Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0606-1247. The contractual start date was in June 2011. The final report began editorial review in September 2012 and was accepted for publication in March 2013. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
David Gunnell, Keith Hawton and Nav Kapur are members of England's National Suicide Prevention Advisory Group. David Gunnell is also a member of the Medicines and Healthcare products Regulatory Agency (MHRA) Pharmacovigilance Expert Advisory Group. Keith Hawton and Sue Simkin acted as temporary advisers to the MHRA for its evaluation of the efficacy and safety profile of co-proxamol. Nav Kapur was chairperson of the Guideline Development Group for the National Institute for Health and Care Excellence 2011 guidelines on the longer-term management of self-harm.
Disclaimer
This report contains transcripts of interviews, and similar, conducted in the course of the research and contains language which may offend some readers.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Gunnell et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Suicide and self-harm are the most serious and devastating consequences of mental illness. More than 4000 people take their lives every year in England and there are over 200,000 hospital presentations for self-harm annually. 1 Almost one-quarter of people who self-harm repeat their act within 12 months. As suicide occurs predominantly in young people – > 50% of deaths occur in those aged < 45 years – it is a major contributor to potential years of life lost (PYLL), accounting for more PYLL than strokes or road traffic accidents. 2 Death by suicide has a profound long-term impact on the family, friends and colleagues of the deceased.
In view of the impact of suicidal behaviour on population health, suicide prevention has been a key area in the health strategies of successive UK governments, and in 2002 the Department of Health (England) launched its National Suicide Prevention Strategy. 3 However, the evidence base to inform the prevention strategy is limited. 4,5 The causes of suicidal behaviour are complex, vary at different phases of the life course and operate both at an individual level and at a societal level;6,7 thus, national prevention strategies include a range of clinical and public health approaches to reduce its incidence. 3,8 In this context and in discussion with major stakeholders, we developed a programme of research to address several key areas of relevance to suicide prevention in England. The following paragraphs outline the rationale for our choice of research questions.
Priority areas in suicide prevention
Suicide statistics
Good-quality suicide statistics are critical to inform suicide prevention priorities and to assess the impact of prevention strategies. However, whether a self-inflicted death is recorded as a suicide, an open verdict, a misadventure or an accidental death by the Office for National Statistics (ONS) depends on the outcome of a coroner's investigation, and coroners differ in their threshold for labelling deaths as suicide. 9 Such differences and changes in coroners' categorisation of possible suicides over time may compromise an assessment of the incidence of suicide and so undermine the evaluation of specific preventative activities using routine data. 10
Medicines commonly taken in fatal overdoses
Suicide may occur in the context of serious mental illness or result from an impulsive act in a moment of crisis. Whether an episode of self-harm results in death depends on the ease of availability of lethal suicide methods, and some of the best evidence concerning suicide prevention concerns restricting access to lethal methods. 5,11 Drugs associated with high case fatality when taken in overdose are therefore a common target for preventative intervention. Overdoses of paracetamol (acetaminophen), co-proxamol and dosulepin account for 10% of suicides in England, and the Medicines and Healthcare products Regulatory Agency (MHRA) has implemented a number of initiatives to reduce the incidence of suicides using these and other medicines. One of the most recent initiatives has been the phased withdrawal of co-proxamol since 2005. The impact of the withdrawal of co-proxamol requires evaluation to inform both international prescribing policies and future interventions of this sort, such as restricting the use of dosulepin. Furthermore, continued deaths from paracetamol overdose since regulatory action in 199812 suggest the need to review existing sales regulations and evaluate the long-term effects of the legislation.
Assessment and management of people who self-harm
Whether someone who attempts suicide and survives later successfully repeats his or her act may depend on the NHS's response to his or her initial attempt. 13 Yet there is uncertainty concerning the most appropriate service structures to assess and manage self-harm patients. This uncertainty was demonstrated in our previous studies showing wide variations between hospitals in their management of self-harm. 14,15 It is unclear whether or not these variations have any implications for patient outcomes; although person-based studies suggest that some aspects of service provision may affect outcome,16–18 these findings may be confounded both because patient characteristics may influence the services they receive and because high-risk patients may be most likely to self-discharge without receiving care. It is crucial to assess whether or not differences in hospital management influence outcomes in this key area.
Trials of interventions to reduce self-harm in high-risk clinical populations
Half of all people who die by suicide have been in contact with health services within a month of their death. 19 The two highest-risk groups are patients who have recently been discharged from psychiatric inpatient care and those who have self-harmed. One-quarter of all people who die by suicide have been under the recent care of psychiatric services,20 and around half have been in contact with services following a previous episode of self-harm. 6 Thus, interventions to reduce suicide risk in these groups are a priority; yet, Cochrane reviews21 and National Institute for Health and Care Excellence (NICE) guidance13 have highlighted the lack of good-quality evidence concerning the management of self-harm. Trials of contact by telephone or letter, or the provision of ‘crisis cards’ facilitating access to urgent care following self-harm have had mixed results. 22 Likewise, only one randomised controlled trial of an intervention to reduce the risk of suicide following psychiatric inpatient discharge has been carried out,23,24 and, although this trial showed promising results, it has not been replicated.
Aim
Our overall aim was to carry out a programme of linked research studies aimed at improving the management of self-harm, reducing the incidence of suicide and providing reliable data to evaluate the impact of the 2002 National Suicide Prevention Strategy for England. 3
Objectives and research questions
Our research programme consisted of four interlinked studies, each of which related to key aspects of the 2002 National Suicide Prevention Strategy for England. 3 Our objectives were to:
-
conduct a review of the inquest records of 12 coroners, spanning a period of 15 years, to quantify the extent to which suicide rates, secular trends in suicide, and suicides from co-proxamol, paracetamol and tricyclic antidepressant (TCA) overdose may be over- or underestimated when they are based on deaths given suicide and open verdicts by coroners
-
carry out a series of pharmacoepidemiological studies using national mortality data together with information from self-harm registers in Oxford and Manchester and coroners' records to investigate:
-
(a) associations between blood paracetamol levels and liver damage (note: because of challenges obtaining relevant data, this was subsequently modified to a comparison of the impact of differing parcetamol regulations in the UK and Ireland)
-
(b) whether or not the current sales limit for paracetamol is appropriate and being adhered to, determined by interviewing a sample of people who have taken a paracetamol overdose about their episode
-
(c) whether or not any compensatory increased use of non-steroidal anti-inflammatory drugs (NSAIDs) has led to increased rates of gastrointestinal (GI) haemorrhage
-
(d) the impact on suicide of the recent withdrawal of co-proxamol
-
(e) whether or not regulatory action is warranted concerning dosulepin (a TCA)
-
-
assess whether or not between-hospital variations in four key aspects of self-harm services (psychosocial assessment, general hospital admission, psychiatric admission and follow-up) influence patient outcome, as indexed by repeat self-harm
-
develop, pilot and evaluate contact-based interventions aimed at reducing:
-
(a) repeat self-harm
-
(b) self-harm following specialist inpatient psychiatric treatment.
-
Structure of this report
Chapters 2–8 present the findings from the component substudies relevant to each of the research objectives described in the previous section. Although these objectives are grouped thematically, they do not reflect the number of different methodologies used to achieve them. Some research objectives were investigated using a single methodology whereas others were investigated using more than one. For this reason the chapters of this report vary in whether they outline the findings related to one or to several of the research objectives:
-
Chapter 2 outlines the study relating to objective 1, examining the influence of changes in coroners' practices on the validity of national suicide rates in England.
-
Chapter 3 outlines the findings of four separate studies relating to objectives 2(a), (b) and (c). Objective 2(b) was investigated in two studies (Chapter 3, Study 2 and Study 3). All of these studies investigate the various impacts of reduced pack sizes of paracetamol for sale in England and Wales.
-
Chapter 4 outlines the research relating to objective 2(d), evaluating the effects of the withdrawal of co-proxamol from the England and Wales markets.
-
Chapter 5 outlines the research on antidepressant toxicity relating to objective 2(e).
-
Chapter 6 details the findings of a study relating to objective 3 regarding variations in self-harm service delivery across 32 centres in England.
-
Chapter 7 relates to objective 4(a) and describes the findings of a study carried out to develop and pilot a contact-based intervention to reduce self-harm.
-
Chapter 8 relates to objective 4(b) and details the pilot testing of a letter-based intervention aimed at reducing self-harm specifically among patients discharged from psychiatric hospitals.
-
The final chapter, Chapter 9, brings together all of our findings and discusses their relevance to suicide prevention practice and policy.
Each of these chapters presents a brief introduction outlining the context of the substudy and relevant previous literature, the methods used, the main findings and a discussion of the key implications of the findings.
Definitions
Throughout the report, ‘self-harm’ is defined as intentional self-poisoning or self-injury, irrespective of type of motivation, including degree of suicidal intent. 25 It therefore includes acts with clear suicidal intent, those with varying lesser degrees of suicidal intent and those in which suicidal intent was absent but the behaviour would have been intended to have other outcomes (e.g. communication of distress, cessation of consciousness, relief of tension). ‘Suicide’ is defined as an act of self-harm that results in death.
Chapter 2 The influence of changes in coroners' practices on the validity of national suicide rates in England
Abstract
Reliable mortality statistics are critical for monitoring trends in suicide and identifying appropriate priorities for prevention. We used coroners' inquest records for possible suicides (n = 2086) carried out in 12 areas of England in 1990–1, 1998 and 2005 together with Ministry of Justice data for all inquests throughout England in 2001–2 and 2008–9 to investigate temporal changes in the validity of national suicide statistics. In addition to the data from these years, we also used the coroners' inquest data from 2006 and 2007 to investigate the possible underestimation of suicide from co-proxamol, paracetamol and TCA poisoning when estimates are based only on deaths given suicide and open verdicts.
Between 1990 and 2005, the proportion of researcher-defined suicides given a suicide verdict by coroners decreased by 7% [p(trend) = 0.001], largely because of an increased use of accident/misadventure verdicts for researcher-defined suicides, particularly for deaths involving poisoning. The numbers of suicides by co-proxamol, paracetamol and TCA poisoning are underestimated by between 12% (co-proxamol) and 26% (paracetamol) when estimates are based on suicide and open verdict deaths alone.
In our analysis of national Ministry of Justice data we found a marked rise in the use of narrative verdicts and wide geographical variation in their use, with up to 50% of deaths in some areas receiving a narrative verdict. Coroners who gave more narrative verdicts gave fewer suicide verdicts (r = − 0.41, p < 0.001). In the 10 coroners' areas where the highest proportions of narrative verdicts were given, the officially recorded incidence of suicide decreased by 16% between 2001–2 and 2008–9, whereas in the areas served by the 10 coroners who used narratives infrequently the officially recorded incidence of suicide increased by 1%. This indicates that the use of narrative verdicts may distort local suicide statistics. Taken together, these findings indicate (1) that the ONS should consider including ‘accidental’ deaths by poisoning with medicines in the statistics available for monitoring trends in national suicide rates and (2) that small-area suicide rates, and changes in these rates over time since 2000, should be interpreted with caution. Further increased use of narrative verdicts will compromise the quality of national suicide statistics.
Background
Reliable mortality statistics are critical for assessing the population burden of suicide, as well as for developing prevention strategies and monitoring their impact on suicide rates. Officially reported suicide rates in England are derived from figures for the underlying cause of death produced by the ONS. ONS suicide statistics are based on death certificates provided by coroners following their investigation of a possible suicide. The cause of death information provided by coroners on death certificates is assessed by ONS coders who follow internationally agreed rules [currently the International Classification of Diseases, Tenth Edition (ICD-10)] to assign an underlying cause of death to all deaths.
The likelihood that a death was self-inflicted is not always clear-cut. The legal criteria used by coroners to determine whether a death was suicide mean that it must be clear beyond reasonable doubt that the deceased had intended to take his or her life. When coroners are uncertain about an individual's intent, or if it is unclear whether the death was self-inflicted or accidental, they may give either an open verdict or, in more recent years, a narrative verdict.
In contrast to the legal definition of suicide, clinicians and researchers assess the likelihood that a death was suicide on the balance of probability, and research has shown that a high proportion of deaths given an open verdict by coroners are highly likely to be suicides. 26–28 For this reason, ONS suicide statistics and monitoring of suicide trends in the National Suicide Prevention Strategy3 are based on deaths given suicide verdicts by coroners as well as a high proportion of open verdict deaths.
Narrative verdicts record in several sentences how, and in what circumstances, the death occurred, rather than giving a single short-form verdict such as suicide, open or accidental death. 10,29 Use of narrative verdicts increased exponentially between 2001 and 2009; they now account for over 10% of all verdicts given by coroners (n = 3012 in 2009). 29 This increased use has potentially important implications for the estimation of national suicide rates, as ONS's interpretation of international death coding rules mean that, when suicide intent is uncertain from such narrative accounts, as is often the case, the ONS code such deaths as accidents. The ONS gave the following example of a narrative verdict in a recent publication:29
Mr X, after being found hanging in his cell at X youth offenders institution on [date], died on [date] at X infirmary. It was a serious omission by X youth offenders institution not to have informed X’s parents on each occasion that X had self-harmed. The jury’s verdict is that X died from hanging.
Because intent was not mentioned within the narrative, the death was classified by the ONS as accidental, but suicide is strongly implied.
As well as the recent impact of narrative verdicts on suicide rates, two further issues are of more long-standing importance in relation to the interpretation of suicide statistics. First, some deaths that are considered by clinicians to be probable suicides are given accidental verdicts by coroners. 30,31 Such deaths are not considered as possible suicides by the ONS, although it recognises that a proportion of these deaths are likely to be ‘missed’ suicides. 32 If coroners' practices regarding their relative use of short-form open verdict and accidental verdict cause of death categories change over time, this may distort apparent secular trends in suicide rates. In Australia, an increasing trend in recording of possible suicides as accidental deaths is thought to have exaggerated an apparent decline in suicide rates, although the degree of impact is debated. 33,34 Second, there are > 100 coroners in England and they vary both in the criteria that they use in determining the likelihood that a death was suicide35,36 and in their use of narrative verdicts. 37 These variations may distort small-area differences in suicide rates as geographical patterning may be influenced by the local coroner's practice as well as real area differences in self-inflicted deaths.
Objectives
The original aim of this element of our research programme was to quantify the extent to which suicide rates and secular trends in suicide may be over- or underestimated when they are based on deaths given suicide and open verdicts by coroners (as was then the case). We were interested in determining whether there had been changes over time in the frequency of use of accidental/misadventure verdicts for possible suicides and their impact on suicide rates. We also used data obtained in this strand of the research programme to investigate whether suicides by co-proxamol, paracetamol and TCA poisoning are underestimated when estimates are based only on those deaths given a suicide or an open verdict by coroners.
As described earlier, an additional emerging issue concerning the accuracy of national suicide statistics – the rise in the use of narrative verdicts by coroners – became apparent over the course of the research programme. We therefore extended the brief of this element of our programme to additionally investigate the impact of the growth in use of narrative verdicts on small-area suicide rate estimates.
Methods
Examination of coroners’ inquest records
To investigate the impact on trends in national suicide rates of possible changes in coroners' use of different verdicts for likely suicides, we examined the inquest records of a sample of 12 of the 107 coroners' jurisdictions in England in 2005. Our sample comprised the three coroners whose jurisdictions covered the three collaborating research centres (the cities of Bristol, Oxford and Manchester) and a random sample of nine further jurisdictions within 90 minutes' travel time of each of these three centres. Four of the study jurisidictions were urban, three were rural and five were mixed urban/rural. We have previously conducted collaborative studies with these 12 coroners. Ministry of Justice data38 indicate that the relative proportions of suicide, accident/misadventure, open and other (mainly narrative) verdicts given by our sample of 12 coroners in 2005 were broadly similar to those in England as a whole in that year (participating vs. non-participating jurisdictions: suicide 14.3% vs. 19.3%; accident/misadventure 62.7% vs. 53.5%; open 13.5% vs. 15.1%; other 9.6% vs. 12.1%).
Sample size
The sample size for this study was based on our experience working with the Bristol coroner in a previous study30 in which 10% of people identified as definite or probable suicides by the research team were given a misadventure or an accident verdict by the coroner (unpublished data). Based on an estimated 400 suicides per year across the areas served by the 12 coroners with whom we had previous collaborative links, we estimated that we were able to detect (80% power, 5% level of statistical significance) a change in the proportion of missed suicides (researcher-defined suicides given accident/misadventure verdicts by coroners) from 10% to 4% (if this practice was decreasing) or from 10% to 17% (if the practice was growing) between 1990 and 2005. Differences of this size are large enough to have an impact on apparent secular trends in suicide.
Data collection
The records available to us in each of the 12 coroners' districts differed somewhat, as did the approach used by coroners to index records according to verdict. We searched coroners' electronic databases and ledgers or, if neither of these was available, we manually searched all inquest files for information on all cases assigned a verdict of suicide or an open, narrative or accident/misadventure verdict when the death had occurred in 1990 (1991 for one jurisdiction where 1990 data were no longer available), 1998 or 2005. A 15-year period was selected based on our desire to examine a long enough period to detect gradual changes in practice and for the practical consideration that, if we had studied a longer time period, older inquest files might have been destroyed. To increase the sample size for our analysis of deaths from co-proxamol, paracetamol and TCA poisoning, we extended our search of coroners' records to include deaths occurring in 2006 and 2007.
Exclusions
We extracted data using a structured form (see Appendix 1) on all suicides and possible suicides assigned open, narrative or accident/misadventure verdicts. We excluded all deaths that occurred outside the UK and those where the deceased was aged < 10 years, as suicide is rare in this age group. We also excluded deaths for which the cause was clearly not suicide, for example industrial disease; post-surgery deaths; burns for which the fire report indicated an accidental cause; falls that were not from a height (e.g. slips on pavements); and other deaths for which suicide was an extremely unlikely cause or impossible to determine, such as decomposed bodies on which, because of the state of the body, blood tests could not be carried out (or were negative) and there was no other evidence of self-harm. Furthermore, we excluded people given accident/misadventure verdicts in which the cause of death was a vehicular accident or poisoning by a drug of abuse only (e.g. alcohol, heroin), as our previous experience suggested that accidental deaths from these causes are difficult to distinguish from suicides. We included cases given open verdicts in which the death had been caused by a traffic accident or drug of abuse if there was any evidence in the records of current or past emotional distress.
Classification of cause of death
After the exclusions listed above, all remaining deaths given open or accident/misadventure verdicts were defined as possible suicides. These deaths included approximately 50% of all open verdict deaths but < 10% of accident verdict deaths across the 12 coroners' districts. For all possible suicides assigned an open, a narrative or an accident/misadventure verdict, data were extracted from coroners' files on sociodemographic and economic characteristics and clinical characteristics of the death, as well as on circumstances leading up to the death and information retrieved from the death scene. In particular, we recorded details of contact with psychiatric services, whether there had been a previous episode of self-harm, whether there had been a suicide note, and the levels of medication and alcohol in post-mortem blood samples. Vignettes of up to 800 words in length, based on information recorded in coroners' inquest records and witness statements, were written for all possible suicide cases. These described in detail the relevant history and circumstances leading to the death.
Three clinical members of the research team (DG, KH, NK) with extensive experience in suicide research read the vignettes and other data recorded about the possible suicides, blind to year of death, the identity of the coroner and the verdict assigned. They then independently rated the likelihood of suicide as high, moderate, low or unclear. When there was disagreement, consensus decisions were reached on whether a case was a probable suicide or not (see Appendix 2 for a description of the protocol followed). Cases rated as being of high or moderate likelihood of suicide were included in our sample of researcher-defined suicides together with those given suicide verdicts by the coroner.
Verdicts given to probable suicides by co-proxamol, paracetamol and tricyclic antidepressant poisoning
We identified all deaths by poisoning with co-proxamol, paracetamol and TCAs that were investigated by the 12 study coroners for the years 1990–1, 1998 and 2005–7. We excluded from this analysis deaths given narrative verdicts, as we could not be sure how such deaths would be coded by the ONS. We analysed separately total deaths for which some mention of one of these particular drugs was made in combination with other drugs and deaths for which no other drugs (except alcohol) were mentioned in the coroners' reports, that is, ‘pure’ poisoning.
Use of Office for National Statistics data
To investigate the relationship between researcher-defined suicides and coding of death by the ONS for use in national statistics, data on the numbers of suicides, undetermined deaths [International Classification of Diseases, Ninth Edition (ICD-9) E980–E989, ICD-10 Y10–Y34] and accidental/misadventure deaths (for which the cause of death, such as self-poisoning, jumping/falling or hanging, was similar to that for the undetermined and suicide cases) during 1998 and 2005 were provided by the ONS for 11 of the 12 coroners' jurisdictions. These data were available for only 9 of the 12 jurisdictions for deaths in 1990.
Data analysis
Analyses were carried out using Stata version 11.2 for Windows (StataCorp LP, College Station, TX, USA). Descriptive and logistic regression analyses were used to assess temporal change in the use of verdicts (suicide and open vs. accidental/misadventure) that might have led to an underestimate of suicides using official data. Using a chi-squared test for trend, we investigated whether there was any statistical evidence that the proportion of researcher-defined suicides receiving an accident/misadventure verdict increased across the three time periods included in this study. We then carried out a logistic regression analysis to determine whether any trends in the proportion of deaths receiving accident/misadventure verdicts were explained by changes in the characteristics of the people who had suicided (in terms of age and sex) or the methods that they used (hanging, self-poisoning, drowning, jumping or other method). The latter characteristic was included because an individual's choice of method influences the verdict that he or she receives: some more ‘ambiguous’ methods such as overdose and drowning are more likely to receive open or accidental verdicts than methods such as hanging. 39 We fitted an unadjusted model including year of death as an ordered categorical variable. We then investigated the impact of including terms for age, sex and suicide method in the model on the association between year of death and verdict. Descriptive data were also used to identify the proportion of researcher-defined suicides with an accident/misadventure verdict, by method, as a proportion of all cases using that method and coded as accidental by the ONS.
Analysis of Ministry of Justice data on narrative verdicts
To investigate the impact on suicide rates of the growth in use of narrative verdicts, we obtained data on the number and types of coroners' verdicts for the 113 jurisdictions in England and Wales for 2008–9 from annual statistics published by the Ministry of Justice. 40 We excluded data for the Isles of Scilly and the Queen's Household because of the very small numbers of deaths in these jurisdictions.
To investigate geographical variation in the use of narrative verdicts we used a proxy measure: the number of verdicts classified as ‘other’ verdicts by the Ministry of Justice. ONS data suggest that approximately 80% of ‘other’ verdicts in 2008 and 2009 were narrative verdicts. 29 We were unable to obtain data on the specific numbers of narrative verdicts by coroner jurisdiction as the Ministry of Justice receives data on the breakdown of ‘other’ verdicts from only around three-quarters of coroners and these data are of varying quality, making the estimation of narrative verdicts at this level difficult (Mark Edwardes, Ministry of Justice, 1 July 2011, personal communication).
To investigate the possible impact of the use of narrative verdicts on apparent trends in suicide we compared changes in suicide rates between 2001–2 and 2008–9 in the English local authorities (LAs) served by the 10 coroners who gave the highest proportion of ‘other’ verdicts and the 10 LAs whose coroners gave the lowest proportion of such verdicts. We combined suicide data for these two 2-year periods to reduce the impact of small-area variations in suicide rates based on small numbers of events. We obtained the suicide data [ICD-10 codes X60–X84 (suicide – ‘Intentional self harm’) and Y10–Y34 (open verdicts – ‘Event of undetermined intent’)] for the LA served by each coroner from the National Compendium of Clinical and Health Indicators. 41 As this source includes data for England only, this part of our analysis was restricted to English LAs. Because many coroners serve more than one LA, we present rates for all LAs within relevant coroners' jurisdictions and pooled LA rates for the top and bottom 10 coroners' jurisdictions.
Data analysis
We used Spearman's rank correlation coefficients to investigate associations between use of ‘other’ verdicts and deaths certified as suicide, open, due to natural causes, accidental or due to industrial disease – the five most frequently used verdicts. Weighted mean rates of suicide for the 10 coroners making the most frequent use of narrative verdicts and the 10 using them least often were calculated by summing the total number of suicides in each LA and dividing this by the sum of the populations of these LAs.
Results
Examination of coroners’ records
Search of the coroners' records for 1990–1, 1998 and 2005 led to the retrieval of 1296 coroner-defined suicides and 790 cases of possible suicide. Amongst the 790 cases of possible suicide, 518 (65.6%) had been assigned an open verdict, 240 (30.4%) a verdict of accident or misadventure and 32 (4.1%) a narrative verdict.
The 790 possible suicides were reviewed independently by DG, KH and NK. They agreed on the inclusion/exclusion of 632 (80.0%) of the cases without the need for discussion. The remaining 158 (20.0%) cases were discussed face to face or by teleconference. Following this review, more than three-quarters of the possible suicides assigned an open (415/518, 80.1%) or narrative verdict (25/32, 78.1%) by the coroner were rated as suicide, as were about half (131/240, 54.6%) of those with an accident/misadventure verdict. Altogether, 571 (72.3%) of 790 possible suicides with a non-suicide verdict were rated as suicide (Table 1).
| Verdict | No. of cases of possible suicidea | No. (%) rated as suicide |
|---|---|---|
| Open | 518 | 415 (80.1) |
| Accident/misadventure | 240 | 131 (54.6) |
| Narrative | 32 | 25 (78.1) |
| Total | 790 | 571 (72.3) |
Characteristics of researcher-defined suicides
Subsequent analyses were based on the 1867 researcher-defined suicide cases: the 1296 (69.4%) cases assigned a verdict of suicide by the coroners and 571 (30.6%) cases with an open, accidental or narrative verdict assessed as probable suicides by the research team. Three-quarters (1405/1867, 75.3%) of the suicide cases involved males. The median age was 41 years, with males (median age 40 years) slightly younger than females (median age 46 years). The most common methods used for suicide were hanging (689/1867, 36.9%) and self-poisoning (521/1867, 27.9%).
The characteristics of the researcher-defined suicide cases in 2005, stratified by the coroner's verdict, are shown in Table 2. We restricted this analysis to data for 2005 – because of resource constraints we did not record detailed clinical information on cases given a coroner's verdict of suicide in 1990–1 or 1998. Suicide cases tended to be older (mean age 46.2 years) than those receiving open or accident/narrative verdicts (mean age 42.6 years and 40.7 years respectively). Cases given suicide verdicts were somewhat more likely to be male than those given ‘other’ verdicts: 79% of suicide verdicts involved males compared with 69% of open verdicts and 73% of accident/narrative verdicts. The proportion of cases who had previously self-harmed or who had a history of contact with specialist mental health services was similar across the three categories of verdict. Surprisingly, 11% of those given open verdicts and 15% given accidental/narrative verdicts left a suicide note but despite this did not receive a suicide verdict. Method of suicide differed markedly across verdict categories. Deaths by self-poisoning and drowning accounted for over half of open and accident/narrative verdict cases whereas they accounted for less than one-quarter of all cases given a suicide verdict. It is noteworthy that 40 open verdict deaths and 15 accident/narrative verdict deaths (9.6% of all researcher-defined suicides) were by hanging.
| Characteristic | Coroner's verdict | |||
|---|---|---|---|---|
| Suicide (n = 388) | Open (n = 126) | Accident/narrative (n = 79) | Total (n = 593) | |
| Mean age, years | 46.2 | 42.6 | 40.7 | 44.7 |
| Male, n (%) | 307 (79.1) | 87 (69.0) | 58 (73.4) | 452 (76.2) |
| Current or past contact with psychiatric services, n (%)a | 189 (56.3) | 72 (64.9) | 43 (65.2) | 304 (59.3) |
| Suicide note, n (%)b | 193 (50.9) | 14 (11.3) | 12 (15.2) | 219 (37.6) |
| Previous self-harm, n (%)c | 187 (54.5) | 61 (53.0) | 31 (46.3) | 279 (53.1) |
| Suicide method, n (%) | ||||
| Self-poisoning | 66 (17.0) | 55 (43.7) | 37 (46.8) | 158 (26.6) |
| Hanging | 221 (57.0) | 35 (27.8) | 20 (25.3) | 276 (46.5) |
| Car exhaust gas | 18 (4.6) | 1 (0.8) | 0 (0) | 19 (3.2) |
| Jumping/falling | 17 (4.4) | 10 (7.9) | 5 (6.3) | 32 (5.4) |
| Rail | 16 (4.1) | 4 (3.2) | 4 (5.1) | 24 (4.0) |
| Fire/burns | 7 (1.8) | 2 (1.6) | 4 (5.1) | 13 (2.2) |
| Drowning | 6 (1.5) | 11 (8.7) | 7 (8.9) | 24 (4.0) |
| Other | 37 (9.5) | 8 (6.3) | 2 (2.5) | 47 (7.9) |
Temporal change in verdicts assigned by coroners to researcher-defined suicide cases
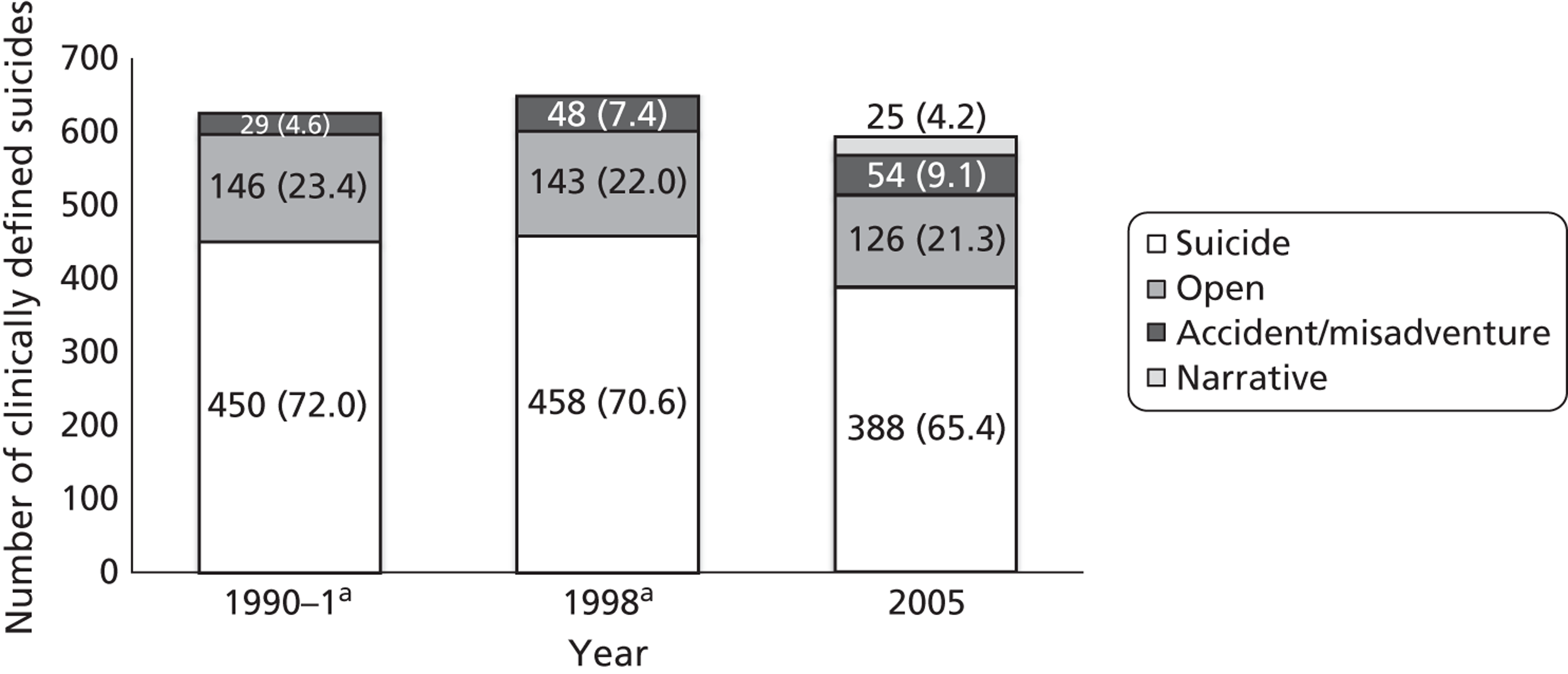
In keeping with national suicide statistics,42 the number of suicide cases that we identified from our sample of 12 coroners rose between 1990 and 1998 before falling between 1998 and 2005. In 1990–1, 72.0% [95% confidence interval (CI) 68.3% to 75.5%] of researcher-defined suicide cases in our sample had been assigned a verdict of suicide by the coroner. By 2005 this had decreased somewhat to 65.4% (95% CI 61.4% to 69.2%) (Figure 1). There was also a slight decrease in researcher-defined suicide cases assigned an open verdict between 1990–1 and 2005. In contrast, the proportion of researcher-defined suicide cases with a coroner's verdict of accident/misadventure nearly doubled between 1990 and 2005, from 4.6% (95% CI 3.1% to 6.6%) to 9.1% [95% CI 6.9% to 11.7%; p(trend) = 0.02]. Most of this rise was due to an increase in the number of cases of researcher-defined suicide by self-poisoning. In 1990–1, 12.3% (20/163) of cases of researcher-defined suicide by self-poisoning had been assigned an accidental verdict by the coroner; this increased to 22.2% (35/158) in 2005. In logistic regression models controlling for age, sex and method of suicide, statistical evidence for the trend towards increasing use of accidental verdicts for probable suicides increased [p(trend) = 0.001]. This indicates that neither changes in the age/sex distribution of suicides nor changes in the methods used account for the observed increase in use of accidental verdicts for probable suicides.
FIGURE 1.
Number (%) of researcher-defined suicide cases (all methods) assigned each verdict for deaths in 1990–1, 1998 and 2005. a, No narrative verdicts were recorded in 1990–1 or 1998. Source: Gunnell D, Bennewith O, Simkin S, Cooper J, Klineberg E, Rodway C, et al. Time trends in coroners' use of different verdicts for possible suicides and their impact on officially reported incidence of suicide in England: 1990–2005 [published online ahead of print 1 November 2012]. Psychol Med 2012. http://dx.doi.org/10.1017/S0033291712002401. Reprinted with the permission of Cambridge University Press.
Temporal change in the use of accident verdicts for researcher-defined suicide across coroners' jurisdictions
An examination of verdicts stratified by coroner jurisdiction showed an increase in the use of the accident/misadventure verdict for researcher-defined suicide between 1990 and subsequent years for most of the 12 coroners' jurisdictions (Table 3). The jurisdiction with the highest number of researcher-defined suicides with a verdict of accident/misadventure in 2005 (n = 24, coroner A) also had the highest increase in the use of that verdict, from 3.4% (4/117) of all researcher-defined suicides in 1990 to 22.6% (24/106) in 2005. When a sensitivity analysis was carried out, excluding data for this coroner, the magnitude of the temporal increase in the use of the accident/misadventure verdict was diminished [1990–1: 25/508, 4.9%, 95% CI 3.2% to 7.2% use of the accident/misadventure verdict; 2005: 30/487, 6.2%, 95% CI 4.2% to 8.7%; p(trend) = 0.3].
| Year | Researcher-defined suicide cases given an accident/misadventure verdict, n (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | K | L | Total | |
| 1990 | 4 (3.4) | 7 (10.3) | 1 (4.6) | 0 (0.0) | 0 (0.0) | 1 (5.6) | 6 (12.0) | 2 (3.1) | 4 (9.1) | 1 (2.2) | 0 (0.0) | 3 (4.8) | 29 (4.6) |
| 1998 | 19 (19.2) | 6 (8.2) | 0 (0.0) | 5 (19.2) | 0 (0.0) | 1 (5.6) | 1 (1.9) | 4 (5.3) | 3 (6.5) | 4 (7.4) | 2 (3.3) | 3 (3.9) | 48 (7.4) |
| 2005 | 24 (22.6) | 2 (3.0) | 0 (0.0) | 3 (14.3) | 2 (8.0) | 2 (10.5) | 3 (4.6) | 1 (2.2) | 4 (9.1) | 3 (5.4) | 2 (3.7) | 8 (11.1) | 54 (9.1) |
Method of death for cases assigned a verdict of accident/misadventure
Using ONS data on the total number of accidental deaths by each method, around half of all poisoning, rail, hanging and car exhaust gas deaths in 1998 and 2005 assigned an accident/misadventure verdict across 11 coroners' jurisdictions were judged to be suicides in our study (Table 4). These proportions are probably somewhat overestimated as information in the coroners' files available to the research team enabled us to clearly identify the suicide method used, but such information was not available to the ONS when it coded the death certificates. For example, the death certificates of some rail suicide cases state cause of death as ‘multiple injuries’ without mentioning that these occurred on the railway; similarly, a few deaths by hanging were recorded on death certificates as due to asphyxiation.
| Suicide method | No. of accident/misadventure deaths recorded by the ONS for the 11 coroners | Researcher-defined suicide cases coded as accident/misadventure, n (%) |
|---|---|---|
| Self-poisoninga | 102 | 51 (50.0) |
| Hanging | 27 | 12 (44.4) |
| Car exhaust gas | 4 | 2 (50.0) |
| Jumping/falling | 645 | 6 (0.9) |
| Rail | 10 | 6 (60.0) |
| Fire/burnsb | 81 | 4 (4.9) |
| Drowning | 42 | 9 (21.4) |
Verdicts given to probable cases of suicide by co-proxamol, paracetamol and tricyclic antidepressant poisoning
In 1990–1, 1998 and 2005–7, the 12 coroners investigated 91 deaths from co-proxamol poisoning, 107 from paracetamol poisoning and 161 from TCA poisoning. Most of these deaths were assigned a researcher-defined verdict of probable suicide (Table 5).
Most deaths from pure co-proxamol poisoning (74/76, 97.4%) were thought by the research team to be likely suicides. Nine (12.2%) of the 74 probable cases of suicide would have been excluded from analyses focusing only on coroner-defined suicide and open verdict deaths because they were given accidental death verdicts. In fact, the research team classified as probable cases of suicide most of the pure co-proxamol poisoning deaths (9/11, 81.8%) receiving accidental verdicts from the coroners.
The research team also classified the majority of deaths from pure paracetamol poisoning (65/81, 80.2%) as probable cases of suicide. Seventeen (26.2%) of the 65 probable suicides from paracetamol would have been excluded from analyses focusing only on coroner-defined suicide and open verdict deaths because they were given accidental death verdicts. In fact, almost two-thirds (17/28, 60.7%) of the pure paracetamol poisoning deaths receiving accidental verdicts were also thought to be probable cases of suicide.
Most deaths from pure TCA poisoning (108/115, 93.9%) were assigned a researcher-defined verdict of suicide. Eighteen (16.7%) of the 108 probable suicides would have been excluded from analyses focusing only on coroner-defined suicide and open verdict deaths because they were given accidental death verdicts. The researcher team also thought that almost three-quarters (18/25, 72.0%) of pure tricyclic poisoning deaths receiving accidental verdicts were probable cases of suicide.
