Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-1210-12011. The contractual start date was in August 2013. The final report began editorial review in October 2020 and was accepted for publication in March 2022. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research, or similar, and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2022 Byng et al. This work was produced by Byng et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Byng et al.
SYNOPSIS
In February 2020, there were over 83,000 people incarcerated in England and Wales, the majority (95%) of whom were male. The rate of mental illness in this group is very high and much higher than the general population1,2 (Table 1). Prevalence rates vary internationally due to methodological differences, but a consistent finding is that about one in seven people in prison have major depression or psychosis. 1 Comorbidity for this group is the norm, as are chaotic lifestyles with a wide range of personal and social problems, including homelessness, unemployment and broken relationships with partners and children. 9 In our earlier descriptive study,10 we found that of 200 offenders (100 offenders serving prison sentences and 100 offenders serving community sentences), 59% reported having common mental health problems, 37% reported problems with family relationships and the majority (65–70%) were unemployed or on long-term sickness benefit. For people leaving prison, the transition into the community is associated with increased rates of suicide and self-harm. For example, the risk of suicide for male offenders leaving prison is eight times the national average. 11,12 Although mental illness rates for female prisoners are consistently higher,13 the Engager project focused on male prison leavers because of the smaller numbers of females in prison estates.
| Mental health condition | Male prisoners (%) | Male general population (%) |
|---|---|---|
| Psychosis3 | 4 | 1 |
| Major depression3 | 10 | 2–4 |
| Affective disorder/anxiety4 | 6–29 | 4–10 |
| Any personality disorder3 | 65 | 5–10 |
| Antisocial personality disorder3 | 47 | 5–7 |
| Alcohol misuse/dependence5 | 18–30 | 14–16 |
| Drug misuse/dependence5 | 10–48 | 14–16 |
| PTSD6 | 4–21 | 2 |
| Intellectual disability7 | 0.5–1.5 | 1 |
| ADHD8 | 26 | 1–5 |
In 2018, 63% of custodial sentences received were for less than 12 months. 14 Short custodial sentences are known to be less effective than community sentences at reducing reoffending,15 with the 12-month proven reoffending rates for short-sentence prisoners currently close to 60%. 16 As well as reoffending, frequent transitions in and out of prison take a high toll on the individual, their family and their social tenure. 17 Comorbidity is high for this group,18 as is the financial cost of failing to address these health and social care issues. 19
In the UK, although the NHS commissions all health services, it appoints a range of providers from NHS, private, and voluntary and community sectors. On the one hand, a prison may have multiple providers and each service will provide a specific service only (e.g. primary care, general physical health care, mental health care). On the other hand, in some cases, a prison may use a number of different providers for services such as primary and secondary mental health care, or drug and alcohol services. However, using a number of different providers can make continuity of care more complex, especially for people who require input from multiple services, as often these providers do not operate in an integrated way. This issue is further complicated at the point of release, as often the health-care providers within a prison will not be the same services that operate in the community.
There has been investment in prison mental health services for those with severe and enduring mental illness. 20 There is research evidence that critical time intervention, that is, a structured, time-limited form of case management,21 can be adapted for people with severe and enduring mental illness who are in prison. In a randomised controlled trial (RCT),22 critical time intervention demonstrated increased engagement with community mental health services at 6 weeks post release from prison.
The identification of common mental health problems may occur during induction, through self-reporting or when staff raise concerns. However, we know from other studies that this will miss many people and will under-represent the level of need. 23 In addition, provision of psychological therapy for people with common mental health problems who are in contact with the criminal justice system (CJS) is limited in both prison and community settings. 10 Once released into the community, ex-prisoners with common mental health problems are, in theory, provided for by mainstream statutory services, including general practice, community mental health teams and Improving Access to Psychological Therapies (IAPT) services; however, few ex-prisoners access these services,10 suggesting that a lack of care on release is the norm. 24
Despite negligible uptake and high need, to the best of our knowledge, worldwide, no systems have been identified for actively engaging people with common mental health problems while in prison, providing support and working with them to engage with community services. Organisational interventions, such as collaborative care (i.e. a complex intervention based on a chronic disease management model), have been shown to be beneficial for those with depression25 and comorbid physical health problems. 26 However, such interventions are yet to be tested with prison leavers. Elements of collaborative care have the potential to ensure continuity over time and co-ordination between teams and practitioners, as well as support for self-care.
The points above provide clear theoretical grounds for the potential health gain in developing an intervention that (1) focuses on short-term prisoners with common mental health problems, (2) takes a collaborative care approach to span all the different agencies/professionals involved and (3) takes into account the wide range of social and health problems individuals may face. There is very limited research into developing and evaluating mental health interventions within prisons. 27 RCTs within the CJS can be more complex than in other settings because of a range of factors, such as organisational difficulties, maintaining trial arm allocation, poor follow-up rates and difficulties selecting appropriate outcome measures. 1,17,28–30
How to navigate the Engager research programme and report
The National Institute for Health and Care Research-funded Engager research programme ran between 2013 and 2020, across two phases. Figure 1 depicts the whole Engager research programme. The Engager research programme was designed to work iteratively between questions relating to intervention development and questions relating to trial science. The Engager research programme included four interlinked workstreams delivered across two phases. Workstream 4, addressing health economics, continued across both phases.
FIGURE 1.
The Engager research programme.
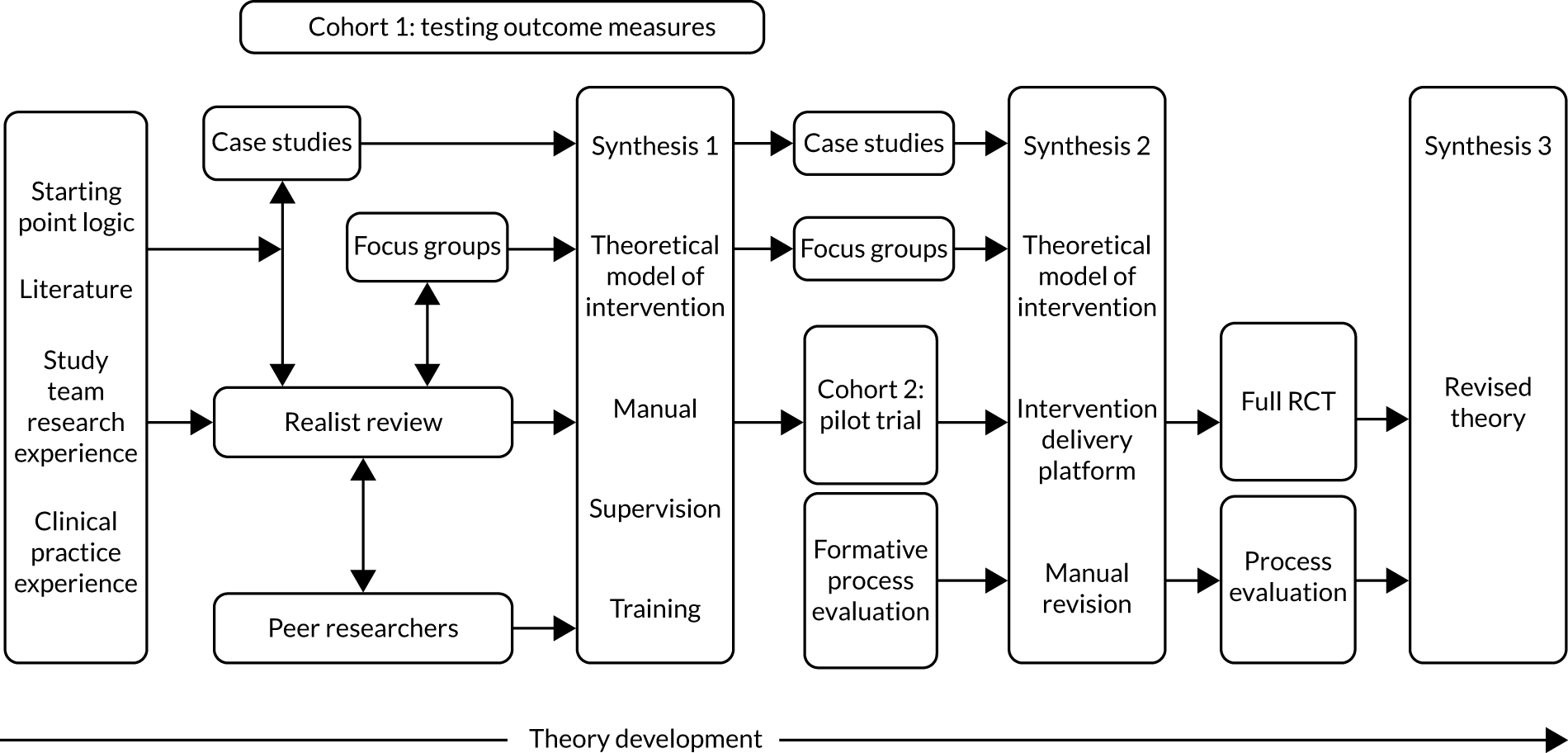
Phase 1: intervention development and trial methodology
A mixed-methods approach was used for the development of a theoretically informed person-centred co-ordinated intervention (workstream 1) and this involved:
-
a realist review
-
organisational case studies
-
focus groups
-
a rapid realist review of implementation
-
a formative process evaluation.
The data were brought together at two time points (i.e. synthesis 1 and synthesis 2) to iteratively develop the theory and practice of the intervention. The Engager intervention is summarised in this synopsis, with more detail provided in Report Supplementary Material 6.
In parallel, we developed the trial science methodology to evaluate the intervention (workstream 2) and this involved:
-
selection of outcome measures
-
development of tools to measure ‘the process of care’
-
a pilot trial to test the trial procedures
-
initial health economics modelling (workstream 3).
Phase 2: trial, process evaluation and cost-effectiveness (workstreams 3 and 4)
In phase 2 we conducted:
-
an RCT
-
a cost-effectiveness analysis and a cost–consequence analysis
-
a mixed-methods process evaluation, which took a realist-informed approach to examining fidelity, problems with implementation and potential improvements to theory.
Our patient and public involvement work was extensive and interwoven through all workstreams and both phases. For ease of reading, workstream 4 has been split into two sections, that is, phase 1 (economic modelling) and phase 2 (cost-effectiveness and cost–consequence analyses).
Alterations to the programme
The initial contract was to develop the intervention and to carry out an exploratory trial. A proposal to switch to a definitive trial was agreed at the mid-programme checkpoint report. An extension to collect data at 12 months was agreed once recruitment viability had been established in the main trial. Owing to the decision to have a definitive trial, along with issues of data availability, it was agreed that the initial plan for decision modelling of economic benefits of a full trial would be replaced by carrying out a trial-based cost–consequence analysis.
Developing a theoretical model of the intervention (phase 1, workstream 1)
Developing solutions to complex problems within complex systems is challenging, as it requires an in-depth understanding of the nature of the intervention and the implementation context. 31 Relatively little attention is paid to the developmental phase of the complex intervention cycle and it has been argued that realist-informed methods may become routine once sufficient empirical examples are available to guide practice. 32,33
The aim of workstream 1 was to develop an empirical example of a theoretical model of the Engager intervention. We used realist methods34 as an overall framework with which to establish the mechanisms involved and the causal pathways and contextual conditions that might lead to positive outcomes. Behaviour change theory35 influenced our understanding of the mechanisms needed to bring about change. Throughout the development, the intervention was seen as a two-step behaviour change model, that is, how the system and research team supported practitioners and then how practitioners supported offenders. The former became the intervention delivery platform (IDP) and the latter was developed into a detailed set of practitioner behaviours that were designed to support a heterogeneous group of offenders towards better well-being and rehabilitation, and is expressed as the programme theory. Through testing this programme theory, we offer empirical examples to guide future practice for other researchers considering realist-informed approaches to developing and evaluating interventions with complex groups.
There were three stages to the theory development. An initial starting point model, articulated in the original funding bid, was based on the team’s clinical and research knowledge and previous patient and public involvement work. The first stage involved a realist review, focus groups and organisational case studies, which were synthesised (i.e. synthesis 1) into a prototype intervention that was then delivered in the pilot trial. The second stage involved a realist formative process evaluation within the pilot trial, a further organisational case study and focus group, and a realist review of implementation literature. The results of these were brought together (i.e. synthesis 2) to inform the intervention theory and IDP (e.g. training, manual, supervision), which were then operationalised in the main trial. Throughout this workstream, the peer researchers commented on the academic researchers’ findings and the intervention development, helping the academic researchers to identify gaps in understanding. The sections below detail the components of workstream 1 and illustrate how each component contributed to the development of the programme theory of the Engager intervention.
Realist review
The realist review has been published36 and, in accordance with RAMESES II (Realist And Meta-narrative Evidence Syntheses: Evolving Standards II) reporting standards,31 the realist review aimed to specify how an integrated person-centred system to improve the mental health of offenders with common mental health problems might work. Therefore, the focus was on in-depth theory-building as a key contribution to the development of the intervention. The review is methodologically novel in the way that it operationalises a realist approach [e.g. use of ‘if–then’ statements, structured questions for synthesis of context–mechanism–outcome (CMO) configurations] in parallel with the timelines and methods of a large research project. The following three-stage process was used:
-
We identified sources providing rich descriptions of interventions (and/or their delivery) providing care for offenders with common mental health problems through hand-searching a core set of 16 journals, citation-chasing, elicitation from experts (including men with lived experience of prison and release) and database searches. Searches were extended beyond offender health where insufficient sources were located. Screening of sources, therefore, included those relating to mental health care, and health and social inclusion service delivery in vulnerable groups.
-
We identified explanatory accounts (i.e. ideas about how a problem can best be addressed) (n = 347). ‘Working backwards’ from outcomes (including those from meetings with the Peer Researcher Group of men with lived experience), explanatory accounts were extracted and tabulated, and then expressed as ‘if–then’ statements, specifying (as far as the source allowed) CMO configurations.
-
We consolidated explanatory accounts (n = 75) and produced a conceptual platform (i.e. a core set of processes about how intended effects could be achieved). To enable feedback about expression and scope, consolidated explanatory accounts were shared throughout the process with our expert group of practitioners and academics.
An overview of the conceptual platform developed for the Engager intervention depicts the key agents and their relationships (Figure 2). The three columns in Figure 2 describe different key interactions relating to participating in a mental health improvement intervention both before and after release from prison. The contextualised interactions can be between practitioners and offenders, between the practitioner/offender and other practitioners, or between the offender and family members, peers or mentors. At the centre of the intervention are the core interactions between practitioners and offenders. It is within these interactions that the intervention had the potential to activate mechanisms that affect offenders’ thinking, emotions and behaviours. In between these core interactions, the interactions of both the practitioner and offender with other people (i.e. the central three circles in Figure 2) can further affect changes in thinking, emotions and behaviours, and how these interact with their contexts. These changes influence the subsequent interaction between the practitioner and offender and generate other potentially beneficial effects.
FIGURE 2.
Conceptual platform developed for Engager. Reproduced with permission from Pearson et al. 36 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the figure.

This realist review contributed substantively to our understanding of how an integrated person-centred system might work. Findings suggested that supporting positive mechanisms for change involved optimising the local support available and minimising the potential for complex relationships with services to destabilise an individual. Box 1 outlines the core set of processes proposed in the conceptual platform.
-
Different systems, in particular health and criminal justice, and having goals that are consistent with one another.
-
Attaining consistency between strategic goals and the goals of practitioners.
-
Making referral pathways and links between organisations comprehensible to practitioners and providing opportunity for the development of constructive working relationships.
-
Practitioners being facilitated and enabled to balance factors that can be in tension, for example ‘knowing how’, as well as ‘knowing that’, analysing one’s own behaviour while remaining attentive to emotions, and working towards an individual’s goals.
