Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR129491. The contractual start date was in September 2020. The draft manuscript began editorial review in March 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Ryan et al. This work was produced by Ryan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Ryan et al.
Chapter 1 Background
Plain language summary
-
We present information about what we know about older people with learning disabilities and family carers.
-
We talk about the language we use in the report.
-
We talk about what the research is about and what it is aiming to do.
-
We describe how this report is organised.
Introduction
Although there are an estimated 1 million people with learning disabilities (PWLD) in England,1 there are few accessible published data about the number of older PWLD. C Hatton (22 March 2019, personal communication) estimates that there are around 81,000 PWLD aged > 50 years, many of whom are not in contact with services. 2–4 The life expectancy of PWLD has been increasing, and it is estimated that the number of people requiring social care will have increased by 68% by 2030. 5 The number of PWLD using adult social services is estimated to double by 2030. 6 We know little about the lives of PWLD as they age, such as how they are affected by health issues or the illness or death of family carers. We also know little about the experiences of family carers as they grow older.
There is an even more pronounced absence in the academic and grey literature regarding the lives and experiences of older PWLD without family support. The World Health Organization7 has underlined the importance of PWLD ageing successfully and productively, and this has been operationalised into the concept of ‘active’ ageing,8 which involves living an active and meaningful life in the local community. A recent systematic review of research from England, the Netherlands, Belgium and France9 found that not all PWLD actively age and, instead, many lead sedentary lives, often overmedicalised and at risk of falling, developing depression and other long-term health conditions, and dying prematurely. The authors found a range of issues, such as unfit housing, poor staffing and attitudes, underpinned by a lack of psychological support and planning.
While little is known about the needs and experiences of older PWLD,10 there are clear destabilising factors for this group that make people vulnerable to distress. These include reductions in services in part due to austerity measures,11 the reliance on family carers who eventually grow too old to provide care, changing health needs through ageing, a risk of early-onset dementia,12 and deteriorating physical health. 13,14 A lack of future planning15,16 increases the risk of people moving at crisis point to more intensive and sometimes out-of-area supported care; it also causes distress and can lead to people being labelled with ‘behaviours that challenge others’ (‘BTCO’). There is a further gap in research around people who have attracted the label of ‘BTCO’ as younger adults and who are growing older, and a lack of effective end-of-life care (EOLC), that is care and support in the last year of life for older carers and PWLD. 17 Our research project was designed in response to the National Institute for Health and Care Research (NIHR) Commissioning Brief 19/14 and addresses remit 2ii:
How can families and professional caregivers be supported to provide care and support for people with learning disabilities and behaviour that challenges?
Learning disabilities and ‘behaviours that challenge others’
We start this report with a note about terminology. Language and definitions of ‘learning disability’ have remained ‘remarkably unstable’ over time, and who is defined as belonging to this group changes ‘due to cultural and social ideas around what constitutes mental faculty’. 18 A static, medicalised model focusing on deficit remains dominant:
A significantly reduced ability to understand new or complex information and to learn and apply new skills (impaired intelligence). This results in a reduced ability to cope independently (impaired social functioning), and begins before adulthood, with a lasting effect on development.
World Health Organization19
The impact of being labelled as having a learning disability can be considerable, as the term remains associated with stigma and shame,20 demonstrated by the speed at which medical terminology translates into lay terms of abuse. 21 While the term ‘intellectual disabilities’ is widely used internationally, evidence suggests that in the UK it generates scepticism and a sense of stepping back in time. 22 Here we use the term learning disabilities and PWLD as a shortened version for pragmatic reasons.
The term ‘challenging behaviours’ is also contested, and we use ‘BTCO’ to acknowledge the inherently relational and socially constructed nature of this concept. 23,24 ‘BTCO’ are a product of environmental factors including responses of support workers and family members, the quality of the material environment and commissioning processes, how well a service is organised and led, and earlier events in someone’s life which may have been traumatic. 23,25 Mansell23 acknowledges that behaviours may be a way to self-soothe or communicate that may remain even with excellent support. The question then becomes in what contexts and by whom are these behaviours considered to be ‘challenging’, and how can support staff, services, families and wider society adapt to this while keeping the person (and others) safe?
While policy and guidance across the UK over 30 years have stressed the socially constructed nature of ‘BTCO’, the term continues to be used to label people,23 enhance the legitimacy of a service, justify service practices or empower management decisions. 26 It can further disrupt the health care that people receive, as symptoms of pain or serious illness can be attributed to ‘BTCO’, leading to misdiagnosis and premature death. 27,28 In this report, we engage with this concept critically to ensure that we do not legitimise or justify certain practices of labelling people in ways that take attention away from the distress they might be experiencing and shift it onto procedures of managing this distress, as opposed to addressing its causes. A large-scale longitudinal Irish study with a nationally representative sample of PWLD aged > 40 years found that > 50% of older PWLD display what the authors describe as ‘problem behaviours’, and these are associated with a psychiatric diagnosis and high rates of psychotropic medication. 29 Concerns have been raised about potentially inappropriate prescribing in older PWLD that can be related to the label of ‘BTCO’. 29
Finally, our research focuses on PWLD aged ≥ 40 years in line with the above evidence that people may experience early onset of long-term conditions such as neurological, cardiovascular, respiratory and gastrointestinal disorders.
Background
Resistance to future planning
We know that parents of PWLD are dissatisfied with statutory and private services and have concerns about the future caring responsibilities of their non-disabled adult children and their own ageing,30,31 although primary research on older family carers of PWLD is sparse in the UK. A body of policies and programmes in the UK, including Valuing People, Valuing People Now and Transforming Care, aimed to enable PWLD to lead independent supported lives. However, family carers remain committed to maintaining long-term care in the family home without support or confidence in existing services. In England in 2021–2, 36% of adults with learning disabilities aged 18–64 years getting long-term social care (47,835 people) were living with their families. 32 There is no equivalent information for PWLD aged ≥ 65 years. The government’s recent Building the Right Support Action Plan33 says very little about supporting people as they grow older.
Six studies were identified in one review34 that found themes of fear for the future, lack of trust in services, lack of proactive support to manage crises and transitions, and declining personal support networks in a period when they are most needed. A systematic review of qualitative studies focusing on the future planning of older family carers found three key themes; reservations about available services, mutual dependency and a sense of helplessness, and that parents were making plans or at least had some idea about what they would like to happen in the future. 35 The authors argue for clarity around who is responsible for starting conversations around the future and what the provider or local authority (LA) are doing, given that parents take responsibility for initiating and facilitating plans. The planning, if it is happening, is not being done early enough or with sufficient clarity. The review also found that the responsibilities of caring for and supporting PWLD do not necessarily end when the person moves from the family home. Gorfin and McGlaughlin36 talked with PWLD and found that participants were aware of the need to think about the future; however, the difficult prospect of leaving behind mutually caring relationships obstructed this.
Comprehensive National Institute for Health and Care Excellence (NICE) guidelines for supporting PWLD as they grow older exist, without consideration of ‘BTCO’, which has its own NICE guidance. 37,38 Recommendations include a multiagency plan to be in place and reviewed annually or as need arises and for health planning. The NICE review for the ‘BTCO’ guideline (to March 2017) includes seven studies that do not include older people. A qualitative synthesis of carer experience with services for this group found concerns about times of crisis and availability of suitable services in later life39 and asking for help from the local community can be particularly difficult for carers from ethnic minorities. 40
The little research that exists focuses on points of contact with health services as people get older, not about how health and social care services could work to support decisions about living arrangements and health services towards end of life (EOL). Studies of carer experience of palliative care, cancer and dementia41 found concerns about how to access palliative care services and how to communicate the prognosis and treatments required to families and to older PWLD with deteriorating health. Social care staff in palliative care settings with people with Down syndrome and dementia experienced dissonance between their enabling role supporting autonomy and their subsequent role of monitoring deteriorating health and diminishing skills. 42 Discrepant views can further exist between PWLD, their families and practitioners on EOLC. 43 In summary, the evidence base points to little focus on PWLD growing older.
Project rationale
We know little about the ageing of PWLD and ‘BTCO’, or how family carers manage their caring role as they themselves age. How can forward planning be introduced in an acceptable and reassuring way to older PWLD and family carers? How can health, social care and EOLC services effectively support carers and older PWLD including where active family involvement is absent? How can commissioners be innovative in developing a service infrastructure that better meets the needs of this group? This study explored the support and health needs of older PWLD and family carers to identify ways of easing the move to different homes and support services through planning ahead and reducing the distress and so-called ‘BTCO’.
Aims and objectives
Research questions
What are the information, health and social care support needs of family carers and older PWLD with ‘BTCO’ that enable effective forward planning around supported living and EOLC for older carers?
What are the characteristics of exemplars of good practice in services and support interventions in the UK for older PWLD (and their carers) towards EOL and how are they delivered?
Aim
The aim is to improve support for family carers and older PWLD (aged ≥ 40 years) with ‘BTCO’ by producing effective and workable recommendations and resources including EOLC planning for carers.
Objectives
-
To develop an understanding of existing evidence about the health (physical, mental and social) needs, service interventions and resources for family carers and older PWLD with a focus on those labelled with ‘BTCO’ who are moving to greater supported care, including EOLC [work package (WP) 1].
-
To identify exemplars of good practice in services and support interventions in the UK for older PWLD, and their family and professional carers, towards the EOL (WP2).
-
To explore how older PWLD and their carers can be better supported in later life by researching the commissioning and delivery of exemplar services using ethnographic case studies (WP3).
-
To co-produce decision aid tools to support future planning and EOLC discussions for carers and future planning for older PWLD and evaluate their initial use (WP4).
-
To co-produce actionable recommendations for commissioners and providers, resources and decision aids for carers and PWLD, and online training materials about care in later life for social workers and professional carers (WP5).
Additional funding
In early 2022 we were awarded additional funding to add a new study site based in the north of England to the ethnographic work, to conduct a new rapid scoping review on the co-ordination of health and social care for older PWLD and ‘BTCO’, and to update one of the existing rapid scoping reviews on the experiences of older PWLD to incorporate searches about access to EOLC provision. We have incorporated the findings of this additional funding into the main body of the report.
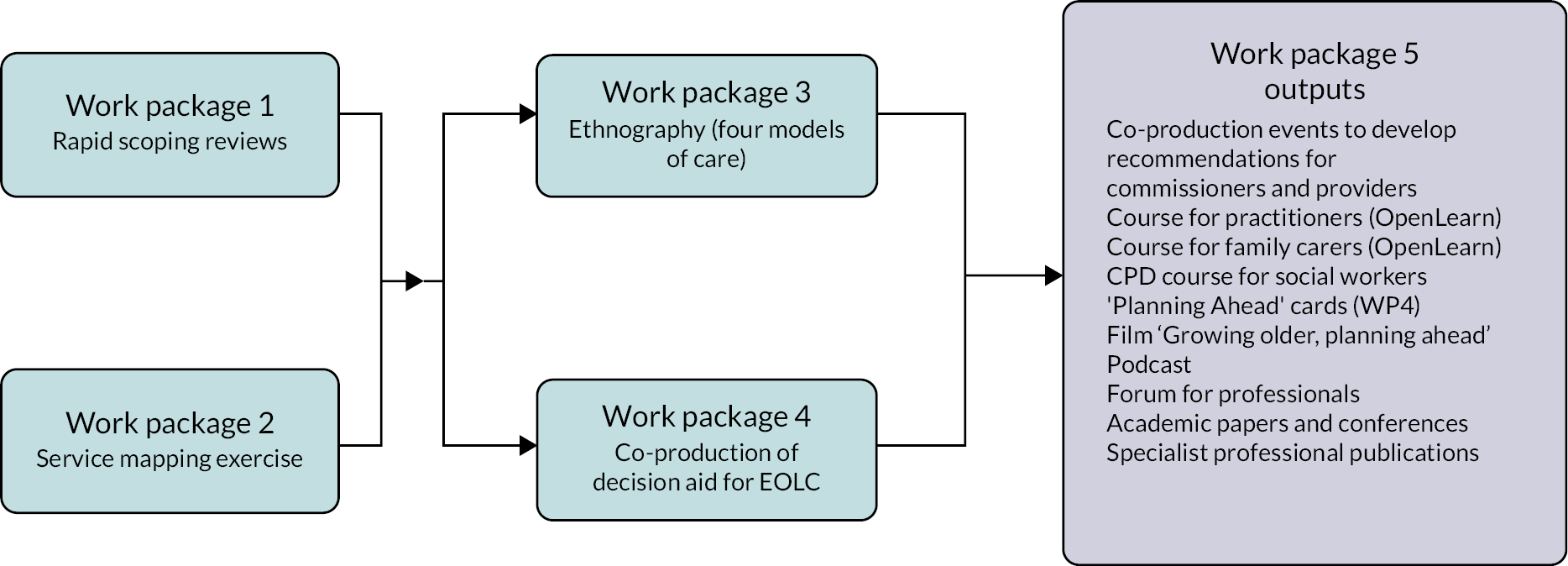
Research plan
This qualitative study comprised five WPs (Figure 1). WP1 and WP2 are scene-setting. WP1 involved three rapid reviews (RRs) focusing on the needs and support of older PWLD and family carers, practice guidance, interventions, resources and the co-ordination of support. WP2 involved a scoping study to identify exemplars of community living services and support interventions across England for older PWLD, including those with so-called ‘BTCO’. In WP3, research teams, including family carers and PWLD, used ethnographic methods of observation, interviewing and documentary analysis to study exemplary provider sites. Case studies were mainly selected from the findings of the scoping exercise in WP2, with one site identified during the proposal development stage (see Chapter 4). WP4 focused on planning ahead and the EOLC planning experiences of older carers and the use of decision aid interventions in forward planning for PWLD. The two central strands of facilitating and enabling forward planning for older PWLD, and EOLC for carers, came together in WP5 when we co-produced the final project outputs.
FIGURE 1.
Flow diagram.
Outline of this report
This report is structured to follow the WPs sequentially, with the methods and findings covered in the same chapter, or in the subsequent chapter in the case of WP3. Chapters 2–6 present the findings from WPs 1–4, and each chapter begins with a plain language summary. The co-production work from WP5 is discussed in Chapter 7 and Chapter 8 discusses public involvement. Chapter 9 draws the project findings together with a discussion of the implications of our findings, recommendations and conclusion.
Chapter 2 Work package 1: reviewing the literature on older people with learning disabilities and ‘behaviours that challenge others’ and their family carers – needs, experiences and care co-ordination
Plain language summary
-
We did three reviews of the literature. This means we read lots of articles and reports and found out what other people said about our topic.
-
Review 1 looked at what is written about the lives of older people with learning disabilities and ‘behaviours that challenge others’.
-
Review 2 looked at what is written about the lives of family carers of older people with learning disabilities and ‘behaviours that challenge others’.
-
Review 3 looked at what is written about how care is co-ordinated for older people with learning disabilities and ‘behaviours that challenge others’.
-
We found there is not enough good support or information available for people and their family carers as they get older. We learnt that more research is needed to understand how things can be improved.
Introduction
Despite the challenges and stresses that can be faced by older PWLD, and their family carers, we know little about their experiences of moving out of the family home or between homes or providers. Two previous systematic reviews that addressed the experiences of PWLD and ‘BTCO’ were focused on younger adults. 44,45 A previous systematic review on support for older PWLD did not include a focus on ‘BTCO’. 46 Previous systematic reviews on ageing carers of older PWLD have not dealt specifically with the experiences and needs of older carers of PWLD and ‘BTCO’. 34,35,47,48
To address this evidence gap, we undertook three rapid scoping reviews. The first (RR1) addressed older PWLD and ‘BTCO’, with a specific focus on ageing, including issues relating to moving home. Additional project funding awarded in 2022 was used to extend RR1 to include a detailed search on EOLC. The second review (RR2) addressed family carers, with a focus on ageing and issues relating to supporting their family member to move home. The third review (RR3), also undertaken with the additional project funding in 2022, explored the effective co-ordination of health and social care for older PWLD and ‘BTCO’ who live in the community.
Objective
Our key objective in WP1 was to develop an understanding of what is known about the health (physical, mental and social) needs, support and resources for older PWLD and ‘BTCO’ and their family carers, with a focus on experiences, interventions and resources related to moving home and care co-ordination.
Methods
Review research questions
What are the health and social care needs, experiences, service interventions and resources of and for older PWLD and ‘BTCO’ as they move to different care contexts in the UK? (RR1)
What are the health and social care needs, experiences, service interventions and resources of and for family carers of older PWLD and ‘BTCO’ as they move to different care contexts in the UK? (RR2)
What enables the best co-ordination of care for older PWLD with ‘BTCO’ living in the community? (RR3)
Rapid scoping reviews: rationale
Systematic rapid scoping reviews were used because our review questions were inclusive and exploratory in nature, designed to capture evidence pertaining to multiple aspects of the health and social care needs and experiences of and service interventions and resources for older PWLD and family carers. Scoping reviews allow evidence drawn from diverse sources, which is typically heterogeneous in nature, to be systematically synthesised. 49 RRs are a streamlined and/or accelerated version of systematic reviews50 and are an increasingly accepted approach to evidence generation. 51,52
The reviews were reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist53 (see Report Supplementary Materials 1–4). We drew on relevant expert guidance. We used the SelecTing Approaches for Rapid Reviews (STARR)54 decision tool to help make broad decisions concerning the overall review process. Regarding specific methods, we drew on guidance from the Oxford Centre for Evidence Based Medicine52 and the World Health Organization. 55
Throughout the review process we consulted with the wider project team, the Professional Advisory Group and Public Advisory Group to ensure that the review remained relevant and useful. 51,52 The groups contributed ideas, discussed ongoing findings, and helped to ensure that the analysis was clear and relevant.
Eligibility criteria
We were interested in the nature and findings of evidence that could be used to draw conclusions about our topics of interest. Published and unpublished (grey) literature, including research articles, reports and policy and practice guidance, were included; discussion papers, position papers, expert opinion pieces, editorials and study protocols were excluded. Within the published research we included primary (using quantitative, qualitative and mixed methods) and secondary (e.g. review) level evidence. For pragmatic reasons, for RR1 and RR2 we included only literature written in English and related to the UK context. This was extended for RR3 to cover international literature written in English to increase the likelihood of retrieving relevant material. RR1 and RR2 included evidence from 2001 onwards, to coincide with the publication of the Valuing People White Paper,56 which included an explicit focus on the needs of older PWLD and people with ‘BTCO’. For RR3, we removed the date restrictions to increase the likelihood of returning relevant hits.
Table 1 sets out the focus of RR1, RR2 and RR3, using the Population, Concepts and Context framework. 57
| Population | Concepts | Context | |
|---|---|---|---|
| RR1 | Older (aged ≥ 40 years) PWLD and ‘BTCO’ | Health and social care needs, experiences, service interventions and resources of and for these older adults | Older (aged ≥ 40 years) PWLD and ‘BTCO’ moving to different contexts of care |
| RR2 | Family carers of older (aged ≥ 40 years) PWLD and ‘BTCO’ | Health and social care needs, experiences, service interventions and resources of and for these family carers | Family carers of older (aged ≥ 40 years) PWLD and ‘BTCO’ moving to different contexts of care |
| RR3 | Older (aged ≥ 40 years) PWLD and ‘BTCO’ | Co-ordination of health and social care; multidisciplinary working for these older adults; age-related care | Older (aged ≥ 40 years) PWLD and behaviours requiring specialist health and social support related to ageing |
Definitions
We defined older PWLD as aged ≥ 40 years, as described in Chapter 1. We adopted a broad and inclusive approach to ‘family carers’ but were particularly interested in the experiences of parents and siblings in alignment with the empirical WPs.
A wide-ranging definition of ‘care contexts’ was used, encompassing service model [independent supported living (ISL), nursing home or family home]; provider type (NHS/LA, private provider, third-sector organisation, family); relationships (family members, paid carers, personal assistants); place (the geographical location of care); and commissioning and funding arrangements such as personal budgets. We focused our search strategy on ‘challenging behaviour’, ‘ageing’ and ‘learning disability’ rather than specific conditions (e.g. dementia) and/or specific forms of behaviour (e.g. self-injury, violence) after an initial trial returned a vast number of returns unmanageable for a rapid scoping review (an initial scan also indicated that many returned items had no relevance to our research question). While we refer to ‘BTCO in our reporting for WP1 in line with the wider report (see discussion in Chapter 1), our search strategy included terms commonly used in the academic and grey literature, for example, ‘challenging behaviour’ and ‘behaviours of concern’. These are nebulous terms and definitions vary according to context, but they are broadly understood to be a form of communication and may refer to aggression, self-injury, stereotypic behaviour, withdrawal, and disruptive or destructive behaviour. 58
Information sources and search strategy
Database selection, search strategies and searches were undertaken with the support of a subject specialist librarian. Given the short timescale and consequent need to achieve a balance between sensitivity and specificity, we focused on priority information sources such as CINAHL (Cumulative Index to Nursing and Allied Health Literature), PsycInfo, SICEN and Scopus. For RR1 (conducted in 2020–1) we used CINAHL, Healthcare Management Information Consortium (HMIC), NHS Evidence, Scopus, Turning Evidence Into Practice (TRIP), Web of Science (WoS), Google (first five pages) and Google Scholar (first five pages); and then MEDLINE, CINAHL, PsycInfo, SCIE (Social Care Institute for Excellence), and Social Policy and Practice for the additional searches for EOLC in 2022. For RR2 (conducted in 2020–1), we used CINAHL, HMIC, NHS Evidence, TRIP, WoS, Google (first five pages), Google Scholar (first five pages), the Carer Research Knowledge Exchange Network (CAREN) and SCIE. For RR3 (conducted in 2022) we used MEDLINE, PsycInfo, CINAHL, SCIE and Social Policy and Practice.
In addition, we used the expertise of the project research team and advisory groups and hand-searched the reference lists of included documents.
For electronic databases, we generated search terms (words and phrases, including synonyms and terminology variations). These terms were combined using the Boolean operators ‘and/or’ and appropriate truncation and phrase symbols to form initial search strategies, which we piloted against selected key databases. Based on this exercise, we confirmed our final search strategies to be used for each of the databases. The same keywords as for the main search were used to search grey literature (see Report Supplementary Material 7).
Selection of sources of evidence
Electronic search data sets were imported into Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and duplicate records were removed prior to screening. For RR1 and RR2, two reviewers independently screened all returned titles and abstracts (where available) against the inclusion criteria. Three reviewers independently screened all returned titles and abstracts for the extended RR1 search on EOLC. For RR3, three reviewers independently screened a selection of 50 returned titles and abstracts and met to discuss decisions and agree criteria for inclusion. All three researchers screened the remaining articles and titles.
Any discrepancies or queries were discussed between the reviewers and, if necessary, with the wider review team.
Full-text copies of potentially relevant articles and reports were obtained. For each review, one researcher independently reviewed full texts, with other members of the team reading a selection. Articles or other sources of evidence excluded based on full-text review were recorded, alongside the reasons for exclusion. Where evidence was not immediately available, we attempted to source it using various means, such as contacting authors. If the evidence did not become available within a 1-month period, it was recorded as missing.
Data extraction
A data extraction form was developed and piloted on three sources of evidence selected to ensure variation in focus and content, and a final version was used to extract data from included evidence. One reviewer led data extraction for each review, and completed forms were shared among the review team to be checked for gaps and inconsistencies.
Critical appraisal of individual sources of evidence
The conduct of critical (quality) appraisal in scoping and RRs is considered optional. 50,55,57 For scoping reviews, the central issue is inclusion of many types of evidence,57 some of which are not amenable to quality appraisal. For RRs the central issues are lack of or limited availability of information on which to base quality assessment decisions55 and time available to complete the review, including in respect of chasing up missing information. 51 Given the variety of included evidence and the project management plan, we took a pragmatic decision not to undertake critical appraisal. However, we considered how included papers framed the concept ‘BTCO’ and the extent to which the research took a critical stance towards this concept. We were alert to papers that presented a medicalised perspective on ‘BTCO’ and considered how this may have impacted on the findings presented.
Synthesis of findings
Alongside primary and secondary empirical research findings, evidence included non-research case studies, and resources providing information and guidance relevant to older (aged ≥ 40 years) PWLD and ‘BTCO’, and family carers. Such diversity necessitated a flexible approach to bringing together the evidence in its entirety. Key characteristics of included evidence were summarised in a table of characteristics for each review (see Appendix 1). Using these tables, we identified patterns and trends in the volume, focus and content of included evidence as the basis of our discussion.
The findings were integrated using a narrative approach. 59,60 An iterative process of reviewing the entirety of the research evidence allowed us to identify patterns in what the evidence was suggesting, however derived and expressed, which we captured in a series of themes and subthemes. The process was led by two researchers per review, with the sustained involvement of review team members from an early stage, and from advisory groups once an initial thematic draft had been developed.
Our aim was to interpret, rather than describe, the original (author-generated) findings to generate new conceptual understandings, set out as analytical themes. Deductively, we took the focus of the review as our point of entry into the data. Inductively, we followed the three-stage process outlined in Table 2.
| Stage | Analysis | Outcome |
|---|---|---|
| Stage 1: development of coding framework | Article-by-article development of codes, which reflected the meaning and content of the author-generated findings | Equivalence of coding/categorisation of data across the collective body of findings |
| Stage 2: development of descriptive themes/subthemes | Iterative review of codes to identify those that clustered together in terms of their meaning to produce ‘descriptive themes’ | Equivalence of ‘descriptive themes’ across the collective body of findings |
| Stage 3: development of analytical themes/subthemes | Iterative review of descriptive themes, including their individual codes and associated segments of data, in terms of their meaning/relevance to the focus of the review. To develop analytical themes Shared research team/ project advisory input to enhance the robustness of the final analytical framework |
Set of conceptually relevant analytical themes/subthemes |
Results
Rapid review 1: health and social care needs of older (aged ≥ 40 years) people with learning disabilities and ‘behaviours that challenge others’ moving to different contexts of care
This review was based on collaborative working with key stakeholders, using systematic methods of data searching, extraction and analysis. It explored what is known about the health and social care needs, experiences, service interventions and resources of and for this population as they transition to different care contexts in the UK.
In the original search in 2020–1, database searches yielded 261 returns, of which 223 were excluded based on initial screening using titles/abstracts. The remaining 38 were read in full, 32 were excluded and 6 were identified for inclusion. A total of 37 returns were identified from the reference lists of database-included articles, all of which were read in full. Of these, one article was included. A total of 40 additional items of evidence were identified by the research team, Professional Advisory Group and Public Advisory Group. Of these, two were included. Therefore, a total of nine items of evidence were included in our review conducted in 2021–2. The extended RR1 search conducted in 2022 on EOLC yielded 355 database returns, of which 346 were excluded based on initial title/abstract screening. The remaining nine papers were excluded after full reading. There was no additional evidence for RR1. Our analysis generated four main themes – transition over the long term: laying the necessary foundations; avoiding the need for unwanted/inappropriate transition; at the point of transition: making it work; and an absence of target resources – which we briefly summarise here:
-
‘Transition over the long term: laying the necessary foundations’ addresses factors that work for and against moving home successfully over the long term, captured in three subthemes: ‘opening up choice’, ‘promoting independence’ and ‘making choice a reality’. Future planning involves proactive planning for circumstances in which PWLD are no longer able to remain in their home, which is typically the family home. 61 Evidence showed limited planning by ageing family carers and PWLD, albeit for various reasons. Professional involvement in supporting a ‘whole family’ approach to future planning is advocated by Forrester-Jones62 and Slevin et al.,61 with the latter stressing the need for planning to start before problems associated with ageing manifest. Commissioners have a responsibility to proactively plan for the delivery of appropriate housing and support. This requires detailed knowledge of the needs of the people involved locally, and how these are likely to change over time, premised on robust databases of ageing family carers and older PWLD. 61
-
‘Avoiding the need for unwanted/inappropriate transition’ addressed factors to help maintain residence and prevent crisis moves in three subthemes: ‘optimising health and social care’, ‘the importance of staff training’ and ‘specialist community teams for people with “BTCO”’. The need to avoid delays in the completion of needs assessment went far beyond the 4–6 weeks specified in the Care Act 2014. Given the relationship between mental and physical health issues and ‘BTCO’, a proactive approach to the effective health care of older PWLD and ‘BTCO’ is particularly needed. Slevin et al. 61 highlight the evidence for annual health checks as a useful preventative strategy, as they can reveal ongoing or changing health needs. That older PWLD have been shown to underuse health services further underscores the need for proactive engagement. 61 Linked to this is the criticality of bespoke staff training, focused on what people need as they age63 and the benefits of community specialist teams who have the breadth of skills and professional knowledge to meet the complex health and care needs of this group. 61
-
‘At the point of transition: making it work’ deals with factors that promote the potential for successful transition in two subthemes: ‘specialist support in making transition happen’ and ‘front-line staff skills and attitudes’. Leaning and Adderly64 identify the benefits of specialist involvement at the point of transition, including community nurses, social services colleagues, psychiatrists and ‘challenging needs specialists’. They also emphasise the need for professionals and family to resist and challenge ‘problem-saturated narratives’ that focus excessively on behavioural concerns, and instead promote alternative narratives that are informed by the person’s capabilities and what makes them happy. The role of creative, compassionate and consistent staff and senior managers is also critical. 65
-
‘An absence of targeted resources’ deals with the limited information and guidance currently available to PWLD as they grow older.
Rapid review 2: health and social care needs and interventions for family carers of older (aged ≥ 40 years) people with learning disabilities and ‘behaviours that challenge others’ moving to different contexts of care
This rapid scoping review of published and unpublished literature explored what is known about the health and social care needs, experiences, service interventions and resources of and for these carers in the context of the transition of their adult family member to different care contexts in the UK.
Database searches yielded 157 returns, of which 110 were excluded based on initial titles/abstract screening. Of the remaining 47 read in full, 45 were excluded and 2 were included. A total of 35 returns were identified from the reference lists of included articles, all of which were read in full. Of these, one article was included. A total of 40 additional items of evidence were identified by the research team alongside our Professional and Public Advisory Groups, all of which were read in full. Of these, four were included. Therefore, a total of seven items of evidence were included in our review. Details of the seven included items are in Appendix 1. RR2 identified four key themes: support for ageing family carers of PWLD and ‘BTCO’; challenges facing carers when considering planning ahead; availability of suitable housing and support; and limited availability of information and guidance:
-
Support for ageing family carers of PWLD and ‘BTCO’. The review highlighted a lack of accessible advice, information and support. Black and McKendrick66 found that 29 out of 36 participants in Northern Ireland reported not knowing what help was available from services. Significantly, 28 out of 36 reported a lack of regular contact with their social worker, meaning that they did not have consistent access to an important source of information. Slevin et al. 61 discuss a range of interventions that can act ‘as a form of prevention, maintenance and also crisis management’, including planning, support groups, support co-ordination, direct services and sibling support, which can provide information, emotional and practical support.
-
Challenges facing carers when considering planning ahead. Forrester-Jones,62 Slevin et al. 61 and Black and McKendrick66 note a tendency for carers to avoid thinking about the future. Forrester-Jones62 found that family carers can be reluctant to relinquish their caring role, which can be a source of profound satisfaction and purpose, within a context of mutual caring and interdependence that develops over time. Using a ‘whole family’ approach to address issues around future planning that are acceptable to carers is strongly advocated. 61,62,66 The potential role of siblings as future main caregivers needs consideration and sensitivity;61,62,66 for example, siblings may not want to or be able to assume a caregiving role. 62,66 The revisiting of plans is recommended so changes in family circumstances and needs can be considered, and plans amended accordingly. 61,62
-
Availability of suitable housing and support. RR2 highlighted the burden on carers of struggling to find appropriate accommodation for their relative. Even when families are ready and prepared for the move the process can be protracted, complex, debilitating and frequently futile. 67 On average, PWLD had been on a housing waiting list for 2–3 years, with two families (out of nine) waiting over 5 years. A key obstacle to progress was communication with social services and housing staff, and meetings were held with no follow-up action. This lack of action was often associated with constant changes in personnel, and the fact that no one professional appeared to take responsibility. Participants described growing distrust of social services and housing department staff, and disillusionment with the system in general.
-
As with RR1, our final theme addressed the limited information and guidance available to aid PWLD to navigate moving from the family home. We found no targeted resources to guide PWLD, family carers or professionals (either front-line or planners/commissioners) in planning ahead.
Rapid review 3: the co-ordination of care for older people with learning disabilities with ‘behaviours that challenge others’ living in the community
Database searches yielded 1449 returns, of which 1391 were excluded based on initial screening using titles/abstracts. The remaining 58 were read in full; 49 were excluded and nine were identified for inclusion. Manual reference list and forward citation searching were undertaken for these 9 papers. Based on initial screening, 6 papers from the reference lists and 108 from the forward citation searching were excluded. The remaining 12 papers were read in full. However, none met the inclusion criteria and all were excluded. Therefore, nine items of evidence were included in our review. See Appendix 1 for details about the nine included items.
Rapid review 3: findings are presented at individual, service and commissioner levels
-
At an individual level, the review emphasises the importance of professionals, PWLD and family members developing positive relationships. This involves effective communication and a sharing of knowledge. 68–73 It also requires the co-ordination of specialised, bespoke and person-centred planning and a focus on pre-empting and responding to ‘health-related loss’, such as a deterioration in mobility. 70 This may involve the recruitment and training of specialist staff teams, with relevant input from both clinical and social care staff. 69,71 The benefits of a family-centred approach to the delivery of primary care to older PWLD was also identified, with the caveat that professionals should ensure that the views of family members are balanced against the wishes and preferences of PWLD. 73
-
At a service level, proactive collaboration between different agencies is critical. 68–70,72–75 This involves bringing together professional expertise within learning disability (e.g. via community learning disability teams), mental health and gerontology services as needed, alongside housing agencies. However, when professionals work with other agencies, there may be knowledge gaps around learning disabilities, particularly for those who do not frequently work with PWLD. 72,74 Training and resources are suggested for professionals who do not regularly work with older PWLD, including experiential training alongside PWLD.
-
At a commissioning level, the review identified that provision for older PWLD was frequently fragmented, leading to critical opportunities for diagnosis and referrals (e.g. for mental health support) being missed. The importance of local strategic frameworks to support planning and resourcing for this group of people as they age was highlighted. This was described as a needs-led service system that ‘has capacity to take account of current and future age-related needs’. 70 There was some consensus that the system should be developed from the bottom up in response to the needs of local people. 68,70–72,76 How well funded and well planned service provision is locally or regionally impacts the potential for success at the individual and service levels. This includes the provision of multidisciplinary outpatient healthcare practices that provide co-ordinated physical and mental healthcare services for PWLD. 76
Discussion
The absence of a critical understanding of ‘BTCO’ as a socially constructed phenomenon, predicated on the understanding of all involved within interpersonal, organisational and systems contexts of interaction, is a limitation in existing research. These social dynamics are critical to promoting and impeding the effective move of PWLD from their family home or from one provider to another. Within the limited evidence available detailing examples of successful moves for older PWLD, the role of suitably trained, consistent and compassionate staff, supported by effective senior service managers, was notable. 65
Our reviews highlight gaps in the promotion of proactive planning, the provision of appropriate housing, effective needs-based assessments, inconsistent or absent approaches to collaborative working across different professionals and agencies, and the availability of timely and consistent professional support, most notably from social workers. The criticality of local strategic frameworks to facilitate effective planning and bespoke service development for PWLD and their families was clearly identified in RR3. RR1 and RR2 also draw attention to the dearth of resources and guidance available to support PWLD and their family members to plan ahead.
We identified several systems issues that need to be addressed in order to build capacity to support people as they age. The importance of proactive preparation and planning across multiple areas of activity is clear. This includes building PWLD’s confidence over time to live outside the family home (thus avoiding an unanticipated move in the context of a crisis), more robust support for family carers from health and social care professionals (particularly social workers) and the strategic commissioning of suitable housing and support services. This means people planning to move out of the family home before services deem that they ‘need’ to. Commissioners across learning disability, older people’s services and mental health need to work collaboratively in such strategic planning. Forrester-Jones62 also highlighted the critical role played by social workers in supporting the transitions of older PWLD as they age (and their families), acknowledging the importance of consistency and relationship building over time. In addition, Forrester-Jones62 identified a widespread lack of a ‘whole family’ approach to needs assessment, with significant implications for planning and the mitigation of crises for people.
Timely and effective engagement with health services is also needed to help identify the onset of conditions that may be labelled as ‘BTCO’ as a result of people becoming unwell or experiencing pain/discomfort. Our reviews show that education and training should be provided to family and front-line professional staff in relation to both the recognition of the early symptoms of dementia and the care of PWLD who develop dementia. 61
Ageing can impact the ability of family carers to care for their adult family member with a learning disability. 61,62,67 The relationship between ageing and diminishing capacity to care in the family home, as well as the profound anxieties engendered, is highlighted in the broader literature. 2,77,78 Evidence also demonstrates the additional distress when this happens in the context of a lack of future planning,35,47,48 exacerbated by (often severe) limitations in the availability of appropriate housing. 13,37,79
Our reviews have confirmed an inadequate evidence base concerning the experiences, needs and support of older carers. That which does exist demonstrates major deficits in how the carers of older adults who may display ‘BTCO’ are being supported when their family member’s preference is to remain at home and/or to consider and achieve a move outside the family home. Although premised on a limited evidence base, our reviews provide important insights into what is required to effectively support PWLD and their family members as they grow older.
Limitations
We note that all three reviews had a low rate of inclusion despite initially promising returns. The key reasons for exclusion were that the evidence was not sufficiently focused on our target population and/or that the substantive content was not relevant to our research questions. Focusing our search strategy on ‘challenging behaviour’ rather than associated conditions (e.g. dementia; profound mental ill health) and/or specific forms of behaviour (e.g. self-injury; aggression) risked missing relevant material. However, a trial of alternative approaches generated an immense number of returns, unmanageable for the purposes of a rapid scoping review. Moreover, on scanning these returns, they showed no relevance to our research question. The possibility that we missed relevant evidence was reduced by strenuous efforts to read a wide body of evidence, and, in addition, the search strategy for RR3 was widened to include international literature and work published before 2001. We also adopted an enhanced RR process, including the use of multiple reviewers alongside consultation with the wider project team and advisory groups to mitigate the risks of missing relevant evidence.
Having undertaken three rapid scoping reviews, the possibility remains that we have missed some relevant evidence. This is reduced by strenuous efforts to read a wide body of evidence that was eventually excluded. In addition, the search strategy for RR3 was widened to include international literature and work published before 2001. We also adopted an enhanced RR process, including the use of multiple reviewers alongside consultation with the wider project team and advisory groups to mitigate the risks of missing relevant evidence.
We found little evidence specifically focused on older PWLD labelled with ‘BTCO’ in the context of moving home. We were therefore largely dependent on evidence that addressed our review questions as part of a broader focus, typically either older PWLD or PWLD labelled with ‘BTCO’ (and their carers). From this evidence, we extracted relevant content. This required close reading of many items that did not contain relevant content. Most of the evidence included in our reviews was over 10 years old, pre-dating significant developments in the UK context, notably the impact of austerity,11 the roll-out of annual health checks by general medical practice from 2009,1 and guidance for strategic commissioning to develop capacity for suitable community provision across the life course, such as Building the Right Support,80 Building the Right Home81 and the Transforming Care programme. 82 Although we have been able to identify some key learning concerning current planning and implementation of transition-related care and support for older PWLD labelled with ‘BTCO’ (and their family carers), gaps in research remain.
Conclusion and recommendations
The reviews show that the needs of older PWLD, and of their family carers, must be afforded greater priority within health and social care policy and commissioning practices. Wider research exploring learning disability and ageing highlights the need for social care staff training to facilitate more nuanced and proactive approaches to support people as they age. 83,84 The promotion of healthy ageing among PWLD relies on services and front-line staff understanding the specific health needs of this population, clearly evidenced through large-scale longitudinal research. 85,86 The policy challenge lies in disseminating this knowledge effectively to practitioners, family carers and PWLD, while developing approaches to healthy ageing in services that are person-centred and responsive. Involving PWLD and their families/advocates (where possible) is also critical to ensuring that well-planned decisions are made – decisions that take account of people’s whole lives, including their relationships, homes, activities and hobbies, as well as health needs.
Research has shown that, despite policy commitments to ageing ‘in place’ (i.e. within their chosen home), progress in developing or adapting existing accommodation for PWLD as they age has been slow across a range of international contexts. 87 Our reviews demonstrate that macro-level strategic commissioning for PWLD and ‘BTCO’ as they age is urgently needed. Fundamentally, contemporary policy for PWLD has not been developed to take account of people growing older. This means that systems are not designed to support comprehensive commissioning for this population, and, in many cases, they prohibit effective, timely and inclusive discussions of future care,47 with consequent distressing, avoidable and costly crisis management.