For all three substances, analyses based on mixed overdoses yielded similar conclusions.
| Cause of death | Suicide | Open | Accident/misadventure | Total deaths, n | Total RD suicides, n (% of total deaths) | |||
|---|---|---|---|---|---|---|---|---|
| CD suicide, n (% of total deaths) | RD suicide, n (% of total RD suicides) | CD open, n (% of total deaths) | RD suicide, n (% of total RD suicides) | CD accident/misadventure, n (% of total deaths) | RD suicide, n (% of total RD suicides) | |||
| Co-proxamol | ||||||||
| ‘Pure’ poisoning deaths | 38 (50.0) | 38 (51.4) | 27 (35.5) | 27 (36.5) | 11 (14.5) | 9 (12.2) | 76 | 74 (97.4) |
| Total poisoning deaths | 47 (51.6) | 47 (52.8) | 31 (34.1) | 31 (34.8) | 13 (14.3) | 11 (12.4) | 91 | 89 (97.8) |
| Paracetamol | ||||||||
| ‘Pure’ poisoning deaths | 32 (39.5) | 32 (49.2) | 21 (25.9) | 16 (24.6) | 28 (34.6) | 17 (26.2) | 81 | 65 (80.2) |
| Total poisoning deaths | 46 (43.0) | 46 (51.1) | 26 (24.3) | 21 (23.3) | 35 (32.7) | 23 (25.6) | 107 | 90 (84.1) |
| TCAs | ||||||||
| ‘Pure’ poisoning deaths | 53 (46.1) | 53 (49.1) | 37 (32.2) | 36 (33.3) | 25 (21.7) | 18 (16.7) | 115 | 107 (93.0) |
| Total poisoning deaths | 76 (47.2) | 76 (51.4) | 47 (29.2) | 45 (30.4) | 38 (23.6) | 27 (18.2) | 161 | 148 (91.9) |
Analysis of Ministry of Justice data on verdicts given by coroners and local authority suicide data
In 2008 and 2009, coroners delivered 58,777 inquest verdicts: 28,996 in 2008 and 29,781 in 2009. The mean annual number of verdicts given per coroner was 262 (range 17–979). Of these, the most common verdict (figures for 2009) was accident or misadventure (n = 8673, 29%), closely followed by natural causes (n = 8281, 28%); there were 3797 (13%) ‘other’ (mainly narrative) verdicts, 3330 (11%) suicide verdicts and 2240 (8%) open verdicts.
There is considerable variation between jurisdictions in the proportion of inquest outcomes recorded as ‘other’ (mainly narrative) verdicts: these ranged from 0% to 50% (median 9%) of all inquests. Table 6 shows the number (%) of verdicts given by the coroners in the 10 jurisdictions with the highest proportionate use of ‘other’ verdicts in 2008 and 2009 and by the coroners in the 10 jurisdictions with the lowest proportionate use of ‘other’ verdicts in 2008 and 2009. Jurisdictions ranked in the top 10 gave ‘other’ verdicts in > 20% of inquests whereas jurisdictions in the bottom 10 gave ‘other’ verdicts in < 2% of cases. In Birmingham and Solihull an ‘other’ verdict was recorded in 985 (50.3%) of the 1958 inquests. The proportions of suicide verdicts were higher in the bottom 10 jurisdictions, with a mean proportion of 15.2% compared with 9.3% in the top 10 jurisdictions. Of note, the jurisdictions with the greatest proportion of ‘other’ verdicts seem to also deal with a higher number of inquests overall, with an average of 669 inquests in 2008 and 2009 compared with an average of 450 across England and Wales. Conversely, jurisdictions with a lower proportion of ‘other’ verdicts dealt with a lower average number of inquests over the same period (mean 218 per year).
Analysis based on all 113 jurisdictions confirmed that the use of ‘other’ (mainly narrative) verdicts was inversely related to the recording of suicide verdicts (r = − 0.41, p < 0.001), although there was only a weak association with the proportion of open verdicts (r = − 0.16, p = 0.09) (Table 7). There was no association between the proportion of natural death verdicts given by coroners and their use of ‘other’ verdict categories (r = 0.01), although the proportion of accidental death verdicts was also inversely associated with ‘other’ verdicts (r = − 0.50, p < 0.001). Surprisingly, there was no association between the proportions of suicide verdicts and open verdicts given by coroners (r = 0.02, p = 0.8).
| Position of Coroner's jurisdiction based on their use of ‘other’ verdicts | Coroner jurisdiction | Populationa | Total no. of inquests | No. (%) of ‘other’ verdicts | No. (%) of suicide verdicts | No. (%) of open verdicts |
|---|---|---|---|---|---|---|
| Top 10 coroners' jurisdictions ranked according to percentage of ‘other’ verdicts | Birmingham and Solihull | 1,233,900 | 1958 | 985 (50.3) | 36 (1.8) | 60 (3.1) |
| Cardiff and Vale of Glamorgan | 460,800 | 830 | 258 (31.1) | 34 (4.1) | 69 (8.3) | |
| Stoke-on-Trent and North Staffordshire | 458,900 | 820 | 237 (28.9) | 50 (6.1) | 36 (4.4) | |
| North Lincolnshire and Grimsby | 318,100 | 290 | 82 (28.3) | 42 (14.5) | 13 (4.5) | |
| Telford and Wrekin | 162,300 | 147 | 38 (25.9) | 20 (13.6) | 10 (6.8) | |
| South and East Cumbria | 226,500 | 329 | 85 (25.8) | 23 (7.0) | 22 (6.7) | |
| Blackburn, Hyndburn and Ribble Valley | 278,700 | 641 | 145 (22.6) | 51 (8.0) | 14 (2.2) | |
| Wolverhampton | 238,500 | 232 | 50 (21.6) | 17 (7.3) | 29 (12.5) | |
| Suffolk | 714,100 | 555 | 116 (20.9) | 94 (16.9) | 78 (14.1) | |
| Preston and West Lancashire | 708,700 | 883 | 184 (20.8) | 117 (13.3) | 39 (4.4) | |
| Bottom 10 coroners' jurisdictions ranked according to percentage of ‘other’ verdicts | Central Hampshire | 347,500 | 388 | 5 (1.3) | 59 (15.2) | 36 (9.3) |
| York City | 198,800 | 197 | 3 (1.5) | 34 (17.3) | 12 (6.1) | |
| North and West Cumbria | 268,700 | 222 | 3 (1.4) | 38 (17.1) | 25 (11.3) | |
| Blackpool/Fylde | 216,300 | 235 | 3 (1.3) | 43 (18.3) | 15 (6.4) | |
| North West Kent | 338,200 | 416 | 3 (0.7) | 59 (14.2) | 39 (9.4) | |
| Isle of Wight | 140,200 | 156 | 2 (1.3) | 15 (9.6) | 27 (17.3) | |
| Ceredigion | 76,400 | 76 | 1 (1.3) | 8 (10.5) | 4 (5.3) | |
| Western Dorset | 160,800 | 156 | 1 (0.6) | 21 (13.5) | 39 (25.0) | |
| Carmarthenshire | 180,800 | 175 | 0 (0.0) | 33 (18.9) | 15 (8.6) | |
| Pembrokeshire | 117,400 | 158 | 0 (0.0) | 27 (17.1) | 4 (2.5) |
| Verdict | r | p-value |
|---|---|---|
| Other and suicide | − 0.41 | < 0.001 |
| Other and open | − 0.16 | 0.090 |
| Other and natural death | 0.01 | 0.904 |
| Other and accidental death | − 0.50 | < 0.001 |
| Other and industrial disease | − 0.03 | 0.715 |
The weighted average change in the rate of suicide between 2001–2 and 2008–9 was − 16% (95% CI − 27% to 5%) in the 30 LA areas served by the 10 English coroners' jurisdictions giving the highest proportions of ‘other’ (mainly narrative) verdicts (Table 8); in the 30 LA areas served by the 10 English coroners' jurisdictions giving the lowest proportions of ‘other’ verdicts the rate did not change (0%, 95% CI − 15% to 6%) (Table 9). There was weak statistical evidence that these two changes in rates differed: difference in rates 1.51 (95% CI − 0.14 to 3.36) per 100,000 (p = 0.09). These findings were based on suicide data for England and so we were unable to include the four Welsh LAs listed in Table 6 in this analysis.
| Coroner jurisdiction | LA | Population | Average rate 2001–2b | Average rate 2008–9b | Difference (%) |
|---|---|---|---|---|---|
| Birmingham and Solihull | Birmingham MCD | 1,028,700 | 10.11 | 7.08 | − 3.03 (− 30) |
| Solihull MCD | 205,200 | 6.14 | 4.48 | − 1.66 (− 27) | |
| Stoke-on-Trent and North Staffordshire | Stoke-on-Trent UA | 239,300 | 13.26 | 6.83 | − 6.44 (− 49) |
| Staffordshire Moorlands CD | 95,400 | 9.53 | 8.61 | − 0.93 (− 10) | |
| Newcastle-under-Lyme CD | 124,200 | 10.01 | 5.59 | − 4.42 (− 44) | |
| North Lincolnshire and Grimsby | North East Lincolnshire UA | 157,100 | 10.64 | 8.48 | − 2.16 (− 20) |
| North Lincolnshire UA | 161,000 | 8.33 | 8.73 | 0.40 (5) | |
| Telford and Wrekin | Telford and Wrekin UA | 162,300 | 10.38 | 7.82 | − 2.57 (− 25) |
| South and East Cumbria | Barrow-in-Furness CD | 70,900 | 11.97 | 7.25 | − 4.73 (− 39) |
| Eden CD | 51,800 | 2.26 | 6.31 | 4.05 (180) | |
| South Lakeland CD | 103,800 | 7.56 | 7.64 | 0.08 (1) | |
| Blackburn, Hyndburn and Ribble Valley | Blackburn with Darwen | 139,900 | 14.98 | 9.96 | − 5.02 (− 33) |
| Hyndburn | 81,100 | 10.76 | 8.74 | − 2.02 (− 19) | |
| Ribble Valley | 57,700 | 7.27 | 11.87 | 4.60 (63) | |
| Wolverhampton | Wolverhampton MCD | 238,500 | 10.30 | 9.85 | − 0.45 (− 4) |
| Suffolk | Waveney CD | 117,700 | 12.04 | 10.50 | − 1.54 (− 13) |
| Suffolk Coastal CD | 124,100 | 6.58 | 7.45 | 0.87 (13) | |
| Ipswich CD | 126,600 | 9.71 | 10.06 | 0.35 (4) | |
| Babergh CD | 85,800 | 9.75 | 7.68 | − 2.07 (− 21) | |
| Mid Suffolk CD | 94,200 | 8.33 | 10.23 | 1.90 (23) | |
| St Edmundsbury CD | 103,500 | 7.60 | 9.18 | 1.58 (21) | |
| Forest Heath CD | 62,200 | 8.56 | 13.41 | 4.85 (57) | |
| Preston and West Lancashire | Chorley | 104,800 | 8.57 | 14.24 | 5.67 (66) |
| Lancaster | 139,800 | 11.33 | 6.18 | − 5.15 (− 45) | |
| Preston | 134,600 | 11.85 | 13.52 | 1.67 (14) | |
| South Ribble | 108,200 | 8.38 | 6.65 | − 1.73 (− 21) | |
| West Lancashire | 110,200 | 3.25 | 9.15 | 5.90 (182) | |
| Wyre | 111,100 | 9.20 | 11.43 | 2.23 (24) | |
| East Riding and Hull | Kingston upon Hull, City of UA | 261,100 | 11.19 | 10.82 | − 0.38 (− 3) |
| East Riding of Yorkshire UA | 336,100 | 10.48 | 5.62 | − 4.86 (− 46) | |
| Weighted means and % mean difference (all 10 jurisdictions) | 9.82 | 8.27 | − 1.55 (− 16) |
| Coroner jurisdiction | LA | Population | Average rate 2001–2b | Average rate 2008–9b | Difference (%) |
|---|---|---|---|---|---|
| Western Dorset | West Dorset CD | 96,500 | 9.18 | 11.77 | 2.60 (28) |
| North Dorset CD | 64,300 | 4.97 | 11.96 | 7.00 (141) | |
| North West Kent | Sevenoaks CD | 113,200 | 5.53 | 4.30 | − 1.24 (− 22) |
| Tunbridge Wells CD | 107,600 | 9.69 | 10.04 | 0.35 (4) | |
| Tonbridge and Malling CD | 117,400 | 4.44 | 8.52 | 4.08 (92) | |
| Blackpool/Fylde | Blackpool UA | 140,000 | 20.99 | 12.34 | − 8.65 (− 41) |
| Fylde CD | 76,300 | 6.67 | 6.25 | − 0.42 (− 6) | |
| Isle of Wight | Isle of Wight UA | 140,200 | 13.16 | 14.68 | 1.52 (12) |
| Central Hampshire | Winchester CD | 113,300 | 7.78 | 11.29 | 3.51 (45) |
| Test Valley CD | 113,400 | 8.28 | 9.36 | 1.09 (13) | |
| Eastleigh CD | 120,800 | 9.41 | 7.20 | − 2.21 (− 23) | |
| North and West Cumbria | Allerdale CD | 94,300 | 8.90 | 13.40 | 4.50 (51) |
| Carlisle CD | 104,700 | 12.38 | 8.79 | − 3.59 (− 29) | |
| Copeland CD | 69,700 | 12.81 | 9.01 | − 3.80 (− 30) | |
| York City | York UA | 198,800 | 5.82 | 8.55 | 2.73 (47) |
| Teesside | Redcar and Cleveland UA | 137,800 | 10.65 | 10.00 | − 0.65 (− 6) |
| Middlesbrough UA | 140,100 | 12.51 | 7.96 | − 4.55 (− 36) | |
| Stockton-on-Tees UA | 189,800 | 7.98 | 8.76 | 0.78 (10) | |
| Spilsby and Louthc | East Lindsey CD | 140,800 | 7.54 | 15.16 | 7.62 (101) |
| Essex and Thurrock | Thurrock UA | 157,200 | 7.96 | 4.11 | − 3.85 (− 48) |
| Brentwood CD | 73,800 | 5.55 | 5.96 | 0.41 (7) | |
| Basildon CD | 174,100 | 7.38 | 7.29 | − 0.09 (− 1) | |
| Epping Forest CD | 124,000 | 9.53 | 4.75 | − 4.78 (− 50) | |
| Chelmsford CD | 167,800 | 4.20 | 7.75 | 3.55 (84) | |
| Maldon CD | 62,900 | 5.74 | 6.85 | 1.11 (19) | |
| Uttlesford CD | 75,600 | 6.11 | 8.56 | 2.45 (40) | |
| Braintree CD | 142,700 | 7.32 | 5.49 | − 1.84 (− 25) | |
| Colchester CD | 177,100 | 6.39 | 7.84 | 1.45 (23) | |
| Tendring CD | 148,000 | 8.31 | 4.49 | − 3.82 (− 46) | |
| Harlow CD | 80,600 | 8.36 | 3.90 | − 4.46 (− 53) | |
| Weighted mean and % mean difference (all 10 jurisdictions) | 8.56 | 8.52 | − 0.04 (0) |
Discussion
Our results support four main conclusions. First, national suicide rates may have been underestimated in recent years both because of the growth in the use of narrative verdicts29 and because of a trend for coroners to give accidental death verdicts to cases that in the past they may have given open or suicide verdicts to. If these trends continue, so too will the underestimation of suicide rates. Second, there is substantial variation between coroners in the extent to which their practices have changed. Such variation means that differences in suicide trends in different areas of England must be treated with extreme caution. Third, the main cause of accidental death where a high proportion of deaths are considered on clinical grounds to be probable suicides is death by medicine poisoning. Approximately half of accidental deaths due to poisoning by medicines are probably suicides. Fourth, estimates of total numbers of suicides by ‘pure’ poisoning with co-proxamol, paracetamol and TCAs may be underestimated by 12.2%, 26.2% and 16.8%, respectively, when these are based only on deaths receiving suicide or open verdicts.
Concerns about the accuracy of national suicide statistics are neither new27,32,35,43 nor unique to English suicide data. 44,45 Nevertheless, the issues that we have investigated suggest that, in the last 20 years, suicide rates are likely to have been underestimated to a greater extent than in previous years, and local trends in suicide may be particularly misleading. For example, health strategists in the areas served by the Birmingham and Solihull coroners, who give narrative verdicts at more than half of their inquests,37 may be falsely reassured that suicide rates in their areas are declining. Any such favourable trends may, in fact, reflect coding difficulties experienced by the ONS when it attempts to classify deaths given narrative verdicts. Similarly, recent downwards trends in English suicide rates may have been overestimated. The ONS has recently assessed the extent of possible underestimation of suicide rates: it reported that, if all deaths from hanging and poisoning given narrative verdicts by coroners and coded as accidents by the ONS were, in fact, suicides, the 2009 suicide rate would have been underestimated by 6% – a difference equivalent to almost one-third of the 2002 National Suicide Prevention Strategy's3 20% reduction target. This may be a conservative assessment because the ONS's analysis did not include other common methods of suicide, such as drowning and jumping; furthermore, Ministry of Justice data for 2010 and 2011 indicate a continuing rise in the use of narrative verdicts.
A possible contributor to changes in the pattern of coroners' verdicts over time may be an increase in the popularity of methods of suicide such as drowning and self-poisoning, in which intent can be more ambiguous. However, between 1990 and 2005, the main changes in the methods used for suicide in England and Wales were a > 50% increase in the use of hanging42 (this method accounted for over half of suicides over the study period) and a reduction in the use of all other methods. In keeping with this, our multivariable analysis controlling for differences in age and sex and methods used by people dying by suicide strengthened the statistical evidence for an increasing trend in the use of accidental verdicts for probable (researcher-defined) suicides.
The ONS suggestion that suicide rates may be underestimated by up to 6% because of the increased use of narrative verdicts, combined with our analysis indicating that 9% of researcher-defined suicides are given accidental death verdicts by coroners, suggest that suicide rates may have been underestimated by approximately 15% in England in recent years. The extent of the problem is likely to be somewhat less than this as some deaths of undetermined intent (around 20%; see Table 1) currently included in national statistics are not suicides. Evidence for the growth in use of accident verdicts for researcher-defined suicides and narrative verdicts when suicide or open verdicts might previously have been given means that decreases in suicide rates since 1990 are likely to have been overestimated. A practical impact of these trends is that they may lead to health policy-makers in England underestimating the impact of the current economic crisis on suicide or providing false reassurance concerning the magnitude of the public health problem caused by suicide in England. 10 Furthermore, the number of suicides from paracetamol poisoning and, to a lesser extent, co-proxamol and TCA poisoning will be underestimated when these are based on deaths receiving suicide and open verdicts alone.
Limitations
In our assessment of the likelihood of suicide among individuals given open, narrative or accidental verdicts by the 12 coroners in our study, there was an initial lack of consensus across the three coders for about one-fifth of the cases examined, illustrating the difficulties involved in deciding whether some cases were suicide or not. Although the coroners' jurisdictions studied comprised 10% of all jurisdictions in England and Wales, the number of jurisdictions and the variability in their size meant that a difference in practice (verdicts assigned) by a single coroner with a large jurisdiction could bias the assessment of a temporal increase in the use of the accident/misadventure verdict. Furthermore, because of resource limitations, we studied only three time periods. An analysis of data for additional years would have increased confidence in our assessment of time trends.
The main limitation of our analysis of Ministry of Justice data is that we used ‘other’ verdicts as a proxy for narrative verdicts. Nevertheless, recent ONS analysis29 indicates that this is a reasonable assumption, with over three-quarters of ‘other’ verdicts in 2008–9 being narratives. It remains possible that there are regional variations in the proportion of narratives amongst ‘other’ verdicts. The Ministry of Justice does not receive consistent nor reliable data from individual coroners on their ‘other’ verdicts, which prevents the accurate reporting of narrative verdict use in each jurisdiction.
Conclusions
National suicide statistics are crucial to public health surveillance and this research has a number of policy and public health implications. First, small area (primary care trust/LA)-specific suicide rates and trends in suicide rates should be treated with caution in those areas where local coroners make high use of narrative verdicts. Second, approaches to ensure the future reliability of national suicide statistics should be taken – these might include asking coroners to both record the short-form verdict and, when appropriate, accompany this with a longer narrative account of the death. LA medical examiners and the post of Chief Coroner may lead to improvements in reporting practices; what is clear is that approaches are needed to ensure consistency in reporting cause of death between coroners. Third, the ONS might consider including in its suicide statistics deaths from medicine poisoning given verdicts of accident/misadventure by coroners. In particular, the assessment of the overall burden of suicide from co-proxamol, paracetamol and TCA poisoning is best achieved by combining deaths from these medicines receiving suicide, open and accidental verdicts.
Chapter 3 Studies to evaluate the impact of the 1998 UK legislation restricting pack sizes of paracetamol
Abstract
In 1998, legislation was introduced restricting pack sizes of paracetamol sold over the counter in an attempt to reduce self-poisonings and paracetamol-induced hepatotoxicity. We conducted four studies related to this legislation. Analysis of mortality data for England and Wales and UK liver unit data showed that the legislation was followed by significant reductions in deaths over an 11-year period (43% or 765 fewer deaths; 990 when accidental deaths were included) and in liver transplantation for paracetamol-induced hepatotoxicity (61% fewer transplantations). Interviews with 60 general hospital patients who had been admitted after taking overdoses of ≥ 16 paracetamol tablets showed that most used paracetamol because it was readily available, although few breaches of sales guidance were reported. Evidence of media (including internet) influence on the choice of paracetamol for self-poisoning was found. Examination of data from the Multicentre Study of Self-harm in England and the National Registry of Deliberate Self Harm in Ireland indicated that, despite smaller pack sizes in Ireland, there was no major difference in overdose size between the two settings. More ‘pack equivalents’ were generally consumed in Ireland, raising questions about whether sales guidance is followed as strictly as in the UK. Finally, GP prescribing data for the UK (from IMS Health) showed that prescribing of NSAIDs following the 1998 legislation increased in line with prescribing of other analgesics, with no evidence of an increase in admissions for GI bleeds in Hospital Episode Statistics (HES) data. However, a gradual increase in use of antiulcerants may have offset any increase in incidence of GI symptoms.
Although the 1998 legislation appears to have been beneficial, the continuing toll of deaths from paracetamol overdose suggests that further initiatives may be necessary. Media (including internet) influences should be addressed.
Background
Paracetamol, an analgesic available over the counter, is the most common drug used for self-poisoning in the UK. 22,46 It is also a frequent cause of poisoning in many other countries. 47–53 If untreated, an overdose of 10–15 g (20–30 tablets) of paracetamol can result in fatal hepatotoxicity. 54,55
In September 1998, legislation was introduced by the UK government following a recommendation by the UK Medicines Control Agency (now the MHRA) restricting pack sizes of paracetamol (and other analgesics) sold through pharmacies to a maximum of 32 tablets and restricting non-pharmacy sales to 16 tablets56,57 (although MHRA guidance in 2009 suggests that up to two packs of 16 tablets can be bought from the latter58). This policy was introduced because of the large number of people taking paracetamol overdoses59–61 and the increasing numbers of deaths62 and liver transplants63 resulting from paracetamol-induced hepatotoxicity. Another motivation for the legislation was the knowledge gained from interviewing people who had presented to hospital following paracetamol overdoses, many of whom reported that the act was often impulsive and involved the use of medication already stored in the home. 64,65
Our research group showed that the UK legislation had beneficial effects in England and Wales during the first few years following its introduction in terms of paracetamol-related deaths, liver transplants and numbers of tablets consumed in overdoses. 12,66 Although other studies supported these findings,67,68 some commentators have questioned the impact of the legislation. 69,70 Furthermore, in Scotland, no evidence of an impact on deaths has been found. 71,72 More long-term studies are therefore required to assess whether or not the legislation has been a success. 68
There is also evidence that some retail outlets have not fully complied with the intention of the legislation, and that it is possible to purchase large quantities of paracetamol over the counter. 73–76 Furthermore, the increase in internet sites from which drugs can be bought is also a potential cause for concern.
In Ireland, similar legislation was introduced in October 2001,77 but pack sizes were restricted to lower maximum amounts than in the UK, namely a maximum pack size of 24 tablets in pharmacies and 12 tablets in non-pharmacy outlets, with just a single pack to be supplied in any one transaction.
One area of concern relating to the introduction of this legislation is whether the reduced paracetamol pack size may have resulted in increased use of NSAIDs, with adverse consequences in terms of GI bleeds,78 which might also be reflected in increased prescribing of drugs for GI disorders.
To investigate some of these issues, we conducted four research studies to address the following questions:
-
What has been the long-term impact of the 1998 legislation to reduce pack sizes of paracetamol in terms of deaths and liver disease?
-
What are the circumstances associated with larger overdoses of paracetamol, and are the intentions of the legislation being complied with?
-
Do differences in pack sizes of paracetamol in the UK and Ireland have an impact on overdoses of the drug?
-
Did the UK legislation on pack sizes of paracetamol result in an increased rate of GI disorders because of greater use of NSAIDs?
STUDY 1: LONG-TERM EVALUATION OF THE IMPACT OF REDUCED PACK SIZES OF PARACETAMOL ON POISONING DEATHS AND LIVER TRANSPLANT ACTIVITY IN ENGLAND AND WALES
Objective
The objective of the study was to investigate the long-term impact in England and Wales of the 1998 introduction of smaller paracetamol pack sizes on poisoning deaths, especially suicides, and liver unit activity for paracetamol-induced hepatotoxicity, in terms of registration for liver transplantation and actual transplants.
Methods
Data sources
Deaths
To evaluate the impact of the legislation on suicides, we used data on deaths receiving a suicide verdict and deaths recorded as being of undetermined intent (open verdicts) (see Chapter 2). The ONS provided quarterly information on drug-poisoning deaths (suicides, open verdicts and accidental poisonings) involving paracetamol, the more common paracetamol compounds used for self-poisoning (paracetamol with codeine, dihydrocodeine, ibuprofen or aspirin) and all drugs, based on death registrations from 1993 to 2009 in England and Wales. We did not include deaths involving the paracetamol/dextropropoxyphene compound (co-proxamol) as dextropropoxyphene is usually the lethal agent in co-proxamol poisonings and the drug was withdrawn in 200779 (see Chapter 4). We have restricted our analyses to deaths involving single drugs (paracetamol or paracetamol compounds) with or without alcohol, for individuals aged ≥ 10 years. Similar data were supplied for all deaths receiving suicide and open verdicts.
Registrations for liver transplantation and actual transplants
We used data supplied by UK Transplant (now NHS Blood and Transplant) on registrations for liver transplantation and actual liver transplants as a result of paracetamol poisoning between 1995 and 2009 in residents of England and Wales aged ≥ 10 years.
Non-fatal self-poisoning with paracetamol
We used data collected through the Oxford Monitoring System for Attempted Suicide25 (which includes all hospital presentations for self-harm) to examine trends in non-fatal overdoses involving paracetamol (in pure or compound form) throughout the period 1993–2009.
Statistical analyses
Analyses were conducted using Stata version 10.0. We used interrupted time-series analysis80 to estimate changes in levels and trends following the 1998 legislation. We compared the mean quarterly numbers of deaths and liver unit registrations and transplantations that might have occurred in the post-intervention period without the legislation with the number that occurred with the legislation. 81 The end of the third quarter of 1998 was chosen as the point of intervention. For more details of this method see Appendix 3.
In addition to the basic regression model for the analysis of paracetamol-related deaths, we included adjustment for potentially confounding trends in ‘all drug-poisoning suicide deaths’ by inclusion of ‘all drug suicide deaths excluding paracetamol' as a covariate. We also calculated a conservative estimate of the absolute effect, which assumed no increase in the number of deaths in the absence of the legislation. The absolute effect of the legislation was determined as the difference between the outcome expected at the last point of the pre-intervention period and the outcome expected at the mid-point of the post-intervention period. For analysis of liver unit registrations and transplantations we also used the basic regression model and the conservative estimate analysis.
We also conducted a sensitivity analysis to determine whether our results changed when January 1998 was used as the intervention point – this corresponds to the date when the packaging changes began to occur (9 months before the legislation).
Results
Deaths
The numbers of deaths in England and Wales between 1993 and 2009 from poisoning with all drugs and from paracetamol specifically that received suicide, open and accidental verdicts are shown in Table 10. Paracetamol poisoning deaths constituted between approximately 9% and 10% of drug-poisoning suicide deaths before the legislation and between approximately 7% and 9% after the legislation.
| Year | All causes, n | All drugs, n (%) | Paracetamol, n (%a) | Paracetamol compounds,b n (%a) | |||
|---|---|---|---|---|---|---|---|
| Suicide, open | Suicide, open | Suicide, open, accidental | Suicide, open | Suicide, open, accidental | Suicide, open | Suicide, open, accidental | |
| 1993 | 5182 | 1314 | 1897 | 132 (10.0) | 181 (9.5) | 17 (1.3) | 22 (1.2) |
| 1994 | 5090 | 1298 | 2003 | 126 (9.7) | 163 (8.1) | 15 (1.2) | 20 (1.0) |
| 1995 | 5127 | 1390 | 2140 | 122 (8.8) | 155 (7.2) | 24 (1.7) | 27 (1.3) |
| 1996 | 4910 | 1325 | 2103 | 121 (9.1) | 158 (7.5) | 24 (1.8) | 26 (1.2) |
| 1997 | 4830 | 1406 | 2252 | 149 (10.6) | 204 (9.1) | 21 (1.5) | 27 (1.2) |
| 1998 | 5347 | 1432 | 2246 | 135 (9.4) | 183 (8.1) | 16 (1.1) | 20 (0.9) |
| 1999 | 5241 | 1414 | 2294 | 113 (8.0) | 150 (6.5) | 29 (2.1) | 33 (1.4) |
| 2000 | 5081 | 1309 | 2143 | 90 (6.9) | 123 (5.7) | 29 (2.2) | 31 (1.4) |
| 2001 | 4904 | 1280 | 2176 | 108 (8.4) | 142 (6.5) | 18 (1.4) | 27 (1.2) |
| 2002 | 4762 | 1227 | 1983 | 90 (7.3) | 124 (6.3) | 22 (1.8) | 28 (1.4) |
| 2003 | 4811 | 1194 | 1843 | 91 (7.6) | 120 (6.5) | 22 (1.8) | 28 (1.5) |
| 2004 | 4883 | 1246 | 2008 | 88 (7.1) | 127 (6.3) | 31 (2.5) | 40 (2.0) |
| 2005 | 4718 | 1154 | 1926 | 92 (8.0) | 126 (6.5) | 33 (2.9) | 37 (1.9) |
| 2006 | 4513 | 979 | 1821 | 92 (9.4) | 131 (7.2) | 35 (3.6) | 46 (2.5) |
| 2007 | 4322 | 888 | 1852 | 66 (7.4) | 90 (4.9) | 23 (2.6) | 36 (1.9) |
| 2008 | 4603 | 884 | 2071 | 61 (6.9) | 106 (5.1) | 26 (2.9) | 44 (2.1) |
| 2009 | 4682 | 898 | 2185 | 69 (7.7) | 125 (5.7) | 26 (2.9) | 39 (1.8) |
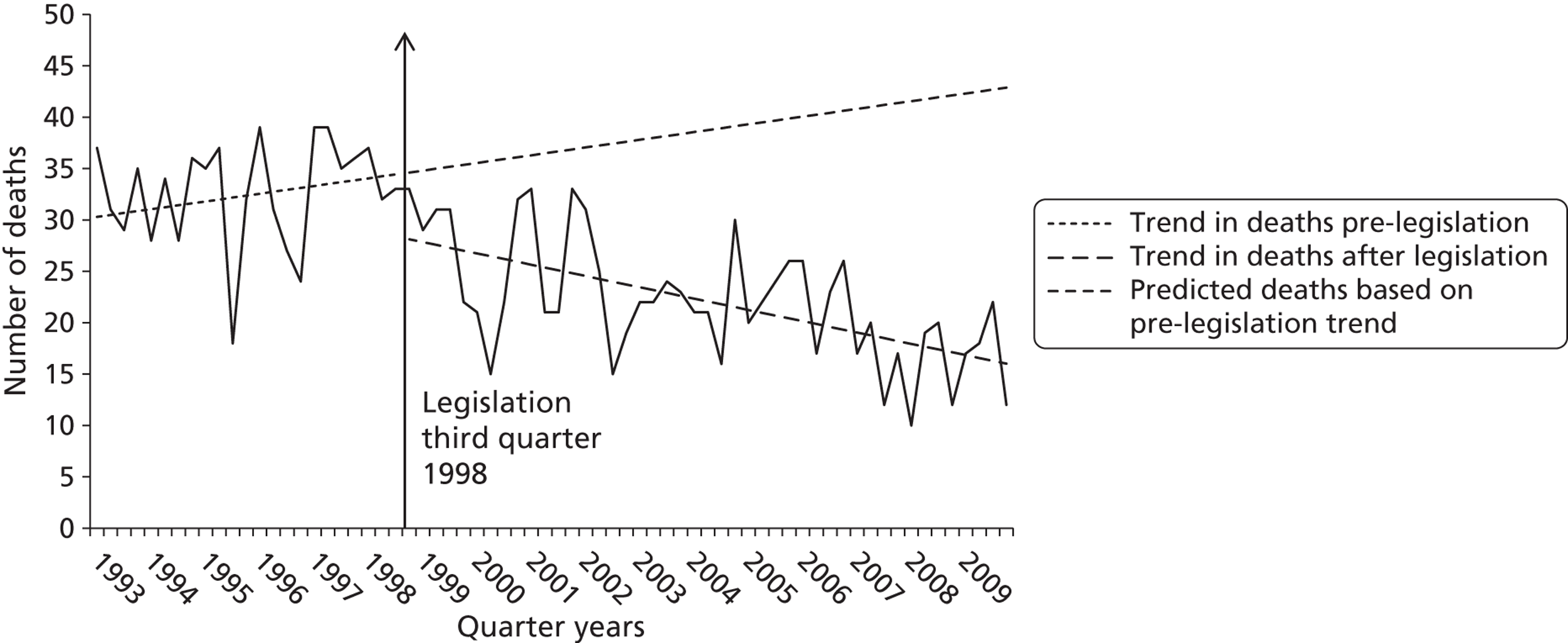
Regression analysis of quarterly data indicated a significant decrease corresponding to the September 1998 legislation in both level (i.e. step change) and trend in deaths involving paracetamol in England and Wales that received a suicide or open verdict (Figure 2 and Table 11).
FIGURE 2.
Number of suicide and open verdict deaths involving paracetamol alone in England and Wales, 1993–2009, by quarter years, and best fit regression lines related to the 1998 legislation.
| Cause of death | Segmented regression models | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Base-level coefficient (β0) | Robust SE | p-value | Base-trend coefficient (β1) | Robust SE | p-value | Step-change coefficienta (β2) | Robust SE | p-value | Trend-change coefficienta (β3) | Robust SE | p-value | |
| Suicide, open | ||||||||||||
| Paracetamol | 30.103 | 1.901 | < 0.001 | 0.188 | 0.116 | 0.111 | − 6.023 | 2.430 | 0.016 | − 0.463 | 0.132 | 0.001 |
| Paracetamol (adjusted)b | 21.085 | 7.208 | 0.005 | 0.149 | 0.113 | 0.194 | − 6.473 | 2.397 | 0.009 | − 0.328 | 0.164 | 0.049 |
| Paracetamol compounds | 4.801 | 1.081 | < 0.001 | 0.007 | 0.087 | 0.933 | 1.249 | 1.534 | 0.419 | 0.013 | 0.095 | 0.892 |
| All drug poisoning except paracetamol | 291.078 | 12.757 | < 0.001 | 1.290 | 0.886 | 0.150 | 12.928 | 12.150 | 0.291 | − 4.347 | 0.925 | < 0.001 |
| All drug poisoning | 321.373 | 14.007 | < 0.001 | 1.462 | 0.966 | 0.135 | 7.142 | 13.067 | 0.587 | − 4.795 | 1.011 | < 0.001 |
| All causes | 1277.176 | 28.050 | < 0.001 | − 1.075 | 2.365 | 0.651 | 36.928 | 41.443 | 0.376 | − 2.893 | 2.574 | 0.265 |
| Suicide, open, accidental | ||||||||||||
| Paracetamol | 39.344 | 2.460 | < 0.001 | 0.309 | 0.158 | 0.055 | − 10.300 | 3.111 | 0.002 | − 0.521 | 0.0176 | 0.004 |
| Paracetamol (adjusted)b | 30.171 | 7.099 | < 0.001 | 0.236 | 0.170 | 0.170 | − 9.959 | 3.085 | 0.002 | − 0.426 | 0.191 | 0.029 |
| Paracetamol compounds | 5.777 | 1.172 | < 0.001 | 0.017 | 0.087 | 0.842 | 0.358 | 1.489 | 0.811 | 0.081 | 0.094 | 0.392 |
| All drug poisoning except paracetamol | 445.966 | 27.361 | < 0.001 | 2.919 | 1.885 | 0.126 | − 10.246 | 29.152 | 0.726 | − 3.931 | 2.042 | 0.059 |
| All drug poisoning | 468.263 | 29.352 | < 0.001 | 3.122 | 1.989 | 0.121 | − 18.461 | 31.001 | 0.554 | − 4.361 | 2.140 | 0.046 |
The estimated average decrease in number of deaths was 17 per quarter (95% CI − 25 to − 9 deaths per quarter) in the post-intervention period compared with the expected number based on trends in the pre-intervention period (Table 12). This change equated to an overall decrease in number of deaths of about 43% in the 11.25 years post legislation, or 765 fewer deaths than would have been predicted based on trends during 1993–September 1998. An overall decrease of 36% was found when a conservative method of analysis was used (see Table 12).
There was also a downwards trend in all drug-poisoning (excluding paracetamol) deaths receiving a suicide or open verdict during the post-legislation period, although this was smaller in magnitude (25%) and was not associated with the step change seen for paracetamol following the introduction of the 1998 legislation. When the change in paracetamol deaths was adjusted to take account of the fall in poisoning deaths involving other drugs, the decline in paracetamol deaths changed very little (see Table 12). Similar results were found when accidental poisoning deaths involving paracetamol were included with suicides and open verdicts (see Table 12). The reduction in deaths in the post-legislation period when accidents were included equated to 990 fewer deaths than expected. Although suicides (including open verdicts) involving any method showed a significant downwards trend during the post-legislation period, there was no step change associated with the legislation (see Table 11).
When the intervention point was moved back 9 months to the beginning of 1998 to take account of earlier introduction of packaging changes, there remained a significant downwards trend in suicide and open verdict deaths involving paracetamol during 1998–2009 but no step change (see Appendix 3, Table 45).
There was no major change in number of deaths involving paracetamol compounds following the 1998 legislation (see Tables 11 and 12). These deaths represented a relatively small proportion of overall paracetamol-related deaths (see Table 10).
| Cause of death | Estimation of the absolute effect of the legislation October 1998–2009a | Conservative estimationb of the absolute effect of the legislation October 1998–2009a | ||||
|---|---|---|---|---|---|---|
| Mean quarterly estimated no. of deaths without legislationc | Mean quarterly estimated no. of deaths with legislationc | Mean quarterly change October 1998–2009d (95% CI)e | Mean quarterly estimated no. of deaths without legislationc | Mean quarterly estimated no. of deaths with legislationc | Mean quarterly change October 1998–2009d (95% CI)e | |
| Suicide, open | ||||||
| Paracetamol | 39 | 22 | − 17 (− 25 to − 9) | 34 | 22 | − 12 (− 20 to − 4) |
| All drug poisoning (except paracetamol) | 350 | 263 | − 87 (− 145 to − 29) | 321 | 263 | − 58 (− 115 to 1) |
| Paracetamol (adjusted)f | 28 | 14 | − 14 (− 23 to − 5) | 24 | 14 | − 10 (− 19 to − 2) |
| Paracetamol compounds | 5 | 6 | 1 (− 5 to 7) | 5 | 6 | 1 (− 5 to 8) |
| All drug poisoning | 388 | 285 | − 103 (− 166 to − 40) | 355 | 285 | − 70 (− 132 to − 7) |
| All causes | 1228 | 1198 | − 30 (− 199 to 140) | 1252 | 1198 | − 54 (− 224 to 115) |
| Suicide, open, accidental | ||||||
| Paracetamol | 53 | 31 | − 22 (− 30 to − 14) | 46 | 31 | − 15 (− 23 to − 7) |
| All drug poisoning (except paracetamol) | 580 | 480 | − 100 (− 225 to 23) | 513 | 480 | − 33 (− 158 to 90) |
| Paracetamol (adjusted)f | 41 | 21 | − 20 (− 32 to − 8) | 35 | 21 | − 14 (− 26 to − 2) |
| Paracetamol compounds | 7 | 9 | 2 (− 4 to 8) | 6 | 9 | 3 (− 3 to 9) |
| All drug poisoning | 612 | 493 | − 119 (− 249 to 11) | 540 | 493 | − 47 (− 177 to 83) |
Liver unit activity
Registration for liver transplantation
There was a decrease in level and trend of the number of registrations for liver transplantation related to paracetamol-induced hepatotoxicity in England and Wales following the 1998 legislation (Figure 3). The mean quarterly change compared with the expected number of registrations based on trends in the pre-intervention period was − 10.7 (95% CI − 20 to − 1), equating to a 61% reduction (mean 6.9 individuals per quarter vs. mean 17.6 in the pre-legislation period) (Table 13). This was equivalent to 482 fewer registrations over the 11.25-year period following the legislation. We obtained a similar result when we used the beginning of 1998 as the legislation point. A conservative estimate of the absolute change in number of registrations for liver transplants was smaller, and was not significant.