-
Practitioners being facilitated and enabled to apply scientific and experiential knowledge judiciously in working with individual offenders and colleagues, and the systems in which services are delivered.
-
Practitioners having sufficient knowledge about mental health and how to develop supportive relationships with people with mental health issues.
-
Recognising the individuality of offenders throughout all interactions in the criminal justice, health and social care systems.
-
Aligning resources to enable offenders to achieve their collaboratively agreed goals.
-
Practitioners supporting reconnection with, and/or development of, networks of support outside prison.
-
Offenders having reasons to trust practitioners, services and systems.
For pragmatic resource reasons, we did not take on the task of reviewing psychological therapies, having made an early decision to use mentalisation-based approaches (MBAs)37 to support existing competencies because of high co-occurrence of traits, such as emotional reactivity linked to the diagnosis of a personality disorder. The realist review also provided a detailed methodological example of theory-driven intervention development. In particular, the conceptual platform was used to help us understand where we had gaps in our understanding and how the organisational case studies, focus groups and peer researchers could help fill these gaps. For example, the conceptual platform highlighted a gap in our understanding of how families and peer mentors may inform the intervention and, therefore, one of the focus groups was developed to look at the role of families and another organisational case study site involved analysis of the use of peer mentors.
Organisational case studies
The organisational case studies article is published. 38
The organisational case studies aimed to augment our emerging core intervention theory by gaining learning from a range of promising services that provided support and/or treatment for people experiencing common mental health problems within the CJS. The organisational case studies also aimed to identify key elements of practice, for example what was and was not effective in engaging people and maintaining contact with the service. Organisational case studies were particularly useful in eliciting grounded knowledge that was unpublished and, therefore, unavailable for the realist review.
Four cases were selected. Organisational case studies 1 and 2 were undertaken prior to the formative evaluation and organisational case studies 3 and 4 were undertaken after the formative evaluation. Data included documents (e.g. service standard operating procedures), field notes and semistructured interviews. Realist-informed interview schedules (see Report Supplementary Material 1) were constructed using the CMO configurations in our developing theory. All documents were analysed using deductive content analysis. Interview data were interrogated through a qualitative framework approach. 39
Seven main themes were identified: (1) collaboration, (2) client engagement, (3) client motivation, (4) supervision, (5) therapeutic approach, (6) peers and (7) preparations for ending. The case studies highlighted that engaging and motivating clients was dependent on the relationship built with the professional. Consistent, respectful, open and honest communication over time was needed to activate mechanisms that produced a sense of trust and rapport. Professionals were often unable to provide this level of support if they did not work in multiagency collaborations, supported by supervision.
Engager organisational case studies highlighted the clear need for an intervention to have in its toolbox a range of psychological therapies. In addition, the case studies suggested that the addition of a MBA would be beneficial to support the relationship between the practitioner and client, as well as to help deal with mood lability. Supporting individual offenders to mentalise effectively about their situations also aligned with the realist notion of activating generative reasoning mechanisms that enable change in thinking, emotions and behaviours.
The organisational case studies were also critical to our understanding of the importance of a ‘strong’ IDP (i.e. manual, training and supervision) that would support the practitioners in operationalising the Engager theory. The findings focused specifically on the role of supervision in ensuring ongoing support for practitioners as part of a team and on the additional need for external supervisors.
Furthermore, the organisational case studies highlighted the importance of preparatory work in prison to build trust, rapport and engagement. The case studies also prioritised the need to prepare clients for the end of the intervention as a positive step in a longer journey, including providing clients with a summary of their progress.
Finally, the initial prototype and the realist review highlighted the use of peers to support engagement and improve outcomes. The organisational case studies evidenced benefits for peers delivering support, but there was less evidence of benefit for the recipient. The Peer Researcher Group strongly asserted the importance of peer support. However, the research team reluctantly decided, following protracted discussions with the Peer Researcher Group, that this potential component was not logistically deliverable within the resources of this project. Instead, Engager practitioners would encourage and facilitate access to peer/mentoring services.
Focus groups
This work has been published. 40
The published work focuses on the methodological development of the focus groups. The aim of the focus groups was to explore the views of subgroups of the target population whose experiences were not represented by previous published data, the realist review and organisational case studies.
The following four focus groups were convened: (1) homelessness on release from prison, (2) young men who had served prison sentences, (3) people with a ‘loved one’ in prison and (4) men recently released from prison. Each group was recruited through a community-based service that already knew the participants and continued to support them afterwards.
Data were coded and analysed deductively using our theorical framework. This analysis consisted of four columns representing time points (i.e. initial meeting with the participant, actions in prison, actions in the community and preparations for endings) and six rows representing the main functions of the intervention (i.e. shared understanding of individual goals, shared action plan to achieve individual goals, therapeutic approach, family and community capabilities, peer or other volunteer mentor support, and liaison by practitioner and participant with other professionals/teams).
Conversations within the focus group predominantly related to the following areas within our framework.
Developing the shared understanding by making links between a person’s emotions, thinking, behaviour and social outcome
Members of the focus groups talked about a reluctance to discuss emotions for fear of appearing weak. Often, emotions were being masked by other behaviour (e.g. using substances or ‘putting on a front’) and this highlighted the need to build trust and engagement before moving too quickly into talking deeply about emotions; however, periods of abstinence may be windows of opportunity for this work.
Developing the shared action plan: matching goals to resources
Men in the focus groups talked about a range of resources within prison that they could use to pass the time and/or could help if they were feeling low, including education, workshops, gym and chaplain. These resources would be key resources that the Engager practitioners could link with in the prison.
Developing the shared action plan: other professionals
The men talked about how, in their experience, a diagnosis of mental illness was often not helpful, as it could limit access to other services or professionals and it may cause professionals to treat them more negatively. This supported our initial thoughts that, although the focus of the Engager intervention is for those with common mental health problems, it would be a person- rather than diagnostic-centred intervention.
Developing the shared action plan: other people as a resource
The roles of other people, especially family members, were talked about at length in the focus groups. The men highlighted that often families receive little information. Family members are often reluctant to ask for information, help or support because of the perceived stigma of having a family member in prison. The men also talked about preparing both the soon-to-be released prisoner and family about expectations. Prisoners cannot always expect to return to situations as they left them. Proactive expectation management can facilitate communication, including creating awareness of how a family member or friend has had to do things differently to manage on their own and has had to make other changes over time. A partner may have grown in confidence and independence; this can be difficult for released prisoners to adjust to and also the family member may feel guilty about this. These discussions highlighted a gap within the developing intervention, that is, the Engager practitioner may also have to work closely with family members to provide information, to support contact with services and, importantly, to prepare both sides for what release would be like.
What to do in prison to prepare for community contact
The focus groups gave us many practical actions that the Engager practitioners could do to prepare released prisoners for contact in the community. The men talked about accommodation and money as key concerns during the initial release period and, therefore, the Engager practitioners could work alongside other services to try to secure accommodation and money on release. We recognised that this would not always be possible and that some people would be homeless upon release. The men suggested making sure that prisoners knew all of the locations a person may present at if they were homeless (e.g. drop-in centres, homeless shelters or soup kitchens).
Community (first meetings)
The men suggested that it can be hard to establish a routine in the first few weeks and this was a key factor in the likelihood of retuning to prison, alongside insecure accommodation and financial issues. This indicated to us that another role the Engager practitioner could have is working with the person to develop a new routine.
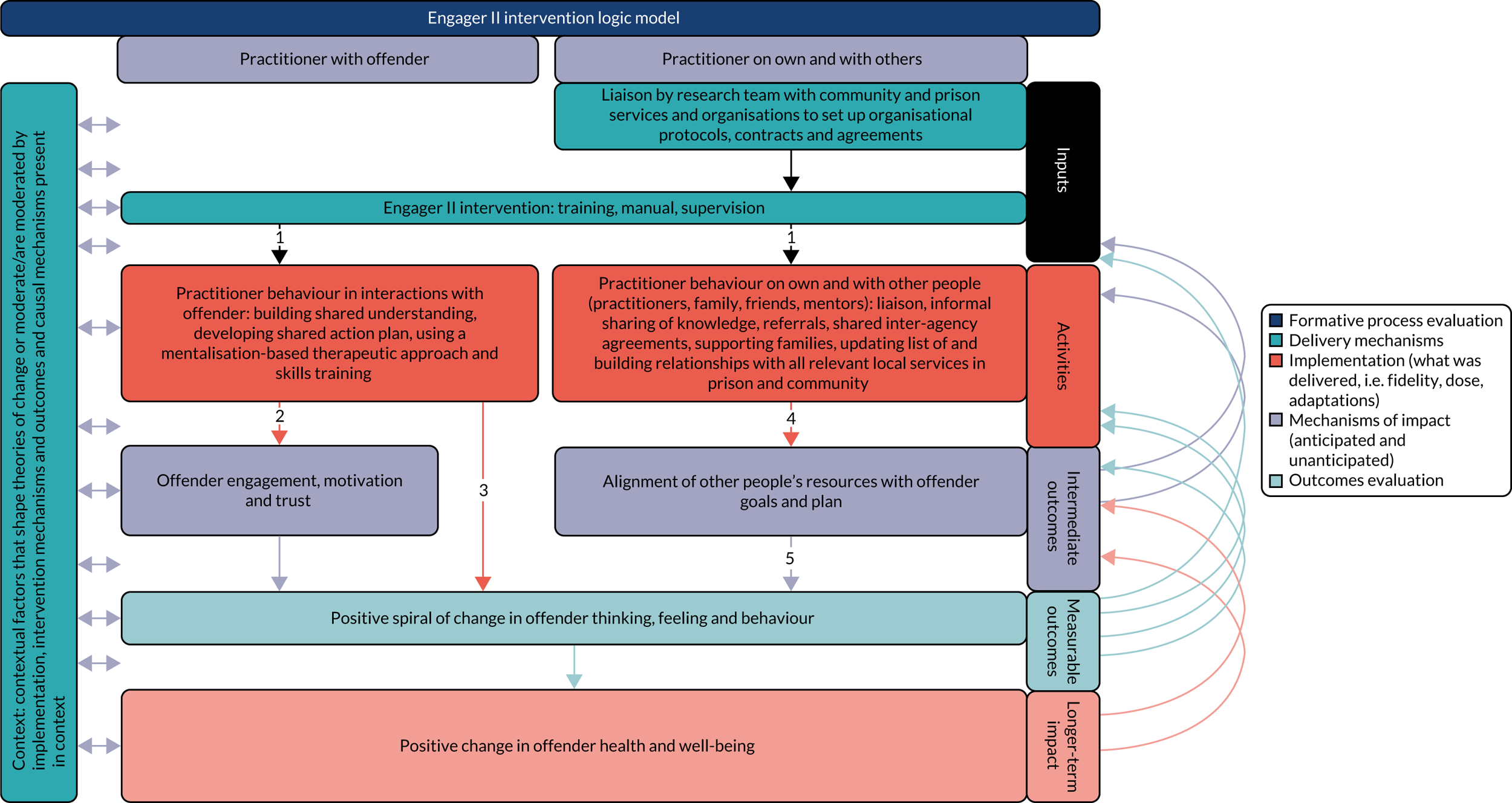
The data from the realist review, focus groups, organisational case studies and peer researcher meetings were synthesised into a prototype intervention (i.e. synthesis 1), which was then delivered and evaluated in the pilot trial and formative process evaluation. Figure 3 depicts the overarching structure of the Engager logic model theory. More detail of that synthesis process is detailed in Report Supplementary Material 2. During the synthesis, narratives were produced of the core components (see Report Supplementary Material 3 for details of the theory for shared understanding, a shared action plan, action in prison and action in the community).
FIGURE 3.
Engager logic model. Reproduced with permission from Brand et al. 41 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for non-commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc/4.0/. The figure includes minor additions and formatting changes to the original figure.
The peer researchers contributed to the discussions and challenged the academic researchers throughout the group meetings. The peer researchers required the academic researchers to prioritise the importance of ‘self-care’ and ‘family support’, even when the published data and financial capabilities suggested that these might not be achievable. Consequently, focus groups addressing these issues were held and a decision was made that Engager practitioners should work with participants’ families when appropriate.
Formative process evaluation
The formative process evaluation is published. 41
The formative process evaluation continued the realist approach. Realist approaches addressed the need to build theory prior to outcome evaluation33 and the need for greater attention to be paid to context during delivery and to effective scale-up during later implementation. 42
Face-to-face semistructured realist interviews were digitally audio-recorded and transcribed verbatim. Interviews were conducted with Engager practitioners, Engager supervisors, prison leavers and CJS, health and/or social care professionals. In addition, Engager practitioners used a pro forma to record notes about what practitioners had carried out in each session with, or on behalf of, participants, and any significant issues that had been discussed. Scanned copies of practitioner notes were examined using a structured pro forma to describe which components of the intervention were delivered, where they were delivered and over what time.
The findings presented in the published paper are both methodological and substantive. The paper provides a consolidated version of the core programme theory, with illustrative examples. A full overview of all the core programme theories examined and not included in the published paper are provided in Report Supplementary Material 4.
Key learning from the formative process evaluation led to direct modifications to the intervention and adjustments to IDP resources to support practitioner teams. The direct modifications included the following:
-
Emphasising the importance of engagement and building a trusting relationship.
-
Activating trust mechanisms (e.g. feeling cared for) as an important mechanism for undertaking meaningful goal-setting.
-
A reinforcement of the importance of ‘quick wins’ for activating trust mechanisms (i.e. the practitioner delivering something for them that may seem small but is of significance to the participant and gives a concrete demonstration of help).
-
The need for a more protocolised sharing of the written plan with the participant and other services at release to help galvanise resources to support personalised goals.
-
Highlighting the difficulties of balancing the competing demands of immediate (often social, but sometimes emotional) crises and working towards longer-term goals.
-
Practitioners needing to anticipate barriers and also respond flexibly when crises emerged.
Adjustments to IDP included the following:
-
The addition of a ‘content of the manual’ session to the training to ensure consistent practice delivery.
-
The need for clearer and more consistent risk assessment processes and support for practitioners in making risk assessments from team supervisors.
-
The need to specify the expected content of the supervision process more clearly. The theory of supervision needed to focus on mechanisms that would develop practitioner competencies to deliver the intervention as intended.
-
The need for a more robust team structure and management at each site, including re-emphasising the importance of joint decision-making and meeting together regularly to reflect on cases.
-
The need to add a section to the manual about practitioners taking care of their own emotional well-being.
Intervention delivery platform: rapid realist review
In recognition of the importance of effective implementation and delivery of complex interventions in challenging contexts, an IDP was developed as a means of supporting practitioners to deliver the intervention as intended. The IDP incorporated training, a manual, supervision and organisational support. Having previously conducted the realist formative process evaluation41 with evidence from the organisational case studies, the research team acknowledged that they lacked adequate, relevant knowledge about intervention implementation. Rather than conducting a second realist review, we decided to use our existing realist review resource to deepen our understanding of relevant implementation issues and supportive strategies.
Studies were identified from the search conducted for the realist review. The flow of sources through the IDP review and information about the 29 included sources are shown in Report Supplementary Material 5. We used the Consolidated Framework for Implementation Research36 as a framework for structuring our identification and synthesis of evidence, and these findings are also shown in Report Supplementary Material 5.
This rapid realist review synthesised knowledge from a wider literature about complex implementation issues. This enabled us to go beyond simple descriptions of ‘practitioners’ experiences’ to provide a sounder, contextually refined foundation on which to base implementation activities. Although the review was not decisive on any one aspect of the implementation strategy, across the board it played a significant role in supporting emerging findings from other parts of the research programme. For example, working iteratively with the formative process evaluation, the review identified the importance of the manual catering for different learning styles and describing the intervention in ways that aligned with existing service design. The review also informed our understanding of how supervision should be delivered in a way that is theoretically consistent with the intervention. Some parts of the review simply played a supportive role, for example by alerting us to areas where there was scant existing research evidence or insufficient detail in the published evidence, and this was particularly the case for organisational agreements. The requirement for these organisational agreements became evident in discussions with practitioners and managers during set-up and delivery, and the agreements were necessary in order to put in place the formal clinical governance requirements that would enable teams to operate under research conditions but within NHS and voluntary sector services.