Chapter 3 Work package 2: scoping and mapping exemplars of good practice in living arrangements for older people with learning disabilities and ‘behaviours that challenge others’ living in the community
Plain language summary
-
We wanted to find out how people describe excellent support for older people with learning disabilities who may be labelled as having ‘behaviours that challenge others’.
-
We read what is written by organisations for people with learning disabilities and those who decide what services should be provided in England.
-
We contacted around 260 people and about 80 organisations and found four key types of support.
-
We talked with professionals and people with lived experience to come up with a shortlist of excellent providers.
-
We made a shortlist of excellent providers for the next stage of our research.
Introduction
Work package 2 aimed to scope out models of service provision and identify exemplars of good practice in services and support interventions in England for older PWLD and ‘BTCO’, and their family and professional carers, towards the end of their life.
Service models focus
Services are defined in this research as those that support people to live in the community. This includes services that support people to live in their family home, housing with a tenancy and with types of paid support, Shared Lives (also known in Northern Ireland as adult placement) where the PWLD lives in a registered care provider’s own home as a family member,37 and residential care homes (with or without nursing care).
Service support includes domiciliary care, personal assistance funded by personal budgets, respite care, support with activities including employment, day-centre-based activities, supported living personal and social care, and a range of health, personal and social care provided in care homes. Individualised care provision can be shared via a team across a group of people living together or provided to one person. Health services are generally provided by generic primary care, specialist learning disability community health teams, and generic secondary and tertiary care services, supported by specialist learning disability liaison nurses. EOLC services provided to the general adult population are also accessed by PWLD. Support services that enable people to be discharged from assessment and treatment units and other inpatient settings are in scope where they are provided in the community and commissioned and/or provided by mainstream health and social care services.
Objective
Our objective in WP2 was to identify exemplars of good practice in services and support interventions in England for older PWLD, and their family and professional carers towards their EOL.
Methods
Criteria of exemplar services
The Professional Advisory Group considered and suggested standards in use by commissioners and providers. Some recommendations of standards related specifically to services for older PWLD and ‘BTCO’, but none were felt to be sufficient in themselves to be criteria of excellence for the purposes of this research, particularly as they addressed different needs, such as EOLC, dementia care and the needs of people leaving inpatient care. Therefore, the approach to defining excellence was developed through the data collection activity with a range of stakeholders.
Selected published standards and guidance, including the grey literature of WP1, with input from the Professional Advisory Group and views of key stakeholders, were analysed. We used a combination of predetermined and emerging categories to extract data supporting one or more of the criteria of excellence (see Criteria of excellence). The first step was a desk-based exercise of examining standards and descriptions of services derived from the literature and consultation. The second step involved using data from mapping interviews and a survey about participants’ relationships to services or those they had experienced, managed or were involved with commissioning.
Rapid analysis was used as described by Taylor et al. 88 for use with interviews and the survey comments using a combination of predetermined and exploratory themes. This was relevant for a subset of 30 participants in the mapping exercise interviews or who completed a survey equivalent (see Report Supplementary Material 5). Comments from interviewees and survey participants related to the general criteria of excellence that emerged from the desktop review were recorded into predetermined categories, and new themes were generated. Quality assurance of the coding was undertaken by a research associate, and differences were resolved by discussion. There were several new criteria describing participants’ relationships to services.
The third step involved both advisory groups commenting on the drafts and suggesting ways to refine the criteria.
Mapping
A mapping approach was adapted from three NIHR service mapping studies. 89–91 The aim was to identify services and whether they met the criteria of excellence while operating in the service models described by participants and the characteristics of older PWLD and ‘BTCO’ for whom these services were provided.
Recruitment of participants to identify services and/or for interview
The mapping approach used multiple routes to identify commissioning and provision of exemplar services and then to find out key information about the service from interviews, an online survey, websites and other documentary sources. Recruitment involved two parallel approaches:
-
NHS and social care commissioners: The initial plan was to use the approach adopted in the evaluation of Building the Right Support. 80 This evaluation used a survey of Transforming Care Partnership (TCP) members to identify case studies at TCP level and a snowballing approach to generate evaluation responses. 92,93 In this scoping exercise, we anticipated identifying, using a cascade approach, one or two key strategic-level participants who could identify relevant exemplar services if these existed in their area. We also anticipated that as the NHS was undergoing significant structural changes there was likely to be geographic variation in the strategic oversight of services over the period of study of 2020–1. Furthermore, TCPs are concerned with a small subset of PWLD with specialised service needs. We approached NHS England (NHSE) Learning Disability and Autism programme leads at regional and integrated care system levels via the Clinical Director for Learning Disability at NHSE. At this level, we sought exemplars and contacts with the Clinical Commissioning Groups (CCGs), LAs and NHS Mental Health partnership trusts. The NHSE Head of Nursing for End-of-Life Care also shared the invitation with her networks and senior clinical leads.
-
Third-sector providers and bodies representing the public: These organisations were contacted via commissioners and NHS providers, contacts from an article in Care Management Matters,94 a press release, the project website (http://wels.open.ac.uk/research/growing-older-planning-ahead) and social media presence (@OlderAhead and #OlderAhead), a subsample of the 386 ‘outstanding rated’ services that included adults or the elderly and PWLD on the Care Quality Commission (CQC) database, an online survey promoted via social media, a web chat with the ‘Our partners — Learning Disability Nurses’ forum, a clinical senate meeting in NHSE Southern region, and a webinar of Shared Lives providers.
Data generation
Data were generated by e-mail or telephone contact with social care professionals who gave information about services and information about others who could inform the study by identifying services and commenting on the criteria of excellence. Those willing to give information directly were offered either a semistructured interview conducted by telephone or online call or an online survey (see Report Supplementary Material 5).
Data analysis
A template was produced (see Report Supplementary Material 8) for summarising data collected from interview transcriptions and the open text survey. Notes were taken when the conversations were primarily referring the researcher to a primary source. This included data on the characteristics of people who use services, and the services themselves as well as the scope of commissioner responsibilities. Further sections were used to record key documents, web content, quotations and reflections relating to both the criteria of excellence (i.e. how they would apply across services) and specific exemplary practices or case examples of personal experiences of the services. These data were used to develop criteria of excellence described above. The interview and survey data were coded to identify descriptions of specific services. Interviews were conducted with up to four managers and commissioners per service to complete the template.
The final templates and supporting summaries of interviews together with a shortlist of exemplars were presented for consideration by both advisory groups and research team. Preparatory work with the research team and advisory groups was conducted virtually (due to pandemic restrictions) to gain views on the emerging criteria of excellence and how these should be applied to derive the shortlist of services from the mapping exercise. Quality assurance of the mapping exercise results was undertaken by the WP3 team considering the service models by reviewing all the data compiled on each service. The Professional Advisory Group considered the finalised criteria of excellence and consideration of the outcome of the mapping work. The Public Advisory Group and Study Steering Committee (SSC) considered the final shortlist of case sites.
Findings
Criteria of excellence
The criteria of excellence in services were derived from four sources: NICE, CQC standards, NHSE and related third-sector body standards. Sources of the standards are summarised in Appendix 2 and the initial criteria are described in this section, with emerging themes summarised in Table 3. The research literature included in the initial scope of WP1 was examined to draw out sources of published evidence for the emergent criteria. Additional evidence from the mapping interviews in support of the criteria is presented in Appendix 3.
| Criteria | Rationale | Selected evidence and references |
|---|---|---|
| Personalisation, assessment, goals, daily plans/activities | Personalisation is a key standard for all learning disability services, as evidenced in NHSE standards. It is a driver of the NHS Long Term Plan:
|
NICE guidance NG96:96
|
| Research evidence: Bissel et al.,97 Forrester-Jones,62 Slevin et al.,61 Bigby and Beadle-Brown98 | ||
| Matching staff to people being supported | Enabling people and families to choose who provides support, or work with the provider to match the values and interests of support staff to the person | NICE guidance NG93 1.9.6:
|
| Personalised living space/and choices of whom this is shared with | For PWLD and ‘BTCO’, the NICE guidance recommends people should have the option to ‘live alone with appropriate support if they prefer this and it is suitable for them’. Alternatively, ‘offer them the option of living with a small number of other people in shared housing that has a small-scale domestic feel. Involve people in choosing how many people, and who, they live with’37 | NICE guidance NG93, section 1.5, housing and related support, including 1.5.4:
|
| CQC standards on campus and congregate living: www.cqc.org.uk/guidance-providers/autistic-people-learning-disability/right-support-right-care-right-culture | ||
| Health; proactive, preventive, primary care, and involvement of NHS MDT | Assessment and planning to meet health needs, prevent lifestyle related disorders and manage comorbidities (such as epilepsy) requires proactive access to generic services such as primary care, and specialist services such as hospital Learning Disability Liaison nurse services, NHS learning disability multidisciplinary health team | NICE NG96 1.5 identifying and managing health needs, (1.2) physical health care96 NHS Long Term Plan commitment annual health checks99 Selected research evidence: Watchman100 |
| Staff recruitment underpinned with the right values and skills | This enables support staff to engage with people’s values, choices and activities they can relate to and share | Core Capabilities Framework for Supporting People with a Learning Disability101 NICE guidance NG93, staff skills and values (1.9), for example, involvement staff recruitment (1.9.6)37 Selected research: Bigby and Beadle-Brown,98 Leaning and Adderley64 |
| High staff retention to provide continuity of care | This was suggested by the Professional Advisory Group as it enables staff to better understand people’s needs and choices and how these might be changing. High turnover and use of agencies can be commented on in CQC inspections | NICE guidance NG96 (1.7 staff skills and expertise) has some relevance but does not cover continuity of care directly96 NICE guidance NG93 – principles – continuity of relationships37 Selected research: Hubert and Hollins65 |
Care Quality Commission standards
The CQC’s key lines of enquiry (KLOEs) focus on safety, effectiveness, caring, responsiveness and organisational leadership. The inspection process centres around five key questions that inspectors use to determine whether a service is fulfilling their duties for care: is the service safe, effective, caring, responsive and well led?
The Professional Advisory Group suggested that we look at ‘outstanding’ reports of services. This rating may involve a service being at the second level of ‘good’ for a minority of KLOEs, and if the next level rating of ‘good’ was used overall, then it was important that the ratings were ‘outstanding’ in the caring and safe domains, as these are most relevant to people labelled with ‘BTCO’. It was also advised that ratings will apply across a whole service, where the unit or service of interest may be a small unit in a larger service or have few if any service users eligible for the study at the time of the rating, or not recently had a new rating [particularly the case during the coronavirus-19 (COVID-19) pandemic]. Not all services (including, in some instances, the accommodation element of supported living services) are registered with the CQC, so some would not have ratings. Where available, we used CQC ratings to identify possible providers and provide additional information on possible candidate services suggested via other routes. CQC ratings were not regarded as sufficient evidence of exemplar services alone because they lack specificity to older PWLD and the rating may be from some years ago.
Service standards
Standards of services commissioned in England have been issued by NHSE, often in collaboration with social care and third-sector providers, disability rights and advocacy organisations, and carer organisations. These were gathered through the research team’s networks, the Professional Advisory Group, the communications activities of the project (website, social media), the WP2 survey (see Report Supplementary Material 5) discussion with senior NHS commissioners and interviews. These relate to EOLC, to standards for learning disability services applied to all adults, and to specialised learning disability services. Various tools have also been developed for providers and commissioners, families and advocates about what to look for in excellent services (see Appendix 3).
From the above sources, the initial criteria were developed (see Table 3). These were triangulated with selected empirical studies, including those reviewed for WP1, and NICE guidance.
Additional themes for criteria of excellence arising from work package 2 data
Our analysis generated additional themes (Table 4); see Appendix 4 for a thematic analysis of interviews and survey data.
| Criteria | Rationale and data from thematic analysis | Selected evidence references |
|---|---|---|
| Inclusive communication methods | Suggested by the Professional Advisory Group as part of personalisation | NICE guidance NG96 (1.1.7), review of changing communication needs as people grow older96 Selected research: Leaning and Adderley64 |
| Good practices such as EOLC planning, dementia assessment and management embedded as routine | Anticipation of the development of early dementia requires systems to risk assess and detect early signs and seek referral for assessment | NICE guidance NG96, consider training of carers/family members in early signs of dementia (1.5.6, 1.5.37), information about dementia (1.5.36). NICE guidance NG96 (1.6), EOLC for PWLD96 |
| Family involvement | Involvement of families in decision-making about provision and daily life. This involvement is in the context of service provision respecting the rights of the PWLD to autonomy and to a family life if they wish it, along with the caring and advocacy roles often assumed to be the concern of family members | This is integral to NICE guidance (e.g. NG96) (1.1.9–1.1.13)96 and the CQC102 and NHSE standards80 above Selected research: Leaning and Adderley64 |
| Community engagement and inclusion | Enabling people to be part of communities: the engagement of local communities includes in-reach by communities with providers and engagement with community activities in the local area in mainstream venues (or services regularly frequented by local people) as part of the daily activity of individuals | NICE guidance NG96 (1.2.5), access to community (1.2.11), social opportunities (1.2.12), community-based physical activity (1.2.13), education, employment and volunteering, accessible travel (1.2.14)96 Selected research: McConkey and Collins,103 Perry et al.,104 Slevin et al.,61 Bigby et al.105 |
| Trauma-informed services including PBS where appropriate | The use of ‘positive behaviour support’ approaches in the design and delivery of services is relevant to PWLD and ‘BTCO’. This approach may be achieved by regular training across staff groups, an in-house expert team and/or access to such expertise in NHS community learning disability services. Trauma-informed practices can be employed to prevent and to manage distress-related behaviours associated with past traumas |
NICE guidance NG93 describes the service requirements for adult37 and NG11 describes the interventions and their context, for example, including staff training (1.1.6), organisation of intraorganisational leadership (1.1.9–1.1.14)38 Selected research: Harvey106 |
| Commissioner endorsement of provider quality and resilience (low placement breakdown) | Health and social care commissioners are key to forecasting and planning for services, the assessment and monitoring of services and individual placements, and stimulating capacity in providers where high-quality capacity is in short supply | NICE guidance NG93 (1.1.10), stability of placements, contingency fund (1.1.5)37 |
| Commissioners are working with providers, PWLD and families building capacity for future services | The strategic role of commissioners has emerged as important in planning for future provision, with knowledge of the local PWLD and those returning from out-of-area placements, building capacity to enable more local provision, and working with providers to enable them to adapt services and facilities to enable older people to stay in their homes rather than in generic older people’s nursing homes | NICE guidance NG96 (1.2), planning and commissioning local services (1.2.1 and 1.2.3), local needs assessment, housing options (1.2.4), family and support options (1.2.5)96 NICE guidance NG93 (1.5), housing, choice of types and who they live with, tenancy, etc.37 Evaluation of TCPs found skilled commissioners able to work strategically (predicting need, at population level, stimulating provider capacity) was the top success factor92 |
A summary of the key criteria of excellence
The final criteria we used are:
-
personalisation, with goals, daily plans and activities shared and updated
-
matching staff to people being supported
-
personalised living space and choice around who this is shared with
-
proactive, preventative healthcare involving primary care, and involvement of NHS multidisciplinary learning disability teams
-
staff recruitment underpinned by the right values and skills
-
high staff retention to provide continuity of care
-
inclusive communication methods
-
family involvement
-
community engagement and inclusion
-
trauma-informed services where appropriate
-
good practices such as EOLC planning, dementia assessment and management, embedded as routine
-
commissioner endorsement of provider quality and resilience (low placement breakdown)
-
commissioners working with providers, PWLD and families building capacity for future services.
Findings of the mapping exercise
The CQC’s database of registered services was searched with the assistance of a CQC analyst in August 2020. This involved the following steps:
-
Categories were selected to focus on the types of services relevant to PWLD and ‘BCTO’ living in the community, aged ≥ 40 years, as no categories are specific to services for this group. These were (1) inspection category – residential social care, community-based adult services; (2) directorate inspection category (adult social) and (3) primary inspection category – residential social care or community-based adult social care services.
-
To narrow the search, it was necessary to specify categories of ‘adult’ (18–64 and ‘65 and over’) and include learning disability in its regulated categories. As services are registered for multiple groups, such as learning disability and physical disability and dementia, the search was expected to show services that did not necessarily currently support PWLD. Some 386 provider locations in England were rated ‘outstanding’ using these selection criteria.
-
Initial sifting of services with potentially relevant registration (B – regulated activity; C – service type; and D – service use user band), resulted in 330 registered locations with outstanding ratings. See Report Supplementary Material 6 for codes.
-
Services were removed that were clearly outside the remit, such as diagnostic screening and community healthcare services (n = 19).
-
Hand-searching the websites and/or title of the provider was carried out to remove ineligible services, such as those specialising in autism alone (n = 6), and one that had recently lost its outstanding rating (n = 1).
-
Providers were contacted that appeared most often (such as franchises) to verify that they included eligible service users and read their CQC report. If the identified provider was not contactable, contact was attempted with head office. This process removed many services that were not contactable or did not currently have eligible service users. The result was a list of four providers involving 74 registered services, and several Shared Lives schemes.
-
Finally, this data set was used to discuss how the criteria of excellence were met according to the views of providers and commissioners of these services.
Data from interviews, surveys and webinars: response rates and coverage of England
The methods described above (see Methods) involved contacting around 260 individuals. Exact numbers are not known as group online meetings are included for which numbers were not available. Many responses were helpful in providing further contacts and suggestions, and, among these, 89 contacts gave information in formal interviews and informal discussions and in e-mails about at least one specific service, with around 3–6 provider and commissioner perspectives collected on the same services.
Some 81 organisations contacted either passed on information to others or responded directly to a request for a conversation about exemplar services: NHSE regions (n = 7), integrated care system learning disability leads, learning disability and autism partnership boards (n = 10), CCGs (n = 13), LA commissioners (n = 3), mental health partnership provider NHS trusts (n = 4), LA provider managers of Shared Lives services (n = 6) and third-sector providers (n = 38). Geographic coverage was greatest in the south-west, south-east, north-west and north-east, with fewer responses about services in East Anglia, London and the Midlands.
From these contacts, informal conversations were conducted and 30 formal interviews, and notes were recorded about further key contacts and service model descriptions about services with 80 people: Expert researchers (n = 6), NHSE national leads (n = 2), NHS regional leads (n = 3), CCG leads (n = 11), LA leads (n = 7) and provider members (n = 51), and a further nine people completed a qualitative survey instead of the interview (see Report Supplementary Material 5), giving a total of 89 responses. Where there was sufficient input from both providers and commissioners, and they met the eligibility criteria described in the three steps above (see Methods, Criteria of excellence), 15 templates were completed. This included residential and supported living services with identified sites provided by six providers and several locally based Shared Lives franchises.
Interpretation and recommendations for work package 3
Who should be included?
Learning disability services are not organised around age criteria. Services specifically commissioned for PWLD and ‘BTCO’ include autistic people and younger people. Two groups emerged whose services are commissioned differently. Group A are older people who may have greater physical and mental health needs than their peers. This is a large group, with several hundred people in each CCG or LA area, and many may not be known to services.
Group B comprises people who have in their recent past been or are about to be discharged from long-term inpatient care. This is the ‘Transforming Care’ group and is much smaller. NHSE figures (personal communication between NHSE and Wallace, 2021) suggested 15 CCGs with up to 5 people aged ≥ 40 years discharged from April 2016 to September 2020 with a continuous length of stay of ≥ 5 years at discharge, and a further 9 CCGs with up to 10 people and 2 CCGs with up to 15 people discharged in the same period.
Which services should be included?
The four broad models of living were identified:
-
People living with their families, possibly with LA-funded day activities and/or personal budgets and domiciliary services.
-
Supported living via home ownership, tenancy and/or shared equity arrangement for accommodation and support provided in a personalised care package.
-
Shared Lives provision with paid care provided by an approved family in their home. This can be for a family break, a step towards independent living or long-term living.
-
Residential accommodation with or without or nursing care.
Shortlisting case studies for work package 3
Data were drawn together to assess providers against the criteria of excellence. A longlist of 15 providers was presented to both Professional and Public Advisory Groups for discussion. Following discussion within the team, eight providers were selected for the ethnographic research in WP3 across the four models and both groups A and B. One of the initial eight providers was replaced when it became clear that the innovative housing model offered was separate from the housing support. Our focus on England limited the identification of exemplars of good practice to England rather than covering all of the UK, which meant that the research did not benefit from the experiences of and differences in health and social care delivery across the four countries.
Chapter 4 Work package 3: methods
Plain language summary
-
In this chapter we talk about how we did this part of the research.
-
We used an approach called ethnography. This means hanging out with people to find out about their lives.
-
Researchers spent time with people in supported living homes, in Shared Lives homes, at day centres and in residential and nursing homes.
-
We interviewed people with learning disabilities, family carers, support workers, managers and local authority staff.
-
We also read and thought about the paperwork the providers had to help staff do a good job.
Introduction
In WP3 we set out to explore the delivery and characteristics of excellent services for older PWLD identified in WP2 using an ethnographic approach. Ethnography involves spending time with people as an observer of and participant in everyday practices and draws on interviews and sometimes documentary analysis. 107 Ethnographic research focusing on PWLD has involved flexibility and innovation as well as more traditional methods. 108,109 We introduced further innovations with co-researchers (PWLD or family carers) as part of the research team and additional online meetings between in-person visits. While this was underpinned by pragmatic considerations relating to periods of lockdown, it worked to strengthen the research and make the outputs more relevant, allowing the distinction between researcher and those being researched to become blurred. 110,111
Objective
The objective of this WP was to explore service exemplars through ethnographic case studies.
Fieldwork
Sampling and recruitment
Eight case study sites demonstrating exemplars of one of four models of provision were approached and invited to take part in the study (Table 5 details the case studies, visits, interviews and timescales for each site). WP2 identified two core groups of older PWLD, those who have greater physical and mental health needs than their peers and those who have recently been, or are about to be, discharged from long-term institutional care – our sample did not include anyone from the latter group. We did, however, include participants who would be characterised as having severe learning disabilities. We included an additional case study site (NCH_2) identified during proposal development as an exemplar in the development of a new provision for older PWLD and complex needs in an inner-city area. The delay in the development of the site led us to treat it as distinct from the other case studies.
| Provider | PWLD participants | Number of visits (days) | Number of online meetings | Number of visits with co-researcher | Number of interviews | Timescale |
|---|---|---|---|---|---|---|
| ISL_1 | 4 (2 male, 2 female) | 10 | 15 | 5 | 8 | June 2021–March 2022 |
| ISL_2 | 5 (3 male, 2 female) | 12 | 12 | 3 | 12 | June 2021–June 2022 |
| ISL_3 | 3 (2 male, 1 female) | 6 | – | – | 11 | February 2022–July 2022 |
| ISL_4 | 6 (2 male, 4 female) | 20 | 0 | 6 | 10 | March 2022–October 2022 |
| DOP_1 (day opportunity centres) | 6 (3 male, 3 female) | 12 | – | 3 | 10 | September 2021–July 2022 |
| SL_1 (Shared Lives) | 4 (3 male, 1 female) | 8 | 2 | 2 | 6 | October 2021 March 2022 |
| SL_2 | 6 (3 male, 3 female) | 8 | 0 | 3 | 8 | October 2021–April 2022 |
| NCH_1 (nursing and residential care home) | 3 (3 female) | 20 | – | 0 | 16 | November 2021–March 2022 |
| Total | 37 | 96 | 29 | 22 | 81 | June 2021–October 2022 |
Access to each case study was negotiated at provider level and then with local managers and support workers. Relevant introductions from contacts developed during WP2 were made and meetings arranged with the provider chief executive offices (CEOs) and, subsequently, other staff members to build relationships and identify potential participants. It was important that staff fully understood the point of the research and what participation would involve. It also allowed the team to find out more about the support offered. Discussions included thinking about the best ways to recruit and engage with participants and to include people who lack capacity via gaining consent by proxy from family members.
Provider DOP_1 asked to delay participation due to staff changeovers and joined the fieldwork 3 months later. Provider ISL_3 was unable to continue to commit the resources to participate because of staff sickness. It withdrew from the study, rejoining 7 months later. This resulted in fewer PWLD participants from this provider (n = 3). One provider declined to take part as the CEO felt that the organisation was not able, in pandemic conditions, to provide excellent support. A replacement provider was selected from the shortlist.
For formal interviews, a framework was produced to sample diversity including age, gender, ethnicity, family context and length of time living or working in the provision. In practice, we were limited to a sample defined by the people living and working at each of the sites, which were a mix of rural, small town, and urban, and our sample was White British. Ages ranged between 40 and 70 years.
Developing co-research training materials and delivering co-researcher training
It was important to involve PWLD and family carers in a form of ‘co-operative experiential inquiry’,112 conducting the research with rather than on PWLD. 113 We co-designed training resources to facilitate the involvement of PWLD and family carers as ethnographers and to support academic researchers to facilitate co-research. We were mindful that people had key skills of observation and listening and wanted to draw these out without imposing constraints on conventional means of research. 114
This work was supported by engagement funding from the NIHR School for Primary Care Research and is reported in Mikulak et al. 115 We recruited a small team comprising academics (n = 3), a Public Involvement co-ordinator and family carer, PWLD (n = 2), and two further family carers. The resources, developed through online workshops and an ethnographic exercise, are publicly available at www.mmu.ac.uk/research/research-centres/hpac/projects/growing-older-planning-ahead.
Ethics
Informed consent was sought from all participants who were deemed to have capacity to consent. Participants with learning disabilities were given Easy Read information sheets about the study and Easy Read consent forms. They were encouraged to complete these with the researcher and a trusted person such as a family member or support team member. The researchers went through the consent form with the participants (and, where appropriate, with their trusted person) and made sure participants had a chance to ask questions and understood their right to withdraw consent at any point, before the consent form was signed on two copies by the participants and the researcher. Participants retained one copy of the consent form. Consent for participants who were deemed to not have capacity was sought through a consultee. In all cases when this process was used, the consultee was a parent of the participant, had an intimate knowledge of and regular contact with the participant and deemed the person’s participation to be in their best interest.
Data generation
The move of co-principal investigator Ryan to Manchester Metropolitan University in May 2021 necessitated an ethics amendment and subsequent delay in starting the fieldwork. In the interim, the time was used to engage with the sites online. We learnt that considerable input and encouragement of support staff, which included making clear the point and importance of the research, was necessary to ensure engagement, particularly given staff shortages and other constraints.
Longitudinal observations, interviews and documentary analysis were used to understand how people were supported in their everyday lives, how they negotiated ageing, and how ‘BTCO’ were understood and ameliorated. In total, researchers spent between 12 and 25 days, including some weekends and evenings, at sites within the four models of care. Co-researchers were present at around 30% of the visits. While originally structured to take place an average of 2 days a week, the geographical location of the sites, and COVID-19-related disruption, meant that visits were organised flexibly, working around last-minute changes to plans caused by illness or staff absences. The number of visits was balanced against their duration (fewer visits meant the visits were longer).
Detailed field notes were kept that included a description of the setting, interactions between people, objects and the environment, emotions, impressions and reflections. Interviews with PWLD, their family members, support workers, provider managers and commissioners were conducted for each site allowing us to develop our understanding of the conditions necessary to provide excellent support (Table 6). An interview schedule was used (see Report Supplementary Material 9), although the process was flexible, allowing participants to introduce issues they felt were important. Interviews, at a participant’s home or online/by telephone, lasted 20 minutes to 2 hours, were recorded with permission and were transcribed verbatim.
| PWLD interview and observations | PWLD ethnographic observations only | Interviews: carers/family | Interviews: support workers and local staff | Interviews: commissioners and service managers | Total | |
|---|---|---|---|---|---|---|
| ISL_1 | 1 | 3 | 1 | 2 | 1 | 8 |
| ISL_2 | 1 | 4 | 1 | 4 | 2 | 12 |
| ISL_3 | 1 | 2 | 1 | 4 | 3 | 11 |
| ISL_4 | 4 | 2 | 1 | 3 | 2 | 12 |
| DOP_1 | 3 | 3 | 3 | 2 | 2 | 13 |
| SL_1 | 0 | 4 | 1 | 2 | 2 | 9 |
| SL_2 | 0 | 6 | 3 | 4 | 1 | 14 |
| NCH_1 | 3 | 0 | 6 | 5 | 2 | 16 |
| Total | 13 | 24 | 17 | 26 | 15 | 95 |
Independent supported living
Based on WP2 (see Chapter 3), three providers offering ISL services were selected: a social enterprise provider in the north of England (ISL_1); a large, not-for-profit national organisation (ISL_2); and a small, limited company provider operating in the south (ISL_3). An add-on site (ISL_4), a not-for-profit charity, was identified that provided exemplary care and support for older PWLD in a deprived area of northern England. Support ranged from 24 hours of one-to-one support with two-to-one support for going out, to a few hours of one-to-one support per week. In-person ethnographic visits lasted 2–6 hours and revolved around participants’ timetables, with researcher(s) taking part in activities or shadowing (arts and crafts, drama, walks in town/city and in nature, shopping, outings for coffee, going to the cinema, picnics and drives, going to a day centre) and spending time in participants’ homes. Most visits took place on weekdays, including evenings; however, a minimum of one weekend visit was included for each provider. Online meetings took place between in-person visits, during weekdays, and lasted between 15 and 30 minutes.
Day centres
One provider (DOP_1), a charity operating community hubs in the Midlands, was included. Participants were recruited from two hubs with older PWLD. Of the six participants (three from each hub), four lived alone (one person paid for a few hours of support and one person had a few hours of support from the provider), one lived with their parents and one person lived next door to their sister.
In-person visits lasted 3–7 hours during hub opening hours (9 a.m.–4 p.m.), with researcher(s) taking part in and/or shadowing activities (arts, crafts, cooking, board games, computer games, chair yoga) and shadowing participants on outings. The hubs closed at weekends.
Shared Lives
Shared Lives is a model in which people with a wide range of support needs, including PWLD, autistic people, young care leavers and people with dementia, live in their local community with families. Two exemplary schemes were selected from WP2: one based in a northern city (SL_1) and one in the south-west (SL_2). Participants used respite Shared Lives or lived full time with families, and visits included spending time at the Shared Lives home or going out with the Shared Lives carer and participants.
Nursing care home
Nursing and Residential Care Home_1 is a nursing care home in a large market town in northern England. The service provides support to 4 households of 6 PWLD and additional nursing care needs (24 people in total).
Ethnographic observations focused on three participants. Visits to the site lasted approximately 3–4 hours, including mornings, afternoons, evenings and weekends. The stories of two men who had died in the nursing care home before the research took place were included in interviews with their relatives and the staff team.
The co-research team
We recruited and trained a team of co-researchers, PWLD (n = 8) and family carers (n = 1) using the co-designed training resource discussed above. The aim was for 50% of the visits to sites to be with a co-researcher other than the two nursing home sites. In practice, this was not possible, due to individual preferences of participants, inaccessibility of certain sites, and availability of co-researchers.
Observations from co-researchers were documented in various ways. The team’s preference where possible was for the researcher and co-researcher to go somewhere quiet to talk about the day and the researcher to take notes. This was not always possible and a debrief was sometimes held online, or by telephone, later in the day, or the following day. Three informal online meetings were held with the co-research team, which generated additional observations about the sites.
Co-researchers brought their knowledge and expertise to the research. For example, one researcher drew on her experiences as a wheelchair user to comment on the lives and home of two participants who used wheelchairs. Others were able to reflect on their experiences as quality checkers for the CQC. Co-researchers local to the site area also brought expert knowledge of local places, venues and self-advocacy.
Policy documentary review
Relevant policy documents were requested from each site. These focused on how the organisations support PWLD and ‘BTCO’ as well as on the design and delivery of support around growing older and EOLC. ‘BTCO’-related documents included those explicitly focused on ‘BTCO’ and those relating to reducing restrictive practice and physical interventions, and mental capacity. For sites without EOLC documents, documents relating to health and well-being were reviewed. See Report Supplementary Material 10 for included documents.
Data analysis
Data analysis was conducted alongside fieldwork, with researchers comprehensively familiarising themselves with the observation notes, interview transcripts and policy documents. These data sets were entered into NVivo (QSR International, Warrington, UK) and thematically analysed. The research team open-coded data, meeting to discuss developing coding frameworks. Coding categories were flexible, and an iterative approach to this first stage of analysis incorporated alternating between transcripts, notes, codes and categories as new codes was identified. A more conceptual analysis involved selecting particularly rich and relevant categories, reading and re-reading the data, generating themes, making links, identifying patterns and thinking about the data in a less linear and descriptive way. Meaning, action and process were used as an interpretive analytic lens to understand how participants understand and make sense of their lives, their actions and their interactions. Our aim was to capture the micro-detail of how participants live their lives and engage with other people at home and in the community.
The policy documents were also analysed using NVivo. In addition to the content, we reviewed their intended audience and authorship, references to research and external standards, accessibility of language, and the process of reviewing and updating them. Existing policies were aimed predominantly at staff. The documents were up to date, with frequent revisions and version history stated.
We did not plan to involve co-researchers in data analysis because of the quantity of textual data involved. 116 However, insights generated during fieldwork led us to revise this. Two analysis workshops were held with two co-researchers and a support worker, which involved close audio examination of data extracts where participants talked about ‘BTCO’ (Mikulak et al., in preparation).
Nursing Care Home 2: the commissioning and development of a new inner-city service
Nursing Care Home 2 (NCH_2) was identified during the original proposal design development; however, the opening of this service was delayed. Following discussions with the project team and Advisory Groups, we agreed to continue to research NCH_2 to generate insights into the process of planning a new service specifically for this group. In addition, NCH_2 enabled us to consider the potential benefits and challenges involved in commissioning an inner-city service for older PWLD and ‘BTCO’, in the light of key policy drivers to keep people within their local communities. 23,80,102,117,118
The local context and proposed site
The provision is for a large residential care home with nursing (up to 70 beds), with 10 beds reserved specifically for a ‘household’ for older PWLD and those with complex physical and mental health needs (including people with ‘BTCO’). The planned build is on the site of a previous older people’s care home. It is a spacious inner-city site in the heart of the community. Plans involve the development of an outward-facing community café to support community engagement.
Data generation and analysis
The team drew on ethnographic methods, mirroring other sites with certain methodological adaptations. For example, documentary data gathering included Cabinet Meeting minutes, Equality Impact Assessments, public consultations, and responses to public consultations that detailed the closure of the existing care home and the plans for its redevelopment. Interviews were recorded with the service development project manager, lead commissioner, a local councillor, and the chairperson of a parent carer group. The interview schedule was adapted to include questions about the co-design process. Further information was requested from the project data analyst, who provided a snapshot of data about PWLD currently receiving a package from the LA. Observation notes were made at a ‘co-design group’ meeting held to discuss the plans for the 10-bed household. Data were thematically analysed in NVivo. The analysis was further discussed and refined in a series of team workshops.
Chapter 5 Findings of the ethnographic research
Plain language summary
-
What we found can be divided into things that relate to the person’s home and where it is, how support is organised and how people with learning disabilities are supported to have a social life.
-
We saw examples of good practice that helped people to lead fulfilling, healthy lives as they got older, which included making sure people were supported by staff they liked and knew well.
-
We were surprised to find some people had very little choice about where they lived, who they lived with, who supported them, and how they spent their time.
-
We also found out that most services and staff were not thinking enough about how to support people as they grow older.
-
We found that ‘behaviours that challenge others’ sometimes decreased or stopped when people started getting good support.
Here we present our ethnographic findings, which we have organised around three key factors, environmental, organisational and social, that are interconnected but can be analysed as distinct themes. We draw together similarities, differences and strengths of the four models in the Discussion section (Table 7).
| Independent supported living (ISL_1, ISL_2, ISL_3, ISL_4) | Shared Lives (SL_1, SL_2) |
| Day opportunity centres (DOP_1) | Nursing and residential care home (NCH_1) |
Environmental factors
Environmental factors relate to the person’s house, flat or room, its location and its characteristics. It is important that people live in accessible accommodation that can be adapted as they grow older. It should feel like home and be secure, permanent and personal.
Homely homes
Independent supported living
There were varying configurations within the ISL model that ranged from people living alone in their own home to having a one-bedroom flat in a purpose-built block with shared living spaces. Some participants lived in shared houses with four other PWLD. Participants who lived by themselves with appropriate levels of support reported feeling house proud and happy:
‘You’ve got a lovely home, Z’, I say. ‘I do, don’t I’, says Z proudly. I think that’s what ‘house-proud’ looks like. The place feels homely, simple, but warm (figuratively and literally as the heating is on) and lived in … ‘Z is very proud of it [the house]’, says B, ‘yeah, I hope I can stay here forever and ever’, says Z.
ISL_2, ethnography notes 26 October 2021
‘How long have you lived here then, N?’ ‘5 years,’ C says. ‘And you live just around the corner?’ I ask her. ‘Yes, just down there’, she gestures. ‘That’s nice’. ‘Yes’, says N. C then tells me they were looking for a house for N and this came on the market. She thought it was perfect. Close to hers. Close to N’s brother – he lives nearby too.
ISL_3, ethnography notes 7 February 2022
Shared Lives
Because Shared Lives homes are precisely that, homes, their comfort, homeliness, and welcoming environment was apparent. H, for example, described her home as ‘very posh and nice’, and researcher notes describe how:
I arrived at the house and made my way through the small, pretty and extremely neat garden. Adorned with garden ornaments, plants and a water feature, it felt cheerful. R answered the door and welcomed me in. I have met R and H before – online and at [day centre] – but this was my first visit to their home. It was lovely. Very clean and fresh, cosy and homely. […] Photos and art covered the walls, and the furnishings were in cosy reds, green, oranges. There were lots of ornaments and trinkets – everything seemed to have a place.
SL_1, ethnography notes 13 October 2021
Nursing care home
NCH_1 is set in a cul-de-sac in the suburbs of a large market town and made up of four bungalows, each of which has six residents. The buildings are light and airy and welcoming. There is a large lounge, a small kitchen, a quiet room, an office, six bedrooms and several bathrooms.
While six people live in the home, staff are aware of the importance of the space being homely and support people to create spaces that are theirs. This includes shared spaces (e.g. S displaying her cards, flowers, framed photos, and other family mementos in a deep window recess in the shared lounge) and bedrooms.
C’s room appears very warm and comfortably furnished. Everything is co-ordinated in shades of purple – cushions, sheet, duvet cover, blankets, chair upholstery, blind, walls, lamp shade, vase, artificial flowers … C has a single bed in the middle of the room and wardrobes, chests of drawers, dressing table and sink against the walls.
NCH_1, ethnography notes 30 November 2021
Access to the outdoors
It is important to be able to enjoy the outdoors, by, for example, having a garden where people can grow plants and food, display their art, and relax. Across the four models there were various examples of participants enjoying being outside. ISL_4 has a small, enclosed garden where people are encouraged and supported to grow plants and vegetables. G (SL_2) lives on a smallholding with geese, chickens, ducks, pigs, sheep and goats; he loves working on it and spends most of his time outside. The nursing home bungalows have gardens with plants in big pots, garden ornaments, bird feeders and several places to sit:
R [SL carer] suggested that C take us up to the chickens when she feeds them. The garden was amazing. It was full of lots of different plants and trees around the edges and in the middle there was a big lawn. At the very top of the garden there were lots of chickens and 3 running ducks … I followed C to the chicken pen, together they let the three ducks out into the main garden to go for a run, they set the water going and placed the hose into an inflatable paddling pool so that the ducks could have a splash around in that.
SL_2, ethnography notes 30 April 2022
Z shows me around the garden. The space is beautiful, sunny and there are more sculptures than last time. They are all full of character and just fun … Cups of tea still in hand we walk to a small sitting area in the far corner of the garden. C, who is at the sink in the kitchen opens the window and says ‘you can bring the chairs here, Z’. Z and I carry a chair each and put them next to one that is already by the house, in a half circle facing the garden, and the sculptures.
ISL_2, ethnography notes 26 March 2022
Accessibility of location and transport links
Location is important for accessibility and access to public transport. Being able to walk or get around the neighbourhood and access local amenities meant that participants were not reliant on support staff driving and were less likely to become isolated:
It is a beautiful, warm, sunny day and the town where C lives is lovely, so we (researcher and participant) are going to go for a stroll and have coffee out. As I approach the flats where C live, I can see him and T [support worker] waiting at the gate … ‘Hello!’ ‘Hello! Hi, C, hi, T!’ … Then T says ‘right, C is all set, he has some money to treat you to a coffee. He knows where he wants to go … There is a café in a garden centre, C likes it there’.