FIGURE 3.
Paracetamol-related registrations for liver transplantation waiting list in England and Wales, 1995–2009, by quarter years, and best fit regression lines related to the 1998 legislation.
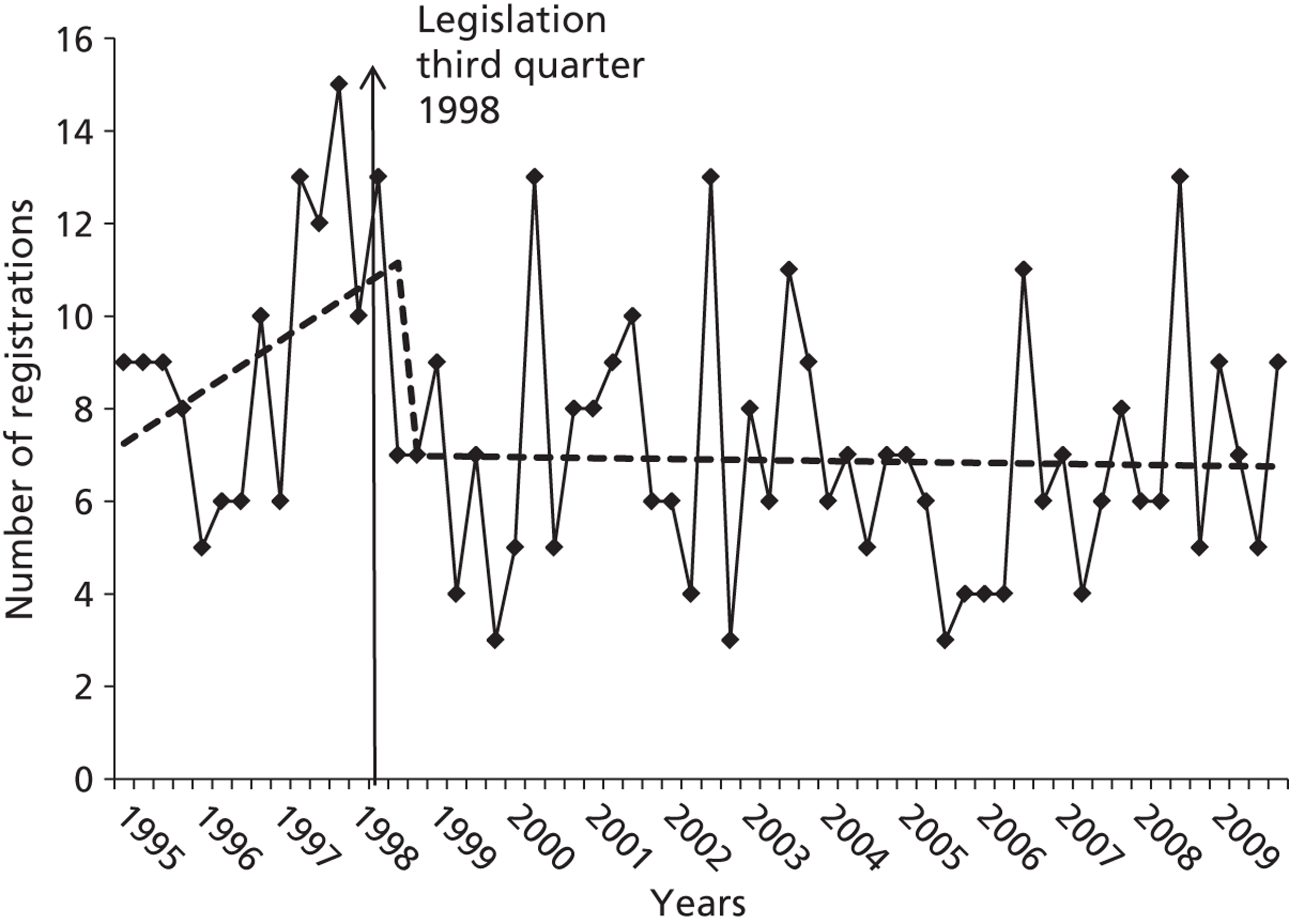
| Estimation of the absolute effect of the legislation October 1998–2009a | Conservative estimation of the absolute effect of the legislation October 1998–2009a | |||||
|---|---|---|---|---|---|---|
| Liver unit registrations and transplants | Mean quarterly estimated no. without legislationb | Mean quarterly estimated no. with legislationb | Mean quarterly change October 1998–2009c (95% CId) | Mean quarterly estimated no. without legislationb | Mean quarterly estimated no. with legislationb | Mean quarterly change October 1998–2009c (95% CId) |
| Paracetamol-related | ||||||
| Registrations | 17.6 | 6.9 | − 10.7 (− 20 to − 1) | 11.1 | 6.9 | − 4.3 (− 14 to 5) |
| Transplants | 8.2 | 4.8 | − 3.4 (− 12 to 6) | 6.8 | 4.8 | − 2.0 (− 11 to 7) |
| All liver transplants | 132.3 | 148.8 | 16.5 (− 30 to 63) | 138.9 | 148.8 | 9.9 (− 37 to 57) |
Liver transplantation
There was a non-significant reduction in number of liver transplantations for paracetamol-induced hepatotoxicity in England and Wales in the period October 1998–2009 following the legislation compared with the estimated level based on the 1995–September 1998 trend (Figure 4). The estimated mean quarterly change was − 3.4 (95% CI − 12 to 6) transplantations (see Table 13). The number of liver transplantations for all causes in the UK showed a small but non-significant increase during the post-legislation period (from a mean estimated quarterly number of 132.3 before the legislation to 148.8 after).
FIGURE 4.
Paracetamol-related liver transplantations in England and Wales, 1995–2009, by quarter years, and best fit regression lines related to the 1998 legislation.
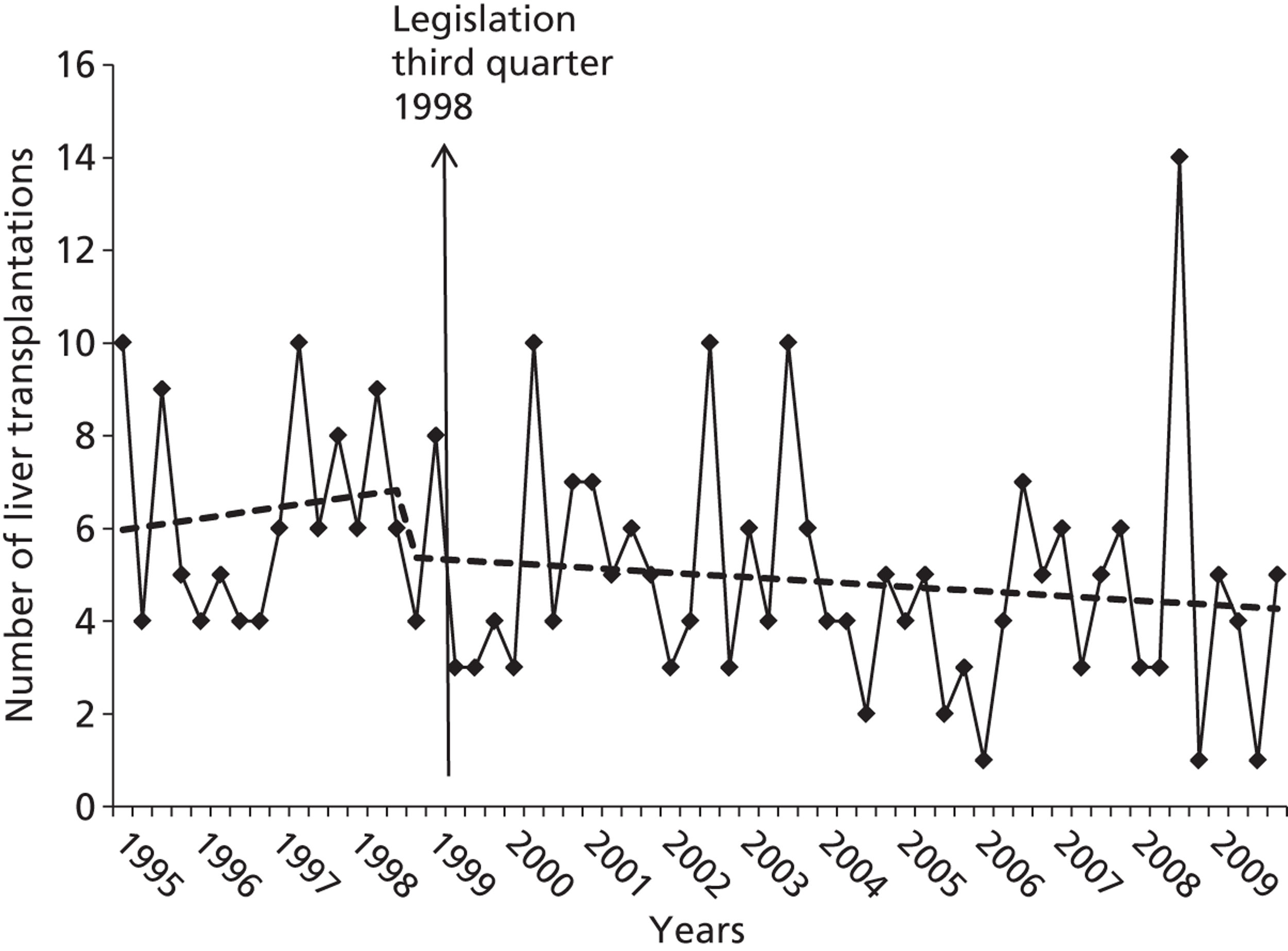
Non-fatal self-poisoning with paracetamol
There was no decline in the number of hospital presentations in Oxford between 1993 and 2009 for non-fatal overdoses involving paracetamol (pure or compound form) (1993–8 mean = 567.0 per year vs. 1999–2009 mean = 601.6 per year).
Discussion
We have shown that the 1998 legislation to restrict pack sizes of paracetamol was associated with a significant reduction in the number of deaths from paracetamol poisoning in England and Wales over an 11-year period, in terms of both deaths receiving a suicide or an open verdict from the coroner and deaths receiving a suicide, an open or an accidental verdict from the coroner. This effect was found in analyses with estimates based on a continuation of the pre-legislation trend, as well as with more conservative estimates assuming no increasing trend in the absence of the legislation. The downwards step change was not apparent when the intervention point was moved back to the beginning of 1998.
There was no significant change in number of deaths from fatal poisoning with paracetamol compounds, but these constituted a relatively small proportion of paracetamol-related deaths. There was also a significant reduction in number of deaths from poisoning with drugs excluding paracetamol between 1998 and 2009, but to a lesser extent than was found for paracetamol and without the step change associated with the 1998 paracetamol legislation. When we repeated the analyses for paracetamol with an adjustment for underlying trends in poisoning deaths (excluding those that were paracetamol related) the findings for paracetamol deaths were largely unaltered.
Following the legislation a significant reduction was also found in the number of registrations for liver transplantation in England and Wales for paracetamol-induced hepatotoxicity, although a downwards step change was also apparent when the beginning of 1998 was used as the intervention point, and the change was not significant using a conservative estimate of the effect. Although there was also a reduction in the number of liver transplants of a similar order to that for registrations, this was not statistically significant because of the smaller numbers involved. It is interesting that the decline in liver unit activity (see Figures 3 and 4) shows a somewhat different pattern from that for paracetamol poisoning deaths (see Figure 2), with the former flatlining after an initial abrupt reduction and the latter a more continuous reduction. The reasons for this are unclear.
The reduction in number of registrations for liver transplantation is particularly striking because in 2005 the criteria for registration were broadened, with a lowering of the thresholds for consideration for surgery. 83 It is possible that some of the reduction in liver transplant registrations may have resulted from improvements in the early management of patients presenting to hospital with paracetamol poisoning, including administration of the antidote N-acetylcysteine and the increasing sophistication and success of intensive care support provided to patients with paracetamol-induced acute liver failure. 84 These factors could also have accounted for some of the downwards trend in numbers of paracetamol deaths observed over the study period; however, the process of change has been one of continuous evolution and would be unlikely to account for the step change seen in outcomes coincident with the introduction of pack size restrictions. It is important to note, however, that, based on data from Oxford, presentations of non-fatal overdoses to hospital involving paracetamol did not decrease during the study period.
The impact of the 1998 legislation restricting pack sizes of paracetamol is likely to reflect the fact that many people who self-poison with paracetamol take what is available in the household,65,85 especially if the overdose is impulsive. Also, when individuals buy paracetamol specifically for the purpose of an overdose, the quantity per purchase is limited. Perhaps the most convincing evidence that reduced pack sizes of paracetamol have contributed to a reduced occurrence of hepatotoxicity and mortality is our earlier finding that the legislation was followed by a reduction in the number of tablets taken in paracetamol overdoses and in the number of large overdoses. 12,65
Strengths and limitations
One limitation of this study is that we used only data on deaths from poisoning with paracetamol (with or without alcohol) in pure or compound form, not deaths in which paracetamol was consumed with other drugs. This approach, however, ensured that the findings of the study were restricted primarily to paracetamol and not substantially affected by the toxicity of other drugs or compounds. One strength of the study is that it was based on national data for both deaths and liver unit activity.
We have not been able to estimate the number of possible substitutions of paracetamol overdoses with other methods of poisoning or self-harm, but the trend in total suicides (all methods) during the post-1998 legislation period was downwards, as was the trend in suicides by ingestion. This downwards trend in all suicides probably reflects other factors that have favourably influenced suicide rates and, hence, may have contributed to the findings for paracetamol poisoning deaths. A further limitation was that data on non-fatal overdoses of paracetamol were restricted to one hospital, but this included all presentations, not just admissions.
Conclusions
The legislation introduced in 1998 to restrict pack sizes of paracetamol was associated with long-term benefits in terms of reduced numbers of deaths from paracetamol poisoning and registrations for liver transplantation. The number of deaths annually from paracetamol poisoning suggests, however, that further methods of prevention should be sought.
STUDY 2: AN INTERVIEW STUDY OF PATIENTS WHO HAVE TAKEN LARGER PARACETAMOL OVERDOSES
Objectives
The objectives were to conduct an interview study to investigate the characteristics of larger paracetamol overdoses and the people who use this method of self-poisoning, and to assess whether the intention of the legislation to restrict sales of large numbers of tablets is being complied with by shops and pharmacies.
Methods
Patients were eligible for inclusion if they had taken an overdose of > 16 pure paracetamol tablets, were aged ≥ 16 years and had received a psychosocial assessment by a member of the clinical self-harm team in the Department of Psychological Medicine at the John Radcliffe Hospital in Oxford.
The research interview consisted of standardised and open-ended questions regarding the circumstances of the act, the number of tablets consumed, the number available, the source of the tablets, whether the patient had tried to buy more than the recommended amount and his or her expectations of the physical effects of overdose (see Appendix 4).
Patients were shown cards with common motives for overdoses written on them (modified from Bancroft et al. 197986) and were asked to choose those that best explained their own motivation. They were also asked about previous paracetamol overdoses and potential influences on their decision to take the current overdose. Scores on the Suicidal Intent Scale (SIS)87 were recorded, using data collected by the clinician during the psychosocial assessment. At the end of the research interview, patients completed the Hospital Anxiety and Depression Scale (HADS). 88
The patients' verbatim responses to open-ended questions were recorded manually by the interviewer. The interviews were carried out between November 2008 and July 2010 by a research interviewer, members of the clinical self-harm team and a research support facilitator.
The study received ethical approval from Oxfordshire Research Ethics Committee C (REC reference 08/H0606/45) and from the Research and Development Departments of the Oxford Radcliffe Hospitals NHS Trust and Oxford Health NHS Foundation Trust.
Quantitative data were analysed with SPSS for Windows version 14 (SPSS Inc., Chicago, IL, USA) using descriptive statistics, including chi-squared and Mann–Whitney tests. A simplified thematic approach was used to examine qualitative data arising from the patients' responses to open-ended questions. Themes were identified by SS from the written comments and reviewed and approved by KH.
Results
Sixty patients were included in the study. Figure 5 shows the flow diagram for inclusion and exclusion of potential participants.
FIGURE 5.
Flow chart of recruitment to the study. Source: Simkin S, Hawton K, Kapur N, Gunnell D. What can be done to reduce mortality from paracetamol overdoses? A patient interview study. Q J Med 2012;105:41–51. By permission of Oxford University Press.
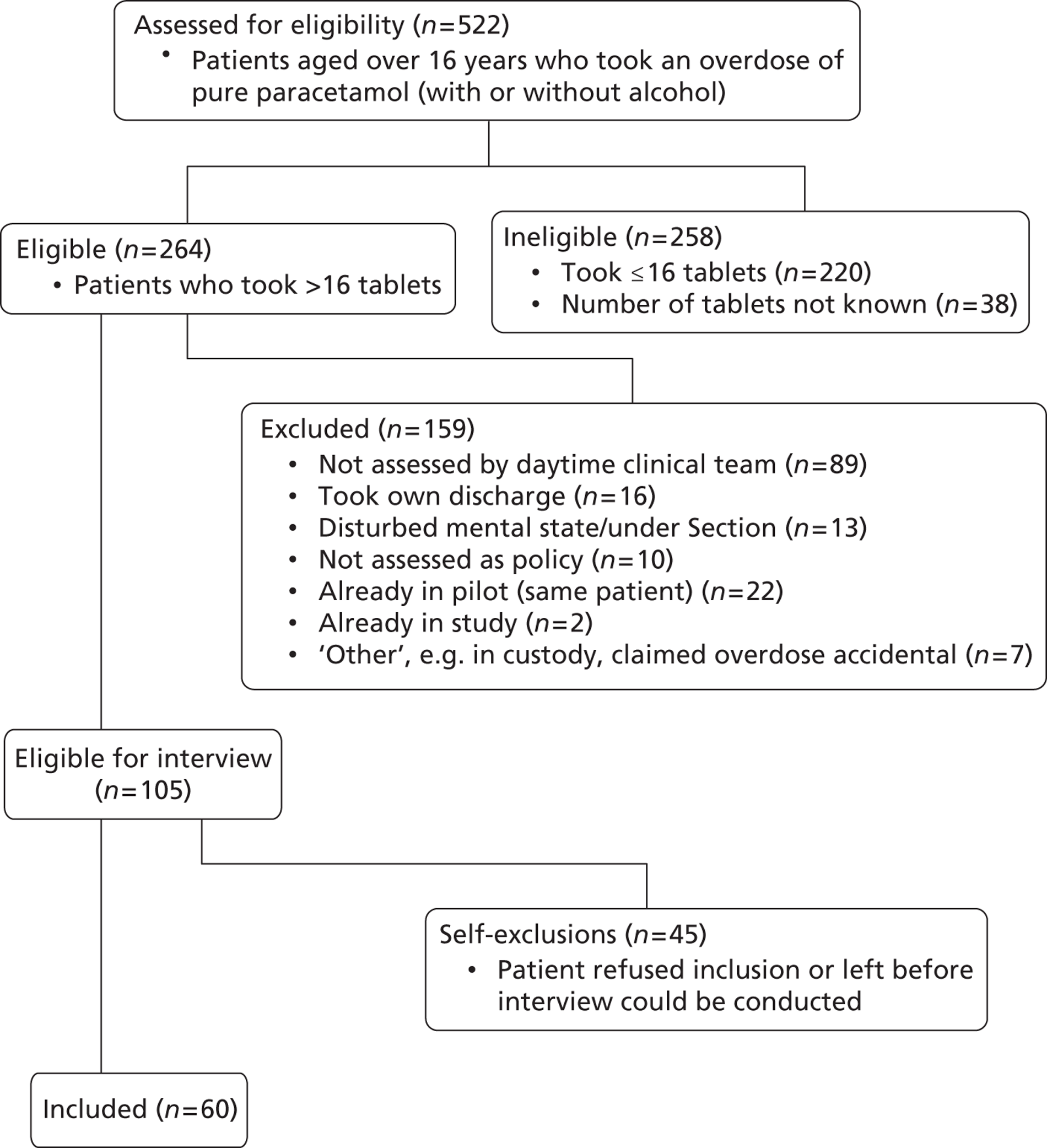
Patient characteristics
The study sample included 35 females [mean age 29.9 years, standard deviation (SD) 13.2 years, range 16–65 years] and 25 males (mean age 33.3 years, SD 14.9 years, range 19–65 years) (Table 14). For 24 patients (40.0%) this was their first overdose, but 10 patients (16.7%) were multiple repeaters, having taken at least five previous overdoses (see Table 14). Over half (n = 32, 53.3%) had taken a previous overdose of paracetamol. The SIS was completed for 59 patients. High (13–20) or very high (21+) scores were recorded for over half (n = 33, 56.0%) of these patients. At the time of the research interview, 43 patients (72.9%) reached case status for anxiety (score > 9) on the HADS and 37 (62.7%) reached case status for depression (score > 9).
Nature of the overdose
Over one-third of the patients had consumed alcohol at the time of the overdose (Table 15). Presentation to hospital was delayed by > 6 hours after taking the tablets in 22 cases (36.7%). The majority (n = 50, 83.3%) were treated with the antidote N-acetylcysteine. Seventeen patients took one or more other drugs in their overdose.
The number of paracetamol tablets taken ranged from 18 to 224. Over three-quarters of the patients took fewer than 50 tablets, but over half (n = 35, 58.3%) took all of the tablets available. Half of the patients had taken the overdose impulsively, within an hour of first thinking about it (see Table 15). One-quarter said that they had thought about the act for < 15 minutes before taking the tablets. However, seven people had considered the overdose for more than a week.
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Female | 35 | 58.3 |
| Male | 25 | 41.7 |
| Age, years | ||
| 16–20 | 17 | 28.3 |
| 21–40 | 28 | 46.7 |
| 41+ | 15 | 25.0 |
| Previous overdoses | ||
| 0 | 24 | 40.0 |
| 1 | 15 | 25.0 |
| 2–4 | 9 | 15.0 |
| 5+ | 10 | 16.7 |
| Yes, number not known | 2 | 3.3 |
| Previous paracetamol overdose | 32 | 53.3 |
| SIS score (n = 59) | ||
| Low (0–6) | 4 | 6.8 |
| Moderate (7–12) | 22 | 37.3 |
| High (13–20) | 27 | 45.8 |
| Very high (21+) | 6 | 10.2 |
| HADS score (n = 59) | ||
| Case – anxiety (> 9) | 43 | 72.9 |
| Case – depression (> 9) | 37 | 62.7 |
Source of the paracetamol
In many cases (n = 32, 53.3%) the tablets were already in the home, mostly for general pain relief. Three people had boxes of 100 tablets, which had been prescribed after operations or for back pain. Over half (n = 32, 58.3%) bought tablets specifically for the overdose (nine of these also had supplies at home). Most purchases were made from a supermarket or pharmacy (see Table 15). Other outlets included four garages and an online pharmacy site.
Ten people tried to buy > 32 tablets in one transaction; four succeeded. Of these, one was able to buy in bulk from a cash and carry outlet, one purchased 14 packs of 16 tablets from an online pharmacy, and one obtained multiple packs by telling pharmacy staff that he was going away on holiday and needed supplies to take with him. The fourth bought three packs of 16 tablets from a supermarket. Nine patients commented that they were aware of the limit on sales and had therefore bought supplies in more than one transaction.
Anticipated effects of the overdose
When asked what they had thought the physical effects of the overdose would be if untreated, the majority (n = 53, 88.3%) said that they knew that a paracetamol overdose could cause death or permanent damage (see Table 15). Over three-quarters (n = 48, 80.0%) knew that excess paracetamol could harm the liver. However, 42 (70.0%) thought that they would lose consciousness after the overdose. Over half of these (n = 23, 54.8%) said that they would not have taken paracetamol if they had known that they would not lose consciousness and that the effects would not be immediate.
The patients were asked how many tablets they thought would cause death. Twelve (20.0%) did not know. Of the rest, the number chosen ranged from 7 to 200. Five people (8.3%) thought that ≤ 16 tablets could kill, and 17 (28.3%) thought that 17–32 tablets would be lethal. Nine (15.0%) thought that ≥ 100 tablets would be necessary to cause death. Some people's opinion was influenced by the pack sizes: ‘I thought that over 32 tablets would be toxic, as that is the limit you can buy over the counter'; ‘Ten tablets could kill, because it says on the pack not to take over eight’.
| Characteristic | n | % |
|---|---|---|
| Alcohol | ||
| Within 6 hours of the overdose | 19 | 31.7 |
| At the time of the overdose | 23 | 38.3 |
| Delayed presentation to hospital | 22 | 36.7 |
| Treatment in hospital | ||
| N-acetylcysteine | 50 | 83.3 |
| No treatment | 10 | 16.7 |
| Number of tablets taken | ||
| ≤ 32 (> 1–2 packs) | 27 | 45.0 |
| 33–48 (> 2–3 packs) | 20 | 33.3 |
| > 48 (> 3 packs) | 13 | 21.7 |
| Took all the tablets available | 35 | 58.3 |
| Bought tablets specially for the overdose | 35 | 58.3 |
| Source of the tabletsa | ||
| Already in the home | 32 | 53.3 |
| Pharmacy | 17 | 28.3 |
| Supermarket | 21 | 35.0 |
| Local shop | 8 | 13.3 |
| Other outlet (e.g. garage, internet) | 7 | 11.7 |
| Time spent planning the overdose | ||
| 0 to < 15 minutes | 15 | 25.0 |
| 15 to < 60 minutes | 15 | 25.0 |
| 1 to < 24 hours | 14 | 23.3 |
| 1 to < 7 days | 9 | 15.0 |
| 1+ weeks | 7 | 11.7 |
| Anticipated effects if untreated | ||
| Completely safe | 0 | 0 |
| Mild, short-lived effects | 0 | 0 |
| Harmful but short-lasting effects | 4 | 6.7 |
| Permanent damage or harm | 11 | 18.3 |
| Could cause death | 42 | 70.0 |
| Not known | 3 | 5.0 |
Paracetamol packs include a warning about the dangers of overdose. Just under half of the patients (n = 29, 48.3%) said that they had noticed this, but in most of these cases (23/29, 79.3%) this had not affected their decision to take the tablets. Six people reported that the warning had strengthened their decision, for example, ‘The wording [i.e. go straight to doctor if you take more than eight] implies that it would be good to overdose on . . . The warning made it seem that an overdose would be effective.'
Most of those who had not noticed the warning said that they would still have taken the overdose if they had seen it (24/30, 80.0%). Only five people thought that seeing the warning would have deterred them from taking the tablets. Almost all (52/58, 89.7%) said that they would still have taken a paracetamol overdose even if the packs had contained fewer tablets.
Motivation
When asked to indicate which of the motives shown on cards best explained why they had taken their overdose (they could choose as many as they liked), over three-quarters said that they had wanted to die (Table 16). Other common reasons were ‘to get relief from a terrible state of mind’ and ‘to escape from an unbearable situation’.
| Reason for overdosea | n | % |
|---|---|---|
| To die | 46 | 76.7 |
| To get relief from a terrible state of mind | 45 | 75.0 |
| To escape from an unbearable situation | 44 | 73.3 |
| To show how desperate they were feeling | 32 | 53.3 |
| To get help | 26 | 43.3 |
| To find out whether someone really loved them | 9 | 15.0 |
| To make someone feel sorry | 9 | 15.0 |
| To influence someone | 3 | 5.0 |
Influences and reasons for taking paracetamol
Over one-third of the patients (n = 23, 38.3%) knew someone else who had taken an overdose of paracetamol. Twenty-one patients (35.0%) had seen or read about paracetamol overdoses in the media; nine (42.9%) of these thought that this had influenced their decision to take an overdose. For example, two people had read newspaper articles that specified the number of tablets taken in fatal overdoses and then took the same number of tablets in their own overdose. Another person saw a local news item about someone who had taken paracetamol together with alcohol and other medication; she went out the next day to buy paracetamol to take with her own prescribed medication and alcohol. Eight people had used the internet to obtain information on suicide methods. Five of them said that this had influenced their decision to take paracetamol and had provided them with information on toxic amounts.
When asked why they had chosen to take paracetamol in their overdose, over one-third (n = 23, 38.3%) said that the tablets were already in the household. Twelve (20.0%) bought paracetamol because it was cheap and readily available. Sixteen people (26.7%) had chosen paracetamol because they knew that it was effective: ‘. . . catastrophic effect on the liver’.
Although patients were aware of the unpleasant effects of paracetamol, this did not deter them: ‘I heard it was a slow and painful death’; ‘I don't deserve any better than a horrible death’. Five people (8.3%) said that they had taken paracetamol because they had done so in the past: ‘I've always done paracetamol – I know it's a nasty killer, it takes a long time to do it’; ‘I've always done so in the past and always managed to get through it’.
Discussion
The overall aim of this study was to obtain information that might assist in the identification of further initiatives to reduce paracetamol overdoses, especially those involving large and hence potentially life-threatening numbers of tablets.
As found in other studies,26,64 the main reasons that patients gave for using paracetamol for overdose were that it was cheap and easily available (either already in the household or easy to buy from multiple outlets). Over half of the patients took all of the tablets that were available to them, compared with one-third of patients in an earlier interview study in Oxford65 (in which patients who took smaller overdoses were included). In both studies, similar proportions of patients had bought tablets specifically for the overdose: 58.3% in the current study compared with 52.5% in the earlier study. In a study of patients who took paracetamol overdoses and presented to an emergency department in south London after the legislation, 48% of patients who had ingested > 16 tablets had purchased paracetamol specifically for the act, whereas those who had taken < 16 tablets were more likely to have taken tablets already in the household. 74
Nearly one-third of those who bought tablets specifically for the act had spent < 1 hour planning it. If their distress was apparent, this might suggest the potential for intervention at the point of sale, but it is probably unrealistic to expect sales staff to identify such individuals and to intervene in any positive way, apart from refusing to supply more than the recommended number of tablets.
Four of the 10 people in our study who tried to buy more than the recommended amount of paracetamol in one transaction were able to do so, including a person who bought 224 tablets from an online pharmacy. We alerted the MHRA about the internet sale, and the online outlet subsequently restricted purchases of paracetamol to 32 tablets.
One of the intentions behind the pack size legislation was to reduce the dangers of impulsive overdoses by limiting the number of tablets available in the household at any one time. Half of the patients in our study had taken the overdose within an hour of first seriously contemplating it, including one-quarter who had thought about the act for < 15 minutes.
Public knowledge of the dangers of paracetamol overdose has increased considerably since the late 1970s. 31 In our study, 88% of patients knew that an overdose could cause death or permanent damage, a similar figure to the 78% of patients in the earlier (1992–3) Oxford study. 64 However, 80% in the present study knew of the potential for hepatotoxicity compared with 43% in the earlier study. Despite being aware of the harmful effects of paracetamol overdose, a high proportion of the patients thought that they would quickly become unconscious. This finding is consistent with that from other studies. 26,31,64 If people who take a paracetamol overdose expect to lose consciousness but do not, they may think that they have not taken a dangerous amount and may not seek medical attention until symptoms of liver damage appear, by which time it may be too late to treat successfully. Half of the patients in our study who were unaware that they would not lose consciousness immediately said that they would not have taken the paracetamol overdose if they had known this. There may be potential for educational initiatives highlighting this aspect of paracetamol toxicity, although it is possible that this may have a reverse effect (e.g. an episode of a popular television drama featuring a fatal paracetamol overdose was followed by an increase in similar overdoses among viewers89).
Nearly half of the patients had noticed the warnings about the dangers of overdose printed on the pack, but in most cases this did not affect their decision to take the tablets; indeed, for some people the warning had reinforced their decision by confirming that an overdose could be lethal. This apparent lack of a positive impact of warning signs on packs in this sample was also found in the earlier Oxford study. 65
The role of the media and the internet in providing information about paracetamol overdose was clear in some cases. It is important that media guidelines that emphasise the importance of not providing precise details of suicide methods be followed. 90,91
Limitations
The study was based in a single large general hospital and so it is uncertain if the findings are generalisable to patients presenting to other hospitals. However, the characteristics of people presenting to the hospital in Oxford with paracetamol overdoses are similar to those seen elsewhere. 46 We relied on patient report of the number of tablets that they had taken in overdose, and this may be unreliable. 42,46,92
Conclusions
The characteristics of the patients in our study who took paracetamol overdoses were remarkably similar to those in the previous Oxford study64 over 15 years earlier. The impulsive nature of many of the overdoses and the fact that a substantial proportion of patients used household supplies of paracetamol for self-poisoning mean that special attention needs to continue to be paid to the availability of paracetamol, especially in quantities that can cause hepatotoxicity. There appears to be reasonable adherence to the sales guidance. Media influences on use of paracetamol for self-poisoning, including through the internet, are important in some cases.
STUDY 3: A COMPARATIVE STUDY OF THE IMPACT OF DIFFERENT PACK SIZES OF PARACETAMOL ON INTENTIONAL OVERDOSES IN ENGLAND AND IRELAND
Objective
The objective of this study was to compare sizes of overdoses of paracetamol taken in England and in Ireland to answer the question of whether or not it might be beneficial to further reduce pack sizes of paracetamol in the UK.
Methods
We investigated the number of tablets of paracetamol consumed in overdoses that resulted in presentation to six general hospitals in three centres in England and all general hospitals in Ireland between 2002 and 2007 for those aged ≥ 10 years. Data were restricted to non-fatal, intentional self-poisoning episodes in which paracetamol was the sole medicinal agent consumed (with or without co-ingestion of alcohol) and at least four tablets were taken at one time (i.e. double the maximum recommended single therapeutic dose of two tablets). The data collected in the study hospitals included patient sex and age, drugs used for self-poisoning, numbers of tablets, and alcohol involvement at the time of the overdose.
Data sources
Multicentre Study of Self-harm in England
The Multicentre Study of Self-harm in England project is based on data collected on general hospital presentations for self-harm in six major general hospitals in England:1,93 one in Oxford, three in Manchester and two in Derby.
National Registry of Deliberate Self Harm in Ireland
Information is collected in the National Registry of Deliberate Self Harm for all presentations for intentional self-poisoning and self-injury to general hospitals in Ireland. 53
Ethical approval
The monitoring systems in Oxford, Manchester and Derby all have approval from local ethics committees to collect data on self-harm for local and multicentre projects. The National Registry of Deliberate Self Harm in Ireland has ethical approval from the National Research Ethics Committee of the Faculty of Public Health Medicine, and from the relevant hospitals and Health Service Executive ethics committees.
Data analysis
We used SPSS for Windows version 14 to compare overdoses of paracetamol in England and Ireland. Analyses comparing the numbers of tablets consumed, and numbers of packs used, in overdoses of paracetamol in England and Ireland were conducted using the chi-squared test, Mann–Whitney U-test and Kruskal–Wallis test. Analyses were conducted on combined data and separately by sex, age group and alcohol involvement with the overdose (data from the English study on alcohol consumed during the 6 hours before self-poisoning and/or as part of the overdose were combined for this analysis). The number of packs used was calculated as a multiple of the non-pharmacy maximum pack size in each country, from one pack to nine or more packs (e.g. in England an overdose involving up to one pack was 4–16 tablets, two packs was 17–32 tablets, three packs was 33–48 tablets, and so on; in Ireland, up to one pack was 4–12 tablets, two packs was 13–24 tablets, three packs was 25–36 tablets, and so on).
Results
Study samples
During the 6-year study period (2002–7) there were 31,107 hospital presentations for self-poisoning (alone) in the three English centres (six hospitals) and 42,877 in Ireland (up to 40 hospitals: 34 in 2002, 37 in 2003, 38 in 2004–5 and 40 in 2006–7). Of these, paracetamol was involved in 10,208 (32.8%) episodes in the English centres and in 9057 (21.1%) episodes in Ireland. Paracetamol alone (with or without alcohol) was involved in 5444 episodes in the English centres and in 3886 episodes in Ireland.
Of the episodes involving paracetamol alone, data on number of tablets taken in overdose were missing for 559 (10.3%) episodes in the English centres and 358 (9.2%) in Ireland. We also excluded episodes in which fewer than four tablets were taken, data on sex or age were missing or patients were < 10 years old [totalling 27 (0.5%) in the English centres and 19 (0.5%) in Ireland]. Thus, the samples for inclusion in the study consisted of 4858 episodes in the English centres and 3509 in Ireland.
The female to male ratio for episodes was somewhat larger among the Irish sample (2.1 : 1) than among the English sample (1.8 : 1) (Table 17). The age distributions of the two samples showed a greater proportion of younger individuals among the Irish sample and a greater proportion of older people among the English sample. Alcohol use at the time of overdose occurred with similar frequency in the English and the Irish samples.
| Characteristic | England (n = 4858), n (%) | Ireland (n = 3509), n (%) | Chi-square | p-value |
|---|---|---|---|---|
| Sex | ||||
| Male | 1736 (35.7) | 1146 (32.7) | ||
| Female | 3122 (64.3) | 2363 (67.3) | 8.537 | 0.003 |
| Age group, years | ||||
| 10–24 | 2186 (45.0) | 1682 (47.9) | ||
| 25–34 | 962 (19.8) | 753 (21.5) | ||
| 35+ | 1710 (35.2) | 1074 (30.6) | 19.442 (df = 2) | < 0.001 |
| Alcohol use | ||||
| Yes | 1851 (38.1) | 1259 (35.9) | ||
| No or not known | 3007 (61.9) | 2250 (64.1) | 4.311 | 0.038 |
Number of tablets taken in overdoses
The distribution of the number of tablets taken in paracetamol overdose in the English centres and in Ireland is shown in Figure 6. There were clear peaks in each of the countries corresponding to the pack size limits for non-pharmacy and pharmacy sales. Thus, in the English sample there were peaks at 16 and 32 tablets and in the Irish sample there were peaks at 12 and 24 tablets. There were also peaks at multiples of these pack sizes. There were, in addition, peaks in both samples at 10 and multiples of 10 tablets.
FIGURE 6.
Distribution of the number of tablets taken in paracetamol overdose by those aged ≥ 10 years in England (n = 4858) and Ireland (n = 3509), 2002–7, shown as percentages of the total number of overdoses of paracetamol in each country.
