Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/60/01. The contractual start date was in June 2013. The draft report began editorial review in February 2016 and was accepted for publication in August 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Judith Watson reports grants from the National Institute for Health Research (NIHR) Health Technology Assessment programme during the conduct of the study. Ed Day reports grants from the NIHR Health Technology Assessment programme, personal fees from PCM Scientific and personal fees from Public Health England outside the submitted work and he is the author of the treatment manuals Routes to Recovery via Criminal Justice and Routes to Recovery via the Community. Materials from these manuals influenced the final treatment manual in this study. He produced these manuals with the aid of a small grant from Public Health England and they are now freely available in the public domain [see www.nta.nhs.uk/routes-to-recovery.aspx (accessed 29 November 2016)]. Louca-Mai Brady reports that public involvement of young people in this study has also formed a case study for her PhD thesis, for which she received a bursary from the University of the West of England. This does not constitute a conflict of interest and any claims to intellectual property have been waived. Caroline Fairhurst reports grants from the NIHR Health Technology Assessment programme during the conduct of the study. Kim Cocks reports grants from the NIHR Health Technology Assessment programme during the conduct of the study. Eilish Gilvarry reports grants from the NIHR Health Technology Assessment programme during the conduct of the study. Alex Copello reports having a patent relating to Social Behaviour and Network Therapy for Alcohol Problems (Adult), broadly relevant to this work, with royalties paid.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Watson et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
This report presents the findings from a National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme-funded programme of work to develop and explore the feasibility of a new family and social network intervention for young people who misuse drugs and alcohol. This study had three main aims: first, to adapt a British, evidence-based, adult-focused family and social network intervention (social behaviour and network therapy or SBNT) to the under 18 years age group; second, to assess the feasibility and acceptability of this intervention; and, third, to explore the potential for evaluating its clinical effectiveness and cost-effectiveness through a future, definitive trial. The new intervention has been named youth SBNT (hereafter Y-SBNT).
This chapter provides the background context in terms of the extent of substance use problems among young people, the effectiveness of current family interventions and barriers to implementation of interventions in the UK. The remainder of the report is divided into the following chapters:
-
Chapter 2 – intervention adaptation
-
Chapter 3 – feasibility trial methods
-
Chapter 4 – protocol changes
-
Chapter 5 – results
-
Chapter 6 – qualitative results
-
Chapter 7 – treatment fidelity rating
-
Chapter 8 – involving young people in the study
-
Chapter 9 – discussion.
Background
Substance use among children and young people
The two most commonly consumed substances by young people, accounting for 90% of treatment admissions, are cannabis and alcohol. 1 Statistics on drinking and drug use among young people are divided between those drawn from surveys of school-age children and those drawn from surveys of adult populations, including young adults. Among children of school age, although the proportion of those drinking at all has dropped slightly since 1988, the average number of units consumed increased markedly between 1990 and 2006 and has since stabilised at this level. 2,3 On the other hand, contrary to media reporting, average alcohol consumption among young adults (aged 16–24 years) has fallen since a peak in 2000–2. Nonetheless, 15- to 16-year-olds in the UK still come third highest out of 36 European countries in the proportion self-reporting drunkenness in the past 30 days (26%). 4 Cannabis use has also shown a decline among school-age children since reaching a peak in 2000–33 and a longer decline among young adults since 1998. 5 However, the UK is among the 10 European countries with the highest proportion of 15- to 16-year-old students reporting smoking cannabis within the past 30 days. 4
Since the commissioning of the current study, there has been increasing public concern about the use of novel psychoactive substances (NPSs) or ‘legal highs’ among young people. Accordingly, new questions were introduced to the smoking, drinking and drug use school survey conducted in 2014 in participating secondary schools across England, with 2% of pupils in Years 7–11 reporting using a NPS/legal high in the past year. 3 In addition, employing a generic definition of NPS use for the first time, data from the most recent Crime Survey for England and Wales show only slightly higher NPS use among 16- to 24-year-olds (2.8%) in 2014. 5
Early onset of drug use, including alcohol, has been associated with later problematic use. 6,7 Early onset of use and early hazardous use have also been associated with a range of other problems including risky sexual behaviour, injury, antisocial behaviour, violence and changes in brain development. 8,9 Moreover, in considering the impact of substance use on the family, research has shown that substance use among young people can adversely affect relationships with parents, carers and other family members,10 but also that family involvement in interventions can influence the course of the problem in a positive way. 11
Family-based interventions
Research has highlighted the pivotal role that families play as both a risk for, but also a protection against, substance-related problems. 11 As a consequence, a range of preventative and treatment approaches has focused on the family. In the UK there has been a strong focus on preventative programmes. A systematic review by Foxcroft et al. 12 identified the Strengthening Families Programme (SFP),13 developed in the USA, as the most promising, with positive outcomes in both the short and the long term. Emerging findings from the application of this model to the UK context have also been promising. 14
Turning to the treatment field, reviews of evaluations of family-based interventions with young substance users have tended to show that the most empirically supported family interventions are multidimensional family therapy (MDFT), multisystemic therapy (MST), brief strategic family therapy (BSFT) and functional family therapy (FFT) (Carmel Bennett, School of Psychology, University of Birmingham, 2013, unpublished review). Eleven literature reviews were included in a two-part review undertaken as part of the current feasibility study of Y-SBNT (Carmel Bennett, unpublished review). Although there is growing evidence for the effectiveness of these interventions (particularly MDFT and MST), problems exist concerning initiation, engagement and retention, treatment decay and translating research into practice.
Initiation, engagement and retention
The initiation, engagement and retention of young people and their families in substance use treatment has long been recognised in the literature as a significant issue. 15–17 Initiation, engagement and retention therefore formed a key focus of the review undertaken for this project (Carmel Bennett, unpublished review) and has also formed the main focus of a subsequent article from the USA. 18 Despite the widespread recognition of the saliency of the issue, there is notable inconsistency and lack of analysis among studies in this field with regard to the definition of initiation, retention and, particularly, engagement18 (Carmel Bennett, unpublished review). Nevertheless, there is clearly variation in the degree to which programmes have been able to involve young people and their families and maintain treatment through to completion. Dembo et al. 19 report completion rates of 40% for adolescents and their families attending brief intervention services. Similarly, Dakof et al. 16 found engagement rates as low as 53%. However, structured family interventions studied as part of well-resourced evaluations show much higher completion rates of between 70% and 90% (e.g. Pullmann et al. ,18 Rigter et al. 20 and Henggeler et al. 21). In addition, comparative studies have shown that a family component can reduce dropout. In a study by Hendriks et al. ,22 of the 54 participants allocated to cognitive–behavioural therapy only 16 completed treatment, whereas 44 of the 55 participants allocated to MDFT completed treatment.
A key issue affecting the initiation and retention of young people and families in treatment is the extent to which perceived ‘coercion’ is involved. In the UK context, criminal justice referrals constitute the largest referral source for young people in specialist substance misuse services (29%) followed by education (26%). 1 As Pullmann et al. 18 point out, initiation and attendance are ‘usually driven through compliance with family, court, school or employer demands, rather than intrinsic motivation’ (p. 348). In this context, defining engagement in behavioural terms as turning up for treatment sessions is likely to be primarily measuring the degree and nature of coercion and the penalties for not ‘engaging’. Researchers have therefore sought to explore other definitions of engagement that are rooted in active participation,23 with one such commonly used measure being therapeutic alliance. 24
Recognising the importance of retention and engagement, one of the aims of the review undertaken for the current study (Carmel Bennett, unpublished review) was to identify the characteristics of interventions that appear to be associated with successful retention. To achieve this, the four family programmes associated with the best outcomes (MDFT, MST, FFT and BSFT) were selected for detailed study, including research papers, literature reviews, clinical papers and direct communication with authors and programme developers. As a result, a number of key components were identified.
An overview of intervention components associated with retention and engagement can be seen in Table 1. They have been subdivided into components related to therapist style and orientation, structural factors, therapy orientation and additional factors.
| Therapist style and orientation | Structural factors | Therapy orientation | Additional factors |
|---|---|---|---|
| Reflective listening (MDFT, MST, BSFT, FFT) | Flexibility (MDFT, MST, FFT) | Goal setting (MST) | Contingency management |
| Realistic hope and reinforcement (MDFT, MST, BSFT, FFT) | More frequent client contact based on need (MST, FFT) | Therapeutic alliance (parent–therapist) (MDFT) | Waiting time |
| Authenticity (MDFT, MST, BSFT, FFT) | Individualised service (MDFT, MST, FFT) | Strength focused (MST) | Use of social and mobile media |
| Productive communication (MDFT, MST, BSFT, FFT) | Tracking family members by telephone or in person (BSFT) | Reduction of parent burden (MDFT) | |
| Empathy (MDFT, MST, BSFT, FFT) | Preparing families for their own disengagement (MST) | Intrapersonal restructuring by telephone and strategic structural systems (BSFT) |
Therapist style and orientation
Therapist style and orientation factors that have been related to retention and engagement focus on the individual therapist’s interpersonal communication and interaction skills. Being able to listen to and reflect on a family’s thoughts, feelings and concerns, especially during the early stages of the intervention when participants and therapists need to build a good therapeutic alliance, have been outlined by all four selected intervention approaches. 25,26 In addition, instilling realistic hopes and providing pragmatic and proportionate reinforcement when progress is made and presenting oneself as an authentic individual by being honest and consistent are crucial aspects that develop family engagement and subsequently retention in the intervention. 27 Two further factors that have been highlighted by all four therapeutic approaches are a therapist’s ability to maintain and improve productive communication between family members and between the therapist and the family, and the universally named ability to show empathy. 27
Structural factors
A range of structural factors have been highlighted as fostering family engagement and retention. Being flexible with regard to the time of therapy sessions and places in which these sessions are held is embraced by approaches such as MDFT, MST and FFT. 21 It is suggested that sessions may be held in the family home, temporary accommodation and public places such as restaurants. MST and FFT manuals also indicate that flexibility with regard to the frequency of client contact is a crucial element of these interventions, which improves engagement and retention. 26 MST therapists are available 24/7, allowing for crisis management and greater assistance during times of heightened need within the family. 21 Being able to individualise services for families also plays a role in maintaining a family’s engagement as multiple and changing needs can be addressed in a timely manner, ensuring that families feel that an intervention addresses pressing issues relevant to them rather than following a strict plan that does not address their current concerns and problems. 21 Actively working towards a family’s engagement has also been cited as a means by which engagement and retention can be improved.
Similarly, Tuerk et al. 27 suggest that families need to consider their own potential disengagement from an early stage, allowing effective structures to be put in place to avoid the dropout of families from interventions. A therapist may be able to access some of the family’s supports, getting to know some other people in their social circle such as neighbours and friends, who the therapist could contact and ask for information should the family become less involved in the therapy at any point. Other approaches include ‘the foot in the door technique’ for initially resistant families, whereby the therapist seeks to engage such families through persistence in arranging meetings and offering short drop-in sessions to check up on families rather than longer more intense sessions. The idea here is that, once families have agreed to such a drop-in session, the likelihood of extending the visit and engaging with the family more intensely is increased. Tuerk et al. 27 also describe ‘going above and beyond’ by bringing food to meetings, for example, or by leaving food on the family’s doorstep. Bringing food may reduce the burden of purchasing and cooking meals for some families in which parents are very busy or economically unstable. In addition, this and other techniques and tools emphasise and reflect the therapist’s commitment and enthusiasm to work with a family. 27
Therapy orientation
Therapy orientation factors related to engagement and retention include focusing on strengths rather than weaknesses and setting goals, both of which aid the development of a successful therapeutic alliance. 28 A strong therapeutic alliance in turn has also been highlighted as a crucial factor for engagement and retention. By preparing families for, and guiding them through, criminal and educational proceedings (e.g. court hearings, meetings with schools), therapists are able to significantly reduce the parental burden, which is also thought to improve engagement and retention. 29 Specific therapeutic interventions directly aimed at increasing engagement by families have been put in place in BSFT. Here, strategic structural systems engagement procedures (joining, family pattern diagnosis and restructuring) are used to change those types of interactions that maintain a family’s resistance to engage with the intervention. 15,30 Joining involves keeping track of individual family members’ personal needs and goals, as well as of their specific agendas. It may also involve a discussion of the therapy’s focus on addressing these issues, thereby increasing the probability of attendance at the first meeting. Family pattern diagnosis involves the identification of maladaptive family interactions, which are linked to problems with engagement (and which may also perpetuate the substance use problems). Finally, restructuring involves the modification of the maladaptive family interactions through clinical tools such as reframing and shifting of alliances. 30
Additional factors
Additional factors including rewarding families for engagement and the use of social and mobile media have also shown promising results for engagement and retention in substance abuse programmes. In contrast, other factors such as long waiting times have been identified as possible barriers to treatment entry and engagement.
Branson et al. 31 investigated the efficacy of low-cost contingency management in a sample of substance abusing adolescents aged 12–17 years. Adolescents who attended on time were able to select a slip from a ‘fishbowl’ and to immediately exchange this slip for a prize. The prizes ranged from verbally delivered social reinforcements to large prizes worth £20, with the probability of drawing low-cost prizes being proportionally higher than the probability of drawing high-value prizes. Additionally, perfect attendance (attending all three sessions in 1 week) was associated with a bonus draw. Branson et al. 31 found that those adolescents who were in the contingency management condition showed higher levels of engagement with the intervention (indicated by the percentage of attended sessions) than their peers in the treatment as usual (TAU) control condition.
Waiting time is a potential barrier to treatment engagement in evidence-based treatments. Westin et al. 32 found that families who had to wait longer before starting an intervention were more likely to prematurely exit treatment. The same authors carried out post hoc analyses on their data, revealing that, although longer waiting times were related to a higher likelihood of treatment dropout in FFT, this was not true for MST. These findings indicate that individual treatment modalities are associated with different engagement strategies, which differentially moderate the relationship between waiting time and treatment engagement.
Finally, factors such as the use of social and mobile media may be useful when trying to engage and retain families. Therapists commonly contact individuals through Short Message Service (SMS or ‘texting’) to confirm appointments and to send reminders about upcoming sessions. Although other forms of communication through social media websites such as Facebook (Facebook, Inc., Menlo Park, CA, USA) or Twitter (Twitter, Inc., San Francisco, CA, USA) may be possible, it remains unclear how data protection and confidentiality issues could be dealt with. Nevertheless, these areas will prove interesting for future research into successful engagement and retention techniques.
Barriers to implementation in the UK
In terms of translating research into practice, specialist training is needed for family interventions, which can be an obstacle to their implementation. 33 Public Health England statistics suggest that < 1% of interventions with the under-18s consisted of ‘family work’. 1 The large majority of young people with substance misuse problems receive psychosocial or harm reduction interventions that focus on the individual user and do not engage family members. Likewise, a survey conducted in the UK with services for adult family members showed that even those family interventions recommended by the National Institute for Health and Care Excellence (NICE),34 such as behavioural couples therapy,35 are rarely implemented in services. 36 It should also be noted that some of the components and techniques described above and in Table 1 assume a level of resources – and a level of assertiveness – that may not be achievable or acceptable in a UK context. Finally, there are problems with defining ‘the family’, a contested concept that carries implications for the delivery of family interventions. 37 Young people with substance use problems frequently come from disrupted families and may be looked after by single parents, grandparents, other relations or the state (e.g. Lloyd7 and Boys et al. 38). Traditional, systemic family approaches may be difficult to deliver in such situations.
In summary, the research evidence shows that there is a high prevalence of substance use among young people in the UK. Early onset and high levels of use are associated with a range of negative outcomes, including increased risk of later problematic use and dependence. A growing body of research has identified family interventions to be effective at treating young people’s substance use problems and a range of techniques has been identified to encourage engagement and retention. However, despite this evidence, take-up of family-based approaches, at least in the UK, has been low. A key factor appears to be the resource-intensive nature of many family interventions, making them difficult to implement and deliver in many service settings, especially in the context of funding cuts to drug and alcohol services for young people. 39 Another potential barrier may be the cultural adaptation of approaches developed in the USA to a UK setting. There is a growing awareness of the need to adapt evidence-based treatments to different cultural groups and settings to ensure successful implementation. 40–42 Finally, it should be noted that a key distinguishing feature of drug treatment with young people is the coercive context in which it frequently takes place. This may encourage physical attendance but does not necessarily encourage therapeutic engagement.
Social behaviour and network therapy
Social behaviour and network therapy is an intervention developed in the UK that has been shown to be effective with harmful drinkers43 and is recommended in recent NICE guidance. 44 The original SBNT intervention was developed and tested as part of the UK Alcohol Treatment Trial (UKATT) conducted in UK alcohol treatment services. 43 It was later developed further for use with people with other drug problems. The conceptual underpinning of the approach is the positive influence of social as well as more addiction-specific (or abstinence-related) support on the improvement and eventual resolution of addictive behaviour. General social support, alcohol-specific social support and the drinking behaviour of the social network of alcohol users, for example, have all been shown to be unique predictors of positive alcohol treatment outcomes (for examples see Beattie et al. ,45 Havassy et al. ,46 Longabaugh et al. ,47 McCrady,48 Wasserman et al. 49 and Mohr et al. 50). SBNT brings together elements of network therapy,51 social aspects of the community reinforcement approach (e.g. Meyers et al. 52), relapse prevention (e.g. Chaney et al. 53) and approaches with family and concerned others (e.g. Copello et al. 10).
Utilising cognitive and behavioural strategies, SBNT helps clients to develop family and social networks that are supportive of change. A key strength of the approach is the primary focus on addressing drug and alcohol problems by engaging with a network of positive support for lifestyle change. SBNT has additional advantages to help sustain engagement with vulnerable young people, who may be disconnected from their families, by broadening the reach of the intervention beyond the traditional family to include supportive peers. Core strategies such as motivational techniques, improving communication and coping mechanisms are used, as well as (given the nature of substance misuse) developing a network-based relapse management plan. Using such a therapeutic approach also provides scope to address client-focused elective areas such as educational requirements. 54
Involving young people in research
Involving those who are the focus of research can have a positive impact on what is researched, how research is conducted and the impact of research findings (e.g. Brett et al. 55 and Staley56). In recent years there has been increasing interest in children and young people’s involvement in research,57–60 both as sources of data and through their active involvement in the planning and process of research. Although there is less of an evidence base in relation to children and young people’s involvement in research compared with the involvement of adults, the case for this involvement has been explored in a number of publications. 57,61,62 Research that actively involves children and young people should lead to research, and ultimately services, that better reflect their priorities and concerns63,64 and enhance the opportunity for optimal health outcomes. 65 However, the voices of children and young people who are less frequently heard, for example users of mental health services66,67 and looked-after children,59 are often absent from the literature on children and young people’s involvement in health and social care research.
As well as being located within the wider traditions of public involvement in research, young people’s involvement in this study was also developed with reference to children and young people’s involvement in the development and delivery of health and social care services. 64,68,69 Article 12 of the United Nations Convention on the Rights of the Child70 states that all children have the right to express their views in all matters that affect them, and this applies to children’s involvement in both decisions about their own experience as patients and service users and the development of health services and research. 68 In addition to drawing on previous work by the research team and other published studies, the Y-SBNT study sought from the outset to actively involve young people with experience of substance misuse services throughout the study. Young people’s involvement in the study was key to ensuring that the research addressed the concerns and issues faced by young people with substance misuse problems and we hope that this will also be an important addition to the wider evidence bases on public involvement and young people’s involvement in research.
Believing that SBNT could be successfully adapted to the youth context and would have great potential as a clinically effective and cost-effective intervention that could be readily and widely implemented in services for young people, the research team adapted the current SBNT approach to produce a purpose-designed therapy manual and resource kit. The feasibility of recruiting young people to receive this specifically developed family- and network-based intervention was then investigated in a feasibility study to establish the acceptability of the intervention to young people, their therapists and network members.
Research objectives
Intervention development phase
-
To adapt an evidence-based family and social network intervention developed and tested with adult substance misusers to the youth context.
-
To undertake a review of the evaluation and implementation literature to inform this adaptation.
-
To involve young people, parents and therapists in the adaptation process to improve acceptability to these groups and ensure ready implementation in routine services.
-
To develop a manual, resource kit and training programme for the delivery of the adapted intervention in a feasibility trial.
Feasibility randomised controlled trial phase
-
To demonstrate the feasibility of recruiting young people to a family- and network-based intervention (Y-SBNT) across two service sites.
-
To test the feasibility of training staff from existing young people’s addiction services to deliver the family and social network intervention.
-
To evaluate the level of treatment retention among participants randomised to the family and social network intervention.
-
To explore through qualitative interviews the participants’ views, acceptability and experiences of the intervention and the study process.
-
To explore through qualitative interviews the views and experiences of those attending treatment sessions as members of the young person’s network and whether the intervention was acceptable.
-
To establish treatment effectiveness through 3- and 12-month quantitative outcome data.
-
To explore cost-effectiveness in preparation for a large definitive randomised controlled trial.
-
To explore and develop models of public involvement that support the involvement of young people in a study of this nature.
Chapter 2 Intervention adaptation
The overall aim of the intervention adaptation phase was to adapt the original evidence-based family and social network intervention (SBNT) developed and tested with adult substance misusers to the youth context. The related tasks were to:
-
undertake a review of the evaluation and implementation research literature on family interventions for young people with substance misuse problems
-
involve young people, parents and therapists in the adaptation process to improve acceptability to these groups and ensure ready implementation in routine services
-
adapt the manual and develop any necessary additional materials to support a training programme for the delivery and ongoing monitoring of the adapted intervention in a feasibility trial.
To achieve the aim and tasks, the published manual for SBNT in adults,54 which was tested in the UKATT and subsequent studies with drug users (e.g. Copello et al. 71 and Day et al. 72), provided a platform for the adaptation work. The output of this phase was the development of an intervention that could be delivered to young people (aged 12–18 years) with substance use problems within the context of existing UK services. The work undertaken is described in the following sections, followed by a description of the adaptations made to the final intervention used in the pilot.
Review of the family-based substance misuse intervention evaluation and implementation literature
The first step in the adaptation process involved undertaking a systematic review of reviews of family interventions in young people with drug and alcohol problems (Carmel Bennett, unpublished review), described in the previous chapter. The search strategy used is provided in Appendix 1. This review highlighted that a number of family-focused interventions have been shown to be effective in young people with substance misuse problems and a number of intervention components are conducive to increased engagement and retention. These factors were illustrated previously in Table 1 and included therapist style and orientation, structural factors, therapy orientation and additional factors. Each of the components identified was considered with respect to the adaptation process. Some were already part of the social and family approach, for example flexibility, goal setting and productive communication. Others were considered carefully and discussed but, for pragmatic and resource reasons, were not incorporated, for example contingency management strategies. All of these components were explored as part of therapist training and a brief description of each was included in the revised set of materials to supplement the training manual.
Involvement of/consultation with young people, family members and therapists in the adaptation process
The study sought to actively involve young people with experience of substance misuse services from the outset, to ensure that the intervention was relevant to, and addressed the issues faced by, young people in treatment. Public involvement activity during the development of the intervention therefore focused on ensuring that the treatment was acceptable and relevant to the study’s target group and reflected the views of service users and their families. In addition, the views of therapists were sought within this early phase and process.
Young people with experience of services
Involvement of young people was based on a series of young advisor and consultation meetings (see Chapter 8 and Appendix 2). During these meetings, the two public involvement leads and other members of the study team worked with young people to explore the principles behind the intervention (i.e. social networks, social support, engaging with services) as well as to obtain young people’s input/comments on the content and components of the intervention itself. The core principles and aspects of the Y-SBNT approach were retained, as the young advisors considered these to be relevant to their experience, but they also suggested adaptations to aspects of the approach and associated materials to make them more relevant to young people.
Activities undertaken with young people in relation to the content of the intervention included considering the nature of social networks and how these may differ between young people and adults using substance misuse services, such as thinking about the important people in young people’s lives and why they might be helpful/supportive or unhelpful/unsupportive (examples in Box 1).
-
Supportive GPs willing to suggest helpful ideas.
-
Supportive family members who understand, willing to help.
-
Getting involved in work, college, voluntary work, etc., with new friends, activities, etc.
-
Different types of help from different therapists regarding different issues.
-
Supportive partner.
-
Friends with the same problems and willingness to seek help.
-
A really helpful key worker who has looked at me as an individual and helped me to change my life.
-
Friends who do not use.
-
Supportive and educated hostel staff.
-
Family members who know about the issue but who do not take an active part in your use.
-
Other users in group sessions or work, etc. They can suggest going outside to use.
-
Fellow family users – because they might not want to stop and you do.
-
Friends who are going through the same problems as you but who are not willing to stop.
-
Therapists who are disinterested or not helping, just there!
-
A friend who is staying with me and smoking cannabis in my house when I am trying to quit.
Examples of young people’s input into the development of the youth social behaviour and network therapy intervention
Structured discussions with young advisors generated materials used in the adapted intervention training resources, including examples from the young people in terms of processes perceived as important to obtain social network support; good and unhelpful aspects of services; and examples of social network diagrams from young people (later used to develop examples in the revised training materials). Some examples are included below and in Appendix 3.
-
Exploring the components of the original adult SBNT intervention and asking the young people to reflect on how these may or may not be relevant to young people (examples in Table 2).
-
Exploring what young people find helpful or what the barriers are to engaging with substance misuse services.
-
Using an exercise that involved writing an open letter to an important person about what it is like to have a problem with alcohol or drugs and how the young person would like that important person to help and support them. Excerpts from these letters were subsequently used (with permission) in the intervention training materials given to staff in the pilot services. Extracts from an open letter can be seen in Box 2 and Appendix 3.
| Component | What young people wrote |
|---|---|
| That I spend less time with those who are not helpful or encourage drug and alcohol use | Although it’s hard to cut off your friends completely, it was important to try and stay away from friends who use. Most of my friends used drugs so it can also isolate people. Solution: going to groups with YP who want to change their drug use. Time away from drug users/stressful situations |
| That we communicate well and openly and we solved problems together | Everyone involved needs to remain involved, and in contact with everyone else, and needs to be on the same page as everyone else to ensure the correct support is given. Consistency is importantTrust is important, if you can trust people you can be honest about the problems you are facing. All services working with the person need to stay in contact and also keep the person they’re working with included in decisions/stuff that affects them |
| We all have positive views of the value of supporting each other | It’s nice to help people and be able to make a change to someone’s life. I think it’s important people can see the value of supporting each other and the benefits the person they are supporting will get – there needs to be advice/support for the person helping the YP with an issue |
| We all have the same understanding of the problem | We all have our own thoughts on drugs/alcohol but we all need the understanding what’s best for the young person |
| That we all know specifically what we are doing to support each other | All people involved need to be clear on what is going to help the personAll understand and know their role and involvement in the support of a young person, and how to communicate with each other |
| That I manage to get over barriers that get in the way of getting support from others – young people identified trust as a barrier | It is important you can trust them, you need to be reassured as many YPs may have been through many services, been let down by family/friends and have trust issuesSome young people aren’t close to parents or other support that may be very beneficial to them and maybe the first stage is to build relationships |
| That I know how to ask and to give emotional, practical and social support | It’s important to know where to get support/ask for advice and after sorting your own stuff out, be able to support and help others through their issuesSupport also needs to be offered as much as possible as some people will just not ask for support or just support on some topics/problems |
| That those who support me have support themselves | Some people that are supporting young people may need support themselves. Example: a parent may want to support their child but may be a user themselves and may need/have an adult service to support them |
| That I spend time doing fun things with positive friends and family members | It is important to have fun, have a hobby that you can enjoy with friends/family. Mediation may be needed to get to this pointIt is good to have fun with friends and family away from all the ‘crap’Everything costs money! Have a list of open days and free activities for families to do for fun |
You’ve supported me through many dark times and I can see that you care deeply for me (as I, you). However, your lack of experience with drugs completely dominates your treatment of me and I want you to know that it’s not helping me. You’re a caring, strong and loyal person, but you seem to think I am oblivious to the dangers surrounding drugs and that’s simply not true.
. . . Maybe instead of judging me, you could have come with me to my drug counselling. Instead of making a formal complaint about my social worker because she knew and didn’t tell you, you could have recognised that she could see I was responsible and mature . . . .
There are a number of ways you could have handled the situation in a much more helpful and supportive way. Don’t ban me from smoking weed entirely, straight away. Talk to me about the feelings that make me want to be stoned all day and work with me to identify replacement activities, or distractions . . . perhaps an incentive would have helped. Something small but worth it, to keep me going when all I want is a joint, and to show me that you recognise how hard I’ve worked when I cut down.
The identification of potential network support that was wider than the biological family and included peers and support workers was seen as very important. This was particularly relevant for the target group of young people, who in some instances experienced fragmented family networks and family breakdown and who had contacts with a range of services that were experienced as significant and important sources of support to them. A range of ways of drawing social network diagrams was also suggested including more use of colours and drawings if the young person preferred this way of representing networks. Some of these methods of generating social networks were also later explored with therapists during the initial pilot casework with young people.
The challenges in developing an intervention based on the idea of bringing others into the therapy sessions led to important discussions, as many young advisors were unsure about this aspect. We therefore explored with them how best to develop and deliver a network-centred intervention with young people who do not want others in their sessions. In addition, the clear and sensitive way in which the notion of developing social support from others was introduced to young people at the beginning of the intervention was seen as highly important.
Finally, the notion of treatment goals was discussed and young people felt that it was important to identify goals in a wide number of areas, not only substance use. Young people recognised that it was not always the case that those entering services perceived their substance use problem as something that they wanted to change straight away, despite possibly being aware of the difficulties and problems that it was creating in their lives. The broadening of goals to include other aspects that may have contributed to their problem was seen as important during public involvement. This was seen as a vehicle to maximise early engagement with some young people. A goal-setting diagram to be used within sessions was therefore adapted with active advice from the young people, who suggested the domains that were later included in the identification of the goals resource handout. The following domains were used: drug or alcohol use, family relationships, friends and other important people, living arrangements, problems with the law and ‘other’ areas identified by the young person.
Family/network members
The involvement of family members as part of this adaptation phase consisted of a focus group discussion with two adults (woman with foster daughter and mother with adopted son). The discussions highlighted the challenges faced by these two women that would influence both their engagement and that of the young people in something like Y-SBNT. The participants felt that, to some extent, social network support was already in existence for young people, although it was not always positive as some contacts promoted continued substance use behaviour. They identified communication between themselves and the young person to be ‘poor’ and that the intervention may help with this aspect. However, they felt that the work would depend on the extent to which the young person was ready to engage, for example ‘I just feel that mine would only engage as much as she wanted to engage . . . she would only share what she wanted to share’, and being able to be open and honest about their substance use was perceived to be central, for example ‘I don’t think she’s ready or in the frame of mind where she could open up to a different network’. The theme of ‘honesty’ from the young person was prominent in the discussions. Both participants felt that they would ‘definitely’ get involved in an intervention such as Y-SBNT if invited and would find the ‘opportunity to talk to the young person helpful and useful . . . if you are hearing it from a user’s point of view I can understand it a bit more’. One of the participants stated that involvement in sessions may help her as a mother to have more ‘tolerance and understanding’ as it was not something she had been brought up with or understood. Also, the idea of working together and supporting the young person was discussed; for example, ‘it would be the unison of it, both of us working towards a common goal which we’ve both got an understanding of’. Therefore, in summary, the two participants felt that the intervention was feasible and acceptable. There were some perceived potential benefits of the intervention including the potential for better and more open communication, increased understanding and supporting agreed goals. Potential challenges were identified in terms of the young person being ready to be ‘open and honest’ about their difficulties and being able to discuss them with potentially supportive people.
Therapists
Consultation was conducted with seven therapists as an early part of the training workshops. In addition, therapists were interviewed at the end of the study (see Chapter 6) when their experiences of intervention delivery were explored in more detail using one small group interview (two therapists) and individual interviews.
As part of the adaptation work, an early session with therapists involved providing them with a detailed description of the intervention including some of the additional materials developed following the work with young people described earlier in this chapter. This was followed by a discussion about the feasibility of delivering the intervention in their services as well as their views on its acceptability to young people. The components (core and elective sessions) of the intervention presented in Box 3 were discussed one at a time. These were perceived as appropriate by therapists and contrasted to routine practice. Some of the strategies, for example talking to teachers, hostel workers or other important people as part as the development of network support, were said by the therapists to be performed occasionally in routine work with young people. But the perception was that the structure of the Y-SBNT intervention and the coherent focus on positive help and support made it easier to deliver it in a more planned, consistent and coherent way.
-
Communication.
-
Coping.
-
Enhancing social support networks.
-
Developing a network-based relapse management plan.
-
Basic education on drugs/alcohol.
-
Increasing pleasant activities.
-
Employment.
-
Minimising support for drug/alcohol use.
-
Active development of positive support.
The overall feedback stressed that more emphasis was needed on the different experiences and social contexts of young people but that there was no need to change the structure or content of the psychological components and strategies of the original SBNT intervention. An additional map/framework of the intervention journey (illustrated in Figure 1) was produced and included with the revised materials.
FIGURE 1.
The treatment map.

The adapted youth social behaviour and network therapy intervention
The final intervention, termed Y-SBNT, retained the original structure, timings and components of the adult version. The revised treatment map guided therapists through the clinical delivery and decision-making process. As in the original approach, there was a blend of structure yet an element of flexibility that allowed clinician decision-making in terms of what topics to deliver for each particular case. As far as it was possible at this stage, additional case materials were produced based on cases involving young people, although more materials and examples became available as the feasibility pilot progressed and could potentially inform further adaptation work.
Following adaptation work, a decision was made, which was discussed with the project Trial Steering Committee (TSC), to retain the original SBNT manual as part of the set of training materials rather than rewriting large sections that needed minimal change but to supplement this with an additional shorter manual that made reference to relevant sections of the original manual when appropriate. Additional resources in the form of treatment maps for young people were also produced. The final revised sections included (1) new examples of social network diagrams based on young people, (2) a revised treatment journey map outlining the various stages of the intervention and (3) broadening of goal setting to include a range of areas and production of a new resource handout. In addition, further resources were produced as handouts to support the therapists’ work for some of the core topics including communication and coping.
The final set of resources given to all therapists as part of training and ongoing supervision for the pilot study were:
-
the original published SBNT manual54
-
the Y-SBNT brief companion manual, including a summary of the evidence on family interventions with young people with substance misuse problems, the intervention aims and philosophy and the revised/adapted materials.
Summary
In summary, the stages of adaptation undertaken led to the conclusion that the intervention was adaptable to use with younger people. This was reported by all three stakeholder groups including young people with experience of substance misuse treatment, family members and therapists. There were areas where the materials needed to be changed to reflect the realities of the younger population, in particular the potential different composition of social networks and the identification of broader goals beyond substance use. In addition, the introduction of the intervention to young people in terms of developing support from others (family and wider networks) had to be tackled sensitively and explained clearly, with the value of support emphasised as well as the fact that young people were always in control of who to engage when/if seeking support. There were some strengths and limitations of this work phase. The stakeholder consultation element was a strength but some of the challenges in involving young people and family members were evident and are discussed in more detail in Chapter 8 as part of the proposed development of models of public involvement of young people in a study of this nature.
Chapter 3 Feasibility trial methods
This chapter is based on the study protocol, which has been previously published (© Watson et al. ; licensee BioMed Central. 2015). 73 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Trial design
The adapted Y-SBNT intervention trial was a pragmatic, two-armed, randomised controlled open feasibility trial with equal randomisation delivered in two young people’s services. Young people aged 12–18 years, newly referred and accepted for structured interventions for drug and/or alcohol problems and who consented to participate, were randomised (1 : 1) to receive either:
-
Y-SBNT – an adaptation of SBNT developed during the early phases of the project, consisting of social network identification, goal setting, improving communication and coping mechanisms and, when relevant, developing a network-based relapse management plan, with an initial appointment followed by five further sessions over a maximum of 12 weeks (aiming for one per week when possible) or
-
TAU – usual care delivered by the two services with appointments offered as required.
Sample size
Treatment service outcome data collected in the 6 months prior to the commencement of the trial showed that one of the participating services received approximately 45 new referrals per month, with a caseload of > 200 clients. The second service was accessed by approximately 280 young people in the previous year.
As a feasibility study, the main purpose here was to assess the acceptability and feasibility of, and to obtain information that would inform the design of, a larger full-scale trial. A sample size calculation was used so that the feasibility study could rule out the likelihood of an effect smaller than that desired being observed in the main trial. 74
For the main trial we would want to detect an effect size of magnitude 0.3 of a standard deviation (SD) between the two groups in the primary outcome, which would require a sample size of approximately 350 patients. Cocks and Torgerson74 estimate that feasibility trials should have at least 9% of the sample size of the main future trial. They suggest that a sample size for a pilot trial should be a sufficient size such that, if the observed difference between the two groups in the pilot trial is zero, then the upper confidence limit of an 80% one-sided confidence interval (CI) will exclude the estimate that is considered ‘clinically significant’ in the planned definitive trial. A sample size of 32 patients was required to exclude an effect size of 0.3 in the event of a zero or negative intervention effect (using a one-sided 80% CI). Unless there was a clear explanation, we considered that there was poor justification for moving towards a fully powered trial if the upper 80% confidence limit of the effect size for the main clinical outcome was < 0.3 as it would be unlikely that an effect size of ≥ 0.3 would be found in a main trial. If there was a positive intervention effect in the pilot study, we would conclude that the main trial was worthwhile, as long as adequate recruitment and an adequate follow-up rate were observed.
Allowing for the reasonably high level of attrition that was expected in this patient population, it was felt that 60 participants needed to be recruited to the trial to achieve the required 32 patients with outcome data.
Approvals obtained
West Midlands – Coventry and Warwickshire Research Ethics Committee approved the study on 24 February 2014 (reference number 14/WM/0021). Local research and development (R&D) approval was obtained as well as agreement to participate from the relevant services. The trial was assigned the International Standard Randomised Controlled Trial number ISRCTN93446265 and the UK Clinical Research Network ID 16111.
Trial sites
The study was conducted in two young people’s services in England based on existing professional relationships and for pragmatic reasons:
-
West Midlands A tier 3 service providing information, advice and treatment for issues related to the use of drugs, alcohol and other substances for people aged ≤ 18 years. The service consisted of a multidisciplinary team including therapists from various backgrounds supported by psychiatry and nursing staff, offering individual and group services to young people with substance misuse problems and complex needs.
-
North East A specialist service that links with a number of tier 2 generic youth services and with other primary care services, such as general practitioners (GPs) and school nurses. There were therapists from various backgrounds such as social work, third sector, primary care and offender management, with considerable experience in addictions and youth development. This service was for those aged ≤ 18 years, with a mean age of service users of 15/16 years.
Participant eligibility
Inclusion criteria
Young people were considered potentially eligible if they met all of the following criteria:
-
were aged 12–18 years inclusive
-
had drug and/or alcohol problems and were newly referred and accepted for treatment by one of the two agencies during the period of recruitment
-
were willing and able to provide written informed consent.
Exclusion criteria
Young people were excluded if they met any of the following criteria:
-
had a concurrent severe mental illness that precluded them from active participation
-
suffered from severe mental or physical illness likely to preclude active participation in treatment or follow-up
-
were unable or unwilling to provide written informed consent.
Recruitment into the trial
All young people newly referred to the two treatment services during the recruitment period were considered potential participants.
Eligibility assessment
All referred young people initially took part in an assessment session (routine part of the service referral and assessment processes) at the treatment agency, at home or at the usual place of treatment. Before conducting the assessment, a competency test based on the Gillick test was routinely administered to ensure that the young person was ‘competent’ to understand the implications of treatment as well as provide independent and valid consent. This UK assessment refers to a legal case that looked specifically at whether doctors should be able to give contraceptive advice or treatment to those aged < 16 years without parental consent. 75 Since then, it has been more widely used to help assess whether a child aged < 16 years has the capacity to consent to treatment without parental or guardian consent. Those found to be appropriately referred and meeting the inclusion criteria were deemed potentially eligible for the trial. Eligible young people who did not wish to take part (i.e. unwilling to give consent) and those found to be ineligible went on to receive usual care from the service outside of the trial. When proffered, reasons for non-participation were collected to inform future studies. Eligible young people and their parents/person with parental responsibility were given a leaflet (see Appendix 4) and patient information sheet (see Appendix 5) by the assessment staff. If the young person remained interested in taking part in the trial after reading the materials, a face-to-face meeting was conducted by a researcher allocated to the centre.
Consent procedure
During the meeting with those eligible and interested in participating, the researcher fully explained the study and provided an opportunity for the young person to ask questions.
The research process was conducted in a manner that ensured that informed decisions were made by the young person and his or her parents/person with parental responsibility. This included bearing in mind that competence is not related to age in a simple way but depends on a child’s ability to understand, weigh the options and reach an informed decision. 76
As the research in question was integral to the service that the young person was already involved in, and the parents or person with parental responsibility would have already given consent for the young person to attend that service, it was not deemed necessary to additionally obtain consent from the parents/person with parental responsibility for the child to participate in this study. This was in line with National Children’s Bureau (NCB) guidelines. 60 Conversely, there may have been situations when, given the nature of the service, seeking parental consent would have potentially breached the young person’s right to confidentiality if he or she was attending the service without his or her parent’s knowledge. NCB guidelines state that in such situations parental/person with parental responsibility consent may be waived. 60
For the purpose of this study, the following was applied.
-
If consent was not forthcoming from a parent/person with parental responsibility, but the young person (aged 12–15 years) did consent, he or she entered the trial.
-
For those aged ≥ 16 years, consent was sought only from the young person, as those aged between 16 and 18 years were presumed to be competent to give consent.
-
If consent was given by a parent/person with parental responsibility but the young person did not consent, the young person did not enter the trial.
However, the potentially complex lives of the young people were considered and consent in all cases was handled in a sensitive and pragmatic manner.
Baseline assessment
After written informed consent had been obtained (see Appendix 5), baseline data were collected by the researcher. The following data were collected in the baseline questionnaire (see Appendix 6) prior to randomisation:
Demographics
Details including age, sex, sexual identity (if aged ≥ 16 years), ethnicity, nationality, religion, education, employment and current living arrangements were collected.
Timeline Follow-Back interview
The Timeline Follow-Back (TLFB) interview77 records substance use, particularly the proportion of days on which the main problem substance was used in the preceding 90-day period. This interview is based on a retrospective calendar review of each day’s consumption and has previously been validated and widely used with adolescent populations. 78–80 It has been shown to demonstrate high comparability with the Global Appraisal of Individual Needs (GAIN) (r = 0.7–0.8) in a population of adolescents aged 12–18 years admitted to a residential treatment programme for substance abuse or dependence. 78 Applying the TLFB interview allowed the collection of detailed data on the full range of licit and illicit drugs used by participants. Participants were asked to recall on which days they had used their primary problem substance in the last 90 days. The number of days was summed and divided by 90 to obtain the proportion (from 0 to 1).
Strengths and Difficulties Questionnaire
The self-report Strengths and Difficulties Questionnaire (SDQ) is a brief behavioural screening questionnaire designed to be completed by adolescents. 81,82 The 25-item questionnaire has five separate subscales for different aspects of problems or behaviours: emotional problems, conduct/behaviour problems, inattention/hyperactivity, relationships with peers and prosocial behaviour. Scores for the first four scales can be added together to produce a score for total difficulties ranging from 0 to 40, with a lower score indicating greater emotional well-being and a score of ≥ 20 indicating an ‘abnormal’ score. The SDQ has been used extensively and has demonstrated high levels of reliability and validity. 83,84 In a factor analysis with 3983 11- to 15-year-olds, all 25 items loaded on the predicted factors relating to the five subscales (> |0.33|). 84 A few items also loaded on additional factors > 0.30, but the loadings on the predicted factors were higher than the loadings on the additional factors for all but one item. The total SDQ score demonstrated good reliability with a Cronbach’s alpha coefficient of 0.80 and test–retest reliability of no less than 0.62.
Important People Drug and Alcohol interview
Given the emphasis on family and peer support of the intervention, social network support was measured using the Important People Drug and Alcohol (IPDA) interview85 to understand the influence of social support on treatment for substance misuse, assess the degree to which social network changes had been achieved and assess the extent to which these changes still needed to be made. This interview requires the participant to provide information on up to 12 significant people who have featured in their lives in the previous 3 months. Data collected on these people include their relationship with the young person, frequency of contact, importance, supportiveness and use of drugs and alcohol. This instrument has a three-factor structure of substance involvement (α = 0.92), general/treatment support (α = 0.84) and support for substance use (α = 0.85),85 established in an adult population.
Family Environment Scale: Family Relationships Index
The 27-item relationship dimension of the Family Environment Scale (FES)86 consists of cohesion, expressiveness and conflict subscales (nine items each), for which a raw score from 0 to 9 can be calculated and converted to a standard score. 87 The standard scores range from 4 to 65 for the cohesion subscale, from 16 to 71 for the expressiveness subscale and from 33 to 80 for the conflict subscale; a higher standard score indicates greater cohesion and expressiveness and lower levels of conflict among family members, respectively.
The Family Relationships Index (FRI) is designed to look at the atmosphere in the family household with subscales that measure support, expression of opinions and angry conflict within a family. This was completed by the young person (other family members were not asked to complete this instrument). This measure has been used previously in similar populations88,89 and has undergone extensive development and validation work. It has shown acceptable levels of internal consistency in a validation study with 1298 pupils aged 11–18 years from 16 schools in Victoria, Australia (Cronbach’s alpha of 0.39 for the expressiveness scale, 0.67 for the cohesion scale and 0.72 for the conflict scale),90 test–retest reliability of each subscale of at least 0.73 and good content and construct validity. 91
Health-related quality of life
The EuroQol-5 Dimensions five-level version (EQ-5D-5L)92 is a standardised measure of health status developed by the EuroQol Group to provide a simple, generic measure of health for clinical and economic appraisal, with health characterised on five dimensions (mobility, self-care, ability to undertake usual activities, pain and anxiety/depression). Participants were asked to describe their level of health on each dimension using one of five levels: no problems, slight problems, moderate problems, severe problems or extreme problems. 93 These dimensions were accompanied by a visual analogue scale (VAS), with participants asked to assign a number between 0 and 100 to measure their perceived health status.
Health and social care resource use
The feasibility of collecting details regarding hospital and primary health-care services use, contact with the police and criminal justice system and social care services use was tested in this participant group. Participants indicated how many times in the previous 12 months they had seen a GP or practice nurse or received hospital care. They were asked about any accidents that they may have had in the past 12 months and attendance and absenteeism from school or employment was recorded. In addition, contact with the police, criminal justice system and social services was documented.
This collection of self-reported resource use data was continued until participants had been in the study for 12 months or until they withdrew from follow-up or fully withdrew from the study.
Randomisation
Participants were randomised equally between the two trial arms: the Y-SBNT intervention and TAU. Randomisation was carried out using random permuted blocks, stratified by centre. To maintain allocation concealment, the generation of the randomisation sequence was undertaken by an independent statistician at the University of York and treatment allocation was performed by a secure, remote, telephone randomisation service based at the University of York. The computerised randomisation system was checked periodically during the trial following standard operating procedures. Because of the nature of the intervention, it was not possible to conceal treatment allocation from the participants or the professionals delivering the intervention.
Trial interventions
Participants were randomised to receive either Y-SBNT or TAU.
-
Y-SBNT An adaptation of SBNT consisting of social network identification, goal setting, improving communication and coping skills and, when relevant, development of a network-based relapse management plan delivered by a trained therapist as an initial appointment and followed by five further sessions over a maximum of 12 weeks (aiming for one per week where possible).
-
TAU Generally focused on engagement, description of substance use, current issues that the young person brings to sessions and that seem relevant to the substance use and practical matters such as housing or school exclusion. It generally does not involve analysis of comorbidity, discussion with family or multiagency work. Those allocated to TAU had an initial appointment with a therapist not trained in the Y-SBNT, with further appointments as required.
After allocation, participants were provided with an appointment to see the therapist appropriate to their allocation.
Training in the delivery of youth social behaviour and network therapy
Training was delivered by two professionals during two workshops in each site – West Midlands and the North East. Volunteers from the therapists’ pool in each of the two services were trained to deliver the Y-SBNT intervention (five in the West Midlands and two in the North East). Once allocated, therapists delivered Y-SBNT to participants only for the duration of the trial, with the non-trained therapists in each service delivering TAU within the other arm; hence, there was no overlap between therapists across the two trial arms.
The training took place from 0930 to 1500 on each day. After the first day, trainees conducted practice cases in their respective services before coming back to training approximately a month later for the second day when this work was reviewed.
As soon as recruitment commenced and throughout the trial period when treatment was delivered, the Y-SBNT therapists in each site received group supervision twice a month for 1 hour each time. In the West Midlands, supervision was face-to-face whereas in the North East it was delivered over the telephone. Most of the supervisions were delivered by one of the group trainers, with a couple of supervisions delivered jointly by both trainers. The group supervision sessions focused on discussion of each individual case that therapists were working with.
At one meeting during the trial all Y-SBNT therapists came together in the West Midlands for an afternoon supervision session. This was delivered by both trainers.
Supervision finished once the last client was seen within the Y-SBNT arm.
An early additional session was provided by the researchers covering protocol issues and research processes including the rationale for the study, patient eligibility, the randomisation process, study paperwork completion, digital recorder use and handling of participant withdrawal.
Intervention content
Youth social behaviour and network therapy arm
Youth social behaviour and network therapy is an adaptation of adult SBNT developed during phase 1 of the study and described in Chapter 2. The intervention was delivered by a trained therapist. The developed therapy consisted of social network identification, goal setting, improving communication and coping mechanisms and developing a network-based relapse management plan. This therapeutic approach also provided the scope to address client-focused elective areas, for example educational requirements. An initial appointment was followed by five further sessions within a maximum of 12 weeks (aiming for one session per week when possible).
Treatment as usual arm
Those participants randomised to receive TAU continued to receive the usual care delivered by the service that they were referred to. After triage, participants allocated to TAU were seen for an initial appointment with one of the therapists in the team not trained in Y-SBNT, with further appointments made as required.
Participant follow-up
Appendix 7 shows a summary of the Y-SBNT trial and the timing of follow-ups.
Trial completion
Participants were deemed to have completed the trial when their final follow-up had been completed.
Participants were deemed to have fully withdrawn from the trial when:
-
they wished to exit the trial fully
-
their therapist withdrew them fully from the trial.
Instead of withdrawing fully from the trial, participants had the option of:
-
withdrawing only from receiving trial treatment but continuing to complete follow-up data collection
-
withdrawing only from follow-up data collection but continuing to receive trial treatment.
Participants electing to withdraw from both the trial treatment and the follow-up data collection were deemed to be full withdrawals.
Measurement and verification of the primary outcome
In conjunction with the qualitative data, the primary outcome of the trial was the feasibility of recruiting young people to a family- and network-based intervention across two service sites and the potential for a future large-scale study. This feasibility was measured by:
-
recruitment rates – a quantitative assessment of the acceptability of the research was carried out using numbers referred, numbers eligible and those agreeing to participate
-
retention in treatment – evaluated by the number of sessions attended as a measure of acceptability of the intervention to participants
-
follow-up completion rates – a quantitative assessment of the number of follow-up interviews completed
-
outcome assessment – the following outcome measures were also collected at 3 and 12 months post randomisation (see Appendix 6):
-
TLFB interview
-
SDQ
-
IPDA interview
-
FES
-
health-related quality of life (HRQoL)
-
a resource use questionnaire.
-
In addition, the following data were collected.
-
Qualitative interviews The acceptability of the Y-SBNT intervention to the young people and the wider context of the impact of the intervention were explored through semistructured qualitative interviews conducted at 3 months post randomisation. In addition, the acceptability of the intervention to those attending as network members was explored through similar semistructured interviews at 3 months post randomisation. Interviews were also conducted with the therapists and a service manager at a single time point following the completion of the interviews with young people. There were separate topic guides for each participant group (see Appendix 8), exploring their experiences and the acceptability of the active components of the new approach and study processes.
-
Working Alliance Inventory (WAI)94 The WAI was to be administered at the end of treatment sessions 1 and 3 to the young people and also to the therapists delivering the intervention and TAU (see Appendix 6). The questionnaire measures the perceived strength of the working alliance between therapists and their clients during therapy sessions. The young people were provided with an envelope in which to seal their completed WAI.
-
Treatment fidelity Participants were asked to provide consent to have all treatment sessions recorded for the purpose of assessing staff fidelity and adherence to the intervention protocol. Assessment of fidelity and adherence to the protocol was conducted by rating the frequency of use and quality of behaviour change techniques using an adaption of the fidelity assessment scale developed as part of the UKATT trial. 95 This was carried out on all available Y-SBNT recordings. In addition, the intention had been to assess 10–20% of the TAU sessions to identify the components of TAU. However, as only a small number of sessions was ultimately available, all TAU recordings were rated. The aim was to collect samples from across all therapists from both centres from the beginning, middle and end of the therapy.
Adverse events
There were no anticipated risks in relation to either treatment arm and there was no documented evidence of adverse events arising as a results of either TAU or Y-SBNT, but a mechanism for recording them was in place if any arose (see Appendix 9).
Statistical methods
Primary analysis
As this was a feasibility study, outcomes were primarily summarised only descriptively. The end point of main clinical interest, the TLFB interview, was analysed to obtain the effect size and CI. Analysis was conducted in Stata 13 (StataCorp LP, College Station, TX, USA).
Primary outcomes
Recruitment rates
Graphs showing the number of patients entering the study each month and the cumulative monthly recruitment rate are presented. An average recruitment rate was calculated for the period between randomisation of the first participant and randomisation of the last participant.
Baseline data
Patient baseline characteristics are summarised descriptively by treatment group using mean, SD, median, minimum and maximum for continuous measures and number and percentage for categorical measures. The referral route of participants is also described.
Follow-up completion rates
A Consolidated Standards of Reporting Trials (CONSORT) diagram is used to summarise the flow of patients through the study. 96 The number and percentage of participants remaining in the study and attending follow-up at each time point is reported by treatment group, with reasons for discontinuation given when possible.
Retention in treatment
The total number of treatment sessions attended, and the median number per participant, are presented by treatment group, as a measure of retention in treatment.
Intervention effectiveness
The main clinical outcome measure was based on the TLFB interview. At baseline, month 3 and month 12, participants were asked to recall on which days they had used their primary problem substance in the previous 90 days. The number of days was summed and divided by 90 to obtain the proportion. The primary problem substance was classified as alcohol, cannabis or another substance (such as ecstasy, cocaine or ‘legal highs’). The main effectiveness outcome was the proportion of days that the primary problem substance was used in the preceding 90-day period. This outcome is summarised descriptively by treatment group, time point and therapist. A participant’s ‘primary therapist’ was the therapist who delivered most of his or her treatment sessions (the first therapist whom they saw was selected in the event of a tie).
A covariance pattern model was used to compare the proportion of days between the Y-SBNT arm and the TAU arm, adjusting for baseline proportion, treatment group, time and a treatment group × time interaction as fixed effects and primary therapist as a random effect. The model included all participants who provided baseline TLFB data and outcome data at month 3, month 12 or both. Missing data patterns for the TLFB outcome are summarised as monotone (missing after a certain time point) and intermittent (missing but then present at a later time point). Different covariance structures for the repeated measurements (independent, exchangeable, banded, unstructured) were applied to the model. The most appropriate pattern for the final model was chosen by comparing the Akaike information criterion (smaller value preferred). 97 An adjusted mean is presented for each treatment group and time point with associated standard error (SE) and 95% CI. An adjusted mean difference (AMD), 95% CI and p-value is given for each time point. The primary end point is month 12 and the treatment effect at month 3 serves as a secondary outcome. An effect size (Cohen’s d) for the mean difference at each time point is reported with a one-sided 80% confidence limit to compare with the desired effect size of 0.3 for the main trial.
A sensitivity analysis was conducted excluding participants from the model who had their 12-month follow-up conducted > 4 weeks early.
As outlined in Chapter 1, a key issue affecting the initiation and retention of young people and families in treatment is the extent to which perceived ‘coercion’ is involved. In the UK, criminal justice referrals constitute the largest referral source for young people attending specialist substance services and, as such, it was thought important to explore the effect of referral source to provide some indication of the level of perceived ‘coercion’. In particular, it was hypothesised that participants referred from the criminal justice system [youth offending teams (YOTs)] were likely to be less engaged/motivated than participants referred from the community. In addition, inspection of comparative baseline data indicated that more participants in the TAU group reported having religious beliefs, with religiosity having been shown to be associated with better outcomes in young people using substances. 98–100 Therefore, in a post hoc analysis, whether or not participants reporting having religious beliefs and referral route were included as covariates in the analysis model to obtain adjusted means for these subgroups at month 12.
Secondary outcomes
Strengths and Difficulties Questionnaire
The SDQ consists of 25 items and each item has three response categories: not true, somewhat true and certainly true. These are coded as 0, 1 and 2, respectively, for all items except items 7, 11, 14, 21 and 25, which are reverse scored (i.e. not true = 2, somewhat true = 1, certainly true = 0). For analysis, if a participant had ticked two options or ticked between the two options, their response was assumed to be ‘somewhat true’. A score for each subscale was obtained by summing the item scores in that scale. Scale scores were pro-rated if at least three items were completed, so scores range from 0 to 10. The total difficulties score was generated by summing the scores from all of the scales except for the prosocial scale. The resultant score could range from 0 to 40 and is missing if one of the component scores is missing. A lower score indicates greater emotional well-being. The version of the SDQ used in this trial included an ‘impact supplement’, the items for which can be summed to generate an impact score that ranges from 0 to 10, with 10 indicating that difficulties distress the participant a great deal and interfere with his or her life. SDQ scores can be used as continuous variables or can be classified as normal, borderline and abnormal, as in Table 3.
| Subscale | Normal | Borderline | Abnormal |
|---|---|---|---|
| Emotional symptoms scale | 0–5 | 6 | 7–10 |
| Conduct problems scale | 0–3 | 4 | 5–10 |
| Hyperactivity scale | 0–5 | 6 | 7–10 |
| Peer problems scale | 0–3 | 4–5 | 6–10 |
| Prosocial scale | 6–10 | 5 | 0–4 |
| Total difficulties score | 0–15 | 16–19 | 20–40 |
| Impact score | 0 | 1 | 2–10 |
Each of the five subscale scores, the total score and the impact score for the SDQ was summarised descriptively by treatment group and time point using number with valid response, mean, 95% CI for the mean, SD, SE, median, minimum and maximum. The mean difference between the groups is presented with a 95% CI for months 3 and 12 and graphs of mean score over time by treatment group have been produced. Effect sizes are given with a one-sided 80% upper confidence limit. The number and percentage of young people in each banding (normal, borderline and abnormal) are presented by scale, treatment group and time point.
Important People Drug and Alcohol interview
The IPDA interview was scored according to the instructions in Appendix 10. The total number of people discussed and the median number per young person are presented, in addition to summaries of the proportion of the network with whom the young person has daily contact; family members in the network; and number in the network who use alcohol, cannabis and other illicit substances. Z-scores for network size, daily network size, importance of the four most important people and the three components (network substance involvement, general/treatment support and network support for substance use) were calculated. These are summarised descriptively by treatment group and time point. A z-score is a statistical measurement of a score’s relationship to the mean in a group of scores. A z-score of 0 means that the score is the same as the mean. A z-score can also be positive or negative, indicating whether it is above or below the mean and by how many SDs.
Family Environment Scale: Family Relationships Index
The scale consists of conflict, cohesion and expressiveness subscales (nine items each). A true or false response is given for each item and a score of 1 is assigned for a ‘positive’ response. For analysis, if a participant had ticked both true and false or had ticked between the two options, a ‘worst case scenario’ response was assumed (i.e. one that indicated greater conflict or less cohesion and expressiveness). A raw score was calculated for each subscale in the range 0–9, which was then converted to a standard score using the scoring manual. 87 The standard scores range from 33 to 80 for the conflict subscale, from 4 to 65 for the cohesion subscale and from 16 to 71 for the expressiveness subscale; a higher standard score indicates greater cohesion and expressiveness and lower levels of conflict among family members.
The extent of missing data per item at each time point was investigated to assess whether there were any issues with using this questionnaire in the study population. Floor/ceiling effects were explored using bar charts of individual items. Standard scores for the cohesion, expressiveness and conflict subscales are summarised by treatment group and session number using number with valid response, mean, 95% CI for the mean, SD, SE, median, minimum and maximum. The mean difference between the groups is presented with a 95% CI for months 3 and 12 and graphs of mean scores over time by treatment group have been produced. Effect sizes are given with a one-sided 80% upper confidence limit.
Working Alliance Inventory
This 12-item questionnaire measures the perceived strength of the working alliance between the therapist and his or her clients during therapy sessions and is formed of three scales (task, bond and goal). Items are measured on a scale from 1 to 7 (‘never’ to ‘always’), with some items reverse scored, as indicated in Table 4.
| Scale | Item number | Item direction |
|---|---|---|
| Task | 1 | + |
| 2 | + | |
| 8 | + | |
| 12 | + | |
| Bond | 3 | + |
| 5 | + | |
| 7 | + | |
| 9 | + | |
| Goal | 4 | – |
| 6 | + | |
| 10 | – | |
| 11 | + |
Scale scores are obtained by summing the responses for the four items in that scale when there are no missing item responses. Higher scores represent a greater perceived strength of the working alliance. Task, bond and goal subscales are summarised for participants and therapists by treatment group and session number using number with valid response, mean, 95% CI for the mean, SD, SE, median, minimum and maximum. The mean difference between the groups is presented with a 95% CI for months 3 and 12 and graphs of mean scores over time by treatment group have been produced.
Other end points
School attendance and engagement at month 12 are reported descriptively.
Economic analysis methods
The economic component of the study was designed to assess the feasibility of conducting a cost-effectiveness analysis of a full trial. This involved piloting a questionnaire, analysing responses and calculating quality-adjusted life-years (QALYs) using the EQ-5D-5L. 92 As per NICE guidance, the primary outcomes were reported from a NHS and personal and social services perspective. 101 Furthermore, because of the potential impact of this particular intervention on society, an attempt was also made in the questionnaire to collect information regarding participants’ contacts with the police and the criminal justice system. The primary analysis was a complete case analysis with costs and quality of life adjusted for baseline values, treatment sessions and therapist as random effect. A mean imputation was used as a sensitivity analysis. The non-parametric bootstrap resampling technique was employed to explore the uncertainty of the cost data. 102–105 The adjusted cost was bootstrapped by group to account for skewness, sampling with replacement observations 5000 times to generate a new population of sample means with an approximate normal distribution. From this, 95% CIs were constructed for the mean total costs. All costs are presented in UK pounds sterling at 2013/14 prices.
A full cost-effectiveness analysis was not conducted as this was a pilot trial and was not powered to detect significant differences. The economic component of this trial examined the feasibility of conducting a full incremental cost-effectiveness analysis of Y-SBNT compared with TAU.
Intervention
Intervention costs encompassed staff costs of the therapists delivering the intervention and the trainers who delivered the training and supervision to these therapists, travel costs and overheads. The therapists’ remuneration was recorded by the research team and a 12% overhead was added based on the information provided by the service providers. Hourly earnings were then multiplied by the time that participants spent in contact with the therapist, which included both appointment length and the time that the therapist spent travelling to the appointment, as recorded in the treatment log. Travel costs were estimated using the NHS reimbursement rate and we did not distinguish between vehicles (e.g. car, bus, motorcycle). 106
Training costs included staff costs for training sessions and supervision sessions and travel costs when applicable. For each site in the trial, 2 days of training was delivered by two professionals, whose hourly wage including overheads was obtained from their finance departments. Staff costs of the therapists who attended the training were also taken into account. Supervision costs included twice-monthly 1-hour group meetings for each site.
Service use
Participants’ use of health care was identified retrospectively by self-report using a service use questionnaire at baseline and 12 months’ follow-up. It covered primary care, secondary care and social services. A set of national average unit costs (see Table 23) was then applied to the usage recorded to estimate the total cost of health-care and social services during the previous 12-month period.
Similarly, contacts with the police and the criminal justice system were also recorded by self-report by completion of a service use questionnaire at baseline and 12 months’ follow-up. In this case it was limited to arrests, court appearances, probation and prison days because of the complexity of the procedures involved. A set of national average unit costs (see Table 23) was applied when applicable, as with health-care and social services use.
Health-related quality of life
During the pilot trial, HRQoL measured by the EQ-5D-5L was collected at baseline and 3 and 12 months’ follow-up. Although by conventional approach we would estimate QALYs by calculating the area under the curve, for this feasibility study we did not intend to do so. 107 As this was a pilot trial with a small number of participants, calculated QALYs could appear conclusive and misleading. Instead, the mean index scores and the VAS scores were investigated.
Qualitative analysis methods
A key aim of this feasibility study was to establish the acceptability of the Y-SBNT intervention to young people, their families/network members and the therapists/clinical sites delivering the new intervention. Participant interviews were conducted to explore their views and experiences of the intervention and the study process. The interviews were semistructured in nature and built on the qualitative work conducted as part of the UKATT (e.g. Orford et al. 108) and previous studies of SBNT with drug users (e.g. Copello et al. 71) to explore perceptions of the effectiveness and utility of the adapted intervention.
Qualitative data collection took place with participants in the experimental group and their families/network members at 3 months post randomisation. Interviews with therapists and a service manager in the two clinical sites were conducted at a single time point following the completion of the interviews with young people. Written informed consent was gained from all participants prior to their qualitative interviews. Interviews were digitally recorded, fully transcribed and imported into NVivo 10 (QSR International, Warrington, UK) for the management and analysis of data.
Thematic analysis was used to analyse the data. 109,110 This is a flexible approach that allows themes to be generated inductively from the raw data or deductively from theory and previous research. Both inductive and deductive techniques were used to explore the data. Themes were generated from what the young people, network members, therapists and service manager said about their experiences and also from evidenced-based components of the Y-SBNT approach (e.g. involving important others in treatment, goal setting). Themes were identified by their frequency, intensity and extensiveness. 110 An experienced mixed-methods researcher completed the qualitative analysis (PT). In addition, an experienced qualitative researcher (LT) independently analysed a subsample of transcripts, with discussions undertaken to develop an agreed coding framework. This framework and emerging findings were also subjected to interpretive feedback from young people representatives at meetings convened specifically to seek young people’s views on the qualitative findings. The following steps were conducted: data immersion; data coding; initial, refined and agreed coding framework; and identification of themes.
Public involvement
As part of the significant public involvement component of this study, the project team actively sought to involve a sample of young people with a history of treatment for substance misuse through a young people’s advisory group (YPAG). We also planned to involve a sample of parents of young people with substance abuse problems throughout the research process.
Our initial intention, as outlined in the project proposal, was that young people with a history of treatment for substance misuse, as well as parents of young people with substance misuse problems, would ‘be supported to work alongside the research team in order to ensure that the intervention is acceptable and relevant to our target groups, and reflects the views of service users and their families’. We hoped to establish a YPAG of 10–12 young advisors aged 12–18 years who would be actively engaged throughout the project. They would be young people with previous experience of accessing substance misuse treatment services but who were not currently in treatment. These young people would be involved primarily through a series of group meetings held over the course of the study, either in a convenient central location or alternating between the sites from which the young people were recruited. Up to 12 meetings were planned to coincide with key milestones in the project. Clear ground rules for making these meetings accessible to young people would be agreed at the start by all involved, based on INVOLVE and other guidance to support this work. 57,63,111
We also hoped that one or two young advisors would attend TSC meetings to ensure that young people’s views directly informed strategic project decisions, but that, depending on the wishes of the group, these representatives could change over the course of the study. We also proposed that a small number of parents, unrelated to the young people involved in the study either through involvement activity or as participants would also be involved in the study through representation on the study advisory group.
Although the model of involvement that emerged during the course of the study was rather different from our initial plans (see Chapters 4 and 8), young advisors were nonetheless involved throughout the study to varying degrees. Appendices 2 and 3 contain more information on activities, outputs and outcomes related to these meetings.
Future involvement
We hope to be able to support young people’s involvement in the development of a lay summary and other publications related to public involvement in the study, as well as in dissemination and planning of a possible follow-on project to establish a stand-alone young people’s group or panel.
Chapter 4 Protocol changes
Change to data collection
It was decided to remove the collection of the health economic data from the 3-month follow-up questionnaire. As the health economic assessment was intended to collect information (i.e. education, employment, crime, etc.) retrospectively over a ’12-month’ time frame, the 3-month assessment became redundant as any information captured at 3 months would be captured again at 12 months. Removal of this information also reduced the burden on young people of data being collected by the researchers.
Public involvement
We had originally planned to recruit a YPAG who would be actively engaged throughout the project on an ongoing basis. However, to adapt to the needs and preferences of the young people who became involved in the project, this model changed over the course of the project. These changes are discussed further in Chapter 8.
Involving young people in the Trial Steering Committee
In early 2014 we also reviewed our initial plans to have young people as lay members at TSC meetings. The emerging model of young people’s involvement did not include the planned core group of young people engaged with the project regularly on an ongoing basis, who would not only have an understanding of the study itself but also have insights into the process and management of randomised controlled trials. It was felt by the Trial Management Group (TMG) that this would have made it more difficult to make any involvement in the meetings accessible and meaningful for lay members. The public involvement leads therefore agreed to report to TSC meetings and offer young people involved in the study the chance to contribute to this report or to attend the meetings if they wanted to do so, in which case we would seek to make the meetings as accessible as possible. However, the one young person who did express an interest in coming to a TMG and TSC meeting was unable to do so because of ill health.
Involving parents and carers
We had initially proposed that a small number of parents and carers, unrelated to the young people involved in the study either through involvement activity or as participants, would also be involved in the project through representation on the study advisory group. In July 2014 we ran a focus group with two adults (a woman with a foster daughter and a mother with an adopted son). Both focus group participants said that they would be keen to be kept updated on the project and were invited to participate further, but neither made any commitment to future involvement. It is also true that parental involvement, as a small part of the overall public involvement element of the study, perhaps got rather lost amid all of the additional work involved in the recruitment and retention of young advisors.
Chapter 5 Results
This chapter presents the results of both the clinical analysis and the health economic analysis, as detailed in Chapter 3.
Clinical data
Trial recruitment
Young people’s services in two UK regions participated in the study: the West Midlands and the North East. Our initial aim was to recruit 60 participants between 1 May 2014 and 31 October 2014 at a rate of 10 participants a month. In practice, recruitment did not open until 19 May 2014, with the first participant recruited on 30 May and the last on 14 November 2014 (Figure 2). In total, 53 participants were randomised, 26 (49.1%) to the Y-SBNT arm and 27 (50.9%) to the TAU arm. This equates to an approximate average recruitment rate of nine young people every 4 weeks of active recruitment (Figure 3). The number of participants recruited in the West Midlands was 33 (62.3%) and in the North East was 20 (37.7%).
FIGURE 2.
Cumulative recruitment against target recruitment by month in the Y-SBNT trial.
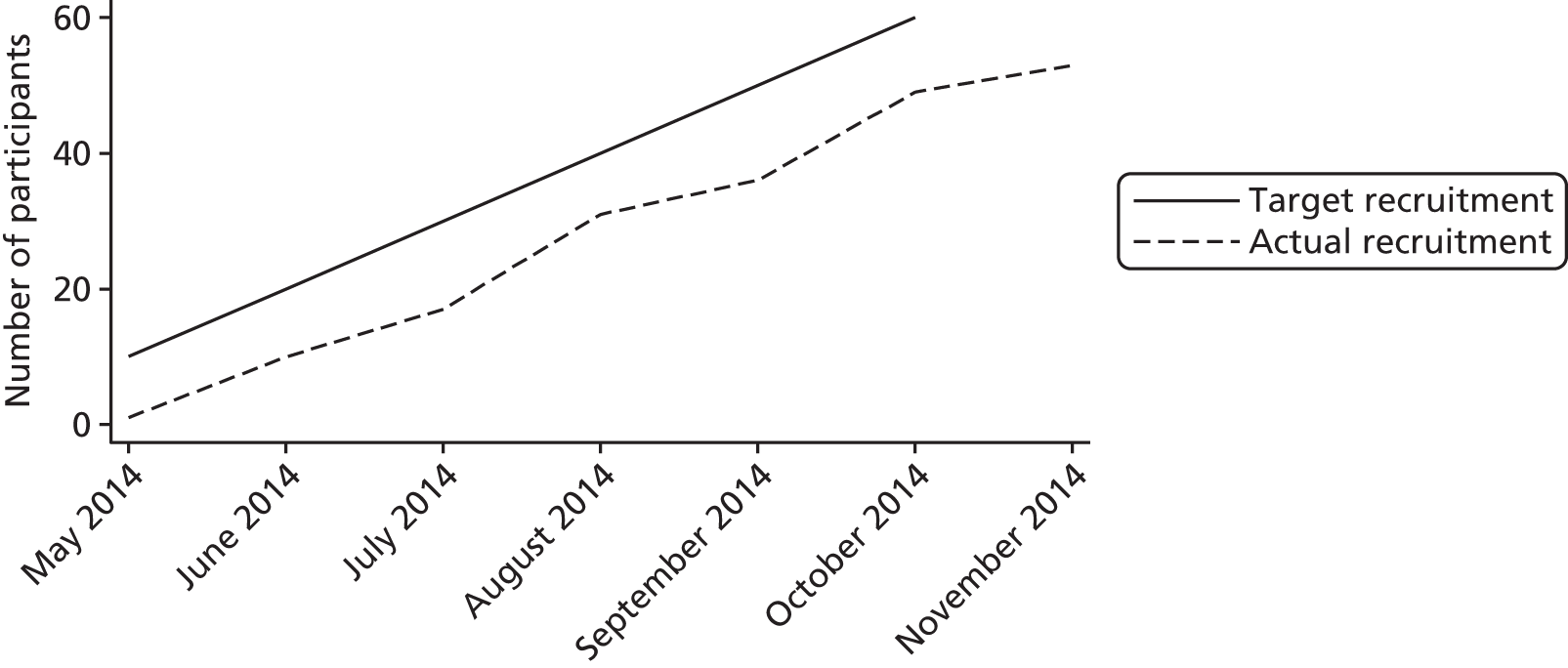
FIGURE 3.
Monthly recruitment of young people into the Y-SBNT trial.