ISL_2, ethnography notes 23 March 2022
The day activity hubs (DOP_1) were distinct in terms of their location and physical layout, which impacted how welcoming, integrated and convivial they felt. The first hub, located in the town centre, was closely linked to the local community, with easy access to leisure, shopping and food venues. People could access it by public transport (S), on foot (N) or by mobility scooter (J). This contributed to a vibrant atmosphere and constant flow of people, visitors and family members. Although not open to the public, the hub felt welcoming, where people could come in to have a chat and a cup of tea. The main large, open-space room was conducive to social interaction and banter, facilitated by friendly, approachable and caring staff. The managers’ office, located next to the reception, staffed mainly by people who use the hub, was open to all and the door was rarely closed. Additional rooms (new, spacious kitchen, a large meeting room) provided space for activities. There was a sense of community, togetherness and familiarity between the people who use the hub and work there.
The second hub, located in a business park, did not share the same characteristics, and people using it were shuttled in and out by staff. This meant that shortages of staff could result in cancelled activities/outings. Its physical layout across two buildings, with a myriad of small rooms, was also less conducive to socialising; however, the large, bright kitchen functioned as a meeting space, where people and staff interacted organically, outside the assigned rooms and groups.
Use of day centres
The Shared Lives sites also involved the use of day centres, which is an integral part of the scheme. This generates contradiction when living an ordinary life is fractured with segregated day activities. This was discussed in an interview with a commissioner:
And I keep thinking and going back to that Adult Family Placement – those days when it was Adult Family Placement – because I think things changed from then when it moved to Shared Lives. And there’s a focus around having to have the day provision element. I think it loses that sense of being part of the family, when you start looking at the fact that somebody needs to have a day provision or respite.
SL_1
Researchers spent time at a day centre associated with SL_1 and found that people of different ages spent a long time indoors, doing activities that might not be of much interest to them:
The Group, including H, were very engaged with the activity about Christmas words. We are now moving on to seated yoga and people seem to be less interested in this. They have been in the same place for quite some time now and I get the impression that there is a shared feeling of restlessness. Some people from the group are stood or wandering around the room, and this increases over the next 30 minutes.
SL_1, ethnography notes 30 November 2021
The importance of who you live with
For some participants, related to the sense of security that comes with having a home that feels permanent is living alone (or with a partner). This allows people to have control over their private lives in ways that PWLD have historically been denied, and in some settings continue to be denied. This view was reflected by some ISL providers who framed the right to live alone as a question of social justice. One commissioner, for example, said that people should be entitled to have their own front door, with support, while the ISL_3 CEO stated:
When you do really good planning with people, the right thing was for people to have their own home, the same as you and I. So that was the first principle, was people having their own home.
ISL_3, emphasis added
The value of having one’s own home was echoed in conversations with participants and their families. For example, one mother described how her son had always wanted his own house and two cats. We found that people tended to be grouped together in supported living settings, creating situations where they lack agency and security. When people live in groups of four or five, their private lives are intertwined with that of their housemates, who may be strangers, in ways that reproduce models of institutional care. This can be of particular concern for older PWLD, who can find house sharing busy, noisy and detrimental to their well-being. Lack of privacy and conflict with housemates were additional sources of stress:
When I get to (participant’s) room I ask if I should close the door and she (participant) says ‘yeah, close it’. With the door closed, the room feels much cosier and calmer. The door is a two-part situation, with stops at the bottom on both sides. I doubt C can close and open it herself … The house is noisy … I then remember C moved to this house recently so I ask her about that … ‘Remind me why you wanted to leave the last place?’ ‘It was because of M, he was always making noises, was loud. Was getting on my nerves’, C says. ‘And is it better here?’ I ask. ‘Not really’, C says.
ISL_1, ethnography notes 7 June 2022
Within the nursing home there was a question about the appropriateness of the collective setting for one participant. The history of abuse and institutionalisation some PWLD have experienced has led to conflict between residents:
The clinical nurse shared that staff query whether C’s current placement is suitable as they predominantly support people with profound disability and complex health needs, but also asked ‘where else would she go’? The residents who share the bungalow with C are vulnerable because they cannot get out of her way, which is why we try to manage her behaviours in the way we do.
NCH_1, interview with clinical lead nurse
Organisational factors
Careful staff matching, good relationships with support staff and consistency and continuity of support teams are key to leading a good life in older age. In addition, excellent practice includes involving people in the recruitment process of their support staff. These organisational factors reflect the ethos of the organisation, which is translated into management and daily operations.
Staff recruitment, matching, support and consistency
Our research found that the culture and practices around staff recruitment, matching and consistency are key for people leading good lives and dying well.
Involvement of people with learning disabilities in recruitment
Including people and their families in staff recruitment allows an additional level of control, honouring people’s agency and preferences in a crucial aspect of people’s lives. The CEO of ISL_3 explained the careful process and deliberate design behind staff matching, which includes finding out about the person’s background and what support has worked well and what has not to create the job advert:
People would put their names forward if they thought they were a match to that and then they would be interviewed by us and the family or us and the person, depending on how that goes and we’ll work it out from that point to see if they are a match or not, even if they are, the person has a third-party agreement and the contract is a third-party agreement which means that person or their family can say this is not working and then we would take that person out the team … So family and people have total empowerment about who works with them.
ISL_3, interview with CEO
Staff consistency and matching
Staff consistency is also important in enabling relationships and friendships to develop and flourish over time:
‘How long have you two known each other?’ I ask. ’11 years’, says D. ‘Wow! That’s long’. ‘Yes, I’ve been on your team from the start, haven’t’ I, H?’ H nods.
ISL_3, ethnography notes 7 February 2022
B goes over to S and asks if she’d like a picture on her table. S chooses (actor) B says ‘How could I forget? You love her. Shall I sit with you for a while and chat about her?’ B sits very close to S and chats about the TV programmes the actor has been in and what is so lovely about her. They have a very quiet and intimate chat for about 20 minutes. S is asleep in her wheelchair, hugging the cushion with her mother’s photo on it.
NCH_1, ethnography notes 1 March 2022
Well from the first time I went through the door I got a really good feeling about it and the way they responded to her and communicated with her and she’s chatting back … And she treats them all as a friend and she’s cheeky to them, they’re cheeky to her and it’s just so personal, it really is … I think basically it’s a case of people who genuinely care about what they’re doing. And it’s not just a job.
NCH_1, interview with S’s brother
A careful matching process also happens between Shared Lives carers and the people they support. On the part of the provider, this requires detailed knowledge of their workforce and their strengths:
We really hone in on what their (SL carers’) skills are and who they want to support. So when the referral comes in, we’re quickly able to align those two up. So if you get a mental health referral in, or if you get a referral in for dementia, we know very quickly from our database what carers we’ve got that will match those skills up.
SL_2, interview with Shared Lives co-ordinator
Staff recruitment at the nursing home is similarly informed by the ethos of the organisation, and the interview process is designed to identify people who are right for the job because they have the right values, are kind and compassionate and treat people with dignity:
It’s really difficult to get that balance right … I mean, we did some interviews the other week, me and [manager], but we didn’t employ either of the staff because they just didn’t seem to have the right qualities … but it is difficult with recruitment because obviously you know we have … vacancies, we have 1:1 hours. So it’s almost like you do want to fill the hours, but I think we are … trying to make sure we only take on people who do seem to have them qualities.
NCH_1, interview with clinical lead nurse
In practice, commitment to staffing consistency goes hand in hand with the ambition to not replicate institutional models of care, and this is operationalised by not relying on agency staff:
I’ve also worked for organisations where they’ve just, you know, an agency member will turn up and they haven’t even been able to read the working policy (support plan) … they don’t know the person, they know nothing about the person and to these people (PWLD), it’s all they have in hospitals and institutes, so why the hell would you replicate that in their own home? It’s something that we’ve said is going to be theirs. With the safety and the security of knowing the people around them, that they know who’s who.
ISL_3, interview with team leader, emphasis added
So the care workers and the nurses work across the whole of the bungalows and there’s not a big change round of staff. So that again as a commissioner is we look at that and think, you know, the sort of camaraderie is always one of the most important things. We always look at whether, turnover of staff, whether they use agency staff, it’s that continuity of care, you know, and look at the CQC reports, and they’ve always been really, really good.
NCH_1, interview with CCG care commissioner
For people who do not communicate with words
For people who do not communicate with words, having staff who knew and understood their preferences and who ‘got them’ was key to their receiving good support:
I ask A (support worker) how long she has known N (participant) and she says it’s been ‘good few years’; she then explains that she used to work with (the provider) and support N before moving to (region) for a bit, she got back this year and started working for DOP_1 again. She says people often come to her to ask about N, cause of how long and how well she knows her … She says that N is very different with different people who support her and that she is very chill with A. ‘Maybe cause I’m chill’, she adds.
DOP_1, ethnography notes 17 November 2021
In palliative care
Staff retention is known to contribute to consistency of care and the deepening of reciprocal relationships between staff and residents. In NCH_1 all staff have training in specialist palliative care, which means that people who are approaching the end of their lives can stay with and receive care from the people who know them well and have strong links with their families. Consistency of staffing provides an additional level of comfort and familiarity to people receiving palliative care:
When I go to do reviews, there’s always the, you know where (the nursing care home) is, right next door is the hospice. Now the majority of people that come to end-of-life care will go to the hospice. But it’s written in all the care plans and support plans, and they’ve gone through best interest, capacity, and everything that the person will remain in-house for that end-of-life care. All the staff have been trained for palliative care, and because of the qualified nurses that are there, that person has got that continuity and that regular person that they see every day and that fully supports in their end-of-life care.
NCH_1, interview with CCG care commissioner
Although not all staff stayed in their roles, the nursing home had many long-term employees. Opportunities to develop their knowledge and skills and the supportive management team contributed to staff retention. Positive feedback from families of people who died in NCH_1 also mattered:
You’ve got some staff that’s been there for 30 years. I’ve been there 7 years now, so anywhere between 5 and 30 years we’ve got quite a big number of staff. But then we still seem to have some that come and go. It’s really difficult, we don’t know how we retain them? I’d hope the staff that we have retained it’s because they like (NCH_1) and the way we work and … the homely atmosphere, the fact that it does seem caring. And the different families we’ve had come through the years and the positive feedback, I think helps. So, the families of the clients we’ve got now that were really positive and the clients who have died well with us after living there for however long, we’ve had really positive feedback from them.
NCH_1, interview with clinical lead nurse
Good support was also reflected in staff at times going above and beyond what was expected in their roles, and it meant that family members felt confident that their relatives were safe, valued and cared for. M’s brother said that one staff member had stayed with a resident overnight in hospital during her own time.
Network of professionals
A strong element of the working culture at the nursing home was the way in which enduring relationships had been established with a wide range of fellow healthcare professionals, including the learning disability physiotherapist, learning disability occupational therapists, the complex needs matron, the hospice and the epilepsy nurse. A commissioner flagged up that the provider was open to new suggestions and ideas and how they looked for help from outside services. In practice, this resulted in people’s health needs being addressed quickly, often through staff advocating on their behalf. The collaborative approach, active promotion and maintenance of professional networking resulted in better care as well as consideration of people’s futures. The ethos of the organisation was described as ‘helping people to live well until they die’, which involved supporting people to live life without limits, making decisions about their lives and their future:
We want people to feel there is no restrictions on what they want to do, what they want to achieve and think health-wise from a health point of view thinking about some people have been born with life-limiting conditions and that, whether we like that or not, will have some impact on the life expectancy or their quality of life. So we need to know that now so that we can plan for that time in the future … And it’s no good finding yourself suddenly trying to find a special bed for someone or a special service, you’ve got to have already done that legwork and know where you’re going to get things from and who you’re going to go to.
NCH_1, interview with training and development officer
Open doors culture
In DOP_1, long-standing relationships with staff, particularly managers, who made themselves available to people through an open-door culture and kept in touch on a regular basis, regardless of allocated support hours at the hub, were important. An open-door culture meant that managers were close to people and knew them as individuals:
NW leaves and I (the researcher) stop at H’s office to mention a couple of the things NW has talked about and that she might need checking in, ‘cause some of it was clearly upsetting to her. H thanks me for letting her know and says that even though NW only has a couple of hours of support weekly, they speak every day and that she will phone her now so she can come back for a cup of tea and a chat ‘just to make sure she is ok’.
DOP_1, ethnography notes 12 May 2022
It’s almost 4 and R (support worker) tells J (participant) he needs to get ready to leave. J gets up and goes to F (manager) office. R says J cannot leave without talking to F … Before I leave I stop at F’s office too. I tell her I’ll be back to see J and S on Friday. She says that’s great and that it might be good to play a game of (board game) with J. ‘Would be a good way to engage him’.
DOP_1, ethnography notes 16 November 2021
Trust, recovery and moving on from the label of ‘behaviours that challenge others’
The trust that is built by staff matching and consistency, and good relationships, means that PWLD can be supported to recover from past institutional trauma and, at times, shed the label of ‘BTCO’. This was apparent across the four models of support:
And then over time, H has just no need to engage in those types of behaviours any more – trusts the people that are supporting her, she trusts that they have her best [interest] kind of at heart … I was always told the idea is to eventually do ourselves out of a job. And that is true. I’ve just said to you with [ISL_3H] we’ve gone from 24 hours 7 days a week to the 10-hour shifts, 8- to 10-hour shifts and I know she’ll be half that once she’s married, so you can see, that is the achievement, that is the goal.
ISL_3, interview with service manager
I never thought I would be able to live like this, to have a house, to have a fiancé.
ISL_3, ethnography notes 7 February 2022
I:So that’s really interesting, so basically she was considered ‘challenging’ at a time when she wasn’t supported well.
P:Yeah, it wasn’t her … So you know, if she tells me anything like that then I will most generally be on F’s side because it would mean that there was something wrong … generally if she’s being treated properly, then she’s fine … Well … the whole set-up was not that good, but there was one particular carer who I think she was just very bossy and very domineering like that, and I think F hit her. But that was because … well, she was effectively bullying her (…).
I:And that has never happened at (the hub) and there were never any issues?
P:No … we’ve never had anything like that with (the provider). Not at all.
DOP_1, interview with sister
She was in (ATU) before she came here … When she came here her behaviours were really challenging. We couldn’t shower her, no personal care. She would hardly wear clothes and we have to actually work from that stage to where she is now. I can say we’ve come a far way because now we can shower her, we can actually get her out. We’ve taken her out, which she wouldn’t leave the bungalow at any time.
NCH_1, interview with C’s key worker
The long-term impact of experiences of abuse can be substantial. G was assaulted as a young adult and moved from his family farm to an institution where he lived for several decades, eventually moving in with two Shared Lives carers in a rural setting:
Now, on an evening, G sometimes – when he is in his chair in front of the fire – will say ‘they didn’t need to put I in there’ and ‘they shouldn’t have done that to I’.
SL_2, ethnography notes 3 November 2021
Values and ethos on paper and in practice
A further factor in good support is the culture, values and ethos of the organisation and how these are operationalised in the daily work of staff. In practice, putting the interests of the people being supported first could be seen as a benchmark of person-centred support. The CEO of ISL_3 described how important it is to not let:
the money and the business to turn your head and not allowing, not also wanting to be popular at the expense of somebody else’s life. If you put the person at the centre, you’ve got to stand up to that. (emphasis added)
ISL_4 was described as value-based with person-centredness at its core. There are house champions who take on various roles, and this aims to help people develop skills:
And you know we’ve got one client who if you park in the wrong space or you haven’t moved your car further up, he’ll try and find you to tell you to move it up or if he knows a staff member’s leaving and you might be parked behind them, he’ll try to find you to tell you to move your car. So we looked at that and we said, ‘Well that’s something he likes doing and it’s a strength’, so we made him Car Park Champion.
ISL_4, interview with manager
These values are captured in the documents and policies of the organisations. Most policies analysed referred to relevant legal frameworks and regulations and policies on restrictive practice and ‘BTCO’ referred to The Mental Capacity Act 2005,119 Mental Health Act Code of Practice120 and Deprivation of Liberty Safeguards. 121 Some policies were notable for also including clear value statements and additional references to external standards such as the Equality and Human Rights Commission (EHRC)122 in the definition of restraint:
The Human Rights Framework for Restraint (2019) by the EHRC defines restraint as an act carried out with the purpose of restricting an individual’s movement, liberty and/or freedom to act independently. […] The main aim of this policy is to promote the prevention and to minimise the use of any restrictive practice […]
Reducing Restrictive Practice policy from ISL_3, pp. 3, 15
More nuanced policy examples included clear, concise language and consistently value-driven and value-focused language:
We believe we need to meet people’s needs proactively – that is, before they must resort to challenging behaviour. The first step in meeting people’s needs is to improve their quality of life. In addition to reflecting an ethical approach, improving quality of life often eliminates or minimises many of the triggers for challenging behaviour.
Employee handbook, DOP_1
Clear and concise language was supplemented by concrete examples that were informative and simple to understand:
We do not allow the use of punishment. Here are some examples of punishment strategies which are not acceptable in [provider] services:
A man is smacked or told off because he smashed a window.
A woman who urinates on the bathroom floor is made to mop the floor and then clean the entire bathroom.
Employee handbook, DOP_1, p. 206
Ambitious and aspirational support
While respect for people and being committed to their well-being and safety are characteristic of all good support, excellent support goes further in also being ambitious and aspirational in supporting people to live full lives:
It can be a lowest common denominator industry sometimes. By that I mean sometimes it’s not very aspirational for people, it’s almost a bit paternalistic … I’m not interested in the local authority payment and going making sure someone gets a sandwich. Now that’s important. But what’s more important to me is that they get a life, because the sandwich will not be important if they get a life.
ISL_3, interview with CEO
Active commissioning
There was evidence of active and thoughtful commissioners behind some of the excellent support we observed. One commissioner, for example, described how they had got the providers together in a room to listen to the problems they had identified in the area. This had led to the decision to provide a weekend and annual contingency fund for each provider to enable PWLD to lead a good life. The commissioner described how this is done:
You’ve got the information, you know, let’s go back to the guy that likes surfing, likes to feel the sand between his toes, likes to run in and out of the water, take him away for the weekend. Take him surfing. Does he miss his parents? Pay for his parents to come down on the train and see them. Take him away for a little holiday with his parents. Whatever it is. Do something that is not restricted, do something that is not ‘care delivery’ [participant makes air quotes signs].
ISL_3, commissioner
Ageing, health and end-of-life care
Many providers did not have a specific EOLC policy document, pointing to a gap in how ageing and EOLC are approached. The policies that exist drew on external guidelines and could signal the values of the organisation. One EOLC policy, for example, stated ‘It is our policy to ensure that those near the EOL are comfortable and that their wishes and rights are upheld and respected’, before going on to list guidelines by NICE and the Department of Health and Social Care (End of Life Care and Death Policy and Procedure 2020, ISL_1).
ISL_1 also had a mechanism to record the wishes of people they support through a ‘life celebration’ booklet, which also served as a means to have ‘open discussions about death and dying’ (End of Life Care and Death Policy and Procedure 2020). Similarly, SL_2 had a booklet about when a person dies that includes yes/no questions around EOLC, for example, ‘I have decided that I would like to be cremated; Yes No (circle choice)’.
There was little focus on death and dying or EOLC in the support offered by DOP_1. At the same time, despite the level of the support people received (often limited to a few hours a week) explicit attention was paid to forward planning and ageing that involved working with families and social workers:
We work very closely with social workers. So currently I’m working with a social worker, and the family of somebody we support. Currently she lives quite independently. But receives a lot of support from her elderly parents as well. They’re both in their 80s. So we’re working at the moment with the view to her having some different accommodation in the near future, which then obviously alleviates the position, you know, takes the pressure off of mum and dad as well. She’s also a lady … she’s not that old herself, but she has got cerebral palsy, so as she grows older her needs will significantly change. So yeah, it’s sort of like working alongside social care really. And the families.
DOP_1, interview with hub manager
End-of-life care plans were mandatory in ISL_4, unless the person supported clearly objected to such plans. A Death and Dying Policy was also in place to structure the phase after a PWLD has died. This underlined the importance of staff and PWLD being able to talk freely about their emotions and feelings. Our analysis suggests a weighting towards the well-being of staff in this area, which could be to enable good EOLC care.
Managers can support staff to do this in one-to-one meetings and in group settings. This acknowledges the importance of staff and confirms the importance and value of their contribution to good care. ‘It is important to recognise that grief may take some time to surface in staff’ (Dealing with the Death of a Client Policy, ISL_4).
The policies related to EOLC from this provider highlighted choice and dignity as goals for people dying in the service.
In the year before fieldwork began in ISL_4, the service had dealt with the sudden deaths of two people, and this resonated throughout the visits, offering examples of how death was dealt with. For example, there was an obituary on the lobby blackboard about one of the people who died, and an annual remembrance event was reported for another person:
Then, support worker tells me that N was a lover of fish and chips and when her death anniversary came up recently, [the service] organised Fish and Chips for everyone to have a remembrance dinner for her. Support worker continues: ‘They are very good at doing such things’.
ISL_4, ethnography notes 12 July 2022
The advice to hold annual remembrances is part of the provider’s EOL policy, and this was discussed in interviews with staff:
And then right at the back is their funeral plans, where they want to be buried. And even down to, I mean, some of them in there have got their funerals paid for. They know exactly what, even down to what flowers they want on the coffin, what hymns they want, which vicar they want, which kind of made me smile, because I thought by the time you’ll get to your place, that place in life, that vicar has probably gone way before you. They’ve picked the church, so yeah, they are encouraged.
ISL_4, interview with staff member
Staff received mandatory EOL training, which, in principle, meant that people could live at home with knowledgeable and skilled staff to support them:
But if the staff are well informed and well trained, they can support people to stay at [the service]. Is about, that question about where people want to die, and whether the service could accommodate that person as well.
ISL_4, interview with senior administrative staff member
There were some tensions in practice around these policies. For example, one participant frequently pointed out that he was not allowed to talk about his grief when certain staff members were around. This was raised in a staff interview, and it was explained that while the participant has the right to grieve, other people living there may not want to think about death, so staff try to manage this in a one-to-one situation. This points to a difficulty around congregate living settings. Some staff described being emotionally affected by the deaths of the people they supported and avoided talking about their experiences on this subject.
The nursing home has also developed a comprehensive guide to EOLC. The plan focuses on living well and acknowledges that people might have health issues that will probably be exacerbated as they get older. Using this guide, the support team can anticipate the health problems that people may experience and be proactive in addressing these.
It’s a lifelong package of care […] and we’ve got a leaflet explaining what that is, but it starts off at optimum health. So that is the best that somebody is going to be mentally, physically, emotionally. But that’s the stage you would involve families because that is the best that somebody’s going to ever be. But then you move up. It’s like a ladder, so you move up. So it moves to congenital abnormalities. So a lot of our clients are born with conditions or health issues as they’re born which will have an impact on their life. But it’s looking at all these, like Down’s syndrome, cerebral palsy, all those conditions in themselves will have health issues as somebody gets older, but it’s looking at those issues early, anticipating, so that you’re being proactive all the time.
NCH_1, interview with nurse
Besides planning for health-related changes, ageing well involves being supported to write a will and plan one’s funeral. The brother of one participant talked about the living will they had written with his sister and a member of staff:
We also, at the same time we discussed her funeral. We’ve all got, if I’m still around, everybody’s got to wear pink, her favourite colour. And that’s stuff we’re going to do, we’ll go through and sort it out and it’s paid for it’s for any funeral, it’s all sorted out, done and dusted, paid for … So it’s all in place and as I say she’s aware that you get older and eventually you go. Oh yes, she certainly put her point of view across about everything, don’t worry.
NCH_1, interview with S’s brother
The programme around ‘living life to the full’ at NCH_1 is a key element of training and is mandatory for all staff. Alongside the bespoke training programmes, staff team learning is a core part of the culture. Staff learn from each other, find out what they need to know to provide good support, and ask for guidance from the professionals who are in and out of the nursing care home at regular intervals. Family members are asked to join staff training, which contributes to an environment where everyone is working together to provide the best support for people.
Dementia
In SL_2 there was an explicit focus on continuing to support people who might develop dementia to remain living with their carer. An interview with a Shared Lives co-ordinator described the steps taken to enable people to remain at home, which included providing additional respite for the carer and involving health and social care to make sure there was a full understanding of the diagnosis. The multidisciplinary meeting, including the geriatric consultant for psychiatry, psychologist, speech and language therapist and primary care liaison nurse, was held where the person lives, which helped the PWLD and carer feel comfortable and able to ask questions.
However, as people grow older, dementia might also affect their loved ones and their relationships with their loved ones, which in turn might lead to distress for PWLD if they struggle to understand what is happening:
S, she can be quite verbally … I don’t know if challenging is the right word, but she can be quite volatile. It’s always towards G, her [Shared Lives] carer … we did have an incident 2 weeks ago, and that was as a result of her not being able to see Mum. So Mum is very unwell at the moment … she’s going through quite a difficult time with dementia. And obviously it’s not easy to share with S in a way that she’s able to understand about the disease dementia. And Dad’s really not been wanting too much information to be passed to her. So it’s difficult, because S can’t understand the changes in Mum.
SL_2, interview with Shared Lives co-ordinator
This highlights the need for developing accessible ways of explaining dementia and its impact on a PWLD. ISL_3 commissioners described an ageing initiative that helped to identify people with early-onset dementia and other changing needs.
Shared Lives carers are also carers
As is apparent above, successful Shared Lives placements were long-lasting, with people being able to stay in their Shared Lives home for decades:
And when I think about individuals that are on my caseload, I’ve got a carer that’s gonna be 80 on Sunday, I’ve got joint carers that are 76 and 77 … They’ve supported both those gentlemen [in their care] for 30+ years. And every time I go and visit, I just think ‘Wow. I am extremely lucky’. And I think that epitomises Shared Lives really and why they do the role that they do.
SL_2, interview with Shared Lives co-ordinator
Social factors
Social factors relevant to the design and delivery of good support include working closely with families, facilitating the maintenance of existing, and the development of new, relationships, interests and skills. Relationships with family and friends and community belonging are key to well-being, and we found that excellent support included a strong emphasis on these relationships. Furthermore, good support centres being together and being part of a community:
T [support worker] says Z has lots of friends. I ask if they ever come and visit. ‘They used to come visit before COVID. Stupid COVID’, says Z. ‘But are you doing something for Halloween’, says T. ‘Going to a party’, says Z. ‘At J’s’, she adds. ‘Are you going to dress up?’ ‘I don’t know yet. Maybe’. ‘Is J your friend?’ I ask ‘He is. Yeah’.
ISL_2, ethnography notes 26 October 2021
I think about the time we spent together and about how lovely today has been. […] I think it’s the ease of being that I like the most, the getting out, meeting people, the leisurely coffee, the beautiful beach, the ease of interactions facilitated by C [support worker]. I think that the being together is the thing … not the mechanical ‘doing’, but the being, that feels like the support is not in the way of having a good time, like the person at work, supporting Z [the participant] is not always thinking about ‘doing’, about the next thing that needs ‘doing’.
ISL_2, ethnography notes 26 March 2022
A social factor that relates closely to organisational factors is working with families (when they are present) in constructive and positive ways. This involves acknowledgement that families’ trust is something that needs to be earned. Another is well-planned leisure (or work) activities that centre on the preferences and interests of the person. These are also key to the PWLD maintaining social connections with the community:
I ask Z how she has been and what she has been up to and she lists her activities … ‘Monday – pottery, Tuesday – drama, Wednesday – shopping, Thursday – Aqua Fit, Friday – work’. What about the weekends? I want to know. ‘Don’t know, see my sister maybe’. ‘And what are you making in pottery these days?’ ‘A stump’. ‘A what?’ ‘A stump. Like tree stump’. ‘Ah, cool!’ ‘It’s for an exhibition’ … B [support worker] says Z likes her routine, but also to try new things every now and again. She adds they are looking for a choir she can join.
ISL_2, ethnography notes 22 March 2022
Some participants did a range of activities they clearly enjoyed. H, for example, did Tai Chi, drama and British Sign Language at the day centre. External activities undertaken during the visits included bowling, shopping, a trip to a shopping centre, a bar, a coffee shop, Zumba class, swimming and lunch at fast food restaurants and cafes. Observation notes regularly capture enjoyment, care and belonging:
The class begins; SL_1H sings along and clearly loves it. She looks confident in the moves that she knows (and knows most) and talks a little with others during the change of tracks. Every so often SL_1H turns round and gives me a thumbs up and asks if I’m OK. I confirm that I am. I notice she has forgotten to bring some water into the studio and a few minutes into the class SL_1R pops her head around the door and passes her a bottle.
SL_1, ethnography notes 17 November 2021
A broad range of activities in or outside DOP_1 allows people to find something they enjoy doing and try out new things:
I have a look around and notice one wall is full of lists of names of people who have signed up for different ‘groups’ … There are: Farm group, Horse riding, Walking group, Bowling, Coffee out, Ladies group, Games in the park, Pottery, Gym, Arts + crafts, Music group, Explore the UK, Swimming, [Name] Theatre Company, Baking, Zumba, Golf, Yoga and Cooking … There is also Gents’ club with 4 dates listed that have the following activities next to them: Bowling, Birds of prey, Mini golf, Movie.
DOP_1, ethnography notes 9 May 2022
D [co-researcher] and I watch F colouring … In between that we ask F about the details of her days [at the hub] … she does gardening group on Tuesdays; they sometimes go on drives and for coffee … F [says she] likes coming to SA; she’s been coming many years.
DOP_1, ethnography notes 17 November 2021
I:And do they ever like … I guess … come up with activities based on what she would like to do? So instead of what they have, kind of look for things that she might want to do?
P:I think they do. Although I’m not ever so aware of that, but I think that they do. F’s quite set in her ways, so partly, I mean she loves the garden club, so that’s good. She likes doing her computers and … they do, they have got a list, I know, of activities, which I have been sent before and I’ve said to F, ‘would you like to do any of these?’
DOP_1, interview with sister
Activities, age and belonging in day activity centres
Despite the broad offering in DOP_1, there were no activities tailored specifically to older people, although some activities, such as chair yoga, allow people with reduced mobility and older people to take part. At times, the activities that older people took part in were a way to be together with others as opposed to being of real interest to the person:
P:But I only go [to the hub] one day a week now, and that’s on a Monday … Mainly for cooking … And doing reception. Because I’ve recently took at doing reception work, working on the reception. Letting people in and out. If the phone [intercom] goes off.
I:Yeah. So when you do the cooking, what kind of things do you do?
P:Lasagne. Anything really, anything easy … (..)
I:Do you ever cook these things back at home for yourself then?
P:No.
I:No?
P:I only do microwave stuff at home.
I:Right … So why do you do the cooking at [the hub] if you don’t use it at home then?
P:I don’t know, I just … just come down just to make myself, give myself something to do really.
DOP_1, interview with N, PWLD
This example suggests that the value of the activity is thus not so much in its content, or for teaching a skill, such as cooking, but in it being a way to fill the time, and bring people to the hub, where they get to socialise and receive support from the community that the hub holds, a point also acknowledged by F’s sister:
I don’t know if it’s to do with timings and people available and things like that, but obviously sometimes the weather’s not good for gardening so that’s fair enough, but some days when she should be doing say, computers, or something like that, it doesn’t seem to happen and she just seems to be doing a jigsaw or something like that. Which F’s very easy-going … so she’ll just go along with it, and I have said to her, you know, you can say you want to do something and I think she’s very happy to have company, so sometimes she’s not bothered that they’re not doing anything in particular.
DOP_1, interview with sister, emphasis added
The DOP_1 day activity hubs offered a sense of community and belonging for people, enabling people to stay in touch with their peers and develop new social connections. N and S have limited hours of support, but both come to one of the hubs weekly:
I think that tends to be sort of like, we would encourage people to join in an activity. But at the same time, we do also appreciate that that’s not always for them, and that they probably want just to come in, just to see people, socialise. Have a game of pool and have a cup of coffee. Have a chat with somebody. […] Or, you know, even myself, yeah, I’d come out of the office and have a game of pool with somebody and have a chat with somebody.
DOP_1, interview with hub manager
N comes in and comes over us. It turns out him and S know each other very well ‘12 years’, explains N. ‘Must be’, says S … N calls S ‘Pumpkin’. ‘Why Pumpkin?’ ‘I don’t know, it’s always been that. My wife called him Pumpkin, my brother called him that, we all call him that’ … ‘We are there for each other’, asserts N. He says S phones him up when he’s got a problem and they talk about it and try to help.
DOP_1, ethnography notes 16 November 2021
For people who received support in group settings, 1 : 3, for example, the group played an additional role of both support and knowledge bank about their members. Over the years, people developed strong bonds and a sense of belonging. This created an atmosphere where people looked out for and supported each other:
K does not communicate with words but points at things and makes sounds as M [support worker] guesses what K wants; the coffee is obvious, K always starts her day with that, the radio takes a bit more guesswork. K points and M asks ‘is it the window? Do you want it closed?’ K makes a sound that is a clear negative. ‘Is it the drawing, do you want that?’ Another no from K. ‘Is it the radio?’ MA [person in K’s group] suggests. K nods energetically and makes happy sounds. M puts the radio on and K smiles.
DOP_1, ethnography notes 11 May 2022
N says the card J sent him [after his mother died] meant a lot. J asks about N’s brother; he seems not to know he passed away this year too. N says he died. ‘Oh no! You’ve had a bad one this year’, says J. The two men keep talking and J says he was always asking about N, ‘I wanted to know you are okay’, he says and he looks concerned. ‘I’m all right’, says N.
DOP_1, ethnography notes 16 November 2021
Understanding and affection in Shared Lives
A core feature of the Shared Lives model involved the in-depth knowledge and understanding Shared Lives carers develop about the person or people they support and what appears to be genuine affection. Observation notes include examples of humour, ‘banter’ and thoughtfulness as participants were involved in family life, including celebrations and holidays:
They [Shared Lives carers] went on to say that if possible, everyone that is living with them will be living with them for as long as they wish to – which they assume will be forever. This was particularly in relation to G, as he is older than everyone, aged 75. There was what seemed like obvious love in their voices when they spoke. More than once [Shared Lives carers] referred to themselves, their children and the people that lived with them as an ‘extended family’ or a ‘family’.
SL_2, ethnography notes 23 October 2021
[Shared Lives carer shared that] W loves to celebrate things. When they went out to lunch today, as they do every Friday after shopping in town for themselves and for food, W raised her glass and said ‘here’s to summer’. It’s a really warm, lovely day today. S [Shared Lives carer] says they put the Christmas decorations up early every year because W is eager to start the celebrations. They make a big celebration of Valentine’s Day, Easter, Halloween, New Year’s Eve, birthdays etc.
SL_2, ethnography notes 29 April 2022
The intimate knowledge of people they support meant that Shared Lives carers could be responsive and adaptable. For example, plans for one visit were changed at the last minute from a restaurant meal to a trip to the bowling complex with less emphasis on eating, as one participant had recently had increased seizure activity and eating could be a trigger for this:
E […] said she has one person who stays that does not want to go out. She likes to go to the shop for snacks and watch films in the quiet room. E said that when this person started staying with her she felt like she was failing her in that they didn’t do anything – over time and through discussions with the person, other support staff and the person’s family, she has realised that her home is used as a time away from a busy environment and that this person likes to spend quiet time on their own in this way when they get the opportunity.
SL_1, ethnography notes 6 October 2021
The final aspect to thriving was the sense of belonging apparent through participants’ talk and actions, and observations of wider interactions within the community. Participants were involved with the extended family of their Shared Lives carer, including their children and grandparents. In this extract, the researcher talks about the relationship between the Shared Lives carer’s (Gl) parents and G:
GI’s parents shoot game. When Gl’s parents visit, her dad is really coming to see G and will head down to see him in the fields before seeing anyone else. They have a lot in common and are quite alike in their personalities as well. G will mention him often and will pick up little gifts for him such as a mug with a pheasant on when they were recently in a shop.
SL_2, ethnography notes 3 November 2021
One visit involved a trip to a charity shop where a staff member had put aside CDs for the participant. There were also examples of the blurring of formal support and hanging out:
A, who we will meet there is not staying at E’s today but she thought it would be nice if he was able to join us as all three men get along well and enjoy each other’s company. It will also be nice because this is like a Christmas celebration for the group, she explains.
SL_1, ethnography notes 8 December 2021
A further feature of the Shared Lives model was the planning ahead that was characteristic of the relationship between the PWLD and carer, or respite carer. During visits, researchers noted conversations about future holidays and activities, including a karaoke evening in the pub that was to happen during a future respite visit:
There are brochures on the table for coach trip holidays. A is flicking through one and Ronnie has one in front of him. A tells me that they are going on holiday together, motioning to R. ‘Yes’, R smiles. In the summer and to Scotland, A explains. E elaborates that they are thinking, Fort William, Loch Ness and Isle of Skye. E says that supporting two people to go on holiday this is not the norm, it is more often a one-to-one holiday or with the family of the SL carer.
SL_1, ethnography notes 19 January 2022
Lives shared with pets
An additional feature of Shared Lives, which was less pronounced in supported living, was that people shared their lives with pets. However, careful matching is also key here, as pets could present as a barrier to placement for some people:
Another excitable dog appears. G sits on the sofa, next to excited dog no.1. They are good friends and the dog licks G’s hand … G didn’t say much when we were in the house and when he had finished his tea, he petted the dog some more. He looked very relaxed. I spoke to G a couple of times, using the dog as a subject; he listened and either said ‘aye’ or ‘right’ – I wasn’t sure. The dog got down from the sofa and it seems that was all that was keeping G anchored to the house.
SL_2, ethnography notes 23 October 2021
W then asked S [Shared Lives carer] if [dog] was going to come [to a fair] too – [dog] was the long-haired Chihuahua who was paying particular attention to me and W at this point. S said no, [dog] wasn’t going to come because she would only bark at all of the dogs there if she did. W found this comment amusing and helped [dog] onto the sofa, looking at her lovingly.
SL_2, ethnography notes 29 April 2022
Even as something as simple as pets now can be very difficult. We’ve had a number of referrals that have come through that individuals don’t want to live in a household that’s got dogs. And you think, all of a sudden, you start looking at your carers that you’ve got vacancies in and you think, ‘My goodness. I haven’t got any that haven’t got dogs’.
SL_2, interview with Shared Lives co-ordinator
How much support? How much independence in independent supported living?
Supported living, in particular, appears to function as an umbrella term under which levels of independence and support vary significantly, producing mixed results for older PWLD, even within providers rated excellent. In addition to grouping people together in what resembles small-scale institutions rather than living in the community with support, we found examples of poor support, which could be grouped into two categories:
-
People’s lives subordinated to inflexible staff schedules and routines, and at the mercy of staff shortages (illustrated by people having to wait an unreasonably long time for activities, however simple; fun activities being interrupted or cut short due to staff shift changes).
-
Support is minimal, meaning that while people are kept physically safe, their lives are constrained, limited and characterised by abject boredom (this included spending entire days inside with the TV on; being put to bed for the night as early as 5 p.m. with the radio on). These findings are particularly troubling, given the good reputation of all the providers in our sample.
Relatedly, our research suggests that small providers with strong values, where management are connected to what is happening, are more able to offer consistently good support than larger organisations where good practice and excellent support can exist alongside examples of support that is less good, or outright poor. These issues can be exacerbated by big providers expanding and absorbing staff from other organisations.
There were further contradictions and inconsistencies in the findings. Some features designed to prepare people to live independently seemed to counter the values of the organisation, such as choice and being person centred. For example, regular rental inspections are arranged in ISL_4:
So we do it sort of above board so they’ll get a letter in their letterbox or handed to them seven days prior to the inspection and then we’ll let them know that we’ll come and inspect the flat in 7-day time. And they’re involved in that as well and then come the end of that if there is anything they’ll be set whatever actions they need to get done. And then we give them maybe another week or two weeks depending on what needs doing.
ISL_4, interview with manager
This provider also took an alternative approach to staff consistency in that each person had at least one key support worker who overlooked and co-ordinated the support provided. Key workers were changed every 6 months so that people did not get too dependent on one staff member. There was also some contradiction between perceptions of staffing levels at this site and the use of agency staff. There was criticism that working with agency staff put the staff members under additional pressure, as the time needed to update the new member of staff took away from support time. The use of agency staff was also raised by a family carer:
They try, I know they try to employ the same ones. But I find it very upsetting that somebody goes in and gives her very personal care and [she] doesn’t know their name.