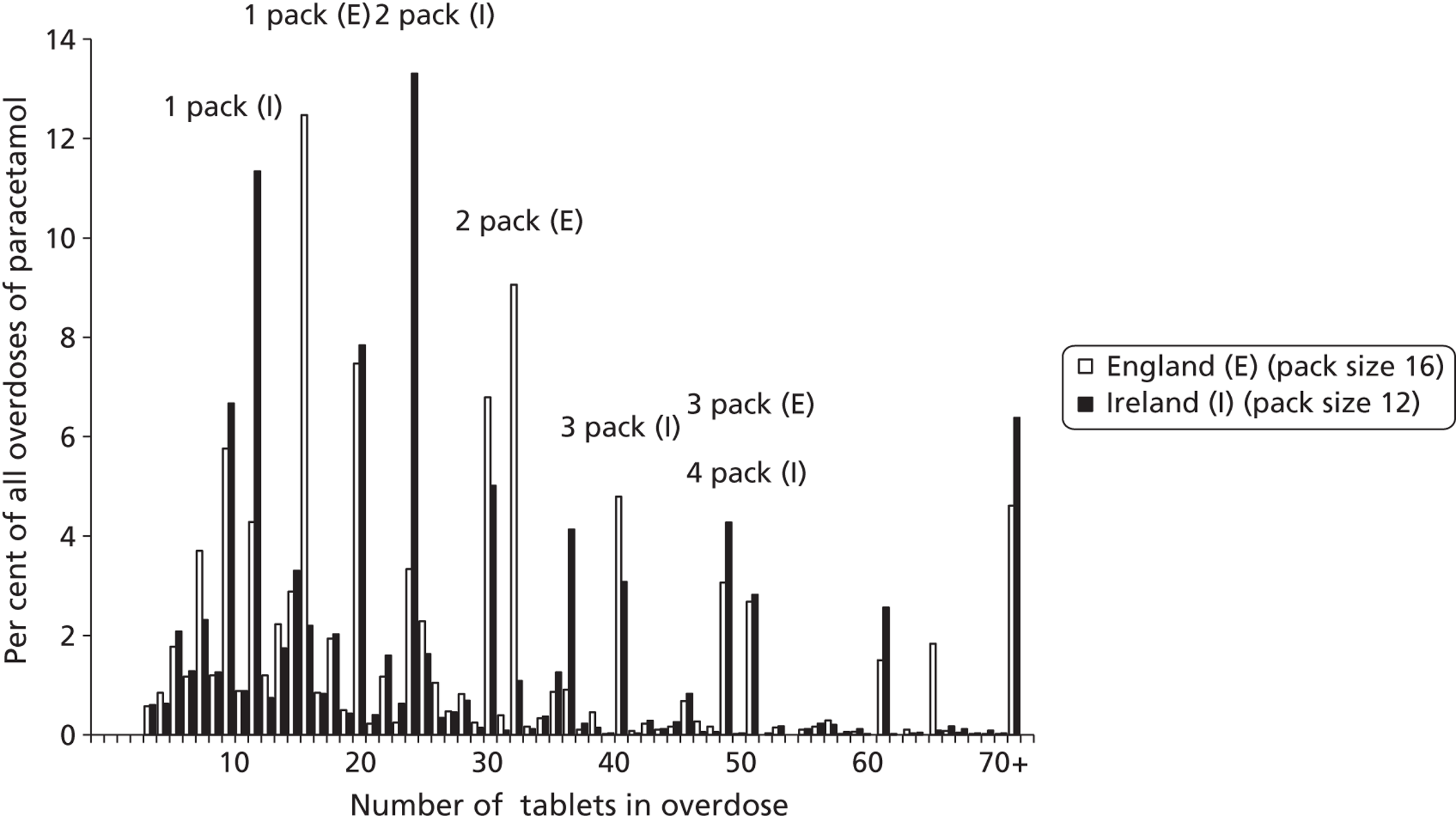
The median number of tablets consumed in paracetamol overdoses did not differ significantly between the English (median 22 tablets) and the Irish (median 24 tablets) samples (Table 18). When the samples were divided into three age groups and the two countries compared, a small but statistically significant difference in the median number of paracetamol tablets consumed between the English (median = 24) and the Irish (median = 23) samples was found among women in the ≥ 35 years age group (see Table 18).
| Characteristic | England (n = 4858) | Ireland (n = 3509) | Mann–Whitney U | p-value | ||
|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Z | ||
| Sex | ||||||
| Both | 22 | 15–32 | 24 | 12–36 | − 0.758 | 0.449 |
| Males | 28 | 16–40 | 27 | 18–48 | − 2.015 | 0.044 |
| Females | 20 | 13–32 | 20 | 12–30 | − 1.651 | 0.099 |
| Age range, years | ||||||
| 10–24 | 19 | 12–32 | 20 | 12–30 | − 1.179 | 0.239 |
| 25–34 | 24 | 16–40 | 24 | 15–45 | − 1.509 | 0.131 |
| 35+ | 26 | 16–40 | 24 | 12–40 | − 2.862 | 0.004 |
| Age range males, years | ||||||
| 10–24 | 22 | 15–32 | 24 | 14–36 | − 1.364 | 0.173 |
| 25–34 | 30 | 16–45 | 30 | 20–50 | − 2.128 | 0.033 |
| 35+ | 30 | 16–48 | 30 | 20–49 | − 1.083 | 0.279 |
| Age range females, years | ||||||
| 10–24 | 16 | 12–30 | 20 | 12–28 | − 0.655 | 0.513 |
| 25–34 | 20 | 14–32 | 24 | 12–36 | − 0.543 | 0.587 |
| 35+ | 24 | 16–32 | 23 | 12–32 | − 3.843 | < 0.001 |
In both England and Ireland, more paracetamol tablets tended to be taken by men but not women when alcohol was involved in overdoses (England: Z = − 3.141, p = 0.002; Ireland: Z = − 2.105, p = 0.035) (Table 19). There was a non-significant trend for smaller overdoses in males in Ireland who had not consumed alcohol than in those in England who had not consumed alcohol.
| Alcohol use | England (n = 4858) | Ireland (n = 3509) | Mann–Whitney U | p-value | ||
|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Z | ||
| Both sexes | ||||||
| Alcohol use | 24 | 16–35 | 24 | 13–36 | − 0.619 | 0.536 |
| No/not known | 20 | 14–32 | 24 | 12–36 | − 0.328 | 0.743 |
| Males | ||||||
| Alcohol use | 30 | 16–40 | 30 | 18–48 | − 1.086 | 0.277 |
| No/not known | 28 | 16–40 | 25.5 | 16–48 | − 1.739 | 0.082 |
| Females | ||||||
| Alcohol use | 20 | 14–32 | 20 | 12–30 | − 1.496 | 0.135 |
| No/not known | 20 | 13–32 | 20 | 12–30 | − 0.954 | 0.340 |
Number of packs used in overdoses
When the numbers of tablets consumed in overdoses by individuals in each country were categorised into numbers of pack equivalents used, the mean number of packs used was greater in Ireland (2.63, 95% CI 2.57 to 2.69 packs) than in England (2.07, 95% CI 2.03 to 2.10 packs). For both sexes combined, the largest proportion of overdoses in England (39.0%) involved one pack only, but the largest proportion of overdoses in Ireland (37.9%) involved three or more packs (Table 20). Females and the younger age group (15–24 years) in England were more likely to use one pack, but two packs were more likely in Ireland in these groups. Males and older age groups (25–34 years and 35+ years) were far more likely to use three or more packs in Ireland than in England.
| No. of packs | England (n = 4858), n (%) | Ireland (n = 3509), n (%) | Chi-square (df = 2) | p-value |
|---|---|---|---|---|
| Both sexes | ||||
| 1 | 1893 (39.0) | 949 (27.0) | ||
| 2 | 1790 (36.8) | 1229 (35.0) | ||
| 3+ | 1175 (24.2) | 1331 (37.9) | 215.6 | < 0.001 |
| Males | ||||
| 1 | 521 (30.0) | 217 (18.9) | ||
| 2 | 638 (36.8) | 327 (28.5) | ||
| 3+ | 577 (33.2) | 602 (52.5) | 109.8 | < 0.001 |
| Females | ||||
| 1 | 1372 (43.9) | 732 (31.0) | ||
| 2 | 1152 (36.9) | 902 (38.2) | ||
| 3+ | 598 (19.2) | 729 (30.9) | 135.6 | < 0.001 |
| Age 15–24 | ||||
| 1 | 1019 (46.6) | 495 (29.4) | ||
| 2 | 768 (35.1) | 657 (39.1) | ||
| 3+ | 399 (18.3) | 530 (31.5) | 145.3 | < 0.001 |
| Age 25–34 | ||||
| 1 | 324 (33.7) | 160 (21.2) | ||
| 2 | 354 (36.8) | 244 (32.4) | ||
| 3+ | 284 (29.5) | 349 (46.3) | 57.9 | < 0.001 |
| Age 35+ | ||||
| 1 | 550 (32.2) | 294 (27.4) | ||
| 2 | 668 (39.1) | 328 (30.5) | ||
| 3+ | 492 (28.8) | 452 (42.1) | 52.9 | < 0.001 |
Discussion
We found little evidence that different restrictions on paracetamol pack sizes in England and Ireland had an impact on sizes of overdoses taken in the two countries. There were peaks in the numbers of tablets taken in paracetamol overdoses in both England and Ireland that reflected the maximum pack sizes in the respective countries. Peaks were also found for multiples of these pack sizes, which could reflect overdoses in which multiple packs were purchased for the acts. The additional peaks in both samples at 10 and multiples of 10 tablets presumably reflect effects of rounding or approximation by patients and possibly clinicians.
There was a marked difference between England and Ireland in terms of the number of pack equivalents of paracetamol taken in overdoses. More pack equivalents were in general consumed in overdoses in Ireland. This difference was found for both sexes and across all three age groups examined. This raises the following questions:
-
Is advice on sales of packs being followed to the same extent in the two countries?
-
Do purchasing patterns differ, with paracetamol packs being bought with greater frequency in Ireland, so that more are available in households?
-
Are there differences in patient characteristics between the two countries influencing patterns of self-poisoning?
-
Are individuals in Ireland who have taken paracetamol overdoses less likely to present to hospital when the amount taken is relatively small?
Unfortunately, we do not have access to over-the-counter (OTC) sales data for the two countries. We have no reason to believe that there are major differences between the sociodemographic characteristics of patients who take paracetamol overdoses in England and the characteristics of patients who take paracetamol overdoses in Ireland, except that it appears that paracetamol is taken more frequently in overdose in England, that the female to male ratio is greater in Ireland, and a somewhat greater proportion of patients in Ireland are in the youngest age group. These differences do not, however, appear large enough to explain the extent of the difference in patterns of pack consumption in overdoses. However, there might be differences in other characteristics that contributed to the findings but which we were unable to compare, such as degree of suicidal intent and other psychological factors. We do not have information in this study on the frequency of hospital presentations in relation to the size of overdoses in the two countries. One important difference between the two countries is that many individuals who present to emergency departments in Ireland are subject to a fee, whereas this is not the case in England. Also, obtaining general practitioner care in Ireland often involves a fee, which could influence willingness to seek help for emotional problems and therefore increase the risk of self-poisoning. The more rural nature of Ireland, and hence larger distances to hospitals for many residents, could also influence presentation to emergency departments.
An important possible explanation for the difference in number of packs used for overdoses in England and Ireland may be less rigorous enforcement of sales advice contained in regulatory notices in Ireland than in England. A study conducted before the Irish legislation was introduced indicated that sales advice for non-pharmacy outlets from the Irish Medicines Board was often not being followed. 94 Following the introduction of the legislation, researchers visiting pharmacy and non-pharmacy outlets in Dublin were able to purchase in excess of statutory limits of paracetamol in a single transaction in half of all pharmacies and the majority of non-pharmacy outlets – a situation that largely persisted when the researchers revisited outlets a year later. 95 Although there is also evidence of breaches of the legislation in non-pharmacy outlets in England,74 this appears to happen to a far lesser degree than in the post-legislation study in Ireland95 (see earlier in this chapter).
Strengths and limitations
The study involved large numbers of patients in both countries: the Irish sample included all overdose presentations to general hospitals in Ireland, and the English sample included presentations to six general hospitals in three centres (although these may not be fully representative of all general hospitals in England). The recording of the number of tablets taken in overdoses relied largely on patient self-report, which is known to be subject to inaccuracy. 42,54,92
It is not known whether or not there was any change in the sizes of overdoses in Ireland following the introduction of the 2001 legislation on pack sizes there. 77 However, the size of overdose for which calls were made to the National Poisons Centre decreased in the first 2 years after the legislation was introduced. 96
We have not been able to examine the impact on actual suicides of the differing legislation in the two countries because data for suicide deaths according to specific drugs ingested are not currently available in Ireland.
Conclusions
No major difference was found between England and Ireland in the size of paracetamol overdose, in spite of differences in maximum pack sizes between the two countries. Although this may suggest that further reductions in pack sizes in the UK would not be effective in further reducing self-poisoning with paracetamol, the finding may reflect differences in adherence to sales guidance in Ireland compared with England, and other factors such as patient characteristics and ease of access to clinical care.
STUDY 4: THE IMPACT OF LIMITATIONS ON PACK SIZES OF ANALGESICS ON USE OF NON-STEROIDAL ANTI-INFLAMMATORY DRUGS AND CONSEQUENT GASTROINTESTINAL BLEEDING AND USE OF MEDICATION FOR GASTROINTESTINAL DISORDERS
Objectives
To investigate whether 1998 legislation to reduce pack sizes of paracetamol (and other analgesics) was followed by increased prescribing of NSAIDs with possible adverse effects on GI bleeding.
Methods
We examined prescriptions for NSAIDs and other analgesics, plus those for medication for GI symptoms, and hospital admissions for GI haemorrhage for the period 1994–2004. We limited the study period to 1994–2004 because in 2004 prescribing of NSAIDs changed markedly because of the withdrawal of some COX-2 inhibitor drugs. 97
Sources of data
Prescriptions
IMS Health provided quarterly data from Disease Analyzer UK on the numbers of patients prescribed drugs in the therapy classes listed below, by age groups 15–34, 35–54, 55–64 and 65+ years, for the years 1994–2004. IMS Disease Analyzer UK is a primary care database containing de-identified general practice patient records continuously collected from around 210 computerised practices throughout the UK. The sample is designed to be representative of the UK population. The drugs for which we analysed data were non-narcotic analgesics (including NSAIDs), antirheumatic non-steroidal drugs, and drugs that might be prescribed to alleviate GI symptoms, including antiulcerants as one category and all other GI drugs as a second category (antacids, antiflatulents, antispasmodics, anticholinergics and gastroprokinetics). The Disease Analyzer data set also contains the number of patients available for diagnosis/treatment.
Hospital admissions
We used the Department of Health's Hospital Episode Statistics Database for England98 to extract quarterly data on the number of hospital admissions for GI haemorrhage between 1994 and 2004, for age groups 15–34, 35–54, 55–64 and 65+ years. Admission rates were calculated using quarterly population figures interpolated from the corresponding annual mid-year population estimates for England from the ONS. 99
Statistical analysis
Gastrointestinal admission and prescription rates (number of admissions and prescriptions per 100,000 population) for each age group were calculated on a quarterly basis using the population data. The impact of the legislation on numbers of GI admissions and prescriptions and trends in GI admission and prescription rates was analysed using interrupted time-series analysis. This method controls for baseline rate and trend when estimating expected changes in the number of GI admissions (or prescriptions) due to the intervention. The third quarter of 1998 was chosen as the point of intervention. All analysis was carried out using Stata version 11.2.
Results
Prescriptions for non-steroidal anti-inflammatory drugs and other analgesics
There was a significant increase in the rate of prescribing of NSAIDs following the 1998 legislation regarding pack sizes of paracetamol of 31.5 per 100,000 per quarter (p = 0.009). There was also an increase in prescribing of other non-narcotic analgesics (p = 0.05) (Table 21 and Figure 7).
| Drug category | Mean quarterly estimated no. of prescriptions at the mid-point after the intervention (per 100,000) | Mean quarterly changea (95% CI) | Change in the trend from before to after the legislation (95% CI) | |
|---|---|---|---|---|
| Without legislationa | With legislationa | |||
| NSAIDs | 3902.7 | 4213.7 | 311 (− 10 to 632) | 31.50 (8.40 to 55.50) |
| Other non-narcotic analgesics | 4832.8 | 5280.3 | 448 (53 to 843) | 31.40 (0.78 to 62.01) |
| Antiulcerants | 2487.0 | 3187.3 | 700 (264 to 1136) | 57.74 (21.11 to 94.36) |
| Other GI drugs | 1974.1 | 2024.0 | 50 (− 93 to 192) | − 0.84 (− 9.74 to 8.05) |
FIGURE 7.
Rates of prescribing of NSAIDs, other non-narcotic analgesics, antiulcerants and other GI drugs, 1994–2004 (second quarter), from a UK primary care database. Source: IMS Health.
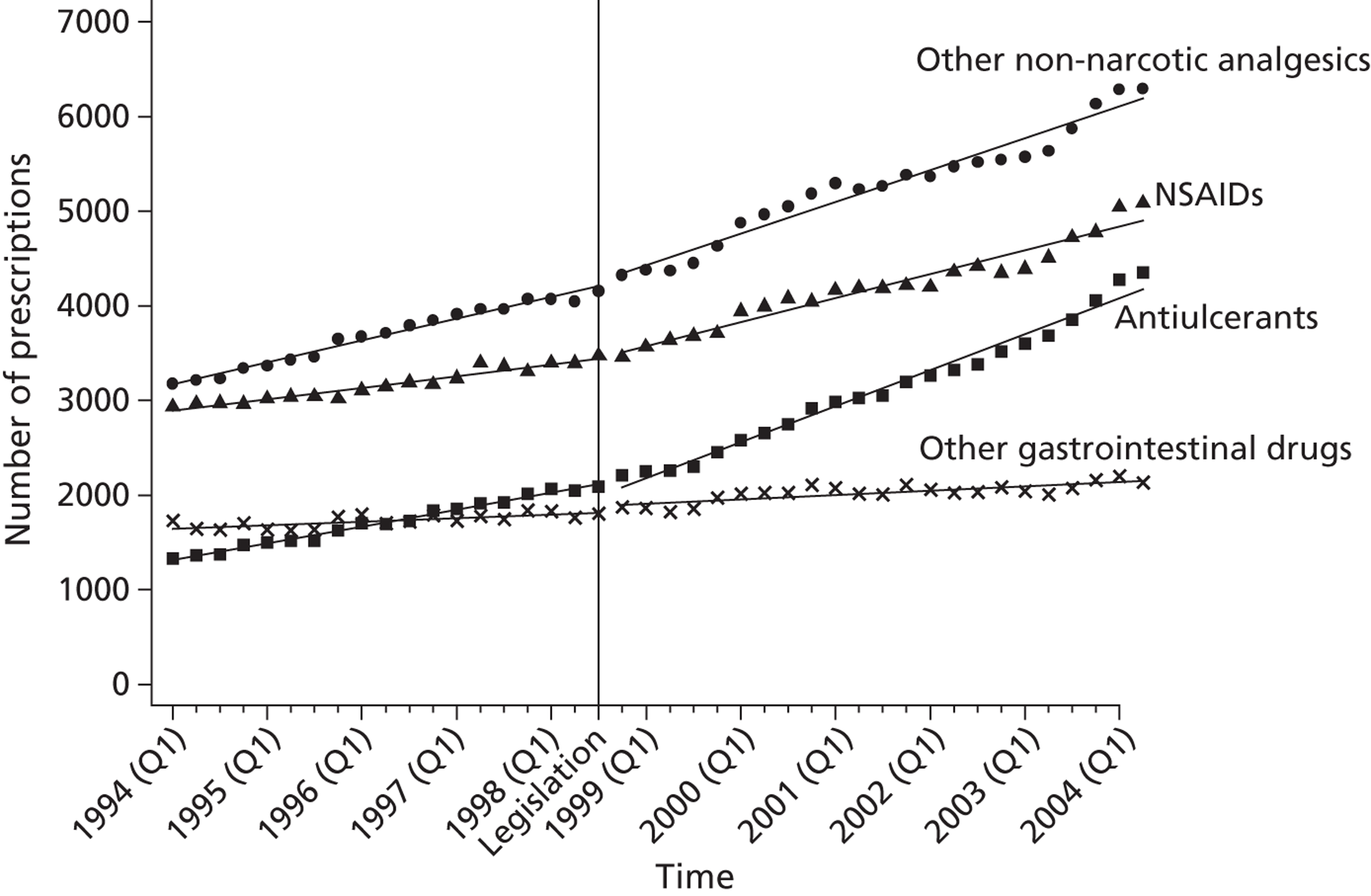
Hospital admissions for gastrointestinal bleeds
There was an immediate increase in the hospital admission rate for GI bleeds of 3.66 per 100,000 per quarter after the 1998 legislation (p = 0.012). However, the rate of change of GI admissions during the whole post-legislation period declined by 0.4 per 100,000 per quarter (p = 0.012) compared with beforehand (Table 22 and Figure 8).
| Mean quarterly estimated no. of GI admissions at the mid-point after the intervention (per 100,000) | Mean quarterly changea (95% CI) | Change in the trend from before to after the legislation (95% CI) | |
|---|---|---|---|
| Without legislation | With legislation | ||
| 70.802 | 69.661 | − 1 (− 6 to 4) | − 0.40 (− 0.71 to − 0.09) |
FIGURE 8.
Rates of hospital admissions in England for GI haemorrhage, 1994–2004 (second quarter).
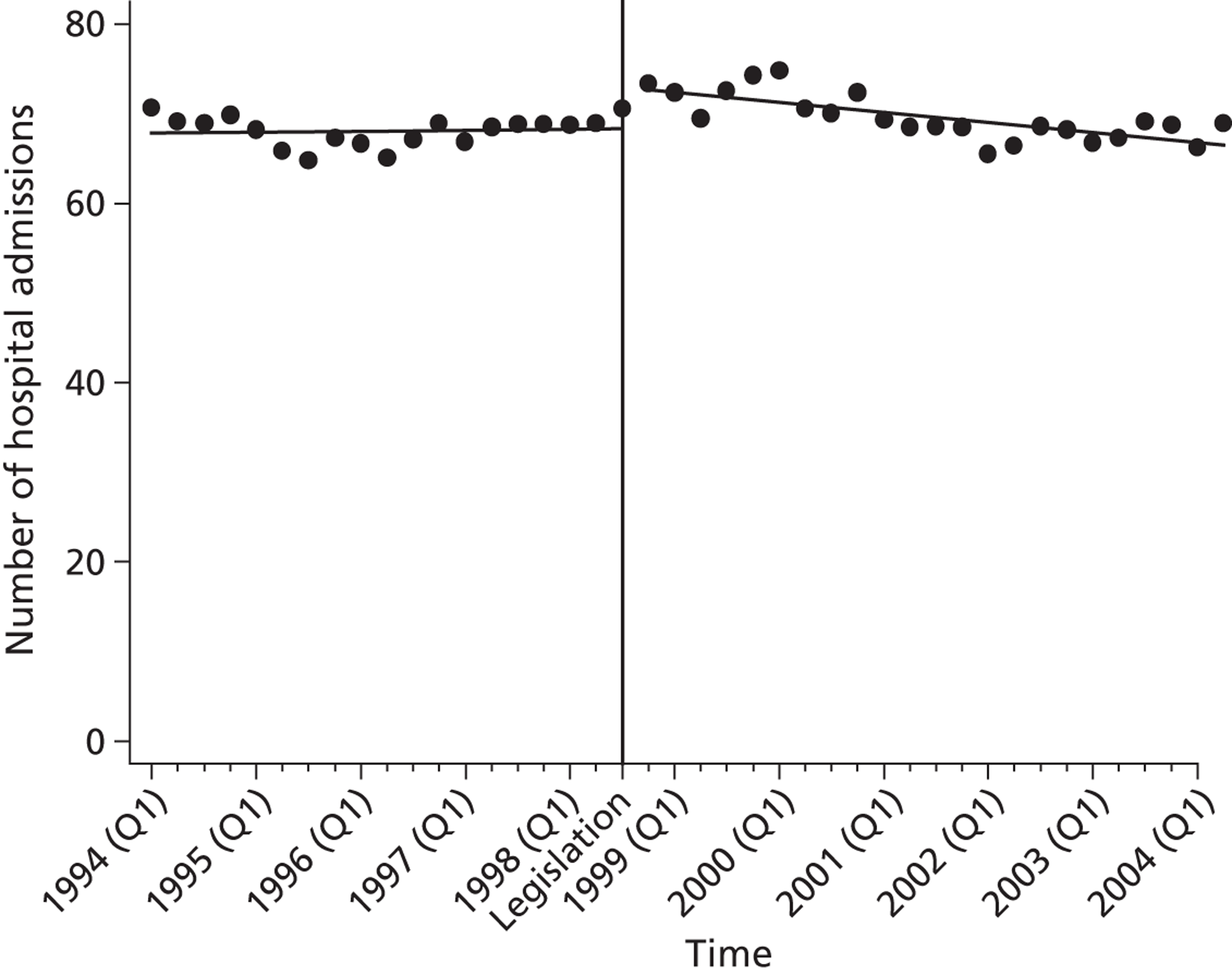
During the study period, the rate of admission for GI bleeds was highest in the 65+ years age group and lowest in the 15–34 years age group. Trends in admission rates showed a decline after the legislation in some age groups (Figure 9), including in those aged 55–64 years (estimated mean change in the trend from before to after the legislation = − 0.63, 95% CI − 1.12 to − 0.14, p = 0.014) and 65+ years (mean change in trend = − 1.34, 95% CI − 2.06 to − 0.62, p = 0.001).
FIGURE 9.
Rates of hospital admissions in England for GI haemorrhage, 1994–2004 (second quarter), by age group.
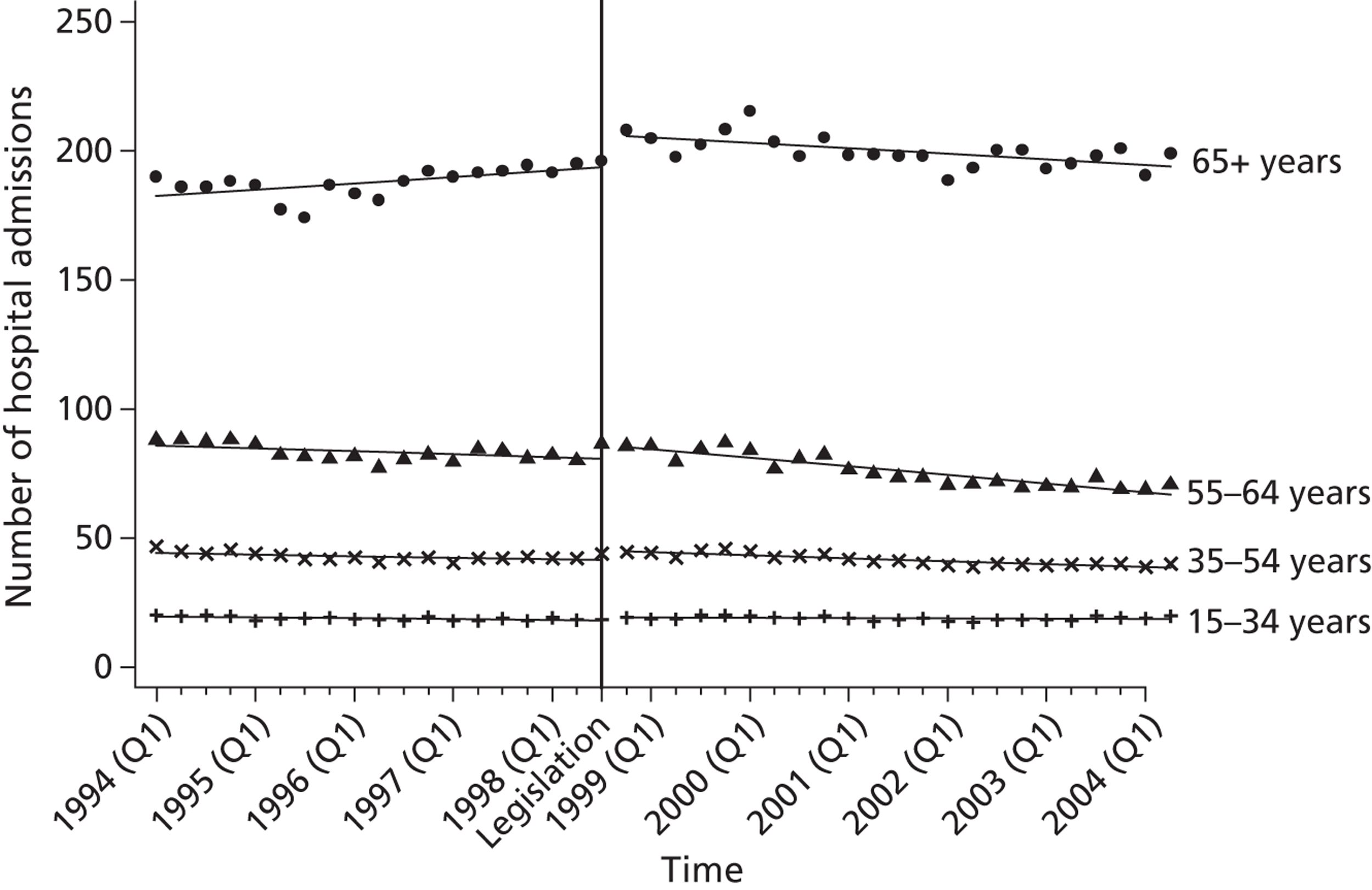
Prescriptions for gastrointestinal drugs
There was a steady overall increase in prescriptions for antiulcerants following the legislation (p < 0.001) (see Table 21 and Figure 7). The increase was significant in the younger age groups [mean change in trend (95% CI) for those aged 15–34 years, 35–54 years and 55–64 years = 9.41 (7.03 to 11.79), 38.25 (17.09 to 59.42) and 90.37 (69.80 to 110.94), respectively (all p ≤ 0.001)], but not in those aged 65+ years [mean change in trend (95% CI) = 22.21 (− 130.76 to 175.17), p = 0.77].
There was no evidence of an increase in prescribing of other GI drugs following the legislation (p = 0.85) (see Table 21). This applied to all age groups except those aged 15–34 years, in whom there was a gradual rise in prescribing over time [mean change in trend (95% CI) = 9.55 (3.32 to 15.77), p = 0.004].
Discussion
The 1998 legislation that limited pack sizes of paracetamol and aspirin was followed by increased prescribing of NSAIDs. There was also an increase in prescribing of other non-narcotic analgesics (which included paracetamol and aspirin). However, these changes were gradual, with no indication of a specific effect of the legislation.
There was no convincing evidence that the legislation had a major secondary impact on hospital admissions for GI bleeds. Although there was an immediate increase in admissions for GI bleeds following the legislation, it was relatively small and was followed by a decreasing trend in hospital admissions (possibly related to increased prescribing of antiulcerants). This decline in admissions was found only in age groups 55–64 years and 65+ years.
Although prescribing of antiulcerants increased following the 1998 legislation, there was no evidence of a stepwise increase, just a rising trend. There was no major change in prescribing of other GI drugs except for an increased trend in the 15–34 years age group. This is in keeping with an earlier finding in relation to the withdrawal of COX-2 inhibitors that no consistent evidence was seen of an adverse influence on trends in the incidence of GI haemorrhages. 97
Limitations
We were unable to examine the impact of the legislation on OTC sales of analgesics, as this information was not available. This is important as any impact might be expected to occur primarily in relation to OTC sales. However, use of the data on admissions for GI bleeds and drugs used to treat GI disturbances allowed us to examine any negative effects of possible changes in use of NSAIDs on gastric health.
Conclusions
Prescribing of NSAIDs increased following the 1998 legislation on pack sizes of paracetamol and other analgesics. However, there was no clear evidence that the legislation had a specific impact on prescribing of NSAIDs as the gradual increase in prescribing of these drugs over time was also seen for other analgesics. There was also no evidence that GI bleeds increased as a result of any altered prescribing (or changes in OTC sales) associated with the legislation. However, a gradual increase in prescribing of antiulcerants could have offset changes in the incidence of GI symptoms.
Chapter 4 Evaluation of the impact of co-proxamol withdrawal in England and Wales on prescribing and deaths
Abstract
Before 2005, the analgesic co-proxamol (a paracetamol and dextropropoxyphene combination) was involved in about 20% of all drug-poisoning suicides and a substantial number of accidental poisonings in the UK. In January 2005, following a review of the efficacy/safety profile of co-proxamol by the MHRA, the Committee on Safety of Medicines (CSM) advised that co-proxamol should be withdrawn from use in the UK; the final date for withdrawal was 31 December 2007. Using interrupted time-series analyses of 1998–2010 data for England and Wales on deaths and prescribing of analgesics, we have shown that withdrawal of co-proxamol has had major beneficial effects on the number of poisoning deaths involving this drug, including deaths by suicide and by accidental poisoning. Furthermore, there is no evidence of significant substitution by poisoning with other analgesics, in spite of their increased prescribing. There were an estimated 500 fewer deaths from suicide between 2005 and 2010 than would be expected without the withdrawal, and 600 fewer deaths when accidental poisonings were included. During the full withdrawal phase (2008–10) there was an average of just 19 suicide and open verdict deaths involving co-proxamol per year (23 per year including accidents), compared with 228 deaths per year during 1998–2004 (271 per year including accidents). In 2009, following the UK lead, the European Medicines Agency recommended that dextropropoxyphene-containing medication be withdrawn throughout the European Union, and a similar initiative has been introduced in the USA and Canada.
Background
For many years concerns have been expressed about the extent of fatal poisoning with the analgesic co-proxamol (a combination of paracetamol and dextropropoxyphene) and, in particular, its use for suicide. 100,101 Death from poisoning with co-proxamol occurs largely because of the toxic effects of high levels of dextropropoxyphene on respiration and cardiac conduction. 102,103 There is also a relatively narrow margin between therapeutic and potentially lethal levels. 104 Between 1997 and 1999, co-proxamol was the single drug used most frequently for suicide in England and Wales (766 deaths over the 3-year period), being implicated in nearly one-fifth of all drug-related poisoning suicides. 101,105
In January 2005, after the MHRA conducted a review of the efficacy/safety profile of co-proxamol,106 the CSM advised that co-proxamol should be withdrawn from use in the UK; the final date of withdrawal was 31 December 2007. 107 During the intervening period (2005–7), doctors were advised not to prescribe co-proxamol to any new patients and to make efforts to move patients currently taking the drug to suitable alternative medication (although patients for whom this was difficult could continue to receive the drug through normal prescribing).
We have conducted two evaluations assessing the impact of co-proxamol withdrawal on prescribing of co-proxamol and other analgesics, and on deaths involving these drugs, in England and Wales. The first evaluation was of the impact of the initial withdrawal phase (2005–7). The second evaluation was of the overall impact of this phase and the 3 subsequent years of full withdrawal. We have investigated drug-poisoning deaths that received a suicide or an open verdict, and also those with a verdict of accidental death, some of which may have been suicidal acts (see Chapter 2 for a full discussion of these terms). Substitution of method is a potential concern when a common means used for suicide becomes less available, particularly when the substituted method has a higher case fatality than the restricted method. 108 For this reason we have also investigated the impact of the withdrawal of co-proxamol on the prescribing of, and deaths involving, other analgesics.
Objective
To investigate the impact of the withdrawal of co-proxamol on the prescribing of analgesics and their use in poisoning deaths, both suicidal and accidental.
Methods
Data types
Prescriptions
Quarterly data for 1998–2010 on prescriptions of co-proxamol, co-codamol, codeine, co-dydramol, dihydrocodeine, NSAIDs, paracetamol and tramadol in England and Wales were obtained from the NHS Health and Social Care Information Centre (England) and Prescribing Services Partneriaeth Cydwasanaethau GIG Cymru (Wales). Prescription data for Wales were not available for the first quarter of 1998 and so figures for this quarter were estimated using least-squares methods to extrapolate from trend data for subsequent quarters.
We also obtained prescription data for oral morphine and oxycodone for England only between 1998 and 2010 (data for Wales were unavailable for some of this period).
Deaths
To evaluate the impact of the withdrawal of co-proxamol on suicide, we have used data on deaths receiving a suicide verdict and those coded as injury or poisoning of undetermined intent (open verdicts) by the ONS (see Chapter 2). In England and Wales it has been customary to assume that most of the latter are cases in which the harm was self-inflicted but there was insufficient evidence to prove intent to die. 32,109
The ONS provided quarterly data on drug-poisoning deaths (suicides, open verdicts and accidental poisonings) involving co-proxamol, co-codamol, codeine, co-dydramol, dihydrocodeine, NSAIDs, paracetamol and tramadol based on death registrations during 1998–2010 in England and Wales. We also received annual death data for oxycodone. Data were obtained from the ONS database of deaths related to drug poisoning, which is extracted from the national mortality database for England and Wales. 110 Analyses were restricted to deaths involving single drugs or single drugs and alcohol. Similar data were supplied for overall drug-poisoning deaths.
Statistical analyses
Analyses of trends in prescribing and deaths were conducted using Stata version 10.0. We used interrupted time-series analysis to estimate changes in levels and trends in prescribing and deaths following the CSM announcement of the withdrawal of co-proxamol. This method controls for baseline level and trend when estimating expected changes in the number of prescriptions (or deaths) due to the intervention. 81
Specifically, segmented regression analysis80 was used to estimate the mean quarterly numbers of prescriptions and deaths that might have occurred in the post-intervention period without the CSM announcement, and the numbers of prescriptions and deaths that actually occurred following the CSM announcement. The latter were obtained from best-fitted data lines from the regressions and are better estimates than taking the average of the actual values. The beginning of 2005 was chosen as the point of intervention. Thus, our data comprised 28 quarters in the pre-intervention segment and 12 in the post-intervention segment for the evaluation of the initial impact of the withdrawal (2005–7) and 24 for the evaluation of the longer-term impact (2005–10). Slope and level regression coefficients were used to estimate the mean quarterly absolute differences in prescriptions and deaths (first, at the mid-point of the withdrawal phase, midway between quarter two and quarter three of 2006; and, second, at the mid-point of the post-intervention period, midway between quarter four of 2007 and quarter one of 2008).
Preliminary analyses indicated some autocorrelation in the data; therefore, the Cochrane–Orcutt autoregression procedure was used (rather than ordinary linear regression) to correct for first-order serially correlated errors. The Durbin–Watson statistic of all final models was close to the preferred value of 2, indicating that no serious autocorrelation remained.
Results
Impact of initial withdrawal phase (2005–7)
Because the impact of the initial withdrawal phase is included in our longer-term evaluation to the end of 2010 (see below), we will only summarise the results of our investigation of this phase.
Prescriptions
There was a 59% reduction in prescribing of co-proxamol in the initial withdrawal period (Table 23 and Figure 10), with increased prescribing of some other analgesics but also decreased prescribing of NSAIDs and dihydrocodeine.
| Data type | Estimation of the absolute effect of the CSM announcement, 2005–7a | ||
|---|---|---|---|
| Mean quarterly estimated no. without announcementb | Mean quarterly estimated no. with announcementb | Mean quarterly change, 2005–7c (95% CId) | |
| Prescriptions (×1000) | |||
| Co-proxamol | 1465.1 | 605.7 | − 859 (− 1065 to − 653) |
| Co-codamol | 2524.7 | 3024.6 | 500 (459 to 540) |
| Codeine | 534.6 | 578.0 | 43 (31 to 55) |
| Co-dydramol | 1018.2 | 1140.0 | 122 (99 to 145) |
| Dihydrocodeine | 634.6 | 600.0 | − 35 (− 68 to − 2) |
| NSAIDs | 5633.8 | 4581.0 | − 1053 (− 1186 to − 920) |
| Paracetamol | 2947.0 | 3330.0 | 383 (268 to 497) |
| Tramadol | 1130.1 | 1193.9 | 64 (− 5 to 133) |
| Deaths: suicide and open | |||
| Co-proxamol | 39 | 20 | − 19 (− 29 to − 8) |
| Other analgesicse | 40 | 45 | 6 (− 4 to 16) |
| All drugs (except co-proxamol and other analgesics) | 204 | 186 | − 18 (− 39 to 3) |
| All drugs | 283 | 252 | − 31 (− 66 to 3) |
| All causes | 1152 | 1130 | − 22 (− 89 to 45) |
| Deaths: suicide, open and accidental | |||
| Co-proxamol | 47 | 25 | − 22 (− 32 to − 13) |
| Other analgesicse | 57 | 62 | 5 (− 9 to 19) |
| All drugs (except co-proxamol and other analgesics) | 350 | 379 | 29 (− 18 to 76) |
| All drugs | 452 | 466 | 14 (− 46 to 74) |
FIGURE 10.