In Figure 4, the CONSORT flow chart shows the progress of participants through the trial.
FIGURE 4.
The CONSORT flow diagram for the Y-SBNT trial.
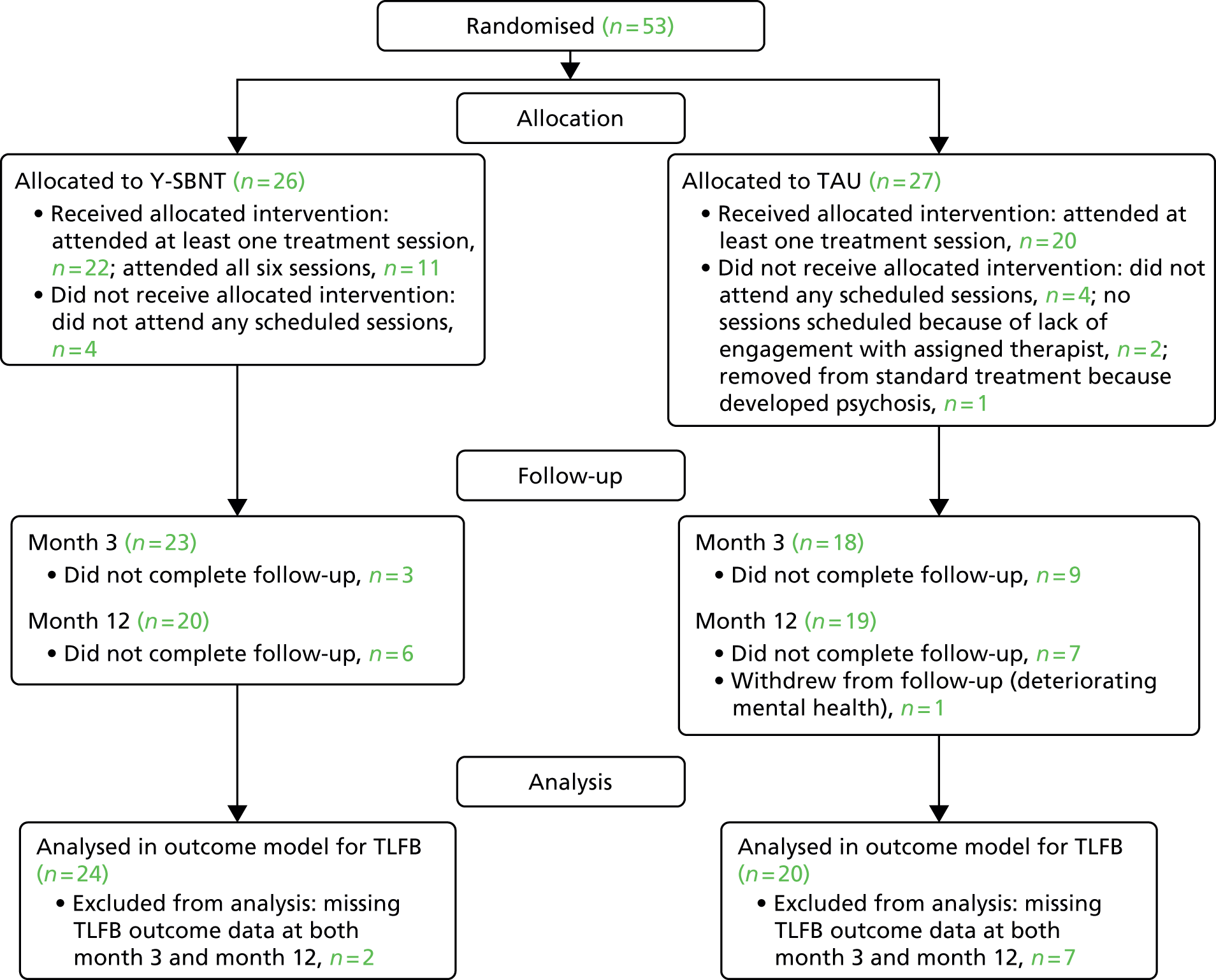
The majority of participants were male (n = 40, 75.5%) and the average age was 16.1 years (range 12–18 years) (Table 5). Participants were mostly of white British ethnicity (n = 40, 75.5%) but there were also participants with Caribbean, African and Asian ethnicity. Over half of the participants were still in education (n = 32, 60.4%) and most lived with their parent(s) or carer(s) (n = 32, 60.4%). A number of young people reported religious beliefs, with a higher proportion of young people with religious beliefs in the TAU group (29.6% vs. 7.7%).
| Characteristic | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 21 (80.8) | 19 (70.4) | 40 (75.5) |
| Female | 5 (19.2) | 8 (29.6) | 13 (24.5) |
| Age (years) | |||
| Mean (SD) | 16.1 (1.5) | 16.0 (1.4) | |
| Median (min., max.) | 17 (12, 18) | 16 (13, 18) | |
| Sexual identity, n (%) | |||
| Heterosexual | 24 (92.3) | 24 (88.9) | 48 (90.6) |
| Gay | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Bisexual | 1 (3.8) | 2 (7.4) | 3 (5.7) |
| Missinga | 1 (3.8) | 1 (3.7) | 2 (3.8) |
| Ethnic group, n (%) | |||
| White British | 20 (76.9) | 20 (74.1) | 40 (75.5) |
| Other | 6 (23.1) | 7 (25.9) | 13 (24.5)b |
| Nationality, n (%) | |||
| British | 25 (96.2) | 27 (100.0) | 52 (98.1) |
| Other | 1 (3.8)c | 0 (0.0) | 1 (1.9) |
| Religion, n (%) | |||
| Christian | 1 (3.8) | 5 (18.5) | 6 (11.3) |
| Muslim | 1 (3.8) | 3 (11.1) | 4 (7.5) |
| No religion | 24 (92.3) | 19 (70.4) | 43 (81.1) |
| In full- or part-time education, n (%) | 15 (57.7) | 17 (63.0) | 32 (60.4) |
| Qualifications, n (%) | |||
| Not yet taken GCSEs | 15 (57.7) | 14 (51.9) | 29 (54.7) |
| One or more GCSE | 10 (38.5) | 7 (25.9) | 17 (32.1) |
| One or more AS/A level | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Left with no qualifications | 0 (0.0) | 4 (14.8) | 4 (7.5) |
| Other | 1 (3.8) | 2 (7.4) | 3 (5.7) |
| Current employment, n (%) | |||
| Student | 13 (50.0) | 14 (51.9) | 27 (50.9) |
| Seeking work/apprenticeship | 7 (26.9) | 7 (25.9) | 14 (26.4) |
| Seeking to return to education | 2 (7.7) | 3 (11.1) | 5 (9.4) |
| In training | 2 (7.7) | 3 (11.1) | 5 (9.4) |
| Other | 1 (3.8) | 0 (0.0) | 1 (1.9) |
| Missing | 1 (3.8) | 0 (0.0) | 1 (1.9) |
| Living arrangements, n (%) | |||
| With parent(s)/carer(s) | 14 (53.8) | 18 (66.7) | 32 (60.4) |
| In a hostel | 4 (15.4) | 4 (14.8) | 8 (15.1) |
| With other relative | 4 (15.4) | 3 (11.1) | 7 (13.2) |
| Alone | 2 (7.7) | 0 (0.0) | 2 (3.8) |
| With someone not related/friends | 1 (3.8) | 1 (3.7) | 2 (3.8) |
| With a foster family/in care | 1 (3.8) | 1 (3.7) | 2 (3.8) |
For those randomised into the trial from the North East, 12 (60.0%) were referred from the community, seven (35.0%) were referred from YOTs and one (5%) self-referred from the YOT. In the West Midlands, a lower proportion was referred from the community (n = 9, 27.3%) and a higher proportion was referred from YOTs (n = 24, 72.7%). Overall, the referral routes were reasonably well balanced between the two treatment groups. In the Y-SBNT group, nine (34.6%) were referred from the community and16 (61.5%) from YOTs, with one (3.8%) self-referring whereas in the TAU group 12 (44.4%) were referred from the community and 15 (55.6%) were referred from YOTs.
Participants were followed up at 3 and 12 months post randomisation. Each follow-up consisted of a face-to-face meeting with a member of the study research team. Significant efforts were made to ensure high follow-up rates. Attempts were made to follow up all participants at each time point, except at month 12 for one participant in the TAU group who formally withdrew from follow-up after the intervention because of deteriorating mental health. In total, 41 (77.4%) participants were followed up at month 3 (Y-SBNT, n = 23; TAU, n = 18) and 39 (73.6%) were followed up at month 12 (Y-SBNT, n = 20; TAU, n = 19) (Table 6). Because of delays in the study set-up, patients recruited in the last 2 months of recruitment were followed up at a time point earlier than 12 months to enable the study to be completed within the study timeline (median length of follow-up 12.5 months, range 10.0–15.3 months). Participant follow-up ended on 6 October 2015, at which point the study ended.
| Time point | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) |
|---|---|---|---|
| Baseline, n (%) | 26 (100) | 27 (100) | 53 (100) |
| Month 3, n (%) | 23 (88.5) | 18 (66.7) | 41 (77.4) |
| Month 12, n (%) | 20 (76.9) | 19a (70.4) | 39 (73.6) |
Treatment sessions
Treatment sessions took place between 12 June 2014 and 26 March 2015 for the Y-SBNT group and between 4 July 2014 and 26 August 2015 for the TAU group; in total, 103 Y-SBNT sessions and 62 TAU sessions were attended (Table 7). It was intended that the Y-SBNT intervention would consist of six 50-minute SBNT sessions delivered over a maximum of 12 weeks. In total, 22 Y-SBNT participants attended at least one session and 11 participants attended all six sessions (median number of sessions attended 5, range 0–6). For the 11 participants who attended all six sessions, the time between the first and sixth session ranged from 8 to 20 weeks (median 12 weeks). The median length of the Y-SBNT sessions attended was 60 minutes (range 15–90 minutes). In the TAU group, 20 participants attended at least one session during their 12-month follow-up (median number of sessions attended 2, range 0–15).
| Treatment sessions | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) |
|---|---|---|---|
| Total number of sessions scheduled | 141 | 122 | 263 |
| Total number of sessions attended, n (% of scheduled) | 103 (73.0) | 62 (50.8) | 165 (62.7) |
| West Midlands | 53 | 30 | 83 |
| North East | 50 | 32 | 82 |
| Number of sessions attended, n (%) | |||
| 0 | 4 (15.4) | 7 (25.9) | 11 (20.8) |
| 1 | 2 (7.7) | 5 (18.5) | 7 (13.2) |
| 2 | 2 (7.7) | 7 (25.9) | 9 (17.0) |
| 3 | 1 (3.8) | 3 (11.1) | 4 (7.5) |
| 4 | 2 (7.7) | 2 (7.4) | 4 (7.5) |
| 5 | 4 (15.4) | 1 (3.7) | 5 (9.4) |
| 6 | 11 (42.3) | 1 (3.7) | 12 (22.6) |
| 15 | 0 (0.0) | 1 (3.7) | 1 (1.9) |
| Appointments scheduled before young person attended first session, n (%) | |||
| 1 | 19 (86.4) | 16 (80.0) | 35 (83.3) |
| 2 | 1 (4.5) | 2 (10.0) | 3 (7.1) |
| 3 | 1 (4.5) | 0 (0.0) | 1 (2.4) |
| 4 | 0 (0.0) | 1 (5.0) | 1 (2.4) |
| 5 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 6 | 1 (4.5) | 0 (0.0) | 1 (2.4) |
| 7 | 0 (0.0) | 1 (5.0) | 1 (2.4) |
| Length of sessions (minutes) | |||
| Median (min., max.) | 60 (15, 90) | 45 (10, 180) | 45 (10, 180) |
| Reason for non-attendance, n (%) | |||
| Cancelled by young person/carer | 13 (34.2) | 7 (11.7) | 20 (20.4) |
| Cancelled by therapist/service | 3 (7.9) | 2 (3.3) | 5 (5.1) |
| Participant did not attend | 3 (7.9) | 21 (35.0) | 24 (24.5) |
| No reason given | 19 (50.0) | 30 (50.0) | 49 (50.0) |
| Session audio-recorded, n (%) | 46 (44.7) | 10 (16.1) | 56 (33.9) |
| Reason session not audio-recorded, n (%) | |||
| Young person declined | 41 (71.9) | 18 (34.6) | 59 (54.1) |
| Problem with recorder | 3 (5.3) | 2 (3.8) | 5 (4.6) |
| Other reason | 2 (3.5) | 2 (3.8) | 4 (3.7) |
| No reason given | 11 (19.3) | 30 (57.7) | 41 (37.6) |
| Mean time of travel to appointment by therapists (all scheduled appointments) (minutes) | 20 | 11 | |
| Mean time of travel to appointment by therapists per participant (all scheduled appointments) (hours) | 2.11 | 0.86 | |
Overall, among participants referred from the community, the median number of sessions attended was four (range 0–6), whereas among participants referred from YOTs (including self-referral), the median number of sessions attended was two (range 0–15).
Intervention effectiveness: Timeline Follow-Back interview
Data for the proportion of days that the primary substance was used in the preceding 90 days were missing for 12 participants at month 3 and for 14 participants at month 12 (Table 8).
| Pattern of missing data | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) |
|---|---|---|---|
| No missing data, n (%) | 19 (73.1) | 17 (63.0) | 36 (67.9) |
| Monotone | |||
| Missing month 3 and month 12, n (%) | 2 (7.7) | 7 (25.9) | 9 (17.0) |
| Missing month 12 only, n (%) | 4 (15.4) | 1 (3.7) | 5 (9.4) |
| Intermittent | |||
| Missing month 3 only, n (%) | 1 (3.8) | 2 (7.4) | 3 (5.7) |
The primary problem substances for participants were alcohol (Y-SBNT, n = 2; TAU, n = 3), cannabis (Y-SBNT, n = 19; TAU, n = 20) and other substances including legal highs (Y-SBNT, n = 5; TAU, n = 4). Other substances included NPSs [n = 7; specifically mentioned were synthetic cannabinoid (n = 1) and mephedrone (n = 2)] and solvents (n = 2). The mean number of days that participants reported using their primary substance in the preceding 90 days was higher in the Y-SBNT group than in the TAU group at baseline, month 3 and month 12 (Table 9).
| Time point | Number of days main problem substance was used in preceding 90 days, unadjusted | ||
|---|---|---|---|
| Y-SBNT (N = 27) | TAU (N = 26) | Total (N = 53) | |
| Baseline | |||
| Valid n | 26 | 27 | 53 |
| Mean (SD) | 61.2 (32.6) | 55.5 (31.0) | 58.3 (31.6) |
| Median (min., max.) | 80.5 (1, 90) | 50 (3, 90) | 55 (1, 90) |
| Month 3 | |||
| Valid n | 23 | 18 | 41 |
| Mean (SD) | 43.2 (36.1) | 38.8 (32.9) | 41.3 (34.4) |
| Median (min., max.) | 35 (0, 90) | 34.5 (0, 9) | 35 (0, 90) |
| Month 12 | |||
| Valid n | 20 | 19 | 39 |
| Mean (SD) | 48.7 (38.0) | 36.7 (36.3) | 42.8 (37.2) |
| Median (min., max.) | 51 (0, 90) | 31 (0, 90) | 37 (0, 90) |
The main clinical outcome is summarised by treatment group and time point in Table 10. The Y-SBNT group had a higher mean proportion at all time points.
| Time point | Proportion of days primary substance was used in preceding 90 days | |||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusteda | |||||
| Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) | Y-SBNT, mean (SE) (95% CI) | TAU, mean (SE) (95% CI) | Mean difference (95% CI); p-value; effect sizeb | |
| Baseline | ||||||
| Valid n | 26 | 27 | 53 | – | – | – |
| Mean (SD) | 0.68 (0.36) | 0.62 (0.34) | 0.65 (0.35) | |||
| Median (min., max.) | 0.89 (0.01, 1) | 0.56 (0.03, 1) | 0.61 (0.01, 1) | |||
| Month 3 | ||||||
| Valid n | 23 | 18 | 41 | 0.47 (0.09) (0.29 to 0.65) | 0.41 (0.09) (0.23 to 0.59) | 0.06 (–0.19 to 0.32); p = 0.63; –0.15 (0.11) |
| Mean (SD) | 0.48 (0.40) | 0.43 (0.37) | 0.46 (0.38) | |||
| Median (min., max.) | 0.39 (0, 1) | 0.38 (0, 1) | 0.39 (0, 1) | |||
| Month 12 | ||||||
| Valid n | 20 | 19 | 39 | 0.52 (0.09) (0.34 to 0.71) | 0.39 (0.09) (0.21 to 0.57) | 0.13 (–0.12 to 0.39); p = 0.30; –0.32 (–0.05) |
| Mean (SD) | 0.54 (0.42) | 0.41 (0.40) | 0.48 (0.41) | |||
| Median (min., max.) | 0.57 (0, 1) | 0.34 (0, 1) | 0.41 (0, 1) | |||
| Sensitivity analysis excluding the 11 participants who had their 12-month follow-up conducted > 4 weeks early | ||||||
| Baseline | ||||||
| Valid n | 23 | 19 | 42 | – | – | – |
| Mean (SD) | 0.64 (0.37) | 0.63 (0.35) | 0.63 (0.35) | |||
| Median (min., max.) | 0.61 (0.01, 1) | 0.57 (0.03, 1) | 0.59 (0.01, 1) | |||
| Month 3 | ||||||
| Valid n | 21 | 11 | 32 | 0.45 (0.09) (0.26 to 0.63) | 0.50 (0.12) (0.27 to 0.73) | –0.05 (–0.35 to 0.24); p = 0.72; 0.13 (0.43) |
| Mean (SD) | 0.43 (0.39) | 0.52 (0.37) | 0.46 (0.38) | |||
| Median (min., max.) | 0.36 (0, 1) | 0.60 (0.01, 1) | 0.42 (0, 1) | |||
| Month 12 | ||||||
| Valid n | 17 | 11 | 28 | 0.52 (0.10) (0.33 to 0.72) | 0.48 (0.11) (0.25 to 0.70) | 0.05 (–0.25 to 0.34); p = 0.76; –0.11 (0.20) |
| Mean (SD) | 0.51 (0.42) | 0.50 (0.42) | 0.51 (0.41) | |||
| Median (min., max.) | 0.56 (0, 1) | 0.41 (0, 1) | 0.48 (0, 1) | |||
Data for the outcome at baseline were complete but nine participants were missing data at both month 3 and month 12 and so the model was based on 44/53 (83.0%) participants [Y-SBNT, n = 24 (92.3%); TAU, n = 20 (74.1%)].
The baseline characteristics of the participants included in the TLFB analysis model are compared between the treatment groups in Table 11. It does not appear that the loss of the nine participants with missing outcome data significantly impacted on the balance achieved at randomisation between the treatment groups.
| Characteristic | Y-SBNT (N = 24) | TAU (N = 20) | Total (N = 44) |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 20 (83.3) | 16 (80.0) | 36 (81.8) |
| Female | 4 (16.7) | 4 (20.0) | 8 (18.2) |
| Age, years | |||
| Mean (SD) | 16.0 (1.5) | 15.9 (1.5) | 16.0 (1.5) |
| Median (min., max.) | 17 (12, 18) | 16 (13, 18) | 16 (12, 18) |
| Sexual identity, n (%) | |||
| Heterosexual | 22 (91.7) | 17 (85.0) | 39 (88.6) |
| Gay | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Bisexual | 1 (4.2) | 2 (10.0) | 3 (6.8) |
| Missinga | 1 (4.2) | 1 (5.0) | 2 (4.5) |
| Ethnic group, n (%) | |||
| White British | 18 (75.0) | 16 (80.0) | 34 (77.3) |
| Other | 6 (25.0) | 4 (20.0) | 10 (22.7)b |
| Nationality, n (%) | |||
| British | 23 (95.8) | 20 (100.0) | 43 (97.7) |
| Other | 1 (4.2)c | 0 (0.0) | 1 (2.3) |
| Religion, n (%) | |||
| Christian | 1 (4.2) | 5 (25.0) | 6 (13.6) |
| Muslim | 1 (4.2) | 3 (15.0) | 4 (9.1) |
| No religion | 22 (91.7) | 12 (60.0) | 34 (77.3) |
| In full- or part-time education, n (%) | 14 (58.3) | 12 (60.0) | 26 (59.1) |
| Qualifications, n (%) | |||
| Not yet taken GCSEs | 14 (58.3) | 11 (55.0) | 25 (56.8) |
| One or more GCSEs | 9 (37.5) | 4 (20.0) | 13 (29.5) |
| One or more AS/A level | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Left with no qualifications | 0 (0.0) | 3 (15.0) | 3 (6.8) |
| Other | 1 (4.2) | 2 (10.0) | 3 (6.8) |
| Current employment, n (%) | |||
| Student | 12 (50.0) | 10 (50.0) | 22 (50.0) |
| Seeking work/apprenticeship | 6 (25.0) | 4 (20.0) | 10 (22.7) |
| Seeking return to education | 2 (8.3) | 3 (15.0) | 5 (11.4) |
| In training | 2 (8.3) | 3 (15.0) | 5 (11.4) |
| Other | 1 (4.2) | 0 (0.0) | 1 (2.3) |
| Missing | 1 (4.2) | 0 (0.0) | 1 (2.3) |
| Living arrangements, n (%) | |||
| With parent(s)/carer(s) | 13 (54.2) | 14 (70.0) | 27 (61.4) |
| In a hostel | 3 (12.5) | 2 (10.0) | 5 (11.4) |
| With other relative | 4 (16.7) | 3 (15.0) | 7 (15.9) |
| Alone | 2 (8.3) | 0 (0.0) | 2 (4.5) |
| With someone unrelated/friends | 1 (4.2) | 1 (5.0) | 2 (4.5) |
| With a foster family/in care | 1 (4.2) | 1 (0.0) | 1 (2.3) |
An exchangeable (compound symmetric) covariance pattern was used for the analysis model. The assumptions of the model were checked visually. The normality of the standardised residuals was assessed using a Q–Q plot and the homoscedasticity of the errors was checked by plotting the residuals against the fitted values (see Appendix 11). The Q–Q plot is used as a graphical method of comparing the distribution of the residuals to a normal distribution. The quantiles of the distributions are plotted against each other. If the residuals are normally distributed, the points will lie on the straight line, which represents the normal distribution. Deviations from the straight line indicate skewness in the distribution of the residuals. These plots gave no reason to be concerned about the validity of the assumptions.
Treatment effect at 12 months
There was no evidence of a difference between the Y-SBNT group and the TAU group at month 12 in the proportion of days that the main problem substance was used in the preceding 90-day period (AMD 0.13, 95% CI –0.12 to 0.39; p = 0.30; see Table 10), that is, the Y-SBNT group had a slightly higher average proportion at 12 months but this difference was not statistically significant (Figure 5). The effect size was calculated as –0.32 (upper limit for one-sided 80% CI –0.05).
FIGURE 5.
Adjusted means for the proportion of days that the primary problem substance was used in the preceding 90-day period by treatment group over time.

Treatment effect at 3 months
There was no evidence of a difference between the Y-SBNT and TAU groups at month 3 in the proportion of days that the main problem substance was used in the preceding 90-day period (AMD 0.06, 95% CI –0.19 to 0.32; p = 0.63; see Table 10), that is, the Y-SBNT group had a slightly higher average proportion at month 3 but this difference was not statistically significant. The effect size was calculated as –0.15 (upper limit for one-sided 80% CI 0.11).
The proportion of days that the primary substance was used in the preceding 90 days at month 12 is summarised by primary therapist in Table 12.
| Treatment group | Therapist ID | Participant, n, proportion of days, mean (SD) |
|---|---|---|
| Y-SBNT | 1 | 2, 0.86 (0.20) |
| 2 | 4, 0.07 (0.14) | |
| 3 | 5, 0.63 (0.41) | |
| 4 | 5, 0.45 (0.44) | |
| 5 | 4, 0.85 (0.30) | |
| TAU | 6 | 2, 0.34 (0.24) |
| 7 | 3, 0.56 (0.35) | |
| 8 | 6, 0.63 (0.43) | |
| 9 | 3, 0.01 (0.02) | |
| 10 | 2, 0.50 (0.71) | |
| 11 | 2, 0.01 (0.02) | |
| 12 | 1, 0.57 (–) |
Each therapist was associated with between one and six participants (median 3). The mean proportion of days that the primary problem substance was used in the preceding 90 days at month 12 varied across the therapists from 0.01 to 0.86.
Sensitivity analysis
The TLFB analysis was repeated excluding the subgroup of 11 participants (Y-SBNT, n = 3; TAU, n = 8) who had their 12-month follow-up conducted > 4 weeks early. There was no evidence of a difference in the proportion of days that the main problem substance was used in the preceding 90-day period between the Y-SBNT group and the TAU group at month 3 or month 12 (see Table 10). The Y-SBNT group had a lower adjusted mean proportion than the TAU group at month 3 (AMD –0.05, 95% CI –0.35 to 0.24; p = 0.72) but not at month 12 (AMD 0.05, 95% CI –0.25 to 0.34; p = 0.76). The respective effect sizes were 0.13 (upper limit for one-sided 80% CI 0.43) and –0.11 (upper limit for one-sided 80% CI 0.20).
Timeline Follow-Back interview outcome by referral route and religion
At month 12, participants referred initially from YOTs had a higher TLFB outcome (adjusted mean proportion of days 0.50) than those referred from the community (adjusted mean proportion 0.41; AMD 0.09, 95% CI –0.07 to 0.25). Participants who reported religious beliefs had a lower predicted outcome than those with no reported religious beliefs (0.28 vs. 0.53; AMD –0.25, 95% CI –0.45 to 0.04).
Secondary analyses
Strengths and Difficulties Questionnaire
The five subscales and the total score for the SDQ are summarised descriptively by intervention group and time point in Table 13.
| SDQ subscale/total scorea | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) | Mean difference (95% CI); effect sizeb |
|---|---|---|---|---|
| Emotional symptoms scale | ||||
| Baseline | ||||
| Valid n | 25 | 26 | 51 | – |
| Mean (95% CI) | 3.5 (2.5 to 4.5) | 3.9 (2.9 to 4.8) | 3.7 (3.0 to 4.3) | |
| SD, SE | 2.4, 0.48 | 2.4, 0.47 | 2.4, 0.33 | |
| Median (min., max.) | 4 (0, 9) | 4 (0, 9) | 4 (0, 9) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | –0.8 (–2.2 to 0.6); 0.35 (0.61) |
| Mean (95% CI) | 3.2 (2.2 to 4.1) | 3.9 (2.9 to 5.0) | 3.5 (2.8 to 4.2) | |
| SD, SE | 2.3, 0.47 | 2.2, 0.51 | 2.2, 0.35 | |
| Median (min., max.) | 2.5 (1, 10) | 3.5 (0, 7) | 3 (0, 10) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | 0.6 (–1.2 to 2.3); –0.20 (0.06) |
| Mean (95% CI) | 3.4 (1.9 to 4.9) | 2.8 (1.8 to 3.9) | 3.1 (2.3 to 4.0) | |
| SD, SE | 3.1, 0.69 | 2.2, 0.50 | 2.7, 0.43 | |
| Median (min., max.) | 3 (0, 10) | 3 (0, 7) | 3 (0, 10) | |
| Conduct problems scale | ||||
| Baseline | ||||
| Valid n | 25 | 26 | 51 | – |
| Mean (95% CI) | 3.7 (2.9 to 4.4) | 3.9 (3.2 to 4.6) | 3.8 (3.3 to 4.3) | |
| SD, SE | 1.8, 0.35 | 1.8, 0.36 | 1.8, 0.25 | |
| Median (min., max.) | 3 (1, 7) | 4 (0, 8) | 4 (0, 8) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | 0.4 (–0.8 to 1.7); –0.22 (0.04) |
| Mean (95% CI) | 3.7 (2.9 to 4.4) | 3.2 (2.1 to 4.3) | 3.5 (2.8 to 4.1) | |
| SD, SE | 1.8, 0.37 | 2.2, 0.53 | 2.0, 0.31 | |
| Median (min., max.) | 4 (1, 7) | 2.3 (1, 8) | 3 (1, 8) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | 0.7 (–0.5 to 1.9); –0.38 (–0.11) |
| Mean (95% CI) | 3.5 (2.6 to 4.4) | 2.8 (1.9 to 3.6) | 3.2 (2.6 to 3.8) | |
| SD, SE | 1.9, 0.43 | 1.8, 0.41 | 1.9, 0.30 | |
| Median (min., max.) | 3 (1, 8) | 3 (0, 6) | 3 (0, 8) | |
| Hyperactivity scale | ||||
| Baseline | ||||
| Valid n | 25 | 26 | 51 | – |
| Mean (95% CI) | 5.4 (4.7 to 6.2) | 6.9 (6.0 to 7.9) | 6.2 (5.6 to 6.8) | |
| SD, SE | 1.9, 0.38 | 2.3, 0.45 | 2.2, 0.31 | |
| Median (min., max.) | 5 (2, 9) | 7 (1, 10) | 6 (1, 10) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | –0.5 (–1.8 to 0.9); 0.21 (0.47) |
| Mean (95% CI) | 5.8 (5.0 to 6.6) | 6.3 (5.1 to 7.4) | 6.0 (5.4 to 6.7) | |
| SD, SE | 1.9, 0.40 | 2.3, 0.54 | 2.1, 0.32 | |
| Median (min., max.) | 5 (2, 10) | 6 (3, 10) | 6 (2, 10) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | 0.03 (–1.2 to 1.3); –0.02 (0.25) |
| Mean (95% CI) | 5.4 (4.6 to 6.1) | 5.3 (4.3 to 6.3) | 5.3 (4.7 to 5.9) | |
| SD, SE | 1.7, 0.37 | 2.1, 0.48 | 1.9, 0.30 | |
| Median (min., max.) | 5 (2, 8) | 6 (1, 9) | 5 (1, 9) | |
| Peer problems scale | ||||
| Baseline | ||||
| Valid n | 25 | 26 | 51 | – |
| Mean (95% CI) | 2.8 (2.3 to 3.3) | 3.2 (2.4 to 3.9) | 3.0 (2.6 to 3.4) | |
| SD, SE | 1.2, 0.24 | 1.8, 0.36 | 1.6, 0.22 | |
| Median (min., max.) | 3 (0, 5) | 3 (0, 7) | 3 (0, 7) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | 0.1 (–0.8 to 1.0); –0.08 (0.19) |
| Mean (95% CI) | 3.0 (2.4 to 3.6) | 2.9 (2.1 to 3.6) | 3.0 (2.5 to 3.4) | |
| SD, SE | 1.4, 0.29 | 1.5, 0.36 | 1.4, 0.22 | |
| Median (min., max.) | 3 (1, 6) | 2 (1, 7) | 3 (1, 7) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | –0.5 (–1.3, 0.4); 0.33 (0.60) |
| Mean (95% CI) | 2.8 (2.3 to 3.3) | 3.3 (2.5 to 4.0) | 3.0 (2.6 to 3.5) | |
| SD, SE | 1.2, 0.26 | 1.6, 0.36 | 1.4, 0.22 | |
| Median (min., max.) | 2.5 (1, 5) | 3 (1, 7) | 3 (1, 7) | |
| Prosocial scale | ||||
| Baseline | ||||
| Valid n | 25 | 26 | 51 | – |
| Mean (95% CI) | 6.8 (6.0 to 7.5) | 6.5 (5.6 to 7.4) | 6.6 (6.1 to 7.2) | |
| SD, SE | 1.8, 0.37 | 2.2, 0.42 | 2.0, 0.28 | |
| Median (min., max.) | 7 (2, 10) | 6 (2, 10) | 6 (2, 10) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | 0.5 (–0.7 to 1.7); 0.26 (0.52) |
| Mean (95% CI) | 7.0 (6.2 to 7.8) | 6.5 (5.5 to 7.5) | 6.8 (6.2 to 7.4) | |
| SD, SE | 1.9, 0.39 | 1.9, 0.46 | 1.9, 0.30 | |
| Median (min., max.) | 7 (2, 10) | 7 (3, 10) | 7 (2, 10) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | 0.6 (–0.8 to 1.9); 0.27 (0.53) |
| Mean (95% CI) | 7.4 (6.4 to 8.3) | 6.8 (5.8 to 7.8) | 7.1 (6.4 to 7.7) | |
| SD, SE | 2.1, 0.46 | 2.1, 0.47 | 2.1, 0.33 | |
| Median (min., max.) | 8 (2, 10) | 7 (3, 10) | 7 (2, 10) | |
| Total SDQ score | ||||
| Baseline | ||||
| Valid n | 25 | 26 | 51 | – |
| Mean (95% CI) | 15.4 (13.6 to 17.2) | 17.8 (15.1 to 20.6) | 16.6 (15.0 to 18.3) | |
| SD, SE | 4.3, 0.85 | 6.8, 1.33 | 5.7, 0.80 | |
| Median (min., max.) | 15 (7, 23) | 20 (3, 29) | 17 (3, 29) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | –0.7 (–3.9 to 2.5); 0.13 (0.39) |
| Mean (95% CI) | 15.6 (13.6 to 17.6) | 16.3 (13.6 to 19.1) | 15.9 (14.4 to 17.5) | |
| SD, SE | 4.6, 0.97 | 5.5, 1.30 | 5.0, 0.78 | |
| Median (min., max.) | 15 (9, 24) | 18 (7, 25) | 16 (7, 25) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | 0.8 (–2.6 to 4.3); –0.15 (0.11) |
| Mean (95% CI) | 15.1 (12.7 to 17.4) | 14.2 (11.5 to 16.9) | 14.6 (12.9 to 16.4) | |
| SD, SE | 5.0, 1.13 | 5.6, 1.29 | 5.3, 0.85 | |
| Median (min., max.) | 15 (8, 25) | 14 (5, 25) | 14 (5, 25) | |
At month 3, the Y-SBNT group had a slightly lower average total SDQ score than the TAU group, with a mean difference of –0.7 points (95% CI –3.9 to 2.5), indicating that the Y-SBNT group experienced, on average, greater emotional well-being at month 3 than the TAU group. The associated treatment effect was calculated as 0.13 with an 80% one-sided confidence limit of 0.39. However, the direction of the effect reversed at month 12 to –0.15 in favour of the TAU group (Figure 6).
FIGURE 6.
Mean scores by treatment group for the subscales and the total score of the SDQ: (a) emotional symptoms scale; (b) conduct problems scale; (c) hyperactivity scale; (d) peer problems scale; (e) prosocial scale; and (f) total SDQ score. BL, baseline; M3, month 3; M12, month 12.

