDiPPPP) study was designed with specific objectives aimed at answering key questions (Table 1).
| Research questions | Study objectives |
|---|---|
| RQ1a: Potential – What is the potential for ED in HPC and HC? RQ1b: What consequences will any increase in ED from these settings have for NHSBT tissue and eye services in relation to resources/infrastructure/logistics? |
Objective 1: To scope the size and clinical characteristics of the potential ED population from research sites. Objective 2: To map the donation climate of each research site via a systematic assessment tool RAPiD. |
| RQ2: Practice, Preference and Perceptions – What system-based/attitudinal and educational barriers/facilitators to ED influence the identification and referral of potential eye donors in clinical settings and the embedding of ED in EoLC planning? | Objective 3: To identify factors (attitudinal, behavioural) that enable or challenge service providers to consider and propose the option of ED as part of EoLC planning from a local and national perspective. Objective 4: To identify service users’ views regarding the option of ED and the propriety of discussing ED as part of admission procedures or as part of EoLC planning conversations. |
| RQ3: What behaviour change strategies will be effective in increasing ED across the community of service providers and service users within HPC and HC? | Objective 5: To develop an empirically based theoretically informed intervention designed to change behaviours in relation to the identification, approach/request and referral of patients from HPC and HC for ED. |
Chapter 2 Methodology and study design
Changes to protocol – summary
Changes to the study protocol and related procedures were made in response to the COVID-19 pandemic (2020 onwards). All data collection was paused at sites on 18 March 2020 owing to the COVID-19 pandemic. Data collection resumed on 2 July 2020 following approval of a non-substantial amendment from the University of Southampton institutional ethics committee (ERGO REF – 59185).
Prior to this, amendment data collection, as per the study protocol, had been completed at two sites (S01 and S02) using in-person methods (researcher embedded at the site undertaking observation, interviews and facilitating focus groups). Following the ethics amendment, data collection recommenced using remote data collection methods. Therefore, data collection methods were adapted at four sites (S03–S06) to comply with social-distancing guidelines provided by the government, NIHR and the sponsor (University of Southampton).
Post COVID-19 ethical amendment key changes were: Data collection: WP1 and 2: all interviews with service providers and service users were conducted via telephone as the first-line option, with Microsoft Teams added as a second-line option if preferred by the participant [this was the case in several instances in hospital-based palliative care (HPC) settings where mobile telephone reception was poor, but Wi-Fi was available]. Where Microsoft Teams was used, only audio was recorded (in line with existing procedures for data collection). In-person, on-site observations ceased with the observation of multidisciplinary team meetings moving online via Microsoft Teams.
On 6 May 2021, the University of Southampton ethics committee (ERGO) approved a non-substantial amendment (ERGO ID 59185.A1) to allow the transparent expert committee (TEC) process to be conducted online using the Microsoft Teams platform, as opposed to in-person as originally stated in the protocol.
All other TEC processes were unaffected, with recruitment and consent documents being updated to reflect the new format. See Report Supplementary Material 1 for a summary of documents changed in response to both amendments.
Study design – overview
This section describes the overall study design and methods used for data collection and analysis across EDiPPPP. The project is structured in line with the six steps in quality intervention development (6SQuID) framework. 16 Study design incorporates applying qualitative17–20 and quantitative methodologies,21–23 theoretical perspectives24,25 and intervention mapping methodologies26–30 to deliver three interlinked and developmental WPs that answer the research questions and meet the study objectives (Table 2).
| Steps (6sQuID) | Research questions and objectives |
|---|---|
| Step 1: Define and understand the problem and its causes (WP1) | RQ1a: Potential – What is the potential for ED in HPC and HC? Objective 1: To scope the size and clinical characteristics of the potential ED population from research sites. Objective 2: To map the donation climate of each research site via a systematic assessment tool: the RAPiD. |
| Step 2: Clarify causes/contextual factors that are malleable (WP1 and 2) | RQ2: Practice, Preference and Perceptions – What system-based/attitudinal and educational barriers/facilitators to ED influence the identification and referral of potential eye donors in clinical settings and the embedding of ED in EoLC planning? Objective 3: Identify factors (attitudinal, behavioural) that enable or challenge service providers to consider and propose the option of ED as part of EoLC planning from a local and national perspective. Objective 4: Identify service users’ views regarding the option of ED and the propriety of discussing ED as part of admission procedures or as part of EoLC planning conversations. |
|
Step 3: Identify how to bring about change: the change mechanism
Step 4: Identify how to deliver the change mechanism (WP2 and 3) |
RQ3: What behaviour change strategies will be effective in increasing ED across the community of service providers and service users within HPC and HCS? Objective 5: Develop an empirically based theoretically informed intervention designed to change behaviours in relation to the identification, approach/request and referral of patients from HPC and HC for ED. |
| Steps 5: Test and refine on a small scale conduct a small proof of concept study (WP3) | RQ1b: What consequences will any increase in ED from these settings have for TS in relation to resources/infrastructure/logistics? |
| Step 6: Establish the evidence that the intervention would warrant a large-scale test | Objective 6: Pilot and evaluate the empirically based theoretically informed intervention described in step 4. |
Changes to theoretical perspectives
Our intention had been to apply two theoretical perspectives to the analyses of data (interviews with service providers and service users): the Theory of Paradoxical Death (ToPD)31 and Burden of Treatment (BoT) Theory. 32 It became apparent as interviews were reviewed that the ToPD was not relevant to these data, as service providers and service users did not articulate cognitive dissonance regarding the topic of ED. In addition, no carers were interviewed post death and the ToPD is specific to that situation. Similarly, BoT was not supported in patient/carer interviews as they did not perceive ED as adding to their burden of action and work as they were not aware of the option of ED and so it was not on their radar as ‘another thing to do’.
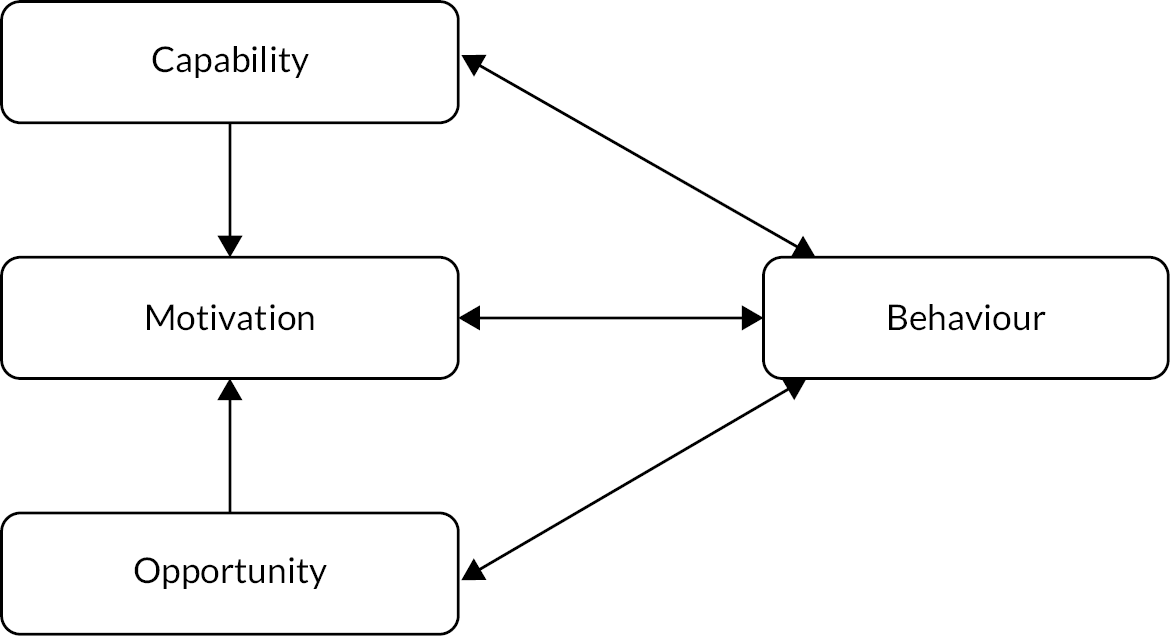
However, our hypothesis that service providers may perceive raising the issue of ED with patients as a burden was supported by our data, and for some service providers, this resulted in a decision not to raise the topic. We, therefore, drew on UK Medical Research Council guidance on the development of complex intervention studies, and sought to ‘refine [the] programme theory’ underpinning EDiPPPP in light of these and other observations encountered as the research progressed. 33 These included observations indicating: that service providers align their behaviour; and their lack of action (to raise the issue of ED with patients or family members) to knowledge gaps, missing skills, absent processes and guidance. These factors acted as barriers to ED. We, therefore, looked towards the behaviour change literature (individual and organisational) to identify relevant theory to frame intervention development. As early findings indicated that context-specific behaviour change initiatives would be a key factor in increasing the ED rates, and as the capability, opportunity, motivation – behaviour change model (COM-B) behaviours change model24 is proposed to articulate what needs to change in order for a behaviour change intervention to be effective, this theoretical framework was applied specifically in intervention design (see Chapter 9).
Project structure
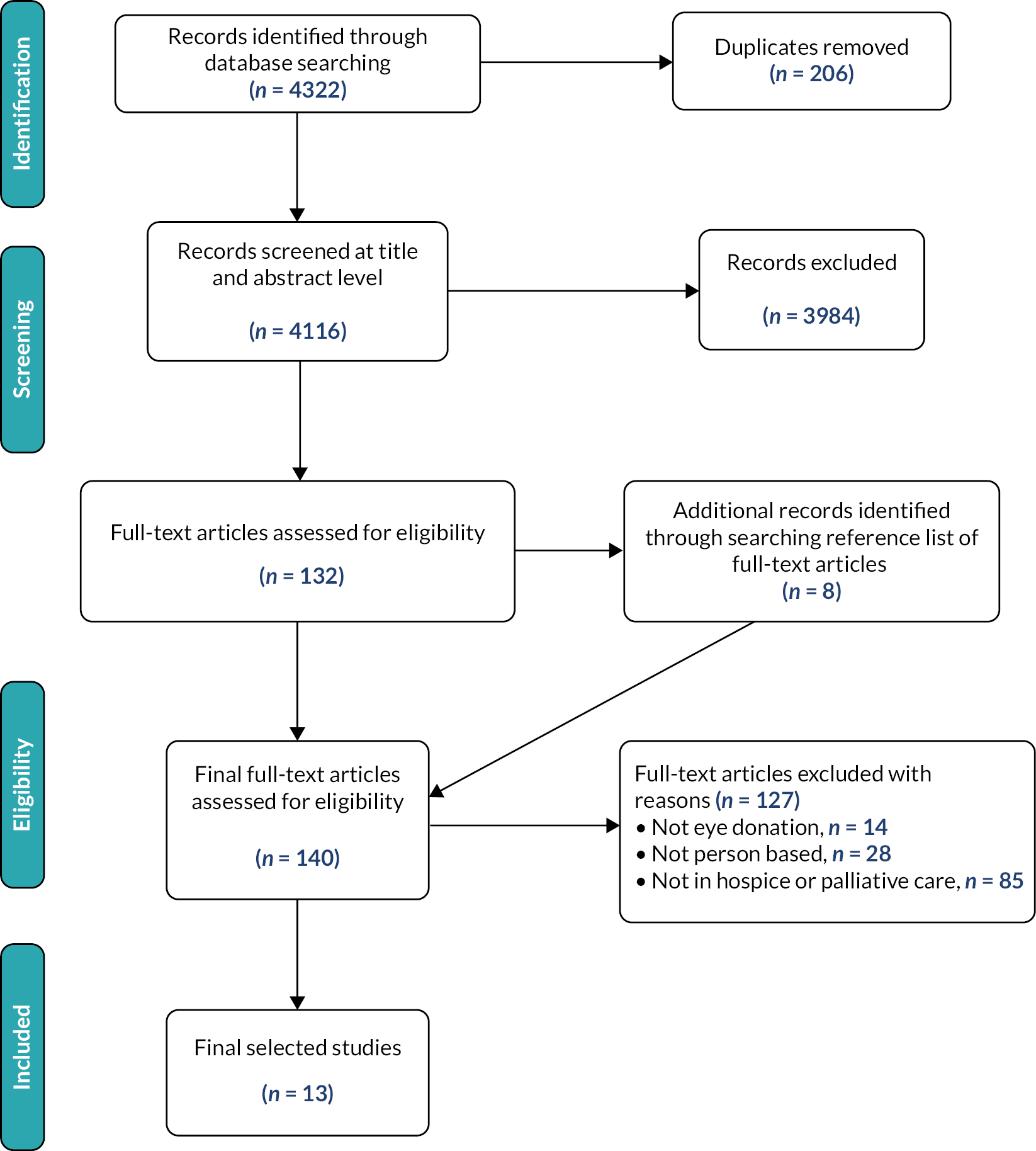
The objectives and research questions specified in Table 1 were addressed through three related WPs. Figure 1 provides an overview of these WPs and their constituent stages; henceforth, WP indicates a work package, and S indicates a stage within the WP – for example, WP1S1 indicates WP1, stage 1.
FIGURE 1.
Summary of work packages and stages for the EDiPPPP project.
Work package 1 explored the potential for, and current clinical practice relating to, ED within participating sites across England. WP1S1 involved a retrospective review of case notes from patients deceased at these sites to establish current referral rates, and clinical characteristics of patient populations. WP1S2 explored the current clinical practice and preferences of HCPs related to ED (e.g. if, when and how a conversation about ED should be initiated with patients and/or their families/carers). This stage involved interviews with HCPs in strategic and/or managerial roles (HCP-Str/Man, i.e. those actually or potentially in positions to affect organisational behaviour relating to ED) and focus groups or interviews with HCPs in front-line roles (HCP-FL, i.e. those actually or potentially involved in processes relating to ED, such as: participating in conversations with patients or providing information relating to ED, but who typically would not be involved in strategic decision-making processes affecting ED). It also involved observations of ED-related practice in clinical environments.
Work package 2 involved analysis of secondary qualitative data17 from three sources34–36 reporting hospice care (HC) and HPC stakeholders’ views of ED, findings from HCP interviews/focus groups and interviews with service users. These were used as a foundation to develop the questionnaire applied in the national survey undertaken in WP2S3, aimed at exploring the current practice, preferences and perceptions relating to ED across the wider population of HCPs in the UK.
Work package 2 also included interviews with patients and carers to explore their attitudes, knowledge and preferences concerning conversations about ED within EoLC.
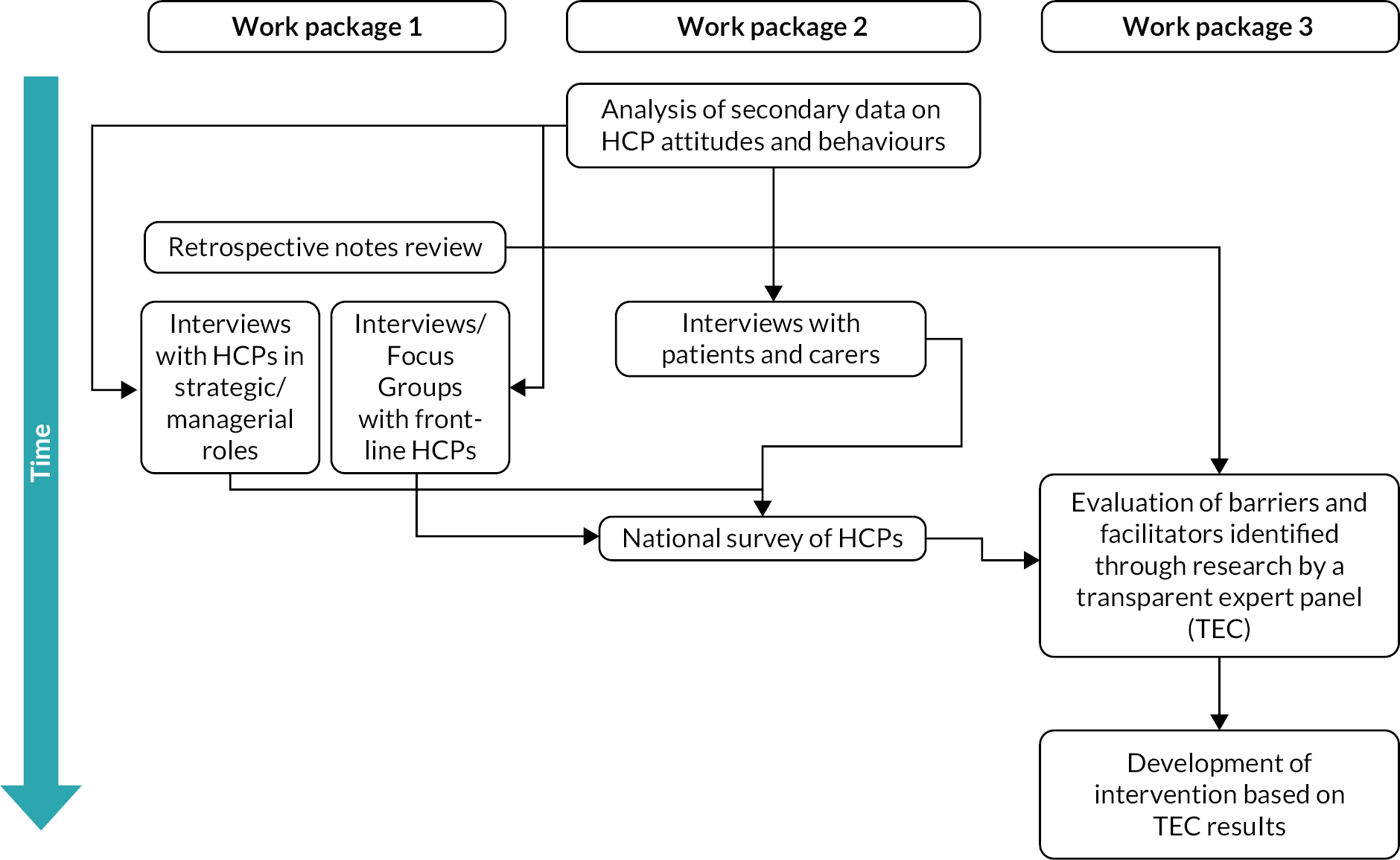
Work package 3 aimed to develop an intervention package aimed at improving ED rates, which could inform practice development and national strategy at NHSBT with respect to engagement with HC and HPC partners. WP3 involved evaluation of evidence presented in the form of reports from WP1 and 2 by a TEC37 comprised of EDiPPPP study co-applicants, patient and public involvement (PPI) representatives, researchers and EDiPPPP Project Steering Committee (PSC) members. A scalable intervention to support development of capacity for ED and embedding ED within routine EoLC practice entitled Support Toolkit for Eye donation in Palliative care Settings (STEPS) was agreed with follow-up pilot testing of two components of the operational aspects of the intervention. Figure 2 summarises the relationships between different WPs and stages across the progress of the project.
FIGURE 2.
Flow diagram summarising relationship between WP activities across the project (arrows indicate information flows between activities, i.e. how they inform each other across the project).
Partner sites and participants
Hospice care service and HPC sites in the North, Midlands and South of England were selected as study sites, informed by data indicating a difference in donation rates in these regions. 38 Donation sites were paired by region (one HC and one HPC site per region; see Table 3).
| Site1 ID | Region (England) | Site type |
|---|---|---|
| S01 | South | HC |
| S02 | South | HPC |
| S03 | Midlands | HC |
| S04 | North | HPC |
| S05 | North | HC |
| S06 | Midlands | HPC |
In describing participants from each site and activity, henceforth we use the system of anonymisation combining a participant descriptor (e.g. ‘P’ for patient interview participants) with unique ID numbers assigned in order of participation, and the associated site ID. For healthcare professionals in front-line roles, there are two descriptors (HCPF or HCPL) depending on whether the participant is involved in a focus group (‘F’ suffix) or remote interview (‘L’ suffix; Table 4).
| Participant group | Participant descriptor | Example full ID |
|---|---|---|
| Patient | P | First patient to participate at S04 = P00104 |
| Carer | C | First carer to participate at S04 = C00104 |
| Healthcare professional in strategic or managerial role | HCPI | First HCP to participate at S04 = HCPI00104 |
| Healthcare professional in front-line role | HCPF (if focus group) or HCPL (if remote interview) | First healthcare professional to participate (if focus group) at S04 = HCPF00104 First healthcare professional to participate at S04 (if interview) = HCPL00104 |
Data collection
As each WP involved differing data collection methods, including note review, participant observations, interviews, focus groups, survey and consensus methodologies (TEC), data collection methods aligned with each WP are outlined in subsequent chapters.
Data analysis
Analytic approaches for the retrospective note review, survey and TEC are presented in associated chapters. Analysis of data gained in observations, interviews and focus groups followed the five-level qualitative data analysis (QDA) method.
Data management and analysis (interview, focus group and observational data)
Following data collection, audio data from interviews and focus groups were passed to two university-approved (and contracted) transcribers who generated transcripts from an audio source. Anonymised transcription data from interviews and focus groups, and material gathered through observations, were managed and analysed using ATLAS.ti software39 following a study-specific process guided by the five-level QDA method. 40
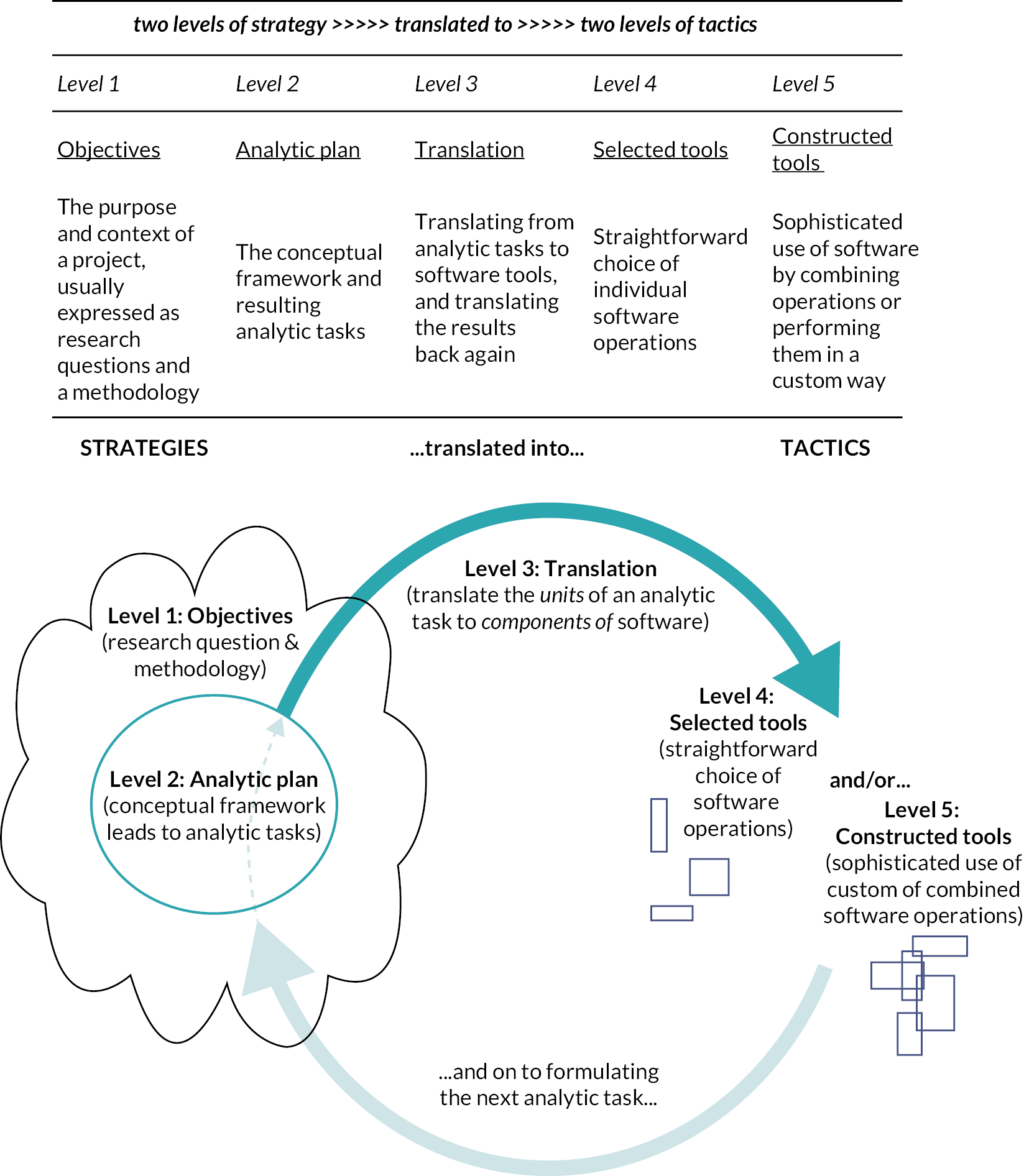
The five-level QDA method applied to all interview, focus group and observational data of HCPs, patients, and carers
The five-level method provides a framework for planning and conduct of data management, analysis and audit trail maintenance for qualitative and mixed-methods projects (Figure 3). This approach proposes two initial stages (levels) of planning (strategy) in which project objectives are defined (level 1), and specific analytic tasks relating to these objectives are identified (level 2). This is followed by an intermediary stage (level 3) in which analytic tasks are then translated into specific software operations. Following the strategic and intermediary stages, two further levels are specified with respect to use of software tools: level four involves use of single or straightforward software operations for given analytic tasks, while level five involves generating more complex (constructed) operations which may involve multiple software operations (the fifth level may not be necessary in all projects). Though the process follows a broad progression, as indicated in Figure 3, this is not strictly linear but can involve several repeated cycles across a project, in which activities at stages four and five amend study objectives (level 1) and/or analytic tasks (level 2). This framework was used in iterative development of the data management and analysis processes used in the EDiPPPP project, as discussed in the following sections.
FIGURE 3.
Components of the five-level method (images reproduced from Silver and Woolf, 201641 p. 101. n.b. permission for replication of image gained from Routledge books 1 August 2020).
Data management and analysis within the EDiPPPP project
At level 1, study objectives included in analysis are: Objective 2: to map the donation climate of each research; Objective 3: identify factors (attitudinal, behavioural) that enable or challenge service providers to consider and propose the option of ED as part of EoLC planning from a local and national perspective, and Objective 4: identify service users’ views regarding the option of ED and the propriety of discussing ED as part of admission procedures or as part of EoLC planning conversations.
At level 2, specific analytic tasks (T) were defined in relation to the objectives and data collection activities defined at stage 1, and then translated into specific software tools (either simple or complex).
T1 – Initial familiarisation and verification of data prior to loading into ATLAS.ti (software) involved reading and checking of transcripts received from transcribers against the recorded audio. The aims of this task were to verify the integrity of transcripts relative to the source audio, ensure anonymisation throughout the document and allow researchers to familiarise themselves with the data prior to beginning content analysis in ATLAS.ti (T3). These tasks were completed using Microsoft Word (Microsoft Corporation, Redmond, WA, USA) (transcriptions) and Windows Media player (audio) software.
T2 – Load and organise data into ATLAS.ti. Data were loaded into ATLAS.ti software and stored using a combination of document group (categories into which sources can be loaded for organisation) and code functions (codes are identifiers that can be applied to sources, or parts of sources, within ATLAS.ti providing an index to facilitate data management and analysis). 40 Document groups were used to organise data according to relevant attributes (e.g. site ID, participant group, work package/stage and demographic characteristics). Codes (and code groups) were used to identify parts of documents relating to specific areas of interest (e.g. specific domains and questions from interview schedules, study objectives). This process created a data structure and index for navigation, which facilitated content analysis conducted at T3.
T3 – Content analysis of organised data to address study Objectives 2–4. Content analysis of qualitative data involves identification of analytically relevant content, and organisation of these observations into categories of interest through the application of codes. 42 Both inductive codes (as derived from observations of the data) and deductive codes (applied from a pre-determined framework such as a theory, or observation schedule)42 were applied in EDiPPPP analysis. For example, T3 step 1 (Table 5) codes were aligned with components of the objective and organised into a code group covering the whole objective (see Column 3: Code group). These codes were then applied to transcription data across the data set that related to study Objective 2.
| Objective 2 | Component codes | Code group |
|---|---|---|
| To map system-based barriers to operationalising eye donation, including how potential donors are currently identified and referred to NHSBT-TES, and what services, resources, documentation are in place to: raise awareness and embed eye and tissue donation in EoLC planning. | Obj2 – Identification of eligibility | Obj2 |
| Obj2 – Referral to NHSBT | ||
| Obj2 – Services, resources, documentation for EoLC Planning |
T3, step 2 involved using the coded data from step 1 in combination with demographic codes applied at T2, to subset observations of interest by objective component and participant type. This was performed using Smart Codes, a feature of ATLAS.ti that allows data to be automatically assigned to codes based on a set of specific criteria. For example, where data had been assigned both an objective code and demographic code [e.g. the smart code (SmC) SmC1a-Obj2-Identification of Eligibility + HCP (FL) will return data coded at the code Obj2 – Identification of Eligibility and any codes within the code group HCP (FL) Focus Group/Interview Questions (HCPF)].
T3, step 3 involved inductive coding of data to provide more detailed description of content. This process proceeded sequentially through collections of data created by smart codes created at step 2. The researcher responsible for data collection within each site type took primary responsibility for analysis of resulting data (BMS for HC settings, MJB for HPC). The research team held regular meetings to discuss development of codes (i.e. new codes, revisions to codes, grouping, combinations/consolidation, etc.) and recorded relevant analytic decisions affecting interpretation in written notes attached to codes within ATLAS.ti. Subsamples of coded data were also shared with the project chief investigator (TLS), who provided further feedback on development of the descriptive coding framework.
This inductive descriptive process resulted in a set of codes derived from, and applied across, the entire data set (i.e. across objectives and participant groups). In combination with those created through deductive processes at steps one and two of T3, descriptive codes supported the of findings of this report, as described in step five below.
T3, step 4 involved the addition of further codes to allow findings to be mapped to general stages of the ED pathway: for example, Pre-referral (to NHSBT); Referral; Retrieval (of eye tissue); Post-donation; and All (for observations affecting the entire pathway). This additional deductive coding allowed for greater flexibility in exploration of and reporting from the coded data set at step five.
T3, step 5 involved reporting of descriptive analysis. This involved establishing a reporting structure in Microsoft Word in relation to each of the study objectives, their constituent components and findings relating to specific site and participant types within each of these areas (reflecting the data index created by the combination of deductive and inductive coding processes).
Chapter 3 Review of the literature
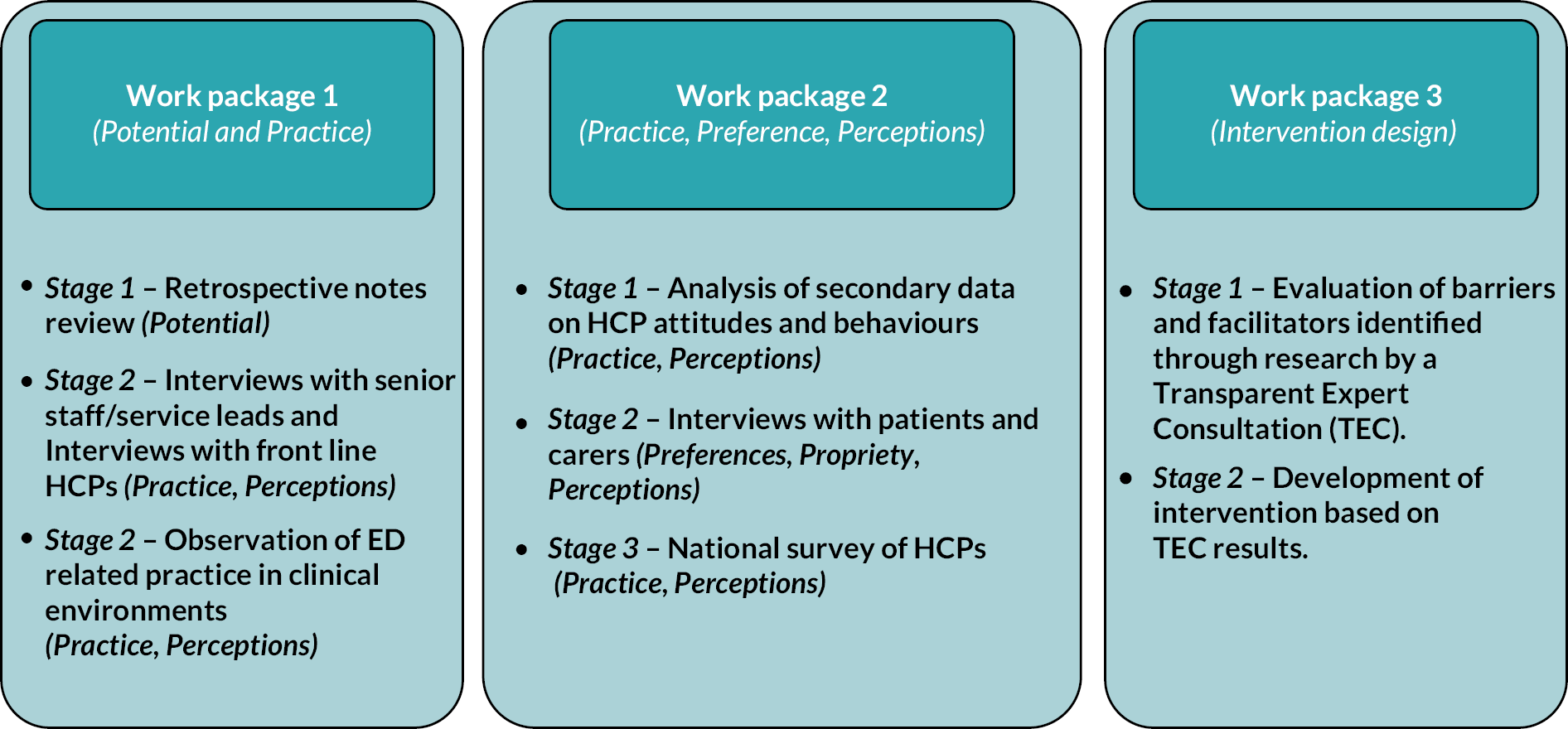
Chapter 3 provides an overview of what has been learnt from searches of the literature undertaken at specific time points in the time frame of the study, including development of the proposal (2017–18), EDiPPPP scoping review (January 2020) and a further check of the literature carried out in January 2022.
The full search strategy (see Appendix 1), inclusion criteria (see Appendix 2, Table 25), search outcomes (see Appendix 3, Table 26), study selection (see Appendix 4, Figure 14) and outcomes (see Appendix 5, Table 27) for the scoping review undertaken to seek literature specifically speaking to Perceptions and Practice in HC and HPC settings is presented. Some text in this section has been reproduced from Barriers and Facilitators to Eye Donation in Hospice and Palliative Care Settings: A Scoping Review in the journal Palliative Medicine Reports in 2021). 43 This is an open access article distributed under the Creative Commons Attribution License 4.0 (CCBY), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Supply of eye tissue is a global concern
Low levels of eye tissue are a global issue. 3 Studies from Brazil,44 France,45 the USA,46 Canada,47 Australia48 and the Netherlands49 report barriers such as low levels of referral (to retrieval services) for ED outside of areas where organ donation is carried out; negative attitude towards ED held by HCPs across a variety of care settings;48–52 and lack of knowledge among the general public regarding the needs for and uses of eye tissue for transplant and research. 53,54 There are low levels of support for this option on the Organ Donor Register (ODR) with ED being the most ‘restricted’ option (individuals can restrict which organ and tissue they would donate) on the ODR. 55 There is also evidence of HCP reluctance to raise the issue of tissue donation as part of usual EoLC discussions56–59 despite national guideline recommendations,8,60–62 and a failure to recognise potential donors due to poor knowledge among HCPs of the medical contraindications and donor suitability criteria. 63,64
Perceptions of service providers in palliative and hospice care settings towards eye donation
Healthcare providers are reported to be generally favourable towards ED, perceiving it as worthwhile. 34,47,65 Authors report that although participants felt uncomfortable discussing ED, the majority felt it was their professional responsibility to do so. 64 Authors exploring the attitudes, knowledge, practice and experiences of corneal donation across a sample of 410 HCPs respondents reported that 70% (291/410) perceived corneal donation as a rewarding opportunity for patients and/or their families, with 82% (345/410) indicating that corneal donation was compatible with their personal beliefs. 34 Furthermore, survey findings indicate that 42% (8/14) of doctors who had raised the issue of ED reported that, based on their experience, the option of ED was perceived by patients and family members as a way of giving something back to society. 66
Practice of service providers in HC and HPC in raising the option of eye donation
While HCPs often acknowledge that ED is worthwhile, evidence indicates that discussing ED is not common practice,58,65,67,68 with two surveys, including HCPs, reporting that 92% (92/100) and 93% (399/431) never or rarely raise the subject of corneal donation with patients or relatives. 34,65
Research surveying HCPs within a large UK HC setting reported that 90% of 434 staff hardly ever, or never, initiated discussions regarding corneal donation with their patients or families. 34 Other authors surveying 76 hospice staff, reported that while 49/76 (65.3%) of the staff would discuss donation if the topic was raised by relatives, ‘only one respondent reported routinely discussing the issue’ (p. 100) with family members. 35
Healthcare professionals’ reasons for not initiating conversations about ED with patients include: concerns about the impact on patients and families (i.e. potential for distress),50,58,69 perception that donation is not part of hospice culture, and the personal significance of eyes making such conversations potentially detrimental with respect to maintaining a supportive environment within the hospice,70 and a perception that donation requests could cause patients and their families physical and psychological harm. 64 However, service evaluation data from other HC settings indicate that 86% (12/14) of doctors reported that conversations did not cause additional distress with 57% (8/14) reporting that the conversations about ED were perceived by patients and families as a positive outcome from the death. 68
Service providers knowledge: assets and deficits
Healthcare professionals report knowledge deficits as barriers to raising the option of ED, including not having sufficient knowledge about the process of ED44,46,47,64 and the eligibility criteria for ED,45,48,49 and lacking confidence to initiate ED conversations. 35,50–52 While evidence confirms the facilitative impact of education and training, and that a willingness to discuss donation is positively associated with knowledge about the process of ED (referral and retrieval), and being aware of local policy and guidance,58,71 training is not a guarantee that ED would be discussed. 34
Palliative care service users’ perceptions of eye donation
Evidence about what patients feel towards discussing ED is in short supply. However, one study72 reported that HCP introduction of the topic of ED at admission to an HC setting did not elicit concerns from family members (e.g. distress or concern at the option being raised). HCPs at this site also indicated that both patients and families were not aware that they could donate. These findings are supported by work from co-applicants to the EDiPPPP study, reporting that patients within HC settings were in favour of having discussions about ED,36,73 and that some patients changed their minds regarding ED (from negative to positive) after a conversation. 65,73 Patients are reported to be willing to participate in discussions about the option of ED, but were unaware of the option of ED or assumed that they were ineligible. 65 Furthermore, participating patients were motivated to be eye donors and felt positive about the possibility of helping others. 65,73
A survey of inpatients65 found that the majority of participants, that is 73% (8/11), reported that they did not find it upsetting to discuss ED and that asking about donation enabled them to make an informed decision about donation. A further potentially important finding is that participants reported their preference to talk about ED while they were still well, rather than when deteriorating. 73
Comments from nursing logs after the introduction of an admission script that included questions about ED indicated that the patients (n = 121) and families were not aware of their eligibility to donate their eyes, but they were not concerned about the topic of ED being mentioned during admission. 66 Furthermore, nurses were positive about introducing the option of donation at admission in view of these findings. 66
Publications that reported family/carer attitudes towards donation found a lack of awareness of their dying family member’s eligibility to be a potential eye donor. 58,66 Findings indicated a range of beliefs including that donation was right, that it is a social duty to donate and that it would be ‘wasteful’ not to. 74 Family members’ decision to decline ED was based on the prior stated wishes of the patient not to donate or the family’s uncertainty about the patient’s wishes. 68,74
However, retrieved publications indicate that HC and HPC patients are generally unaware about ED and eligibility criteria. For example, in two studies, patients thought they could transmit their cancer to recipients via donated corneal tissue,73,75 or that their eyes would not be good enough for use in transplantation. 65,73,75 Furthermore, next of kin (NoK) are unaware that their dying family member with cancer could donate their eyes. 74 Retrieved evidence further indicates that not knowing the beliefs/wishes of the deceased regarding ED is a key barrier to increasing ED. 68,74
Commentary on findings – literature review
Little evidence exploring barriers and facilitators to ED from palliative and hospice care settings was available before 2001, with a limited range of study designs/evidence synthesis methodologies being adopted in the reported empirical work (see Appendix 1). The UK has generated most literature, with comparatively little literature from other countries and cultures. The USA and India reportedly supply 55% of all corneas available globally,3 and it is surprising that there is no literature from these countries.
Although the evidence available includes representation from relevant participant groups (i.e. patients, family members and healthcare providers), sample sizes are frequently small; however, the themes generated by the retrieved publications speak to recurring barriers and facilitators. To date, the available literature base is very slim with a lack of high-quality primary research adopting mixed methods of investigation/exploration that would support practice and policy development.
The retrieved evidence indicates that patients and family members are not averse to, nor distressed by, discussions around the option of ED; however, as with all end-of-life discussions, timing is key. Evidence supports the benefits in ‘introducing’ this issue at admission with this discussion being merely to assess donation status. 66
Key findings from the review were that studies that reported retrospective note reviews (n = 3) indicated that the potential for ED from HC settings was: 52/100 (52%),67 67/77 (87%) and 30/85 (35%)65 of deceased patients, while in HPC settings the potential was 229/704 (32%). 56 These figures are of concern as they clearly show that large numbers of potential donors are being cared for in HC settings in particular and that these potential sources of supply are not being realised.
This review highlights a number of key barriers to increasing ED from HC and HPC settings, including:
-
reluctance of HCPs to raise this issue to avoid causing perceived distress to patients and their NoK
-
evidenced knowledge deficits related to the process of ED in these settings
-
lack of awareness on the part of patients and family members about their own or their relative’s eligibility, donation options and wishes in relation to these.
In the next chapter, we begin our exploration of issues raised in our discussion thus far, reporting on the results of our retrospective review of deceased patient case notes from six partner sites, in order to develop a detailed and systematic understanding of the potential for ED from HPC and HC settings in the UK.
Chapter 4 Potential (retrospective note review WP1S1)
Chapter 4 responds to study Objective 1: to scope the size and clinical characteristics of the potential ED population from research sites. This chapter describes data collection, analysis and findings from a retrospective review of case notes from patients deceased within partner organisations (HC and HPC). Aims were to establish current potential, referral rates and clinical characteristics of patient populations.
Methods
Data collection
Eligibility for ED was assessed against criteria specified by NHSBT-TES (see Report Supplementary Material 2) that constitute a list of contraindications (conditions) barring the use of eye tissue in transplant operations. If patient case notes were assessed as indicating that the patient had any of the contraindications listed, then the patient would be assessed ineligible for referral for ED. Assessment of HPC or HC case notes alone can only ever provide evidence sufficient to satisfy the referral threshold, as further checks would be carried out by NHSBT-TES prior to retrieval if a patient were referred to them. Therefore, when referring to eligibility with respect to the outcome of the EDiPPPP notes review, this always refers to the threshold needed to refer to NHSBT-TES for final determination of ED eligibility.
Each clinical principal investigator (JS, CF, CR, SM, AH, JW) (from here on reviewers) was asked to assess 200 of their sites’ deceased patient notes from the previous 2 years against eligibility criteria (with FJ, SG, NS and KG also contributing to clinical review at these sites). Reviewers completed a data collection proforma in Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). 76
Proformas incorporated both closed responses and free-text (written) options (see Report Supplementary Material 3). Free-text fields were intended to capture issues not covered by closed measures, with free-text options aiming to identify contraindications that were particularly challenging for reviewers to assess with respect to ED eligibility (and thereby identify areas potential information and/or training needs).
Video guidance on proforma completion was provided to reviewers, providing an on-demand reference (created using OBS Studio screen recording software). 77 Reviewers then returned completed proformas to the study team for missing data checks (MJB). Sharing of proformas was undertaken using the University of Southampton’s secure filesharing service (SafeSend).
Data analysis
Proformas submitted to the study team (MJB) were then circulated for evaluation by specialist colleagues at NHSBT-TES (MB and JJ), using an evaluation proforma developed by the team [also completed using Microsoft Excel (see Report Supplementary Material 4)]. Evaluation was intended to assess agreement between reviewer and evaluator regarding patient eligibility for referral to NHSBT-TS for ED with respect to established criteria.
Numerical data underwent descriptive statistical analysis to identify numbers and proportions of cases deemed eligible/ineligible. Data were also interrogated with respect to differences in the assessment between reviewers and evaluators, with free-text comment boxes offering the option to comment on the decision made. All percentage figures have been rounded up or down to full numbers following the usual convention in reporting.
Results of deceased patient note review
Site characteristics
Clinical reviewers at the six partner sites completed retrospective note reviews of 1199 (missing data on one case) deceased patients’ notes for patients who had died between February 2019 and March 2021. Median deaths per year for all sites for this period was 429 (range = 120–1984 deaths per year). For HC settings, the median number of deaths per year was 250 (range = 120–386), while for HPC, median deaths per year was 513 (range = 250–1984). Notes review was completed between January 2020 and March 2021, with evaluation taking place between March 2020 and August 2021. The mean time required for review was 21.3 minutes per case (SD = 45.4; range = 12.5–27).