Trends in prescriptions dispensed for co-proxamol and seven other analgesics in England and Wales, 1998–2010.
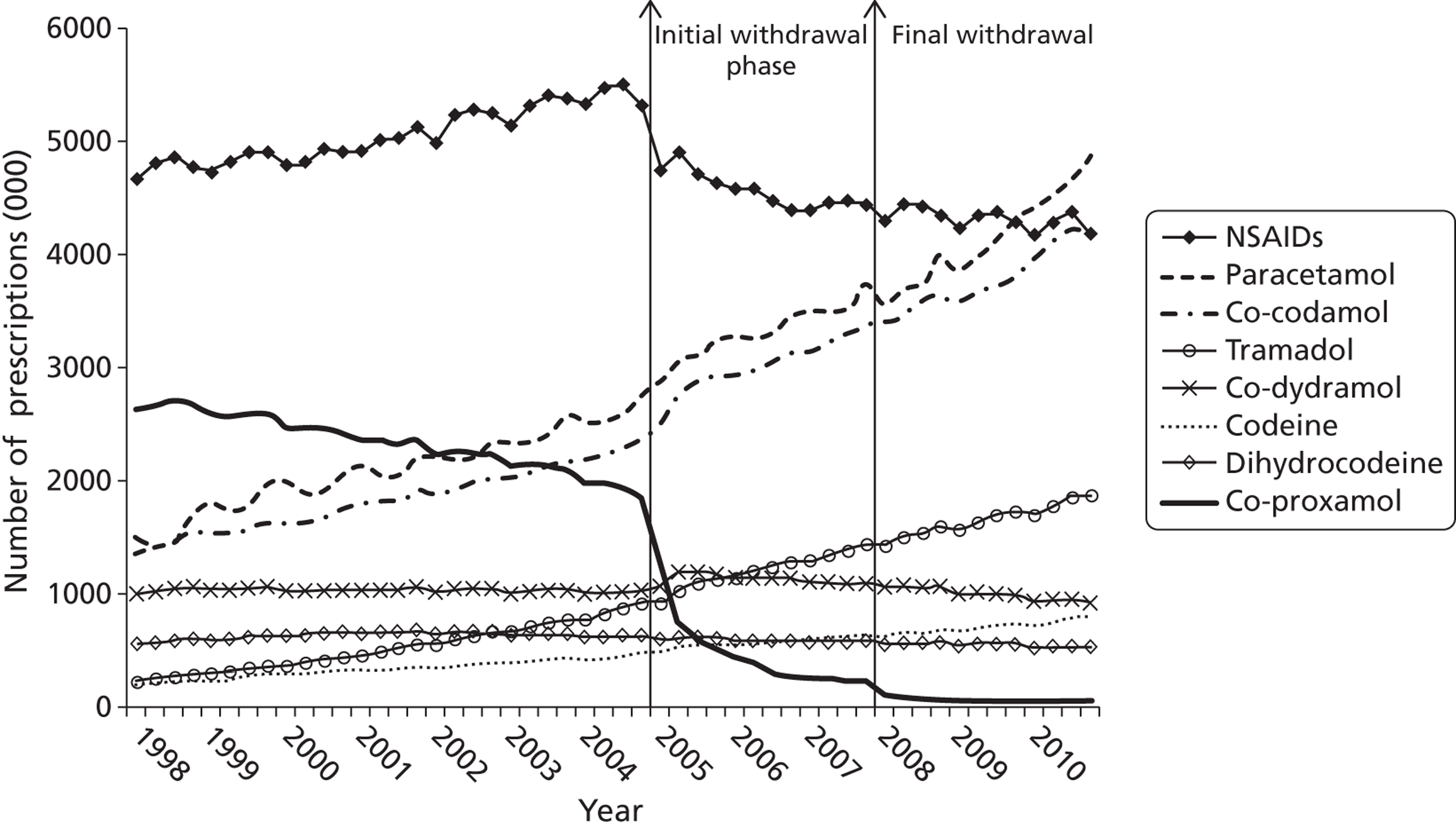
Deaths
There was a marked reduction in the numbers of suicides and open verdicts involving co-proxamol between 2005 and 2007 (Figure 11 and Table 24). Before 2005, deaths from poisoning with co-proxamol alone made up 17.5% of all drug-poisoning suicides (95% CI 15.5% to 19.5%), whereas between 2005 and 2007 they constituted just 8.3% (95% CI 4.3 to 12.3%) (see Table 24).
| Year | All causes, n | All drugs, n | Co-proxamol alone, n (% of all drug-poisoning deaths) | Other analgesicsa alone, n (% of all drug-poisoning deaths) | |||
|---|---|---|---|---|---|---|---|
| Suicide and open | Suicide and open | Suicide, open and accidental | Suicide and open | Suicide, open and accidental | Suicide and open | Suicide, open and accidental | |
| 1998 | 5347 | 1432 | 2246 | 259 (18.1) | 309 (13.8) | 202 (14.1) | 277 (12.3) |
| 1999 | 5241 | 1414 | 2294 | 260 (18.4) | 316 (13.8) | 207 (14.6) | 279 (12.2) |
| 2000 | 5081 | 1309 | 2143 | 261 (19.9) | 303 (14.1) | 175 (13.4) | 230 (10.7) |
| 2001 | 4904 | 1279 | 2180 | 232 (18.1) | 276 (12.7) | 195 (15.2) | 257 (11.8) |
| 2002 | 4762 | 1225 | 1983 | 204 (16.7) | 247 (12.5) | 182 (14.9) | 237 (12.0) |
| 2003 | 4811 | 1194 | 1843 | 188 (15.7) | 218 (11.8) | 166 (13.9) | 237 (12.9) |
| 2004 | 4883 | 1246 | 2006 | 189 (15.2) | 230 (11.5) | 168 (13.5) | 233 (11.6) |
| 2005 | 4718 | 1154 | 1926 | 131 (11.4) | 157 (8.2) | 196 (17.0) | 254 (13.2) |
| 2006 | 4513 | 979 | 1821 | 67 (6.8) | 81 (4.4) | 200 (20.4) | 287 (15.8) |
| 2007 | 4322 | 888 | 1852 | 52 (5.9) | 61 (3.3) | 151 (17.0) | 209 (11.3) |
| 2008 | 4603 | 884 | 2071 | 29 (3.3) | 34 (1.6) | 157 (17.8) | 257 (12.4) |
| 2009 | 4682 | 898 | 2185 | 21 (2.3) | 26 (1.2) | 155 (17.3) | 267 (12.2) |
| 2010 | 4528 | 873 | 2137 | 8 (0.9) | 10 (0.5) | 150 (17.2) | 257 (12.0) |
Regression analyses indicated a significant decrease in both level and slope for deaths involving co-proxamol that received a suicide or an open verdict (Table 25). The number of deaths decreased by an average of 19 per quarter in the post-intervention period (95% CI 8 to 29 deaths per quarter) (see Table 23). This equated to an estimated overall decrease of 226 deaths (95% CI 190 to 262 deaths), approximately 48%, in the 3-year post-intervention period (2005–7) compared with 1998–2004.
When accidental poisoning deaths involving co-proxamol were included, there was a mean quarterly decrease of 22 deaths (95% CI 13 to 32 deaths), which equated to an overall decrease of 268 deaths (95% CI 235 to 300 deaths), approximately 47%, in the 3-year post-intervention period (2005–7) (see Table 23).
There were no statistically significant changes in level or slope in the post-intervention period for deaths involving the other analgesics, both for those deaths that received a suicide or open verdict (mean quarterly change = 6, 95% CI − 4 to 16 deaths) and when accidental poisoning deaths were also included (mean quarterly change = 5, 95% CI − 9 to 19 deaths).
| Data type | Regression coefficients and standard errors (SEs) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre interventiona | Post interventiona | |||||||||||
| Base-level coefficient (β0) | SE | p-value | Base-trend coefficient (β1) | SE | p-value | Change in level (β2) | SE | p-value | Change in trend (β3) | SE | p-value | |
| Prescriptions (×1000) | ||||||||||||
| Co-proxamol | 3263.058 | 350.294 | < 0.001 | − 55.438 | 13.813 | < 0.001 | − 581.900 | 48.575 | < 0.001 | 3.712 | 16.499 | 0.823 |
| Co-codamol | 1337.508 | 18.694 | < 0.001 | 35.189 | 1.194 | < 0.001 | 245.072 | 69.509 | 0.001 | 31.573 | 4.052 | < 0.001 |
| Codeine | 204.962 | 3.943 | < 0.001 | 9.543 | 0.230 | < 0.001 | 23.098 | 7.359 | 0.003 | 2.711 | 0.527 | < 0.001 |
| Co-dydramol | 1054.915 | 6.092 | < 0.001 | − 1.018 | 0.355 | 0.006 | 178.873 | 25.633 | < 0.001 | − 9.476 | 1.499 | < 0.001 |
| Dihydrocodeine | 659.523 | 21.364 | < 0.001 | − 0.394 | 0.998 | 0.695 | − 29.717 | 4.751 | < 0.001 | − 2.703 | 1.570 | 0.092 |
| NSAIDs | 4655.803 | 47.083 | < 0.001 | 28.125 | 3.000 | < 0.001 | − 707.122 | 68.453 | < 0.001 | − 50.755 | 4.981 | < 0.001 |
| Paracetamol | 1488.220 | 99.268 | < 0.001 | 42.798 | 5.124 | < 0.001 | 94.470 | 61.795 | 0.133 | 34.323 | 7.741 | < 0.001 |
| Tramadol | 158.794 | 14.675 | < 0.001 | 25.882 | 0.913 | < 0.001 | 74.309 | 33.695 | 0.032 | 12.756 | 1.856 | < 0.001 |
| Other analgesics (excluding NSAIDs)b | 4880.483 | 72.010 | < 0.001 | 112.492 | 4.332 | < 0.001 | 642.097 | 156.145 | < 0.001 | 64.849 | 10.046 | < 0.001 |
| Other analgesicsb | 9533.461 | 60.185 | < 0.001 | 14.086 | 3.613 | < 0.001 | − 72.139 | 163.290 | 0.661 | 14.006 | 11.198 | 0.217 |
| Deaths: suicide and open | ||||||||||||
| Co-proxamol | 70.111 | 3.478 | < 0.001 | − 0.890 | 0.239 | < 0.001 | − 15.558 | 4.932 | 0.003 | − 0.430 | 0.331 | 0.201 |
| Co-codamol | 2.482 | 1.327 | 0.068 | 0.045 | 0.073 | 0.538 | 1.310 | 1.567 | 0.407 | − 0.044 | 0.104 | 0.673 |
| Codeine | 0.913 | 0.542 | 0.099 | 0.096 | 0.052 | 0.072 | − 0.167 | 1.403 | 0.906 | 0.016 | 0.101 | 0.875 |
| Co-dydramol | 1.753 | 0.302 | < 0.001 | − 0.022 | 0.017 | 0.206 | 1.229 | 0.653 | 0.066 | − 0.075 | 0.038 | 0.054 |
| Dihydrocodeine | 9.474 | 2.281 | < 0.001 | − 0.107 | 0.113 | 0.346 | 1.069 | 1.512 | 0.483 | − 0.007 | 0.129 | 0.958 |
| NSAIDs | 4.834 | 1.016 | < 0.001 | − 0.120 | 0.056 | 0.039 | 0.968 | 0.936 | 0.306 | 0.068 | 0.069 | 0.327 |
| Paracetamol | 30.002 | 2.341 | < 0.001 | − 0.323 | 0.139 | 0.025 | 2.289 | 2.837 | 0.424 | − 0.097 | 0.179 | 0.592 |
| Tramadol | 0.908 | 0.557 | 0.110 | 0.127 | 0.032 | 0.000 | 0.378 | 1.192 | 0.752 | − 0.116 | 0.074 | 0.125 |
| Other analgesics (excluding NSAIDs)b | 45.471 | 3.236 | < 0.001 | − 0.173 | 0.199 | 0.388 | 5.426 | 4.710 | 0.255 | − 0.297 | 0.282 | 0.298 |
| Other analgesicsb | 50.406 | 2.828 | < 0.001 | − 0.305 | 0.198 | 0.132 | 6.976 | 4.870 | 0.159 | − 0.243 | 0.276 | 0.383 |
| All drugs except co-proxamol and other analgesics | 232.587 | 8.993 | < 0.001 | − 0.780 | 0.545 | 0.159 | − 20.377 | 11.118 | 0.073 | 0.080 | 0.740 | 0.915 |
| All drugs | 351.810 | 12.579 | < 0.001 | − 1.890 | 0.848 | 0.031 | − 31.642 | 18.168 | 0.088 | − 0.592 | 1.161 | 0.612 |
| All causes | 1316.784 | 26.003 | < 0.001 | − 4.632 | 1.601 | 0.006 | − 56.336 | 37.768 | 0.142 | 5.415 | 2.360 | 0.026 |
| Deaths: suicide, open and accidental | ||||||||||||
| Co-proxamol | 83.199 | 3.398 | < 0.001 | − 1.054 | 0.221 | < 0.001 | − 18.161 | 4.983 | 0.001 | − 0.554 | 0.324 | 0.094 |
| Other analgesics (excluding NSAIDs)b | 60.399 | 3.945 | < 0.001 | − 0.147 | 0.244 | 0.549 | 2.052 | 7.096 | 0.774 | 0.387 | 0.447 | 0.390 |
| Other analgesicsb | 66.354 | 3.942 | < 0.001 | − 0.279 | 0.258 | 0.285 | 2.401 | 7.677 | 0.756 | 0.488 | 0.462 | 0.295 |
| All drugs except co-proxamol and other analgesics | 428.311 | 13.917 | < 0.001 | − 2.274 | 0.967 | 0.023 | − 24.940 | 21.317 | 0.248 | 8.740 | 1.681 | < 0.001 |
| All drugs | 578.543 | 18.273 | < 0.001 | − 3.647 | 1.289 | 0.007 | − 39.643 | 27.992 | 0.163 | 8.658 | 2.091 | < 0.001 |
Impact of longer-term withdrawal (2005–10)
Prescriptions
At the beginning of 2008, following the initial step-change reduction in prescribing of co-proxamol in England and Wales during 2005–7 compared with the trend in prescribing during 1998–2004, there was a further downwards step in prescribing such that there were very few prescriptions dispensed during 2008–10 (see Figure 10). Overall, between 2005 and 2010 there was a 53% reduction in prescribing of co-proxamol compared with previous trends (Table 26).
There were significant increases in prescribing of co-codamol (+ 23%), paracetamol (+ 16%), codeine (+ 10%), co-dydramol (+ 6%) and tramadol (+ 19%) during 2005–10 (see Figure 10 and Tables 25 and 26), and a sharp decrease in prescribing of NSAIDs (which was due to safety concerns about COX-2 inhibitors114), which began shortly before the withdrawal of co-proxamol. There was also a decrease in prescribing of dihydrocodeine (− 10%) in 2005–10. Overall, when all seven analgesics (excluding co-proxamol) were combined, there was no significant change in prescriptions, in either level or trend, associated with the withdrawal of co-proxamol. With NSAIDs excluded, however, there was a significant 15% increase in prescribing of the other six analgesics combined.
Prescription data for morphine were available only for England for the study period. Our analysis showed a significant mean quarterly increase in the number of prescriptions of morphine associated with the CSM announcement, up to 71,000 prescriptions (95% CI 62,000 to 79,000 prescriptions), equating to a 35% increase in the period 2005 to 2010.
Prescription data for oxycodone were also available only for England for the study period. The number of prescriptions increased steadily from very low levels (mean of 69,000 per year in 1998–2004) to a mean of 527,000 per year in 2005–10. Because of small numbers, an interrupted time-series analysis (as conducted on other prescription data) did not generate meaningful estimates.
| Prescriptions (×1000) | Estimation of the absolute effect of the CSM announcement during 2005–10a | ||
|---|---|---|---|
| Mean quarterly estimated no. without announcementb | Mean quarterly estimated no. with announcementb | Mean quarterly change 2005–10c (95% CId) | |
| Co-proxamol | 1018 | 482 | − 536 (− 941 to − 130) |
| Co-codamol | 2762 | 3402 | 640 (554 to 726) |
| Codeine | 591 | 648 | 57 (44 to 70) |
| Co-dydramol | 1014 | 1074 | 60 (36 to 85) |
| Dihydrocodeine | 643 | 580 | − 63 (− 105 to − 22) |
| NSAIDs | 5794 | 4453 | − 1341 (− 1507 to − 1176) |
| Paracetamol | 3222 | 3745 | 523 (288 to 759) |
| Tramadol | 1207 | 1440 | 233 (179 to 288) |
| All analgesics except co-proxamol | 10,104 | 10,207 | 103 (− 132 to 337) |
| All analgesics except co-proxamol and NSAIDs | 9436 | 10,889 | 1453 (1200 to 1706) |
Deaths involving co-proxamol and other analgesics
Table 24 shows the numbers of deaths reported as suicide (including open verdicts) or accidental poisoning between 1998 and 2010 involving co-proxamol alone and those involving the seven other analgesics alone (both with and without alcohol), together with all drug-poisoning deaths and all suicides. Between 2005 and 2010 there was a marked reduction in the number and proportion of all poisoning deaths recorded as suicide that involved co-proxamol. Although the number of deaths involving other analgesics receiving a suicide or an open verdict was lower in 2007–10 than in earlier years, their proportionate contribution to total drug-poisoning deaths increased somewhat (presumably because the overall number of deaths declined in line with the reduction in co-proxamol deaths). There was a similar marked decrease in number of deaths involving co-proxamol when accidental deaths were included, but without an increase in percentage of poisoning deaths involving other analgesics (although the number of accidental poisonings with other analgesics increased slightly in 2008–10). Exclusion of NSAIDs made little difference to the results of these analyses.
Figure 11 shows graphically the impact of the initial withdrawal phase (2005–7) and the full withdrawal (2008–10) on both deaths involving co-proxamol and deaths involving other analgesics. There was some reduction in number of deaths involving co-proxamol in the years preceding the beginning of the initial withdrawal phase (1998–2005), then a steady, marked reduction during the initial withdrawal phase (2005–7), with a further, smaller reduction during the first 3 years of the full withdrawal (2008–10). The number of deaths involving other analgesics did not appear to change markedly during these periods.
The overall apparent beneficial changes following the withdrawal of co-proxamol were confirmed when the data were subjected to interrupted time-series regression analyses (Table 27). During the 2005–10 period, there was a highly significant mean quarterly reduction in number of deaths involving co-proxamol alone that received a suicide (including open) verdict (− 21, 95% CI − 34 to − 8 deaths), and a similar reduction when accidental deaths were included (− 25, 95% CI − 38 to − 12 deaths). There was no significant change in number of deaths involving the seven other analgesics combined. When we examined these drugs separately (see Table 25), none showed a significant step or trend change associated with the withdrawal of co-proxamol. There were increases in numbers of deaths involving co-codamol and codeine during the overall study period, but these began well before the withdrawal of co-proxamol. All drug-poisoning deaths (excluding those involving co-proxamol and other analgesics) receiving a suicide or open verdict were reduced following the withdrawal of co-proxamol, although when accidental deaths were included there was a significant increase of 84 deaths per quarter (95% CI 28 to 141 deaths per quarter) (see Table 27).
FIGURE 11.
Deaths in England and Wales from poisoning with co-proxamol and other analgesics, 1998–2010 (suicide and open verdicts, substances taken alone, with or without alcohol).
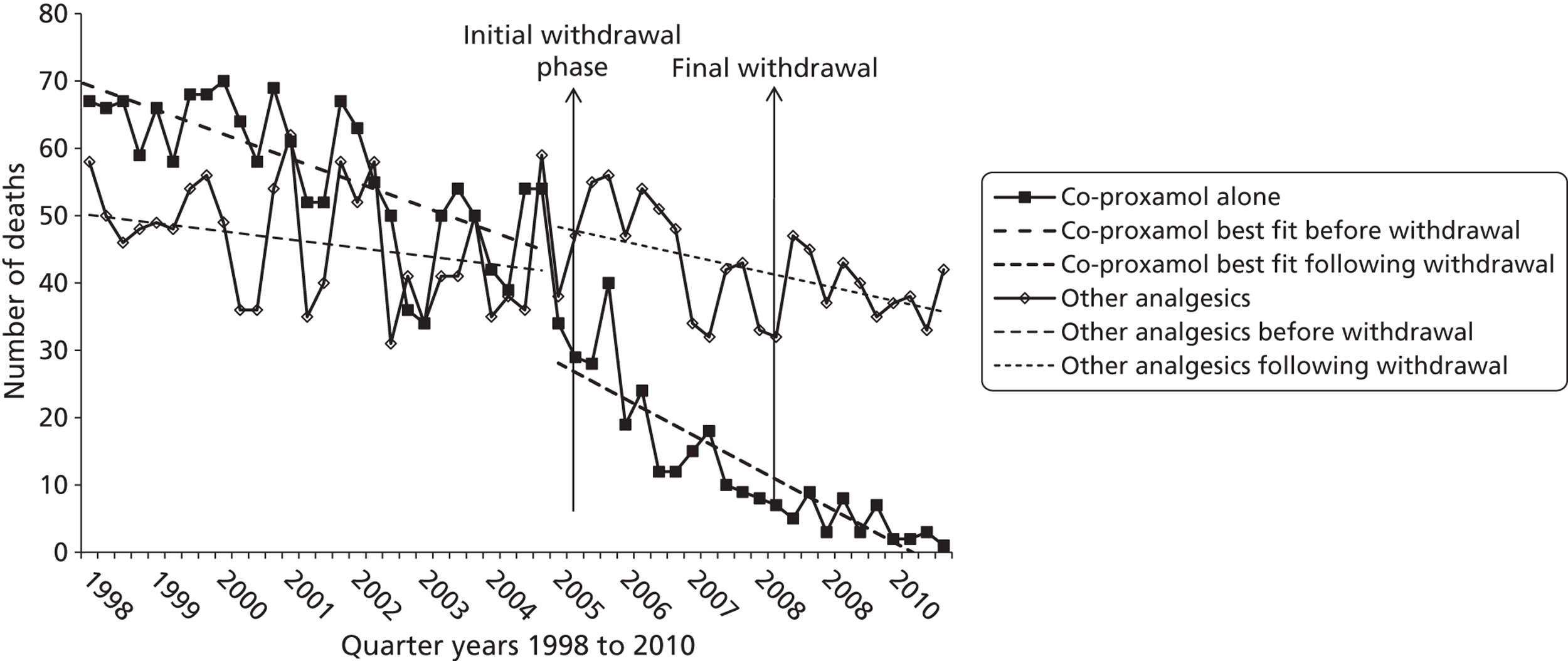
| Cause of death | Estimation of the absolute effect of the CSM announcement during 2005–10a | ||
|---|---|---|---|
| Mean quarterly estimated no. without announcementb | Mean quarterly estimated no. with announcementb | Mean quarterly change 2005–10c (95% CId) | |
| Suicide and open | |||
| Co-proxamol | 34 | 13 | − 21 (− 34 to − 8) |
| Other analgesicse | 38 | 42 | 4 (− 8 to 16) |
| Other analgesicse (except NSAIDs) | 38 | 40 | 2 (− 10 to 13) |
| All drugs (except co-proxamol and other analgesics) | 201 | 181 | − 19 (− 49 to 10) |
| All drugs | 275 | 236 | − 39 (− 87 to 9) |
| All causes | 1129 | 1140 | 11 (− 81 to 104) |
| Suicide, open and accidental | |||
| Co-proxamol | 40 | 15 | − 25 (− 38 to − 12) |
| Other analgesicse | 55 | 63 | 8 (− 7 to 24) |
| Other analgesicse (except NSAIDs) | 54 | 61 | 7 (− 7 to 21) |
| All drugs (except co-proxamol and other analgesics) | 336 | 420 | 84 (28 to 141) |
| All drugs | 430 | 499 | 69 (− 7 to 144) |
The estimated reduction in number of deaths involving co-proxamol alone between 1998–2004 and 2005–10 was 61% for suicide and open verdict deaths and 62% when accidental deaths were included. This reduction equated to approximately 500 fewer deaths from suicide between 2005 and 2010 than would be expected without the withdrawal, and 600 fewer deaths when accidental poisonings were included. As can be seen in Table 24, during the full withdrawal phase (2008–10) there was an average of just 19 deaths per year (23 per year including accidents). This figure is in contrast to the 228 deaths per year during 1998–2004 (271 per year including accidents).
We have not presented data on deaths involving morphine because the ONS cannot distinguish between deaths resulting from oral administration and deaths resulting from intravenous administration (and between those due to morphine and those due to heroin). Deaths involving oxycodone alone and receiving suicide, open or accidental verdicts increased during the study period from a mean of 2.3 per year between 2001 and 2004 to a mean of 8.2 per year between 2005 and 2010 (including 15 in 2010).
Discussion
We have demonstrated an apparent beneficial effect of withdrawal of co-proxamol in England and Wales during the initial 3-year withdrawal phase (2005–7) in terms of numbers of deaths (suicides, open verdicts and accidents). We have also shown that there were further significant changes following full withdrawal of co-proxamol in January 2008, in terms of not only the expected reduced prescribing of co-proxamol, but also the increased prescribing of some other analgesics suggested by the CSM as substitutes for co-proxamol (paracetamol, co-codamol, codeine and co-dydramol; and, for progressive chronic pain, oxycodone and morphine), and also tramadol. During 2005–10 there was a 61% reduction in deaths from co-proxamol poisoning, equating to approximately 500 fewer deaths receiving suicide or open verdicts, and 600 when accidental poisonings were included. Some of the accidental poisonings are also likely to have been probable suicides, especially because of the recent increase in narrative verdicts by coroners, as highlighted in Chapter 2, and the fact that those responsible for coding cause of death at the ONS have difficulty in deciding the cause from the narrative and are therefore obliged by international convention to record the death as accidental. 29 Most importantly, the major reduction in number of deaths involving co-proxamol was not associated with a compensatory overall increase in number of deaths from poisoning with other analgesics (although the number of accidental poisonings with other analgesics increased in the period 2008–10).
During the full withdrawal phase, prescribing of co-proxamol did not cease completely, presumably because of off-licence prescribing. Also, deaths from poisoning with co-proxamol did not reach zero (although there were just eight suicide deaths involving co-proxamol in 2010, and 10 including accidental poisonings); again, this may be partly because of off-licence prescribing, but also because of residual supplies remaining in homes, and possibly supplies obtained through the internet. The acute reduction in prescribing of NSAIDs that began just before the withdrawal of co-proxamol because of concerns about COX-2 inhibitors111 would have been unlikely to have affected the findings as NSAIDs alone are rarely implicated in poisoning deaths, especially by suicide. 12
There was an overall reduction in number of poisoning deaths receiving suicide or open verdicts in England and Wales in 2005–10, although this did not reach statistical significance and was not paralleled by a decline in number of overall drug-poisoning deaths (possibly because of an increase in narrative verdicts; see Chapter 2). However, the number of suicides overall was not reduced, possibly because of the effects of the recession that began in 2008. 112,113 The increase in number of overall poisoning deaths during 2005–10 appears to be related to increased numbers of deaths involving methadone and also benzodiazepines, usually combined with other drugs. 110
Strengths and limitations
One strength of this study is that it is based on national data and includes reasonably long pre-intervention (7 years) and post-intervention (6 years) periods. Also, the method of statistical analysis (interrupted time-series regression) controls for baseline trends when estimating effects of the intervention on prescribing and deaths, which is preferable to methods such as comparison of changes in proportions before and after the intervention. However, estimates of overall effects do involve extrapolation and hence are subject to some degree of uncertainty. Also, percentage changes during the post-intervention period compared with the pre-intervention period are based on mean quarterly change estimates, which have associated uncertainty, and therefore should be interpreted with caution.
To ensure that we were examining deaths due to specific drugs, we based our mortality calculations solely on deaths involving single analgesics alone (with or without alcohol). There are also considerable numbers of poisoning deaths involving multiple drugs. 110 When co-proxamol is one of the drugs, it is very likely to have been the lethal agent, given its high toxicity. It is possible, therefore, that our findings underestimate the full effects of the withdrawal of co-proxamol. The increasing number of narrative verdicts recorded by coroners in England and Wales29 could have influenced the findings through a small reduction in suicide verdicts, although this would probably have equally affected poisonings with co-proxamol and the other analgesics, and any impact would have been included in our analysis of suicide, open and accidental deaths combined.
We have presented prescription data for the analgesics that we have investigated. For some analgesics, notably paracetamol and co-codamol, sales will mainly be OTC rather than through prescription. Comprehensive OTC sales data are unfortunately not available; this would not, of course, affect the validity of the mortality data.
As noted above, we were unable to investigate the impact of the withdrawal of co-proxamol on deaths involving morphine; however, most of such deaths result from illicit drug use. 110
Finally, we have not been able to assess possible compensatory increases in numbers of deaths involving methods other than poisoning that may have occurred following the withdrawal of co-proxamol. This is because of the range of other potential methods of suicide and also the likely temporal effects of other influences, such as the economic recession. However, as individuals tend to show a preference for particular methods of suicide,108 it is unlikely that any such effect would have been substantial.
Conclusions
Withdrawal of co-proxamol in the UK appears to have had major beneficial effects on the number of poisoning deaths involving this drug, including suicides and accidental poisonings, with no evidence of significant substitution by poisoning with other analgesics, in spite of their increased prescribing. In June 2009, following the UK lead, the European Medicines Agency recommended that dextropropoxyphene-containing medication be withdrawn throughout the European Union. 114 This became European policy in June 2010, with full withdrawal by September 2011. In 2009, a US Food and Drug Administration (FDA) panel recommended that the FDA should withdraw dextropropoxyphene from the US market,115 and in 2010 the FDA instructed manufacturers to cease production. 116 Also, in 2010 all dextropropoxyphene products were withdrawn in Canada. 117 The impact of this initiative should now be evaluated on a larger scale.
Chapter 5 Toxicity of antidepressants: study of rates of suicide relative to prescribing and non-fatal overdose
Abstract
We have assessed the relative toxicity of antidepressants, including specific TCAs, a serotonin–noradrenaline reuptake inhibitor (SNRI), a noradrenergic and specific serotonergic antidepressant (NaSSA) and selective serotonin reuptake inhibitors (SSRIs). We conducted an observational study between 2000 and 2006 of prescriptions (UK), poisoning deaths involving single antidepressants receiving a coroner's verdict of suicide or an open verdict (England and Wales), and non-fatal self-poisoning episodes presenting to six general hospitals (in Oxford, Manchester and Derby). We calculated toxicity based on (1) the ratio of rate of deaths to rate of prescriptions (fatal toxicity index) and (2) the ratio of rate of deaths to rate of non-fatal self-poisonings (case fatality index). Fatal toxicity and case fatality indices provided very similar results (rho for relative ranking of indices = 0.99). Case fatality rate ratios showed greater toxicity for TCAs (13.8, 95% CI 13.0 to 14.7) than for the SNRI venlafaxine (2.5, 95% CI 2.0 to 3.1) and the NaSSA mirtazapine (1.9, 95% CI 1.1 to 2.9), both of which had greater toxicity than the SSRIs (0.5, 95% CI 0.4 to 0.7). Within the TCAs, compared with amitriptyline, both dosulepin (relative toxicity index 2.7) and doxepin (Sinepin®, Marlborough) (relative toxicity index 2.6) were more toxic. Within the SSRIs, citalopram had a higher case fatality than the other SSRIs (1.1, 95% CI 0.8 to 1.4, vs. 0.3, 95% CI 0.2 to 0.4). The results showed wide differences in toxicity not only between classes of antidepressants, but also within classes. The findings are relevant to prescribing decisions, especially in individuals at risk, and to regulatory policy.
Background
Self-poisoning is a common method of suicide, especially among women. 9 Antidepressants are frequently used for self-poisoning, being involved in around 20% of all poisoning suicides in the UK9 and in 20–30% of non-fatal overdoses. 1 This reflects the facts that depression is the most frequent psychiatric disorder in people dying by suicide,118 the method used for suicidal acts is often determined by availability11 and self-poisoning in depressed individuals often involves antidepressants prescribed for them. 119
Relative toxicity is an important factor likely to determine the outcome of an antidepressant overdose. Studies using different approaches have shown wide variation in the relative toxicity of antidepressants,120,121 with the older TCAs generally being more toxic than the newer SSRIs. 120,121 In this component study of our research programme, we have used two approaches to assessing the relative toxicity of classes of antidepressants and individual antidepressants. The first approach was to relate drug-specific poisoning mortality rates to prescription rates – termed the ‘fatal toxicity index’. 122 The second, and generally less-used, approach is to compare the rate of death with the rate of non-fatal self-poisoning,121,123 which generates a ‘case fatality index’. The fatal toxicity index approach is probably less accurate because it is more heavily influenced by prescribing policies, including the use of some antidepressants for conditions other than depression,124 and selective prescribing, for example based on the clinician's assessment of suicide risk (i.e. confounding by indication).
Objectives
The specific aims of the study were to provide up-to-date information on the relative toxicity of individual antidepressants to assist clinicians in making decisions about prescribing and to inform interventions by regulatory authorities.
Methods
The antidepressants investigated in this study were the TCAs amitriptyline, clomipramine, dosulepin, doxepin, imipramine, nortriptyline and trimipramine; the SNRI venlafaxine; the NaSSA mirtazapine; and the SSRIs citalopram, fluoxetine, fluvoxamine, paroxetine and sertraline. The period covered by the study was 2000–6. Escitalopram was not included as it first became available in the UK in 2003.
Prescriptions
Quarterly estimates for the years 2000–6 for the UK for the numbers of antidepressant prescriptions dispensed in the community were obtained from the Medical Data Index and supplied by IMS Health. 125 Mid-year population estimates for the UK for the years 2000–6 were obtained from the ONS. 126 Rates of prescribing were calculated per 100,000 population for people of all ages for the years 2000–6 combined. We were unable to take account of average numbers of prescriptions per course of treatment.
Deaths
Information on drug-poisoning deaths receiving a verdict of suicide or death of undetermined intent that involved the antidepressants under investigation was provided by the ONS based on death registrations during 2000–6 in England and Wales. In England and Wales it has been customary to assume that the majority of injuries and poisonings of undetermined intent are cases in which the harm was self-inflicted but there was insufficient evidence to prove that the deceased deliberately intended to kill him- or herself. 32,109 In our investigation of coroners' practices (see Chapter 2) we found that 80% of possible suicide deaths given an open verdict were judged by the research team to be probable suicides. We have restricted our analyses to deaths involving single drugs, or single drugs and alcohol. Data were obtained for males and females separately. Mortality rates were calculated as the number of deaths per 100,000 population in England and Wales for those aged ≥ 10 years.
Self-poisoning
Self-poisoning data came from three centres currently involved in the Multicentre Study of Self-harm in England. 1 Data in the present study were for all patients who presented to emergency departments at general hospitals in Oxford (one hospital), Manchester (three hospitals) and Derby (two hospitals) during the study period with an overdose of antidepressants, including those involving other drugs (with or without alcohol).
Episodes of self-poisoning involving the antidepressants in those aged ≥ 10 years for the defined population areas of Oxford City, Manchester City and Derby Unitary Area were included in the study. Mid-year population estimates for these areas for the years 2000–6 were obtained from the ONS. 126 Rates of self-poisoning per 100,000 population were calculated for these areas combined.
Statistical analysis
Fatal toxicity index
Rate ratios for drug-specific poisoning mortality rate relative to prescribing rate were calculated from the mortality rate (numerator) and the prescription rate (denominator).
Case fatality index
Rate ratios for poisoning mortality relative to non-fatal self-poisoning for specific drugs were calculated from the mortality rate (numerator) and the self-poisoning rate (denominator). As noted in the Glossary, this represents a slight deviation from the usual approach, which would be to compare deaths against a combination of non-fatal and fatal poisonings for specific methods. We have used this alternative approach because national figures for non-fatal self-poisonings are not available.
Relative toxicity indices were calculated by standardising the rate ratios to amitriptyline. This drug is used as the reference preparation in many studies.
Rate ratios and 95% CIs, Spearman's rho and heterogeneity were calculated using Stata version 10.0.
Results
The numbers of deaths, prescriptions and episodes of self-poisoning are given for both sexes in Table 28, for males in Table 29 and for females in Table 30. The antidepressants most frequently involved in suicide deaths were (in descending order) dosulepin, amitriptyline, venlafaxine and citalopram. For non-fatal poisonings the most frequently involved antidepressants were (in descending order) fluoxetine, citalopram, amitriptyline, paroxetine, venlafaxine, dosulepin, sertraline and mirtazapine (see Table 28). These patterns were similar in both sexes (see Tables 29 and 30).
| Antidepressant | No. of deathsa | Death rate per 100,000 | No. of prescriptionsb | Prescription rate per 100,000 | No. of self-poisoningsc | Self-poisoning rate per 100,000 |
|---|---|---|---|---|---|---|
| TCAs | ||||||
| Amitriptyline | 395 | 0.1211 | 44,286,108 | 10,606 | 704 | 14.09 |
| Clomipramine | 39 | 0.0120 | 3,544,517 | 849 | 48 | 0.96 |
| Dosulepin | 589 | 0.1807 | 20,812,372 | 4984 | 388 | 7.77 |
| Doxepin | 22 | 0.0067 | 1,001,373 | 240 | 15 | 0.30 |
| Imipramine | 25 | 0.0077 | 2,575,206 | 617 | 30 | 0.60 |
| Nortriptyline | 5 | 0.0015 | 645,175 | 155 | 7 | 0.14 |
| Trimipramine | 13 | 0.0040 | 1,113,166 | 267 | 14 | 0.28 |
| All TCAs | 1088 | 0.3338 | 73,977,917 | 17,717 | 1206 | 24.14 |
| SNRI: venlafaxine | 83 | 0.0255 | 20,100,751 | 4814 | 508 | 10.17 |
| NaSSA: mirtazapine | 18 | 0.0055 | 6,386,479 | 1529 | 149 | 2.98 |
| SSRIs | ||||||
| Citalopram | 50 | 0.0154 | 37,371,364 | 8950 | 719 | 14.39 |
| Fluoxetine | 17 | 0.0052 | 39,818,056 | 9536 | 885 | 17.71 |
| Fluvoxamine | 0 | 0 | 195,897 | 47 | 13 | 0.26 |
| Paroxetine | 10 | 0.0031 | 25,980,311 | 6222 | 556 | 11.13 |
| Sertraline | 8 | 0.0025 | 15,374,325 | 3682 | 315 | 6.31 |
| All SSRIs | 85 | 0.0261 | 118,739,953 | 28,437 | 2488 | 49.80 |
| Antidepressant | No. of deathsa | Death rate per 100,000 | No. of prescriptionsb | Prescription rate per 100,000 | No. of self-poisoningsc | Self-poisoning rate per 100,000 |
|---|---|---|---|---|---|---|
| TCAs | ||||||
| Amitriptyline | 213 | 0.1343 | 13,502,515 | 6617 | 304 | 12.27 |
| Clomipramine | 13 | 0.0082 | 1,055,351 | 517 | 10 | 0.40 |
| Dosulepin | 313 | 0.1974 | 5,711,075 | 2799 | 165 | 6.66 |
| Doxepin | 13 | 0.0082 | 278,542 | 136 | 11 | 0.44 |
| Imipramine | 11 | 0.0069 | 832,451 | 408 | 9 | 0.36 |
| Nortriptyline | 0 | 0 | 164,783 | 81 | 3 | 0.12 |
| Trimipramine | 8 | 0.0050 | 293,191 | 144 | 2 | 0.08 |
| All TCAs | 571 | 0.3602 | 21,837,908 | 10,701 | 504 | 20.34 |
| SNRI: venlafaxine | 46 | 0.0290 | 6,792,071 | 3328 | 181 | 7.31 |
| NaSSA: mirtazapine | 8 | 0.0050 | 2,500,957 | 1226 | 52 | 2.10 |
| SSRIs | ||||||
| Citalopram | 29 | 0.0183 | 11,385,772 | 5579 | 258 | 10.41 |
| Fluoxetine | 5 | 0.0032 | 11,634,141 | 5701 | 299 | 12.07 |
| Fluvoxamine | 0 | 0 | 85,351 | 42 | 4 | 0.16 |
| Paroxetine | 7 | 0.0044 | 8,501,428 | 4166 | 222 | 8.96 |
| Sertraline | 4 | 0.0025 | 4,838,067 | 2371 | 106 | 4.28 |
| All SSRIs | 45 | 0.0284 | 36,444,759 | 17,859 | 889 | 35.89 |
| Antidepressant | No. of deathsa | Death rate per 100,000 | No. of prescriptionsb | Prescription rate per 100,000 | No. of self-poisoningsc | Self-poisoning rate per 100,000 |
|---|---|---|---|---|---|---|
| TCAs | ||||||
| Amitriptyline | 182 | 0.1087 | 30,783,593 | 14 419 | 398 | 15.80 |
| Clomipramine | 26 | 0.0155 | 2,489,079 | 1166 | 38 | 1.51 |
| Dosulepin | 276 | 0.1648 | 15,101,297 | 7074 | 223 | 8.85 |
| Doxepin | 9 | 0.0054 | 722,831 | 339 | 4 | 0.16 |
| Imipramine | 14 | 0.0084 | 1,742,755 | 816 | 21 | 0.83 |
| Nortriptyline | 5 | 0.0030 | 480,392 | 225 | 4 | 0.16 |
| Trimipramine | 5 | 0.0030 | 819,975 | 384 | 12 | 0.48 |
| All TCAs | 517 | 0.3088 | 52,139,922 | 24,423 | 700 | 27.79 |
| SNRI: venlafaxine | 37 | 0.0221 | 13,308,622 | 6234 | 327 | 12.98 |
| NaSSA: mirtazapine | 10 | 0.0060 | 3,885,522 | 1820 | 97 | 3.85 |
| SSRIs | ||||||
| Citalopram | 21 | 0.0125 | 25,985,426 | 12,172 | 461 | 18.30 |
| Fluoxetine | 12 | 0.0072 | 28,183,838 | 13,202 | 586 | 23.26 |
| Fluvoxamine | 0 | 0 | 110,546 | 52 | 9 | 0.36 |
| Paroxetine | 3 | 0.0018 | 17,478,883 | 8187 | 334 | 13.26 |
| Sertraline | 4 | 0.0024 | 10,536,046 | 4935 | 2098 | 8.30 |
| All SSRIs | 40 | 0.0289 | 82,294,739 | 38,548 | 1599 | 63.48 |
Fatal toxicity index (mortality to prescriptions rate ratios)
There was significant heterogeneity in fatal toxicity within the TCA group [χ2 = 365.02, degrees of freedom (df) = 6, p < 0.001]. The mortality to prescriptions rate ratio was considerably higher for dosulepin and doxepin than for amitriptyline (Table 31). This is reflected in the toxicity ratios relative to amitriptyline for these drugs (dosulepin 3.2, doxepin 2.5). The fatal toxicity ratios were generally far higher in males than in females but the relative toxicity indices were mostly similar in males and females.