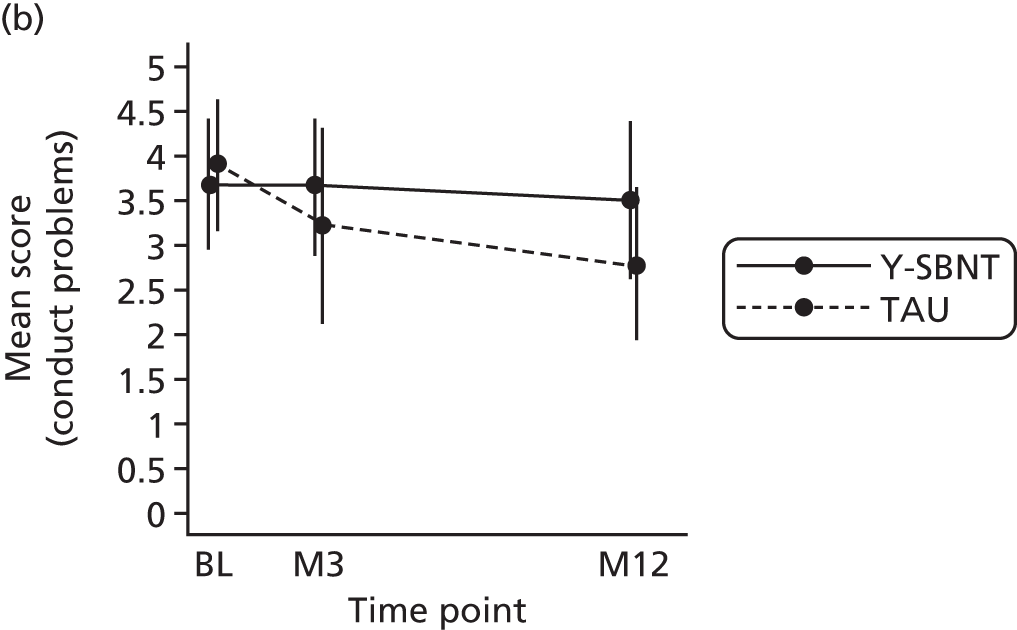


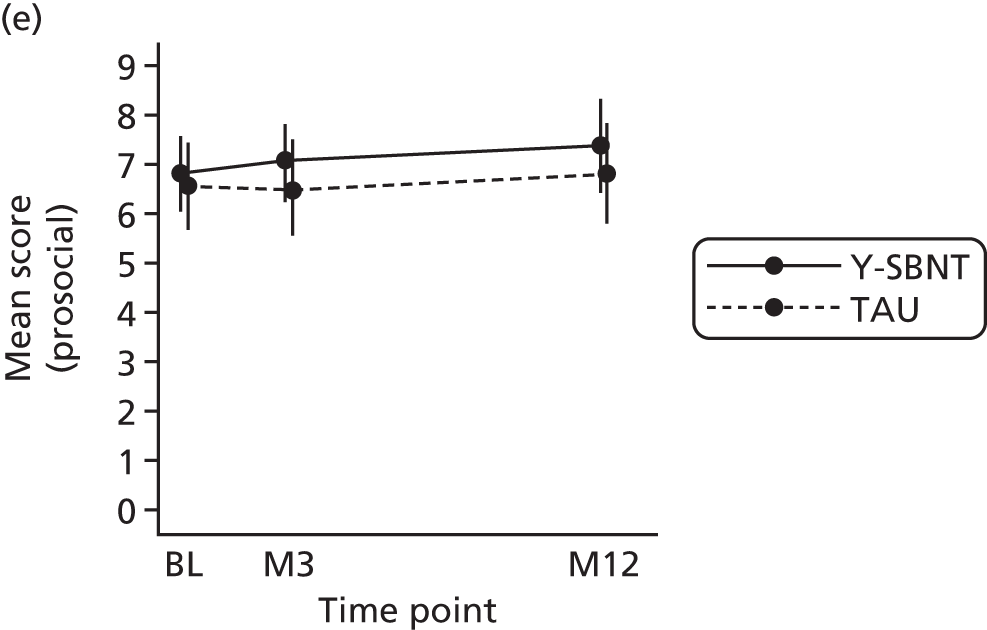
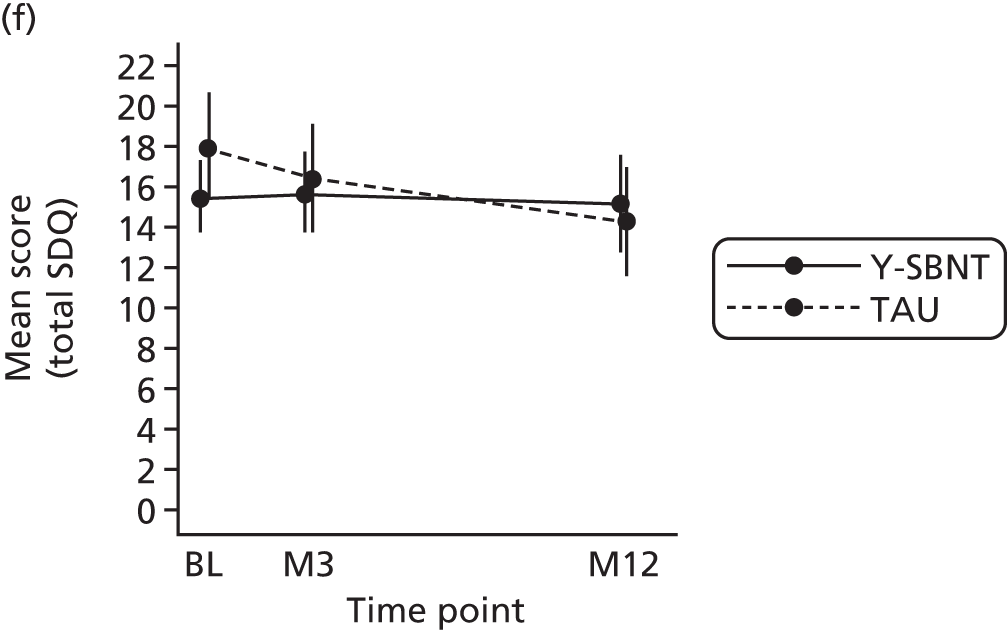
Among the young people who provided data at month 12, 25% in the Y-SBNT group (n = 5) and 15.8% (n = 3) in the TAU group had a total SDQ score that fell into the abnormal banding, which can be used to identify likely cases with mental health disorders (see Appendix 12).
The Y-SBNT group also had a higher mean impact score than the TAU group at month 12 (mean difference 0.5, 95% CI –0.8 to 1.9) and a larger proportion of participants fell into the abnormal banding for the impact score subscale (35.0% vs. 21.1%) (Table 14). In a similar trend to that seen for the total SDQ score, the direction of the effect reversed from being in favour of the Y-SBNT group at month 3 to being in favour of the TAU group at month 12.
| SDQ subscale | Y-SBNT (N = 26) | TAU (N = 27)a | Total (N = 53) | Mean difference (95% CI); effect sizeb |
|---|---|---|---|---|
| Impact scorec | ||||
| Baseline | ||||
| Valid n | 25 | 24 | 49 | – |
| Mean (95% CI) | 1.8 (0.9 to 2.7) | 2.0 (1.1 to 3.0) | 1.9 (1.3 to 2.5) | |
| SD, SE | 2.1, 0.42 | 2.2, 0.46 | 2.2, 0.31 | |
| Median (min., max.) | 1 (0, 6) | 1 (0, 8) | 1 (0, 8) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | –0.5 (–1.9 to 0.8); 0.26 (0.52) |
| Mean (95% CI) | 1.2 (0.6 to 1.7) | 1.7 (0.4 to 3.1) | 1.4 (0.8 to 2.1) | |
| SD, SE | 1.4, 0.29 | 2.7, 0.64 | 2.1, 0.32 | |
| Median (min., max.) | 0 (0, 4) | 0.5 (0, 10) | 0 (0, 10) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | 0.5 (–0.8 to 1.9); –0.25 (0.02) |
| Mean (95% CI) | 1.7 (0.6 to 2.7) | 1.1 (0.1 to 2.1) | 1.4 (0.7 to 2.1) | |
| SD, SE | 2.2, 0.49 | 2.0, 0.46 | 2.1, 0.34 | |
| Median (min., max.) | 1 (0, 7) | 0 (0, 6) | 0 (0, 7) | |
| Impact score bandings, n (%) | ||||
| Baseline | ||||
| Normal | 9 (36.0) | 9 (37.5) | 18 (36.7) | |
| Borderline | 7 (28.0) | 4 (16.7) | 11 (22.5) | |
| Abnormal | 9 (36.0) | 11 (45.8) | 20 (40.8) | |
| Month 3 | ||||
| Normal | 12 (52.2) | 9 (50.0) | 21 (51.2) | |
| Borderline | 2 (8.7) | 4 (22.2) | 6 (14.6) | |
| Abnormal | 9 (39.1) | 5 (27.8) | 14 (34.2) | |
| Month 12 | ||||
| Normal | 9 (45.0) | 13 (68.4) | 22 (56.4) | |
| Borderline | 4 (20.0) | 2 (10.5) | 6 (15.4) | |
| Abnormal | 7 (35.0) | 4 (21.1) | 11 (28.2) | |
| Since coming to the clinic, are your problems, n (%) | ||||
| Month 3 | ||||
| Much worse | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| A bit worse | 2 (8.7) | 1 (5.9) | 3 (7.5) | |
| About the same | 4 (17.4) | 6 (35.3) | 10 (25.0) | |
| A bit better | 9 (39.1) | 4 (23.5) | 13 (32.5) | |
| Much better | 8 (34.8) | 6 (35.3) | 14 (35.0) | |
| Month 12 | ||||
| Much worse | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| A bit worse | 2 (10.0) | 0 (0.0) | 2 (5.1) | |
| About the same | 5 (25.0) | 4 (21.1) | 9 (23.1) | |
| A bit better | 6 (30.0) | 7 (36.8) | 13 (33.3) | |
| Much better | 7 (35.0) | 8 (42.1) | 15 (38.5) | |
| Has coming to the clinic been helpful in other ways, e.g. providing information or making problems more bearable?, n (%) | ||||
| Month 3 | ||||
| Not at all | 2 (8.7) | 6 (33.3) | 8 (19.5) | |
| Only a little | 9 (39.1) | 3 (16.7) | 12 (29.3) | |
| Quite a lot | 8 (34.8) | 5 (27.8) | 13 (31.7) | |
| A great deal | 4 (17.4) | 4 (22.2) | 8 (19.5) | |
| Month 12 | ||||
| Not at all | 1 (5.0) | 1 (5.3) | 2 (5.1) | |
| Only a little | 8 (40.0) | 3 (15.8) | 11 (28.2) | |
| Quite a lot | 6 (30.0) | 14 (73.7) | 20 (51.3) | |
| A great deal | 5 (25.0) | 1 (5.3) | 6 (15.4) | |
A greater proportion of participants in the TAU group (78.9%) than in the Y-SBNT group (65.0%) said at month 12 that their problems were a bit or much better since coming to the clinic. Overall, the TAU group appeared to perform better than the Y-SBNT group in the constructs measured by the SDQ at 12 months post randomisation; those in the TAU group tended to experience slightly greater emotional well-being and the problems that they experienced had a lesser impact on their lives.
Important People Drug and Alcohol interview
At month 12, participants in the Y-SBNT group discussed a median of nine people (range 4–12, total 174) and those in the TAU group discussed a median of seven people (range 3–12, total 132) in the IDPA (Table 15). There were at most seven missing responses to a particular item across all participant responses at any one time point, indicating that missing data are not a significant problem when using the IPDA interview with this population.
| IPDA interview | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) |
|---|---|---|---|
| Network size | |||
| Baseline | |||
| Total number of people discussed | 263 | 249 | 512 |
| Median (min., max.) per YP | 11.5 (4, 12) | 10 (2, 12) | 11 (2, 12) |
| Month 3 | |||
| Total number of people discussed | 215 | 159 | 374 |
| Median (min., max.) per YP | 10 (0, 12) | 10 (3, 12) | 10 (0, 12) |
| Month 12 | |||
| Total number of people discussed | 174 | 132 | 306 |
| Median (min., max.) per YP | 9 (4, 12) | 7 (3, 12) | 7 (3, 12) |
| Proportion of network with whom the YP has daily contact, median (min., max.) per YP | |||
| Baseline | 0.32 (0.00, 0.92) | 0.33 (0.00, 1.00) | 0.33 (0.00, 1.00) |
| Month 3 | 0.33 (0.00, 0.71) | 0.41 (0.00, 1.00) | 0.33 (0.00, 1.00) |
| Month 12 | 0.27 (0.00, 0.67) | 0.38 (0.00, 1.00) | 0.33 (0.00, 1.00) |
| Proportion of family members in network, median (min., max.) per YP | |||
| Baseline | 0.67 (0.25, 0.92) | 0.67 (0.11, 1.00) | 0.67 (0.11, 1.00) |
| Month 3 | 0.67 (0.38, 0.92) | 0.63 (0.33, 1.00) | 0.67 (0.33, 1.00) |
| Month 12 | 0.80 (0.17, 1.00) | 0.89 (0.14, 1.00) | 0.80 (0.14, 1.00) |
| Proportion of network who use cannabis, median (min., max.) per YP | |||
| Baseline | 0.27 (0.00, 0.88) | 0.42 (0.00, 0.82) | 0.29 (0.00, 0.88) |
| Month 3 | 0.18 (0.00, 0.78) | 0.33 (0.00, 0.60) | 0.23 (0.00, 0.78) |
| Month 12 | 0.17 (0.00, 0.55) | 0.20 (0.00, 1.00) | 0.17 (0.00, 1.00) |
| Proportion of network who use other illicit substances, median (min., max.) per YP | |||
| Baseline | 0.00 (0.00, 0.50) | 0.00 (0.00, 0.50) | 0.00 (0.00, 0.50) |
| Month 3 | 0.00 (0.00, 0.25) | 0.00 (0.00, 0.30) | 0.00 (0.00, 0.30) |
| Month 12 | 0.00 (0.00, 0.18) | 0.00 (0.00, 0.57) | 0.00 (0.00, 0.57) |
| Proportion of network who drink alcohol, median (min., max.) per YP | |||
| Baseline | 0.60 (0.08, 1.00) | 0.67 (0.00, 1.00) | 0.63 (0.00, 1.00) |
| Month 3 | 0.58 (0.13, 1.00) | 0.50 (0.00, 0.92) | 0.58 (0.00, 1.00) |
| Month 12 | 0.46 (0.17, 100) | 0.50 (0.00, 0.89) | 0.50 (0.00, 1.00) |
The proportion of the network with whom participants have daily contact, who are family members and who use cannabis, alcohol or other substances is also summarised in Table 15 by treatment group and time point. On average at month 12, participants in the TAU group had daily contact with a greater proportion of their support network than those in the Y-SBNT group and family members tended to make up a greater proportion of their network; however, there was a slightly higher prevalence of cannabis and alcohol use among network members of participants in the TAU group, although the differences were marginal. z-Scores for the three components (network substance involvement, general/treatment support and network support for substance use) were calculated (Table 16 and Figure 7).
| IPDA interview | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) | Mean difference (95% CI); effect sizea |
|---|---|---|---|---|
| Component 1 version 1: network substance involvement | ||||
| Baseline | ||||
| Valid n | 26 | 25 | 51 | – |
| Mean (95% CI) | 0.04 (–0.35 to 0.44) | –0.05 (–0.47 to 0.38) | 0.00 (–0.28 to 0.28) | |
| SD, SE | 0.98, 0.19 | 1.03, 0.21 | 1.00, 0.14 | |
| Median (min., max.) | –0.05 (–1.28, 2.73) | –0.30 (–1.28, 2.01) | –0.09 (–1.28, 2.73) | |
| Month 3 | ||||
| Valid n | 18 | 17 | 35 | –0.11 (–0.80 to 0.59); 0.10 (0.38) |
| Mean (95% CI) | –0.05 (–0.54 to 0.43) | 0.06 (–0.48 to 0.59) | 0.00 (–0.34 to 0.34) | |
| SD, SE | 0.98, 0.23 | 1.05, 0.25 | 1.00, 0.17 | |
| Median (min., max.) | –0.23 (–1.15, 1.71) | –0.44 (–1.15, 1.81) | –0.23 (–1.15, 1.81) | |
| Month 12 | ||||
| Valid n | 16 | 15 | 31 | 0.36 (–0.38 to 1.09); –0.35 (–0.05) |
| Mean (95% CI) | 0.17 (–0.42 to 0.76) | –0.18 (–0.67 to 0.30) | 0.00 (–0.37 to 0.37) | |
| SD, SE | 1.11, 0.28 | 0.87, 0.23 | 1.00, 0.18 | |
| Median (min., max.) | –0.30 (–1.06, 2.09) | –0.31 (–1.06, 2.21) | –0.31 (–1.06, 2.21) | |
| Component 1 version 2: network substance involvement | ||||
| Baseline | ||||
| Valid n | 15 | 17 | 32 | – |
| Mean (95% CI) | 0.20 (–0.38 to 0.78) | –0.17 (–0.67 to 0.32) | 0.00 (–0.36 to 0.36) | |
| SD, SE | 1.05, 0.27 | 0.96, 0.23 | 1.00, 0.18 | |
| Median (min., max.) | 0.13 (–1.13, 2.22) | –0.40 (–1.40, 1.54) | –0.04 (–1.40, 2.22) | |
| Month 3 | ||||
| Valid n | 12 | 13 | 25 | 0.27 (–0.57 to 1.11); –0.26 (0.07) |
| Mean (95% CI) | 0.14 (–0.59 to 0.87) | –0.13 (–0.65 to 0.39) | 0.00 (–0.41 to 0.41) | |
| SD, SE | 1.16, 0.33 | 0.86, 0.24 | 1.00, 0.20 | |
| Median (min., max.) | –0.36 (–1.13, 2.31) | –0.06 (–1.36, 1.63) | –0.20 (–1.36, 2.31) | |
| Month 12 | ||||
| Valid n | 8 | 11 | 19 | 0.27 (–0.7 to 1.27); –0.26 (0.12) |
| Mean (95% CI) | 0.16 (–0.78 to 1.10) | –0.12 (–0.75 to 0.52) | 0.00 (–0.48 to 0.48) | |
| SD, SE | 1.12, 0.40 | 0.94, 0.28 | 1.00, 0.23 | |
| Median (min., max.) | –0.24 (–0.92, 2.07) | –0.49 (–0.96, 2.32) | –0.40 (–0.96, 2.32) | |
| Component 2: general/treatment support | ||||
| Baseline | ||||
| Valid n | 26 | 26 | 52 | – |
| Mean (95% CI) | –0.05 (–0.45 to 0.35) | 0.05 (–0.37 to 0.47) | 0.00 (–0.28 to 0.28) | |
| SD, SE | 0.98, 0.19 | 1.03, 0.20 | 1.00, 0.14 | |
| Median (min., max.) | –0.08 (–1.96, 1.57) | 0.16 (–2.49, 1.57) | 0.05 (–2.49, 1.57) | |
| Month 3 | ||||
| Valid n | 21 | 18 | 39 | –0.30 (–0.96 to 0.35); –0.30 (–0.03) |
| Mean (95% CI) | –0.14 (–0.55 to 0.27) | 0.16 (–0.39 to 0.72) | 0.00 (–0.32 to 0.32) | |
| SD, SE | 0.90, 0.20 | 1.11, 0.26 | 1.00, 0.16 | |
| Median (min., max.) | 0.14 (–2.60, 1.09) | 0.38 (–1.51, 1.48) | 0.23 (–2.60, 1.48) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | 0.13 (–0.53 to 0.78); 0.12 (0.39) |
| Mean (95% CI) | 0.06 (–0.32 to 0.44) | –0.07 (–0.63 to 0.50) | 0.00 (–0.32 to 0.32) | |
| SD, SE | 0.82, 0.18 | 1.18, 0.27 | 1.00, 0.16 | |
| Median (min., max.) | 0.21 (–1.69, 1.33) | 0.00 (–2.15, 1.33) | 0.13 (–2.15, 1.33) | |
| Component 3: network support for substance use | ||||
| Baseline | ||||
| Valid n | 26 | 27 | 53 | – |
| Mean (95% CI) | 0.18 (–0.27, 0.64) | –0.18 (–0.51, 0.16) | 0.00 (–0.28, 0.28) | |
| SD, SE | 1.12, 0.22 | 0.85, 0.16 | 1.00, 0.14 | |
| Median (min., max.) | 0.28 (–1.44, 2.11) | –0.04 (–1.44, 1.03) | 0.17 (–1.44, 2.11) | |
| Month 3 | ||||
| Valid n | 22 | 18 | 40 | 0.08 (–0.58 to 0.73); –0.07 (0.19) |
| Mean (95% CI) | 0.03 (–0.43 to 0.50) | –0.04 (–0.53 to 0.44) | 0.00 (–0.32 to 0.32) | |
| SD, SE | 1.04, 0.22 | 0.98, 0.23 | 1.00, 0.16 | |
| Median (min., max.) | –0.51 (–1.05, 2.39) | –0.51 (–1.58, 2.13) | –0.51 (–1.58, 2.39) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | 0.24 (–0.42 to 0.89); –0.23 (0.04) |
| Mean (95% CI) | 0.11 (–0.35 to 0.58) | –0.12 (–0.61 to 0.37) | 0.00 (–0.32 to 0.32) | |
| SD, SE | 1.00, 0.22 | 1.01, 0.23 | 1.00, 0.16 | |
| Median (min., max.) | –0.40 (–1.03, 1.82) | –0.40 (–1.67, 1.58) | –0.40 (–1.67, 1.82) | |
FIGURE 7.
Mean scores by treatment group for the component z-scores of the IPDA interview: (a) component 1 version 1: network substance involvement (primary substance); (b) component 1 version 2: network substance involvement (all drugs and alcohol); (c) component 2: general/treatment support; and (d) component 3: network support for substance use. BL, baseline; M3, month 3; M12, month 12.




A lower standard score is favourable for the two versions of component 1 and component 3 and indicates lower than average levels of primary substance (version 1) and all drugs and alcohol (version 2) involvement within the support networks and less encouragement of substance misuse, respectively. At month 12, participants in the Y-SNBT group had, on average, scores for both versions of component 1 and for component 3 that were higher than the population average. A higher score for component 2 indicates greater support for treatment and thus is favourable; members of the Y-SBNT group reported, on average, higher levels of support than members of the TAU group.
Family Environment Scale: Family Relationships Index
Each participant provided some data for this instrument at baseline; individual item data were complete for all participants except one (TAU group), who did not provide a response to two items (items 13 and 25). When participants were followed up at months 3 and 12, a response to each item of the FRI was received. There were several cases in which the participant either ticked both boxes or ticked in between the two boxes (baseline: seven items among four participants; month 3: nine items among four participants; month 12: two items among two participants). Standard scores for the cohesion, expressiveness and conflict subscales are summarised by treatment group and time point in Table 17. The Y-SBNT group had lower average scores for all three subscales at month 3 and month 12, indicating that members of the Y-SBNT group tended to experience higher levels of conflict and lower levels of cohesion and expressiveness in their family environment than the TAU group throughout their participation in the trial (Figure 8). The difference for the expressiveness scale was statistically significant. Floor and ceiling effects were explored using bar charts of individual items (see Appendix 13).
| FRI subscalea | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) | Mean difference (95% CI); effect sizeb |
|---|---|---|---|---|
| Conflict subscale | ||||
| Baseline | ||||
| Valid n | 26 | 27 | 53 | – |
| Mean (95% CI) | 62.0 (57.4 to 66.6) | 61.5 (56.7 to 66.2) | 61.7 (58.5 to 64.9) | |
| SD, SE | 11.4, 2.23 | 12.0, 2.32 | 11.6, 1.59 | |
| Median (min., max.) | 60 (39, 80) | 65 (44, 80) | 60 (39, 80) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | –2.7 (–9.8 to 4.3); –0.24 (0.02) |
| Mean (95% CI) | 61.4 (57.0 to 65.9) | 64.2 (58.2 to 70.1) | 62.6 (59.2 to 66.1) | |
| SD, SE | 10.3, 2.14 | 12.0, 2.83 | 11.0, 1.72 | |
| Median (min., max.) | 65 (44, 75) | 65 (44, 80) | 65 (44, 80) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | –2.4 (–9.8 to 4.9); –0.21 (0.06) |
| Mean (95% CI) | 64.2 (58.5 to 69.9) | 66.6 (61.6 to 71.7) | 65.4 (61.7 to 69.0) | |
| SD, SE | 12.1, 2.70 | 10.5, 2.41 | 11.3, 1.80 | |
| Median (min., max.) | 67.5 (33, 80) | 70 (44, 80) | 70 (33, 80) | |
| Cohesion subscale | ||||
| Baseline | ||||
| Valid n | 26 | 26 | 52 | – |
| Mean (95% CI) | 48.5 (43.6 to 53.3) | 45.6 (41.4 to 49.9) | 47.0 (43.9 to 50.2) | |
| SD, SE | 12.1, 2.36 | 10.5, 2.06 | 11.3, 1.56 | |
| Median (min., max.) | 52 (18, 65) | 48.5 (25, 59) | 52 (18, 65) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | –3.0 (–13.6 to 7.6); –0.18 (0.09) |
| Mean (95% CI) | 42.1 (35.1 to 49.1) | 45.1 (36.5 to 53.7) | 43.4 (38.2 to 48.6) | |
| SD, SE | 16.2 (3.38) | 17.3, 4.08 | 16.5, 2.58 | |
| Median (min., max.) | 45 (4, 65) | 52 (11, 65) | 52 (4, 65) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | –7.5 (–16.8 to 1.8); –0.52 (–0.24) |
| Mean (95% CI) | 42.7 (34.9 to 50.5) | 50.2 (44.9 to 55.5) | 46.4 (41.6 to 51.1) | |
| SD, SE | 16.8, 3.75 | 11.1, 2.54 | 14.6, 2.34 | |
| Median (min., max.) | 48.5 (4, 59) | 52 (25, 65) | 52 (4, 65) | |
| Expressiveness subscale | ||||
| Baseline | ||||
| Valid n | 26 | 26 | 52 | – |
| Mean (95% CI) | 41.8 (37.7 to 45.8) | 43.5 (38.7 to 48.4) | 42.7 (39.6 to 45.7) | |
| SD, SE | 10.1, 1.97 | 12.1, 2.37 | 11.0, 1.53 | |
| Median (min., max.) | 40 (22, 59) | 47 (22, 65) | 40 (22, 65) | |
| Month 3 | ||||
| Valid n | 23 | 18 | 41 | –10.8 (–17.6 to –4.0); –1.00 (–0.71) |
| Mean (95% CI) | 37.5 (33.0 to 41.9) | 48.3 (42.8 to 53.8) | 42.2 (38.5 to 46.0) | |
| SD, SE | 10.3, 2.14 | 11.1, 2.61 | 11.8, 1.85 | |
| Median (min., max.) | 40 (22, 53) | 50 (28, 65) | 40 (22, 65) | |
| Month 12 | ||||
| Valid n | 20 | 19 | 39 | –9.0 (–17.5 to –0.57); –0.68 (–0.40) |
| Mean (95% CI) | 40.7 (34.6 to 46.8) | 49.7 (43.5 to 56.0) | 45.1 (40.7 to 49.5) | |
| SD, SE | 13.1, 2.93 | 13.0, 2.98 | 13.7, 2.19 | |
| Median (min., max.) | 40 (16, 65) | 53 (28, 71) | 40 (16, 71) | |
FIGURE 8.
Mean scores by treatment group for the subscales of the FRI: (a) conflict subscale; (b) cohesion subscale; and (c) expressiveness subscale. BL, baseline; M3, month 3; M12, month 12.
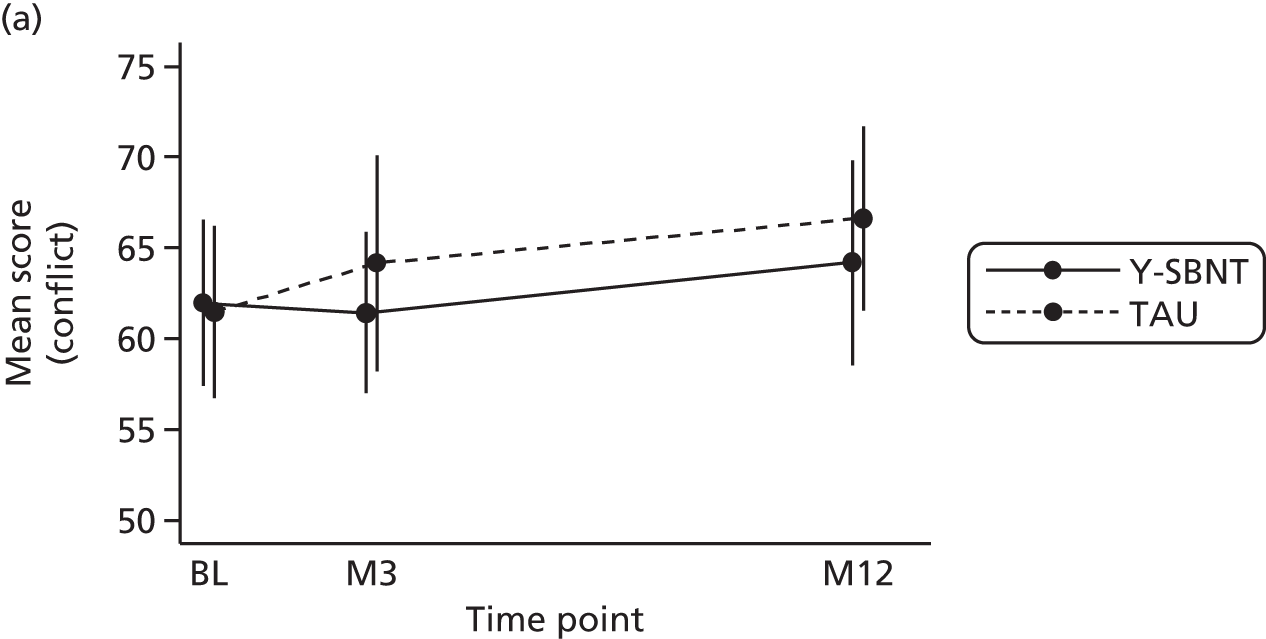
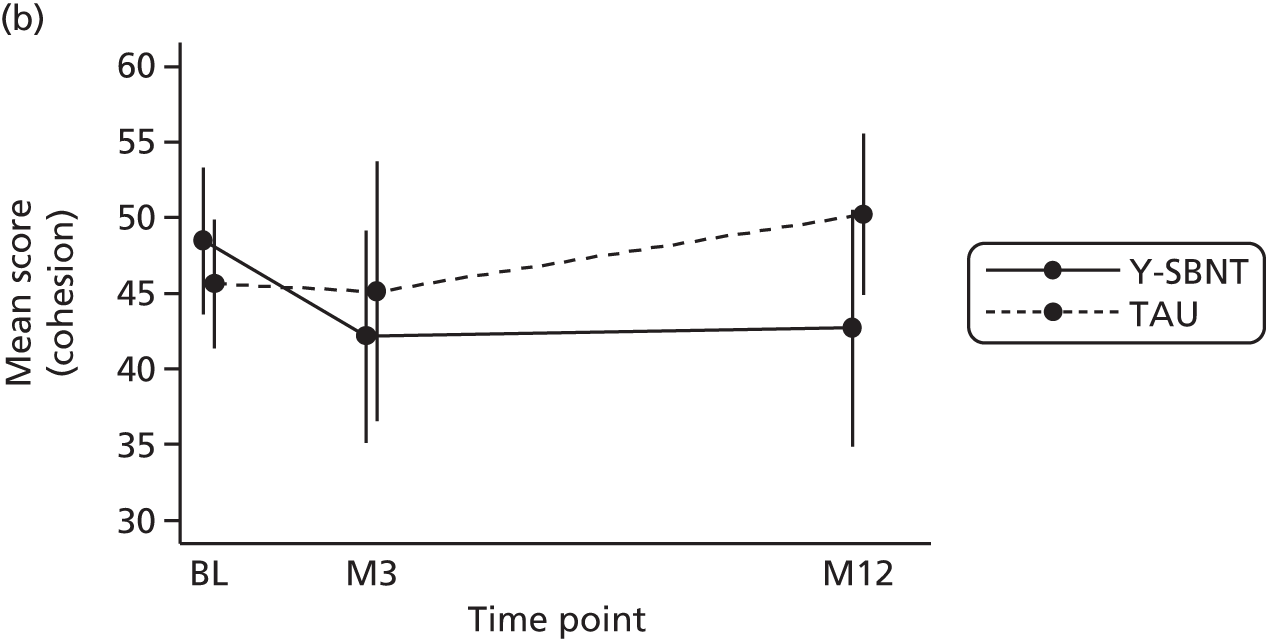

Working Alliance Inventory
Participants and therapists were asked to complete a WAI at the end of sessions 1 and 3. The number received as a percentage of the number of participants and therapists attending these sessions is presented by treatment group, session number and WAI type in Tables 18 and 19, respectively. Response rates in the Y-SBNT group were significantly higher than in the TAU group. The Y-SBNT group had a higher mean score than the TAU group for all three WAI subscales of both the patient and therapist instruments for each session, although the magnitude of the differences was notably larger for the therapist WAI (see Tables 18 and 19). This indicates that, on average, participants and therapists in the Y-SBNT group had a greater perceived strength of working alliance than those in the TAU group. Graphs of mean scores by session and treatment group are provided in Figure 9.
| Patient WAI subscale | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) |
|---|---|---|---|
| Session 1 | |||
| Number received/number expected (%) | 20/22 (90.9) | 8/20 (40.0) | 28/42 (66.7) |
| Tasks scale | |||
| Valid n | 20 | 7 | 27 |
| Mean (95% CI) | 22.6 (21.2 to 24.0) | 21.4 (18.9 to 23.9) | 22.3 (21.1 to 23.5) |
| SD, SE | 3.0, 0.67 | 2.7, 1.02 | 2.9, 0.56 |
| Median (min., max.) | 22.5 (18, 27) | 22 (18, 25) | 22 (18, 27) |
| Bond scale | |||
| Valid n | 18 | 8 | 26 |
| Mean (95% CI) | 23.0 (21.6 to 24.3) | 22.6 (20.4 to 24.9) | 22.9 (21.8 to 24.0) |
| SD, SE | 2.8, 0.65 | 2.7, 0.94 | 2.7, 0.53 |
| Median (min., max.) | 23 (18, 28) | 22.5 (18, 26) | 23 (18, 28) |
| Goal scale | |||
| Valid n | 17 | 8 | 25 |
| Mean (95% CI) | 22.7 (20.8 to 24.5) | 22.0 (19.4 to 24.5) | 22.5 (21.1 to 23.8) |
| SD, SE | 3.6, 0.88 | 3.1, 1.09 | 3.4, 0.68 |
| Median (min., max.) | 24 (17, 28) | 22.5 (17, 26) | 23 (17, 28) |
| Session 3 | |||
| Number received/number expected (%) | 14/18 (77.8) | 3/8 (37.5) | 17/26 (65.4) |
| Tasks scale | |||
| Valid n | 14 | 3 | 17 |
| Mean (95% CI) | 23.8 (21.9 to 25.6) | 21.7 (12.3 to 31.1) | 23.4 (21.7 to 25.1) |
| SD, SE | 3.2, 0.86 | 3.8, 2.19 | 3.3, 0.80 |
| Median (min., max.) | 24 (19, 28) | 20 (19, 26) | 24 (19, 28) |
| Bond scale | |||
| Valid n | 14 | 3 | 17 |
| Mean (95% CI) | 23.4 (21.8 to 25.1) | 22.3 (16.1 to 28.6) | 23.2 (21.8 to 24.6) |
| SD, SE | 2.9, 0.78 | 2.5, 1.45 | 2.8, 0.68 |
| Median (min., max.) | 24 (17, 28) | 22 (20, 25) | 24 (17, 28) |
| Goal scale | |||
| Valid n | 14 | 3 | 17 |
| Mean (95% CI) | 21.5 (19.5 to 23.5) | 20.3 (10.9 to 29.7) | 21.3 (19.5 to 23.1) |
| SD, SE | 3.5, 0.94 | 3.8, 2.19 | 3.5, 0.84 |
| Median (min., max.) | 21 (16, 26) | 22 (16, 23) | 21 (16, 26) |
| Therapist WAI subscale | Y-SBNT (N = 26) | TAU (N = 27) | Total (N = 53) |
|---|---|---|---|
| Session 1 | |||
| Number received/number expected (%) | 20/22 (90.9) | 11/20 (55.0) | 31/42 (73.8) |
| Tasks scale | |||
| Valid n | 20 | 11 | 31 |
| Mean (95% CI) | 23.4 (22.3 to 24.5) | 19.5 (18.2 to 20.9) | 22.0 (21.0 to 23.1) |
| SD, SE | 2.3, 0.50 | 2.0, 0.59 | 2.8, 0.51 |
| Median (min., max.) | 24 (17, 26) | 20 (16, 23) | 23 (16, 26) |
| Bond scale | |||
| Valid n | 19 | 10 | 29 |
| Mean (95% CI) | 24.1 (23.2 to 24.9) | 20.5 (19.5 to 21.5) | 22.8 (21.9 to 23.7) |
| SD, SE | 1.8, 0.41 | 1.4, 0.45 | 2.4, 0.44 |
| Median (min., max.) | 25 (20, 27) | 21 (17, 22) | 23 (17, 27) |
| Goal scale | |||
| Valid n | 19 | 11 | 30 |
| Mean (95% CI) | 23.5 (22.4 to 24.5) | 20.8 (19.4 to 22.3) | 22.5 (21.6 to 23.4) |
| SD, SE | 2.2, 0.50 | 2.2, 0.66 | 2.5, 0.46 |
| Median (min., max.) | 24 (18, 26) | 21 (17, 24) | 23 (17, 26) |
| Session 3 | |||
| Number received/number expected (%) | 16/18 (88.9) | 4/8 (50.0) | 20/26 (76.9) |
| Tasks scale | |||
| Valid n | 16 | 4 | 20 |
| Mean (95% CI) | 24.3 (23.3 to 25.3) | 18.0 (11.4 to 24.6) | 23.1 (21.4 to 24.7) |
| SD, SE | 1.9, 0.48 | 4.2, 2.08 | 3.5, 0.79 |
| Median (min., max.) | 24 (19, 28) | 18 (13, 23) | 24 (13, 28) |
| Bond scale | |||
| Valid n | 16 | 4 | 20 |
| Mean (95% CI) | 24.7 (23.8 to 25.5) | 21.3 (18.5 to 24.0) | 24.0 (23.0 to 25.0) |
| SD, SE | 1.7, 0.42 | 1.7, 0.85 | 2.2, 0.48 |
| Median (min., max.) | 25 (21, 28) | 21.5 (19, 23) | 25 (19, 28) |
| Goal scale | |||
| Valid n | 16 | 4 | 20 |
| Mean (95% CI) | 24.3 (23.4 to 25.1) | 19.5 (15.7 to 23.3) | 23.3 (22.1 to 24.5) |
| SD, SE | 1.6, 0.39 | 2.4, 1.19 | 2.6, 0.58 |
| Median (min., max.) | 25 (19, 26) | 18.5 (18, 23) | 24 (18, 26) |
FIGURE 9.
Mean patient and therapist WAI subscale scores by treatment group and session number: (a) patient tasks scale; (b) patient bond scale; (c) patient goal scale; (d) therapist tasks scale; (e) therapist bond scale; and (f) therapist goal scale.
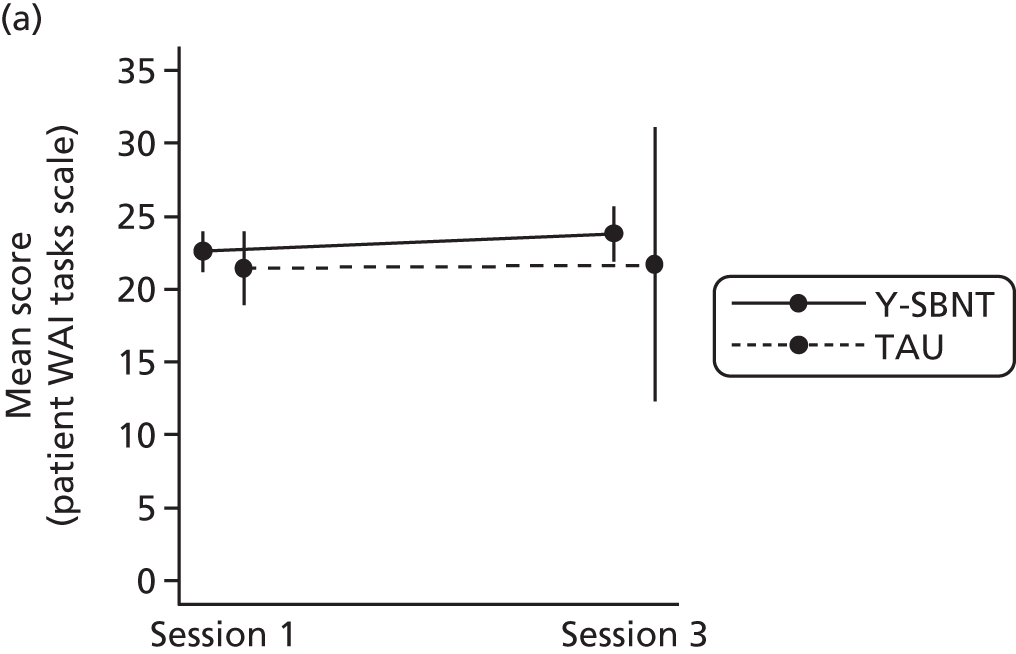
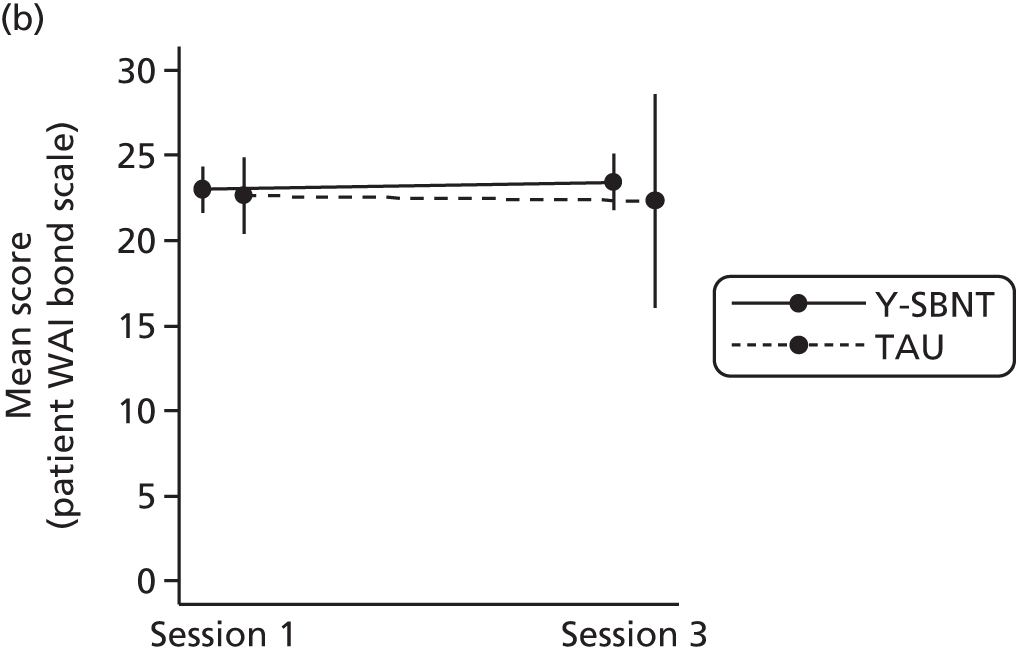
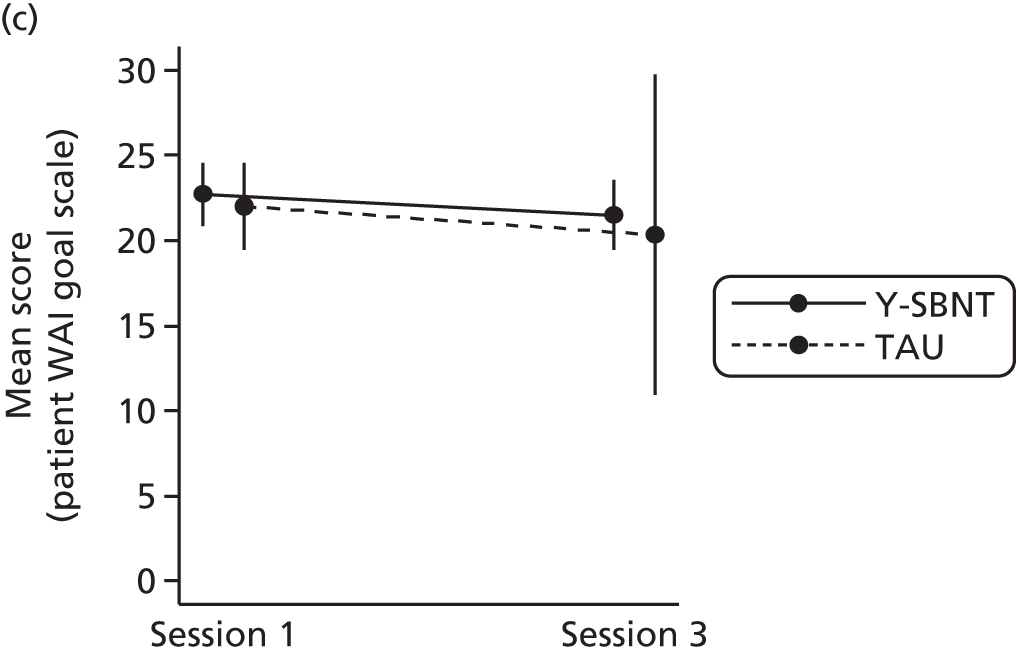
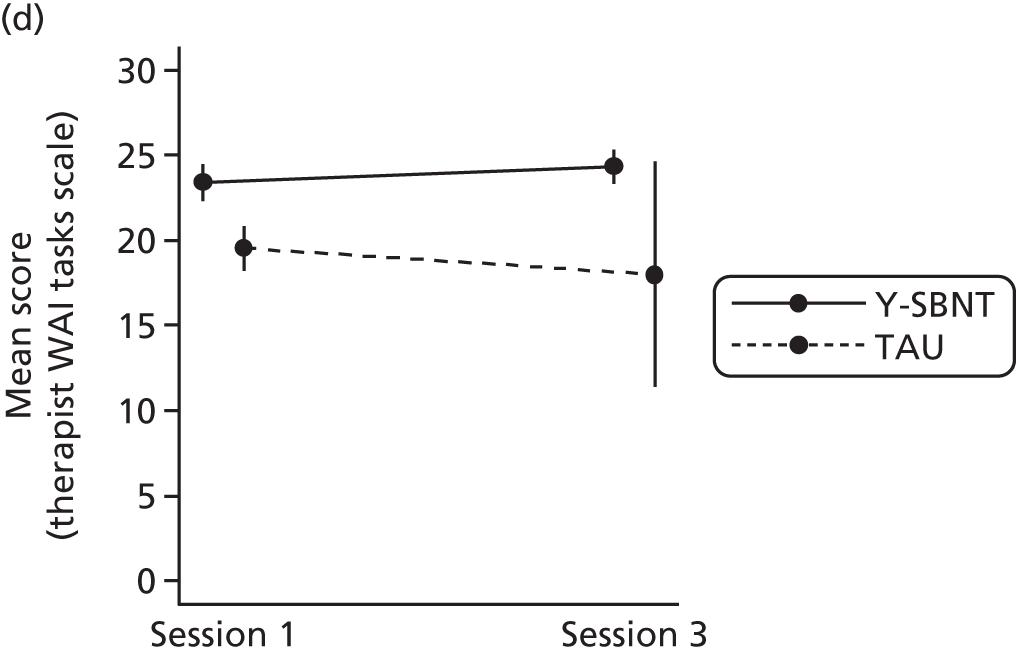