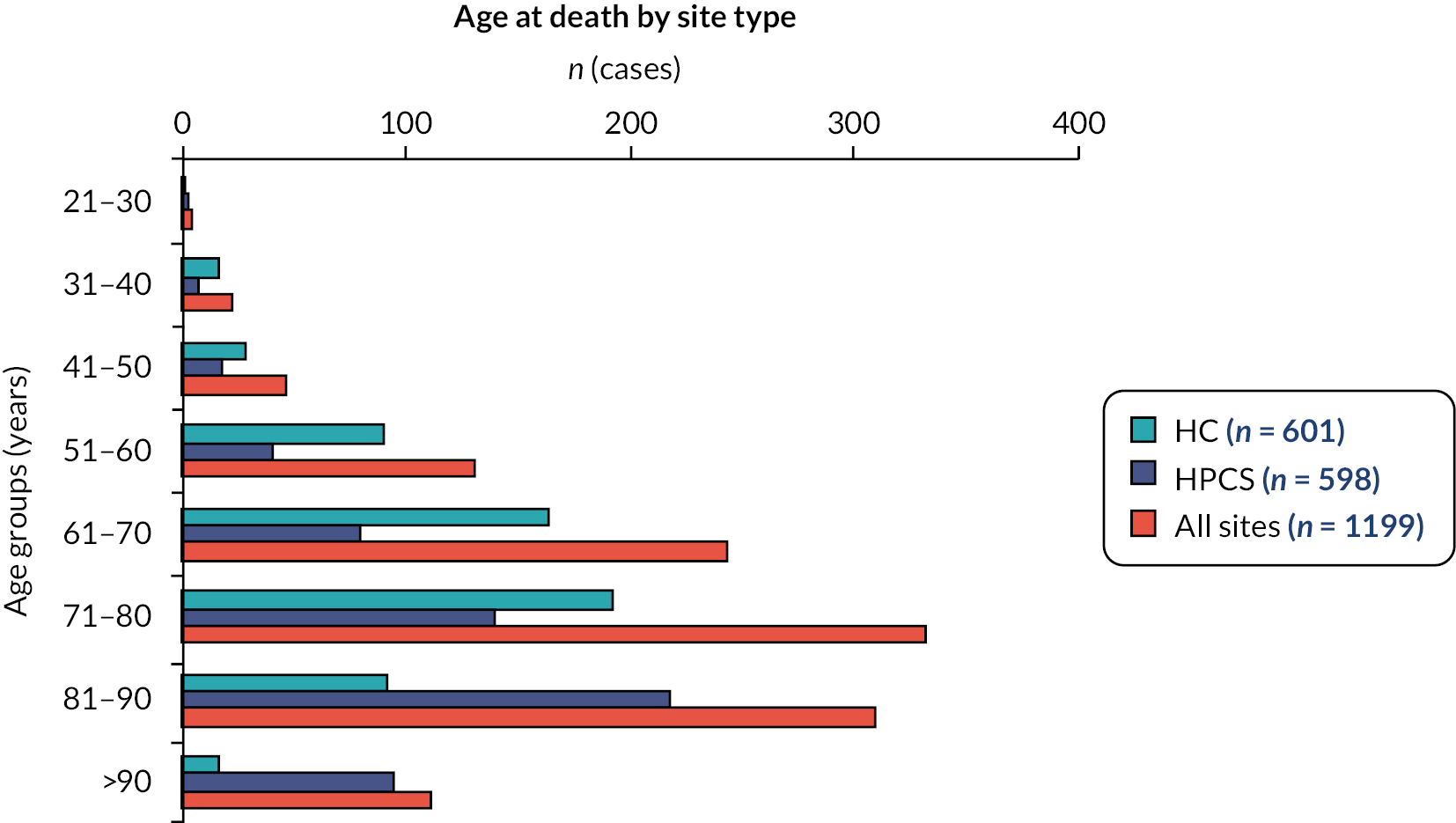
Sample demographics
For all cases (n = 1199), mean age at death was 73.4 years (SD = 13.8; range = 21–105; Figure 4). For HC settings, mean age at death was 68.9 years (SD = 12.6; range = 21–98), while for HPC this was 77.9 years (SD = 13.5; range = 21–150). Female cases represented 47.9% of the total (HC = 48%; HPC = 48%). ‘White British’ was the recorded ethnicity in 82% of total cases. Ethnic diversity was slightly higher in HC settings compared with HPC (HC = 74.0% ‘White British’ vs. HPC = 88% White British) (for full reporting of deceased patient demographics and characteristics see Report Supplementary Material 5).
FIGURE 4.
Age at death by site type.
Agreement rate on eligibility for referral to NHSBT-TES
The total agreement rate (i.e. where reviewer and evaluator agreed the same outcome, whether eligible, ineligible or uncertain re: eligibility) was 81% [n = 972 of 1199 total case (one missing case)]. Differences in outcome of eligibility assessments between reviewers and evaluators occurred in 19% (n = 227 of 1199 total cases).
Agreement rate on eligibility for referral to NHSBT-TES by site
Of the 601 deceased patients’ notes reviewed in HC the agreement rate was 79%, n = 475 cases and of the 598 deceased patients’ notes reviewed in HPC the agreement rate was 83%, n = 497.
Potential for eye donation
Forty-six per cent of (n = 553 of 1199) deceased patients’ notes were agreed by reviewer and evaluator as eligible. Twenty-four per cent (n = 289) of patients’ notes were agreed as ineligible and 11% (n = 130) were logged as uncertain (i.e. the reviewer and evaluator both indicated that further information would be needed to determine eligibility).
Potential for eye donation by site
Of the 601 deceased patients’ notes reviewed from HC settings, 56% (n = 337) were agreed as eligible, 13% (n = 77) ineligible, with 10% (n = 62) requiring further information. Of the 598 deceased patients’ notes reviewed from HPC settings, 36% (n = 216) were agreed as eligible, 35% (n = 212) of cases ineligible and 12% (n = 68) requiring further information.
Record of request for eye donation, family approach and referral to NHSBT from deceased patients’ notes
For all eligible cases (n = 553) the option of ED was recorded as being raised in only 14 cases (3%). In 337 of the eligible cases in HC, the referral rate was 8 cases (2%), and in 216 of the eligible cases in HPC, it was 6 cases (3%). Approaches to family members to discuss ED was recorded in only 13 cases (2%). There were 6 cases recorded for HC (2%) and 7 cases in HPC (3%). Referral to NHSBT-TES for ED was recorded in 14 cases (3% of all cases) with 11 cases recorded for HC (3%) and 3 cases (1%) for HPC. Finally, the ODR status of the patient was recorded in the case notes in only 5 cases (< 1% of total cases – HC = < 1%, 2 cases; HPC = < 1%, 3 cases).
Contraindications for eye donation
For all cases, ‘Intrinsic Eye Disease’ was the most frequent contraindication reported (33%, n = 391 total cases), followed by ‘Neurodegenerative disorders’ (19%, n = 229), ‘Malignancies’ (8%, n = 99), ‘Other’ contraindications (7%, n = 86) and ‘Infections’ (8%, n = 10) (Figure 5).
FIGURE 5.
Contraindications by site type.
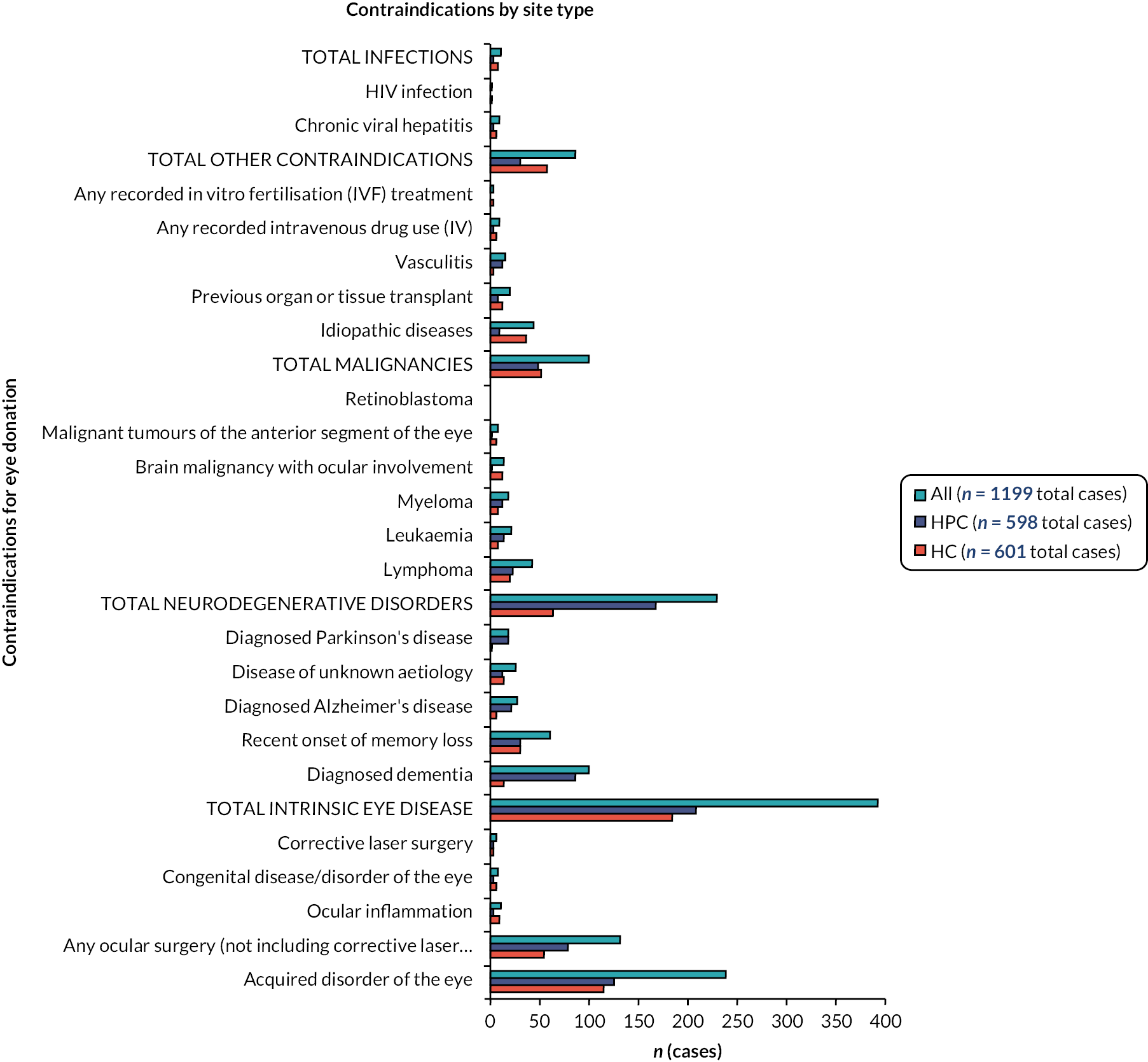
Frequencies for occurrence of contraindication types across HC and HPC sites were comparable (i.e. within a < 5% range of the other), except in the case of ‘Neurodegenerative disorders’ where the proportion of excluded cases was 17% higher in HPC settings compared with HC (11%) (see Report Supplementary Material 6 for full reporting of contraindications by site type).
Disagreement rate from retrospective note review
This section describes numbers and types of differing assessments between reviewers and evaluators as a basis for identifying and clarifying the information support needs of HC and HPC staff, in assessing eligibility for ED through clinical records. Differences in outcome of eligibility assessments between reviewers and evaluators occurred in 19% (n = 227/1199) of cases.
Disagreement rate on eligibility for referral to NHSBT-TES by site
Of the 601 notes reviewed and evaluated for HC settings, there was a disagreement rate of 21% (n = 125 cases), and of the 598 notes reviewed and evaluated for HPC a disagreement rate of 17% (n = 102 cases). The following subsections describe types of difference in assessment outcome. Reviewer decisions are reported first, followed by evaluator decisions in response.
Differences in assessment outcome where the reviewer determined eligibility for referral
Of all cases, 34 (15% of total differences in assessment) involved reviewer determination of eligibility, while the evaluator determined ineligibility or uncertainty (i.e. more information needed – HC, n = 26; HPC, n = 8). Of these cases, the majority (n = 28) involved miscellaneous reasons (e.g. ‘active ocular infection’, ‘Raynaud syndrome’) assessed as not being contraindications for ED by the reviewer but assessed as such by the evaluator.
Differences in assessment outcome where the reviewer determined ineligibility for referral
Forty-three per cent (n = 97) of differences in assessment outcome for all cases involved reviewer determination of ineligibility for ED (HC, n = 32; HPC, n = 65). Of these, 67% (n = 65) involved evaluator assessment that there were no contraindications to exclude ED referral (i.e. that the reviewer had identified factors that would not exclude a patient for ED, or that key information on which to base an ineligibility decision was missing; HC, n = 16; HPC, n = 49). For example, in 31% (n = 30) of cases in this category, reviewers had excluded a patient on the basis of ocular- or vision-related factors (i.e. cataracts, retinopathy, ‘vision impairment due to stroke’), none of which were assessed as contraindications by the evaluator.
In 27% of further cases in this category (n = 26), the reviewer had assessed the patient’s age as exceeding the upper age cut-off for ED; however, evaluators indicated that absence of excluding ocular history or other contraindications meant the patient would be eligible for referral to NHSBT. The remaining 10% of cases in this category (n = 10) involved miscellaneous reasons for ineligibility (e.g. ‘renal transplant’, ‘confusion’) assessed by the evaluator as insufficient grounds for determining ineligibility.
Differences in assessment outcome where the reviewer indicated uncertainty regarding eligibility for referral
Additional differences were found in 96 cases (HC = 67; HPC = 29) with differences in assessment where reviewers had indicated uncertainty regarding eligibility for referral (e.g. ‘unsure if myelodysplasia is a contraindication’), while evaluators indicated either eligibility (n = 51 cases all sites; HC = 34; HPC = 17) or ineligibility (n = 45 cases all sites; HC = 33; HPC = 12).
In 16 cases (HC, n = 13; HPC, n = 3) evaluators determined eligibility, while reviewers indicated uncertainty based on potential issues with eye tissue (e.g. ‘cataract surgery’, ‘ocular issues in posterior chamber of the eye’). Thirty-five further cases (HC = 21; HPC = 14) involved evaluator determination of eligibility where reviewers had indicated uncertainty for miscellaneous reasons (e.g. ‘history of asbestos exposure’, ‘Autism’). All cases in which evaluators determined ineligibility (all sites, n = 45; HC, n = 33; HPC, n = 12) involved reviewer uncertainties that were determined to be grounds for ineligibility by evaluators (reasons were miscellaneous).
Cases in which no cause of death was available
In 18 cases, no cause of death was logged on the reviewer proforma, of which 11 resulted in evaluator determination of ineligibility due to a lack of cause of death; 5 were assessed as requiring further information regarding eligibility; and 2 were assessed as eligible for referral with a note that cause of death could be determined after referral through contact with the coroner or pathologist.
Site-specific feedback
The analysis carried out by the research team facilitated generation of site-specific reports, which were fed back to the principal investigators (PIs) to provide an overview of results relating to their site. This feedback included a summary report, together with a full export of data and review/evaluation results for the site. Summary reports included information on (1) agreement rate between reviewer and evaluator; (2) acceptance rate for referral as agreed by reviewer/evaluator against assessment criteria; (3) other outcomes of assessment (e.g. cases, where the reviewer had indicated that the patient was a decline for referral to NHSBT, the evaluator indicated acceptance).
An example feedback sheet for one participating site is provided in Report Supplementary Material 7. Feedback sheets were provided prior to the TEC in WP3S1 and thus informed discussions with respect to current knowledge and processes for evaluation of ED eligibility. This process also informed the development of the Eligibility Eye Donation Assessment Checklist (EEDAC) (see Appendix 6), which is a key component of the intervention (see Chapter 9) and aims to streamline eligibility assessments of potential donors at prospective partner sites for NHSBT.
Commentary on findings
The retrospective note review reported here demonstrates significant potential for ED across HC and HPC settings, which is currently unrealised. Across 1199 cases, 553 (46%) deceased patients’ notes were agreed as being eligible for referral for ED. However, < 4% of all cases agreed as eligible recorded an approach or referral to the relevant organisation (e.g. NHSBT-TES). Potential for donation is evidenced as higher in HC (56%) than HPC (36%), potentially influenced by patients with greater complexity and comorbidities dying in hospital care settings. Our findings regarding potential are supported in the literature where authors undertaking note reviews in the UK65,67,68 and Australia48 have all identified high potential from hospice care settings [ranging from 52% and 87%,67,68 with lower potential in hospital palliative care settings (hospitals) (32%)]. 56
Key findings supporting potential practice change are that site reviewers (applying the screening tool) reached high levels of agreement with evaluators (81% agreement rate outcome for all sites). In those cases where there was disagreement (n = 113), this was due to a need for further information regarding eligibility from NHSBT-TES. For example, in 13% (n = 30) of total disagreements (n = 113), the reviewer assessed the patient as ineligible on the grounds of age as the information available to them was that the age cut-off was > 84 years and 364 days. However, the evaluator (at NHSBT-TES) subsequently determined eligibility based on the fact that the upper age limit for acceptance had changed during the life of the study to > 85 years and 364 days – information that neither reviewer (clinicians) or researchers were aware of.
This change appears to have taken place in response to the shortage of eye tissue for retrieval exacerbated by the COVID-19 pandemic (i.e. raising the age cut-off to increase the number of potential donors for referral). However, NHSBT-TES evaluators also indicated that age was NOT a definite exclusion for ED (unlike other criteria illustrated in Figure 5) but would be a consideration in decision-making influenced by patient comorbidities and physical condition at death. Therefore, it is essential that clinicians’ decision-making regarding eligibility for referral is supported by systems developed and operationalised by NHSBT-TES that provide access to relevant up-to-date information and advice and minimise additional resource burden on clinicians by providing easy and timely access to these resources. As NHSBT-TES does not currently have any information on their website specifically focused on the needs of referring clinicians (e.g. there is currently no online resource on eligibility criteria or referral processes to which clinicians can easily refer), this is a key service development gap.
Recommendations for practice
-
In view of the potential for ED in HC settings in particular, it is essential that the option of ED is routinely raised with patients and family members so that they are facilitated in making decisions that represent what may be a lifelong wish to be a donor.
-
Healthcare professionals need to proactively inform patients and their families about the option of ED because patients and their carers want the opportunity to make a choice. This information would be best provided as part of normal EoLC conversations.
-
NHSBT-TES need to develop accessible (online via their website) clinically relevant information to support service providers in the early identification and assessment of all patients admitted to HC and HPC settings against eligibility criteria, for example the EDiPPPP developed EEDAC. This website should have updates of changes to donor eligibility (e.g. the upper age limit for eye donation, current stock levels). This change will ensure that the work of clinicians is not increased, as they assess every patient who is admitted to their service for ED before making an approach to the patient.
-
NHSBT-TES need to develop easily accessible web content that clinicians can access when they have a query.
-
Clinical sites require access to the ODR so that they can assess patient status (in or out) via that resource.
Chapter 5 Perceptions, practice, preferences of service providers at research sites (WP1S1 and 2)
Chapter 5 addresses study Objective 2 to map the donation climate of each research site via a systematic assessment tool and Objective 3 to identify factors (attitudinal, behavioural) that enable or challenge service providers to consider and propose the option of ED as part of EoLC planning from a local and national perspective. This chapter describes the recruitment process and data collection methods for interviews with HCPs in strategic and/or managerial roles (HCP-Str/Man) and focus groups or interviews with HCPs in front-line roles (HCP-FL). Data collection also involved observations of ED-related practice in clinical environments. As Chapters 5 and 6 report findings from service providers, the commentary of findings for both chapters is placed at the conclusion of Chapter 6.
Methods
Sampling strategy (interviews and focus groups with HCP-Str/Man and HCP-FL participants)
As an aim for data collection was to explore the current clinical practice and preferences of HCPs related to ED (e.g. if, when and how a conversation about ED should be initiated with patients and/or their families/carers), two main participant types were targeted for recruitment: HCP-Str/Man participants were those actually or potentially in positions to affect organisational behaviour relating to ED (e.g. design and implementation of clinical/practice guidelines), while HCP-FL participants were those actually or potentially involved in processes relating to ED (e.g. advance care planning conversations with patients), but who typically would not be involved in strategic or managerial activities relating to ED.
Understanding current practice as it is enacted within organisations is a key aim of the EDiPPPP study, and it is essential to developing evidence-based complex interventions that can be adapted and scaled across different services. 33 Therefore, first steps were to establish who the people were that we needed to talk to so that we gained an understanding of differing organisational cultures and ED climate.
Mapping eye donation pathways at partner sites
Through discussions with NHSBT-TES colleagues, we identified four generic processes forming the core of the ED pathway, which could be expected to exist at all sites in some form and in which HCPs would be involved. This framework provided a foundation for discussions with PIs at partner sites and construction of a purposive sampling frame by which both HCP-Str/Man and HCP-FL participants who were actually or potentially involved in these different processes could be identified. Processes included:
-
Advance care planning (ACP) – processes relating to plans for EoLC, including wishes for donation.
-
Identification of eligibility for ED – processes within the organisation relating to identification of patient eligibility for ED (prior to contact with NHSBT).
-
Referral of eligible patients to NHSBT – processes relating to referral of potentially eligible patients to NHSBT for further assessment and potential retrieval of eye tissue post-mortem.
-
Retrieval of eye tissue – processes relating to facilitation of retrieval from eligible donors.
Discussions with PIs were held via video conference, using a whiteboard to log results of discussion regarding specific areas/services to target within the organisation (for HCP-FL recruitment) and specific individuals within HCP-Str/Man roles. Figure 6 provides an example outcome of these discussions from one HPC site. This example outlines a range of departments and areas within the organisation (indicated by square boxes) that were understood by the PI to be actually or potentially involved in activities relating to the ED pathway (indicated by coloured lines corresponding to each of the four generic stages illustrated in Figure 6). In addition, specific role groups (indicated by circular boxes) were also identified and linked to different domains. These processes and resulting diagrams were then used to identify areas for interview and focus group recruitment for HCP Str/Man and HCP-FL participants.
FIGURE 6.
Reconstructed example outcome of planning discussion for HCP-FL recruitment at a HPC site (n.b. square boxes denote candidate departments or areas for recruitment; circles indicate specific role groups; coloured lines indicate potential involvement).
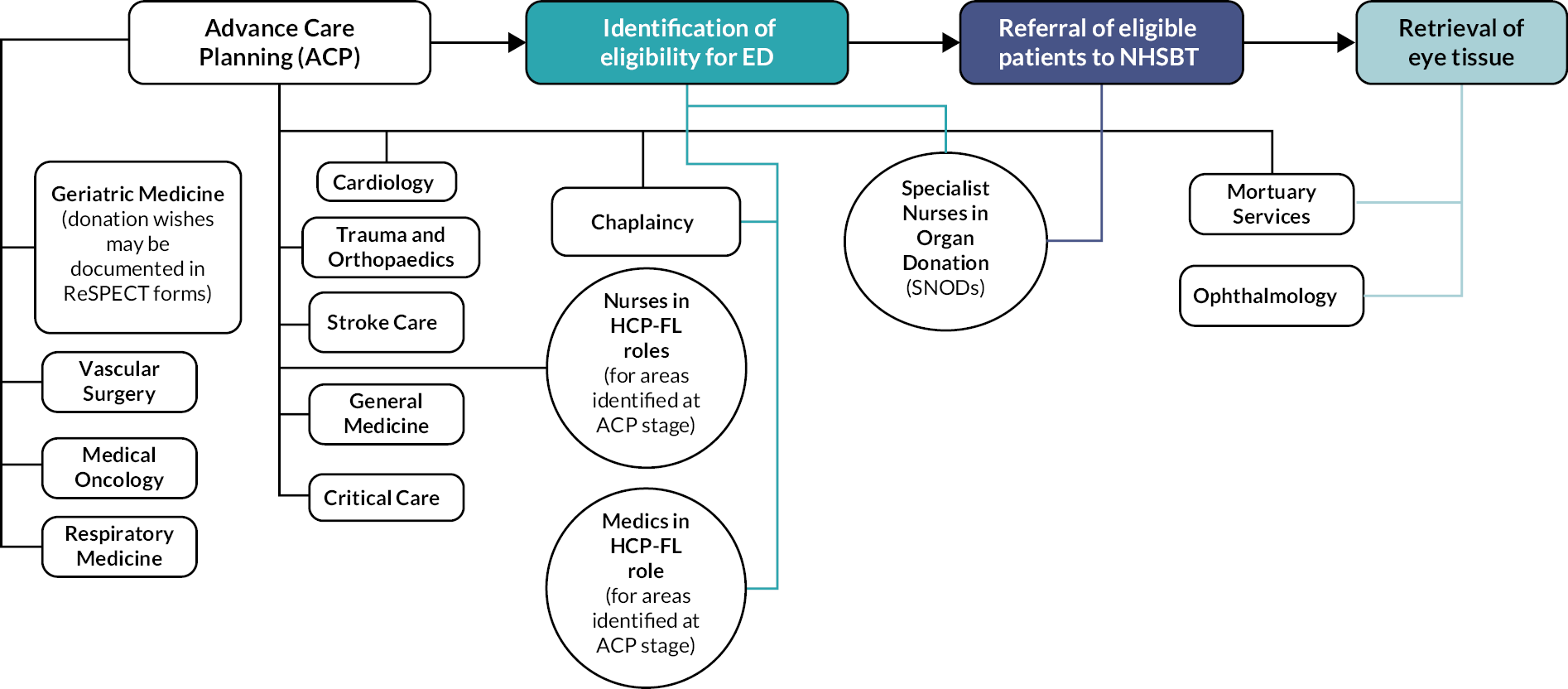
Resulting diagrams also functioned as starting points for investigation of relations between current understanding of service structure as perceived by the PI (i.e. PI understandings of who does what within their organisation in relation to the four generic stages of the ED pathway), and findings from interviews and researcher observation (i.e. do findings support and/or challenge the model of organisational structure agreed in recruitment discussions with PIs?). The significance of this to observations of clinical practice is discussed in the findings section.
Approach and recruitment process (interviews and focus groups with HCP-Str/Man and HCP-FL participants)
Approaches to HCP-Str/Man participants or to gatekeepers within areas of interest (e.g. Heads of Services) were made by the PI responsible for the specific partner site, who provided the participant information sheet (PIS). Contact details of potential participants were shared with the study team (MJB, BMS) via secure systems. Responsible researchers contacted interested participants to discuss the study and confirm participation. All study materials (e.g. letters of invitation, PIS, reply slips) were (where possible) shared with potential participants via electronic means (e.g. e-mail). In instances where this was not possible, information was mailed to the participant following a telephone conversation with the study team. All recruitment data, including demographic information and completed consent documents, were held securely on University of Southampton servers.
Once agreement was in place for the interview to commence, the responsible researcher (MJB or BMS) explained the consent process (i.e. that consent to participate would be audio recorded before the interview commenced). The researcher then read out the consent form over the telephone asking the participant to respond by stating ‘Yes/No’ or ‘I agree/disagree’ to the relevant questions. The researcher recorded (electronically) the responses of the participants on the consent form, adding a countersignature and date of consent.
Electronically returned consent forms were stored in a secure location within the EDiPPPP project drive on the University of Southampton systems, to which only the study team had access. Hard copies of returned consent forms were scanned and saved to the same folder, then shredded and disposed of securely.
Data collection: interviews and focus groups with HCP-Str/Man and HCP-FL participants
Interview schedules (see Report Supplementary Material 8: HCP-Str/man interview schedule, v2, 20 March 2019) and focus group guides (see Report Supplementary Material 9: HCP-FL Focus Group and interview guide, v2, 2 March 2019) were informed by the Rapid Assessment of hospital Procurement barriers in Donation (RAPiD),78 and the available literature.
Direct in-person observation of eye donation-related clinical practice (sites S01 and S02, pre-COVID-19)
Prior to the change in protocol (18 March 2020), observations were carried out at S01 and S02 over a 5-day period (Monday–Friday) by responsible researchers assigned to respective site types: HC (BMS) and HPC (MJB). Information gained from interviews, focus groups and naturally occurring talk informed observation of practice. For example, an interview response indicating uncertainty as to the availability of patient information leaflets for ED in publicly accessible areas of the clinical site led to further investigations by the researcher as to whether this material was in fact available. Data collection also involved identification, observation and (where appropriate) collection of materials relating to ED practice (e.g. images of publicly available information, copies of blank example process documents relating to ED).
The observation schedule (see Report Supplementary Material 10: Direct observation of ED-related practice topic guide, v1, 4 April 2019) was informed by areas of inquiry identified in the RAPiD assessment tool aimed at identifying institutional policies, procedures and other documents that facilitated evaluation of the informational climate (e.g. whether or not clear policies and procedures exist regarding ED; what information is available for patients, carers and HCPs regarding ED; what formal institutional support existed to support ED) of the site.
Observations (both in-person and remote following change to protocol) were thus informed by ongoing interviews and provided a forum to explore congruence between beliefs and knowledge about ED practice, and observable practice. Both data streams also informed a web-based audit of information on ED currently available on public-facing sites. Results and implications for service development (commentary) for each of these activities are presented below.
Findings
Outcome of recruitment
Planned targets for recruitment to interviews at each site were: 36 completed interviews total (6 per site) with HCP-Str/Man participants; and 2 focus groups per site (involving a maximum of 12 participants across both groups) with HCP-FL participants. Following the change to protocol and non-substantial ethics amendment (ERGO ID 59185) in March 2020, targets for HCP-FL participants were revised to a maximum of 10 interviews per site. In total, 105 HCPs participated: 38 HCPs in strategic/managerial roles took part (20 in HC settings, 18 in HPC settings), 67 HCP-FL participants were involved in either focus groups (28 participants) or interviews (39 participants), with 30 participants in HC settings and a further 37 in HPC settings (Table 6). For full participant demographics (see Report Supplementary Material 11).
| Participant group | Recruitment maximum target (pre-ethical amendment due to COVID-19 pandemic) | Recruitment target (post amendment) (n = 105) | Actual participants HC | Actual participants HPC setting | Total participants all sites |
|---|---|---|---|---|---|
| HCP strategic/managerial | 36 (6 per site) | Unchanged | 20 | 18 | 38 |
| HCP frontline | Two focus groups (FGs) per site (maximum 6 participants per FG) Nil interviews |
Maximum 10 interviews per site | 11 FG participants 19 interview participants |
17 FG participants 20 interview participants |
67 |
| Total | 108 | 105 | 50 | 55 | 105 |
Findings – interviews and focus groups
Findings from WP1S2 interviews and focus groups are reported under the EDiPPPP study domains Perceptions, Practice and Preferences. The purpose of this section is to focus discussion of each domain towards implications for service development and intervention design.
Findings for HCPs are combined (i.e. both Str/Man and FL participants are reported together) unless stated, in cases where relevant differences in responses were observed. Exemplar quotes have been selected to illustrate specific points and the diversity of responses that relate to a specific observation. For example, when reporting on HCP perceptions of ED, quotes are selected in this case to illustrate the range of professional, ethical and spiritual perspectives observed. Furthermore, a range of quotes are provided as they reflect both general characterisations of patterns of thinking and also thinking that may be pathway or setting specific (e.g. HCP or HPC). Context-specific data of this type illustrate the variety of HCP motivations and orientations of HCPs towards ED across EoLC settings, thereby providing information relevant to intervention design.
Quotes for HCPs in HC and HPC settings are specified by context. This is necessary because while all roles in HC settings will in some way be focused on EoLC, that is not true of all HPC participants, whose role may be only one part of a larger role within the hospital. The quote below illustrates the relevance of this presentation:
ʻSo, I don’t … I don’t think I’ve ever talked to patients about it [ED] because … because I’m in an emergency physician so, it’s usually … in my experience, unplanned death. If you see what I mean. But family members, as I say, I … in my experience, I usually … well, it’s usually them that raise it with me and therefore they usually respond well to … to knowing it’s a possibility.ʼ
(HCPI00502, HPC, Senior Emergency Medic with additional trust executive role)
We can see that this participant describes a role in which involvement in EoLC planning is limited, in a way that would not be reflected in the typical organisation of HC services. This affects interpretation of the quote because it provides a rationale as to why conversations of this type would not be typical for someone in that role. In this quote, the participant makes this context clear; however, this is not the case for all quoted material and therefore all such examples from HPC area associated with their area of service.
Perceptions
The perceptions domain of EDiPPPP relates to individual attitudes, views, opinions and experiences about donation generally and ED specifically, from a personal or professional perspective.
HCPs’ personal feelings about donating their own organs and/or tissues and organ and tissue donation were generally positive in both HPC and HC settings, reflecting a variety of professional, ethical and spiritual concerns.
ʻSo, I’m for it, I think my, my view is that once, once we die, then our spirit, if you like, separates from our body so our bodies are kind of a, what’s the word, like a vessel if you like, so I think once we die our spirit separates and it doesn’t necessarily matter what happens to our body and I think the value on what could happen for other people from using parts of my body far outweighs the concern I would have over what would happen to my body. So, for example, any part of an eye donation if that could help somebody to see or, you know, to have a better quality of life, that would be more important to me than thinking about what would happen to my body after I’ve died.’
(HCPL00303, HC)1
ʻYeah. I mean, personally, very strong and positive about organ and tissue donation. It’s clearly very important. It’s always a difficult subject to broach but one that we probably should broach more often in advance care planning. But personally, my … my views are that we should be … we need to be talking it more and also there’s been a lot of … of push from, you know, blood and transplant and things to talk about those things more. But, yeah, certainly my feelings about it are quite … you know, that it’s very important. Important to be talking about with our patients.’
(HCPL00204, HPC, Palliative Medicine)
However, while most HCPs said they were in favour of donating eyes, some reported ‘squeamish[ness]’ or reticence on the part of themselves or family members in relation to this option:
ʻOK. Personally, I’m a little bit squeamish. I’m a bit squeamish about eyes. I’m a bit squeamish about eyes because I just don’t really like eyes. The sort of … touching eyes but can see the huge advantages of donating organs for the recipients of those organs.’
(HCPI00204, HPC, Palliative Care)
ʻAnd whilst I have no issue personally donating I do still think about my eyes being tampered with because I believe when I die it doesn’t matter to me, it matters to those who are left behind and that, so my personal beliefs about funerals or my body is, it doesn’t matter to me, what does it matter to my family? My family, I then had a conversation with my family and they are very pro donation, but they also weren’t sure that they liked my eyes being tampered with, so what, what I suppose I came to the conclusion it’s important to talk about it to recognise that in lots of ways, they needn’t know very much about that and what they need to know is that I’m happy with It.’
(HCPI00201, HC)
While a majority expressed generally supportive views of ED, most HCP respondents indicated that they did not discuss the option of ED with patients. One key reason indicated by participants was the perception that they do not have the capability to handle requests for information if they raise the option of ED as part of end-of-life discussions with patients:
ʻI’ve never … had anything to do with those discussions with patients about eye donation. Don’t know if it is something that is regularly discussed with patients kind of almost routinely but I do think that hospice staff who are seeing patients both on the ward and as out patients in community we do have lots of discussions around end-of-life care and advanced care planning and about patients’ wishes into their death and their funeral arrangements and things like that, so I certainly see that we are in a good position to have those conversations about donation with our patients. It feels to me like perhaps it’s something, well that I certainly don’t have a knowledge of, if patients were, if I was to raise it with patients and they were to ask me questions about how, about the procedure and what would happen and all of that, I wouldn’t have those answers, so I feel like I lack the information at this point in time to, to have those discussions. But if I was educated about it, then I certainly would be happy to have those discussions where it felt appropriate, there’s some patients that come to us that don’t want to speak about death or dying or any of their future wishes, you know and makes it clear that they don’t want to have those discussions, so for that kind of patient it wouldn’t be appropriate, but for most people it would.’
(HCPL00205, HC)
ʻI think it’s obviously it’s a very beneficial thing for anybody to consent to do, I just think … from a hospice point of view, there’s probably not that much information available to enable us to potentially sort of pass the information on to our patients. I’ve worked at the hospice for five and a half years, I have actually witnessed one corneal donation in that time and I’m aware of one more patient who has actually volunteered to donate his eyes when he died, but that’s those are the only two patients that I’m aware of over that period, so I think it’s, … people may have been picked up early on in their care planning to give that consent rather than something that was, the hospice was involved in, so I think probably had they not given their consent earlier on in their, potentially in their advanced care planning, then those donations wouldn’t have happened. Yes, so I just think from my point of view it’s probably lack information within the hospice to be able to enable us to pass that information on to our patients.’
(HCPL00605, HC)
HCPs also indicated concerns around the propriety (appropriateness) of raising the issue of ED in case the topic was perceived as distressing by patents and family members, despite indicating that they also raised other potentially sensitive topics with patients (e.g. resuscitation options and funeral plans):
ʻThere’s a lot of patients who are coming in who are distressed for one reason or another and to bring it then up at that point is not necessarily appropriate.’
(HCPI00201, HC)
ʻI think it’s tough for them anyway, thinking about end of life, they’re having to potentially think about their funeral, their Will, there’s many things that need to be put in place. So, and I know that some people don’t want to talk about their death, or don’t want to talk about how it’s going to be, and I would imagine donation could be along that line as well.’
(HCPI00101, HC)
ʻI think, everyone is a bit afraid of having this conversation when their loved one’s just died. I think, everyone is a bit scared of touching that subject after the patient passed away.’
(HCPF00102, HPC, Acute Care)
In some cases, HCP concerns about propriety were linked specifically to perceptions about potential patient/public views that ED may be disfiguring to the body of the donor:
ʻI do feel that in my experience when I was speaking with families, or even just people that I know, a lot of people aren’t very keen for their eyes to be donated. I mean, there’s a lot of sorts of, almost like, you know: ‘the windows to the soul’ and ‘take anything but don’t touch my eye’. So, for me, there needs to be a lot more sort of positive media to promote this and to take away some of that almost fear about what the person may look like afterwards because, you know, for us obviously we can see that the patient looks … you wouldn’t even notice that they’d been removed.’
(HCPI00502, HPC, Senior Emergency Medic with additional trust executive role)
ʻYeah, I think … as I just said, I think, it’s … it’s really sensitive isn’t it because, I think, when you think of people’s eye. I guess, in people’s heads they think that organ will be removed. People will be, you know, sewn back up. You wouldn’t necessarily know that that organ wasn’t there. With the eyes, that’s very different, isn’t it? You’d … you would very much know that the eyes had been taken. So, I think, that’s where the struggle comes for … for patients and families. Feeling it very personally that that would change the outward appearance of somebody even though they have already died.’
(HCPI00504, HPC, Cancer Care HCP)
However, HCPs who indicated that they had raised the issue of ED with patients reported that this option was valued by patients; in addition, no HCP participant in interviews or focus groups described actual experiences of distress caused by raising the topic of ED:
ʻI think … because obviously, the age group I’m looking after is generally pretty much all over the age of eighty so, an older person they generally assume nothing is appropriate at that age. So, when you mention where it’s possible, corneas can be … a lot of them just aren’t particularly bothered in later life. I think probably, they make assumptions that: ‘no one will want my corneas’ at the age of whatever.’
(HCPI00604, HPC, Geriatric Medicine)
ʻSo, for some patients it’ll be straightforward because they all give you cues or they’ll be explicit about their desire for, you know, making a difference or, or being able to see some good coming from what’s happening and for me that makes it very straightforward to raise with them, opportunities to do that, whatever that might be, tissue donation, corneal donation, other things they might be able to do that would give some meaning.’
(HCPI00403, HC)
ʻPeople are really interested to hear that they can still do something and that they … they can make a difference to someone else and … and, I think, that’s probably the point where they reveal themselves as to whether they’re people that find it quite difficult to think about donating eyes as opposed to any other solid organs versus the, you know: ‘have whatever you can’ kind of philosophy.’
(HCPI00202, HPC, Palliative Medicine)
ʻIt normally goes down very well indeed. And especially with things like hospice staff because it gives them the opportunity to offer to people something positive such as eye donation where all the other transplants virtually you can’t do because you’re termed: ‘you’ve got cancer’ and a lot of people want to try and give something back. And certainly, in my experience when I spoke to families, and people prior to them dying that were interested in donation, when you can turn around and say well: ‘there isn’t anything really you can, but you can donate your eyes’. You know, I was getting … I used to get hits of about three out of every five I approached. People saying: ‘that’s brilliant’ and donating. But you’ve got to have a) the knowledge yourself and the experience, I think, to be able to approach the subject correctly with people especially when they’re terminal, and the families, because you’re approaching them at a very bad time.’
(HCPI00304, HPC, Organ and Tissue Donation HCP)
Commentary – perceptions
Our findings are compatible with those of previous studies exploring ED in HC and HPC34–36,73 settings, which indicate that perceptions of HCPs are influential as to whether ED will be raised with patients and family members as part of EoLC planning. Further, they are congruent with those from the global literature that most HCPs have favourable perceptions of ED as worthwhile both for donor recipients and as an option for patients to be discussed as part of EoLC planning. 34,64,65,68 For example, Gillon et al. 34 found, as we did, that HCPs perceived ED as a rewarding opportunity for patients and/or their families, and that ED was compatible with their personal beliefs.
Of note is that HCPs’ perception that discussing ED would cause distress was not supported, in the retrieved records from our scoping review,65,66,73,75 nor in the findings from our interviews with patients (see Chapter 7). Our findings indicate that patients are willing to participate in discussions about the option of ED but that patients are unaware of the option of ED or assume that they are ineligible due to a cancer diagnosis. Our findings support the available evidence in that although HCPs acknowledge that ED is worthwhile, evidence indicates that discussing ED is not common practice. 34,58,65,68
Practice
The practice domain of EDiPPPP relates to knowledge and behaviours in relation to processes associated with ED (e.g. knowledge of eligibility criteria for donation, behaviours such as initiation of a conversation regarding donation during ACP processes).
Knowledge – eligibility and referral
Most HCPs (managerial and frontline, in both HC and HPC settings) did not know how many people are in need of a corneal transplant in the UK:
ʻNo, sorry, If I’m really honest, no, because it’s not something that I … I kind of … falls into my … what I’m required to do at work on a … on a regular basis. So, no, I haven’t if I’m really honest.’
(HCPI00504, HPC, Cancer Care HCP)
ʻOh, gosh. No, I don’t know. I wouldn’t … I’m rubbish with figures like that I imagine a lot though. I should … I should because my husband works for (society) which is a society for the blind. We have a lot of blind clients but, I … yeah, I don’t know that information.’
(HCPL00104, HPC, Cancer Care HCP)
ʻHaven’t got the foggiest but before you asked that question, I was just thinking what we could do with this [information], and there maybe is one and I’ve never looked, but a website where it actually shows how many people need corneas, how many corneas have actually been donated and whether we’re actually supplying enough. And that’s, that’s not just to this hospice, but to all hospital and hospices across the country.’
(HCPI00201, HC)
HCPs also had varying levels of knowledge regarding the eligibility criteria that a patient needs to meet to become a potential ED. For some HCPs’, their knowledge base was informed by previous experience of organ and/or tissue donation processes through, for example, work in co-ordination roles for research and/or transplant activity:
ʻSo, I might get this wrong (laughing) so, you have to bear with me. So, obviously I know where patients have cancer they are … there are certain things they can’t donate but, I was under the impression the eyes were different so they would be able to donate their eyes. So, I would imagine it’s quite a high percentage of patients that could donate eyes or they can donate corneas.’
(HCPI00406, HPC, Cancer Care HCP)
ʻNot off the top of my head. No (laughing) … There’s so many. Eye disease would be a contraindication. I don’t know. Cancer always seems to be a contraindication but normally that should be fine for eyes. So, I … I would refer to the palliative care team who do it if I had to.’
(HCPI00402, HPC, Cancer Care HCP)
ʻPatients who have brain metastasis or brain primaries, if I remember rightly, are the ones that can’t donate their eyes. Most of the other cancer patients can. From memory I think I would have to, well no I would have check with regards to the haematological cancers, but certainly somebody with a prostate cancer or a lung cancer without widespread metastasis would be fine. There’s a slight limit on age, but I think it’s, I think it’s seventy-five or eighty-five, it’s really a lot older than you might think and to be honest, if a patient asked me, I don’t start with, well I would go through a conversation about what that entails if that’s what they’re asking.’
(HCPI00201, HC)
Yes, there’s a … a standard [eligibility] criteria that comes on the boxes and it’s also found online and on the websites. Mainly it’s any undiagnosed neurological disorders. Neurological disorders of unknown aetiology, tumours, intraocular tumours, corneal damage, corneal scarring, cerebral tumours and certain blood-borne viruses, CJD as well.
(HCPI00304, HPC, Organ and Tissue Donation HCP)
Many HCP respondents in both HC and HPC settings also indicated that they would refer to either their institutional intranets or the NHSBT national website as a source of information on eligibility criteria for ED.
Further key knowledge gaps included what a HCP needed to do to refer a patient for ED to NHSBT-TES. Most HCPs could not describe a specific established process for referring a patient, but some were aware of actions that they may need to undertake in order to do so (e.g. access patient records for identification of prior wishes and evaluation of potential eligibility, contact NHSBT-TES if the option of ED was chosen by the patient and/or family):
ʻI don’t know, that would be, I suppose that would be hopefully something that I’d be, that would be something that if we did train on it would be something that we’d be maybe made aware of I think because that would be, I would just follow a process I would imagine. I seem to think there was something from my very vague memory because I’m sure it’s only been this one page that I can think of that I think there was like a, a flow chart almost with a phone number on so that we just had to contact them, I think, but that’s, I mean this is like, I’m really having to rack my brains to think about how we did it.’
(HCPL00601, HC)
ʻHow would I go about referring somebody for eye donation, I would probably at the moment contact one of our education nurses here and find out the process or one of our research nurses might have information, there might be a clinical guideline, I’d have to have a look on our clinical guidelines, I might ask a colleague at the moment about how to go about that, our lead might have some insight, or I might ring UHL the hospitals organ donation team and find out how I could go about it.’