The relative toxicity index for venlafaxine (0.46) was approximately half that for amitriptyline but over five times higher than that for the SSRIs (0.08). The relative toxicity index for mirtazapine (0.32) was slightly lower than that of venlafaxine.
There was significant heterogeneity in fatal toxicity within the SSRI group (χ2 = 28.76, df = 4, p < 0.001). The fatal toxicity index for citalopram was three times higher than that for the other SSRIs (1.7, 95% CI 1.3 to 2.3, vs. 0.6, 95% CI 0.4 to 0.8).
Case fatality index (mortality to self-poisonings rate ratios)
The findings based on mortality to self-poisonings rate ratios were essentially the same as for fatal toxicity, including relatively high case fatality of dosulepin and doxepin within the tricyclics, similar case fatality of venlafaxine and higher case fatality of citalopram than the other SSRIs (Table 32).
| Antidepressant | Both sexes | Males | Females | |||
|---|---|---|---|---|---|---|
| Rate ratio (95% CI) | Relative toxicity indexa | Rate ratio (95% CI) | Relative toxicity indexa | Rate ratio (95% CI) | Relative toxicity indexa | |
| TCAs | ||||||
| Amitriptyline | 11.4 (10.3 to 12.6) | 1.0 | 20.3 (17.7 to 23.2) | 1.0 | 7.5 (6.5 to 8.7) | 1.0 |
| Clomipramine | 14.1 (10.0 to 19.3) | 1.2 | 15.9 (8.4 to 27.1) | 0.8 | 13.3 (8.7 to 19.5) | 1.8 |
| Dosulepin | 36.3 (33.4 to 39.3) | 3.2 | 70.5 (62.9 to 78.8) | 3.5 | 23.3 (20.6 to 26.2) | 3.1 |
| Doxepin | 28.1 (17.6 to 42.6) | 2.5 | 60.1 (32.0 to 102.7) | 3.0 | 15.9 (7.3 to 20.1) | 2.1 |
| Imipramine | 12.4 (8.1 to 18.4) | 1.1 | 17.0 (8.5 to 30.4) | 0.8 | 10.2 (5.6 to 17.2) | 1.4 |
| Nortriptyline | 9.9 (3.2 to 23.2) | 0.9 | 0 | 0 | 13.3 (4.3 to 31.0) | 1.8 |
| Trimipramine | 15.0 (8.0 to 25.6) | 1.3 | 35.1 (15.2 to 69.2) | 1.7 | 7.8 (2.5 to 18.1) | 1.0 |
| All TCAs | 18.8 (17.7 to 20.0) | 1.7 | 33.7 (31.0 to 36.5) | 1.7 | 12.6 (11.6 to 13.8) | 1.7 |
| SNRI: venlafaxine | 5.3 (4.2 to 6.6) | 0.46 | 8.7 (6.4 to 11.6) | 0.43 | 3.5 (2.5 to 4.9) | 0.47 |
| NaSSA: mirtazapine | 3.6 (2.1 to 5.7) | 0.32 | 4.1 (1.8 to 8.1) | 0.20 | 3.3 (1.6 to 6.0) | 0.44 |
| SSRIs | ||||||
| Citalopram | 1.7 (1.3 to 2.3) | 0.15 | 3.3 (2.2 to 4.7) | 0.16 | 1.0 (0.6 to 1.6) | 0.14 |
| Fluoxetine | 0.5 (0.3 to 0.9) | 0.05 | 0.6 (0.2 to 1.3) | 0.03 | 0.5 (0.3 to 1.0) | 0.07 |
| Fluvoxamine | 0 | 0 | 0 | 0 | 0 | 0 |
| Paroxetine | 0.5 (0.2 to 0.9) | 0.04 | 1.1 (0.4 to 2.2) | 0.05 | 0.2 (0.05 to 0.6) | 0.03 |
| Sertraline | 0.7 (0.3 to 1.3) | 0.06 | 1.1 (0.3 to 2.7) | 0.05 | 0.5 (0.1 to 1.2) | 0.06 |
| All SSRIs | 0.9 (0.7 to 1.1) | 0.08 | 1.6 (1.2 to 2.1) | 0.08 | 0.6 (0.4 to 0.8) | 0.08 |
| Antidepressant | Both sexes | Males | Females | |||
|---|---|---|---|---|---|---|
| Rate ratio (95% CI) | Relative toxicity indexa | Rate ratio (95% CI) | Relative toxicity indexa | Rate ratio (95% CI) | Relative toxicity indexa | |
| TCAs | ||||||
| Amitriptyline | 8.6 (7.8 to 9.5) | 1.0 | 11.0 (9.5 to 12.5) | 1.0 | 6.9 (5.9 to 8.0) | 1.0 |
| Clomipramine | 12.5 (8.9 to 17.0) | 1.4 | 20.3 (10.8 to 34.7) | 1.9 | 10.3 (6.7 to 15.1) | 1.5 |
| Dosulepin | 23.3 (21.4 to 25.2) | 2.7 | 29.6 (26.4 to 33.1) | 2.7 | 18.6 (16.5 to 21.0) | 2.7 |
| Doxepin | 22.5 (14.1 to 34.0) | 2.6 | 18.5 (9.8 to 31.6) | 1.7 | 33.9 (15.5 to 64.3) | 4.9 |
| Imipramine | 12.8 (8.3 to 18.9) | 1.5 | 19.1 (9.5 to 34.2) | 1.7 | 10.0 (5.5 to 16.8) | 1.5 |
| Nortriptyline | 11.0 (3.6 to 25.5) | 1.3 | 0 | 0 | 18.8 (6.1 to 43.9) | 2.7 |
| Trimipramine | 14.2 (7.8 to 24.3) | 1.7 | 62.5 (27.0 to 123.1) | 5.7 | 6.3 (2.0 to 14.6) | 0.9 |
| All TCAs | 13.8 (13.0 to 14.7) | 1.6 | 17.7 (16.3 to 19.2) | 1.6 | 11.1 (10.2 to 12.1) | 1.6 |
| SNRI: venlafaxine | 2.5 (2.0 to 3.1) | 0.29 | 4.0 (2.9 to 5.3) | 0.36 | 1.7 (1.2 to 2.3) | 0.25 |
| NaSSA: mirtazapine | 1.9 (1.1 to 2.9) | 0.22 | 2.4 (1.0 to 4.7) | 0.20 | 1.6 (0.7 to 2.9) | 0.23 |
| SSRIs | ||||||
| Citalopram | 1.1 (0.8 to 1.4) | 0.12 | 1.8 (1.2 to 2.5) | 0.12 | 0.7 (0.4 to 1.1) | 0.10 |
| Fluoxetine | 0.3 (0.2 to 0.5) | 0.03 | 0.3 (0.1 to 0.6) | 0.02 | 0.3 (0.2 to 0.5) | 0.04 |
| Fluvoxamine | 0 | 0 | 0 | 0 | 0 | 0 |
| Paroxetine | 0.3 (0.1 to 0.5) | 0.03 | 0.5 (0.2 to 1.0) | 0.05 | 0.1 (0.03 to 0.4) | 0.02 |
| Sertraline | 0.4 (0.2 to 0.8) | 0.05 | 0.6 (0.2 to 1.5) | 0.05 | 0.3 (0.08 to 0.7) | 0.04 |
| All SSRIs | 0.5 (0.4 to 0.7) | 0.06 | 0.8 (0.6 to 1.1) | 0.07 | 0.4 (0.3 to 0.5) | 0.05 |
Comparison of fatal toxicity and case fatality
There was a very high correlation between the rankings of the results of the fatal toxicity and case fatality approaches to estimating relative toxicity of the specific antidepressants (Spearman's ρ = 0.99, p < 0.001).
Discussion
We used two methods for assessing relative toxicity of antidepressants: the fatal toxicity index and the case fatality index. The findings based on both approaches showed that dosulepin and doxepin are considerably more toxic than amitriptyline. Because of extensive prescribing of dosulepin relative to doxepin (see Table 28), attention regarding toxicity has mainly focused on the former drug. In December 2007, the MHRA issued advice regarding dosulepin and measures to reduce the risk of fatal overdose. 127 Since November 2007, pack sizes have been limited and packaging made safer. Our findings support these measures but also highlight the need to extend them to doxepin, although the latter drug is much less frequently prescribed.
Venlafaxine (a SNRI) is clearly far less toxic in overdose than the TCAs. Its relative toxicity index based on both assessment approaches was intermediate between those of the TCAs and the SSRIs. The MHRA issued a warning about the relatively high toxicity of venlafaxine in 2006, recognising that selective prescribing to patients at risk of suicide could be a contributory factor to this finding. 128 The regulatory body also issued prescribing advice, including restricting pack sizes and initial supplies for patients. In our study, the relative toxicity of mirtazapine (a NaSSA) was slightly lower than that of venlafaxine, but considerably greater than for the SSRIs.
Within the SSRIs, citalopram had a higher relative toxicity index, based both on the fatal toxicity measure and that using case fatality. This finding is in keeping with other reported concerns about the toxicity of citalopram129,130 and may reflect known cardiotoxic130 and proconvulsant121 effects of citalopram in overdose. Although the absolute fatal toxicity is low, this finding should nevertheless be considered when making risk/benefit decisions regarding prescribing for individual patients.
A major strength of the study is that we used two approaches to assessing relative toxicity, the findings of which were remarkably similar. Although the findings for fatal toxicity could have been influenced by selective prescribing (e.g. use of less toxic antidepressants for people more at risk of overdose), this is less likely to be the case for case fatality in that this assesses the risk of death once someone takes an overdose. One limitation is that in calculating case fatality we compared deaths with non-fatal poisonings, rather than deaths against a combination of non-fatal and fatal poisonings for specific methods. This is because national figures for non-fatal self-poisoning are not available. However, were these to be available, the addition of fatal cases to the very large number of non-fatal cases would have made little difference to the results.
Conclusions
Of the TCAs, dosulepin and doxepin have the greatest toxicity based on overdose deaths relative to both prescriptions and non-fatal self-poisonings. Venlafaxine appears to be far less toxic than the TCAs but more toxic than the SSRIs and slightly more toxic than mirtazapine. Of the five SSRIs that we examined, citalopram appears to be more toxic than the other four. These findings have been communicated to the MHRA. Our results suggest that when prescribing antidepressants the clinician should take account of the risk that may be associated with an overdose, especially in someone judged to be at risk of self-poisoning, as well as their relative efficacy, acceptability and possible interactions with other medication and alcohol, and patients' concurrent physical morbidity. We suggest that assessment of the relative toxicity of antidepressants should continue as new antidepressants are marketed, and that international comparisons are warranted in view of differences between countries in prescribing practices.
Chapter 6 Variations in self-harm service delivery: an observational study examining outcomes and temporal trends
Abstract
Historically, service provision for self-harm in the UK has been extremely variable. In this study, we aimed to describe the characteristics of individuals attending hospital with self-harm in 32 centres across England in 2010–11 and the management that they received. We also investigated how key aspects of management (assessement, admission, follow-up) related to repetition of self-harm and how management had changed since an earlier study in 2001. Data on service provision were collected through interviews with key staff. Data on individuals who had self-harmed were collected using a specifically designed proforma. Over 6400 individuals presented during the 3-month study period. There was a 3.5-fold difference between hospitals in the proportion of individuals who received a specialist assessment and a fivefold difference in the proportion of individuals receiving specialist follow-up. Overall, 4 out of 10 individuals left hospital without having had an assessment with a mental health specialist. In an ecological analysis there was little evidence that aspects of management were associated with outcome, but an individual-level analysis suggested that specialist psychosocial assessement might be associated with a reduced risk of repetition of self-harm. Comparing our data with data from the earlier time period, levels of specialist assessment had remained static, but scores on a self-reported service quality scale increased by 26%. Overall, there was little evidence that guidelines and policy initiatives to date have had a major impact on the variability of services, but they may have helped to improve markers of service quality.
Background
Every year in England there are around 4500 suicides and it is estimated that hospitals manage approximately 220,000 episodes of self-harm. Our previous studies have demonstrated wide variations in self-harm service delivery. In one study of a representative sample of 32 hospitals in England there was a twofold variation in the level of specialist assessment, a fourfold variation in the level of medical admission, a ninefold variation in the level of psychiatric admission and a twofold variation in arrangements for mental health follow-up. 15 However, it is unclear how such variations relate to the outcome of self-harm in trusts with different approaches to management. Such outcomes research is essential to guide service provision for self-harm,131 especially as randomised trials in this area tend to be underpowered, recruit highly selected samples and be hampered by the poor engagement of participants with treatment. 21
In 2004, two sets of clinical guidelines on the management of self-harm were published. 13,132 In addition, the Royal College of Psychiatrists initiated the Better Services for People who Self-harm project,133 an audit-based quality improvement project involving surveys of service users' experiences, staff attitudes and training, and care pathways. The two sets of guidelines and the Better Services project might be expected to reduce the variability of services and improve the quality of care for self-harm patients.
In the current study we aimed to investigate whether or not aspects of the hospital management of self-harm in 32 hospitals had any impact on patient outcomes, specifically self-harm repetition. Comparison with the results of our previous study carried out in 2001 in the same sites15 also enabled us to explore whether service variability had decreased and service quality had improved in response to guidelines and policy initiatives introduced in the intervening period.
Our main objectives were to:
-
describe patient characteristics and hospital management of self-harm across the 32 sites
-
investigate how key aspects of mangement (e.g. levels of assessment, admission and specialist follow-up) related to the repetition of self-harm
-
compare our findings with those from the earlier 2001 study to ascertain whether the variability in services had decreased and the quality of services had improved.
Methods
Study sites
We intended to carry out the study in the stratified random sample of 32 hospitals in England identified in our earlier investigation. 15 Only hospitals with an emergency department were included in the original sampling process. The sample was stratified so that four hospitals were selected within each of the eight former health regions in England and to ensure that small and large hospitals were included, as well as those with high and low self-harm readmission rates. In total, 31 of the original 32 hospitals agreed to take part in the current study. The one hospital that declined to participate was replaced by an alternative, randomly selected hospital from within the appropriate stratum.
Local approvals
Approval to carry out the study was sought through the research and development departments at each NHS trust through completion of a Site Specific Investigation Form [via the Integrated Research Approval System (IRAS)]. As part of this process we approached potential local collaborators at each trust, commonly through the assistance of appropriate local and national networks [e.g. the Mental Health Research Network (MHRN) and Comprehensive Local Research Network].
Service interviews
Once approval had been obtained, the local collaborators identified the key mental health and emergency deparatment staff involved in the provision of self-harm services. These personnel were interviewed by telephone or in person about current service structures (see Appendix 5). Using the staff reponses, hospitals were then rated on a measure of service quality developed as part of the previous study15 and based on the Royal College of Psychiatrists guidelines for the general hospital management of self-harm132 (Box 1). Each item was scored as ‘1’ or ‘0’ depending on the presence or absence of a particular aspect of the service. For two items (6 and 10), for which such a strict categorisation was not possible, scores of ‘0’, ‘0.5’ or ‘1’ were given in consultation with the research team.
Ethical approval
This study received ethical approval from Tameside and Glossop NHS Research Ethics Committee in August 2009.
-
Is there a protocol/guideline/aide memoire for staff in the A&E department for the immediate medical management of self-harm?
-
Is there a protocol/guideline/aide memoire for staff in the A&E department for the immediate assessment of risk and severe mental disorder in self-harm patients?
-
Is there a designated self-harm specialist clinical service? (include A&E liaison)
-
Is there a local specific planning/working group (of the team who undertake the psychosocial assessments) that meets at least once a year to plan/oversee the service for self-harm patients?
-
Are there psychosocial assessment training sessions for new staff who are involved in the psychosocial assessment of patients?
-
Are there supervision arrangements in place for staff members (new and existing) who undertake psychosocial assessments?
-
Are there written guidelines/a checklist to assist psychiatric clinicians in the psychosocial assessment of self-harm patients?
-
Does the A&E department have 24-hour access to a psychiatrist, psychiatric nurse or social worker who is able to undertake psychosocial assessments?
-
If yes to 8, is immediate (within 15 minutes) advice available over the telephone?
-
If yes to 8, is emergency attendance, when requested, available within 1 hour?
-
Do regular (at least once a year) service planning/strategy meetings take place between the self-harm team/psychiatric service and the general medical service involved in the care of self-harm patients?
-
Are rooms that allow for privacy and confidentiality available for conducting interviews with self-harm patients either in or close to the A&E department?
-
Are rooms that allow for privacy and confidentiality available for conducting interviews with self-harm patients either in or close to the inpatient unit where most of the patients are assessed?
-
Does a formal arrangement exist with social services to visit and offer advice to self-harm patients who have significant social difficulties?
-
Can those admitted as inpatients remain in hospital until they have received a psychosocial assessment?
-
Is there a policy stating that a patient's GP should be contacted within 24 hours of patient discharge from an A&E department?
-
Is there a policy stating that a patient's GP should be contacted within 24 hours of patient discharge from a medical inpatient unit?
-
Are self-harm patients routinely given printed material about local services, voluntary groups and how to obtain access to them?
-
Are there any formal links with non-statutory services (e.g. self-help groups, the Samaritans)?
-
Has a system been set up for the monitoring of hospital attendance/discharge and referral of self-harm patients?
-
Has there been any audit of the service for self-harm patients in the last 2 years?
Potential total scores ranged from 0 to 21, with higher scores indicating better-quality services. Information on the hospital catchment area (estimated size; urban, rural or mixed urban/rural) was collected during interviews with staff or from hospital records.
Service audits
With the assistance of our local collaborators and with subsequent approval of the Information Governance departments allowing data sharing between relevant trusts, we facilitated the set-up of audits of self-harm in each hospital through NHS trust personnel or their equivalent (e.g. clinical studies officers who were employed by the trusts in some centres). For each audit, data were collected on all episodes of self-harm in those aged ≥ 18 years occuring during a 3-month period. Service configurations for young people were likely to be markedly different from adult services and therefore those aged < 18 years were excluded from this study. The exact time period varied between centres but all audits took place between May 2010 and June 2011.
Case definition
As in the previous study, self-harm was defined as ‘a deliberate non-fatal act whether physical, drug over-dosage or poisoning, done in the knowledge that it was potentially harmful and in the case of drug overdose that the amount taken was excessive’ (p. 68). 134 The final decisions on inclusion were made by the clinical staff/data collectors. Definitions were discussed in detail in the pilot phase of each audit and the data collectors were encouraged to contact the research team with any queries.
Case ascertainment
Episodes of self-harm were identified from emergency department records using relevant search terms from our previous study15 and from current self-harm monitoring systems in England. 1,135 The individual medical records of possible cases were examined to confirm case inclusion. The robustness of this methodology was tested in each hospital in a pilot data collection exercise against all presentations for a brief period (1–2 weeks) and/or against lists of presentations compiled by mental health teams, to identify missed cases. Search terms were adjusted accordingly to maximise case ascertainment.
Baseline data collection
Data were recorded on openCDMS (Clinical Decision Management System) (http://opencdms.org/), which is a web-based data entry system supported by the MHRN. Technical support and user training were provided by specialist e-Science Officers working for the MHRN Information Services team. Individual-level data were collected using a simple one-page (electronic) audit form completed by designated staff. The audit form (see Appendix 6) contained items relating to basic demographic and clinical data, details of the drugs taken in overdose and the patient's recent contact with specialist mental health services. Details of in-hospital management were also recorded, specifically whether the individual received a psychosocial assessment [defined as ‘an interview carried out by a member of mental health staff who has been trained in the process, is usually of about 30 minutes duration, and covers the assessment of factors such as the causes and degree of suicidal intent, current mental state and level of social support, psychiatric history, personal and social problems, future risk and need for follow-up' (p. 68)],134 whether he or she was admitted to a psychiatric or medical bed and whether he or she was referred for psychiatric follow-up. Data were collected from both emergency department and mental health medical records systems.
Follow-up data
The index episode for each individual was his or her first self-harm attendance during the 3-month study period. The main outcome was hospital attendance with a repeat episode within 6 months. However, because we collected follow-up data for 6 months after the end of the 3-month audit, follow-up data for individuals were available for between 6 and 9 months. Repeat episodes were identified through hospital databases by matching on name, date of birth and NHS number if available. Data collectors kept a record of individuals' identifying details against their unique openCDMS number, but patient identifiers were not used on the audit forms either in hard copy or in electronic form. All data were anonymised at source (at the participating hospital) before being sent to the research team. A named person within the trust held the key to enable subsequent patient attendances/episodes to be identified.
Sample size
Hospital-level data
To measure the effect of hospital management on the proportion of patients repeating within 6 months, we considered a sample size of 32 hospitals would enable us to detect correlations of 0.31 between continuous predictor variables and self-harm repetition (using Spearman's rank correlation coefficients and two-sided significance levels of 5%). This would enable factors accounting for ≥ 9% of the variability in level of repetition between hospitals to be identified.
Individual-level data
We estimated that approximately 4000 individuals would attend the study centres with a self-harm episode during the 3 months of the audit period. Considering the least common key service factor (admission to a psychiatric bed – occurring in 10% of index episodes), this sample size would give us > 90% power to detect a clinically significant 5% difference in levels of 6-month repetition between those who were admitted and those who were not admitted (7% vs. 12%).
Analysis
Analysis relating aspects of management to repetition was carried out at aggregate hospital level and at individual level. The hospital-based analysis examined associations between hospital level of 6-month repetition and rates of key management/service provision, specifically the proportions of individuals receiving a psychosocial assessment, admitted to a medical bed, admitted to a psychiatric bed and referred for specialist mental health follow-up, and the hospital's total service scale score. Spearman's rank correlation coefficient was used to measure associations between levels of hospital key clinical management and total service score and repetition, and Mann–Whitney tests were used for comparisons of levels of repetition for hospitals with/without individual items from the service scale.
We used meta-regression to further evaluate the relationship between levels of key clinical management and hospital levels of repetition. This method allowed us to take into account the sample size of each hospital and to estimate the combined (pooled) effect of levels of management on the level of repetition. Through these models we obtained an odds ratio (OR) representing the effect of changes in levels of management on the odds of repetition.
In an individual-based analysis we examined the relationship between levels of key hospital management and repetition of self-harm (within 6–9 months) using survival analyses (Cox proportional hazards regression). We adjusted as far as possible for differences in the case mix of patients receiving different types of management. We also adjusted the standard error measurement to account for clustering by hospital.
We measured changes in management and service provision between the present study and the 2001–2 period using episodes of self-harm rather than individuals' index presentation, because data on individuals were not available for the earlier study. Differences in median scores between the two time periods were tested using the matched-pairs sign test.
Analyses were conducted using Stata version 11.0 and SPSS version 19.
Results
Characteristics of the sample
This section is based on each individual's first (index) episode during the 3-month audit period. A total of 6442 individuals presented with 7689 episodes of self-harm at the 32 hospitals during the 3-month audit period. Overall, 56% (n = 3583) of individuals were female and 51% (n = 3274) were aged < 35 years [age range 18–94 years, median age 34 years, interquartile range (IQR) 24–45 years]. Information on ethnicity was not widely available for seven of the hospitals. Data were 85% complete in the remaining hospitals (n = 4333): 93% (n = 4017) of the individuals were white, 3% (n = 124) were South Asian, 2% (n = 78) were black and 3% (n = 114) were from other ethnic groups.
The main method of self-harm was known in 99.7% (n = 6424) of index episodes: self-poisoning with drugs in 79% (n = 5073), self-poisoning (other) in 2% (n = 102), self-cutting in 14% (n = 890) and other methods of harm (including burning, attempted hanging and jumping) in 6% (n = 359). Use of alcohol/drugs with the act was known for 90% (n = 5828) of individuals. Alcohol was taken within 6 hours of the self-harm act in 53% (n = 3111) of cases and recreational drugs in 7% (n = 385). Data were available for previous self-harm episodes in 97% (n = 6237) of individuals and reported as present in 51% (n = 3173) of these. Data were available on whether or not patients were receiving psychiatric treatment at the time of their index self-harm episode for 96% (n = 6181) of individuals, and 32% (n = 1982) of these were known to be in current psychiatric treatment. Data on psychiatric inpatient care were 97% (n = 6269) complete, and 10% (n = 636) of individuals had been an inpatient in a psychiatric ward in the 12 months before the self-harm presentation.
FIGURE 12.
Time of presentation: all episodes during the 3-month audit (n = 7622).
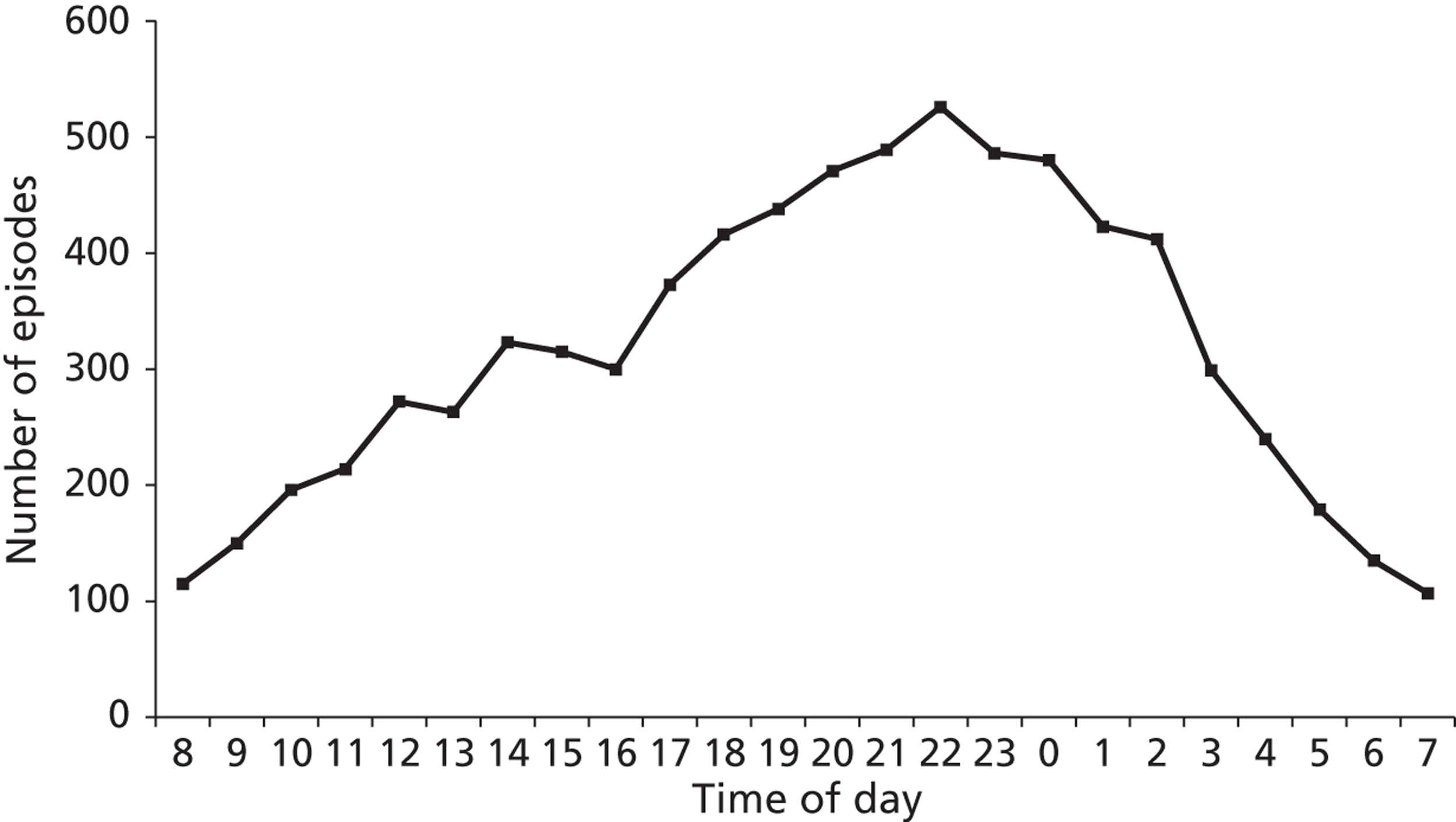
Time of presentation was known in 99% of episodes (n = 7622). There was a steady increase in presentations during the day with a peak time of presentation between 2200 and 2300 (Figure 12). The majority (57%, n = 4362) of presentations occurred out of hours (we considered ‘out of hours’ to be 2000 to 0800 and daytime/evening to be 0800 to 2000, based on information of routine service availability from hospital interviews).
Management in hospital
A psychosocial assessment by a mental health specialist took place in 58% of index episodes (Table 33). A total of 66% (n = 2651) of these were carried out by a mental health nurse (including mental health liaison nurses and those from specialist self-harm teams and crisis teams), 20% (n = 683) by a psychiatrist (any grade) and 4% (n = 142) by another mental health professional (such as a social worker). Out-of-hours presentations were slightly less likely to receive psychosocial assessment than presentations during working hours (56% vs. 60%, p = 0.001). Daytime and evening presentations were more likely to be assessed by a psychiatrist than out-of-hours presentations (22% vs. 18%, p = 0.012).
| Servicea | Overall proportion of cases receiving the service, % (n/Nb) | Range (IQR) (%) |
|---|---|---|
| Specialist mental health assessment | 58 (3574/6154) | 28–91 (46–70) |
| Admission to general medical bed | 56 (3587/6422) | 22–85 (42–67) |
| Psychiatric admission | 7 (433/6036) | 0–20 (4–11) |
| Specialist mental health follow-up | 30 (1828/6036) | 11–61 (21–39) |
| Referral to non-statutory services | 18 (1018/5624) | 3–69 (9–26) |
A total of 2155 out of 2660 individuals (81%) were assessed within 24 hours of their presentation. The median number of hours between time of hospital presentation and time of assessment was 10 hours (IQR 4–20 hours). For those not admitted to a medical bed, the median time to assessment was 5 hours (IQR 3–8 hours) and this did not vary by time of presentation (working hours vs. out of hours). A total of 42% (335/798) of assessments occurred within 4 hours of presentation in this group. Amongst all assessed individuals, those using alcohol at the time of self-harm had a median of 11 hours (IQR 6–20 hours) wait to be assessed compared with 9 hours (IQR 5–20 hours) when alcohol was not used. Over half of the index episodes resulted in admission to a medical bed. Amongst these, 63% (n = 2245) were admitted to an emergency department observation/assessment ward or equivalent, 32% (n = 1145) to a general ward and 5% (n = 194) to other types of medical beds including intensive care units. A total of 7% of presentations resulted in admission to a psychiatric bed and in 30% (n = 1828) of presentations patients were referred to specialist mental health outpatient services (including psychiatric care, crisis teams, community mental health teams and statutory drug and alcohol services). In 18% of episodes patients were referred to other, non-statutory services, most commonly drug/alcohol services (25%, n = 255), counselling/psychotherapy (16%, n = 167), social services (13%, n = 128) and prison/police custody (12%, n = 123).
In total, 20% (n = 1313) of individuals reattended with a repeat episode of self-harm within 6 months of the index episode. This ranged from 6–27% (IQR 18–24%) in the 32 hospitals.
Aggregate-level outcome analysis
This section presents results at the hospital level. Analyses relating to the 21-item service scale and admission to general hospital were conducted using data from 32 hospitals. Those relating to specialist mental health management were carried out on data from the 31 hospitals in which mental health records were accessed.
The Spearman's rank correlation coefficient between the proportion of individuals receiving psychosocial assessment and the rate of 6-month repetition was 0.16 (p = 0.38) (Figure 13). There was no apparent association between 6-month repetition and the rate of hospital medical admission (Spearman's ρ = 0.15, p = 0.413), psychiatric admission (Spearman's ρ = 0.077, p = 0.679) or specialist outpatient referral (Spearman's ρ = 0.20, p = 0.28). The rate of repetition did not vary according to total service scale score (Spearman's ρ = − 0.065, p = 0.73) (Figure 14) or individual aspects of the scale.
FIGURE 13.
Association between level of psychosocial assessment and level of repetition within 6 months.
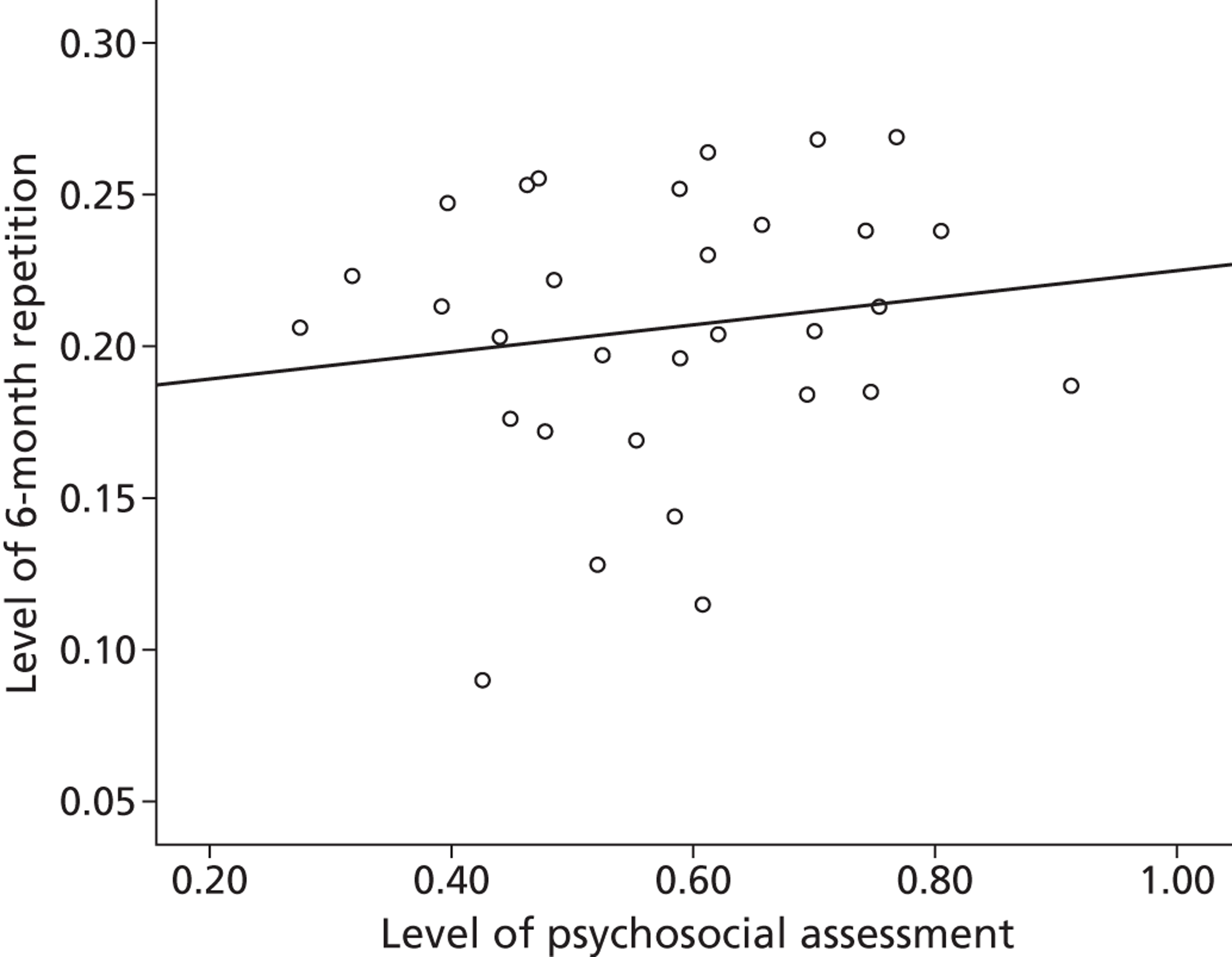
FIGURE 14.
Association between service scale score and level of repetition within 6 months.