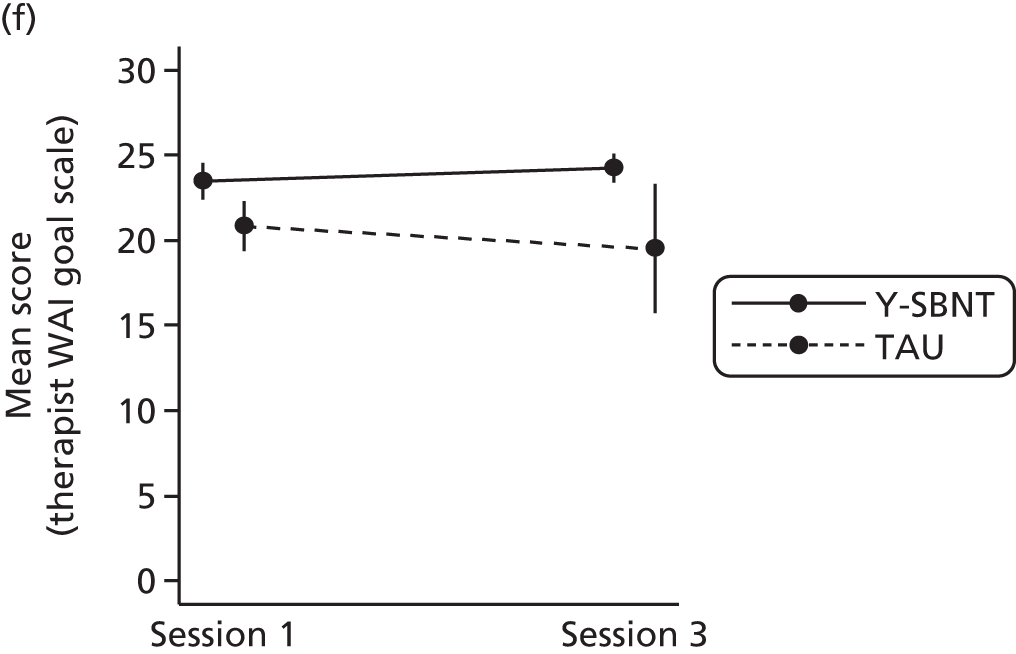
School attendance and engagement
At month 12, 10 (38.5%) participants in the Y-SBNT group and eight (29.6%) in the TAU group reported being in education in the previous 12 months. Among these, participants were absent from school within this time for a median of 4.5 days (range 0–60 days) in the Y-SBNT group and 20.5 days (range 1–140 days) in the TAU group. A median of 0 absent days (range 0–4 days) in the Y-SBNT group and 0 absent days (range 0–50 days) in the TAU group were the result of drug or alcohol misuse. In total, 11 participants (Y-SBNT, n = 4; TAU, n = 7) believed that their performance at school or college had been affected as a result of drug or alcohol misuse over the last 12 months: four slightly (Y-SBNT, n = 1; TAU, n = 3), six moderately (Y-SBNT, n = 3; TAU, n = 3) and one extremely (TAU).
Adverse events
No adverse events were reported.
Health economic data
The objective of the economic analysis was to explore the feasibility of a cost-effectiveness analysis for a full trial.
Missing data
Participants’ responses were considered missing if left blank or if answers were deemed unrealistic. Unrealistic answers included the number of days spent in a secure children’s home/young offender institution exceeding 365 days (in the last 12 months). When the option of ‘not answered’ was possible and selected, questions were considered answered and responses were therefore not considered missing.
Overall, the level of missing data appeared to be low (Table 20). There appeared to be a general missing data pattern, with missing data not more prevalent in the TAU group than in the Y-SBNT group or vice versa. Three questions showed a relatively higher level of missingness: (1) the number of times answered bail, (2) the number of contacts with a probation officer and (3) the total number of appearances at Crown Court. The ‘not answered’ responses were treated as missing in the complete case analysis. Overall, 17 questions had the option of ‘not answered’, of which seven received ‘not answered’ responses. The proportion of participants choosing ‘not answered’ ranged from 1.9% to 43.6%. The question on travelling in an ambulance had the highest percentage of ‘not answered’ responses (41.5% at baseline and 43.6% at 12 months). A slightly higher percentage of ‘not answered’ answers were seen at 12 months than at baseline.
| Service use | Y-SBNT | TAU | ||
|---|---|---|---|---|
| Baseline (n = 26) | 12 months (n = 20) | Baseline (n = 27) | 12 months (n = 19) | |
| Number of times visited by GP at home | 0 | 0 | 1 | 0 |
| Number of times visited by practice nurse at home | 0 | 0 | 1 | 0 |
| Number of times visited walk-in centre | 1 | 0 | 0 | 0 |
| Received prescriptions | 0 | 1 | 0 | 1 |
| Total nights in A&E | 0 | 1 | 2 | 3 |
| Number of times used an emergency (999) ambulance | 12 | 8 | 11 | 9 |
| Motor vehicle accident | 2 | 0 | 0 | 0 |
| Number of times had a motor vehicle accident | 4 | 0 | 0 | 0 |
| Attended hospital as a result of a motor vehicle accident | 4 | 0 | 0 | 0 |
| Personal injury accident | 1 | 0 | 0 | 0 |
| Number of times had a personal injury accident | 2 | 0 | 3 | 0 |
| Attended hospital as a result of a personal injury accident | 3 | 1 | 3 | 0 |
| Injury to another person | 2 | 0 | 0 | 0 |
| Number of times injury to another person | 3 | 0 | 2 | 0 |
| Attended hospital as a result of injury to another person | 5 | 1 | 1 | 0 |
| Description of accident | 2 | 0 | 1 | 0 |
| Accident related to drug or alcohol use | 2 | 0 | 1 | 1 |
| Number of times arrested for violence or assault against person | 0 | 0 | 1 | 0 |
| Number of times committed theft | 0 | 0 | 1 | 1 |
| Number of times committed vehicle theft | 0 | 0 | 1 | 1 |
| Number of times committed criminal damage | 0 | 0 | 1 | 0 |
| Number of times answered bail | 11 | 6 | 12 | 6 |
| Number of times had contact with probation officer | 9 | 2 | 11 | 3 |
| Number of days at Magistrates’ Court | 2 | 2 | 3 | 4 |
| Number of appearances at Crown Court | 12 | 10 | 16 | 10 |
| Number of days in a secure children’s home/young offender institution | 0 | 3 | 2 | 5 |
| Involvement with social services | 0 | 0 | 1 | 0 |
| Number of times visited by social worker at home | 1 | 0 | 4 | 2 |
| Number of times visited social worker at their office | 1 | 0 | 4 | 3 |
Costs
Intervention costs
Training costs for the Y-SBNT group consisted of the costs of 2 training days for each therapist including travel costs, the manual and the resource kit. Group supervision sessions were held twice a month either face-to-face or by telephone and lasted 1 hour at each site. Supervision costs included the cost of the supervisors’ time (n = 2) and the cost of the therapists’ time. We took into account that two therapists did not complete the whole intervention and deducted the associated costs. A whole afternoon group supervision meeting was also costed including travel costs for the therapists when applicable. An average hourly wage of £20 was used based on the information recorded by the research team to estimate the staff cost for the therapists. The supervisors’ hourly wages were recorded as £60.15 and £89.88. The manual and resource kit used for the training were priced at £28.99 each. All travel costs were estimated based on ticket prices from National Rail for the respective train journeys.
In the Y-SBNT group, the duration of three appointments was not known and so the standard session duration stated in the protocol (50 minutes) was used. In the TAU group, when the appointment length was not available, the average duration of the participant’s other attended appointments was used to estimate this value.
Because many participants often cancelled or did not turn up to appointments, some assumptions were made to cost this time. When it was stated in the treatment log that the participant cancelled and the therapist did not travel anywhere, it was assumed that the cancellation occurred with enough time for the therapist to reschedule something else. In this case no cost was incurred. However, if the log stated that the appointment was cancelled and the therapist did travel, we assumed that the therapist still went to the appointment and therefore both the time spent travelling and the 50-minute appointment were costed. If there was no statement of cancellation but the therapist did not put in a travel time, we assumed that there was no cost involved. If there was no statement of cancellation and the therapist travelled, we costed both the 50-minute appointment and the time spent travelling. By costing this way, we minimised the risk of underestimating staff costs. Travel costs were calculated using the NHS reimbursement rate, which is 56p per mile. 112
Table 21 presents a summary of the total intervention costs for both groups. On average, the Y-SBNT group had a higher total cost per person than the TAU group [£595 (SD £80) vs. £58 (SD £75)]. The results showed little difference between these two methods of analysis with regard to cost per person [Y-SBNT £590 (SD £76); TAU £57 (SD £75)].
| Cost component | Y-SBNT (n = 26) (£) | TAU (n = 24) (£) |
|---|---|---|
| Training | 6227 | – |
| Supervision | 5583 | – |
| Interventiona | 3630 | 1558 |
| Total | 15,440 | 1558 |
Health-care and social services costs
Table 22 shows the health service use at each time point by group. At baseline there appeared to be no great differences between the two groups in the numbers of participants reporting usage. Similarly, at 12 months, there was little indication of differences between the two groups in the numbers of participants reporting health service usage. In terms of differences between baseline and 12 months, the absolute numbers tended to show a decline in service use for both groups. However, because of loss to follow-up, the proportions of participants who used services varied. In the Y-SBNT group there was an increase of 18.2% in the proportion of participants receiving prescriptions and in the TAU group there was an increase of 6.6% between baseline and 12 months. The number of nights stayed in hospital as an inpatient in the Y-SBNT group remained the same (5 nights) between baseline and 12 months, but this represented a proportional increase of 30%. On the other hand, there was a decrease in accident and emergency (A&E) visits for both groups. This might indicate no specific trend for either group when loss to follow-up is considered.
| Health service use | Y-SBNT | TAU | ||
|---|---|---|---|---|
| Baseline (n = 26) | 12 months (n = 20) | Baseline (n = 27) | 12 months (n = 19) | |
| GP visits at surgery | 17 (52) | 12 (75) | 16 (78) | 12 (78) |
| Practice nurse visits at surgery | 8 (14) | 3 (9) | 6 (21) | 3 (11) |
| GP visits at home | 0 (0) | 0 (0) | 1 (1) | 0 (0) |
| Practice nurse visits at home | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Contacted NHS Direct (‘yes’) | 3 | 0 | 3 | 2 |
| Visited NHS walk-in centre | 9 (20) | 3 (4) | 9 (21) | 8 (10) |
| Received any prescriptions (‘yes’) | 11 | 10 | 16 | 12 |
| Visited hospital A&E department | 15 (44) | 10 (46) | 14 (33) | 9 (15) |
| Visited hospital A&E department (number of nights) | 4 (8) | 8 (43) | 0 (0) | 3 (6) |
| Travelled in a 999 ambulance | 9 (17) | 7 (37) | 7 (16) | 4 (5) |
| Stayed in hospital as an inpatient (number of nights) | 5 (21) | 5 (111) | 5 (10) | 4 (10) |
| Stayed in hospital as an inpatient (number of times)b | – | 5 (30) | – | 4 (4) |
| Visited hospital as outpatient | 8 (18) | 4 (26) | 9 (18) | 3 (9) |
| Motor vehicle accident | 2 (2) | 1 (1) | 2 (2) | 3 (6) |
| Motor vehicle accident and attended hospital | 1 (1) | 0 (0) | 1(1) | 1(1) |
| Personal injury | 9 (34) | 10 (12) | 9 (23) | 10 (19) |
| Personal injury and attended hospital | 7 (11) | 8 (9) | 6 (17) | 6 (7) |
| Injury to another person | 7 (31) | 5 (20) | 8 (26) | 7 (24) |
| Injury to another person and attended hospital (number of times attended hospital) | 3 (5) | 2 (2) | 2 (6) | 3 (6) |
| Involvement with social services (‘yes’) | 13 | 5 | 15 | 10 |
| Number of times visited by social worker at homec | 8 (133) | 3 (169) | 9 (149) | 6 (45) |
| Number of times visited social worker at their officec | 6 (26) | 3 (13) | 1 (6) | 1 (2) |
For the health service use questions some outliers were found. At 12 months, one participant in the TAU group reported 30 GP visits at surgery and one participant in the Y-SBNT group reported 48 visits. The same participant in the Y-SBNT group was an outlier for three different questions, all at 12 months (30 visits to A&E, 30 nights in A&E and 30 times used an emergency ambulance). Two participants in the Y-SBNT group also reported considerably longer hospital stays than other participants (40 and 45 nights).
A set of national average unit costs was extracted from several sources (Table 23). After excluding those with missing cost or EQ-5D-5L data, the set of unit costs was applied to the usage data presented in Table 22. The resultant health-care and social services costs are presented in Table 24 for the complete case and available case analysis by time point. The complete case analysis shows that both groups appear to have similar level of health-care and social services costs at baseline. However, at 12 months the Y-SBNT group had higher costs, which is partly attributable to one participant with a health-care and social services cost of > £20,000. If this outlier is excluded, the cost per person reduces to £1388. The available case results are slightly lower than the complete case results; however, the differences between the two groups are similar in both analyses.
| Service use | Unit cost (£) | Source |
|---|---|---|
| GP consultation (in surgery) | 38 | Curtis106 |
| GP consultation (home visit) | 62 | Curtis106 |
| Practice nurse consultation (in surgery) | 11 | Curtis106 |
| Practice nurse consultation (home visit) | 18 | Curtis106 |
| NHS walk-in clinic | 56 | Curtis106 |
| Inpatient admission | 562 (per night) | Department of Health113 |
| Emergency medicine | 124 | Department of Health113 |
| Ambulance conveyance | 231 | Department of Health113 |
| Outpatient attendance | 114 | Department of Health113 |
| Prescription cost per year | 163 (average per head) | Health and Social Care Information Centre114 |
| Social worker (home visit) | 66 | Curtis106 |
| Social worker (at office) | 55 | Curtis106 |
| Cost (£) | Y-SBNT | TAU | ||||||
|---|---|---|---|---|---|---|---|---|
| Complete case | Available cases | Complete case | Available cases | |||||
| Baseline (n = 16) | 12 months (n = 16) | Baseline (n = 24) | 12 months (n = 19) | Baseline (n = 11) | 12 months (n = 11) | Baseline (n = 21) | 12 months (n = 13) | |
| Mean (SD) health-care and social services cost per participant | 1933 (2916) | 2150 (5517) | 1719 (2460) | 1899 (5073) | 1564 (2166) | 724 (405) | 1402 (1756) | 683 (384) |
| Total group health-care and social services cost | 30,930 | 34,403 | 41,244 | 36,081 | 17,205 | 7964 | 29,427 | 8876 |
Figure 10 demonstrates the change in cost per person from baseline to 12 months. Whereas costs in the TAU group fall, in the Y-SBNT group there is an increase in costs.
FIGURE 10.
Comparison of health-care and social services costs per person between groups at baseline and 12 months (complete case).
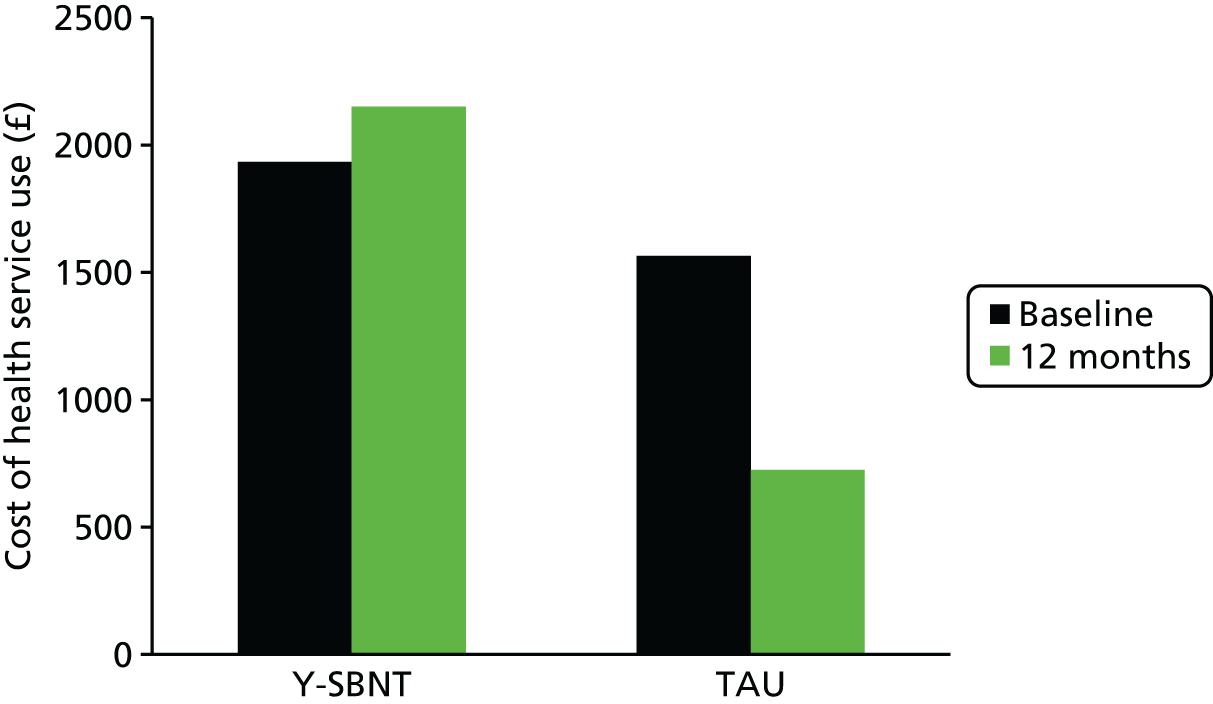
In this section, an open question in the questionnaire regarding social services use should be noted because of its ambiguous phrasing. First, this question did not specify the recall period for involvement with social services as the last 12 months. As a result, some participants recalled contact with social services over their entire life at both baseline and 12 months, which could have resulted in double counting at the 12-month follow-up. Second, the term ‘involvement’ posed confusion with regard to whether this question referred to the participant personally or included other family members as well, with a few answers referring to siblings/parents/children who had received social care. Because of this the costs reported above did not include this question, but did include two other questions regarding use of social services. A summary of the responses for this question can be found in Appendix 14.
Policing and criminal justice costs
Table 25 reports the use of policing and criminal justice services. As for health service use, the results indicate that there were not great differences between groups at baseline in the reporting of involvement with criminal justice services. There appears to be no specific trend in change between baseline and 12 months for either group.
| Service use | Y-SBNT | TAU | ||
|---|---|---|---|---|
| Baseline (n = 26) | 12 months (n = 20) | Baseline (n = 27) | 12 months (n = 19) | |
| Committed violence or assault against a person | 12 (46) | 6 (28) | 16 (61) | 7 (22) |
| Arrested for violence or assault against a person | 9 (16) | 5 (14) | 6 (15) | 2 (2) |
| Committed sexual offence | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Arrested for sexual offence | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Committed robbing/mugging | 5 (6) | 1 (1) | 5 (16) | 0 (0) |
| Arrested for robbing/mugging | 6 (7) | 1 (1) | 2 (2) | 0 (0) |
| Committed burglary in a dwelling or commercial premises | 4 (4) | 3 (3) | 2 (8) | 5 (10) |
| Arrested for burglary in a dwelling or commercial premises | 4 (4) | 3 (3) | 2 (5) | 4 (5) |
| Committed theft (not of vehicle) including shoplifting | 9 (28) | 5 (11) | 7 (159) | 2 (53) |
| Arrested for theft (not of vehicle) including shoplifting | 7 (10) | 4 (8) | 7 (72) | 2 (7) |
| Committed vehicle theft | 2 (253) | 4 (5) | 2 (6) | 1 (8) |
| Arrested for vehicle theft | 1 (1) | 2 (2) | 2 (43)b | 1 (1) |
| Committed criminal damage | 9 (16) | 2 (5) | 10 (23) | 2 (4) |
| Arrested for criminal damage | 6 (9) | 2 (5) | 7 (11) | 2 (4) |
| Committed drink driving | 1 (1) | 1 (1) | 1 (1) | 1 (1) |
| Arrested for drink driving | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Committed other motoring offences | 2 (21) | 1 (3) | 2 (4) | 3 (21) |
| Arrested for other motoring offences | 1 (1) | 1 (3) | 0 (0) | 2 (13) |
| Answered bail | 1 (4) | 5 (9) | 7 (22) | 5 (28) |
| Contact with probation officer | 4 (9) | 3 (70) | 6 (287) | 4 (380) |
| Appeared in court (total number of days in Magistrates’ Court) | 11 (27) | 9 (35) | 17 (53) | 8 (43) |
| Appeared in court (total number of appearances at Crown Court) | 1 (2) | 1 (1) | 3 (12) | 3 (13) |
| Time in secure children’s home/young offender institution (total number of days) | 0 (0) | 1 (60) | 4 (364) | 2 (210) |
There are some noticeable outliers within the criminal justice service use analysis. One participant (Y-SBNT group) recorded 250 incidences of vehicle theft at baseline. Another participant (TAU group) recorded 250 contacts with a probation officer at baseline and 300 contacts at 12 months. The validity of these responses is questionable; however, without further investigation they cannot be ruled out as they are technically feasible. Two participants in the TAU group reported that they spent > 365 days in a secure children’s home/young offender institution (540 days and 600 days), which is implausible. These responses were therefore treated as missing.
A set of national average unit costs was extracted to estimate the policing and criminal justice costs. The costs were inflated when applicable (Table 26).
| Service use | Unit cost (£) | Sources |
|---|---|---|
| Arrest, caution or penalty disorder notice | 2796 | Field,115 Curtis116 and HM Treasury117 |
| Magistrates’ Court appearance | 639 | Phillips and Brown,118 HM Courts & Tribunal Service,119 Legal Services Commission,120 Crown Prosecution Service,121 HM Courts & Tribunal Service Governance and Assurance Data and Information Disclosures, Ministry of Justice, freedom of information request by e-mail (9 April 2014), Crown Prosecution Service, freedom of information request by e-mail (7 April 2014) |
| Crown Court appearance | 11,586 | |
| Probation | 4371 | Ministry of Justice,122 Ministry of Justice and National Offender Management Service123 |
| Young offender institution (for male aged 15–17 years) | 196 (per day) | Ministry of Justice and National Offender Management Service123 |
Table 27 summarises the criminal justice costs for the available cases. The question on appearances in court was assumed to be missing only if both parts were unanswered. If only one part was missing, we assumed that the other part was left blank because the participant did not appear at both courts and so the unanswered section was assumed to be zero usage. The reported appearances at Crown Court seemed unrealistic as young people of this age group are unlikely to attend Crown Court. 124 One participant reported appearing at Crown Court but recorded no arrests. The TAU group had consistently higher criminal justice costs and saw an increase in criminal justice costs per participant from baseline to 12 months. In contrast, the Y-SBNT group saw a fall in mean costs from baseline to 12 months. However, it should be noted that the change in involvement in the criminal justice system does not necessarily reflect participants’ behaviour in the same time period, especially for court proceedings, as there may be a time lapse between the detection of the offence and the court proceedings.
| Cost (£) | Y-SBNT | TAU | ||
|---|---|---|---|---|
| Baseline (n = 24) | 12 months (n = 17) | Baseline (n = 24) | 12 months (n = 16) | |
| Mean (SD) criminal justice cost per participant | 8653 (9139) | 7017 (12,995) | 30,419 (52,976) | 34,694 (54,172) |
| Total group criminal justice cost | 207,677 | 119,289 | 730,048 | 555,106 |
Total costs
The mean total cost per participant over the 12-month trial period is presented in Table 28 for both groups. The results for the complete case and sensitivity analysis, using mean imputation, are shown. For these analyses only intervention and health-care and social services costs are included. Including criminal justice costs for complete cases would result in too few participants and would weaken the results for the primary NHS and personal social services perspective. For the complete case analysis, both the unadjusted and adjusted for baseline total costs results are presented. Bootstrapping was used to generate 95% CIs for these adjusted mean costs. The total costs for the sensitivity analysis were calculated using mean replacement to impute the missing cost data. The results in Table 28 can indicate the direction of the cost impact of the intervention; however, any results should be interpreted with caution because of the small sample size.
| Cost item | Y-SBNT | TAU | ||
|---|---|---|---|---|
| Complete case (n = 16), mean (SD) (£) | Mean imputation (n = 26), mean (SD) (£) | Complete case (n = 11), mean (SD) (£) | Mean imputation (n = 27), mean (SD) (£) | |
| Intervention | 152 (88) | 140 (80) | 42 (45) | 58 (75) |
| Total intervention (including training and supervision) | 605 (88) | 594 (80) | 42 (45) | 58 (75) |
| Health-care and social services costs | 2150 (5517) | 1896 (4304) | 724 (405) | 683 (846) |
| Unadjusted total cost (NHS and personal and social services perspective) | 2756 (5520) | 2490 (4308) | 766 (392) | 740 (259) |
| Complete case (n = 16), mean (bootstrapped 95% CI) (£) | Complete case (n = 11), mean (bootstrapped 95% CI) (£) | |||
| Adjusted total cost (NHS and personal and social services perspective)a | 2756 (1465 to 4464) | 481 (–768 to 2038) | ||
From a NHS and personal and social services perspective, Y-SBNT appears to be more costly because of higher intervention costs and greater health-care and social services costs. This is more evident when total costs are adjusted for baseline. The bootstrapped 95% CIs reveal the uncertainty surrounding these means. In particular, the 95% CI for the TAU group ranges from a negative value to a cost almost four times greater than the presented mean.
Because of the small sample size and the level of missing data, criminal justice costs were not taken into account in this analysis. However, a simple examination of the numbers indicates that, from a wider societal perspective, TAU might be more costly than Y-SBNT.
It should be noted that, although a wider societal perspective was considered, we did not take into account the costs of the network members who attended the intervention sessions. The reason for this is that, although the relationship of the network members to the participants was always recorded, the number of network members was often missing in the questionnaire. Four appointments were attended for which there were no data regarding the presence of network members. Of the 99 appointments attended, 20 were recorded as having network members present. Twelve of the 26 participants recorded having a network member present for at least one appointment. The number of appointments at which a network member was present ranged from one to four, with the majority of participants having a network member present at only one or two appointments. Of these 12 participants all reached at least appointment four, with 58% (n = 7) attending all six sessions. Of the remaining 14 participants, 71% (n = 10) attended at least one appointment and 40% (n = 4) of those completed all six sessions. However, 40% (n = 4) of these participants did not make it past session 2. This could imply that having a network member present for at least one session may help decrease early dropout. However, it is also possible that this is a consequence of the engagement and motivation of the participants themselves. The maximum number of network members present at an appointment was three.
The following categories of network members were involved:
-
parent
-
foster carer
-
teacher
-
substance misuse worker
-
counsellor
-
youth centre staff
-
social worker
-
care worker.
Five of the 12 participants who reported having a network member present for at least one appointment were accompanied to at least one session by a parent and three were accompanied by school-related personnel. The remaining participants were generally accompanied by support workers from social services or charitable organisations. The data also indicate that there was a disparity between therapists in engaging the network members. Two therapists successfully engaged network members for all of their participants (n = 6/6 and 3/3) whereas two other therapists had a very low engagement rate with network members (n = 2/7 and 1/5) and one did not engage with any network members (n = 0/5).
Health-related quality of life
EuroQol-5 Dimensions data were collected with all other components in the questionnaire. Apart from those lost to follow-up there were no missing data in this section.
Figures 11 and 12 show the results for the complete cases, defined as those participants who answered the EQ-5D-5L at baseline, 3 months and 12 months. Figure 11 shows the proportion of severity category in each domain for Y-SBNT. At baseline, the anxiety/depression domain was the only domain in which extreme problems were reported, whereas the self-care domain was the domain with the highest percentage of participants reporting no problems.
FIGURE 11.
EuroQol-5 Dimensions complete case results by domain in the Y-SBNT group at (a) baseline; (b) 3 months; and (c) 12 months.

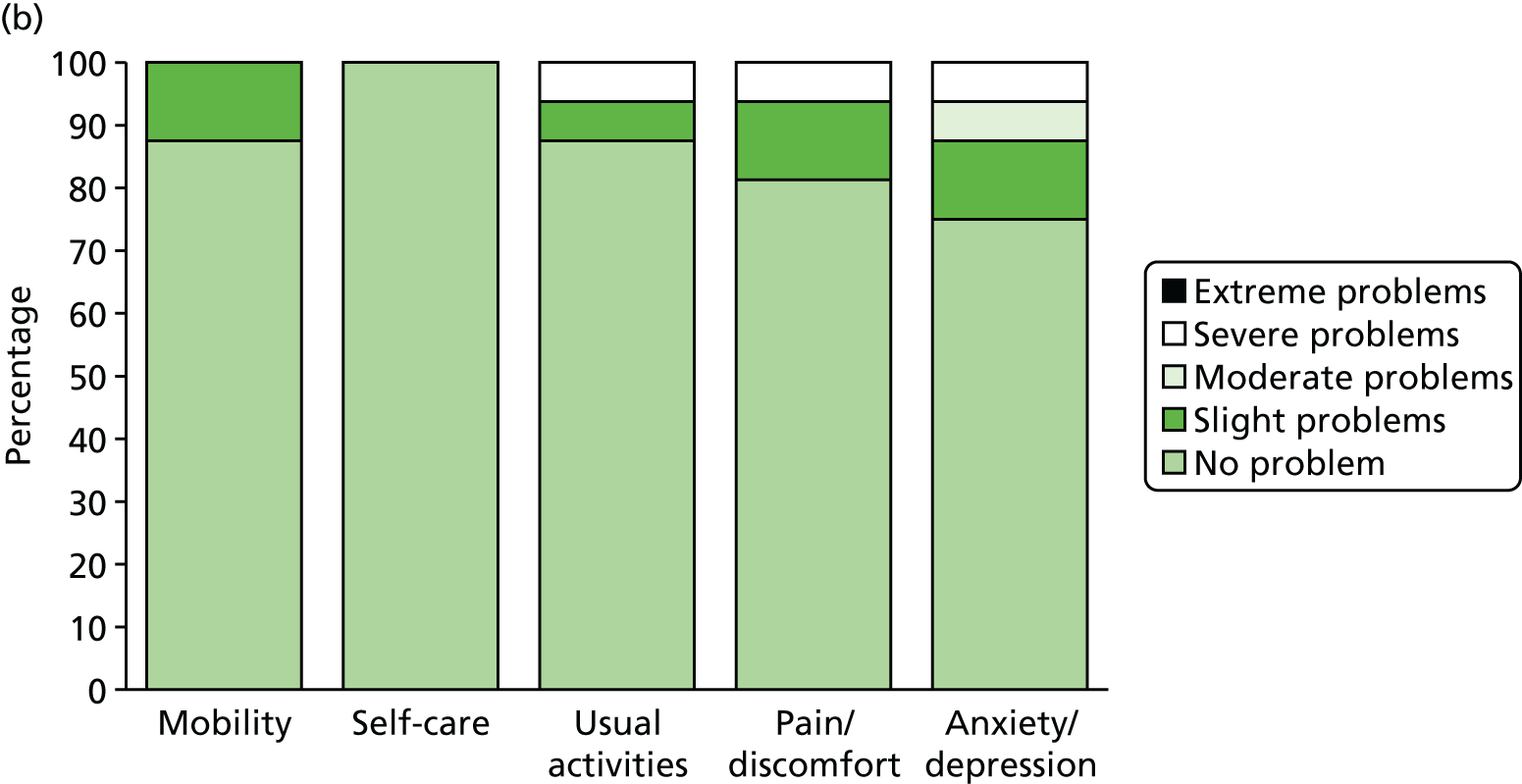

FIGURE 12.
EuroQol-5 Dimensions complete case results by domain in the TAU group at (a) baseline; (b) 3 months; and (c) 12 months.



The results at 3 months reveal an increase in those reporting severe problems within the anxiety/depression, pain/discomfort and usual activities domains. In the anxiety/depression domain there was a fall in the percentage reporting no problems, but now no participants experienced extreme problems in any domain. Overall, Figure 11 demonstrates how there was an increase in the percentage of participants in the Y-SBNT group reporting no problems in the anxiety and depression domain from baseline to 12 months. There was also a general decrease in the percentage reporting slight problems and moderate problems for this domain, but reports of extreme problems were again seen at 12 months.
Figure 12 presents the EQ-5D-5L results at all three time points for the TAU group. A lower percentage of participants in the TAU group than in the Y-SBNT group reported no problems in the mobility, pain/discomfort and anxiety/depressions domains at baseline. Moreover, a larger percentage reported slight problems across the domains, which was particularly prevalent in the anxiety/depression domain. There were no reports of severe or extreme problems across any domain or at any time point. There was an increase in the percentage reporting no problems in the anxiety/depression domain from baseline to 12 months in the TAU group. Overall, the TAU group saw a greater improvement across all domains than the Y-SBNT group.
Figure 13 reports the mean index score for each group at each time point. Although both groups show signs of improvement within the complete case analysis, this improvement is greater for the TAU group because of the group’s lower baseline score but higher 12-month score. The mean imputation results show the TAU score to be much lower than the Y-SBNT score across all three time points. This suggests that, for the TAU group, those with missing data and those lost-to-follow-up are the participants with the worst index scores. This difference is not nearly as pronounced for Y-SBNT, with the mean imputation analysis giving very similar results to the complete case analysis. Adjusting for baseline had little effect on the results for Y-SBNT; however, the overall improvement for TAU was reduced.
FIGURE 13.
EuroQol-5 Dimensions mean index score at each time point. a, Mean imputation; b, complete case analysis adjusted for baseline.

Table 29 presents the mean VAS score at each time point for each group. Three participants were missing at 3 months but were then seen again at 12 months (TAU, n = 2; Y-SBNT, n = 1). The complete case analysis for the VAS includes those participants who had no missing VAS data, without taking into account the missing data for costs and the EQ-5D-5L index, as both are unrelated to the VAS results. The complete case results reveal that the mean VAS scores for the Y-SBNT group are greater at all three time points than the equivalent VAS scores for the TAU group. On the other hand, the available case results show that the TAU group has a greater mean score than the Y-SBNT group at 12 months. This result is more in line with the complete case results for the EQ-5D-5L index score analysis.
| Group | Complete case Y-SBNT | Available case TAU | ||||
|---|---|---|---|---|---|---|
| Baseline | 3 months | 12 months | Baseline | 3 months | 12 months | |
| Y-SBNT | 81.8 (12.4) (n = 19) | 84.3 (19.3) (n = 19) | 80.8 (19.2) (n = 19) | 75.96 (15.75) (n = 26) | 81.60 (18.73) (n = 23) | 78.75 (20.77) (n = 20) |
| TAU | 75.1 (13.9) (n = 17) | 76.7 (18.2) (n = 17) | 80.6 (13) (n = 17) | 70.85 (16.97) (n = 27) | 76.61 (17.63) (n = 18) | 79.47 (12.68) (n = 19) |
Figure 14 shows that the median VAS score for the TAU group increases from baseline to 3 months, but then remains unchanged at 12 months. In contrast, the median VAS score for the Y-SBNT group increases from baseline to 3 months and then falls back to the baseline score at 12 months. Again, this contrasts with the EQ-5D-5L index score results, which showed that those in the Y-SBNT group experience worse scores at 3 months. However, different definitions of ‘complete case’ have been used, which may partly explain this contradiction. The size of the box plot at 12 months shows greater dispersion for Y-SBNT than for TAU. However, more outliers are seen in the TAU group than in the Y-SBNT group across all three time points. The skewness of the data is mostly symmetrical across all box plots except for the TAU group at 12 months, for which the median is lower.
FIGURE 14.
Comparison of VAS scores between groups and across time points (complete case).

Summary
Recruitment to this study was marginally below target but the required sample size of 32 patients (16 per group) with TLFB outcome data was achieved at all time points. In addition, follow-up rates were > 73% and the majority of young people attended at least one treatment session. The effect size for the proportion of days that the main problem substance was used was below zero and the upper one-sided 80% confidence limit was –0.05, indicating that the desired effect size of 0.3 for the main trial is unlikely to be achieved.
It was not an objective of this feasibility trial to investigate the cost-effectiveness of the intervention but rather to pilot the service use questionnaire and assess the feasibility of conducting a full economic evaluation in a hypothetical future definitive trial. Therefore, in this small feasibility study, the results should be interpreted with caution and be seen only as a preliminary indication of impact. Several problems emerged with regard to the structure of the health service questionnaire used within this study and a number of required changes were identified. These are reported in Appendix 15. Because of the more structured and intense nature of Y-SBNT and the necessary initial training costs, the intervention cost was unsurprisingly higher for the Y-SBNT group than for the TAU group. Health-care and social services costs were far greater for the Y-SBNT group than the TAU group at 12 months, partly because of outliers. As for policing and criminal justice costs, they appeared to be considerably higher in the TAU group, which was consistent from baseline to 12 months. The EQ-5D-5L results showed that the TAU group was in a worse condition in terms of quality of life measures than the Y-SBNT group at baseline, but improvement appeared to be more steady and significant in the TAU group. The small sample size can lead to bias, which has been shown by the Y-SBNT group having the high cost of secondary care and the higher baseline EQ-5D-5L scores, and this is particularly prominent when mean imputation is used.
Chapter 6 Qualitative results
This chapter presents data obtained during the follow-up interviews with young people, their families/network members and therapists in the Y-SBNT study arm. The intention of these interviews was to explore the acceptability of the intervention to the young people and the wider context of the impact of the intervention. This was used to complement the analysis of the quantitative data and identify ways in which Y-SBNT may need to be modified in preparation for any future definitive trial. The interviews were semistructured and took place with young people in the Y-SBNT experimental group and their families/network members at 3 months post randomisation. The views of the therapists delivering the intervention and a service manager were explored at a single time point following the completion of the interviews with the young people. Thematic analysis methods109,110 were used to analyse the data. Further details of the methodology used are provided in Chapter 3.
Young people’s views
Seventeen young people were interviewed about their experiences of taking part in the feasibility study and whether or not they found the new treatment approach acceptable. This included nine young people in the West Midlands (all male, aged 15–18 years), whose primary substances were cannabis (n = 8) and alcohol (n = 1), and eight young people in the North East (four males and four females aged 12–17 years), whose primary substances were cannabis (n = 3), mephedrone (n = 2), alcohol (n = 1), NPS (n = 1) and solvents (n = 1). When treatment exposure was low, the young people found it difficult to remember details of the sessions that they attended. In addition, some young people provided one-word responses throughout the interview; this was predominant among those young people referred from the youth offending system. Eight themes were identified from what the young people said about their experiences: young people’s lives before treatment, entry to treatment, involving family/social network, treatment goals, treatment outcomes, treatment experience, treatment suggestions and experience of the research process. Complete and additional quotations for each theme are provided in Appendix 16.
Young people’s lives before treatment
An important theme identified was that of seeing young people in the context of their whole lives and not just focusing on their referral to a drug and alcohol support service. There was a mix of young people who lived with family members or relatives and young people who were in social care or living in a hostel or with foster carers. A few young people aged > 16 years had independent living arrangements with social services involvement. For those involved in the care system this could bring uncertainty to their lives:
Not being able to settle and that, not knowing what’s going to happen and not knowing where I’m going, puts more stress on us.
Young person 1032, female, 14 years, mephedrone
The majority of the young people attended school (both mainstream and pupil referral units)/college or training courses. For those not in training or education this had implications for their well-being. If in care and also not attending school/college or training, this could have a serious impact on how they spent their time:
Because the thing is, when you’re in the [hostel], I was basically independent, so I could go out when I wanted and I could sleep when I wanted.
What were you doing, if you don’t mind me asking?
Begging.
Young person 1031, male, 17 years, NPS
Therefore, any potential intervention should be viewed in the light of the challenging nature of some young people’s lives, in that their substance misuse may be symptomatic of other more challenging circumstances that they are experiencing.
Entry to treatment
For the vast majority of young people it was their first experience of drug and alcohol treatment. Referral sources included school/college, social workers and the youth offending system. Only a few young people perceived their drug or alcohol use as a problem for them:
Yeah, I went into the YOT when I went to collect my money and I had a word with someone there and I said that I think I’ve got a problem.
Young person 1020, female, 17 years, mephedrone
In the main, the young people did not view their substance use as a problem themselves before attending treatment services:
It was strong use, it was nothing major.
Young person 1000, male, 17 years, cannabis
Why did you think it wasn’t a problem for you?
Because it was making me happy.
Young person 1032, female, 14 years, mephedrone
They also said that their friends did not perceive their drug and alcohol use as an issue, as many of them were also using substances:
How about your friends, did they see it as a problem?
No. They see it as fun.
Is it because they’d been taking it with you?
Yeah.
Young person 1001, male, 16 years, cannabis
Nevertheless, they did recognise that their behaviour was causing concern to those close to them, particularly close family members:
They [mum] were really worried ‘cause the way I was dramatically losing weight; the way I looked.
Young person 1020, female, 17 years, mephedrone
None of the young people specifically mentioned coercion or pressure to enter drug and alcohol treatment but for some of them referred from the youth offending system they perceived treatment as part of an order that they were obliged to complete:
What was the reason why you attended the young people’s service?
It was part of my probation order.
Young person 1008, male, 18 years, alcohol
Involving family/social network
The majority of young people recalled identifying positive and negative influences in their social network as part of their treatment and generally said that they found this exercise useful:
Yeah it was useful because you sit back and you analyse the people around you like . . . It makes you actually sit there and think about what I was getting involved in . . . it’s just a wake-up call really.
Young person 1028, male, 17 years, cannabis
Was that [drawing a network diagram] useful for you?
Yeah, that’s why I’ve stopped hanging around with certain people.
Young person 1002, male, 15 years, cannabis
In a number of cases in the West Midlands the young people did not recall being asked to invite supportive others to their treatment sessions:
Did you ever discuss inviting people into your sessions?
No.
Did he [therapist] ever ask you, do you want to bring a friend or a family member?
No, he never said anything like that. I just wouldn’t bring any of my friends into probation with me, you know. I wouldn’t do it.
OK, so things like that you wouldn’t really like to discuss with family?
No, I wouldn’t. I don’t know, I just don’t involve other people in like what are my things.
Young person 1010, male, 17 years, cannabis
Among those young people with whom the therapist discussed inviting supportive others to their treatment, some were very clear that they wanted to receive treatment on a one-to-one basis and that their substance use was something that they preferred to deal with on their own:
No, I would never take my mum.
No, why’s that?
She’d feel embarrassed, I don’t want that.
Young person 1001, male, 16 years, cannabis
I just don’t like talking to people I’m close to. I keep everything in, I don’t like talking.
Young person 1013, female, 14 years, alcohol
It’s about me, no one else [it’s] private.
Young person 1019, male, 17 years, cannabis
The young people mentioned that the involvement of others in their treatment was an individual choice and should be discussed with them before it took place. Young people having an impact on decision-making and being kept informed of what was happening was perceived as important:
If they wanted to ask and you could make it an option, like at the first session you could say, you can have people, like family and friends if you want them here.
Young person 1033, female, 12 years, solvents
Those young people who agreed to have others attend their sessions generally found this to be a positive experience:
Did you find their [teacher] involvement supportive?
Yeah because he was saying like when . . . because stuff that he’s seen me do . . . and I don’t really notice it and he was telling me and I was just laughing because I didn’t even know what I do.
Young person 1002, male, 15 years, cannabis
In addition to attending sessions, young people with network members involved in their treatment were able to provide examples of how supportive others, mostly family members, were better able to help them:
My sister used to just stay in with me and just play on the PlayStation which keeps me out of trouble.
Young person 1021, male, 15 years, cannabis
Treatment goals
For the young people who did not receive their later treatment sessions, discussion of treatment goals did not feature strongly in their accounts. In setting and agreeing treatment goals, some young people really appreciated that the goals did not exclusively focus on their drug and alcohol use. Examples included doing alternative activities and improving family relationships:
I remember that we spoke about positive things taking over the smoking like replacing it with something, like gym or things and I have done that and that’s worked out.
Young person 1014, male, 17 years, cannabis
You said you didn’t really talk about the drug use so much, it was more about getting back with your family or getting a better relationship.
Aye, which . . . well, it’s kind of happened, so . . .
Young person 1031, male, 17 years, NPS
A number of young people also mentioned that it was helpful that there was enough flexibility within the goal-setting component to talk about life objectives:
It was good because . . . it wasn’t always talking about the drugs . . . we were talking about my life and in general . . . so it was like a mixture.
Young person 1032, female, 14 years, mephedrone
What I want to do with my life. Like my future and what I would do and how much better it would be.
Young person 1033, female, 12 years, solvents
For the majority of young people who set goals relating to their substance use this was about cutting down as opposed to abstinence:
Do you remember any of your goals?
Like cutting down and that. Smoking less a week and then certain like specific days when I would and wouldn’t.
Right, yeah, and that’s worked do you think?
Aye, aye, it helped.
Young person 1041, male, 15 years, cannabis
Treatment outcomes
A number of young people reported that treatment had a minimal or no impact on their substance use and/or social relationships. Two main issues appeared to influence the treatment journey of these young people: lack of exposure to the active components of treatment, especially not engaging a network of support and/or setting agreed goals, and/or referral from the youth offending system, with young people tending not to perceive their substance use as problematic and being resistant to involving network members in their treatment:
It hasn’t changed like nothing; you know what I’m saying? Like it hasn’t changed me in any other way like . . .
Young person 1010, male, 17 years, cannabis
For some young people their substance use continued or increased because of external factors such as relationship breakdowns or moving to hostel accommodation with peers who were also using substances:
I was going out with my girlfriend and then I broke up with her. That’s why I started smoking again.
Young person 1002, male, 15 years, cannabis
Yeah it’s got more frequent [drinking] purely on the fact of who I hang around with and who I talk to and that.
Yeah, because you live in a hostel now . . .
Yeah.
Young person 1008, male, 18 years, alcohol
Having close friends who continued to use substances made it challenging for young people to maintain the changes that they had made to their substance use intake:
It’s hard to keep away from it. When you smell it; when [boyfriend’s] got that thing in his mouth and you smell it and you still want it. I mean I wanted to stop it. But you still have that urge because of how happy it makes you.
Young person 1020, female, 17 years, mephedrone
However, other external factors such as having a supportive family could have protective effects on continued use:
It was just trying to like think about my family and that . . . like keeping them happy and that.
Young person 1041, male, 15 years, cannabis
Regardless of positive or negative environmental factors, some of the young people who on entry to treatment did not perceive their substance use as problematic admitted their ambivalence to living a life without continued drug or alcohol use:
Like I said earlier, I would happily cut down on my cannabis, but as long as I can have it when I’m annoyed or if I’m on a weekend and I should be free to have it, as long as I’m in control of it.
Young person 1031, male, 17 years, NPS
The majority of young people who successfully engaged with treatment reported experiencing positive changes in their substance use. One young person in the West Midlands said that he had cut down from up to 20 cannabis joints a week to one:
Before you started seeing [therapist] how much were you smoking then?
10 or 20 a week.
10 or 20 a week, that’s quite a lot because now you’re only smoking . . .?
One joint a week.
About one joint a week and that’s shared?
Yeah.
Young person 1000, male, 17 years, cannabis
Another young person mentioned that he changed his perceptions and drinking habits as he learned from the therapist that it was better to drink occasionally to avoid the consequences of binge drinking. Having the opportunity to reflect on their substance use and realise the impact that it was having on their lives gave some of the young people the motivation to enact change.
Most of the young people who made positive changes in their substance use also reported better relationships with the network supporters who attended treatment sessions and with their family members:
I just speak to him [teacher who took part in sessions] like a normal person because normally I don’t speak to teachers.
You speak to him. You feel that you could talk to him about things?
Yeah, like a mate.
Young person 1002, male, 15 years, cannabis
How did things change with your family?
Just more talking; well me demanding talking and they’d listen.
Young person 1020, female, 17 years, mephedrone
However, for some young people from difficult backgrounds, although they engaged successfully in treatment, any positive changes had to be considered within the wider context of their lives:
Things will never get better with me and my family. I think it’s because I was in care and they feel sorry for us, so that’s what I eventually think it is, because to be fair I’ve never had so much attention within my family since I’ve gone into care. I think it’s just trying to look good on the local authority’s behalf.
Obviously you are not using or anything like that, so you do more fun things?
Well, still like doing things that aren’t allowed by the law.
Young person 1032, female, 14 years, mephedrone
Perhaps an unintended consequence of the Y-SBNT approach of appraising social networks was that, although some young people were able to successfully distance themselves from friends who were a negative influence on their substance use, this could lead to isolation if other supportive friends or peers were not readily accessible:
So why was the relationship with your friends worse do you think?
Because they are different, they had all done the same thing as me, but I didn’t want to do it no more, but they did.
Young person 1013, female, 14 years, alcohol
In what way did it [relationships] change?
My family got closer but I had to push away all my friends. I’ve got no friends now.
You’ve got no friends now? Well who do you hang out with normally?
No-one!
Young person 1028, male, 17 years, cannabis
In terms of wider outcomes, some young people reported other positive changes in their lives. Examples included being able to budget money better, having more energy to perform other pleasant activities to increase well-being and feeling less angry and more content with themselves.
A few young people with more complex needs mentioned that they were not entirely satisfied with the outcomes from the treatment that they received. One young person with co-occurring mental health difficulties said that the treatment that he received was too short and that he was reluctant to accept further help from Child and Adolescent Mental Health Services (CAMHS):
I don’t want to talk to someone because I don’t want to be opening up to them and telling them my problems again and going over it. What’s the point like? He [therapist] hasn’t helped me. I’m still at the same stage when he opened up my case.
Young person 1019, male, 17 years, cannabis
Another young person expressed general satisfaction with his treatment but said that he was still experiencing problems with sleeping.
Treatment experience
It was apparent for the young people who engaged in treatment that their relationship with the therapist was a key factor in maintaining that engagement and the positive changes that they experienced through treatment.
This included having initial trust in the therapist and feeling that the therapist was providing relevant information:
What did you expect when you first sat down with [therapist] then?
I probably thought I was going to get grassed up. That’s what my first thought was but then when he told me it was just between us it was all right.
Young person 1002, male, 15 years, cannabis
Also important was helping the young people gain insight into their behaviour and being supported throughout the process:
It’s the way she [therapist] makes me understand everything like; I’ve still got to understand myself and [therapist] just pushes me to try to understand a little bit more . . . I don’t like talking about my feelings and the way [therapist] puts it, it makes it easier to talk about it . . . Yeah. Even if I didn’t attend them [sessions] I’d come the next day and she’d be there.
Young person 1020, female, 17 years, mephedrone
Finally, feeling able to talk openly about their thoughts and feelings, not just confined to their substance use, and having a therapist who understood their situation and responded appropriately was key:
I liked the fact that we could talk on a level, you know, I didn’t have to worry about saying anything. I could just blurt it out basically and tell him anything that I was worrying about or that I wanted to do and he’d help me with it.
Young person 1014, male, 17 years, cannabis
They [therapist] understand your circumstances and that. There are some people that pretend they know where you are coming from and I’m just, like, you are just lying really. Then you know when someone actually knows where you are coming from because they respond in a way I know that they understand me.
Young person 1032, female, 14 years, mephedrone
However, some young people, particularly those ambivalent about their substance use and referred from the youth offending system, perceived their treatment as part of probation and hence had a more negative view about the treatment that they received, although one young person mentioned that much more support was provided in contrast to their experience of adult probation services, which they were now involved with:
No, it’s just a meeting, isn’t it? So it’s just probation. I just see it as probation really.
Young person 1010, male, 17 years, cannabis
How did you find working with [therapist]?
It’s all right but it was just boring being there.
Was there anything in particular that you found boring?
Just the work!
Was there anything that you thought would improve this?
No. It’s not supposed to be good; same as probation.
And why do you think that didn’t work for you?
I don’t know, because I didn’t want to do anything.
Young person 1043, male, 15 years, cannabis
I got a lot more help from the YOT than what I do now with adult probation. There was more support and meetings every week.
Young person 1028, male, 18 years, cannabis
Treatment suggestions
There were mixed views from the young people about treatment length. A few young people referred from the youth offending system felt that the treatment that they received was too long and that six sessions should be the maximum amount. For some young people, six sessions felt like the right amount for them:
Yeah I think the six sessions were helpful. They were spread out as well. It weren’t like they were every week. Sometimes you’d say, oh I can’t come this week, you know what I mean. It would give me a little break, time to think and stuff like that was helpful. It was right, it was perfect. It was never hurried.
Young person 1014, male, 17 years, cannabis
Even those who were happy with six sessions said that the appropriate amount of sessions should depend on the individual and their perceived level of need. The majority of young people said that they would have preferred more sessions, with responses ranging from eight to twelve 1-hour sessions in a time frame of 3–6 months. A couple of young people mentioned that they would prefer ongoing support depending on their needs and for the treatment not to be time limited:
I would just have preferred for her [therapist] to just always be there . . . I don’t think there should be a limited time because if you are going into depth about something.
Young person 1032, female, 14 years, mephedrone
One young person found early morning sessions problematic and another was sceptical that a treatment based solely on talking was the best approach; a health scare would be required to motivate them to change and they would prefer integrating activities as a better treatment option:
I think if people had more activity, something to occupy their mind, then they might see it a bit different thinking these people took us out to go and do this, we could do that and we’re going to stop smoking this, do you know what I mean?
Young person 1028, male, 17 years, cannabis
Experience of the research process
Despite the fact that several questionnaires had to be completed at baseline and 3 and 12 months’ follow-up the young people tended to find this process acceptable:
Aye. If it were where you were like, oh, write this, it would have been totally different, probably would have got ripped up, but if it’s something where it’s tick or draw, it’s fine.
Young person 1031, male, 17 years, NPS
Aye, I didn’t really mind it. The questions all made like sense, to be honest.
Young person 1041, male, 15 years, cannabis
A number of young people even commented that they found completing the questions quite helpful. Reasons included observing how their substance use and/or social network changed and that young people’s experiences/lives were considered in the questions:
It changed quite a lot. The people that are around have changed. You don’t expect, oh I’ve been doing this much now, this much now, and so on. It actually makes you think about how much the intake actually is.
Young person 1008, male, 18 years, alcohol
Yes, that was interesting, that was, like, interesting to know that someone is actually considering their life, their personal life, if you know what I mean. They were all relevant, yes.
Young person 1032, female, 14 years, mephedrone
One young person suggested making the process more fun to involve some creativity; another found that one of the questions on the FES was not relevant to his situation:
Was there anything that was really difficult or you thought, oh, why are you asking this?
The one about family members hitting each other.
You thought that wasn’t relevant.
No.
So it’s a bit extreme.
Yes.
Young person 1021, male, 15 years, cannabis
In general the young people said that they would be happy to take part in a similar study in the future if they needed help with their substance use and found it a useful experience:
Yes, I wouldn’t feel that I needed it if I was older, but being a kid and under 18 then yes probably.
Why? What’s the difference do you think?
Only because when you’re 18 you’re like a responsible adult I think, so therefore, you make your own choices.
Young person 1032, female, 14 years, mephedrone
Do you think that it was a worthwhile experience taking part?
Yes. You’re going to ask why?
Why?
Because of the gift vouchers and helping other people.
Young person 1033, female, 12 years, solvents
Network members’ views
Perhaps reflecting the focus on following up the young people, which was challenging, and the level of network engagement achieved within treatment, the researchers managed to interview only two network members from the North East. More comprehensive quotations from network members can be found in Appendix 17.
Both network members reported positive experiences of being involved in the young person’s treatment:
It’s been very helpful.
Network member 1021, mother
That’s been very clear and I think that’s been translated to [young person] what those goals are as well. She’s not been left in any doubt as to what the whole idea behind us all working with her was for, so it’s been positive.
Network member 1033, teacher
However, this involvement appeared to be more supportive in nature than involving agreed actions discussed in treatment:
I was more looking after me [sic.] son and making sure he wasn’t going out with the wrong crowd.
And did [therapist] talk to you about that and give advice about what things to do?
Well a little bit.
Network member 1021, mother
I didn’t know specifically what [therapist’s] activities were with [young person] from session to session. I kind of just knew that the overall aim was for [young person] to be aware of her substance abuse and what it could lead to and what the dangers were with it.
Network member 1033, teacher
When specific actions were mentioned these were more practical and based around attendance at sessions or checking that the young person was happy to meet with the therapist:
Did you see your responsibility as making sure that [young person] was attending his sessions?
Yeah, make sure he was here [home] on time.
Network member 1021, mother
I was very much confident that the relationship that was being built up with [therapist] and [young person] was right and that I could see that [young person] was getting a lot out of it. So I didn’t quiz her in any detail about it but I had obviously at other times said, oh [therapist’s] coming in and how do you feel about that? Oh yes its fine. We’d have a little bit of a chat but I wouldn’t ever question her.
Network member 1033, teacher
Despite more peripheral involvement both network members reported positive outcomes of the approach for the young person, particularly in terms of strengthening relationships:
Communication has improved, I know when he has taken green [cannabis] and we are able to talk about it in a certain way.
Network member 1021, mother
I can see a big impact on [young person] just even around school. She seems a lot calmer, just a lot more settled really you know. Obviously through it all as well our relationship with dad’s been strengthened I think. You know the fact that he’s seen that it’s from all of us, you know, multi-agency approach you know we are all having that support there for [young person], it’s definitely helped.
Network member 1033, teacher
Both network members were complimentary about the therapist’s approach and outreach work. The mother of a young person was clear that her son would not have engaged in treatment if the therapist had not shown flexibility in providing home visits.
Therapists’ views
Three therapists from the West Midlands service and two therapists from the North East service were interviewed. Nine themes were identified from their experiences of delivering the new treatment. These were training and supervision for treatment delivery, treatment approach, experience of delivering treatment, treatment engagement, involving family/social network, treatment goals, comparison with TAU, integration with existing practice and experience of the research process. For brevity, extensive illustrative quotations to support the narrative accounts for each theme are provided in Appendix 18.
Training and supervision for treatment delivery
The two North East therapists talked in detail about their experiences of the training and supervision received to deliver the new treatment.
Overall, training was a positive experience. However, because of the fact that they were the first group of therapists to deliver the new approach, they felt that there was a lack of case material relating specifically to young people, which would have been helpful to ground the treatment with likely scenarios that they might face. They also mentioned that it would have been useful to have more guidance on session content while dealing with a young person in crisis:
Just a bit more clarity about sort of crisis sessions and what they should look like. In future training should have examples of what’s the best way to go about that without it impacting on what we’re supposed to be doing.
Nevertheless, they felt that when issues emerged during treatment implementation that were not addressed comprehensively in training, the trainers were very responsive in providing supplementary information. Having expert trainers who they could contact as the need arose was also found to be very beneficial.
The two North East therapists held joint supervision sessions with the trainers and both found this arrangement very helpful in terms of increasing their learning and understanding of the new treatment. As an extension of this they appreciated having the opportunity to share practice with the West Midlands therapists at a group supervision session held in the West Midlands:
Like we could see how the other group [West Midlands] were working, we could see how we were doing it differently [engaging more with young person’s network] and that kind of spurred us on a little bit.
Although both therapists had a generally positive view of the training and supervision provided, in addition they reported performing reflective practice and peer supervision throughout the duration of the study, which really helped to enhance their understanding and application of the new treatment approach:
It [reflective practice] worked really well and we were able to kind of constantly feed back and reflect on our own practices and how we could improve it. We wanted it to be the best it could be for those young people.
Treatment approach
All five therapists were positive about the new treatment and could see value in the approach. They particularly highlighted the structure that it provides as a key strength, with a logical sequence of sessions that provided clarity both to the therapist and to the young person. Although the new treatment was much more structured than their usual practice, the workers appreciated that there was flexibility within the approach, enabling them to respond to the needs of the young person while still achieving therapeutic progress:
What I liked about Y-SBNT, although there may be some leeway about how many sessions that it may take to move through some of these different stages, it’s logical, it’s flexible enough but it is quite an ergonomic sort of approach.
West Midlands therapist
Experience of delivering treatment
In general, the therapists had positive experiences of treatment delivery. They mentioned that it was a learning experience for them and they got a lot out of implementing the new techniques. As they became more familiar with the techniques and materials they were able to see the benefits of the approach.
However, for one of the therapists in the West Midlands service, the study period coincided with a change in his role brought on by organisational change because of a retendering process. This had ramifications for how much personal resource they could devote to the new treatment, particularly in terms of performing outreach work for their cases:
So my experience of delivering the intervention, I really liked it. It made sense to me, I think it’s a really useful way to explore with young people and their families and their wider network change. I have felt throughout and reflecting on it since I don’t feel like I’ve put enough into it to make it work and it sits really uncomfortably with me.
Other therapists in the West Midlands service found the structure and paperwork associated with the study quite challenging. Having to record sessions and being aware of session number and the associated materials and forms could be difficult when having a number of young people in active treatment on their caseload.
Treatment engagement
The North East therapists found that the trial procedures interfered with their normal way of engaging young people. A young person is normally allocated to a therapist and will be with him or her throughout the assessment and treatment journey. However, because of randomisation the therapist might be seeing the young person for the first time and would have to commence the first treatment session of Y-SBNT. Initially, the therapists found this an uneasy process but they became used to it as the study progressed and overall they did not feel that it hindered building a relationship with the young people:
I think it would still be nice to have a little bit of time at the beginning to at least build on a little bit of a relationship because it still felt a little bit disjointed because you’re sort of straight in there, whereas it would be good to try and get to know that young person a bit more first, but again I don’t know this is maybe coming from my side of things.
Randomisation was not highlighted as a problem for the West Midlands therapists, although they said that they had mixed results in terms of treatment retention. This was in part because of ambivalence by some young people, particularly those referred from the youth offending system, towards changing their substance use. For one therapist, a role change within the organisation impacted negatively on treatment retention.
Involving family/social network
Therapists in both the North East and the West Midlands services advocated the benefits of taking a wider approach and engaging a network of support around the young person. Perceived benefits included being able to support the young person beyond treatment sessions; providing the network members with an understanding of what the young person was going through; having a co-ordinated approach to help both the young person and the supporters; and having shared responsibility for change:
It was useful for the young person because they’re getting support from the social network and at the same time for the network members they’re getting to understand what the young person is going through.
West Midlands therapist
It takes the pressure off the young person as well because making changes especially around substance misuse is massive isn’t it? And it’s not something that, you know, you have to do on your own.
North East therapist
However, in practice in both sites the therapists mentioned that for some young people there were practical and logistical restraints that made it difficult to have network members attend sessions. These included co-ordinating diaries, locations and meetings at the youth offending service, particularly in the West Midlands, where it was not normal practice for families or friends to attend appointments.
For some young people, particularly those referred from the criminal justice system and ambivalent about changing their substance use, the therapists reported facing a challenge to convince them of the benefits of including network members in their treatment. Some of this work centred on assuring the young people that they would be in control of the information discussed and that they did not necessarily have to talk about their substance use but their chosen goals.
When it was not possible to include family members as part of the network, one therapist from the West Midlands said that he then focused on supportive others such as residential care staff in the young person’s network. A North East therapist emphasised that it was important to be accommodating to who the young person wanted to be involved in his or her support network:
It’s the young person who decides who’s in their social network and who’s going to be helpful to them . . . you do have to go with what that young person wants to put on there because it’s not who we think should be supporting, it’s about what they want.
Treatment goals
Both sets of therapists felt that the new treatment worked best when they were able to facilitate alignment of the young person’s treatment goals with those of their support network. Ideally, this would involve having network members physically attend sessions. However, this was not always possible and, even in these circumstances, good work could be carried out if network members were on board with the treatment.
The West Midlands therapists tended to speak in general terms about network member involvement supporting the young person in goal setting and did not provide particular examples of this. However, the therapists in the North East spoke at length about the perceived strength of engaging a network of support around the young people to help them work towards their goals. For example, they mentioned that a foster carer had a plan of action all worked out with the young person before the end of treatment and a father had a productive discussion with his daughter by the end of which they understood each other’s position and then were able to set realistic goals:
She had the plan all set up. I just like consolidated it by writing it up and she knew what she needed to do for him and that worked well and it kind of made me feel good because I was thinking, this is good. I love this model. But I do because sometimes walking away, you just think what is going to happen to this young person.
In both sites, the therapists did not go into specifics about what the treatment goals entailed.
The North East therapists stated that the key characteristic of successful network member engagement was establishing understanding and agreement between the young person and the network members on the way forwards in terms of supporting the young person’s chosen goals:
By including network members, like everyone has got a clearer understanding about what the young person is wanting to achieve and work towards and maybe that is something that the young person might not have felt able to discuss with network members before that point.
They also emphasised the utility of the goal-setting materials in helping to plot out appropriate goals for the young person and network members. One therapist felt that the goal-setting sheet was particularly helpful:
That was the most purposeful sheet I think because it was something that could be used in any situation not just substance use. It could be used for anything and that’s why it was so good.
If goal setting facilitated by the materials was successfully carried out by the young people this could increase self-efficacy and motivation for further action.
Comparison with treatment as usual
In both sites therapists said that the new treatment differed from their usual practice. The most common difference mentioned in the West Midlands was establishing a social network of support as part of the young person’s treatment:
We don’t usually go into the details of what that family member brings which I think was a really important aspect because you get the best out of what they want to get for their goal and who could support them.
In addition, because of a new provider in the West Midlands, TAU was not well defined during part of the study period as this was before the launch of their model.
Adopting a more structured approach as part of the new treatment was identified as a key area in both services. In the North East the therapists highlighted the length of treatment time as a departure from their usual practice. In normal practice sessions continue and are as frequent as the young person finds helpful:
It [treatment] will always continue as long as the young person is finding it helpful and wants that support. Whereas obviously with Y-SBNT it was like, right you‘ve got six sessions, and within 3 months . . . We couldn’t equate the 3 months could we? We were like six sessions we’ll be done in about a week and a half [laugh].
However, initial fears about treatment time were not realised as the therapists were able to change the way that they approached providing treatment to the young people in terms of session frequency and ongoing support:
It worked and actually some of our work can be done like that I think and it can be short, sharp, and out.
One therapist from the West Midlands also emphasised the motivational component of the new treatment and associated materials. In both sites, care planning was identified as a core element of both Y-SBNT and usual practice.
Integration with existing practice
Therapists in both services saw merit in the new treatment and had integrated some elements into their usual practice. Examples included being proactive about what can be done now for the young person and not dwelling on past events and giving therapeutic work with family members and others a clear focus and purpose:
What I did like was that actually the model itself is very present. So in that sense it’s like you’re working with the immediate scene.
The therapists in the North East felt that the active components of the Y-SBNT even had applicability in other settings:
I actually feel the model is really good. I think it can be used in any situation and I think in any setting as well as in services.
However, they emphasised that training is required to ensure that the new treatment is understood and utilised to its full potential. The North East therapists felt that they had already incorporated key elements of the new approach into their routine practice.
Me and [other therapist] actually embedded it into our practice and we believed in what we were doing and because of that it kind of spurred us on to make it right in all of the situations. Because we do, if we’re honest, I want it to go to trial. I want it to get to the next stage because it’s worth it. It’s got value to it.
Experience of the research process
In general, the therapists found being involved in the research process acceptable to them. There were some initial issues with study recruitment in the North East, with therapists finding the randomisation process after triage difficult as in usual practice a young person is allocated to a therapist throughout his or her treatment journey:
What I found difficult was how we were doing the assessments at the beginning and I spent time with these young people and then they were not my young people. So it meant that was hard because they’d got to know us and then we were handing them over to someone else.
At both sites there were initial concerns about the structure of the new treatment package and how it could fit in with existing processes within services. In the West Midlands therapists mentioned that having a more structured approach had implications for service-level agreements between the different organisations involved in the care of the young people and internal processes within the agency. However, in practice, with some negotiation the Y-SBNT approach was able to accommodate multiagency action plans. In the North East the therapists mentioned that with only six sessions the new approach would not be recorded as treatment within their existing databases:
Logistically you can’t just put six sessions over a 3-month period because they would never touch the database because it wouldn’t be seen as treatment. I think it ended up being over the period of time. But really why should we have to manipulate it to suit the service rather than the young person but without it, it doesn’t get the value that it deserves.
As the North East service was a small service with some staff turnover, one therapist was allocated young people who were in TAU after the 3-month treatment period. The therapist found this difficult as she had to be careful not to expose the young people to any of the techniques from the Y-SBNT approach.
Service manager’s views
Because of the retendering process and organisational change in the West Midlands service, several managers were in post throughout the duration of the project. Therefore, it was not possible to identify an appropriate person who would have an overview of service involvement with the study. However, there was one manager in place in the North East service throughout the study who was able to provide a full account of his experience from a service perspective. Five themes were identified from his interview: recruitment, treatment engagement, treatment approach, treatment implementation and integration with existing practice. Quotations supporting the descriptive text are provided in Appendix 19.
Recruitment
The North East manager reflected on the initial challenges of under-recruitment to the study in his service and how after discussion the triage system was modified so that young people who previously may not have received structured treatment, for example those in the criminal justice system who may have received an intervention from their YOT worker supported by a substance misuse specialist, were now eligible for the study. The manager reported having mixed feelings about this, as screening is an important part of the successful operation of the service:
I’m not always sure that was dead right either because I do think it’s important to do proper screening to establish whether they have the need for treatment.
He perceived an important place for unstructured education or support for young people with lower levels of substance use.
Treatment engagement
The interviewee thought that the young people should be perceived in the context of their whole lives, as those requiring a structured treatment for their substance use would have other difficulties in their lives (e.g. with regard to their families, school, the police) and should have an existing support team of professionals around them. Furthermore, the role of the substance misuse service should be to provide advice and support to those with an existing relationship with the young person. Supporting this key practitioner to deliver an intervention by having regular meetings with them and ensuring that the young person is kept informed about how the substance misuse service is involved in the treatment process is important:
Rather than having this culture where you’re just constantly looking to refer somebody else on to the next service provider, the next specialist, which in my view leads to disengagement rather than actual engagement. It’s about identifying who’s already got a reasonable relationship and how do you support them to deliver some intervention.
The manager perceived a role for the new treatment approach in facilitating communication and collaboration within the existing referral support network.
Treatment approach
There was thought to be great merit in the new treatment approach, especially the ethos of taking a wider focus on the young person’s life and involving a wider network of support in his or her treatment:
I think the big advantage is it highlights or focuses on recognising that a young person has numerous aspects to their life. Their substance misuse isn’t just the only thing in their life.
The manager highlighted that it is important for therapists to take a directive approach to empowering and facilitating the social network in a way that is helpful for the young person. He strongly believed in engaging a social network as support can be provided on an ongoing basis and is not just limited to treatment sessions. Also, having the needs of network members acknowledged and being able to review ongoing progress without involving a substance misuse specialist were seen as particular strengths of adopting a network approach.
Treatment implementation
In practice, the North East manager felt that, although some good work was carried out with the young people, some of the active components of the Y-SBNT approach were not fully implemented. His comments centred on social network involvement and goal setting. He felt that the social network was not engaged to its full extent in a number of cases. Also, when social networks were engaged there appeared to be an over-reliance on formal or professional sources of support within the network, as these people (e.g. school teachers) were usually time and role limited within the young person’s life:
If you’re sort of concentrating on the outside professionals, they have a take on it I suppose in terms of what they can and can’t do. There’s not unconditional support within that.
Some suggestions were made to address the issue of network composition. These included for the therapists to be proactive in helping the young person identify appropriate supporters; that the supporters understand the nature of their involvement, which is not time or role limited, and the responsibility and commitment required; and the potential benefit of involving positive peers in the young person’s network and not just relying on adult role models.
The North East manager also spoke at length about how he thought that the young people’s social network could have been more fully involved in goal setting. The manager’s feeling was that goals were mostly set individually with limited involvement of the young person’s social network and not having collective goals meant that the young person potentially lacked support for goal attainment from his or her network:
My interpretation of what the staff were doing was spending several sessions setting goals or agreeing stuff with the young people, that wasn’t necessarily understood or much less time was taken about actually involving a network.
Despite the perceived issues of involving networks in goal setting within the current study, the manager saw great benefit in the approach of having a shared understanding and agreement on goals if successfully implemented:
Setting reasonable goals, I suppose when you talk about young people, there is trying to get that as a shared experience almost. A shared agreement that says, so we’re all quite clear what we’re aiming towards.
Integration with existing practice
The North East manager was very positive about the new treatment approach and was keen for the other members of staff who delivered TAU to receive training:
I think understanding the philosophy in what you’re trying to achieve, the idea that actually this whole network effectively becomes the client . . . For me it’s an approach that ought to be fundamental to the way in which we work.
As also mentioned by the North East therapists, the manager believed that the new treatment approach had applicability in other settings beyond substance misuse:
I’m probably very conscious that for me I don’t just see it in terms of being a substance misuse intervention. I think it’s got direct applicability as a model right across the board and we should be utilising it.
As a treatment approach the manager felt that potentially Y-SBNT would work even better as an early intervention (e.g. in school health settings) when young people were using at lower levels and more natural networks existed in which appropriate supporters including positive peers could be identified:
Personally I think it’s got a lot of mileage and I would try and push it further. Bring it into the system earlier as an intervention.
Summary
Overall, young people, network members, therapists and a service manager found the new treatment approach acceptable to them. The majority of participants reported positive experiences of being involved in the study.
Young people’s views
From the young people’s accounts it was apparent that their substance-related problems were symptomatic of other more challenging circumstances in their lives. The majority of young people did not perceive their substance use as a problem on entering treatment nor did their friends, who also tended to use. They were usually referred because of concerns from other agencies or their family when still living together.
The young people reported a range of responses to the new treatment. Some of the young people referred from the youth offending system were ambivalent about changing their substance use and perceived Y-SBNT as compulsory probation meetings that they wished to attend alone. Others who engaged with and were exposed to the active components of Y-SBNT reported positive benefits such as strengthening relationships and network member involvement in non-using activities. These young people appreciated that treatment goals did not have to be specific to their substance use or abstinence focused.
Network members’ views
Only two network members were interviewed, both from the North East, which perhaps reflects a combination of a lack of network member engagement and researcher focus on following up the young people. From both accounts there was a sense that their involvement was more peripheral and supportive in nature rather than carrying out agreed actions discussed in treatment. When actions were mentioned these tended to be more practical such as ensuring that the young person was available and happy to attend his or her sessions. Despite this, network members perceived positive changes for the young people in terms of better communication and strengthening relationships.
Therapists’ views
The therapists from both the West Midlands service and the North East service said that the structure that Y-SBNT provides is a key strength. Having a logical sequence of sessions with flexibility if required gave clarity to both the therapist and the young person. This was a departure from routine practice in which sessions continue and are as frequent as the young person finds helpful. The therapists saw great merit in taking a wider network approach in helping to support the young people beyond their treatment sessions. Therapists in the North East felt that the new treatment worked best when they were able to facilitate alignment of the young person’s treatment goals with those of their support network. However, there were issues with treatment implementation, particularly in the West Midlands service. This was largely because of a service retendering process causing staff upheaval during the study period. In addition, therapists in both services mentioned practical and logistical restraints that made it difficult to have network members attend sessions.
Service manager’s views
Only the views of the service manager in the North East are reported as the retendering process in the West Midlands service meant that there were several managers in post throughout the duration of the study. The North East service manager believed in the ethos behind the Y-SBNT approach of taking a wider view of the young person’s life, as his or her substance use is symptomatic of another malaise. He felt that the new treatment could be helpful for facilitating communication and collaboration within the existing referral networks. As a treatment approach the service manager spoke in glowing terms about Y-SBNT; he thought that having the whole network effectively becoming the client should be fundamental to how services work and had wider applicability. However, he mentioned that, in the current study, social networks were not fully engaged with goal setting and there was an over-reliance on professional supporters. He suggested that Y-SBNT could work better as an early intervention when more natural networks existed.
Chapter 7 Treatment fidelity rating
Evaluation of psychosocial interventions that are manual based requires some means of establishing whether or not they were delivered as described in the manual, resource kit and therapists’ training sessions before efficacy can be compared with that of any other treatment. 125
As such, the measurement of fidelity to treatment is central when assessing psychosocial interventions within trials. In the current pilot trial, fidelity was assessed to establish whether it was feasible to use an adapted process rating measure to identify and rate the key components of the adapted social intervention, Y-SBNT. A further aim was to establish whether Y-SBNT-specific components were delivered sufficiently and to an acceptable standard. In addition, an attempt was made to establish whether there was a clear difference between the trial intervention, Y-SBNT, and TAU delivered within the two participating clinical services.
An additional secondary aim within this study was to attempt to explore the nature of TAU in the participating services.
These questions were important to establish the feasibility of intervention delivery as part of the present study. Detailed analysis of process is needed to inform the assessment of potential treatment effects with relevance to treatment components in a future full-scale randomised definitive trial. Alternatively, if further intervention development work is necessary this work can provide additional information to guide this process.
Methods
All 53 participants who consented to be randomised in the pilot trial were asked for consent for their sessions to be audio recorded. Further details of the sample obtained are provided in Figure 15. All available recorded sessions with young people were rated using an adapted version of the UKATT Process Rating Scale (PRS). 95 Items from the original scale that were related to overall session management and SBNT-specific items were used to examine the extent to which all components specified in the session protocols were delivered in terms of frequency and quality. One further item was added to the scale to measure ‘goal setting’ as it was not part of the original scale yet emerged as an important component as part of the adaptation work.
FIGURE 15.
Flow diagram of provision of consent to record therapy sessions across the trial. YP, young person.