(HCPL00103, HC)
ʻSo, if someone has said they would like to donate their corneas, or a family has sort of given consent on behalf of someone who isn’t able to, we put it in their notes that at the point of death the [team members] should phone the NHS-BT number and we try and sort of reiterate that in every entry. The electronic records in the hospital don’t have a front screen like we do … so here in the hospice, we’ve got sort of a … a home page so that when you log in to someone’s notes you can put alerts on and it’s very obvious that someone wants to be a cornea donator. In the hospital, it’s sort … gets lost and you might put an entry but then three days later you’d have to scroll back several pages to find that entry. So, we’d copy and paste that throughout and try and make sure it’s on the nursing handover for the ward nurses at the point of death if that happens within the hospital. For them to call the NHSBT number and it goes from there.’
(HCPI00202, HPC, Palliative Medicine)
Behaviours – role-specific responsibilities, timing of eye donation-related conversations within end-of-life care pathways
When asked about who should raise the issue of ED, most participants indicated that any HCP could, in principle, be able to lead conversations; however, this was often accompanied by more specific commentary indicating that medical staff and senior nursing staff (e.g. Clinical Nurse Specialists) should be in the driving seat in terms of overall implementation and co-ordination of processes across the pathway:
ʻI think that we all have some kind of responsibility and, I think, on the protocol it does say that. That any nurse in healthcare profession can have this conversation with them. However, when they see the palliative team, they are already thinking. They’re already on that kind of mindset to have this kind of discussions. And the palliative team are already talking about them with this and about what they want to do with the family, and they give support to all of them. So, it’s just easier even for the kind of work that they do to introduce the conversation.’
(HCPF00102, HPC, Acute Care)
ʻYeah. I think, the palliative care team could. We’ve got very confident nurses and their … confident palliative care doctors as well.’
(HCPL00406, HPC, Bereavement Services)
ʻThat’s a really good question and something that is quite difficult because it has to be the person that has the right knowledge around the subject but it also has to be a person that is sensitive in their approach to how they discuss things and as I said to you before I think sometimes, not through any fault of their own but how they’re taught, doctors and medical professionals, can, can sometimes come across as a little insensitive and I think it’s just the way that they’re taught to ask questions. So, I don’t know if it would be most appropriate from them. Perhaps it might be a good thing to come from the nursing team because they are very good at that empathy and that, you know, taking their time with the patients, I don’t know whether that, that could be a priority, or perhaps maybe the team leaders like the nurses in charge could potentially support with them discussions?’
(HCPFL00203, HC)
Most HCP participants indicated that ED discussions should be undertaken as early as possible in the patient’s dying trajectory, or as part of advanced or EoLC planning:
ʻI guess, ideally before they come here [to the hospice], I think that, you know, seventy per cent of our patients will die on admission, well not on admission but, you know, during their stay here. So, I don’t think hospices should be the people who should be having that conversation hours or days before death, ideally it should be a conversation that is part of advanced planning, if the person hasn’t already stated their preferences when they did their driving licence for instance. So, I think it, it can be a question for, I mean when I go to my GP, I will have, he will have or she will have, lots and lots of information on me, you know, actually because I have at some point registered with that GP, given all my information, that information is updated and so therefore, I would hope as we move, move forward that, that’s a fundamental question that’s asked right at the outset. So, so it avoids these conversations, later on in someone’s life.’
(HCPI00601, HC)
ʻYeah. So, I think, it’s best to have these conversations earlier on because, I think, you should involve the patient in it from the earliest point because actually if you then do it at the point that the patient’s unable to communicate or has capacity to make that decision, you’re then relying on next of kin and actually their choices may not be the same as what the patients where they may never have discussed it. So, they may not know. And, I think, if people don’t know they err on the side of not having it occurring rather than: ‘let’s do it’. So, for me, it’s part of that good care of recognising someone towards the end of their life and discussions should be had at that point.’
(HCPI00102, HPC, Senior Manager)
ʻI think, it’s probably at this point when we hit the palliative care phase and, again, that’s a bit of an open-ended time span. So, you know, those conversations can be held quite … we can talk about the sort of last year of life which, again, is say not a precise science that those conversations can be held at any point where you’re starting to have in that year what we call sort of advance care planning and you’re talking about how … where the patient wants to die, what they would like to do. And at that point, is something where you could introduce that conversation so. And we tend to have those roughly in the last year of life.’
(HCPI00402, HPC, Cancer Care HCP)
There was no clear consensus on ‘when’ the option of ED should be raised and ‘who’ should raise the issue of ED. The majority of HCPs in both HC and HPC settings indicated ED was not a routine behaviour.
ʻSo, I don’t think I’ve ever talked to patients about it because I’m in an emergency physician so, it’s usually, in my experience, unplanned death. If you see what I mean. But family members, its usually them that raise it with me and therefore they usually respond well to knowing it’s a possibility.’
(HCPI00502, HPC, Senior Emergency Medic with additional trust executive role)
ʻI think I’m probably guilty of not broaching it on a routine basis, so I recognise the importance of offering the option to patients but maybe find it difficult to shoehorn that into kind of my regular day to day work. I think one of the reasons for agreeing to participate in the study was maybe to challenge myself a little bit about why I don’t discuss it or have the kind of, for me reflections on, you know, what that’s about and whether I should be doing something differently going forward, was maybe something I hope to achieve out of this research interview in some ways.’
(HCPL00103, HC)
ʻSo, we have had one or two occasions whereby patients have requested to have their eyes donated and tissue donated, and we have followed through the process, it’s been very clear, because they’ve had all the documentation, we’ve just phoned the number and then it’s been taken care of from that. I think at the moment it’s very dependent on whether the family or the patient have thought about it, a lot of patients say, you know, they thought about donating their organs and they’ve been told that they can’t donate their organs because of their progression and their type of disease with the cancer, so we sort of very clearly try to talk through it around what our policy says around eye and tissue donation.’
(HCPI00301, HC)
Healthcare professionals are generally reluctant to discuss ED and we sought to establish what they perceived as barriers to raising this issue with patients. Responses indicated concerns about their knowledge base and capability in two main areas: (1) raising the topic with patients/families; (2) the propriety of raising the topic in end-of-life conversations which focus on the needs of the patient (e.g. symptom management):
ʻAnything that would prevent me doing it? As of the moment, the reasons that would prevent me doing it is the lack of knowledge probably and as well as a lack of knowledge, the other … patients that I would … I wouldn’t raise it with, I think, it would depend on the level of distress with the family.’
(HCPI00204, HPC, Palliative Care)
ʻI can think of a number of circumstances. We’ve recently had a gentleman who was hugely distressed, wasn’t able to engage even about his pain, I can’t imagine trying to manoeuvre a conversation about something like that, it would be inappropriate. I think that it was too late to have that conversation. I think that there would be people who would have delirium, a dementia, who it would be difficult to explain what you meant perhaps, so there would be groups of patients. And as I said whilst we have an obligation there are points that would have happened before, where other people may have been able to have those conversations, and it may be that we’re not at the right, we’re not in a place where we can do that now, for some people.’
(HCPI00501, HC)
ʻYou know they might come into us to, to help with symptom management and then if we suddenly start talking about organ donation, you would, you would be steering the conversation away from the priority to them at that time. But we do tend to do end-care planning where we go through a booklet and in that booklet they give the patient the booklet when they come for an initial appointment we’ll give them the booklet and we’ll tell them to take it home and have a read and then come back and ask us questions and I’m almost certain organ donation is in that booklet, it’s an advanced care planning booklet. And more often than not they would come back and say well actually I’ve been looking at donor, you know like, not specifically eye donation, I think we just look at it as in, you know, organ donation.’
(HCPI00105, HC)
In response to questions exploring factors that may help to overcome perceived barriers, and/or embed ED into service as routine practice, many respondents indicated the need for specific knowledge and communication skills to support the conversation, particularly where this may involve raising the topic among other aspects of EoLC planning:
ʻI think, if it’s … if it’s advertised well and there is sufficient information provided to people as well as people who are making the approach in a proper sensitive manner but also have the knowledge to be able to explain all aspects of it, I think, it should … it normally goes down very well indeed.’
(HCPI00304, HPC, Organ and Tissue Donation HCP)
ʻIf you can have the conversation in a certain way if you’ve got the skill to have that conversation. And often the problem with communication is going, goes wrong with the way it’s approached. So, I think that you can have conversations about donation, however, I have still got a block in my own practice or my experience to work out where it fits in the trajectory for somebody, so and what I mean by that is, amidst all the things that people are dealing with it’s hard to work out how to introduce this as a question because it can feel about somebody else and not about them.’
(P00501, HC)
ʻI think, from what I hear in teaching sessions and from the concerns we hear from district nurses about their end-of-life training, I think it’s medical professions in general are frightened to make people cry, or they’re frightened that somebody will find something upsetting and will cry or be upset, probably though, they will worry that somebody will make a complaint against them as well. And despite the best will in the world, the NHS is still very much a blame culture rather than a learn from errors or learn from complaints. So that’s what I see anyway. So, I think its fear of upsetting people, it’s not about a particular conversation itself.’
(HCPI00201, HC)
Commentary – practice
Findings indicate key knowledge gaps for HCPs, knowledge that would potentially act as a stimulus to raise the issue of ED with patients. Data indicate that most HCPs are not aware of the need for eye tissue, that knowledge of and access to specific information to support identification of eligibility and referral (ER) of potentially eligible donors is patchy (and in many cases largely absent), and that HCPs do not routinely raise the issue of ED with potentially eligible patients. There is a suggestion that as ED does not directly benefit the patient, it is not as high a priority as other necessary discussions within EoLC planning.
These findings are compatible with those from the EDiPPPP national survey and other UK-based research63 indicating that most HCPs hardly ever, or never, initiate discussions about ED with their patients or families (with HCPs frequently indicating that the topic is usually only discussed if the topic was raised by patients or relatives). Reluctance to raise the issue proactively was aligned to a lack of knowledge and communication skills necessary to initiate such as discussion. This finding is compatible with commentary in the global literature61,63,65,68,75 indicating knowledge deficits with respect to the process of ED (i.e. assessment of eligibility, referral and retrieval of tissue)34,61,66 and low levels of confidence in the initiation of ED discussions with patient and families. 63,65,75
Preferences
The preferences domain of EDiPPPP aimed to explore participants’ needs with respect to support, guidance and practice-related aspects of the ED pathway (i.e. how they feel this should be supported, and what resources may be necessary). These are discussed under the domain of preferences primarily because HCP responses on current knowledge of/access to resources in both domains indicated that this was scarce, and so any suggestion would involve a preference for further action or resource. Interview responses are grouped into two key areas: guidance and institutional policy and training needs, with data pointing to preferences for further resource and support in these areas.
Internal processes – guidance and institutional policy
To assess what support information was available, including information that might fill knowledge gaps, HCP-interviewed participants were asked about availability of organisational policies, guidelines or procedural documentation that governed or could be used to inform ED practice (produced either by their institution or other professional/national bodies). Some HPC-based HCPs referred in general terms to the presence of such documents on their organisational intranets, whereas hospice-based HCPs were uniformly unaware of policy or guidance documents.
ʻYeah, we do have a tissue donation policy. Organ donation tissue/organ because, I think, it covers both areas … it’s on our policy so, if anybody wanted to see it is on there.’
(HCPI00102, HPC, Lead Nurse)
ʻI’d go on … the hospital intranet which has all the guidelines on it. So, I’d pull it up from there.’
(HCPI00202, HPC, Palliative Medicine)
ʻSo, it’s mentioned in quite a lot of guidelines that we should be offering eye donation. So, things like the last days of life guideline, care after death guideline. It’s mentioned in those. I think, there is also a … oh, what’s the name of the committee? The … the transplant committee which will have guidelines about who … about offering donation. And, I think, it’s mentioned in that as well.’
(HCPI00202, HPC, Palliative Medicine)
ʻI imagine there are but … and that they will be on … we record everything on (hospital) health pathways … all our policies. So, I can’t imagine that there isn’t. And, I think, it would be fairly easy to locate. And if I couldn’t locate it on either (hospital) health pathways or the Trust intranet site, I would probably ‘phone critical care and ask them.’
(HCPI00204, HPC, Palliative Care)
ʻWe don’t, we just, we basically have a few leaflets that our local nurse from (The Trust), and it’s probably over a year ago since we last had contact with her because I know she was on maternity leave, and she just, when we had like a Dying Matters Week and Death Café, and she came to that and brought us some information on organ donation. Don’t have anything specific, it’s just if somebody approached us about organ donation, we would look through these leaflets that were given and direct in the right place, or we would ring up to find out for them. To be honest, we don’t get that many patients asking us.’
(HCPI00105, HC)
HCPs were also asked if they were aware of a donation link person [to NHSBT-orange tissue donation and transplantation (OTDT) or TES]. In HPC settings, HCPs indicated a general awareness of a link person for organ or tissue donation in general [a clinical lead in organ donation (CLOD) or specialist nurse in organ donation (SNOD)], but hospice-based HCPs did not have the support of a link person:
ʻI believe there is but, I can’t remember her name. There is. There is. And, I know, it’s some areas like ED [Emergency Department] and ITU also have nurses that have a heightened … like a link role in it so that they’re more involved in it. So that they are … they try and spread the word a little bit more. So, for example, in ED, you know, there’s a nurse that has more interest so, she makes sure all the bereavement packs are put together and within their own in-house training they talk about that a little bit more. I don’t think we have that role on the wards, but we do have that in ED.’
(HCPI00102, HPC, Lead Nurse)
ʻSo, through our CLOD and our SNODs. So, our CLOD sends out all the information … so, the CLOD is our clinician obviously in charge and then our SNOD is our specialist nurse. So, we … we get all the updates from them by e-mails, regular e-mails, but also regular meetings to discuss donation at our consultant meetings.’
(HCPI00206, HPC, Acute Medicine)
ʻWell, I mean, there’s nobody specifically that’s designated that, to answer your question directly, but there must, there must be somebody, one of the clinical team, presumably one of the consultants, who would be involved in this and they may have a bit more knowledge on this than I would.’(HCPI00405, HC)
Internal processes – training needs
HCPs were asked if they had received any in-service training specifically about ED. While some HCPs working in the HPC reported that training about organ and tissue donation was being provided by Specialist Nurses in Organ Donation, no specific training focused on ED was being provided in either HPC or HC settings:
ʻNot that I’m aware of. I’ve been here eight … I’ve only been in this Trust eighteen months. I’ve not had anything. I don’t know if there’s anything. There’s nothing on induction.’
(HCPI00102, HPC, Lead Nurse)
ʻYeah. So, in the hospital [PI has] done quite a lot. Both sort of general scale. So, sort of to all the consultant body and then at various nursing training days. And obviously having her as part of the team has meant that we’ve sort of had ongoing in-house training from her. So, yes, there has been.’
(HCPI00202, HPC, Palliative Medicine)
ʻSo, probably about maybe about five, six years ago we did have some good education around donation and what was possible, and we agreed to have information on the ward in relation to that. I wonder if that may now have got lost.’
(HCPI00101, HC)
ʻI don’t, I can’t say for certain, I do monitor the education programme, but I’m not recalling anything per se, but and I think many years ago I can, I think I remember somebody coming to talk about eye donation, but that was a long time ago and I’m not aware of anything recently. But I’m probably not privileged to know everything that goes on in education training here.’
(HCPI00601, HC)
ʻSo, there is an education group across the managed clinical network who would, it would be part of their role to deliver training. Otherwise, there isn’t any specific training or education on it, so it’s, it’s a bit of that kind of by word of mouth, by accident, which again is one of the problems that there’s no formalised education about it. So, staff when they start, would get trained in using the documentation that we have, and that might in that training, you might spot that there’s something about organ donation in there, but there isn’t any specific training at all around it, so, you know, nobody’s taking that responsibility.’
(HCPI00505, HC)
Commentary – preferences
There is a dearth of clinical guidance and/or policy to assist HCPs in embedding ED in clinical practice. While many HCPs made general or vague references to the presence of guidance in policy or other institutional documents, none were able to provide details on identifiable documents containing specific information about ED. This is a significant area of concern for service development considering the specific challenges that accompany raising, discussing and fulfilling patient wishes in relation to ED specifically.
There is a lack of centrally generated, validated and incremental (differing levels for differing contexts) training and education about ED aimed at HCPs in HC and HPC services, which is regularly evaluated and monitored (a finding reflected in our national survey of HCPs). It is notable that HCPs working in hospitals have access to information and training about organ and tissue donation, usually from SNODs, whereas HCPs working in HC settings do not. While training will not guarantee that ED will be discussed, findings from our scoping review indicate the facilitative impact of education and training, and that willingness to discuss donation is positively associated with knowledge about the ED process (referral and retrieval) and being aware of local policy and guidance. 33,61
Findings – observations at clinical sites
Institutional policies and availability of ED-specific guidance
Findings from HCP interviews (WP1S2, see Chapter 5) and the national survey of HCPs (WP2S3, see Chapter 6) both indicate widespread assumptions among participants that relevant guidance to support ED pathways is available within their organisation. Typically, this was referred to as being held within institutional policies, and/or on institutional intranets; however, responses were often very general and offered little or no detail on if, where and at what level of detail such guidance existed. To explore this further in relation to our partner sites, we asked PIs to search their intranets and other sources of policy and guidance information, to determine what material was currently available to govern, guide and support ED. PIs undertook searches of trust intranets, as well as other documentary repositories, and contacted relevant colleagues in services that may hold or be aware of such information (e.g. bereavement services).
Information, guidance and policy at hospital palliative care service sites
One HPC (S02) provided a ‘best practice’ example of embedding ED processes within their service. Clinical partners at this site indicated that evaluation of eligibility for corneal donation was embedded within their admissions process in two stages. Firstly, patient records were screened on admission by the team secretary using a bespoke screening tool to exclude those with common contraindications for ED (Table 7). Secondly, patients who did not present with a common contraindication were discussed in multidisciplinary team (MDT) meetings to determine the acceptability/feasibility of raising the option with the patient and/or family as part of ACP.
| Criterion number | Exclusion criteria |
|---|---|
| 1 | Aged over 85 years |
| 2 | Degenerative neurological condition [e.g. known dementia, confusion of unknown cause, Parkinson’s disease, multiple sclerosis (MS), motor neurone disease (MND)] |
| 3 | Haematological malignancy or metastatic melanoma |
| 4 | Significant eye disease [significant among laser treatment to the eye, eye infection, glaucoma if also elderly (aged over 75 years)] |
| 5 | Blood-borne viruses (Hep B or C, HIV) |
Those who were assessed suitable for this option to be raised had an NHSBT Gift of Sight79 public information leaflet included in their ACP documentation to support a potential discussion. Progress along the pathway was tracked according to a staging system which was recorded in the patient’s care record (Figure 7). This site also indicated that bereavement services had access to printed information for families regarding corneal donation. This site had a hospice located at the Trust, and clinicians rotated between the hospital trust and the hospice. The hospice website, as well as guidance regarding organ and tissue donation, included specific information on corneal donation. Practice from this site has informed aspects of the proposed intervention and the hospice website was the benchmark against which we assessed other hospice website content in the web-based public information audit carried out to investigate the level of ED-related information available to patients and carers accessing hospice care.
FIGURE 7.
Staging system in place at alliance site to track HPC patient progress across ED pathway.

Two further sites (S04 and S06) both provided policy guidance and available information regarding donation. In both cases, HPC services had access to literature regarding corneal donation which could be shared with patients and families,79 as well as cards provided by NHSBT for staff with details of how to refer patients for donation.
At both sites, observation of MDT was attempted via Microsoft Teams; however, in both cases, technical issues linked to social distancing in situ (e.g. ability of the responsible researcher to hear speakers in the room that they were observing remotely) prevented this from being completed successfully. Both sites indicated that evaluation of eligibility and appropriateness of raising the option of ED with patients/families was not embedded as a regular process in MDT meetings (one site provided a document describing the standard MDT process, in which donation was not present). Both sites provided institutional policy documents covering donation, both of which referred exclusively to organs and did not refer to eyes. Both sites also provided institutional policies relating to bereavement and care after death, both of which contained single mentions of corneal donation in general terms as one potential tissue for donation but did not provide further guidance.
Information, guidance and policy at hospice care service sites
None of the HC sites had any processes whereby patients were routinely screened for eligibility for ED, nor was ED part of the admission questions for any site. Sites provided access to patient-facing literature, none of which mentioned ED. One site (S01) had extensive support facilities with a range of groups for patients and carers to access, but nothing was included that related to tissue or ED. This site had ‘Dying matters’ leaflets available that mention organ donation and a ‘Future Planning your wishes’ document that patients can complete to ensure that paramedic teams know what the patient has agreed with their clinical team. This document also included the question: ‘I wish to discuss tissue donation further with my clinical team’ (inviting ‘Yes’ or ‘No’ tick box answers). It is not clear who monitors these documents or who would ensure that a discussion about tissue donation has taken place [as the form guides the patient to hand a copy of the form to their general practitioner (GP) receptionist]. However, one benefit of this system is that once completed, the information is included in the patient’s summary care record, which is proposed to be available to emergency teams in particular. Despite comprehensive information regarding EoLC planning (writing ACPs, Wills and a section titled ‘Key considerations for end-of-life care’), nothing in this material directly addresses tissue or ED.
One site (S03) had an information leaflet ‘Factsheet about Eye Donation for corneal transplant’ accessible via their website requiring effort by a patient trying to access information as it was one of 38 leaflets. This site did advertise the EDiPPPP study in their patient-facing locations, but no information about donation was observable (at site set-up visit) or shared with researchers when observations could no longer be undertaken. Site (S05) had a leaflet ‘Organ Donation’ within their planning ahead section of their website. The leaflet did not mention tissue or ED.
There was a notable difference in the availability of ED-related information at HC sites compared with HPC. Firstly, while specific information about ED was available in HPC sites, it was absent from all but one HC site. One reason for this may be that information about organ donation is more likely to be part of standard EoLC planning processes in HPC (as some palliative care patients may be able to donate solid organs), whereas this is far less likely in HC settings. The fact that patients in palliative care settings shared with us their understanding or perception that they could not donate organs (due to cancer, which is correct) may have resulted from conversations stimulated by said information with the outcome that the patient is told they cannot be an organ donor, without the follow-on conversation that they can be an eye donor.
Observations of MDT meetings at HC sites were not available, but PIs reported that evaluation of eligibility and appropriateness of raising the option of ED with patients/families was not embedded as a regular process in MDT meetings.
Web-based public information audit
Following indications from the notes review (WP1S1) that HC settings in particular had significant potential for ED in terms of eligibility rates within their patient populations, we undertook an audit of hospice websites within the UK, to appraise the availability and quality of information regarding ED for patients and families from these sources.
Search strategy – national audit of hospice web pages
Hospices in the UK were identified through a members list provided by our Hospice UK, listing 208 member hospices in the UK, of which all had public-facing websites. Each hospice web page in this list was searched using the Google search engine in April 2021 using the following strategy: site: [INSERT HIGHEST LEVEL HOSPICE WEB DOMAIN ADDRESS] organ OR tissue OR cornea OR eye AND donation. Results from this search process were used to identify whether the website contained: Information about organ donation; Information about tissue donation; Information about ED; Guidance for HCPs; Guidance for Patients/Carers. Results were collated using Microsoft Excel76 [see Report Supplementary Material 12: Hospice website audit (completed 10 January 2022)].
Search strategy – audit of web-based national guidance to inform evaluation of eligibility for eye donation and referral to NHSBT
In response to observations from HCP interviews and national survey responses indicating that the NHSBT website was understood to be a source of information on eligibility criteria/contraindications for ED, the EDiPPPP team attempted to assess the availability, quantity and quality of this information. Site-specific searches of the NHSBT website were conducted in March 2021 (repeated July 2022) using the Google search engine, with the following terms: site: www.nhsbt.nhs.uk cornea OR eligibility OR contraindications.
Search outcomes – national audit of hospice web pages
Of the 208 hospice websites in the UK, only 10 hospices in England and one hospice in Wales had specific information (in leaflet or infographics form) about the option of ED. Three HC websites in Northern Ireland mentioned Organ Donation in the advanced planning document on their websites, with no information about ED. One of the 14 HC websites in Scotland mentioned organ donation (one sentence), and 1 of the 12 HC website in Wales had comprehensive information about ED; however, the information regarding the age cut-off for ED was incorrect (site says 96 years of age when cut-off at the time as specified by NHSBT-TES was 85 and 364 days).
Search outcomes – audit of web-based national guidance to inform evaluation of eligibility for eye donation and referral to NHSBT
The team also sought web-based national guidance on eligibility, referral and retrieval processes to which clinicians could refer. This was especially important as both interview/focus group and survey responses (see Chapter 6) indicated expectation on the part of clinicians that this information would be available if they needed it. The EDiPPPP team could find no such information on eligibility, referral or retrieval processes on either the NHSBT public websites or those of other national bodies (except for an e-mail address and telephone number listed on the NHSBT website for enquiries regarding referral).
These findings indicate a low level of information available to the public, patients and carers about ED as an end-of-life option for those who might be seeking information about hospice care. There is also no publicly available web-based information on eligibility, referral or retrieval that clinicians can refer to, despite many expecting this to be the case. The absence of expected information sources constitutes a significant potential barrier to raising, discussing and facilitating ED discussions in EoLC settings. As public campaigns have been shown to be effective in raising awareness about the need for donation as reported in an analysis of the impact of the deemed consent legislation in Wales,80 these information gaps should be priority areas for service development.
Chapter 6 National survey of service providers (WP2S3)
Chapter 6 addresses study Objective 3 to identify factors (attitudinal, behavioural) that enable or challenge service providers to consider and propose the option of ED as part of EoLC planning from a local and national perspective. Chapter 6 also reports the process of secondary analysis of primary data which unpinned the development of survey questions used in the national survey. Survey tool development, dissemination of survey, data collection, data analysis and results are also discussed.
The national survey of HCPs was undertaken to explore issues relating to current HCP with respect to ED, as well as perceptions regarding the acceptability and feasibility of including ED as an option in EoLC planning. The national survey was undertaken after completion of the notes review and interview/focus group stages, in order to inform question selection and thereby gain a wider perspective beyond that available from partner research sites. Understanding the practice and perceptions of service providers is important, as HCPs often function as gatekeepers to the option of ED by, for example, raising (or not) the issue as part of care planning; providing (or not) information regarding these options; and facilitating (or not) referral to retrieval services to ensure that patient and family wishes for donation are realised.
Chapter 6 concludes with a commentary of results of all data collection activities discussed thus far. This is intended to provide a clear summary picture of what we have learnt about ED processes as they relate to HCPs. Following this, we explore the specific issue of deemed consent legislation as it relates to ED and reflect on EDiPPPP findings relating to this topic. This will conclude the discussion of service user-related findings before we explore the findings of interviews of service users in Chapter 7.
Methods
Data collection for secondary analysis
Prior to EDiPPPP study commencement, the CI (TLS) had been in contact with clinicians (JW, CF, CR, SM), who joined the study as co-applicants, and who had carried out empirical work (published and unpublished) to request access to their work for secondary analysis of primary data to inform survey tool development. 34–36 This work was shared and was the base data for synthesis as all studies had applied a survey design.
Survey instrument development – data synthesis and integration
Questionnaire data from primary studies and interim findings from interviews, focus groups and observations conducted as part of WP1S2 were mapped (MJB/BMS) to the study domains and grouped into three of four domains comprising the EDiPPPP study’s foci: practice, preferences and perceptions. Version one of the survey was reviewed by TLS, who provided feedback and comments resulting in additional items and demographic data in version two, which was created as an online survey using the Microsoft Forms online survey system. 81
Version two of the questionnaire was independently reviewed by co-applicant (MM) who recommended minor amendments (grammar, typos, flow of questions) which were accepted and integrated into the final version (Three) of the questionnaire. The final agreed version of the questionnaire was produced (MJB, BMS, MM, TLS) and piloted with PIs (CR, JS). The final instrument included 61 questions (see Report Supplementary Material 13: National Survey questionnaire). Surveys were completed anonymously, with respondents asked not to provide institutional or other information that could potentially identify themselves, patients or carers.
Survey objectives
-
Map current practice in relation to ED across HC and HPC settings.
-
Identify perceptions of HCPs regarding embedding ED into usual EoLC planning within their practice setting.
-
Investigate the current informational, training or support needs of HCPs relating to integrating ED into EoLC planning and discussions.
Dissemination strategy
Two partner organisations circulated the survey to their members: the Association for Palliative Medicine (UK) and Hospice UK. One thousand two hundred and twenty-two Association for Palliative Medicine members and 672 Hospice UK members were approached via e-mail in the third week of November 2020, with a 2-week follow-up e-mail in the first week of December 2020. The survey closed to responses on 31 December 2020.
Data analysis
Data from closed questions generated descriptive statistics (e.g. percentages of respondents providing a given answer; average completion time for survey), while data from free-text responses were explored through qualitative content analysis. 20
Results
Response rate and completion time
One hundred and fifty-six participants completed the online survey representing an 8% response rate (of n = 1894 approached). Of these, 63% (n = 98) indicated working within HC settings, while 37% (n = 58) indicated HPC. One hundred and three participants responded following the first round of e-mail contact, with a further 53 responding after the second round of e-mails. Median completion time was 16 minutes and 12 seconds (IQR = 10:28–23:46).
Sample demographics
For all participants, 65% (n = 101) were aged between 40 and 59 years, with a further 30% (n = 46) aged 18–39 (Figure 8), 83% (n = 129) identified as female, and 87% (n = 136) identified as White British ethnicity (age and ethnicity characteristics were similar for both HC and HPC groups).
FIGURE 8.
National survey participant age groups by site type. n.b. in two cases, participants used the ‘other’ response to indicate that they worked across both HC and HPC settings – in one case, the participant’s free-text responses referred exclusively to HPC-related services (e.g. services ‘within a trust’, ‘tissue retrieval teams’) and were therefore counted as part of the HPC group; the other case contained HC-specific free-text comments, and was counted as part of that set).
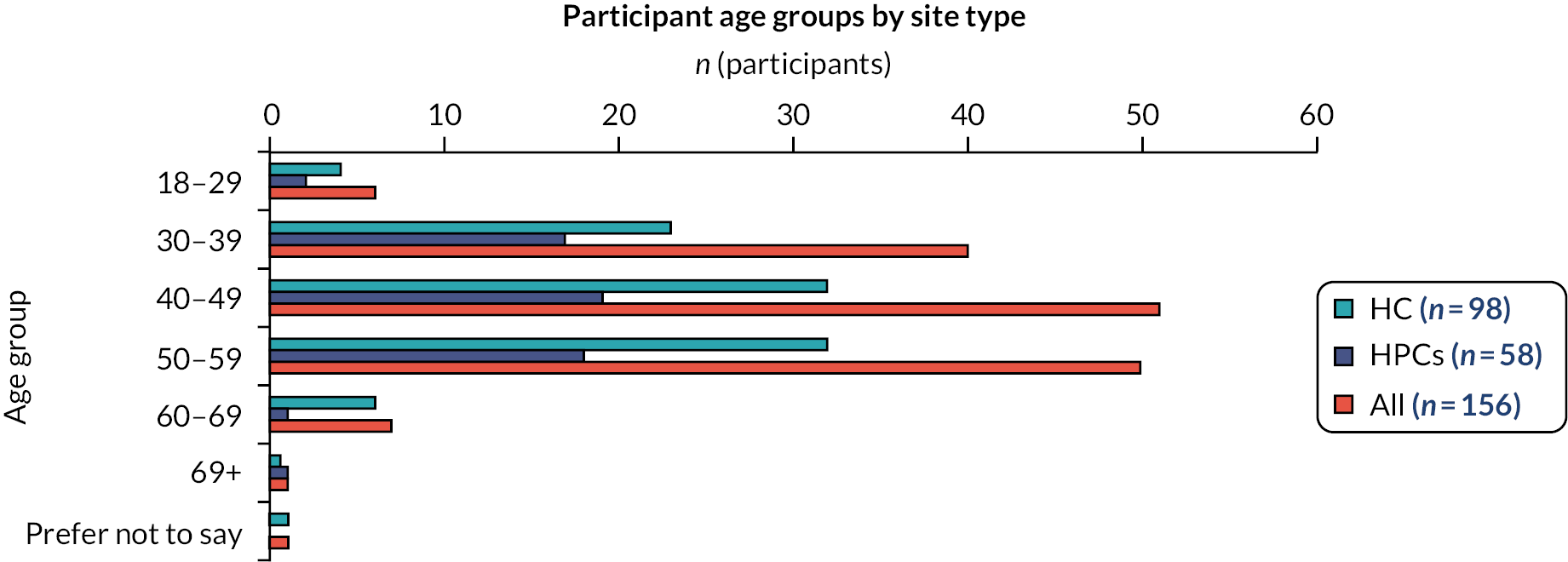
In terms of professional roles, for all participants, 33% (n = 52) identified as a Consultant in Palliative Medicine, 25% (n = 39) as a Palliative Care Physician, 21% (n = 33) with a Managerial/Head of Service role, 11% (n = 17) as a Senior Nurse, 6% with other clinical services (e.g. Counselling, Physiotherapy, ACP Facilitator, Specialist Pharmacist), 4% (n = 6) as Healthcare Assistants, 1% (n = 2) as Nurses (excluding senior roles) and 1% (n = 1) as being in an Administrative/Clerical role (Figure 9).
FIGURE 9.
National survey participant role by site type.
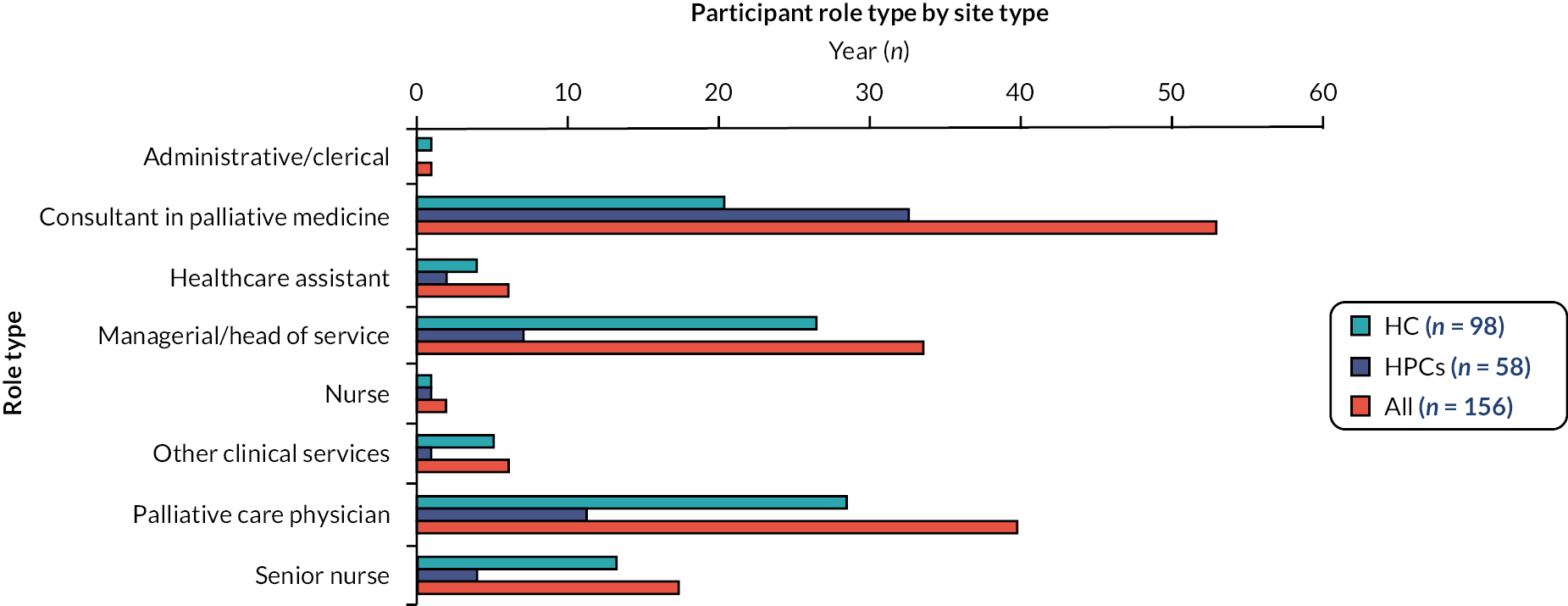
In this section, results from the national survey are reported in relation to Objectives 1–3.
Objective 1: Map current routine practice in relation to eye donation across HC and HPC settings
Respondents were asked to answer a series of questions on their experiences of current practice relating to ED (Table 8). Eighty-four per cent of participants (n = 131) indicated that they were ‘aware that ED is an option that patients can choose as part of advance care/end of life care planning’, with 15% (n = 24) responding that they were not aware of this option. Of participants indicating awareness of the option (n = 131), 48% (n = 63/131) indicated that their clinical setting does not ‘actively encourage the option of ED being discussed with patients and/or their families’, with 35% (n = 46) indicating that this was encouraged within their setting. Of participants selecting ‘Other’ in response to Q19 (n = 23), 15 provided a comment indicating some form of support for EoLC conversations regarding ED, but that this had not become embedded routine practice, for example:
| Participant group | Are you aware that eye donation is an option that patients can choose as part of advance care/end of life care planning? [Q18] | |||||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Othera | ||||||
| n | % | n | % | n | % | |||
| Participant group | [IF YES TO Q18] Does your clinical setting actively encourage the option of eye donation being discussed with patients and/or their families?b [Q19] | |||||||
| Yes | No | Othera | NA | |||||
| n | %a | n | %a | n | %a | n | %a | |
| Participant group | [IF YES TO Q18] Do staff within your clinical setting routinely discuss the option of eye donation in meetings (e.g. team, case conference, multi-disciplinary team meeting (MDT))?b [Q20] | |||||||
| Yes | No | Othera | NA | |||||
| n | % | n | % | n | % | n | % | |
| Participant group | [IF YES TO Q18] Do staff within your clinical setting routinely discuss the option of eye donation in end of life care planning conversations with patients and/or family members?b [Q21] | |||||||
| Yes | No | Othera | NA | |||||
| n | % | n | % | n | % | n | % | |
| Participant group | [IF YES TO Q18] Does your service routinely check the Organ Donor Register status of patients at the point of admission?b [Q22] | |||||||
| Yes | No | Othera | NA | |||||
| n | % | n | % | n | % | n | % | |
| Participant group | Is there a donation link person or champion in your service? [Q35] | |||||||
| Yes | No | Don’t know | ||||||
| n | % | n | % | n | % | |||
| HPC (n = 58) | 51 | 88 | 7 | 12 | 0 | |||
| HC (n = 98) | 80 | 82 | 17 | 17 | 1 | 1 | ||
| All participants (n = 156) | 131 | 84 | 24 | 15 | 1 | 1 | ||
| HPC (n = 58) | 17 | 33 | 24 | 47 | 10 | 20 | 7 | 14 |
| HC (n = 98) | 29 | 36 | 39 | 48 | 13 | 16 | 17 | 21 |
| All participants (n = 156) | 46 | 35 | 63 | 48 | 23 | 17 | 24 | 18 |
| HPC (n = 58) | 3 | 6 | 43 | 84 | 5 | 10 | 7 | 14 |
| HC (n = 98) | 9 | 11 | 66 | 81 | 6 | 7 | 17 | 21 |
| All participants (n = 156) | 12 | 9 | 109 | 83 | 11 | 8 | 24 | 18 |
| HPC (n = 58) | 4 | 8 | 34 | 67 | 13 | 25 | 7 | 14 |
| HC (n = 98) | 13 | 16 | 61 | 75 | 7 | 9 | 17 | 21 |
| All participants (n = 156) | 17 | 13 | 95 | 72 | 20 | 15 | 24 | 18 |
| HPC (n = 58) | 1 | 2 | 44 | 86 | 6 | 12 | 7 | 14 |
| HC (n = 98) | 3 | 4 | 70 | 86 | 8 | 10 | 17 | 21 |
| All participants (n = 156) | 4 | 3 | 114 | 86 | 14 | 11 | 24 | 18 |
| HPC (n = 58) | 13 | 22 | 31 | 53 | 14 | 24 | ||
| HC (n = 98) | 15 | 15 | 59 | 60 | 24 | 24 | ||
| All participants (n = 156) | 28 | 18 | 90 | 58 | 38 | 24 | ||
ʻIt is mentioned on the admission paperwork as an option to possibly discuss (it is rarely appropriate due to their underlying diagnosis of current clinical condition).’
(Palliative Physician, HC setting)
Eighty-three per cent (n = 109) of participants indicated that staff within their clinical setting did not ‘routinely discuss the option of ED in meetings’ (e.g. team, case conference, MDT meeting), while 72% of the participants (n = 95) indicated that staff within their clinical setting did not ‘routinely discuss the option of ED in end-of-life care planning conversations with patients and/or family members’.
Of participants selecting ‘Other’ for Q20 (n = 11), all comments were compatible with ED not being a part of routine meeting discussions in these settings, though some (n = 7) participants indicated attempts to make this happen within their service, for example:
ʻWe try to make this the case, but in practice it doesn’t always happen.’
(Consultant in Palliative Medicine, HC setting)
Twenty participants (15%) selecting ‘Other’ for Q21 provided a free-text comment indicating that discussion about the option of ED was not routine practice at their sites, and/or that this topic was only discussed when raised by patients or family:
ʻUsually only if raised by the Family/Patient. ‘Not routinely with every patient/family but increasingly frequently having these conversations.’
(Manager/Head of Service, HPC setting)
Eighty-six per cent (n = 114) of total participants indicated that their service did not ‘routinely check the Organ Donor Status of patients at the point of admission’, while 58% (n = 90) of total participants indicated that there was not ‘a donation link person or champion in [their] service’ [a further 24% (n = 38) of total participants indicating that they ‘don’t know’ whether this person exists at their site].
Objective 2: Identify the perceptions of healthcare staff regarding embedding eye donation into usual end-of-life care planning within their practice setting
Respondents were asked a series of questions regarding HCP perceptions of acceptability and feasibility of embedding ED into EoLC planning discussions with patients and families.
Perceptions of healthcare professionals regarding propriety and feasibility of discussing eye donation with patients and/or families
Participants were asked to indicate their response (i.e. ‘Agree’, ‘Unsure’ or ‘Disagree’) in relation to a series of statements regarding the option of ED being raised with patients and families (Table 9). Seventy-three per cent (n = 114) of total participants disagreed with the statement ‘discussing ED is too distressing for a patient and/or their family’. Sixty-one per cent (n = 95) of total participants agreed that they ‘feel confident in starting a conversation about ED with a patient and/or their family’. Sixty-three per cent (n = 99) of total participants agreed with the statement ‘[E]ye donation should be discussed routinely with eligible patients and/or their families’.
| Participant group | Discussing eye donation is too distressing for a patient and/or their family [Q11] | |||||
|---|---|---|---|---|---|---|
| Agree | Not sure | Disagree | ||||
| n | % | n | % | n | % | |
| Participant group | I feel confident in starting a conversation about eye donation with a patient and/or their family [Q12] | |||||
| Agree | Not sure | Disagree | ||||
| n | % | n | % | n | % | |
| Participant group | Eye donation should be discussed routinely with eligible patients and/or their families [Q13] | |||||
| Agree | Not sure | Disagree | ||||
| n | % | n | % | n | % | |
| Participant group | It is not my role to raise the option of eye donation with patients and/or their families [Q14] | |||||
| Agree | Not sure | Disagree | ||||
| n | % | n | % | n | % | |
| Participant group | It is important that patients know that they may be eligible for eye donation [Q15] | |||||
| Agree | Not sure | Disagree | ||||
| n | % | n | % | n | % | |
| Participant group | I am concerned about how patients and/or family members might respond to the option of eye donation being raised with them. [Q16] | |||||
| Agree | Not sure | Disagree | ||||
| n | % | n | % | n | % | |
| HPC (n = 58) | 1 | 2 | 12 | 21 | 45 | 78 |
| HC (n = 98) | 4 | 4 | 25 | 26 | 69 | 70 |
| All participants (n = 156) | 5 | 3 | 37 | 24 | 114 | 73 |
| HPC (n = 58) | 39 | 67 | 11 | 19 | 8 | 14 |
| HC (n = 98) | 56 | 57 | 23 | 23 | 19 | 19 |
| All participants (n = 156) | 95 | 61 | 34 | 22 | 27 | 17 |
| HPC (n = 58) | 39 | 67 | 14 | 24 | 5 | 9 |
| HC (n = 98) | 60 | 61 | 30 | 31 | 8 | 8 |
| All participants (n = 156) | 99 | 63 | 44 | 28 | 13 | 8 |
| HPC (n = 58) | 5 | 9 | 10 | 17 | 43 | 74 |
| HC (n = 98) | 12 | 12 | 15 | 15 | 71 | 72 |
| All participants (n = 156) | 17 | 11 | 25 | 16 | 114 | 73 |
| HPC (n = 58) | 52 | 90 | 6 | 10 | 0 | 0 |
| HC (n = 98) | 93 | 95 | 3 | 3 | 2 | 2 |
| All participants (n = 156) | 145 | 93 | 9 | 6 | 2 | 1 |
| HPC (n = 58) | 14 | 24 | 13 | 22 | 31 | 53 |
| HC (n = 98) | 37 | 38 | 14 | 14 | 47 | 48 |
| All participants (n = 156) | 51 | 33 | 27 | 17 | 78 | 50 |
Seventy-three per cent (n = 114) of participants indicated that they disagreed with the statement ‘[i]t is not my role to raise the option of ED with patients and/or their families’. Ninety-three per cent (n = 145) of total participants agreed with the statement ‘[i]t is important that patients know that they may be eligible for ED’. Finally, 50% of participants agreed or were uncertain in relation to the statement ‘I am concerned about how patients and/or family members might respond to the option of ED being raised with them’, while 50% of the remaining total participants (n = 78) disagreed with this statement.