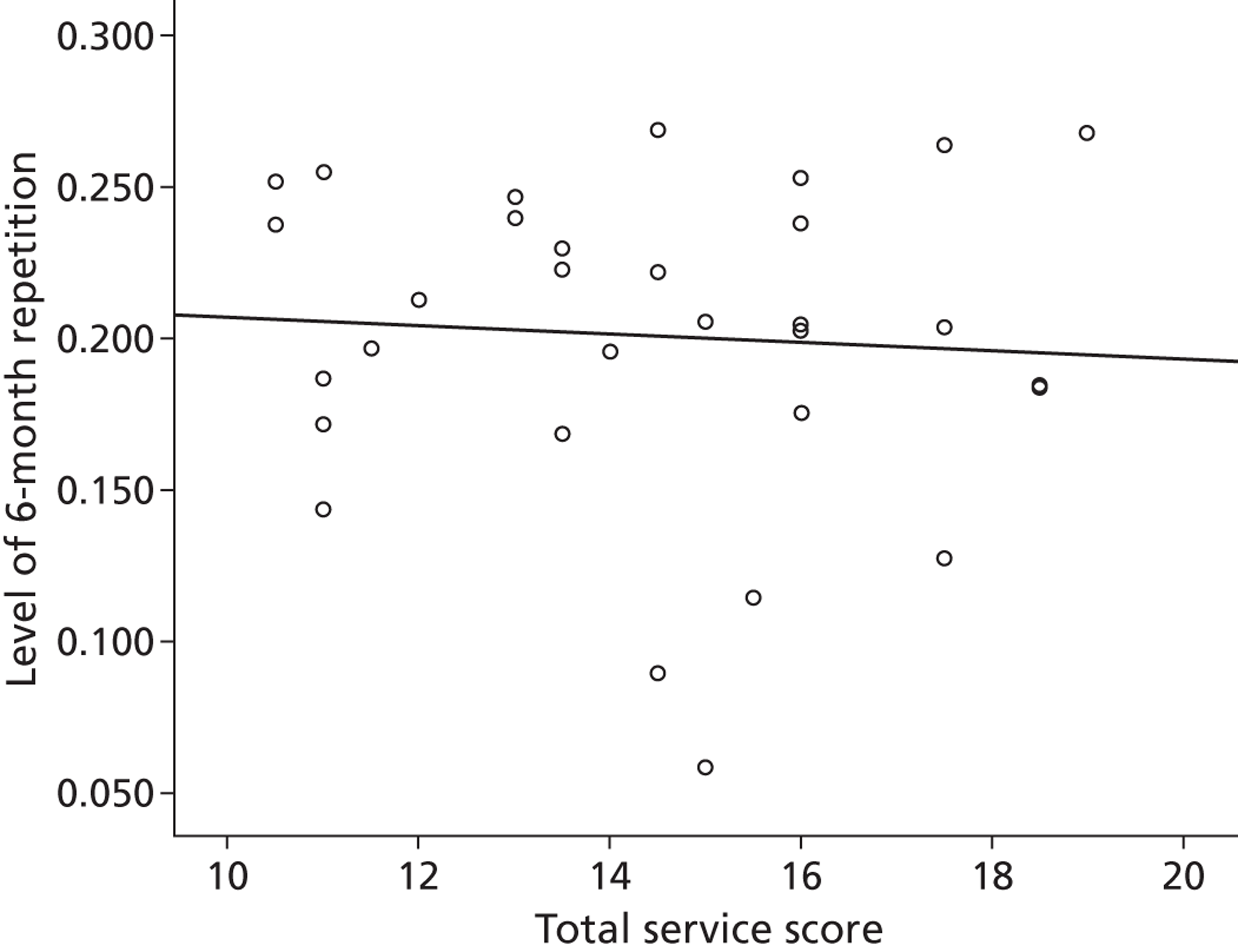
Meta-regression
There were no significant associations between levels of key management by hospitals and the odds of repetition within 6 months (Table 34). The pooled OR for the effect of a 10% increase in the proportion of patients who received a psychosocial assessment on the odds of repetition was 1.04 (95% CI 0.97 to 1.13, p = 0.27).
| Patient management | OR (95% CI) | p-value |
|---|---|---|
| Hospital management | ||
| Specialist mental health assessmenta | 1.04 (0.97 to 1.13) | 0.27 |
| Admission to general medical beda | 1.02 (0.95 to 1.10) | 0.55 |
| Psychiatric admissionb | 1.00 (0.98 to 1.02) | 0.98 |
| Specialist mental health follow-upa | 1.06 (0.98 to 1.15) | 0.16 |
| Service provision | ||
| Total service scale scorec | 0.99 (0.95 to 1.04) | 0.78 |
| Presence of a designated self-harm service | 0.87 (0.59 to 1.30) | 0.49 |
Individual-level outcome analysis
After adjusting for baseline characteristics, we found that psychosocial assessment was associated with a decreased risk of repeat self-harm, although this was non-significant at the p = 0.05 level (Table 35). In a post hoc analysis we compared the association between repetition and main speciality of assessor. The adjusted hazard ratio (HR) for repeat self-harm in individuals assessed by a psychiatrist (n = 629; based on complete data) compared with those not assessed was 0.78 (95% CI 0.64 to 0.94, p = 0.01). Psychosocial assessment by a mental health nurse (n = 2620; based on complete data) was not associated with a significantly decreased risk of repetition (HR 0.89, 95% CI 0.77 to 1.04, p = 0.13).
Specialist mental health follow-up was associated with a significantly increased HR, reflecting the increased risk of this group. Adjusting for characteristics associated with risk reduced the HR somewhat. There was a similar process for psychiatric inpatient admission.
| Management | Unadjusted HR (95% CI, p-value) | Adjusted HR (95% CI, p-value) |
|---|---|---|
| Specialist mental health assessment | 1.13 (0.97 to 1.32, 0.11) | 0.88 (0.76 to 1.01, 0.08) |
| Admission to general medical bed | 0.96 (0.84 to 1.09, 0.50) | 0.99 (0.88 to 1.11, 0.86) |
| Psychiatric admission | 1.54 (1.36 to 1.75, < 0.001a) | 0.91 (0.77 to 1.07, 0.25) |
| Specialist mental health follow-up | 1.47 (1.27 to 1.70, < 0.001a) | 1.01 (0.87 to 1.18, 0.85) |
Comparison between 2001–2 and 2010–11 data
Our earlier study15 in 2001–2 was based on episodes of self-harm, not individuals; therefore, all comparisons here are episode based. Comparisons are based on the 31 hospitals that were included in both studies.
Management
We compared the proportions of episodes receiving key aspects of clinical management in the two time periods (Table 36). The proportion of episodes in which psychosocial assessment occurred was similar between the two study periods (overall 57% in both 2001–2 and in 2010–11). Assessment rates in the present study did not correlate strongly with those in 2001–2 (Spearman's ρ = 0.23, p = 0.22). A higher proportion of episodes in the present study than in the 2001–2 study resulted in admission to a medical ward (55% vs. 44%, an increase of 12%), increasing in 21 out of 31 hospitals. The proportion receiving specialist mental health follow-up, including inpatient admission, was 39% in the present study compared with 54% in 2001–2, a decrease of 15%, and the variability between hospitals appeared to be greater (IQR 26–48% vs. 46–63%).
| Aspect of service | 2001–2 | 2010–11 | p-value |
|---|---|---|---|
| Total episodes | 4150 | 7599 | |
| Specialist mental health assessmenta | |||
| Overall (median), % | 57 (55) | 57 (58) | 0.43 |
| Range (IQR), % | 36–82 (44–71) | 24–88 (45–70) | |
| Admission to medical ward | |||
| Overall (median), % | 44 (39) | 55 (54) | < 0.001 |
| Range (IQR), % | 20–83 (29–58) | 22–85 (41–63) | |
| Specialist mental health follow-up (including admission)a | |||
| Overall (median), % | 54 (51) | 39 (38) | < 0.001 |
| Range (IQR), % | 35–82 (46–63) | 17–67 (26–48) | |
| Psychiatric admissiona | |||
| Overall (median), % | 10 (9) | 8 (7) | < 0.001 |
| Range (IQR), % | 3–24 (7–15) | 0–21 (4–12) | |
| Total service scale score | |||
| Overall score (all hospitals combined) (%) | 375.5/651 (58) | 442/651 (68) | < 0.001 |
| Mean score (median) | 12.0 (11.5) | 14.0 (14.5) | |
| Range (IQR) | 7–20 (10–14) | 10.5–19 (11.5–16) | |
Service provision
The total score from the service scale measure had increased from the earlier study in 23 out of 31 hospitals (Table 37), possibly indicating improved service quality. The median score increased from 11.5 (IQR 10–14) in the earlier study to 14.5 (IQR 11.5–16) in the present study, an increase of 26%. The difference between scores in the two time periods was statistically significant (p = 0.006).
Three individual service scale items improved in half or more of all centres – these were items 6 (availability of supervision to staff undertaking assessments), 11 (joint service planning meetings between mental health and acute services) and 14 (formal arrangements for social services input).
| Hospital | Total score (2001–2) | Total score (2010–11) | Change |
|---|---|---|---|
| 1 | 11 | 17.5 | 6.5 |
| 2 | 11.5 | 13.5 | 2 |
| 3 | 11 | 13.5 | 2.5 |
| 4 | 15 | 10.5 | − 4.5 |
| 5 | 10 | 13.5 | 3.5 |
| 6 | 11 | 11 | 0 |
| 7 | 16 | 11 | − 5 |
| 8 | 14.5 | 15 | 0.5 |
| 9 | 13.5 | 11 | − 2.5 |
| 10 | 14 | 14.5 | 0.5 |
| 11 | 8.5 | 12 | 3.5 |
| 12 | 14 | 11.5 | − 2.5 |
| 13 | 10 | 17.5 | 7.5 |
| 14 | 7.5 | 16 | 8.5 |
| 15 | 15.5 | 18.5 | 3 |
| 16 | 12 | 17.5 | 5.5 |
| 17 | 11.5 | 15 | 3.5 |
| 19 | 8.5 | 11.5 | 3 |
| 20 | 8 | 13 | 5 |
| 21 | 17.5 | 18.5 | 1 |
| 22 | 13.5 | 15.5 | 2 |
| 23 | 8 | 14 | 6 |
| 24 | 7 | 11 | 4 |
| 25 | 10.5 | 16 | 5.5 |
| 26 | 11 | 16 | 5 |
| 27 | 15.5 | 19 | 3.5 |
| 28 | 20 | 13 | − 7 |
| 29 | 9.5 | 16 | 6.5 |
| 30 | 16 | 14.5 | − 1.5 |
| 31 | 10 | 14.5 | 4.5 |
| 32 | 14 | 10.5 | − 3.5 |
| Total | 375.5 | 442 | 66.5 |
Number of episodes
Although it was not possible to identify the number of individuals presenting – and therefore calculate rates of self-harm – in the earlier study period, we were able to compare numbers of episodes (Table 38). We compared the number of self-harm attendances (expressed as the number of attendances per 4-week period) in 2001–2 and 2010–11. Overall, there was a 24% increase in the total number of episodes and a 12% increase in the median number of episodes. In total, 25 out of 31 hospitals had a higher number of episodes in 2010–11 than in 2001–2.
| Episodes | 2001–2 | 2010–11 |
|---|---|---|
| Total no. of episodes, all hospitals | 2075 | 2563 |
| Median no. of episodes | 67 | 75 |
| Range (IQR) | 32–134 (42–80) | 30–173 (54–104) |
There had been various changes relating to individual hospitals since the 2001–2 study period including hospital trust mergers. We anticipated that the self-reported number of beds in each hospital would give an approximate indication of capacity and catchment population. The number of beds increased by 21% overall, and 22 hospitals had a greater number of beds in 2010–11 than in 2001–2. In total, 18 of the 25 hospitals with an increased number of episodes also had an increased number of beds.
Discussion
Main findings in relation to objectives
We collected data on over 6400 individuals who had presented with self-harm to 32 sites across England in a 3-month period. The characteristics of our sample were broadly consistent with those in other hospital-based studies in the UK,1 with the majority of episodes related to self-poisoning, and self-harm being more common in younger age groups and women. Alcohol was involved in over half of the episodes, and over half of the individuals had a previous history of self-harm. There was marked variability in service provision with a 3.5-fold difference between hospitals in the proportion of individuals who received a specialist assessment, a fourfold difference in medical admission and a fivefold difference in the proportion of individuals receiving specialist follow-up. Overall, 4 out of 10 individuals left hospital without having had an assessment with a mental health specialist.
We found little evidence that aspects of care were related to outcome in terms of repetition of self-harm in our aggregate analysis. Findings based on area-level analyses should not be used to necessarily infer individual-level associations (the ecological fallacy); however, aggregate-level associations are really the only means of evaluating services as a whole. It could be that higher levels of assessment and admission are partly markers of good-quality care. This may have the effect of increasing engagement and making individuals more likely to present to hospital when they self-harm. There was limited evidence from the individual-level analyses that psychosocial assessment might be associated with a 12% reduced risk of repetition but, again, these findings are based on observational data and should be interpreted cautiously. We attempted to adjust for individual characteristics at baseline but our findings could simply reflect unmeasured confounding factors. The possible protective effect of assessment is, however, consistent with results from previous studies. 136 In a post hoc analysis there was an interesting possible difference in the effect of assessment according to the main speciality of the assessor. However, these results should be interpreted cautiously as psychiatrists and nursing staff are likely to have assessed distinct groups of patients.
Considering changes over time, we found that the overall number of episodes of self-harm in the study centres increased by around one-quarter. However, our data suggested that this might partly reflect service consolidation rather than a true increase in incidence. Disappointingly, given clinical guidelines and policy emphasis, variations in service provision were as wide as 10 years previously. The proportion of individuals receiving assessment from specialist services had remained static and the level of specialist follow-up had decreased, perhaps because of a greater involvement of voluntary organisations in services (nearly one-fifth of individuals received follow-up from non-statutory services in this study, but these data were not available for the earlier time period). The increased proportion of episodes resulting in admission may well have reflected the greater use of emergency department observation and assessment wards rather than an increase in acute admissions to general medical beds. This may partly have been driven by the policy emphasis on reduced waiting times in emergency departments. 137 A measure of service quality developed as part of the previous study did show an improvement in 23 of the 31 hospitals, with a 26% improvement in the median service quality score. The individual service items that showed an improvement in the greatest number of hospitals related to the availability of supervision, social services input and joint service planning meetings between mental health and acute care services as recommended by NICE guidelines. 13
Permissions and data sharing
One major unanticipated challenge that we encountered was securing local research governance permissions. As this study involved acute and mental health services, this meant making a total of 62 separate applications for local approval (not 64 trusts as some participating mental health trusts provided services over multiple sites). Processes and the time to approval varied between organisations. Even when local approvals had been given, additional permissions were required in some instances (e.g. from IT departments). Because of the nature of the study, acute and mental health services needed to share data. Despite both services providing care to the same group of patients – those who had harmed themselves – data-sharing agreements, when required, were sometimes difficult (and in one case impossible) to achieve within the study period. Identifying local staff who could collect data was also a major challenge but was helped considerably by clinical studies officers (from local and topic-specific research networks).
Strengths and limitations
This was a large study of hospital attendances following self-harm using recent data at individual level and episode level from multiple sites randomly selected from across England. Different electronic systems in the study hospitals required individual methodologies to identify and capture data. However, the robustness of the data was affirmed at each study site by the individual data collectors, and pilot data collection was carried out in each centre.
Nevertheless, our findings should be interpreted in the context of a number of methodological limitations. We collected data on self-harm attendances to hospital only and did not record outcomes or repeat episodes that did not come to the medical attention of the participating hospitals. As a country-wide audit, the data sources were based on clinical records rather than in-depth interviews. If there was no information in the notes of an item of interest then this was coded as absent. As a consequence, some of our findings may underestimate the true prevalence of particular characteristics or associated factors.
Another potential weakness was that we did not collect data on aspects of care offered after discharge from hospital, such as a patient receiving an assessment by the mental health team in the community. In addition, the mental health follow-up variable described referral for such follow-up, but we were unable to determine whether or not patients actually attended.
Although data completeness was high overall and we were able to include 31 of the original 32 sites, there were some difficulties relating to individual hospitals. For example, in one acute trust, patients received mental health care from a variety of mental health providers, so mental health data were unavailable for a small proportion of presentations. Within another site, data-sharing agreements between acute and mental health trusts could not be achieved, which again resulted in missing mental health data.
Implications for future research
One of the main difficulties that we encountered in this study was securing local permissions. Future multicentre work that is national in scope would benefit from a simplified system of centralised approval. Our understanding is that the NHS Health Research Authority (www.hra.nhs.uk/) is currently considering how this might be achieved. Our study demonstrates the invaluable contribution that clinical studies officers can make to the conduct of research when appropriate access permissions have been granted. Future work on this scale would not be possible without such posts.
Research in this area should continue to monitor the variability of self-harm services. In this study we found a discrepancy between process measures (e.g. proportion of people receiving psychosocial assessments), which did not improve, and quality scores, which did. An area of future research might be to determine what aspects of quality are important determinants of outcome and how they should be measured. The impact of management on outcomes is an important but methodologically challenging area. We need to understand which aspects of treatment are beneficial in routine practice and why. We also need to understand in which groups of individuals treatments might have the most impact. The role of psychosocial assessment warrants particular attention. 136 Randomised trials of national service-level interventions are not always possible or practical, and alternative observational designs (e.g. pre–post studies138) may be worthwhile.
Conclusion
Our study suggests that national guidelines and policy initiatives have had little impact on the variability of self-harm service provision. Around 60% of individuals can expect a psychosocial assessment when they attend hospital following an episode of self-harm, and this proportion has remained static over the last decade or so. There is some evidence to suggest that the overall quality score of self-harm services has improved, although this is inconsistent with process measures, and the effect of the quality score on outcomes is unclear. It is possible that the quality scores did not capture true markers of high-quality care or had an inherent response bias as they were based on self-report by providers. New NICE guidelines on the longer-term management of self-harm were published in November 2011139 and included an additional focus on implementation. The guidelines will also inform quality standards for self-harm (www.nice.org.uk/aboutnice/qualitystandards/qualitystandards.jsp), which will be markers of high-quality care and may contribute to the commissioning and monitoring of self-harm services. The question of whether or not new guidance and future policies have a positive effect on the quality of services and patient outcomes will need careful evaluation.
Chapter 7 A pilot randomised controlled trial of an information and contact-based intervention to reduce repeat self-harm
Abstract
Brief interventions of telephone or postal contact following self-harm have shown some promise in reducing the incidence of repeat self-harm, but research findings have been equivocal and mechanisms of action uncertain. In this study we aimed to develop a contact-based intervention and test its feasibility in a randomised controlled trial. We used qualitative methods to develop an intervention that consisted of an information leaflet listing local sources of help, two telephone calls soon after presentation to an emergency department and a series of letters expressing concern sent over a 12-month period. We carried out a pilot randomised controlled trial of the intervention compared with usual treatment in two hospitals in Manchester, using a parallel-group design. Potential participants included patients aged > 18 years and living in Manchester attending the study hospitals following self-harm. Overall, 30% of eligible individuals could not be contacted and a further 28% did not consent to take part; 66 patients were eventually randomised (with 33 patients in each group). The 12-month repeat rate for individuals in the intervention group was 34% (95% CI 20% to 52%) and the rate for the usual treatment group was 12.5% (95% CI 4% to 29%). The total number of repeat episodes of self-harm was higher in the intervention group than in the usual treatment group (41 vs. 7). This pilot trial proved challenging to carry out but showed that the methodology was feasible. Our findings on the repetition of self-harm may partly reflect an unequal distribution of baseline risk factors between groups. However, we cannot rule out the possibility that the intervention was associated with a true increase in the risk of repetition. Future studies of these apparently simple contact interventions need to be alert to this possibility and should aim to identify the active components of therapeutic contact with a view to refining existing interventions or developing new ones.
Background
The evidence base for effective interventions to reduce repetition following an episode of self-harm is limited. The recent NICE guidelines139 suggested that three to 12 sessions of brief psychological intervention might reduce the risk of repetition following self-harm. The effectiveness of low-cost universal interventions such as telephone contact or sending postcards expressing concern following an episode of self-poisoning was also reviewed. The guidelines concluded that there was insufficient evidence of clinical benefit for these low-cost universal interventions, but further research in this area was recommended. In an early study by Motto and Bostrom24 (discussed in the next chapter), provision of letters to patients previously admitted to psychiatric hospitals was associated with a lower risk of suicide in the first 2 years of the study (the proportion of individuals dying by suicide was < 2% in the contact group compared with > 3% in the no contact group; p = 0.043), although the effect diminished over the 15-year follow-up period.
A variant of this intervention was used in a more recent Australian trial of individuals who had intentionally poisoned themselves. 140,141 Participants were randomised to receive either a series of postcards over 12 months (in addition to usual treatment) or usual treatment alone. The postcards included a simple message of concern. The proportion of individuals repeating self-poisoning and presenting to hospital was no different between the two groups (intervention 15%, 95% CI 11.5% to 18.7%, vs. control 17%, 95% CI 13.5% to 21.0%) but the number of repetitions in the intervention group was half that in the usual treatment group [101 vs. 192, incidence risk ratio (IRR) 0.55, 95% CI 0.35 to 0.87]. These treatment effects were maintained at the 2-year follow-up. However, the between-group difference in the number of repetitions was largely accounted for by a small number of women in the control group (n = 18, < 3% of the sample) who had three or more repeat episodes of self-harm during the follow-up period. A replication of this study in New Zealand found that, after adjustment for previous self-harm, there were no significant differences between the control and intervention groups in the proportion of participants re-presenting with self-harm or in the total number of re-presentations for self-harm. 142 A modified version of the intervention (which included greeting cards with pictures rather than just text, and offers in several of the cards to contact the treating toxicologist) was tested in a large sample of patients admitted with self-poisoning at a hospital in Iran. 143 The study found a reduction in number of suicide attempts in the intervention group (relative risk reduction 0.42, 95% CI 0.11 to 0.63) but the treatment context (low levels of mental health care) and overall low incidence of repetition in both the treatment and control groups determined from follow-up interviews (3.0% for the intervention group and 5.1% for the control group) compared with those in Western countries (median repeat rate for hospital-treated episodes 16%)144 mean that it may not be possible to generalise the findings internationally.
A different approach to the use of postcards is the provision of emergency or crisis cards that encourage help-seeking or which offer enhanced access to services. The findings of studies using these methods have also been variable. A British study that examined the effect of emergency cards found that the proportion of individuals repeating self-harm was slightly higher in the intervention group than in the control group (OR 1.20, 95% CI 0.82 to 1.75). 145 However, a subgroup analysis found that, in those without a previous history of self-harm, the intervention was associated with a reduced risk of repetition at 6 months (8% for the intervention vs. 12% for usual treatment; OR 0.64, 95% CI 0.34 to 1.22), although statistical evidence for an effect was weak, whereas, for those with a past history, provision of the card appeared to be associated with an almost doubling in the risk of repetition (27% vs. 16.5%; OR 1.85, 95% CI 1.14 to 3.03). A French study of individuals who had poisoned themselves used telephone contact as an alternative to mail. 146 Participants received telephone contact at 1 month, telephone contact at 3 months or no telephone contact, with experienced psychiatrists (who had not previously met the participants) making the calls. There were few differences in outcomes between the groups in an intention-to-treat analysis.
Combination approaches have also been tried. A recent World Health Organization-sponsored trial in eight hospitals in Brazil, India, Sri Lanka, Iran and China randomised individuals who had made suicide attempts to either ‘brief intervention and contact’ or treatment as usual. 147 The intervention involved provision of a structured 1-hour information session. After discharge, clinicians made nine follow-up contacts over 18 months either by telephone or in person. Referrals to other agencies and services were arranged as appropriate. Although the overall number of deaths was small, the proportion of individuals who died by suicide was lower in the intervention group than in the control group (0.2% vs. 2.2%, p < 0.001). However, methodological issues (e.g. concerning sources of mortality data) mean that the findings of this study need to be interpreted cautiously. When repeat non-fatal suicide attempts in the 18 months following the index attempt were compared, the researchers found little difference between the intervention and treatment-as-usual groups. 148
Simple contact-type interventions may hold some promise in the care of individuals who have harmed themselves, but their effectiveness and potential mechanisms of action remain unclear. Authors have suggested that they enhance ‘social connectedness’ – a sense of being joined to something meaningful outside oneself that acts as a stabilising emotional influence. 24 Alternatively, these interventions might facilitate access to existing health services. This chapter describes two studies: in the first study we used qualitative research methods to help develop and refine a brief contact intervention aimed at reducing repeat self-harm; in the second study we went on to pilot the use of this contact intervention in a small randomised trial.
STUDY 1: DEVELOPING A CONTACT-BASED INTERVENTION FOR SELF-HARM
Objectives
We aimed to gain an understanding of the underlying psychological mechanisms and content of interventions that might be of benefit or detriment to patients in preventing repetition of self-harm. We wanted to further understand the pragmatic barriers to the implementation of various forms of follow-up contact care following hospitalisation from an episode of self-harm by bringing in the perspectives of staff working on the ‘front line’.
Methods
The study was presented to the Bolton Research Ethics Committee, north-west England, who ruled that ethical approval was not required under NHS research governance arrangements as this was a service development study (08/H1009/32).
Using qualitative methodology, we investigated service user and staff experiences of, and attitudes towards, different types of intervention. Both staff and service users consented to the use of verbatim quotations.
Service user interviews
Service users who had recently attended the emergency departments of three hospitals in a city in the north-west of England following self-harm were given information packs inviting them to participate in the study. ‘Non-fatal self-harm’ was defined as intentional self-poisoning or self-injury, irrespective of motivation. 25 We employed purposive sampling149 for service user interviews to select male and female adult patients of varying age and self-harm history and directed the distribution of information packs accordingly. People fulfilling these criteria were likely to have different needs and preferences regarding support following a self-harm episode. Semistructured interviews were conducted using a topic guide (see Appendix 7) with prompts that allowed the researcher flexibility to follow up issues that emerged. During the interviews, the researcher introduced different contact-based interventions and asked the participant to comment on them.
Staff focus group
A purposive sample of key informants from clinical staff in three relevant service areas (emergency department, liaison psychiatry and primary care) and workers from the voluntary sector were recruited. A focus group was conducted with most of the staff participants (n = 8) using a topic guide (see Appendix 8). The focus group was introduced as an open discussion with the aim of informing the development of a pilot intervention for people who had self-harmed. Additional individual interviews were conducted for those unable to attend the focus group, and their contributions within the thematic coding frame identified from the group discussion analysis were included in the results.
Data analysis
We conducted thematic analyses150 of the transcribed interviews with service users (mean time of service user interview was 57 minutes) and staff and the focus group discussion (70 minutes' duration). Analytical themes were identified to summarise the data and were coded using computer-assisted qualitative data analysis software (NVivo version 7; QSR International, Southport, UK), to facilitate comparison and develop descriptive accounts. Quotations were selected to illustrate particular themes.
Researcher orientations
The main investigator (JC) conducted all of the interviews and facilitated the focus group. She is a trained psychiatric nurse, with experience of working with those who self-harm. The other investigators included an academic psychiatrist (NK), an experienced qualitative methodologist (JD) and a doctoral student in qualitative methodology (CH). Two researchers (including the main investigator) (JC, CH) analysed the interview transcripts, with another blind coding the initial interviews (AOS). We acknowledge that our professional backgrounds may have influenced the themes derived from the data, although effort was made through the methods of constant comparison and discussion within the research group to keep our themes grounded in the data.
Results
Participants
Of the 17 service users who expressed interest in the study, 11 (SU1–SU11; six females, five males), aged 18–53 years, participated. The predominant method of harm was self-poisoning (10/11), although four of the participants described mixed methods.
Of 16 clinical staff from relevant service areas (emergency department, liaison psychiatry, primary care and the voluntary sector) invited to participate, eight (SP1–SP8) agreed to take part in the focus group and two (SP9, SP10) in individual staff interviews.
Thematic analysis
A number of themes emerged from the data (Table 39 provides illustrative quotations). These included the need for support and encouragement and for some form of intervention shortly after hospital attendance for self-harm. Staff agreed that the immediate period after discharge was a vulnerable time, and both service users and staff expressed a need for contact to be proactive, as service users might find it difficult to initiate obtaining help.
An important aspect of care mentioned by both groups was the ‘genuineness of the service’, although there was a subtle difference in interpretation. Staff were more concerned with the style of the service, whereas service users were more concerned with the manner of the clinicians' responses. Staff felt that, for the intervention to be worthwhile and perceived as genuine, it should be integrated into current services, and there should be some consistency of staff delivering the intervention.
Potential mechanisms emerged from the transcripts that provided insight into how a contact-based intervention might be of benefit. Letters expressing concern were perceived as a gesture of caring that was ultimately reassuring for the recipient as he or she experienced being looked after (‘contained’). For some, this would prevent further self-harm, as contact with other people would counter against loneliness and fear of abandonment, and acknowledging their pain might reduce their sense of isolation or suffering alone.
| Theme | Illustrative quotations |
|---|---|
| Support and encouragement | ‘Just give me some more encouragement not to do stupid things, instead of being kicked out the front door and thinking what you're going to do yourself, if you got a bit more encouragement then it helps you along’ (SU8) |
| ‘I like the idea of somebody following them up (. . .) the fact that there's somebody else also looking into it to make sure that there's a safety net in place’ (SP10) | |
| Time of greatest need is directly after discharge | ‘because there's that window when they're more likely to self-harm, and from my experience, that impulsivity is sort of greatest in the 24 hours after [discharge from A&E]’ (SP4) |
| Gesture of caring | ‘Well, it [letters] just gives you . . . you think someone's caring for you – someone's doing something for you and thinking of you’ (SU8) |
| Genuine in delivery | ‘I think it has to be given out with, sort of, sincerity and meaning . . . You want them to feel that this is a genuine support service’ (SP9) |
| ‘If the person on the other end of the phone wasn't bothered because it's half past four in the morning, she's just waiting to get off the phone or something, you can just tell in her voice’ (SU8) | |
| Mode of delivery | ‘I just think it's quicker and easier on the phone’ (SU10) |
| ‘the phone calls would have helped initially in the first few weeks but letters might also help, . . . at a later stage’ (SU1) | |
| Mitigates against loneliness | ‘that would be good if you could read [in the letters]: “I missed you today I hope everything is OK”, that's reassuring, someone gives a shit. That's what it boils down to – I'm alone and isolated’ (SU1) |
| Integrated into current services | ‘if they say “no, things aren't right” . . . you can't just say “oh sorry to hear that”, you then have to get them a service, so then services have to be able to respond’ (SP6) |
| Promoting engagement with services (signposting) | ‘they struggle to, you know, initiate any contact with the GPs or anything themselves, so there has to be that element of chasing them, I think’ (SP4) |
| ‘extending that to people, you know, even if you don't feel able to make this call, there are other services available to you and listing out some generalised services with some details’ (SP2) | |
| ‘for me the more you're aware what's out there the more choices you've got’ (SU1) | |
| Delivery by mental health specialists | ‘It would be better if they were trained in mental health problems, because they have more understanding then’ (SU7) |
| ‘it's very difficult to answer telephone calls to people in crisis when you've never met them before, and I think you've just got to bear that in mind when you're trying to set up a service’ (SP5) |
Promoting engagement with services by providing people with relevant support information was viewed by staff as an important function, particularly for those who did not engage with statutory treatment. Raising awareness of other options was a particular benefit highlighted by the service users.
Practical issues and problems relating to the proposed interventions included a preference by service users for a mode of contact that was immediate (at least initially), perhaps by telephone; however, it was stated that letters might be acceptable later. The letters were viewed as potentially counteracting feelings of loneliness, and the proposed wording was considered caring, although there was no consensus on the preferred frequency of contact. There was agreement between service users and staff that the intervention should be delivered by mental health specialists, as they had the necessary skills and experience of dealing with people in crisis; however, they suggested that the impact on the staff of dealing with these situations should be considered. Issues of privacy, confidentiality and access were raised in the context of using the internet as a means of communication, similar to concerns relating to text messaging in the Bristol-led pilot study (see Chapter 8). As in the Bristol study, letters and the telephone were seen as the preferred mode of contact, although illiteracy, no fixed address, not having a telephone and not having any telephone credit were raised as potential barriers to a contact-based intervention.
Strengths and limitations
As with many qualitative studies, the small sample size limits the generalisability of the findings and our results need therefore to be interpreted with caution. 151 Those who self-harm are a difficult group to engage in research,152,153 and it may be that the views presented here differ from those of potential participants who did not respond to the invitation to participate in the study.
Informing the design of the proposed intervention
Preferences around timing, content, duration, method and delivery of contact were highlighted in the service user accounts. We identified some of the aspects of contact interventions that people valued, in particular the need for encouragement and support soon after discharge. Telephone calls were mentioned as providing immediacy of contact and a means of proactively engaging the service users. Service users also expressed positive views of simple messages of concern delivered by post. They considered that any contact provided should be genuine and caring, with, for example, letters being worded appropriately. Awareness of other service options was also considered useful.
The findings suggested that an appropriate design for an intervention might be the provision of an information leaflet, telephone calls (soon after discharge) and then letters (offering continuity of contact). In the next phase of the work we piloted an intervention informed by these findings.
STUDY 2: PILOTING A CONTACT-BASED INTERVENTION FOR SELF-HARM
Objectives
-
To investigate the utility and feasibility of aspects of our methodology for a contact-based intervention for preventing repetition of self-harm (particularly recruitment and randomisation).
-
To assess the acceptability of the contact-based intervention to patients, and to further refine the intervention in response to feedback.
-
To determine the proportion of patients with at least one repeat episode of self-harm in 12 months, and the number of repeat episodes of self-harm over 12 months in both the intervention group and the control group.
Methods
Design
The design for this pilot study was a parallel-group randomised controlled trial. Individuals were randomised to the intervention and treatment as usual or to treatment as usual alone.
Inclusion criteria
Potentially eligible participants were adults aged > 18 years who presented to the emergency departments of two study hospitals with self-harm during a 6-month period and were resident in Manchester. ‘Self-harm’ was defined as ‘an act of intentional self-injury or poisoning irrespective of the apparent purpose of the act’. This included acts of self-harm regardless of the associated degree of suicidal intent or medical seriousness.
Exclusion criteria
The following groups of patients were excluded from the study: psychiatric inpatients, patients with a general hospital admission of > 7 days, those of no fixed abode or with no telephone access and those unable to give informed consent during the first telephone call. Patients who were not able to understand English were also excluded from the study as the intervention involved telephone calls and would not be suitable for this group.
Sample size
We aimed to achieve a maximum of 50 patients in each of the intervention and usual treatment groups. This was a pilot study designed to inform a larger multicentre trial and provide preliminary data that would enable a more precise calculation of sample size in a main trial. We estimated that recruitment would be required for a minimum of 3 months.
Recruitment and consent procedure
Once clinicians working in the clinical teams at the two hospitals had ascertained patients' eligibility, patients were sent by post an invitation letter, an information sheet about the study and a copy of the consent sheet. Patients were contacted by a clinical researcher by telephone at least 3 working days later, who then invited them to take part in the study and audio recorded their verbal consent. Contact details available on hospital medical records systems were verified with the patients' GPs if required. The patients' GPs and/or care co-ordinators were contacted with the consents to inform them of their patients' participation in the study. Those patients randomised to the intervention arm were sent an advice leaflet (see Appendix 9) and a notification of change of address form. Participants in both groups were advised that their routine treatment would not be affected by their participation in the study.
Randomisation procedures
The randomisation process was conducted by a remote internet-based randomisation service (www.sealedenvelope.com). The allocation sequence used a computer random number generator to select randomised permuted blocks with randomly varying block sizes. Separate allocation sequences were generated for each of the two collaborating hospitals/centres, and patients had an equal probability of assignment to each group. Patients were then informed of their allocation status. An e-mail confirmation of the identification number, the allocated treatment and the date and time of randomisation was sent to the clinical researcher. The randomisation list was kept separately from the collection of outcomes.
Blinding
Because of the nature of the intervention, all patients were unblinded and fully aware of their allocation to the intervention group or the control group. A researcher who was also unblinded administered the intervention, including the initial telephone call and the mailing of the letters. However, a researcher blind to allocation status collected outcome data using self-harm databases.
Intervention
Patients in the intervention group received an information leaflet (see Appendix 9) listing local sources of help, two telephone calls and then a series of letters. The leaflet provided information on national and local sources of help and was reviewed by the local service provider (Manchester Mental Health and Social Care Trust). It was posted to participants as soon as possible after consent, and another copy was included in the first letter. The telephone calls were made by clinical researchers using a semistructured format. The purpose of the telephone calls was to make contact and facilitate access to appropriate treatment. The first telephone call was attempted at least 3 days after the invitation letter was sent. The second telephone call was made a week later. The letters were sent to the participants over a 12-month period (schedule: 1, 2, 4, 6, 8 and 12 months), which is similar to the methodology used in other studies. The format of the letters followed a standard pattern and included a general statement of concern (see Appendix 10 for an example of a typical letter), but they were modified when indicated to personalise them in response to individual circumstances (e.g. ‘we are sorry to hear that you have been in hospital recently’). The first letter included further details of how to opt out of the study and a request that participants notify us of any change of address.
Usual treatment
Both the intervention and control groups received usual treatment, which was similar at the two participating sites. A mental health liaison nursing team was in operation 7 days a week between 0900 and 2100, with out-of-hours care provided by the duty psychiatrist. One-quarter of patients in the centres are referred for mental health follow-up after a specialist assessment, with one-fifth referred to social services or to the voluntary sector. 135
Study outcomes
We assessed the proportion of patients who accepted the invitation to join the study and gave informed consent. We recorded the proportion of patients with at least one repeat episode of self-harm resulting in attendance at a study hospital within 12 months, identified from hospital information systems. In addition, we noted the number of repeat episodes during the same time period. For all participants we also investigated use of health services to pilot collection of such data for the future economic evaluation of a full trial. Repetition and resource use data were obtained from routine information systems and hospital databases. In addition, patients receiving the intervention were asked in their final letter if they could be approached for their views on the intervention, and a stamped addressed envelope was enclosed for their reply. Within this self-selected group of patients who responded, qualitative interviews (see topic guide in Appendix 11) were conducted after the study period ended to assess the acceptability of the intervention and to help refine it.
Statistical analysis plan
In accordance with the CONSORT (Consolidated Standards of Reporting Trials) principles,154 we have reported all participant flow in the pilot study. All primary analysis was based on intention to treat. Because this was a feasibility study and was not powered to test for a difference between the intervention and usual treatment groups, our analyses were primarily descriptive in nature. We examined the incidence of any repeat self-harm as well as the number of repeat episodes.
Data analysis for the follow-up qualitative interviews
Data analysis for the qualitative interviews (see topic guide in Appendix 11) used methods of constant comparison with repeated scrutinising of transcripts to determine the themes emerging from the data.
Ethical approval
The study was ethically approved by Greater Manchester West North West 9 Research Ethics Committee and the International Standard Randomised Controlled Trial Number is ISRCTN65171515.
Results
Recruitment statistics
In total, there were 250 adult patients resident in the Manchester area who presented to the two study hospitals from 1 November 2010 to 17 May 2011 and who were identified as having harmed themselves. Figure 15 summarises the recruitment of participants to the study.
FIGURE 15.
Flow chart of recruitment to the study. Reproduced with permission from the British Journal of Psychiatry (URL: http://bjp.rcpsych.org/content/203/1/73/suppl/DC1).