Given the exploratory nature of this work no formal statistical analyses were carried out but ratings are presented descriptively.
The rating scale
All available Y-SBNT and TAU sessions were rated using the adapted UKATT PRS, which included three sections: session management (maintaining structure, agenda setting, explanation of philosophy of treatment or treatment session, reviewing intersession change, consistency of problem focus, end-of-session summary); specific Y-SBNT tasks (homework, alternative activities to drinking, social support for change – general, involvement of others in behaviour change, identification of sources of support for change); and therapist style (therapist as task orientated, therapist as active agent for change, collaboration, interpersonal focus). In addition to these three sections, ‘goal setting’ was included as a task within Y-SBNT and so was also rated for all taped sessions.
The items within each section were rated in terms of frequency (the extent to which the therapist carried out each specific item) and quality (of the therapist’s behaviour) on a 5-point Likert scale ranging from 0 to 4. In line with Tober et al. ,95 for frequency, the question ‘To what extent did the therapist . . .?’ was scored as 0 = ‘not at all’; 1 = ‘a little’; 2 = ‘somewhat’; 3 = ‘considerably’; and 4 = ‘extensively’. For quality, the question ‘How well did the therapist perform the behaviour within each item?’ was scored from 0 = ‘not at all well’ to 4 = ‘very well’.
The rating manual
A rating manual was specifically adapted from the original UKATT PRS. 95 Guidelines were available for the process rating. Item definitions with examples and guidelines for rating were adapted and used for rater training.
Rater training and supervision
All ratings were conducted by an independent rater who had previous experience of rating therapy sessions utilising the adult UKATT process rating manual from a previous study. 72 Initially, the rater and supervisor (one of the developers of the treatment approach) scored the same three sessions (early, middle and end) independently; they then came together to discuss scores, referring to the manual and any notes made to ensure calibration and rater agreement. Once satisfactory agreement was achieved, the rater proceeded to rate all treatment sessions available. The main rater received weekly supervision to discuss independently rated sessions.
The sample
A flow diagram illustrating the numbers of participants who provided consent to have sessions recorded as part of the whole trial sample is provided in Figure 15. In total, 51 sessions were available for rating (Y-SBNT, n = 42; TAU, n = 9). The length of the sessions varied, with the shortest session lasting 14.4 minutes and the longest session lasting 116.1 minutes (Y-SBNT, range 17.5–116.1 minutes; TAU, range 14.4–68.5 minutes).
Considering the rates of consent is important in terms of feasibility for future work. About half of the young people (or more in the case of TAU) who consented to trial participation refused consent for session recording. Further challenges were experienced in the TAU arm even when consent had been given by the participant. Tables 30 and 31 display the number of sessions received, the number of sessions recorded and the number of sessions available for rating for each consenting young person in the Y-SBNT and TAU trial arms, respectively. In addition to the sessions with young people, there were four recordings of what were termed ‘unilateral sessions’. These were sessions delivered to members of the young person’s social network in his or her absence (but having had his or her consent). These sessions were an important component of the intervention but were not rated as the available rating scale was not designed for this purpose.
| Young person (n = 13) | Number of sessions delivered | Number of sessions recorded | Number of sessions available for rating |
|---|---|---|---|
| 1 | 6 (5 + 1a) | 6 (5 + 1a) | 5 |
| 2 | 6 | 6 | 6 |
| 3 | 5 | 5 | 5 |
| 4 | 6 | 4 | 4 |
| 5 | 8 (6 + 2b) | 8 (6 + 2b) | 6 |
| 6 | 4 | 2 | 2 |
| 7 | 6 (5 + 1a) | 6 (5 + 1a) | 4 |
| 8 | 2 | 1 | 1 |
| 9 | 3 | 1 | 1 |
| 10 | 4 | 1 | 1 |
| 11 | 2 | 1 | 1 |
| 12 | 6 | 6 | 6 |
| 13 | 0 | 0 | 0 |
| Total | 58 | 47 | 42 |
| Young person (n = 10) | Number of sessions delivered | Number of sessions recorded | Number of sessions available for rating |
|---|---|---|---|
| 1 | 4 | 4 | 4 |
| 2 | 2 | 1 | 1 |
| 3 | 6 | 6 | 4 |
| 4 | 0 | 0 | 0 |
| 5 | 0 | 0 | 0 |
| 6 | 0 | 0 | 0 |
| 7 | 0 | 0 | 0 |
| 8 | 2 | 0 | 0 |
| 9 | 1 | 0 | 0 |
| 10 | 1 | 0 | 0 |
| Total | 16 | 11 | 9a |
Analyses
In line with our stated aims, the main analyses were exploratory in nature and aimed to address four key questions:
-
Was the adapted PRS feasible to use with the pilot trial recorded sessions?
-
Were the therapists able to deliver key components of Y-SBNT within the sessions recorded?
-
Were the ratings for the Y-SBNT sessions and the TAU sessions different in relation to Y-SBNT components?
-
What were the components of the recorded TAU sessions?
The questions and the methods used to explore each are outlined in the following sections.
Question 1: Feasibility of the adapted measure – ‘was the adapted Process Rating Scale feasible to use with the pilot trial recorded sessions?’
As reported, the PRS measure was adapted and used by two raters for initial calibration and then by a single rater to rate the full sample of recorded sessions. All scale items were observed (albeit to different degrees) in the Y-SBNT sessions and it was concluded that the adapted PRS was feasible to implement. Having established its usability the scale results were used to explore the various further questions outlined.
The scale consisted of general session management components as well as specific Y-SBNT components.
Table 32 shows the ratings for the general session management scale components for both Y-SBNT and TAU. No specific differences were predicted for general session management between the two arms.
| Session management scale component items | Mean frequency score | Mean quality score | ||
|---|---|---|---|---|
| Y-SBNT (n = 42) | TAU (n = 9) | Y-SBNT (n = 42) | TAU (n = 9) | |
| Maintaining structure | 3.60 | 3.17 | 3.80 | 2.92 |
| Agenda setting | 2.98 | 0.67 | 2.90 | 0.50 |
| Explanation of philosophy of treatment session | 2.85 | 1.89 | 2.87 | 1.89 |
| Reviewing intersession change | 1.37 | 0.53 | 2.60 | 0.45 |
| Consistency of problem focus | 3.65 | 3.03 | 3.61 | 2.78 |
| End-of-session summary | 0.85 | 0.00 | 1.70 | 0.00 |
All components of the adapted session management scale were identified within the Y-SBNT sessions. The component end-of-session summary was not observed in the TAU arm. In addition, agenda setting was observed at a higher frequency within Y-SBNT sessions than within TAU sessions. Planning and agenda setting within TAU is further explored and discussed within the qualitative analyses section of treatment described later in this chapter (see Question 4: A qualitative analysis of the components of the treatment as usual sessions recorded – ‘what were the components of the recorded treatment as usual sessions?‘). Overall, except for end-of session summary, all components were relevant and applicable to both intervention sessions. In terms of quality ratings, for all of the session management components present, the quality scores were higher in the Y-SBNT sessions than in the TAU sessions. This is particularly noticeable for agenda setting and reviewing intersession change.
Question 2: Components of Y-SBNT – ‘were the therapists able to deliver key components of Y-SBNT within the sessions recorded?’
To explore this question, all 42 Y-SBNT sessions were rated using the adapted measure. Those nine components identified as being specific to Y-SBNT are reported in Table 33. The ratings obtained for the present study are presented alongside those reported by Tober et al. 95 as part of the development and validation of the measure in the UKATT trial, in which it was used to rate a total of 193 sessions. As goal setting was not included in the original scale, there were no ratings for this component in the UKATT sample presented in the table.
| Scale component items | Mean (SD) frequency score | Mean (SD) quality score | ||
|---|---|---|---|---|
| Y-SBNT (n = 42) | UKATT (n = 193) | Y-SBNT (n = 42) | UKATT (n = 193) | |
| Homework | 1.27 (1.81) | 0.97 (1.20) | 2.15 (1.87) | 2.32 (1.05) |
| Alternative activities to drinking | 1.18 (1.55) | 0.93 (1.22) | 2.23 (1.64) | 1.91 (0.98) |
| Social support for change – general | 1.91 (1.57) | 1.25 (1.08) | 2.38 (1.58) | 2.06 (0.92) |
| Involvement of others in behaviour change | 2.43 (1.60) | 2.40 (1.20) | 3.10 (1.62) | 2.22 (1.02) |
| Identify sources of support for change | 3.47 (1.06) | 1.31 (1.54) | 3.47 (1.09) | 2.55 (1.12) |
| Therapist as task orientated | 3.62 (0.72) | 2.55 (1.35) | 3.45 (0.54) | 2.49 (0.99) |
| Therapist as active agent for change | 0.58 (1.55) | 0.32 (0.76) | 1.90 (1.83) | 2.18 (1.18) |
| Collaboration | 2.04 (1.48) | 0.45 (0.65) | 2.76 (1.53) | 1.93 (0.78) |
| Interpersonal focus | 3.21 (0.94) | 2.56 (1.52) | 3.21 (0.94) | 2.82 (1.10) |
| Goal setting (only for Y-SBNT)b | 1.41 (1.89) | 2.48 (1.91) | ||
As Table 33 illustrates, all key components related to Y-SBNT appeared to have been delivered to a similar level of frequency as, or a higher level of frequency than, in the UKATT 193 SBNT sessions rated by Tober et al. 95 All of the nine original components were delivered as well as the additional component related to goal setting. The ratings suggest that some of the social components, that is, identifying sources of support for change, having an interpersonal focus and involvement of others in behaviour change, were among the most frequently performed components. Quality ratings for all of the individual components except for homework and therapist as active agent for change were slightly higher in the Y-SBNT group than in the UKATT study. Those social components that were more frequently observed had higher quality ratings.
Question 3: Components of Y-SBNT in both treatment arm sessions – ‘were the ratings for the Y-SBNT sessions and the treatment as usual sessions different in relation to Y-SBNT components?’
To explore this question, ratings of all 51 sessions (TAU and Y-SBNT) were analysed, with a specific focus on Y-SBNT scale components. As shown in Table 34, four of the components were absent from the TAU sessions: homework, social support for change – general, involvement of others in behaviour change and identifying sources of support for change. Within the TAU sessions, the component therapist as task orientated had the highest frequency rating of all components, with a similar rating to that obtained for Y-SBNT sessions. There were elements of interpersonal focus, goal setting and collaboration and some evidence of alternative activities to drinking; however, delivery of all of these components was less frequent in the TAU sessions rated than in the Y-SBNT sessions rated. The quality ratings of the components present in the TAU sessions were all lower than the quality rating in the Y-SBNT sessions. Further specific details of the content of the TAU sessions are provided in the next section based on qualitative exploration.
| Scale component items | Mean (SD) frequency score | Mean (SD) quality score | ||
|---|---|---|---|---|
| TAU (n = 9) | Y-SBNT (n = 42) | TAU (n = 9) | Y-SBNT (n = 42) | |
| Homework | 0.00 (0.00) | 1.27 (1.81) | 0.00 (0.00) | 2.15 (1.87) |
| Alternative activities to drinking | 0.61 (1.13) | 1.18 (1.55) | 0.45 (0.88) | 2.23 (1.64) |
| Social support for change – general | 0.00 (0.00) | 1.91 (1.57) | 0.00 (0.00) | 2.38 (1.58) |
| Involvement of others in behaviour change | 0.00 (0.00) | 2.43 (1.60) | 0.00 (0.00) | 3.10 (1.62) |
| Identify sources of support for change | 0.00 (0.00) | 3.47 (1.06) | 0.00 (0.00) | 3.47 (1.09) |
| Therapist as task orientated | 3.28 (0.60) | 3.62 (0.72) | 2.95 (0.83) | 3.08 (0.54) |
| Therapist as active agent for change | 0.42 (1.32) | 0.58 (1.55) | 0.39 (1.41) | 2.08 (1.83) |
| Collaboration | 0.75 (1.32) | 2.04 (1.48) | 0.50 (0.88) | 2.76 (1.53) |
| Interpersonal focus | 0.78 (1.36) | 3.21 (0.94) | 0.61 (1.20) | 3.21 (0.94) |
| Goal settingb | 0.83 (1.13) | 1.41 (1.89) | 0.83 (1.13) | 2.48 (1.91) |
Question 4: A qualitative analysis of the components of the treatment as usual sessions recorded – ‘what were the components of the recorded treatment as usual sessions?’
In addition to the use of the PRS, for all TAU sessions a qualitative exploration of the session recording was undertaken.
The nine TAU sessions available were delivered by two therapists. One therapist completed four TAU sessions with one young person and one session with another young person. The other therapist completed four sessions with one young person. Characterising the nine TAU sessions involved listening to each session carefully and noting the presence of topics/themes under specific categories. Although it was not intended that the sessions would be compared, this occurred naturally as a consequence of the small number of TAU sessions that the researcher had to work with. The results of this exploration are very preliminary, partly because few sessions were available compared with the expected number of sessions. There were a number of reasons for this ranging from lack of consent to problems with equipment and therapists not recording sessions on some occasions when consent had been given.
The session content varied across all nine sessions with limited similarities. Some sessions were informal, brief and less structured whereas others were more formal, detailed and structured.
The sessions included a variety of topics such as information gathering, travel, exploration of drug/alcohol use and impact, completion of paperwork, education, alternatives to drug use and the future, learning difficulties, activities, place of living, harm reduction, relationships/family, goal setting, court orders, services, medication, sharing of information, communication, care plans, alcohol, techniques to aid recovery, physical, intellectual, emotional and social health, alternative therapies and general talk.
The sessions appeared to focus on information gathering about past events, recent events and the current circumstances of the young person. Information gathering at one session included finding out the circumstances of the young person leaving home, the length of time stayed at different places and any future plans related to leaving home. At another session the therapist gathered details of the events that led to a court order, the length of time of the order and what triggered the offence.
Both agenda setting and the planning of future sessions took place briefly in a few sessions. In two of the sessions, the therapist emphasised that the young person had ‘ownership’ of the sessions because they were about ‘him’ and therefore it was up to ‘him’ to make decisions about session content and change. In addition, the therapist explained that his role was a supportive one, to enable change. Generally, there was good co-operation between the therapists and the young people but during one session one of the therapists found it challenging to engage the young person because he was not communicating and remained almost silent throughout the session.
Drug and alcohol use and its impact was explored in some detail, including the length of time in treatment, the drug of choice, the frequency of drug use, the quantity used, the reasons for using, whether the drug was used alone or with others, reducing/stopping drug use or alcohol consumption, asking about a timeline for drug or alcohol reduction, triggers, cravings and thoughts and feelings after drug use.
In nearly all of the sessions, a variety of paperwork was either referred to or completed by the therapist and the young person. Paperwork included drug diaries, rating scales tapping into how things were for the young person, the therapeutic alliance questionnaire for research purposes, case closure forms and copies of the young person’s care plan and strengths. In one session consent was gained from the young person for the sharing of information to enable a letter received from a doctor to be responded to and to ascertain who the young person would like to share her care plan with. Another therapist asked one young person if he had any learning difficulties and, on discovering that he was colour-blind, offered to fill out the paperwork on his behalf. The paperwork listed earlier was not used systematically across all sessions but was used as and when it was appropriate for individual sessions. A drug diary was completed in three sessions, reference to and discussion about a care plan occurred in one session, rating scales including the therapeutic alliance questionnaire were completed in two sessions and discharge forms were completed in one session. In almost all of the sessions there was mention of a network member, usually a family member such as a mother, father, sister or brother but sometimes a partner or friends and, a couple of times, a professional, including a social worker. The therapists briefly explored the relationships that the young person had with these individuals and gauged whether there had been any recent contact. However, despite some overlap this work was not conducted in the same level of depth and detail as in the Y-SBNT sessions.
During most of the available sessions health was a topic that at times was initiated by the therapist and at times was initiated by the young person, but which was not always explored fully. In response to one young person mentioning spending more time with her boyfriend, the therapist enquired whether she was using contraception. In the main, emotional health was discussed in most of the sessions in terms of the mood of the young person, tearfulness, anger, energy levels, not eating and feeling like dying. This discussion led to one young person expressing her thoughts, linking her increased consumption of alcohol to her depression. In response, an alternative therapy (acupuncture) was explained and it was suggested that the young person consider this for the sleep problems and depression she was experiencing to complement her current prescribed medication. In addition to this, harm reduction was also a topic that was discussed and explored in some sessions, with the positive and negative effects on the body mentioned, as well as the impact on mental health and the dangers of interactions between prescribed medication and non-prescribed drugs (and therefore the importance of sharing information with the prescribing doctor). On one occasion an information leaflet about the effects of cannabis was given to the young person. In two sessions the techniques used to aid recovery were described (not implemented) to the young person: motivational interviewing/intervention, solution-focused techniques, roots to recovery, maps, the use of tools, solution-focused questions, looking forward to the future, identification and brief advice (IBA), harm reduction, coping strategies, the importance of identifying internal/external triggers in developing coping strategies and self-talk.
Fewer than half of the sessions included asking the young people to think about the future and, although goals were set in two sessions, a detailed plan was not devised to determine how educational goals would be achieved or how the young person would get involved in alternative activities to drug or alcohol use. In one session there was a review of goals set previously. There was a brief mention of three other services during two sessions to check whether the young person was still a patient and whether the young person had accessed other services.
Examples of general talk were limited to two sessions: on one occasion there was a discussion about a website that the young person had asked the therapist to visit and on another occasion there was a discussion about mobile phones. In terms of travel, one young person requested a day saver bus ticket on three occasions.
In summary, the sessions were focused on past and current circumstances. There was a high level of variation in terms of content and strategies used between sessions, with limited planning or formal agenda setting. However, this interpretation of the evidence needs to be treated with caution given the small number of sessions available and the potential for bias. The tentative results offer an initial exploration of the delivery of TAU for young people in substance misuse services that can contribute to further work. A summary of the identified components and definitions and examples, along with the frequency with which each component was identified, is provided in Table 35.
| (Frequency) Components | Definitions and examples |
|---|---|
| (8) Completion of paperwork | For TAU: drug diary; rating scale of ‘how things are’; case closure paperwork; copies of care plan and strengths |
| For research: therapeutic alliance questionnaire; copies of paperwork | |
| (7) Physical, intellectual, emotional and social health | Immune system low; emotionally low; not eating; spending more time with boyfriend – contraception; tearful; felt depressed – does not like taking medication for depression; feels like she has no energy; feels angry; feels like dying; started drinking more when became depressed |
| (7) Relationships/family/professionals | Therapist emphasises here to support; checks everything is OK with mum, sister; ‘ups and downs’ with mum and brother; father does not respond to messages; friends are users; boyfriend clingy – feel claustrophobic; unsure about relationship with boyfriend; boyfriend has apprenticeship; withdrawn from friends; social worker |
| (6) Sessions and support | Your sessions; plan for next session; case closure; therapist highlights not very talkative; agenda set briefly; attendance because of court order; difficult to engage; brief mention of what the next session will be about |
| (5) Information gathering | Includes gathering information about past events, recent events and current situations in terms of drug/alcohol use, relationships, education and bullying |
| (5) Alcohol | Reduction of alcohol consumption; consumption of alcohol; frequency of alcohol consumption; corner shop temptation; thoughts about consequences of drinking prior to alcohol consumption; triggers |
| (5) Exploration of drug use and impact | Length of time in treatment; drug of choice; frequency of drug use; quantity used; most enjoyed time of the day to use drugs; explores whether client can identify gains from using; checks whether client is using alone or with others; reducing/stopping drug use; probes client about when he thinks he can reduce his drug use; triggers; cravings; thoughts and feelings after drug use; therapist makes client aware that he can smell beer on him |
| (4) Education, alternatives to drug use and the future | Encourages young person to plan ahead for when school comes to an end; poses question about where young person sees himself or herself in 5 years’ time; interests; courses; commencing college course; GCSEs; sent home from school when falls asleep; explores how young person spends his or her spare time |
| (3) Medication | Risperidone for hearing voices; antidepressant for depression |
| (3) Harm reduction | Positive and negative effects on body; mental health; dangers of interaction between prescribed and non-prescribed drugs; provision of information leaflet about effects of cannabis to young person |
| (3) Travel | Client wants a day saver bus ticket |
| (2) Others identified on only two occasions | Alternative therapies; techniques discussed to aid recovery; goal setting; general talk; court orders; other services |
| (1) Others identified on only one occasion | Learning difficulties; discussion of activities; sharing of information; place of living; communication; care plan |
One further analysis was conducted to ascertain how key components of Y-SBNT were delivered across the early, middle and end stages of the recorded intervention sessions. This was important to explore whether there was potential ‘therapist drift’ resulting in aspects of the intervention being applied at early stages, with therapists reverting back to usual practice at later stages when the Y-SBNT components would not be so evident. To explore this, all available recorded Y-SBNT sessions were categorised into ‘early’ (consisting of session 1), ‘middle’ (consisting of sessions 2–5) and ‘end’ (consisting of session 6, the final session; when session 6 did not take place but session 5 did, the latter was placed in the ‘end’ category). All 10 components involving Y-SBNT-specific tasks as well as therapist styles were then represented in a series of graphs (Figures 16 and 17), which illustrate the mean frequency ratings across the three stages (the full data table can be seen in Appendix 20). As shown in the graphs, there was no marked drop in frequency of key rated Y-SBNT-specific components during the middle part of the intervention, suggesting little evidence of therapists moving away from these components as therapy progressed.
FIGURE 16.
Mean frequency scores for Y-SBNT: specific tasks. (a) Homework; (b) alternative activities to drinking; (c) social support for change: general; (d) involvement of others in behaviour change; and (e) identify sources of support for change.


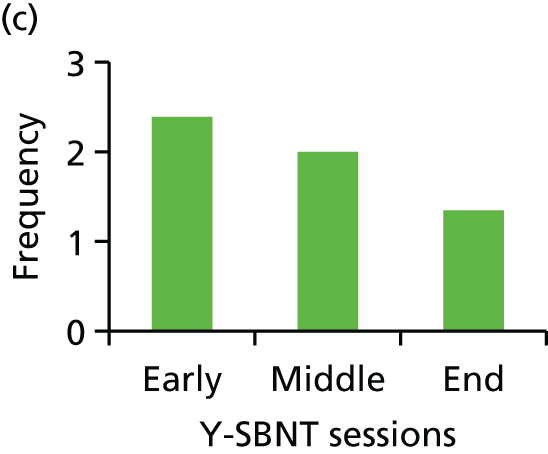


FIGURE 17.
Mean frequency scores for Y-SBNT: therapist style. (a) Therapist as task orientated; (b) therapist as active agent for change; (c) collaboration; (d) interpersonal focus; and (e) goal setting.
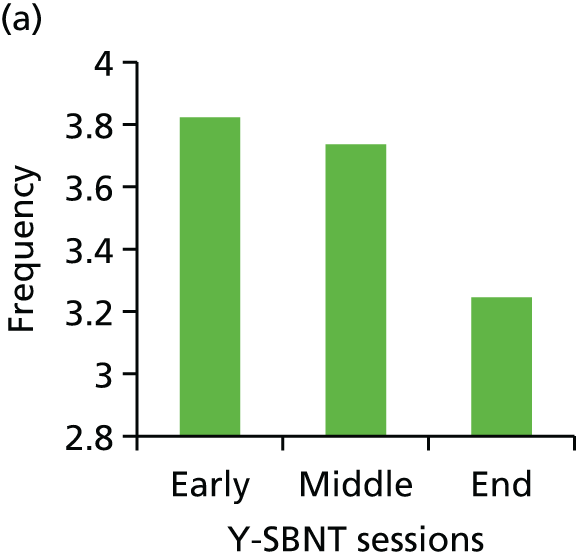