After the formative evaluation, the IDP was strengthened through acknowledging the need for top-up training and additional supervision for mentalisation. A decision was made to combine the role of Engager team leader and supervisor to create coherence and promote decisions in the local setting, taking into consideration the whole caseload and workload, as well as fidelity to the model for each individual (see Report Supplementary Material 3 for our developing theory of supervision).
The Engager model going into the trial
At this point, the results of the realist formative process evaluation and of the realist review of implementation literature, plus synthesis 1, were brought together in a second round of synthesis (i.e. synthesis 2). This synthesis was to inform the intervention theory (i.e. what practitioners do and why) and the IDP (i.e. training, manual and supervision), which would be then operationalised in the main trial.
Details of synthesis 2 are detailed in Report Supplementary Material 2.
There are several ways of gaining a description of the Engager intervention in addition to what is already presented:
-
Box 2 describes the key elements and rationale behind the intervention theory going into the main trial.
-
Report Supplementary Material 6 describes the details of the practitioners, training and supervision arrangements in place going into the trial.
-
The Engager programme provides a link for requesting a copy of the trial version of the Engager manual (URL: www.plymouth.ac.uk/research/primarycare/criminal-justice/engager; accessed 9 June 2022).
The intervention was originally conceived to be an adaptation of collaborative care intervention proven to be effective for individuals with depression. The principles of collaborative care – a psychological intervention, joint working between professionals and case-based supervision – were extended on the basis of the findings of the realist review and case studies to incorporate flexibility of delivery and practitioner behaviours to overcome distrust; co-ordination across all services involved in an individual’s care and continuity with a single practitioner, if possible; engagement in prison; meeting on the day of release; and continued care for 3–5 months following release.
Specific evidence-informed mental health and psychological therapy components were included. Early on, a MBA was selected as the supportive psychological method most likely able to assist practitioners in dealing with emotional lability (an aspect of personality disorder) and to help them to understand different perspectives and support psychological thinking. A generic approach to psychological formulation was taken, and simplified, as a shared understanding and action plan to be comprehensible for support workers with limited training and offenders with limited capacities. The shared understanding aims to understand the links for the individual between emotions, thinking, behaviour and current situation. The aim was to identify the means to enhance positive behaviours and to reduce negative ones, such as substance use, self-harm and aggressive behaviour.
The concept of the plan was also extended beyond what services could deliver to bring together all the relevant available resources to address those goals individuals had selected as the most important. Resources included not just the therapeutic support of practitioners, but the potential support of other teams, friends and family and the individual’s own personal resources for self-care. Finally, the concept of ‘discharge’ was transformed into the possibility of next steps, either alone or supported by other services.
Development of trial methodology (phase 1, workstreams 2 and 4)
Conducting RCTs in prisons presents numerous practical and methodological challenges. Simply gaining access to prisons to conduct research and to deliver an intervention can be a difficult and lengthy process. There are uncertainties about the number of people who might be eligible to participate, the level of acceptability and the level of compliance with the intervention and research procedures. There are additional challenges when trying to follow up recently released prisoners in the community. Low retention rates are a common problem for studies that involve following up recently released prisoners. 28 Our preparatory work for the programme demonstrated our ability to follow up 65% of released prisoners at 3 months after release. 29 Some people experience homelessness when released from prison, and for people who do have accommodation this is often temporary, which makes contacting them post release difficult. Even when researchers are able to contact people after release, people need to be willing to meet up with a researcher, answer questions and complete outcome measures. There are also fundamental uncertainties about how to measure the effectiveness of a complex intervention, as this population frequently has a complex array of inter-related problems. Therefore, it is not clear which problems are the most important, which should be the target of an intervention and, once these are decided, how to measure them as outcomes in the context of a RCT.
When the Engager team began this programme of work, there were, to the best of our knowledge, no published studies of evaluations of through-the-gate mental health interventions for incarcerated men with common mental health problems. Therefore, alongside the intervention development work in workstream 1, we conducted a separate workstream to develop the trial science methodology to evaluate the intervention.
This work programme aimed to address the following methodological questions:
-
What outcome measures should be used to evaluate a through-the-gate intervention for incarcerated men with common mental health problems?
-
What trial procedures are required to deliver a RCT of a through-the-gate intervention for incarcerated men with common mental health problems?
-
How can we measure the process of care of a collaborative care intervention designed to support incarcerated men with common mental health problems near to, and following, release from prison?
Addressing these questions in the first phase of the programme was a prerequisite for continuing to a full trial. Specifically, to proceed to a full trial we needed to demonstrate that we could achieve a follow-up of at least 50% and also demonstrate intervention acceptability in a pilot trial.
Development of a set of outcomes for a randomised controlled trial to evaluate the effectiveness of the Engager intervention
Our aim was to select a set of outcome measures that captured the most important areas of outcome using measures that were acceptable to the target population and, as far as possible, met scientific validity criteria.
We adopted a four-stage approach, involving:
-
a single-round Delphi survey to identify the most important outcome domains
-
a focused review to identify potentially suitable measures within the three most highly rated outcome domains
-
testing of these measures in the target population to assess acceptability and the psychometric viability of the measures43
-
a consensus panel meeting to select the primary outcome measure for the RCT and key secondary outcome measures.
More detailed description of these stages can be found in Report Supplementary Material 7.
We actively sought the input of our Peer Research Group, with 10 members of the group completing the Delphi survey and four members of the group attending the consensus meeting.
In the single-round Delphi exercise, although the most important areas that people thought we should be capturing outcome data for were mental health symptoms, substance misuse and social inclusion, many of the other outcome domains were rated as important. Although the outcomes of this exercise were clear and, we believed, unlikely to change much in a second round, we recognised that not all outcome domains would be relevant to all participants or amenable to change through an intervention.
To address this, we tested using a measure that captured outcomes across multiple domains and two measures that captured personalised goals. Specifically, we included the Camberwell Assessment of Need – Forensic Version (CAN-FOR),44 which captured outcomes across multiple domains and has been used as a composite measure for offenders with mental health problems. We also included the PSYCHLOPS measure45 and the Goal Attainment Scale (GAS),46 both of which allow the participants to specify personalised goals and, therefore, enabled the capturing of idiographic outcomes that were not specific to one domain.
When we tested potential measures on men in prison who were close to release, we found that we were unable to identify a measure of social inclusion that had the psychometric properties necessary to be included as an outcome measure in the RCT. The use of PSYCHLOPS was problematic in that participants tended to identify problems that were primarily due to their situation of being in prison, and these problems no longer existed once they had been released. Similarly, the GAS was also problematic in that goals were often poorly specified and, therefore, measuring change in a systematic and standardised way at follow-up was difficult. Consequently, PSYCHLOPS and the GAS were not included in our considerations for the primary or secondary outcome measures.
At the consensus meeting, we first discussed measures by domain before focusing on the primary outcome. Of the measures tested within the mental health symptom domain, the Clinical Outcomes in Routine Evaluation – Outcome Measure (CORE-OM)47 was selected as the preferred measure over the General Health Questionnaire-1248 because of its wider range of constructs. The Patient Health Questionnaire-949 and General Anxiety Disorder-750 were not selected as many individuals were subthreshold on one or the other measure. The data we collected using the CAN-FOR also indicated that it would be a psychometrically viable option to be included as an outcome measure. No other composite measures were considered.
Two-thirds of participants reported having a substance misuse problem and, although it was decided that a substance misuse measure should not be the primary outcome, two short measures were included as secondary outcomes, with one capturing information on which substances were being used and the other capturing level of dependence.
After discussion about outcome measure criteria for trials and close reading of the measures, and with peer researchers supported to ask questions, the CORE-OM and CAN-FOR received the same number of votes to be the primary outcome measure. We opted for the CORE-OM as the primary outcome measure, as it had marginally superior psychometric properties and could be administered in a highly scripted fashion that would reduce researcher bias.
The four-stage process we conducted, incorporating the opinions of our Peer Research Group, enabled us to be confident that the outcome measures we selected focused on important areas of outcome and were acceptable to our target population. The outcome measures also demonstrated psychometric properties that indicated that they would be suitable for evaluating the effectiveness of the Engager intervention. However, some questions arise on this latter point. None of the selected instruments was specifically designed for, or validated on, prison populations and, therefore, may not accurately reflect the acutely stressful effects of custodial environments. Moreover, the transition from custody to community may itself have a significant impact on mental health, perhaps ‘swamping’ effects brought about by the intervention. As most of our data testing was undertaken when the participants were still in prison, we did not establish the efficacy of the measures in community settings. Although the above are clearly limitations of this study, it should be added that trials are usually expected to use validated and established instruments, which greatly restricts choice, and that any trial measuring change ‘through the gate’ is likely to be complicated by recovery among both arms simply as a consequence of leaving prison.
Finally, we considered using outcomes based on practitioner records, such as those from the Offender Assessment System (OASys) and other assessments entered by offender managers on nDelius, the Probation Service case management system (URL: https://data.gov.uk/dataset/8dae5fb2-82a2-4232-ae79-87e9c9fcfe46/ndelius; accessed 1 August 2022). However, it quickly became clear that these records were not recorded in a sufficiently consistent way to merit inclusion: they were not undertaken at set time points, were often subjective in terms of focus and they suffered from missing data. Above all, mental health was an issue that received relatively little attention.
Development and piloting procedures for a randomised controlled trial
This work is published. 43
Alongside the work undertaken in selecting a set of outcomes, we piloted RCT procedures to test the feasibility of a larger RCT. A key objective was to demonstrate that we could achieve a retention rate of > 50% when following up participants at 3 months post release from prison. Additional aims of the pilot RCT were to test out trial procedures, such as recruitment, consent and randomisation, to assess the levels of participation with the intervention, to test our ability to maintain research blinding and to model workforce requirements for the research team for a larger trial.
We reviewed the records of 864 individuals and identified 182 records of individuals who met the initial eligibility criteria. Of these individuals, we screened 110 potential participants to identify 60 eligible participants who were randomised at a ratio of 2 : 1 to receive either the Engager intervention plus usual care (i.e. the intervention group) or usual care alone (i.e. the control group). We achieved follow-up rates of 73% at 1 month and 47% at 3 months post release from prison.
No participants withdrew from the trial between consent and up to, and including, the point of randomisation, indicating that the trial procedures relating to recruitment, screening and randomisation were acceptable. However, maintaining researcher blinding was problematic and by the time of the 1-month follow-up the researchers were aware of the allocation of practically every participant. This was usually a consequence of participants sharing their allocation with the researchers who they frequently came across in the closed prison environment.
There were very high levels of data collection and completion across all the measures used at baseline and at follow-up, with few missing data. However, during the pilot trial we were still testing a range of potential outcome measures to use in the full trial and, therefore, not all participants completed the same set of outcome measures. Given the relatively small number of participants that completed each set of outcomes, we were unable to establish whether the intervention was able to bring about change on the measures, and whether or not such a change would be discernible over and above any change in scores that may have been due to whether the participants were in prison or the community. This issue was a key limitation of the pilot trial.
With regard to intervention acceptability, 90% of participants allocated to the intervention group received some of the intervention. Of the four participants who did not receive any intervention, three were either released or transferred to another prison before being seen by a practitioner and one decided the intervention was not for him prior to having contact with the practitioners. Of the 36 participants who did receive the intervention, 28 met with their practitioners in the community following their release from prison. There was strong indication that receiving support on the day of release led to ongoing contact in the community.
Overall, we found the trial procedures and intervention to be feasible to deliver, as well as acceptable to participants. With regard to contamination between the intervention and usual care, we found no evidence of this and, as the Engager practitioners were a stand-alone team, with many not working within the prison prior to the Engager intervention, there was little risk of contamination. The one major exception was in maintaining researcher blinding, which was a problem that was almost universal at both sites. We considered possible solutions to this problem, but it was felt that any solution created potentially more challenging problems. For example, we considered using a different researcher to collect data at follow-up, but felt that this might have a negative impact on follow-up rates, as participants may not be willing to meet a researcher they had not built up trust and rapport with. Ultimately, we opted to accept that unblinding would occur in the trial and to focus attention on reducing biases by training researchers to apply measures consistently, while continuing to allow flexibility for the whole schedule.
The retention rate for the 3-month follow-up was 46%, which was lower than hoped. To address this for the full trial, we broadened the window of time during which follow-ups could be completed. Participants often led chaotic lives and were very difficult to contact for periods of time and so it was felt that giving researchers longer to make contact with and meet participants in the community would increase the follow-up rate. In addition, we also decided to offer ‘thank you’ vouchers to compensate participants for their time when we interviewed them in the community, and we received approval from the Ministry of Justice to do this. Last, many of the participants worked with a range of services on their release from prison, and the introduction of the community rehabilitation companies (around the time of the pilot trial) meant that all people leaving prison were to be provided with support from probation for 12 months following their release. We developed closer working practices with services in the community, including establishing information-sharing agreements, to help researchers contact participants in the community.
The whole of the feasibility study also allowed us to test and develop the intervention and to model researcher workforce requirements and recruitment rates for small or more extensive geographical follow-up areas and different participant eligibility criteria, and this was critical for both assessing viability of and planning for the full trial.
Developing a process of care framework
In addition to developing a set of outcome measures for a RCT to evaluate the Engager intervention, we sought to develop a framework for capturing the care that prisoners received during their participation in the trial from the Engager intervention and standard services. A detailed description of the work we undertook in developing methods to capture the process of care is provided in Report Supplementary Material 8.
Measuring routine care
We recognised that the RCT was going to take place at a time of considerable change within the probation service, as well as at a time of ongoing changes in the NHS environment. Therefore, it was also important to capture what ‘usual care’ comprised. One of the key components of the Engager intervention was to support participants to work with services that could help them work towards achieving their goals. This might involve the Engager practitioners identifying appropriate organisations, liaising with those organisations and supporting the participant in meeting with those organisations. Therefore, it was anticipated that the Engager intervention could increase the amount of care received from other organisations and, potentially, improve the effectiveness of that care in meeting the participants’ needs.
To capture the care received from organisations, we adapted the service use elements of the Client Service Receipt Inventory. 51 Specifically, we expanded the list of organisations to include third-sector organisations and organisations providing social support (e.g. accommodation, employment and benefits). To help participants recall the services they had been in contact with, we split the services up by the type of service and asked about each type of service contact at relevant points in the interview schedule. For example, service use relating to accommodation was captured immediately after asking participants about their current accommodation situation and level of need in relation to accommodation. This also created a more coherent conversation and reduced annoyance induced by revisiting topics.
In addition, we included questions on how helpful the contact with each organisation was as a proxy measure of the effectiveness of the support received from each organisation. We asked participants about who initiated contact with each organisation (e.g. self, CJS, health service or the Engager practitioner) to provide an indication of how much service contact was initiated by the Engager practitioner.
Last, we asked participants to complete the Brief Inspire,52 which is a tool designed to assess a service user’s experience of the support they receive. We supplemented the five questions used in the Brief Inspire with a further nine items that were identified in workstream 1 as important for participants to have a good experience with a service (e.g. participants can trust the service and participants feel that the service listens to them). Although participants were likely to engage with many services, we decided to ask participants to provide ratings of their experiences of working with services in general, using the Brief Inspire to reduce participant burden.