ISL_4, interview with family member
Nursing Care Home 2 (NCH_2): reflections on the commissioning and development of a new inner-city service
The proposed service in many ways runs counter to examples of good practice observed in other sites and to the direction of travel as set out in wider policy (e.g. Building the Right Home,81 NHSE;81 CQC). Plans for NCH_2 evolved around the development of three key types of provision for the 10-bed household:
-
intermediate and therapeutic nursing care for people with complex needs to both treat and assess, for example, after a hospital discharge
-
respite care for people requiring more intensive clinical support
-
sheltered housing flats for people considering a longer-term move to residential care provision.
A co-design group included two family carers, a manager of a residential care home for autistic people, three LA representatives, three architects and two interior designers. Our analysis showed that a key dilemma facing this group was balancing the need to secure an in-demand site alongside the commissioning of 10 local beds specifically to support older PWLD against critiquing the model of care on offer (a large nursing care home). Learning disability best practice guidance emphasises the need to move away from institutional models. However, in practice this had to be offset against the potential benefits of remaining near family, friends and familiar places. The co-design group attended to this tension by considering how to best personalise the space, arguing that it had to be flexible and future-proofed while acknowledging the need to adopt a ‘try it out and learn’ approach. A key concern was how to create homeliness within an environment that needed to (1) support physical health needs and (2) meet the emotional and sensory needs of people with complex behaviours. We observed a lively discussion about the potential positioning of a ‘nurses’ station’ and active resistance to both the term and the concept from family members who felt that it overly medicalised someone’s home.
Nursing Care Home_2 offered useful insights into the challenges involved in growing capacity for local services for PWLD as they get older, while adhering to models of excellent care. We observed commissioners, LA representatives, family carers and design experts working collaboratively to address some of the resulting dilemmas, while acknowledging that they were working within the constraints of the site afforded to them. There was little engagement with PWLD about the evolving plans, although the project manager indicated that this was forthcoming. Critically, it became clear through our research that there is a significant gap in the current research and practice literature regarding best practice guidelines for the commissioning and design of housing for older PWLD with complex health needs.
Discussion
In Chapter 1, we outlined the importance of PWLD being supported to age successfully and productively. 7 Our analysis demonstrates scant evidence of thinking about growing older across the sites outside the nursing home. Participants were excluded from the normative life cycle of work, relationships and retirement, which, in turn, meant that there were no definitive markers of time passing. While there is considerable attention to ‘transitions’ to adulthood in existing literature (e.g. Pallisera et al.,123 Salt et al. 124), once people become adults, they face years of growing older with little differentiation across their adult life course. Indeed, we suggest that the chronic ill health or death of the family carers makes ‘visible’ the ageing of PWLD, which, in turn, means that people are denied the planning and organisation necessary to age actively and be living in a home for their later life with good support.
Considering excellence
The premise of WP3 was to conduct an ethnographic study of providers identified as excellent from WP2. The criteria for judging excellence are outlined in Chapter 2 (see Table 3). Our analysis allowed us to identify the key factors, environmental, organisational and social, that shape excellent support, and we consider these below. Because of the variation across and within models, we suggest that lives that are visibly growing (in myriad ways) are a measure of excellence no matter what the model of support. Being supported to live on one’s own terms and to grow and expand relationships, interests and aspirations are defining aspects of excellence.
We also found evidence of static or constrained lives even when the provision was identified as excellent. This suggests a disconnect between those who commission services and what is happening on the ground. While the quality of provision may change in a short period of time due to staff shortages and other factors, our fieldwork and analysis revealed long-standing examples of poor practice, such as people being put to bed early and spending the day watching the television. There was also little consideration for supporting people to work and uneven support for people to have romantic and other social relationships.
Critical look at the factors that enable or impede excellence
Environmentally sound
Across the different models, we teased out the environmental factors that contribute to excellence. Physical environments, locations, and, relatedly, how well and easily they are linked to the community matter and influence the quality of life for PWLD as they age.
For some people, the importance of living alone or with a partner to enable independence and cultivate agency and autonomy was apparent in the data relating to ISL, and yet some ISL providers group people together in settings that resemble small-scale institutions rather than homes, where people were grouped together with strangers (with up to five people living together) in houses that did not feel homely (apart from personalised bedrooms) and support that was often minimal. Similarly, the Shared Lives model is premised on the PWLD living with a family into older age, which can be incommensurate with leading an independent life. The interdependence and conviviality of Shared Lives must therefore be considered in the context where having a sense of autonomy and choice is key for PWLD, particularly for people denied these in the past. Furthermore, while our Shared Lives data highlight how participants were living an ordinary life, and very much part of a local community, this was upended by segregated day activities, and sometimes inadequate provision, as an integral part of the scheme, rather than mainstream activities.
The use of day centres occupies an ambiguous location in relation to notions of choice and autonomy. Extensive closures of day centres have taken place in the UK over the past two decades as an outcome of the personalisation agenda,125 without the materialisation of the promised ‘alternative shared spaces or community hubs’. 126 It is argued the closure of place-based care service led to a ‘post-service landscape’ where people were expected to receive individualised, community-based support. 125 Day centres featured substantially in our research, raising questions around the re-emergence of this model of service and what it might mean for the people who attend these settings.
The day centres used by ISL_1 were unappealing venues, and people attending spent the day in one room with the television on, clearly bored at times. The DOP_1 hubs were more dynamic, with thoughtful staff, an inviting atmosphere and a good range of activities to choose from. There was a sense of community and belonging and of sustained relationships that were important to participants. It was difficult to disentangle, however, whether people genuinely enjoyed attending these hubs or if these simply filled time. A lack of activities targeted specifically at older PWLD potentially compounded this issue.
Residential nursing care is arguably essential for some people because of complex health needs. The organisation of NHC_1 with a strong network of health professionals within and outside, together with a comprehensive EOLC plan and associated training, meant that participants could be supported well as they grew older. This was coupled with good staff retention. It was, however, not the right setting for one participant, who was unhappy because of a tense relationship with another resident (albeit exacerbated by the lockdown context, which meant that they were spending significantly more time in each other’s company than usual). This poses questions about commissioning appropriate services for PWLD, as this mismatch between person and service appeared to be accepted and had continued for around 10 years.
As mentioned above, variation existed in the quality of support within each of the models and within one setting. There were instances, for example, in which researchers noted questions about privacy boundaries being breached during visits as Shared Lives carers openly discussed aspects of participants’ lives in front of them. What was an excellent home for G was less appropriate for S, who appeared to feel socially isolated on the smallholding. This raises issues around the matching of not just Shared Lives carers to PWLD but also to locations. Within the Shared Lives model, there is also the obvious issue of longevity of placements that can lead to the same challenges as family support, as carers age and/or become less able to continue to support people.
Importance of staff knowledge, matching, consistency and retention
Staff consistency is a factor central to excellence in our analysis. There is a relationship between staff retention and the best support we observed, which is an outcome of organisational values and approach to recruitment and staff retention, and the relationship between the support worker and the person being supported.
Careful and deliberate matching of staff with people they support plays an important role in excellent support. Giving PWLD and their families a say in the recruitment process is key to this approach and should be introduced more widely. The best support is arguably when the distinction between carer and cared for appears blurred and there is recognition of reciprocity and genuine affection. At the level of organisation, this is reflected in an ethos that embraces people being supported as part of the organisation, avoiding the distinction between ‘us’ and ‘them’.
An example of this was accounts of staff or carers ‘going over and beyond’ what was expected of them, such as staying overnight with PWLD in hospital. Related to this is the advocacy role staff undertook, which could extend beyond the immediate remit of their role. While DOP_1 was a place-based care service, for example, staff helped people and their families think about the future.
The staffing crisis in social care and the practice of bringing in agency staff to fill in vacancies creates an impediment to the flourishing of long-lasting relationships, and reproduces institutional models of support, where a person being supported does not know who will be there on the day to support them. This problem was explicitly avoided by some sites and presented as a form of deliberate distancing from institutional care as a sign of social responsibility and social justice practice.
Smaller providers were better able to develop a deeper knowledge about the people they supported and a sense of responsibility for everyone they supported, and developed sophisticated approaches to matching people. Shared Lives carers likewise were able to know and understand the person they supported, and scheme managers tried to carefully match people. Staff consistency is of key importance as people grow older and reach EOLC. The approach to death and dying in NCH_1 was impressive, particularly as an integral part to the policy was the importance of living a full life, whilst proactively anticipating health challenges and changes as people aged.
The commissioners we interviewed were knowledgeable about the support they commissioned, although they tended to be budget focused rather than focused on consideration of excellence. There was also uneven consideration of ageing through our analysis, which suggests that this issue is becoming more prominent as people are living longer.
Thinking about ‘behaviours that challenge others’
We found a mix of approaches to the label of ‘BTCO’ among our sample of providers. Documentary analysis and interviews suggest that most providers understand ‘BTCO’ as situational and/or resultant from unmet needs (physical, environmental, social or emotional). However, many continue to channel staff energy, time and resources into ‘positive behaviour support’ interventions, which by their very virtue of being designed to ‘deal’ with ‘BTCO’ reify and pathologise them. Moreover, the broad definitions of ‘BTCO’ lend themselves easily to diagnostic overshadowing, where genuine distress or responses to unfair treatment can be classified as ‘BTCO’, which in turn can have negative consequences for the person’s future, as the label follows them throughout their life, unchallenged. The decrease in or disappearing of so-called ‘BTCO’ with good support suggests that it is frequently support that is challenging and inadequate, and not behaviours, or individuals (Mikulak et al., in preparation).
Conclusion
In WP3 we set out to undertake ethnographic case studies that provide contrasting approaches to support and services to older PWLD. While the criteria of excellence from WP2 were reflected in our analysis, we also found a mixed picture in terms of the provision of support for older PWLD. We found evidence of re-institutionalisation as some people lived in congregate settings with little opportunity to lead active and fulfilling lives. The absence of examples of people being supported to work or have intimate relationships points to a lack of support and aspiration in people’s lives and, apart from the residential nursing home and one supported living site, we observed little focus on growing older and EOLC.
We also found examples of excellent provision where people were supported by staff whom they sometimes were involved in recruiting and who they liked and who understood them well. With the right support, organisation and environment, people can develop relationships, interests and aspirations allowing them to lead fulfilling lives, even after experiencing trauma and abuse. Indeed, excellent provision leads to the reduction of support required and of evidence of so-called ‘BTCO’.
Chapter 6 Work package 4: co-producing and evaluating resources to support preparations for parental loss, transitions in care, and end-of-life care for carers
Plain language summary
-
This part of the research was about the support needs of families of older people with learning disabilities living at home with elderly parents.
-
We wanted to find out what is important to older people with learning disabilities and their families.
-
We wanted to make and test resources to help families to prepare for what is going to happen in the future and end-of-life care for carers.
-
We found out what approaches older people with learning disabilities and family carers prefer, and designed and tested a set of discussion cards for families.
Introduction
A lack of viable alternative living arrangements and limited information and support for families means that family carers too often end up supporting their adult children into their older age. 15,127 Families needed to develop plans for living and support arrangements that enable PWLD to lead independent and autonomous lives. For elderly parents’ own EOLC planning, considering what will happen to their daughter or son is a crucial aspect. However, studies have found a lack of such future planning. 15,16,36
We used a co-design approach128 to developing future planning resources, which involved PWLD, parent carers and siblings throughout. The co-design process was split into three stages. Stage 1 involved interviews and focus groups with older PWLD living at home with parents; and with parents and siblings of older PWLD. Analysis showed participants’ varied experiences, hopes and concerns about future planning and changes to living and support arrangements. These findings fed into stage 2: a series of 12 online meetings with PWLD and families with the aim of co-designing a set of resources to support families with preparations for parental loss, moving, and EOLC for carers. This included a catalyst film presenting the stage 1 findings to stimulate group discussions about what resources are needed. The co-design group developed a set of ‘Planning Ahead’ cards to help families to think about the future. Stage 3, a small-scale evaluation study, tested the cards over a 2-month period, and relevant stakeholder groups provided feedback. Feedback was used to refine the cards before making them publicly available.
Stage 1: understanding experiences, hopes and concerns about future planning
Objective
The objective was to understand experiences, hopes and concerns about future planning, from the perspectives of older PWLD currently living at home with parent(s), and of their parents and their siblings.
Sample
Participants were recruited through family and carer organisations, including the Public Co-ordinator Vaid, and via social media. The sample comprised:
-
nine PWLD living at home with their parent(s) (aged ≥ 40 years, mean age 46 years)
-
eleven parents of a daughter/son aged ≥ 40 years who lived with them (mean age 73 years)
-
nine siblings of a sister/brother aged ≥ 40 years who lived with their parent(s) (mean age 50 years)
-
seven siblings of a sister/brother who had lived with their parent(s) until age ≥ 35 years but whose circumstances changed following parental death or otherwise (mean age 61 years).
Thirty-two participants were white/White British, three were black/Black British, and one was Asian/Asian British. Eleven participants were male and 25 were female.
Data generation
Semistructured interviews and focus groups took place January 2021–May 2022. Focus groups can help participants with learning disabilities feel supported to express their opinions and hear other similar experiences. 129,130 Participants were given the choice of an online interview or in-person focus group, which was conducted by a researcher and co-researcher.
Interviews and focus groups with PWLD took place over two or three meetings to ensure participants felt comfortable, and to enable meaningful participation. PWLD were given the option of having someone (not a family member) present to support them. Flexible methods included adapted versions of Books Beyond Words (wordless stories in picture format) and Talking Mats™ (a visual framework that helps people to understand and respond more effectively).
Data analysis
The team held debriefing sessions and the interviews and focus groups were recorded, transcribed verbatim, and analysed using Framework analysis. 131 This is a systematic way of organising the data by creating a matrix that summarises themes and participants. It is an adaptable and flexible method that has the advantage of allowing the engagement of people without qualitative experience, including co-researchers. Transcripts were read several times and key themes were identified. The research team discussed the themes using pictures and sticky notes with additional reflections in an analysis workshop. This workshop led to the development of four questions, presented in Figure 2. A coding framework was developed and applied to the transcripts. Themes, subthemes and interpretations were discussed within the team as the analysis developed. Comparisons were made across participants to identify different experiences, hopes and concerns, and to ensure that the analysis represented the data set. Pseudonyms are used throughout this chapter.
FIGURE 2.
Themes identified in WP4 stage 1 interviews and focus groups.
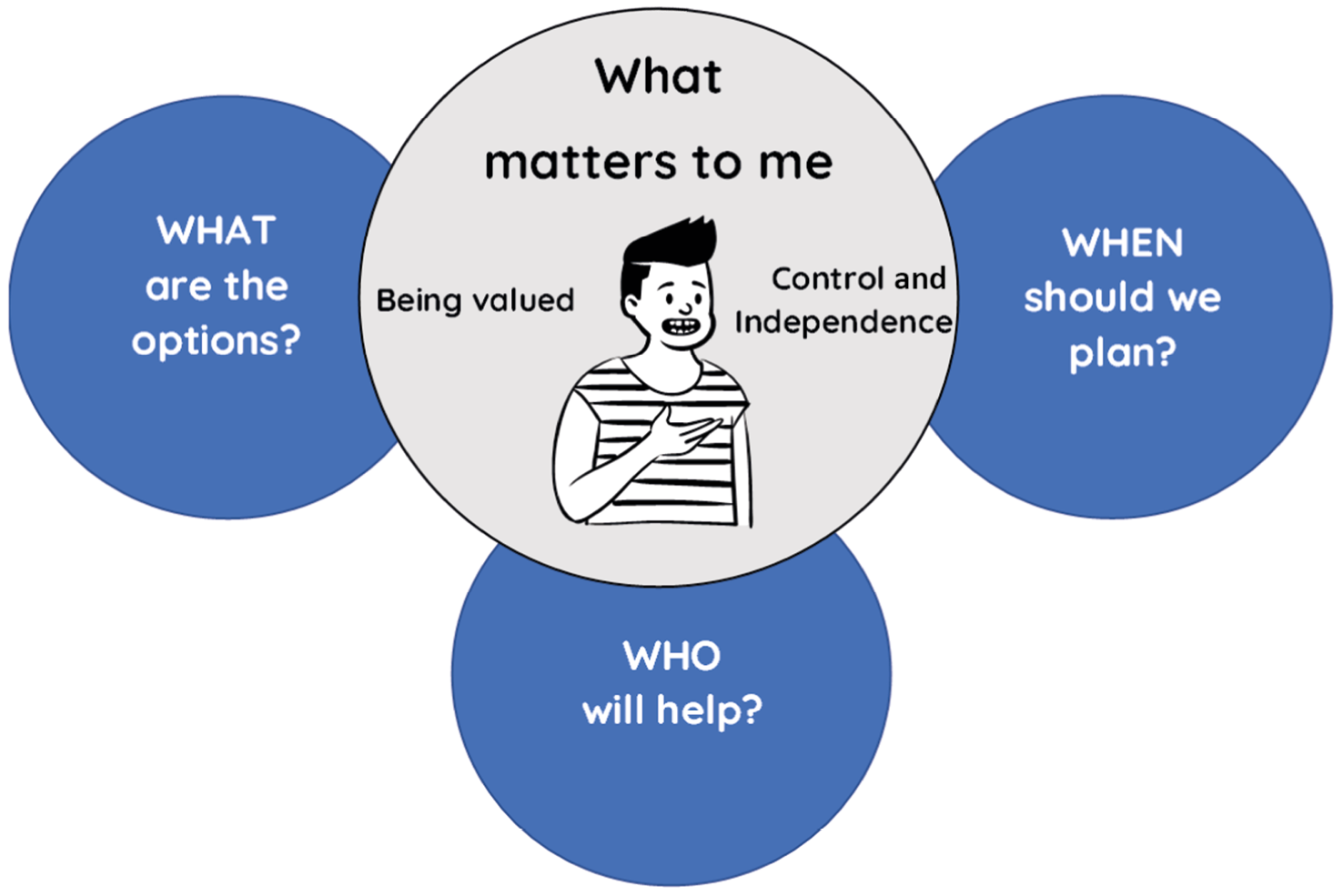
Stage 1 findings
Families were acutely aware of the importance of planning ahead. This was an urgent and crucial component of their own EOL planning. How this was addressed varied from actively looking for solutions to ignoring the issue. Participants had clear ideas about what they would like to happen in the future, but they were not sure what future options were, or had become convinced that suitable solutions were lacking.
The central concern was what matters for the PWLD to ensure that they have a good, happy life. ‘Having control and independence’ and ‘being valued’ were crucial to this. Participants raised questions about what the options were, when planning should happen, and who could help with planning.
What matters to me: control and independence
Moving away from parents was seen by some as increasing independence, while others felt that it could be a threat to independence and control. Not being able to continue doing the things they love was a concern for PWLD, parents and siblings alike:
He needs to live somewhere where he feels that he can do his own thing, live independently as much as possible. But with that safety net of somebody who can do his personal care, do his meals and make sure it’s safe … My mum dresses him really quite trendy and he has his hair spiked up and stuff and just keeping him living the way that he has always been used to and for things not to slip.
Claire, sibling
Andy had a busy life of sporting competitions and day trips. He knew of friends who were limited in what they could do each day and was worried that he might live somewhere without transport:
Well if you live in the countryside though you can’t do what you want on a Sunday, it takes Sundays out completely doesn’t it. Depending where you live though, if you live in the countryside you’ve got Sundays out really because there’s no transport.
Andy, PWLD
Most people preferred the idea of living on their own or with family, putting the ‘living with others’ card into the ‘very worried’ column of the Talking Mat. Some PWLD felt this following negative experiences in the past. Others simply did not want the potential stress, noise and other difficulties of house-sharing.
Oh, hell, no. [Laughs] No. No, it’s not that, it’s just that, no, I’d rather live by myself, or live with my boyfriend or whatever the case may be … With other people? Oh, no. Gosh, I can’t even – the noise will be like ‘Whoo!’ No.
Rochelle, PWLD
This reflects findings from WP3 that living alone or with a partner provides privacy, security and agency.
What matters to me: being valued
People with learning disabilities were valued members of the family, but there were concerns that entering the social care system would mean that support would become institutionalised. Participants described the importance of spending time with people you love and who love you. While some PWLD described some difficulties of living with their parents, family were central in their lives and regular family contact would be important for them if they were to move out:
That he’s somewhere where he feels secure with people that he knows and trusts. I think that’s it basically. It would be sort of a place and people that he knows. I wouldn’t think that it would be at all suitable for him to suddenly be uprooted and be among strangers … [he would need] somebody to give him a big hug and to be there for him.
Rose, mother
When should we plan?
While families were aware of the need to plan, the sense of urgency varied. For some there was a sense of a ‘time bomb’ waiting to go off and they described the ‘dread’ of what would happen when they died or became too frail to support their son/daughter at home. Anthony described himself as ‘desperate’ to find a solution:
Although, I can actually manage for the time being, I’m actually working on the basis that I can’t manage, because otherwise I’m never going to get there, and my nightmare will come true. I’ll drop dead, and then he’ll be down being sectioned and in a secure unit for the rest of his life, and that will happen.
Anthony, father
By contrast, some participants found this fear was too overwhelming to think about. They instead focused on their current caring role and delaying any possible crisis for as long as possible:
I’ve pushed it away. It’s not something that I can think about … I’m hoping to go on and on, and continue my caring role, because I can’t see no way out of it.
Margaret, mother
Many siblings were concerned that their parents would keep going until a crisis occurred. They struggled to talk to their parents about this:
In an ideal world, I would want to start talking a bit more now with my parents, but I honestly don’t think that they’ll want to deal with it until crisis point … I’ve tried. It’s met with, ‘Oh you’re talking as if me and your dad are gonna pop our clogs tomorrow’.
Claire, sibling
Other participants felt that there was little point planning while things were working well and the future could not be predicted. This could be frustrating for some PWLD who wanted to take the risk to have the opportunity for more independence. Sharon was asked about what was happening in a Books Beyond Words picture of a PWLD, parent and social worker looking at a picture of a house:
The mum’s listening but I think she’s nervous, because I’ve been there myself, so I kind of recognise the body language. He looks more enthusiastic where he’s like, ‘Great, this is great’. [The mum] looks like she wants to die. She looks like she’s like, ‘Don’t do it, don’t do it’.
Sharon, PWLD
Participants also thought that there was too much uncertainty around future support needs, how much funding they would be eligible for, and which services might be available by the time they felt ready to move. Some participants felt that the LA went through phases of preferring support models (e.g. residential communities) that would fall out of favour:
You can’t plan, because there’ll be something else come out where it will all be different … So there’s no tool out there, because things change too quickly.
Fern, mother
Some families were starting to plan and making smaller changes in their lives, as parents were beginning to struggle to give as much support as before. This could include trying to help the PWLD to be more independent. Siblings were also aware of this need:
She has a lot of abilities that we need to expand and give her that confidence that she can do it away from [the family] … to do shopping with somebody else, to travel in a bus, go to the shops, do the shopping for dinner and then come back and cook a meal with somebody else that’s not us.
Sofia, sibling
What are the options?
Participants thought that living alone with support was the best option for the future, either in a new flat or in the family home following the parents’ death. Clarity was needed about what was possible and how it might work. Some participants, particularly those with limited input from social services, did not know what was possible. There was little information available, and parents of people with profound learning disabilities worried that they would be pushed towards residential care settings.
Some participants did not think that any feasible, sustainable options were available. This was in part based on negative experiences of respite or setting up alternative living arrangements in the past:
That broke down. And it’s still the case now if what’s available is still off-the-shelf council services … Having experienced it once, you don’t have confidence in doing it and trying it again.
George, sibling, discussing respite care
Who will help?
Participants acknowledged that social services would need to be involved, but this was seen as a hoop to jump through, rather than as help or support. Experiences of support services were inconsistent, and participants were concerned about the lack of knowledge about the PWLD. Many felt that social workers deal with crises rather than proactively acting to prevent these crises:
I would feel like I would need to go with them with a fait accompli, I will need to go to them and say, this is what I’ve come up with, will you sign it off? I don’t feel like I could go to a social worker today and say this is where I’m at now I don’t need anything yet, but can we talk about it.
Claire, sibling
Support network is more to do with your family more than social worker, because social worker is a bit, some social workers are a bit hit and miss … If you want to people to live in their own house, well, then, give them a better social worker, and stop cutting them.
Rochelle, PWLD
The importance of knowing and valuing the person was key to that person leading a good life. Concerns about who would be there for their relative were most salient for families of people with more profound learning disabilities. Alongside concerns about finding appropriate professional support for their physical needs, they worried that, without family advocacy, people’s social lives would fall away:
We’ve done the Circles of Support and, obviously, the people with support needs have always got more people in their lives that are in paid roles, and less people in their inner circles. So because we work so hard at Max being present in the community and things like that, but without our facilitating, I think it would be less easy for him to have those contacts.
Louise, sibling
Summary of stage 1 results
-
Families were acutely aware of the need to plan ahead, and worried about the future.
-
PWLD were aware that their situation would need to change in the future.
-
Participants were concerned about the loss of independence and control, and of not being valued.
-
Participants did not know how to find suitable future solutions.
-
Participants felt that there was a lack of suitable options and a lack of support from social services.
-
Participants did not know who to talk to, and most did not talk about the future with their family.
-
Some participants actively sought solutions, while others did not engage in planning alternative living arrangements.
-
This further reduced opportunities for PWLD to lead autonomous lives.
Stage 2: co-designing resources to support older people with learning disabilities and their families to prepare for the future
Objective
The objective was to co-design resources for supporting older PWLD who live in the parental home, and their families, to prepare for parental death and transitions in care.
Design and data collection
There is increasing recognition of the importance of involving patients and the public in research and service improvement through co-design and co-production methods. 132 Stage 2 used a modified version of experience-based co-design as described by the Point of Care Foundation. 128 This approach aims to make meaningful changes to services by centring service users and health and social care staff experiences, and collaborating with these stakeholders to develop solutions to the issues they raise. The adaptation version focused on the experiences of families and PWLD, who chose to invite staff views and input where relevant. Key areas of concern were identified through a process of workshops and working together to address them.
The process involved creating a ‘catalyst film’ using film extracts from the interviews from stage 1. This film included the following sections:
-
When should we plan?
-
What are the options?
-
Can I keep my independence?
-
Who will help us to make plans?
-
Will it work?
-
Who will support us in the future?
A co-design group was created and attended 12 online workshops to co-design resources to help older PWLD and their families plan ahead. Each session lasted 2 hours. This was followed by an in-person celebration event. Feedback on the sessions was collected after sessions 3 and 12 using Easy Read questionnaires (see Report Supplementary Material 13).
Sample
Participants were selected from the stage 1 participants. Eleven people consented to participate, of whom eight regularly attended meetings. A core group comprised four PWLD and four parents. Two sets of participants were from the same family (with both the PWLD and their parent taking part).
Data analysis
The co-design sessions were recorded, but the data were not formally analysed as this stage straddled service development and research. There was a continuous appraisal and feedback loop, with team discussions, during the development of the resources.
Results of stage 2
Co-design sessions
Sessions 1 and 2: introduction, catalyst film and deciding how to run the group
These sessions included ice-breaker games, a discussion of the aims of the group and how the sessions would be run and watching the catalyst film.
Sessions 3–5: deciding approach, design and topics for resources
Over three sessions, the group discussed what sort of resources would be helpful, what they should look like, and what topics should be covered. Resources discussed included films, booklets, decision aids and conversation starters. The group wanted help to think in detail about what is important and what might be possible before talking to social workers.
It would be nice to have some sort of Easy Read process to go through. Like asking them would you like to live with a friend, would you like to live with someone else? Really detailed and think of all the different questions that would make them think what they want. Like John doesn’t like noise from other people. Then you could write in that book and then if you have your meeting with your social worker, you can say, this is what I want.
Fern, mother
The group decided to make a set of cards to help families start conversations and think and talk about the important things to tell social workers, along with a template to write this down.
Design
The group wanted accessible resources using pictures and large text that would help to start conversations:
I think it would be best to have both (pictures and headings) because some people can understand the picture and some people can understand the words.
Sharon, PWLD
I think having tips on the back of what to talk about might be great as well because it’s easy to forget about something important and get sidetracked.
Alison, mother
We discussed whether pictures from Photosymbols™ (a photo library featuring actors with learning disabilities) or illustrations would be better. While Photosymbols had the benefit of familiarity as they are regularly used in Easy Read documents, some parents said that their daughter/son would find these photos distracting:
I think [Photosymbols] tends to give the impression you’re talking about those particular people whereas the drawing can kind of direct their focus where you want it to go.
Anthony, father
The group decided to make cards with illustrations, simple headings, and tips about what to talk about in preparation for planning or assessment meetings with social workers.
Topics
An existing set of conversation cards, developed as part of the REACH Standards Toolkit133 to help support workers to talk with the people they support and ask questions to make sure they provide the support that person wants and needs, were shared with the group. These highlighted the need for resources to cover doing the things the PWLD wants to do, not just their daily support needs. Similarly, Alison pointed out they should cover the little things that are important but might be forgotten:
I think you need to be a little bit clear yourself before you engage with a social worker … Little things like my daughter really likes to get the newspaper. That’s the sort of thing we’d probably forget to tell people but it makes a big difference to her week … It would probably come up in the cards and you’d think, oh yeah we need to jot that down.
Alison, mother
One decision was how the prompts on the cards should be worded, asking about what is important now to build a picture of that person or asking specific questions about the future. In smaller groups, we discussed the potential topic of ‘where you live now’:
We’re talking about plans for the future so obviously experiences of where you live now would be crucial, but the main objective is what happens next … I think ‘where I live now’ is too specific, maybe ‘what’s important’, or ‘what do I want to carry forward’.
Anthony, father
In a wider group discussion, we agreed that the cards needed to help people to build on knowledge about what is important now to think about what would be needed in the future.
We asked about other topics that should be included:
How to pay a bill, how to get the balance of being independent, and getting the right support and advice.
Sharon, PWLD
What about financial advice? You know what it costs and how much money you can have in the bank before you get the help and all stuff like that.
Linda, mother
Information about what your rights are about choosing where you want to live.
Fern, mother
This led to the inclusion of a set of ‘information cards’, alongside the conversation starter cards.
We brought mocked-up examples of topic cards to the group and asked people to try them out. This particularly helped the development of the detailed prompts on the backs of the cards.
Sessions 6–9: guest speakers
In the subsequent four sessions, we invited guest speakers, based on what the group said would be helpful. Speakers included:
-
users of ‘Shared Lives’ services (a man with a learning disability and his Shared Lives carer)
-
the head of a community-based learning disability service and someone supported by that service
-
a social worker
-
the head of an organisation supporting PWLD to design their support using ‘life planning’.
These sessions started with ice-breaker games. Guest speakers were then asked to give a brief introduction about who they were and what they did. Guest speakers with learning disabilities were asked to talk about their experiences of their living situations. The members of the group were then invited to ask questions. The Q&A was structured as a conversation between the guest speakers and group members, with minimal input from the research team.
This helped to identify key issues to include in the conversation cards. The sessions about Shared Lives and community-based services highlighted questions around deciding where people might like to live (e.g. who they would like to live with or near, how much choice they would have over this). Several group members had no knowledge of the different sorts of service models, highlighting the need for information cards as well as conversation prompts. Conversations with the social worker and life planner about how they work showed that families needed to be able to explain in detail what their wants and needs are and why these are important and should be funded. It helped to focus the cards to prompt families to think about:
-
What are the big and small things that are important in your life?
-
What are the big and small things you need help with?
-
What would happen if you did not get this help?
-
What types of places to live would be appropriate or not and why?
Over the 2-month period of sessions 6–9, the research team developed an initial set of cards based on the feedback from the first five sessions and learnings from the guest speaker sessions.
Sessions 10–12: finalising resources
A full set of conversation cards were sent to group members for feedback. The initial set used Photosymbols images as a placeholder while an illustrator was commissioned. Sessions 10 and 11 focused on the content of the cards. An illustrator came to session 11 to get initial ideas from the group and show sample images. Between sessions 11 and 12 (7 weeks) the co-design group members were sent images of the cards as these were developed and provided feedback on the illustrations and format of the cards. Feedback led to decisions including:
-
Using illustrations rather than Photosymbols: ‘I think that most photos are too specific and don’t convey the concept or meaning … Your sketches would get the conversation going’ (Anthony, father); ‘It makes it feel a bit cosy and nice to approach’ (Alison, mother).
-
Keeping images and writing in separate white boxes: ‘I like it in the box’ (John, PWLD); ‘The box one seems clearer though, that’s like the picture there and the subject underneath’ (Andy, PWLD).
-
Changing from a picture on the front and prompts on the back to both a picture and prompts on the back so that people could see the picture and writing at the same time.
-
Font size was increased. Abbreviations were removed.
-
Creating an online version with downloadable, editable PDFs for notes.
-
Black and white illustrations: ‘Love the black and white one, colour ones are OK but guess would cost more and not sure they’re better’ (Alison, mother).
-
Changes to hairstyles and clothes to make people look less ‘dowdy’, more people with mobility aids, more people from different ethnic backgrounds, changes to individual pictures that were unclear.
-
Keeping the information content despite its density. ‘It seems like a lot but you’ve got a lot to cover, it’s good to have choice and pick out the relevant ones’ (Fern, mother). Clear instructions were included to emphasise that people did not need to look at all the cards.
-
Adding topics such as menopause and seeing a dentist.
-
Adding further detail to prompts, for example, having a lock on your door, having your girlfriend/boyfriend stay over.
-
Moving ‘ideas and tips’ to a separate card so that they do not distract from the conversation prompts.
-
Calling the cards ‘Planning Ahead’ cards and the booklet ‘Me and my plans’.
Celebration event
Group members chose to have an in-person event. This was an opportunity to meet in person and celebrate their achievements. The event included games, a quiz, group members bringing in their art, and time to socialise. Each group member was presented with a ‘goodie’ bag, including the finished cards and booklet, a card thanking them for their contribution, and a star ornament. Those who could attend fed back that this was an important event to end the project and meet other group members.
Feedback on sessions
Tables 8 and 9 show comments from the feedback questionnaires. Six group members gave feedback after the third session, and four after the final session (before the celebration event at which the final ‘Planning Ahead’ cards were shown).
| Question | Comments |
|---|---|
| How did you feel about seeing the film of PWLD and families? |
Love it
The film made useful watching, many thanks to those who took part and were open to sharing their thoughts – I think this could be useful tool for other professionals |
| How did you feel about talking in the group? |
Learn to listen to each other
I can talk when I want to Lovely group of people from different backgrounds You ain’t alone in a group there are others who listen and will tell their stories |
| How did you feel about deciding the important things for the group to do? |
Group do have lots of choices of what they want to do
It is difficult to know what is the most important thing for the group to do as I am not as clear on aims and deadlines as those of who you leading the project |
| Was there anything you wanted to share that you didn’t have the chance to in the group? | 5/5 ticked ‘no’ |
| What could we do better for future meetings? | Nothing I feel they work really well. Especially as due to COVID it has all been done on Zoom which is sometimes hard for PWLD Not sure keep doing what we are trying Arrange for actual service providers to describe what they have to offer … we have been exploring what we would like future planning to include BUT we also need to discover just how, practically, we can go about achieving this, AND with whom |
| Is there anything else you want to tell us about the group meetings? | I think they have been well planned and managed to ensure that all have an opportunity to give their input |
| Question | Comments |
|---|---|
| How did you feel about talking in the whole group? |
I preferred working in larger groups
I thought this was well managed by the team – those that had not spoken were invited to give their views. I always felt I was able to say what I wanted |
| How did you feel about working in smaller groups? |
OK but preferred larger group
Worked well – would have liked more opportunities to do this – so clever how Zoom could be used to send you into a group |
| How did you feel about talks from guest speakers? |
Very good, essential for the project
Excellent – so valuable – a real perk of being part of this |
| How did you feel about the amount of work you had to do for the group meetings? | No issues – felt I could have done more but difficult to be motivated outside of the meetings – not sure the group ‘gelled’ together effectively to make working outside of the meetings happen |
| How did you feel about the final resources we made in the group? |
I thought it was good and, hopefully, helpful to others
Hard to comment at present – but what we have seen looks good |
| Who made most of the decisions in the group meetings? How did you feel about this? |
Multiple choice of ‘group members’, ‘researchers’, ‘group members and researchers together’: 3/3 picked ‘group members and researchers together’ Knowledge and experience from all was most useful Group members and researchers together – decision-making went well on the whole- only once did I feel that feedback from a small group session was seen as wrong by one of the researchers |
| What could we do better if we did this again? |
Few more members in the group? Would be nice to have slightly larger group to increase different views/ideas especially if folk unable to attend a session
First time using Zoom for this type of work and think it was harder as did not have the informal chats that happen before and after face-to-face meetings |
| Is there anything else you want to tell us about the group meetings? | I thought the way it all went was good because everyone involved was prepared to listen to other people’s life experiences and often act upon them without argument or disagreement |
This feedback led to inviting service providers as guest speakers and further clarifying plans for future sessions.
Reflections on the co-design process
Online meetings
The initial decision to run the groups online was practical as there was a wide geographical spread of participants and ongoing concerns about COVID-19 infections. Two PWLD who lived locally and could not use video-conferencing attended in person and joined online with support from the research team. There were some downsides to the online format, which reduced opportunities for informal conversations, and one participant commented that they were not sure if ‘the group “gelled” together effectively to make working outside of the meetings happen’. A WhatsApp (Meta, Menlo Park, CA, USA) group was set up in the final months of the co-design process, but this could have been done at the start of the project to encourage group members to stay in touch between sessions. The celebration event allowed the group to meet in person, although several members were unable to attend due to illness.
Flexibility
Flexibility was key to the co-design process. The workshops were originally planned to take place over 6 months, but this was extended to 8 months to allow time for the illustrator to design the cards and for the group to review and feedback on the cards. This meant that there was time to really listen to group members and make changes based on their feedback. Plans for stage 3 were adjusted to fit these timelines, ensuring that the decisions could be implemented and that maximising the group input into resource development could be prioritised. Similarly, by not planning all the sessions in advance, there was flexibility in the type of resources that could be developed, who would be invited as guest speakers, and how sessions were run.
The downside was it was harder to give group members a clear picture of the plans for the group sessions. This was reflected in the feedback that a group member said was ‘not as clear on aims and deadlines as those of you leading the project’. This could have been set out more clearly in the first sessions, and the group could have been reminded of the aims, progress and outstanding tasks at the beginning of each session.
Involving different perspectives
Keagan-Bull’s role co-facilitating the meetings was a key factor in the success of the group. He reflected, ‘I think that me giving my own experiences helped people to be able to talk a bit more’. PWLD and parents working together also enabled participants to share their perspectives. Feedback showed that group members particularly enjoyed the sessions involving guest speakers. Reciprocity is a key principle of co-production,134 and the opportunity to speak with professionals and people who used services was a benefit to the group.
Stage 2 output
A newly developed set of 102 ‘Planning Ahead’ cards (available in physical and digital formats; https://sway.office.com/5LjAwlV0OFsHjBAj) are designed to help families to prepare for meetings with social workers to discuss future plans (Figure 3). They are accompanied by a ‘Me and my plans’ booklet in which families can write down what they discuss and write a ‘to do’ list for future planning.
FIGURE 3.
Example ‘Planning Ahead’ card.