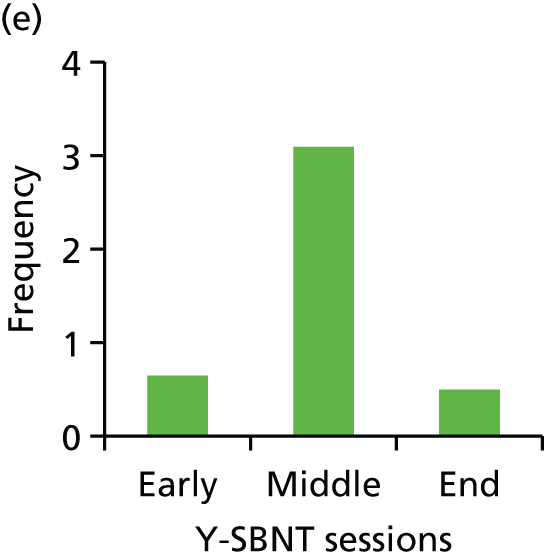
Summary
One of the main aims of the fidelity assessment work in the pilot study was to establish whether the adapted PRS95 was suitable for use in rating Y-SBNT sessions. We concluded that the adapted process rating measure was feasible to use (with minimal adaptation) to identify and rate the key components of the adapted social intervention (Y-SBNT). There was evidence from the rating process to suggest that a number of the key components of Y-SBNT were delivered in line with what was required of therapists. The social/interpersonal aspects of the adapted intervention were evident during the sessions that were analysed. These components were delivered as frequently as during rated sessions from the UKATT trial95 and often more frequently. They also appeared to be delivered consistently across all relevant stages of the intervention. Considering both the rating of sessions and the qualitative exploration of TAU, there appeared to be differences between the content of the experimental intervention and the content of control interventions.
Overall, we concluded that, in those sessions rated, key components of the Y-SBNT intervention were delivered by therapists. In terms of feasibility, however, there were challenges with regard to obtaining consent to record sessions, in particular in the TAU arm. These involved a combination of a lower level of participant consent and therapist problems with recording. This is important to consider in future work with this group of young people.
Chapter 8 Involving young people in the study
Introduction
As discussed in Chapter 1, there is increasing interest in children and young people’s active involvement in the planning and process of research. 57–60 The Y-SBNT study team, in addition to drawing on previous work by the team and other published studies, wanted from the outset to actively involve young people with experience of substance misuse services throughout the study. It was hoped that young people’s involvement in the project would ensure that the study, and the Y-SBNT intervention itself, were relevant to, and addressed the issues faced by, young people with substance misuse problems.
This chapter:
-
describes the processes around young people’s involvement in the Y-SBNT study
-
reflects on key issues that arose within the context of the relevant literature
-
suggests a new model for young people’s involvement in similar future studies.
Why we got involved: young people’s perspectives
As well as writing about young people’s involvement, we wanted to stay true to our intention of involving young people in all aspects of the study, including writing up. This section of the chapter was therefore written by the two young advisors who had the most longstanding involvement in the project (20 and 23 months) and who also commented on drafts of the full chapter. One of the final young advisor meetings in November 2015, attended by three young people (one of whom was one of the young people with the longest involvement in the project), focused on the draft chapter to which these two young people had contributed. Further comments and contributions from the young advisors at that meeting, and the therapist who accompanied them, have been incorporated into this final draft.
I think it’s important to involve young people in the Y-SBNT project because it’s actually about young people, and I think they should have an input into it and not just the adults. I think it’s important to involve young people who have used drug and alcohol services as they can understand what it’s like for others who are in the shoes that they’ve been in – no offence to people that have got degrees! We have sort of walked the walk, so we know that stuff that other young people using services have to go through on a daily basis. Now that we’ve come out of it we can explain things in a deeper level than adults who’ve got degrees and read about it in text books. They haven’t felt that emotional and physical turmoil, and the same with young people who haven’t had drug problems, they haven’t gone through what I’ve had to go through and wouldn’t understand what it’s like. I wanted to get involved with this project because I’ve always wanted to do something like this to show others that it is possible and there is light at the end of the tunnel – and that no matter what circumstances they’re in they’ve always got a voice. I’m involved in the Y-SBNT project so I can pass on my experience and if I can help one person that’s another person who might not die and become a statistic. I want to make things better, I actually don’t care as much what I get out of it, I just don’t want to see any other young person suffering the way I had to, or end up dead or in prison. If I can help develop something that prevents that then I will.
Young advisor A
I got involved in the project because I think that it’s important that young people can get the help that they need in the most helpful and supportive way so it doesn’t damage them. I think I’ve gained an insight into research with young people and the opinions of young people held by social agencies and professional networks. A project for young people should definitely consult young people and should be based around their views. Young people who have used drug and alcohol services will be able to reflect on their past use of services and give relevant feedback. The fact that you’ve included so much of material from young people in this chapter completely personifies the whole point of the project. Reading the chapter and all the findings and the work you’ve done, and I’ve done, made me feel quite special. It made me feel like my views are important.
I also didn’t realise just how useful I’d find it, hearing everyone’s experiences is wonderful, everyone’s unique and that’s very comforting. Being involved in the Y-SBNT study makes you think about things, I think about my situation differently now, the way I’ve isolated people in my life and what factors they had and how they’ve contributed and everything. It’s a good way to detach yourself from it and look at it in a more scientific way but at the same time you are like ‘this is my life, this was what was going on with me’. I think it’s quite interesting, it’s not very often you get to put these things down on paper and step out of your own shoes and look back and say ‘let’s be honest about this’, no emotion. It’s the first time a group of professionals have taken things I’ve said and made use of it, and benefited from it, in an academic project. I’m very much used to discussing my substance use history in a very negative light with no real benefit at the end but this project has helped me realise that a negative experience has made me wiser.
Young advisor B
At the November 2015 meeting the two other young people also said that they thought that it was important to involve young people:
. . . because it is about us . . . we know about the services and how to make them better. We are the people they are meant to be working for. It also keeps you out of trouble and gives us something to do. It is good for my CV and helps me understand more about services.
Because they [young people] can help others and share their knowledge and experience. The researchers will get real information about young people’s experiences and understand things from young people’s points of view. [Being involved in research] gives young people more insight. They realise that they’re not alone in the world and can do more with their lives.
Processes of involvement
Overview of young people’s involvement in the study
As discussed in Chapter 2, during phase 1 young people were supported to work alongside the research team to ensure that the intervention was acceptable and relevant to our target groups and reflected the views of service users and their families. During phases 2 and 3 (see Chapter 3) young people were involved in tasks associated with the feasibility trial, including the design of key trial documents such as the recruitment leaflet and information sheet, the production of training materials, advising on data collection tools, data analysis and interpretation, reporting and dissemination. Further details on activity, outputs and outcomes are available in Appendices 2 and 3.
Summary of young people’s involvement in the study
-
In total, 17 young people were involved as young advisors in some capacity.
-
The young people came from five areas of England (the West Midlands, the north-east and the west of England, London and Oxfordshire).
-
The 17 young people included 12 females and five males ranging in age from 16 to 21 years, with an average age of 18 years.
-
We met 10 young people once, five twice and two on five or more occasions.
-
Over the course of the study we held a total of 20 face-to-face meetings with young people. In between meetings, contact was maintained by post, text message, e-mail or telephone call, depending on the preferences of the young people involved.
-
Seven newsletters were sent to young people during the course of the study with updates on the project, information about how young people had been involved and upcoming opportunities.
Young people’s involvement in the study was led by two members of the research study team (LM-B and LT) with expertise in public involvement and research with young people affected by substance misuse, respectively. They contributed to the development of the initial proposals and were then employed as public involvement leads to recruit young people and organise meetings with young people and family members, develop methods for the involvement process in collaboration with other co-investigators and produce reports of the results of this work. Various research team members contributed to the meetings with young people through presentations, planning and facilitating sessions and feeding back on how this involvement had informed the study (see Appendix 2). Public involvement was also a standing item on all TMG and TSC meetings, at which the public involvement leads reported back on public involvement activity and sought feedback and ideas from the TMG and TSC. As the project progressed and the need to adapt initial plans for public involvement became apparent, TMG and TSC meetings were key to the development of new ideas on how best to involve young people in the study.
Who was involved in the study and how: plans and reality
Initial plans
The original plan for young people’s involvement in the study, as outlined in Chapter 3, was to have a YPAG of 10–12 young advisors aged 12–18 years with previous experience of accessing substance misuse treatment services who would be actively engaged throughout the project. This is a common model for young people’s involvement in health and social care research used by, among others, the Medicines for Children Research Network (now the Clinical Research Network Children,126 the National Young People’s Mental Health Advisory Group, the DECIPHer (Development and Evaluation of Complex Interventions for Public Health Improvement) ALPHA (Advice Leading to Public Health Advancement) young people’s group127 and the National Children’s Bureau’s public health advisory group known as PEAR (public health, education, awareness, research).
However, recruiting young people to an advisory group proved problematic. In the first instance there were delays that arose from a request by the NHS host institution for NHS ethical review and approval for this phase of the project if recruiting young people through trust NHS services. Normally, ethical approval is not needed for the active involvement element of NIHR research, even when people are recruited through the NHS128 but, as young people’s involvement in the study was also part of a Doctor of Philosophy (PhD) research study by one of the public involvement leads, the trust requested NHS ethical review. The National Research Ethics Service (NRES) was consulted during February 2013 and confirmed that no NHS ethics review was required for public involvement in the study, with most aspects in the early phase of adaptation of the intervention seen as a service-related evaluation. However, ethical review was needed for the aspects of this work that were being used for the PhD research study. This was obtained from the University of the West of England Life Sciences Faculty Research Ethics Committee (reference number HLS/13/06/88) following which full approval to proceed with plans for public involvement and the associated PhD work was given by the NHS host institution.
These discussions and processes led to some delays and also a review and widening of recruitment sites for young advisors. Initially, we worked with a national drug and alcohol treatment charity, as it expressed an interest in the project and thought that it could be an exciting opportunity for young people who had used its young people’s services. However, initial recruitment proved a lot slower than we, or the charity, had anticipated and the first three meetings (in September, October and December 2013) were poorly attended. At each meeting four to six young people were expected but only two attended on the day and the young people who did attend varied from meeting to meeting.
Revising plans
By early 2014 we realised that the traditional format of a single-location advisory group would not on its own be the right model for working with the young people whom we wished to engage. We therefore moved to a more flexible model that focused on fitting involvement activity around what worked for the young people whom we were trying to involve. Young people’s involvement was no longer centred on regular meetings in London, but started with smaller consultations based at services or other locations that were familiar to them and also included e-mails, text messages, telephone conversations and correspondence by post when this was more convenient for the young people or timely for the project (e.g. if young people’s input was needed in between scheduled meetings). If interested, young people involved in these consultations were then given the option of ongoing involvement and invited to become a young advisor, but there was no obligation to do so. We hoped that this more flexible approach would give young people, and services, a chance to find out more about the study and potential involvement without making an ongoing commitment at the outset. We also sent out regular newsletters to all young people with whom we were in contact so that, even if they were unable to be involved for a period of time, they were kept informed:
It’s been good to get the newsletters and read about what we did and how it’s helped the project.
Young advisor at November 2015 meeting
Another factor that affected how and when young people were involved in the project was that many of them were also working, often in low-paid jobs for which they would not be paid if they did not work or from which it was difficult to take time off. In many YPAGs young people are given a gift voucher for their time and this was the model that we initially adopted: all young people involved received reimbursement of travel expenses and, initially, a £20 voucher for each meeting attended (payment was later revised; see below). However, when we realised that we were going to have fewer young people involved in the project and that loss of income was a barrier to involvement for some, we decided to adopt a different approach. After considering INVOLVE and other guidance on payment for public involvement,129 the TMG agreed in September 2014 to offer young people involved in the study payment at a rate of £10 per hour on an ongoing basis for involvement activity, plus travel and subsistence expenses as before. The time needed for any work undertaken remotely (such as commenting on draft documents or, writing sections of articles and reports) was negotiated in advance. Payments could be in the form of Love to Shop vouchers as before or could be paid directly into a bank account via a claim form. Young people could also choose not to accept payment. If young people were working they were advised that this income would need to be declared for the purposes of tax and national insurance and that it was their responsibility to do this. If they were claiming benefits they were advised about the necessary rules on earnings and signposted to relevant guidance and sources of information on these matters. One young person was supported by the NIHR Benefits Advice Service for involvement130 to manage issues around payment for involvement and benefits.
This new approach led to the following engagement with young people (further details are provided in Chapter 3 and Appendix 2):
-
January 2014 – Consultation meeting in the West of England attended by three young people, one of whom continued to be involved for the remainder of the project, mainly on a one-to-one basis, and is one of the young contributors to this chapter.
-
March 2014 – Consultation meeting with two young people at a service in Oxfordshire. This led to two completed young advisor applications and both young people saying that they wanted ongoing involvement, but this did not materialise despite following up with both the young people and the service.
-
April 2014 – Piloting questionnaires with two young people in the West Midlands led to one young person expressing an interest in ongoing involvement. She has been involved on an ongoing basis ever since, mainly one-to-one but also attending one meeting with other young advisors, and is one of the young contributors to this chapter.
-
Contact with a service in the North East (also one of the clinical sites for the feasibility trial) where Y-SBNT therapists were really enthusiastic about supporting young people’s involvement. This resulted in two therapists accompanying young people to three Y-SBNT young advisor meetings during 2015: four to a meeting at Birmingham University in April, three to a meeting in York in September and two to a meeting in York in November.
Evaluation and feedback from young advisor meetings
Young people’s views on the meetings were captured through a range of evaluation activities, as well as through summary notes produced by the public involvement leads and circulated to the research team after every meeting. These evaluation data informed both future meetings during the study (Table 36) and also plans for a new model of involvement.
| What young people said | What we did |
|---|---|
| Less ‘talking at us’ and more hands-on interactive activities | Made presentations shorter and eventually dispensed with formal presentations all together. Gave young people information before meetings and, when they were supported by services, asked the services to go through the information with them before meetings, giving us more time for discussion and hands-on activities |
| Different timing and more breaks | Start and finish times for meetings were determined by where young people were travelling from, with the aim of avoiding overly long travel times and early starts. We ended up with a format that started with lunch and included at least two breaks during a 3.5- to 4-hour meeting. We also encouraged young people to take informal breaks if they needed them and included this in ground rules |
| Don’t mind travelling but would like the chance to see new places and have some fun, not just sit in a room | Moved meetings from university campus to city centre location, with time for some sightseeing before getting the train back. Went out for pizza after the meeting instead of having sandwiches in the room |
| Sometimes difficult to talk about personal experience | All young people were given a sheet with sources of further information and support and we included the following in the ground rules:
|
| Get more young people at the meetings | Those young people who were involved were keen, as were we, to increase the numbers of young people at meetings. Some young people helped with this by encouraging friends to get involved. However, for reasons discussed elsewhere in this chapter, this often did not happen despite our best efforts |
| Important to meet members of the research team as well as the public involvement leads | Whenever possible members of the research team attended meetings and led sessions in group meetings, but this was more difficult in informal meetings with individual young people |
| Some of us need support from staff to be involved | Worked with therapists in the last two meetings to support young people to complete application forms and attend the meetings. At the young people’s request therapists also remained in the room during the meetings and supported young people with activities when required, as well as being some young people’s nominated point of contact in between meetings |
Reflections on young people’s involvement in the study
Quotations in this section come from interviews with young people involved in the study and focus groups with the TMG and TSC to review learning from public involvement.
Models of involvement
Much of the limited but growing literature on young people’s involvement in health research focuses on the benefits, impact and outcomes of that involvement (e.g. Boeck and Fleming,131 Moules132). As outlined at the start of this chapter, young people’s involvement in health research is also dominated by the model of the YPAG. But there has as yet been relatively little discussion in the literature about who is, or is not, involved in research and how different models of involvement might work for different young people.
‘Children and young people’ are not a homogeneous group: age and other aspects of social background such as race and ethnicity, disability, social class, family background and use of services ‘intersect as aspects of who [young people] are, their social position, and what researchers need to consider’133 in designing research approaches appropriate to the young people they wish to involve. As outlined earlier, it became apparent fairly early on that our original plan for an advisory group of 10–12 young people, who would be actively engaged throughout the project, was unlikely to be successful with a group of young people who had complex lives and little or no experience of either involvement or research. We found that input from young people to this research study needed instead to be dynamic and flexible; this enabled us to create new opportunities and ways of working more suited to those we wished to involve (p. 221),131 in this case young people who had experience of using substance misuse services:
Perhaps that sort of [YPAG] group structure isn’t going to work with these sorts of young people in a project like this. And I think it is good to have a group and people fire off each other . . . but I still think the individual-level stuff that we’ve had has been really good and that’s worked well and in a more natural way and perhaps this group need that level of support . . . because they’re pretty chaotic, [with] multiple problems so you have to go to them, they’re not going to come and travel to some place and so this individual level and trying to hold them over the course of the project might be an alternative model.
Researcher, TMG public involvement review focus group
My mental health has sometimes made it difficult for me to be involved [in the project] . . . for example that [recent young advisors] meeting, I would have liked to have been part of it but due to my mental health I couldn’t even come out to meet in a coffee shop, let alone travel to a meeting . . . But I like how, if I can’t come to a meeting, we can have a phone call instead or you’re just a text [message] away, or we can do stuff by post. I’ve not always been well enough to come and see people face-to-face but that doesn’t mean I couldn’t be involved in things, whereas some organisations I’ve been involved with would have said ‘you’re ill or you couldn’t come to a meeting so you can’t be involved’.
Young advisor A
What I’ve liked is the flexibility. I’ve never had to make my own way to one of these meetings . . . of course it is a research project so there is a certain amount of formality about it but [individual participation] keeps it relevant and convenient for to the young person which is always good . . . . I have spent the majority of my time with [public involvement lead] in this project and I like to think we have also built a friendship as well.
Young advisor B
However, the individual model of one-to-one work with one of the public involvement leads could lead to young people being more isolated. One young person, who was mainly involved in this way because of availability and geography, said that, although she appreciated the flexibility and convenience of meeting at a time and place that suited her, she would have liked to meet other young people involved in the study and that working in a group might help young people feel ‘less of a guinea pig’:
The individual model, while it’s worked very well in some ways, I wonder because [young person] has said to us it would be great to meet the more of the [research] team and other young people, and we’ve not been able to get to a stage where we’ve been able to do that.
Public involvement lead, TMG public involvement review focus group
Hanley et al. 134 identify the different levels of public involvement in research as consultation, collaboration and user controlled. Although we had started with the intention of this being a collaborative project, what we ended up with was something that actually started more as consultation (i.e. one-off meetings) and built up to more collaborative working if this was something that young people were interested in. This echoes Kirby et al. ’s135 non-hierarchical model of young people’s participation, in which the appropriate level of involvement is determined by the circumstances and young people involved:
Being on their journey with them is more important than getting results or directing them. We have to do this [involvement] at their pace.
Therapist supporting young people’s involvement
Franks136 talks about the need when ‘doing participatory research with children and young people at the margins of society’ to consider ‘creating pockets of participation’ (p. 15). This is often what happens by default in many projects but, by making it transparent and intentional, young people can better understand their potential role and discuss with researchers when, how and in what ways they would like to be involved in the research process. 136
Not the usual suspects
Another question we had to consider was whether some, or indeed many, of the young people we were seeking to engage were ‘hard to reach’ because they were not interested in or were unsure about the project:
Young people in my age group are in a very transitional stage of life, hard to commit long term. Some young people relapse, or simply don’t like discussing their problem in depth.
Young advisor B
Young people might not know how services work. They may still be using or have other unresolved issues.
Young advisor at November 2015 meeting
As well as having a right to have a say in matters that affect them,70 young people also have the right to choose whether or not to get involved in research. Individuals who may be under significant stress might see limited personal benefit of being involved as a research collaborator. 137 It can be particularly difficult to involve young people in research on sensitive topics, such as those that are private, stressful or ‘potentially expose stigmatising, or incriminating information’ (Lee,138 cited in Powell and Smith59). The young advisors raised this as a reason why, in some instances, they felt that individual involvement was better than group involvement:
This project talks about really personal stuff and the only way I can talk openly and honestly is because I’ve had a chance to get to know you [public involvement lead] face-to-face and because I trust you. It wouldn’t work otherwise.
Young advisor A
Yeah we are young people as well so there’s always that level of vulnerability and it’s quite a sensitive issue . . . [substance misuse] is quite a shameful thing to some people . . . I find it very awkward to talk about it with people I don’t know.
Young advisor B
Involvement in the study required young advisors to draw on their own experiences as users of substance misuse services and consider the way in which their family and wider networks had helped or hindered their recovery. But the commonly cited benefit of young people gaining useful skills and experience through involvement was potentially problematic in this study:
As much as I would love to put on my CV that I’ve been involved . . . people might wonder why I’ve been an advisor to a drug project . . . it just raises a few question marks . . . I do always have that worry that they’re going to think ‘Oh she was a druggie’ and yes it’s the truth but I don’t want every employer knowing that stuff.
Young advisor B
In addition to the issue of the complex lives of the young people, as discussed earlier, we also had the challenge of trying to identify young people who had used substance misuse services in the past but who were now in a position to reflect back on their experience. Feedback from services suggested that many young people who fit this description may have moved on and may no longer be in contact with services, may not wish to look back on a difficult period in their lives or indeed may have relapsed. Either way they may no longer be engaged with services. In fact, some of the young people who became involved in the study were actually still using (both substances and services) and the model of involvement had to be adapted accordingly. Waldman139 points out that young people with complex needs, especially if they are living in care or in crisis, as was the case for many of the young people involved in the Y-SBNT study, may have felt powerless about decisions affecting their life and find it difficult to actively say ‘no’ to involvement, instead opting out by remaining silent or not responding to contact. This was certainly our experience as, despite various attempts to obtain feedback from young people involved early on in the project, all of the young people who opted out of further involvement did so by not responding to contact rather than actively opting out. However, both of the young people who contributed to this chapter have had periods when they have been unable to be involved in the project but have subsequently re-engaged with it when their circumstances changed. We found that there was a balance between keeping in contact and leaving the door open and not making young people, many of whom were still using services and being contacted regularly by professionals about appointments and commitments, feel ‘hassled’. The resulting lack of evaluation data or other feedback means that we can only hypothesise about why other young people given information on the project did not choose to become, or stay, involved. However, the role of services appears to be key, as were our initial attempts to recruit mainly through e-mail contact with services and written information sheets for young people:
Personally, if I was to see something on the internet or on a piece of paper, I probably wouldn’t be that interested, I like to see people and be able to find out about things face-to-face if I can.
Young advisor A
Keeping in touch was sometimes problematic, as many of the young people involved were in hostel or other temporary accommodation and moved several times during the course of the project, as well as changing mobile phones. Lack of internet access and other personal reasons also meant that many of the young people we involved did not have regular access to a computer or the internet and/or chose not to use e-mail or social media. Although social media can be a really useful tool for public involvement in research140 and some young people were quite enthusiastic about it in principle, others had reservations:
I don’t really like to mix work with any other part of my social life basically . . . closed [Facebook] groups are a great way to stay in touch for some people but there’s always those other difficulties like what boundaries you’re going to have about what to say, it’s difficult because social media is such an open network . . . I prefer e-mails and texts because that’s just to me.
Young advisor B
Not social media as anything could be said, creating additional issues for the young person.
Young advisor at 11/15 meeting
Again, a flexible approach was needed and we found that most of our communication with young people was actually by text message, mobile phone call, post or face-to-face meeting.
The role of services
Researchers’ access to children and young people is tightly controlled141,142 and generally requires the permission of adults. 143 The involvement of young people requires working with gatekeepers, including professionals and parents, who can influence consent and can both enable and constrain young people’s involvement. 143,144 Young people can be powerless in this process and reliant on significant adults to decide what information they should be given and whether they can participate. 59 Although gatekeepers often play an important role in safeguarding the interests of young people, ‘they can also act to exert power over young people to prevent their voices being heard’ (p. 142). 132 Children in care or otherwise deemed to be ‘vulnerable’ may also be denied the opportunity to be involved in research because of this perceived vulnerability145 or because services do not have a culture of participation themselves:
I really liked how I’m being heard for once [as an advisor in the Y-SBNT study] . . . I’ve been in many services where I’ve had to bite my tongue or I’m just not being heard, and I’ve not got that freedom of speech the way I should.
Young advisor A
In the Y-SBNT study services proved to be both barriers to, and enablers of, young people’s involvement. It was sometimes difficult to engage the interest of services in the potential opportunities that involvement could provide for young people:
Some professionals don’t see the value of these projects and don’t commit to recruiting young people. Without this you just can’t engage young people and do projects like this.
Young advisor B
Some services were also reluctant to pass information on to young people because they were concerned about young people being too vulnerable or, conversely, because they thought that young people might not be ‘academic’ or reliable enough. The young people who did get involved in the project felt that it was important to emphasise that this was not in fact the case:
[Tell young people that] you don’t have to be a scientist, you don’t have to be a genius, all you have to do is have experience of using these services and that’s the skill [required].
Young advisor B
The challenge for us was often getting the information to young people so that they could make their own informed choice about whether or not they were interested in getting involved. On the other hand, when we were able to successfully involve young people in the project the role of services was crucial – both in recruitment and in supporting their ongoing engagement:
The young people who have become engaged have almost all done so because someone in a service has got what we’re doing and has actively promoted it.
Public involvement lead, TMG public involvement review focus group
I went [to initial Y-SBNT consultation meeting] because [support worker] told me about it and she was very enthusiastic about it . . . You need to make [therapist] understand the importance of this so they don’t go to the kid and they say ‘oh well there’s this thing and I don’t really know much about it’ . . . the lack of enthusiasm and the lack of belief in it definitely comes across if the social worker doesn’t think it’s worth your time . . . a lot of [therapists] are very protective over their clients if they feel that they’re a little too vulnerable or, I hate that term, chaotic.
Young advisor B
All of these issues were identified at some point in our attempts to involve young people in the Y-SBNT study, as discussed above. In this model we have added ‘current circumstances’ to the characteristics of young people, to reflect the complex lives and sometimes frequently changing circumstances of the young people with whom we were working. In addition, we have added ‘interest and understanding’ to attitudes of adults as it was the therapists who ‘got’ the study and the potential benefits of involvement for young people who were key to getting and keeping young people involved in the project. This is linked to, but different from, beliefs and values (e.g. understanding the importance of young people having a voice) and time constraints (the services we contacted had many other demands on their time and many were also going through organisational change).
Developing a different approach to involving young people
As well as developing and piloting the Y-SBNT intervention the study aimed to explore ways in which young people with experience of using substance misuse services could be involved in a study of this nature. This chapter therefore concludes with a suggested model for the involvement of young people in similar future studies.
A young advisor’s perspective
You need to go out to more substance misuse services and say ‘can you help us . . . can you provide us with [access to] young people if they are interested?’ and explore different avenues. Put the word out: maybe get a day with a drug and alcohol service, ask them how many young people they’ve got on their caseloads, just introduce the project and give them more information about what we’re doing and what we want to do, and seeing if they are interested. If you don’t get the results you want from one place I’m sure there will be a different service to go to.
To get young people interested in a project like this I think you need another young person, someone who’s walked the walk sort of thing, so they can understand on a deeper level. Personally, if I was to see something on the internet or on a piece of paper, I probably wouldn’t be that interested, I like to see people and be able to find out about things face-to-face if I can. But if you can arrange a day at a service you could see if you can talk to some young people while you’re there. Then you can give them the options of just having a chat or getting more involved, but with no rush and no pressure so more like: ‘what do you lot think about the project? Would you like to get involved or not like to get involved? If so how would you like to be involved?’ Just get them to talk to you.
Young advisor A
Facilitators’ summary of feedback from young advisors at the April 2015 meeting on what future involvement could look like
-
The idea of involvement being linked closely to a few services was seen as important. For example, some of us would probably have been unlikely to attend this first meeting without support from staff.
-
Some form of group with ongoing involvement based around face-to-face meetings is still the best way to do involvement, but this should be flexible as people might want or need to move in and out of the study and one-to-one meetings might work better for some young people.
-
There should also be the opportunity for us to be involved between group meetings. This could be by e-mail or post and/or face-to-face, for example one-to-one meetings and/or service-based local groups combined with longer meetings where everyone comes together from different areas.
-
Ideally you should start setting up a group of young advisors a year or so before the study begins. Young people could then be involved in proposal development and possibly developing films and other materials about their experiences, which could be used in training and recruitment. We would also like to be involved in a few different projects, not just one.
The young people, research team and TSC felt that, ultimately, some form of ongoing group was the best way to involve young people, but that this needed to be more flexible and young people centred than a fixed-location YPAG with a largely static membership. As outlined by the young advisors above, any model for involvement should ideally be developed in consultation with young people – recruiting those with an interest and then working out with them what they would like to be involved in and how best to do this. Young people and researchers both said that they preferred face-to-face meetings, either in groups or individually, if possible. This could be combined with telephone calls and communication by post when input was needed in between meetings.
Proposed involvement model
-
Hub and spoke model with a core ongoing group of young people, who might change over time, alongside one-to-one and small group work and one-off consultations. Depending on the availability and interests of the young people involved, this group could meet regionally (e.g. with support from substance misuse services working with young people) as well as coming together nationally (e.g. through day meetings or longer residential meetings) and possibly provide advice and support to other studies in the field.
-
The group could be a combination of older young people (e.g. mid- to late 20s) who are able to look back on their experiences and possibly more short-term and flexible involvement with young people currently using services. Some of these may be young people in adult services.
-
Involvement would be closely linked to a few services, with an element of a public involvement budget set aside for these services to recruit and provide ongoing support to young advisors as well as hosting young advisor and/or consultation meetings.
-
Young people would be involved in recruitment for public involvement, both initially during visits to services and through ‘snowballing’ through young people recruited as advisors.
-
Ideally, a group would be established before a project started, so that young people are able to be involved in the development of the proposal and support the recruitment of a new group of young advisors, as well as possibly being able to be involved in other studies in the field:
Before you even get to a full trial, if you are working with a group of young people you can build up trust with them, build up a relationship with them in the hope that they might go on to be a kind of core network.
TSC public involvement review focus group
-
Young people would be involved at all stages of the research, from proposal development to dissemination and, when possible, would be given opportunities to be actively involved as part of the research team as well as being consulted by them.
-
The main role of the public involvement lead(s) in this model would be to plan involvement activity, facilitate links between young people and researchers through the services and evaluate this involvement, with services taking the lead on recruitment and retention as above. All members of the research team would ideally also be allocated time to feed into, and plan for, public involvement (particularly those who, unlike the public involvement leads, are directly involved in the study on a day-to-day basis). Management support is also essential to embedding young people’s involvement in the study rather than it being seen as an ‘add-on’:
What embedding participation in a project like this would mean is that we don’t think of it as special or anything different it’s just normal to think about it as part of the project. To have the young people there in a reciprocal relationship.
Researcher, TMG public involvement review focus group
-
Linked to wider discussions within the NIHR and elsewhere about making young people’s involvement in research more inclusive, diverse and accessible.
-
Parental involvement should also be considered but, given the complicated family relationships of many young people involved in the study, it may be necessary to broaden this out to other people who have played an important role in young people’s lives and recovery.
Summary
Although we had originally planned to have a standing YPAG of 10–12 young people who would be actively engaged throughout the project, the model we ended up with was rather different. We faced challenges in identifying and recruiting young people affected by substance misuse who might be interested in being involved and young people who did express an interest were also often at points in their lives or living in circumstances that made it difficult for them to commit to ongoing involvement. Nonetheless, young people were actively involved throughout the project and their input informed key elements of the intervention and research process, recruitment and training materials, data collection tools, data analysis and interpretation and reporting (including this chapter), as well as plans for involvement in dissemination, The revised model for young people’s involvement that emerged from this process was more flexible and focused on what worked best for the young people involved.
Chapter 9 Discussion
The primary objectives of this feasibility trial were to assess the acceptability of the adapted family and social network intervention, investigate the likely recruitment and retention rates and obtain information that could be used in the planning and conduct of a future large definitive trial. In addition, we set out to explore and develop models of patient and public involvement that could support the involvement of young people in a study of this nature in the future.
Within the context of significant service changes that took place during the study period the delivery of the pilot posed a number of significant practical challenges (e.g. both of participating young people’s services taking part went through retendering processes part-way through the study, with one of the sites changing to a different provider organisation). There were changes not only in the organisational management and processes of the participating services but also to staff teams. Early work with provider organisations had to be revisited with the new organisations and their managers. These challenges had to be faced and resolved to deliver the study. The recent current policy of UK substance misuse service regular retendering146 poses significant problems for service continuity and delivery that can also potentially impact on the delivery of clinical research trials.
Despite these challenges, the study team managed to deliver the research study to achieve the stated aims. The early adaptation work led to the conclusion that, overall, the components and structure of the original adult SBNT intervention were relevant and acceptable to the younger age group and therapists delivering interventions in young people’s services. Materials were developed based on consultation with young people and were used for training that was perceived as appropriate by the therapists and managers in the service sites. Organisational change led to the loss of two therapists early in the trial period but sufficient therapists remained engaged to deliver the pilot treatment.
Interviews with the therapists delivering Y-SBNT in the trial and one of their managers demonstrated that the new intervention was received enthusiastically. Although there were familiar frustrations and challenges regarding the research process (in terms of data collection and randomisation), all five therapists and the manager were positive about the new treatment approach and saw potential value in it. Key elements appeared to be taking a wider perspective on a young person’s problems, involvement of a support network and the intervention’s structured approach. From the perspective of those delivering the treatment intervention, it was therefore found to be acceptable and promising and indeed participating therapists reported that some aspects have been integrated into their routine work since the trial.
The training provided as part of the trial was well received by therapists and supervision was perceived to be helpful. It was also contrasted with regular ongoing routine supervision for TAU, which appears to be less structured and frequent. Ongoing case-based clinical supervision appears to be rare in routine UK addiction practice and yet it is at the heart of psychosocial intervention delivery. The impact of different models of supervision in current services may need further exploration.
The sample of young people recruited into the study appeared to be representative of those young people entering UK treatment for substance misuse in terms of demographics, substance use and other associated problems (e.g. Public Health England1). The young people displayed a complex picture of substance use and mental health problems, with both treatment arms improving over time in terms of the main outcome.
The quantitative findings demonstrated that the Y-SBNT intervention also appeared to be acceptable to the young people, with 85% (n = 22) of participants in the Y-SBNT group attending at least one treatment session and 42% (n = 11) attending all six. In terms of areas of further intervention development, the high (42%) level of treatment completion in the sample is promising and important. We aimed to recruit 60 participants to ensure that we obtained outcome data from at least 32 participants at both 3 and 12 months post randomisation. Although the final recruitment figure fell marginally shy of this target at 53 randomised participants, the required sample size of 32 participants (16 per group) providing primary outcome data at each time point was achieved as attrition rates were lower than anticipated due to extensive efforts to maintain high follow-up rates by researchers. Thirty-nine of the 53 randomised (74%) participants provided data for the end point of primary clinical interest, the TLFB interview at month 12, specifically the proportion of days on which the participants used their primary substance in the 90 days before this time point. These data were analysed to obtain the effect size and one-sided 80% confidence limit. The effect size for the main clinical outcome at month 12 was negative (–0.32), indicating that the average proportion was lower in the TAU group than in the Y-SBNT group (0.41 vs. 0.54). The upper 80% confidence limit of –0.05 suggests that the desired effect size of 0.3 is unlikely to be achieved in a definitive, powered trial. The equivalent confidence limit at month 3 was greater at 0.11 but still lower than our prespecified threshold. As an exploration we conducted secondary analyses using different frequency scoring methods for the TLFB interview (e.g. 90 vs. 30 days; main substance vs. polysubstance use); however, we did not find that the results differed significantly from the preplanned main clinical outcome analyses reported.
There appeared to potentially be a short-term effect of the intervention on the emotional well-being of the participants. Average scores for the total SDQ score and the impact subscale of the SDQ favoured the Y-SBNT group at 3 months post randomisation, but the effect reversed at month 12 so that the TAU group appeared to perform better. At month 12, the TAU group tended to experience slightly greater emotional well-being and the problems that they did experience had a lesser impact on their lives than in the Y-SBNT group. In addition, the treatment effect was negative for all three subscales of the FRI at both month 3 and month 12, indicating that members of the Y-SBNT group tended to experience higher levels of conflict and lower levels of cohesion and expressiveness in their family environment than the TAU group throughout their participation in the trial. However, the WAI results suggest that participants and their therapists in the Y-SBNT group had a greater perceived relationship than in the TAU group; however, these results might be greatly influenced by the low response rates for the WAI in the TAU group. Although the TAU group seemed to report that important people in their lives used less of their primary substance and fewer supported their use of the substance, the Y-SBNT group reported greater levels of support for accessing treatment from members of their support network. It was feasible to measure network size and components of network substance use in this trial, which have been shown to be important in predicting treatment outcomes in adult populations;85 however, the sample size was too small in this study to draw meaningful conclusions in terms of the impact of the intervention. The use of the IPDA interview is not recommended as the scoring schema is complex and the results are difficult to interpret in a meaningful way. It is difficult to draw any robust conclusions from the results of the analyses of the secondary outcomes as all analyses were intended to be purely exploratory.
The results from the health economic analyses are limited to some extent by the small sample size. Because of this small sample size, high-cost cases fell into either group by chance and this resulted in direct comparisons of the two groups being inconclusive. Despite this, the results from both groups indicate a higher than average use of health-care resources for this age group. 147 The number of contacts with policing and the criminal justice system in both groups also suggest that, to capture the whole impact of the intervention, a perspective beyond the NHS should be considered in a future trial. A number of more specific recommendations also emerged.
The complete case analysis shows that there was a similar EQ-5D-5L index score at baseline in both groups. The TAU group appeared to have a slightly better improvement in index score than the Y-SBNT group over the 12 months. However, the mean imputed data show that those lost to follow-up in the TAU group are likely to have lower EQ-5D-5L index scores at baseline, whereas the same is not seen for Y-SBNT group. The difference in EQ-5D-5L index scores at baseline between groups may be a result of the small sample size. The specific age group (12–18 years) of the young people in this study might have limited the applicability of the EQ-5D-5L, which was developed and validated among an adult population (aged ≥ 18 years). The youth version of the EQ-5D (EQ-5D-Y) is not suitable either, given that the target population of this measure is those aged 7–12 years. The suitability of the EQ-5D-5L for use with young people would require further study, which is beyond the scope of this research project. The EQ-5D-5L is a relatively new measurement and to the best of our knowledge it has not been validated against the other outcome measures in this trial.
The piloting of the health-care, social services and criminal justice services resource use questionnaire proved that it is feasible to collect such information through self-report in this population. However, a few structural issues and ambiguous phrasing in questions were also revealed, resulting in some of the data being unusable but also providing ample scope for improvement in the future. Moreover, responses to the open question, although incomplete and unusable in analysis, point out certain services that should be looked into more closely among this population, such as the social service for children in need and foster care. Because of the complexity of the services, a more specific section for social services resource use should be developed. Finally, the long recall period of 12 months for the resource use questionnaire could have impacted on the reliability of the results. Although we were aware of this potential unreliability, the burden on participants of completing this questionnaire at an additional follow-up point may have been too great and may have resulted in more missing data. Completing the resource use questionnaire as part of the 3-month follow-up may have been confusing for participants as there would have been different lengths of recall at each follow-up point and this could have resulted in double counting. Ideally, follow-up at 6 months would have been carried out, but health economic data collection was constrained by the trial design. Given that we did not have any other sources for this information, the 12-month recall period was the best that we could do.
In terms of intervention delivery and acceptability, we found that all stakeholders had positive views of the intervention while also identifying several challenges. Whether a young person with a substance misuse problem was ready or able to talk to important people in their social network and seek their support was a major theme both in the early adaptation work and in the later qualitative exploration. This in turn may have led to challenges in achieving the involvement of network members during sessions. The result of this may have been that, although therapists were able to review young people’s social networks during sessions using some of the therapeutic tools (e.g. social network diagram) and discussing how the young people could access their support, the more active ingredient of inviting network members to participate in sessions, and actively to develop further ways of supporting the young people’s efforts to change, occurred less often. The extent to which this is essential for further improved outcomes remains a question for future research. One possible conclusion is that, overall, Y-SBNT was well received, but perhaps more time needs to be spent with the young people to achieve greater network member participation and, in general, more thought needs to be given to this issue, perhaps along the lines suggested during the qualitative interview with the service manager. This would suggest that further development and process exploration work is necessary before moving to further trial research. Furthermore, it was evident from the results that some therapists were more able to engage network members in sessions than others and the underlying reasons for this difference need to be explored further.
The process rating measure adapted from the UKATT PRS95 provided a feasible tool for the assessment of the Y-SBNT intervention. It was feasible to use with the available recorded sessions and it appeared to differentiate between the experimental intervention and TAU. The main differences between the two arms appeared to be related to both the social focus of the therapeutic work and the more structured approach of Y-SBNT, which contrasted with TAU. There were challenges, however, in obtaining recorded sessions because of participants refusing consent for sessions to be recorded even though consent was given for trial participation. This tendency was more marked in the TAU group and has implications for future work of this nature with this population. The precise reasons behind the refusal of consent need to be better explored and understood.
Is it possible that the intervention is better suited to some cases than others? The notion of treatment matching has been explored with adult addiction treatments, although little evidence has been found to support this. 148,149 In our study we could not explore this quantitatively given the low number of participants but some of the qualitative data suggest that some participants may be more open/receptive to this type of approach. As previous research has shown,18 many young people experience, at least to some degree, an element of ‘coercion’ into treatment that may impact on motivation to engage and pursue change. One interesting indication from the quantitative data was that those young people referred into treatment through the YOTs had worse outcomes than those referred through other means. The qualitative research showed that many participants did not appear to regard their substance use as particularly problematic. Some young people attended treatment because they had been in trouble with school authorities and/or criminal justice agencies or because their parents were worried about them, rather than because they wished themselves to do something to change their substance use. It will be important to address in future research how different processes of referral are associated with young people’s perceptions of their substance problems, motivation to change, treatment engagement and ultimately outcomes.
Although we had originally planned to have a standing YPAG of 10–12 young people who would be actively engaged throughout the project, the model that we achieved was rather different. We faced challenges in identifying and recruiting young people affected by substance misuse who might be interested in being involved and young people who did express an interest were also often at points in their lives or living in circumstances that made it difficult for them to commit to ongoing regular sustained involvement. There were also difficulties in maintaining contact with many of the young people.
Children and young people are not a homogeneous group and we found that the standard public involvement model of a fixed-location YPAG was not sufficiently inclusive and flexible for the young people with complex needs whom we wished to involve in this study. Despite these challenges young people were actively involved throughout the project and their input has informed key elements of the intervention and the research process, including analysis and writing. We also found that services were fundamental in keeping many young people involved, not just as gatekeepers through whom we could recruit but also as a source of ongoing support.
Strengths and limitations of the study
There are a number of strengths and limitations of this pilot feasibility study. The successful implementation of the intervention in routine UK services constitutes a strength and occurred despite the upheaval caused to both services by the current policies of addiction service retendering. There was some attrition from the workers trained in Y-SBNT in the West Midlands service, two of whom could not be included in the qualitative sample. The changes in management in the West Midlands service also meant that it was not possible to interview a service manager who had insight into the trial implementation at that site over a sufficient time period to provide a perspective.
We faced significant challenges in engaging family and network members, both in the public involvement aspects of the work and in the qualitative interviews. The limited representation of this group is a weakness. Only two network members were interviewed in the North East whereas our original target was 10 network members, five from each site, which would have allowed us to achieve a better overview of the experiences of treatment of the different types of network members involved.
Engagement of wider social networks of young people affected by substance misuse problems in services and research remains a challenge. There appeared to be a number of factors at play that led to the limited engagement of network members in both the intervention and the research aspects of the study. First, the more practical aspect of co-ordinating diaries and locations with the network members and young people for sessions added a level of complexity and on some occasions proved challenging.
In addition, there appears to be a more fundamental conceptual question of the more dominant individual orientation of substance misuse services for both young people and adults, which places less emphasis on the social context of substance use and impacts. 150,151 There appeared to be some resistance from some young people towards the engagement of social networks, for example those referred from the YOT were used to working on a one-to-one basis and looked on information sharing and involving others in their treatment with suspicion, particularly if having to talk openly about their substance use. Equally, more work could be carried out with therapists to increase clarity over the way that the intervention is presented to young people and the nature of network member involvement. It is important to ensure that young people are aware that it is their choice who to include and that network member involvement does not have to focus on substance use but, for example, network members can help with activities that take young people away from their drug or alcohol use. Lessons learnt from the qualitative and public involvement work about network member involvement include the use of more innovative approaches to who constitutes a network member by, for example, concentrating on natural networks (where they still exist) and involving positive peers. Network members should be aware of and agree on the nature of their involvement, providing support that is not time or role limited (this is particularly salient for young people whose networks are composed of professional supporters).
We would argue that there needs to be an organisational shift to support working in a contextual and family-focused way, with resources available for outreach work and flexibility for appointment times, with lunchtime and early evening sessions available, adequate support and supervision for socially focused work. Previous work has shown the need to consider several factors when developing family-focused practice, including those at the service provider, organisational and wider health system levels (e.g. Hampson152).
For research purposes it would be useful to have more flexibility in terms of being able to carry out telephone interviews with network members, which may lead to increased recruitment of family samples. The challenges in engaging family and wider social network members as well as measuring any potential benefits of social and family interventions for this group of young people are not new, remain a limitation and constitute an important area for future research. In future studies we will seek to ensure that public involvement includes family and other members of young people’s social networks, taking into account the lessons learnt.
The robust public involvement aspects of the study were a strength, with many positive contributions from young people in terms of the adaptation of the intervention and the production of materials for trial recruitment, as well as trial conduct and the analyses and interpretation of the trial results. Despite challenges in implementing a regular, stable, ongoing advisory group, which was our original plan, we managed to develop recommendations for the involvement of this important and often neglected group of young people in future studies based on the evidence from the trial. The time taken to establish a group of young advisors with ongoing involvement also meant that it was difficult for many young people to have involvement in the initial stages of the project. We therefore plan to explore the possibility of establishing a group or network of young advisors prior to the start of future research studies so that they can be actively involved in planning both the research and how young people can best be involved. We hope that the learning from this study, and the model for involvement that emerged, will contribute to the wider literature on young people’s involvement in health research, particularly in relation to studies and other involvement activity with young people whose voices are less frequently heard.
The main clinical outcome measure was based on the primary problem substance use over the previous 90 days using the TLFB interview. 77 It became clear during the trial that a number of young people were using a range of substances including ‘legal highs’ in addition to their main problem substance and the narrow focus on only one substance in the current context of multiple substance use may be limited as a primary outcome. Appendix 21 describes the substance use of the whole sample recruited at baseline, illustrating the extent of use of different substances. Of particular importance here is also the fact that many young people reported in both the qualitative and the public involvement work that their aim on entering treatment was not always focused on substance-related change but on other aspects of their lives. Hence, significant changes in substance use over a relatively short period of time may be unrealistic.
We aimed to explore in detail the components of TAU as delivered to young people within the two participating sites. Because of the refusal of consent to record sessions, the number of recordings available to carry out this work was small and hence the conclusions (reported in Chapter 7) can be only very preliminary at this stage.
Overall, the health economics work led to important learning points. Although there were some ambiguous questions in the resource use questionnaire, the measure managed to capture the general picture of resource use in this population. The inclusion of the policing and criminal justice system contacts provided the preliminary evidence that would support using a wider perspective for the analysis of this intervention.
Generalisability of the results
There are limitations with regard to the generalisability of the intervention given the nature of the results.
However, some of the findings from a feasibility point of view, including trial implementation in routine practice, methods for the recruitment and retention of young people, the findings in terms of broader mental health care and service use, the criminal costs that characterise this group of young people with complex needs and the recommendations for patient and public involvement in relation to this group of young people can all inform future UK research in this area within routine addiction services.
The health-care resource and social services use in both groups was higher than average. This result, although preliminary, indicates both a high demand for both resources and a potentially very large impact of interventions on health-care and social services costs for this group.
Implications for future research/development of the intervention
The findings of this feasibility trial do not support a recommendation for a full trial of the Y-SBNT intervention compared with TAU at this stage without further intervention development work. However, a number of possible implications emerged for future research on interventions with young people with substance misuse problems, which are as follows.
-
Lessons learnt from recruitment and retention have wider implications for trial delivery with this participant group. The impacts of referral source are important in determining samples for future studies.
-
There are implications also for measurement both in terms of the main primary outcomes but also in terms of some secondary outcomes: focusing on one substance, as with the TLFB interview, in the current context of multiple substance use may be limited as a primary outcome; the use of the IPDA interview is not recommended as the results are difficult to interpret in a meaningful way.
-
There are also recommendations regarding the collection of data related to health economics: validation of the EQ-5D for the 12–18 years age group needs to be considered; there should be appropriate follow-up periods to aid recall and reduce possible double counting; ambiguous phrasing in questions should be avoided; and careful consideration should be given to the complexity of service use among this participant group, indicating a requirement for a more specific, tailored section for the collection of social services resource use.
-
The challenges for trial implementation created by service systems going through regular retendering processes are significant and should be taken into consideration when planning future implementation in the UK of addiction clinical trials. The level of complexity and impact on timings can be significant.
-
Involvement of young people in research studies is crucial, as seen by the important contribution made by the young people in this study, yet models need to be flexible to achieve inclusive representation throughout all aspects of the research process.
-
Obtaining consent to record sessions proved problematic and, as this has implications for future similar work with this population, the precise reasons behind the refusal of consent need to be better explored and understood.
-
The qualitative findings suggest that some young people may be more open to family- and social network-type work or that a longer period of time may be necessary to achieve this stance. A participant’s perceived treatment goals and expectations as well as the duration of the intervention may all need to be considered in future research.
-
In line with research with adult substance users, there is also a need to focus in future studies on processes of change, individual components of interventions, service systems and structures and therapists’ characteristics.
-
The differential success of therapists in engaging network members in sessions provides an example of the importance of therapist factors. As Orford153 suggests, there needs to be a shift to study interventions within the broader, longer-acting systems of which treatment is a part.
Implications for practice
-
Many young people reported in both the qualitative and the public involvement work that, on entering treatment, their aim was not always focused on a change related to their substance use but on a change related to other aspects of their lives.
-
The widening of the focus of substance use interventions to incorporate careful consideration, engagement and, if appropriate, involvement of families and other social network members was well received by all stakeholders.
-
Important considerations suggested by all stakeholders need to be taken into account in future development of social and family-focused interventions and addiction treatment research.
-
The supervision provided in the study arm was positively received by workers and contrasted with usual practice in a way that suggests a need to consider the implementation of this aspect of intervention delivery carefully, particularly at current times of financial constraints on services.
-
Service recommissioning needs to consider carefully impacts on service users and research studies taking place in addition to financial considerations.
-
Further development work is necessary to establish whether the particular strategies of the Y-SBNT approach are best suited to young people at particular stages of their problem recognition. This may involve a more flexible approach, responding to motivational aspects early on before considering the involvement of social networks.
-
Services on the whole can enhance family orientation at the level of practitioner skills, service and organisational policies and systems and wider policy responses.
Acknowledgements
We would like to thank the young people for taking part in this trial, as well as the therapists for recruitment, treatment and completing the trial documentation. Thank you also to the young people’s substance misuse services in Birmingham and Newcastle for accommodating this study and for all of the help received in set-up.
Thank you to all of the young people who were involved in this study as young advisors, particularly BB, SB, CF and SK for their contributions to Chapter 8 of this report. Also, thank you to the service managers and therapists who supported their involvement.
The research group would like to thank Joshan Kadirgamar for his help with secondary analyses of the TLFB interview data.
Finally, we would like to express our gratitude to the TSC and the Data Monitoring Committee member for overseeing the study.
Collaborators
The Y-SBNT collaborators (current and past) are Shabana Akhtar, Sangeeta Ambegaokar, Donna Back, Matthew Bailey, Carmel Bennett, Louca-Mai Brady, Kim Cocks, Alex Copello, Ed Day, Caroline Fairhurst, Annette Fleming, Sarah Gardner, Eilish Gilvarry, Jinshuo Li, Charlie Lloyd, Paul McArdle, Steve Parrott, Tanya Pawson, Charlotte Renwick, Lorna Templeton, Paul Toner, David Torgerson, Val Wadsworth and Judith Watson.
Independent Trial Steering Committee members
Dr Gillian Tober (Chair), Dr Joanne Neale, Professor Jim Orford and Dr Clare Mackie.
Data Monitoring Committee member
Professor Nick Freemantle.
Contributions of authors
Judith Watson (Senior Research Fellow) managed the daily running of the feasibility trial, provided methodological support throughout and co-ordinated the writing of the report.
Paul Toner (Research Fellow) co-designed the study, carried out recruitment and conducted the follow-up data collection and interviews in the North East site, conducted the qualitative data analyses and prepared Chapter 6 of the report.
Ed Day (Senior Clinical Lecturer in Addiction Psychiatry) took part in adaptation of the intervention and production of the new adapted training materials and provided the intervention training and supervision and clinical support.
Donna Back (Research Fellow) co-ordinated the study, carried out recruitment and conducted the follow-up data collection and interviews in the West Midlands site.
Louca-Mai Brady (Independent Researcher) co-led on the design and delivery of public involvement aspects of the study and prepared Chapter 8 of the report.
Caroline Fairhurst (Statistician) conducted the quantitative analyses and prepared Chapter 5 of the report.
Charlotte Renwick (Health Economist) conducted the health economic analyses and prepared Chapter 5 of the report
Lorna Templeton (Independent Researcher) co-led on the design and delivery of public involvement aspects of the study and prepared Chapter 8 of the report.
Shabana Akhtar (Research Fellow) conducted the treatment fidelity rating analyses.
Charlie Lloyd (Senior Lecturer) co-designed the study, provided methodological and qualitative advice throughout the study and provided advice on the qualitative analyses.
Jinshuo Li (Health Economist) conducted the health economic analyses and prepared Chapter 5 of the report.
Kim Cocks (Senior Statistician) provided methodological and statistical support, assisted in developing the data collection questionnaires and prepared the statistical analysis plan.
Sangeeta Ambegaokar (Consultant Child and Adolescent Psychiatrist) provided clinical and trial management support and liaised with the West Midlands services.
Steve Parrott (Senior Health Economist) provided expertise in developing the resource use questionnaire and supervised the health economic analyses.
Paul McArdle (Consultant Child and Adolescent Psychiatrist) provided clinical and methodological support.
Eilish Gilvarry (Clinical Director of Specialties) provided clinical and methodological support and liaised with the North East services.
Alex Copello (Professor of Addiction Research) was chief investigator, co-designed and led all aspects of the study and prepared the final report.
Publication
Watson J, Back D, Toner P, Lloyd C, Day E, Brady L-M, et al. A randomised controlled feasibility trial of family and social network intervention for young people who misuse alcohol and drugs: study protocol (Y-SBNT). Pilot Feasibility Stud 2015;1:8.
Data sharing statement
Full information on all aspects of the trial is available on request from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Young People’s Statistics from the National Drug Treatment Monitoring System (NDTMS) 1 April 2013 to 31 March 2014. London: Public Health England; 2015.
- Smith L, Foxcroft D. Drinking in the UK. An Exploration of Trends. York: Joseph Rowntree Foundation; 2009.
- Fuller E. Smoking, Drinking and Drug Use among Young People in England in 2014. London: National Statistics; 2015.
- Hibell B, Guttormsson U, Ahlström S, Balakireva O, Bjamason T, Kokkevi A, et al. The 2011 ESPAD Report: Substance Use among Students in 36 European Countries. Stockholm: Swedish Council for Information on Alcohol and Other Drugs; 2012.
- Lader D. Drug Misuse: Findings from the 2014/15 Crime Survey for England and Wales. London: Home Office; 2015.
- Hingson RW, Heeren T, Winter MR. Age of alcohol-dependence onset: associations with severity of dependence and seeking treatment. Pediatrics 2006;118:e755-63. http://dx.doi.org/10.1542/peds.2006-0223.
- Lloyd C. Risk factors for problem drug use: identifying vulnerable groups. Drugs 1998;5:217-32.
- Mistral W, Templeton L, Aggleton P, Dennison C, Warwick I. Promoting Health and Wellbeing through Schools. Abingdon: Routledge; 2010.
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, et al. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics 2008;121:290-31. http://dx.doi.org/10.1542/peds.2007-2243D.
- Copello AG, Velleman RD, Templeton LJ. Family interventions in the treatment of alcohol and drug problems. Drug Alcohol Rev 2005;24:369-85. http://dx.doi.org/10.1080/09595230500302356.
- Velleman RD, Templeton LJ, Copello AG. The role of the family in preventing and intervening with substance use and misuse: a comprehensive review of family interventions, with a focus on young people. Drug Alcohol Rev 2005;24:93-109. http://dx.doi.org/10.1080/09595230500167478.
- Foxcroft DR, Ireland D, Lister-Sharp DJ, Lowe G, Breen R. Longer-term primary prevention for alcohol misuse in young people: a systematic review. Addiction 2003;98:397-411. https://doi.org/10.1046/j.1360-0443.2003.00355.x.
- Spoth RL, Redmond C, Trudeau L, Shin C. Longitudinal substance initiation outcomes for a universal preventive intervention combining family and school programs. Psychol Addict Behav 2002;16:129-34. https://doi.org/10.1037/0893-164X.16.2.129.
- Coombes L, Allen D, Marsh M, Foxcroft D. The Strengthening Families Programme (SFP) 10–14 and substance misuse in Barnsley: the perspectives of facilitators and families. Child Abuse Rev 2009;18:41-59. https://doi.org/10.1002/car.1055.
- Szapocznik J, Perez-Vidal A, Brickman AL, Foote FH, Santisteban D, Hervis O, et al. Engaging adolescent drug abusers and their families in treatment: a strategic structural systems approach. J Consult Clin Psychol 1988;56:552-7. https://doi.org/10.1037/0022-006X.56.4.552.
- Dakof GA, Tejeda M, Liddle HA. Predictors of engagement in adolescent drug abuse treatment. J Am Acad Child Adolesc Psychiatry 2001;40:274-81. https://doi.org/10.1097/00004583-200103000-00006.
- Hogue A, Liddle HA. Family-based treatment for adolescent substance abuse: controlled trials and new horizons in services research. J Fam Ther 2009;31.
- Pullmann MD, Ague S, Johnson T, Lane S, Beaver K, Jetton E, et al. Defining engagement in adolescent substance abuse treatment. Am J Community Psychol 2013;52:347-58. http://dx.doi.org/10.1007/s10464-013-9600-8.
- Dembo R, Gulledge L, Robinson RB, Winters KC. Enrolling and engaging high-risk youths and families in community-based, brief intervention services. J Child Adolesc Subst 2011;20:330-50. https://doi.org/10.1080/1067828X.2011.598837.
- Rigter H, Henderson CE, Pelc I, Tossmann P, Phan O, Hendriks V, et al. Multidimensional family therapy lowers the rate of cannabis dependence in adolescents: a randomised controlled trial in Western European outpatient settings. Drug Alcohol Depend 2013;130:85-93. http://dx.doi.org/10.1016/j.drugalcdep.2012.10.013.
- Henggeler SW, Pickrel SG, Brondino MJ, Crouch JL. Eliminating (almost) treatment dropout of substance abusing or dependent delinquents through home-based multisystemic therapy. Am J Psychiatry 1996;153:427-8. http://dx.doi.org/10.1176/ajp.153.3.427.
- Hendriks V, van der Schee E, Blanken P. Treatment of adolescents with a cannabis use disorder: main findings of a randomized controlled trial comparing multidimensional family therapy and cognitive behavioral therapy in the Netherlands. Drug Alcohol Depend 2011;119:64-71.
- Hock R, Priester MA, Iachini AL, Browne T, DeHart D, Clone S. A review of family engagement measures for adolescent substance use services. J Child Fam Stud 2015;24:3700-10.
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy Theory Res Pract 1979;16:252-60.
- Diamond GM, Liddle HA, Hogue A, Dakof GA. Alliance building interventions with adolescents in family therapy: a process study. Psychotherapy 1999;36:355-68.
- Sexton TL, Alexander JF. Functional Family Therapy Clinical Training Manual. Baltimore, MD: Annie E. Casey Foundation; 2004.
- Tuerk EH, McCart MR, Henggeler SW. Collaboration in family therapy. J Clin Psychol 2012;68:168-78. http://dx.doi.org/10.1002/jclp.21833.
- Robbins MS, Liddle HA, Turner CW, Dakof GA, Alexander JF, Kogan SM. Adolescent and parent therapeutic alliances as predictors of dropout in multidimensional family therapy. J Fam Psychol 2006;20:108-16. http://dx.doi.org/10.1037/0893-3200.20.1.108.
- Liddle HA, Dakof GA, Henderson C, Rowe C. Implementation outcomes of Multidimensional Family Therapy-Detention to Community: a reintegration program for drug-using juvenile detainees. Int J Offender Ther Comp Criminol 2011;55:587-604. http://dx.doi.org/10.1177/0306624X10366960.
- Coatsworth JD, Santisteban DA, McBride CK, Szapocznik J. Brief strategic family therapy versus community control: engagement, retention, and an exploration of the moderating role of adolescent symptom severity. Fam Process 2001;40:313-32. https://doi.org/10.1111/j.1545-5300.2001.4030100313.x.
- Branson CE, Barbuti AM, Clemmey P, Herman L, Bhutia P. A pilot study of low-cost contingency management to increase attendance in an adolescent substance abuse program. Am J Addict 2012;21:126-9. http://dx.doi.org/10.1111/j.1521-0391.2011.00204.x.
- Westin AML, Barksdale CL, Stephan SH. The effect of waiting time on youth engagement to evidence based treatments. Community Ment Health J 2014;50:221-8. https://doi.org/10.1007/s10597-012-9585-z.
- Liddle H. Family-based therapies for adolescent alcohol and drug use: research contributions and future research needs. Addiction 2004;9:76-92. https://doi.org/10.1111/j.1360-0443.2004.00856.x.
- Drug Misuse: Psychosocial Interventions. London: NICE; 2007.
- Fals-Stewart W, Kashdan TB, O’Farrell TJ, Birchler GR. Behavioral couples therapy for drug-abusing patients: effects on partner violence. J Subst Abuse Treat 2002;22:87-96. https://doi.org/10.1016/S0740-5472(01)00218-5.
- Copello A, Templeton L. The Forgotten Carers: Support for Adult Family Members Affected by a Relative’s Drug Problems. London: UK Drug Policy Commission; 2012.
- Asen E. Outcome research in family therapy. Adv Psychiatr Treat 2002;8.
- Boys A, Farrell M, Taylor C, Marsden J, Goodman R, Brugha T, et al. Psychiatric morbidity and substance use in young people aged 13-15 years: results from the Child and Adolescent Survey of Mental Health. Br J Psychiatry 2003;182:509-17. https://doi.org/10.1192/bjp.182.6.509.
- McNicoll A. Young people’s drug support hit by ‘devastating’ cuts. Druglink 2011;26. www.drugwise.org.uk/wp-content/uploads/Druglink-Jul-Aug-2011.pdf (accessed 13 December 2016).
- Cortese CA. Drug services and cultural adaptation. Drugs 1999;6:361-6.
- Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training. Clin Psychol Sci Pract 2006;13:295-310.
- Bernal G, Jimenez-Chafey M, Domenech Rodriquez MM. Cultural adaptation of treatments: a resource for considering culture in evidence-based practice. Prof Psychol Res Pract 2009;40:361-8.
- UKATT Research Team . Cost effectiveness of treatment for alcohol problems: findings of the randomised UK Alcohol Treatment Trial (UKATT). BMJ 2005;331. http://dx.doi.org/10.1136/bmj.331.7516.544.
- Alcohol-Use Disorders. Diagnosis, Assessment and Management of Harmful Drinking and Alcohol Dependence. London: British Psychological Society and Royal College of Psychiatrists; 2011.
- Beattie MC, Longabaugh R, Elliott G, Stout RL, Fava J, Noel NE. Effect of the social environment on alcohol involvement and subjective well-being prior to alcoholism treatment. J Stud Alcohol 1993;54:283-96. https://doi.org/10.15288/jsa.1993.54.283.
- Havassy BE, Hall SM, Wasserman DA. Social support and relapse: commonalities among alcoholics, opiate users, and cigarette smokers. Addict Behav 1991;16:235-46. https://doi.org/10.1016/0306-4603(91)90016-B.
- Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network support for drinking, Alcoholics Anonymous and long-term matching effects. Addiction 1998;93:1313-33. https://doi.org/10.1046/j.1360-0443.1998.93913133.x.
- McCrady BS. To have but one true friend: implications for practice of research on alcohol use disorders and social network. Psychol Addict Behav 2004;18:113-21. http://dx.doi.org/10.1037/0893-164X.18.2.113.
- Wasserman DA, Stewart AL, Delucchi KL. Social support and abstinence from opiates and cocaine during opioid maintenance treatment. Drug Alcohol Depend 2001;65:65-7. https://doi.org/10.1016/S0376-8716(01)00151-X.
- Mohr CD, Averna S, Kenny DA, Del Boca FK. ‘Getting by (or getting high) with a little help from my friends’: an examination of adult alcoholics’ friendships. J Stud Alcohol 2001;62:637-45. https://doi.org/10.15288/jsa.2001.62.637.
- Galanter M. Network Therapy for Alcohol and Drug Abuse (Expanded Edition). New York, NY: Guilford; 1999.
- Meyers RJ, Dominguez TP, Smith JE, Van Hasselt VB, Hersen RK. Sourcebook of Psychological Treatment Manual for Adult Disorders. New York, NY: Plenum; 1996.
- Chaney EF, O’Leary MR, Marlatt GA. Skill training with alcoholics. J Consult Clin Psychol 1978;46:1092-104. https://doi.org/10.1037/0022-006X.46.5.1092.
- Copello A, Orford J, Hodgson R, Tober G. Social Behaviour and Network Therapy for Alcohol Problems. London: Brunner Routledge; 2009.
- Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expect 2014;17:637-50. http://dx.doi.org/10.1111/j.1369-7625.2012.00795.x.
- Staley K. Exploring Impact: Public Involvement in NHS, Public Health and Social Care Research. Eastleigh: INVOLVE; 2009.
- Kirby P. A Guide to Actively Involving Young People in Research: For Researchers, Research Commissioners, and Managers. Eastleigh: INVOLVE; 2004.
- Including Children in Social Research. London: National Children’s Bureau; 2002.
- Powell MA, Smith AB. Children’s participation rights in research. Childhood 2009;16:124-42. https://doi.org/10.1177/0907568208101694.
- Shaw C, Brady L-M, Davey C. Guidelines for Research with Children and Young People. London: National Children’s Bureau Research Centre; 2011.
- Alderson P. Research by children. Int J Soc Res Methodol 2001;4:139-53.
- Kellett M. How to Develop Children as Researchers: a Step by Step Guide to Teaching the Research Process. London: Sage; 2005.
- Brady LM, Davey C, Shaw C, Blades R, Beresford P, Carr S. Social Care, Service Users and User Involvement: Building on Research. London: Jessica Kingsley; 2012.
- Fleming J, Boeke T. Involving Children and Young People in Health and Social Care Research. London: Routledge; 2012.
- Jamal F, Langford R, Daniels P, Thomas J, Harden A, Bonell C. Consulting with young people to inform systematic reviews: an example from a review on the effects of schools on health. Health Expect 2015;18:3225-35. http://dx.doi.org/10.1111/hex.12312.
- Boote J. Patient and Public Involvement in Health and Social Care Research: A Bibliography 2011. www.nottingham.ac.uk/clahrc-ndl-nihr/documents/ppi/08-boote-2011-ppi-bibliography.pdf (accessed 15 May 2016).
- Mawn L, Welsh P, Stain HJ, Windebank P. Youth Speak: increasing engagement of young people in mental health research. J Ment Health 2015;24:271-5. http://dx.doi.org/10.3109/09638237.2014.998810.
- Franklin A, Sloper P. Listening and responding? Children’s participation in health care within England. Int J Child Rights 2005;13:11-29. https://doi.org/10.1163/1571818054545277.
- Webb E, Horrocks L, Crowley A, Lessof N. Using the UN Convention on the Rights of Children to improve the health of children. Paediatr Child Health 2009;19:430-4. https://doi.org/10.1016/j.paed.2009.05.006.
- United Nations . Convention on the Rights of the Child 1989. www.ohchr.org/EN/ProfessionalInterest/Pages/CRC.aspx (accessed 26 May 2016).
- Copello A, Williamson E, Orford J, Day E. Implementing and evaluating social behaviour and network therapy in drug treatment practice in the UK: a feasibility study. Addict Behav 2006;31:802-10. http://dx.doi.org/10.1016/j.addbeh.2005.06.005.
- Day E, Copello A, Seddon J, Christie M, Bamber D, Powell C, et al. Pilot study of a social network intervention for heroin users in opiate substitution treatment: study protocol for a randomized controlled trial. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-264.
- Watson J, Back D, Toner P, Lloyd C, Day E, Brady L-M, et al. A randomised controlled feasibility trial of family and social network intervention for young people who misuse alcohol and drugs: study protocol (Y-SBNT). Pilot Feasibil Stud 2015;1. https://doi.org/10.1186/s40814-015-0004-4.
- Cocks K, Torgerson DJ. Sample size calculations for pilot randomized trials: a confidence interval approach. J Clin Epidemiol 2013;66:197-201. http://dx.doi.org/10.1016/j.jclinepi.2012.09.002.
- Gillick v. West Norfolk and Wisbech Area Health Authority and Department of Health and Social Security 1985.
- MRC Ethics Guide. Medical Research Involving Children. London: MRC; 2004.
- Sobell MB, Maisto SA, Sobell LC, Cooper AM, Cooper T, Sanders B, et al. Evaluating Alcohol and Drug Abuse Treatment Effectiveness: Recent Advances. New York, NY: Pergamon Press; 1980.
- Dennis ML, Funk R, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction 2004;99:120-8. http://dx.doi.org/10.1111/j.1360-0443.2004.00859.x.
- Waldron HB, Kern-Jones S, Turner CW, Peterson TR, Ozechowski TJ. Engaging resistant adolescents in drug abuse treatment. J Subst Abuse Treat 2007;32:133-42. http://dx.doi.org/10.1016/j.jsat.2006.07.007.
- Levy S, Sherritt L, Harris SK, Gates EC, Holder DW, Kulig JW, et al. Test–retest reliability of adolescents’ self-report of substance use. Alcohol Clin Exp Res 2004;28:1236-41. https://doi.org/10.1097/01.ALC.0000134216.22162.A5.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: a pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry 1998;7:125-30.
- Achenbach TM, Rescorla L. Manual for the ASEBA School-Age Forms and Profiles: an Integrated System of Multi-informant Assessment. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families; 2001.
- Goodman R. Psychometric properties of the Strengths and Difficulties Questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45. https://doi.org/10.1097/00004583-200111000-00015.
- Zywiak WH, Neighbors CJ, Martin RA, Johnson JE, Eaton CA, Rohsenow DJ. The Important People Drug and Alcohol interview: psychometric properties, predictive validity, and implications for treatment. J Subst Abuse Treat 2009;36:321-30. http://dx.doi.org/10.1016/j.jsat.2008.08.001.
- Moos RH, Moos R. Family Environment Scale Manual. Palo Alto, CA: Consulting Psychologists Press; 1986.
- Moos RH, Moos BS. Family Environment Scale Manual and Sampler Set: Development, Applications and Research. Palo Alto, CA: Mind Garden, Inc.; 2009.
- Kumpfer KL, Xie J, O’Driscoll R. Effectiveness of a culturally adapted strengthening families program 12–16 years for high-risk Irish families. Child Youth Care Forum 2012;41:173-95.
- Henderson CE, Dakof GA, Greenbaum PE, Liddle HA. Effectiveness of multidimensional family therapy with higher severity substance-abusing adolescents: report from two randomized controlled trials. J Consult Clin Psychol 2010;78:885-97. http://dx.doi.org/10.1037/a0020620.
- Boyd CP, Gullone E, Needleman GL, Burt T. The Family Environment Scale: reliability and normative data for an adolescent sample. Fam Process 1997;36:369-73. https://doi.org/10.1111/j.1545-5300.1997.00369.x.
- Moos RH, Moos BS. Environment Scales Manual, Development, Applications and Research. Palo Alto, CA: Mind Garden, Inc.; 2009.
- The EuroQol Group . EQ-5D-5L User Guide: Basic Information on How to Use the EQ-5D-5L Instrument (Version 2.0) n.d. www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/UserGuide_EQ-5D-5L_v2.0_October_2013.pdf (accessed 4 March 2015).
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. http://dx.doi.org/10.1007/s11136-011-9903-x.
- Horvath A, Greenberg L. Development and validation of the Working Alliance Inventory. J Couns Psychol 1989;36:223-33. https://doi.org/10.1037/0022-0167.36.2.223.
- Tober G, Clyne W, Finnegan O, Farrin A, Russell I. UKATT Research Team . Validation of a scale for rating the delivery of psycho-social treatments for alcohol dependence and misuse: the UKATT Process Rating Scale (PRS). Alcohol Alcohol 2008;43:675-82. http://dx.doi.org/10.1093/alcalc/agn064.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2010;152:726-32.
- Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr 1974;19:716-23.
- Battjes RJ, Gordon MS, O’Grady KE, Kinlock TW, Carswell MA. Factors that predict adolescent motivation for substance abuse treatment. J Subst Abuse Treat 2003;24:221-32. https://doi.org/10.1016/S0740-5472(03)00022-9.
- Miller L, Davies M, Greenwald S. Religiosity and substance use and abuse among adolescents in the National Comorbidity Survey. J Am Acad Child Adolesc Psychiatry 2000;39:1190-7. https://doi.org/10.1097/00004583-200009000-00020.
- Patrick ME, Schulenberg JE. Prevalence and predictors of adolescent alcohol use and binge drinking in the United States. Alcohol Res 2013;35:193-200.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Efron B, Tibshirani R. An Introduction to the Bootstrap. New York, NY: Chapman & Hall; 1993.
- Chaudhary MA, Stearns SC. Estimating confidence intervals for cost-effectiveness ratios: an example from a randomized trial. Stat Med 1996;15:1447-58. https://doi.org/10.1002/(SICI)1097-0258(19960715)15:13<1447::AID-SIM267>3.0.CO;2-V.
- Willan AR, O’Brien BJ. Confidence intervals for cost-effectiveness ratios: an application of Fieller’s theorem. Health Econ 1996;5:297-305. https://doi.org/10.1002/(SICI)1099-1050(199607)5:4<297::AID-HEC216>3.0.CO;2-T.
- Severens JL, De Boo TM, Konst EM. Uncertainty of incremental cost-effectiveness ratios. A comparison of Fieller and bootstrap confidence intervals. Int J Technol Assess Health Care 1999;15:608-14.
- Curtis L. Unit Costs of Health and Social Care 2014. Canterbury: PSSRU, University of Kent; 2014.
- Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ 2004;13:1203-10. http://dx.doi.org/10.1002/hec.901.
- Orford J, Hodgson R, Copello A, John B, Smith M, Black R, et al. The clients’ perspective on change during treatment for an alcohol problem: qualitative analysis of follow-up interviews in the UK Alcohol Treatment Trial. Addiction 2006;101:60-8. http://dx.doi.org/10.1111/j.1360-0443.2005.01291.x.
- Boyatzis R. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage Publications; 1998.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Young People in Research: How to Involve Us. Guidance for Researchers from the PEAR Young People’s Public Health Group. London: National Children’s Bureau; 2010.
- NHS Staff Council . NHS Terms and Conditions of Service Handbook. Amendment Number 36 – Pay and Conditions Circulars (AfC) Number 1 2016 and Number 2 2016 2016. www.nhsemployers.org/∼/media/Employers/Documents/Pay%20and%20reward/afc_tc_of_service_handbook_fb_version_36.pdf (accessed 15 December 2016).
- NHS Reference Costs 2013/14. London: Department of Health; 2014.
- Prescription Cost Analysis England 2013. London: HSCIC; 2014.
- Field S. Flows and Costs in the Criminal Process. London: Home Office; 1997.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: PSSRU, University of Kent; 2013.
- Public Expenditure Statistical Analyses 2013. London: The Stationery Office; 2013.
- Phillips C, Brown D. Entry into the Criminal Justice System: a Survey of Police Arrests and their Outcomes. London: Home Office; 1998.
- HM Courts & Tribunals Service Annual Report and Accounts 2012–13. London: The Stationery Office; 2013.
- Legal Services Commission Annual Report and Accounts 2012–13. London: The Stationery Office; 2013.
- Crown Prosecution Service Annual Report and Accounts 2012–13. London: The Stationery Office; 2013.
- Offender Management Statistics Bulletin, England and Wales (Quarterly – January to March 2014). London: Ministry of Justice; 2014.
- Prison and Probation Performance Statistics 2014 to 2015. The Management Information Addendum (NOMS Annual Report). London: Ministry of Justice; 2015.
- Gibson B, Cavadino P. The Criminal Justice System – An Introduction. Hook: Waterside Press; 2008.
- Barber JP, Mercer D, Krakauer I, Calvo N. Development of an adherence/competence rating scale for individual drug counseling. Drug Alcohol Depend 1996;43:125-32. https://doi.org/10.1016/S0376-8716(96)01305-1.
- National Institute for Health Research . Young Person’s Advisory Group n.d. www.nihr.ac.uk/nihr-in-your-area/children/young-persons-advisory-group.htm (accessed 12 December 2016).
- DECIPHer . What Is ALPHA? n.d. http://decipher.uk.net/public-involvement/young-people/ (accessed 12 December 2016).
- Patient and Public Involvement in Research and Research Ethics Committee Review. Eastleigh: INVOLVE; 2016.
- INVOLVE . Payment and Recognition for Public Involvement n.d. www.invo.org.uk/resource-centre/payment/ (accessed 12 December 2016).
- INVOLVE . Benefits Advice Service for Involvement n.d. www.invo.org.uk/resource-centre/benefits-advice-service/ (accessed 17 January 2017).
- Boeck T, Fleming J, Fleming J, Boeke T. Involving Children and Young People in Health and Social Care Research. London: Routledge; 2012.
- Moules T, Lowes L, Hulatt I. Involving Service Users in Health and Social Care Research. London: Routledge; 2005.
- Clavering EK, McLaughlin J. Children’s participation in health research: from objects to agents?. Child Care Health Dev 2010;36:603-11. http://dx.doi.org/10.1111/j.1365-2214.2010.01094.x.
- Hanley B, Bradburn J, Barnes M. Involving the Public in NHS, Public Health and Social Care Research: Briefing Notes for Researchers. Eastleigh: INVOLVE; 2004.
- Kirby P, Lanyon C, Cronin K, Sinclair R. Building a Culture of Participation: Involving Children and Young People in Policy, Service Planning, Delivery and Evaluation. London: Department for Education and Skills; 2003.
- Franks M. Pockets of participation: revisiting child-centred participation research. Child Soc 2011;25:15-2. https://doi.org/10.1111/j.1099-0860.2009.00258.x.
- Beresford P. Service users’ knowledges and social work theory: conflict or collaboration?. Br J Soc Work 2000;30:489-503. https://doi.org/10.1093/bjsw/30.4.489.
- Lee RM. Doing Research on Sensitive Topics. London: Sage Publications; 1993.
- Waldman J, Lowes L, Hulatt I. Involving Service Users in Health and Social Care Research. London: Routledge; 2005.
- Guidance on the Use of Social Media to Actively Involve People in Research. Eastleigh: INVOLVE; 2014.
- Alderson P, Fraser S, Lewis V, Ding S, Kellett, M, Robinson C. Doing Research with Children and Young People. London: Sage; 2004.
- Sinclair R. Participation in practice: making it meaningful, effective and sustainable. Child Soc 2004;18:106-18. https://doi.org/10.1002/chi.817.
- Hood S, Kelley P, Berry M. Children as research subjects: a risky enterprise. Child Soc 1996;10:117-28. https://doi.org/10.1002/(SICI)1099-0860(199606)10:2<117::AID-CHI17>3.0.CO;2-U.
- Cree VE, Kay H, Tisdall K. Research with children: sharing the dilemmas. Child Fam Soc Work 2002;7:47-56. https://doi.org/10.1046/j.1365-2206.2002.00223.x.
- Berrick J, Frasch K, Fox A. Assessing children’s experiences of out of home care: methodological challenges and opportunities. Soc Work Res 2000;24:119-27. https://doi.org/10.1093/swr/24.2.119.
- Mohammadi D. Addiction services in England: in need of an intervention. Lancet Psychiatry 2014;1:421-2. http://dx.doi.org/10.1016/S2215-0366(14)00015-7.
- Hippisley-Cox J, Vinogradova Y. Trends in Consultation Rates in General Practice 1995/1996 to 2008/2009: Analysis of the QResearch Database. London: NHS Information Centre for Health and Social Care; 2009.
- Project MATCH Research Group . Matching alcoholism treatments to client heterogeneity: Project MATCH three year drinking outcomes. Alcohol Clin Exp Res 1998;22:1300-11. https://doi.org/10.1111/j.1530-0277.1998.tb03912.x.
- UKATT Research Team . UK Alcohol Treatment Trial: client–treatment matching effects. Addiction 2007;103:228-38. https://doi.org/10.1111/j.1360-0443.2007.02060.x.
- Copello A, Orford J. Addiction and the family: is it time for services to take notice of the evidence?. Addiction 2002;97:1361-3. https://doi.org/10.1046/j.1360-0443.2002.00259.x.
- Adams P. Switching to a social approach to addiction: implications for theory and practice. Int J Ment Health Addict 2016;14:86-94. https://doi.org/10.1007/s11469-015-9588-4.
- Hampson C. Integrating Family-Focused Practice into Routine Addiction Services 2013.
- Orford J. Asking the right questions in the right way: the need for a shift in research on psychological treatments for addiction. Addiction 2008;103:875-85. http://dx.doi.org/10.1111/j.1360-0443.2007.02092.x.
- Brady LM, Templeton L. SB and BB (young advisors) . Involving children and young people in research: not the usual suspects. INVOLVE Newsletter n.d.:1-2. www.invo.org.uk/posttypenewsletter/winter-2014-15/ (accessed 1 March 2015).
Appendix 1 Review of reviews: search strategy
The PsycINFO, EMBASE, Web of Knowledge, PubMed and MEDLINE databases were searched from 1996 until June Week 2 2013. The following strategies were used.
Search terms:
A. child* or adolescent*
B. AND alcohol or “alcohol abuse” or ethanol or “alcohol dependence” or “substance abuse” or “substance use disorder*”
C. AND Family Intervention (subject heading)
D. AND review or “meta analysis” or “meta-analysis”
E. Combine searches A, B, C, and D
Results = 690 (17 sources from PsycINFO, 185 sources from EMBASE, 336 sources from Web of Knowledge, 142 sources from PubMed and 10 sources from MEDLINE).
Criteria for exclusion
Articles were excluded if they met any of the following criteria.
-
They were not written in English.
-
They were not peer-reviewed articles.
-
They did not specifically focus on interventions but on preventions.
-
They did not focus on children and/or adolescents.
-
They did not evaluate the efficacy of a minimum of two different family-based interventions.
In addition, the references of the selected articles were screened for further relevant sources. This process yielded one further reference.
Total number of selected articles = 11.
Appendix 2 Patient and public involvement: summary of young people’s involvement and how this informed the study (September 2013–September 2015)
| Date | Young people involved | Meeting/contact | PPI activity | How PPI activity informed the study |
|---|---|---|---|---|
| 13 September 2013 | Attended meeting: F1 and F2 YPs in contact prior to meeting: 6 |
London (plus L-MB and LT) | YA meeting – introduction to the study and PPI; discussion of ways in which YPs might like to be involved | General learning about YPs’ views on getting help and the potential of involving families and networks. Also, learning about how we could involve the YPs attending and others going forward. Discussions informed the development of intervention and supporting materials. The materials generated from discussion with YPs that enhanced the adapted intervention included examples from the YPs in terms of processes perceived as important to obtain social network support; good and bad aspects of services; examples of social network diagrams from YPs that were used to develop examples in the manual; and an example of an open letter from a YP to a family member included as an appendix to the manual. In addition, the discussion about how to present the intervention to YPs and how to introduce the idea of social network support was incorporated into the materials that were used for therapist training |
| 24 October 2013 | Attended meeting: F1 and F3 YPs in contact prior to meeting: 4 |
London (plus L-MB, LT, AC and DB) | YA meeting – discussion, about YPs’ views on the Y-SBNT study and intervention; exercise to explore YPs’ perceptions of what makes a good and bad experience of a service and what facilitates them to engage with, and stay engaged with, services; introduction to idea of networks and exercise to explore whom YPs perceive to be important in their lives, who supported them with regard to their substance misuse and why and when they found people unhelpful or unsupportive; discussion on the first draft of the trial leaflet and information sheet | General learning about YPs’ views on getting help and the potential of involving families and networks. Discussions informed the development of intervention and supporting materials as presented above. The trial leaflet and information sheet were significantly revised as a result of YPs’ input, including wording, presentation and the use of simple language |
| 3 December 2013 | Attended meeting: F3 and F4 YPs in contact prior to meeting: 5 |
London (plus L-MB, LT, AC and DB) | YA meeting – update on project/activity to date; discussion of revised recruitment materials following last meeting and newsletter sent to YPs after meetings; exercise to explore YPs’ views on the mechanisms of change involved in Y-SBNT; discussion of YPs’ thoughts and responses to the key components of Y-SBNT and their relevance to YPs | General learning about YPs’ views on getting help, the potential of involving families and networks and things to think about when developing the new intervention. Discussions informed the development of the intervention and supporting materials as already outlined above. Comments influenced the style and content of future newsletters |
| 15 January 2014 | F2 | London (plus L-MB) | One-to-one meeting in lieu of F2 attending the December 2013 meeting | Incorporated into outcomes from the December 2013 YA meeting |
| 23 January 2014 | Attended meeting: F5, F6 and M1 | Bristol (plus LT and Bristol worker) | YA meeting – general discussion about the project, the intervention and how YPs could get involved; repeated two exercises completed with other YPs (sort card regarding helpful interventions and networks – see notes on 24 October 2013 meeting for details of exercises and their rationale) | General learning about YPs’ views on getting help, the potential of involving families and networks and things to think about when developing the new intervention. Discussions informed the development of intervention and supporting materials as already described. F5 has remained engaged since this time; attempts were made to keep in touch with F6 and M1 but they did not remain engaged |
| 5 March 2014 | F5 | Bristol (plus LT) | One-to-one meeting – supported YP to write an open letter to someone important to her outlining how that person has supported her to date, when they have been unhelpful and what they could have done differently to support her; discussed and obtained content for newsletter to be circulated to all YPs engaged with the PPI element of the study to date | Open letter included with the intervention materials as an example of the type of communication strategy that could be used as part of the intervention work with YPs. Quotations from YPs used in newsletter and also in later publications (conferences and article) |
| 19 March 2014 | F5 | Bristol (plus LT) | One-to-one meeting – asked YP for her views on a ‘setting goals worksheet’ drafted by other team members for the intervention manual (used to explore areas of life YP might want to work on during Y-SBNT treatment sessions); asked YP to draw her social support diagram (a core component of the intervention) to detail all those who are important to her, who has been important with regard to support (and how) and who has not (and why not) | The ‘setting goals’ worksheet was revised in light of comments. The goal-setting worksheet was adapted to the areas that the YP felt were relevant and important for this client group. The social network diagrams developed informed examples that were used for training and training materials once details were carefully anonymised |
| 6 March 2014 | M2 and M3 | Didcot (plus L-MB and two workers) | General introduction to the project and PPI – exercise to map YPs’ social networks; commenting on a draft ‘setting goals’ worksheet to be used to explore areas of life YPs might want to work on during Y-SBNT treatment sessions | General learning about YPs’ views on getting help, the potential of involving families and networks and things to think about when developing the new intervention. Discussions informed the development of the intervention and supporting materials. The ‘setting goals’ worksheet was revised in light of YPs’ feedback. Note that network exercises completed at several of the above meetings were used to develop sample YP networks, which were included as part of the intervention materials. Both of the YPs said that they were interested in further involvement but contact then faded between them and the project workers despite several attempts to contact them and keep them updated on opportunities |
| 24 April 2014 | F5 | Bristol (plus PT, BD and LT) | The two research fellows spent some time with the YP, piloting all of the trial questionnaires and how they would be introduced to YP in the trial and discussing any queries/comments, etc., raised by the YP | Informed data collection processes with YP (see meeting on 30 April 2014 with F7 and F8) |
| 30 April 2014 | None directly | Cutting Edge conference (L-MB and LT) | Conference presentation to substance misuse project workers based in the south-west about the Y-SBNT project and some of the emerging learning from PPI about engaging and working with YPs who use substance misuse services | Raised awareness of the study and our attempts to involve YPs in the research. Useful feedback from project workers and others present about working with this ‘hard-to-reach’ group of YPs |
| 30 April 2014 | F7 and F8 | Birmingham (plus PT and DB) | Meeting with YPs to pilot questionnaires – see 24 April 2014 | This and the meeting on 24 April 2014 helped researchers to come to a better understanding of how they could be more consistent in their approach to both administering the questionnaires and introducing the assessment. The YPs’ feedback helped to identify the most effective way to get information about the assessment across to study participants (e.g. mentioning at the start that they would have to complete a consent form to take part, etc.). Going through the TLFB interview with YPs gave the researchers an appreciation of the importance of building up a picture of a YP’s recent life before asking about his or her substance use and suggested some useful prompts for doing this. For both the TLFB interview and the IPDA interview the YPs highlighted potential issues with recall and how to best capture poly-drug use, as well as giving insights into potential difficulties with some of the assessments and the need for consistent prompts. The YPs also highlighted some potential problems with the IPDA questions for professionals, which were taken into consideration by the research team |
| 6 May 2014 | F5 | Bristol (plus LT) | An update meeting to keep engaged – updated YP on the project and how YP could get involved; gave her the opportunity to ask questions, etc. | Update meeting – general discussions informed learning of research team about issues around involving this group of YP (e.g. payment of YP, future involvement of YP in the project, measuring drug use) |
| 12 June 2014 | F5 | Bristol (plus LT) | Update meeting to keep YP engaged – at the request of other members of the research team discussed measuring drug use, particularly when YPs are using multiple drugs and do not always know what they are taking | |
| 22 September 2014 | F5 | Bristol (plus LT and L-MB) | Update meeting – discussed proposed changes to involvement of YP in the project including increase in payment rate, ideas for future meetings and involvement in next stages of the project; also discussed some of the challenges faced in recruiting and retaining YP for PPI in the study and YP’s thoughts on how we could do things differently in the rest of the study and a possible full trial | Discussions informed the revised plan for Y-SBNT PPI and subsequent involvement of YP |
| 12 November 2014 | F7 | Birmingham (plus L-MB and LT) | Brief introduction meeting to tell YP a bit about the project and PPI and see if she was interested in being involved | A new young advisor |
| 17 November 2014 | F7 | INVOLVE conference (plus L-MB and LT) | Conference presentation about emerging learning from involving YP in the Y-SBNT study. YP talked about her experience of being involved and why she thought it was important for YP with direct experience of substance misuse services to be involved in a study such as the Y-SBNT study | Raised awareness of PPI in the Y-SBNT study and our efforts to involve ‘less frequently heard’ YP in clinical research. Also raised issues of who does and does not get involved in research and whether the usual model for PPI with YP (standing advisory groups) may work better for some YP than others Presentation led to invitation to write an article (which we co-authored with F5 and F7) for the INVOLVE newsletter,154 which equally raised awareness |
| January/February 2015 | F7 | Telephone conversation and one-to-one meeting in Birmingham | Discussions about payment and revised payment for PPI plus opportunities for and interest in involvement in the next stages of the research; also discussion about contribution to the INVOLVE newsletter article and possible attendance at future TMG and TSC meetings; discussed qualitative interview schedule | Article submitted to INVOLVE with contributions from F5 and F7. F7 was due to attend both the TSC and the TMG meetings in February 2015 but was unable to do so because of illness/other issues. Comments on the qualitative interview schedule were fed back and incorporated into the revised schedule when possible (feedback on what was and was not changed was then fed back to F7) |
| 1 April 2015 | F7, F9, F10 and M4 YP in contact prior to meeting: 6 |
Birmingham (plus L-MB, AC, DB, PT and two workers from Newcastle) | YA meeting – overview of project, how we have involved YPs in the project so far, how this involvement has informed the project to date and emerging learning on YPs’ involvement; session led by research fellows on retention and engagement, with the YPs asked to pair up and, with support from the therapists, record their thoughts on the best way of keeping in touch with YPs taking part in the study, payment and the presence of social network members in treatment sessions; discussion on how YPs might be involved in the remainder of the study and how involvement might look in a full trial | Discussions and exercises informed research team learning about future involvement of YPs in the remainder of the study and a possible full trial. In discussions on retention and engagement the YPs reported that they preferred contact with one key person whom they trusted. The researchers used this model and liaised through therapists with YPs still engaged with the service. This was a positive experience and resulted in positive feedback from staff involved:You’ll be pleased to know one of my YP whom you interviewed has just asked when you were coming back to re-interview himTAU therapist |
| 29 September 2015 | Attended meeting: F9, F11 and M5 YP in contact prior to meeting: 7 |
York (plus L-MB, LT, CL, PT and two workers from Newcastle) | YA meeting focused on obtaining YPs’ input into qualitative analysis – introduced the YPs to the key concepts in qualitative data analysis and then gave them a selection of quotations from the qualitative interviews with YPs and asked them to see if they could identify any ways in which this information could be grouped together; research fellow (PT) then led a session to get YPs’ input on emerging findings from the analysis to date; meeting ended with an evaluation and discussion about if and how YPs might want to be involved in writing up and dissemination | Further explanation provided by the YAs was used to help interpret key quotations, for example why some YPs appeared to benefit from the intervention, whereas others did not. Also, the themes that the YAs suggested were integrated with the researchers’ initial themes to add further descriptive detail to the qualitative analysis. Evaluation feedback was used to inform plans for the location, timing and content of future meetings as well as to inform a model of how YPs who have used substance misuse services might be involved in other studies |
| Ongoing contact | Mainly F5 and F7 but some contact with Newcastle YPs | By post, text, telephone and e-mail | All YPs were sent letters and a newsletter about the April 2015 and September 2015 meetings and potential opportunities for involvement in analysis, writing up and dissemination. This was followed up with e-mails, texts and contact with services as applicable. Additional contact with F5 and F7 mainly to keep in touch and keep them updated on the project and opportunities for involvement | One YP (F7) contributed to the draft PPI chapter via a telephone interview. The telephone interview was recorded and quotations were used, with the YP’s consent, in the chapter. Material from the meeting with F5 in September 2014 was also used in the draft chapter in a similar fashion |
Summary of engagement
-
Engaged a total of 16 young people in patient and public involvement activity over the course of the project (as well as those involved in piloting).
-
The young people came from five locations (London, Bristol, Birmingham, Didcot and Newcastle), 11 were female and five were male and the age range of the young people was 16–21 years, with an average age of 18 years.
-
Met with 10 young people once, four twice and two on five or more occasions.
-
Held a total of 18 face-to-face meetings with young people by the end of the study, plus presentations at two conferences (with a young person involved with one of these). In between meetings contact was mainly by post, text message or telephone call as most young people involved in the project did not have access to e-mail.
-
Seven newsletters were sent to young people over the course of the project, mainly linked to meetings: October, November and December 2013, March and October 2014 and March and October 2015.
Appendix 3 Examples of outputs from young people’s involvement in the study
This appendix summarises seven activities that involved young people, supported with illustrative examples from activities and discussions.
1. Young advisor meeting (October 2013): exploring issues emerging from the literature review
Young people were given cards that summarised features of interventions identified through the literature review and were asked to identify things that were important to them and whether there was anything that they would add to the list (Box 4).
Young people were given cards that summarised features of interventions identified through the literature review and were asked to identify things that were important to them and whether or not there was anything that they would add to the list.
Cards that the YPs stickered as important (in no particular order)-
Keeping in touch with me by telephone or in person.
-
More frequent contact with a service or counsellor if I need it or want it.
-
Preparing me/others for the end of contact with the service/counsellor.
-
Flexible help to meet my needs. There are options available and I can choose what will best meet my needs. Help with everyday things like budgeting and shopping.
-
Worker understands me and what I have to say. Listens! It’s not just a form filling exercise.
-
Good communication that has a clear goal and is focused on what’s important.
-
Having a good relationship with the counsellor.
-
Setting goals and targets to achieve them.
-
Services that are appropriate and are for YPs with similar problems. A gap in services for YPs aged 18–24 years and need for transition services.
-
Suitable workers matched with YPs (i.e. male–male, female–female, preferences). Mentoring support?
-
Make sure that the service recognises dual diagnosis and offers the appropriate support.
-
Alternative therapies (e.g. homeopathy, acupuncture, seeds, shiatsu, etc.).
-
Having an overall structure to the service and a clear ending.
-
Worker listens carefully to what I say and understands what I am saying. Why would they not listen?
-
Someone who understands how I feel – they can see things from my point of view.
-
Giving realistic hope about change.
-
Not having to wait long to get help or to have counselling sessions.
-
Being rewarded for attendance and/or good progress. Why should we be rewarded?
-
Using text, Twitter, etc. to keep in touch. Keep it formal by text, telephone; do not use social media.
-
Help that focuses on my strengths rather than negative or bad things.
-
An individualised service that is tailored to my needs, it’s not a ‘one size fits all’. One YP mentioned the need for out-of-hours support.
YP, young person.
Italic text highlights comments from the young people.
2. Young advisor meeting (October 2013): network exercise
Young people were asked to think about important people in their lives and whether they were helpful/supportive or unhelpful/unsupportive to their recovery and record this on two pieces of flip chart paper using sticky notes. One young person suggested a third ‘neutral’ category of people who were neither helpful nor unhelpful. The results of this exercise are detailed in Box 1.
3. Young advisor meeting (December 2013): key components of social behaviour and network therapy
Young people were presented with the key components of SBNT (the adult intervention) and asked to think about how they might be important or relevant to young people. Their views of the key components of SBNT and their relevance to young people are detailed in Table 2.
4. Excerpts from an open letter written by a young person for the youth social behaviour and network therapy training materials (March 2014)
To an important person in my life,
I want to try and help you understand drugs. I’m not going to try and persuade you that drugs are great or that I don’t have problems, because I know that both statements are wrong.
. . . You’ve supported me through many dark times and I can see that you care deeply for me (as I, you). However, your lack of experience with drugs completely dominates your treatment of me and I want you to know that it’s not helping me. You’re a caring, strong and loyal person, but you seem to think I am oblivious to the dangers surrounding drugs and that’s simply not true.
Growing up in a family with drug, alcohol, mental health and financial problems, I’m fully aware of the effect drugs can have . . . I think about it every day and in fact it still affects me today . . . .
At the end of the day, your strict rules and dictatorship will never motivate me to stop using . . . you are just further demonstrating not only your lack of understanding, but your lack of desire to understand. I don’t want you to sit back and let me smoke weed 24/7 either. Simply display an interest in my perspective. That way, I’ll know that you’re trying and that you see me as an equal; two things that are necessary for me to want to listen to you . . . .
. . . Maybe instead of judging me, you could have come with me to my drug counselling. Instead of making a formal complaint about my social worker because she knew and didn’t tell you, you could have recognised that she could see I was responsible and mature . . . .
. . . There are a number of ways you could have handled the situation in a much more helpful and supportive way. Don’t ban me from smoking weed entirely, straight away. Talk to me about the feelings that make me want to be stoned all day and work with me to identify replacement activities, or distractions . . . perhaps an incentive would have helped. Something small but worth it, to keep me going when all I want is a joint, and to show me that you recognise how hard I’ve worked when I cut down.
I can’t stress enough how your totalitarian approach to me doing drugs made me feel. I felt misunderstood, patronised and so, so guilty. These three emotions only work to strengthen my desire to smoke, and lessen my willpower to stop. Threatening to kick me out and shouting at me for having weed in my room in front of the neighbours was very damaging, and it pushed you and me further apart. I need to be able to freely talk to you if I’m to make progress.
After everything, I completely understand why you acted the way you did . . . You care about me and you genuinely thought you were doing the right thing . . . .
Thank you for reading.
5. Consultation meeting (March 2014): comments on the worksheet
Young people discussed a draft worksheet for practitioners, which suggested areas of life that young people might want to work on during treatment sessions in the Y-SBNT pilot. Feedback included:
-
‘Drug and alcohol use’ needs to come first, but young people liked the idea that this was not the only area to be worked on.
-
‘Legal/crime’ makes an assumption that all young people accessing services are engaged in criminal activity; it will not be relevant to everyone and could put people off. Young people suggested a more general category around what young people were doing (‘regular/recent activity’), including education/work, accessing other services and legal/criminal activity.
-
‘Family relationships’ is important but could be problematic for some young people who are estranged from their families or whose parents have problems of their own. Also, where do girlfriends/boyfriends or other relationships fit into these categories? – they are often key enablers/barriers to recovery. How about ‘family and other significant relationships’?
-
‘Social life and friends’ could be broader; how about ‘free time’.
-
Young people suggested a fifth category of ‘living arrangements’. Many of the young people to whom we have spoken have lived in hostels or institutional care; where and how young people live can be key to recovery.
6. Young advisor meeting (April 2015): discussion on retention and engagement
Young people were asked to pair up and record their thoughts on each of the questions below using Post-it notes. We then put the Post-it notes (text written in italics) on flip chart paper and had a whole group discussion (text written in bold). Responses included:
-
What is the best way of keeping in touch with young people taking part in the study?
-
How do we avoid them feeling too pressured by this contact? Do you think asking if we can contact young people on social media (e.g. Facebook, Twitter) is OK? What about text, WhatsApp [WhatsApp Inc., Mountain View, CA, USA] or letter? How would you feel about a researcher contacting you through these methods?
-
consistency and persistence I think is the best way to stay in contact. Be flexible
ask them when and how is the best way to contact them
Facebook, text, phone, e-mail and letter
family, friends, carers and strangers
Facebook–work = kept separate
Well, maybe in that bigger gap (between 3–12 months) phone people two times a month instead of once just to jog their memory because that is quite a long time for just one phone call.
Young people agreed that having a list of preferred ways to be contacted (including social media such as WhatsApp and Twitter) should be included as part of the consent procedure.
-
Payment – do you think that a £10 voucher for a 1-hour interview with a researcher is enough?
-
What sort of rewards would make you want to take part/stay involved in a study like this?
-
I suppose the young person has to question their motives. I personally think it’s ok. Bearing in mind majority of young people would like to be paid in cash due to financial difficulties
money instead of vouchers, activities (e.g. Blackpool, Alton Towers)
You could get a voucher for coming in and you know then when you come back for the final one, everybody that have done it like, could go on a trip.
Young people also suggested a competition or prize draw.
-
Social network involvement – would you be happy to have important people in your life taking part in your treatment sessions?
-
What do you think would help other young people to have important people involved in their treatment?
-
I suppose to express the importance of positive people in one’s life and to help the young people to identify positive people and if young people can’t identify positive people, introduce them to fellowships that might also help them and benefit them in more than one way
people would be less likely to talk about drug and alcohol problems with important people in the session
7. Young advisor meeting (September 2015): input into qualitative analysis
Young people were given a selection of quotations from the qualitative interviews with young people and asked to identify any ways in which this information could be grouped together. Examples included:
The first three themes relate to family life:
They feel as if they are being confronted when family members are in the room – family reaction.
There is a pattern with family life being bad when young people are on drugs – problems with family.
They all want to keep their mams happy and don’t want to worry their family – worries of the parents.
Following a role-play activity in which two transcripts were read out by researchers and young people the group then reflected on why there may be differences in responses. Young people mentioned the following:
I think they need to take the time to get to know the person and not put an act on as if they really care they have to actually really care about the person.
You have got to be ready to engage with someone.
You would want to go to see someone like [Y-SBNT therapist]. She just understands, she just loves her job and she just cares. Like she just doesn’t give up until she gets somewhere with you, you know what I mean, she’s just lovely.
The final part of the session involved getting the young people’s interpretations and insights into the initial themes identified from the data analysis. The young people provided their feedback on the themes and suggested alternative headings including one they titled ‘realisation’:
Cos you don’t even realise, like you don’t realise what you are doing and you don’t realise how bad it is until the penny drops.
Like ending up in hospital or getting a criminal record or ending up being like really ill.
That’s realisation – having to move away from existing friends.
You could be getting forced to go or doing it for other people [getting help] but then actually end up wanting to do it yourself.
Appendix 4 Study leaflet
Appendix 5 Young person information sheet and consent form
Appendix 6 Data collection forms
Working Alliance Inventory Y-SBNT Therapist and Client forms redacted for copyright reasons.
Appendix 7 Summary of the youth social behaviour and network therapy study
FIGURE 18.
The Y-SBNT study summary.