Raising and discussing the topic of eye donation with patients and families
Participants were asked a series of questions relating to raising and discussing the topic of ED (Table 10).
| Participant group | Which of the following best describes your current practice? [Q28] | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I discuss eye donation only when the subject is raised by patients or families | I never discuss eye donation with patients or families | I routinely discuss the option of donation with patients and families | NA | Other | ||||||||||
| n | % | n | % | n | % | n | % | n | % | |||||
| Participant group | At what point in a patient’s care should the option of eye donation be discussed? (Please select all that apply). [Q29] | |||||||||||||
| At first assessment by palliative care services | Before admission | During admission | During advanced care planning | During in patient stay | Never | Other | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Participant group | How many times in the past year have you raised the option of eye donation with a family member? [Q30] | |||||||||||||
| 0 | 1–5 | 6–10 | 11–15 | 15–20 | More than 20 | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |||
| Participant group | Reflecting back on the last time you discussed eye donation with a patient and/or relative, how did you feel having that conversation? [Q31] | |||||||||||||
| Very uncomfortable | Somewhat uncomfortable | Neither comfortable nor uncomfortable | Somewhat comfortable | Very comfortable | ED never discussed | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |||
| Participant group | If you have had a discussion with a family member, was this discussion pre or post death of the patient? (please select all that apply) [Q32] | |||||||||||||
| I have not had a discussion with a family member | Pre-death | Post-death | NA | |||||||||||
| n | % | n | % | n | % | n | % | |||||||
| Participant group | Who do you think should raise the issue of eye donation with a patient or family member? (Please select all that apply) [Q33] | |||||||||||||
| A donation specialist | It is my role | Other palliative care specialist (e.g. CNS) | The Consultant referring the patient to Palliative Care | The GP should have this conversation | All of the above | Other | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| HC (n = 58) | 26 | 45 | 10 | 17 | 10 | 17 | 1 | 2 | 11 | 19 | ||||
| HPC (n = 98) | 42 | 43 | 24 | 24 | 10 | 10 | 7 | 7 | 15 | 15 | ||||
| All participants (n = 156) | 68 | 44 | 34 | 22 | 20 | 13 | 8 | 5 | 26 | 17 | ||||
| HC (n = 58) | 12 | 21 | 18 | 31 | 25 | 43 | 47 | 81 | 27 | 47 | 0 | 0 | 14 | 24% |
| HPC (n = 98) | 32 | 33 | 37 | 38 | 47 | 48 | 78 | 80 | 44 | 45 | 0 | 0 | 15 | 15% |
| All participants (n = 156) | 44 | 28 | 55 | 35 | 72 | 46 | 125 | 80 | 71 | 46 | 0 | 0 | 29 | 19% |
| HC (n = 58) | 23 | 40 | 25 | 43 | 6 | 10 | 1 | 2 | 1 | 2 | 2 | 3 | ||
| HPC (n = 98) | 52 | 53 | 30 | 31 | 7 | 7 | 2 | 2 | 0 | 0 | 7 | 7 | ||
| All participants (n = 156) | 75 | 48 | 55 | 35 | 13 | 8 | 3 | 2 | 1 | 1 | 9 | 6 | ||
| HC (n = 58) | 0 | 0 | 5 | 16 | 15 | 47 | 21 | 66 | 9 | 28 | 8 | 14 | ||
| HPC (n = 98) | 2 | 5 | 7 | 16 | 17 | 39 | 27 | 61 | 12 | 27 | 33 | 34 | ||
| All participants (n = 156) | 2 | 3 | 12 | 16 | 32 | 42 | 48 | 63 | 21 | 28 | 41 | 26 | ||
| HC (n = 58) | 4 | 8 | 44 | 88 | 6 | 12 | 8 | 14 | ||||||
| HPC (n = 98) | 1 | 1 | 57 | 77 | 17 | 23 | 33 | 34 | ||||||
| All participants (n = 156) | 5 | 4 | 101 | 81 | 23 | 19 | 41 | 26 | ||||||
| HC (n = 58) | 9 | 16 | 16 | 28 | 14 | 24 | 6 | 10 | 9 | 16 | 39 | 67 | 6 | 10 |
| HPC (n = 98) | 17 | 17 | 25 | 26 | 26 | 27 | 16 | 16 | 22 | 22 | 69 | 70 | 15 | 15 |
| All participants (n = 156) | 26 | 17 | 41 | 26 | 40 | 26 | 22 | 14 | 31 | 20 | 108 | 69 | 21 | 13 |
In response to the question, ‘Which of the following best describes your current practice?’, 44% (n = 68) of total participants indicated that they discuss the option ‘only when the subject is raised by patients or families’ with 22% indicating that they ‘never discuss ED with patients or families’. Thirteen per cent (n = 20) of total participants indicated that they ‘routinely discuss [this option] with patients and family members.
Responding to the question, ‘At what point in a patient’s care should the option of ED be discussed? (Please select all that apply)’, a majority (80%, n = 125) of total participants indicated that this should occur ‘during advanced care planning’, 46% (n = 71) ‘during in-patient stay’, 46% (n = 72) ‘during admission’, 35% (n = 55) ‘before admission’ and 28% (n = 44) ‘at first assessment by palliative care services’.
Forty-eight per cent (n = 75) of total participants had not raised the option of ED with a family member in the past year, while 35% (n = 55) had raised the issue between one and five times. Ten per cent (n = 16) had raised the issue between 6 and 15 times, while 7% (n = 10) had raised the issue 15 times or more.
Questions 31 and 32 explored experiences of discussing ED with patients and/or families. The following findings are limited to those participants who indicated that they had experience of discussing ED with patients or family members (n = 115). Eighty-eight per cent (n = 101) of these (n = 115) participants had discussed ED with family pre death of a patient, with 20% (n = 23) reporting post-death discussions with family.
In response to the question, ‘reflecting back on the last time you discussed ED with a patient and/or relative, how did you feel having that conversation’, 60% (n = 69) of participants indicated that they were ‘very’ or ‘somewhat’ comfortable, and 28% (n = 32) indicated that they were ‘neither comfortable nor uncomfortable’. A further 12% (n = 14) of participants indicated that they were ‘somewhat’ or ‘very’ uncomfortable.
Responding to the question: ‘Who do you think should raise the issue of ED with a patient or family member?’ (Please select all that apply):
-
Twenty-six per cent (n = 41) indicated ‘it is my role’, 26% (n = 40) indicated that it was someone else’s role from within the palliative care specialist team (‘other palliative care specialist’ (e.g. CNS).
-
Twenty per cent (n = 31) indicated that ‘the GP should have this conversation’.
-
Seventeen per cent (n = 26) indicated ‘a donation specialist’.
-
Fourteen per cent (n = 22) indicated ‘the consultant referring to Palliative Care’.
-
Sixty-nine per cent (n = 108) of total participants selected ‘all of the above’ (indicating all previous responses in this list).
Of the 21 participants using the ‘Other’ option to provide a free-text comment, most responses (n = 14) were compatible with raising the issue being a general responsibility for staff across the pathway, for example:
ʻWhoever is comfortable having ACP discussions or whoever the patient chooses to have that discussion with.’
(Consultant in Palliative Medicine, HPC setting)
Availability of clinical guidance and information to support eye donation conversations with patients/families
Participants were asked a series of questions regarding their access to guidance and support information regarding ED conversations (Table 11). Almost half of survey participants (46%, n = 61) indicated that their clinical setting does not ‘have clinical guidelines in written form that include ED’, with a further 37% of participants indicating that this information does exist at their site. Twenty-two participants selected ‘Other’ in response to this question, of which 17 indicated that they were ‘Unsure’ whether clinical guidelines existed and a further 5 indicated that guidelines were in preparation or referred to some other form of information.
| Participant group | [IF YES TO Q18] Does your clinical setting have clinical guidelines in written form that include eye donation?a [Q24] | [IF YES TO Q18] Does your clinical setting have information in written form that staff can refer to if eye donation is raised by a patient or family member?a [Q25] | [IF YES TO Q18] Does your clinical setting include eye donation in its admission documentation?a [Q26] | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Otherb | NA | Yes | No | Otherb | NA | Yes | No | Otherb | NA | |||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Participant group | [IF YES TO Q18] Does your clinical setting have information in written form that staff can refer to if eye donation is raised by a patient or family member?a [Q25] | |||||||||||||||||||||||
| Yes | No | Otherb | NA | |||||||||||||||||||||
| n | % | n | % | n | % | n | % | |||||||||||||||||
| Participant group | [IF YES TO Q18] Does your clinical setting include eye donation in its admission documentation?a [Q26] | |||||||||||||||||||||||
| Yes | No | Otherb | NA | |||||||||||||||||||||
| n | % | n | % | n | % | n | % | |||||||||||||||||
| HPC (n = 58) | 20 | 0.39 | 21 | 0.41 | 10 | 0.17 | 7 | 0.14 | 26 | 0.51 | 15 | 0.29 | 10 | 0.20 | 7 | 0.14 | 8 | 0.16 | 36 | 0.71 | 7 | 0.14 | 7 | 0.14 |
| HC (n = 98) | 29 | 0.36 | 40 | 0.49 | 12 | 0.12 | 17 | 0.21 | 54 | 0.67 | 18 | 0.22 | 9 | 0.11 | 17 | 0.21 | 24 | 0.30 | 45 | 0.56 | 12 | 0.15 | 17 | 0.21 |
| All participants (n = 156) | 49 | 0.37 | 61 | 0.46 | 22 | 0.14 | 24 | 0.18 | 80 | 0.61 | 33 | 0.25 | 19 | 0.14 | 24 | 0.18 | 32 | 0.24 | 81 | 0.61 | 19 | 0.14 | 24 | 0.18 |
| HPC (n = 58) | 26 | 0.51 | 15 | 0.29 | 10 | 0.20 | 7 | 0.14 | ||||||||||||||||
| HC (n = 98) | 54 | 0.67 | 18 | 0.22 | 9 | 0.11 | 17 | 0.21 | ||||||||||||||||
| All participants (n = 156) | 80 | 0.61 | 33 | 0.25 | 19 | 0.14 | 24 | 0.18 | ||||||||||||||||
| HPC (n = 58) | 8 | 0.16 | 36 | 0.71 | 7 | 0.14 | 7 | 0.14 | ||||||||||||||||
| HC (n = 98) | 24 | 0.30 | 45 | 0.56 | 12 | 0.15 | 17 | 0.21 | ||||||||||||||||
| All participants (n = 156) | 32 | 0.24 | 81 | 0.61 | 19 | 0.14 | 24 | 0.18 | ||||||||||||||||
Sixty-one per cent of participants (n = 81) indicated that their clinical setting had ‘information in written form that staff can refer to if ED was raised by a patient or family member’, while 25% of participants (n = 33) indicated that this information is not available at their site. Of 19 participants selecting ‘Other’, 13 indicated uncertainty as to availability of this information.
Most participants (61%, n = 81) indicated that their setting does not ‘include ED in its admission documentation’, whereas 32% of participants indicated that ED was included in admission documentation at their site. Of 19 participants giving ‘Other’ type responses, 13 were uncertain whether this information was included in admission documentation at their site.
Objective 3: Investigate the current informational, training or support needs of healthcare professionals relating to integrating eye donation into end-of-life care planning and discussions
Knowledge and experience relating to eye donation
To assess HCPs’ current knowledge base regarding ED, we included a short section ‘flash quiz’, exploring three key questions about the ED pathway. Content analysis was performed on the free-text responses to categorise them by type, with results summarised in Table 12. Responses to the question ‘how long after death can ED take place?’ indicated that just over half of all participants (53%, n = 83 of 156) understood that ED can take place up to 24 hours after death. Eighteen per cent of participants (n = 28 of 156) indicated that they did not know the time limit, with a greater proportion of HC respondents (22%, n = 22 of 98) selecting this option when compared with HPC (10%, n = 6 of 58).
| Q57 - How long after death can eye donation take place? | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Participant group | Unsure/don’t know | Less than 24 hours | Up to 24 hours | Up to 48 hours | ||||||||
| n | % | n | % | n | % | n | % | |||||
| Q58 – What are the definite contraindications for eye donation? | ||||||||||||
| Participant group | Unsure/don’t know | Neurological/CJD | Age | Infections | Cancers | Eye diseases | ||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Q59 - Is there anything that needs to happen before eye donation can take place? | ||||||||||||
| Participant group | Unsure/don’t know | Nothing | Consent | Care of eyes | Blood sample | Inform NHSBT/transplant coordinator | ||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| HC (n = 98) | 21 | 21 | 10 | 10 | 56 | 57 | 8 | 8 | ||||
| HPC (n = 58) | 6 | 10 | 4 | 7 | 29 | 50 | 7 | 12 | ||||
| All = 156 | 27 | 17 | 14 | 9 | 85 | 54 | 15 | 10 | ||||
| HC (n = 98) | 22 | 22 | 32 | 33 | 12 | 12 | 31 | 32 | 33 | 34 | 24 | 24 |
| HPC (n = 58) | 9 | 16 | 16 | 28 | 5 | 9 | 32 | 55 | 21 | 36 | 20 | 34 |
| All (n = 155) | 31 | 20 | 48 | 31 | 17 | 11 | 63 | 41 | 54 | 35 | 44 | 29 |
| HC (n = 98) | 32 | 11 | 2 | 2 | 30 | 31 | 4 | 4 | 12 | 12 | 10 | 10 |
| HPC (n = 58) | 11 | 19 | 1 | 2 | 27 | 47 | 4 | 7 | 7 | 12 | 7 | 12 |
| All (n = 156) | 43 | 28 | 3 | 2 | 57 | 37 | 8 | 5 | 19 | 12 | 17 | 11 |
When asked to identify definite contraindications for ED (in free-text responses), infections were most commonly indicated (41%, n = 63 of 156 responses), followed by cancers (35%, n = 54) and neurological conditions (31%, n = 48). When asked what should happen before ED can take place, 37% (n = 57 of 156) of participants indicated that either patient or family consent was required, while 12% (n = 19) indicated that a blood sample is required.
Availability and experience of training and resources to support eye donation
Participants were asked about the training received and where information about ED is held in their organisation (Table 13). Sixty-nine per cent of total respondents (n = 108) indicated that they knew where to find information about ED if needed; however, a majority also responded indicating that they had not received any in-service training about ED (61%, 95/156). Of those who had received training (n = 61), 44% received it from their hospital or hospice with a further 56% having received training from other sources. In addition, 54% of participants (n = 33 of 61) indicated that the training was undertaken at least 24 months previously.
| Participant group | Have you received any in-service training about eye donation? (Q47) | [IF YES TO Q47] Who provided the training? (Q48)a | [IF YES TO Q47] How long ago did you undertake the training? (Q49)a | [IF YES TO Q47] Did the training provide you with the information you needed to be confident in discussing eye donation with patients/family members? (Q50) | Do you know where to find out information about eye donation if you need to? (Q53) | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | My employer (e.g. hospital or hospice) | Other | In the last 6 months | 6-12 months ago | 13-24 months ago | More than 24 months ago | Yes | Somewhat | No | Yes | No | ||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| HPC (n = 58) | 25 | 43 | 33 | 57 | 13 | 52 | 12 | 48 | 2 | 0.08 | 3 | 0.12 | 4 | 0.16 | 16 | 64 | 15 | 26 | 8 | 14 | 2 | 3 | 43 | 74 | 15 | 26 |
| HC (n = 98) | 36 | 37 | 62 | 63 | 14 | 39 | 22 | 61 | 2 | 0.06 | 4 | 0.11 | 13 | 0.36 | 17 | 47 | 29 | 30 | 7 | 7 | 0 | 0 | 65 | 66 | 33 | 34 |
| All participants (n = 156) | 61 | 39 | 95 | 61 | 27 | 44 | 34 | 56 | 4 | 0.07 | 7 | 0.11 | 17 | 0.28 | 33 | 54 | 44 | 28 | 15 | 10 | 2 | 1 | 108 | 69 | 48 | 31 |
Finally, 72% (n = 44 of 61) of participants who had completed training reported that this had ‘provided [them] with the information [they] needed to be confident in discussing ED with patients/family members’, with 25% (n = 15) indicating that this has been provided ‘somewhat’. Two further participants indicated that their training had not provided information necessary to give them sufficient confidence in these discussions.
To explore the content and quality of the training completed by participants (n = 61), we asked if they had any comments on the positive or negative aspects of the training they received. Twenty-two participants provided free-text responses, which indicated several areas of need: eligibility criteria, the process of ED, communication skills, change in legislation and how to access the ODR.
ʻI definitely feel a refresher and update for the whole service would be very welcome’
ʻI really don’t know what I don’t know. I am rusty on how to start the conversation, how to instruct a patient, what to say to the family about the process, the eligibility criteria, the register, etc.’
ʻTraining around communication with families’
ʻI would need training in all aspects. my current knowledge is rudimentary’
‘The process for eye donation where I now work, as it will differ from my previous job’
In addition, several participants highlighted the positive effect on training alongside the need for additional measures to embed ED within routine care in the long run.
ʻIt has a brief effect on practice and then it fades!’
ʻEveryone is very enthusiastic but it has not been effectively implemented’
ʻIt was the impetus to promote corneal donation in our hospice’
ʻGenerally, the training has been useful for me and the feedback of my training to other staff has been very positive. We have researched our donation project and audited it and the staff feedback questionnaire was very positive about the process’
Commentary on results
As reported in our scoping review and supported by our findings, HCPs are generally favourable towards ED, perceiving it as worthwhile. 34,47,50,65 However, while other authors report that although participants feel uncomfortable discussing ED, the majority felt it was their professional responsibility to do so,69 but this was not the case in our findings. Our findings are more in line with research reporting that despite HCPs acknowledging that ED is worthwhile, it is not embedded in routine practice. 34,65,67,68
While HCPs agree that patients should be made aware of ED and should have the option of ED discussed with them, their confidence and motivation to undertake these conversations often appears undermined by concerns regarding the potential impact on patients and/or families (despite the evidence indicating that patients are willing and able to be involved in such discussions). 34,73,82 This points to a clear disconnect between the perceptions and beliefs of service providers and the perceptions of services users as reported in the existing literature.
HCPs should be reassured by an increasing body of knowledge indicating that patients are willing and able to have this conversation, as most do not see this topic as different to discussing their wishes/views regarding, for example, preferred place of death, resuscitation wishes, etc. Evidence from previous studies gained directly from patients indicated that the introduction of the topic of ED during admission to a HC setting did not elicit concerns from patients (e.g. distress or concern at the option being raised). 65,66 In fact, in one study where patients in a HC setting were provided with a short survey regarding the propriety of discussing ED, it was reported that that some patients changed their minds regarding ED (from negative to positive) after a conversation. 36 While a limitation of these studies was that a survey methodology was applied which limits the potential to explore some of the sensitive aspects around discussing donation at the end of life, the findings from the interviews with patients and carers in EDiPPPP support these findings and go further in identifying the views of patients regarding ‘How’ the topic should be raised, by ‘Whom’ and ‘When’, which are vital components for informing service development and individual clinical practice.
A further barrier to embedding ED in routine practice is confirmed from site observations and interviews indicating the lack of policy and clinical guidance; ED not being included in most clinical sites local written information for patients and families or admission documentation (with exceptions, as outlined in our analysis of hospice websites); and the lack of public-facing information across the palliative care sector. This information deficit means that ED is fundamentally invisible to service users and the wider public, and therefore compromises the efforts of HCPs who are motivated to offer the option of ED as part of EoLC planning conversations.
A pervasive barrier to embedding ED in routine practice is that most HCP participants in our survey and interviews had no formal training regarding ED, and of those who had, the majority completed this more than 24 months prior to participation. EDiPPPP findings thus corroborate and extend a range of observations from existing literature regarding knowledge deficits, including not having sufficient knowledge about the process of ED,44,46,47,69 lack of knowledge regarding eligibility criteria45,48,49 and lacking confidence to initiate ED discussions. 35,50–52
Completion of training is no guarantee that ED will be discussed, as indicated by the fact that some participants in the EDiPPPP study had received training. However, the motivating and confidence building impact that education and training can have is indicated in previous work,83 and therefore must be part of any intervention that aims to achieve behaviour change.
Findings from EDiPPPP confirm findings from the wider literature indicating a range of barriers in current HCP practice to the option of ED being raised. The value of raising the option of ED is recognised by HCPs, but the action of doing so is impeded by wider organisational factors relating to knowledge deficits, perceived limited resources and the norms of routine practice, or as we term this, the donation climate and organisational culture in which HCPs are working.
The implications of this are clear – even if there is high potential (based on eligibility assessment), this is unlikely to be realised if the climate within the site is not ‘donation ready’. Key components of this organisational readiness include demonstrating positive HCPs views; routine clinical assessment of patient eligibly; mandated practice supported by accessible clinical guidelines and information. In view of these findings, we have developed the Organisational Readiness for ED Assessment Checklist (OREDAC) (see Appendix 7) by which the ED climate of a site can be assessed, in order to support selection of sites for strategic partnership with NHSBT-TES. Where the EEDAC proposed in Chapter 4 facilitates identification of sites with high potential, OREDAC enables context-specific evaluation of those sites, specifically in relation to the capability (knowledge and skills deficits) of HCPs; the perceived opportunity to raise the issue of ED in clinical settings; and the level of individual and organisational motivation to ensure that patients are aware of, and offered the option of ED.
This knowledge can support service development strategies that target the needs of specific institutions. Taken together, OREDAC and EEDAC provide a process for service development planning that is sensitive to organisational context and will therefore be useful in helping NHSBT-TES achieve its strategic aim of realising donation at high-potential sites, which may differ in their organisational culture, resources and donation climate. Further discussion of these tools within the context of the complex intervention package (STEPS) proposed by EDiPPPP will be discussed in Chapter 9.
Deemed consent legislation
We were asked to include questions about HCPs’ awareness, views and knowledge regarding deemed consent legislation by NHSBT-TES and we therefore included this question in the interview schedules and national survey. The findings from interviews and results from the survey are integrated into this section.
Deemed consent legislation (also known as Max and Keira’s Law) was introduced to England in May 2020 (www.organdonation.nhs.uk/get-involved/news/max-and-keira-s-law-comes-into-effect-in-england/). Under this legislation, all adults in England are deemed to have agreed to donate their own organs and tissues at death, unless they have opted out or are in excluded groups (for more details, please see www.organdonation.nhs.uk/uk-laws/organ-donation-law-in-england/).
Findings – knowledge, perceptions and information needs regarding deemed consent legislation in England (interviews)
Our findings from interviews indicated that most HCPs were aware of the change in law; however, understanding of implications for practice was highly variable and, in many cases, vague or unclear. Some respondents also voiced concerns about a perceived lack of institutional and/or national preparation for the change in terms of its implications for practice:
ʻI thought that was just for organ donation. I didn’t think it was for the rest.’
(HCPF00102, HPC, Acute Care)
ʻSo, in my mind, my knowledge which is limited, and I apologise for it is I thought that the rules had changed in Wales quite some time ago and that the rules had now changed in England. What I’m not clear about is whether that’s about organ donation or tissue donation and, I think, eyes come into tissue but, I could well be wrong. So, I thought the rules had changed and, I don’t know whether that’s just about organ donation or organ and tissue donation.’
(HCPI00204, HPC, Palliative Care)
ʻI mean, I’ve seen information about it but, I’ve not seen, you know, like public … a lot of publicity about it. So, from a … from a patient point of view, it might be something that might be quite difficult to enforce if you have, you know, not been given clear … or you’ve not got clear understanding really or the patients or the families have not got clear understanding about what that actually means so. I know that it’s changed and, I’m aware of that but I’m not sure how … how much the general public have been … you know, the … the information has been sort of, you know, given to them.’
(HCPL00104, HPC, Cancer Care)
ʻI think we’ve not prepared brilliantly for it; I think we still don’t proactively have those conversations despite the change in law and I think that’s something that we need to improve on as a hospice actually. You know, there’s something for me about standardising the conversation and the approach and making it a kind of, you know, we discuss this with everybody because it’s part of the law, is it something you’ve thought about, rather than turning it into a kind of, oh gosh this is a tricky conversation to have, kind of normalising that as part of the admission process and we have discussed doing that, but I’m not absolutely certain whether that has happened. I don’t know whether the doctors still do, do that.’
(HCPI00505, HC)
ʻSo, the straight answer is that was just mentioned now [legislation], that things will become clearer as it was put to me, but I, I am confident in saying I think we haven’t done any preparation for that as yet and maybe, you know, a recent study or a call such as this will get it more higher, higher up the agenda for us to be tackling as an organisation.’
(HCPI00103, HC)
Most managerial and front-line HCPs at all sites viewed the legislation positively. Despite concerns about specific implications for practice, positive sentiments were voiced in that any increase in available organs or tissue for transplant was to be welcomed:
ʻI think, it’s fantastic. I think, it’s not necessarily something that you would think about or consider until you found yourself in a situation and particularly for relatives of people wanting to make the best decision for either somebody that’s … that’s deceased or, you know, might be in a position to donate organs. I think, it just … I … I think, a lot of relatives and family want to do the right thing and would maybe not have donate because of that. Because they didn’t know the wishes of their loved ones and so, I think, having an opt-out system is … it just gives them a much clearer indication of where somebody stands about it.’
(HCPL00704, HPC, Cancer Care)
ʻYes, of course. I think, it’s a much better way of approaching things. It hopefully will make more tissues and organs available to be used because, hopefully, it will mean people talk about it more and approach the subject more rather than waiting for the donor or the donor’s family to come forward and suggest it. Hopefully it will make it easier of everybody else to talk about it either before … obviously, hopefully before the event so the patients or people are able to express their views or after a sad event, you know, broaching the family to give their input in the decision-making process.’
(HCPL00106, HCPS, Cardiology Care)
ʻI think … that I know that some people are quite sceptical of … sceptical about it and, I … I don’t know whether or not everybody has enough information about it but generally, I’m … yeah, pro the change.’
(HCPL00306, HPC, Internal Medicine)
Findings – knowledge, perceptions and information needs regarding deemed consent legislation in England (national survey)
Survey participants were asked to respond ‘true’ ‘false’ or ‘unsure’ to questions about deemed consent legislation (Table 14). Of 156 respondents, 90% (n = 140) correctly indicated that deceased patients in England are assumed to consent to organ and tissue donation unless they opt out. Most participants (97%, n = 152) were aware that patients could be selective in relation to the organs and tissues that they do/do not wish to donate. However, respondents were less clear on whether family members could overrule the wishes of the deceased, with 42% (n = 65) choosing ‘false’ to the statement ‘in the case of a patient 18 years or older with mental capacity, their next-of-kin cannot refuse donation unless the patient has indicated their wish to opt out prior to death’. If the family can provide evidence that the deceased had indicated their reluctance to be an organ/tissue donor based on previous conversations, the family can decline donation on behalf of the deceased who has not ‘opted out’ on the ODR (therefore the correct response is ‘True’).
| Participant group | Patients in England are assumed to consent to organ and tissue donation unless they opt out. (Q37.1) | In the case of a patient 18 years or older with mental capacity, family/next of kin (NoK) cannot refuse donation unless the patient had indicated their wish to opt out prior to death. (Q37.2) | Patients can opt out of donating specific organs or tissues while maintaining a wish to donate others. (Q37.3) | I am aware of the procedure for opting out of organ and tissue donation in England. (Q38.1) | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TRUE | FALSE | UNSURE | TRUE | FALSE | UNSURE | TRUE | FALSE | UNSURE | Strongly disagree | Somewhat disagree | Neither agree nor disagree | Somewhat Agree | Strongly agree | ||||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||
| I am aware of the procedure for specifying organs and tissues that I do/do not wish to donate. (Q38.2) | I am confident in my ability to talk through with patients and/or families the necessary processes for opting out of organ or tissue donation in England. (Q38.3) | Overall, the move to the opt out system has affected my clinical practice… (Q40.1) | |||||||||||||||||||||||||||
| Strongly disagree | Somewhat disagree | Neither agree nor disagree | Somewhat agree | Strongly agree | Strongly disagree | Somewhat disagree | Neither agree nor disagree | Somewhat Agree | Strongly agree | Very negatively | Somewhat negatively | Neither positively nor negatively | Somewhat positively | Very positively | |||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| Overall, the move to an opt out system has affected patients and families/NoK within my service... (Q40.2) | Have you received any information regarding the move to opt out legislation? (e.g. from your institution, or from other bodies such as NHS Blood and Transplant) (Q42) | For the information I have received regarding general implications of the legislation changes, I am... (Q43.1)a | |||||||||||||||||||||||||||
| Very negatively | Somewhat negatively | Neither positively nor negatively | Somewhat positively | Very positively | Yes | No | Completely unsatisfied | Somewhat unsatisfied | Neither satisfied nor unsatisfied | Somewhat satisfied | Completely satisfied | ||||||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||||||
| For the information I have received regarding general implications of the legislation changes, I am... (Q43.2)a | Overall, how effective do you believe the new opt out system will be in increasing supply of eye tissue? (Q45)a | ||||||||||||||||||||||||||||
| Completely unsatisfied | Somewhat unsatisfied | Neither satisfied nor unsatisfied | Somewhat satisfied | Completely satisfied | Not at all effective | Not very effective | Somewhat effective | Highly effective | Unsure how effective | ||||||||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||||||||||
| HPC (n = 58) | 51 | 52 | 3 | 3 | 4 | 4 | 20 | 34 | 28 | 48 | 10 | 17 | 57 | 98 | 1 | 2 | 0 | 0 | 6 | 10 | 8 | 14 | 10 | 17 | 24 | 41 | 10 | 17 | |
| HC (n = 98) | 89 | 88 | 5 | 5 | 4 | 7 | 40 | 41 | 37 | 38 | 21 | 21 | 95 | 97 | 0 | 0 | 3 | 3 | 11 | 11 | 15 | 15 | 12 | 12 | 42 | 43 | 18 | 18 | |
| All participants (n = 156) | 140 | 90 | 6 | 4 | 8 | 5 | 60 | 38 | 65 | 42 | 31 | 20 | 152 | 97 | 1 | 1 | 3 | 2 | 17 | 11 | 23 | 15 | 22 | 14 | 66 | 42 | 28 | 18 | |
| 5 | 9 | 7 | 12 | 8 | 14 | 24 | 41 | 14 | 24 | 7 | 12 | 15 | 26 | 13 | 22 | 16 | 28 | 7 | 12 | 0 | 0 | 0 | 0 | 55 | 95 | 3 | 5 | 0 | 0 |
| 10 | 10 | 12 | 12 | 14 | 14 | 46 | 47 | 16 | 16 | 16 | 16 | 24 | 24 | 27 | 28 | 24 | 24 | 7 | 7 | 0 | 0 | 1 | 1 | 89 | 91 | 7 | 7 | 1 | 1 |
| 15 | 10 | 19 | 12 | 22 | 14 | 70 | 45 | 30 | 19 | 23 | 15 | 39 | 25 | 40 | 26 | 40 | 26 | 14 | 9 | 0 | 0 | 1 | 1 | 144 | 92 | 10 | 6 | 1 | 1 |
| 0 | 0 | 0 | 0 | 58 | 100 | 0 | 0 | 0 | 0 | 2 | 3 | 56 | 97 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 100 | 0 | 0 | ||||||
| 0 | 0 | 1 | 1 | 93 | 95 | 3 | 3 | 1 | 1 | 10 | 10 | 88 | 90 | 0 | 0 | 2 | 20 | 3 | 30 | 3 | 30 | 2 | 20 | ||||||
| 0 | 0 | 1 | 1 | 151 | 97 | 3 | 2 | 1 | 1 | 12 | 8 | 144 | 92 | 0 | 0 | 2 | 17 | 3 | 25 | 5 | 42 | 2 | 17 | ||||||
| 0 | 0 | 1 | 50 | 0 | 0 | 1 | 50 | 0 | 0 | 1 | 2 | 11 | 19 | 31 | 53 | 3 | 5 | 12 | 21 | ||||||||||
| 0 | 0 | 1 | 10 | 4 | 40 | 3 | 30 | 2 | 20 | 0 | 0 | 10 | 10 | 50 | 51 | 22 | 22 | 16 | 16 | ||||||||||
| 0 | 0 | 2 | 17 | 4 | 33 | 4 | 33 | 2 | 17 | 1 | 1 | 21 | 13 | 81 | 52 | 25 | 16 | 28 | 18 | ||||||||||
The majority of respondents (60%, n = 94) indicated that they ‘somewhat agree’ or ‘strongly agree’ to the statement: ‘I am aware of the procedure for opting out of organ and tissue donation in England’ (Table 15). However, despite respondents being aware of the legislation, 40% (n = 62) indicated some level of disagreement with the statement ‘I am confident in my ability to talk through with patients and/or families the necessary processes for opting out of organ or tissue donation in England’.
| Participant group | I am aware of the procedure for opting out of organ and tissue donation in England. (Q38.1) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Strongly disagree | Somewhat disagree | Neither agree nor disagree | Somewhat agree | Strongly agree | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Participant group | I am aware of the procedure for specifying organs and tissues that I do/do not wish to donate. (Q38.2) | |||||||||
| Strongly disagree | Somewhat disagree | Neither agree nor disagree | Somewhat agree | Strongly agree | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Participant group | I am aware of the procedure for specifying organs and tissues that I do/do not wish to donate. (Q38.3) | |||||||||
| Strongly disagree | Somewhat disagree | Neither agree nor disagree | Somewhat agree | Strongly agree | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| HC (n = 58) | 6 | 10 | 8 | 14 | 10 | 17 | 24 | 41 | 10 | 17 |
| HPC (n = 98) | 11 | 11 | 15 | 15 | 12 | 12 | 42 | 43 | 18 | 18 |
| All participants (n = 156) | 17 | 11 | 23 | 15 | 22 | 14 | 66 | 42 | 28 | 18 |
| HC (n = 58) | 5 | 9 | 7 | 12 | 8 | 14 | 24 | 41 | 14 | 24 |
| HPC (n = 98) | 10 | 10 | 12 | 12 | 14 | 14 | 46 | 47 | 16 | 16 |
| All participants (n = 156) | 15 | 10 | 19 | 12 | 22 | 14 | 70 | 45 | 30 | 19 |
| HC (n = 58) | 7 | 12 | 15 | 26 | 13 | 22 | 16 | 28 | 7 | 12 |
| HPC (n = 98) | 16 | 16 | 24 | 24 | 27 | 28 | 24 | 24 | 7 | 7 |
| All participants (n = 156) | 23 | 15 | 39 | 25 | 40 | 26 | 40 | 26 | 14 | 9 |
When asked to summarise their understanding of processes for opting out of organ or tissue donation, participants’ free-text responses indicated a range of knowledge about deemed consent legislation and further knowledge gaps and information needs:
ʻThe individual has to go onto the NHS Organ Donation website and register their decision either opt in or opt out.’
ʻVia organ donation website – able to complete a form with your details and wishes – either to opt out completely or specify organs which you would not wish to be donated. If unable to access internet, there is a telephone service where you can complete the process. Information leaflets are available (although we don’t have any at my place of work)’
ʻI need to be updated to the law, the process where I am now working and the regional need’
ʻMore information about the law change and how to challenge family attempts to overrule patient wishes- in practice, this tends to prevent the procedure occurring’
ʻI need to improve my understanding. The change in law came in the midst of COVID and has gone by without us taking appropriate notice of it’
Participants were also asked to evaluate the impact of the legislation change on their clinical practice, as well as patients and/or families (Table 16). Most respondents (92%, n = 144/156) indicated that the introduction of opt-out legislation had ‘neither positively nor negatively’ impacted on participants’ clinical practice; most participants also gave the same response in relation to the perceived impact on patients and families (97%, n = 151/156).
| Participant group | Overall, the move to the opt out system has affected my clinical practice… (Q40.1) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Very negatively | Somewhat negatively | Neither positively nor negatively | Somewhat positively | Very positively | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Participant group | Overall, the move to an opt out system has affected patients and families/NoK within my service... (Q40.2) | |||||||||
| Very negatively | Somewhat negatively | Neither positively nor negatively | Somewhat positively | Very positively | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| HC (n = 58) | 0 | 0 | 0 | 0 | 55 | 95 | 3 | 5 | 0 | 0 |
| HPC (n = 98) | 0 | 0 | 1 | 1 | 89 | 91 | 7 | 7 | 1 | 1 |
| All participants (n = 156) | 0 | 0 | 1 | 1 | 144 | 92 | 10 | 6 | 1 | 1 |
| HC (n = 58) | 0 | 0 | 0 | 0 | 58 | 100 | 0 | 0 | 0 | 0 |
| HPC (n = 98) | 0 | 0 | 1 | 1 | 93 | 95 | 3 | 3 | 1 | 1 |
| All participants (n = 156) | 0 | 0 | 1 | 1 | 151 | 97 | 3 | 2 | 1 | 1 |
Participants were asked to elaborate on their answers regarding the impact of opt-out legislation. Several responses indicated uncertainty around impact of the legislation change stemmed from outstanding knowledge needs regarding the implications of this change, as well as resources to support implementation into existing services:
ʻI’m not sure the legislative change has really made a difference; it still relies on the culture of working positively to support this process, and promoting this culture needs ongoing work.’
ʻNo impact seen as yet, but I think this is because we need to change our practice and get up to speed with the possibility of donation.’
ʻNil change to my practice, although made this more aware to team members. Large amount of the clinical and non-clinical MDT as well as patients still do not know about this system.’
ʻAs mentioned earlier, it may increase organ and eye donation in ITU setting but in hospice/palliative care setting, I would not use opt-out system as a means of assuming consent and would always discuss eye donation with the patient as part of ACP. Sometimes I have discussed donation with relatives prior or just after death if the patient was unable to participate in any ACP discussions and donations have happened when the NoK has confirmed it would have been the patient’s wish to donate eyes. I feel it would be inappropriate to use the ‘opt-out’ system alone to try and increase eye donations in hospices, if families disagreed, they would just refuse to cooperate with eye bank anyway and it would cause bereavement issues and complaints.’
Participants reported that the change in legislation had not been sufficiently covered in the media, possibly related to the COVID-19 pandemic, although a few felt that the media attention had supported discussion of ED.
ʻI think the change in law was lost as it came during the pandemic when we all had other focuses/priorities. I remember seeing the opt out at the time (and trying to establish from the blood and tissue authority website whether donations could still occur during covid pandemic- website didn’t answer this question at the time) and to be honest I’d forgotten about the change in law until I saw the question here and remembered. It all perhaps needs a relaunch to both professionals and the public when we’re not side-tracked by other things- feels a bit like it slipped in under the radar and I’m sure there will be some members of the public who would want to opt out and would feel a bit tricked by not realising the law has changed.’
ʻI think due to covid emergency, the move to opt out has had virtually no publicity or training alongside it. The public are not aware at all, and a lot of professionals aren’t either’
ʻI think the media attention surrounding the opt-out system has enabled the discussions surrounding donation to be normalised more and has encouraged families to talk more about their wishes, so when we ask patients about cornea donation it is not such a taboo subject.’
When asked about information received regarding the move to opt-out legislation (Table 17), 92% of all the participants (n = 144) indicated that they had not received any such material from either their institution or national bodies such as NHSBT. Twelve participants indicated that they had received material of this type, of which seven indicated some degree of satisfaction with information on the general impact of legislation changes, and six indicated some degree of satisfaction with information regarding the impact of legislation on their specific service.
| Participant group | For the information I have received regarding general implications of the legislation changes, I am... (Q43.1)a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Completely unsatisfied | Somewhat unsatisfied | Neither satisfied nor unsatisfied | Somewhat satisfied | Completely satisfied | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Participant group | For the information I have received regarding general implications of the legislation changes, I am... (Q43.2)a | |||||||||
| Completely unsatisfied | Somewhat unsatisfied | Neither satisfied nor unsatisfied | Somewhat satisfied | Completely satisfied | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Participant group | Overall, how effective do you believe the new opt out system will be in increasing supply of eye tissue? (Q45)a | |||||||||
| Not at all effective | Not very effective | Somewhat effective | Highly effective | Unsure how effective | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| HC (n = 58) | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 100 | 0 | 0 |
| HPC (n = 98) | 0 | 0 | 2 | 20 | 3 | 30 | 3 | 30 | 2 | 20 |
| All participants (n = 156) | 0 | 0 | 2 | 17 | 3 | 25 | 5 | 42 | 2 | 17 |
| HC (n = 58) | 0 | 0 | 1 | 50 | 0 | 0 | 1 | 50 | 0 | 0 |
| HPC (n = 98) | 0 | 0 | 1 | 10 | 4 | 40 | 3 | 30 | 2 | 20 |
| All participants (n = 156) | 0 | 0 | 2 | 17 | 4 | 33 | 4 | 33 | 2 | 17 |
| HC (n = 58) | 1 | 2 | 11 | 19 | 31 | 53 | 3 | 5 | 12 | 21 |
| HPC (n = 98) | 0 | 0 | 10 | 10 | 50 | 51 | 22 | 22 | 16 | 16 |
| All participants (n = 156) | 1 | 1 | 21 | 13 | 81 | 52 | 25 | 16 | 28 | 18 |
While 71 participants (46% of n = 156) provided free-text comments indicating that they did not have any outstanding information/training needs (Q44), a further 22 participants (14%) identified a range of information and training needs (however, there was no discernible pattern to these responses).
Commentary – deemed consent legislation
Findings indicate that while most participants were aware that the ‘new’ deemed consent legislation in England is for patients to opt out of organ and tissue donation, and that specific organs and tissues could be ‘excluded on the ODR’ by potential donors, clinicians were not able to access the ODR and were, therefore, not able to gain information about the patient’s donation status ahead of any conversations.
Furthermore, as no participants in HC settings and most in HPC had not received any training or guidance from NHSBT-OTDT or NHSBT-TES about implementation of the new legislation, it is not surprising that participants were uncertain regarding family involvement in donation decision-making under the new legislation, with participants indicating low confidence if they were asked about procedures for opting out of donation by patients and families.
A key knowledge gap compromising perceptions of capability is the lack of any specific guidance to clinicians working in HC and HPC services regarding deemed consent legislation and its operationalisation into practice by NHSBT. The gap is noted at both study site level and nationally. Current training in deemed consent legislation has not been shared with the majority of clinicians working in HC and HPC settings despite the greater potential for ED from these contexts and this lack of knowledge in how to implement deemed consent legation is a key barrier to this option becoming routine practice. Of note is that there appears to be an assumption by organisations such as NHSBT that the change in legislation ‘will’ address the shortage of organs, tissue and eyes despite evidence indicating this is not the case. Research into the barriers to donation (operational, organisation) is needed to fully explicate the continuing supply issues.
Recommendations for practice
-
By applying the Organisational Readiness for ED Assessment Checklist (OREDAC) NHSBT-TES can assess the ED climate of a site as part of a strategic process of future site selection and development.
-
NHSBT-TES need to develop accessible (online via their website) clinically relevant information to support service providers in the early identification and assessment of all patients admitted to HC and HPC settings against eligibility criteria.
-
Clinical sites need access to the ODR so that they can assess patient status.
-
Provision of feedback data regarding their referral rates, donation rates and use of donated eye tissue would impact motivation to embed ED in routine practice.
-
A dedicated link nurse (employed by NHSTB-TES) would act as a resource and champion working in close partnership with referring sites.
-
An evidence-based, centrally generated (by NHSBT-TES) education and training programme that could be rolled out nationally via various modalities (e-learning for health platforms, in-house education teams, donation champions, etc.) would ensure clinicians have up to date, and regularly updated, training to support their practice.
-
Specific information and guidance regarding implementation of deemed consent legislation is urgently needed by HCPs working in palliative care settings.
-
Public awareness-raising initiatives are needed to inform patients in HC and HPC services about the option of ED. This can be achieved by ensuring that centrally generated (by NHSBT-TES) web content is shared with the UK-based HC and HPC organisations via their professional bodies (e.g. Association for Palliative Medicine and Hospice UK).
Chapter 7 Perceptions, preferences and propriety – service users (WP2S2)
Chapter 7 addresses study Objective 4: identify service users’ views regarding the option of ED and the propriety of discussing ED as part of admission procedures or as part of EoLC planning conversations. Chapter 7 also describes recruitment and data collection processes for interviews with patients and families/carers under the care of HC and HPC services.
Methods
Identification and eligibility criteria
Potential participants were identified from existing clinic lists by PIs at partner sites. Eligible participants were patients or families/carers of those currently (or previously in the case of families/carers) under the care of HC or HPC services, aged 18 years or over, who had capacity to provide informed consent and to participate in the interview (in English). For those families/carers who were bereaved but may have been willing to discuss their experiences, approach for participation was at the discretion of the site PI.
Recruitment (sites S03–S06)
Following the ethics amendment (ERGO ID 59185) and change to protocol, approaches to potential participants continued to be made through PIs or their delegates in the first instance. The PI discussed the study with potential participants, and (participant-willing) shared their contact details with the research team.
Contact details of potential participants were shared with the study team (MJB, BMS) via secure systems. Team members contacted interested participants to discuss the study and agree next steps for providing study information. All study materials (e.g. letters of invitation, PISs, reply slips) were shared with potential participants via electronic means (e.g. e-mail). In instances where this was not possible, information was mailed to the participant following a telephone conversation with the study team.