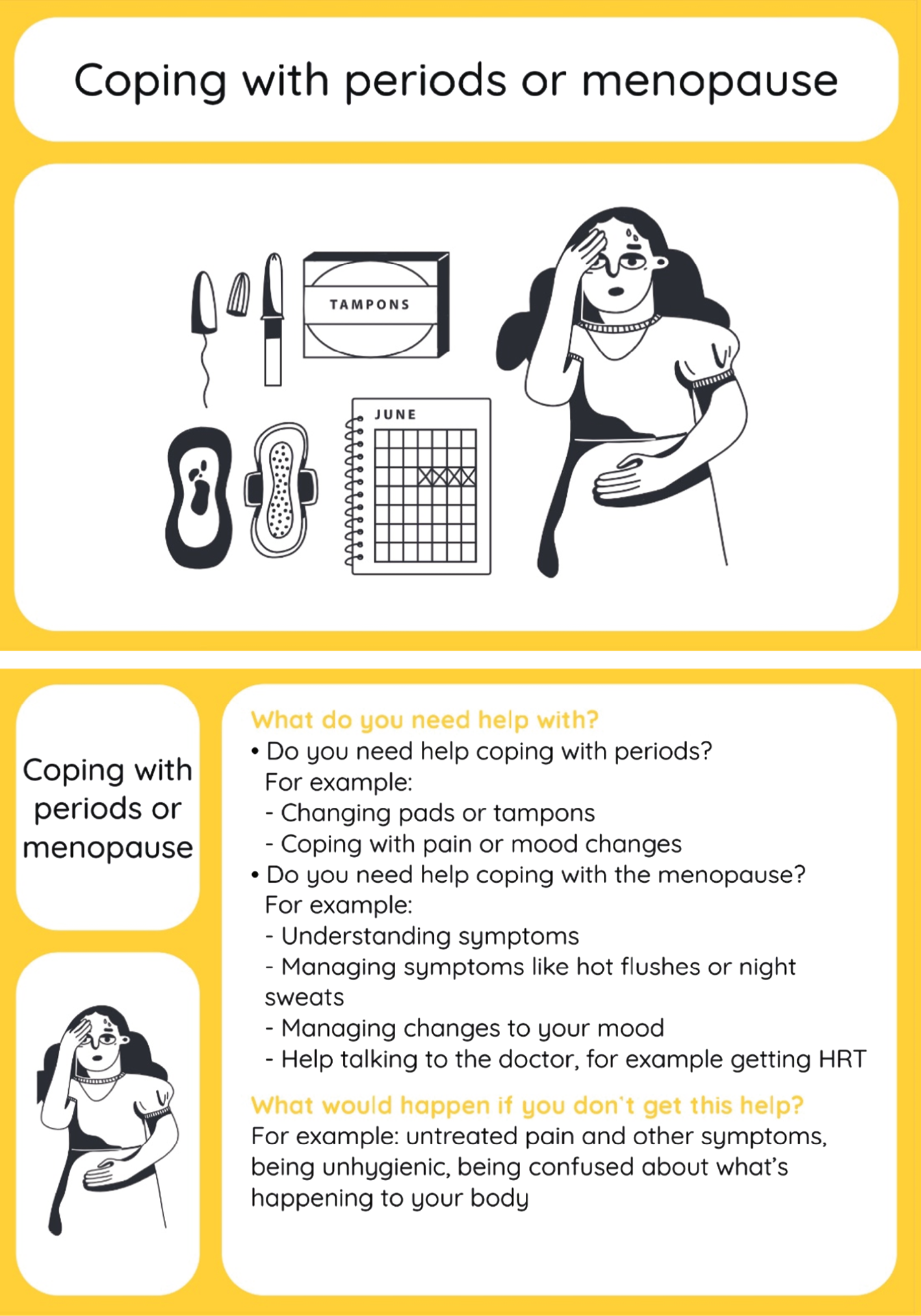
Cards are A5 size and include a picture, a label and prompts for discussions. There are seven categories of cards:
-
things I like to do
-
things I might need help with
-
home: what is important?
-
people in my life
-
about me
-
mum and dad getting ill or dying
-
information cards.
Stage 3: introducing and evaluating ‘Planning Ahead’ cards
Objective
The objective was to introduce and evaluate planning cards to support older PWLD and their families to prepare for parental loss and alternative living arrangements.
Design
Small-scale evaluation study and stakeholder feedback sessions.
Sample
The sample included eight families of PWLD (aged ≥ 35 years) who live at home with their parent(s). The cards were aimed primarily at family carers (parent, sibling or other close relative), but their relatives with learning disabilities were included as study participants if they were able (and wanted) to give informed consent. Seven parents, 1 sibling and 4 participants with learning disabilities were included (a total of 12 participants).
There were five relevant stakeholder groups, including the Public Advisory Group and the Greater Manchester Growing Older with Learning Disabilities (GM GOLD) group, and PWLD from 3 day centres who were interested in planning ahead.
Stage 1 participants who had not been part of the stage 2 co-design group were invited to take part in stage 3; gatekeepers from relevant organisations passed on study information to potential participants; and social media was used to publicise the study.
Data collection
Family feedback
Participating families were sent the following by post, with online links to the same material sent by e-mail:
-
baseline questionnaire
-
a set of ‘Planning Ahead’ cards and ‘Me and my plans’ booklet with information about using them
-
feedback questionnaire.
A follow-up questionnaire was sent 2 months after ‘Planning Ahead’ cards had been used.
Baseline questionnaire
This questionnaire asked for demographic data and participants’ current views on planning ahead, with regard to (1) level of concern about the future, (2) preparedness for the future and (3) steps taken to plan for the future in the last 6 months (see Report Supplementary Material 11).
Using the ‘Planning Ahead’ cards
We provided written information and a video about how to use the cards. The cards were designed to allow flexibility and so this included different ways of using them (with and without the family member with a learning disability, and using only some cards). Families were asked to use the cards on at least one occasion but had 2 months to use them as much as they wanted.
Feedback questionnaires
Participants were asked to complete a brief feedback questionnaire each time they used the cards. Family members and PWLD could complete this together. The questionnaire was sent via post and/or e-mail, according to the participants’ preference. It was developed specifically for this study and included questions about how they had used the cards, what they liked or did not like about them, and any thoughts, feelings or actions the cards prompted (see Report Supplementary Material 12).
Follow-up questionnaire
Two months after receiving the cards, participants were asked to complete the follow-up questionnaire (see Report Supplementary Material 13). This contained the same questions as the baseline questionnaire, with additional questions about the extent to which plans had been influenced by using the cards.
Stakeholder feedback
Five stakeholder groups were sent the cards, the booklet and a link to the online version. They were asked to provide feedback on how useful they thought the cards would be, how the cards might be used, and what changes might be needed.
Results of stage 3
Feedback on the cards from 12 family participants (7 parents, 1 sibling and 4 PWLD) and 5 stakeholder groups is presented below alongside an outline of actions taken as a result of this feedback. Family participants indicated that they used the cards one to three times over the 2-month period, sending the feedback questionnaires back at the end of this period. Those who provided feedback on individual cards did so for four to seven cards (all looked at cards from several different categories). Two families provided feedback on whole categories for two to four categories. Stakeholder groups gave general feedback about the cards as a set, with some comments about specific cards.
Design and content of cards
Overall, the design and content of the cards were well received, particularly the size, bright colours and pictures (Table 10). The number of cards could be overwhelming, but families said that they could choose the cards that were relevant to them and that the cards covered a good range of topics. The prompts on the backs of the cards were viewed as useful and helped families to think about details that they would not have considered without the cards. The ‘Mum and Dad getting ill or dying’ cards were challenging to look at, but families felt that this was an important topic to cover.
| Feedback | Quotes |
|---|---|
| Size, colours and pictures are helpful | Perfect size. The black on white background makes the pictures and writing stand outCS28, motherThe group feel that they are bright, good size, simple images Day centre 1[Son] liked them, especially the ones smiling … I liked the girlfriend and boyfriend one – it’s like me and my girlfriendMA9, mother, and M5, PWLD |
| Talking about dying is difficult but worthwhile | It was good because it shows you can be sad and it is okCS28a, PWLD[Son] got a bit upset about losing his dad, but he’s got to face the other part about losing me MA9, mother |
| Prompts encouraged detailed discussions | Good range of questions to prompt discussion – led to good answersLW19, motherThe discussion points on the back of the cards were very helpful. They were good prompts that I maybe would not have thought of otherwiseCS28, mother |
| Cards were accessible to PWLD | It was surprising and refreshing how the cards we used were understood therefore making the ensuing use of them fun and pleasurableCS28, motherVery informative. They asked a question but it wasn’t too hard for people with special needs to answer … [M5]: I like them, they were easy to understand the picture on themMA9, mother, and M5, PWLD |
| Prompts could be difficult for PWLD | Some of the cards we found difficult to use as [daughter] always needs someone with her to help with tasks LW19, motherThere are too many words. Some people may be able to read what the words are but not understand what they mean. Most people would need support to use these. Some people would like to look at the cards on their own so that they can think about them and make their own decisions. The font size needs to be bigger GM GOLD |
The main criticism of the cards was that prompts on the back were not accessible to PWLD, meaning that they could not be used without support. While the cards were designed to be used within families, some people wanted to be able to look at them alone and some parents thought they would be easier to use together if the prompts were more accessible.
Table 10 provides examples of quotations from free-text feedback on the design and content of the cards.
Impact on planning
Feedback from participants suggested that the cards have the potential to aid future planning. Table 11 presents descriptive data on participants’ concerns, preparedness and steps towards planning for the future, at baseline and follow-up. Descriptive statistics show little change in average scores on these items, but the free-text responses show more nuance. Whereas some scores on these items improved, other participants felt more concerned and less prepared after using the cards. The free-text responses showed that this was often because the cards had prompted them to think about the future. For example, one mother whose ‘concern’ score increased from 1 to 8 stated, ‘My daughter is more concerned than me. Talking to my daughter has made me realise we need to sit down and have a proper family chat’. Her preparedness score increased from 4 to 6. Table 11 shows that the mean helpfulness score for the cards was 8.3 out of 10 (range = 6–10).
| Baseline, mean (range) | Follow-up, mean (range) | |
|---|---|---|
| Level of concern about family’s future living/caring situation | 6.8 (1–10) | 6.3 (1–10) |
| Level of preparedness for future changes in family’s circumstances (including living and caring set-up) | 5.5 (3–10) | 5.5 (2–10) |
| Extent to which family has taken steps or action for planning ahead | 5.9 (2–10) | 5.3 (3–9) |
| Extent to which planning steps/actions have been influenced by the use of the planning cards | N/A | 8.0 (6–10) |
| Helpfulness of cards | N/A | 8.3 (6–10) |
The free-text responses gave detail about the impact the cards had on families’ planning (Table 12). Some cards, particularly the ‘Things I like to do’ set, prompted some shorter-term planning, such as plans to go on holiday, try different foods or restart attending a day centre. The cards also stimulated thinking and discussions about longer-term plans, including where the person may live in the future and what might be needed to put plans in place. In some cases, families used the cards to add to existing plans. Some feedback suggested that the cards would need to be used in collaboration with social care professionals for the plans to be put into place. There was frustration with the lack of support in this from professionals.
| Feedback | Quotations |
|---|---|
| Cards stimulated short-/medium-term planning | Talked about wanting to go on holiday again with her day centre as they haven’t been since pre-COVIDLW19, motherDay centre: It made me think about how [son] would see it from his eyes. It helped me to think about what he would like and what is available. Helped to think of questions I want to ask LS19, mother |
| Cards stimulated longer-term thinking/planning | The cards have certainly brought to the fore how much there is to take into account when life decisions have to be made for future care CS28, motherLiving near people I know: The future. To live in the same area. To live near family. Sister: I would want to live with [sister] in the futureCS28a, PWLDMum card: [Daughter] suggested a place she would like to live LW19, motherLiving at home: Clearer about what [son] needs to stay at home. Realistic about what that would look like. A bit more positive LS19, mother |
| Families added to existing plans | I looked at the Plans we already have in place. [Daughter] and I looked at the questions to see if we needed to incorporate more information in our existing Plans … I’d never thought about writing about how my daughter’s moods are and what help she would need during her period but the questions on the cards acted as prompts and really helped me to include more detailed information in her ‘Hospital Passport’MAF, mother |
| Role for professionals | The cards could be useful for people in supported living when they do their care plan GM GOLDProfessionals need to be involved as parents need to be able to explore all options in depth and detail … I want to know what a residential unit would offer [son] but don’t know where to look or start. I have asked for support but am still waiting. This makes me feel sad, lonely and frustratedLS19, mother |
Actions following feedback
The feedback on the prompts on the back of the cards was mixed. The level of detail was reported to be important to generate conversations and suggest details that families had not previously considered. However, the prompts were inaccessible to some PWLD. Rather than reduce the level of detail and lose the benefits of the prompts, we developed new cards with two to four simple questions for each topic set that could be used when families did not want to use detailed prompts. The information about using the cards was updated so that it was clearer about how to use the prompts.
The cards were designed to be used by families in advance of meetings with professionals. However, feedback showed that involving social care professionals when looking at the cards could be beneficial. The information was updated to include reference to involving professionals. The cards will be included in the OpenLearn courses for families and professionals (see Chapter 7), and we are working with other organisations to ensure that the cards can be made widely available. We have also highlighted the ‘ideas and tips’ and ‘information’ cards, which give suggestions for putting plans into action and finding the right support, to address the lack of support from professionals that participants experienced.
Summary of stage 3 outcome
-
Families found the ‘Planning Ahead’ cards useful and fed back that the cards were well designed and covered relevant topics.
-
The cards have the potential to help families of PWLD begin to make plans for their future care/living situation. However, without professional support to put plans in place, families could end up feeling more concerned but unable to take actions to address these concerns.
-
Feedback suggested that the cards could be used more widely than within families and that social care professionals could be involved.
-
Changes to cards and accompanying information were made including an additional six ‘questions’ cards to make prompts more accessible.
-
Cards will be made available to PWLD, families and professionals.
Discussion
Across the three stages of WP4, findings showed that older PWLD and their families were aware of the need to make changes to their support and living arrangements, and many had made attempts to do so. However, they faced significant barriers to planning for such changes and had not received the support they needed.
What people want and need
A key barrier to planning was not seeing viable alternative living situations that would allow people to live a life based on being valued and having control and independence. Moving out of the parental home should be an opportunity for increased autonomy and independence, but PWLD and their families were concerned that it could have the opposite effect without the support to continue choose what the person does, with whom, and when.
Similar to WP3 findings, participants wanted to live alone (or with someone else they chose); be near family and friends; be supported by people who know them well and care for them; live in a location that suits their lives; and have control over what they do and when. However, this felt out of reach for many families and in some cases led to parents not making plans. Although WP3 findings show that good support is possible, it also found poor practice even in apparently excellent providers, suggesting that parents’ fears are well founded.
The planning process
Once PWLD and their families decided to plan for future support, they needed information about what might be available and how to start the planning process. Many worried that they would be slotted into ‘voids’ rather than having support built around what they need. There were concerns, particularly from families of people with more profound learning disabilities, that institutional, residential care would be their only option, reflecting concerns raised in previous studies. 34 Families wanted information about alternative models of support, including examples from other PWLD who had moved and were living good, independent lives, supported by people who know them well.
Most participants found a lack of professional support to make plans. Conversations with social workers or other LA staff were seen as a hoop to be jumped through or a barrier to planning. Participants presented a picture of an overstretched system only able to respond to a crisis, reflecting WP1 findings of a lack of systemic approaches and support for planning for older age for PWLD and their families. The issue of reactive social services was highlighted in the 2012 government White Paper Caring for our Future: Reforming Care and Support,135 which called for people to have the information and support to make a choice between high-quality options. Our findings suggest that little has changed in the last decade.
‘Planning Ahead’ cards
Work package 4 originally proposed developing a ‘decision aid’ to use with social care professionals to plan ahead. Stage 1 showed that barriers extended beyond families needing help to make a defined set of decisions. Co-design participants wanted resources to give them confidence to tell social workers what they want and need. The ‘Planning Ahead’ cards were designed to help start conversations within families, highlight in detail what is important to the person and what they need, and help them to make the case to social workers and LAs about why these factors are important and should be supported. Initial testing of these cards suggested they have the potential to be a helpful first step for PWLD and their families wanting to make plans for changes to their living and support arrangements.
Conclusion
Work package 4 highlights the significant barriers that PWLD and their families face in making plans for changes to living situations and preparations for parental death. PWLD should be supported to live independent lives well in advance of their parents dying or becoming too unwell to support them at home, but many families were worried they would reach a crisis point without plans for this. The co-designed ‘Planning Ahead’ cards are a promising resource for families but are one small part of what is needed. PWLD and their families need to be confident that there are viable alternatives providing excellent support and help to choose the option that will enable them to live in a way they want and need.
Chapter 7 Work package 5: co-production of resources and training materials
Plain language summary
-
We describe the workshops we held to work with different people to produce our project recommendations.
-
We talk about the Easy Read resources we shared with self-advocacy groups so they could join in this work.
-
We describe what kind of issues were talked about in the workshops.
-
We describe two resources that have been produced to help professionals and family carers support older people with learning disabilities on the Open University website.
This WP was designed to deliver the final project objective (5):
To co-produce actionable recommendations for commissioners and providers, resources and decision-aids for carers and PWLD and ‘BTCO’, and online training materials about care in later life for social workers and professional carers.
Two co-production events were held, a hybrid event in Manchester and online event, with an Easy Read pack cascaded to self-advocacy and family carer groups across the UK. Our dissemination plan (see Appendix 4) included the production of decision aid tools and resources for family carers, two courses on the OU OpenLearn platform, one aimed at family carers and one at support workers and health and social care professionals, and a course published on the British Association of Social Workers (BASW) website.
An additional stakeholder event was added to the project design after the award of additional funding to extend our focus on the provision of support in the north of England.
Co-production events
Two co-production events were held to share preliminary findings and discuss the implications of these with a stakeholder audience. These were designed to be formative, with the discussion in the first event feeding into the design of the second. The first event was hybrid and took place on 16 November 2022. Forty-five people attended (16 online and 29 in person at Manchester Metropolitan University). The second event took place on 14 December 2022 online and was attended by 32 participants. Both events lasted 2 hours 15 minutes. Participating stakeholders represented a variety of organisations including self-advocacy group members, family carers, representatives from NHSE and regional trusts, the CQC, LA delegates, disability charity organisations, service providers, commissioners and academics. The event was also attended by members of the research team, co-researchers and some Professional and Public Advisory Group members.
The two events had a similar structure. The research team introduced the research project and explained work done in WPs 1–4. An ice-breaker activity focused on collecting excuses for poor support used to justify poor practice. This was followed by two short films based on initial findings from WPs 3 and 4.
The WP3 film, ‘Living well, ageing well’, presented the ethnography work, summarising early findings around what it means to live well and age well with a learning disability. A case study described what excellent individualised support looks like and highlighted the role of providers. The film also flagged some negative findings and raised questions around these to be considered by the audience.
The WP4 film, ‘Thinking ahead’, focused on co-produced research on thinking ahead and EOLC. The film showed examples of proactive EOL planning and challenges the research identified as well as details of the discussion cards (see Chapter 6, section Stage 2: co-designing resources to support older people with learning disabilities and their families to prepare for the future).
The audiences broke into small groups to discuss key questions emerging from the research. The first event focused on questions arising from our developing analysis:
-
Where are the social workers?
-
Why are families still so concerned about the future of their children?
-
Why is good support still so rare?
-
Who is responsible for older PWLD who do not have a family?
-
Why is there so little focus on people ageing?
In the second event, we focused on four broader questions about support practice that reflected our ongoing analysis and feedback from the first event. There was inevitable overlap in places:
-
How do you know if support is good or excellent?
-
What helps you to know that or could help you?
-
Why did our research find poor practice?
-
Who is and who should be responsible for making sure people have good lives?
What did we learn?
In the following section, we summarise the discussion in relation to the questions asked and present our developing co-produced recommendations.
Where are the social workers?
Attendees discussed current pressures within social work including poor pay and conditions and how the role has become one of reactive practices largely focused on crisis management. The question of who is responsible for co-ordinating support and being the first point of contact for PWLD and their families was discussed. Should or do social workers have an elevated responsibility to oversee support for PWLD as they grow older?
Why are families still so concerned about the future of their children?
Attendees stressed that most families love and care, but are also scared to think ahead. Stories about abuses in social care settings and previous experiences with support services further erode trust that the system will support their relatives. Concern was raised that families will be prevented from being involved in the lives of their adult children in the future.
Why is good support still so rare?
A lack of money and resources, and the unequal distribution of these, was discussed, as were related staffing issues around pay, poor conditions and retention, poor service culture and lack of effective leadership. There is a lack of knowledge about what support is available and a lack of awareness of what good support looks like. Good practice examples need to be amplified and shared, and a focus on values-based recruitment is needed to change organisational culture.
There are further systemic barriers to employment and other opportunities for PWLD, and the lack of recognition that people are growing older means that changing support needs can be misinterpreted as somehow ‘going backwards’ or failing.
This question was challenged by some attendees, who attributed the lack of good support to individual staff members.
Who is responsible for older people with learning disabilities who do not have a family?
Answers included PWLD themselves, the state, and all of us, although the last position is ambiguous, and there was acknowledgement that while ideally society would be there to take responsibility, in practice the negative views that many people still hold about PWLD undermine this aspiration. Discussion touched on unsupportive families or families who lack trust in social care provision, the way in which older PWLD are framed negatively, and the interdependency that can develop between PWLD and family members as they grow older. The well-being and preventative strategies embedded within the Care Act were acknowledged as failing in practice.
Why is there so little focus on people ageing?
There was consensus there is a broad assumption that PWLD do not live to older age. Furthermore, the focus on independence as the goal can potentially skew views on people becoming dependent. This in turn can be seen as a failure of services, as opposed to being considered part of growing older.
How do you know that support is good or excellent?
The importance of ongoing feedback from people being supported and their families and evidence that feedback is acted on was seen as central, alongside observing interactions between PWLD and staff or asking if people are happy. The respectful use of language and connections and affection between people were flagged as important, together with evidence of person-centred solutions and the importance of supporting relationships and enabling PWLD to learn new skills. Evidence that people are supported to be part of their community is a further indicator of good support. Asking service managers was suggested, as this group have a good idea about what is happening on the ground. The point was made that you need to experience good support before you can recognise it.
What helps or could help people to find good or excellent examples of support?
Here answers included sharing knowledge about good support and being familiar with what is important to people. The use of paid quality checkers with lived experience to generate knowledge about good service provision was supported, and questions were again raised about people who may not have family advocates, for example, people in long-term institutionalised care.
Why did we find poor support when the services were judged to be excellent?
This was a fundamental question to our project, and feedback was wide-ranging. Attendees commented that there is a wider lack of aspiration around the lives of PWLD, which allows the drift of staff into doing little, particularly in early post-pandemic conditions when new staff might have thought limited activities were the norm. Commissioners and PWLD and their families may have different priorities. Attendees discussed the lack of knowledge that some commissioners have about services, while there was acknowledgement about the engaged commissioners who participated in WP3 and, indeed, some of those in attendance at the event. While the importance of spending time in services was again raised, commissioners responded that this is not practical given the number of services involved. The question of social worker involvement re-emerged, and it was suggested that commissioners (or social workers) could approach potential issues in a more collaborative way by asking ‘We have noticed that this is an issue; how can we support you?’.
Issues around resources for service commission and ensuring that staff match the person’s needs with consistency over time came up again. The paradoxical consequence of family members sometimes accepting poor support because they did not want to disrupt the person’s life with a potential move was linked to discussion about situations in which part of a service may not be good rather than the whole.
Who is and who should be responsible for making sure people have good lives?
In the second event this wider question again led to a lack of clarity or consensus. ‘All of us’ (including local councillors and members of Parliament), commissioners, social workers, ‘decision-makers’, PWLD themselves, and family members were suggested by some attendees. The point that ‘everyone’ can mean ‘no one’ in practice was made, as was concern that family carers should not be expected to take responsibility across their lifetime. The importance of good leadership, co-operation and a collective responsibility were again highlighted.
Key points identified across both events:
-
a lack of attention to PWLD growing older
-
a lack of resources for commissioning and provision
-
reactive rather than proactive practices and a lack of sharing or recognising good practice
-
a lack of resources to provide excellent services
-
a shortage of information and knowledge about good services
-
ambiguity around who is responsible for co-ordinating the support for people as they grow older
-
the failure of the Care Act to improve the lives of PWLD
-
high turnover and failure to match staff with needs and interests of PWLD
-
a lack of trust in services on the part of family carers and PWLD.
Emerging recommendations from stakeholder groups and the cascaded materials
The stakeholder events were designed to get audiences to think about issues arising from developing project findings, discuss and raise further questions, and identify potential solutions to how the support for PWLD and their families can be improved as they grow older. From this, we developed a list of recommendations that can be grouped into recommendations that improve (1) information, (2) oversight and lesson learning and (3) individual support.
Recommendations that raise awareness and improve access to information
-
Accessible information should be provided about options and good support for PWLD, family members, commissioners, providers and staff. Provide opportunities for families/people to find out what their and their loved ones’ options are, what good support is available and give them an opportunity to visit places that offer excellent support. It is important that PWLD and family carers are aware of what good support looks and feels like. Sharing examples of good support among commissioners, providers and support is important.
-
Produce better statistics about how many PWLD there are and what support they may need in the future. This is particularly crucial for families not known to LAs.
-
Start conversations earlier about where people want to live in the future.
Recommendations that improve oversight and lesson learning across the sector
-
Introduce peer learning and critical friends among providers and commissioners. Make good practice well known and have an open and supportive peer-learning set-up.
-
Fund self-advocacy groups to support people in making choices locally.
-
Regularly and proactively listen to people and their families.
Recommendations that improve individual support
-
Match staff to people, encourage and sustain good relationships between the person and staff and avoid frequent changes of key workers.
-
Change staff appraisal processes to become more celebratory and focus on the small things that make a difference.
Cascading session plans and materials
To reach a wider range of stakeholders and enable the involvement of self-advocacy groups in the co-production of recommendations, we created three 1-hour session plans for self-advocacy groups to engage with independently. Each session plan was produced in standard and Easy Read versions (see Appendix 5). The sessions focused on growing older well, making plans (including EOL plans) and how providers can work better. Each session included a short activity (a wordsearch or simple crossword in the standard version; a spot-the-difference colouring picture in the Easy Read version), a comic (standard version) or Easy Read information about the topic of the session based on our preliminary findings and a set of questions for the groups to consider and engage with (example questions: ‘Can you think of some things that help to make a home a caring place?’; ‘Do you have any ideas about what might help PWLD grow older well?’).
The session plans were shared with seven organisations that expressed interest via social media or team networks. We received feedback from a self-advocacy group based in the north. The feedback carried similar recommendations around relationship building and community belonging of PWLD, as well as around person-centred support. Additional issues around ageing were highlighted, such as those faced by PWLD who cannot rely on their family for support and advocacy. The sessions also offered additional recommendations around:
-
Healthy ageing, with focus on regular health checks, general practitioner (GP) appointments, and related follow-up measures. The need to increase awareness of health inequalities, healthy nutrition and physical activity was also identified.
-
Staff recruitment and values, where staff should be recruited based on being kind, encouraging and knowledgeable. Staff should also be able to take on difficult conversations and have capacity to build relationships with people they support.
-
Support choice, with ‘try before you buy’ schemes to ensure that people are not stuck with support that is not well matched to the person.
The additional stakeholder event
A third stakeholder event was held online on 17 February 2023. This had a dual purpose: to share the project findings and further discuss the developing recommendations, and to discuss with attendees largely based in the north of England (outside the research team) what their research priorities were.
There were 22 attendees, made up of PWLD, family carers, and representatives from northern self-advocacy groups and support organisations such as Inclusion North and Mencap Kirklees. Ahead of the event we shared an Easy Read document ‘Things that matter’ (Figure 4) and asked people to think about their priorities.
FIGURE 4.
Things that matter.

The initial discussion after the two films had been shown again covered the following points:
-
One voluntary organisation in the north of England (Mencap in Kirklees) encourages thinking about growing older, but cited obstacles such as sourcing buildings that meet people’s needs in the right places that commissioners will not fund.
-
Challenges around finding and recognising good support led to discussion around the importance of word of mouth, and the idea of a TripAdvisor-like system. There was mention of ‘glossy brochures’ that present providers well, and the need for a ‘try before you buy’ approach as well as a tendency for commissioners to become fixed on one offering rather than a range of options.
-
Again, the question of who is responsible for co-ordinating the support for older PWLD was raised.
-
The issue of waiting lists for a social worker if someone wants to move home was raised, and even if good provision was identified, it might not be offered by commissioners if funding is not available, or people may be told they are not eligible for support. Decisions could take several years when they need not do so.
In response to the ‘Things that matter’ exercise, there was largely consensus around being supported to stay healthy, living in a house you choose with people you choose, and being supported by people you know and like. It was noted that some people do not have family. One family carer thought the remaining points would follow on from living where you choose and being supported by people you know and like. For her, the least important point was planning for old age and death as she thought that this would not be at the forefront of her daughter’s mind. The importance of friendships (beyond support staff) and intimate relationships were highlighted by attendees, as were the opportunities to work in a paid or voluntary capacity. There was a suggestion there should be a Minister for PWLD, and the way in which PWLD are excluded from mainstream support for older people was raised.
The final section focused on what issues people felt were important to address in future research. This generated the following areas:
-
transport in rural areas
-
a focus on the aspiration of home ownership among PWLD with caution that this may not be ‘utopia’, as it can be expensive and people may become isolated living alone
-
the importance of pet ownership
-
the importance of friendships and intimate relationships
-
loneliness among older PWLD
-
how difficult it is for PWLD to access mainstream support for older people
-
knowing your employment rights and benefits-related issues.
Inclusion North representatives offered to cascade project findings across the north-east.
OpenLearn resources
In year 3 of the project, the OU team (Tilley, Larkin and Pawlyn) commenced work on two free OpenLearn courses. They liaised with the WP3 team to identify key findings to shape the development of learning materials for (1) health and social care practitioners and (2) family carers of older PWLD. The authors drew on interview transcripts, field notes and extensive case study material to ensure the educational materials were research informed and evidenced based. The findings were presented within three themes: ‘Supporting people to live well’, ‘Supporting people to age well’ and ‘A caring culture’. When these three areas of practice are in place, excellence emerges. We used the visual motif of a quilt to represent best practice, and the OpenLearn editors created an animation to facilitate learning around these themes (the ‘Quilt of excellence’).
To generate a more critical focus on our research findings and further support the learning journey, we included filmed interviews with expert panel members, who included two self-advocates, a family carer with considerable professional experience of supporting older PWLD and their families, and a community learning disability nurse. Panel members discuss their responses to course activities and case study material, offering guidance and reflections from their personal and professional experiences.
Supporting older people with learning disabilities and their families: a course for health and social care practitioners
This is a 6-hour module, comprising six ‘sessions’. The introduction outlines the course structure and approach, provides details about the underpinning research and sets out the core learning outcomes. It introduces the ‘Quilt of excellence’ and invites practitioners to reflect on their understanding and experience of the term ‘BTCO’ and what this might mean in the context of people getting older. The next four sessions are organised around individual case studies: ‘Becky’, a woman in her 40s, currently living with her parents and preparing to move; ‘Geoff’ a man in his seventies, who living with Shared Lives carers; ‘Robin’, a man with a history of being moved around services (often out of area), now settled in a Supported Living home in his local community; and ‘Susie’, a woman in her fifties with complex health needs, living in a residential care home with nursing provision. Students are invited to engage with extracts of empirical data relating to each person, reflecting on the implications for their own practice. For each case study, we sought additional consent from the person and/or their family members to include their material. The course concludes with a session synthesising the key learning points, an activity exploring how to use the WP4 ‘Planning Ahead’ cards and revisiting the ‘Quilt of excellence’ with an eye to broader systems-based issues.
Supporting an older family member with learning disabilities: a course for family carers
This 4-hour module comprises six sessions focused on providing family carers with practical advice to support planning ahead and to help build resilience. The introduction outlines the course structure and core learning outcomes. Throughout the course, learners are encouraged to keep a log of ‘top tips’ that they can return to (during the course and in the future) and adapt to their own circumstances.
Session 2 explores what is meant by planning ahead in the context of an older family member with learning disabilities, using case material from ‘Becky’ and her parents. Session 3 focuses on developing a plan and draws on the example of ‘Sam’ and his sibling ‘Mel’, reflecting on the experience of planning ahead in the context of Shared Lives provision. Session 4 supports learners to develop skills to advocate for an older family member (and for oneself) to successfully plan ahead. Session 5 explores how family carers can look after themselves and protect their health and well-being in the context of planning ahead and advocating in older age. The final session brings the learning together and introduces students to the ‘Planning Ahead’ cards and ‘Quilt of excellence’. Students are invited to reflect on their top tips list and decide on some next steps.
The courses can be found here:
www.open.edu/openlearn/health-sports-psychology/supporting-older-people-learning-disabilities-and-their-families/content-section-overview?active-tab=description-tab www.open.edu/openlearn/health-sports-psychology/caring-older-family-member-learning-disabilities/content-section-overview?active-tab=description-tab
Full project outputs are listed in Appendix 4.
Chapter 8 Public involvement, contributions and reflections
In this chapter, we describe how members of the public contributed to the project design and funding proposal, the conduct of the research programme, the study’s oversight and management, and development of resources, with suggestions for routes to impact. The study was advised throughout by the public involvement lead, a family carer, who shared:
This project has brought people with learning disabilities, family carers and paid support workers together as participants, whilst also providing an opportunity for people with lived experience to work as partners (that is public representatives). We have been involved from the start of this research – in the earliest conversations to shape the research proposal. We have been welcomed, encouraged and supported by the study team and made decisions across all five work packages at every stage in the research pathway.
Proposal development
The initial thinking behind the proposal and the development of the research questions were informed by PWLD and family carers. The Embolden project, a National Lottery-funded project lead by Oxfordshire Family Support Network (OxFSN) and involving the Co-PI and public involvement lead, focused on the experiences of older carers aged ≥ 70 years. The Embolden project highlighted systemic issues within the social care system to identify older family carers and anticipate and respond to their needs. This gap increased family carers’ anxiety and contributed to a care crisis for their family member with learning disabilities.
The development of the proposal also involved PWLD and family carers. One family carer and two self-advocates were co-applicants. Support was incorporated into the proposal to enable their meaningful involvement.
A family carer who also held a professional role with a national provider and a sibling carer who is also chief executive of SIBS (a charity for siblings of PWLD) were consulted about WP2; they commented on the needs of people with early dementia who are most likely to be living in the community, often with older carers, but whose caring support may become insufficient to enable them to remain at home or in supported accommodation.
Public Advisory Group and Study Steering Committee
To perform a function separate from but complementary to the Professional Advisory Group, we assembled a Public Advisory Group, which comprised four family carers and three self-advocates. The panel was chaired by the public involvement lead, who provided a template for the Public Advisory Group members and project team to each provide a one-page profile to enable everyone to better support each other. One member preferred the term ‘life enabler’ to ‘carer’; the difference was fundamental to that person and emphasised that good support is built on relationships with mutual respect.
After initial larger meetings involving all members, we changed to smaller meetings to make them more accessible.
The separate SSC involved an autistic member of the public who contributed to oversight meetings.
Greater Manchester Growing Older with Learning Disabilities
The GM GOLD group is a team of approximately 15 older PWLD and their supporters that was established in 2019 as part of a study to reduce social isolation among older PWLD in the Greater Manchester area. The team has been supported by Manchester Metropolitan University and other partner organisations since 2018. The study team drew on the experiences and perspectives of the GM GOLD members throughout. Relationships with families, the loss of family members and choice about where people live were important issues arising in the original GM GOLD research. The project was included as an agenda item at GM GOLD meetings across the project.
Researchers and co-researchers with learning disabilities
Participatory research has been key to the success of this study (see Chapters 4–6). Eight self-advocates trained to work as co-researchers on the WP3 ethnography alongside the public involvement lead.
Work package 4 was designed to be conducted with significant involvement by a researcher with learning disabilities, supported by an assistant researcher The WP4 team experienced multiple hurdles in obtaining institutional approval for the adjustments required for the appointment of a researcher with learning disabilities. 136
Public training
Co-applicant training
Training in the value and importance of being public contributors, ethical issues and how to participate with confidence in research was provided by an experienced public contributor. This training provided a short introduction to the research world and emphasised that the public bring an essential perspective.
Key members of the study team attended online Easy Read training. Aside from being enjoyable as an initial team event, this training set the tone for communications across the whole study team and the length of the project. It is an outcome that the public involvement lead is particularly proud of.
Co-researcher training
Co-researchers were trained through a bespoke course developed through a related NIHR School for Primary Care Research-funded grant (see Chapter 4).
To prepare for WP4 data collection, four video-conference training sessions on conducting online interviews and focus groups with PWLD were attended by three self-advocate team members and three PWLD who were graduates of a previous research training course.
Public involvement throughout the study
The public involvement lead introduced changes to the organisation and delivery of the project. This included introducing the use of an illustrated Easy Read orientation slide at the start of meetings to remind members what the project was about, what month we were at in the timeline, and which WPs we were focusing on at the meeting. Presentations and key information were presented visually. As the project progressed researchers presented their reports in a more accessible way using photos, drawings, and plain language/Easy Read. By the mid-point of the study, the public involvement lead considered that she was able to ‘think in Easy Read’, a skill that benefited materials she produced in other contexts. The project logo had artwork produced by a person with learning disabilities (Figure 5).
FIGURE 5.
‘Growing older, planning ahead’ Twitter feed with logo.

We held additional meetings with individual members if they requested them or if we felt there was not enough time at the previous meeting for the member to be fully involved. This was made easier by the use of online meetings due to COVID-19 restrictions. We realised that meeting minutes required high levels of reading and processing skills, and we introduced and circulated minutes as an audio file, which consisted of a more conversational and accessible chat about the meeting content. This format was appreciated by members of the wider team.
Recruitment of staff
Co-applicants with learning disabilities were on the interview panel for project researchers. Public representation on these panels provided insights into candidates’ abilities to communicate with family carers and PWLD. Candidates were asked to consider how they would fully include family carers and PWLD in the study. This was vital when deciding who would be best placed to work on the project.
Work package 1: rapid literature reviews
The public involvement lead commented on draft protocols for the first two reviews. Given the paucity of published research, the authors considered combining the two reviews when writing up the findings. The Public Advisory Group advised the authors to keep these separate to make it easier to communicate the key messages.
Work package 2: service mapping
The WP2 mapping exercise was explained to the Public Advisory Group. Members found the work interesting but were keen to learn of the perspectives of PWLD and family carers in WP3, which they thought would show what was excellent provision.
Work packages 3 and 4: case study ethnography and end-of-life care qualitative studies
The Public Advisory Group and GM GOLD team provided the study team with insights to help with the fieldwork. This included:
-
Advice on how people cope during difficult times, to help identify relevant issues for researchers, to inform the wording of interview questions and to explore how PWLD might deal with challenging times.
-
Thoughts on what was important for the ethnography to look at such as work, holidays, activities, relationships, home décor, and belonging to self-advocacy groups.
-
Discussion about what is important for researchers to consider when they go into people’s homes. This included the possibility of being told to leave at any point in the fieldwork.
-
Discussion of issues around payment and practicalities of carrying out fieldwork.
-
The use of one-page personal profiles for researchers to give to participants ahead of fieldwork.
-
Ensuring participants had time to prepare and were given advance notice of what would be covered in interviews.
-
Thinking about formats in addition to the Talking Mats communication tool used in WP4.
The public involvement lead suggested that participants with learning disabilities should be encouraged to be supported by an advocate or close family member and that participants should be ‘checked in’ with afterwards.
Team members attended GM GOLD meetings. Co-researchers discussed how they felt about travelling to some of the more distant study sites and what support they would need to do this. The meetings also gave academic researchers and co-researchers opportunities to get to know each other.
The Public Advisory Group was instrumental in retaining a case study site which temporarily withdrew from the project because of COVID-19 pressures. The group advised the team to work with the provider, offering extra support to make it easier for them to take part in the research. The study site was retained.
Recruitment in WP4 stage 1 was challenging due to the very specific inclusion criteria. The public involvement lead participated in a recruitment video and snowballed recruitment materials through a carers’ organisation. The Public Advisory Group also encouraged us to revise the inclusion criteria for participation, which resulted in a change to the protocol and ethics approval and enabled additional perspectives to be included in the research.
The group contributed ideas on the format and design of the WP4 ‘Planning Ahead’ cards across the process of development, printing and evaluation.
Work package 5: co-production of resources and training materials
Public contributors played a central role in the three stakeholder groups, chairing the first two events and contributing across all three events. Some members of the Public Advisory Panel and GM GOLD team attended.
Public Advisory Group members contributed to the development of the two OpenLearn courses, notably through involvement in the expert panel format that was used for both courses and agreeing overarching themes and learning outcomes for the two courses. Feedback was provided on Easy Read materials for the stakeholder events and cascaded session plans.
The training resources for doing ethnography were used in a February 2023 event with organisations that work with PWLD across the UK, reviewing how quality checks of health and social care services by PWLD and family carers are conducted.
Public engagement and dissemination
Public team members provided comments on the Easy Read briefing sheets, press release and the project plain language summary, and co-authored a Care Management Matters article. 94
Having co-researchers with learning disabilities led to several benefits for the research:
-
Initiating and opening up conversations: one GM GOLD team member started talking with a participant about their experiences of using walking aids, a topic that the researcher would not have considered. Another team member started a conversation about video games that led to the participant being more engaged with the fieldwork.
-
One co-researcher knew people at one of the sites. This was useful in helping to gain access and people’s trust; however, the co-researcher (and probably participants) found it strange at first to ask people questions about things they already knew.
-
A WP4 participant asked the researcher with learning disabilities about his experiences of moving into a supported living setting, leading to a rich conversation.
Practicalities of challenges faced and lessons learnt
We recognised the need to be responsive and open to new ways of working with public contributors throughout the project. This was particularly important at the early stages of setting up ways of working. A 4 + 1 evaluation tool (a person-centred thinking tool) was used to analyse what was working and not working in the Public Advisory Group meetings to make them more accessible. This led to better ways of working together with changes to processes agreed with public contributors before implementation.