Appendix 8 Topic guides
Interview schedule: young people
-
Context of the young person
-
Can you tell me what you’re doing at the moment (e.g. studying/working?) and where you live (e.g. still at home/hostel etc.)?
-
Could you tell me how things were in your life before you saw (therapist name) at (service)?
-
Do you think your substance use was a problem then? Did your family/friends see it as a problem?
-
Why did you attend (service name)? Was there pressure put on you to attend? (From family/friends, criminal justice system, school etc. )
-
Could you tell me whether this was your first experience of getting help from a service to look at your substance use?
-
If you have received previous treatment, how did this new intervention compare with this?
-
-
Experience of the new intervention
-
Did you attend all six treatment sessions? If not, why did you not attend some of your sessions?
-
Could you tell me about your experience of receiving this help? Anything you can think of.
-
How did you find the sessions you attended? (What liked most? What liked least?)
-
Were there things about your work with (therapist name) that you found useful? (Ask for specific examples and why this was the case)
-
Were there things about your work with (therapist name) that you didn’t find useful? (Ask for specific examples and why this was the case)
-
Did your worker help you identify who was in your social network?
-
Did you discuss inviting people to join your sessions? Were there any worries you had about inviting family/friends to sessions? Do you have ideas on how this can be done in future? (If not done successfully)
-
Were friends/family involved in your treatment? (Who? Did they turn up at sessions? How much were they involved?) If so, did you find their involvement supportive?
-
Did your relationship with friends/family change over the course of your treatment and in what ways? Have you found friends/family to be helpful and supportive as a result of your treatment? (In what ways?) If not, why not?
-
Did you discuss things that you wanted to achieve with your worker?
-
Has there been any change to your substance use? (In what way has your substance use changed? If no change, why no change?) If there has been a change, what impact has this had on your life in general?
-
Have there been any other changes? (Ask for specific examples and the impact of these changes)
-
Have there been particular issues going on in your life that have made change difficult?
-
Do you think six sessions are enough? How long should these sessions be?
-
Would you have changed anything about your treatment? Do you have any suggestions about how to improve things?
-
-
Summary
-
How did you find filling in the questionnaire after accepting to take part in the study? Did you find the questions relevant/useful?
-
Was there anything that put you off taking part? Would you be happy to take part in a similar study in the future?
-
Interview schedule: therapists
The interview aimed to establish how acceptable clinical staff found Y-SBNT to deliver and their satisfaction with the therapy.
-
How would you describe your experience of delivering Y-SBNT?
-
How have you found the training in Y-SBNT. Was this sufficient? Are there any improvements you could suggest?
-
How have you found the process of including family members and friends as part of the treatment process? (Have any network members come to treatment sessions? How else have they been involved? What are the barriers to their involvement?)
-
Have there been any aspects of the process that you have found particularly useful for promoting substance use change? (What aspects of the therapy in particular and why do you think this was the case?)
-
Have there been any aspects of the process that you have found difficult? (Why do you think this might have been the case? How did you overcome this?)
-
Do you think there is any benefit of including the client’s social network as part of the treatment process? (Any benefit for the substance misuse client? Any benefit for network members?)
-
How do you feel Y-SBNT compares with treatment as usual?
-
Do you think there would be worth in making the approach available more widely? (if so, what sort of training/support would be needed?)
-
If you could change anything about the method what would you change? (Why would you change this? How would you change it?)
Interview schedule: service manager
-
How would you describe your experience of taking part in the Y-SBNT trial?
-
What would you say were the advantages and disadvantages of involvement with the study?
-
Are there any changes you would recommend for a future trial?
-
How do you feel Y-SBNT compares with treatment as usual? (Structure, length of intervention)
-
Do you think there is any benefit in including the client’s social network as part of the treatment process? (Any benefit for the substance misuse client? Any benefit for network members?)
-
Are there other positive aspects of the intervention?
-
What are the negative aspects? If you could change anything about the method what would you change? (Why would you change this? How would you change it?)
-
Do you think there would be worth in making the approach available more widely? (If so, what sort of training/support would be needed?)
-
Are there any plans to continue using Y-SBNT within your service?
-
Describe whether learning from involvement in the study/the intervention will inform future practice?
Interview schedule: network members (clearly involved in the process)
The interview aimed to explore the experiences of family and social network members who took part in Y-SBNT. In particular, it aimed to identify specific aspects of the process perceived to be important in helping and supporting network members, aspects of the intervention that impacted on the young person’s substance use, the impact of their involvement on their relationship with the young person and the acceptability of the intervention.
-
Can you tell me a little about your experience of taking part in your relative’s/friend’s treatment, including treatment sessions (when applicable)?
-
How have you found this experience? How well were you supported in taking part?
-
Do you feel that it has been beneficial for you in any way? (What have you found to be helpful? How has this helped? This could be in relation to their method of coping, their feeling of support, developing a better understanding of substance use, improving the relationship with the young person, etc. )
-
Are there any aspects of the process that you did not find helpful? (Why was this? Can you suggest how this could be improved?)
-
Do you feel taking part in treatment has had any effect on your relative’s/ friend’s substance use? (Are there any aspects of Y-SBNT that you feel were especially important in bringing about such a change?)
Appendix 9 Adverse event documentation
Appendix 10 Important People Drug and Alcohol interview scoring: revised for the Y-SBNT study
Scoring rules for the drug and alcohol version of the Important People instrument
Note: when administering the Important People instrument, best guesses are preferred over ‘don’t knows.’ ‘Don’t knows’ can be coded in drinking status, drinking frequency, drug use status, drug use frequency, reaction to drug use and support for treatment. These are treated as missing data. If a network member has missing data for one of two variables used to calculate a product, the product is treated as missing data as well.
Question topics (see instrument for exact content):
-
name
-
relationship
-
amount of contact
-
importance
-
general support
-
cannabis status
-
illicit drug status
-
alcohol status
-
cannabis frequency
-
illicit drug frequency
-
alcohol frequency
-
reaction to drink or drugs
-
support for treatment.
Index 1: Network size
For each participant, count the number of people (network members) for whom a response to question 9 (‘How has this person felt about your coming for treatment?’) was provided. Take the square root of this number, then convert to a z-score based on the mean and SD of the sample at baseline.
Index 2: Daily network size
Count the number of people who the person has daily (rated 7 on question 3) contact with. Then convert to a z-score based on the mean and SD of the sample at baseline.
Index 3: Importance of the four most important people
The ratings from question 4 are ranked and the four highest values are averaged. Then convert to a z-score based on the mean and SD of the sample at baseline.
Component 1: Network substance involvement
We intend to calculate this in two ways.
Component 1v1: Network substance involvement – version 1 (primary problem substance only)
Select the column relating to the primary problem substance (marked on the top of the IPDA form), that is, cannabis, other illicit drug or alcohol. This version of component 1 consists of substance status and substance frequency of the network members.
C.1.A. Primary problem substance status of network members
To compute this index, a revised primary problem substance status code is created (i.e. recode of question 6a, question 6b or question 6c depending on which is the primary problem).
| Old | Status | New |
|---|---|---|
| 5 | Heavy drinker/user | 3 |
| 4 | Moderate drinker/user | 2 |
| 3 | Light drinker/user | 1 |
| 2 | Abstainer | 0 |
| 1 | Recovering alcoholic/drug user | 0 |
| 8 | Don’t know | 8 |
For each network member, the new substance status code is multiplied by the amount of contact (range 1–7). If the primary problem substance status is 8, then the product is not computed for that person. These products are then summed across the network members and this sum is divided by the number of people whose products were actually computed. This is called VAR01. VAR02 is the number of people in the network with a primary problem substance status (even if this is equal to 8).
Then convert to a z-score based on the mean and SD of the sample at baseline.
C.1.B. Frequency with which network members use the primary problem substance (question 7a, 7b or 7c)
For each person with contact from 1 to 7 and primary substance frequency from 0 to 7, compute the product of contact and the primary problem substance frequency (if the primary problem substance frequency is 8, then this product is not computed). Sum these products to give VAR03. Divide VAR03 by the number of people whose products were actually computed to give VAR04. Divide VAR04 by 49 (7 × 7) to give VAR05. Multiply VAR05 by the number of people with any primary problem substance frequency (even if this is equal to 8) and convert to a z-score to give C.1.B.
To calculate component 1v1, sum the two z-scores C.1.A and C.1.B and then convert to a z-score.
Component 1v2: Network substance involvement – version 2 (all drug and alcohol use)
This component consists of drinking status, drinking frequency, drug use status and drug use frequency of the network members.
C.1.C. Cannabis status of network members
To compute this index, a revised cannabis status code is created from question 6a.
| Old | Status | New |
|---|---|---|
| 5 | Heavy cannabis user | 3 |
| 4 | Moderate cannabis user | 2 |
| 3 | Light cannabis user | 1 |
| 2 | Abstainer | 0 |
| 1 | Recovering cannabis use | 0 |
| 8 | Don’t know | 8 |
For each network member, the new cannabis status code is multiplied by the amount of contact (range 1–7). If the cannabis status is 8, then the product is not computed for that person. These products are then summed across the network members and this sum is divided by the number of people whose products were actually computed. This is called VAR06. VAR07 is the number of people in the network with a cannabis status (even if this is equal to 8).
Then convert to a z-score based on the mean and SD of the sample at baseline.
C.1.D. Frequency with which network members use cannabis (question 7a)
For each person with contact from 1 to 7 and cannabis frequency from 0 to 7, compute the product of the contact and cannabis frequency (if the drinking frequency is 8, then this product is not computed). Sum these products to give VAR08. Divide VAR08 by the number of people whose products were actually computed to give VAR09. Divide VAR09 by 49 (7 × 7) to give VAR10. Multiply VAR10 by the number of people with any cannabis frequency (even if this is equal to 8) and convert to a z-score to give C.1.D.
C.1.E. Other illicit drug use status of network members
To compute this index, a revised drug use status code is created from question 6b.
| Old | Status | New |
|---|---|---|
| 5 | Heavy illicit drug user | 3 |
| 4 | Moderate illicit drug user | 2 |
| 3 | Light illicit drug user | 1 |
| 2 | Abstainer | 0 |
| 1 | Recovering illicit drug use | 0 |
| 8 | Don’t know | 8 |
For each network member, the new other illicit drug use status code is multiplied by the amount of contact (range 1–7). If the other illicit drug use status is 8, then the product is not computed for that person. These products are then summed across the network members and this sum is divided by the number of people who products were actually computed for. This is called VAR11. VAR12 is the number of people in the network with an other illicit drug use status (even if this is equal to 8).
Then convert to a z-score based on the mean and SD of the sample at baseline.
C.1.F. Frequency with which network members use other illicit drugs (question 7b)
For each person with contact from 1 to 7 and other illicit drug use frequency from 0 to 7, compute the product of the contact and drug use frequency (if the other illicit drug use frequency is 8, then this product is not computed). Sum these products to give VAR13. Divide VAR13 by the number of people whose products were actually computed to give VAR14. Divide VAR14 by 49 (7 × 7) to give VAR15. Multiply VAR15 by the number of people with any other illicit drug use frequency (even if this is equal to 8) and convert to a z-score to get C.1.F.
C.1.G. Drinking status of network members
To compute this index, a revised drinking status code is created (from question 6c).
| Old | Status | New |
|---|---|---|
| 5 | Heavy drinker | 3 |
| 4 | Moderate drinker | 2 |
| 3 | Light drinker | 1 |
| 2 | Abstainer | 0 |
| 1 | Recovering alcoholic | 0 |
| 8 | Don’t know | 8 |
For each network member, the new drinking status code is multiplied by the amount of contact (range 1–7). If the drinking status is 8, then the product is not computed for that person. These products are then summed across the network members and this sum is divided by the number of people who products were actually computed for. This is called VAR16. VAR17 is the number of people in the network with a drinking status (even if this is equal to 8).
Then convert to a z-score based on the mean and SD of the sample at baseline.
C.1.H. Frequency with which network members drink (question 7c)
For each person with contact from 1 to 7 and a drinking frequency from 0 to 7, compute the product of the contact and drinking frequency (if the drinking frequency is 8, then this product is not computed). Sum these products to give VAR18. Divide VAR18 by the number of people whose products were actually computed to give VAR19. Divide VAR19 by 49 (7 × 7) to give VAR20. Multiply VAR20 by the number of people with any drinking frequency (even if this is equal to 8) and convert to a z-score to get C.1.H.
To calculate component 1v2, sum the six z-scores C.1.C–C.1.H and then convert to a z-score.
Component 2: General/treatment support
For components 2 and 3 an equivalent to the four most important people listed needs to be determined. When there are four or fewer people listed on the IPDA form, this is very simple: it is just those people listed, whether this is one, two, three or four people. When there are five or more people listed, then the four or more most important people are identified using the ratings from question 4. For example, if five people are listed with ‘importance’ ratings of 6, 5, 4, 3 and 2 then the top four people would be used. If the ratings are 6, 5, 4, 2 and 2 then the top five people would be used. In rare instances 12 people would be used (the lowest eight ratings are identical). This subset of people named on the IPDA form will be referred to as the ‘most important people’.
C.2.A. The most general support among the most important people
The maximum rating across the most important people on question 5. This is converted to a z-score.
C.2.B. The least general support among the most important people
The minimum rating across the most important people on question 5. This is converted to a z-score.
C.2.C. The average general support among the most important people
Create a new variable for question 5 (general support).
| Old | Status | New |
|---|---|---|
| 6 | Extremely | 4 |
| 5 | Very | 3 |
| 4 | Supportive | 2 |
| 3 | Somewhat | 1 |
| 2 | Not very | 0 |
| 1 | Not at all | 0 |
Create a new variable for question 4 (importance)
| Old | Status | New |
|---|---|---|
| 6 | Extremely | 5 |
| 5 | Very | 4 |
| 4 | Important | 3 |
| 3 | Somewhat | 2 |
| 2 | Not very | 1 |
| 1 | Not at all | 0 |
Now, for each person identified as being among the most important people compute the products after conducting the recodes detailed above. Average these products and then convert to a z-score.
C.2.D. The most support for treatment among the most important people
The maximum rating across the most important people on question 9. This is converted to a z-score.
C.2.E. The least support for treatment among the most important people
The minimum rating across the most important people on question 9. This is converted to a z-score.
C.2.F. The average support for treatment among the most important people
Create a new variable for question 9 (support for treatment)
| Old | Status | New |
|---|---|---|
| 6 | Strongly supports | 2 |
| 5 | Supports | 1 |
| 4 | Neutral | 0 |
| 3 | Mixed | 0 |
| 2 | Opposes | 0 |
| 1 | Strongly opposes | 0 |
| 8 | Doesn’t know | 8 |
Now, for each person among the most important people with valid values for this variable, multiply this new variable with the recode for question 4 from C.2.C. If a person has a value of 8 for question 8, do not multiply his/her ratings together. Take the average of these products (divide the total by the number of valid products) to give VAR21. Convert to a z-score to give C.2.F.
To calculate component 2, sum the six z-scores C.2.A–C.2.F and then convert to a z-score.
Component 3: Network support for substance use
C.3.A. Most support for drinking or drug use among the most important people (question 8)
The maximum rating across the most important people on question 8 (values of 8 do not count). This is converted to a z-score.
C.3.B. Average support for drinking or drug use among the most important people (question 8)
Create a new variable for reacted to drinking or drug use (question 8)
| Old | Status | New |
|---|---|---|
| 5 | Encouraged | 2 |
| 4 | Accepted | 1 |
| 3 | Neutral | 0 |
| 2 | Didn’t accept | 0 |
| 1 | Left, made you leave | 0 |
| 8 | Don’t know | 8 |
Now, for each person among the most important people with valid values for this variable, multiply this new variable with the recode for question 4 from C.2.C. If a person has a value of 8 for question 8, do not multiply his/her ratings together. Take the average of these products (divide the total by the number of valid products) to give VAR22. Convert to a z-score to give C.3.B.
To calculate component 3, sum the two z-scores C.3.A and C.3.B. and then convert to a z-score.
Appendix 11 Q–Q plot of the standardised residuals and scatterplot for the primary effectiveness model
FIGURE 19.
(a) Q–Q plot of the standardised residuals and (b) scatterplot of fitted values against the standardised residuals to check the assumptions for the primary effectiveness model.
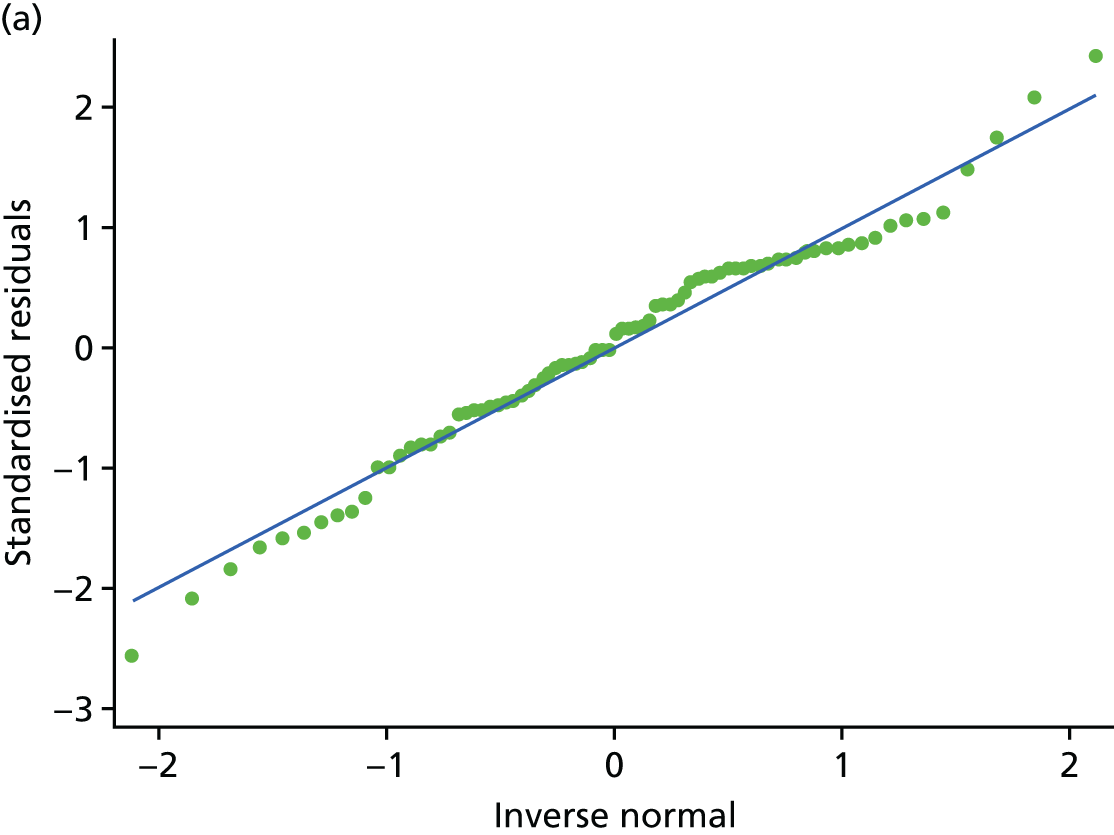

Appendix 12 Bandings for scale scores for the Strengths and Difficulties Questionnaire by treatment group and time point
| SDQ subscale | Y-SBNT (N = 26), n (%) | TAU (N = 27), n (%) | Total (N = 53), n (%) |
|---|---|---|---|
| Emotional symptoms scale | |||
| Baseline | |||
| Normal | 21 (84.0) | 19 (73.1) | 40 (78.43) |
| Borderline | 2 (8.0) | 5 (19.2) | 7 (13.7) |
| Abnormal | 2 (8.0) | 2 (7.7) | 4 (7.8) |
| Month 3 | |||
| Normal | 19 (82.6) | 14 (77.8) | 33 (80.5) |
| Borderline | 3 (13.0) | 0 (0.0) | 3 (7.3) |
| Abnormal | 1 (4.3) | 4 (22.2) | 5 (12.2) |
| Month 12 | |||
| Normal | 15 (75.0) | 16 (84.2) | 31 (79.5) |
| Borderline | 2 (10.0) | 2 (10.5) | 4 (10.3) |
| Abnormal | 3 (15.0) | 1 (5.3) | 4 (10.3) |
| Conduct problems scale | |||
| Baseline | |||
| Normal | 14 (56.0) | 10 (38.5) | 24 (47.1) |
| Borderline | 3 (12.0) | 5 (19.2) | 8 (15.7) |
| Abnormal | 8 (32.0) | 11 (42.3) | 19 (37.3) |
| Month 3 | |||
| Normal | 10 (43.5) | 12 (66.7) | 22 (53.7) |
| Borderline | 6 (26.1) | 2 (11.1) | 8 (19.5) |
| Abnormal | 7 (30.4) | 4 (22.2) | 11 (26.8) |
| Month 12 | |||
| Normal | 13 (65.0) | 14 (73.7) | 27 (69.2) |
| Borderline | 1 (5.0) | 1 (5.3) | 2 (5.1) |
| Abnormal | 6 (30.0) | 4 (21.1) | 10 (25.6) |
| Hyperactivity scale | |||
| Baseline | |||
| Normal | 13 (52.0) | 9 (34.6) | 22 (43.1) |
| Borderline | 3 (12.0) | 1 (3.8) | 4 (7.8) |
| Abnormal | 9 (36.0) | 16 (61.5) | 25 (49.0) |
| Month 3 | |||
| Normal | 12 (52.2) | 7 (38.9) | 19 (46.3) |
| Borderline | 6 (26.1) | 4 (22.2) | 10 (24.4) |
| Abnormal | 5 (21.7) | 7 (38.9) | 12 (29.3) |
| Month 12 | |||
| Normal | 12 (60.0) | 8 (42.1) | 20 (51.3) |
| Borderline | 2 (10.0) | 6 (31.6) | 8 (20.5) |
| Abnormal | 6 (30.0) | 5 (26.3) | 11 (28.2) |
| Peer problems scale | |||
| Baseline | |||
| Normal | 18 (72.0) | 14 (53.8) | 32 (62.8) |
| Borderline | 7 (28.0) | 10 (38.5) | 17 (33.3) |
| Abnormal | 0 (0.0) | 2 (7.7) | 2 (3.9) |
| Month 3 | |||
| Normal | 18 (78.3) | 12 (66.7) | 30 (73.2) |
| Borderline | 3 (13.0) | 5 (27.8) | 8 (19.5) |
| Abnormal | 2 (8.7) | 1 (5.6) | 3 (7.3) |
| Month 12 | |||
| Normal | 13 (65.0) | 11 (57.9) | 24 (61.5) |
| Borderline | 7 (35.0) | 7 (36.8) | 14 (35.9) |
| Abnormal | 0 (0.0) | 1 (5.3) | 1 (2.6) |
| Prosocial scale | |||
| Baseline | |||
| Normal | 20 (80.0) | 18 (69.2) | 38 (74.5) |
| Borderline | 3 (12.0) | 3 (11.5) | 6 (11.8) |
| Abnormal | 2 (8.0) | 5 (19.2) | 7 (13.7) |
| Month 3 | |||
| Normal | 19 (82.6) | 12 (66.7) | 31 (75.6) |
| Borderline | 3 (13.0) | 2 (11.1) | 5 (12.2) |
| Abnormal | 1 (4.3) | 4 (22.2) | 5 (12.2) |
| Month 12 | |||
| Normal | 17 (85.0) | 13 (68.4) | 30 (76.9) |
| Borderline | 1 (5.0) | 3 (15.8) | 4 (10.3) |
| Abnormal | 2 (10.0) | 3 (15.8) | 5 (12.8) |
| Total SDQ score | |||
| Baseline | |||
| Normal | 14 (56.0) | 8 (30.8) | 22 (43.1) |
| Borderline | 5 (20.0) | 4 (15.4) | 9 (17.7) |
| Abnormal | 6 (24.0) | 14 (53.8) | 20 (39.2) |
| Month 3 | |||
| Normal | 12 (52.2) | 7 (38.9) | 19 (46.3) |
| Borderline | 5 (21.7) | 6 (33.3) | 11 (26.8) |
| Abnormal | 6 (26.1) | 5 (27.8) | 11 (26.8) |
| Month 12 | |||
| Normal | 10 (50.0) | 10 (52.6) | 20 (51.3) |
| Borderline | 5 (25.0) | 6 (31.6) | 11 (28.2) |
| Abnormal | 5 (25.0) | 3 (15.8) | 8 (20.5) |
Appendix 13 Family Environment Scale individual items charts
FIGURE 20.
Items from the FES conflict scale, for which 1 point is added for a false response: (a) FES item 1; (b) FES item 2; (c) FES item 3; (d) FES item 4; and (e) FES item 5.


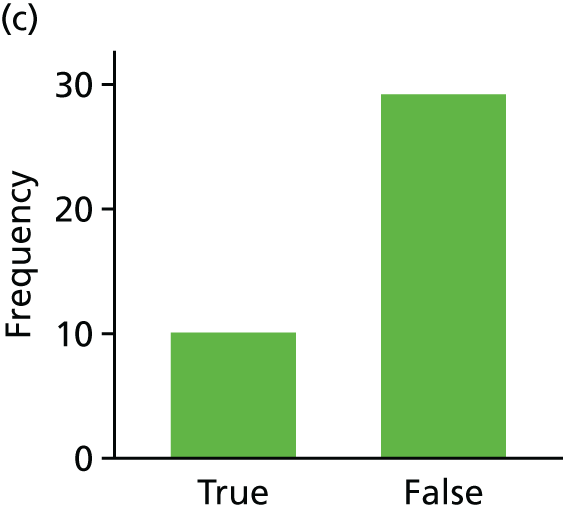
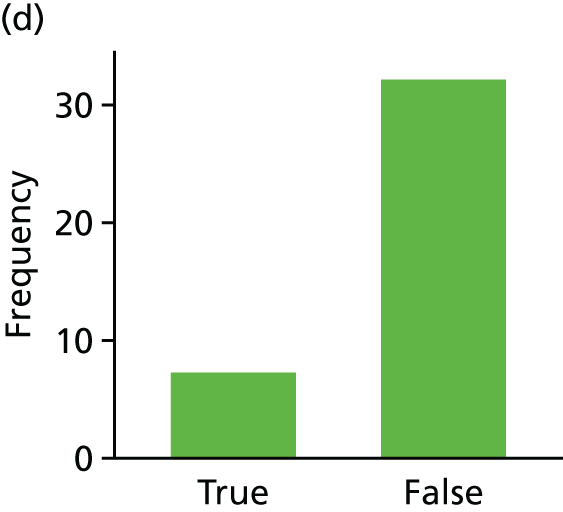

FIGURE 21.
Items from the FES conflict scale, for which 1 point is added for a true response: (a) FES item 6; (b) FES item 7; (c) FES item 8; and (d) FES item 9.


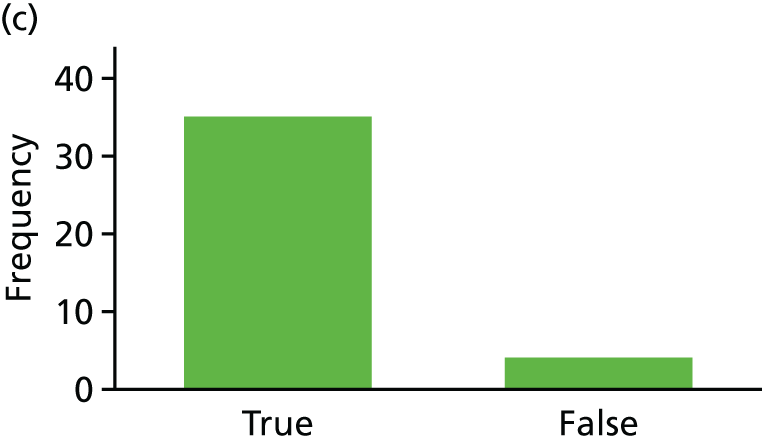

FIGURE 22.
Items from the FES cohesion scale, for which 1 point is added for a true response: (a) FES item 10; (b) FES item 11; (c) FES item 12; (d) FES item 13; (e) FES item 14; and (f) FES item 15.

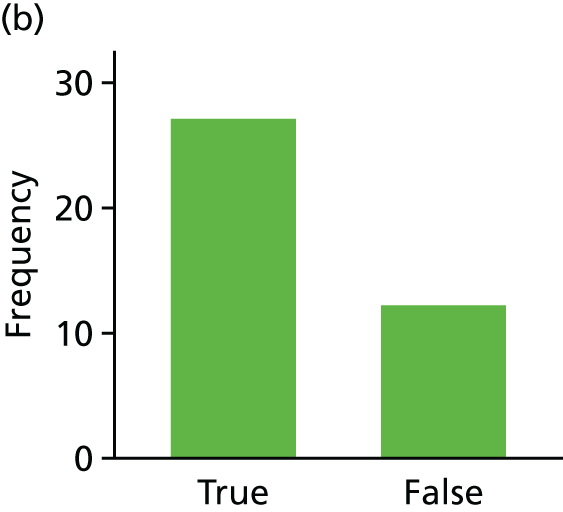



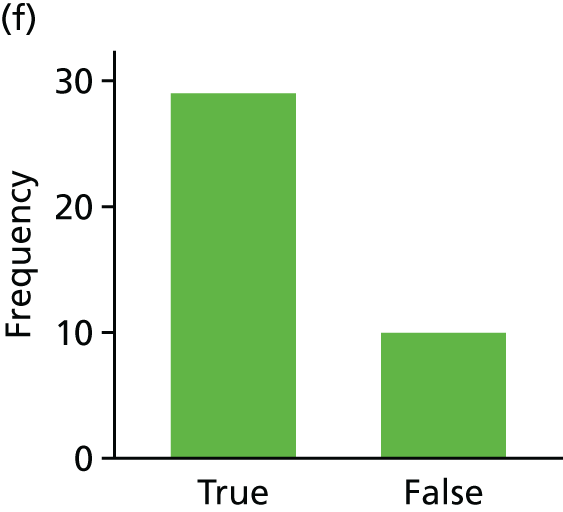
FIGURE 23.
Items from the FES cohesion scale, for which 1 point is added for a false response: (a) FES item 16; (b) FES item 17; and (c) FES item 18.