Once agreement was in place for the interview to commence, the responsible researcher (MJB or BMS) explained the consent process (i.e. that consent to participate would be audio recorded before the interview commenced). The researcher then read out the consent form over the telephone asking the participant to respond by stating ‘Yes/No’ or ‘I agree/disagree’ to the relevant questions. The researcher recorded (electronically) the responses of the participants on the consent form, adding a countersignature and date of consent.
Electronically returned consent forms were stored in a secure location within the EDiPPPP project drive on the University of Southampton systems, to which only the study team had access. Hard copies of returned consent forms were scanned and saved to the same folder, then shredded and disposed of securely.
Data collection
Interview and focus group schedules for data collection were informed by the literature base and the RAPiD tool for identification of barriers to donor information and referral. 78 Interview schedules involved questions mapped to the following areas of interest: Perceptions (of ED and related processes); Propriety (of whether this topic should be discussed with patients); and Preferences (related to who should raise the issue of ED, when should these conversation take place and who should make decisions about ED) (see Report Supplementary Material 14: Patient interview schedule, v2, 20 March 2019, for patient interview schedule and Report Supplementary Material 15: Carer interview and focus group guide, v2, 20 March 2019, for carer interview schedule).
Data management and analysis
Data management and analysis for interviews with patients and carers followed the same process as for HCPs, as described in Chapter 2.
Findings
Findings from WP2S2 interviews are reported under the EDiPPPP study domains Perceptions, Propriety and Preferences. Reporting of each domain concludes with a commentary section in which findings are discussed in relation to relevant findings in extant literature. The purpose of the commentary sections is to focus discussion towards implications for service development and intervention design. Findings for patients are presented first, followed by findings from carers with synthesis in the commentary sections. Findings are supported by exemplar quotes with tags indicating the location of the patient’s care context (e.g. whether HC or HPC), and whether the respondent is a patient or carer. The chapter concludes with recommendations for practice.
Outcome of recruitment – patients and carers
Thirty-nine patients (21 HC, 18 HPC) completed interviews. Most participants (90%, n = 35) were aged 50 years or older, with 24% (n = 9) aged 80 years or over. Fifty-four per cent of participants were female, a further 54% were in a relationship (i.e. ‘Married’ or ‘In a partnership’), 85% (n = 33) were of White British ethnicity and 69% (n = 27) were retired from work (Table 18).
| Category | Group | Patients (n = 39) | Carers (n = 23) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HPC (n = 21) | SPCS (n = 18) | All (n = 39) | HPC (n = 13) | SPCS (n = 10) | All (n = 23) | ||||||||||||
| n | % (of site type total) | n | % (of site type total) | n | % (of site type total) | n | % (of site type total) | n | % (of site type total) | n | % (of site type total) | ||||||
| Age group (years) | 18–29 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||
| 30–39 | 0 | 0 | 1 | 6 | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| 40–49 | 1 | 5 | 2 | 11 | 3 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| 50–59 | 5 | 24 | 4 | 22 | 9 | 23 | 2 | 15 | 3 | 30 | 5 | 22 | |||||
| 60–69 | 8 | 38 | 3 | 17 | 11 | 28 | 4 | 31 | 2 | 20 | 6 | 26 | |||||
| 70–79 | 3 | 14 | 3 | 17 | 6 | 15 | 5 | 38 | 3 | 30 | 8 | 35 | |||||
| 80–89 | 4 | 19 | 1 | 6 | 4 | 13 | 2 | 15 | 0 | 0 | 2 | 9 | |||||
| 90+ | 0 | 0 | 1 | 6 | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Prefer not to say | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Missing data | 0 | 00 | 3 | 17 | 3 | 8 | 0 | 0 | 2 | 20 | 2 | 9 | |||||
| Gender | Female | 12 | 57 | 9 | 50 | 21 | 54 | 8 | 62 | 9 | 90 | 17 | 74 | ||||
| Male | 9 | 43 | 9 | 50 | 18 | 46 | 5 | 38 | 1 | 10 | 6 | 26 | |||||
| Prefer not to say | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Relationship to patient | Child | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 0 | 2 | 20 | 2 | 9 | ||||
| Parent | N/A | N/A | N/A | N/A | N/A | N/A | 1 | 8 | 0 | 0 | 1 | 4 | |||||
| Sibling | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 0 | 1 | 10 | 1 | 4 | |||||
| Spouse/partner | N/A | N/A | N/A | N/A | N/A | N/A | 12 | 92 | 7 | 70 | 19 | 83 | |||||
| Missing data | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Ethnicity | White British | 19 | 90 | 14 | 78 | 33 | 85 | 13 | 100 | 8 | 80 | 21 | 91 | ||||
| White Irish | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Other white | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| White and Black Caribbean | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| White and Black African | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| White and Asian | 1 | 5 | 0 | 0 | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Other mixed | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Indian | 1 | 5 | 0 | 0 | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Pakistani | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Bangladeshi | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Other Asian | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Prefer not to say | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Missing data | 2 | 0 | 4 | 22 | 4 | 10 | 0 | 0 | 2 | 20 | 2 | 9 | |||||
| Occupation | Employed/working | 2 | 10 | 2 | 11 | 4 | 10 | 1 | 8 | 2 | 20 | 3 | 13 | ||||
| Unemployed | 0 | 0 | 2 | 11 | 2 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Retired | 18 | 86 | 9 | 50 | 27 | 69 | 12 | 92 | 5 | 50 | 17 | 74 | |||||
| No response | 1 | 5 | 1 | 6 | 2 | 5 | 0 | 0 | 3 | 0 | 0 | 0 | |||||
| Missing data | 0 | 0 | 4 | 22 | 4 | 10 | 0 | 0 | 0 | 30 | 3 | 13 | |||||
Twenty three carers completed interviews (13 HC, 10 HPC). Most participants (83%, n = 19) were aged 50–79 years. Seventy-four per cent of participants (n = 17) were female, 83% (n = 19) were a spouse or partner of an HC or HPC patient, 91% (n = 21) were of White British ethnicity and 74% (n = 17) were retired from work (see Table 18).
Perceptions regarding the option of eye donation
The perceptions domain of EDiPPPP relates to individual attitudes, views, opinions and experiences about donation generally and ED specifically.
Perceptions – patients
Patients being cared for in HC and HPC settings were asked about their views regarding donation in general, before being asked about ED specifically. Most patients were positive about donation, while for a minority, the issue of donation did not align with their personal or faith-based views. For those who were positive about donation in general, a key motivating factor was the opportunity to help other people, aligned with a belief that the donated tissues would not be needed by the donor after their death:
ʻYes, I am quite happy for donation … to donate my body and/or any organ that needs … that’s needed for anyone. Yes. Well, I won’t need them. So, they could be useful for somebody else. I’m quite happy for that.’
(P00302, HPC Patient)
ʻI’m not going to be about (laughing). If I can help somebody else then … then, I’m quite happy to do that.’
(P00406, HPC Patient)
ʻI’ve never, I’m not one for donating, I’ve always thought I’ve been against it like really ... Sorry I’ve never thought about it really in depth. Yes, that’s all I could think of really, I’ve never thought about it.’
(P00305, HC Patient)
ʻI don’t mind other people donating and I would, but my faith doesn’t allow me to, we have to be cremated and I wouldn’t want to leave bits of me out of being cremated, you know, a little bit like those Egyptians, I mean they even took their stuff with them in case, you know, this is what the thinking is, I mean if you’re going to go down that road, then you want to go the whole of you or none of you.’
(P00903, HC Patient)
Patients were asked if they were aware about the option of ED before they had been approached to be part of the EDiPPPP study. Most patients were unaware of the specific option of ED, with those that were aware either unclear how they became aware, or providing indications of general awareness through media sources:
ʻNot a lot really. No, I can’t really, I don’t really know that much about it … obviously, you know, if somebody’s passed away and the donation, same as the donation for any other parts, kidneys or anything like that, I’d assume that the eye donation is the same thing.’
(P00703, HC Patient)
ʻNever heard of it, my personal view was, this is what my perception was, that if you detach the eye from the retinae or the optic nerve or something, the whole thing does not work and I hear a lot about organ donations, specifically kidneys and livers and this kind of thing but never have I seen in any advert on television or any kind of media [on] eye donation.’
(P00903, HC Patient)
ʻYeah. Yeah, but more in a … a comic book scientific sort of like manner. Well, what it … yeah, there was a record in 1977 called … by the Adverts called: ‘Gary Gilmore’s Eyes’ and it was about someone had a … a … an eye transplant and then you … with this merging his eyes called Gary Gilmore and it was taking over their … their mind.’
(P00604, HPC Patient)
ʻI didn’t know it existed, no, I really didn’t.’
(P00201, HC Patient)
ʻIt was (name) that came in. Yeah, (about the study) because when I had cancer the first time … I used to be a blood donor and, I was told that: ‘you can’t get involved in anything once you’ve got cancer’. So, of course, that all had to stop.’
(P00602, HPC Patient)
Patients were asked about their views regarding ED. Most participants specifically mentioned that they would be willing to consider ED, with a minority having some reservations linked to a lack of awareness as to whether or not they would be eligible to donate given their health status:
ʻI just thought that when we go, I don’t think your eyes are going to be any good to you but they’re going to do good for somebody else. And when I see people that … you know, like TV programmes where children are going blind and … and it … it just … it puts it all into perspective and that it seems to have … sort of lately, there’s a lot of adverts about children losing their sights and so … and, I thought, you know: ‘don’t be selfish’ and that’s … that’s … and it’s … it … it didn’t take long to change my mind, if I’m honest. So, I … that’s how I felt about it so.’
(P00404, HPC Patient)
ʻI’m fully in favour of that. At eighty-four, I didn’t think much of my organs would be any good so I was quite surprised to find that eyes can still be used even at this age, which was a rather nice thought for me, because I thought well if and when something happens to me, I can still be of use to somebody else in this world then that would be a very positive.’
(P00401, HC Patient)
ʻI’m all for it, I think yes, we should all … we don’t need them, we don’t need the parts anymore so why not let somebody else have a better quality of life.’
(P00605, HC Patient)
ʻI think, what happens to you after you’ve died is irrelevant. I really do, after all they’re only going to burn you, so if you keep your eyes, they’re not going to do you any good. That’s my general view on that particular topic.’
(P00201, HC Patient)
ʻBefore I got diagnosed with cancer, I thought it was a very good idea, no matter what part of your body you were donating, but as long as you were a match to the other person. For me now, having cancer, I don’t know whether my organs would be any good for anybody else.’
(P00603, HC Patient)
Within the group of patients reporting reservations regarding ED, some indicated that their reticence was due to beliefs that the eyes would be needed in the afterlife, or that they wanted to be buried whole:
ʻThe eyes though have a little bit more difficulty and I think it’s the same for most people. They can cope with the idea of, because their hearts stopped and whatever, that those type of our organs can be used, but when it comes to eyes, it’s a bit more, oh dear, what happens on the other side? This is how I see it. I do believe that there is life after death and giving my corneas up, then how am I going to see, what am I going to see with, that I find quite scary.’
(P00101, HC)
ʻMy personal views are I’m a Christian so, even though I believe that when I die it’s my shell that’s left, I’m quite … I … I want to be buried whole really. Part of me would like to donate but the other part of me wants to be buried whole. I don’t want to be cremated definitely. I’ve already arranged my funeral. So, that side of it is all sorted out. So, my feelings are … and your eyes are very personal, I think. Personally, I wouldn’t want my eyes donated. I’d probably say yes to a lot of my innards if … you know, if they were needed. But it’s not for me. Not the … the eye donation. Possibly the other organs. But really, I think, I want to be buried whole unfortunately. I feel bad saying it really because we’re all encouraged to do it as medical people and as … generally as a public, we’re all encouraged to do it anyway because there’s not enough organ donation on … you know, people on the register. So, I do feel a bit guilty about that really but, yeah, that’s it.’
(P00202, HPC)
Perceptions – carers
Carers were also asked what their views were regarding donation in general, followed by their views about ED specifically:
ʻYeah. Well (laughing), my husband had for many years a donor card and, I wasn’t for it because I … I’m … I’m not happy about the idea. Somebody whom I love being dissected if you know what I mean (laughing). So, I wasn’t for a donation in those days at the beginning but, I respect his wishes. You know if he wants to do that, you know, I’m fine with it now. I had time to think about it and accept it although originally, I … I wouldn’t have and if you would have his eyes and that, I don’t want to know what you’re going to do with it. I’m sorry (laughing), it might seem a bit blasé but, I … I don’t want to know what you’re going to do with his … I don’t mind if he makes the donation. It’s up to him but, I wouldn’t want to know about it. I … I … I’d find it emotionally a bit draining, I think, and I’m worried about having nightmares about it as well (laughing).’
(C00506, HPC Carer)
ʻMe, personally, my thoughts are … that when I’m dead, that basically my body is just … you know, the carcass of … of what I was and that if there’s anything of any use to anybody, including my eyes, anything ... what’s the point of just burning me when … if … if there’s bits of me that could keep somebody else alive? So, you know, personally I think, it’s really important.’
(C00206, HPC Carer)
ʻWell I’m a, I’m a very strong believer in organ donation, I have family members who have actually received organs, which has actually made it, you know, brought it home even more to me and yes, and I don’t see why eyes or anything in fact should be at stake, so I wouldn’t have a problem at all if someone was to ask me if one of my relatives could, or we could donate eyes.’
(C00401, HC Carer)
ʻI, I don’t think there’s a problem with it at all because I believe once, once somebody’s passed away then basically, you know, the body’s just not human any more, so if, if any of the parts can be put to good use to help people who are alive and require those parts, then I think there’s nothing wrong with transplanting things.’
(C00305, HC Carer)
While carer participants from the HPC and HC settings perceived organ donation in a positive light, some expressed reservations about ED specifically, while others did not see that ED was any different from organ donation:
ʻI’m completely for it. I … although it’s interesting that the eye donation … because it’s such a personal aspect of a person’s, you know, make-up, physical make-up, it’s actually one of the … one of the few areas where I would have some reservations, I think. But with all other non-identifiable organs, I … I one hundred per cent believe it’s a great thing and … and needs to happen …’
(C00402, HPC Carer)
Yeah, funny enough, I’ve been thinking about this since this cropped up [invitation to participate in the study] and … to see how I would personally feel about eye donation because, as I say, I don’t have a problem in … in general with donation at all but obviously, eyes are, I suppose, a little bit more personal if you … if you … because … because you can see them and I … I started to think would it matter to me or not? And as I’ve had time to think about it, no, I don’t think it would matter if my eyes were taken from me because I’m not going to need them. So, I’d be happy … I … I’ve decided now, I would actually be happy to donate my eyes.
(C00106, HPC Carer)
ʻI don’t quite understand why the difference to do with eyes as anywhere else (laughs) if you’re really willing to give your body, you’re willing to give every part of it that might be useful. I mean, my personal … my eyes I can’t imagine that they’d be used, of use to anyone, but they might be (laughs) because I’m so short sighted, I’ve got lots of, you know, so I can’t imagine they’d be any use, but I would expect if I had offered my body for organ donation that eyes would be part of that.’
(C00103, HC Carer)
ʻWell, personally I don’t think it’s an issue for the reasons I’ve given, because obviously once, once a person’s died that’s just flesh and blood I don’t think there’s, the person has any feelings or it’s actually the person that we, we associate with the person that we know, it’s just, it’s just a corpse so the corpse is going to get buried or cremated, it’s a waste of body parts if the body parts could be used to help somebody else.’
(C00305, HC Carer)
Carers were asked about their awareness of ED. There was a general level of awareness, mainly from the media, but not from the clinical or health-related sources:
ʻWell, I … I … yeah, because as far as I was concerned, you could … there’s so much of somebody that you can … that can be donated to help somebody else. Yeah. So, I’m sure I’d heard of eyes being donated.’
(C00102, HPC Carer)
ʻGenera l … general information through TV and media stuff. Yeah, I just … no, I don’t actually … it’s something. Certainly, corneal transplants I’ve heard of.’
(C00202, HPC Carer)
ʻNo, I hadn’t given it a thought and, I hadn’t had it … it’s not very wide-spread. Like your saying: ‘how many people leave these donations?’ and: ‘you’re only doing a drop in the ocean’. So, no, I hadn’t realised that.’
(C00406, HPC Carer)
ʻWell, when I first read the information sheet, I thought, woah eyes, yes right. I didn’t realise it was the whole eye, because I asked the doctor there, the consultant, is it your whole eye or is it just your lens or what and she said ‘no it’s the whole eye’. And I said is it before death or after death. After death. So, in the short time, because I only saw her yesterday, so in the short time of thinking about this I, I think it’s a good idea and I, I would be comfortable with it, but I would, I would like to have known about it for longer and I think it’s the surprise of it coming along, you know.’
(C00205, HC Carer)
ʻI think, I think I just heard about it on the news or some article there being the concerns about some people not wanting to, they were alright to offer their other organs but for some reason they didn’t seem very keen on donating their eyes.’
(C00305, HC Carer)
Commentary – perceptions
Findings from interviews indicated that patients and carers held positive views towards donation, and the majority were also positive about ED when asked. For those who had reservations, their views resonated with findings from extant literature indicating that eyes may be needed in the afterlife,5,6 or that the idea of ED may be perceived as unpleasant,4 stimulating the ‘ick response’ or feelings of squeamishness. 7 However, what is clear from findings is that almost all patient and carer participants were not aware about this option, and believed that a patient with a cancer diagnosis could not be an eye donor. In fact, most patients were surprised that they could donate their eyes due to their age (i.e. believing themselves too old) or believing that other health conditions would prevent this. For those patients and carers who were positive about ED, the general view was that if the eyes could be of use to someone else, that would be a good thing.
Propriety of discussing eye donation within end-of-life care planning
Propriety – patients
In view of research indicating a view that the issue of ED should not be raised with patients moving towards their end of life (proposed by HCPs and some family members),38,41 patient participants were asked whether the option of ED should be offered to patients under the care of palliative care and hospice care services:
ʻYes, I think, everybody should be asked if they want to do it because sometimes … it’s not something you think about. Even when you know you’re … not going to be here for much longer … It … might be the one thing that they want to … to donate and they don’t want to donate anything else. So, if you ask them it’s … it’s up to them, isn't it? It’s their choice.’
(P00404, HPC Patient)
ʻOh yes, I do. I do. Yes. Yes, it is … for the least they’re … they’re … they’re given the opportunity to say yes or no. I was going to say that you … obviously, it’s try … trying to pick the right moment to bring it up which … that’s the difficulty, I suppose. But I … in my experience, I would say that the … the sooner the better to bring it up.’
(P00804, HPC Patient)
ʻI am quite forward planned. I like, you know, to know it’s ticked off and then I can relax knowing that what I want no one else is gonna have to deal with when I pass away. You know, I don’t want my friends to have to worry about that because, I haven’t got any family anymore and, I’ve not been very well.’
(P00202, HPC)
ʻYes, because it makes you feel that you’ve given something back which is worthwhile, you know.’
(P00201, HC)
ʻI think possibly, I think a lot of people wouldn’t be thinking about eye donation, they’re thinking of hearts and lungs and all that, and some people don’t like the idea of the eyes, I’m not quite sure why but I think maybe it should be discussed a little bit more than just on the donating form sort of thing, or people in that position should be asked a little bit more about it perhaps. So yes, I think it’s not well known enough that even over eighties, they can still use your eyes, I don’t know whether the government’s new ruling that you have to opt out of being donated, rather than opt in, does that include eyes, I don’t know.’
(P00401, HC)
Propriety – carers
Carers were also asked if this topic should be raised with their family member as part of end-of-life planning:
ʻAbsolutely when … when they go into palliative care, they’ve already been asked all … all the other questions of: ‘how … how do you feel about … if … if your heart stops, do you want to be revived?’. All those things. So, why isn’t that just an extra question in there? What … I don’t understand … I really don’t understand where there’s a problem there. If you’re going to go into palliative care, you don’t go into palliative care without being asked all the right questions, I would hope. And that’s just another question.’
(C00202, HPC)
ʻI guess … I guess it … it’s probably on a case-by-case basis because it all depends on how aware that individual patient is of being … of the … you know, the prognosis for them. You know, in the case of my Dad, I would say he perhaps doesn’t really understand what’s happening and therefore … yeah, it has to be informed consent, I suppose, as … as with any medical decision. So … so, yeah, I … I think, where a patient is able to cope emotionally with a decision of that nature then, I think, it … I think, it’s … the … I think, it’s a good thing.’
(C00402)
ʻYou see at end of life, I would imagine there may be other things that appear to the individual that’s coming to end of their life as being more important. But at the same time, I would have thought it would have given a lot of people a lot of strength to think that they’re still participating in a social activity that’s really going to benefit someone else. So, clearly there are exceptions to prove the rule, but I would imagine as long as the person delivering the information has an empathetic, caring delivery system, I personally wouldn’t see any issue with it whatsoever.’
(C00101, HC)
ʻI think the timing is crucial, you see if you ask somebody when they’re, they’re loved one is in a hospice or about to die, you know, will you donate your eyes, I would think that’s the last thing they want to actually think about at that point. It needs to be, have been agreed or, or accepted at a much earlier stage I think, so that some of the emotion around it is taken away because my own personal view is that I, I, my family know that I was willing to donate before it became, is it law, is that the right way to say it? Before it became law, I was willing to donate anyway … So, in terms of eye donation for people in hospices and things, it is about the timing of when that question is asked or when that expectation is understood … I know that I myself prior to that new legislation was down as a donor and anything worth having they’re welcome to. So, yes, I personally would be quite aggrieved if my useful parts were not put to use if I were to have an untimely death and everyone who knows me is aware of that, so there’d be no excuse for it not to happen.’
(C00205, HC)
In view of research indicating that HCPs are reluctant to raise the issue of donation as part of care planning,33,38,41 carer participants were asked if they thought that HCPs should raise this issue with patients and/or families. All carers indicated that the topic should be raised, and acknowledging that this would be perceived as a challenging conversation:
ʻI don’t see a problem raising it, except personal. If someone’s got a personal reluctance, I’m not sure we can do much about that because you’re not … you … there’s no way you want to legislate for it therefore maybe they could … if … if need be … effectively pass the buck and actually say: ‘look, I’m not prepared to do this’. But the … there’s usually a team so, there must be someone on the team that will do it.’
(C00202, HPC Patient)
ʻYes, I … I do actually. I mean, recently the issue was raised. [HUSBAND] had to go into hospital and he was … it was raised about arranging a DNR. Well, if you can do something of that nature and obviously you know what that is, it … then I don’t see why it couldn’t be raised about how people feel about donating their eyes or any other part of their body after their death.’
(C00106, HPC Patient)
ʻI can understand that I’m sure an awful lot of people are particularly sensitive about eyesight, or so I’ve been led to believe. I can understand why but if providers need more training or assistance to help them better meet the needs. It’s a discussion, if it’s all part of, end of life, I have no real experience of it personally, but end-of-life discussions I can’t imagine it’s an easy conversation to have, but it’s still part of an important process to go through, I would imagine. I mean it’s not just another thing, but it’s all encompassed in a well-delivered empathetic, kindly environment I really don’t see any issue with it personally.’
(C00101, HC Patient)
ʻAgain, I think it, it’s a very, very, very difficult subject to broach and it’s also a difficult subject for certain healthcare professionals to approach the person about. And then, you know, this patient comes in, they’re clearly not well, they make them comfortable, they do what they’ve got to do, but that’s it, nothing else is talked about … So I just think, I think people need, they need to be, I know there’s an organ, organ donation team that, you know, collect organs because as I say we’ve had this with the family, but I don’t think there’s enough special, just we say specialist healthcare professionals out there, trained in awkward conversation. Because again, it’s a conversation that, you know, somebody asks you, and you think actually, no, I can’t deal with this, you know, you’ve got too much going on and yes, you know, you have lost that opportunity if you like, but that family are aware. And it could be a couple of days down the line that you think actually, do you know what, that makes so much sense.’
(C00401, HC Patient)
Commentary – propriety
All but one patient and all carers participating in this research indicated that ED should be an agenda item for discussions as part of ongoing care planning. Participants acknowledged that not everyone would want to have this discussion, and that the conversation must be introduced at an appropriate time; however, there was no clear consensus from participants as to what constitutes ‘appropriate timing’.
Patients across the data set made comments about not knowing about the option of ED, or being told they could not be a donor due to their clinical condition despite being in favour of donation and, for some, being blood donors or registering organ and/or tissue donors during their lifetime. The view reported by HCPs and family members in previous research that raising this topic would be distressing is not supported in the data set. Findings indicate that patients should be asked about their preferences, and if they do not want to discuss the topic, they will say so.
Preferences around discussing eye donation
Preferences – patients
Interviews with patient participants indicated that none of them (100%) had been approached about the option of ED in their current clinical care context or in previous settings. We asked patients their preferences with respect to who they thought should raise the issue of ED, participants indicated a range of views:
ʻI think the nurses that are looking after them, I mean I’ve been in the hospice twice and the nurses in the hospice are a cut above and they know how to treat a person. I think they know generally if you’re talking about it whether or not the patient would be willing to do that.’
(P00105, HC Patient)
ʻIt doesn’t necessarily have to be a doctor, but they have to be like a nurse practitioner or something like that or somebody who knows about the body because if you had a social worker for instance saying how, about this, they wouldn’t really be able to answer the question would they. Because people would wander off the subject and go on to other questions about medical things.’
(P00201, HC Patient)
ʻI think, it should be the consultant.’
(P00304, HPC Patient)
ʻI think, it should be … the doctor … Nurses have enough sort of dealing with the pain and upset of it all without having to bring something like that up.’
(P00404, HPC Patient)
Patients were asked about their preference as to when the option of ED should be raised:
ʻProbably quite early on, I would have thought. Yeah. Just to get … plant the seed. I mean, like I’ve said, I’ve seen here when it’s been talked … not with eyes obviously but in general and people get angry. So, I would probably want to plant the seed early on and just mention, you know … start it off a little bit, you know, and … so, I would say early on. Yeah. I think, … in somebody’s care plan oh yeah … raise the discussion, definitely.’
(P00202, HPC Patient)
ʻObviously, it’s got to be done when the person is compos mentis it’s got to be while the patient is of reasonable sound and mind, you know.’
(P00502, HPC Patient)
ʻThe right time for me, may not be the right time for you or for Mary or Jane or Sarah. The right time for everybody is different, some people won’t be able to discuss it at all. It’s a really deep, provoking question, when is the right time. I don’t have an answer for that, I really don’t. At the moment, now is the right time, while I’m still of perfectly sound mind and before I’m too weak to be able to think about things and decide, so, but that’s how I feel. But I do, I think, I think places like the [day centre] should attempt to have discussions about donation with all patients and maybe it should be a question on their enrolment type form that they have the discussion with people very early on.’
(P00101, HC Patient)
Patients were asked who should make any decision regarding ED, themselves or their family members, whose decision should take priority and whether they felt that their family/carers would be supportive of their decision:
ʻIn my particular case, no. It’s my decision and … but I haven’t got children so, it … it is totally my decision.’
(P00602, HPC Patient)
ʻIf I hadn’t got the donor card then, they [family should decide]. With the donor card, I think, it’s got nothing really to do with them.’
(P00402, HPC Patient)
ʻSo, I’ve seen it enough times to know what the reaction is and having seen that reaction I can imagine what the reaction is of families when they’re asked will you donate your loved one’s corneas. And it shouldn’t be the loved ones [family members] who make that decision. It’s not their decision to make, it’s the patient’s decision and in order to get that patient’s decision is the discussions need to take place, much, much earlier than they do and it’s the same with any other organ.’
(P00101, HC Patient)
ʻWell, I guess if I’ve made it clear that I want organs to be donated then they shouldn’t be able to override that.’
(P00103, HC Patient)
ʻI think ultimately it should be my decision, but if I’m not able to make that decision then yes, they have the right to make that decision on my behalf. But if I have got, if I am able to make that decision then it’s my choice, nobody’s else’s and it’s not up to anybody else.’
(P00605, HC Patient)
ʻBecause if I’ve made the decision while I’m alive to donate my organs or my eyes, my wishes should be respected and carried out, it’s my wish.’
(P00705, HC Patient)
Very few patients thought that their family would not support their decision, but no patients had discussed ED with their family member at the time of data collection:
ʻNo, I don’t … I don’t think they will feel the same as me. I think, they … they have a bit of an aversion to it. Yeah. So, I … they definitely don’t think the same, I’m sure.’
(P00302, HPC Patient)
ʻI’ve never had the discussion with the family regarding donation, but I know we’ve just, not long had a new law come in that’s saying you’re all on the donor register list, but you have to then ring if you want to take yourself off. Although I haven’t rang, I’ve also had the conversation with family regarding it and it’s probably something I should do, I am terminal, to help other people that would be something that I would feel, I’m doing something, but obviously I would need to make family aware if the doctor does ask you that question then this is what I’ve said. But, yes, I’ve not yet had that conversation, but I probably should.’
(P00603, HC Patient)
ʻOur daughter has very set … distinct views on subjects. She doesn’t … won’t let you persuade her without, you know, a competent argument/discussion/debate so. And my wife, I think, she’ll go more with the sort of gut feel. So, I suspect that she’d probably say: ‘no’ being she still wants to be stuck in a hole in the ground and, I don’t see the point of that at all. We haven’t got that many holes left. I think I’m going to go home and start writing it down. Maybe that’s maudlin, I don’t know, don’t think so, I think it’s being practical, I really do think I’m being practical because I don’t want them, to make that decision and potentially arguing over the decision.’
(P00101, HC Patient)
Patients were asked what their preferences were related to information about ED donation, with responses varying in both qualitative content (e.g. whether about eligibility criteria, processes for retrieval) and level of detail:
ʻFor me, definitely a pamphlet (laughing) or … or even a little book because even though I might be dead, I’d like to know what’s going to happen and how it was done. And then to know what’s then going to … how the recipient receives it and how long it … the healing process is or, you know, the chance of it working and the chance of failure because I know it doesn’t always work and it can … with the lens it can cloud and all kinds of things.’
(P00202, HPC Patient)
ʻThey would want to know, one, that is it possible to use for all ages, they would want to know what exact part can be used or not used, they would want to know whether it would be, although it would be a bit too late by then for that person, they would want to know what sort of intrusion it would amount to, you know …. Say they are going to be buried or cremated or something, What part would be seen or not seen …. They would want to know how long such a part would last, like, you know, in other body parts they put it in these packs with ice or freeze it in nitrogen, you know, like cells, like sperm cells for example, would an eye organ be utilised like that, would it last that long. Would it have to be repetitively rejuvenated, would there be rejection in the new person receiving it. And that’s my question, you see, it doesn’t explain to me why do you need to take the whole of the eye out if you just need the cornea?’
(P00903, HC Patient)
ʻI don’t think I, to be quite honest, I don’t think I need any information apart from the fact that I would need to know if there was a form that I could fill in to donate my eyes or any parts, that I could actually fill in and send so that you can look after that paperwork in the event of my death, raise, raise it at that point.’
(P00301, HC Patient)
ʻAbout … like how useful it would be going to somebody else, the opportunity of giving somebody else sight maybe or things like that, teaching and even for doctors to practice on and learn.’
(P00705, HC Patient)
ʻYes, I … I would have to look into it a little bit … a little bit more because, as I say, I know very little … well, I virtually know nothing about the actual system itself. How would it work? Would it work … obviously, how long I’ve got … how long will it last before it becomes useless? Because it only lasts … lasts for a certain amount of time, doesn’t it?’
(P00502, HPC Patient)
Preferences – carers
Of note is that none of the carers who participated in the study had been involved in a discussion about ED; we therefore asked carers about their preferences regarding who they thought should raise the issue of ED:
ʻWell, I think, possibly the palliative care people are … are the very best to do that. They deal with death all the time, you know, and they spend a lot of time with their patient.’
(C00406, HPC)
ʻI think, it would be the person … probably the consultants. I think … yeah, I think, it would be the most senior person in charge of that person’s care.’
(C00402, HPC)
ʻIt should be a trained healthcare professional. I think, or it could, yes, somebody coming in from the outside specifically to, to do that would, perhaps if somebody was not convinced or had special questions you could bring in some, a specialist in that area to explain things. I think a healthcare professional, I mean most people working, particularly in palliative care, or, I mean most consultants are trained to give bad news, you know, but this is a positive thing that can come out of the bad news.’
(C00103, HC)
ʻGood question. Probably, probably the doctor or the consultant who’s dealing specifically with the patient, the person that has the final say on the patient’s medication and the patient’s treatment because they’ll have a, I would imagine, they’ll have full access to the patient’s notes and the case.’
(C00305, HC)
Carers were asked about their preference as to when the option of ED should be raised with a patient/family member. Carers in HPC and HC agreed that ED should be raised early in the EoLC pathway, with the caveat that this would depend on the patient’s clinical condition:
ʻMy general thought, I think it’s something along with all organ donation that should be discussed at the early stage really in peoples’ care at the hospice. Yes, we’ve had conversations with L*F* who is a consultant at the hospice and I guess coming from a point of view where we’re quite open to organ donation it, it would seem perfectly natural. But I gather, you know, I would understand if people would feel shocked by that at an early stage, but for us it would have been fine to have been asked.’
(C00103, HC)
ʻIt should be raised with the patient when they decide that … that … I mean, they’re … they’re thinking about palliative care. Right at that earliest possible moment to say: ‘this is a … ’. You’re doing it all … you’re doing it already. You’re saying: ‘listen, if you’re … if you go into cardiac arrest, do we re … do we revive you?’. And they’re saying: ‘no’ basically. So, why not say at the … ‘if … if we get into a situation where you … you do pass then why … why not … what about donation?’. I don’t see a problem with that.’
(C00202, HPC)
ʻI don’t know, I don’t really know, it just, I think it depends on the health of the patient, if they’re well enough to discuss it at that time, I think it’s just, you’ve just got to wait and see when it is right for the actual patient, which I know, I know that’s difficult but if they think, they could just mention it and if they sort of shy away then you don’t probably say anything, I think it just depends on the individual at the time.’
(C00303, HC)
In view of commentary from the literature indicating that availability of information about donation could negatively impact the aimed-for tranquil environment of palliative care setting, we asked carers what their preferences would be about information being available in the form of leaflets, posters, etc. Carers agreed that information on ED should be available to patients and carers/families, regardless of whether they supported the option being raised directly with patients. Some carers felt that the topic should first be raised in a conversation:
ʻI suppose [information about], just how … how are they used and how are they … I mean, are they used to donate to other people? Are they used for research? Are they used for both? That’s more probably my questions on that. And … how does it help a person.’
(C00106, HPC)
ʻI think there should. Yes. There should be some … there should be information. I mean … and if the information is done right at the start of the diagnosis programme … procedure, you know, then it would be … it would give people longer to get used to the idea.’
(C00502, HPC)
ʻI think it needs to be, it needs to be discussed, you know, probably needs to be mentioned, it needs to, let me think, it probably needs to be, an overall leaflet or pamphlet, a general sort of introduction to it just for the patient and family to get some background knowledge of it before the actual consultant starts to discuss it initially and then once they’ve discussed it with the patient and family if the patient needs the family to hear, you know, to discuss it, then the, you know, the consultant could then go into greater detail. But I think basically a leaflet of some sort to give an overall view, you know, like a general guidance and what it’s all about, a brief chat, explanation with the consultant would supplement the information in the pamphlet and the consultant would come back once the patient has had time to read and digest and think about the pamphlet information, then they could take it further. Obviously if at that time, having done all that the patient turns round and says, well no I’ve heard the facts and the information and it’s not something I want, then obviously that would be the end of it, but if the patient’s actually read the information and given it some thought and decided to continue with it, that would be the time that the consultant could then go into greater detail and answer their questions if necessary.’
(C00305, HC)
As the level of public awareness is reported to influence donation decision-making, we asked carers if they knew how many people are in need of a corneal transplant in the UK? No carers were aware prior to participation in EDiPPPP, with one participant stating that they only became aware when they read the Participant Information Sheet for the study:
ʻNot really no to be honest I, I don’t really know.’
(C00301, HC)
ʻDid I read there are five thousand a year is it and there’s only three and a half thousand donations?’
(C00101, HC)
Commentary – preferences
Participants indicated a clear preference that information about ED should be made available to patients and their families by HCPs early in the EoLC pathway. Participants acknowledged that ED is a sensitive issue but indicated an expectation that HCPs would have the communicative and empathetic skills to raise the topic in an appropriate and timely manner.
Patient and carer participants agreed that HCPs involved in the care of the patient should be able to have this discussion with patients and that HCPs should take the lead in facilitating this conversation. However, there was no agreement on which HCPs (either by role group or by level of seniority) this should be (through several carers indicated their preferences for ‘medical staff’ to do this). Both participant groups indicated that the issue of ED is best raised early in the patient’s dying trajectory (after the initial phase of transition to EoLC had taken place) or when other end-of-life planning topics are being discussed (e.g. resuscitation). All participants agreed that a judgement as to when to introduce the topic must be based on the patient’s physical, emotional and cognitive state – and that these issues should be assessed by HCPs before raising the issue. Patient responses indicated a greater general concern with how this topic would be raised, rather than when.
Most patients were of the view that their wishes should take priority and that family members’ views should not overrule patient wishes unless there was no statement of wishes given by the patient prior to death. As can be seen from the quoted data, there were a range of views about what sort of information should be available to patients, from very in-depth material to the basic summary information. This range of views could be a barrier to HCPs engaging in conversations with patients if they do not personally feel confident and competent to answer in-depth questions, or if sufficient information is not available.
Commentary on findings
The overriding message from interviews with patients is that they want to be offered the option of ED and that they want to make this decision and share that information with their family (if the family is not initially included in conversations). The majority were surprised, but encouraged, that they might be able to donate eye tissue and were positive about the potential contribution to helping others.
Retrieved publications report that HCPs believed that discussing ED would detract from the tranquil environment of a hospice and that donation requests could cause patients and their families physical and psychological harm. 69 However, service evaluation data indicate that doctors who had raised the issue of ED reported that conversations did not cause additional distress and were, in fact, perceived by patients and families as a positive outcome from the death. 36
Furthermore, the perception that discussing ED would cause distress is not supported in our findings nor in the wider literature. 65,66,68,73,75 EDiPPPP findings, in line with other research,65,73,75 indicate that key barriers to the topic of ED being discussed include the option not being discussed or brought to the attention of patients; patients and carers being unaware that ED is an option for them; being told that a cancer diagnosis rules them out of donation (a belief that appeared to be held by some HCPs); and patient perceptions that they may be too old to contribute despite potentially wanting to be a donor. Most participating patients in EDiPPPP were motivated to be eye donors, and they felt positive about the possibility of helping others in line with views reported across a limited (in size) body of knowledge. 65,73
The patients interviewed clearly indicated that it was important to have donation discussions when the person was well and had the mental capacity to make the decision and share their decision with family members.
As we see from the data with HCPs that those who do discuss ED only do so if the issue is raised by the patient or family member and the interviews with patients and carers show us that only a small proportion were aware of the possibility of ED, very few patients or family members are likely to raise the topic of ED. In line with the wider research, our findings indicate that donation was viewed positively by patients, that it is a social duty to donate and that it would be ‘wasteful’ not to. 74 Therefore, there is an ethical imperative to ensure that donation options are presented where possible, both in order to fulfil patients’ wishes for EoLC and to maximise the potential for donation. 74
Finally, we are unable to speak broadly to the potential for cultural beliefs or religious beliefs to act as barriers other than to clarify that religious beliefs were raised by two patient participants and these beliefs did act as a barrier to donation. In our scoping review, only one study was located that linked religious beliefs (e.g. that the body must remain untouched for 8 hours after death to allow the spirit to depart and remain intact as the spirit should be able to see in the afterlife)75 as a reason for patients to decline the option of ED.
The paucity of this information in our findings may be related to our patient and carer cohorts being predominantly self-defined as ‘White British’ (with HC showing a greater ethnic diversity than HPCs, see Appendix 6). Historically black, Asian and minority ethnic groups are reported to not access hospice care in the UK, although a recent literature review has indicated that this picture is changing. 84
Recommendations for practice (Section 2)
-
In view of the potential for ED in hospice care settings, it is essential that the option of ED is routinely raised with patients and family members. It is imperative that they are enabled to fulfil what may be a lifelong wish to donate organs and tissues.
-
As patients and carers are unaware of the option of ED, this topic is a priority for service development for local and national organisations supporting patients in EoLC planning.
-
Clinical guidance indicates that HCPs should proactively inform patients and their families about the option of ED. This information needs to be provided as part of normal EoLC conversations.
-
Public awareness-raising initiatives are needed that inform patients in HC and HPC services about the option of ED. This can be achieved by ensuring that evidence-based, co-constructed, centrally generated (NHSBT-TES) and validated web content is shared with UK-based HC and HPC organisations and their professional bodies, for example the Association of Palliative Medicine, and Hospice UK.
Chapter 8 Intervention development transparent expert consultation (WP3S1)
Chapter 8 addresses study Objective 5, to develop an empirically based theoretically informed intervention designed to change behaviours in relation to the identification, approach/request and referral of patients from HPC and HC for ED. This chapter outlines the process of the TEC, the aim of which was to agree the necessary elements of an evidence-based intervention that was endorsed by stakeholders. The outcome of this process was the identification of key priorities and components to underpin development of a complex intervention to realise the potential for supply of eye tissue from palliative care settings. This chapter describes the design, conduct and outcomes of this process, before the resulting complex intervention design (STEPS) is described in Chapter 9.
Methods
The TEC is a systematic process for expert appraisal of evidence by a range of stakeholders underpinned by a rigorous audit trail aiming to generate robust, auditable intervention points (IP) or a set of priorities for complex intervention development. 37
Participant identification and recruitment
The aim of recruitment for the TEC was to ensure panel composition reflected the diversity of stakeholders represented in the ED process. These included:
-
clinicians from Hospital and HC settings
-
representatives of national and regional healthcare bodies with responsibility for/involvement in ED
-
representatives of national and regional organisations supporting and/or representing:
-
patients and carers receiving EoLC
-
families of donors
-
patients waiting for or in receipt of a corneal transplant.
-
-
steering group members
-
PPI representative
-
research team members.
Participants were identified for approach through a range of routes, including:
-
study co-applicants
-
invited representatives from:
-
HC and HPC professional networks
-
patient and donor family support organisations
-
regional and national bodies involved in ED.
-
-
contacts encountered through research activities in WP1 and 2, or who had made unsolicited contact with the study team to express interest in the EDiPPPP study (via CRN, viewing study website, etc.).
Transparent expert consultation participants
Thirty-two participants were formally invited to participate in the TEC. Invitations were sent by e-mail with a personal paragraph indicating the specific relevance of the potential participant’s expertise to the TEC and including the PIS.
Twenty-three participants initially agreed to take part in the EDiPPPP TEC, of which 21 finally took part. Establishing a TEC panel during COVID-19 restrictions was challenging, with some potential participants subsequently becoming unavailable due to clinical pressure/demands at short notice.
To facilitate engagement and efficient use of time, participants were grouped into two panels aligned to their expertise or role: Group 1: Education, Training and Awareness (ETA), Group 2: Process and Technical (PT). Participants and the rationale for grouping of participants are presented in Table 19.
| Panel group | Panel member | Job role/title | Job/role category relevant activity | How identified |
|---|---|---|---|---|
| ETA (n = 13 participants) | 1a | Interim Head of Operations (NHSBT-TES) | Regional or national body involved in ED | During research activity |
| 2 | Legislation Project Lead-Education and Governance (NHSBT-OTDT) | Regional or national body involved in ED – NHSBT – ODT | Co-applicant | |
| 3 | Hospice Development Nurse Practitioner (NHSBT-TES) | Regional or national body involved in ED – NHSBT-TES | During research activity | |
| 4 | Education Lead (Hospice) | HCP working in HC or HPC setting | Co-applicant | |
| 5 | Consultant in Palliative Medicine (NHS Foundation Trust) | HCP working in HC or HPC setting | Unsolicited contact [following alert from clinical research network (CRN)] | |
| 6 | Education and Professional Development Manager (NHSBT-OTDT) | Regional or national body involved in ED – NHSBT – ODT | During research activity | |
| 7 | Hospital Development Nurse Practitioner (NHSBT-TES) | Regional or national body involved in ED – NHSBT-TES | During research activity | |
| 8 | Consultant in Palliative Medicine (NHS Foundation Trust) | HCP working in HC or HPC setting | During research activity | |
| 9 | Senior Bereavement Support and Medical Examiner Officer (NHS Foundation Trust) | HCP working in HC or HPC setting | Unsolicited contact (following alert from CRN) | |
| ETA subgroup public awareness | 1 | PPI member | PPI representative and Member of DAG – NHSBT-TES | Co-applicant |
| 2 | Chair Organ and Tissue Donation Committee (NHS Foundation Trust) | Regional or national body involved in ED | Unsolicited contact (following alert from CRN) | |
| 3 | EDiPPPP Project Steering Group Chair | Research/Service Development | Chief investigator network | |
| 4 | PPI member and locum GP | PPI representative and member of DAG – NHSBT-TES | Co-applicant | |
| PT (n = 8) | 1 | Consultant in Palliative Medicine (NHS Foundation Trust) | HCP working in HC or HPC setting | Co-applicant |
| 2a | Interim Head of Operations (NHS Blood and Transplant) | Regional or national body involved in ED | During research activity | |
| 3 | F2 Senior Adult Medicine (NHS Foundation Trust) | HCP working in HC or HPC setting | During research activity | |
| 4 | Consultant in Palliative Medicine and Research Lead (Hospice) | HCP working in HC or HPC setting | Co-applicant | |
| 5 | Consultant in Palliative Medicine (Hospice) | HCP working in HC or HPC setting | Co-applicant | |
| 6 | Director of Clinical Services/Matron (Hospice) | HCP working in HC or HPC setting | Co-applicant | |
| 7 | Consultant in Palliative Medicine (NHS Trust) | HCP working in HC or HPC setting | During research activity | |
| 8 | Consultant in Palliative Medicine (Hospice and NHS Trust) | HCP working in HC or HPC setting | Co-applicant |
Preparation for transparent expert panels
Interim findings from across the study were collated into two panel focused reports and one overview document. Each report followed the same outline: role of the report (including the questions to be answered by that group) followed by the summary of findings outlined under the study domains (potential, practice, perceptions).