The public involvement lead spoke to WP4 researchers about the experience and value of public involvement in co-producing resources for family carers and health and social care professionals to use. Public members described how there were times when meetings moved at pace so that they did ‘more listening and less contributing’. They would have liked more face-to-face meetings, especially at the early stages of the project. Due to COVID-19, this was not possible, although more in-person work took place towards the end.
As the research was NIHR-funded we had access to the citizens’ benefits advice service, and four co-researchers were supported to individually attend a meeting to check that their benefits would not be affected. This was important to reassure the co-researchers. The project co-ordinator submitted the forms to the Department for Work and Pensions along with the initial invoice to reduce the administrative burden on co-researchers.
University systems for including and paying co-researchers were burdensome and inaccessible. Legal agreements were not in Easy Read and initially individual co-researchers were expected to provide their own indemnity insurance, which would have been expensive and complicated. After discussion this clause was removed and an Easy Read guide for co-researchers was developed. The university payment processes were also not accessible, involving online entry of bank details. Co-researchers were supported to set this up and project manager logged co-researcher hours, and produced and submitted the invoices on their behalf. There was some delay in getting contracts in place, which led to some delay in payment.
Communication methods were key to ensure that the research team engaged with the Public Advisory Group in accessible and appropriate ways. The practicalities of carrying out fieldwork with co-researchers, including travel, needed careful consideration. Occasionally fieldwork visits were arranged at short notice to fit around the needs of the sites, which was difficult for the co-researchers to manage, and sometimes visits were cancelled at short notice, which was disappointing.
Why public involvement is important in a study like this
The public involvement lead worked with the team to ensure that involvement was interwoven throughout the study rather than being a standalone activity, and, as a co-applicant, a member of the Professional Advisory Group and the chairperson of the Public Advisory Group, she was ideally placed to do this. For example, she critiqued and suggested amendments to the overall project video and produced an audio update posted on Twitter and Facebook that described the project aims and early findings to accompany an early interim report to the funder.
Public involvement was essential for the team to ensure the accessibility of study information, gain the trust of participants and acquire knowledge and understanding of specific issues of importance to PWLD. The team acquired insights into the lives of PWLD by working alongside them, for example, practicalities of travel, commitments and life experiences.
There was clear impact on others involved in the project. For example, co-researchers were introduced as colleagues at ethnography sites, which demonstrated to providers and staff members that they were important. This helps to shift the narrative from a deficit model and demonstrates how research can become a space in which people’s contributions are recognised, valued and shared. There was also a visible shift in the confidence, involvement, enjoyment and skills among public contributors (and researchers).
Finally, a public involvement lead can help to create sense of continuity over a long project by being visible at meetings and events. It is important this role is filled by a person with lived experience so that public contributors may more easily relate to them.
Chapter 9 Conclusions and recommendations
In this final chapter, we bring together the main project findings and the implications of these, discuss the strengths and limitations of the project and highlight areas for future research. We finish by presenting recommendations to improve the support for older PWLD and family carers.
We outlined in Chapter 1 how there is little focus in research literature on older PWLD, many of whom continue to live with their families. This is in part due to the reluctance of family carers to support their relative to move from the family home because of a lack of clarity around what support is available and who is responsible for starting these conversations and a lack. Of trust in social care support. Our findings underline this literature while providing evidence of examples of older PWLD leading good lives with exemplary support.
Main findings and implications
Person with learning disabilities can be supported to age well
We found the conditions necessary to support people to live good lives as they grow older are not exceptional: being supported to live alone (or with a partner) in a home that is comfortable, adaptable, personalised, in a community, possibly with pets, a garden or access to outside space, with the support of people they like and who like them.
Achieving this involves knowing the person well, matching staff and having staff consistency, working with families, and proactively engaging with professionals and services that support people to age well, and having the requisite skills and knowledge to understand and recognise the physical and mental health, social and emotional changes associated with ageing. The relationships between PWLD, support workers, professionals and family members are key to living a good life, and this involves effective communication, time and a sharing of knowledge, the co-ordination of specialised, bespoke and person-centred planning and a focus on pre-empting and responding to ‘health-related loss’,70 including the involvement of primary care and, where required, the learning disability multidisciplinary team (MDT). The sharing of experiences of what works for each person with commissioners is key to planning for that person and informing future commissioning for others. Good practices such as EOLC planning, dementia assessment and management need to be embedded as routine.
An absence of engagement with, or recognition of, the ageing of people with learning disabilities
There is a lack of relevant expertise around how to commission, design and deliver services for this group well. There is an absence of specialist knowledge or even recognition about the needs of this group, including issues around good support (health and social care) and design. We found the LA was trying to find evidence or examples to help with designing the new service in NCH_2.
While there is growing research around good service design for older people, including people with dementia, a large gap remains for older PWLD, including those with additional needs. This lack of attention or consideration paid to the ageing of PWLD leads to a lack of opportunities for people to lead fulfilling and meaningful lives as they grow older. This absence is also reflected in the literature as our reviews demonstrate. In effect, active ageing8 is denied to this group.
Consistently low levels of ambition and aspiration
While we found that people living lives that continue to grow and expand is a measure of excellence, we also found evidence of static and constrained lives that were unnoticed or unremarked upon by social care staff. The low levels of ambition and aspiration ascribed to this group are underpinned by common assumptions. For example, existing research and our findings reflect a consistent assumption that family carers should be supported to provide care for as long as possible, individualising caring responsibilities while, at times, also failing to engage with the views, wishes and ambitions of PWLD. Related to this is the tendency for discussion around planning ahead to be tied to people who are already older.
The potential development of mutual caring interdependencies that obstruct or block future planning36 should be viewed as a concern rather than an explanation for the lack of future planning. There is an uncomfortable circularity here that runs counter to policy rhetoric around PWLD having independence, autonomy and control. The strengths of a Shared Lives model are ultimately undermined by this model mirroring the experiences of older family carers and PWLD who continue to live together. It therefore presents the same challenges of carers growing older and unable to continue to provide support. The use of day centres embedded within this model also runs counter to the notion of people living ordinary lives. While we found that well-designed day services can function as sites of belonging and community, we question whether the stated aims of a day service – that is a day opportunity – is really met. Although it seemed to meet the need to belong with peers, it did not support belonging to the wider community, and we question the actual opportunities on offer. We were left unsure whether they are places people go because it gives them something to do, and why are they do not offer access to wider community activities.
A lack of knowledge about what good support looks like is also part of this problem. Again, here the needs of the family carer can over-ride those of the PWLD, as people can remain living in a place that is not appropriate because the family carer thinks it is safe and familiar. This, in turn, may relate to the reported disillusionment and lack of trust family carers have in the ‘system’.
A lack of current and accessible information, resources, support and ambiguity around the responsibilities
There is a lack of up-to-date and accessible information about what support is available in local areas and more generally a lack of knowledge about support options and rights. Evidence underlines the importance of the role of social work in supporting people to move to a new home before ageing associated problems begin (and interdependency develops). However, the lack of social work involvement or even visibility is striking in our findings. There is, furthermore, a lack of clarity around who is responsible for co-ordinating the future planning for PWLD, meaning that family carers take this role by default, which can be burdensome. It also leaves older PWLD who do not have family unsupported. The stress and sense of panic that family carers feel was part of the rationale for this study and has been confirmed and explained by it.
The unhelpfulness of the label ‘behaviours that challenge others’
Our findings underline how the use of this label is problematic and can be used to legitimise and justify practices of poor support. Attention should always be paid to addressing causes of distress rather than labelling it. This is particularly pressing given the financial costs of managing ‘BTCO’ through bespoke training and programmes. WP3 findings demonstrate that when people are supported to live good lives, the label of ‘BTCO’ they might have acquired in the past becomes irrelevant. We therefore need to refocus our attention away from labelling people and behaviours and towards quality support and solutions that allow PWLD to thrive as they grow older.
Finding poor support in services identified as ‘excellent’
The fact that WP3 found examples of poor support within the carefully selected – through WP2 – exemplary services points to an issue in how excellence is identified and monitored. This has implications for how commissioners monitor the quality of services, how often they do so, what evidence they seek and from whom they seek it. WP2 commissioners cited a shortage of consistently good provision, so innovations such as the proactive approach by one large CCG and its LAs to invite their best and other new providers to work with them on a new commissioning framework are promising. How this delivers over future years will also require a more proactive approach to quality monitoring involving feedback from PWLDs, families, and health and social care agencies. Strategic oversight at integrated care system level as modelled from the Safe and Wellbeing Reviews of people in long-term inpatient care, including an NHS senior responsible officer for learning disability and autism, people with lived experience, provider collaborative representatives, and clinical and LA input, may be well positioned to both monitor provision and forecast so that provision can be commissioned enabling people to plan ahead with confidence.
Limitations
The project was conducted against a backdrop of COVID-19 and the associated government lockdown restrictions. This had an impact in terms of sites withdrawing from the project and the rescheduling of fieldwork (WP3) and difficulty recruiting people (WP4). Despite this disruption, we were able to complete the project on time and largely to plan. Our reliance on providers for the recruitment of WP3 participants resulted in a homogeneous sample in terms of ethnic background; all PWLD participants were White British. Our project was further limited to England rather than including all four nations.
The discussion cards produced in WP4 may be in formats and have content that exclude some people, which needs further testing. Attempts to plan by families may be frustrated by insufficient resource and options to achieve what people want, raising expectations that cannot be met.
Our focus on ‘BTCO’ has proven to be both a limitation and a resource. There was a circularity to the research design in that we were focusing on something we found to have little explanatory potential. This was apparent in the first two scoping reviews in WP1. This can also be seen as a strength, however, as it led us to an understanding of the consequences of the application of the label that emerged through the research process and was not an a priori assumption about the term.
Patient and public involvement
As described in Chapter 8, our ‘formal’ public contributors were involved from the design stage, across the five WPs and in project outputs. We took a flexible and iterative approach to involvement, thinking about how people could contribute, and how we could improve communications and engagement during the project. We developed excellent working relationships across the team that were productive and helped us develop confidence in working together. Overlap with NIHR projects (NIHR128616 and NIHR SSCR P150) helped us learn how to better work with and involve members of the public in research.
We will produce an accessible and engaging findings document and short film to share with our contributors and more widely.
Equality, diversity and inclusion
Recruitment in WP2 involved England-wide stakeholders in health and social care; the geographical spread achieved included where NIHR research has least reach. Participants in WP3 were, however, White British, while in WP4 there was a diverse sample reflecting the local London population. Diversity of the WP4 sample was increased by prioritising participants from other ethnic minority backgrounds and approaching ‘gatekeeper’ organisations in more diverse areas. Easy Read versions (with video alternatives in WP4) were created of all participant information. Inclusive data collection approaches (e.g. Talking Mats and Books Beyond Words) were used. A key output, the ‘Planning Ahead’ cards, were co-designed by PWLD and families. These include pictures, large text and an information video about how to use them. The illustrator was instructed to include images of people with different impairments and from different ethnic backgrounds.
Work package 4 did not include people without the capacity to consent, which excluded many PWLD. However, we included family members, which meant that these experiences were included and the cards were designed with these families in mind. Inclusive approaches were used for information, consent and data collection to include different participants.
Capacity-building
Opportunities for junior researchers in the team included an advisory role for an OU-employed lecturer in learning disability nursing to shadow project management meetings and contribute to outputs. Anderson has been provided with development opportunities including leadership courses and taking on increasing responsibility on the project. Anderson is now a co-principal investigator (alongside Tuffrey-Wijne) on an NIHR grant to improve EOLC planning for PWLD (NIHR202963). Keagan-Bull is a co-applicant and research assistant on the same project and research assistant on the Learning from Deaths Review (LeDeR) Project. Keagan-Bull’s work on the project has set the template for employing and working with researchers with learning disabilities at Kingston University. Other researchers have contacted the team for advice on doing the same in their institutions. Mikulak has been promoted to Senior Research Fellow and given a permanent contract at Manchester Metropolitan University.
Implications for practice
Our main project recommendation is the urgent need for a new strategy for older PWLD and family carers that encompasses commissioning practices (including sharing of best practice, better knowledge and understanding of these groups, more joined-up work between commissioners, LAs and providers around producing good outcomes for older PWLD); professional input (clearly delineated roles and responsibilities including the role of social workers, skills, training); good support to live and age well (including knowledge and understanding of ageing well); and excellent service design (appropriate, sustainable, local and adaptable housing that enables people to age and die in place). We suggest that this strategy could invite a national conversation around older PWLD and develop specific guidance to ensure that housing strategies and other age-related areas address the needs of this group.
Below this umbrella recommendation we have three subsets of recommendations. To improve oversight and lesson learning across the sector:
-
introduce peer learning and critical friends among providers and commissioners; make the good well-known and have an open and supportive peer learning set-up
-
fund self-advocacy groups to support decision-making by people locally
-
have services and commissioners proactively listen to people and their families.
To improve individual support:
-
introduce flexibility with ‘try before you buy’ schemes to ensure that people are not stuck with support that is not well matched to the person
-
match staff (values, interests and skills) to people
-
recruit staff based on being kind, encouraging and knowledgeable and focus on staff retention strategies
-
change staff appraisal processes to become more celebratory and focus on the small things that make a difference.
To ensure people age well:
-
ensure a focus on healthy ageing, with regular health checks with GPs and related follow-up measures, recognition of health inequalities, and the importance of health nutrition and physical activity.
Project resources and outputs
Appendix 4 includes a full list of the project resources and outputs, which include training materials to support researchers, PWLD and family carers to work together and undertake ethnographic research.
Details of the two OpenLearn courses will be shared with LA learning disability teams, learning disability regional nursing networks, university social work departments and family carer groups online.
The BASW resource for social workers will be published with a ‘Research Findings and Implications for Practice’ briefing on the BASW website along with a launch webinar. This resource will also be published on the Paradigm website and disseminated via the Gr8Support Movement to ensure that it reaches support workers.
The ‘Planning Ahead’ cards, project film and podcast will be shared via social media. The cards are being used in the National Lottery-funded Embolden 2 project.
Future research needs
This research has led to the identification of future research needs. Most important are the experiences of older people from diverse ethnic backgrounds, and we highlight the importance of building relationships with organisations with ethnically diverse membership early in the research design process. Other areas include supporting people to age and die ‘in place’; best practice in designing/commissioning services, particularly around housing; the role of social workers in supporting people to plan ahead; access to nature; accessing mainstream support; and wider evaluation of the ‘Planning Ahead’ cards.
Conclusions
Our project focus on exemplary services for older PWLD meant that we were able to find examples of older PWLD with fulfilled lives and identify the conditions enabling this, which include knowing the person well, matching staff and staff consistency, and having proactive engagement between PWLD, families and knowledgeable professionals and services.
This project has identified a lack of consideration of and engagement with PWLD growing older. This is a concerning gap given what is known about the changing health needs of PWLD through ageing including early onset of chronic health issues such as dementia.
It means that this group are largely denied the opportunity to live an active and meaningful life in the community as they grow older, and family carers continue to experience anxiety and fear about a future that remains uncertain and precarious. There is a lack of information about alternative living arrangements, support, options and proactive planning on the part of social care services to enable people to begin to think about where they would like to live and with whom.
Our key recommendation for a new strategy for this group is particularly urgent as contemporary policy has not been developed to take account of PWLD growing older. Given the lack of trust in statutory and private services, this increases the burden on family carers to do the work of planning ahead into their older age, and leaves PWLD without family support even more vulnerable.
Additional information
Acknowledgements
The authors would like to thank the following:
The members of the Public Advisory Group, Jenny Carter, Mary Langan, Mary O’Toole and Frances Steepe, who together acted as a sounding board to the research team and provided advice across all aspects of the work.
The members of the Professional Advisory Group, who together gave their expertise specifically to inform the protocols for the WP1 rapid reviews and the criteria for excellence for the WP2 mapping work that informed the selection of case study sites for WP3. They engaged with the study as ‘critical friends’ for the later WPs from a senior policy, commissioning and practice perspective.
The external members of the independent SSC, chaired by Ruth Northway (Professor of Learning Disability Nursing, University of South Wales), Philippa Russell (Vice-President of Carers UK and family carer), Jill Manthorpe (Professor of Social Work, King’s College London), Elizabeth Tilly (founder of Building Bridges social enterprise), Sally Warren (Managing Director, Paradigm, a development and training organisation) and John Lish (expert by experience), for their support and guidance.
The GM GOLD team of older PWLD and their supporters who regularly included discussion of the study at their meetings and encouraged the researchers to seek their views as issues arose.
The research participants who agreed to take part in WP2, WP3 and WP4 and who variously gave interviews, attended focus groups, completed questionnaires, contributed to co-design work and let us ‘hang out’ with them as they lived their lives at the case study sites.
Jenny Carter, Sam Bennett and Kathy Liddell, who as PWLD or family carers contributed to the ethnography resources developed through engagement funding from the NIHR School for Primary Care Research.
Co-researchers Kerry Martin, Dawn Wiltshire, Shirley Odell and Richard Hughes on the WP3 ethnography and insights substantially increased the value of the work.
Chris Hatton, co-investigator, for his contribution to the overall study design, guidance throughout the study and insights during the development of the final resources and recommendations, providing specific expertise on health and social inequalities experienced by PWLD.
George Julian, freelance knowledge transfer consultant, who constantly challenged the research team to greatly improve the applicability of the research and the quality and utility of the research outputs.
Melanie Chapman, co-investigator at Manchester Metropolitan University, who contributed to the WP3 ethnography data collection and supporting co-researchers to contribute throughout. She convened and led the GM GOLD meetings and contributed text to the corresponding section of the report.
Jillian Pawlyn, Registered Nurse and lecturer in Learning Disabilities Nursing at the OU, who contributed to the WP1 rapid reviews, promoted the survey for WP2 and raised awareness of the study on social media and co-authored the OpenLearn course for health and social care practitioners.
Susan Ledger, a visiting fellow at the OU, who contributed to the WP3 ethnography by providing expertise on learning disability policy, legislation and practice guidance and contributed to data analysis at one site.
Noelle McCormack, visiting research fellow at the OU, who conducted the ethnography at two WP3 case study sites and contributed to the development of the WP3 coding framework.
Arne Mueller, researcher, who conducted the ethnography at one case study site and provided editorial assistance.
Luke Geohegan, Head of Policy and Research at the BASW, who as co-investigator advised on how the research findings might influence practice, leading the development of a practice guide for social workers.
Joanne Jordan, research fellow at the OU, who co-authored the protocol paper, conducted and co-authored the first two WP1 rapid reviews, and contributed to the third rapid review. She contributed analysis of interviews in WP2.
Mary Larkin, co-investigator, who contributed peer reviewed outputs for two WP1 reviews, lead author for an OpenLearn resource for carers in WP5, and set up a forum of best practice for carers linked to the OU’s Carer Research and Knowledge Exchange Network.
Jitka Vseteckova, co-investigator, who took a lead role in the WP1 protocols, contributed to the first two WP1 reviews and co-authored the papers describing that work.
Victoria Byrne, researcher at Manchester Metropolitan University, who contributed to the WP3 ethnography data collection and conducted the WP1 third rapid review at the OU.
Daniel Docherty, co-investigator with lived experience, for his contributions towards the study inception, as a member of the study team and through the GM GOLD meetings.
Lisa Davidson from the self-advocacy organisation My Life My Choice, Oxford, who supported Public Involvement co-investigator Bebbington throughout.
Vanessa Eade, who was instrumental in obtaining the necessary ethics approvals for WP3, and Elizabeth Woolliams, who provided unwavering practical help and administrative support when the study was led from the University of Oxford.
Sally Warren (Managing Director of Paradigm) and Jo Giles (research assistant from Kingston University and also of Paradigm), who together developed the Continuing Professional Development course for social workers. Giles also supported Richard Keagan-Bull in his role as a researcher on WP4.
The OpenLearn team at the OU for supporting the production of two OpenLearn courses, one for family carers and one for practitioners.
Gail Hanrahan and Ben Briggs for forming part of the critical panel for the OpenLearn resources.
Jennifer Bostock, an experienced patient and public involvement representative for NIHR, for delivering training to public contributors on how to participate in research studies effectively as a lay participant.
Grace Barnes for illustrating the ‘Planning Ahead’ cards.
The team at Opening Doors, an organisation run by PWLD, for providing the research team with training in producing Easy Read materials.
Martin Simpson-Scott, Monitoring Programme Manager at NIHR, for providing support and sound advice.
Contributions of authors
Sara Ryan (https://orcid.org/0000-0002-7406-1610) (Professor of Social Care, Co-Principal Investigator) co-led the overall design and provided academic leadership for the study, supervised the WP3 ethnography, contributed to the WP5 OpenLearn resources and led the development of the course for social workers and the film, sat on the SSC, led the writing of the final report including as lead author for Chapters 1, 4, 5, 7 and 9 and gave final approval of the manuscript.
Louise Wallace (https://orcid.org/0000-0003-3770-0580) (Professor of Psychology and Health, Co-Principal Investigator) co-led the overall design and provided academic leadership for the study, chaired the Professional Advisory Group, co-authored the papers describing WP1 rapid reviews 1 and 2, conducted the WP2 work to identify exemplars of good practice, contributed to the WP5 OpenLearn resources, set up and managed the project website, contributed expertise to the other WPs, was a member of the SSC, authored Chapter 3, contributed to other chapters of the final report, and gave final approval of the manuscript.
Elizabeth Tilley (https://orcid.org/0000-0003-4665-394X) Senior Lecturer in Health and Social Care, co-investigator) contributed to the overall study design, led the WP1 rapid reviews, the WP3 ethnography at two case study sites and the WP5 OpenLearn courses, contributed expertise to the other WPs, was lead author of Chapter 2, contributed to other chapters of the final report, particularly Chapters 4, 5 and 7, and gave final approval of the manuscript.
Irene Tuffrey-Wijne (https://orcid.org/0000-0002-7288-9529) (Professor of Intellectual Disability and Palliative Care, co-investigator) contributed to the overall study design, led the WP4 end-of-life planning work, contributed expertise to the other WPs, co-authored Chapter 6, contributed to other chapters of the final report and gave final approval of the manuscript.
Magdalena Mikulak (https://orcid.org/0000-0002-1519-7673) (Senior Research Fellow in Health and Social Care) contributed to the design of the WP3 ethnography, conducted the ethnography at four case study sites, contributed to the WP5 resources, co-authored Chapters 4 and 5, contributed to other chapters of the final report and gave final approval of the manuscript.
Rebecca Anderson (https://orcid.org/0000-0002-7095-8914) (Research Associate in Health and Social Care) contributed to the design of and conducted the WP4 end-of-life planning work, was lead author for Chapter 6, contributed to other chapters of the final report and gave final approval of the manuscript.
Angeli Vaid (https://orcid.org/0009-0007-4102-1165) (Public Involvement Lead, Co-investigator) contributed to the overall study design, led patient and public involvement activities and input throughout the study, chaired the Public Advisory Group and supported other public members, was a co-researcher on the WP3 ethnography, contributed to the WP5 resources, co-authored Chapter 8, contributed to other chapters of the final report and gave final approval of the manuscript.
Pam Bebbington (https://orcid.org/0000-0002-4274-9883) (expert by experience, co-investigator) contributed a lay perspective to the overall study design, and provided expert by experience advice throughout the study, was a co-researcher on the WP3 ethnography, contributed to the WP5 resources, contributed to the final report and gave final approval of the manuscript.
Richard Keagan-Bull (https://orcid.org/0009-0006-0278-8112) (Research Assistant and expert by experience) contributed the perspective of a person with learning disabilities to the design of the WP4 end of life planning work, jointly conducted the WP4 work with support from Anderson, provided expert by experience advice throughout the study, contributed to the final report and gave final approval of the manuscript.
Emmie Morrissey (https://orcid.org/0000-0003-0801-8128) (Research Project Manager, project management) contributed to specific aspects of the study design and managed the conduct of the study with Martin, contributed to the final report and gave final approval of the manuscript.
Angela Martin (https://orcid.org/0000-0001-6196-0409) (Research Operations Manager) project management, contributed to the overall study design and managed the conduct of the study, co-authored Chapter 8 on patient and public involvement, co-ordinated and contributed to the authorship of the final report and gave final approval of the manuscript.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/MTHW2644.
Primary conflicts of interest: Each named author has competed the ICMJE Uniform Disclosure Form for potential conflicts of interest (COI).
Sara Ryan declares membership of the National Institute for Health and Care Research (NIHR) Research for Social Care (RfSC) Funding Committee and that she is a Trustee of LMCP Care Link, was principal investigator of NIHR128616 and is co-principal investigator of NIHR135080 and NIHR131322. Irene Tuffrey-Wijne is principal investigator of the NIHR RfSC-funded project (NIHR202963). Elizabeth Tilley is a co-applicant on NIHR202963. Rebecca Anderson is co-principal investigator on NIHR202963. Louise Wallace was co-investigator of NIHR130995, NIHR Health and Social Care Delivery Research (HSDR) 17/05/30 and is co-principal investigator of NIHR131322 and NIHR205625. Louise Wallace was a member of the NIHR HSDR Commissioned Funding Committee 1 November 2019–30 November 2022, HSDR Remit and Competitiveness commissioned workstream 2015–19, SDO – NHS Evaluations Panel Member 2009–11 and HSDR Funding Committee (Seacole) 2020–22.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to all deidentified data may be granted following review.
Ethics statement
The WP2 scoping and mapping exercise was approved by the Human Research Ethics Committee, the Open University (reference HREC/3636/Wallace, obtained 14 July 2020). The WP3 ethnography was approved by the London – Camden and Kings Cross Research Ethics Committee (reference 12/LO/0062, obtained 1 February 2021). The WP4 stage 1 interviews and focus groups was approved by the Social Care Research Ethics Committee (reference 20/IEC08/0035, obtained 13 November 2020); the stage 2 co-designing resources was approved by the London – Camberwell St Giles Research Ethics Committee (reference 21/LO/0494, obtained 9 August 2021); and the stage 3 evaluation of the resources was approved by the Yorkshire and the Humber – Bradford Leeds Research Ethics Committee (reference 22/YH/0138, obtained 25 July 2022).
Information governance statement
Manchester Metropolitan University is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, Manchester Metropolitan University is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer at (www.mmu.ac.uk/data-protection).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publication
Mikulak M, Ryan S, Tilley E, Ledger S, Davidson L, Bebbigton P, Wiltshire D. Sticky categories and their negative consequences: people with learning disabilities and ‘behaviours that challenge others’. Scand J Disabil Res 2024;26(1):110–23. https://doi.org/10.16993/sjdr.1069
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Public Health England . Learning Disabilities Observatory. People With Learning Disabilities in England 2015: Main Report 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/613182/PWLDIE_2015_main_report_NB090517.pdf (accessed 7 February 2023).
- Cairns D, Tolson D, Brown J, Darbyshire C. The need for future alternatives: an investigation of the experiences and future of older parents caring for offspring with learning disabilities over a prolonged period of time. Br J Learn Disabil 2013;41:73-82. https://doi.org/10.1111/j.1468-3156.2012.00729.x.
- Cairns D, Brown J, Tolson D, Darbyshire C. Caring for a child with learning disabilities over a prolonged period of time: an exploratory survey on the experiences and health of older parent carers living in Scotland. J Appl Res Intellect Disabil 2014;27:471-80. https://doi.org/10.1111/jar.12071.
- Walker C, Walker A. Uncertain Futures: People with Learning Disabilities and Ageing Family Carers. Brighton: Pavilion; 1998.
- Emerson E, Robertson J, Coles B, Hatton C. Research Findings: The Future Need for Social Care Services for Adults with Disabilities in England 2012–2030. London: NIHR School for Social Care Research; 2012.
- Emerson E, Hatton C. People with Learning Disabilities in England. Lancaster: Centre for Disability Research, Lancaster University; 2008.
- World Health Organization . Ageing and Intellectual Disabilities: Improving Longevity and Promoting Healthy Ageing. Summative Report 2000. www.who.int/publications/i/item/WHO-MSD-HPS-MDP-00.3 (accessed 23 February 2023).
- Fesko SL, Hall AC, Quinlan J, Jockell C. Active aging for individuals with intellectual disability: meaningful community participation through employment, retirement, service, and volunteerism. Am J Intellect Dev Disabil 2012;117:497-508. https://doi.org/10.1352/1944-7558-117-6.497.
- Schepens HRMM, Van Puyenbroeck J, Maes B. How to improve the quality of life of elderly people with intellectual disability: a systematic literature review of support strategies. J Appl Res Intellect Disabil 2019;32:483-521. https://doi.org/10.1111/jar.12559.
- Foundation for People with Learning Disabilities . Older People With Learning Disabilities: A Review of the Literature in Residential Services and Family Caregiving 1998. www.learningdisabilities.org.uk/learning-disabilities/publications/older-people-learning-disabilities (accessed 7 February 2023).
- Malli MA, Sams L, Forrester-Jones R, Murphy G, Henwood M. Austerity and the lives of people with learning disabilities. A thematic synthesis of current literature. Disabil Soc 2018;33:1412-35. https://doi.org/10.1080/09687599.2018.1497950.
- Strydom A, Shooshtari S, Lee L, Raykar V, Torr J, Tsiouris J, et al. Dementia in older adults with intellectual disabilities: epidemiology, presentation, and diagnosis. J Policy Pract Intellect Disabil 2010;7:96-110. https://doi.org/10.1111/j.1741-1130.2010.00253.x.
- Grey JM, Totsika V, Hastings RP. Physical and psychological health of family carers co-residing with an adult relative with an intellectual disability. J Appl Res Intellect Disabil 2018;31:191-202. https://doi.org/10.1111/jar.12353.
- NHS Digital . Health and Care of People With Learning Disabilities: 2017–18 2019. https://files.digital.nhs.uk/BA/4F4C1D/health-care-learning-disabilities-1718-sum.pdf (accessed 7 February 2023).
- Bibby R. ‘I hope he goes first’: exploring determinants of engagement in future planning for adults with a learning disability living with ageing parents. What are the issues?. Br J Learn Disabil 2013;41:94-105. https://doi.org/10.1111/j.1468-3156.2012.00727.x.
- Dillenburger K, McKerr L. ‘How long are we able to go on?’ Issues faced by older family caregivers of adults with disabilities. Br J Learn Disabil 2011;39:29-38. https://doi.org/10.1111/j.1468-3156.2010.00613.x.
- Tuffrey-Wijne I, Wicki M, Heslop P, McCarron M, Todd S, Oliver D, et al. Developing research priorities for palliative care of people with intellectual disabilities in Europe: a consultation process using nominal group technique. BMC Palliat Care 2016;15. https://doi.org/10.1186/s12904-016-0108-5.
- Walmsley J, Jarrett S. Intellectual Disability in the Twentieth Century: Transnational Perspectives on People, Policy and Practice. Bristol: Policy Press; 2019.
- World Health Organization . The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostics Guidelines 1992. www.who.int/publications/i/item/9241544228 (accessed 23 February 2023).
- Thomas GM. Dis-mantling stigma: parenting disabled children in an age of ‘neoliberal-ableism’. Sociol Rev 2021;69:451-67. https://doi.org/10.1177/0038026120963481.
- Cluley V, Pilnick A, Fyson R. Talking about learning disability: discursive acts in managing an ideological dilemma. SSM Qual Res Health 2022;2. https://doi.org/10.1016/j.ssmqr.2022.100088.
- Cluley V. From ‘learning disability to intellectual disability’: perceptions of the increasing use of the term ‘intellectual disability’ in learning disability policy, research and practice. Br J Learn Disabil 2018;46:24-32. https://doi.org/10.1111/bld.12209.
- Mansell J, Knapp M, Beadle-Brown J, Beecham J. Deinstitutionalisation and Community Living: Outcomes and Costs: Report of a European Study. Volume 2: Main Report. Canterbury: University of Kent; 2007.
- Royal College of Psychiatrists . Challenging Behaviour: A Unified Approach – Clinical and Service Guidelines for Supporting People With Learning Disabilities Who Are at Risk of Receiving Abusive or Restrictive Practices 2007. www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/college-reports/college-report-cr144.pdf?sfvrsn=73e437e8_2 (accessed 23 February 2023).
- Norfolk Safeguarding Adults Board . Guidance for Care Homes: Moving Away from a ‘Medication-First’ Approach to Challenging Behaviour 2020. www.norfolksafeguardingadultsboard.info/document/697/Guidance-to-Care-Providers-Behaviours-That-Challenge-May20-v3.pdf? (accessed 23 February 2023).
- Haydon-Laurelut M, Nunkoosing K. Causing trouble: the language of learning disability and challenging behaviour. Tizard Learn Disabil Rev 2016;21:144-9. https://doi.org/10.1108/TLDR-11-2014-0038.
- Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Independent Inquiry into Access to Healthcare for People with Learning Disabilities; 2008.
- Heslop P, Blair P, Fleming P, Hoghton M, Marriott A, Russ L. Confidential Inquiry into Premature Deaths of People With Learning Disabilities (CIPOLD). Final Report 2013. www.bristol.ac.uk/media-library/sites/cipold/migrated/documents/fullfinalreport.pdf (accessed 23 February 2023).
- O’Dwyer C, McCallion P, Henman M, McCarron M, O’Leary E, Burke E, et al. Prevalence and patterns of antipsychotic use and their associations with mental health and problem behaviours among older adults with intellectual disabilities. J Appl Res Intellect Disabil 2019;32:981-93. https://doi.org/10.1111/jar.12591.
- Davys D, Mitchell D, Haigh C. Futures planning: adult sibling perspectives. Br J Learn Disabil 2015;43:219-26. https://doi.org/10.1111/bld.12099.
- Davys D, Haigh C. Older parents of people who have a learning disability: perceptions of future accommodation needs. Br J Learn Disabil 2008;36:66-72. https://doi.org/10.1111/j.1468-3156.2007.00447.x.
- NHS Digital . Adult Social Care Activity and Finance Report, England, 2021–22 2022. https://digital.nhs.uk/data-and-information/publications/statistical/adult-social-care-activity-and-finance-report/2021-22# (accessed 7 March 2023).
- n.d. www.gov.uk/government/publications/building-the-right-support-for-people-with-a-learning-disability-and-autistic-people/building-the-right-support-action-plan (accessed 18 December 2023).
- Mahon A, Tilley E, Randhawa G, Pappas Y, Vseteckova J. Ageing carers and intellectual disability: a scoping review. Qual Ageing Older Adults 2019;20:162-78. https://doi.org/10.1108/QAOA-11-2018-0057.
- Walker R, Hutchinson C. Planning for the future among older parents of adult offspring with intellectual disability living at home and in the community: a systematic review of qualitative studies. J Intellect Dev Disabil 2018;43:453-62. https://doi.org/10.3109/13668250.2017.1310823.
- Gorfin L, McGlaughlin A. Planning for the future with adults with a learning disability living with older carers. Hous Care Support 2004;7:20-4. https://doi.org/10.1108/14608790200400020.
- National Institute for Health and Care Excellence . NICE Full Guideline: Learning Disabilities and Behaviour That Challenges: Service Design and Delivery [NG93] 2018. www.nice.org.uk/guidance/ng93/resources/learning-disabilities-and-behaviour-that-challenges-service-design-and-delivery-pdf-1837753480645 (accessed 7 February 2023).
- National Institute for Health and Care Excellence . NG11: Challenging Behaviour and Learning Disabilities: Prevention and Interventions for People With Learning Disabilities Whose Behaviour Challenges 2015. www.nice.org.uk/guidance/ng11 (accessed 7 February 2023).
- Griffith GM, Hastings RP. ‘He’s hard work, but he’s worth it’. The experience of caregivers of individuals with intellectual disabilities and challenging behaviour: a meta-synthesis of qualitative research. J Appl Res Intellect Disabil 2014;27:401-19. https://doi.org/10.1111/jar.12073.
- Hatton C, Emerson E, Kirby S, Kotwal H, Baines S, Hutchinson C, et al. Majority and minority ethnic family carers of adults with intellectual disabilities: perceptions of challenging behaviour and family impact. J Appl Res Intellect Disabil 2010;23:63-74. https://doi.org/10.1111/j.1468-3148.2009.00544.x.
- Tuffrey-Wijne I, Bernal J, Hubert J, Butler G, Hollins S. People with learning disabilities who have cancer: an ethnographic study. Br J Gen Pract 2009;59:503-9. https://doi.org/10.3399/bjgp09X453413.
- Watchman K. Practitioner-raised issues and end-of-life care for adults with down syndrome and dementia. J Policy Pract Intellect Disabil 2005;2:156-62. https://doi.org/10.1111/j.1741-1130.2005.00026.x.
- Tuffrey-Wijne I, Giatras N, Butler G, Cresswell A, Manners P, Bernal J. Developing guidelines for disclosure or non-disclosure of bad news around life-limiting illness and death to people with intellectual disabilities. J Appl Res Intellect Disabil 2013;26:231-42. https://doi.org/10.1111/jar.12026.
- Hastings RP, Allen D, Baker P, Gore NJ, Hughes JC, McGill P, et al. A conceptual framework for understanding why challenging behaviours occur in people with developmental disabilities. J Posit Behav Interv 2013;3:5-13.
- Griffith GM, Hutchinson L, Hastings RP. ‘I’m not a patient, I’m a person’: the experiences of individuals with intellectual disabilities and challenging behavior – a thematic synthesis of qualitative studies. Clin Psychol: Sci Pract 2013;20:469-88. https://doi.org/10.1111/cpsp.12053.
- Innes A, McCabe L, Watchman K. Caring for older people with an intellectual disability: a systematic review. Maturitas 2012;72:286-95. https://doi.org/10.1016/j.maturitas.2012.05.008.
- Brennan D, McCausland D, O’Donovan MA, Eustace-Cook J, McCallion P, McCarron M. Approaches to and outcomes of future planning for family carers of adults with an intellectual disability: a systematic review. J Appl Res Intellect Disabil 2020;33:1221-33. https://doi.org/10.1111/jar.12742.
- Lee CE, Burke MM. Future planning among families of individuals with intellectual and developmental disabilities: a systematic review. J Policy Pract Intellect Disabil 2020;17:94-107. https://doi.org/10.1111/jppi.12324.
- Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141-6. https://doi.org/10.1097/XEB.0000000000000050.
- Stevens A, Garritty C, Hersi M, Moher D. Developing PRISMA-RR, a Reporting Guideline for Rapid Reviews of Primary Studies (Protocol). 2018.
- Langlois EV, Straus SE, Antony J, King VJ, Tricco AC. Using rapid reviews to strengthen health policy and systems and progress towards universal health coverage. BMJ Glob Health 2019;4. https://doi.org/10.1136/bmjgh-2018-001178.
- Plüddemann A, Aronson JK, Onakpoya I, Heneghan C, Mahtani KR. Redefining rapid reviews: a flexible framework for restricted systematic reviews. BMJ Evid Based Med 2018;23:201-3. https://doi.org/10.1136/bmjebm-2018-110990.
- Tricco AC, Lillie E, Wasifa Z, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467-73. https://doi.org/10.7326/m18-0850.
- Pandor A, Kaltenthaler E, Martyn-St James M, Wong R, Cooper K, Dimairo M, et al. Delphi consensus reached to produce a decision tool for SelecTing Approaches for Rapid Reviews (STARR). J Clin Epidemiol 2019;114:22-9. https://doi.org/10.1016/j.jclinepi.2019.06.005.
- Tricco AC, Langlois EV, Straus SE. Rapid Reviews to Strengthen Health Policy and Systems: A Practical Guide. Geneva: World Health Organization; 2017.
- Department of Health and Social Care . Valuing People: A New Strategy for Learning Disability for the 21st Century: A White Paper 2001. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/250877/5086.pdf (accessed 23 February 2023).
- Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. JBI Manual for Evidence Synthesis. Adelaide, SA: JBI; 2020.
- National Institute for Health and Care Excellence . Challenging Behaviour and Learning Disabilities: Prevention and Interventions for People With Learning Disabilities Whose Behaviour Challenges n.d. www.nice.org.uk/guidance/ng11 (accessed 18 December 2023).
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews 2006. www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf (accessed 7 February 2023).
- Ryan R. Cochrane Consumers and Communication Review Group . Cochrane Consumers and Communication Review Group: Data Synthesis and Analysis 2013. https://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/Analysis.pdf (accessed 7 February 2023).
- Slevin E, Taggart L, McConkey R, Cousins W, Truesdale-Kennedy M, Dowling L. A Rapid Review of Literature Relating to Support for People with Intellectual Disabilities and Their Family Carers When the Person Has Behaviours that Challenge and/or Mental Health Problems; or They Are Advancing in Age. Coleraine: Ulster University; 2011.