Quantifying care from the Engager intervention
We sought to capture the amount of support participants received from the Engager practitioner and information regarding the response to this support. This was important to assess fidelity to the intervention and in understanding whether or not the intervention worked in the way we anticipated from the logic model. 41
To capture the process of care provided by the Engager practitioners, we developed a range of tools. First, to capture the amount (i.e. extent and dose) of contact between participants and the Engager practitioners, practitioners were asked to complete timesheets detailing every contact they had with the participant, providing details of the length of each contact and the location (i.e. prison or community). In addition, the Engager practitioners wrote clinical notes for each session they had with participants. The notes acted as a confirmation of the information recorded in the timesheets and provided details of the nature of the meetings between the practitioner and participant, as well as which components of the intervention were delivered (e.g. practical or psychological).
Last, to capture information regarding which components of the intervention were delivered, and whether or not they had the intended consequences, we developed a series of ‘if–then’ statements. The ‘if’ statement captured information relating to how often a component was delivered and the ‘then’ statement captured the extent to which it had its intended consequence, according to the Engager programme theory. The ‘if–then’ statements were rated by practitioners for each participant they had on their caseload, and were also rated by each participant. More expansive qualitative comments were also recorded.
The programmatic nature of the grant allowed us to focus on developing bespoke ways of capturing usual care and intervention content, which is required both for interpretation of the trial and understanding the way in which the intervention might work. However, such development work often requires iterative mixed-methods approaches and we were not able to fully test and refine the measures for the Engager intervention.
Economic modelling
This part of the economic analyses comprised conceptual model development, decision model specification and assessment of the feasibility of conducting estimated value of perfect information analysis (see Report Supplementary Material 10).
Development and testing of a simulation model to estimate the outcomes of the Engager intervention
A discrete event simulation model of the short-term outcomes and costs of the Engager intervention was developed based on (1) two previous relevant models (i.e. the revolving doors agency financial analysis model53 and the Home Office’s model for the economic and social costs of crime54) and (2) a systematic review of economic evaluations and cost-of-illness studies relating to the commonly overlapping problems that many prisoners and ex-prisoners face, such as drug or alcohol misuse. For both treatment strategies, that is, the Engager intervention and usual care, the model simulates an individual’s pathway through different events, recording the events experienced and calculating the total costs and outcomes associated with that pathway. The model assumed that prisoners had 4 months in prison before release, and then incorporated contact with health services in the community, medications, non-fatal self-harm events and deaths.
For people receiving the Engager intervention, there would be a probability of an improvement in mental health within prison once treatment with the Engager intervention started. After release from prison, there would be an increase in the probability of planned contact with health services (with probabilities differing depending on the type of health service) and a subsequent decrease in the probability of unplanned contact with services.
Modelled outcomes
This initial stage of modelling was based on a model with service use for mental health and drug misuse, as well as general practitioner (general practice) attendances in the pilot work. The challenges of obtaining and using data that could potentially be available from the full trial to enable these basic models to generate plausible cost and cost-effectiveness were expected to be considerable. The challenges would certainly prevent the possibility of the kinds of cross-sectoral estimated value of perfect information analysis that were originally planned. Along with the shift to a definitive RCT, the challenges informed the decision to make the economic evaluation of the main trial a combination of three cost-effectiveness analyses (using the three main trial outcomes) alongside a cost–consequence analysis.
Evaluation of Engager: randomised controlled trial and cost-effectiveness analysis (phase 2, workstreams 3 and 4)
Randomised controlled trial
The results of the RCT have been published. 55 To date, there has been a dearth of research developing and evaluating mental health interventions for prison leavers. 27 Trials within prison settings are particularly challenging to undertake because of a range of factors, such as organisational difficulties, maintaining masking, poor follow-up rates and selecting appropriate outcomes measures. 1,17,28–30
Design
The individually randomised superiority trial of the Engager intervention was set in three prisons (south-west of England, n = 2; north-west of England, n = 1) and nearby communities between 2016 and 2019.
To detect a change of 3.5 units for the primary outcome measure (i.e. CORE-OM43) with 90% power and a significance threshold of 0.05, assuming a standard deviation (SD) of 7.556 and allowing for 30% attrition, 280 participants were recruited and randomised [1 : 1 allocation; stratified by site (i.e. Devon or Manchester)] to either the Engager intervention plus usual care (n = 140) or usual care only (n = 140).
Intervention
The Engager intervention was a manualised person-centred intervention that aimed to address mental health needs, as well as to support wider issues, such as accommodation, education, social relationships and money management. Experienced support workers and a supervisor with experience of psychological therapy delivered the Engager intervention. A mentalisation-informed approach underpinned all elements of the intervention. At the pre-release stage, the practitioner and participant developed a shared understanding of the participant’s needs and goals, recognising the links between emotion, thinking, behaviour and social outcomes. A goal attainment plan was developed and followed, including liaison with relevant agencies and the participant’s social networks.
Engagement was maintained throughout the pre-release period and, when required, all-day support was given on the release day. Following release, the practitioner provided support for the participant to re-enter the community and engage with services. The practitioner continued to work with the participant and any relevant organisations to help them achieve their goals, while encouraging the participant to take responsibility for self-care. The practitioner also prepared the participant for the end of the intervention, while liaising with relevant community organisations regarding continuity of care.
Participants
Individuals recruited into the trial needed to be released to defined geographical areas and were required to score ≥ 10 points on the Patient Health Questionnaire-949 to indicate depression, ≥ 10 points on the General Anxiety Disorder-750 to indicate anxiety or score ≥ 3 points on a bespoke questionnaire to indicate likelihood of difficulties on release. Those individuals with psychosis under the care of prison in reach teams or part of the personality disorder service were excluded. All participants were assessed at six time points, that is, at baseline (before randomisation), during the week before release from prison, and then at 1, 3, 6 and 12 months post release from prison.
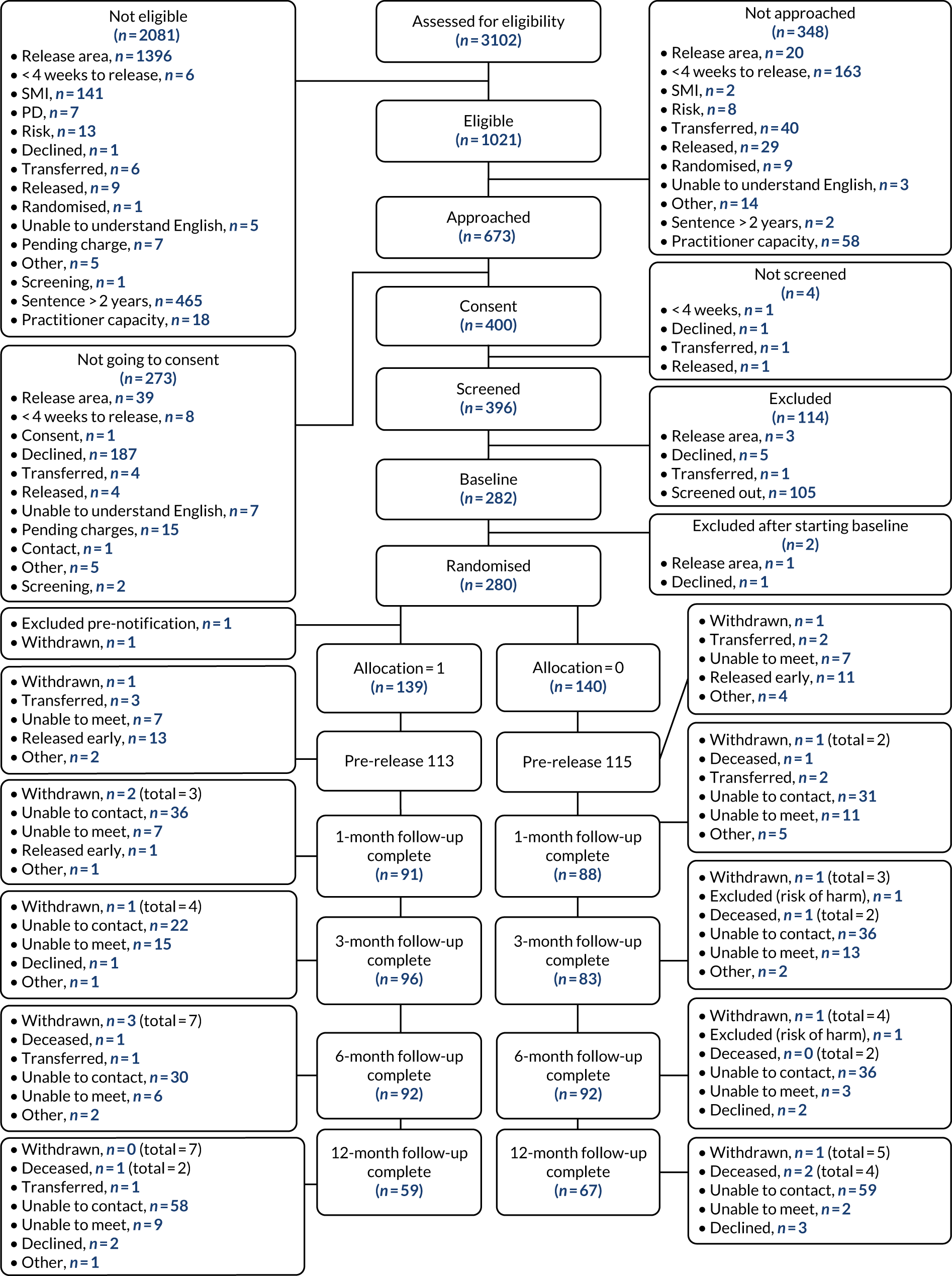
A total of 3102 prisoners received assessment for eligibility. Of these prisoners, 673 were identified as potentially eligible for the trial and approached for consent. One hundred and eighty-seven of the 673 prisoners declined involvement and a further 90 prisoners were found not to be eligible or were excluded for other reasons, leaving 396 prisoners to be screened for common mental health problems. Of these prisoners, 78% were found to be eligible and, therefore, selected to take part. After a small number of withdrawals, the 280 prisoners who remained were randomised into two groups of 140. Figure 4 depicts the CONSORT (Consolidated Standards of Reporting Trials) diagram.
FIGURE 4.
A CONSORT flow diagram. Reproduced with permission from Byng et al. 55 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
Analysis
Demographic data and participant characteristics were reported descriptively at baseline, using mean and SD, with median and minimum and maximum, as appropriate, for continuous measures, and percentages for categorical measures.
For the primary analyses of the outcome variables, the intention-to-treat principle was used, with participants being analysed according to their randomised allocation irrespective of treatment actually received. Only participants with observed data were included for the primary analyses. Primary analyses used linear regression models for continuous outcomes and logistic models for binary outcomes.
Sensitivity analyses were performed for comparison with the primary analyses, that is, per-protocol analysis, complier-average causal effect analysis and inclusion of only those participants whose follow-up assessments took place within the specified ‘window’. The definition of per protocol for the Engager intervention plus usual-care group was receipt of at least two contacts prior to initial release and at least eight contacts following initial release. As a secondary analysis, mixed-effects models (random effect on participant intercept) were performed including participants with data available at any of the four follow-up time points. Results of all inferential analyses were reported as between-group differences with 95% confidence intervals (CIs). Global p-values were also provided with regard to categorical explanatory variables. The threshold for determining significant effects was set at p < 0.05. No adjustment of p-values was made in the light of multiple testing.
All analyses were adjusted for baseline values of continuous outcomes and study site. Baseline participant characteristics were to be compared by treatment group, with any covariates found to be unbalanced included in the analyses if thought to be predictive of outcome.
For the CORE-OM at 6- and 12-month follow-up, we investigated interactions (i.e. moderation effects) between intervention and specific participant characteristics, including study site, personality disorder (based on the Standardised Assessment of Personality – Abbreviated Scale), previous trauma, pre-prison accommodation and alcohol/substance abuse. Further sensitivity analyses were performed to address missing data, based on the assumption that missing data were missing at random. The level of missingness for the CORE-OM was evaluated, with 55% of participants found to have missing data at 12 months. Sensitivity analyses were performed using combined observed and imputed data.
Results
There were some imbalances between the two groups at baseline. The Engager intervention group had a higher proportion of people with unstable accommodation [n = 76 (54%) vs. n = 58 (41%)], a higher proportion of people who were unemployed [n = 104 (75%) vs. n = 85 (61%)] and a higher proportion of people with physical health problems [n = 64 (45%) vs. n = 48 (34%)]. A higher proportion of people in the usual-care group had experienced relational trauma [n = 89 (64%) vs. n = 74 (53%)]. At 6 months, 184 (66%) participants were followed up, with 45% of participants followed up at 12 months.
There were between-group imbalances in participant characteristics at baseline for type of accommodation (people in the usual-care group had more stable accommodation before prison), employment (people in the usual-care group were more likely to be employed), previous trauma (people in the usual-care group had experienced more relational trauma) and physical health problems (people in the usual-care group had fewer problems). Therefore, these characteristics were included as covariates in all analyses.
Of 140 participants allocated to the intervention, 92% received at least one session in prison [mean 5.7 (SD 3.9)] and 108 (77%) participants received at least one post-release community session [mean 12.9 (SD 11.6)].
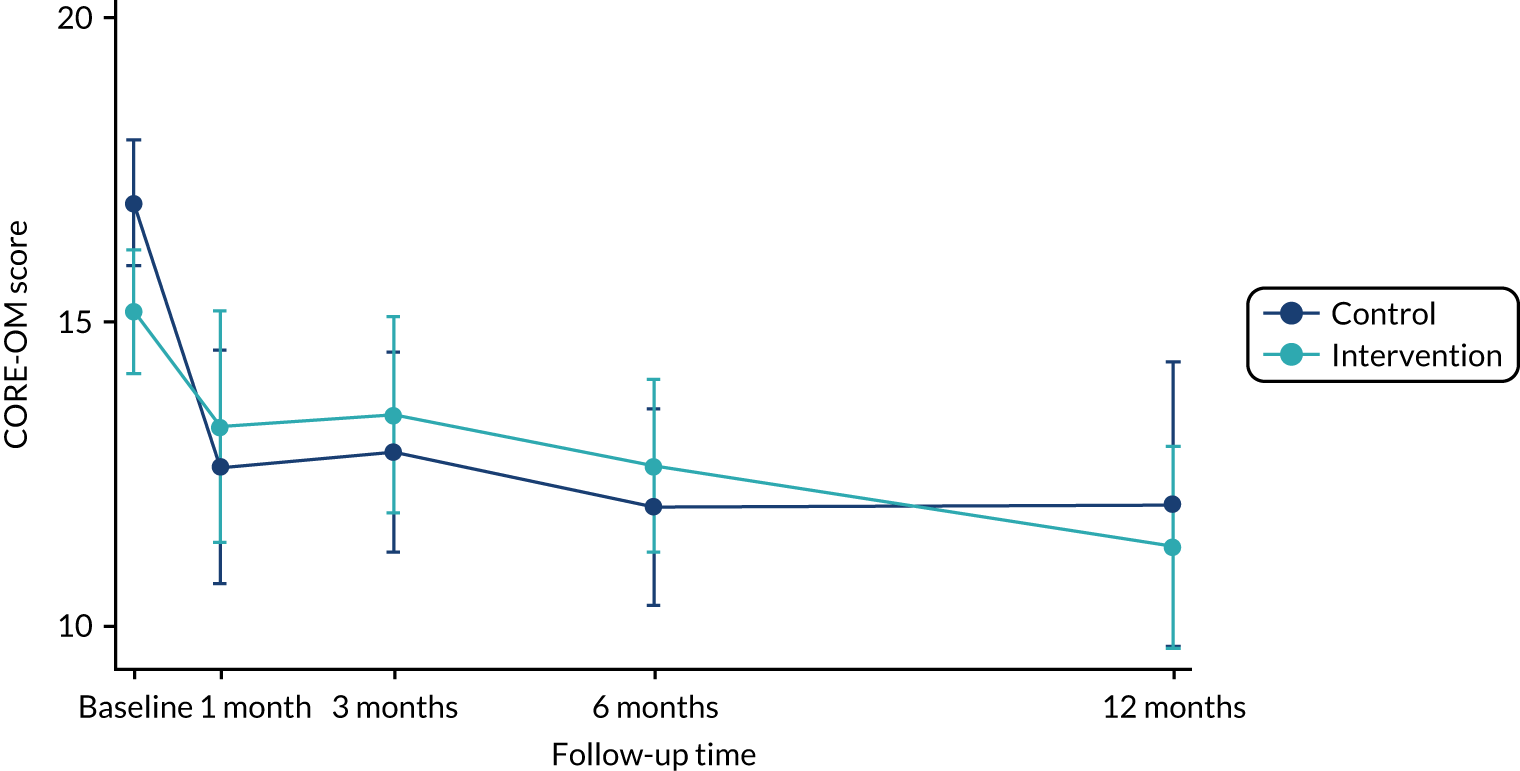
There were no significant differences in mean CORE-OM (primary outcome) scores between the groups at 6 months [Engager intervention group mean 12.6 (SD 6.9), n = 92; usual-care group mean 11.9 (SD = 7.7), n = 90; between-group difference 1.1 (95% CI –1.1 to 3.2); p-value 0.325]. Figure 5 depicts the change in CORE-OM score over the four time points.