-
Report 1. ETA. The goal of this group was to confirm key areas for organisational, logistical and individual practice change with respect to education and training of HCPs in relation to ED, and public awareness campaigns to inform patients, families and the wider public.
-
Report 2. PT. The goal of this group was to confirm key areas for organisational, logistical and individual practice change with respect to local and national processes, systems and resources to support implementation of ED.
Prior to the TEC, clinical PIs had also received site-specific feedback on the outcome of ED eligibility assessment for their sample of patients in the notes review. This information informed discussion of current knowledge and processes for evaluation of ED eligibility and the challenges faced by clinical PIs in undertaking eligibility screening against the current ED criteria.
Convening the transparent expert panel meeting
Participant availability was assessed via Doodle online availability polls and once dates were confirmed participants received meeting documents via e-mail 2 weeks ahead of the meeting (to facilitate review of documents ahead of the meeting):
-
agenda and joining instructions via Microsoft Teams including guidance of panel membership and use of break out rooms
-
a consent form for completion and return prior to the consultation meeting
-
TEC documents:
-
interim findings summary report (see Appendix 8)
-
interim findings PowerPoint
-
ETA-report (see Appendix 9)
-
PT report (see Appendix 10)
-
a copy of the study protocol.
-
Conduct of transparent expert panels
Both TEC panels took place via Microsoft Teams and were video-recorded with the consent of participants for the purpose of review of commentary by the study team. The TEC was chaired by TLS, with BMS monitoring the group chat, and MJB providing technical support and accessing further study information as requested by participants.
Both groups began with introductions of group members, and a restatement of the guidance for participation and functions of Microsoft Teams. Participants were then asked to review the questions for discussion and indicate any suggested additions or amendments (none were provided in either group). TEC panels then proceeded to discussion of agreed questions, which were:
-
For the ETA panel:
-
What key activities are necessary to inform: education, training and public awareness raising initiatives?
-
For all activities in all EDiPPPP study domains:
-
What specific content is needed? (e.g. education/training focus points; key public awareness messages).
-
What form should this content take? (e.g. online information, e-learning or in-person training, format of public awareness campaigns).
-
-
-
For the PT panel:
-
What processes need to be generated or amended in response to the findings of this report?
-
What technical resources (e.g. IT, clinical knowledge base) are needed to support these processes?
-
Due to its size and composition, the ETA panel was split into two (see Table 19), which ran concurrently to consider the questions in relation to two specific areas: Public Awareness and Education and Training. Following the parallel discussions, the groups reconvened as a single panel to discuss their thoughts with the wider group. For the PT group, questions were discussed as a single panel group.
Collation and synthesis of findings
Meetings were audio- and video-recorded using Microsoft Teams software, and recordings were subject to inductive content analysis42 using Microsoft Excel. The first step in this process was to produce written notes based on participant comments to study findings. The second step involved categorising notes to create a taxonomy of general areas of agreement on what was needed to enable behaviour change (e.g. Staff Training and Awareness), which were highlighted as IP for service development.
Table 20 provides an example illustration of this process for one of the IP identified from discussion notes from the ETA panel in response to study findings regarding the lack of information about ED for patients and carers at study sites. This table shows the study findings in the left-hand column, meeting notes [with initials indicating the speaker(s) and a timestamp indicating the start point at which this observation was identified] in the middle column and finally the right-most column describes the intervention point that was derived from the notes and areas of concern that map to it.
| Study findings – areas for change | Meeting notes | IP |
|---|---|---|
| Lack of information resources (patients and carers) | GM @ 29 minutes 50 seconds – leaflets often are not picked up because patients assume it does not apply to them unless raised by HCP. Virtual teaching/bitesize training is better and more flexible than formal in-person training – link nurses valuable but can move around and change the subject | ETA-IP1 – Information for patients needs to be embedded within routine processes as: |
| GM @ 1 hour 3 minutes 50 seconds – relatives’ access to information – if patients go home to die, they have information on the process for when contact is made around or after death |
|
|
| TLS @ 1 hour 5 minutes 45 seconds – [re: Public Awareness] online resources are important but it’s about the process by which those resources are made available/relevant to staff, patients and families in context | ||
| GF @ 1 hour 12 minutes 50 seconds – building information resources into the process [natural encounters – MJB terms] | ||
| GF @ 1 hour 22 minutes 00 seconds – have provided forms before, but ‘fell flat’ because held by patients, HCPs not aware, did not enter into the formal decision-making system | ||
| Lack of staff training and awareness | GM @ 13 minutes 0 seconds – confusion around ODR and opt-out – patients = signed ODR so everything should be in place, HCPs know what to do; HCPs = confusion around how deemed consent legislation should be operationalised | |
| TR @ 15 minutes 50 seconds – does reticence (HCPs and patients) relate to knowledge of retrieval processes and outcomes (i.e. how the body will look afterwards)? |
Findings
In this section, we outline findings identified as areas for change, and related intervention points identified from each of the TEC panels (ETA and PT).
Education, Training and Awareness transparent expert panel
Following discussion of findings, panel members identified four key areas for behaviour and practice change regarding education, training and awareness of ED: Information resources (staff); Institutional policies and procedures (local); Public Awareness; and Staff Training and Awareness. Eight intervention points were identified relating to these areas of concern, which are described in Table 21.
| Study findings – areas for change | IP |
|---|---|
| Lack of information resources (patients and carers) Low levels of staff training and awareness |
ETA-IP1 – Information for patients needs to be embedded within routine processes – that is, currently they may emerge as part of natural encounters within pathways or require addition work for the patient or carer, for example patients have to go looking for information |
| Lack of information resources (patients and carers) Lack of accessible information resources (staff) Low levels of staff training and awareness |
ETA-IP2 – HCPs need access to donation information (for themselves and for patients) that is easy to access, ‘on-demand’ format |
| Lack of accessible information resources (staff) | ETA-IP3 – Information for staff regarding ER, and resources to support conversations with patients and families, needs to be embedded within routine processes |
| Low public awareness | ETA-IP4 – Public awareness strategy for legislation change and its implications for EoLC decision-making needs to be evaluated and (most likely, based on current evidence) relaunched/revised |
| Lack of institutional policies and procedures (local) Low levels of staff training and awareness |
ETA-IP5 – Service development ‘toolkit’ to be developed for use by practice development nurses in targeted engagement with sites with high potential drawing on EDiPPPP findings and existing resources developed by sites |
| Lack of institutional policies and procedures (local) | ETA-IP6 – National strategy for targeted service development to be developed for NHSBT (in tandem with the ‘toolkit’ – ETASPCh5) |
| Lack of institutional policies and procedures (local and national) Low levels of staff training and awareness |
ETA-IP7 – Training and service development resources need to reflect the necessity of embedding ED conversations within HCP-initiated processes |
| Low public awareness Low levels of staff training and awareness |
ETA-IP8 – Broader public awareness campaign for ED (evaluation and further development) |
Process and technical transparent expert panel
Following discussion of findings, panel members identified two broad areas for behaviour and practice change: ER and communication with patients and family/carers. Seven intervention points were agreed regarding ER (Table 22) and seven for Communication with Patients and Families/Carers (CPF; Table 23).
| Study findings – areas for change | IPs |
|---|---|
| Lack of access to eligibility information | PT-ER-IP1: HCPs need to access to opt-out information PT-ER-IP2: Checking opt-out needs to become a normalised, embedded practice within care pathways |
| Lack of access to eligibility information Lack of access to information on retrieval and use Low levels of support and guidance from NHSBT |
PT-ER-IP3: HCPs need access to information from the clinical record relevant to assessing eligibility PT-ER-IP4: HCPs need guidance and support for assessment of eligibility (site level) PT-ER-IP5: HCPs need guidance and support for assessment of eligibility (national level) |
| Lack of access to information regarding outcomes Low levels of support and guidance from NHSBT |
PT-ER-IP6: HCPs need assurance re likelihood of completion to have confidence to approach PT-ER-IP7: HCPs need information/feedback on retrieval and impact for both recipients and families |
| Study findings – areas for change | IPs |
|---|---|
| Lack of behavioural prompts to initiate conversation Lack of consensus of ‘When’ conversations should be undertaken (within care pathways) Lack of consensus re ‘Who’ makes the approach Lack of institutional legitimacy, importance, prioritisation, confidence |
PT-CPF-IP1: implementing ED conversations within ACP across pathways PT-CPF-IP2: embed conversation within ReSPECT forms PT-CPF-IP3: emphasise to HCPs evidence indicating the importance of ED being raised with patients PT-CPF-IP4: embedding ED conversations within EoLC conversations as part of routine practice |
| Lack of institutional legitimacy, importance, prioritisation, confidence | PT-CPF-IP5: ensuring that information about ED becomes central to the core activity of ACP (that the issue of ED is encountered naturally in planning encounters across pathways |
| Lack of institutional legitimacy, importance, prioritisation, confidence | PT-CPF-IP6: creating professional legitimacy for implementation and embedding of ED within EoLC practice |
| Lack of institutional legitimacy, importance, prioritisation, confidence | PT-CPF-IP7: building resilience to organisational turbulence (e.g. staff turnover) |
Intervention development
The starting point for intervention design was mapping the intervention points from the TEC (see Tables 21–23) to the agreed key components the intervention must address:
-
processes to ensure identification, assessment (against eligibility criteria) and referral of potential donors
-
assessing and facilitating organisational readiness to operationalise ED;
-
initiatives to underpin individual and organisational capability, motivation and opportunity to embed ED in routine practice
-
development, monitoring and assessment of context-specific public awareness initiatives.
Table 24 provides an example mapping of IPs to intervention design (this process took place for all intervention points from each panel).
| IP | Incorporated into intervention design (steps) |
|---|---|
| ETA-IP1 – Information for patients needs to be embedded within routine processes that is, currently they may emerge as part of natural encounters within pathways or require additional work for the patient or carer, for example patients have to go looking for information | Assessing and facilitating organisational readiness to operationalise ED |
| ETA-IP2 – HCPs need access to donation information (for themselves and for patients) that is easy to access, ‘on demand’ format | Initiatives to underpin individual and organisational capability, motivation and opportunity to embed ED in routine practice |
| ETA-IP3 – Information for staff regarding ER, and resources to support conversations with patients and families, needs to be embedded within routine processes | Processes to ensure identification, assessment (against eligibility criteria) and referral of potential donors |
| ETA-IP4 – Public awareness strategy for legislation change and its implications for EoLC decision-making needs to be evaluated and (most likely, based on current evidence) relaunched/revised) | Development, monitoring, assessment of context-specific public awareness initiatives |
| ETA-IP5 – Service development ‘toolkit’ to be developed for use by practice development nurses in targeted engagement with sites with high potential (drawing on EDiPPPP findings and existing resources developed by sites) | Assessing and facilitating organisational readiness to operationalise ED Initiatives to underpin individual and organisational capability, motivation and opportunity to embed ED in routine practice |
| ETA-IP6 – National strategy for targeted service development to be developed for NHSBT (in tandem with the ‘toolkit’ – ETASPCh5) | Assessing and facilitating organisational readiness to operationalise ED Initiatives to underpin individual and organisational capability, motivation and opportunity to embed ED in routine practice |
| ETA-IP7 – Training and service development resources need to reflect the necessity of embedding ED conversations within HCP-initiated processes | Assessing and facilitating organisational readiness to operationalise ED Processes to ensure identification, assessment (against eligibility criteria) and referral of potential donors Initiatives to underpin individual and organisational capability, motivation and opportunity to embed ED in routine practice |
| ETA-IP8 – Broader public awareness campaign for ED (evaluation and further development) | Development of context-specific public awareness initiatives |
Following this synthesis and integration of findings, and TEC outcomes to intervention points, the research team generated the STEPS intervention that was presented to the project steering group, clinical PIs and members of NHSBT-TES at the final steering group meeting for the project.
Commentary on findings
Panel members were generally surprised on hearing the study findings regarding the high potential for ED at each site (as per summary document and PowerPoint presentation). These figures generated discussion around the importance of behaviour and practice change, and the need for change to move at pace to increase the supply of eye tissue. One panel member, whose comment was met with agreement by fellow members, said simply:
ʻWe (HCPs) just need to get on and raise this option.’
(GF)
Panel members agreed that key facilitators to practice change and development included: the evidenced motivation of HCPs to facilitate offering the option of ED; evidenced patient willingness to have discussions about ED; and expectation that HCPs will raise this issue with patients during their end-of-life trajectory. Panel members agreed that study findings to date were compatible with their own clinical or personal experience, and agreed that any intervention needed to address the following key issues:
-
processes to ensure identification, assessment (against eligibility criteria) and referral of potential donors
-
assessment and facilitation of organisational readiness to operationalise ED
-
initiatives to underpin individual and organisational capability, motivation and opportunity to embed ED in routine practice
-
development, monitoring and assessment of context-specific public awareness initiatives.
In view of the level of agreement reached across the TEC, and in view of significant clinical pressures for most of the TEC membership with ongoing COVID-19-related demands, we did not carry out a Delphi process to gain further commentary as this was felt unnecessary by the TEC panel members and the study team.
Chapter 9 Support Toolkit for Eye donation in Palliative care Settings
Chapter 9 presents the intervention developed following the TEC and completion of all data analyses. Chapter 9 outlines the process of the intervention development, the theoretical perspective applied in development of the intervention, and presents the intervention illustrated as a logic model STEPS. Chapter 9 also details the necessary actions (what, who, how) that are essential components of the intervention.
Intervention design has been a collaborative undertaking informed by the 6SQuID framework,16 application of the research findings and theoretical perspectives (as laid out in this report), discussion and feedback from members of the TEC panel, the PSC, and ongoing bi-weekly planning meetings with key stakeholders, informally throughout the project with co-applicant EW – Lead Nurse Tissue Donation, and formally (since January 2020) with the NHSBT-TES implementation team: Head of Service Development – NHSBT-OTDT, Lead Nurse Tissue Donation – NHSBT-TES, Lead Nurse Education and training, NHSBT-OTDT, Senior Marketing and Campaigns Officer – NHSBT). Meetings have engaged with all research findings presented in short reports, presentations or infographics by the research team and the piloted and validated EEDAC (see Appendix 5) and OREDAC (see Appendix 7). Outcomes from planning meetings to date include the convening of the strategic ED Hospice implementation working party and the Hospice ED education and training working party whose membership includes authors TLS and SM of this report.
Intervention design – Support Toolkit for Eye donation in Palliative care Settings
Theoretical underpinnings applied to intervention design
Despite guidance from the UK Medical Research Council recommending the use of theory in the development, planning and evaluation of complex interventions,33 many intervention designers do not use existing frameworks as a basis for intervention development. 85,86 A key finding from the EDiPPPP study is that behaviour change needs to occur at both an individual and organisational level and therefore early on in the research process we reassessed the applicability of theory that we had proposed to apply during analysis, and following a review of the literature related to models of behaviour change, the COM-B behaviour change model24 was chosen to inform analysis and our thinking as we developed component parts of the intervention (Figure 10). This model assisted in articulating the contextually specific, necessary, practical, psychological and organisational actions and processes that are required to support behaviour change with the aim of enabling the current potential for ED in hospice care settings to be realised and end the supply deficit.
Authors33,88 recommend that any model should be able to map those mechanisms that underpin change, for example physical, psychological, environmental. These concepts align with the domains of EDiPPPP: Potential, Practice, Preferences, Perceptions, which, in combination, reflect the donation climate of an institution. The COM-B model is proposed to articulate what needs to change in order for a behaviour change intervention to be effective with authors proposing that the COM-B model ‘identifies three factors that need to be present for any behaviour to occur: Capability (C), Opportunity (O) and Motivation (M). 24 These factors interact over time so that behaviour can be seen as part of a dynamic system with positive and negative feedback loops’. 87 Each of the factors in Figure 11 can influence each other. For example, a lack of capability can reduce motivation to undertake a behaviour and therefore opportunities to enact the behaviour will be avoided. Likewise, a perceived lack of opportunity to enact a behaviour may reduce motivation and over time impact perceptions of capability (you lose it if you don’t use it).
FIGURE 11.
COM-B aligned to intervention STEPS.
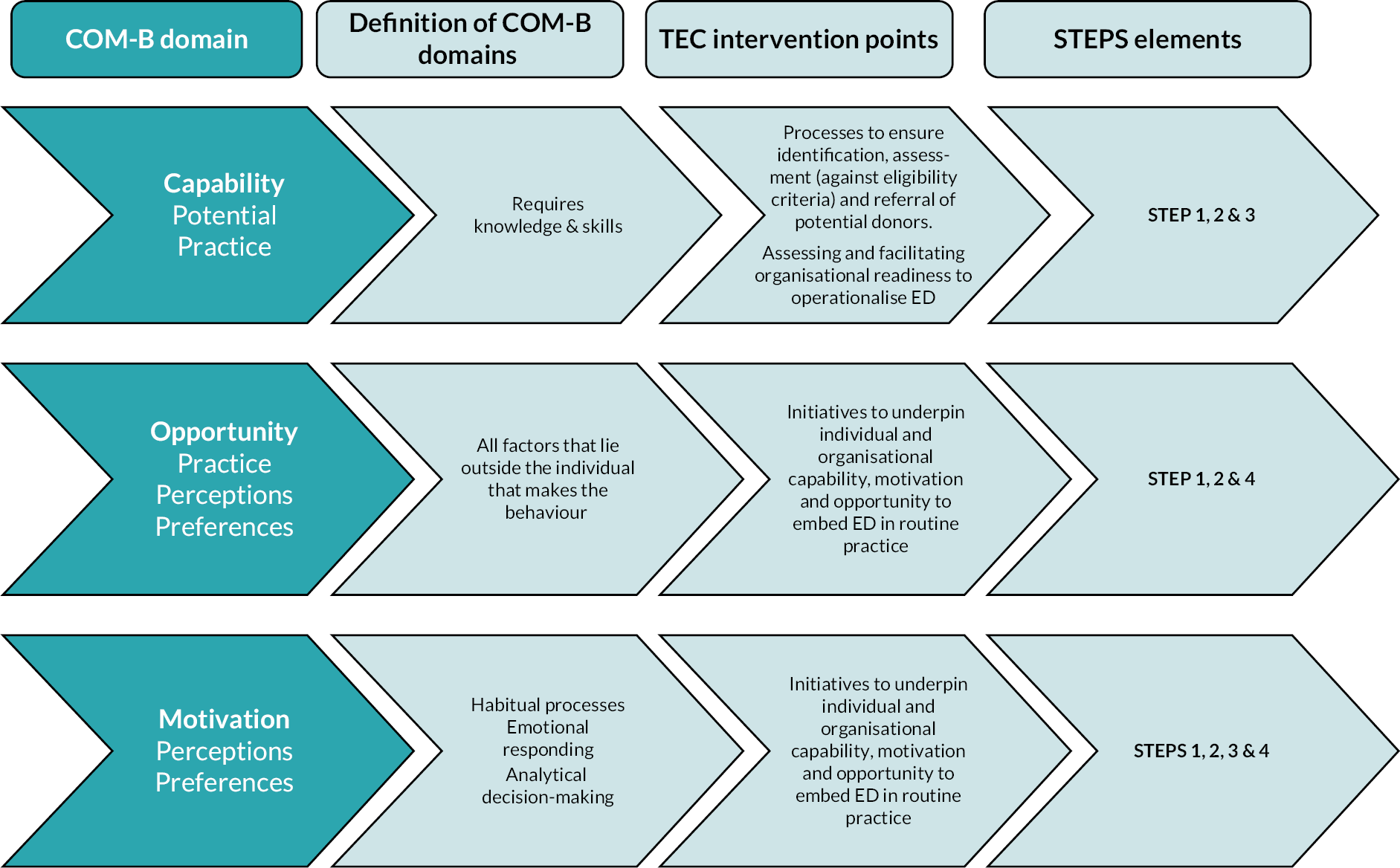
Aligning COM-B with EDiPPPP domains and intervention STEPS
Figure 11 illustrates how COM-B components align with the study domains (Potential, Practice, Preferences and Perceptions), how the COM-B components are defined and how the TEC intervention points align with the STEPS.
Capability: Currently, most HCPs do not feel that they are capable of facilitating ED as they lack knowledge and skills to ‘identify’ potential donors, ‘assess’ potential donors, ‘approach’ potential donors’ and complete associated tasks facilitating ED. Perceptions of capability will influence HCPs motivation to enact behaviours and undermine recognition of ‘triggers’ that stimulate opportunities to engage in the behaviour of raising the option of ED. The knowledge and skills deficit at potential ED sites must be assessed and addressed to bring about change (Intervention STEP 1).
Opportunity: HCPs lack opportunities to embed ED as organisations do not have routinised processes to identify potential donors or discuss potential donors at a team level and therefore no one ‘is allocated’ to engage in a discussion with the patient. Systems do not facilitate knowledge of the patient’s ODR status, and the NHSBT-TES website does not provide clinically up-to-date information that is accessible to clinicians. Opportunity supports motivation to engage in a behaviour and acts as a de-motivator if opportunities are not visible (routine) and not accessible (requiring extensive extra work). Opportunity to raise the option of ED needs to become habitual, emotionally rewarding and easy to enact. The formal and informal ‘opportunities’ to raise ED must be identified and agreed in order for change to occur and be maintained (Intervention STEPS 2 and 3).
Motivation: Many HCPs are motivated to include ED in end-of-life planning conversations and patients are motivated to have these conversations, but HCPs are de-motivated by their reported lack of capability (knowledge and skills) and opportunity (lack of accessible systems). Motivation will be reduced in situations where individuals perceive they lack competence as this often leads to lack of confidence, especially in situations that are new, or in which the individual has little experience (the confidence/competence feedback loop) for as Bandura states, ‘Unless people believe they can produce desired results (in this case raising the issue of ED) and forestall detrimental ones by their actions (e.g. negative reactions by patients or family member, increased workload), they have little incentive to act or to persevere in the face of difficulties’. 88:p179 The barriers that de-motivate and facilitators that motivate ED-related behaviours in potential ED sites must be analysed and understood in order to bring about change (Intervention STEPS 2 and 3).
Service users report that they have the capability to make decisions and are motivated to engage in conversations in view of positive perceptions of the benefits of ED, but currently they are not provided with the opportunity to discuss this option. Opportunities to inform (awareness raising) service users of the option of ED are lacking (at local service and national levels), which undermine capability and motivation. The opportunities to raise awareness and inform patients and carers of the option of ED within HC and HPC must be assessed and addressed in order to bring about change (Intervention STEPS: 1, 2, 3, 4) Furthermore, evidence-based public awareness-raising initiatives at the national level need to be developed, implemented and evaluated. 33
Operationalisation of Support Toolkit for Eye donation in Palliative care Settings
STEPS (Figure 12) is what we are referring to as a complex intervention33 as there are a number of components required for successful implementation, including increased perceptions of capability (expertise and skills of differing levels), routinised opportunities to underpin enduring motivation to raise the topic of ED in HC settings and engagement of a range of stakeholders. If these components are not synthesised, this will undermine the potential of the intervention to meets its aim. The aim of the intervention is to increase the supply of eye tissue gained via ED from patients within hospice care settings. Implementation of the proposed STEPS intervention requires a respectful relationship between hospices and NHSBT-TES to ensure a sustained and reliable increase in the supply of eye tissue from hospice care settings.
FIGURE 12.
Logic model of STEPS. n.b. dotted lines indicate linked explanations of roles [Regional Specialist Nurses Tissue Donation (RSPTD)], or where roles are aligned with but not responsible for the outcome (e.g. RSNED (Regional Specialist Nurses Tissue Donation) will help design website content in STEP 4), or where ongoing monitoring is needed (e.g. sites not meeting selection criteria by NHSBT-TES).
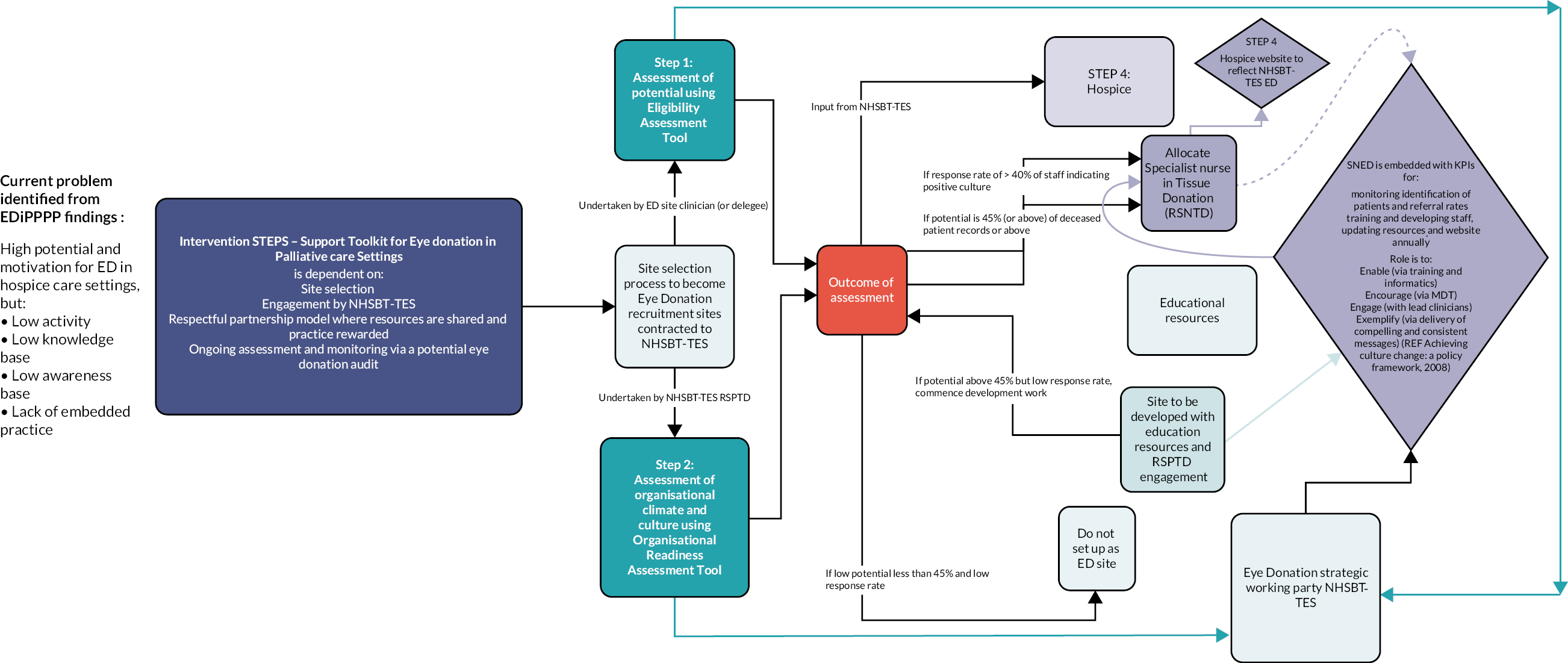
The following sections detail the intervention indicating what actions need to be taken, how actions need to be taken and who needs to take action to achieve the intended outcome of an increase in the supply of eye tissue for use in sight-saving and sight-restoring surgery and medical research from selected hospice care settings. These sections aim to illustrate the mechanism of change that is needed within the context that the intervention is bounded by. The logic model of how outcomes are generated is illustrated in Figure 12 and explained in the following sections.
STEP 1: Establish processes to ensure identification, assessment against eligibility criteria and referral of potential donors.
The first requirement to increase the supply of ED from hospice sites is the systematic assessment of the donation climate (potential and organisational readiness) of each hospice that NHSBT-TES aims to partner with. Partnerships should be formalised with service-level agreements outlining responsibility and financial assistance and aligned with the site becoming an affiliated ED site. Assessment is needed due to the fact that, as evidenced in this report, if the site has high potential but low readiness, referral and donation rates will not increase. If there is high readiness and low potential, referral and donation rates will also not increase.
Selection of sites should be based on the following assessment process
The following model of assessment is recommended to NHSBT-TES as a process for selecting potential ED affiliated sites.
-
An assessment of potential donors using the EEDAC (see Appendix 6) developed during EDiPPPP from note review methodology (WP1) and amended for ease of use by reducing the eligibility criteria to a core group of patient characteristics that are absolute exclusions for ED. Assessment of 100 deceased patients’ notes should be undertaken (as a UK-based study using this figure generated a similar figure to that of EDiPPPP over 10 years ago). 67
-
The EEDAC form has been developed on the Microsoft forms platform to facilitate ease of use (as accessible via PC or phone). The EEDAC in Microsoft forms was piloted at a clinical site (site 01) and reviewed by members of the Clinical Support Team at the National Referral Centre (NRC) for NHSBT-TES. Feedback from both the clinical site and NHSBT-TES was positive and the EEDAC is now under review by the digital team at NHSBT-TES for assessment and integration into their technical systems.
-
An assessment of organisational readiness (the donation climate within the clinical sites) indicating barriers to successful implementation of an ED process within that site. An evidence-based assessment can be undertaken via application of the OREDAC (developed within the study as a survey tool) in a shortened format (see Appendix 7). The OREDAC was piloted at one clinical site (site 01) via Microsoft forms platform for use on PC or mobile phone. Using this assessment tool will ensure that NHSBT-TES will have immediate access to the views, attitudes towards, barriers and training needs of HCPs within that clinical site.
-
The OREDAC needs to be implemented by the RSPTD who will be site specific and responsible for implementation of key STEP components for that clinical site.
-
Outcomes of both assessments then need to be reviewed by the ED strategic working party members to guide decisions about which sites become an ED partner site.
-
The outcomes of both the EEDAC and OREDAC would inform which clinical sites have the potential and capability of generating high-quality eye donors.
-
Sites that show high potential, but low readiness can be supported by the provision of leadership (STEP 2) and education and training (STEP 3) in developing the ED climate in their setting.
STEP 2: Initiatives to underpin organisational capability, motivation and opportunity to embed ED in routine practice
Sustained leadership and liaison are key to embedding ED in hospice care settings. This was well demonstrated in Site (02) where the RSPTD and clinical lead have developed a robust working relationship and flexible systems including baseline assessment of patients entering the clinical site for ED against five criteria (see Table 7), with those patients meeting the criteria ‘tagged’ for discussion in the clinical MDT. This model of ongoing assessment of all patients entering the clinical site is recommended to ensure that assessment becomes and embedded ‘routine’ behaviour. We recommend that NHSBT-TES makes a financial contribution (as part of contractual arrangements of a service-level agreement) to the agreed affiliated hospice site to support ongoing assessment of patients against eligibility criteria. This is important as most hospices receive little monies from the NHS. Analysis of Hospice Account reports (covering all charitable hospices in England) indicates that ‘statutory funding covered around 37% (median) of charity expenditure’ for financial years 2011/12 through 2017/18. 89 Liaison is essential and should be provided by the site-specific RSPTD who would have responsibility for ‘Engaging ‘with lead clinicians (nursing, medical, education), encouraging the inclusion of ED in all clinical development agendas and attending MDT meetings; ‘Enabling’ the site leadership team to ‘Embed’ ED into routine EoLC planning, via ‘Encouraging’ staff to engage with centrally generated informatics regarding current stock levels, use of eye tissue, etc., engagement with centrally developed and validated training resources; and to ‘Exemplify’ ‘via delivery of compelling narratives and consistent evidence-based messages’90 including the perceptions of patients that ED is a ‘safe topic to raise’ to underpin ongoing motivation to include ED in EoLC planning.
Compelling narratives are available from the recently developed blogs and videos from the NHSBT marketing team,91,92 but this alone will not change behaviours as busy HCPs may only ‘peripherally process’93 the message embedded in the resource. However, if these resources are included in in-person education sessions and simulations, the target audience is more likely to ‘closely scrutinise’ the messages.
Likewise, with service users who are not aware of the option, need for and benefits to others of ED, these resources need to be part of a guided session on ED, where potential donors can ask questions stimulated by the videos. Resources for service users should include ‘leaflets’ (as reported) providing basic information regarding ED that service users could share with family members, and aligned with in-person sessions for maximum impact as multimodal information is reported as being more effective in stimulating behaviour change. 83
Ongoing monitoring and evaluation of ED sites is essential in maintaining donation potential. As noted in the findings, most HCPs had not received any training or guidance in the previous 24 months and while some were aware of the new deemed consent legislation, HCPs were not clear on how this should inform their practice. This is a key role for the RSPTD who should be undertaking an annual potential donor audit (of potential, referrals, outcomes, education undertaken, etc.) that is shared with the strategic ED Hospice implementation working party.
STEP 3: Education and training initiatives to underpin individual capability, motivation and opportunity to embed ED in routine practice
An evidence-based, context informed, educational strategy has been generated (Figure 13), which has been shared with the strategic team at NHSBT-TES and is aimed at individual HCP development. The evidence-based strategy indicates the content needed at each of the steps within it. As is shown in Figure 13, the expectation is that:
FIGURE 13.
Logic model of stepped education strategy for implementation.
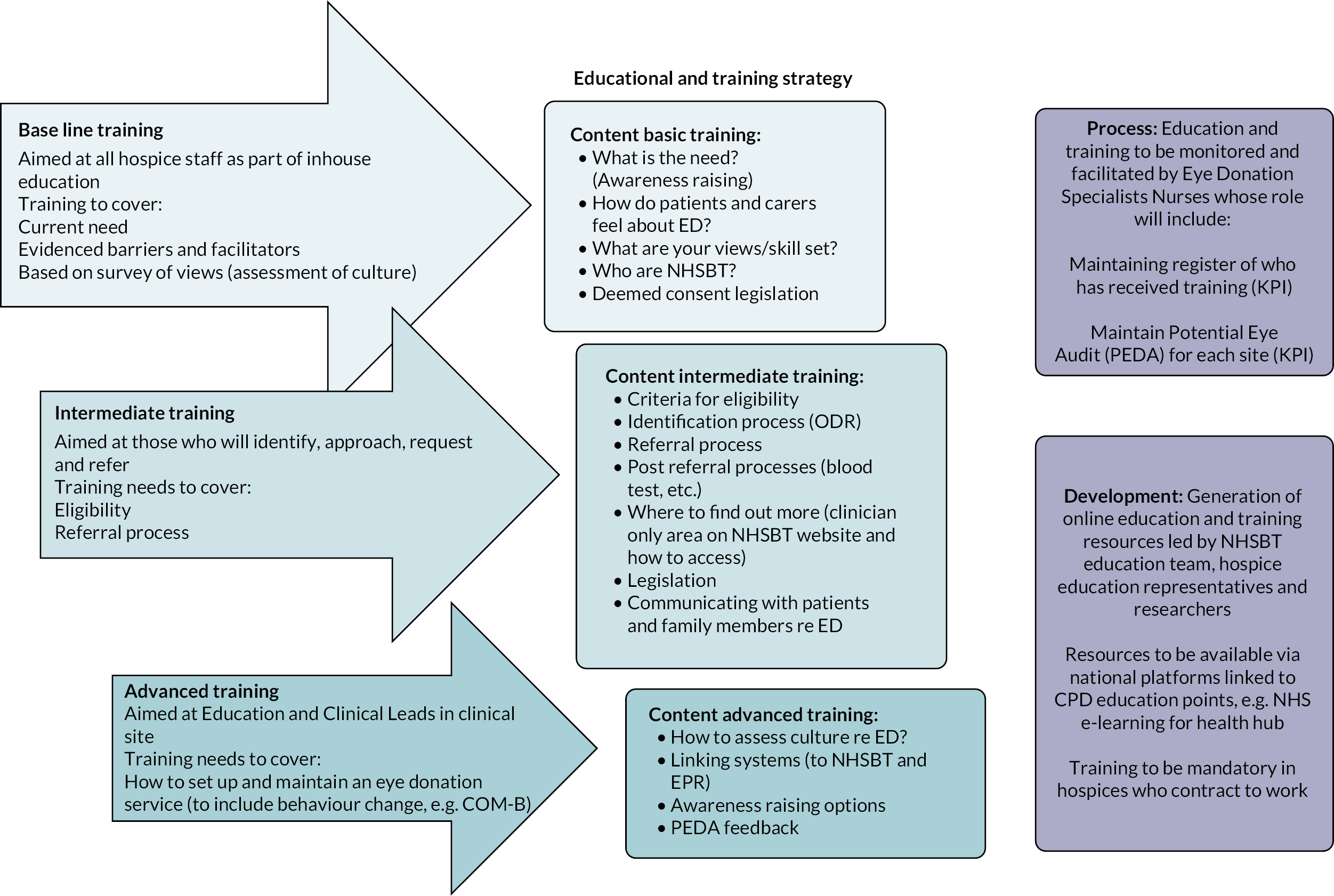
-
educational resources (baseline-level training) will be embedded in induction programmes for all new staff joining the hospice
-
with (intermediate-level training) being shared with those healthcare professionals who as part of their clinical role undertake EoLC planning discussions. Currently, this role is undertaken by medical practitioners at either consultant or registrar level, specialty doctors and clinical nurse specialists
-
a final suite of resources (advanced training) will be developed which would guide chief Executives of hospices in how to set up, monitor and evaluate service and contract with NHSBT-TES
-
RSPTD will be responsible for implementing training and education and will be responsible for the development, delivery, monitoring and amendment of the centrally agreed, validated, evidence-based educational strategy (supported by NHSBT education and research team)
-
resources should be evaluated on a yearly basis and presented to the strategic ED Hospice implementation working party, and Hospice ED education and training working party for review and, if needed, further intervention.
STEP 4: Development, monitoring, assessment of context-specific public awareness initiatives
Website development
An audit of 208 hospice websites in the UK showed that only 10 hospices have information about ED. Eight hospice sites in England had information about ED (in two cases very detailed information), 2 of the 12 hospice websites in Wales held information about ED (with one referring to OD in dying matters and one referring to OD in the ACP document available on the website). None of the three hospice websites in Northern Ireland had information about ED (but did mention organ donation in the advanced planning document on their websites) and none of the 14 hospice websites in Scotland mentioned organ, tissue or ED (see Report Supplementary Material 12: Hospice website audit) for details. These findings indicate a low level of information available to the public, patients, carers, etc. about ED as an end-of-life option for those who might be seeking information about hospice care. Therefore, social triggers to talk about ED are lacking. The public is not aware of ED, what it entails etc., and the triggers to search for information are lacking at the clinical level.
National Health Service Blood and Transplant-Tissue and Eye Services therefore need to develop centrally agreed, validated awareness-raising web content for integration into hospice websites. This content should be reviewed annually (by NHSBT-TES RSPTD), and changes agreed centrally (NHSBT-TES strategic ED implementation working party) and amended with hospice agreement. Costs for changes should be met by NHSBT-TES. The site used as the benchmark for our audit is recommended as a model of best practice to inform web resources.
Challenges to implementation
Current NHSBT-TES practice regarding eye donation in hospice care settings
In view of the findings that there is evidenced potential for ED across the hospice and palliative care services involved in this study, but with the greater potential in the hospice care settings, the proposed intervention is planned for implementation by NHSBT-TES into four hospice care settings from October 2022. The sites are geographically located within the remit of one of four retrieval teams currently available in England.
Currently, NHSBT-TES does not strategically select palliative care ED sites (other than to work more closely with those within the geographic location of retrieval teams); no assessment of potential or organisation readiness is carried out. Five (three at start of EDiPPPP) RSPTDs currently provide support to hospices across large geographic locations (North West and North Wales; London and South East; South West and South Wales; and Cheltenham and Gloucester). In view of the intervention steps, NHSBT-TES needs to invest in this team increasing their number to maximise implementation. ED numbers will also be limited if the agreed tissue cannot be retrieved and so NHSBT-TES need to review this resource also. Currently, there are four retrieval teams; however, if as stated in this report, there is an increasing number of hospices referring patients (increases stimulated by the EDiPPPP study presentations at local and national conferences) from 41 hospices (March 2021) to 63 hospices (March 2022), this increase will put pressure on these teams in facilitating retrieval. Lack of retrieval is a key de-motivator as if HCPs have approached family members, and the tissue cannot be retrieved, they are unlikely to raise this option going forward. Furthermore, if family members are informed that despite their deceased family member agreeing to ED, this was not completed, this story will stay with them and act as a negative ‘narrative’ shared on social media platforms.
Currently, 63 hospices in England are generating, on average, only seven referrals each to NHSBT-TES annually. 94 The current model is not a robust process for increasing the supply of eye tissue in the current climate of demand and limited supply and therefore we recommend STEPS to NHSBT-TES as this model takes into account the complexity that any intervention in this context needs to consider in designing an intervention that is adaptable and scalable.
Conclusion
We propose that if HCPs have the ‘capability’, ‘opportunity’ and ‘motivation’ to embed ED in EoLC planning, and that if NHSBT-TES follow a strategic selection process for ED sites as illustrated in STEPS providing key resources [RSPTD, resources (educational, financial (patient assessment admin support), website content development], there will be an increase in the supply of eye tissue for use in sight-restoring and sight-saving surgery and medical research.
Chapter 10 Concluding discussion
Chapter 10 represents the research questions and study objectives of the EDiPPPP study and indicates how these have been addressed by the EDiPPPP study. Given the specific commentary and recommendations that have been included in preceding chapters covering each of the study activities, the discussion here will be general in nature, and will not repeat details previously covered unless directly relevant to the discussion herein. The chapter continues by outlining the study limitations, proposing areas for future research and acknowledging the contribution of study partners and stakeholders.
Research question (RQ) 1a asked: ‘What is the potential for ED in HC and HPC services?’, with RQ1b asking: What consequences will any increase in ED from these settings have for NHSBT-TES in relation to resources, infrastructure, logistics?’ To answer these questions, we scoped the size and clinical characteristics of the potential ED population from research sites (Objective 1) and mapped the donation climate of each research site (Objective 2).
Currently, ED is rare in the HC and HPC settings. The lack of a donation climate and unclear processes are a key barrier to increasing the supply of eye tissue from palliative care settings as staff lack capability in undertaking the behaviour of identifying, approaching and referring potential donors, and they miss opportunities to enact the behaviour of discussing ED with patients. Findings from the note review undertaken in WP1 clearly indicate the potential for ED in HC services in particular, but low activity aligned to ED across the research settings. The EDiPPPP study has identified the challenges to healthcare professionals in both identifying and assessing patients for eligibility in the current information and knowledge landscape available to them. These challenges are a product of an institutional culture that does not facilitate ED; ED is not an embedded end-of-life option for patients to consider during EoLC planning.
If the reported potential in HC sites (56%, n = 337) was realised, this would equate to potentially 674 eyes (two eyes per donor) entering the supply chain (dependent on screening of donated tissue), and this is from just three HC sites across England. Figures from 202012 report that there were 25,498 deaths in HC settings in the UK (no significant change in this figure reported since previous figures in 2019) equating to 4.5% of all deaths in UK. However, from April 2021 to March 2022, NHSBT-TES only received 443 referrals from 63 hospice locations with 293 of those referrals generating eyes. If the potential from HC sites was accessed, this supply could potentially end the shortage, but not without engagement with, and investment (time, resources, finance) in these sites. Financial incentives are important as most hospices receive little monies from the NHS (around 37% for charitable hospices in England). 89 Other considerations include the current provision of retrieval teams (four in place across UK), regional specialist nurses in tissue donation (five in place across the UK), processing and storage capacity would have to be reviewed by NHSBT-TES. However, until an evaluation of the implemented intervention is carried out, we cannot be definitive about future potential ED potential from HS and HPC sites.
Research question 2 posed the question: ‘What system-based/attitudinal and educational barriers/facilitators to ED influence the identification and referral of potential eye donors in clinical settings and the embedding of ED in EoLC planning?’ Objectives 3 and 4 focused on identifying factors (attitudinal, behavioural) that enable or challenge service providers to consider and propose the option of ED as part of EoLC planning from a local and national perspective, to identify service users’ views regarding the option of ED and the propriety of discussing ED as part of admission procedures or as part of EoLC planning conversations.
Findings (WP1 and 2) indicate low levels of knowledge about the process of ED, the lack of any operational process (or routine) for considering the option of ED as part of an admissions process or ongoing EoLC planning discussions. There is a lack of routine processes facilitating the identification of potential donors, no orchestrated application of eligibility criteria to confirm donation status, low levels of knowledge regarding referral processes (to NHSBT-TES) or about what happens after a patient has been referred to NHSBT-TES. While other authors have reported that healthcare professionals lack confidence to initiate ED discussions, research to date has not provided the constituents of ‘confidence’. Findings from the EDiPPPP study have identified the specific areas HCPs perceive they need education and training around and which would underpin feelings of capability to engage in conversations that include ED.
Empirical research has reported that the possession of subjective and objective knowledge about organ donation, in general, facilitates donation discussions and has the potential to change attitudes and increase donation. 95,96 It is also known that a lack of education and training, to prepare for difficult conversations, prevents HCPs from being able to support patients and family members from having these conversations. 51,52 Of note is that no literature has been found that articulates or illustrates the educational content required by healthcare professionals when engaging in conversations about the option of ED and therefore our recommendation is that an evidence-based, co-constructed (with site clinicians) centrally generated (by NHSBT-TES) education and training programme needs to be developed that can be rolled out nationally via various modalities (e-learning for health platforms, in-house education teams, donation champions, etc.). Training needs to be mandatory for new staff (as part of induction) and regularly updated to support HCP practice. We propose that education and training is fundamental to HCPs’ perceptions of their ‘capability’ in implementing ED into usual EoLC planning.