- Forrester-Jones R. Confronting a Looming Crisis. People with Learning Disabilities or Autism and Their Carers Getting Older. Bath: University of Bath; 2019.
- Perry J, Allen DG, Pimm C, Meek A, Lowe K, Groves S, et al. Adults with intellectual disabilities and challenging behaviour: the costs and outcomes of in- and out-of-area placements. J Intellect Disabil Res 2013;57:139-52. https://doi.org/10.1111/j.1365-2788.2012.01558.x.
- Leaning B, Adderley H. From long-stay hospitals to community care: reconstructing the narratives of people with learning disabilities. Br J Learn Disabil 2016;44:167-71. https://doi.org/10.1111/bld.12139.
- Hubert J, Hollins S. A study of post-institutionalized men with severe intellectual disabilities and challenging behavior. J Policy Pract Intellect Disabil 2010;7:189-95. https://doi.org/10.1111/j.1741-1130.2010.00264.x.
- Black LA, McKendrick V. Careful Plans Report 2010.
- Grey JM, Griffith GM, Totsika V, Hastings RP. Families’ experiences of seeking out-of-home accommodation for their adult child with an intellectual disability. J Policy Pract Intellect Disabil 2015;12:47-5. https://doi.org/10.1111/jppi.12106.
- Campbell M. The importance of good quality services for people with complex health needs. Br J Learn Disabil 2008;36:32-7. https://doi.org/10.1111/j.1468-3156.2007.00449.x.
- Care Quality Commission . Home for Good: Successful Community Support for People With a Learning Disability, a Mental Health Need and Autistic People 2021. www.cqc.org.uk/publications/themed-work/home-good-successful-community-support-people-learning-disability-mental (accessed 22 February 2023).
- Hatzidimitriadou E, Milne A. Planning ahead: meeting the needs of older people with intellectual disabilities in the United Kingdom. Dementia 2005;4:341-59. https://doi.org/10.1177/1471301205055027.
- Jenkins R. Nurses’ views about services for older people with learning disabilities. Nurs Older People 2009;21:23-7. https://doi.org/10.7748/nop2009.04.21.3.23.c7013.
- Savarimuthu D. The potential role of nurses in leading positive behaviour support. Br J Nurs 2020;29:414-8. https://doi.org/10.12968/bjon.2020.29.7.414.
- Welch ML, Hodgson JL, Didericksen KW, Lamson AL, Forbes TH. Family-centered primary care for older adults with cognitive impairment. Contemp Fam Ther 2022;44:67-8. https://doi.org/10.1007/s10591-021-09617-2.
- Mahoney WJ, Ceballos J, Amir N. Occupational therapy practitioners’ perceptions about older adults with developmental disabilities in traditional health care settings. Am J Occup Ther 2019;73:7303345010p1-6. https://doi.org/10.5014/ajot.2019.029835.
- Tremblay A, Morin D. Assessment of an expert committee as a referral process within health and social services. J Policy Pract Intellect Disabil 2015;12:162-71. https://doi.org/10.1111/jppi.12092.
- Levy JM, Botuck S, Damiani MR, Levy PH, Dern TA, Freeman SE. Medical conditions and healthcare utilization among adults with intellectual disabilities living in group Homes in New York City. J Policy Pract Intellect Disabil 2006;3:195-202. https://doi.org/10.1111/j.1741-1130.2006.00079.x.
- Carers Trust. Voluntary Community and Social Enterprise (VCSE) Health and Wellbeing Alliance (HW Alliance) . No Longer Able to Care: Supporting Older Carers and Ageing Parent Carers to Plan for a Future When They Are Less Able or Unable to Care 2020. https://carers.org/downloads/resources-pdfs/no-longer-able-to-care/no-longer-able-to-care.pdf (accessed 7 February 2023).
- Pryce L, Tweed A, Hilton A, Priest HM. Tolerating uncertainty: perceptions of the future for ageing parent carers and their adult children with intellectual disabilities. J Appl Res Intellect Disabil 2017;30:84-96. https://doi.org/10.1111/jar.12221.
- Taggart L, Hanna-Trainor L. Supporting Older Adults with a Learning Disability and Their Ageing Family Carers: A Family and Community Support Model. Public Health Agency, Northern Ireland; 2017.
- NHS England . National Plan – Building the Right Support 2015. www.england.nhs.uk/learning-disabilities/natplan/ (accessed 7 May 2019).
- NHS England . Building the Right Home: Guidance for Commissioners of Health and Care Services for Children, Young People and Adults With Learning Disabilities and Or Autism Who Display Behaviour That Challenges 2016. www.england.nhs.uk/learningdisabilities/wp-content/uploads/sites/34/2015/11/building-right-home-guidance-housing.pdf (accessed 23 February 2023).
- NHS England . Transforming Care. Model Service Specifications: Supporting Implementation of the Service Model 2017. www.england.nhs.uk/wp-content/uploads/2017/02/model-service-spec-2017.pdf (accessed 7 February 2023).
- Alftberg A, Johansson M, Ahlström G. Ambivalence among staff regarding ageing with intellectual disabilities: experiences and reflections. J Intellect Disabil 2021;25:192-209. https://doi.org/10.1177/1744629519874997.
- Northway R, Jenkins R, Holland-Hart D. Training of residential social care staff to meet the needs of older people with intellectual disabilities who develop age-related health problems: an exploratory study. J Appl Res Intellect Disabil 2017;30:911-21. https://doi.org/10.1111/jar.12283.
- de Leeuw MJ, Oppewal A, Elbers RG, Knulst MWEJ, van Maurik MC, van Bruggen MC, et al. Healthy Ageing and Intellectual Disability study: summary of findings and the protocol for the 10-year follow-up study. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-053499.
- McCausland D, McCallion P, Cleary E, McCarron M. Social connections for older people with intellectual disability in Ireland: results from wave one of IDS-TILDA. J Appl Res Intellect Disabil 2016;29:71-82. https://doi.org/10.1111/jar.12159.
- Bigby C. A five-country comparative review of accommodation support policies for older people with intellectual disability. J Policy Pract Intellect Disabil 2010;7:3-15. https://doi.org/10.1111/j.1741-1130.2010.00242.x.
- Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019993.
- Pryjmachuk S, Elvey R, Kirk S, Kendal S, Bower P, Catchpole R. Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study. Health Soc Care Deliv Res 2014;2. https://doi.org/10.3310/hsdr02180.
- Combs R, Turner L, Whittle S. ‘Gender Identity Services in England’: The Mapping Project Report 2008.
- Barnes D, Devanney C, Parker E, Wistow R. A Profile of Children’s Health Services, Child and Adolescent Mental Health Services and Maternity Services in England 2007/8. Technical Report. Durham: School of Applied Sciences, University of Durham; 2009.
- Moss A, Miller R, Battye F, Higgins B, Smith K, Mason P, et al. Evaluation of Building the Right Support: Phase 2 Case Study Findings Report 2018. www.strategyunitwm.nhs.uk/sites/default/files/2019-01/4%20Case%20Study%20Report.pdf (accessed 7 February 2023).
- Battye F, Moss A, Miller R, Higgins B, Smith K. Evaluation of Building the Right Support. Survey Results, December 2017. Final Report 2017.
- Wallace LM, Ryan S, Vaid A. Planning Ahead for Older People with Learning Disabilities. Croydon: Care Management Matters; 2020.
- NHS England . What Is Personalised Care? n.d. www.england.nhs.uk/personalisedcare/what-is-personalised-care/ (accessed 7 February 2023).
- National Institute for Health and Care Excellence . Care and Support of People Growing Older With Learning Disabilities (NG96) 2018. www.nice.org.uk/guidance/ng96/resources/care-and-support-of-people-growing-older-with-learning-disabilities-pdf-1837758519493 (accessed 7 February 2023).
- Bissell L, Phillips N, Kroese BS. The experience of a man with severe challenging behaviour following resettlement from hospital: a single case design. Br J Learn Disabil 2005;33:166-73. https://doi.org/10.1111/j.1354-4187.2005.00302.x.
- Bigby C, Beadle-Brown J. Culture in better group homes for people with intellectual disability at severe levels. Intellect Dev Disabil 2016;54:316-31. https://doi.org/10.1352/1934-9556-54.5.316.
- NHS England . NHS Long Term Plan, Chapter 3: Further Progress on Care Quality and Outcomes 2019. www.longtermplan.nhs.uk/online-version/chapter-3-further-progress-on-care-quality-and-outcomes/ (accessed 7 February 2023).
- Watchman K. Critical issues for service planners and providers of care for people with Down’s syndrome and dementia. Br J Learn Disabil 2003;31:81-4. https://doi.org/10.1046/j.1468-3156.2003.00228.x.
- Skills for Health, Health Education England and NHS England . Core Capabilities Framework for Supporting People With a Learning Disability 2019. www.skillsforhealth.org.uk/wp-content/uploads/2020/11/Learning-Disability-Framework-Oct-2019.pdf (accessed 7 February 2023).
- Care Quality Commission . CQC Updates Guidance on the Regulation of Services for Autistic People and Or People With a Learning Disability 2020. www.cqc.org.uk/news/releases/cqc-updates-guidance-regulation-services-autistic-people-andor-people-learning (accessed 7 February 2023).
- McConkey R, Collins S. The role of support staff in promoting the social inclusion of persons with an intellectual disability. J Intellect Disabil Res 2010;54:691-700. https://doi.org/10.1111/j.1365-2788.2010.01295.x.
- Perry J, Felce D, Allen D, Meek A. Resettlement outcomes for people with severe challenging behaviour moving from institutional to community living. J Appl Res Intellect Disabil 2011;24:1-17. https://doi.org/10.1111/j.1468-3148.2010.00567.x.
- Bigby C, Knox M, Beadle-Brown J, Bould E. Identifying good group homes: qualitative indicators using a quality of life framework. Intellect Dev Disabil 2014;52:348-66. https://doi.org/10.1352/1934-9556-52.5.348.
- Harvey K. Trauma-Informed Behavioral Interventions: What Works and What Doesn’t. Silver Spring, MD: American Association on Intellectual and Developmental Disabilities; 2012.
- Hammersley M. problems and prospects. Ethnogr Educ 2006;1:3-14. https://doi.org/10.1080/17457820500512697.
- Kaley A, Hatton C, Milligan C. More than words: the use of video in ethnographic research with people with intellectual disabilities. Qual Health Res 2019;29:931-43. https://doi.org/10.1177/1049732318811704.
- Devi N, Prodinger B, Pennycott A, Sooben R, Bickenbach J. Investigating supported decision‐making for persons with mild to moderate intellectual disability using institutional ethnography. J Policy Pract Intellect Disabil 2020;17:143-56. https://doi.org/10.1111/jppi.12314.
- Murray V. Co-producing knowledge: reflections on research on the residential geographies of learning disability. Area 2019;51:423-32. https://doi.org/10.1111/area.12491.
- Ryan S, Mikulak M, Hatton C. Whose uncertainty? Learning disability research in a time of COVID-19. Int J Soc Res Methodol 2023;26:535-47. https://doi.org/10.1080/13645579.2023.2173425.
- Kiernan C. Participation in research by people with learning disability: origins and issues. Br J Learn Disabil 1999;27:43-7. https://doi.org/10.1111/j.1468-3156.1999.tb00084.x.
- Macpherson H, Hart A, Heaver B. Impacts between academic researchers and community partners: some critical reflections on impact agendas in a ‘visual arts for resilience’ research project. ACME: Int E-J Crit Geogr 2014;13:27-32.
- Aldridge J. Picture this: the use of participatory photographic research methods with people with learning disabilities. Disabil Soc 2007;22:1-17. https://doi.org/10.1080/09687590601056006.
- Mikulak M, Ryan S, Bebbington P, Bennett S, Carter J, Davidson L, et al. ‘Ethno…graphy?!? I can’t even say it': Co-designing training for ethnographic research for people with learning disabilities and carers. Br J Learn Disabil 2022;50:52-60. https://doi.org/10.1111/bld.12424.
- Boahen G. Researching the Mental Capacity Act 2005: reflections on governance, field relationships, and ethics with an adult who did not consent. Ethics Soc Welf 2015;9:375-89. https://doi.org/10.1080/17496535.2015.1072571.
- Bubb S. Winterbourne View – Time for Change: Transforming the Commissioning of Services for People With Learning Disabilities and Or Autism 2014. www.england.nhs.uk/wp-content/uploads/2014/11/transforming-commissioning-services.pdf (accessed 23 February 2023).
- Department of Health and Social Care . DH Winterbourne View Review. Concordat: Programme of Action 2012. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213217/Concordat.pdf (accessed 23 February 2023).
- Great Britain . Mental Capacity Act 2005.
- Great Britain . Mental Health Act 1983: Code of Practice 2015.
- Ministry of Justice . Mental Health Act 2005: Deprivation of Liberty Safeguards. Code of Practice to Supplement the Main Mental Capacity Act 2005 Code of Practice 2008. www.cqc.org.uk/sites/default/files/Deprivation%20of%20liberty%20safeguards%20code%20of%20practice.pdf (accessed 7 February 2023).
- Equality and Human Rights Commission . Human Rights Framework for Restraint: Principles for the Lawful Use of Physical, Chemical, Mechanical and Coercive Restrictive Interventions 2019. www.equalityhumanrights.com/sites/default/files/human-rights-framework-restraint.pdf (accessed 7 March 2023).
- Pallisera M, Fullana J, Puyaltó C, Vilà M. Changes and challenges in the transition to adulthood: views and experiences of young people with learning disabilities and their families. Eur J Spec Needs Educ 2016;31:391-406. https://doi.org/10.1080/08856257.2016.1163014.
- Salt E, Melville C, Jahoda A. Transitioning to adulthood with a mild intellectual disability – young people’s experiences, expectations and aspirations. J Appl Res Intellect Disabil 2019;32:901-12. https://doi.org/10.1111/jar.12582.
- Power A, Bartlett R. Self-building safe havens in a post-service landscape: how adults with learning disabilities are reclaiming the welcoming communities agenda. Soc Cult Geogr 2018;19:336-56. https://doi.org/10.1080/14649365.2015.1031686.
- Needham C. Personalization: from day centres to community hubs?. Crit Soc Policy 2014;34:90-108. https://doi.org/10.1177/0261018313483492.
- Burke M, Arnold C, Owen A. Identifying the correlates and barriers of future planning among parents of individuals with intellectual and developmental disabilities. Intellect Dev Disabil 2018;56:90-100. https://doi.org/10.1352/1934-9556-56.2.90.
- Point of Care Foundation . EBCD: Experience-Based Co-Design Toolkit 2020. www.pointofcarefoundation.org.uk/resource/experience-based-co-design-ebcd-toolkit/ (accessed 7 February 2023).
- Llewellyn P. Supporting people with intellectual disabilities to take part in focus groups: reflections on a research project. Disabil Soc 2009;24:845-56. https://doi.org/10.1080/09687590903283431.
- Cambridge P, McCarthy M. User focus groups and Best Value in services for people with learning disabilities. Health Soc Care Community 2001;9:476-89. https://doi.org/10.1046/j.0966-0410.2001.00328.x.
- Ritchie J, Spencer L, O’Connor W. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Greenhalgh T, Jackson C, Shaw S, Janamian T. Achieving research impact through co-creation in community-based health services: literature review and case study. Milbank Q 2016;94:392-429. https://doi.org/10.1111/1468-0009.12197.
- Paradigm . REACH Support for Living n.d. https://paradigm-uk.org/what-we-do/reach-support-for-living/ (accessed 15 February 2023).
- National Institute for Health and Care Research . Guidance on Co-Producing a Research Project 2021. www.learningforinvolvement.org.uk/?opportunity=nihr-guidance-on-co-producing-a-research-project (accessed 15 February 2023).
- Department of Health and Social Care . Caring for Our Future: Reforming Care and Support 2012. www.gov.uk/government/publications/caring-for-our-future-reforming-care-and-support (accessed 27 February 2023).
- Anderson RJ, Keagan-Bull R, Giles J, Tuffrey-Wijne I. ‘My name on the door by the Professor’s name’: the process of recruiting a researcher with a learning disability at a UK university. Br J Learn Disabil 2023;51:460-8. https://doi.org/10.1111/bld.12477.
- Sense . Decisions to Make, Steps to Take, a Guide to Planning Long-Term Care and Support to Disabled Families and Their Carers. A Sense Toolkit 2018.
- The Housing and Support Partnership . Planning and Commissioning Housing for People With Learning Disabilities. A Toolkit for Local Authorities 2011. www.housingandsupport.co.uk/publications-downloads/toolkit-local-authorities.pdf.
- Towers C. Thinking Ahead: A Planning Guide for Families. London: Foundation for People with Learning Disabilities; 2015.
Appendix 1 Characteristics of included evidence for rapid reviews 1, 2 and 3
Rapid review 1: characteristics of included evidence
| Authors/date of publication | Title | Type of evidence | Stated aim/purpose | How evidence assembled | Population | Definition or examples of ‘behaviour that challenges others’ | Country | Main findings |
|---|---|---|---|---|---|---|---|---|
| 1. Bissell et al.,97 2005 | The experience of a man with severe challenging behaviour following resettlement from hospital: a single case design | Peer-reviewed journal article | To investigate the effectiveness of a behavioural intervention in the management of problem behaviours | Single client case study, based on clinical psychology caseload notes | Single client (55-year-old male) with severe learning disabilities. Other conditions: epilepsy | Examples of behaviour provided: shouting, screaming, destruction of environment, smearing faeces, physical aggression towards residents and staff | England | Significant decrease in challenging behaviour after implementation of guidelines. Effective dental treatment produced further reduction in challenging behaviour |
| 2. Forrester-Jones,62 2019 | Confronting a looming crisis. People with learning disabilities or autism and their carers getting older | Report | To explore the experiences of older family carers as they continue to care for their older adult relatives with learning disabilities | Research: qualitative; data collection = interviews with older family carers; data analysis = interpretative phenomenological analysis (IPA) | Carers (aged ≥ 50 years) of adults (n = 16; average age = 45 years; 50% over age of 50; gender not stated, but mixed gender) with mild to severe learning disabilities. Other conditions: Smith–Magenis syndrome; Down syndrome (n = 5); cerebral palsy (n = 2); autism (n = 7). Two participants described as displaying ‘behaviours that challenge others‘ | None provided | England | Family carers’ avoidance of future planning unintentionally thwarts opportunities for older people with learning disabilities to learn about options for transition. Issue of choice by individuals not straightforward in all situations, with possibility of conflict with family carers. Reduced effectiveness of social work support due to frequent staff turnover. Early and proactive professional involvement in supporting a ‘whole family’ approach to transition planning is required. Lack of/delays to needs assessment of people with learning disabilities, and lack of functional assessments or positive behaviour support plans. People’s transition ‘stifled’ because of carers’ aversion to sending adult family members to accommodation they considered unsuitable |
| 3. Hubert and Hollins,65 2010 | A study of post-institutionalised men with severe intellectual disabilities and challenging behaviour | Peer-reviewed journal article | To examine the after-effects of moving from institutional care to small group homes among adults with challenging behaviours | Research: ethnography undertaken longitudinally (6 years) | Men (n = 20; age range 29–46 years) resident in institutional hospital, with profound to severe learning disabilities. Other conditions: majority with autistic spectrum disorder and ‘concomitant’ (p. 190) mental health problems | Examples of behaviour provided: physical aggression, self-injury, taking off clothes, ripping up clothes, spreading urine and faeces, eating unsuitable objects | Not stated | Participants’ lives improved materially after taking up residence in new homes, but they continued to experience social exclusion and denial of individual identity and autonomy. Few fundamental changes in professional and social attitudes towards them |
| 4. Leaning and Adderley,64 2015 | From long-stay hospitals to community care: reconstructing the narratives of people with learning disabilities | Peer-reviewed journal article | To describe the journey taken by a man from institutional care to community living | Single client case study, based on clinical psychology caseload notes | Single client (62-year-old male) with severe and profound learning disabilities. Other conditions: autistic spectrum disorder | Examples of behaviour provided: aggression, self-injury, biting, hitting, shouting | England | Over extended period of time, the man was resettled in community. Involved: clinical psychologist’s intense support and advocacy; wider psychology team support, including development and implementation of PBS plan; training for home care staff team and development of transition and subsequent care plan; and involvement of the man’s family and the man himself, with appropriate support. Process complicated by need to adhere to/pass numerous legal requirements |
| 5. Perry et al.,104 2011 | Resettlement outcomes for people with severe challenging behaviour moving from institutional to community living | Peer-reviewed journal article | To evaluate the quality-of-life consequences of resettlement from a learning disability hospital to new purpose-built accommodation | Research: undertaken longitudinally (12–18 months); data collected on quality of care and lifestyle indictors | Adults (n = 18; 13 male/6 female; age range 36–67 years; mean 47 years) with learning disabilities, ranging from lower to upper scores on the Adaptive Behaviour Scale (Nihira et al., 1993). Other conditions: epilepsy (n = 4); autism (n = 3); mental ill-health (n = 7) | Participants classified using the Aberrant Behaviour Checklist (Aman and Singh, 1986): irritability, lethargy, stereotypy, hyperactivity, inappropriate speech | Wales | Quality-of-care and quality-of-life outcomes were generally equivalent or superior to previous hospital levels. Improvement over time was demonstrated in respect of greater family contact and reduction in staff-reported challenging behaviour |
| 6. Perry et al.,63 2013 | Adults with intellectual disabilities and challenging behaviour: the costs and outcomes of in- and out-of-area placements | Peer-reviewed journal article | To compare the costs and outcomes of in- and out-of-area placements for people with learning disabilities and challenging behaviour | Costs, quality-of-care and quality-of-life outcomes | Adults (n = 76; 48 male/28 female; mean age of men 46 years/mean age of women 35 years) with learning disabilities, ranging from lower to upper scores on the ABS (Nihira et al., 1993). Other conditions: mental illness (28.9% in-area and 15.8% out-of-area); autistic spectrum disorder (47.4% in-area and 44.7% out-of-area) |
None provided | Wales | There was a mixed pattern of quality-of-care and quality-of-outcome advantages between the two types of setting. In-area placements had a greater number of advantages than out-of-area placements. Out-of-area placements had lower total costs, accommodation costs and daytime activity costs |
| 7. Sense,137 2018 | Decisions to make, steps to take. A guide to planning long-term care and support for disabled adults and their families. A Sense Toolkit | Resource – sets out information, guidance, and tools | To provide information for people with learning disabilities and their families to start making plans for the future | Non-research; no information provided | People with learning disabilities; family carers of people with learning disabilities | None provided | Not stated: Sense is a UK-based organisation | Comprehensive, easy-to-read guide, setting out main options available, legal rights possessed, and key decisions that need to be made regarding making plans for the future care for people with learning disabilities |
| 8. Slevin et al.,61 2011 | A rapid review of the literature relating to support for people with intellectual disabilities and their family carers when the person has behaviours that challenge and/or mental health problems; or they are advancing in age | Report | (1) What services and support do people with learning disabilities who display behaviours that challenge and their caregivers require to meet their needs? (2) What services and support do older people with learning disabilities and their caregivers require to meet their needs? | Rapid review, using a framework adapted from the NHS Centre for Reviews and Dissemination (2009) and the Rapid Review Methodology (NHS, Wales 2006) | People with learning disabilities who display behaviours that challenge; carers of people with learning disabilities who display behaviours that challenge. Older people with learning disabilities; carers of older people with learning disabilities. Other conditions: no information provided but ‘behaviours that challenge others’ is ‘inclusive of mental health problems’ (p. 9) | Working definition of ‘behaviours that challenge others’ provided (p. 9):… severely challenging behaviour refers to culturally abnormal behaviour(s) of such an intensity, frequency or duration that the physical safety of the person or others is likely to be placed in serious jeopardy, or behaviour that is likely to seriously limit use of, or result in the person being denied access to ordinary community facilities Emerson, 1995, p. 44 | Only studies published in English included | People whose behaviour challenges
Support should be based on the use of resources to maintain the person in their own home, if this is their wish. Identified interventions and services (e.g. PBS, use of community specialist teams, short breaks, teaching and supporting caregivers) were found to be successful in doing so. Appropriate day opportunities are also essential, but have not been adequately researched, as is family support to allow people with learning disabilities and behaviours that challenge and their family to lead fulfilling lives. Medication highly used, but behavioural management should be pursued as appropriate. Interventions most likely to be effective when delivered via a family support and education approach, in partnership with formal carers. Active support appears a promising approach. Specialist community teams are a highly effective service. Specialist assessment and treatment units can provide a useful service, but admission should be for a short period, with aim of return to the community. To this end, a model that provides combined specialist support services is recommended. Evidence suggests limited use of full range of mental health services, suggesting deficits in terms of their accessibility and value for people with learning disabilities and behaviours that challenge |
| Older people with learning disabilities Most older people with learning disabilities and behaviours that challenge wish to continue to live in their family home, and ageing family carers want to continue caring. However, lack of future planning persists. Ageing people with learning disability may face same range of health-related issues as others earlier in their lives. In addition, there are higher rates of some conditions (e.g. dementia). Medications that can help are seldom offered. Appropriate health screening is needed, but scarce evidence that this happens, or that detected health problems are properly investigated and treated. Positive mental health is promoted by such health-improving behaviours, continuing to remain active and having a meaningful and valued life. Relevant training is required for front-line staff to develop skills to provide appropriate care, both in supported living arrangements and in partnership with family carers. Evidence suggests that facilities geared towards the needs of older people with learning disabilities are at best scarce and at worst non-existent. Nursing or residential placement should not be the ‘go-to’ option; a range of intermediate care facilities should be used as appropriate to promote opportunity to return to their home. It should not be assumed that because a person is a particular age that they may not be able to return to their normal home or residence | ||||||||
| 9. The Housing and Support Partnership,138 2011 | Planning and commissioning housing for people with learning disabilities. A toolkit for local authorities | Report | Resource (‘toolkit’) | Non-research; no information provided | LAs responsible for the planning/commissioning of housing for people with learning disabilities | None provided | All references made in respect of England, and all examples drawn from England | Toolkit – to assist LAs/their partners to plan for the housing requirements of local people with learning disability. Set out in two parts. Planning – the steps likely to be required to plan for a wider choice of housing options. Delivery – the steps and actions likely to be required to commission a choice of housing options. Each section contains a checklist series of questions and suggestions for possible approaches to make progress. Toolkit designed so that each section can be used independently or sequentially |
Rapid review 2: characteristics of included evidence
| Authors/date of publication | Title | Source/type of evidence | Stated aim/purpose | How evidence assembled | Population/sample | Location | Main findings |
|---|---|---|---|---|---|---|---|
| 1. Black and McKendrick,66 2010 | Careful plans report. Positive futures report | Report | Scoping study of the self-identified needs of all older carers of people with learning disabilities known to the local health and social care trust | Empirical research; data collected via semistructured questionnaire survey; descriptive and inferential statistical analysis | Older carers (aged ≥ 50 years) currently caring for a family member with learning disabilities (n = 36) | Northern Ireland, UK | Support (formal and informal) considered vitally important in helping carers to cope. Many carers ill-prepared, pessimistic, anxious and sad about the future. Emergency planning typically arranged with other family members to ‘step in’ until crisis is over. Only 47% of families reported having a plan for the future care of their family member. Most popular future housing option was to remain in the family home with support. If moving out of the home, carers’ consistent preference was for the family member to remain near to current accommodation, and that other family do not take over caring to the same level of commitment. Future care of person with a learning disability is a difficult and emotional subject for families |
| 2. Forrester-Jones,62 2019 | Confronting a looming crisis. People with learning disabilities or autism and their carers getting older | Report | To explore the experiences of older family carers as they continue to care for their older adult relatives with learning disabilities | Empirical research; data collected via interviews; data analysed using interpretative phenomenological analysis | Older carers (aged ≥ 50 years) of adults with learning disabilities (n = 16) | Hampshire, England | Older carers struggle to continue to care for their family members with learning disabilities. Few opportunities for respite and the possibility of meaningful retirement is remote. Lack of continuity of social worker input, variable levels of expertise and pejorative attitudes towards carers. Carers remain understanding of pressures on health and social care service providers. Carers fear for the future in terms of who will care for their family member when they are no longer able to do so |
| 3. Grey et al.,67 2015 | Families’ experiences of seeking out-of-home accommodation for their adult child with an intellectual disability | Journal article | To understand the dynamics of the latter stages of the placement process within families actively seeking out-of-home accommodation for an adult son or daughter currently living in the family home | Empirical research; data collected via interviews; data analysed using Braun and Clarke’s (2006) thematic analysis | Older carers (aged ≥ 50 years) of adults with learning disabilities (n = 9) (including those with ‘behaviours that challenge others’) | Wales, UK | Parents’ ageing and increased health problems along with their offspring’s wish for greater independence were the main reasons for seeking out-of-home accommodation. The all-consuming nature of providing ongoing support to an adult child with high support needs meant that parents did not have time to pursue their own interests. Parents often wanted to plan ahead but were prevented from doing so as the housing system prioritises ‘housing crises’. All spoke of the process of gaining appropriate housing for their adult son or daughter as a very long and stressful process. Communication with social services and housing staff was considered the most frustrating part of the process. Families would like to see social care and housing professionals acknowledge them as collaborative partners in the process |
| 4. Sense,137 2018 | Decisions to make, steps to take. A guide to planning long-term care and support for disabled adults and their families. A Sense toolkit | Resource – sets out information, guidance and tools | To provide information for people with learning disabilities and their families to start making plans for the future | Non-research; no information provided | People with learning disabilities; family carers of people with learning disabilities | Not made explicit; Sense is a UK-based organisation | Comprehensive, easy-to-read guide, setting out main options available, legal rights possessed, and key decisions that need to be made regarding making plans for the future care for people with learning disabilities. Also includes tools to help with decision-making |
| 5. Slevin et al.,61 2011 | A rapid review of the literature relating to support for people with learning disabilities and their family carers when the person has behaviours that challenge and/or mental health problems; or they are advancing in age | Report | (1) What services and support do people with learning disabilities who display behaviours that challenge and their caregivers require to meet their needs? (2) What services and support do older people with learning disabilities and their caregivers require to meet their needs? | Rapid review, using a framework adapted from the NHS Centre for Reviews and Dissemination (CRD, 2009) and the Rapid Review Methodology (NHS, Wales 2006) | People with learning disabilities who display behaviours that challenge; carers of people with learning disabilities who display behaviours that challenge; older people with learning disabilities; carers of older people with learning disabilities | No geographical restriction, only studies published in English included | People with ‘behaviours that challenge others’ Support should be based on the use of resources to maintain the person in their own home, if this is their wish. Identified interventions and services (e.g. PBS, use of community specialist teams, short breaks, teaching and supporting caregivers) were found to be successful in doing so. Appropriate day opportunities also essential, but have not been adequately researched, as is family support to allow people with learning disabled adults with ‘BTCO’ and their family to lead fulfilling lives. Use of medication is high, but behavioural management should be pursued as appropriate. Interventions most likely to be effective when delivered via a family support and education approach, in partnership with formal carers. Active support appears a promising approach. Specialist community teams are a highly effective service. Specialist assessment and treatment units can provide a useful service, but admission should be for a short period, with aim of return to the community. To this end, a model that provides combined specialist support services is recommended. Evidence suggests limited use of full range of mental health services, suggesting deficits in terms of their accessibility and value for learning disabled adults with ‘BTCO’ |
| Older people Most older learning disabled adults wish to continue to live in their family home, and ageing family carers want to continue caring. However, lack of future planning is the norm. Ageing learning disabled adults may face same range of health-related issues as others earlier in their lives. In addition, there are higher rates of some conditions (e.g. dementia). Medications that can help are seldom offered. Appropriate health screening is needed, but scarce evidence that this happens, or that detected health problems are properly investigated and treated. Positive mental health is promoted by such health-improving behaviours, continuing to remain active, and having a meaningful and valued life. Relevant training is required for frontline staff to develop skills to provide appropriate care, both in supported living arrangements or in partnership with family carers. Evidence suggests that facilities geared towards the needs of older learning disabled adults are at best scarce and at worst non-existent. Nursing or residential placement should not be the ‘go-to’ option; a range of intermediate care facilities should be used as appropriate to promote opportunity to return to their home. It should not be assumed that because a person is a particular age that they may not be able to return to their normal home or residence | |||||||
| 6. The Housing and Support Partnership,138 2011 | Planning and commissioning housing for people with learning disabilities. A toolkit for local authorities | Report | Resource (‘toolkit’) | Non-research; no information provided | LAs responsible for the planning/commissioning of housing for people with learning disabilities | All references made in respect of England, and all examples drawn from England | Toolkit, to assist LAs/their partners to plan for the housing requirements of learning disabled adults. Set out in two parts: (1) planning – the steps likely to be required to plan for a wider choice of housing options; (2) delivery – the steps and actions likely to be required to commission a choice of housing options. Each section of the toolkit is designed for independent or sequential use and contains a checklist series of questions and suggestions for possible approaches to make progress |
| 7. Towers,139 2015 | Thinking ahead: a planning guide for families | Resource – planning guide for families with an adult relative with intellectual disabilities to help them think about and plan for the future | To provide information and ideas about how different people can help parents, and contribute to thinking and planning for the future | Resource based on series of workshops held with PWLD, their parents and siblings and a national survey of parents. All consultation focused on what participants thought about making plans for the future | Learning disabled adults, their parents and siblings | Not made explicit; Thinking Ahead is a UK-based organisation | Comprehensive, easy-to-read resource, divided into nine sections that cover different aspects of thinking about and preparing for the future. Sets out a wide range of options and ideas, and includes templates for people to use when undertaking specific tasks, and to record information and ideas |
Rapid review 3: characteristics of included evidence
| Authors/date of publication | Title | Source/type of evidence | Stated aim/purpose | How evidence assembled | Population/ sample | Definition of ‘behaviour that challenges others’ | Location | Main findings |
|---|---|---|---|---|---|---|---|---|
| 1. Hatzidimitriadou and Milne,70 2005 | Planning ahead: meeting the needs of older people with intellectual disabilities in the United Kingdom | Journal article | Drawing together evidence about the nature, extent and quality of policy and services and exploring future directions | Literature review | Older people with learning disabilities; carers of older people with learning disabilities | None provided | UK | Despite some evidence of positive development in this field, much work remains to be done to ensure continuity of care across the life course, particularly in the later stages; consistency of provision within and across areas and agencies; a coherent, effective and well-funded service planning system; access to flexible care for users and carers when it is needed; and, where required, the development of dedicated provision. The current picture is one of inconsistency and fragmentation characterised by limited choice, access, resources and specialist care; this is particularly acute in long-term settings. |
| A lack of underpinning principles and frameworks and a mixed evidence base articulating ‘what works’ hampers development and undermines commitment; this is made worse by the marginal status of older PWLD and the invisibility of many family carers. There is a considerable co-joined service development and research challenge in this emerging field. Much can be learnt from services for younger PWLD, the extensive sphere of gerontology and from developments in dementia care; drawing on good practice in the USA also offers considerable opportunity. Understanding the experience of ageing with a learning disability and evaluating the effectiveness of services are two of the main research deficits | ||||||||
| 2. Campbell,68 2008 | The importance of good quality services for people with complex health needs | Journal article | Measuring the quality of health services in each of the 15 main health boards areas in Scotland | Empirical research: peer-review teams visited each of the 15 geographical areas using a set of quality indicators | The 15 main health boards in Scotland | ‘People with learning disabilities and complex health needs include those who: • present with challenging behaviour or have mental health problems’ [a further five criteria follow this point] (p. 33) | Scotland | There is some evidence that the health boards providing the best-quality services to people with complex health needs were the ones providing good-quality services overall |
| 3. Care Quality Commission,69 2021 | Home For Good: Successful community support for people with a learning disability, a mental health need and autistic people | Report | This report celebrates successful community support, telling the stories of eight people with learning disabilities | Empirical research: case studies [analysis information not provided] | People with a learning disability, people with a mental health need and autistic people | ‘When people are labelled as having “challenging behaviour” – which includes self-harm and physical or verbal aggression – this should be understood as communication of distress or need’ (p. 2) | England | While there is no formula that – if applied – can guarantee success, there are recurring markers of successful community services. There will be evidence of multiagency partnership working, during service planning and delivery. All partners will be committed to making things work and be willing to collaborate. This includes embracing positive planned risk-taking. Housing will be specially built or adapted, and generally close to a person’s family. That family will be engaged and involved in the service. Most of all, the person at the heart of it all – the one for whom the service exists – will be listened to. Their behaviour, which has challenged and may continue to do so, will be recognised as a means of communication. And it will be the provider’s job to understand that communication and respond accordingly. Then the service becomes truly person-centred |
| 4. Jenkins,71 2009 | Nurses’ views about services for older people with learning disabilities | Journal article | To explore nurses’ views of the strengths and weaknesses of current patterns of service provision for older people with learning disabilities in relation to three service models and parent/carer needs | Empirical research: case studies; focus groups; analysed systematically using interpretative phenomenological analysis | People with learning disabilities (case studies); mental health nurses, practice nurses and nurses specialising in the care of people with a learning disability (focus groups) | None provided | Not stated, but the author is divisional head of learning disability at the University of Glamorgan, Wales | This study has highlighted some of the difficulties that older people with learning disabilities may face as they age. There are a number of different service models in operation, although they do not address the particular needs of this population. There still appears to be an expectation that people need to fit into a particular service rather than that the service should be individually tailored to meet the needs of clients and their carers. Nurses have a role in ensuring that older people with learning disabilities have access to both generic and specialist services |
| 5. Levy et al.,76 2006 | Medical conditions and healthcare utilization among adults with intellectual disabilities living in group homes in New York City | Journal article | Identify disability characteristics, medical conditions, and outpatient healthcare utilisation in a sample of PWLD living in several group homes operated by a single voluntary provider and accessing healthcare from a single healthcare practice | Quantitative descriptive data about individuals (age; sex; ethnicity; living situation; level of learning disability; presence of autism, cerebral palsy or sensory impairment; and total number of frequently occurring challenging behaviours) gathered from various sources; analysed using SPSS | 103 adults with learning and other developmental disabilities (nearly 71% of the adults engaged in challenging behaviours that occurred weekly or more often) | None provided | New York, USA | The findings suggest that the adults in this sample represent a diverse group in terms of functioning, behaviours and medical conditions. The findings appear to confirm the conclusions of Mansell et al. (2002) that serving the needs of people with intellectual disabilities in residential homes has become more complex and diverse as an increasing number of individuals become integrated in their communities. The findings from this study indicate that more than one-fifth of the adults in this sample had a level of learning disability that was either severe or profound, and that some 15% were diagnosed with autism spectrum disorder. It is noteworthy that, in this group, autism was associated with age such that younger adults were more likely to have a diagnosis of autism spectrum disorder than older. Nearly 71% of the adults engaged in challenging behaviours that occurred weekly or more often. As the incidence of autism spectrum disorder continues to rise, there is a need to conduct studies that specifically examine the medical trajectories of people with autism spectrum disorder over time in order to plan for their healthcare needs |
| 6. Mahoney et al.,74 2019 | Occupational therapy practitioners’ perceptions about older adults with developmental disabilities in traditional health care settings | Brief report | To determine occupational therapy practitioners’ views about working with older adults with developmental disabilities in traditional healthcare settings | Empirical research: quantitative survey; analysed using descriptive statistics with Microsoft Excel | 310 practitioners from the American Occupational Therapy Association’s gerontology and physical disabilities special interest sections working in traditional healthcare settings | None provided | USA | Most occupational therapy practitioners in traditional healthcare settings found working with older PWLD challenging, and many did not feel sufficiently knowledgeable to meet the needs of this population. Similar to other health professionals, occupational therapy practitioners may benefit from additional resources to provide services to this population |
| 7. Savarimuthu,72 2020 | The potential role of nurses in leading positive behaviour support | Journal article | (The views of nurses about their role in developing PBS plans) | Empirical research: semistructured interviews; analysed through thematic analysis | Six nurses from both mental health and learning disability inpatient settings | None provided | England | Nurses are passive in PBS plan development while other professionals, such as clinical psychologists, often take the lead. While nurses see clinical psychologists as experts in PBS, they feel this could create a barrier that hinders its full potential and a more multidisciplinary approach would be beneficial. Nurses could take a pivotal role in delivering PBS plans if they were able to take a leading role, and this would benefit service users, as nurses work far more closely with them than other professionals |
| 8. Tremblay and Morin,75 2015 | Assessment of an expert committee as a referral process within health and social services | Journal article | This study sought to propose a structured assessment and referral method within the network of public services. Specifically, it evaluated the correspondence between the currently received level of care and an expert committee’s determination. Furthermore, it examined client-related variables that were associated with the level of services. An expert committee evaluated the level of specialisation of services | Empirical research: participants’ [people with learning disabilities] files and presentations by their primary case worker; analysed using descriptive statistics | 30 people with learning disabilities | None provided | Quebec, Canada | This study underscores the primacy of clinical judgement, rather than a predetermined list of participant characteristics, in order to refer persons with learning disability to services that best meet their specific needs. It also highlights the importance of taking into account challenging behaviours |
| 9. Welch et al.,73 2022 | Family‐centred primary care for older adults with cognitive impairment | Journal article | This in-depth systematic review was completed to address three aims: (1) identify the ways in which families of older-adult patients with cognitive impairment are engaged in primary care settings, (2) examine the outcomes of family engagement practices, and (3) organise and discuss the findings using CJ Peek’s Three World View. Researchers searched PubMed, EMBASE and PsycInfo databases to July 2019 | In-depth systematic review | Families of older-adult patients with cognitive impairment | None provided | UK | It revealed that family-centred care and family engagement yields promising results, including improved health outcomes, quality care, patient experience and caregiver satisfaction. Furthermore, it promotes and advances the core values of medical family therapy: agency and communion. This review also exposed the inconsistent application of family-centred practices and the need for improved interprofessional education of primary care providers to prepare MDTs to deliver family-centred care. Utilising the vision of patient- and family-centred care and the lens of the Three World View, this systematic review provides medical family therapists, healthcare administrators, policy-makers, educators and clinicians with information related to family engagement and how it can be implemented and enhanced in the care of patients with cognitive impairment |
Appendix 2 Work package 2: sources of evidence
| Source and status | Standards |
|---|---|
| Learning disability services | |
| REACH Standards – Paradigm, Sally Warren, Jo Giles, 2019 (voluntary standards developed to hold to account and enable conversations about supported living) | (Linked to CQC KLOEs)
|
| CQC. Right Support Right Care Right Culture. How CQC Regulates Providers Supporting Autistic People and People with a Learning Disability. October 2020 Housing with Care: Guidance on Regulated Activities for Providers of Supported Living and Extra Care Housing. October 2015 (regulatory guidance for providers) |
Right support: Model of care setting maximises people’s choice, control and independence Right care: Care is person-centred and promotes people’s dignity, privacy and human rights Right culture: Ethos, values, attitudes and behaviours of leaders and care staff ensure people using services lead confident, inclusive and empowered lives KLOEs: Safe, effective, caring, responsive, well led For example: Care is client-centred and integrated |
|
|
| NHSE, with Local Government Association, Association of Directors of Adult Social Services (ADASS). Building the Right Support: A National Plan to Develop Community Services and Close Inpatient Facilities for People with a Learning Disability and/or Autism who Display Behaviour that Challenges Others, Including Those with a Mental Health Condition. October 2015, p. 25 | Describes and links to a national service model to be delivered by March 2019, aiming to reduce institutional care in campuses and long stay hospitals and the overuse of in-patient treatment, reducing provision by 35–50%, replaced with community commissioned provision. Implementation through 49 TCPs. The National Service model is summarised below: |
|
|
Building the ‘right support’ and the accompanying NHSE ‘service model’ require:
|
|
|
|
| McGill P, Bradshaw J, Smyth G, Hurman M, and Roy A. Capable Environments. King’s College London; 2014 (recommendations to commissioners based in research) | A theoretically driven approach recognising that social and environmental ‘motivating operations’ can provoke or reduce challenging behaviour, includes: Positive social interactions, support for communication, support for meaningful activity, provision of predictable and consistent environments, opportunities for choice, encouragement of greater independence, support to establish and maintain relationships, personal care and health support, mindful (empathic) and skilled family/carers and paid support/care staff, effective management and organisational support Standards: People at risk of displaying challenging behaviour should be: |
|
|
| Thornely J, Lawley J. NHSE Reflective Framework- Confirm and Challenge Toolkit. NHSE Northwest Resettlement Hub; 2017 (an advisory reflective tool for individual and organisational uses) | Putting people first, staff and culture, systems and processes and partnerships along with the five ‘golden threads’ of transforming care should be considered using the six safeguarding adult principles along with each of the 6 Cs underpinning values of ‘Leading Change; Adding Value’; (National Nursing and Care Strategy 2016) For example: Putting people first and Empowerment-Care, compassion, commitment and courage – Is there evidence that the organisation promotes choice, listens to the individual and their family, advocate and other members of the individual’s circle of support? Compassion, communication and competence – Is there evidence that the organisation supports staff to make decisions with the individual and their family? Courage, care and commitment – Is there evidence of positive and collective risk taking? Compassion and competence – staff are encouraged to be creative and innovative, training and supervision in place and robust supporting achievement of person-centred goals? Approximately 63 ‘Wicked questions’ support the above Confirm and Challenge tool. Examples: |
|
|
| End-of-life care (EOLC) | |
| NHSE. Delivering High Quality EOLC for People who have a Learning Disability. 2017 (guide for health and social care commissioners, providers and those delivering care) | NHSE and the Palliative Care for People with Learning Disabilities Network (PCPLD) developed a resource for commissions, providers and those delivering services linked to the NHSE 6 Ambitions Six ambitions for local health and social care providers should use to build the accessible, responsive, effective and personal care needed at the EOL: |
|
|
| NHS Improving Quality. The Route to Success in EOLC – Achieving Quality for People with Learning Disabilities. 2011 (guide for individuals and those delivering care) | This guide was developed by the National End of Life Care Programme (NEoLCP) and GOLD (Growing Older with Learning Disabilities) programme, which is a facilitated group of older people with learning disabilities: It is aimed at families, and those caring infrequently for people with learning disabilities, and takes them through 6 steps in the process. It is underpinned by four principles: |
|
|
| College of Social Work, NHS Improving Quality with College of Social Work. The Route to Success in EOLC – Achieving Quality for Social Work. 2015 (guide for social workers and managers) | A guide for practitioners and their managers to identify issues, tips, reflective questions and case studies. It links to social work core values around rights-based approaches and the individual in context. It uses the six-step approach in related ‘routes to success’ guides |
Appendix 3 Work package 2: quotations from interviews by criteria of excellence
| Criteria of excellence | Quotation |
|---|---|
| 1. Personalisation – assessment, goals, daily plans/activities | (Provider): but we need to think about people want in relation to all sorts of things, you know, down to the most simplest thing like having your knitting wool under your pillow. And that’s important to one person. That was important to one person that both [XXXX] and I supported throughout her life at different occasions. And for somebody else that might be totally insignificant. Why would you want to put their knitting wool under their pillow, but for her it was so important. With her teeth, and her teeth yes |
| 2. Matching placement to person – for example, care staff organised and selected for that person’s needs | (Provider): Yeah he’s got six members of staff who are in his team. He selects them. He’s involved in selecting them. We employ people on the basis of who he is, people that will match very well with him, people that got on well with him. The other important thing to say is in each member of staff’s contract. So each person we support has got their own staff team. Some of those staff team might work with one other person, but we prefer people just to work with one person. Because it’s really complicated work that we’re doing and you’ve got to have so much detail |
| 3. Personalised living space/and choices of whom this is shared with | (Provider): So we opened it, it’s probably about seven or eight years ago now, and there were three families who were leading the project. And the person with the complex behaviour, his family weren’t particularly active in it. […] And I really do believe that if that hadn’t happened the likelihood is he would have ended up in inpatient services, because I don’t think he would have coped. […] the families were well connected, but also the people who moved had known each other nearly all their lives and are genuine friends. That kind of compatibility is so important […] they were coming from home. The families were worried about their age […] And five of those parents have died since that happened (Provider): Their own bedroom is decorated how they want it to, so currently we’ve got, a Dr Who fanatic has got his whole room in Dr Who wallpaper. Literally you walk in, it’s like a museum. We’ve got guitars on walls, we’ve got James Bond posters. Yeah, it’s been painted in their favourite colour. That is theirs to do what they want with |
| 4. Health; proactive, preventive, primary care, and involvement of NHS MDT | (Provider): So again we’ve got […] an amazing learning disability service for the dentistry. […] So he allowed us to go in after hours, or when he was having his office day, for our residents to just get to know him and see the examination room. […] They have secondary {care} learning disability nurses who allow those reasonable adjustments, and really advocate for PWLD. So I think when it comes to [county] we are fairly lucky in our area for having those additional resources really (Provider): So we tend to, generally speaking we use one surgery. They’ve all got their own GPs […] and therefore they’ve known them for a long time and they’ve kept the same surgery. […] We then also have the primary care liaison nurses who are part of the learning disability team. […] Then we also have the IAT team, which is the intensive assessment and treatment team, and they are basically specialists. So they’ve got a speech and language therapist, psychologist, they’ve got a psychiatrist attached to them, learning disability nurses. So anything which is more complex and to do with behaviours, and looking at anxieties or antipsychotic medication where it’s needed, we’ve got the team of specialists that we involved for that as well. And we can either direct refer for that, or we can go through the GPs. And I have to say actually particularly in our area the team is very responsive […] so they all have annual health checks as a minimum. We go up to the surgery for them, done by the GPs. Where there is a resident that is too anxious to do that, which can occasionally happen, primary care team again will come out and do that within the home |
| 5. Staff recruited with the values and skills matched to the person | (Provider/personal carer): The staff that I’ve been in contact with, appear to have good relationships with the people that they support, and I think that’s key isn’t it? You have to care. It has to matter when the GP says whatever. You have to have somebody with that says that’s not good enough. You have to have people that care about who they support. […] And that’s what you want isn’t it, as a mum I want to know when I’m dead, she’s surrounded by people who will care if a GP says ‘nah, you don’t need a smear test’. You know, like you can manage without your flu jab because it’s hard work giving you flu jab and talking, you know, it takes a bit too long. I’d want somebody that would say well no take the time
(Commissioner): But what I would expect to happen with the design and the approach to the model of care would very much be reflective of their individual needs and what’s going to work for them. […] And I would expect the care and support provider to be recruiting a staff team to that individual specification of those needs. If you’ve got a really quite active individual who likes walking, and your staff team are very sedentary, that’s really not going to deliver to those needs. So it is quite an iterative process and certainly developed around the individual’s needs when they identified. So there’d be a referral process dependent on who would be best fit, and that would help shape the model and that co-design |
| 6. Staff retention is high to give continuity of care and experience sharing with significant decision-makers | (Provider/manager): Rather than somebody going from a family home into a house where staff come in and out, and you might have unfamiliar people coming in and out, I suppose the beauty of Shared Lives is the continuity of the carer. […] So sometimes we will have it where people you, so families use Shared Lives for short breaks too. […] And so that family already builds up that relationship and trust with a Shared Lives carer, so does the customer. And then that is always an option then, people will often say if I gave him up would you take him?