FIGURE 5.
Graph of CORE-OM score over time. Reproduced with permission from Byng et al. 55 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
There were a small number of statistically significant differences between the two groups on the secondary outcomes [including CAN-FOR, Intermediate Outcomes Measurement Instrument, EuroQol-5 Dimensions, five-level version (EQ-5D-5L) and ICEpop CAPability measure for Adults (ICECAP-A)] for a variety of sensitivity analyses (i.e. complier-average causal effect and per protocol), but this is most likely due to the effects of multiple testing. At the time of writing, it had still not been possible to obtain Police National Computer data on reoffending.
Further exploratory analysis
After our neutral finding was revealed and the baseline imbalances were identified, we carried out some further exploratory analyses to rule out or put forward any contributing factors or possible explanations for the neutral finding. The details of this exploratory analysis are found in Report Supplementary Material 9. We found imbalances in CORE-OM scores at baseline, with the Engager intervention group scoring as less mentally unwell (mean 15.2 vs. 16.9). It is possible that the people in the usual-care group were more willing to acknowledge their common mental health problems or may have struggled with being in prison but may have had less social disadvantage on release into the community. Conversely, people in the Engager intervention group may be less likely to report their difficulties in the prison environment, as they may not wish to show their vulnerabilities.
We identified that the mean scores for the CORE-OM dropped differentially over time, depending on which trial arm participants were in and whether or not the participants were serving a new prison sentence at time of follow-up.
Health economic analyses
We conducted a trial-based economic evaluation to identify the mean incremental cost per quality-adjusted life-year (QALY) gained with the Engager intervention compared with current practice. Report Supplementary Material 10 describes in detail the health economics modelling, and the results of the health economic analyses are published. 57
The cost of the Engager intervention included the cost of training and supervision based on practitioner-reported activities. As a conservative estimate, the cost per participant of training and supervision was calculated as the total cost of training and supervision for the Engager trial divided by the number of participants in the intervention arm of the trial.
Unit costs for accommodation-, education-, training-, employment-, money-, relationship- and criminal justice-related service use are reported in Hunter et al. 57 table 1. All costs are reported in 2017/18 GBP (i.e. the most recent year costing data were available), with costs for earlier years adjusted to 2017/18 values.
The trial primary outcome CORE-OM was converted to the Clinical Outcomes in Routine Evaluation – 6D (CORE-6D) utility to calculate QALYs. QALYs were calculated as the area under the curve using the CORE-6D responses at baseline and at 1, 3, 6 and 12 months post release. QALYs were also calculated and reported in a similar manner using responses to the EQ-5D-5L at baseline and at 3, 6 and 12 months post release and (1) the mapping algorithm and (2) the EQ-5D-5L value set. Years of full capability (YFCs) (equivalent) were calculated for the Engager intervention compared with usual care using patient-level responses to the ICECAP-A at baseline and at 3, 6 and 12 months post release.
We assumed that data missing at follow-up were missing at random. No predictors of ‘missingness’ were found. Costs, utility scores and the ICECAP-A tariff were imputed for the number of 30 data sets using chained equations [i.e. multiple imputation using chained equations (MICE)] and predictive mean matching.
For the incremental cost-effectiveness ratio, we used regression to account for the correlation between costs and outcomes to calculate the incremental mean cost per QALY or per YFC gained of the Engager intervention compared with usual care. The primary analysis was calculated using the multiple imputation data set and was bootstrapped. The incremental mean cost per QALY and per YFC were used to calculate cost-effectiveness acceptability curves and cost-effectiveness planes. A range of sensitivity analyses and a cost–consequences analysis were also conducted.
The total cost of training and supervision for the duration of the Engager trial was £59,303. If the total cost of the training and supervision is divided by the 140 participants randomised to the intervention, then the training and supervision cost was £424 per participant. The total average cost per participant of delivering all intervention sessions (i.e. prison, meeting at the gate and community) was £467 (SD £475). When the cost of training and supervision is added, then this results in an average cost per participant in the Engager arm of £891.
Descriptive statistics for CORE-6D, EQ-5D-5L (cross-walk and time trade-off tariff) and ICECAP-A tariff are reported. 57 There were no significant differences between trial arms.
The bias-corrected bootstrapped difference in health-care costs, adjusting for baseline, of the Engager intervention compared with usual care is £751 (95% CI –£1593 to £3096). When the cost of the Engager intervention is added (including the cost of training and supervision), the difference in costs is £1795 (95% CI –£575 to £4164). The cost difference for CJS costs including the cost of the intervention is £8166 (95% CI £1692 to £14,640). If productivity gains/losses are included, then the cost difference is £5344 (95% CI –£1228 to £11,916).
For the primary economic evaluation (i.e. a health and social care cost perspective, QALYs calculated from the CORE-6D and using MICE for missing data), the mean cost difference was £2133 (95% of iterations between £997 to £3374) and mean QALY was a difference of –0.017 (95% of iterations between –0.042 to 0.007) and, therefore, the Engager intervention is less effective and more costly than usual care. The cost-effectiveness plane is shown in Figure 6. There is a 0% probability that the intervention is cost-effective at the £20,000–30,000 willingness-to-pay threshold for a QALY gained (i.e. the standard willingness-to-pay threshold for recommending treatments for the NHS).
FIGURE 6.
Cost-effectiveness plane of the Engager intervention compared with usual care from a health and social care cost perspective over 12 months.
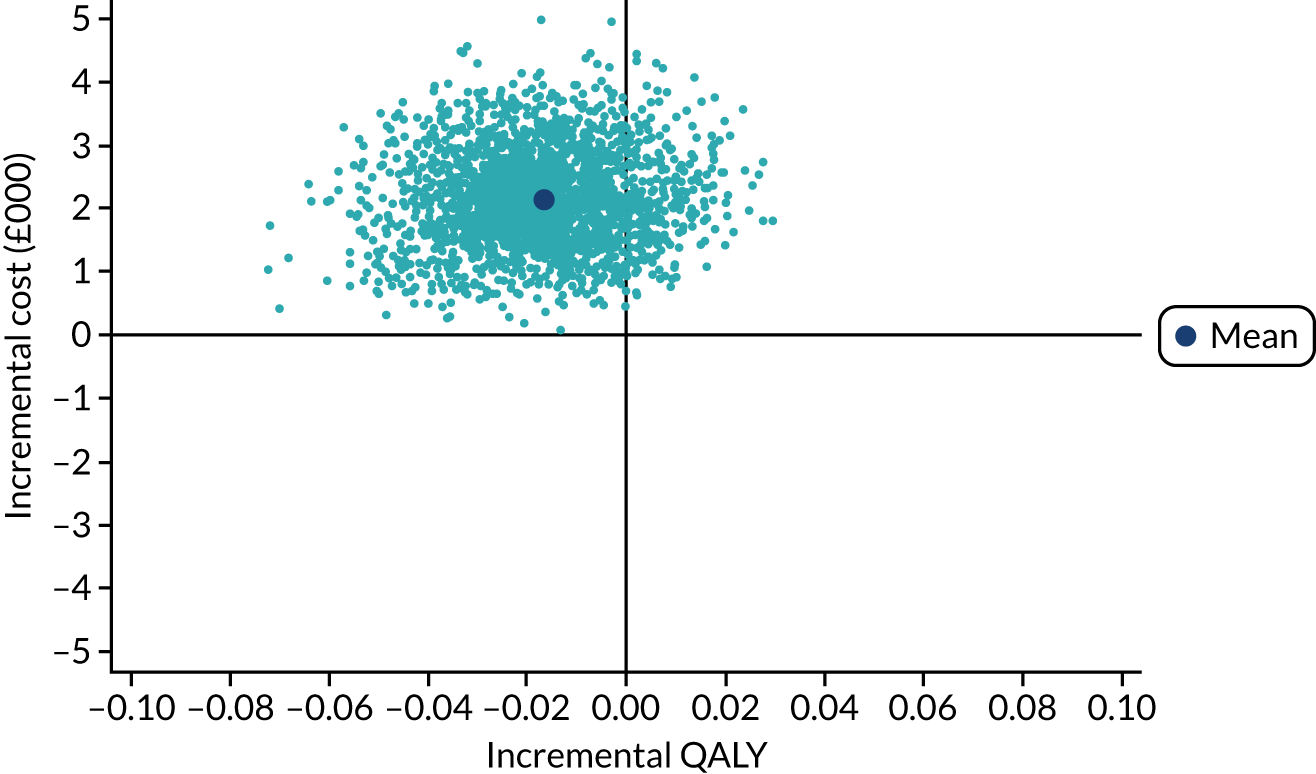
The Engager intervention had a very low probability of being cost-effective and this was the case across all secondary and sensitivity analyses. The Engager intervention group cost significantly more from a health service perspective, and had higher CJS costs. On the other hand, the Engager intervention group also showed greater productivity gains, although caution should be taken in interpreting these results, particularly given the number of analyses run. Very few cost-effectiveness analyses are carried out in CJS settings, with self-reported outcomes in this group being particularly hard to collect because of this population’s transient nature. This trial demonstrates the complexity of economic evaluations in this area and represents a significant contribution to the health economic evidence base for this population group.
Engager evaluation: parallel process evaluation (phase 2, workstream 3)
The objectives of the mixed-methods process evaluation, with data collected in parallel to the trial, were to:
-
determine the extent to which the intervention was delivered as outlined in the Engager manual
-
evaluate the extent to which the core components and mechanisms of the intervention produced the intended outcomes
-
support the interpretation of the RCT
-
identify aspects of the intervention and delivery that could be improved
-
explore unintended consequences of the intervention
-
understand how to deliver the intervention in real-world settings (including training, supervision, meta-supervision).
The process evaluation carried out the following analyses:
-
A fidelity analysis that quantified the extent of the intervention delivery.
-
A thematic analysis that demonstrated the wider issues that may have supported or inhibited the delivery of the intervention.
-
An analysis of the extent to which individuals and practitioners experienced the intervention components as having been delivered and having a positive impact.
-
A realist-informed in-depth case study analysis that explored:
-
how the quality of delivery of various components of the intervention related to individual responses
-
how key outcomes were or were not generated through practitioner activity.
-
Each analysis is summarised below. Data were collected from a range of sources and a table detailing which data sources were used for each analysis is shown in Report Supplementary Material 11.
Fidelity analysis
More detail on the fidelity analysis can be found in Report Supplementary Material 12.
The fidelity analysis aimed to quantify the extent to which the intervention was delivered as hypothesised. The primary objectives were to examine (1) adherence to delivery of the components of the intervention, as specified in the logic model, and (2) delivery of the team model throughout the trial. Data were extracted from practitioner logs and records for 129 of the 140 intervention participants. We were able to identify participants who had received the minimum dose of the intervention thought necessary for impact (i.e. two prison sessions and eight community sessions) and the extent of delivery for other participants.
Less than half (n = 62, 48%) of the participants received the minimum dose and just over one-third (n = 48, 36%) of the participants received any release day contact. Variations in intervention delivery were observed across sites. Information on the content of sessions was available for 45% (n = 332) of prison sessions and 47% (n = 701) of community sessions. Based on the content of records, just over two-thirds (67%) of the sessions were assessed as practically focused (e.g. focused on housing issues), 23% contained both practical and therapeutic content and just 10% were predominantly of a therapeutic nature (e.g. focus on thoughts, feelings and behaviours).
Overall, the fidelity analysis based on records highlighted that intervention delivery was not as therapeutically focused as was intended. Staff turnover, long-term sickness and the prison context (e.g. regime and lockdowns) presented barriers to the planned team model delivery of the intervention.
Thematic analysis of barriers and facilitators
This thematic analysis aimed to explore the individual- and organisational-level barriers to and facilitators of intervention delivery and implementation. A full description of the methods and results can be found in Report Supplementary Material 13 and 14.
Five key cross-cutting themes were identified.
Perceived usefulness of Engager resources
A shorter version of the manual could have more effectively supported daily delivery. More regular training sessions tailored to the competency gaps of practitioners and focused on the most complex aspects of the intervention (e.g. MBA and shared understanding/action plan) could have improved quality of delivery.
Intrateam and interteam dynamics
Intervention delivery was compromised, at times, by long-term sickness, practitioner turnover and unhelpful team dynamics.
Individual contributions of practitioners and clients
Practitioners’ lack of experience in working with this client group, and in a psychologically informed way, limited their ability to deliver the intervention. Some participants were difficult to get hold of and hard to engage, and this influenced delivery.
Context within the prison and community
The prison environment was a volatile context to deliver the key values of the intervention. Outside the mandated atmosphere of the prison environment a chaotic community context, with participants less likely to attend appointments, was also often challenging for ongoing intervention delivery and for planning formal endings.
Extent of delivery and impact of key intervention components
This component of the process evaluation provided more granularity as to the extent to which intervention components were delivered and whether or not these had an impact. The development of the practitioner and participant perspective checklists are reported in Report Supplementary Material 11. The two ‘if–then’ checklists were based on the realist-informed programme theory and were used to record ‘if’ individual components of the intervention had been delivered and, as a result of that delivery, whether or not the hypothesised outcome had ‘then’ been achieved.
Data from the practitioner perspective were available for 121 out of 140 intervention participants; however, because of late introduction of this measure, low follow-up rates at 12 months and participant burden, data from the participant perspective are reported for only 35 participants. The key findings were as follows.
Trust and practical support
Practitioners reported that they treated participants with respect (n = 120, 99%) and showed that they cared by helping participants and offering practical support (n = 103, 85%), which led to participants having trust in practitioners in most cases (n = 96, 81%). All 35 participants reported that they felt respected, 32 (91%) said that practical support was given and 28 (86%) reported that this led to trust.
Mentalisation-based approach
Delivery of the key mentalisation techniques (i.e. stop/listen/look, micro-slicing, rewind) was reported by practitioners as being delivered regularly (n = 50, 40%) and as not being achieved at all (n = 33, 25%). When using strengths-based work, practitioners reported participants becoming more self-reliant in 38% (n = 45) of cases. Seventy-three per cent (n = 25) of participants reported that being able to talk through things meant that they were more able to understand their thoughts, feelings and behaviours, and 50% (n = 17) of participants said that it helped them to get on with others.
Resource mobilisation
Practitioners ‘always’ or ‘frequently’ liaised with other services to galvanise support in almost two-thirds of cases (n = 70, 58%). Practitioners reported that 53% (n = 61) of participants maintained engagement with other services as a result.