While most respondents reported a lack of knowledge, and some a lack of confidence, in ED-related discussion, one area that was a key knowledge deficit was the still ‘new to many’ deemed consent legislation. As far as we can see from literature searches, our findings are the first to report the views, knowledge and understanding of HCPs in HC and HPC regarding deemed consent legislation and its operationalisation into practice. Findings from WP1 and 2, clearly indicate that HCPs are unsure about ‘how’ deemed consent legislation should be operationalised in practice as HCPs (especially in the HC sector) have not received any policy guidance, clinical guidelines or engagement by NHSBT about the new legislation. Of note is that there appears to be an assumption by organisations such as NHSBT that the change in legislation ‘will’ address the shortage of organs, tissue and eyes despite evidence indicating that no country has achieved a sustained increase in donation rates (solid organs) after modifying the law. 97 It is only by identifying the specific barriers to donation that changes will take place.
Positive and encouraging findings from WP1 and 2 are an evidenced climate of preferences supporting embedding ED into EoLC planning discussions, and a motivation by both HCPs and patients to be part of these discussions. Our findings indicate key facilitators, including high levels of motivation, for the option of ED to be embedded in routine practice and for patients to be asked (pre death) about their donation views regarding ED. Patients have voiced their preferences that: they should be asked about ED as part of planning, that HCPs should raise the issue (and not rely on patients or family members to raise the issue), that the approach should take place when the patients have the cognitive and emotional capacity to make decisions and that patient themselves should make the decision regarding whether they will or will not go forward to donation. Patients are clear that a conversation about ED should take place.
Our findings that patients are reporting that they would not find discussing the topic of ED distressing is supported by other researchers undertaking small-scale survey65 and interview studies73 with patients in UK Hospice settings. EDiPPPP findings provide clarification around patient preferences as to ‘when’ the conversation should take place and ‘who’ ultimately should make the decision about whether the patient becomes an eye donor. We provide a wider perspective by including carers of patients undergoing current palliative care in our study population who provide confirmation that the lack of awareness about the option of ED does not solely lay with the patient, but that family members are also unaware of this EoLC option.
Along with other researchers, we have identified that healthcare professionals have concerns about raising the option of ED and causing distress to patients and family members,34,58,64,68 and yet not one HCP participant provided us with any example of their experiences of what ‘distress’ was caused to a patient or family member when they have raised the issue. As none of the patients in our study had been approached about the option of ED, this perception of HCPs appears to be more of a ‘fable’ than fact. Decisions not to raise the issue of ED in the EDiPPPP study appeared linked to issues such as the physical situation of the patient (needed pain management or lack of capacity), which are important issues to bear in mind, and in fact align with the views of patients that they want to be asked when they have emotional and cognitive capacity to discuss. However, this will not be the case for the majority of patients (especially those attending as an outpatient or attending one of the ‘living well centres’ run by hospices) and so it is still not clear why patients outside of this cohort (in pain, lack of capacity) are not having the option of ED discussed as part of planning, especially in view of other sensitive (and potentially distressing topics) are being discussed, for example, do not attempt resuscitation orders and plans for funerals.
A key consideration, not explicated or stressed in research to date, is our contention that the context within which discussions around ED need to take place, the context of death, is an influence on the behaviour of HCPs. Apart from living donation, all donation options cannot proceed until someone has died; therefore, raising a topic that so profoundly signals impending death may be why HCPs are reluctant to raise the option of ED. A further consideration is that ED does not benefit the patient (unlike other topics raised in EoLC planning conversations, e.g. DNACPR orders), which are perceived to do so. ED will benefit someone who the HCP and patient do not know and whose need is not understood (or in fact who HCPs and patients are aware of).
A further consideration is that death not only denies the NoK of a significant relationship but also robs them of many of their usual coping mechanisms, imposing a sequence of events that leave family members feeling dispossessed of physical and psychological equilibrium;31 therefore, HCPs may avoid conversation in view of concerns about the reactions of family members.
Including the views of patients and carers in education and training initiatives may reduce the concerns voiced by HCPs. Embedding the ED conversation into routine practice, will, in time, normalise the subject and will lead to an increase in opportunity and capacity. Evidence supports the benefits in ‘introducing’ this issue at admission with the discussion being merely to assess donation status (as per ODR). 66 Adding ED to admission protocols would offer the opportunity to clarify the potentially long-held plans of the patient to be a donor, which with the onset of a cancer diagnosis was perceived as no longer an option. Furthermore, in raising this issue as part of the usual admission process, patients and family members are then able to discuss this option if they wish to and seek further information and guidance. As reported by the Organ Donation Taskforce, making donation ‘usual’ as opposed to ‘unusual’ is essential if donation rates are to increase. 8
Finally, Research question 3 asked: ‘What behaviour change strategies will be effective in increasing ED across the community of service providers and service users within HPC and HCS?’ with the aim of developing an empirically based, theoretically informed intervention designed to change behaviours in relation to the identification, approach, request and referral of patients from HPC and HC for ED (Objective 5). In explicating the barriers and facilitators to the practice, perceptions and preferences of service providers and service users related to all aspects of ED in HC and HPC settings and drawing on validated behaviour change theory, we have developed STEPS. Tools (EEDAC and OREDAC) from the toolkit have been tested for proof of concept and have been reported as ‘just what we need’ by clinical PIs and clinical support team members at NHSBT-TES; however, a full evaluation of STEPS is needed to assess if its implementation has achieved the aim for behaviour change leading to an increased supply of eye tissue from HC settings.
Limitations
COVID-19 pandemic
The impact of the COVID-19 pandemic cannot be overstated as almost all aspects of the study were impacted by the disruption to clinical services (and the research team) caused by the COVID-19 pandemic. While the EDiPPPP study has generated a complex intervention, this has not been pilot tested, while components of it, the EEDAC and OREDAC tools, have undergone proof-of-concept testing. A pilot study testing the intervention, implemented by NHSBT-OTDT, is due to commence in March 2023.
Arranging PSC and PI meetings was especially challenging as everyone’s time was compromised. To make the best use of time, we developed all presentations as recorded presentations that were sent to PSC members ahead of all meetings so that they could review and prepare questions and comments beforehand. Meetings were limited to key agenda items and Q and A.
Methodology
An innovative, and what was initially proving to be an extremely informative, element of study design (participant observation in clinical sites) had to cease having taken place at only two sites due to restrictions in access across healthcare setting in the UK imposed by the COVID-19 pandemic. This was frustrating as those PIs who experienced an embedded researcher were very positive about this data collection method as it streamlined the identification of, recruitment to and undertaking of interviews and focus groups. Primarily, this method provided access to the context of care and practice facilitating independent observation of processes and the informational climate that became less visible to researchers as the study progressed.
Likewise, we are confident that the pressures on, and changes to working practices, experienced by HCPs contributed to the 8% response rate in the national survey. The fact that Hospice UK sent out the survey on their COVID hospice contact list (being accessed only by their COVID link) was a factor in low response and a learning note for future research. Despite this low response rate, the depth of information provided in the free-text option of the survey was indicative of HCPs making time to engage in questions about a topic that they see as an important element of their care provision.
Patient and public involvement in the study
The aim of PPI involvement (see Report Supplementary Material 16: GRIPP2) in the EDiPPPP study was to gain the insights of PPI members (DC and SC) who had both experienced being asked about the option of tissue donation as family members of a deceased patient. DC had raised the option of tissue donation with HCPs (as the issue had not been raised at the death of her husband and daughter, who died in different circumstances and at different times). SC had experienced an unsolicited call regarding the option of tissue donation and had in fact raised a complaint regarding the call. Subsequently, DC and SC joined the donor advisory group (DAG) convened by NHSBT-TES as family members.
DC has championed tissue donation for many years, with DC being interviewed by organisations such as Sky TV about the option of ED. As members of the DAG, DC and SC were part of the group where the idea for the EDiPPPP study was first discussed. Both DC and SC agreed to be PPI co-applicants on the EDiPPPP study contributing to the study protocol (PES for all applications and final report, Interview schedules, etc.). DC has attended all PSC meetings, reviewed documents, commented on issues arising in data collection and been a ‘sounding’ board for the research team. SC had attended all but the last PSC meeting (due to a close bereavement) and has likewise reviewed and commented on all study documentation. Both DC and SC were members of the TEC in which they challenged the views of some HCPs that ED was not something that should be raised as part of EoLC planning. Neither of our PPI members has read the final report due to personal commitments and annual leave. PPI involvement in this study has been uniformly positive, with both PPI members being engaged, informed, positive about the research and motivated to fulfil their roles.
Equality and diversity
From the start, the EDiPPPP study aimed to ensure equity of opportunity for diverse groups to participate. Site selection was intended to gain representation from across England and across ethnic groups as donation rates are reported to differ by region and ethnicity94 (see Report Supplementary Material 11 for service providers demographics and Table 18 for service user participant demographics).
Despite these efforts, our patient and carer cohorts were dominated by cohorts who self-defined as ‘White British’ [with HC showing a greater ethnic diversity than HPC (see Table 18)]. Historically black, Asian and minority ethnic groups are reported to not access hospice care in the UK, but a recent literature review has indicated that this picture is changing. 84
Our PSC had wide representation (clinicians, PPI, charity representatives, partner organisations) and was predominantly female. TEC membership (see Table 19) gained a similar representation to the steering committee and again was predominantly female.
All materials, meeting notes and presentations were prepared with the aim of ensuring that members had the time to connect with materials and that materials met member needs (one member had visual deficits and one member was registered deaf).
The research team was diverse with two members being female (White British and Black African) and one male (White British). The CI was female and disabled (visually impaired) with two team members disclosing neurodiversity diagnoses. The clinical co-applicants were predominantly female (one male), which is not unusual in palliative care settings. Research experience ranged from extensive (TLS, MB, MM, CF) to moderate (AH, CR, SM, JW, BMS) to low experience of undertaking research and publishing research (JS, EL, EW, SC, DC). Junior team members of the research team (BMS) were provided with training (funded by the study) in use of ATLAS.ti software, undertaking systematic literature reviews, writing successful bids. BMS was also supported to be first author on the scoping review generated during the study and present at conferences (see Study outputs for details of publications and conference presentations). MB undertook training in project management and ATLAS.ti software. Co-applicant SM was funded to attend the EEBA conference in March 2020 and AK (a trainee palliative care doctor) who participated in the free-text analysis of survey data as part of personal development, was funded to attend the Hospice UK conference in November 2021 with the aim of developing her network. AK will be hosting a webinar about ED for the Royal Society of Medicine in March 2023 with TLS and EW agreeing to participate.
Acknowledgements
Contribution of authors
Tracy Long-Sutehall (https://orcid.org/0000-0002-6661-9215) (Associate Professor in Applied Health Research) jointly led on writing the final report with contributions from the other authors. She was the Chief Investigator who conceptualised the study, developed the study design and led on gaining ethical approval, PPI engagement and intervention design.
Mike Bracher (https://orcid.org/0000-0001-5861-2657) (Senior Research Fellow) jointly led on writing the final report with contributions from the other authors. He managed the project on a day-to-day basis and collected data in all work packages.
Sarah Mollart (https://orcid.org/0000-0003-0250-3456) (Consultant in Palliative Medicine) contributed to the writing of the report and undertook all recruitment and data collection in WP1, she also facilitated site participant observation.
Jane Wale (https://orcid.org/0000-0002-4747-4751) (Consultant in Palliative Medicine) contributed to the writing of the report and undertook all recruitment and data collection in WP1.
All authors reviewed and approved the final report.
Participants
As a team, we would like to thank all participants in this study (HCPs, patients and carers) who gave up their time and shared their experiences with us. Their contribution has generated new knowledge and informed the development of an intervention that could change the landscape in relationship to the supply of eye tissue for use in sight-saving and sight-restoring surgery and research in the UK.
Project Steering Committee members
We would like to thank members of our PSC who despite the challenges imposed by the COVID-19 pandemic engaged with the study materials and provided guidance on issues raised by the research team. PSC members: Professor Myfanwy Morgan (Chair), Anna Klepacz (Keratoconus Society), Jim Fellows (Donor Family Network), Diana Comfort (PPI), Sian Cheverton (PPI), Parwaz Hossain (Ophthalmic surgeon), Cathy Miller (Education lead NHSBT).
Partner sites and study co-applicants
We wish to extend special thanks to our clinical PIs who, in the face of extreme challenges imposed on them by the COVID-19 pandemic, remained engaged and motivated to complete the EDiPPPP study despite huge clinical pressure. Thank you to: Professor Christina Faull (CF), Professor in Palliative Medicine, LOROS Hospice, UK; Adam Hurlow (AH), Consultant in Palliative Medicine, Leeds Teaching Hospitals NHS Trust, UK; Erika Lipscombe (EL), Director of Clinical Services/Matron, Rowans Hospice, UK; Dr Sarah Mollart (SM), Consultant in Palliative Medicine, West Suffolk Hospital NHS Foundation Trust, UK; Clare Rayment (CR), Consultant in Palliative Medicine Marie Curie Hospice Bradford, UK; Jill Short (JS), Education Lead, Rowans Hospice, UK; Dr Jane Wale (JW), Consultant in Palliative Medicine, Milton Keynes University Hospital NHS Foundation Trust, UK; Emma Winstanley (EW), Lead Nurse for Tissue Donation NHSBT-TES).
Thanks are extended to Michelle Myall (MM), School of Health Sciences, University of Southampton, UK for her early input into survey tool design and support of research team members.
NHSBT-TES contributors
We extend our thanks to Mark Brown (clinical support team NHSBT-TES) and Julie Johnson (ex-lead of clinical support team NHSBT-TES) who evaluated note review proforma in WP1S1.
Other contributions
Dr Banyana C. Madi-Segwagwe (BMS) was the study research fellow and collected data in all work packages. Data analysis was undertaken by the core team (MB, BMS, TLS) with Dr Michelle Myall contributing to the design of the survey tool in WP2S3.
We extend our thanks to Anna Zatorska (Trainee in palliative care medicine) who participated in the free-text analysis from the scoping review (with BMS) as part of personal development and interest in, and championing of ED, during palliative care placements.
EDiPPPP study outputs
Conference presentations:
European Eye Bank Association March 2022
-
Current practice of healthcare professionals in hospice and hospital palliative care settings related to Eye Donation as part of EoLC: a national survey – Findings from the Eye Donation from Palliative and Hospice care contexts: investigating Potential, Practice, Preference and Perceptions (EDiPPPP) study. Presenter: Dr Tracy Long-Sutehall. Awarded best oral presentation.
-
Eye donation in Palliative and Hospice care settings: patient views and missed opportunities – Findings from the EDiPPPP study. Presenter: Dr Banyana Madi-Segwagwe.
-
The potential for ED from hospice and palliative care clinical settings in England – a retrospective case notes review of deceased patient records – Findings from the EDiPPPP study. Presenter: Dr Tracy Long-Sutehall.
Hospice UK National conference, Liverpool, November 2021:
Eye donation in palliative and hospice care settings: patient views and missed opportunities. BMJ Supportive and Palliative Care; 30 November 2021|
DOI: 10.1136/spcare-2021-Hospice.18. Presenter: Dr Tracy Long-Sutehall.
BSA Medical Sociology Group Sept 2021:
‘If they want, they can go and get more information’
BSA Medical Sociology Group 2021, 17/09/21. Presenter: Dr Michael Bracher.
MC Bradford Virtual Research morning Sept 2020:
Eye Donation from Palliative and Hospice care contexts: investigating Potential, Practice, Preference and Perceptions (EDiPPPP) – Study summary. Presenter: Dr Banyana Magi-Segwagwe.
Journal publications
Long-Sutehall T, Madi-Segwagwe BC, Hurlow A, Faull C, Rayment C, Jacob F, et al. The potential for eye donation from hospice and palliative care clinical settings in England: a retrospective case note review of deceased patients' records. Cell Tissue Bank 2023;24:341–9. https://doi.org/10.1007/s10561-022-10036-2
Madi-Segwagwe BC, Bracher, Myall M, Long-Sutehall T. Barriers and facilitators to eye donation in hospice and palliative care settings: a scoping review. Palliat Med Rep 2021;2(1):175–87. https://doi.org/10.1089/pmr.2021.0017
Ethical approval
Prior to commencement of the study in 2019, ethical approval was gained from the University of Southampton’s Ethics and Research Governance Online (ERGO) service (Study ID: 591850) and the UK NHS Health Research Authority (IRAS ID: 256351).
Two non-substantial amendments were approved – the first following pause of data collection on 18 March 2020 due to the COVID-19 pandemic with resumption on 2 July 2020 (University of Southampton institutional ethics committee ERGO REF – 59185 and the second non-substantial amendment in May 2021, to allow the Transparent Expert Committee (TEC) process to be conducted online using the Microsoft Teams platform, as opposed to in-person as originally stated in the protocol (ERGO ID 59185.A1).
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review. The qualitative data included in the study are not suitable for sharing beyond that contained within the report. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives
You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Information Governance Statement
The University of Southampton is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Southampton is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer at www.southampton.ac.uk/legalservices/what-we-do/data-protection-and-foi.page.
Department of Health disclaimer
This report presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, CCF, NETSCC, the HSDR programme or the Department of Health.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012;96:614-8.
- College of Optometrists . Eye Health Research 2019. www.college-optometrists.org/the-college/research.html (accessed November 2022).
- Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, et al. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol 2016;134:167-73.
- Bracher M, Madi-Segwagwe BC, Winstanley E, Gillan H, Long-Sutehall T. Family refusal of eye tissue donation from potential solid organ donors: a retrospective analysis of summary and free-text data from the UK National Health Service Blood and Transplant Services (NHS-BT) National Referral Centre (1 April 2014 to 31 March 2). BMJ Open 2021;11.
- Lawlor M, Kerridge I. Anything but the eyes: culture, identity, and the selective refusal of corneal donation. Transplantation 2011;92:1188-90.
- Lawlor M, Kerridge I. Understanding selective refusal of eye donation: identity, beauty, and interpersonal relationships. J Bioeth Inq 2014;11:57-64. https://doi.org/10.1007/s11673-013-9497-9.
- O’Carroll RE, Foster C, McGeechan G, Sandford K, Ferguson E. The ‘ick’ factor, anticipated regret, and willingness to become an organ donor. Health Psychol 2011;30:236-45. https://doi.org/10.1037/a0022379.
- Department of Health . Organs for Transplants: A Report from the Organ Donation Taskforce 2008. www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwihlpqUveb2AhXpQUEAHduKC_AQFnoECAYQAQ&url=https%3A%2F%2Fnhsbtdbe.blob.core.windows.net%2Fumbraco-assets-corp%2F4245%2Forgansfortransplantstheorgandonortaskforce1streport.pdf&usg=AOvV (accessed January 2020).
- Gaum L, Reynolds I, Jones MNAA, Clarkson AJ, Gillan HL, Kaye SB. Tissue and corneal donation and transplantation in the UK. Br J Anaesth 2012;108:i43-7. https://doi.org/10.1093/bja/aer398.
- NHSBT . Organ Donation and Transplantation: Activity Report 2019 20 2020.
- Office for National Statistics . Deaths at Home Increased by a Third in 2020, While Deaths in Hospitals Fell Except for COVID-19 2021. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/deathsathomeincreasedbyathirdin2020whiledeathsinhospitalsfellexceptforcovid19/2021-05-07 (accessed November 2021).
- Office for Health Improvement and Disparities . Palliative and End of Life Care Profiles 2020. https://fingertips.phe.org.uk/profile/end-of-life/data (accessed August 2020).
- NHSBT . NHS Blood and Transplant: Eye and Tissue Strategy 2016.
- Royal College of Ophthalmologists . Standards for the Retrieval of Human Ocular Tissue Used in Transplantation, Research and Training 2013. www.rcophth.ac.uk/publications/current-clinical-guidelines/ (accessed July 2018).
- NHSBT, NHS-BT Organ and Tissue Advisory Group (OTAG) . NHSBT Ocular Tissue Advisory Group Meeting Held at 12.30 Pm on Wednesday 29th June 2016 at ODT, Bristol 2016. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/4946/otag_minutes_290616.pdf (accessed July 2018).
- Wight D, Wimbush E, Jepson R, Doi L. Six steps in quality intervention development (6SQuID). J Epidemiol Community Health 2016;70:520-5. https://doi.org/10.1136/jech-2015-205952.
- Long-Sutehall T, Sque M, Addington-Hall J. Secondary analysis of qualitative data: a valuable method for exploring sensitive issues with an elusive population?. J Res Nurs 2011;16:335-44. https://doi.org/10.1177/1744987110381553.
- Morgan D. Focus Groups as Qualitative Research. Thousand Oaks, CA: SAGE; 1997.
- Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Health 2015;13:141-6. https://doi.org/10.1097/XEB.0000000000000050.
- Krippendorff K. Content Analysis: An Introduction to Its Methodology. Thousand Oaks, CA: SAGE; 2018.
- de Meyrick J. The Delphi method and health research. Health Educ 2003;103:7-16. https://doi.org/10.1108/09654280310459112.
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs 2000;32:1008-15. https://pubmed.ncbi.nlm.nih.gov/11095242/ (accessed November 2022).
- Bowling A. Research Methods in Health: Investigating Health and Health Services. New York, NY: McGraw Hill; Open University Press; 2014.
- West R, Michie S. A Brief Introduction to the COM-B Model of Behaviour and the PRIME Theory of Motivation. Qeios. 2020 n.d. www.qeios.com/read/WW04E6 (accessed November 2022).
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Heal Care 2005;14:26-33. https://doi.org/10.1136/qshc.2004.011155.
- Goodstadt M. The Use of Logic Models in Health Promotion Practice 2005. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://institute.welcoa.org/wp/wp-content/uploads/2016/04/Goodstadt-Logic-Models.pdf (accessed November 2022).
- McLaughlin JA, Jordan GB. Logic models: a tool for telling your program’s performance story. Eval Program Plann 1999;22:65-72. www.studocu.com/es-mx/document/universidad-iberoamericana-mexico/crecimiento-economico/logic-models-a-tool-for-telling-your-programs-performance-story/12872146 (accessed November 2022).
- Millar A, Simeone RS, Carnevale JT. Logic models: a systems tool for performance management. Eval Program Plann 2001;24:73-81. www.researchgate.net/publication/4949267_Logic_Models_A_Systems_Tool_for_Performance_Management (accessed July 2019).
- Siminoff LA, Traino H. Improving donation outcomes: hospital development and the rapid assessment of hospital procurement barriers in donation. Prog Transplant 2009;19:180-7. https://doi.org/10.1177/152692480901900213.
- Alolod GP, Traino HM, Siminoff LA. Utility and Usability of the Rapid Assessment of Hospital Procurement Barriers in Donation (RAPiD) as a tool for OPO hospital development staff. Prog Transplant 2016;26:241-8. https://doi.org/10.1177/1526924816655960.
- Long T, Sque M, Addington-Hall J. Conflict rationalisation: how family members cope with a diagnosis of brain stem death. Soc Sci Med 2008;67:253-61. https://doi.org/10.1016/j.socscimed.2008.03.039.
- Jani B, Blane D, Browne S, Montori V, May C, Shippee N, et al. Identifying treatment burden as an important concept for end of life care in those with advanced heart failure. Curr Opin Support Palliat Care 2013;7:3-7. https://doi.org/10.1097/SPC.0b013e32835c071f.
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021;374:1-11.
- Gillon S, Hurlow A, Rayment C, Zacharias H, Lennard R. Obstacles to corneal donation amongst hospice inpatients: a questionnaire survey of multi-disciplinary team member’s attitudes, knowledge, practice and experience. Palliat Med 2012;26:939-46. https://doi.org/10.1177/0269216311420482.
- Wale J, Arthur A, Faull C. An analysis of knowledge and attitudes of hospice staff towards organ and tissue donation. BMJ Support Palliat Care 2014;4:98-103.
- Tregenna E, Mollart S. Corneal Donation within a Hospice Setting: Hospice Patients’ Experience of the Routine Discussion of Corneal Donation Options on Admission to the Inpatient Ward at St Nicholas Hospice Care [Unpublished Service Evaluation]. London: Bury St. Edmunds; 2018.
- Higginson IJ, Evans CJ, Grande G, Preston N, Morgan M, McCrone P, et al. MORECare . Evaluating complex interventions in end of life care: the MORECare Statement on good practice generated by a synthesis of transparent expert consultations and systematic reviews. BMC Med 2013;11.
- NHS-BT Organ and Tissue Advisory Group (OTAG) . Tissue and Eye Procurement from Solid Organ Donors (TEPSOD) Activity Report 2016. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/2790/eye_procurement_solid_organ_donors_june16.pdf (accessed November 2021).
- ATLAS.ti . Berlin, Heidelberg, DE: ATLAS.ti Scientific Software Development GmbH; 2022. https://atlasti.com/.
- Woolf NH, Silver C. Qualitative Analysis Using ATLAS.ti: The Five-Level QDATM Method. London: Taylor & Francis; 2017.
- Silver C, Woolf NH. Five-Level QDA. Digital Tools for Qualitative Research 2016. https://digitaltoolsforqualitativeresearch.org/2016/11/15/five-level-qda/.
- Schreier M. The SAGE Handbook of Qualitative Data Analysis. London: SAGE; 2014.
- Madi-Segwagwe BC, Bracher M, Myall M, Long-Sutehall T. Barriers and facilitators to eye donation in hospice and palliative care settings: a scoping review. Palliat Med Reports 2021;2:175-87. https://doi.org/10.1089/pmr.2021.0017.
- Rocon PC, Ribeiro LP, Scárdua RF, De Almeida AV, Gomes LM, Azeredo HC, et al. Main causes of nonfulfillment of corneal donation in five hospitals of a Brazilian State. Transp Proc 2013;45:1038-42. https://doi.org/10.1016/j.transproceed.2013.02.008.
- Muraine M, Toubeau D, Menguy E, Brasseur G. Analysing the various obstacles to cornea postmortem procurement. Br J Ophthalmol 2002;86:864-8. https://doi.org/10.1136/bjo.86.8.864.
- Mack RJ, Mason P, Mathers WD. Obstacles to donor eye procurement and their solutions at the University of Iowa. Cornea 1995;14:249-52. https://doi.org/10.1097/00003226-199505000-00004.
- Prous M, Ponto M. Barriers to ocular tissue donation in acute clinical settings. Prog Heal Sci 2015;5:134-41. https://search.ebscohost.com/login.aspx?direct=true&db=a9h&AN=112045113&authtype=sso&custid=s8993828&site=ehost-live (accessed July 2020).
- Roach R, Broadbent AM. Eye donation in Sydney metropolitan palliative care units. J Palliat Med 2010;13:121-3. https://doi.org/10.1089/jpm.2009.0213.
- Vorstius Kruijff PE, Jansen NE, Muitjens BSM, Blok-Singerling JGC, Tecklenburg BDA, De Vos MLG, et al. Are all tissue donors recognised? A cohort study in three Dutch hospitals. Cell Tissue Bank 2014;15:483-90. https://doi.org/10.1007/s10561-013-9418-5.
- Kent B, Owens RG. Conflicting attitudes to corneal and organ donation: a study of nurses’ attitudes to organ donation. Int J Nurs Stud 1995;32:484-92. https://doi.org/10.1016/0020-7489(95)00009-M.
- van Loo M, Rabbetts C, Scott T. Emergency nurse initiation of discussion about tissue donation with suddenly bereaved relatives. Int Emerg Nurs 2008;16:257-65. https://doi.org/10.1016/j.ienj.2008.07.002.
- Collins TJ. Organ and tissue donation: a survey of nurse’s knowledge and educational needs in an adult ITU. Inten Crit Care Nurs 2005;21:226-33. https://doi.org/10.1016/j.iccn.2004.10.006.
- Long-Sutehall T, Winstanley E, Clarkson AJ, Sque M. Evaluation of the experiences of family members whose deceased relative donated tissues at the NHSBT dedicated donation facility in Speke, Liverpool. Cell Tissue Bank 2012;13:537-46. https://doi.org/10.1007/s10561-011-9269-x.
- Thompson TL, Robinson JD, Kenny RW. Gender differences in family communication about organ donation. Sex Roles 2003;49:587-96. https://link.springer.com/article/10.1023/B:SERS.0000003129.25173.ad (accessed November 2022).
- National Health Service Blood and Transplants . Cornea Activ 2021;650:97-104. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/23475/section-10-cornea-activity.pdf (accessed November 2021).
- Stiel S, Hermel M, Radbruch L. Cornea donation from patients deceased at a palliative care unit. Palliat Med 2011;25:183-4. https://doi.org/10.1177/0269216310385602.
- Douville F, Godin G, Légaré F, Germain M. Implementation intentions as a strategy to increase the notification rate of potential ocular tissue donors by nurses: a clustered randomized trial in hospital settings. Nurs Res Pract 2014;2014:1-7. https://doi.org/10.1155/2014/921263.
- Edwards P. Corneal donation within palliative care: a review of the literature. Int J Palliat Nurs 2005;11:481-6. https://doi.org/10.12968/ijpn.2005.11.9.19783.
- Sebach AM, McDowell D. Developing a tissue donation advocacy program in a rural emergency department. J Emerg Nurs 2012;38:63-8. https://doi.org/10.1016/j.jen.2011.01.013.
- National Institute for Health and Care Excellence (NICE) . Organ Donation for Transplantation: Improving Donor Identification and Consent Rates for Deceased Organ Donation (Clinical Guideline) 2011. www.nice.org.uk/guidance/cg135/resources/organ-donation-for-transplantation-improving-donor-identification-and-consent-rates-for-deceased-organ-donation-pdf-35109512048581 (accessed August 2019).
- Leadership Alliance for the Care of Dying People . One Chance to Get It Right 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/323188/One_chance_to_get_it_right.pdf (accessed August 2021).
- Royal College of Nursing (RCN) . Consent for Organ and Tissue Donation After Death 2018. www.rcn.org.uk/Professional-Development/publications/pdf-006698 (accessed August 2020).
- Taylor H, Langford L, Long-Sutehall T, Tilsley D. Specialist Family Approach Audit. Liverpool; 2012.
- Wells J, Sque M. ‘Living choice’: the commitment to tissue donation in palliative care. Int J Palliat Nurs 2002;8:22-7. https://doi.org/10.12968/ijpn.2002.8.1.10231.
- Ng I, Astle J, Tregenna E, Eades H, Mollart S. Improving corneal donation rates: a three-phase analysis of professional and patient factors. Futur Healthc J 2019;6. www.rcpjournals.org/lookup/doi/10.7861/futurehosp.6-1-s38.
- Niday P, Painter C, Peak J, Bennett E, Wiley M, McCartt L, et al. Family and staff responses to a scripted introduction to tissue donation for hospice inpatients on admission. Prog Transp 2007;17:289-94. https://doi.org/10.1177/152692480701700406.
- Gillon S, Hurlow A, Rayment C, Zacharias H, Lennard R. Eligibility for corneal donation within the hospice population. Palliat Med 2010;24:551-2.
- Tredgett K, Ward-Davies L. Responding to the public’s voice: changing cornea donation practice in a hospice. BMJ Support Palliat Care 2019;9:112-3.
- Wells J, Sque M. Living choice: the commitment to tissue donation in palliative care. Int J Palliat Nurs 2002;8:22-7. www.magonlinelibrary.com/doi/10.12968/ijpn.2002.8.1.10231.
- Kent BC. Protection behaviour: a phenomenon affecting organ and tissue donation in the 21st century?. Int J Nurs Stud 2004;41:273-84. https://doi.org/10.1016/j.ijnurstu.2003.09.001.
- Spencer M. The barriers to organ and tissue donation in palliative care. Medicine 2012;2:1-11. https://doi.org/10.1136/EOLJNL-02-02.5.
- Lerpiniere C, Verble M. Requesting tissue donation. Emerg Nurse 2009;16:22-5.
- Walker L, Neoh K, Gilkes H, Rayment C. A qualitative study using semi-structured interviews of palliative care patients’ views on corneal donation and the timing of its discussion. Palliat Med 2018;32:1428-37. https://doi.org/10.1177/0269216318784210.
- Carey I, Forbes K. The experiences of donor families in the hospice. Palliat Med 2003;17:241-7. https://doi.org/10.1191/0269216303pm694oa.
- Kuo SC, Chou PL, Liao YC, Chen YF, Cheng JF, Sun JL. Perspectives of decision-making for corneal donation: a qualitative research among cancer patients. Omega 2020;80:648-65. https://doi.org/10.1177/0030222818754666.
- Microsoft Excel . Microsoft Excel 2021. www.microsoft.com/en-us/microsoft-365/excel.
- OBS Studio Contributors . Open Broadcaster Software 2021. https://obsproject.com/.
- Siminoff LA, Marshall HM. The rapid assessment of hospital procurement barriers in donation: assessing hospitals for change. J Healthc Qual 2009;31:24-33. https://doi.org/10.1111/j.1945-1474.2009.00034.x.
- Gift of Sight . Gift of Sight 2020. www.giftofsight.org.uk/ (accessed 7 July 2020).
- Albertsen A. Deemed consent: assessing the new opt-out approach to organ procurement in Wales. J Med Ethics 2018;44:314-8. https://doi.org/10.1136/medethics-2017-104475.
- Redmond, WA: Microsoft Corporation; 2021.
- Lépine J, Leiva Portocarrero ME, Delanoë A, Robitaille H, Lévesque I, Rousseau F, et al. What factors influence health professionals to use decision aids for Down syndrome prenatal screening?. BMC Pregn Childb 2016;16.
- Robertson R. 2008. www.kingsfund.org.uk/sites/files/kf/field/field_document/information-promote-healthy-behaviours-kicking-bad-habits-supporting-paper-ruth-robertson.pdf (accessed August 2021).
- Tobin J, Rogers A, Winterburn I, Tullie S, Kalyanasundaram A, Kuhn I, et al. Hospice care access inequalities: a systematic review and narrative synthesis. BMJ Support Palliat Care 2022;12:142-51. https://doi.org/10.1136/bmjspcare-2020-00271.
- Leeman J, Baernholdt M, Sandelowski M. Developing a theory-based taxonomy of methods for implementing change in practice. J Adv Nurs 2007;58:191-200. https://doi.org/10.1111/j.1365-2648.2006.04207.x.
- Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implement Sci 2010;5:1-6. https://doi.org/10.1186/1748-5908-5-14.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Bandura A. The Blackwell Handbook of Principles of Organizational Behavior. Oxford: Blackwell; 2000.
- von Petersdorff C, Patrignani P, Landzaat W, Jones S. Modelling Demand and Costs for Palliative Care Services in England: A Final Report for Sue Ryder 2021. https://www.sueryder.org/sites/default/files/2021-03/Modelling_Demand_and_Costs_for_Palliative_Care_Services_in_England%20%281%29.pdf (accessed March 2022).
- Knott D, Muers S, Aldridge S. Achieving Culture Change: January 2008 – A Discussion Paper by the Strategy Unit. London Prime Minister Strategy Unit; 2008.
- National Health Service Blood and Transplant (NHSBT) . Laura, Cornea Transplant Recipient n.d. https://www.organdonation.nhs.uk/helping-you-to-decide/personal-stories/how-organ-donors-change-lives/laura-cornea-transplant-recipient/ (accessed August 2022).
- National Health Service Blood and Transplant (NHSBT) . Someone Gave Me the Gift of Sight n.d. https://en-gb.facebook.com/nhsorgandonor/videos/give-the-gift-of-sight/273381224869291 (accessed November 2021).
- Cacioppa JT, Petty RE, Kao CF, Rodriguez R. Central and peripheral routes to persuasion: an individual difference perspective. J Personal Adn Soc Psychol 1986;51:1032-42. https://doi.org/10.1037/0022-3514.51.5.1032.
- NHS Blood and Transplant . Organ and Tissue Donation and Transplantation Activity Report 2020 21 2021. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/23461/activity-report-2020-2021.pdf (accessed July 2021).
- Potenza R, Guermani A, Peluso M, Casciola A, Ginosa I, Sperlinga R, et al. Effectiveness of an education program on donation and transplant aimed at students of the nursing degree course. Transplant Proc 2015;47:2097-101. https://doi.org/10.1016/j.transproceed.2014.11.074.
- Witjes M, Jansen NE, Van Der Hoeven JG, Abdo WF. Interventions aimed at healthcare professionals to increase the number of organ donors: a systematic review. Crit Care 2019;23. https://doi.org/10.1186/s13054-019-2509-3.
- Matesanz R, Domínguez-Gil B. Opt-out legislations: the mysterious viability of the false. Kidney Int 2019;95:1301-3. https://doi.org/10.1016/j.kint.2019.02.028.
- JBI Manual for Evidence Synthesis. Adelaide, SA: JBI; 2020.
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467-73.
Appendix 1 EDiPPPP scoping review search strategy
Review question: The question guiding the review was: What are the evidenced barriers and facilitators to ED in hospice and palliative care settings?
Review objectives
-
Objective 1: To systematically map the current international evidence base relating to ED in hospice and palliative care settings.
-
Objective 2: To identify the factors that are evidenced as informing or influencing the option of ED being discussed with service users in hospice and palliative care settings.
Methodology: Scoping review methodology was adopted in order to identify the scope, coverage and type of research currently available on a topic, map the available evidence and generate a synthesis of the available knowledge. 98
Design and conduct of this were informed by the Joanna Briggs Institute (JBI) framework for scoping review98 and the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR). 99
Inclusion criteria
The inclusion/exclusion criteria were developed in line with the JBI framework clarifying the Population (P) Concept (C) and clinical Context (C) (PCC), type of evidence sought and other limiters within which the search was bounded (see Table 1).
Appendix 2 EDiPPPP scoping review inclusion/exclusion criteria
Evidence searching
Search strategy development
| Component | Inclusion | Exclusion |
|---|---|---|
| Population | Patients (donor, deceased donor and potential donor) Carers (relative, NoK, family member and informal carer) Members of the public Healthcare professionals (physician, doctor and nurse) |
Children, young people and adolescents |
| Concept | Barriers and facilitators to eye tissue donation (perceptions, preferences, practice, potential, views, attitudes, beliefs, experience and knowledge) | Organ, body, egg, sperm donation and surgery to the eye |
| Context | Hospice and palliative care settings | Acute care areas, for example intensive care units, critical care units, emergency departments, eye banks, process of retrieval, storage and treatment of eye tissue |
| Type of study | Empirical research, clinical guidelines, expert opinion, letters to editors, initial reporting of findings and literature reviews | |
| Language | Full article in English language | Non-English language |
| Year of publication | 1983–2020 |
An initial search of PubMed was conducted using the terms ‘Eye [Medical Subject Heading (MeSH)] AND Tissue Donation [MeSH]’. The search was limited to articles published during or after the establishment of the UK Corneal Transplant service. Results (190 articles) did not include several key articles known to the review team, and therefore a set of 23 verified articles which met inclusion criteria (the development set) and were compiled and checked for indexing in PubMed. Of these, only five (28%) were retrieved by the initial search, and further exploration of PubMed indices was undertaken to identify reasons for non-retrieval and inform search strategy development.
Investigations revealed that 17 of 18 development set articles were not retrieved by the initial search as they were not indexed under the MeSH term ‘Eye [MeSH]’, despite six including eye-related terms in the title and/or abstract. The remainder contained eye-relevant material in the full text, but not in the title, abstract, keywords or other metadata visible to searches. As the lack of consistency in indexing of eye-related studies was found using MeSH terms, further searches only applied plain text and Boolean operators.
Final agreed search terms were repeated across five additional databases returning a total of 4322 records from all sources (see Table 2).
Appendix 3 EDiPPPP scoping review final search strategy and results by database
| Final search terms | ||
|---|---|---|
| (Eye OR cornea* OR ocular) AND (donat* OR donor*) NOT ‛eye drop*’ NOT acqueous NOT genetics NOT histology* NOT membrane NOT microscopy NOT MRI NOT oculoplast* NOT oocyte NOT endotheli* NOT keratoplat* | ||
| Database | Results | Limits applied |
| PubMed | 3602 | Species: Humans |
| CINAHL | 141 | Exclude MEDLINE records |
| Embase Classic+Embase | 288 | Exclude MEDLINE records |
| PsychInfo | 186 | None |
| Epistemonikos | 34 | No PMC (PubMed) |
| Cochrane reviews | 71 | None |
| Total records retrieved | 4322 | |
Selecting the evidence
Screening and selection of retrieved records is described using the PRISMA-ScR framework99 (see Prisma Figure 1). Following duplicate removal (n = 206 of 4322 records), 4116 records were exported to Microsoft Excel for title and abstract review. This resulted in exclusion of 3984 additional articles, with 132 proceeding to full-text review. The reference lists of these 132 articles were hand-searched, resulting in 8 additional articles identified for full-text review undertaken by two authors (BMS and MJB), with disagreements resolved by a third reviewer (TLS).
Appendix 4 Study selection – Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Following full paper review, 127 articles (of 140) were excluded, of which 14 records did not relate to ED (i.e. lacking a significant focus on, or containing only incidental references to ED); 28 did not relate to any of the ‘perceptions, preferences, views, attitudes, beliefs, experience, knowledge’ elements of our PCC criteria; and 85 did not indicate coverage of HC or HPC contexts. Thirteen records met inclusion criteria and were included in the final review.
Extracting the evidence
Authors, aims/purpose; study design/methodology, participants/sample size, method of data collection and analysis, findings and limitations were extracted from the final 13 records (see Table 3).
Charting the evidence
Thirteen records that met the inclusion criteria were exported to ATLAS.ti 839 for management and analysis. Articles were analysed in line with review objectives.