(Provider): So we’ve got a really longstanding staff team. […] so the staff members have worked with the people we support for ages, so we get to know the people we’re supporting very well, but it’s also the person we support knows that they can rely on that person that’s supporting them. And yeah, it makes hospital appointments, doctors’ appointments a lot easier, because we can recognise signs of pain and distress very quickly. So yeah, it has worked really well. And then obviously having longstanding members of staff helps induct new staff, because then they can share all their experience with our new staff |
| 7. Communication methods are inclusive as used by provider staff and others | (Provider): … we’re training the [site] staff in communication with people with a learning disability on Thursday night. And we do training for like the hospice as well. So that if their staff come across people with a learning disability, they’ll more prepared in communicating with them, and looking for those subtle signs of communication, which might be just a facial expression or a movement of the hand or something
(Provider): we’ve got good paperwork, so we do our initial communication passport, and we work closely with the SALT [speech and language therapy] team here. […] So we’ve got a manager who’s a bit more expert in communication that other managers can go to, rather than trying to train everybody in everything, and that’s how we work with lots of different areas here. So we’ve sent her on all the most up to date training, and then we use local intensive interaction training, total communication. We do lots, and we cover it in our induction, which is led by me for day one for all staff |
| 8. Family involvement | (Provider-executive): Also I think a fundamental principle of what we do is that it’s, when we say ‘nothing about me without me’, we also include the family in that, it’s not just the single person. So the cultural message I suppose that families are part of the planning and part of someone’s life is so very key
(Commissioner): Sometimes we have a conflict in terms of parental family views on what somebody needs and what might be in their best interest. So certainly, if people don’t have mental capacity, we need to ensure there’s capacity assessments in place, and that if family do have lasting power of attorney or deputyship for welfare and finance, that their views certainly help shape anything that we consider, but it must be in the individual’s best interest, but it’s on a case-by-case basis (Provider): But in the contracts of our staff there’s this thing called the third party agreement, which means the person or the family or the representative has got to agree to that person’s recruitment, and if they don’t we can legally then move that staff person out of that team |
| 9. Engagement and inclusion in community/friendships | (Provider): As it normally is we try and support them out at least once a day. Whether it’s literally they’ve chosen just to go for a car ride, because some of them just want to go out in the car and don’t want to walk down the high street or whatever. We’d support them, I mean they’ve been to zoos, proper trips out, [name of city] to the docks and things like that. Or it might just be a walk down to the local shop to get them out and about. So we do encourage that at least once a day. […] We would go to church at our local church, and we did artwork for them. We’d take part in tea and coffee afterwards, get to know the community that way. The local fish and chip shop, we know them as well. That’s a weekly tradition, and we’d go down and get some fish and chips
(Commissioner): They really focus on what is meaningful for each individual. So they don’t, when we talk about daytime activities, it’s not like the whole house goes and does the same thing, because that’s convenient for the organisation and the staff. Everybody gets to do what they actually want to do. And everybody’s support plan is different based on their needs. So you really do have proper person-centred care |
| 10. Services to prevent and support behaviours that challenge, trauma informed | (Provider): … and he shouts and he threatens to stab. He’s in flats with two other neighbours and flats, and the landlord of course gave him notice. […] So when we said to him you’re going to have to move, well he nearly went through the roof. Threatening to stab and kill. Now he doesn’t do any of it, but it’s very scary when he threatens all of that stuff. But we did have to move him. […] So the landlord found us these two new flats. We moved all his stuff. We took a picture of everything, where it was in his old house and where we put it in his new house. And then we brought him back. […] We go to the nth degree to get people out of hospital and keep them out
(Provider): So our PBS approach […] there are 10 elements, which are things like touch, warmth, positioning, so getting to the same height as somebody. Communication, observation, reflection […] they’re used in training to help staff understand how to have great interactions and how to make sure that, you know, the catchphrase is ain’t what you do, it’s the way that you do it. […] Often it needs the staff to stop and reflect on how they’re supporting, and to make sure they’re getting those core things like communication right for the person. And so often getting that stuff right, or getting the stuff in place for somebody who may be going down the dementia pathway to help with their anxieties early on, might actually negate or minimise the need for the PBS to have heavy involvement |
| (Provider): It’s looking at everything, not just prescribing people medication to be able to reduce behaviours. […] one-to-one, two-to-one, predominantly two-to-one [carer–client ratio]. […] They were challenging, the people that lived there. And they had an incredible amount of hours going in, incredible. So there were three people living there. There were probably I would say 10 staff on duty […] and we said this is not right. This is aggravating people and it’s contributing to the behaviours. There’s too much going on. There’s too many staff there. So we have worked with the local authorities and we’ve reduced the hours going in. So it’s not necessarily the right thing to throw hours and staff at situations, because that can itself be a trigger
(Provider): Encourage people to see the strengths that they have within them in other areas. Someone might come and be classed as an arsonist or a fire setter, and people they haven’t got much, there’s not much time for them to learn, they’re not going to be able to do anything else in the community. And we say well hang on a minute, let’s see what it is that we can do. If we get the team right, if we get the environment right, we work really closely with people in a community setting |
|
| (Provider): … so the personal agreement I think is a key aspect of the beginning to form that relationship, because I guess our relationships are formed on compromise and giving and taking and reciprocation. And a lot of the time I think that the people that we support have been done unto, and there hasn’t been reciprocation because they’ve been in hospitals, and they’ve been directed around, told where to go, taken to schools that they might not have wanted to be in and stuff like that. So we’re giving them that power to make choices at that point
(Provider): So we’re really big on not only doing that personal agreement, but also having a really lengthy transition. If you want it to sustain, and you want someone to be a success, and you want them to start almost calling the shots as it were, or dictating how they want to be supported. You have to invest in an awful lot of transition. […] And I think what we have to try and do is educate and show commissioners that actually this big outlay in the beginning pays dividends in the long run |
|
| 11. Good practices, such as in EOLC planning, dementia assessment and management, are embedded as routine | (Provider): So one of the things that [name of provider] particularly is good at is data collection. So in terms of a person’s challenging behaviour, we have a good functional understanding, and how the person manages the everyday challenges. So when there is a variation and there is a discrepancy in the presentation of their behaviour, we have quite a lot of evidence to put forward a compelling argument that this isn’t this person’s normal challenging behaviour, there is something wrong
(Commissioner): But by being part of the design of such provision, we can future proof that provision. So you might have younger adults in their 50s, particularly maybe with Down’s syndrome that maybe are starting to show early onset of dementia. So if we can get environments right from that development stage, it means that we can afford more security for those people so they don’t have to move into larger care home type provision. So it’s a case of really being a bit more individual and person-centred in that development stage so that we’ve got longevity of provision for people |
| 12. Commissioner endorsement of provider quality and resilience (low placement breakdown) | (Commissioner): And then also as well as worked with housing particularly, that was really critical to get the right accommodation. And we had a very proactive approach around shared ownership for people with learning disabilities. Because one of the things that we didn’t want happening is when they came out of hospital for them to be moved by their landlord, or evicted or anything like that, and so we really needed to create that security of tenure. And we thought certainly actually getting people shared ownership was a really positive way of doing that
(Commissioner): Other things that helped were things like we did contingency funding for some people, where the provider would have an extra pot of money to draw on, without having to go back through a panel and get funding. They just had money that they could say ‘Oh yeah, so-and-so is really, she’s getting a bit stuck in her behaviour, what can we do? Why don’t we pop down to [county] for a weekend away?’ and that was money there, and they could just go and do something like that. And that really helped avoid re-admission |
| 13. Commissioners are planning ahead with providers and individuals and families around the client group – building capacity for future services | (Commissioner): We had like monthly meetings between the commissioner, I would attend with members of the multidisciplinary team, and the psychiatrist would be there, and the clinical staff, and the provider. And we would actually structure our agenda around individuals and say well how’s [name] doing, you know, is she OK? And then they could talk about things like the care plan. […] And we also used it for planning people coming out of hospital as well. So it was a way of monitoring and supporting those people who’d already come out, planning for moving, and just checking up how are our transition plans happening for that person
(Commissioner): And then the other group of people that we’ve worked very closely with around some individuals were the police, as well as our hospitals. We developed a pilot around police passports. We also had work around hospital passports so that people could make reasonable adjustments and knew what they should be for each person |
| (Commissioner): We have agreed that for each package of care we commission, we will give the provider a contingency fund of £5000. And again that was met with a sharp intake of breath from them, because they were like what, you’re going to give us £5000 and what do you want us to do with it? And we said be imaginative, be innovative. If someone’s having a bit of a wobble on a Friday night, don’t bring in two other members of staff to stand in the same room as them and stare at them. But think about what is important to that individual, do they like surfing, do they like going on holiday, do they like going to a farm, go for walk, anything, but use it. […] It was going to be held on a prepayment card and we would monitor it every month. But they didn’t have to seek prior approval from us in order to spend it
(Commissioner): Try and reduce some of the issues I commissioned the dementia service, specialist dementia service from [county] and borders. So what we now have is a situation where they will do baseline assessments, one of them was particularly for Down’s syndrome. So they will do a baseline assessment at age 30 of anybody who is on the GP register with Down’s syndrome. […] And it basically gives a really good benchmark of where the person is when they’re well. So that when they start to experience changes later in life, they then are referred back to the service […] they then are allocated a nurse within the CTPLD [community team for PWLD] and a member of the dementia team who then do the ongoing support |


Appendix 4 Work package 5: dissemination plan
| Output/activity type | Title | WP | Audience | Available |
|---|---|---|---|---|
| Press release | New research to improve support for older people with learning disabilities and end-of-life planning for carers: GOPA Growing older/Planning Ahead | All | Academics, policy, voluntary sector, public | n/a |
| Website | Improving the support for older people with learning disabilities and BTCO, family and professional carers, and supporting EOLC planning for carers | All | Academics, policy, voluntary sector, public | http://wels.open.ac.uk/research/growing-older-planning-ahead |
| Academic paper British Journal of Learning Disabilities (BJLD) |
‘Ethno … graphy?!? I can’t even say it’: Co-designing training for ethnographic research for people with learning disabilities and carers | WP3 | Academics and co-researchers | https://onlinelibrary.wiley.com/doi/full/10.1111/bld.12424 |
| Academic paper response BJLD |
Response to ‘Ethno … graphy?!? I can’t even say it’: Co‐designing training for ethnographic research for people with learning disabilities and carers | WP3 | Academics and co-researchers | https://onlinelibrary.wiley.com/doi/full/10.1111/bld.12452 |
| Academic paper Systematic Reviews |
Transitions for older people with learning disabilities and BTCO, and their family carers: a merged protocol for two rapid scoping reviews of evidence | WP1 | Academics | https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-021-01883-3 |
| Academic paper BJLD |
‘My name on the door by the Professor’s name’: The process of recruiting a researcher with a learning disability at a UK university | WP4 | Academics | https://onlinelibrary.wiley.com/doi/full/10.1111/bld.12477 |
| Easy Read academic paper | Easy Read report for the paper: ‘My name on the door by the Professor’s name’: The process of recruiting a researcher with a learning disability at a UK university (a case study) | WP4 | PWLD, carers, public | https://onlinelibrary.wiley.com/action/downloadSupplement?doi=10.1111%2Fbld.12477&file=bld12477-sup-0004-Appendix_4_Easy_read_version_of_paper.pdf |
| Academic paper BJLD |
‘Internet is easy if you know how to use it’: doing online research with people with learning disabilities during the COVID‐19 pandemic | WP3 | Academics | https://onlinelibrary.wiley.com/doi/full/10.1111/bld.12495 |
| Academic paper Journal of Applied Research in Intellectual Disabilities |
Transitions for older people with intellectual disabilities and BTCO: a rapid scoping review | WP1 | Academics | https://pubmed.ncbi.nlm.nih.gov/36433739/ |
| Academic paper submitted to Health and Social Care in the Community | Transition-related support for ageing family carers of older people with intellectual disabilities and BTCO: a systematic scoping review | WP1 | Academics | Under review |
| Academic paper International Journal of Social Research Methodology |
Whose uncertainty? Learning disability research in a time of COVID-19 | WP3 | Academics | www.tandfonline.com/doi/full/10.1080/13645579.2023.2173425 |
| Academic paper Journal of Applied Research in Intellectual Disabilities |
'There's a timebomb': Planning for parental death and transitions in care for older people with intellectual disabilities and their families | WP4 | Academics | https://onlinelibrary.wiley.com/doi/full/10.1111/jar.13174 |
| Professional literature (Care Management Matters) | Improving the support for older people with learning disabilities and behaviours that challenge, family and professional carers, and EOLC planning for carers | All | Social work professionals | www.caremanagementmatters.co.uk/cmm-ebook-november-2020/ |
| Professional literature (Care Management Matters) | An update to the above piece sharing some project findings | All | Social work professionals | www.caremanagementmatters.co.uk/feature/paving-the-way-in-excellence-supporting-older-people-with-learning-disabilities-to-lead-good-lives/ |
| Professional literature (Community Living) | Putting research right | WP3 | Social work professionals, PWLD, carers, voluntary sector | www.cl-initiatives.co.uk/putting-research-right/ |
| Professional literature (Community Living) | The foundations on which to build a real home Having a good life requires having a place you feel is truly home. While research has found three common themes underpinning this, what fulfils these can change over time |
WP3 | Social work professionals, PWLD, carers, voluntary sector | April 2023 |
| Blog | Planning ahead, older people with learning disabilities and a shake-up of ‘tired’ research practices | All | Academics | ]https://enrich.nihr.ac.uk/blogpost/ |
| Blog | Services and support for older people with learning disabilities with BTCO: what does good look like? | WP2 | Academics, commissioners | Growing Older – Planning Ahead | An Open University research study |
| Twitter chat | Learning Disability nursing web forum (WeLD) Nursing Twitter chat | All | Health and social care professionals | www.wecommunities.org/tweet-chats/chat-details/5600 |
| Training (delivered by University of Aberdeen and Point of Care Foundation) | Foundations in patient experience – screenshots of materials and links to resources | WP3 | Health professionals | n/a |
| Film | Short film of project at time of funder interim report | All | PWLD, carers, public | Facebook, Twitter |
| Film | Video abstract for ‘My name on the door by the Professor’s name’: The process of recruiting a researcher with a learning disability at a UK university | WP4 | PWLD, carers, public | www.youtube.com/watch?v=BaoMF9HLwV4 |
| Evidence blog | How to employ people with learning disabilities in research | WP4 | PWLD, carers, public | https://evidence.nihr.ac.uk/alert/blog-how-to-employ-people-with-learning-disabilities-in-research/ |
| Film | Living well and ageing well | WP3 | PWLD, carers, public, voluntary sector, providers | Available March 2024 |
| Film | Planning ahead and EOLC | WP4 | PWLD, carers, public, voluntary sector, providers | https://kingston.box.com/s/0eoshdfrpj3t6lbdw5o17nrw3ocycpvp |
| Film | Growing Older, Planning Ahead | All | Academics, PWLD, carers, public, voluntary sector, providers, commissioners, policy | Available from March 2024 on Socialcaretalk.org |
| Podcast | Doing research! What’s it like?! | All | Available from March 2024 | |
| Media report | ‘A Fundamental Lack of Awareness that these People are Actually Human’: How the Government is Failing Older People with Learning Disabilities | All | Wider public | https://bylinetimes.com/2023/05/03/a-fundamental-lack-of-awareness-that-these-people-are-actually-human-how-the-government-is-failing-older-people-with-learning-disabilities/ |
| Course (OpenLearn) | Supporting older PWLD and their families: a course for health and social care practitioners | WP3, WP4 | Social care professionals | www.open.edu/openlearn/health-sports-psychology/supporting-older-people-learning-disabilities-and-their-families/content-section-overview?active-tab=description-tab |
| Course (OpenLearn) | Supporting an older family member with learning disabilities | WP3, WP4 | PWLD, family carers | www.open.edu/openlearn/health-sports-psychology/caring-older-family-member-learning-disabilities/content-section-overview?active-tab=description-tab |
| Course (CPD) | Growing Older, Planning Ahead | WP3, WP4 | Social workers | Available from March 2024 |
| Forum the OU | Moderated forum to share best practice hosted by the OU and linked to CAREN | All | Social care professionals | https://wels.open.ac.uk/research/projects/carers-research-group available from November 2023. |
| Planning ahead cards | Physical and online conversation cards | WP4 | PWLD, family carers | https://sway.office.com/5LjAwlV0OFsHjBAj |
| Session plans | Session plans for PWLD and family carers to think about good service provision and growing older well | WP3 | PWLD, family carers | See Appendix 5 |
| Conference (SPCR public engagement event) | Co-designing training materials for Growing Older, Planning Ahead | WP3 | PWLD, family carers | n/a |
| Conference (Hospice UK) | Planning for parental death and transitions in care for older people with learning disabilities: An adapted experience-based co-design project | WP4 | Academics | https://spcare.bmj.com/content/12/Suppl_3/A1.1 |
| Conference (International Association for the scientific study of intellectual and developmental disabilities) | Recruiting a Research Assistant with intellectual disabilities at a UK university: A case study | WP4 | Academics | n/a |
| Conference (European Association of Palliative Care) | Co-producing a Decision Aid Tool to Support Future Planning and EOLC Planning Discussions with Older Family Carers of People with Intellectual Disabilities | WP4 | Academics | June 2023 |
| Conference (Nordic Network on Disability Research) | Experts by Experience on the Flourishing Lives and Growing Older projects | All | Academics, PWLD, carers, public | May 2023 |
| Conference (Nordic Network on Disability Research) | Inside out: The experience of being PPI Coordinator and family carer on the Flourishing Lives and Growing Older projects | All | Academics, PWLD, carers, public | May 2023 |
| Conference (Nordic Network on Disability Research) | Sticky labels and their consequences: people with learning disabilities and ‘behaviours that challenge others’ | All | Academics | May 2023 |
| Conference (The Social History of Learning Disability Group, OU, 2023) | Belonging and Community for Older People with Learning Disabilities: past, present and future | All | Academics, PWLD, carers, public | July 2023 |
Appendix 5 Example of a work package 5 session plan, including the Easy Read version
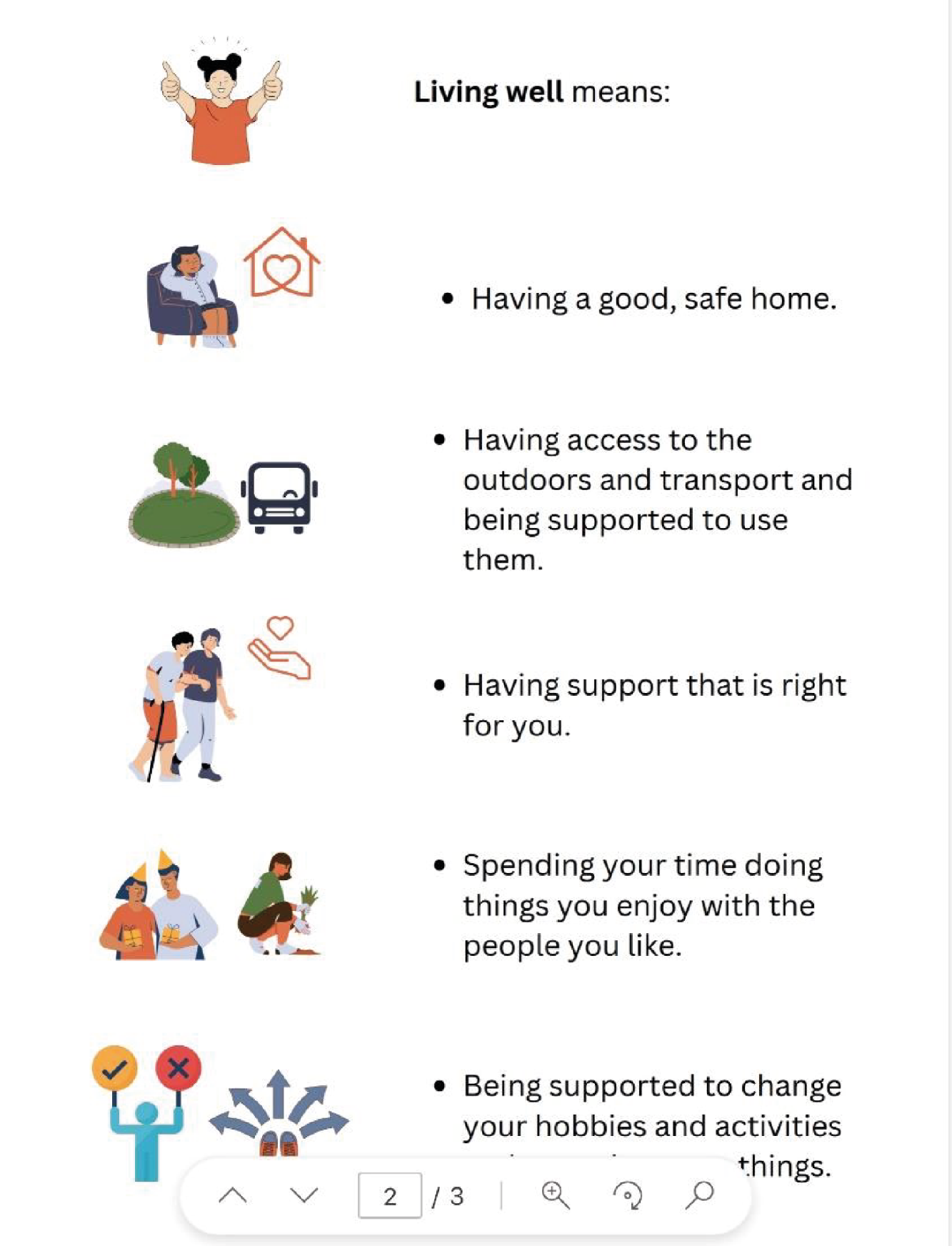
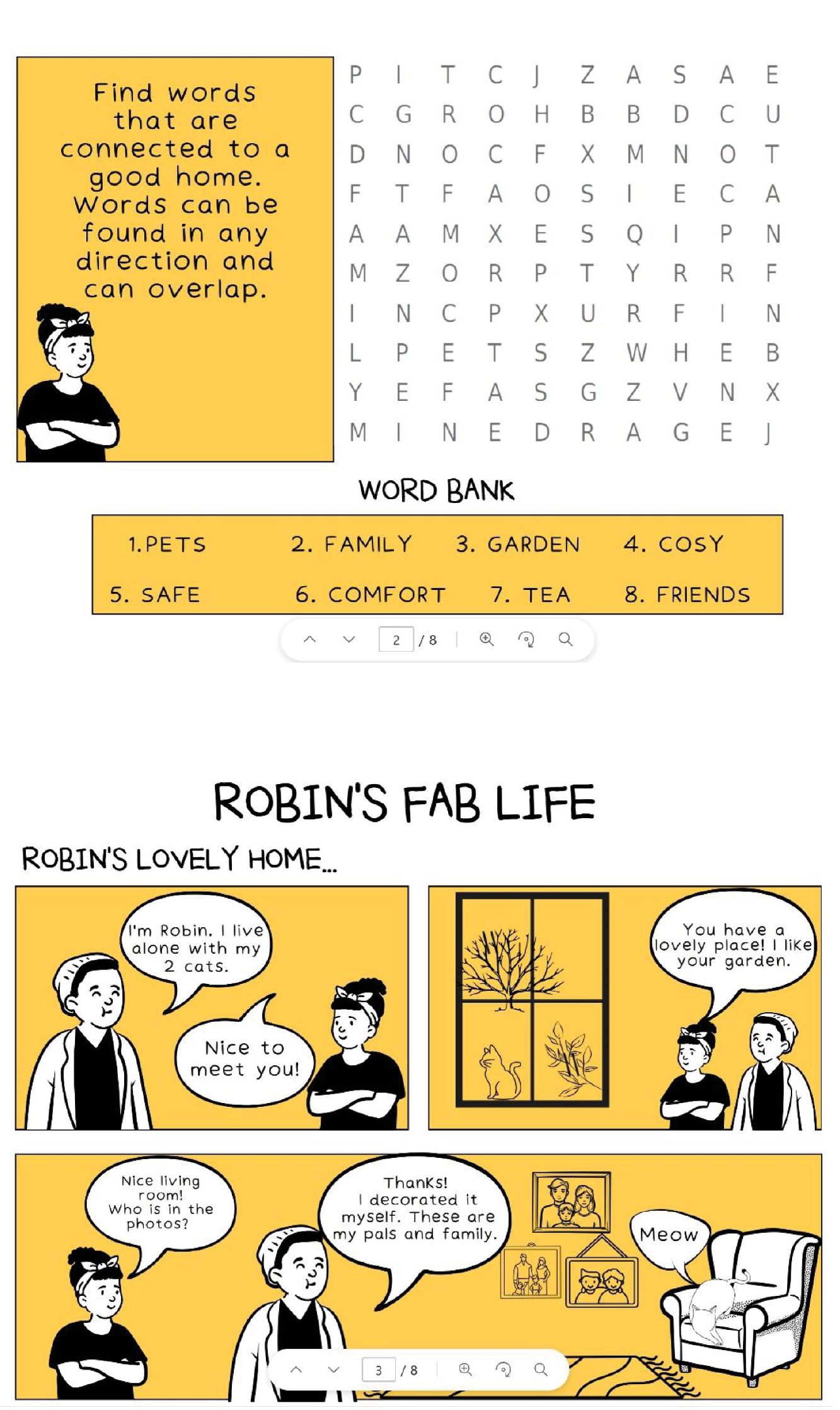
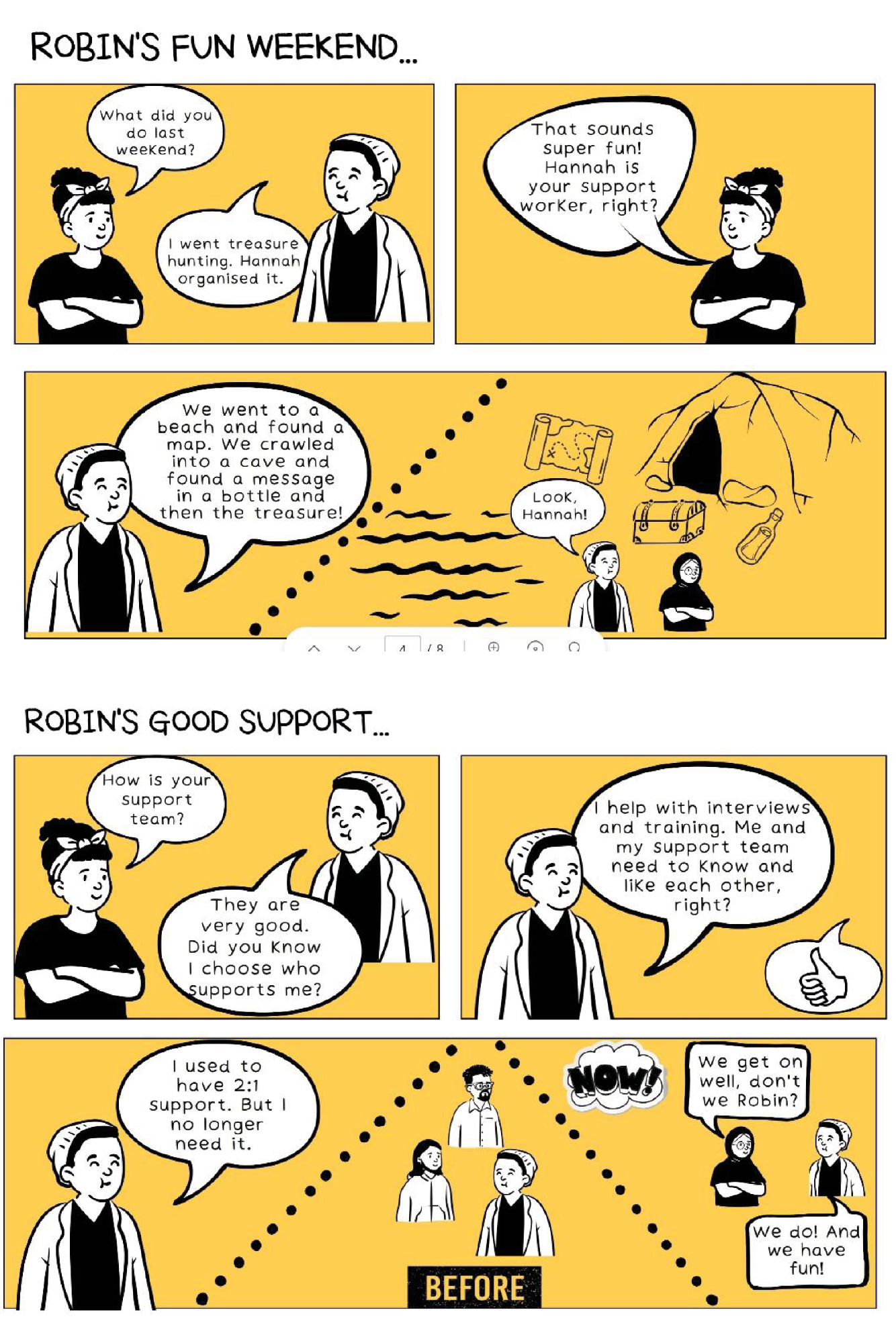

List of abbreviations
- BASW
- British Association of Social Workers
- BTCO
- behaviours that challenge others
- CAREN
- Carer Research Knowledge Exchange Network
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CQC
- Care Quality Commission
- EOL
- end of life
- EOLC
- end-of-life care
- GM GOLD
- Greater Manchester Growing Older with Learning Disabilities
- GP
- general practitioner
- HMIC
- Healthcare Management Information Consortium
- ISL
- independent supported living
- KLOE
- key lines of enquiry
- LA
- local authority
- MDT
- multidisciplinary team
- NHSE
- NHS England
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- OU
- Open University
- PWLD
- people with learning disabilities
- RR
- rapid review
- SSC
- Study Steering Committee
- TCP
- Transforming Care Partnership
- TRIP
- Turning Evidence Into Practice
- WoS
- Web of Science
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/MTHW2644).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