A positive ending
According to practitioners, less than half (n = 46, 45%) of the participants received support around ending the intervention, often due to loss of contact. However, of the 46% (n = 13) of participants who reported a planned ending, all said that they would be more able to continue working towards their goals after the Engager intervention ended.
Although there was greater practitioner than participant data completion, the multiperspectival approach contributed towards a degree of data triangulation by adding weight to the health records-based fidelity analysis that practitioners were empathic and provided practical support, but delivered psychological interventions less often.
Realist-informed case studies
Twenty-four longitudinal realist-informed in-depth case studies were conducted to examine how participants engaged and responded to intervention offers. Two papers reporting this part of the process evaluation have been published. 58,59 Report Supplementary Material 15 presents more details of the ‘if–then’ checklist and Report Supplementary Material 16 details the purposive sampling strategy that was used to select case study participants and provides an overview of the data collection strategy and interview schedules.
Typologies of engagement and response to the intervention
We showed that the intervention was delivered with varying degrees of fidelity. We identified five typologies of participants as follows.
Crises but coping
The participants in the ‘crises but coping’ group engage with the intervention and appreciate Engager intervention support, but continue to experience problems. The participant makes positive incremental changes over time, despite setbacks, leading to a better life situation. However, it is of note that the positive outcomes achieved by these individuals did not correlate with the standard measures when the case study outcomes and trial outcomes were compared after both analyses had been completed.
Resigned acceptance
Participants in the ‘resigned acceptance’ group initially engaged with the intervention, but problems and challenges continued and the participants became resigned that their circumstances would not change and concluded that they were not able to pursue goals.
Crises and in chaos
Participants in the ‘crises and in chaos’ group were unsure about their ability to make changes, but appreciated offers of support and initially engaged with the intervention. However, this was short-lived and was not accompanied by the development of a shared understanding. When confronted by problems and challenges, these participants soon became overwhelmed by their circumstances and disengaged from the intervention.
Wilful withdrawal
Participants in the ‘wilful withdrawal’ group declined support early on. These participants received minimal contact with their Engager practitioner in prison and so trust was never established.
Honeymoon
Participants in the ‘honeymoon’ group were motivated to make changes at the outset; however, soon after their release, they believed that they could manage without support. Therapeutic work was, therefore, ineffective as Engager practitioners appeared to struggle to challenge the overoptimistic participants to develop a realistic understanding of their ability to manage their situation. Subsequently, participants would hit crisis soon after release and would not be able to sustain motivation to pursue their goals.
Effect to cause analysis
We attempted to understand what enabled, or limited, the intervention mechanisms (i.e. practitioner resource offers and offender responses) in achieving the intended outcomes. The main areas explored are as follows.
Emotional competencies (motivation and agency)
Practical and therapeutic support offered by the practitioners did help participants to feel motivated towards changes. However, often the support was too practical and not informed by a shared understanding of the underlying issues that would help participants manage challenges after their release and of the skills they needed to develop to sustain change.
Psychological competencies (coping, emotion regulation, coping strategies)
Participants who received more intensive therapeutic support continued to engage with their practitioner during setbacks and were helped to mentalise about where things had gone wrong. However, as above, therapeutic work was often absent, shallow and superficial, and the resources offered to participants were often practical and did not offer opportunities to reflect on dysregulated thinking.
Social skills and capital (behaviours, building positive relationships)
Participants needed repeated opportunities to reflect before mechanisms had a sustained effect. For some participants, initial engagement with the intervention was a means to foster a favourable impression to other services; however, this is not to say that participants were deliberately disingenuous about wanting to make changes with their lives. Participants believed (fallibly) that their own willpower and motivation would be enough to cease compulsive behaviours. Practitioners were sometimes met with guarded responses and found it difficult to challenge a participant’s overly optimistic perception of life outside prison to enable participants to develop a more realistic perception of the challenges that they faced.
Synthesis 3
The five analyses from the parallel process evaluation were brought together, assessed and discussed by team members. Details of this informal synthesis and analysis can be found in Report Supplementary Material 17. The results were used to further develop the Engager intervention theory. The three main refinements identified were:
-
increased support for practitioners to understand fluctuating emotional states
-
making mentalisation more central
-
developing epistemic trust between the participant and the practitioners as a key mechanism to improve the effectiveness of the therapeutic work.
Patient and public involvement
Active involvement of men who had previously served prison sentences was an integral part of the Engager intervention development and evaluation. 60 The group of people who were self-coined as ‘peer researchers’ reflected that they brought their lived experience, the research team brought their academic experience, and that they all worked together as ‘peers’. The peer researchers contributed to the design, delivery and evaluation of the Engager intervention, inputting into:
-
trial science, including refining study documents (e.g. invitation letters, consent forms, interview schedules), deciding on outcome measures and explaining randomisation
-
qualitative data capture (e.g. co-facilitating focus groups, allowing participants to feel more comfortable to contribute) and analysis (e.g. reviewing focus groups transcripts ‘line by line’ with an academic researcher)
-
training new academic researchers in delivering interview schedules
-
intervention theory development
-
dissemination.
The peer researchers validated, challenged and actively contributed to the research team’s findings. 60 The Engager team committed to the importance of resourcing meaningful involvement as a central part of the research funding bid. The team used their previous experience to support and facilitate the Peer Researcher Group, dedicating time, specific skills and a method of quick and easy payment for participants. A member of staff was appointed as a ‘bridge’ between those with academic experience and those with lived experience, and this member of staff functioned as a key contact point for the peer researchers and facilitated discussions between the two types of expertise.
The Peer Researcher Group was developed through working with local community organisations. The group first met at a local drug and alcohol charity, which provided a neutral and unthreatening environment. Once relationships and trust developed, the group held some meetings on the university campus, which helped the peer researchers to feel respected and part of the Engager team.
Group membership was maintained by regular contact with participants by text, telephone, Facebook (Meta Platforms, Inc., Menlo Park, CA, USA) and e-mail. The group maintained its size through a rolling membership and consisted of a core group of around eight peer researchers aged 25–56 years. During the intervention development phase, the group met 18 times, fortnightly. Ongoing relationships with the individuals in the group were maintained, where possible, through regular updates on the project’s progress. Members with whom contact had been maintained reconvened to develop a dissemination strategy, meeting eight times over a 5-month period, with an average of seven participants per meeting.
Delivering group activities in interactive, accessible and bite-size pieces facilitated peer researcher engagement, understanding, concentration and self-reflection. During the first iteration of the intervention, the academic researchers spoke about their areas of expertise within the project, which the peer researchers then contributed to and critiqued. These sessions included collaborative discussions within which the academic researchers were open to having their conceptions challenged and changed. Positive relationships were built because the atmosphere was relaxed, as one peer researcher said:
. . . so relaxed, I mean people haven’t got much confidence it makes it so much easier for them to come out with stuff.
Lee
The peer researchers reported that the academic researchers were ‘not seeing the barriers’, allowing them to feel ‘the same’ (Steve) and this helped the peer researchers to be ‘open and not to be held back by guilt and shame’ and to feel that they were ‘not getting judged’ (Lee). A key moment was resolving how peer researchers would be referenced. This report uses their first names so that they can evidence to others their achievements, but not their family names, therefore avoiding harming subsequent employment opportunities.
Demonstrating tangible impacts helped maintain engagement. The group sessions helped the peer researchers to build an understanding of the developing intervention, to critique and challenge project decisions and to receive feedback on how their previous contributions had contributed to the project’s progress. The peer researchers said that the academic researchers keeping in touch made them feel that ‘the project genuinely had an interest in our well-being’ (Steve).
Peer researchers felt that involvement in the Engager project gave them a sense of purpose and self-worth and aided their progressive levels of self-confidence. The group also valued being able to make a positive contribution:
. . . it’s nice to be involved in something pro-social rather than anti-social.
Eddie
The Engager project experience demonstrated the positive contributions, as well as challenges, to intervention development and evaluation. The academic researchers felt particularly validated when they presented the integrated intervention and the peer researchers, jokingly, asked the academic researchers what they had been doing throughout the project because what the academic researchers had presented to them was how they had conceptualised and understood the intervention.
Discussion
Overview of results and interpretation
The Engager research programme has run over 7 years and has incorporated several substudies within the two phases and across the four workstreams. The results of the RCT inevitably dominate the findings. The primary outcome showed no difference between arms at 3, 6 or 12 months. The secondary outcomes measured in the trial showed a pattern of null effect. The small number of statistically significant changes were most likely due to multiple testing. There was no evidence for the Engager intervention being cost-effective.
Despite the development of a substantive IDP, implementation of the Engager intervention was suboptimal. Reasons for this included some individuals becoming disengaged from the intervention and delivery of intervention being affected by illness among practitioners, staff changes, conflicts within team cultures and temporary gaps in the practitioners’ capacity to deliver the intervention. Challenges in delivering in the prison setting (e.g. lockdowns, violence and staff cuts) and the well-evidenced underperformance of community rehabilitation companies are also likely to have had an impact on outcomes achieved by the Engager intervention.
The in-depth case studies broadly supported these findings, with suboptimal fidelity to the model and most intervention participants not achieving positive outcomes. However, when Engager was delivered optimally, a significant minority of participants engaged well with the intervention and made important steps towards rehabilitation. However, the positive outcomes achieved by individuals did not correlate with the standard measures when the case study outcomes and trial outcomes were compared after both analyses had been completed. These individual-level case studies also provided evidence that, although most components of the intervention were helpful for at least some individuals, there were also weaknesses in the intervention theory in that it had not proposed specific practitioner activities in relation to individuals who were overoptimistic or resigned in hopelessness.
Overall, we found evidence for three contributors to the neutral results, that is, suboptimal implementation, weak delivery in certain areas of the intervention and the inability of standard trial outcome measures to detect small unpredictable steps in recovery resultant from the intervention for individuals with lifelong experiences of adversity.
Reflections on achievements and challenges
Although we succeeded in many areas, such as recruitment, retention and our iterative intervention development, we are particularly proud of the work the academic researchers produced in partnership with the peer researchers. 60
Phase 1: intervention development and trial science
The main output of phase 1 was the development of a coherent, acceptable and feasible complex intervention for prison leavers with common metal health problems. This iterative process, with realist-informed syntheses, offers other complex intervention developers a blueprint for how to build evidence-based programme theory and evaluate it. This detailed worked example is, to the best of our knowledge, one of few research studies that have used realist-informed approaches in the initial throes of the complex intervention development cycle advocated by the Medical Research Council. Box 3 summarises the key methods of intervention development used.
-
Peer researcher engagement throughout.
-
Development of realist- and behaviour change-informed analytic strategy.
-
Realist review bringing knowledge.
-
Focus groups with populations not covered well in the review.
-
Case studies to learn from promising services elsewhere.
-
Development of an IDP to enhance implementation.
-
A multistep analytical yet flexible system of synthesis of evidence.
-
Realist formative evaluation during feasibility pilot, with rapid feedback and in-depth analysis of underpinning mechanisms.
-
Consensus meeting to agree changes for intervention to go forward to trial.
-
Quantitative assessment of the extent of delivery and fidelity.
-
Broad thematic analysis of implementation barriers and facilitators.
-
Multiple in-depth realist individual case studies to determine mechanisms of impact.
-
Final synthesis to propose further adaptation and elaboration.
Our programme theory separated out the theory of what practitioners should deliver and the theory articulating how this should be achieved. For the latter, a substantive IDP was developed. The Engager manual provides evidence-based guidance for carrying out person-centred and integrated care for prison leavers. The rich detail in the manual provides agencies with descriptions of what supports to offer and also how the supports should be delivered to optimise engagement with different people in differing situations and circumstances. The IDP includes a set of measures detailing how practitioners should be supported throughout delivery, and this includes having a team supervisor, a meta-supervisor (i.e. a clinical lead) who takes overall responsibility for the intervention delivery and top-up training, and MBA top-up training and supervision. The manual, along with a detailed description of the products used to develop it (e.g. narratives, logic model), and our proposed changes, are available on the Engager website [URL: www.plymouth.ac.uk/research/primarycare/criminal-justice/engager (accessed 9 June 2022)].
We documented the developmental processes used to build a theory. Although significant efforts were made to ensure transparency, it was not possible to document all decisions made in the course of developing the theory for the intervention. Therefore, owing to the number of data identified and obtained, and the quality of those data, it is possible that some learning and/or relevant theories were missed, minimised or overemphasised.
Our trial science work was extensive and in-depth. We incorporated two consensus procedures, a review of the literature and a significant period of testing to select the most appropriate outcomes (a process not undertaken by many other programmes). Our pilot demonstrated feasibility in terms of recruitment, follow-up and trial procedures, and also highlighted that traditional gold-standard trial methods, such as blinding, can be difficult to manage within a prison context. However, this does not mean that trials of prison leavers should be avoided.
Phase 2: intervention evaluation
The delivery of the trial was a significant logistical achievement. High proportions of people eligible consented to screening and were recruited to the trial, enhancing generalisability. This achievement was based on our substantial feasibility work30 and piloting. 61 Credit must be given to our motivated and dedicated team of researchers who worked assertively with flexible operating procedures to maintain engagement. We successfully followed up 66% of our participants at 6 months, and this is considered an impressive rate for this population; however, the rate is still lower than that of other community-based depression studies. 25,26
There is currently very little literature on calculating QALYs for people in prison, and this is one of the first studies, to our knowledge, to collect patient-reported preference-based outcome measures in this population. We have collected costs across a range of sectors to provide a more complete picture of where costs fall for people with common mental health problems in prison. Our cost–consequence analysis allowed us to examine the impact further on in the patient care pathway, including facilitating access to services, which allowed us to examine the impact of improving access to planned care on unplanned costs, something not commonly carried out in economic evaluations.
The parallel mixed-method process evaluation, one of the most in-depth completed for a complex health intervention, was a significant success and was especially important given the neutral trial finding. The process evaluation not only provided evidence of breadth and depth, and from multiple perspectives about what was delivered to participants, but also allowed us to hone in on how team dynamics and underlying beliefs and values affected implementation. Subsequently, this allows us to propose what might be done to support practitioners further to optimise delivery. Documenting suboptimal implementation, especially of the MBA and the use of the ‘shared understanding’ formulations, was important for trial result interpretation and development of future practice.
The realist-informed methods allowed us to interrogate the intervention mechanisms by assessing if delivering the specified intervention components produced the hypothesised outcomes, and this gave us insight into how the intervention can have a sustained effect when delivered well. We showed how consistent delivery across time could lead to several mechanisms being activated, often repeatedly, to achieve incremental but sustainable change. The process evaluation also enabled us to identify areas that need refinement in the intervention theory, such as the tools to build a therapeutic relationship for those who might dismiss the need for support, as well as the importance of developing the therapeutic skills of practitioners delivering the intervention.
In the process evaluation, our analyses were limited by the completeness of data collection and longitudinal changes in the context of the intervention delivery across wide geographical areas. Completeness of data collection was particularly challenging for audio-recordings of practitioner/participant sessions and of supervision sessions. There was also a lack of data completeness in the practitioner time logs and session notes. Therefore, greater emphasis was placed on the content of retrospective interviews than we would have preferred.
The trial had some key limitations. Despite standard randomisation procedures being applied, there were imbalances between the two arms at baseline, which indicated that people in the Engager intervention arm were more socially excluded but less emotionally distressed. These differences were controlled for in the analysis; however, there is a chance that people in the Engager intervention arm may also have been more criminogenic, but, unfortunately, we were unable to access CJS data (e.g. offending history) from the Ministry of Justice to examine this (and control for it if needed). In addition, mental health trials of prison leavers will suffer from the problem that distress is relieved for most prison leavers following release, making assessments of benefit more complex.