Appendix 5 EDiPPPP scoping review data extraction summary
| Study references, country, context | Aims/purpose | Study design, participants | Data collection and analysis methods | Findings |
|---|---|---|---|---|
| Wells J, Sque M. ‘Living choice’: the commitment to tissue donation in palliative care. Int J Palliat Nurs 2002;8:22–7. United Kingdom, Palliative care setting64 |
To explore how nurses and doctors feel about tissue donation in palliative care | Grounded theory study HCPs (n = 8) |
Data collection: Semistructured interviews Data analysis: Grounded theory analysis |
Patients in palliative care should have the opportunity to be consulted about their wishes and expect to be informed and consulted about tissue donation. However, in units where donation was routinely discussed, participants generally consulted relatives rather than patients resulting in concerns that patients were not involved in decision-making. Patients or family members ‘openness’ to discussing end-of-life planning led to HCPs being more comfortable raising the option of donation. |
| Discussing donation should be a multiprofessional role. Timing of the discussion is crucial to the outcome. A main concern was whether the request for donation and the donation process would cause the patients and families any physical or psychological harm. |
||||
| Carey I, Forbes K. The experiences of donor families in the hospice. Palliat Med 2003;17:241–7. United Kingdom, Hospice care setting74 |
To evaluate the experiences, attitudes and feelings of relatives who had consented to the donation of corneas of a loved one within a palliative setting | Semistructured interviews with 12 family members (carers/relatives) | Data collection: Semistructured interviews Data analysis: Framework analysis |
Awareness of eligibility: almost all participants were not aware that their deceased relative was eligible for donation and reported that they would not have reached the decision to donate on their own. Participants stated that they would have been distressed if they had not been given the option to donate and later realised, they could. Raising the topic of ED: discussions were initiated by nurses generally after the death of the patient. The timing and approach were acceptable to families although they felt it would have been easier If they had known participant’s views of ED beforehand. Most participants felt that donation was right and had a positive experience with the process and felt they had done something worthwhile. |
| Social policy: 10 participants stated that the patient should make the decision about donation. All participants felt that there should be publicity and discussion about organ donation preferably before the person was faced with incurable disease or imminent death. |
||||
| Gillon S, Hurlow A, Rayment C, et al. Obstacles to corneal donation amongst hospice inpatients: a questionnaire survey of multidisciplinary team member’s attitudes, knowledge, practice and experience. Palliat Med. 2012;26:939–46. United Kingdom, Hospice care setting34 |
To explore the attitudes, knowledge, practice and experience of corneal donation from hospice staff with direct clinical contact with patients | Survey shared with 704 clinical multidisciplinary team members in 12 hospices | Data collection: paper questionnaire with fixed response and free-text option Data analysis: descriptive statistics and thematic analysis of free text comments |
70% (n = 291/418) of respondents perceived corneal donation to be a rewarding opportunity for patients and/or their families. 88% (n = 375/425) stated it was important that patients knew that they could donate. 43% (n = 118/427) (43%) indicated that corneal donation should be discussed routinely with eligible patients. 17% (n = 72/418) felt that discussing corneal donation would be too distressing for a patient and/or their family. 37% (n = 156/422) were not sure whether they were comfortable enough to start a conversation about corneal donation with a patient or a family member. |
| 34% felt that it was part of their role and 39% (n = 161/421) felt that it was someone else’s role to raise the issue of corneal donation with patients and/or their family members. 93% (n = 399/431) rarely or never raised the option of ED. Key reasons for not engaging in discussions were: Concerns about the impact of the discussion on patients and families A belief HCPs lacked essential knowledge, about the process of ED. A perception that donation is not part of hospice culture. |
||||
| Kuo S, Chou P, Liao Y, et al.: Perspectives of decision-making for corneal donation: a qualitative research among cancer patients. Omega J Death Dying 2018;0:1–8. Taiwan, Palliative care setting75 |
To identify the views of terminal cancer patients towards corneal donation | Exploratory qualitative study with 25 cancer patients | Data collection: Semistructured interviews Data analysis: content analysis |
Key findings were that: Participants felt that the issue required family members to indicate their preferences. Participants preferred to maintain their bodies intact because of the deeply held beliefs that the body must remain intact after death. Participants believed that corneal donation was against their Buddhist religious beliefs as they believe that the body should be untouched for eight hours after death. Participants also believe that spirit should be able to see and, therefore, eyes should not be removed. |
| Walker L, Neoh K, Gilkes H, Rayment C. A qualitative study using semistructured interviews of palliative care patients’ views on corneal donation and the timing of its discussion. Palliat Med 2018;32:1428–37. United Kingdom, Palliative care setting73 |
To understand views and feelings of patients in palliative care settings towards corneal donation | Exploratory qualitative study with nine patients | Data collection: Semistructured interviews Data analysis: Thematic analysis |
Patients’ baseline knowledge was very limited, and most did not know anything about corneal donation before the study. Altruism was a key influence; patients felt positive about being able to help someone else. Eyes were not perceived as being different to other organs and participants valued sight and felt it would be important to help someone see again. All participants acknowledged the role played by their family in decision-making and were keen to involve them. Participants felt they would prefer to talk about donation when they were well rather than when vulnerable and close to death. |
| Participants felt discussions about donation were a covert way to tell someone that they were dying. Participants were open to discussing donation with healthcare professionals and felt it would be easier with someone they already had relationship with. Although participants said they did not know anything about donation, they, however, felt they would not be eligible to donate. Some thought they could pass on their cancer if they donated. |
||||
| Ng I, Astle J, Tregenna E, et al. Improving corneal donation rates: a three-phase analysis of professional and patient factors. Future Healthcare J 2019;6:s1:38. United Kingdom, Hospice care setting65 |
To assess factors that influence corneal donation within the palliative care service | Survey of 37 HCPs and 11 patients Retrospective note review of 84 deceased patient records 2016 |
Data collection: Retrospective note review Questionnaire (developed by Gillon et al.) distributed to healthcare providers in 2014. Questionnaire to patients admitted to the service between June and August 2015. Data analysis: descriptive statistics |
Results of retrospective note review: 85 deceased patients’ notes were reviewed against eye donation criteria. Of these, 35% (n = 30) were judged to be eligible for corneal donation with a further 11% (n = 10 patients) potentially eligible. Results of survey healthcare professionals: 92% (n = 92) of respondents never or rarely raised the subject of corneal donation with patients or relatives. 76% (n = 76) of respondents had not received any information or training regarding corneal donation. 81% (n = 81) of respondents felt they did not know enough about corneal donation to discuss it with patients or relatives. Knowledge and training were identified as significant barriers to raising these discussions. |
| Results of questionnaire with inpatients: 6/11 (54.5%) participants had not heard of corneal donation, and all were either glad or neutral about being informed about corneal donation. 8/11 (73%) participants did not find it upsetting to discuss corneal donation and the remaining 3/11 (27%) indicated although they found it upsetting, they would rather have a conversation than not. Patients’ decisions about donation changed after discussions of ED. Before discussion, none of the patients were planning to donate their corneas, whereas after the discussion, 7/11 (64%) were planning to donate. |
||||
| Niday P, Painter C, Peak J, et al. Family and staff responses to a scripted introduction to tissue donation for hospice inpatients on admission. Prog Transplant 2007;17(4):289–94. USA, Hospice care setting66 |
To implement and evaluate a change in practice to offer information about tissue donation as part of admission process | Service evaluation-written logs of 12 healthcare providers | Data collection review of nurses’ logs | Comments on nurses’ logs indicated no concerns from patients and families to receiving information about donation at admission. There was less frustration from families at the time of death and introduction of donation Nurses were more positive about introducing the option of donation at admission compared with when donation was introduced at the time of death. Nurses’ logs confirmed that patients and families were not aware that they could donate. Corneal donation increased by 250% during a 6-month period from 2 out of 32 eligible corneal donors to 7 out of 34 eligible donors. |
| Tredgett K, Ward-Davis L. Responding to the public’s voice: changing cornea donation practice in a hospice (Letter to the editor). BMJ Support Palliat Care 2017;9(1):112–3. United Kingdom, Hospice care setting68 |
Service evaluation of the introduction of personalised plan of care for dying patients that included the option for tissue and organ donation | Service evaluation reporting outcome of retrospective note review, staff survey of 14 HCPs Telephone interviews with five family members |
Data collection: questionnaire with HCPs Retrospective note review Telephone interviews with family members of deceased hospice inpatients Data analysis: Descriptive statistics |
Findings from questionnaire with HCPs 12/14 (86%) of doctors felt that discussing eye donation did not cause additional distress to patients. 8/14 (57%) of doctors reported that the discussions had been helpful to patients and families as donation provided an opportunity to give something back and enabled a positive outcome from the death. Note review: On average, 240 deaths occurred each year at this hospice. Before 2015, no patients had been referred for ED. 67/77 (87%) were eligible to donate. 34/67 (51%) of eligible patients’ relatives were approached about donation before the patient’s death. |
| 15/34 (44%) of those invited to consider donation subsequently donated their corneas. Reasons for non-discussion of eye donation: Speed of deterioration, concern about exacerbating already significant distress and lack of clinician clarity on eligibility criteria were common reasons. Reasons for declining donation: Previously expressed wish by patient not to donate or family’s uncertainties about the patient’s wishes were reasons for decline. Findings from telephone interviews: Interviews with relatives of the deceased indicated that relatives felt it was acceptable to raise the option of donation and felt that it did not add to their distress. |
||||
| Roach R, Broadbent AM. Eye donation in Sydney metropolitan palliative care (Letter to the editor). J Palliat Med 2010;13:121–3. Australia, Palliative care setting48 |
To identify factors contributing to low rate of ED from palliative care unit in Sydney metropolitan area | Retrospective audit of 2000 deceased patient records | Data collection: Retrospective note review Data analysis: Descriptive statistics |
Two thousand deceased patients’ notes were reviewed over a 1-year period. Fifty (2.5%) patients became eye donors. Donors came from only four out of the nine palliative care units (44%). Two (22%) units provided 90% (n = 45) of the EDs. Palliative care units do not appear to discuss or promote ED with patients or their families. |
| Gillon S, Hurlow A, Rayment C, et al. Eligibility for corneal donation within the hospice population (Letter to the editor). Palliat Med 2010;24(5):551–2. United Kingdom, Hospice care setting67 |
To quantify percentage of inpatients eligible to donate corneas and number with whom donation is discussed | Observational retrospective note review of 100 deceased patient records (September–December 2008) | Data collection: patient note review Date analysis: Descriptive statistics |
One hundred deceased patients’ notes were reviewed. There were no contraindications to ED for 52 patients (52%), whereas 15 (15%) had definite contraindications. No documentation regarding discussion of corneal donation was recorded. |
| Stiel S, Hermel M, Radbruch L. Cornea donation from patients deceased at a palliative care unit (Letter to the editor). Palliat Med 2011;25(2):183–4. Germany, Palliative care setting56 |
To assess the potential for corneal donation and the relative rate of actual donation | Observational retrospective note review of 704 deceased patient records | Data collection: Review of patient electronic records Data analysis: Descriptive statistics |
704 deceased patients’ notes were reviewed between 2003 and 2009. 229/704 (32.5%) patients were potential donors. 112/704 (49%) patients gave consent for cornea donation. |
| Edwards P.Corneal donation within palliative care: a review of the literature. Int J Palliat Nurs 2005;11(9):481–6. United Kingdom, Palliative care setting58 |
To examine whether the option of donation is being offered in a systematic manner To explore the moral dilemmas involved in corneal donation and the implications for nursing practice and research |
Literature review in MEDLINE and CINAHL databases | Data collection: Review of studies covering period 1995–2005 Data analysis thematic analysis |
Findings from literature review: Corneal donation is rarely offered. Cumulative findings indicated that family members were surprised that their relative could donate. Family members would have been distressed if they had not been offered the option to donate and found out later that this could have been an option; low numbers of family members raise the issue of ED. |
| Families felt that donation did not have any effect on their bereavement. Family members desire to fulfil deceased wishes, give meaning to the death and the families’ own views about donation influenced donation decisions. Healthcare professionals often do not raise the issue of corneal donation, often they just respond to requests by patients or family members. |
||||
| Spencer M. The barriers to organ and tissue donation in palliative care. End Life J 2012;2:1–11. United Kingdom, Palliative care setting71 |
To explore the involvement of palliative care patients in decisions about donating their tissues. To explore why families may be reluctant to consent to donating organs/tissues of deceased loved ones. To explore why nurses are wary of discussing the possibility of donation with patients and/or their NoK |
Literature review in British nursing index, CIHAHL, MEDLINE, EMBASE and PsycINFO | Data collection: Review of the literature with no date limits Data analysis Thematic analysis |
Findings from literature review: There is no consensus among palliative healthcare professionals about whether and/or when patients should be involved in discussions about donation. Patients often spontaneously discuss end-of-life matters such as their funeral arrangements, their will and expectations for the time they have left, but they rarely spontaneously discuss organ or tissue donation. Introducing donation discussions increased donation rates. Patients should be given appropriate information to enable them to make choices about donation. |
| Knowing the wishes of the deceased regarding donation influences NoK donation decision-making. Healthcare professionals find it challenging to talk about donation even though they frequently have difficult discussions about death and dying. HCPs are fearful of the reaction of patients and families to the request for donation. The attitudes of healthcare providers influence their practice, those with negative views and less knowledge about donation are less likely to discuss it compared with those who are positive and have more knowledge. |
Appendix 6 Eligibility Eye Donation Assessment Checklist
This is version 2 of the model eligibility screening tool developed from the assessment criteria used in the EDiPPPP notes review (WP1S1).
This tool is intended to support screening of patient suitability for referral to NHSBT-TES for the purpose of determining eligibility for donation of eye tissue.
Please answer the questions below, and the tool will return a result indicating whether the patient may or may not be eligible for ED.
Contraindications (malignancies)
Please indicate below whether any of the following contraindications are present.
Leukaemia
-
⃝ Yes
-
⃝ No
Lymphoma
-
⃝ Yes
-
⃝ No
Myeloma
-
⃝ Yes
-
⃝ No
Brain malignancy with ocular involvement
-
⃝ Yes
-
⃝ No
Retinoblastoma
-
⃝ Yes
-
⃝ No
Malignant tumours of the anterior segment of the eye
-
⃝ Yes
-
⃝ No
Contraindications (intrinsic eye disease)
Please indicate below whether any of the following contraindications are present.
Corrective laser surgery (if aged under 55 years at death)
-
⃝ Yes
-
⃝ No
Contraindications (neurodegenerative disorders)
Please indicate below whether any of the following contraindications are present.
Creutzfeldt–Jakob disease (CJD) or other prion disease
-
⃝ Yes
-
⃝ No
Diagnosed Parkinson’s disease
-
⃝ Yes
-
⃝ No
Diagnosed Alzheimer’s disease
-
⃝ Yes
-
⃝ No
Recent onset of memory loss
-
⃝ Yes
-
⃝ No
Disease of unknown aetiology
-
⃝ Yes
-
⃝ No
Contraindications (infections)
Please indicate below whether any of the following contraindications are present.
Current viral hepatitis (B, C or E)
-
⃝ Yes
-
⃝ No
HIV infection
-
⃝ Yes
-
⃝ No
Contraindications (other)
Please indicate below whether any of the following contraindications are present.
Previous organ transplant
-
⃝ Yes
-
⃝ No
Any recorded IV drug use in the past 12 months
-
⃝ Yes
-
⃝ No
Referral to NHSBT recommended
Based on the information provided, this patient is suitable for referral to NHSBT for further assessment of eligibility for eye donation. You can do this via [ENTER CONTACT INFORMATION]
Referral to NHSBT Not Recommended
Based on the information provided, this patient is not suitable for referral to NHSBT for further assessment of eligibility for eye donation. However, if you feel further information or clarification is required, you can contact NHSBT via [ENTER CONTACT INFORMATION]
This content is neither created nor endorsed by Microsoft. The data you submit will be sent to the form owner.
Appendix 7 Organisational Readiness for Eye Donation Assessment Checklist
[INSERT INSTITUTION name and logo]
Healthcare Professionals Online Survey for staff at [INSERT INSTITUTION]
* Required
Consent for participation
-
Please tick (check) this box to indicate that you consent to taking part in this survey.*
-
⃝ I agree to participate in this survey
-
Demographics
The following questions are about you and your role.
-
What is your age?*
-
⃝ 30–39
-
⃝ 40–49
-
⃝ 50–59
-
⃝ 60–69
-
⃝ 69+
-
⃝ Prefer not to say
-
-
Please indicate if you identify as:*
-
⃝ Female
-
⃝ Prefer not to say
-
-
Please indicate which ethnic group you most identify with*
-
⃝ White British
-
⃝ White Irish
-
⃝ Other white
-
⃝ White and Black Caribbean
-
⃝ White and Black African
-
⃝ White and Asian
-
⃝ Other mixed Indian
-
⃝ Pakistani
-
⃝ Bangladesh
-
⃝ Other Asian
-
⃝ Prefer not to say
-
⃝ Don’t know
-
-
What is your current role?*
-
How many years have you worked in palliative or hospice care settings? Please indicate number of years below.*
Perceptions
Questions in this section ask about your views towards organ and tissue donation in general, and eye donation in particular.
-
Are you currently registered to be an organ/tissue donor?*
-
⃝ Yes
-
⃝ No
-
⃝ Prefer not to say
-
-
Have you stipulated any organs and/or tissues that you do not want to donate?*
-
⃝ Yes
-
⃝ No
-
⃝ Prefer not to say
-
-
If yes, please indicate below which organs or tissues you have indicated that you do not want to donate.*
The following questions are about how you feel about ED.
Please indicate whether you agree or disagree with the following statements.
-
Discussing ED is too distressing for a patient and/or their family*
-
⃝ Agree
-
⃝ Not sure
-
⃝ Disagree
-
-
I feel confident in starting a conversation about eye donation with a patient and/or their family*
-
⃝ Agree
-
⃝ Not sure
-
⃝ Disagree
-
-
Eye donation should be discussed routinely with eligible patients and/or their families*
-
⃝ Agree
-
⃝ Not sure
-
⃝ Disagree
-
-
It is not my role to raise the option of ED with patients and/or their families*
-
⃝ Agree
-
⃝ Not sure
-
⃝ Disagree
-
-
It is important that patients know that they may be eligible for ED*
-
⃝ Agree
-
⃝ Not sure
-
⃝ Disagree
-
-
I am concerned about how patients and/or family members might respond to the option of ED being raised with them*
-
⃝ Agree
-
⃝ Not sure
-
⃝ Disagree
-
-
If you wish to add any comments regarding how you feel about the option of ED, please use the space below.
Practice
The following questions are about your knowledge and current practice relating to the option of ED as part of EoLC.
-
Are you aware that ED is an option that patients can choose as part of advance care/EoLC planning?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
Does your clinical setting actively encourage the option of ED being discussed with patients and/or their families?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
Do staff within your clinical setting routinely discuss the option of ED in meetings (e.g. team, case conference, MDT)?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
Do staff within your clinical setting routinely discuss the option of ED in EoLC planning conversations with patients and/or family members?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
Does your service routinely check the ODR status of patients at the point of admission?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
Does your clinical setting have clinical guidelines in written form that include ED?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
Does your clinical setting have information in written form that staff can refer to if ED is raised by a patient or family member?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
Does your clinical setting include ED in its admission documentation?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
Which of the following best describes your current practice?
-
⃝ I never discuss ED with patients or families
-
⃝ I discuss ED only when the subject is raised by patients or families
-
⃝ I routinely discuss the option of donation with patients and families
-
-
At what point in a patient’s care should the option of ED be discussed? (Please select all that apply.)
-
Before admission
-
During admission
-
At first assessment by palliative care services
-
During in-patient stay
-
During advanced care planning
-
Never
-
-
How many times in the past year have you raised the option of ED with a family member?*
-
⃝ 0
-
⃝ 1–5
-
⃝ 6–10
-
⃝ 11–15
-
⃝ 15–20
-
⃝ More than 20
-
-
Reflecting back on the last time you discussed ED with a patient and/or relative, how did you feel having that conversation?
-
⃝ I have never discussed ED with a patient or family member
-
⃝ Somewhat uncomfortable
-
⃝ Very uncomfortable
-
⃝ Neither comfortable nor uncomfortable
-
⃝ Somewhat comfortable
-
⃝ Very comfortable
-
-
If you have had a discussion with a family member, was this discussion pre or post death of the patient? (Please select all that apply.)
-
Pre death
-
Post death
-
I have not had a discussion with a family member
-
-
Who do you think should raise the issue of ED with a patient or family member? (Please select all that apply.)
-
It is my role
-
The GP should have this conversation
-
The Consultant referring the patient to Palliative Care
-
Other palliative care specialist (e.g. CNS)
-
A donation specialist
-
All of the above
-
-
Is there a donation link person or champion in your service?
-
⃝ Yes
-
⃝ No
-
⃝ Don’t know
-
-
If yes, what is the position of the link person or champion in your service?
-
Please indicate your response to the following statement:
-
⃝ True⃝ False⃝ Unsure
-
Under current legislation in England, everyone is ‘deemed’ to agree to being a donor (organ, tissue, eye) unless they opt out.
-
-
Have you received any information regarding the move to opt-out legislation? (e.g. from [INSERT INSTITUTION], or from other bodies such as NHS Blood and Transplant)
-
⃝ Yes
-
⃝ No
-
Preferences
The following questions are about provision and needs relating to knowledge and training about ED.
-
Have you received any in-service training about ED?*
-
⃝ Yes
-
⃝ No
-
-
Who provided the training?*
-
⃝ [INSERT INSTITUTION]
-
⃝ Other
-
-
How long ago did you undertake the training?*
-
⃝ In the last 6 months
-
⃝ 6–12 months ago
-
⃝ 13–24 months ago
-
⃝ More than 24 months ago
-
-
Did the training provide you with the information you needed to be confident in discussing ED with patients/family members?*
-
⃝ Yes
-
⃝ Somewhat
-
⃝ No
-
-
If you feel that you have unmet knowledge or training needs relating to ED, please describe these below
-
(If none, please enter ‘none’)*
-
-
Do you know where to find out information about ED if you need to?*
-
⃝ Yes
-
⃝ No
-
-
Please describe below the information currently available to you regarding ED (e.g. policies and procedures, information for patients and families, etc.) (If unsure, please write ‘unsure’)
-
Please indicate below where this information about ED is held in your organisation (if unsure, please write ‘unsure’)*
Thank you
We appreciate you taking the time to complete this survey.
For any questions about the survey, please contact: m.j.bracher@soton.ac.uk
When you are ready to complete, please click the ‘Submit’ button below.
This content is neither created nor endorsed by Microsoft. The data you submit will be sent to the form owner.
Microsoft Forms
Appendix 8 Transparent Expert Consultation interim findings report
EDiPPPP Interim Findings Summary Full (22 June 2021)
HCPs n = 105 (HC n = 50; HPC n = 55)
Potential
Notes review
Eight hundred and sixty-two records reviewed by PIs and peer-evaluated thus far.
Four hundred and ninety-seven records HC; 365 records HPC.
Of these, 723 results have consensus between PI and peer evaluator (PE; 84% agreement rate).
Eighty per cent agreement HC (n = 396); 90% agreement HPC (n = 327).
Of the agreed results, 51% (n = 371) of patients were assessed as eligible for eye donation.
Fifty-eight per cent agreed eligibility HC (n = 228); 44% agreed eligibility HPC (n = 143).
Practice
Barrier: knowledge and resources to support assessment of eligibility are not readily available, either locally or nationally (though in many cases believed to be – e.g. NHSBT website, trust intranet).
Notes review
In 226 cases (19% of total), PIs reported being unsure of eligibility for eye donation [128 HC cases (21%) and 98 HPC cases (16%)]:
-
Of these 226 cases, most common areas of uncertainty included:
-
eye damage or disease (acquired or intrinsic) 19% (n = 42) of cases
-
age cut-off for eligibility 18% (n = 41) of the cases
-
brain malignancies 6% (n = 13) of the cases.
Of 862 records reviewed by both PIs and PEs, there was disagreement regarding eligibility for ED in 139 (16%) cases:
-
Of these 139 cases, the main reasons for disagreement include:
-
PI exclusion where PE has indicated patient is a candidate for ED based on information provided (23% of disagreements, n = 32)
-
PI exclusion based on history of eye surgery where PE indication that this is not a contraindication per se and/or that more information would be needed to confirm (12% of disagreements, n = 17)
-
analysis of free-text comments indicating ambiguity in the degree of certainty needed to determine eligibility at the site level (i.e. how certain those screening at sites need to be based on the evidence they have, before referring to NHSBT).
Interviews
-
A majority of both strategic/managerial and front-line participants [65% (n = 13) of interview participants and 88% (n = 15) of focus group participants] across all role groups and levels were not aware of standard criteria for ED, and/or able to indicate where relevant information may be accessed.
ʻAgain, that is something I wouldn’t specifically know, and I think that is something we would all need to know to be able to pass this information forward ….
(Front-line HCP – HCPL00605)
National Survey
-
Majority of participants across both HC (61%, n = 62) and HPC (68%, n = 31) did not have or were unsure about the existence of clinical guidelines regarding eligibility or ED process within their institution [Q25].
Barrier: Raising of the topic of eye donation by HCPs is infrequent (despite eligibility)
Notes review
-
ED is recorded as being raised with the patient in only 4% (n = 24) of cases and with family members in 1% of cases assessed as eligible in the note review (n = 588).
Interviews
-
ED is not routinely raised by HCPs or patients or across services.
ʻNot routinely … Not routinely … We have information in, well, you could say routinely, we have information in our, in our patient booklet that we give out in the (anonymised location) and on the ward when somebody has contact with us and there is information in there about donation … But we wouldn’t leave the leaflets lying around on the ward.
(Strategic/Managerial HCP; HCPI00101)
ʻI recognise the importance of it, I think I haven’t yet found a way of prioritising it or found a way of finding a script that feels kind of acceptable to either myself or patients. I suppose the only time I engage in conversations around organ donation or were it to be eye donation would be if a patient or relative brought it up, not that I initiate that conversation …. Things that are almost mandatory that I feel I really need to talk about and make sure that there are certain things in place to support the patient or relative as that person is approaching end of life. And maybe organ donation doesn’t fit into that neatly for me or I haven’t found a way of prioritising it or making it fit, is my assessment to date if that makes sense.
(Front-line HCP; HCPL00103)
National Survey
-
Forty-eight per cent (n = 63) of participants indicated that their service did not actively encourage the option of ED being discussed with patients and/or their families (48% HC participants and 47% HPC participants).
-
Seventy-two per cent (n = 95) of participants indicated that the option of ED is not routinely discussed in EoLC planning conversations with patients and/or family members within their service (67% HPC participants and 75% HC participants).
-
Sixty-one per cent (n = 81) of participants indicated that their clinical setting did not include ED in its admission documentation (71% HPC participants and 56% HC participants).
-
Sixty-six per cent (n = 54) of participants indicated that they either never discussed ED with patients or families (22%) or only when raised by patients or families (44%).
-
Sixty-six per cent (n = 99) of total participants rated ‘healthcare provide[r] reluctance to discuss the option of ED due to concerns that they will cause distress’ in the highest quartile of five-point scale.
Barrier: Many participants unfamiliar with processes for referral for ED (to NHSBT)
Interviews
-
Fifty-two per cent (n = 33) of interview participants were unsure of the process in referring a patient to NHSBT [for HPC – 42% (n = 14) and HC – 63% (n = 19)].
-
Forty-four per cent (n = 17) of interview participants with a front-line role indicated that they would like more information on retrieval processes to support ED conversations with patients and families [for HPC – 55% (n = 11) and HC – 32% (n = 6)].
ʻWell, I would say that would be in the hands of the tissue donation team or the eye team, I’m sure what the team, is that specific, I don’t know if they’ve got a specific eye team name, that’s a gap in my knowledge. So, I would say that obviously, the team would be contacted to say that, you know, the person had died, and would they come and, you know, and to do the, to take donation.
(Strategic/Managerial HCP; HCPI00401)
Barrier: Donation options are not regularly discussed in team meetings.
Interviews
-
Sixty-one per cent (n = 23) of interview participants with front-line roles indicated that ED conversations are not currently part of team meetings within their service [HPC – 72% (n = 13 front-line participants) and HC – 50% (n = 10 front-line participants)]. Front-line HCPs also indicated that ED was not discussed in staff meetings.
ʻWhereas occasionally it comes up in MDT in, we have a weekly MDT with consultants and registrars and things and occasionally it’ll come up, but only if it’s a specific thing like a patient that wants their body to be given to medical science or something because there are special papers for that so that’s the only time that anything like that would get brought up that I would know about. But no, it’s not, we don’t have any training or education about it at all.
(Front-line HCP; HCPL00303)
National Survey
-
Eighty-three per cent (n = 109 participants) reported that the option of ED is not routinely discussed in meetings within their service (e.g. team, case conference or multidisciplinary team meetings).
Barrier: HCPs do not have or are unaware of who key people are within their organisation (note: exception was ITU respondents in HPC settings, where local SNODS were indicated).
Interviews
-
Fifty per cent (n = 19) of participants with strategic or managerial roles could not identify a key person or champion for ED within their service.
National Survey
-
Eighty-two per cent (n = 128) of participants reported not having, or being unaware of having, a donation link person or champion within their service.
Barrier: Majority of participants have not had training relating to ED from any source (e.g. own service, NHSBT); majority of those who had did so before November 2019.
Interviews
-
Seventy-nine per cent (n = 30) of participants with a strategic or managerial role could not identify ED training being offered to staff within their institution [HPC – 78% (n = 14 participants) and HC – 80% (n = 16 participants)]
-
Thirty-eight per cent of front-line interview participants reported lack of knowledge on ED processes that would be relevant to discussing the option of ED with patients and/or families.
National Survey
-
Sixty-one per cent (n = 95) of total participants had not received any training regarding ED from any source [HPC – 57% (n = 33 participants) and HC – 63% (n = 62 participants)].
-
Of participants who had received training (n = 61), 82% (n = 50) had completed training 13–24 months prior to completion of the survey.
-
Forty-eight per cent (n = 72) of participants rated ‘healthcare providers lack knowledge in what needs to be done to organise eye donation’ in the highest quartile of a five-point scale.
-
Thirty-one per cent (n = 49) of participants provided a free-text comment indicating that education and support for CPD were ‘key barriers to ED’ (HPC – 22% participants and HC – 37% of participants).
Perceptions
Barrier: HCPs perceive that failure to embed ED processes within routine practice in EoLC is a key barrier to increasing donation rates
National Survey
-
Seventy-six per cent (n = 115) of participants rated ‘option of ED is not ‘embedded’ as a routine part of EoLC clinical practice’ in the highest two categories when responding to questions regarding barriers to ED.
-
Sixty-three per cent (n = 99) of participants agreed with the statement ‘ED should be discussed routinely with eligible patients and/or their families’ – most other answers fell in the ‘not sure’ category.
-
Seventy-three per cent (n = 114) of participants disagreed with the statement ‘Discussing ED is too distressing for a patient and/or their family’.
-
Fifty per cent (n = 78) of participants agreed with or were unsure regarding the statement ‘I am concerned about how patients and/or family members might respond to the option of ED being raised with them’.
-
Eighty-four per cent (n = 131) of all national survey participants were aware that ED is an option that patients can choose as part of advance care/EoLC planning.
Barrier: Multiple Electronic Patient Record Systems (EPRS) (e.g. SystemOne, eCare) exist with varying degrees of support for recording and retrieval of information relating to ED – these vary between sites and across pathways (e.g. between GP, hospital and hospice services within the same pathway).
Interviews
Both HC (n = 1) and HPC (n = 8) participants in interviews or focus groups commented on the capability of EPRS systems – highlighting the variability of these systems across and within institutions, and also for HPC settings that EPRS systems at the user side are often already highly information-saturated (particularly within busy departments such as ED and ITU).
-
One participant within a HPC setting with health informatics experience gave a detailed description of how a hypothetical system could link databases nationally – however, in doing this, they also highlighted the current state of systems across the pathway as highly variable in design, capability and ability to link to other systems/institutions.
National Survey
-
Several (n = 3) free-text comments indicated variability in admission and advanced care planning processes (e.g. some sites entirely on paper, others entirely electronic, others a combination).
Asset: High levels of support for embedding of ED conversations within ACP processes
Interviews
-
Forty-eight per cent (n = 37) of interview participants indicated a preference for conversations to take place earlier in the EoLC pathway, with many (HPC, 58%; HC, 39%) identifying EoLC/ACP conversations as an appropriate point at which to raise the option of ED.
ʻBecause if we’re putting an advanced care plan together, it is obviously an important thing to discuss isn’t it, not just where you want your chosen place of care and death to be if you have that choice. If it, you know, the legislation is that now you have to opt out that your wishes are known that if you didn’t want anything to be donated, I think that is an important part of having them discussions really isn’t it, that’s the time to bring that out.
(Strategic/Managerial HCP; HCPI00205)
National Survey
-
Eighty per cent (n = 125) of participants indicated that ED should be discussed during advanced care planning (81% of HPC participants and 80% of HC participants).
-
Sixty-one per cent (n = 80) of respondents indicated that written information was available to support conversations regarding ED if the issue were raised by a patient or family member.
Preferences
Asset: HCPs support involvement of a range of staff across the EoLC pathway in raising ED conversations with patients/families.
Interviews
-
Sixty-nine per cent (n = 27) of interview participants with a front-line role indicated that knowledge and capacity to raise the option of ED with patients should be available to support them in discussions with patients and family members.
National Survey
-
Sixty-nine per cent (n = 108) of participants indicated that ‘all’ role types should raise the issue of ED with patient or family member (when given a multiple-choice list).
-
Forty-eight per cent (n = 75) of participants provided a follow-up free-text comment emphasising the importance of different members of the palliative care team being able to engage in discussion around the option of ED so that differing patient/familial needs at different stages of the pathway can be met.
Patient interviews n = 35 (HC = 19; HPC = 16)
Potential
-
Ninety-one per cent (n = 32) of patients interviewed were in favour of ED [HC – 94% (n = 15) and HPC – 89% (n = 17)].
-
Ninety-four per cent (n = 33) of patients interviewed indicated that they were in favour of ED being raised with patients receiving EoLC [HPC – 94% (n = 15 participants) and HC – 95% (n = 18)].
ʻI think, it’s something that we really need to do, and I don’t see there’s any point in just wasting things that we could use in research or use to give somebody else a better quality of life.
(P00704)
ʻIt’s making me think, so, no I haven’t got a problem about being asked, if I did, I’d say I’m sorry I don’t want to talk about that.
(P00803)
Practice
-
Ninety-seven per cent (n = 38) of patient interview participants indicated that they were not aware of ED as an option and/or that this had not been raised with them during their current treatment programme.
-
Forty per cent (n = 14) of patients interviewed made a comment indicating that ED should be raised on first contact with services or during ACP processes.
-
Thirty-one per cent (n = 11) of patients indicated that a key consideration in ‘when’ the option of ED should be raised is that the conversation should take place when the patient has ‘mental capacity’.
-
When asked ‘who should raise the issue [of ED]’, patients named a range of HCPs (i.e. individuals such as consultant medics, nurses – or groups such as ‘the palliative care team’).
-
All but one patient indicated that HCPs (rather than patients or families) should raise the option of ED and not rely on the patient or family bringing this up.
Preference
-
Ninety-one per cent (n = 32) of patients interviewed indicated that patients should make the decision about becoming an eye donor, and that their views should take priority (as opposed to family) [HPC – 81% (n = 13 participants) and HC – 100% (n = 19)].
-
When asked how their wishes regarding ED should be recorded, participants provided a variety of answers (e.g. will, DNACPR, ACP, medical notes).
-
However, none were clear about where this information can be held.
ʻI thought like the health profession that would be part of their job to inform, I know they inform patients of everything that’s going on, but for people like myself that are terminal, I’m not deluded, I know what’s coming, you know, although I haven’t got a time, I know what’s coming and I would prefer my nurse or somebody in that profession to approach me to ask me whether I want to donate or not, because then that could be written up on your paperwork without the doctor having to go and ask distressed family members at the time of when they need to go and ask the question. But I don’t, I don’t understand why they’re reluctant to bring it up, maybe it’s because we’re all on a database and all they’ve got to do is go onto the database to check whether you’re still on it for donation, you’ve telephoned to say no, I want, I want you to take me off it, but in my opinion, if that is part of their job then they should be raising the question.
(P00603)
Perceptions
-
Sixty-nine per cent (n = 24) of patient interview participants had no knowledge of ED (i.e. need for, process or benefits of) [SCPS – 63% (n = 10 participants) and HC – 74% (n = 15)].
-
A minority of patients said they had seen something about ED from TV/Magazine and only one participant was aware was well informed of process and benefits.
-
Seventy-one per cent (n = 25) of patient interview participants were unaware of ED as an option for patients receiving EoLC; the majority of those who were aware of this as an option only knew this as a result of being asked to participate in the EDiPPPP study [HPC – 69% (n = 11 participants) and HC – 74% (n = 14)].
ʻNo, I didn’t (know that ED was an option). I thought once you got cancer that were, you might as well as just cut up your donor card.
(P00605)
ʻAbsolutely not, nobody at all, up until N* coming in yesterday to arrange this interview, nobody’s said a single word to me, no. And I’ve been, I’m not. I’m not very often in hospital, but when I’ve been in and obviously this time we are talking, I am heading towards the end, I’m not, I’ve not got five years left anymore, you know, so, but no, nothing has been said at all, maybe it’s not near enough the time yet, I don’t know how close do you need to get. I might have six months, you know, I don’t know.
(P00803)
Prepared by: Bracher, M; Madi-Segwagwe, B; Long-Sutehall, T.
Appendix 9 EDiPPPP TEC Meeting – Education, Training and Awareness (1 July 2021 @ 2 pm)
Note: this report contains interim findings from ongoing analysis.
Role of this report
-
This report is intended to support members of the ETA group in their discussions by providing a summary of key interim findings from the EDiPPPP study, indicating specific areas to inform intervention design.
-
The goal for this group is to identify key areas for organisational, logistical and individual practice change with respect to education and training of HCPs in relation to ED, and public awareness campaigns to inform patients, families and the wider public.
The questions to be answered in this group are:
-
What key activities are necessary to inform education, training and public awareness raising initiatives?
-
For all activities in all domains:
-
What specific content is needed? (e.g. education/training focus points; key public awareness messages)
-
What form should this content take? (e.g. online information, e-learning or in-person training, format of public awareness campaigns)
-
Summary of findings
-
The ‘Summary of Findings’ section of the report provides key points from the larger report (the ‘Interim Findings Summary Full ‘document) and are outlined here to inform group discussion.
-
This arrow symbol highlights recommendations and focus points relevant to discussion of intervention design.
-
-
Sections are ordered by the four ‘P’s of EDiPPPP (potential, practice, preference, perceptions).
Potential
-
High rates of eligibility for ED are present across in both HPC and HC settings.
-
Patients are in favour of ED; however, almost all patient interview participants indicated that they were not aware of ED as an option and/or that this had not been raised with them during their current treatment programme.
-
Evidence from multiple data collection streams indicates that assessment of eligibility, approach to patients/families and referral of eligible patients is low relative to eligibility.
-
Embedding ED conversations in routine care planning is necessary to ensure that patients/families who wish to choose this option are able to do so.
Practice
-
Awareness of criteria for ED eligibility is low across all three data collection streams.
-
Training and resources for HCPs need to clarify contraindications/exclusion criteria.
-
Guidance is needed to clarify the distinction between threshold of evidence needed to refer to NHSBT, and the threshold needed for retrieval to occur (following NHSBT assessment) – to inform ER practice at site level.
-
-
Resources to support assessment of eligibility (e.g. information on contraindications) are not widely available through participants believe this already exists – (e.g. NHSBT website, trust intranet).
-
There is an urgent need for a web-based resource to allow sites to access information to support ER processes.
-
-
Raising of the topic of ED by HCPs with either patients or families is infrequent relative to eligibility rate despite:
-
almost all patients interviewed indicating that they were in favour of ED being raised with patients receiving EoLC;
-
a large number of patients interviewed making a comment indicating that ED should be raised on first contact with services or during ACP processes.
-
Education and training resources should look to explore what organisational or behavioural processes need to be put in place to embed ED discussions in care planning.
-
-
-
When asked how their wishes regarding ED should be recorded, participants provided a variety of answers (e.g. will, DNACPR, ACP, medical notes); however, none were clear about where this information can be held.
-
There is a need to clarify, both for HCPs and patients, how wishes regarding donation can be recorded and retrieved/accessed.
-
-
Access to written information to support discussion about ED with patients and family members is variable across sites and contexts.
-
Context-specific, nationally developed and circulated written materials need to be agreed.
-
-
The majority of participants have not had training relating to ED from any source (e.g. own service, NHSBT); majority of those who had did so before November 2019.
-
There is an urgent need for easily accessible training resources to support ED processes across the pathway.
-
-
Many participants are unfamiliar with processes for referral for ED (to NHSBT).
-
Training and supporting resources needed to clarify referral process for all relevant HCP groups (currently many either do not know or appear to rely on an assumed key person who may or may not exist).
-
-
Participants requested more information on the processes post donation in the context of supporting the family (i.e. information about the impact of eye tissue, contact family would receive from NHSBT after retrieval, etc.).
-
Training/CPD needed to clarify the above and support this information being used in conversations with patients and families.
-
Perceptions
-
Most patients had no knowledge of ED (i.e. as a process, the use and impact of eye tissue) and were unaware that ED was an option for patients receiving EoLC.
-
A large majority of HCP participants do not agree that ED is too distressing to be discussed with patients and/or families.
-
There are high levels of support for embedding ED conversations within ACP processes and a majority of HCPs are in favour of discussing ED options routinely with patients/families in EoLC.
-
However, some HCP interview participants expressed doubts regarding their knowledge of ED processes necessary to discuss the option with patients and/or families.
-
Education and training resources should look to explore what organisational or behavioural processes need to be put in place to embed ED discussions in care planning.
-
-
Prepared by: Bracher, M; Madi-Segwagwe, B; Long-Sutehall, T.
Appendix 10 EDiPPPP TEC Meeting – Process and Technical (30 June 2021 @ 2 pm)
Note: this report contains interim findings from ongoing analysis.
Role of this report
-
This report is intended to support members of the PT group in their discussions by providing a summary of key interim findings from the EDiPPPP study, indicating specific areas to inform intervention design.
-
The goal for this group is to identify key areas for organisational, logistical and individual practice change with respect to local and national processes, systems and resources to support implementation of ED.
The questions to be answered in this group are:
-
What processes need to be generated or amended in response to the findings of this report?
-
What technical resources (e.g. IT, clinical knowledge base) are needed to support these processes?
Summary of findings
-
The ‘Summary of Findings’ section of the report provides key points from the larger report (the ‘Interim Findings Summary full ‘document) and are provided to support group discussion:
-
This arrow symbol highlights recommendations and focus points relevant to discussion of intervention design.
-
-
Sections are ordered by the four ‘P’s of EDiPPPP (potential, practice, preference, perceptions).
Potential
-
High rates of eligibility for ED are present across in both HPC and HC settings (notes review).
-
Patients are in favour of ED; however, the majority of patients interviewed made a comment indicating that ED had not been raised with them during their current treatment programme.
-
Evidence from multiple data collection streams indicates that assessment of eligibility, approach to patients/families and referral of eligible patients is low.
-
Embedding ED conversations in routine care planning is necessary to ensure that patients/families who wish to choose this option are able to do so.
-
-
Raising of the topic of ED by HCPs with either patients or families is infrequent.
-
Patients indicated that they were in favour of ED being raised with patients receiving EoLC.
-
Patients indicated that ED should be raised on first contact with services or during ACP processes.
-
Patients indicated that HCPs (rather than patients or families) are seen as key people to raise this issue:
-
There is a need to develop processes for embedding discussion of ED as an option within existing processes of ACP/EoLC planning.
-
Practice
-
HCP participants from across data collection streams report that ED conversations are not currently part of regular conversations (e.g. MDT meetings, training needs discussions) within their service.
-
HCP participants from across data streams report not having or being unaware of a donation link person or champion within their service.
-
HCP participants from across data streams were unsure about the existence of any written clinical policies or procedures related to ED within their institution.
-
Many HCPs perceive that failure to embed ED processes within routine practice in EoLC is a key barrier to increasing donation rates:
-
Any intervention must consider how organisational behaviour change can be initiated and sustained over time (i.e. how will these changes ‘stick’ in the medium to long term).
-
-
Multiple Electronic Patient Record Systems (e.g. SystemOne, eCare) exist with varying degrees of support for recording and retrieval of information relating to ED.
-
System design needs to be based on a detailed map of the current informational infrastructure currently in place across different environments (e.g. whether EPRS or non-IT systems such as written patient notes).
-
Where possible, national systems for information retrieval are preferable to multiple local versions of the same information (e.g. eligibility criteria for ED).
-
Where local processes are involved, consideration should be given to the adaptability and scalability of these interventions (i.e. how feasible will implementation be within different systems).
-
-
Awareness of and access to standard criteria for assessment of ED eligibility is low across all three data collection streams.
-
Guidance is needed to clarify the distinction between threshold of evidence needed to refer to NHSBT, and the threshold needed for retrieval to occur.
-
-
Resources to support assessment for eligibility (e.g. information on contraindications) are not widely available although participants believe this already exists – (e.g. NHSBT website, trust intranet).
-
There is an urgent need for a publicly available web-based resource to allow sites to access information to support ER processes.
-
-
Access to written information to support discussion of ED with a patient or family member is variable across sites and context.
-
Context-specific, nationally developed and circulated written materials need to be agreed.
-
-
When asked how their wishes regarding ED should be recorded, patient participants provided a variety of answers (e.g. will, DNACPR, ACP, medical notes); however, none were clear about where this information can be held.
-
A nationally agreed record system for requests regarding ED is needed.
-
Perceptions
-
Most patients had no knowledge of ED (i.e. as a process, the use and impact of eye tissue) and were unaware that ED was an option for patients receiving EoLC.
-
A large majority of HCP participants do not agree that ED is too distressing to be discussed with patients and/or families.
-
There are high levels of support for embedding ED conversations within ACP processes and a majority of HCPs are in favour of discussing ED options routinely with patients/families in EoLC.
-
There is a need for processes that support HCPs in embedding ED into routine practice to meet the needs of patients.
-
Prepared by: Bracher, M; Madi-Segwagwe, B; Long-Sutehall, T
List of abbreviations
- 6SQuID
- six steps in quality intervention development
- ACP
- advance care planning
- BoT
- Burden of Treatment
- CI
- chief investigator
- COM-B
- capability, opportunity, motivation – behaviour change model
- CPF
- Communication with Patients and Families/Carers
- ED
- eye donation
- EDiPPPP
- eye donation from palliative and hospice care contexts: investigating potential, practice, preference and perceptions
- EEDAC
- Eligibility Eye Donation Assessment Checklist
- EoLC
- end-of-life care
- EPRS
- Electronic Patient Record System
- EPSOD
- eye donation from solid organ donors
- ER
- eligibility and referral
- ERGO
- Ethics Research Governance Office (University of Southampton)
- ETA
- Education, Training and Awareness
- Fuchs Corneal Dystrophy
- Fuchs’ endothelial dystrophy is a non-inflammatory, sporadic or autosomal dominant, dystrophy involving the endothelial layer of the cornea
- GP
- general practitioner
- HC
- hospice care service
- HCP
- healthcare professional
- HCP-FL
- healthcare professional in front-line role
- HCP-Str/Man
- healthcare professional in strategic and/or managerial role
- HPC
- hospital palliative care service
- ICU
- intensive care unit
- IP
- intervention points
- JBI
- Johanna Briggs Institute
- Keratoconus
- condition where the cornea of the eye changes in shape, strength and thickness over time impacting on vision
- MDT
- multidisciplinary team
- MeSH
- medical subject headings (PubMed and Medline databases)
- NHSBT
- National Health Service Blood and Transplant
- NHSBT-TES
- National Health Service Blood and Transplant-Tissue and Eye Services
- NoK
- next of kin
- ODR
- Organ Donor Register
- OREDAC
- organisation readiness for eye donation assessment checklist
- PI
- principal investigator
- PIS
- participant information sheet
- PPI
- patient and public involvement
- PRISMA-ScR
- preferred reporting of systematic review and meta-analysis extension for scoping reviews
- PSC
- Project Steering Committee
- PT
- Process and Technical
- QDA
- qualitative data analysis
- RAPiD
- Rapid Assessment of hospital Procurement barriers in Donation
- ReSPECT
- recommended summary plan for emergency care and treatment
- RNIB
- Royal National Institute for the Blind (UK)
- RQ
- research question
- RSPTD
- regional Specialist Nurse in tissue donation
- Service users
- user of hospice or hospital-based palliative care services
- Service providers
- provider of services in hospice or hospital- based palliative care services
- SNOD
- specialist nurse in organ donation
- STEPS
- Support Toolkit for Eye donation in Palliative care Settings
- ToPD
- Theory of Paradoxical Death
- TEC
- transparent expert consultation
- WHO
- World Health Organization
- WP
- work package
Notes
-
Summary of changed documents resulting from non-substantial amendment (ERGO ID 59185) 29 June 2020 and (ERGO ID 59185 A1) (6 May 2021)
-
Blank review proforma incorporating assessment criteria for ED eligibility specified by NHS blood and transplant tissue services division
-
Example site-specific report on results from notes review (WP1S1)
-
Direct observation of ED related practice topic guide (v1, 4 April 2019)
-
Demographic characteristics of HCPs involved in interviews and focus groups
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/KJWA6741).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.