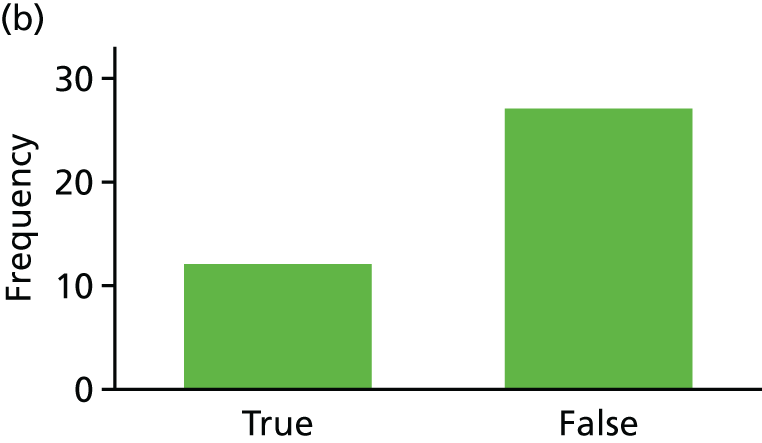

FIGURE 24.
Items from the FES expressiveness scale, for which 1 point is added for a true response: (a) FES item 19; (b) FES item 20; (c) FES item 21; (d) FES item 22; and (e) FES item 23.
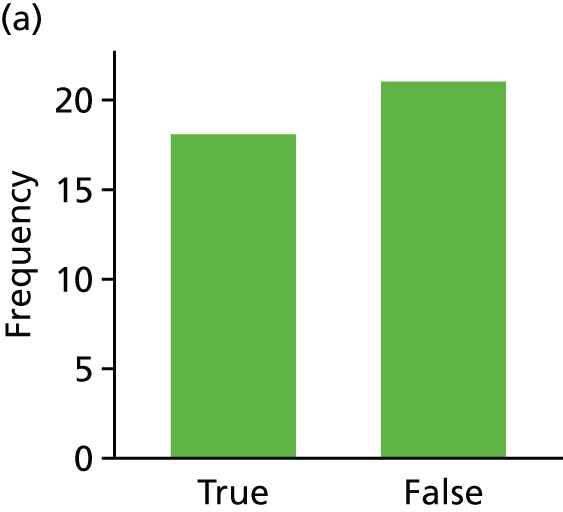



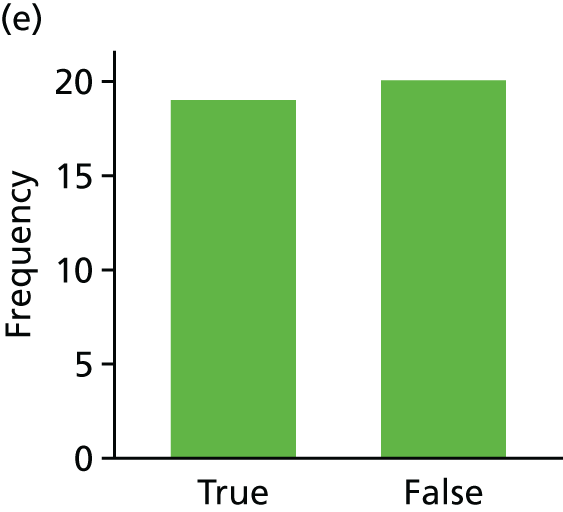
FIGURE 25.
Items from the FES expressiveness scale, for which 1 point is added for a false response: (a) FES item 24; (b) FES item 25; (c) FES item 26; and (d) FES item 27.
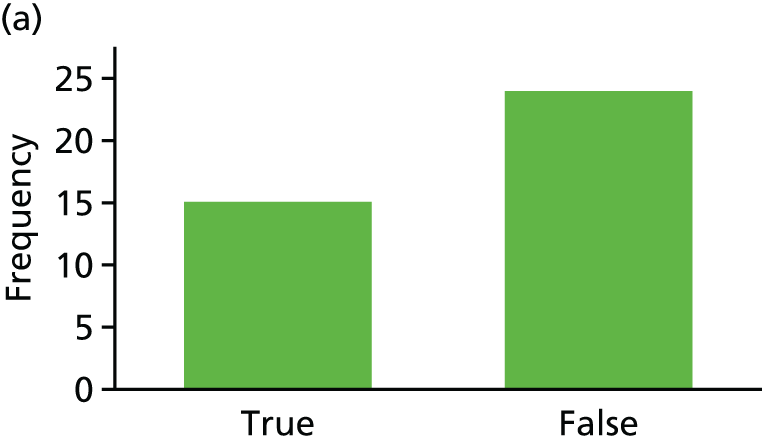



Appendix 14 Twelve-month follow-up social services involvement question
Have you had any involvement with social services? If ‘yes’, please explain (open question).
| Social services use | Y-SBNT | TAU | ||
|---|---|---|---|---|
| Baseline (n = 26) | 12 months (n = 20) | Baseline (n = 27) | 12 months (n = 19) | |
| None | 12 | 15 | 13 | 9 |
| Children in need – abuse/neglect | 3 | 0 | 1 | 0 |
| Children in need – family in acute stress | 1 | 0 | 0 | 1 |
| Local authority foster care | 2 | 3 | 4 | 2 |
| Social worker (children’s services) | 2 | 0 | 3 | 2 |
| Children looked after | 0 | 0 | 1 | 0 |
| Children in need – socially unacceptable behaviour | 0 | 0 | 1 | 2 |
| Key worker services for disabled children | 1 | 0 | 0 | 0 |
| Voluntary and private sector care homes | 0 | 0 | 1 | 0 |
| Children in need – parental illness or disability | 1 | 1 | 0 | 1 |
| Children in need – absent parenting | 1 | 0 | 0 | 0 |
| Drug services (children and adolescents) | 0 | 0 | 0 | 1 |
Appendix 15 Identified changes required to health service questionnaire
To investigate the feasibility of a full economic evaluation a health service questionnaire was used. This included a comprehensive list of services but the analysis of the data raised problems with regard to the structure of the questionnaire:
-
The ‘not answered’ option for some questions, if kept in a full trial, might have to be considered missing. Therefore, it would be worthwhile to emphasise in the training for the research team that the interviewers, when conducting the follow-up survey, should encourage participants to answer as much as they can.
-
Within the health service section, the question on NHS Direct is now out of date as NHS Direct was discontinued in March 2014 (before trial randomisation). This question could be substituted with one referring to calling NHS 111, which has subsequently replaced NHS Direct.
-
The open question on involvement with social services did not specify in the last 12 months and could not be costed. The answers could, however, be categorised to highlight the breadth of social services available, with the categories of children in need and foster care the most frequently reported. Vague answers such as ‘when I was little’, ‘too young to remember’, ‘safety issues’, etc., could not be categorised reasonably and therefore were not included (see Appendix 14 for the full list of categories). An additional question specific to whether or not the participant was taken into care would be useful to distinguish between contact with social services and taken into care by social services. As the latter is much more costly than the former, the social service cost in our analysis could be hugely underestimated. Lastly, the term ‘involvement’ caused confusion over whether this referred only to personal contact or included other family members as well. For example, if the young person is a teenage mother who has her child taken into care this should count as her social service usage. However, if a sibling of the young person is taken into care this should not count as the participant’s usage. This distinction of what involvement includes needs to be made clearer in the questionnaire.
-
Within the crime section of the questionnaire, the question referring to criminal acts requires the participant to move on if they answer ‘yes’ to criminal damage. Consequently, the remaining parts of the question may be missed. This redirection is unnecessary as all participants must answer the next question anyway, regardless of how they answered the previous question. A summary question at the beginning would help to avoid unnecessary inference as to what is missing and what is unanswered because it is not applicable. The missing data within this section suggest a problem with participants’ ability to recall how many times they answered bail or had contact with the probation officer. It further suggests that the answers were left blank if, for example, they did not appear at Crown Court. The use of ‘appeared’ could be misleading to participants as some evidence suggests that they appeared in court but not as the defendant. Missing and implausible answers could be reduced by more frequent follow-up, resulting in better estimates.
Appendix 16 Young people’s illustrative quotations
Young people’s lives before treatment
Well I’m not happy about getting kicked out of school, I wished I would have stayed now.
Young person 1013; female, 14 years, alcohol
Entry to treatment
No, I just knew that I had a problem that needed to be dealt with.
So it was you that asked for the referral?
Yeah, I went into the YOT when I went to collect my money and I had a word with someone there and I said that I think I’ve got a problem.
Young person 1020, female, 17 years, mephedrone
No, it wasn’t a problem for me, but it was a problem for my family.
Young person 1032, female, 14 years, mephedrone
They [mum] were really worried ‘cause the way I was dramatically losing weight; the way I looked – I didn’t look well at all – I didn’t . . . what my mam’s saying about being dead and worried about it and everything. My mam doesn’t come across that way. If she’s upset she’ll look like she’s angry rather than . . . and I never seen her fully upset. And I did.
Young person 1020, female, 17 years, mephedrone
Involving family/social network
Yeah it was useful because you sit back and you analyse the people around you like. It makes you think about all the people around you . . . It makes you actually sit there and think about what I was getting involved in . . . it’s just a wake-up call really.
Young person 1028, male, 17 years, cannabis
I just didn’t really want to invite anyone . . . I just didn’t really think there was any need for her [my mum] to be there . . . I’d rather do it just me.
Young person 1041, male, 15 years, cannabis
If they’re like me, then I’d probably suggest talking about it first for a little while, then towards the end, doing it.
Young person 1020, female, 17 years, mephedrone
OK, things that you wouldn’t normally think about he [teacher] notices it . . .
Yeah.
Young person 1002, male, 15 years, cannabis
In what way did your sister support you, apart from attending that one session? What else did she do for you?
Whenever no-one was at home I used to go to hers.
So you’ve spent time with her instead of . . .
Spending time with them [friends who smoke cannabis].
Young person 1001, male, 16 years, cannabis
Treatment goals
Thinking about your goal, do you remember what goals you set?
Aye, it was cutting down and that, which I have.
Young person 1021, male, 15 years, cannabis
Treatment outcomes
And was there any particular reason at all why [therapist] wasn’t able to successfully help you reduce it [cannabis use]?
Not enough time.
Young person 1019, male, 17 years, cannabis
I’ve had dreams of taking it; how bad it is. But I know for a fact I don’t want my life to be like that. I don’t; but it’s hard to keep away from it. When you smell it; when [boyfriends] got that thing in his mouth and you smell it and you still want it. I mean I wanted to stop it. But you still have that urge because of how happy it makes you; how . . . the smell even just makes you . . . basically it makes you go insane. It’s not very nice.
Young person 1020, female, 17 years, mephedrone
Like I said earlier, I would happily cut down on my cannabis, but as long as I can have it when I’m annoyed or if I’m on a weekend and I should be free to have it, as long as I’m in control of it. I just like it. I’m just one of these . . . I’m a very impatient person, so if I’ve got tabs [cigarettes] or . . . if I’ve got something, I want to make it last, the Thursday just gone I ended up buying 40 tabs and they only lasted us 2 days.
Young person 1031, male, 17 years, NPS
Before you started seeing [therapist] how much were you smoking then?
10 or 20 a week.
10 or 20 a week, that’s quite a lot because now you’re only smoking?
One joint a week.
Young person 1000, male, 17 years, cannabis
It was positive. It gave me a different way to look at things; how I was drinking and all that. It changed how I drink because as I learnt from [therapist] it’s better to drink occasionally rather than piling it all up in one massive.
Young person 1008, male, 18 years, alcohol
It’s better because I know for a fact I’m not going to wake up every day and wonder where I’m going to get my next bag. So that’s definitely better.
Young person 1020, female, 17 years, mephedrone
Yeah, it was good, just like made us think more about what I was doing and that and I realised that I needed to sort it out . . . talking about it and that really.
Young person 1041, male, 15 years, cannabis
He [therapist] helped me with everything, even budgeting. Helped me to save my money, like learn how not to spend it as fast as I used to.
Young person 1014, male, 17 years, cannabis
I feel better, better in myself. I don’t get angry that much now. Just like I want to do more stuff that I couldn’t do before because it used to just tire me out easier.
Young person 1021, male, 15 years, cannabis
I’ll like play a game or I can read a book and I like watching TV and chilling out. I just feel happier and good in myself.
Young person 1033, female, 12 years, solvents
I don’t want to talk someone because I don’t want to be opening up to them and telling them my problems again and going over it. What’s the point like? He [therapist] hasn’t helped me. I’m still at the same stage when he opened up my case.
What do you think happened then? Why . . .?
It was too short. You can’t help someone in like a couple of months of walking in there.
Young person 1019, male, 17 years, cannabis
Did taking part in treatment meet your expectations?
In everything except one.
Oh, what was that one?
The sleep one.
The sleep. You’re still having problems with your sleep?
Yeah.
Young person 1001, male, 16 years, cannabis
Treatment experience
Would you say things got better, improved or did it get worse?
The cannabis, yeah, kind of. I wouldn’t say made a major effect but he still helped me.
He helped you, in what way?
Yeah, just the information it was giving me.
What sort of information was this? Was this related to your cannabis or how to relate to your family?
Both.
Young person 1000, male, 17 years, cannabis
It’s the way she [therapist] makes me understand everything like; I’ve still got to understand myself and [therapist] just pushes me to try to understand a little bit more. And the fact that I don’t think it helps as well how confused I am about it; about myself and how I feel and what I’m like and all the personality and all that. It makes it easier as well and she’ll help me through it. Also help me through the times like the [boyfriend] situation. I don’t like talking about my feelings and the way [therapist] puts it, it makes it easier to talk about it . . . Yeah. Even if I didn’t attend them [sessions] I’d come the next day and she’d be there.
Young person 1020, female, 17 years, mephedrone
It’s when someone is talking to you about it. It just makes you actually sit there and think about what I was getting involved in, what I was getting myself into. It’s just a wake-up call really. I got a lot more help from the YOT than what I do now with adult probation. There was more support and meetings every week.
Young person 1028, male, 18 years, cannabis
I liked the fact that we could talk on a level, you know, I didn’t have to worry about saying anything. I could just blurt it out basically and tell him anything that I was worrying about or that I wanted to do and he’d help me with it. I don’t think he did anything wrong to be fair. Every week was like positive and good.
Young person 1014, male, 17 years, cannabis
It was good because it wasn’t, with [therapist] it wasn’t always talking about the drugs as well. We were talking about my life and in general, sort of, thing, so it was like a mixture. It was like as if it was a counsellor, because I’ve had one before, as if she was a counsellor along with her actual job, like your drugs worker . . . They understand your circumstances and that. There are some people that pretend where they know where you are coming from and I’m just, like, you are just lying really. Then you know when someone actually knows where you are coming from because they respond in a way I know that they understand me.
Young person 1032, female, 14 years, mephedrone
How did you find the experience of working with [therapist]?
Quite annoying. It’s like . . . well, put it this way, with me going a month every day with cannabis and then just all of a sudden stopping and having it once in a month, I think I don’t need any help at all, I just think I can just do it on my own. I think I could stop if I wanted to any time.
Young person 1031, male, 17 years, NPS
Yeah I just didn’t like the sessions at all.
You didn’t like the sessions?
No.
You didn’t like what you talked about or what is it about it?
I think it’s just mainly the name, youth offending team. I don’t really offend any more.
Young person 1047, male, 17 years, cannabis
Treatment suggestions
How many sessions do you think there should be?
They are shouldn’t be more than six.
Young person 1043, male, 15 years, cannabis
How many sessions do you think were appropriate?
I would say about three.
Young person 1047, male, 17 years, cannabis
I thought six was enough but some people might think different maybe.
Right, do you think they would want more?
I don’t know, it depends how like bad they are on it or whatever.
Young person 1041, male, 15 years, cannabis
How many sessions do you think should be offered?
Two more.
Young person 1001, male, 16 years, cannabis
Probably once a week roughly.
Once a week? Over how long?
Over the 3-month period.
Young person 1008, male, 18 years, alcohol
Well longer than he [therapist] does because he only does them for like 20 minutes.
How many sessions do you think?
12.
For how long?
An hour.
Young person 1019, male, 17 years, cannabis
At least 12 sessions over about 6 months.
Young person 1020, female, 17 years, mephedrone
Every week, for as long as you need?
Yeah, basically until you . . . until you want to stop.
Young person 1000, male, 17 years, cannabis
I’d rather just get scared from it, do you know what I mean. I’d rather have a spliff and fit off it or something like that to make me wake up and go, I’m not touching that again, do you know what I mean, something that will scare me from it . . . Make it more like activity wise, if you know what I mean. I think if people had more activity, something to occupy their mind, then they might see it a bit different thinking these people took us out to go and do this, we could do that and we’re going to stop smoking this, do you know what I mean?
Young person 1028, male, 17 years, cannabis
Research process
How did you find filling in the questionnaire with me in the past, today actually? Did you find it OK, was it too long?
It was all right. It was cool.
Young person 1000, male, 17 years, cannabis
Even the paperwork, did you find the questions relevant, those types of questions we asked?
Aye. If it were where you were like, oh, write this, it would have been totally different, probably would have got ripped up, but if it’s something where it’s tick or draw, it’s fine.
Young person 1031, male, 17 years, NPS
Aye, I didn’t really mind it. The questions all made like sense, to be honest.
Young person 1041, male, 15 years, cannabis
How did you find the questionnaires that we did 3 months ago and today?
It changed quite a lot. The people that are around have changed. You don’t expect, oh I’ve been doing this much now, this much now, and so on. It actually makes you think about how much the intake actually is.
Young person 1008, male, 18 years, alcohol
How do you find filling out the questionnaires that we did?
The tick boxes?
The tick boxes and the questions that I was asking.
Yes, that was interesting, that was, like, interesting to know that someone actually considering their life, their personal life, if you know what I mean. They were all relevant, yes.
Young person 1032, female, 14 years, mephedrone
Did you find any of the questions relevant?
Yeah, but boring.
How do you suggest that we could do it differently?
Put SpongeBob in it. I love creative stuff. Yeah, make it a bit more fun.
Young person 1020, female, 17 years, mephedrone
I’m not sure. I don’t know because I reckon I could finish the rest off on my own but at the same time . . . I don’t know. Probably, yeah.
Young person 1000, male, 17 years, cannabis
Appendix 17 Network members’ illustrative quotations
That’s been very clear and I think that’s been translated to [young person] what those goals are as well. She’s not been left in any doubt as to what the whole idea behind us all working with her was for, so it’s been positive. I think especially for somebody like in [young person’s] case where family is a little bit disjointed in terms of [young person] knowing who she can go to have support with and who she can go and speak to. I think from her point of view just seeing that all the different professionals have been talking to one another and working with one another I could imagine us being quite a comfort for her at that particular point.
Network member 1033, teacher
Conversations that I’ve had with [young person] would be generally about, do you feel like you’re going in the right direction, do you feel like you’re on top of things? I didn’t know specifically what [therapist’s] activities were with [young person] from session to session. I kind of just knew that the overall aim was for [young person] to be aware of her substance abuse and what it could lead to and what the dangers were with it.
Network member 1033, teacher
In terms of having that kind of relationship with [therapist] certainly in terms of all the support she’s received for [young person] herself I can see a big impact on her just even around school. She seems a lot calmer, just a lot more settled really you know. Obviously through it all as well our relationship with dad’s been strengthened I think. You know the fact that he’s seen that it’s from all of us, you know, multi-agency approach you know we are all having that support there for [young person], it’s definitely helped.
Network member 1033, teacher
I think that in terms of her feeling a lot more supported I think she’s definitely felt that. I think she’s just had that opportunity to talk through her feelings and the chance to actually address her concerns, I think that that’s been very positive.
Network member 1033, teacher
He wouldn’t have gone [to the agency].
Network member 1021, mother
While we do have people within the school [our parent support officer] that would go out and visit the home, there had been a little bit of difficulty getting into the home. So any more information like that from [therapist] really helped build up our picture and our understanding of what was going on and what the needs were for [young person] at that particular time.
Network member 1033, teacher
Appendix 18 Therapists’ illustrative quotations
Training and supervision for treatment delivery
I think the training was good in terms of just getting us used to what the materials were going to be. At the time we discussed how it would have been really helpful to have worked through those tools with examples with actual cases and that would have been helpful to relate it to the young person because some of the worksheets were quite similar to things that we were already using in usual treatment but I guess it was just getting our heads round how that was going to be applied and how that was going to be kept to just the six sessions.
North East therapist
I think the other thing we were saying was about maybe just a bit more clarity about sort of crisis sessions and what they should look like. In future training should have examples of what’s the best way to go about that without it impacting on what we’re supposed to be doing.
North East therapist:
When we highlighted certain things that maybe weren’t in the sort of materials that we were provided on the training, like that was taken on board and we were sent further ones. We asked for some more materials on communication skills and that was sorted straight away and that was helpful.
North East therapist
Yeah we had joint supervision, I think at one point [therapist] was a bit ahead of me with one of her young people and so hearing how her sessions had gone and maybe what she’d do differently, then I could bear that in mind for mine and it was just good to share those sorts of things and how effective they’d been.
North East therapist
I think supervision is important. Now whether that happens as in you get peer supervision first off together and then it goes into a big community peer supervision with the likes of how [trainer] did it, I guess consultation sort of role, in the sense that we all talked about our cases but we all helped each other as well and see the way of working because that has so many benefits. Like we could see how the other group [West Midlands] were working, we could see how we were doing it differently and that kind of spurred us on a little bit in a way and I think it needs to be at least once a year where everyone gets together to talk about it because I see the benefit.
North East therapist
We were talking to [trainer] regularly which was really useful and we could always e-mail him and so I liked the idea of that as well but maybe having a central person who would oversee that sort of side of it.
North East therapist
I mean me and [therapist] actually worked through the way each of the sessions needed to be in order for the young person and once we got into the flow of it, it worked really well and we were able to kind of constantly feed back and reflect on our own practices and how we could improve it. We wanted it to be the best it could be for those young people.
North East therapist
So aside from the supervision that we got from [trainer], I think actually having a case to discuss and talk through about what worked and what didn’t, I think that’s really important to do because I think without that, you could get quite lost in what you’re trying to do.
North East therapist
When you’re doing the training that should be highlighted that reflective practice is an essential part of it because it firms it up, it makes it more concrete as a model for the people that are delivering it and it brings the value to it for us.
North East therapist
Treatment approach
So it still isn’t quite as structured [TAU] but what I liked about Y-SBNT, although there may be some leeway about how many sessions that may take to move through some of these different stages, it’s logical, it’s flexible enough but it is quite an ergonomic sort of approach.
West Midlands therapist
I think it’s a really clear structured principle of a treatment journey. There is a good clear structure for the practitioner, it’s not rigid, there are stages but there is some flexibility in that and I like it because it starts off with a visual representation of what’s going on in that young person’s life, who was involved in their network and quite quickly drawing out who may be supports for change and understanding what the young person is getting from different people within their social network. So it leads on quite nicely to be able to look at goals and to be quite practical goal focused.
West Midlands therapist
In promoting substance use change, so we can start off with a picture of understanding who is in that network and who is facilitating unhelpful behaviours who may be kind of easier social connection to recruit into a team around that young person. So I think that it is a useful model for promoting change in that the young person doesn’t always need to be there for that team to work.
West Midlands therapist
The model itself is good and sharp. I feel that the structure actually could be used with any situation. So for a lot of the young people no matter what they presented with, the actual worksheet fitted that situation and it meant that, I guess, we all got good outcomes from it.
North East therapist
It was a very clear set-up so you knew what the structure was. You knew where you were going with it. You knew what was going to be happening next. I think because we were clear about it, the young people were clear about it. We all knew what was going to be happening and it kept everything sort of contained in a way, so you felt like you had actually achieved something by the end of the session even just on a one-off session.
North East therapist
Experience of delivering treatment
I really enjoyed it. I found it a learning curve for me and how I could incorporate a different process of working with young people, so the network maps and the care plan settings that we did.
West Midlands therapist
I got a lot out of it and I felt that it was very structured and that kind of helped the process of me understanding and developing the skills and tools around the actual model, so I found it really useful.
North East therapist
I think the more that we used the tools and things like that and we could see the benefit of doing it even if the young person did quite make it for the six sessions, you could even see like progress that was made even in the ones that you did do and then obviously we did a lot of reflective practice afterwards and learnt from each other’s cases as well, so that helped us feel more confident in what we were doing.
North East therapist
We were under one organisation [agency] and then during the process my role changed, so I think my experience of it was set within a context of lots of change. So my experience of delivering the intervention, I really liked it. It made sense to me, I think it’s a really useful way to explore with young people and their families and their wider network change. I have felt throughout and reflecting on it since I don’t feel like I’ve put enough into it to make it work and it sits really uncomfortably with me that if I had been more flexible in being able to go out and see the young people much more at home. I think I could have just done more, so that the intervention would have worked better for those young people.
West Midlands therapist
It’s different because of the recording, the forms you have to complete and it’s structured. I suppose it was just because it was structured, getting the sessions in was a bit difficult but I got round that by blocking them all in straight after the first meeting really. I got them to put it on their phone but not everyone is consistent as others, especially young people forget. So it’s all about trying to get people to remind them.
West Midlands therapist
It was quite challenging to make sure that all the steps were followed. Getting the forms filled out and seeing the young person because sometimes doing it with five or six young people and then they don’t show and then it got a bit tricky and confusing in that aspect but apart from that I generally knew what I was doing with the young people.
West Midlands therapist
Treatment engagement
There was a lot of stop start before we even got to do the model. Like some of them would have been seen quite a few times by different people. That was all different and I think that’s where I got a little bit, oh I hope I can achieve what I need to achieve with this young person because already we were different in the way we were working before. But I’ve got to be honest in that sense for all my young people it didn’t have an impact on the work. I don’t think that really was that apparent for the young person, it was more our concerns and worries about it as opposed to it being something that they told us.
North East therapist
I think it would still be nice to have a little bit of time at the beginning to at least build on a little bit of a relationship because it still felt a little bit disjointed because you’re sort of straight in there, whereas it would be good to try and get to know that young person a bit more first, but again I don’t know this is maybe coming from my side of things.
North East therapist
Some of the young people they engaged very well and then one or two was just – it wasn’t the best time for them I’m guessing it was quite difficult in that sense but generally the young people that I had managed to complete their six sessions, there was just one or two that it was a bit difficult to complete and track them down.
West Midlands therapist
I didn’t get to the end of an intervention with any of those young people but I think that is much more about the context of me as a practitioner and it doesn’t sit comfortably with me to say it, but I think that’s the honest reality but I do think that it is a really helpful process. At the time certainly around 50% of the young people that were in treatment were open to the youth offending service and a lot those were not actively seeking support. So although we could take perhaps a bit of a motivational sort of approach to support young people to want to come back and perhaps move from pre-contemplation to thinking about change then at that point it’s quite tricky to then engage them in wanting to have other people come in and that’s so different to adults because of course adults very often are coming to you at a point where they really want help.
West Midlands therapist
Involving family/social network
It was useful for the young person because they’re getting support from the social network and at the same time for the network members they’re getting to understand what the young person is going through.
West Midlands therapist
It’s really helpful if there were different people that would see that young person in different parts of their lives and have more continuity than you may have as a practitioner, that’s really helpful. So being part of a more co-ordinated plan involving the focal client principally I think that’s a more supportive thing for the concerned other.
West Midlands therapist
Obviously we can only support them to a certain extent whereas the network members are there a lot more of the time than we are, so having them involved means they’ve got that continued support, you know, out of sessions and things like that at times where they probably need it more than when they’re in the sessions with us. So I do think it’s a massive benefit.
North East therapist
It takes the pressure off the young person as well because making changes especially around substance misuse is massive isn’t it and it’s not something that, you know, you have to do on your own and so I think by using network members it does take that pressure off to go like, oh actually I can do this because I’ve got people that are backing me, that are behind me and supporting me and I think that means that they’re in a greater start of trying to make those changes because they’re not feeling it’s all on them to be doing such a massive big change.
North East therapist
I think one of the barriers was getting an appointment where three people could meet up because sometimes it’s difficult with just two people for diaries, say someone is working or if someone lives at the other end of the city and all that kind of thing to take into account.
West Midlands therapist
It’s difficult in that we had lots of referrals from the youth offending service, so there was issues there with having appointments, parents and other people who were not offenders coming in to appointments, so that’s a difficulty. Then some of the other referrals they were young people who had moved away from their networks so were staying with relatives in a new place. There were a number of factors I think that made it tricky to get people into the room.
West Midlands therapist
For the others I guess it was more difficult in terms of like the location of where I saw them, so another of my young people I saw in school which then was sort of going around the teacher’s timetable but also trying to get mum into school and things, it was just more sort of a practical view as opposed to him not wanting them in there, but he wanted to be seen in school.
North East therapist
So I did find that quite difficult to try and get him on board because he sort of said like from the beginning, well if I want to make changes, I’ll do it myself, I don’t need anybody else’s support and it was like ‘aargh’ even though we’d discussed the benefits and he’d go, yeah, yeah, yeah. But actually like that’s what he believed and that’s what he wanted to do. I think he got a bit stuck on the idea that all of his network were going to specifically help him with the substance misuse by talking about it all the time and all this kind of thing and I think once the penny dropped that it didn’t necessarily have to mention anything about his substance misuse, it was more support in a different way in terms of distraction techniques, or whatever it may be. Once that clicked you could just see that he was, oh OK I get it now. I think that’s when he realised how important it was to have that network around him to be able to help him out.
North East therapist
So it was very good then to speak to the parents directly and say, can you support your children by doing this for their development, so it was very useful in that aspect. There was one or two that were resistant but generally a lot of them when you mention their family it kind of made them open up a bit more. We were able then to get their mum or dad or cousin or whoever it was who was directly involved and they gave me permission to speak to them directly to encourage that they’d be part of the treatment.
West Midlands therapist
I mean some family members are really quite accommodating towards being part of the treatment but some young people didn’t want family members to be part of the sessions but we got around that by using say like staff members like the children’s home. I mean it was also clear to them as well how their substance use impacted them and how that social network member could get self-esteem in supporting them in their journey as well and it was more clear.
West Midlands therapist
It’s the young person who decides who’s in their social network and who’s going to be helpful to them and even if they do like live with mum or whoever, but if they don’t feel that that is someone who can be supportive for whatever reason or feels that there’s too much emphasis placed on to that network member, then you do have to go with what that young person wants to put on there because it’s not who we think should be supporting, it’s about what they want.
North East therapist
Treatment goals
Although network members didn’t necessarily come to the session, we sort of planned on how the young person could get support from the network in terms of what discussions and conversations they would have with them and explanation of where they were at, what their goals were, how that network member could support them with making progress with those goals and things and then that was obviously reviewed at the session after to see whether that discussion had taken place and things.
North East therapist
Well yeah because it involves people in their treatment to support them and to get through their issues and it enables the young person to know exactly what the plan is and what we’re going to be doing and if they get a bit stuck they can then go back to their parents and talk to that support network and that support network will be there to kind of just guide them and highlight things as a reminder really. So yeah it was very beneficial.
West Midlands therapist
I was fortunate in that sense because I think that most of my young people and network members were wanting to help, were wanting to be a part of it, were wanting to follow through with it and like the last one in one of them, she was just amazing. She had the plan all set up. I just like consolidated it by writing it up and she knew what she needed to do for him and that worked well and it kind of made me feel good because I was thinking, this is good. I love this model. But I do because sometimes walking away, you just think what is going to happen to this young person but this particular one I knew it was going to be OK because he had someone really looking out for him and I wouldn’t have known that if I hadn’t brought in the network member.
North East therapist
I recall one session where the father was there and he was to kind of able to understand where his daughter was coming from because of that situation and I felt that she was being helped once I left which was quite positive and productive for that whole family looking at the changes and trying to make those changes together. She [young person] ended up coming back in and it ended up being a really good session because they were, not arguing, but discussing it and we reflected on the fact that how they’ve approached this can help in other ways as well. I see the benefits in all of it because you can’t work in isolation. I don’t think it’s helpful to anybody to be fair.
North East therapist
Yeah I had another young person that had a network member attend one of the sessions and that worked really, really well. It was a positive session and it did actually flow quite nicely because we were just sort of all involved in what was going on and it was quite a positive feel to the session because the young person was quite eager to listen to what the network member [support worker] had to say and how that network member could support her and it was good.
North East therapist
By including network members, like everyone has got a clearer understanding about what the young person is wanting to achieve and work towards and maybe that is something that the young person might not have felt able to discuss with network members before that point but using sort of the Y-SBNT that gives them the confidence to be able to do that and the network members, although they may have different views and opinions about what that young person is doing, they’re agreeing to help them with that and work towards what it is that they’re wanting to do.
North East therapist
I really felt that the goal setting was really good and what it did because for me that sheet kind of emphasised a lot of the skills and resources for that young person, so it meant that I was able and they were able to kind of keep reflecting back on what they used and how they used it and what they did with that. In a way that was the most purposeful sheet I think because it was something that could be used in any situation not just substance use. It could be used for anything and that’s why it was so good.
North East therapist
I guess it’s just having a better understanding from exactly what the young person wants to work towards. Obviously if the network members are actually in the sessions, then that’s brilliant because then they have that understanding about where they’re coming from with that and from that point they can go, right OK I’ve got a clearer understanding now about what we’re actually all trying to do.
North East therapist
I like the fact that it was amazing that sheet particularly for me because it kind of give them skills that they may never have necessarily knew they had or even thought of and it meant that their thinking, everything was changing because they’d already had the idea of it, they tried to action it and then through actioning it they knew they could achieve it. That gave them more incentive and motivation I guess but it was teaching them that they already had the skills to be able to use them.
North East therapist
Comparison with treatment as usual
Yeah I mean I think there is a big difference because not everyone does that kind of social network. I know we do an assessment and we talk about family but we don’t usually go into the details of what that family member brings which I think was a really important aspect because you get the best out of what they want to get for their goal and who could support them.
West Midlands therapist
So there wasn’t a lot coming from [previous agency] that this is our model of doing things and then for [current agency] we didn’t officially launch a model until really quite late into starting the contract, so treatment as usual was not a structured process, so it relied much more on the varying experience of practitioners and the variant perspectives of those practitioners . . . I really liked having that right at the start, so early on having that social network diagram to be able to locate in my mind what’s going on and to be able to work with that young person early on about identifying a team around them essentially. So that’s a really useful thing. So that compares more favourably to me than trying to work in a traditional one-to-one way.
West Midlands therapist
I think the main thing was the length of time you’re involved with the young person because although in treatment as usual we have like care plans and we sort of review it and everything, it will always continue as long as the young person is finding it helpful and wants that support. Whereas obviously with Y-SBNT it was like, right you’ve got six sessions, and within 3 months.
North East therapist
Yeah I think we were both a bit, like, apprehensive because we’re not used to working in sort of a short burst of sessions. We’re used to having the time to sort of get to know a young person, build up a bit of a relationship and then start doing the work when it was appropriate whereas this seemed a bit like, right you meet the young person and you sort of crack on with it. We couldn’t equate the 3 months could we? We were like six sessions we’ll be done in about a week and a half [laugh].
North East therapist
Normally if it’s just this young person in a normal situation, whatever normal is, that would be once a week at least, at the very least. If there were any issues then that would be increased. If not, if they were so chaotic, every day and sometimes a few times in that day as well. So, for me, there were huge differences . . . But it worked and actually some of our work can be done like that I think and it can be short, sharp, and out. It may not have been 100% working but it worked for that time and I think the skills and the resources they built up over that time is going to last them.
North East therapist
You’re just kind of continuing the drug and alcohol work in treatment as usual whereas this one [Y-SBNT] is more a motivational sort of approach with resources that you’ve given us to try and encourage positive changes but with that social network and with that support.
West Midlands therapist
Care planning I think it’s a common approach to both approaches and there are lots and lots of good overlap there I think.
West Midlands therapist
Integration with existing practice
It was a learning curve for me and I felt like I’d learnt a lot from it and after the Y-SBNT process finished I was able to continue with some of the skills and techniques that we’d learnt from doing that for my day-to-day work.
West Midlands therapist
What I did like was that actually the model itself is very present, so in that sense it’s like you’re working with the immediate scene, you’re working with what’s happening at this moment and what I liked about it was that it wasn’t looking into their past and how that was impacting, it was about now. What can we do now? How can we be proactive now? How could we change this to make it better for that young person and themselves? And everyone, the majority of the time, was on board with it.
North East therapist
Yeah I do it as part of my job anyway [involve network members] but it kind of consolidated it a little bit more because it gives it the right purpose.
North East therapist
So I do think it could, in the right way with the right training and things, I think it could be used across different settings. Potentially as a prevention tool as long as that young person has got the tools and they know how to use that, then it could prevent them from getting on to that point of needing treatment . . . I actually feel the model is really good. I think it can be used in any situation and I think in any setting as well as in services.
North East therapist
And understanding it properly and if they don’t understand it then it’s about everybody communicating what they’re not understanding because they’ll be people there the same because for me it felt like me and [other therapist] actually embedded it into our practice and we believed in what we were doing and because of that it kind of spurred us on to make it right in all of the situations. Because we do if we’re honest, I want it to go to trial. I want it to get to the next stage because it’s worth it. It’s got value to it.
North East therapist
Experience of the research process
What I found difficult was how we were doing the assessments at the beginning and I spent time with these young people and then they were not my young people. So it meant that was hard because they’d got to know us and then we were handing them over to someone else and OK, it worked out well and it was OK and everything was all right but it kind of – it felt like for me I would want to work with them I guess. So the difficulties weren’t necessarily in the model or with the network or with the young person, it was more to do with what was happening with me at the beginning.
North East therapist
So actually changing mindset and having a more structured approach that was quite a shift but that’s absolutely not a bad thing but I think that perhaps it was difficult to fit almost the research project into a fairly kind of set organisational approach. Trying to work out things around the service-level agreement for different organisations, the different internal processes that we’ve had and whether they could be changed to accommodate different elements of research.
West Midlands therapist
So there are multiple different assessments and action plans going and trying to fit the approach into all of those existing systems is difficult. So how would I change the method? I like the Y-SBNT approach but it does have to have room for those different multi-agency action plans . . . Whereas for me, I think on reflection, now look back and there’s really very limited situations where the Y-SBNT approach isn’t more useful actually, you know, we could accommodate having CAMHS come in and what have you at different points, so yes that was it, it was organisationally more than the actual practical delivery of the facilitation of the intervention.
West Midlands therapist
The model I feel could be used in any situation given the right people using it for the right reasons. I think it can be used literally in anything. Logistically you can’t just put six sessions over a 3-month period because they would never touch the database because it wouldn’t be seen as treatment. I think it ended up being over the period of time. But really why should we have to manipulate it to suit the service rather than the young person but without it, it doesn’t get the value that it deserves.
North East therapist
The fact that some of them were treatment as usual and some of them got handed over to myself, that was difficult because you can’t unlearn what you learn and it wasn’t in no way around the model, it was actually just around the beforehand and the afterwards some were handed over to us because I was conscious that I had that training and some of that would come through and we didn’t want any of it to dilute it, so I had to be so removed from the model that I had to make sure that I was being very congruent.
North East therapist
Appendix 19 Service manager’s illustrative quotations
Recruitment
Well the problem wasn’t identifying young people that might be suitable, it was about the process by through which we actually identify whether or not they actually require ongoing treatment or not and I think almost by default we sort of get to a position where get triaged where you automatically get a treatment service.
I’m not always sure that was dead right either because I do think it’s important to do proper screening to establish whether they have the need for treatment or whether they have the need for something else in terms of some sort of education or support but not too structured.
Treatment engagement
When you’re needing the level of intervention from specialism it’s symptomatic of wider malaise, that’s why I always argue if they’re being referred in and there is already a team around them or ought to be because actually they’ll be massive other problems. They’ll have been problems, you know, at school, problems at home, they’re offending. There ought to be a team effectively around the family/child already in place because substance misuse is symptomatic hiding a number of issues.
Rather than having this culture where you’re just constantly looking to refer somebody else on to the next service provider, the next specialist, which in my view leads to disengagement rather than actual engagement it’s about identifying who’s already got a reasonable relationship and how do you support them to deliver some intervention. Say it’s a youth offending team worker or social worker or residential worker, who doesn’t quite feel skilled to do everything or is lacking in materials. That’s exactly what I think a team like [agency] should be providing, is providing that person with some additional support, meeting with them on a regular basis. I think it’s also dead important to ensure that the young person understands that that’s the process that’s happening so they don’t think that it’s all been forgotten about.
There are times when people don’t get the relationships because there’s so many people involved and no one understands what we’re doing and sometimes the bigger the net gets the potential for miscommunication gets bigger as well. I mean in fairness when people work together I think it works extremely well. That’s where Y-SBNT can play a part because it is in a sense a model of collaboration as much as anything else.
Treatment approach
I think the big advantage is it highlights or focuses on recognising that a young person has numerous aspects to their life. Their substance misuse isn’t just the only thing in their life and getting focused on, and I like the idea about taking a wider focus on what else we can do to support, so I like that aspect of it.
I like the approach I suppose of actually trying to think a bit more widely about who’s involved. I think historically it was very individualistic based around the service user as in a young person and I suppose one of the things I’ve always wanted to move much greater towards is a greater sharing of that sort of intervention where you’re actually trying to involve other people to better support the young person.
It’s not about beating anybody up but it is about enabling people to face some of the challenge and utilising the work almost to facilitate and control that, so it’s not simply about you all come in and argue and stuff like that. It’s about facilitation and directing. It’s not about being non-directive, it’s directing in the right way but you need to empower people to do that.
My view would be wherever possible the parent/carer should be involved with that agreement with that plan of intervention with the review process and I think that’s why Y-SBNT appeals to me because it’s actually recognising that basically as a specialist you’re there for maybe what an hour maybe more but you’re there for a very limited period of time in any one week, in any one day and for anybody to sustain the change that they’re looking to do, they will need support from a network, people that they’re engaged with and more often than not young people obviously see that you’re looking at the family element to it and if they’re on board and also being supported which is again what I like about the sort of Y-SBNT model because it recognises that they also have needs as well and highlighting that I think is particularly useful.
They [network members] can continue to review the goals themselves without needing the specialist to constantly hold the reins as it were.
Treatment implementation
Instead of seeing them as troubled, we tend to see them as troublesome and I think one of the things I like about Y-SBNT per se is that ideally what you’re trying to do is empower a number of people to actually – and it’s about the active listening, hearing what people have got to say, how the various issues have potential impact. Bringing people together so that sometimes they can hear how they’re doing as well. I think we probably heard what the young people had to say. I’m not sure we got the network, support network fully in place to actually enable that information.
If you’re sort of concentrating on the outside professionals, they have a take on it I suppose in terms of what they can and can’t do. There’s not unconditional support within that.
My slight concern with it was when I started to look at who was in their network. It would be things like a school teacher and they were in the process of being excluded, so where do they get the support? I think the default position seems to be school teachers, YOT workers and other professions and I’m not sure that that’s always the best. Not for any other reason other than if – I think you’ve got to recognise if they’re only going to be around for a very limited period of time, how useful are they?
Maybe the young people is also about a role for the practitioner to do some of that contacting, clearing, facilitating, identifying what the role ought to be about what they’re going to do trying to bring people in to facilitate. But I think that’s got to be part of a discussion so that they can actually recognise where the supports are.
Will they be able to support that young person and it may be that’s also part of – if someone is going to come on and be accepted as a supporter, do they have to somehow acknowledge that they’re there for the long haul and not just there for, well I’m teaching you this year, well actually you’re got excluded so therefore I’m not but that may be just the reality. So I think we need some more thought about who ought to be included and get that quite focused fairly early.
Yes if you’ve got a very positive adult role model, that’s great and maybe that’s something to look at in terms of whether we could better utilise a peer mentor and introduce them into the process and give them a role that is longer lasting because I do worry that especially some of the young people that we are working with, coming through quite troubled situations, so they might only be in the pupil referral unit, for example, or they’re just at the point of schooling is not quite working for them. So there are some weakness that needs to be looked at.
My interpretation of what the staff were doing was spending several sessions setting goals or agreeing stuff with the young people, that wasn’t necessarily understood or much less time was taken about actually involving a network.
I know this could be wrong, so this is just me sort of listening to, hearing from what some of the staff are doing, it felt like they were spending too much time in meeting with the child individually but never getting to a network thing, so the goal was never set collectively, it was simply set by the young person. Well if you don’t involve the support network in the goal setting, how will you know when you’ve reached it?
I like the idea of setting goals involving people. Slight disadvantage, I think I’m less clear with the young people’s one because when I read the adult one, one of the things I’m conscious of it talks very clearly about equality of relationships and stuff like that and avoiding power imbalance and one of the things that I felt with the young person’s study, I wondered if we’d got too much time trying to set goals without involving other people. I wasn’t clear that we were bringing in the network.
Trying to make sure you get people to recognise where they’re at in terms of wanting to bring about some change and I think you need to sometimes bring on board the families within that as well because they’re trying to cope with a situation. Now some of them already to some degree feel like they just don’t know what to do, some of them blame themselves. But setting reasonable goals, I suppose when you talk about young people, there is trying to get that as a shared experience almost. A shared agreement that says, so we’re all quite clear what we’re aiming towards.
Integration with existing practice
I thought the [Y-SBNT] manual made absolute sense and I think understanding the philosophy in what you’re trying to achieve the idea that actually this whole network effectively becomes the client.
Well I suppose if I’m honest, I’m waiting for the rest of the promised training but as I say for me it’s an approach that we just should be adapting, you know, it’s a very good approach to adopt to involve in people in the process. Part of the toolkit and they should be very much aware of I have shared, I’ve spoken to some colleagues in other services about this, so I have given them links into and said I think it’s an approach that ought to be considered.
As I say as a model I really like the idea of it, I really do. I know that staff, those that have done it enjoy it and are continuing to make use of it. I think it’s a central approach but clearly it’s not for everybody and we know that we have some young people that really struggle with identifying any sort of network, I still don’t think that means we shouldn’t do it but there will be people you try to empower. For me it’s an approach that ought to be fundamental to the way in which we work.
I’m probably very conscious that for me I don’t just see it in terms of being a substance misuse intervention. I think it’s got direct applicability as a model right across the board and we should be utilising it. Very much in the same way that if you look at MSTs and all the rest of it, this is even easier as far as I’m concerned, it makes more rational sense.
I like the approach per se across the board in terms of an approach that all staff should adopt in terms of empowering people, trying to involve the support networks that they’ve got, try to identify them to agree goals. I think this particular model also would work extremely well earlier in the system where I would say for me, I would like people to be doing IBAs and rather than just simply doing that extending IBAs, I would like it to be incorporated into an extended IBA because I think that would fit very neatly as part of the process. I think it’s short, it’s sweet and it gets to the point very quickly and I think you can get it working very well.
Personally I think it’s got a lot of mileage and I would try and push it further. Bring it into the system earlier as an intervention as part of, you know, if you had school health or whatever . . . My suspicion would be that it’s less sustainable if we haven’t got the support network properly in place. Whereas if you did it earlier you’ll probably get a lower level, you’re actually almost preventing a lot of, before the behaviour itself becomes entrenched, you have to get it in soon.
Appendix 20 Overall averages for each stage of intervention (West Midlands and North East combined): youth social behavioural network therapy sessions
| Activity | Early (n = 11) | Middle (n = 24) | Late (n = 7) | |||
|---|---|---|---|---|---|---|
| Frequency | Quality | Frequency | Quality | Frequency | Quality | |
| Session management | ||||||
| 1. Maintaining structure | 3.90 | 3.80 | 3.90 | 3.90 | 3.00 | 3.00 |
| 2. Agenda setting | 4.00 | 4.00 | 2.85 | 2.83 | 2.09 | 2.09 |
| 3. Explanation of philosophy of treatment or treatment session | 3.75 | 3.75 | 2.48 | 2.48 | 2.34 | 2.34 |
| 4. Reviewing intersession change | 0.00 | 0.00 | 1.53 | 1.43 | 2.59 | 2.59 |
| 5. Consistency of problem focus | 3.92 | 4.00 | 3.70 | 3.70 | 3.34 | 3.34 |
| 6. End-of-session summary | 1.25 | 1.34 | 0.70 | 0.70 | 0.59 | 0.59 |
| Specific tasks | ||||||
| 7. Homework | 1.24 | 1.24 | 1.75 | 1.80 | 0.84 | 0.84 |
| 8. Alternative activities to drinking | 0.77 | 0.77 | 2.03 | 2.05 | 0.75 | 0.84 |
| 9. Social support for change – general | 2.40 | 2.30 | 2.00 | 2.00 | 1.34 | 1.34 |
| 10. Involvement of others in behaviour change | 1.17 | 1.07 | 3.45 | 3.33 | 2.67 | 2.17 |
| 11. Identify sources of support for change | 3.80 | 3.70 | 3.85 | 3.85 | 2.75 | 2.75 |
| Therapist style | ||||||
| 12. Therapist as task orientated | 3.82 | 3.82 | 3.73 | 3.80 | 3.25 | 2.75 |
| 13. Therapist as active agent for change | 0.00 | 0.00 | 0.80 | 0.90 | 0.84 | 1.00 |
| 14. Collaboration | 1.65 | 1.65 | 2.30 | 2.33 | 2.17 | 2.17 |
| 15. Interpersonal focus | 3.82 | 3.82 | 3.40 | 3.40 | 2.42 | 2.42 |
| 16. Goal setting | 0.64 | 0.55 | 3.10 | 2.98 | 0.50 | 0.67 |
Appendix 21 Descriptive report of baseline substance use
This table summarises the substance use of the full sample (n = 53) at baseline (preceding 90 days).
| Analysis | Main problem substance | Total | ||||
|---|---|---|---|---|---|---|
| Cannabis | Alcohol | Legal highs | Mephedrone | Solvents | ||
| Frequency | 39 | 5 | 5 | 2 | 2 | 53 |
| Percentage | 74 | 9 | 9 | 4 | 4 | 100 |
Number of substances used over the baseline assessment period:
-
median: 2 (range 1–5)
-
mean: 2.15 (SD 1.06)
| Participant | Main problem substance | Number of substances used | Substance(s) used | Substance use pattern notes |
|---|---|---|---|---|
| 1000 | Cannabis | 1 | Cannabis | 0.5 g of cannabis 3–5 days a week (2.5 g per week) |
| 1001 | Cannabis | 4 | Cannabis, alcohol, cocaine, legal high | 1 spliff of cannabis almost every day; 12 units of vodka most days; one instance of cocaine use (one line); one instance of legal high use (1 g) |
| 1002 | Cannabis | 1 | Cannabis | 0.5 g of cannabis 3–5 days a week |
| 1003 | Cannabis | 1 | Cannabis | 1 g of cannabis daily |
| 1004 | Alcohol | 4 | Alcohol, cannabis, legal high, mephedrone | One joint of cannabis 3 days a week; most Fridays drinks 25–35 units (of vodka, mixed spirits or beer); one instance of legal high use (one joint); one instance of mephedrone use (one line) |
| 1005 | Cannabis | 3 | Cannabis, alcohol, legal high | 1 g of cannabis 4 days a week; of vodka every other Saturday, occasionally of rum (four times); one instance of legal high use (‘looked like cannabis’) |
| 1006 | Cannabis | 3 | Cannabis, alcohol, cocaine | 1 g of cannabis daily; drank 5 units 1–2 days a week and then moved up to 10–15 units 5 days a week, hospitalised after one instance of drinking 25–30 units; 2 g of cocaine twice a month |
| 1007 | Cannabis | 2 | Cannabis, alcohol | 0.25–1 g of cannabis 5 days a week; three drinking occasions (20, 10 and 4 units) |
| 1008 | Alcohol | 1 | Alcohol | 1–8 units approximately 2 days a week, three parties where drank 30–50 units |
| 1009 | Legal high | 3 | Legal high (Exodus) cannabis, alcohol | 15 spiffs of Exodus or three spliffs of cannabis 3 days a week; drank 14 units on one drinking occasion (grandad’s birthday) |
| 1010 | Cannabis | 2 | Cannabis, alcohol | 0.5–1 g of cannabis 3–4 days a week; drank 2 units on two occasions (friend’s birthday party) |
| 1011 | Legal high | 3 | Legal high (Cyclone), alcohol, cannabis | 3–9 joints of Cyclone 0–6 days a week; 1.5 joints of cannabis once a week (Friday); 5 l of cider once a week (Friday) |
| 1012 | Cannabis | 2 | Cannabis, legal high (Exodus) | 0.5–8 g of cannabis daily; one instance of Exodus use (2 g) |
| 1013 | Alcohol | 4 | Cannabis, alcohol, speed, cocaine | One bucket and/or joint of cannabis most days; 2 weeks of a small line of speed daily; 10 drinking days (4–10 units); one instance of cocaine use (one line) |
| 1014 | Cannabis | 2 | Cannabis, alcohol | 0.28–0.57 g of cannabis daily; drank 2 units on one occasion (sister’s birthday) |
| 1015 | Cannabis | 1 | Cannabis | Two buckets of cannabis six times a week |
| 1016 | Legal high | 1 | Legal high | Two joints of legal high daily |
| 1017 | Cannabis | 3 | Cannabis, legal high (Exodus), alcohol | 0.5 g of Exodus or 0.66–1 g of cannabis 6–7 days a week; drank 20 units on one occasion |
| 1018 | Cannabis | 2 | Cannabis, alcohol | 0.66–2 g of cannabis 6 days a week; drinks 12 units once a week (Saturdays) |
| 1019 | Cannabis | 1 | Cannabis | 1 g of cannabis daily |
| 1020 | Mephedrone | 4 | Mephedrone, alcohol, legal high, cocaine | 10–30 lines of mephedrone 6 days a week for 7 weeks; two drinking occasions (12 and 20 units); one instance of legal high use (one joint); one instance of cocaine use (5 g) |
| 1021 | Cannabis | 2 | Cannabis, alcohol | Three joints of cannabis 6 days a week; three drinking occasions (8–25 units) |
| 1022 | Alcohol | 1 | Alcohol | In young offender institute for approximately 8 weeks. Three drinking occasions (8, 20 and 40 units) |
| 1023 | Cannabis | 2 | Cannabis, alcohol | Four joints of cannabis 2–3 days a week; one drinking occasion (10 units) |
| 1024 | Cannabis | 2 | Cannabis, alcohol | Two joints of cannabis 1 day a week; drinks about 8 units approximately every other week, drank 40 units on one occasion |
| 1025 | Cannabis | 1 | Cannabis | 0.86 g of cannabis daily |
| 1026 | Cannabis | 2 | Cannabis, alcohol | 0.14 g of cannabis daily; drinks 15–25 units most Saturdays |
| 1027 | Cannabis | 1 | Cannabis | 0.35–0.86 g of cannabis 3 days a week |
| 1028 | Cannabis | 2 | Cannabis, alcohol | 1.88–3.12 g of cannabis daily; drinks 22.5 units every weekend |
| 1029 | Cannabis | 2 | Cannabis, alcohol | 0.28–0.43 g of cannabis daily; one drinking occasion (10 units) |
| 1030 | Legal high | 1 | Legal high | 10–14 joints of legal high daily |
| 1031 | Legal high | 2 | Legal high, cannabis | Three joints of cannabis 2 days a week (weekends) for 5 weeks; 0.5–2 joints of legal high 5 days a week (weekdays) for 5 weeks |
| 1032 | Mephedrone | 5 | Mephedrone, alcohol, speed, legal high, MDMA | 1–2 g of mephedrone daily; one drinking occasion (45 units); three instances of MDMA use (0.5 g); one instance of speed use (three bombs); one instance of legal high use (one skin pipe) |
| 1033 | Solvent | 1 | Solvent | One can of deodorant/lighter refill 3 days a week |
| 1034 | Cannabis | 2 | Cannabis, alcohol | In custody for 1 month. 0.33 g of cannabis daily; drinks 25 units most weekends |
| 1035 | Cannabis | 1 | Cannabis | 0.5 g of cannabis daily |
| 1036 | Cannabis | 3 | Cannabis, alcohol, cocaine | 2.5 g of cannabis daily, until pregnancy; two drinking occasions (15 units); two instances of cocaine use (1 g) |
| 1037 | Cannabis | 2 | Cannabis, alcohol | 0.28–3.5 g of cannabis daily; drank 5 units of vodka daily for 3 weeks before returning to parents’ home |
| 1038 | Cannabis | 3 | Cannabis, alcohol, mephedrone | 1–2 g of cannabis daily; drinks 20–35 units most weekends (more when birthdays); three instances of mephedrone use (2 g) (all birthdays) |
| 1039 | Cannabis | 2 | Cannabis, alcohol | 0.5–1.5 spliffs of cannabis daily; four drinking occasions (2–30 units) |
| 1040 | Cannabis | 2 | Cannabis, alcohol | 0.36–0.61 g of cannabis daily; five drinking occasions (7–10 units) (birthdays and death anniversaries) |
| 1041 | Cannabis | 2 | Cannabis, alcohol | Two to three buckets of cannabis daily; five drinking occasions (10–20 units) |
| 1042 | Cannabis | 2 | Cannabis, alcohol | 3–15 joints of cannabis daily; four drinking occasions (30–40 units) |
| 1043 | Cannabis | 2 | Cannabis, alcohol | One to two joints of cannabis and four to seven cannabis bongs daily; drinks 10 units once a week (Fridays) |
| 1044 | Cannabis | 2 | Cannabis, alcohol | 0.5 g of cannabis daily; drinks 30 units approximately every other weekend (birthdays, out with friends) |
| 1045 | Cannabis | 1 | Cannabis | In custody for 2 months. 0.11–0.22 g of cannabis daily |
| 1046 | Cannabis | 2 | Cannabis, alcohol | Only one occasion of any substance use (friend’s birthday): 1 g of cannabis and one shot of whisky |
| 1047 | Cannabis | 2 | Cannabis, alcohol | One occasion of cannabis use (1 g); one occasion of drinking (8 units) |
| 1048 | Cannabis | 2 | Cannabis, alcohol | 0.25 g of cannabis a day for 1 week, then sporadic use; one drinking occasion (barbecue) (4 units) |
| 1049 | Alcohol | 2 | Alcohol, cannabis | Drinks 45 units every weekend; 1–2 g of cannabis every other weekend |
| 1050 | Solvent | 1 | Solvent | 0.25 of a can of gas for 8 days |
| 1051 | Cannabis | 5 | Cannabis, alcohol, diazepam, cocaine, speed | Four buckets + two joints of cannabis daily; three drinking occasions (30–35 units); two instances of cocaine use (two lines); two instances of speed use (four to eight lines); six instances of diazepam use (70 mg) |
| 1052 | Cannabis | 4 | Cannabis, alcohol, cocaine, legal high | Two joints of cannabis daily; one joint of legal high 3 days a week for 6 weeks; five drinking occasions (6–12 units); five instances of cocaine use (two lines) |
List of abbreviations
- A&E
- accident and emergency
- AMD
- adjusted mean difference
- BSFT
- brief strategic family therapy
- CAMHS
- Child and Adolescent Mental Health Services
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions five-level version
- FES
- Family Environment Scale
- FFT
- functional family therapy
- FRI
- Family Relationships Index
- GP
- general practitioner
- HRQoL
- health-related quality of life
- IBA
- identification and brief advice
- IPDA
- Important People Drug and Alcohol
- MDFT
- multidimensional family therapy
- MST
- multisystemic therapy
- NCB
- National Children’s Bureau
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPS
- novel psychoactive substance
- PhD
- Doctor of Philosophy
- PRS
- Process Rating Scale
- QALY
- quality-adjusted life-year
- SBNT
- social behaviour and network therapy
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SE
- standard error
- TAU
- treatment as usual
- TLFB
- Timeline Follow-Back
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
- UKATT
- UK Alcohol Treatment Trial
- VAS
- visual analogue scale
- WAI
- Working Alliance Inventory
- YOT
- youth offending team
- YPAG
- young people’s advisory group
- Y-SBNT
- youth social behaviour and network therapy