The outcomes selected are potentially the greatest weakness of the trial. The deliberately flexible intervention, designed to support whatever pathway an individual needed, creates problems for measuring small but potentially critical changes for an individual. The weakness was not in our relatively robust process of selection, but in that there are no outcome measures that have been developed to reflect nuanced individual, but critical, improvements in response to person-centred complex interventions. The in-depth cases studies evidenced small changes that were important to, and valued by, participants and their loved ones; however, these changes were not measurable on the trial outcome measures we had selected.
The development of an iterative and substantive IDP was not sufficient to achieve consistent intervention delivery. Intervention participants’ individual circumstances and personalities, and the context within which Engager practitioners were working (i.e. practitioner illness, staff changes, capacity limitations), limited the intervention being able to be delivered as hypothesised. Participants in the usual-care arm reported experiencing meeting with researchers who demonstrated an interest in them and their lives as helpful and supportive and even referred to this as the ‘Engager intervention’. This degree of interaction was necessary to ensure the retention rates required by RCT methodologies. However, receiving proactive follow-up from researchers who were trained in the intervention’s engagement values to achieve retention rates (i.e. listening without requiring participants to challenge their behaviours) could be seen as a different and even more palatable intervention. The positive impact of the follow-up process may have reduced the ability of the trial to show a difference between people receiving the Engager intervention and those in the usual-care arm.
The intervention resources, as delivered, were insufficient to challenge the wider socioeconomic determinants that framed the trial participants’ life experiences. Despite generous funding and resources, the outstanding questions that this programme has not been able to address are as follows:
-
Given the overwhelming challenges and disadvantages that this population faces, what would be required to achieve sustained change for this population?
-
Would the costs and resources required for this sustained change be economically prohibitive when set against wider national crime, victim and societal costs, as well as familial costs (particularly the legacy for the children of the participants)?
Implications
Considerations for future research
The Engager research programme demonstrated that it is possible to recruit and follow up individuals with common mental health problems into the community following release from prison in a RCT. However, the cost per individual recruited and followed up is significant. At trial mid-point three researchers were required at each site to manage recruitment of final participants alongside follow-ups. In addition, outcome measures for mental health interventions for individuals with complex needs and, in particular, individuals in contact with the CJS, need to be selected carefully along with the length of follow-up. There is a very real question as to whether or not it is possible to measure changes in outcomes using standard outcome measures for individuals with such great heterogeneity of need. Therefore, it may be that new outcome measures or systems of measurement need to be developed. However, it is also uncertain whether or not interventions of a relatively short nature can overcome years of adversity and maladaptive behaviour.
There were additional challenges to trial integrity. We were not able to ensure that researchers were blinded. We had a significant proportion of follow-ups located in prison, potentially contributing to bias. We needed (and had) caring dedicated researchers to achieve follow-up and they were often seen as helpful by control participants (with some mistakenly believing that they were receiving the intervention). It is unclear whether or not RCT methodologists can overcome all these challenges when attempting to evaluate complex interventions delivered within the CJS and, therefore, we suggest that future trials should allow for creativity alongside rigour.
Alternative methods of research using whole-system approaches, for example focusing on quantification of access and examining pathways over time, alongside qualitative approaches to understanding the likely but not definitive effectiveness of various approaches, is an alternative overarching method to the RCT. Such approaches may also be more easily integrated with system redesign and continuous quality improvement. Whether using a RCT or alternative methods including routine data, we suggest that there is sufficient evidence to support an evaluation of the deployment of Engager intervention components by existing criminal justice, housing and substance misuse services.
Implications for practice and policy
The Engager research programme points to a range of potential implications for practice; however, given the mixed results, none is definitive.
Mentalisation-based approaches
The MBA and psychological formulation underpinning the shared understanding and plan were suboptimally delivered, but showed promise. Mentalisation has a good, but still relatively small, evidence base, and the Engager intervention demonstrated (and evidenced at some points for some people) the potential for applying the approach flexibly to a population with complex needs outside the traditional hour-long therapy sessions. The integration of MBA alongside a ‘shared understanding’ formulation showed promise in some of the in-depth cases, indicating an area for further development. In addition, as has been found in other recent interventions aimed primarily at offenders,62 working as Engager practitioners led to increased competencies and transferable skills. The research showed that some practitioners working in Engager support worker roles were able to use mentalisation-based and formulation-type approaches outside mental health systems. If MBA and other similar psychological approaches are to be embedded into other service settings, such as housing, substance misuse and probation, then this needs to be carried out by staff with suitable capabilities and supported by excellent training and ongoing mental health supervision. It is important to identify the key components of a MBA that is essential in working with this client group, recognising that development in practice may best be carried out with in-depth research, including analysis of interactions.
‘Through the gate’ practices
Engager showed that it is possible to consistently carry out practical ‘through the gate’ work, which would often take most of a day. The working practices used within the Engager programme included systems for reliably meeting individuals, safely using a car for transport, protocols for leaving individuals who may still be without accommodation, supporting attendance at two or more meetings and the use of this work to develop trust for ongoing work or for transfer of trust to other services.
Pre-release work
Pre-release practical and psychological work was perhaps the least successfully delivered component of the Engager intervention. The process evaluation suggested that pre-release practical and psychological work was not accepted when it was tried, and often it was only intermittently attempted (especially for people who were randomised months before release). Practitioners may have been unclear about the importance of the pre-release practical and psychological work and may not have felt confident about what to focus on. The Engager programme, therefore, provides little new evidence on how to best carry out pre-release psychological work, including regarding if focus needs to be placed on developing a trusting relationship to optimise opportunities for engagement post release. We also found little evidence of other mental health support occurring in the prison in line with the lack of progress of delivering the IAPT in prisons, and all of these issues point to the need for a review of psychological support leading up to release as a whole.
Supervision
Team-based working and supervision was shown to be important. If team-based working and supervision was not operating effectively, then it contributed to poorly functioning teams and suboptimal delivery of intervention components, particularly of psychological components. There was also evidence that effective team-based formal and informal supervision helped practitioners in this very challenging work. For example, as well as supporting use of MBA and formulation with individuals who were engaged, supervision supported decision-making about when not to pursue work that was futile. In particular, the Engager supervision structure of having the mental health supervisor not just providing supervision through discussion, but also often seeing individuals and leading a team of professionally unqualified practitioners, is a model that is aligned with national clinical policies and shows promise.
Supporting mental health care within other services for individuals with complex needs
In our view, training existing probation and third-sector staff to deliver the core Engager psychological functions provides the most promising avenue for policy development. These staff, already commissioned to carry out the practical support of resettlement, and often providing emotional support informally, would need additional supervision from mental health experts. A model of embedding mental care into existing non-health teams for individuals with complex needs is the opposite of the current practice of aiming, but nearly always failing, to secure an onward pathway to standard mental health services. It is, however, in keeping with current policies being developed for community mental health provision, which aim to address inequities across voluntary and community sectors and primary care, breaking down barriers between teams, as well as supporting positive mental health function across the system.
High-quality delivery of the mental health functions within existing services offers the possibility of a whole-system person-centred response for individuals with enduring complex needs and one that is substantially less expensive than the stand-alone Engager team with caseloads of 10–12 individuals. If just a few prison sentences could be avoided, then provision of mental health care in this integrated way could be cost-effective.
Conclusions
The Engager research programme allowed for substantial theoretical development and trial science work, building up to a fully powered trial, cost-effectiveness evaluation and an exemplar in-depth multimethod process evaluation in an area of health care that has very limited previous research and development. The Engager research programme saw the realist-informed development of a comprehensive evidence-based complex intervention for prison leavers with mental health problems, which was underpinned by a person-centred approach and supported by a flexible team-based delivery.
Although the Engager intervention, as delivered, was shown not to be effective using standard mental health trial outcome measures, conclusions are not straightforward. The weakness in measurement of improvement for personal goals is a weakness of current methodology for complex intervention evaluation. Our in-depth process evaluation showed that, although implementation problems may also have contributed to the neutral result, when delivered well, there was activation of mechanisms that produced short-term outcomes, such as engagement and emotional competencies, which we had hypothesised. The delivery of MBA and the ‘shared understanding’ were both particularly challenging to achieve, but were also both shown to be potentially critical for the generation of such outcomes. Other promising elements included the through-the-gate function and team-based supervision. Overall, although investing in new stand-alone Engager teams is not justified by the results, we conclude that it is worth testing whether or not core aspects of the intervention could be delivered by existing substance misuse, probation and homeless services, if supported by supervisors with skills in psychological therapy.
Acknowledgements
The research team would like to thank all individuals, that is, both individuals in contact with the CJS and individuals working in services, involved in allowing data to be collected and who gave up valuable time to be interviewed for this programme of work. We are indebted to the peer researchers for their contributions and candour that helped shape the research. We are particularly grateful for the support and advice of all the local health, voluntary and community sector and criminal justice agencies, especially those providing the Engager intervention, working in Imagine Independence (Liverpool, UK), Lancashire and South Cumbria NHS Foundation Trust, Hamoaze House (Plymouth, UK) and Devon Partnership NHS Trust (Devon, UK). We would like to express our appreciation to Her Majesty’s Prison Service and the National Probation Service. We would like to thank the members of the Programme Steering Group, the Research Design Service, the Clinical Research Network and the sponsor, Devon Partnership NHS Trust. We thank the funding body (i.e. the National Institute for Health Research Programme Grants for Applied Research programme), as well as the Peninsula Applied Research Collaboration for additional support. Last, we would like to acknowledge the important role of Gill McGauley, one of the original research team, who helped develop our MBA, but who sadly died at the height of her career soon after delivering some of the initial Engager training.
Contributions of authors
Richard Byng (https://orcid.org/0000-0001-7411-9467) (Professor in Primary Care Research) was responsible for programme design and management, intervention development and formative evaluation, trial science development, the RCT, process evaluation and report writing.
Charlotte Lennox (https://orcid.org/0000-0001-9014-9965) (Research Fellow and Lecturer) was responsible for programme design and management, intervention development and formative evaluation, trial science development, the RCT, process evaluation, report writing and health economics.
Tim Kirkpatrick (https://orcid.org/0000-0002-1693-0742) (Research Fellow, Complex Intervention Trial Development) was responsible for programme design and management, intervention development and formative evaluation, trial science development, the RCT, process evaluation, report writing and health economics.
Cath Quinn (https://orcid.org/0000-0003-4644-4603) (Senior Research Fellow, Complex Intervention Trial Development) was responsible for programme design and management, intervention development and formative evaluation, trial science development, process evaluation and report writing.
Rob Anderson (https://orcid.org/0000-0002-3523-8559) (Professor of Health Services and Implementation Research) was responsible for programme design and management, intervention development and formative evaluation, the RCT, report writing and health economics.
Sarah Louise Brand (https://orcid.org/0000-0001-5979-2442) (Research Fellow) was responsible for intervention development and formative evaluation, and report writing.
Lynne Callaghan (https://orcid.org/0000-0002-0766-645X) (Senior Research Fellow) was responsible for intervention development and formative evaluation, trial science development and report writing.
Lauren Carroll (https://orcid.org/0000-0003-1203-0672) (Research Assistant) was responsible for trial science development, the RCT and report writing.
Graham Durcan (https://orcid.org/0000-0001-7947-0651) (Associate Director, Centre for Mental Health) was responsible for intervention development and formative evaluation, process evaluation and report writing.
Laura Gill (https://orcid.org/0000-0001-6224-5693) (Research Group Co-ordinator) was responsible for programme design and management, intervention development and formative evaluation, trial science development and report writing.
Sara Goodier (https://orcid.org/0000-0003-1843-3915) (Research Assistant) was responsible for the RCT and report writing.
Jonathan Graham (https://orcid.org/0000-0002-3845-3289) (Research Assistant) was responsible for process evaluation and report writing.
Rebecca Greer (https://orcid.org/0000-0001-5552-2429) (Research Assistant) was responsible for the RCT and report writing.
Mark Haddad (https://orcid.org/0000-0002-4822-5482) (Senior Lecturer in Health Service Research) was responsible for trial science development, the RCT and report writing.
Tirril Harris (https://orcid.org/0000-0003-1769-665X) (Honorary Research Fellow, Psychology and Social Science) was responsible for intervention development and formative evaluation, trial science development, report writing and health economics.
William Henley (https://orcid.org/0000-0001-6273-2619) (Professor of Medical Statistics) was responsible for trial science development, process evaluation and health economics.
Rachael Hunter (https://orcid.org/0000-0002-7447-8934) (Associate Professor, Health Economics) was responsible for the RCT, report writing and health economics.
Mike Maguire (https://orcid.org/0000-0002-8379-6475) (Emeritus Professor of Criminology and Criminal Justice) was responsible for programme design and management, intervention development and formative evaluation, trial science development, the RCT, process evaluation, report writing and health economics.
Sarah Leonard (https://orcid.org/0000-0002-1729-0556) (Research Associate) was responsible for process evaluation and report writing.
Susan Michie (https://orcid.org/0000-0003-0063-6378) (Professor of Health Psychology) was responsible for intervention development and formative evaluation, process evaluation and report writing.
Christabel Owens (https://orcid.org/0000-0001-9846-0889) (Associate Professor of Public Mental Health) was responsible for intervention development and formative evaluation, process evaluation and report writing.
Mark Pearson (https://orcid.org/0000-0001-7628-7421) (Senior Lecturer in Implementation Science and Knowledge Mobilisation) was responsible for intervention development and formative evaluation, and report writing.
Sarah Rybczynska-Bunt (https://orcid.org/0000-0002-4284-1081) (Research Fellow) was responsible for process evaluation and report writing.
Caroline Stevenson (https://orcid.org/0000-0002-1176-5231) (Research Assistant) was responsible for trial science development, the RCT and report writing.
Amy Stewart (https://orcid.org/0000-0002-5324-2025) (Research Assistant) was responsible for trial science development, the RCT and report writing.
Alex Stirzaker (https://orcid.org/0000-0001-6755-7848) (Clinical Lead, IAPT Severe and Enduring Mental Illness) was responsible for intervention development and formative evaluation, the RCT, process evaluation and report writing.
Rod Taylor (https://orcid.org/0000-0002-3043-6011) (Professor of Health Services Research) was responsible for programme design and management, trial science development, process evaluation, report writing and health economics.
Roxanne Todd (https://orcid.org/0000-0001-5651-6549) (Research Assistant) was responsible for trial science development, the RCT and report writing.
Florian Walter (https://orcid.org/0000-0002-1877-2792) (Research Associate) was responsible for the RCT and report writing.
Fiona C Warren (https://orcid.org/0000-0002-3833-0182) (Senior Lecturer in Medical Statistics) was responsible for the RCT and report writing.
Lauren Weston (https://orcid.org/0000-0001-8735-2292) (Research Assistant) was responsible for intervention development and formative evaluation, trial science development, the RCT, process evaluation and report writing.
Nat Wright (https://orcid.org/0000-0003-3547-3724) (Clinical Research Director, Spectrum Community Health CIC) was responsible for trial science development, the RCT and report writing.
Jenny Shaw (https://orcid.org/0000-0003-2569-7687) (Professor of Forensic Psychiatry) was responsible for programme design and management, intervention development and formative evaluation, trial science development, the RCT, process evaluation, report writing and health economics.
Publications
Pearson M, Brand SL, Quinn C, Shaw J, Maguire M, Michie S, et al. Using realist review to inform intervention development: methodological illustration and conceptual platform for collaborative care in offender mental health. Implement Sci 2015;10:134. https://doi.org/10.1186/s13012-015-0321-2
Kirkpatrick T, Lennox C, Taylor R, Anderson R, Maguire M, Haddad M, et al. Evaluation of a complex intervention (Engager) for prisoners with common mental health problems, near to and after release: study protocol for a randomised controlled trial. BMJ Open 2018;8:e017931. https://doi.org/10.1136/bmjopen-2017-017931
Lennox C, Kirkpatrick T, Taylor RS, Todd R, Greenwood C, Haddad M, et al. Pilot randomised controlled trial of the ENGAGER collaborative care intervention for prisoners with common mental health problems, near to and after release. Pilot Feasibility Stud 2018;4:15. https://doi.org/10.1186/s40814-017-0163-6
Owens C, Carter M, Shenton D, Byng R, Quinn C. Engaging without exposing: use of a fictional character to facilitate mental health talk in focus groups with men who have been subject to the criminal justice system. Qual Health Res 2018;28:2102–14. https://doi.org/10.1177/1049732318785359
Taylor C, Gill L, Gibson A, Byng R, Quinn C. Engaging ‘seldom heard’ groups in research and intervention development: offender mental health. Health Expect 2018;21:1104–10. https://doi.org/10.1111/hex.12807
Brand SL, Quinn C, Pearson M, Lennox C, Owens C, Kirkpatrick T, et al. Building programme theory to develop more adaptable and scalable complex interventions: realist formative process evaluation prior to full trial. Evaluation 2019;25:149–70. https://doi.org/10.1177/1356389018802134
Lennox C, Stevenson R, Owens C, Byng R, Brand SL, Maguire M, et al. Using multiple case studies of health and justice services to inform the development of a new complex intervention for prison-leavers with common mental health problems (Engager). Health Justice 2021;9:6. https://doi.org/10.1186/s40352-021-00131-z
Rybczynska-Bunt S, Weston L, Byng R, Stirzaker A, Lennox C, Pearson M, et al. Clarifying realist analytic and interdisciplinary consensus processes in a complex health intervention: a worked example of judgemental rationality in action. Evaluation 2021;27. https://doi.org/10.1177/13563890211037699
Hunter RM, Anderson R, Kirkpatrick T, Lennox C, Warren F, Taylor R, et al. Economic evaluation of a complex intervention (Engager) for prisoners with common mental health problems, near to and after release: a cost-utility and cost-consequences analysis. Eur J Health Econ 2022;22:193–210. https://doi.org/10.1007/s10198-021-01360-7
Byng R, Kirkpatrick T, Lennox C, Warren FC, Anderson R, Brand SL, et al. Evaluation of a complex intervention for prisoners with common mental health problems, near to and after release: The Engager randomised controlled trial [published online ahead of print August 18 2022]. Br J Psych 2022.
Weston L, Rybczynska-Bunt S, Quinn C, Lennox C, Maguire M, Pearson M, et al. Interrogating intervention delivery and participants’ emotional states to improve engagement and implementation: a realist informed multiple case study evaluation of Engager. PLOS ONE 2022;17:e0270691.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PGfAR programme or the Department of Health and Social Care.
References
- Fazel S, Hayes AJ, Bartellas K, Clerici M, Trestman R. Mental health of prisoners: prevalence, adverse outcomes, and interventions. Lancet Psychiatry 2016;3:871-81. https://doi.org/10.1016/S2215-0366(16)30142-0.
- Fazel S, Seewald K. Severe mental illness in 33,588 prisoners worldwide: systematic review and meta-regression analysis. Br J Psychiatry 2012;200:364-73. https://doi.org/10.1192/bjp.bp.111.096370.
- Fazel S, Danesh J. Serious mental disorder in 23 000 prisoners: a systematic review of 62 surveys. Lancet 2002;359:545-50. https://doi.org/10.1016/S0140-6736(02)07740-1.
- Blaauw E, Roesch R, Kerkhof A. Mental disorders in European prison systems: arrangements for mentally disordered prisoners in the prison systems of 13 European countries. Int J Law Psychiatry 2000;5–6:649-63. https://doi.org/10.1016/S0160-2527(00)00050-9.
- Fazel S, Bains P, Doll H. Substance abuse and dependence in prisoners: a systematic review. Addiction 2006;101:181-91. https://doi.org/10.1111/j.1360-0443.2006.01316.x.
- Goff A, Rose E, Rose S, Purves D. Does PTSD occur in sentenced prison populations? A systematic literature review. Crim Behav Ment Health 2007;17:152-62. https://doi.org/10.1002/cbm.653.
- Fazel S, Xenitidis K, Powell J. The prevalence of intellectual disabilities among 12,000 prisoners – a systematic review. Int J Law Psychiatry 2008;31:369-73. https://doi.org/10.1016/j.ijlp.2008.06.001.
- Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta-analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psychol Med 2015;45:247-58. https://doi.org/10.1017/S0033291714000762.
- May C, Sharma N, Stewart D. Factors Linked to Reoffending: A One-Year Follow-up of Prisoners Who Took Part in the Resettlement Surveys 2001, 2003 and 2004. London: Ministry of Justice; 2008.
- Byng R, Weyer Brown C, Sheaff R, Samele C, Duggan S, Harrison D, et al. COCOA: Care for Offenders: Continuity of Access. Southampton: NIHR Service Delivery and Organisation Programme; 2012.
- Pratt D, Piper M, Appleby L, Webb R, Shaw J. Suicide in recently released prisoners: a population-based cohort study. Lancet 2006;368:119-23. https://doi.org/10.1016/S0140-6736(06)69002-8.
- Borschmann R, Thomas E, Moran P, Carroll M, Heffernan E, Spittal MJ, et al. Self-harm following release from prison: a prospective data linkage study. Aust N Z J Psychiatry 2017;51:250-9. https://doi.org/10.1177/0004867416640090.
- Corston J. The Corston Report 2007.
- Ministry of Justice . Offender Management Statistics: Prison Receptions 2018 2019.
- Ministry of Justice . Compendium of Re-Offending Statistics and Analysis 2013.
- Ministry of Justice . Proven Re-Offending Statistics Quarterly, April 2014 to March 2015 2017.
- Lennox C, Stevenson C, Edge D, Hopkins G, Thornicroft G, Susser S, et al. Critical time intervention: a qualitative study of the perspectives of prisoners and staff. J Forens Psychiatry Psychol 2019;31:76-89. https://doi.org/10.1080/14789949.2019.1665699.
- Howerton A, Burnett R, Byng R, Campbell J. The consolations of going back to prison: what ‘revolving door’ prisoners think of their prospects. J Offender Rehabil 2009;48:439-61. https://doi.org/10.1080/10509670902979710.
- Home Office . IOM Efficiency Toolkit Phase 2: Revised Unit Costs of Crime and Multipliers 2011.
- Steel J, Thornicroft G, Birmingham L, Brooker C, Mills A, Harty M, et al. Prison mental health inreach services. Br J Psychiatry 2007;190:373-4. https://doi.org/10.1192/bjp.bp.106.031294.
- Herman DB, Conover S, Gorroochurn P, Hinterland K, Hoepner L, Susser ES. Randomized trial of critical time intervention to prevent homelessness after hospital discharge. Psychiatr Serv 2011;62:713-19. https://doi.org/10.1176/ps.62.7.pss6207_0713.
- Shaw J, Conover S, Herman D, Jarrett M, Leese M, McCrone P, et al. Critical time Intervention for Severely mentally ill Prisoners (CrISP): a randomised controlled trial. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05080.
- Senior J, Birmingham L, Harty MA, Hassan L, Hayes AJ, Kendall K, et al. Identification and management of prisoners with severe psychiatric illness by specialist mental health services. Psychol Med 2013;43:1511-20. https://doi.org/10.1017/S0033291712002073.
- Thomas EG, Spittal MJ, Heffernan EB, Taxman FS, Alati R, Kinner SA. Trajectories of psychological distress after prison release: implications for mental health service need in ex-prisoners. Psychol Med 2016;46:611-21. https://doi.org/10.1017/S0033291715002123.
- Coventry PA, Hudson JL, Kontopantelis E, Archer J, Richards DA, Gilbody S, et al. Characteristics of effective collaborative care for treatment of depression: a systematic review and meta-regression of 74 randomised controlled trials. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0108114.
- Ekers D, Murphy R, Archer J, Ebenezer C, Kemp D, Gilbody S. Nurse-delivered collaborative care for depression and long-term physical conditions: a systematic review and meta-analysis. J Affect Disord 2013;149:14-22. https://doi.org/10.1016/j.jad.2013.02.032.
- Kouyoumdjian FG, McIsaac KE, Liauw J, Green S, Karachiwalla F, Siu W, et al. A systematic review of randomized controlled trials of interventions to improve the health of persons during imprisonment and in the year after release. Am J Public Health 2015;105:e13-33. https://doi.org/10.2105/AJPH.2014.302498.
- Apa ZL, Bai R, Mukherejee DV, Herzig CT, Koenigsmann C, Lowy FD, et al. Challenges and strategies for research in prisons. Public Health Nurs 2012;29:467-72. https://doi.org/10.1111/j.1525-1446.2012.01027.x.
- Quinn C, Byng R, Shenton D, Smart C, Michie S, Stewart A, et al. The feasibility of following up prisoners, with mental health problems, after release: a pilot trial employing an innovative system, for engagement and retention in research, with a harder-to-engage population. Trials 2018;19. https://doi.org/10.1186/s13063-018-2911-1.
- Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet 2009;374:86-9. https://doi.org/10.1016/S0140-6736(09)60329-9.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0643-1.
- Craig P, Petticrew M. Developing and evaluating complex interventions: reflections on the 2008 MRC guidance. Int J Nurs Stud 2013;50:585-7. https://doi.org/10.1016/j.ijnurstu.2012.09.009.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud 2013;50:587-92. https://doi.org/10.1016/j.ijnurstu.2012.09.010.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 2017.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Pearson M, Brand SL, Quinn C, Shaw J, Maguire M, Michie S, et al. Using realist review to inform intervention development: methodological illustration and conceptual platform for collaborative care in offender mental health. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0321-2.
- Bateman AW, Fonagy P. Mechanism of change in metallisation based treatment of borderline personality disorder. J Clin Psychol 2006;62:411-30. https://doi.org/10.1002/jclp.20241.
- Lennox C, Stevenson R, Owens C, Byng R, Brand SL, Maguire M, et al. Using multiple case studies of health and justice services to inform the development of a new complex intervention for prison-leavers with common mental health problems (Engager). Health Justice 2021;9. https://doi.org/10.1186/s40352-021-00131-z.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. Abingdon: Routledge; 1994.
- Owens C, Carter M, Shenton D, Byng R, Quinn C. Engaging without exposing: use of a fictional character to facilitate mental health talk in focus groups with men who have been subject to the criminal justice system. Qual Health Res 2018;28:2102-14. https://doi.org/10.1177/1049732318785359.
- Brand SL, Quinn C, Pearson M, Lennox C, Owens C, Kirkpatrick T, et al. Building programme theory to develop more adaptable and scalable complex interventions: realist formative process evaluation prior to full trial. Evaluation 2019;25:149-70. https://doi.org/10.1177/1356389018802134.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Lennox C, Kirkpatrick T, Taylor RS, Todd R, Greenwood C, Haddad M, et al. Pilot randomised controlled trial of the ENGAGER collaborative care intervention for prisoners with common mental health problems, near to and after release. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-017-0163-6.
- Thomas S, Harty MA, Parrott J, McCrone P, Slade M, Thornicroft G. CANFOR: Camberwell Assessment of Need – Forensic Version. London: The Royal College of Psychiatrists; 2003.
- Ashworth M, Robinson S, Godfrey E, Shepherd M, Evans C, Seed P, et al. Measuring mental health outcomes in primary care: the psychometric properties of a new patient-generated outcome measure, PSYCHLOPS (Psychological Outcome Profiles). Prim Care Ment Health 2005;3:261-70.
- Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil 2009;23:362-70. https://doi.org/10.1177/0269215508101742.
- Evans C, Mellor-Clark J, Margison F, Barkham M, Audin K, Connell J, et al. CORE: Clinical outcomes in routine evaluation. J Ment Health 2000;9:247-55. https://doi.org/10.1080/jmh.9.3.247.255.
- Goldberg DP, Williams P. A User’s Guide to the General Health Questionnaire. Basingstoke: Nelson; 1998.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13.
- Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing Generalised Anxiety Disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. https://doi.org/10.1001/archinte.166.10.1092.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- Williams J, Leamy M, Bird V, Le Boutillier C, Norton S, Pesola F, et al. Development and evaluation of the INSPIRE measure of staff support for personal recovery. Soc Psychiatry Psychiatr Epidemiol 2015;50:777-86. https://doi.org/10.1007/s00127-014-0983-0.
- Revolving doors . Response to Breaking the Cycle 2011. https://revolving-doors.org.uk/wp-content/uploads/2022/02/2010-12-Response-to-Breaking-the-Cycle-3.pdf (accessed 3 February 2020).
- Dubourg R, Hamed J. The Economic and Social Costs of Crime Against Individuals and Households 2003–04. Home Office Report 30 05 2005.
- Byng R, Kirkpatrick T, Lennox C, Warren FC, Anderson R, Brand SL, et al. Evaluation of a complex intervention for prisoners with common mental health problems, near to and after release: The Engager randomised controlled trial [published online ahead of print August 18 2022]. Br J Psych 2022.
- Lucock M, Padgett K, Noble R, Westley A, Atha C, Horsefield C, et al. Controlled clinical trial of a self-help for anxiety intervention for patients waiting for psychological therapy. Behav Cogn Psychother 2008;36. https://doi.org/10.1017/S1352465808004591.
- Hunter RM, Anderson R, Kirkpatrick T, Lennox C, Warren F, Taylor R, et al. Economic evaluation of a complex intervention (Engager) for prisoners with common mental health problems, near to and after release: a cost-utility and cost-consequences analysis. Eur J Health Econ 2022;22:193-210. https://doi.org/10.1007/s10198-021-01360-7.
- Rybczynska-Bunt S, Weston L, Byng R, Stirzaker A, Lennox C, Pearson M, et al. Clarifying realist analytic and interdisciplinary consensus processes in a complex health intervention: a worked example of judgemental rationality in action. Evaluation 2021;27. https://doi.org/10.1177/13563890211037699.
- Weston L, Rybczynska-Bunt S, Quinn C, Lennox C, Maguire M, Pearson M, et al. Interrogating intervention delivery and participants’ emotional states to improve engagement and implementation: a realist informed multiple case study evaluation of Engager. PLOS ONE 2022;17.
- Taylor C, Gill L, Gibson A, Byng R, Quinn C. Engaging ‘seldom heard’ groups in research and intervention development: offender mental health. Health Expect 2018;21:1104-10. https://doi.org/10.1111/hex.12807.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health service research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- National Offender Management Service and NHS . The Offender Personality Disorder Pathway Strategy 2015.
List of abbreviations
- CAN-FOR
- Camberwell Assessment of Need – Forensic Version
- CI
- confidence interval
- CJS
- criminal justice system
- CMO
- context–mechanism–outcome
- CONSORT
- Consolidated Standards of Reporting Trials
- CORE-6D
- Clinical Outcomes in Routine Evaluation – 6D
- CORE-OM
- Clinical Outcomes in Routine Evaluation – Outcome Measure
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GAS
- Goal Attainment Scale
- IAPT
- Improving Access to Psychological Therapies
- ICECAP-A
- ICEpop CAPability measure for Adults
- IDP
- intervention delivery platform
- MBA
- mentalisation-based approach
- MICE
- multivariate imputation via chained equations
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- YFC
- year of full capability
Notes
-
Realist-informed interview schedule for the organisational case study
-
Additional programme theories not covered in the formative process evaluation paper
-
Rapid realist review using the Consolidated Framework for Implementation Research (CFIR) to inform the implementation delivery platform for the ‘Engager’ intervention
-
Post hoc exploratory analysis of the Engager randomised controlled trial data
-
Fidelity of delivery for ‘Engager’: a complex intervention for prisoner leavers with common mental health problems
-
Process evaluation: individual- and organisational-level barriers to and facilitators of implementation
-
Data examples for individual- and organisational-level barriers to and facilitators of implementation
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/MMWC3761).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