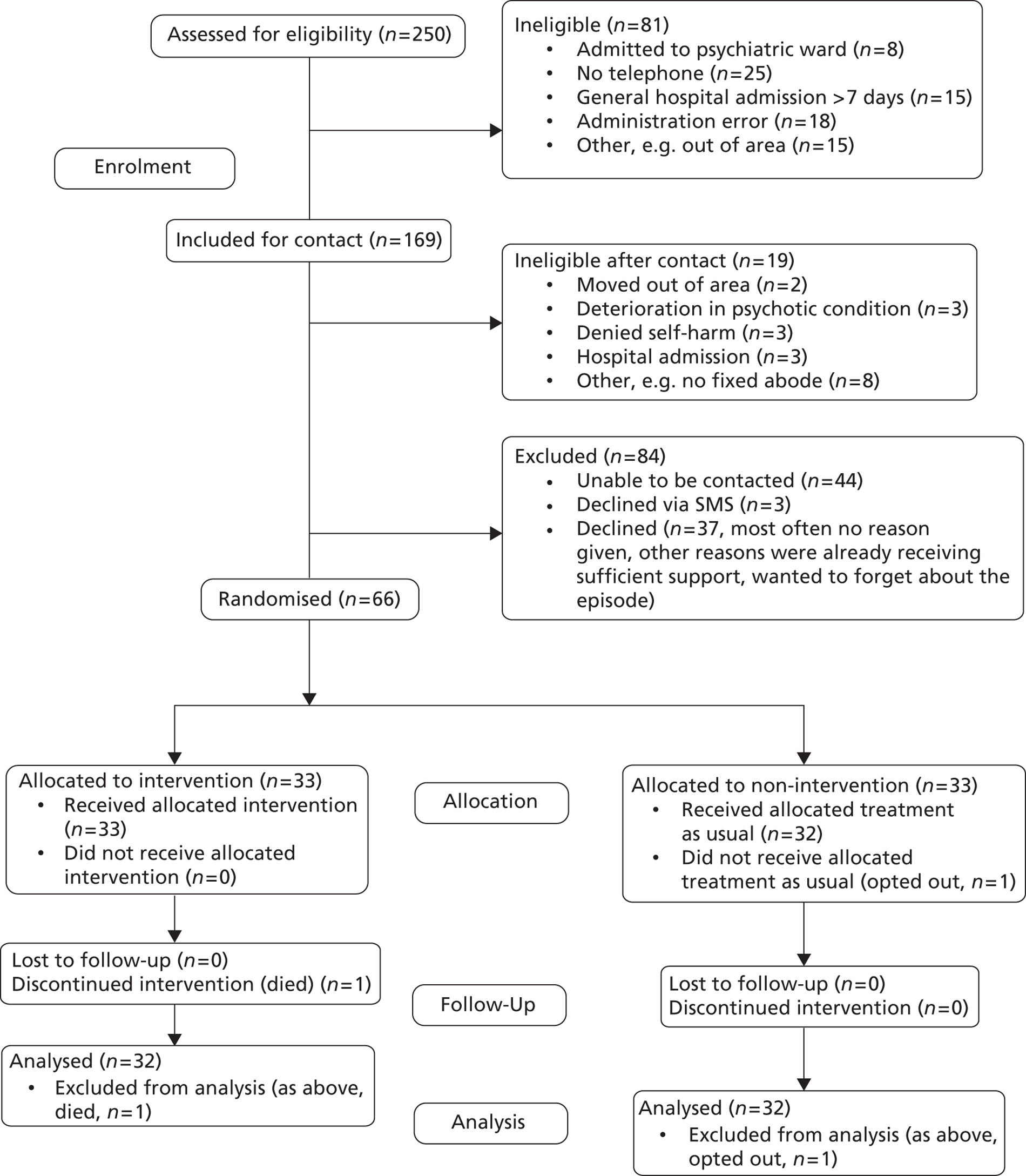
Comparison of study participants with eligible non-participants
Four clinical researchers recruited 66 participants from two emergency departments (hospitals A and B) during the study period. The median time between presentation to the emergency department and the information pack being sent was 2 days (IQR 1–6.25 days, range 0–64 days) and between presentation to the emergency department and recruitment to the study was 20 days (IQR 14–29 days, range 5–89 days).
When we compared study participants (n = 66) and eligible non-participants (i.e. those who we were unable to contact and those who declined, n = 84), we found that the two groups were similar in terms of sex (consented participants: males 34.8%, females 65.2%; eligible non-participants: males 42.9%, females 57.1%; χ2 = 0.993, p = 0.40) and age [consented participants: mean (SD) age 33.3 (10.2) years; eligible non-participants: mean (SD) age 35.9 (13.4) years].
Comparisons between the intervention group and the treatment as usual group
The two groups were similar with respect to sociodemographic characteristics (Table 40). However, participants in the intervention group were slightly more likely to be white, be unemployed, use methods other than poisoning to self-harm and have a past history of psychiatric treatment or previous self-harm; however, none of these differences reached a conventional level of statistical significance.
| Characteristic | Intervention group, n (%) | Treatment as usual group, n (%) |
|---|---|---|
| Sex (n = 65) | ||
| Female | 22 (66.7) | 20 (62.5) |
| Male | 11 (33.3) | 12 (37.5) |
| Age (years) (n = 65) | ||
| < 35 | 19 (57.6) | 17 (53.1) |
| ≥ 35 | 14 (42.4) | 15 (46.9) |
| Ethnicity (n = 40) | ||
| White | 19 (100.0) | 19 (90.5) |
| Non-white | 0 (0.0) | 2 (9.5) |
| Marital status (n = 60) | ||
| Married/partner | 6 (20.7) | 7 (22.6) |
| Not married | 23 (79.3) | 24 (77.4) |
| Employment status (n = 58) | ||
| Not employed/registered sick | 20 (69.0) | 17 (58.6) |
| All others (employed, student, houseperson/carer) | 9 (31.0) | 12 (41.4) |
| Main method of self-harm (n = 63) | ||
| Self-poisoning (drugs/other) | 24 (77.4) | 29 (90.6) |
| All other methods | 7 (22.6) | 3 (9.4) |
| Psychiatric treatment | ||
| Current psychiatric treatment | 14/32 (43.8) | 14/33 (42.4) |
| Previous psychiatric treatment | 21/33 (63.6) | 17/32 (53.1) |
| Previous self-harm | 22/33 (66.7) | 17/32 (53.1) |
Repetition of self-harm within 12 months
The repeat rate for individuals in the intervention group was 34% (95% CI 20% to 52%) whereas the repeat rate for individuals in the usual treatment group was 12.5% (95% CI 4% to 29%). The total number of episodes of repeat self-harm was also higher in the intervention group than in the usual treatment group (41 vs. 7). These differences were statistically significant when tested using logistic regression and negative binomial regression models respectively. The distribution of repeat self-harm episodes in any sample is highly skewed with a small number of individuals accounting for a large number of repeats. 1 In this study, in the analysis of number of self-harm episodes, there was one extreme outlier in the intervention group who alone accounted for nearly half of the total number of repeat episodes. Excluding this individual, the total number of repeat self-harm episodes was 21 compared with 7 (IRR = 3.0, 95% CI 0.84 to 10.68).
In analyses adjusting for baseline clinical factors (Table 41), the OR for repetition and the IRR for number of repeat episodes remained elevated; however, in the case of the OR, this was no longer statistically significant.
One person in the intervention group died following a drug overdose but was not included in the repeat self-harm group in the main analyses, as they did not re-present to the study hospitals with self-harm during the study period. As they had incomplete follow-up they were excluded from the main analyses (see Figure 15). Including this person in the repeat group increased the OR and IRR slightly (adjusted OR 4.97, 95% CI 1.10 to 22.50, p = 0.037; adjusted IRR 7.34, 95% CI 1.61 to 33.45, p = 0.01).
The death was reported to the study sponsor, the ethics committee and the research and development department of the NHS trust. The research team was given access to medical records and the hospital's own serious untoward incident investigation and spoke to the consultant psychiatrist providing care for the patient. There was no indication that the study procedures resulted in the death.
| Intervention group (n = 32) | Usual treatment group (n = 32) | OR | IRR | 95% CI | p-value | Adjusted ORa | Adjusted IRRa | 95% CI | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|
| No. repeating (%, 95% CI) | 11 (34, 20 to 52) | 4 (12.5, 4 to 29) | 3.67 | – | 1.0 to 13.1 | 0.05 | 4.35 | – | 0.9 to 19.8 | 0.06 |
| No. of repeat episodes (median, IQR) | 41 (0, 0–1) | 7 (0, 0–0) | – | 5.86 | 1.4 to 24.7 | 0.02 | – | 7.16 | 1.6 to 32.8 | 0.01 |
Intervention telephone calls
Most of the telephone calls by clinical researchers to the participants in the intervention arm of the trial (29/33) were rated as ‘good’ in terms of engagement with the patient.
The first intervention call in most cases focused on identifying and reinforcing available support and encouraging self-support, for example discussing triggers to self-harm, anticipating problems and related coping mechanisms and helpful activities, and discussing support that had been useful in the past. The clinical researcher would often signpost relevant support services listed in the information leaflet. Some patients expressed that they were receiving adequate support and were already aware of the information provided in the leaflet; others thought that they might use the information on the leaflet in the future if they needed help. Some participants found the telephone call supportive whereas others thought the face-to-face contact that they were already receiving from mental health staff was adequate.
The second telephone call focused on encouraging engagement with treatment (attending appointments, following up missed appointments, etc.), sometimes clarifying referral status from medical records (in one case because the patient felt unwell at the time of assessment and was unable to assimilate information, and in another case because the mental health worker called at the wrong address and subsequently closed the case as a ‘did not attend’).
Resource use
From hospital records and databases we collected resource use data retrospectively for both the intervention group and the treatment as usual group, from the index episode date to 12 months following the recruitment date. We assessed the feasibility of accessing records and extracting these data, and described the health service activity in both groups. From the emergency department records we recorded the number and types of presentations and disposal from the emergency department (estimated time taken to retrieve information = 5 minutes per individual record). From the mental health records we recorded the number of face-to-face contacts with each patient and the discipline of the person contacting (approximately 10 minutes per individual record). These data are summarised in Table 42. It was interesting to note that, despite a higher number of repeat episodes of self-harm in the intervention group, the overall number of emergency department presentations in the two groups was similar. The non-self-harm presentations in the usual treatment group resulted from a variety of physical complaints as well as specific mental health problems. The intervention group had a greater number of contacts with specialist mental health services [median (IQR) = 2 (0–9) vs. 0 (0–2), p = 0.053].
| Resource use | Intervention group (n = 32) | Usual treatment group (n = 32) | Mann–Whitney U | Chi-square | p-value |
|---|---|---|---|---|---|
| Emergency department attendances, median (IQR) | 1 (0–3) | 1 (0–2) | − 0.65 | 0.52 | |
| Medical inpatient days, median (IQR)a | 0 (0–1) | 0 (0–1) | 0.07 | 0.98 | |
| Face-to-face contacts with mental health services, median (IQR) | 2 (0–9) | 0 (0–2) | − 1.94 | 0.05 | |
| Admitted to a psychiatric bed, n (%) | 1 (3.1) | 2 (6.3) | 0.35 | 0.55 |
Evaluation of the intervention by participants
In the final letter (at 12 months after recruitment), participants receiving the intervention were invited to contact the research team to provide their opinion of the intervention and to suggest ways that it could be improved. Out of 33 participants, four responded (all male) but only three were interviewed as one respondent was unable to be contacted subsequently by telephone or letter. Of the three respondents, one repeated self-harm on multiple occasions, one repeated on two occasions and one did not repeat. Five themes emerged from these interviews (see Appendix 12 for illustrations of themes): (1) support received from other services, which was valued but, in the case of a participant receiving care from the voluntary sector only, not always enough; (2) participant needs were too great and the intervention did not meet, or was irrelevant to, needs; (3) useful for signposting/promoting help-seeking behaviour (telephone contact); (4) effects of letters/telephone contact (mitigates against loneliness, calming, prevents further self-harm and provides extra support); and (5) practical issues around the design of the intervention (easy to read, good intervals between letters, wanted letters to continue for a longer time in some cases).
Discussion
Feasibility
Overall, our proposed methodology proved feasible. Approximately 60% of those who were screened were found to be eligible for participation in the trial. Of those who were eligible, 30% could not be contacted and just over one-quarter (28%) declined. This refusal rate was very similar to refusal rates in previous studies in Western health-care settings140,142,146 but higher than that in an Iranian study. 143 Only one individual dropped out of the trial.
The process of online randomisation worked well and permitted real-time allocation of intervention status during the recruitment telephone call. The trial database allowed efficient tracking of participants and the scheduling and mailing of letters was not associated with any difficulties. There were no adverse incidents associated with trial processes, for example we recorded no instances of letters being sent to incorrect addresses or therapeutic telephone calls to individuals who were not the participants. Comparatively novel aspects of our methodology such as digital recording of consent and opting opt out by SMS were feasible. We restricted ourselves to basic resource use data within secondary care as these resources make up the majority of the costs of self-harm,155 and such data were relatively straightforward to collect.
Recruitment to the study was more challenging than we had anticipated. This may have been in part because we restricted ourselves to adult patients resident in Manchester (who on the basis of previous data make up approximately 60–70% of presentations to the study hospitals135). We did this because of differences in service provision for young people in the study centres, because of lack of evidence of efficacy of contact-type interventions in this group and because the information leaflet contained contact details for Manchester-specific services and helping agencies. Including individuals from a wider catchment area would have necessitated a number of different leaflets and would have added to the complexity of this pilot trial.
Contact information obtained from emergency departments was not always valid. Accessing mental health and GP medical records, when required, improved the accuracy of this information. The recruitment pathway involved multiple staff members involved in a multistage recruitment process. Clinical staff entered names of potentially eligible participants into the database. Designated members of the team screened participants for eligibility and then sent out recruitment packs. If individuals did not opt out they were contacted by one of four clinical researchers. The process from entry by clinicians to determine eligibility to the sending out of information packs created delays in recruitment.
Acceptability
Just over one-quarter of individuals who were eligible for the study refused to take part, but there was only one dropout from the study. Data from the post-intervention telephone interviews were limited but seemed to suggest that individuals found the intervention acceptable and helpful to some extent.
Differences in outcome between groups
We found that a higher proportion of individuals repeated self-harm in the intervention group than in the usual treatment group (33% vs. 13%). We also found that there was a higher number of repeat episodes in the intervention group than in the usual treatment group (41 vs. 7) and this reached conventional levels of statistical significance (p < 0.05). This difference was less marked when one potential outlier was excluded (21 vs. 7). We found an increased number of contacts from specialist mental health staff in the intervention group after recruitment to the trial compared with the treatment as usual group, but interestingly there was no difference in emergency department contacts. In addition, there was one death in the intervention group from an overdose of drugs. Baseline markers of increased risk (previous self-harm, psychiatric history, method of harm other than self-poisoning) appeared to be more common in the intervention group than in the usual treatment group. However, the differences between the groups persisted when we carried out a limited adjustment for these confounders.
Limitations
Our findings need to be interpreted in the context of the methodological limitations of the study. It was a small pilot study in just two centres and we were able to randomise just under half of the eligible participants. Although participants and non-participants were similar in terms of age and sex, it is possible that the two groups differed on other important variables, which could have meant that those included in our study were not typical of others who had harmed themselves. We included only adults resident in Manchester, an area with high rates of deprivation, self-harm and suicide, factors that could feasibly have limited the impact of the intervention. There may also have been problems with our main outcome measure as we considered only repeat self-harm behaviour that presented to the study hospitals. We did not record self-reported or community episodes of self-harm nor consider wider treatment outcomes156 because this would have been beyond the scope of the project. The lower than expected number of participants in the post-intervention interview also meant that we were unable to draw meaningful conclusions from this part of the study.
Implications for future work
In this trial, baseline risk factors appeared to be somewhat unequally distributed between the groups. We do not think this represented a problem with our randomisation (which was carried out using a commercially available online package), but rather was more likely to be a chance occurrence made more likely by our small sample size. The importance of stratifying for baseline variables, particularly previous self-harm, has been highlighted in previous work. 142,157
With respect to recruitment, a simpler and more flexible process could lead to higher recruitment rates. Perhaps the most productive measure would be to embed recruiting staff within clinical teams or to give existing staff dedicated time to carry out recruitment. Ensuring that administrative staff in emergency departments check patient details at reception is likely to be important, but was apparently routine practice in the centres in this study. Individuals who have harmed themselves may be a hard-to-reach population and one possibility would be to recruit patients in the emergency department before they leave (assuming of course that they have the capacity to consent). For those who are not approached in this way, recruitment by telephone, SMS or mail could also be tried. It should be noted that recruitment of sufficient numbers of individuals might be less challenging in hospitals with geographically defined catchments than it was in the current study. Researchers involved in recruitment need to be experienced clinical staff. At times they will be required to manage distressed patients and they also need to engage participants who have complex needs and who may be regarded by some staff as hard to help.
Some flexibility in the intervention might also improve delivery. For example, individuals who prove difficult to reach by telephone might receive only the information leaflet and letter components of the intervention.
This study considered repeat presentations to hospital for self-harm at 12 months as a main outcome. However, this may not be the most important measure of a treatment effect. 144 It does not take into account repeat episodes not resulting in presentation to hospital. Equally, it could be that increased hospital presentation for self-harm is a positive treatment outcome for some people, representing better engagement with services. A broader range of outcomes might be collected in future work (e.g. self-reported repetition, depression, hopelessness, suicidal ideation), but of course this will increase the complexity and cost of such studies.
Conclusions
Using qualitative methods we developed a contact-based intervention for individuals following self-harm. This consisted of an information leaflet, telephone calls soon after presentation and a series of letters over a 12-month period. In many ways this was a composite of interventions to date,146 and similar to a planned intervention in France. 158 With respect to the main aim of our study, we found that carrying out a pilot randomised trial of our intervention was challenging but feasible.
Our study was small and not designed to be an efficacy trial, but those who received the intervention appeared to be more likely to repeat self-harm and had higher rates of contact with specialist mental health services than those who received usual treatment alone. This could have been a chance occurrence or may have partly reflected an unequal distribution of baseline risk factors between groups. It should also be noted that we may have recruited a sample that was not representative of the wider population, particularly as the study was carried out in only one centre in the UK. Equally, it is possible that repeat self-harm presenting to hospital may not, in fact, represent a negative outcome but could be a positive marker of increased engagement. On the basis of our results, we cannot rule out the possibility that the intervention was associated with a true increase in the risk of repetition, but these findings should be regarded as tentative.
Future studies of these apparently simple contact interventions need to be alert to the possibility of increased repetition and should also record adverse effects. Studies to date of the effect of contact interventions on repeat self-harm have had mixed results, but some have suggested possible beneficial effects. Further work is needed to elucidate the active components of therapeutic contact following self-harm in these studies and to refine existing interventions or develop new ones.
Chapter 8 Development and pilot study of an intervention aimed at reducing the incidence of fatal and non-fatal self-harm in the period after psychiatric hospital discharge
Abstract
People recently discharged from inpatient psychiatric care are at high risk of suicide, with about 250 suicides (6% of all suicides) in England each year occurring in the 3 months after discharge. There is trial evidence from the USA that supportive letters sent by psychiatrists to patients in the period following hospital discharge resulted in a reduction in suicide. We aimed to assess the feasibility of conducting a similar trial in the context of present-day UK clinical practice. We developed and piloted a letter-based intervention suitable for all people discharged from a psychiatric unit. Up to eight letters were sent to patients over the 12 months after discharge. The intervention was relatively easy to operationalise, with the process of patient contact taking at most 7 hours per week per ward. Altogether, 102 patients discharged from the three wards in different hospitals in the south-west region received at least one letter, but only 45 (44.1%) received the full series of letters. The main reasons for dropout were patients opting out (n = 24) or readmission (n = 26). However, in the context of new policy initiatives of intensive follow-up post discharge in present-day UK practice, qualitative interviews with service users showed that most already felt adequately supported and the intervention added little to this. Those interviewed felt that it was possible that the intervention might benefit people new to, or with little follow-up from, mental health services, but that fewer letters should be mailed. Although there is a need for interventions in this period of high risk for suicide and self-harm, contact-based interventions may be more beneficial in areas where there is less intensive post-discharge support.
Background
The first few weeks after discharge from inpatient psychiatric care are associated with a greatly elevated risk of suicide. 159–163 An analysis of HES data for England carried out in the early stages of this research programme showed that the risk of non-fatal self-harm is similarly elevated in the period after hospital discharge. 164 In total, > 6% of patients discharged from psychiatric inpatient care were admitted to a general hospital bed as a result of self-harm in the subsequent 12 months.
Our understanding of why suicide risk is so high in this period and what can be done to reduce risk is limited. The Department of Health's guidance for mental health services in 2003165 recommended that (1) inpatient and community teams carry out a joint case review before discharge, (2) care plans should take into account the heightened risk of suicide in the first 3 months after discharge, with specific reference to the first week, and (3) patients who were thought to be at high risk of suicide during their admission should be followed up within 48 hours of discharge. However, no studies have investigated whether or not these recommendations have had an impact on post-discharge suicide rates.
A number of studies of letter-based contacts with patients in the period after hospital attendance for self-harm or psychiatric inpatient discharge have shown promising results in reducing repeat self-harm and suicide. 22 These interventions involved the mailing of a series of short letters from the hospital of discharge expressing concern about the person's well-being since discharge. In particular, a randomised controlled trial of letter-based contacts over a 5-year period with 843 patients who had been discharged from inpatient psychiatric care in the USA between 1968 and 1974 provided some evidence that those in receipt of such an intervention have a reduced risk of suicide. 23,24 A recent pilot study has demonstrated the feasibility of running a similar intervention amongst people discharged from military hospitals in the USA, although e-mail contacts were preferred by the (mainly male) participants. 166
The only randomised trials of contact-based interventions since Motto's original work23 have involved a different patient group: people who have attended an acute hospital following an episode of self-harm. In a recent study in Australia, eight letters, similar to those used in the original Motto study, were mailed over a 12-month period following discharge to people who had attended a toxicology unit following self-poisoning. 140 Similar interventions have been trialled in New Zealand and Iran among people who have attended hospital for treatment following self-harm. Findings from these trials have been mixed. 22 To the best of our knowledge, none has used qualitative interviews to explore patient attitudes to the intervention. 142,143
Objective
The aim of this element of our programme was to develop and pilot a contact-based intervention aimed at reducing the incidence of self-harm after discharge from psychiatric inpatient care. This chapter describes the development and piloting of the intervention. It was piloted with people discharged from inpatient psychiatric wards at three hospitals managed by two NHS trusts in the south-west of England (Bristol and Gloucester). Motto's 1976 study23 was used as the starting point for developing the intervention. At the time of recruiting the wards to the study, they did not have a process of intensive post-discharge follow-up in place, although this changed as the study progressed.
Methods
Intervention development
We carried out a questionnaire survey of current and recent psychiatric inpatients and conducted some qualitative interviews to inform the design of the contact-based intervention. The aim of these studies was to assess (1) patients' preferred means of contact (letter/e-mail/text/telephone); (2) whether or not they might find such letters useful; (3) the wording/contents of the letters; (4) the best frequency of contact; (5) who the letters should be sent by; and (6) any other issues that patients felt were relevant.
Exploratory interviews were undertaken with 10 recently discharged service users sampled from five general adult wards in two acute psychiatric hospitals in Bristol. Initially, consecutive patients were approached on the wards prior to discharge to obtain their consent for a post-discharge interview. As the interviews progressed we then used purposive sampling to identify patient groups who had not been interviewed, including people who lived alone, who had a history of self-harm or depression/affective disorder or who abused alcohol. Ward managers used their professional judgement with regard to which service users should be approached, and were guided by the research team as to which characteristics were of particular interest (see above). The aim of the interviews was to explore participants' attitudes to discharge, their experiences since discharge and their views about the proposed contact-based intervention.
A questionnaire was administered to 71 patients on four general adult psychiatric inpatient wards in Bristol. The questionnaires asked about patients' access to and use of different forms of communication technology and their preferred method of post-discharge contact.
To allow further development of the intervention and to ensure that its implementation was feasible and appropriate within existing discharge arrangements for psychiatric inpatients, we then presented the findings from these studies to groups of ward and community staff associated with the psychiatric inpatient units where the intervention would be piloted.
Pilot study
Aims and setting
The contact intervention was piloted on three wards in three psychiatric inpatient units managed by two mental health trusts in the south-west of England.
We used a cohort study design to assess:
-
the usefulness of the intervention to service users
-
the feasibility of running the intervention as a national study and ultimately as a service within the NHS
-
the feasibility of collecting data to identify the costs of the intervention (an economic evaluation) and outcome data.
Two of the participating inpatient psychiatric wards were located in Bristol with contrasting inner-city (ward A, a 23-bed unit) and suburban (ward B, a 19-bed unit) catchment populations. A third ward (ward C), with 22 beds, was located in Gloucester and served a mixed urban/rural population.
The Gloucester ward was recruited to the pilot 1 year after piloting began in Bristol and, because of time constraints and participant feedback from the qualitative interviews, the letters were mailed for the first 6 months following discharge only, so these patients received just six letters. Furthermore, some of the outcome data were not available for the Gloucester ward (ward C), and data on non-completion of the intervention were available for 6 months post discharge only, so most analyses focus on the two Bristol wards with comparable 12-month post-discharge data. Data are reported for the Gloucester ward when these are available and relevant.
Inclusion criteria
Consecutive patients discharged from the two Bristol wards over a 6-month period in 2009–10 and from the Gloucester ward over a 3-month period in 2011 were eligible to receive the intervention.
Exclusion criteria
We excluded the following psychiatric discharges from the pilot: (1) people who lived outside the catchment areas served by the study wards (as contact information on study leaflets was tailored to those living within the intervention wards' catchment areas); (2) people with no known or fixed address or who were discharged to prison or another psychiatric unit; and (3) patients whose discharge was notified to the person administering the study database > 4 weeks after discharge.
The contact intervention
The intervention that we developed consisted of a series of eight letters mailed out at increasing intervals over the 12 months following inpatient psychiatric discharge (at 1, 2 and 4 weeks and at 2, 4, 6, 9 and 12 months post discharge). Examples of the letters are given in Appendix 13.
The letters were signed by either the ward manager or a member of ward staff familiar to the patient. Each of the letters differed in the wording and was tailored to be appropriate to the patient's stage of care and whether or not he or she was still in contact with psychiatric services. In contrast to Motto's original study,23 recipients of the letters were not invited to make contact with the person signing the letter, as this was felt to be inappropriate within the context of local mental health-care service pathways. However, when patients responded to letters (this was very infrequent), individualised responses were added to subsequent letters. Patients who were readmitted and discharged again within the recruitment period received a further series of letters. Patients who were readmitted and discharged outside the recruitment period received no further letters. Copies of each letter were sent to the patients' care co-ordinators.
A support and advice leaflet (see Appendix 14) listing contact details of organisations offering telephone and face-to-face support was included with each mailing.
Letter administration was aided by a bespoke database installed on each unit's computer system and managed by a member of ward staff or a MHRN clinical studies officer. The database included automatic prompts when the next letter was due to be sent to a patient, and checks on the database ensured that patients were not sent letters if they had opted out of the study, had been readmitted or had died.
With ethical committee approval, individual patient consent was not sought for sending the letters as the letters were considered to be a service development. However, all letters included an opt-out slip giving patients the opportunity to opt out from receiving any further letters at any stage. In our qualitative evaluation of the pilot, for which we gained individual patient consent, we explored issues around the lack of consent with patients.
Process and outcome measures
We collected both qualitative and quantitative data during piloting. Qualitative interviews were conducted with 13 patients; this was complemented by a brief questionnaire on patient views of the intervention, sent by post to all patients who received one or more letters up to October 2010. Using trust information systems, we compared the number of readmissions to the two study wards in Bristol with the number of readmissions to other acute wards in Bristol for the periods before and during the intervention. We also searched emergency department records to quantify the incidence of post-discharge self-harm among patients discharged from the two study wards in Bristol during the intervention period.
We collected process data on whether participants (1) opted out of the intervention, (2) attended an emergency department/had a general hospital admission for self-harm (Bristol-based patients only) or (3) were readmitted to a psychiatric hospital.
We piloted the methods for collecting data for an economic evaluation of the intervention in a full trial by collecting relevant data from hospital information systems. We were given anonymised data on the number and type (face-to-face vs. telephone) of mental health community service contacts for a subset of 12 Bristol-based patients in the 12 months following discharge.
Ethics
Ethical approval was obtained from the Southmead Research Ethics Committee.
Results
Development studies
Questionnaire survey
In total, 48 of the 71 (67.6%) psychiatric inpatients at the time of the survey completed a questionnaire about their use of mobile phones and e-mail, as well as their preferred method of contact. Seventeen (35.4%) were aged < 36 years and 18 (37.5%) were male.
Two-thirds (32/48, 66.7%) of the respondents owned a mobile phone. Some respondents who owned mobile phones did not complete all items on the questionnaire, so the following figures are based on the number of participants who responded to each item. The majority (28/31, 90.3%) of responders used their phone to send text messages. One-third (9/27, 33.3%) thought that at home someone else might read their text messages and so it would be difficult to keep them private. Just over one-quarter (13/46, 28.3%) of patients had an e-mail address.
Only 26 patients responded to the final item on the questionnaire about how they would prefer to be contacted following discharge. Nearly one-quarter (6/26, 23.1%) of these patients stated that they would prefer not to be contacted. Of the remaining 20 individuals, eight selected more than one preferred mode so that there were 30 responses in all. Of the 15 individuals who owned a mobile phone and selected a preferred mode of contact, only four (26.7%) selected text messages. The most popular methods were telephone (13/15, 86.7%) and letter (11/15, 73.3%). Less than half (4/10, 40%) of those who used e-mail stated that they would like to be contacted by this method.
Exploratory interviews
Although most patients felt well supported after discharge, a few had felt unsupported and alone. Most interviewees said that it would be helpful to receive regular messages from people who have cared for them in hospital to ask how they were getting on. However, others thought that it would be better to be contacted by someone in the community care team, such as the community psychiatric nurse or social worker.
Most interviewees thought that messages from the ward should be received on a weekly basis after discharge, although some were concerned that this could become intrusive if it went on for too long. Most preferred the idea of receiving a letter rather than a telephone call as they felt that telephone calls could be intrusive. It was local NHS policy at the time of these interviews for ward staff to telephone patients twice in the first 2 weeks after hospital discharge, and a number of interviewees reported that they found these calls rather contrived and functional, and most did not find these supportive or helpful.
All those interviewed thought that having a ‘crisis card’ with a number to call if they were feeling very distressed would be helpful, and many said that just knowing that it is there would make them feel better. The importance of having a reliable response to crisis calls was stressed, as was the importance that the person answering the phone is both sympathetic and offers useful advice.
All interviewees said that the usefulness of any intervention would vary considerably according to the person and his or her situation, particularly depending on how long he or she had been in hospital and who he or she had around at home for support.
Summary
Findings from the above two studies were fed back to the research group and groups of inpatients and community mental health staff. It was agreed that the best form of contact would be by letter and that community staff should be sent copies of all communications. The wording of some letters was altered based on the feedback from interviewees and staff to include reminders about when patients might expect to be contacted by community services and to remind patients of the crisis contact numbers. A leaflet with further information about crisis contacts and other mental health-related sources of help and advice in the statutory and voluntary sectors was developed.
Pilot study
Participants
Table 43 shows the number and characteristics of patients who participated in the pilot. Altogether, 102 patients (66% males), with a mean age of 38 years, received one or more intervention letters. The main diagnostic group was schizophrenia/psychosis, comprising 44% of discharges over the study period, although information on diagnosis from ward records was not available for nearly two-thirds (27/43, 62.8%) of participants from ward B.
| Characteristic | Ward A (Bristol) | Ward B (Bristol) | Ward C (Gloucester) | All wards |
|---|---|---|---|---|
| Recruitment start and end dates | November 2009–April 2010 | January–July 2010 | February–May 2011 | November 2009–May 2011 |
| No. of patients recruited | 37 | 43 | 22 | 102 |
| Age (years), mean (range) | 39.2 (18–70) | 38.2 (20–67) | 35.4 (18–57) | 37.8 (18–70) |
| Sex, n (%) | ||||
| Male | 26 (70.3) | 23 (53.5) | 18 (81.8) | 67 (65.7) |
| Female | 11 (29.7) | 20 (46.5) | 4 (18.2) | 35 (34.3) |
| Diagnosis,a n (%) | ||||
| Affective disorders | 15 (45.5) | 3 (18.8) | 6 (27.3) | 24 (33.8) |
| Schizophrenia and other psychoses | 10 (30.3) | 12 (75.0) | 9 (40.9) | 31 (43.7) |
| Personality disorders | 3 (9.1) | 0 | 5 (22.7) | 8 (11.3) |
| Substance-related disorders | 3 (9.1) | 0 | 1 (4.5) | 4 (5.6) |
| Other | 2 (6.1) | 1 (6.3) | 1 (4.5) | 4 (5.6) |
| Follow-up end date | 18 May 2011 | 11 August 2011 | 25 November 2011 | 25 November 2011 |
Acceptability and usefulness of the intervention
Nearly two-thirds (102/162, 63.0%) of patients discharged from wards A and B over the recruitment period received at least one letter (Figure 16). The main reason for non-recruitment was residence out of the ward's catchment area. Of those who received at least one study letter, only 45 (44.1%) received all of the study letters (see Figure 16). These represent 27.8% (45/162) of all discharges over the relevant recruitment periods.
An opt-out slip and stamped addressed envelope were enclosed with each mailing so that, if they wished, participants could opt out of receiving the letters. The main reasons for cessation of mailings were patient opt-out (24/102, 23.5%) and readmission (26/102, 25.5%). Although a lower proportion of patients opted out from ward C (18.2%), this was most likely because of the shorter period over which letters were mailed from that ward.
Some people who opted out or who were excluded for other reasons were also subsequently readmitted but were not then recorded as excluded for that reason.
FIGURE 16.
Patient flow for recruitment and mailings.
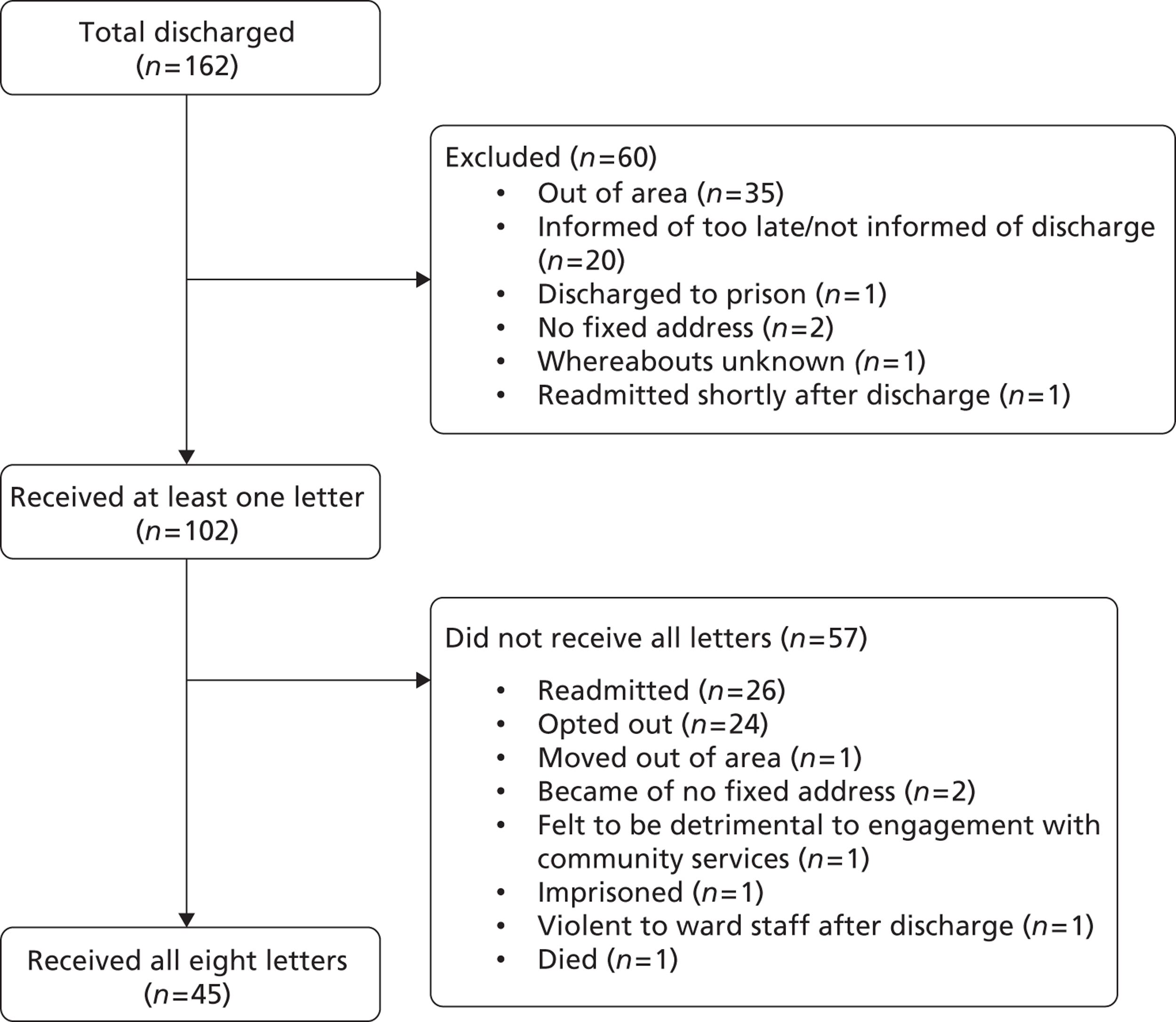
Data on post-discharge self-harm
Because of resource limitations and time constraints we collected information on post-discharge self-harm for patients from the Bristol A&E units only. Twelve (15.0%, 95% CI 6% to 21%) of the people discharged from the Bristol inpatient psychiatric wards attended a local A&E unit for treatment following a self-harm episode in the 12 months post discharge; of these, eight (10% of those discharged, 95% CI 3% to 17%) were admitted to a hospital bed. In addition, one person died by suicide. There was no evidence that the intervention was implicated in precipitating any of these episodes.
Two study participants self-harmed within 2 weeks of discharge (one the same day), a further eight within the first 6 months after discharge and two during the 6–12 months after discharge. Most of these participants were still receiving the letters at the time of self-harm [only 3/11 (27.3%) were not – one had self-harmed 6 months after their first inpatient discharge within the study period and had opted out of the intervention 4 months earlier and the other two had self-harmed following a further psychiatric admission and discharge].
Readmissions
We were able to use trust data to crudely compare levels of readmissions within 12 months to wards A and B with levels of readmissions to other acute wards in the same hospitals before and during the study period (Table 44). There was no evidence of a reduction in readmissions on ward A – 35.3% of people were readmitted pre intervention and 35.7% of people were readmitted during the intervention period. In contrast, readmission rates fell on the two comparator wards. Although readmissions did fall on ward B (from 44.1% to 36.2%), equivalent reductions were seen on the other acute ward at that hospital.
| Hospital A | Hospital B | ||||
|---|---|---|---|---|---|
| Intervention period | Ward A (intervention) | Ward X (non-intervention) | Ward Y (non-intervention) | Ward B (intervention) | Ward Z (non-intervention) |
| Pre-intervention perioda | |||||
| Total no. of discharges | 51 | 62 | 89 | 68 | 52 |
| Total no. (%) readmitted within 12 months | 18 (35.3) | 21 (33.9) | 36 (40.4) | 30 (44.1) | 24 (46.2) |
| Intervention periodb | |||||
| Total no. of discharges | 56 | 48 | 69 | 58 | 102 |
| Total no. (%) readmitted within 12 months | 20 (35.7) | 15 (31.3) | 20 (29.0) | 21 (36.2) | 37 (36.3) |
| Difference in readmissions across the two time points, % | 0.4 | − 2.6 | − 11.4 | − 7.9 | − 9.9 |
Service contacts during the 12 months post index discharge
To pilot data collection for an economic evaluation, we collected detailed data on post-discharge contacts made by mental health-care staff with 12 individuals. On average they made 12 contacts (either face-to-face or by telephone) during the first month after discharge (Figure 17). Eleven of the 12 individuals had at least two follow-up contacts in the first week following discharge. The one individual who had no contact during the first week had three face-to-face contacts during the second week. When we stratified our sample to investigate whether or not the distribution of contact timings was affected by readmissions to hospital we found no evidence that such readmissions contributed to the observed rise in contacts in months 6 and 7.
FIGURE 17.
Mean number of face-to-face and telephone contacts by month over the 12 months following the index inpatient discharge (n = 12 patients).
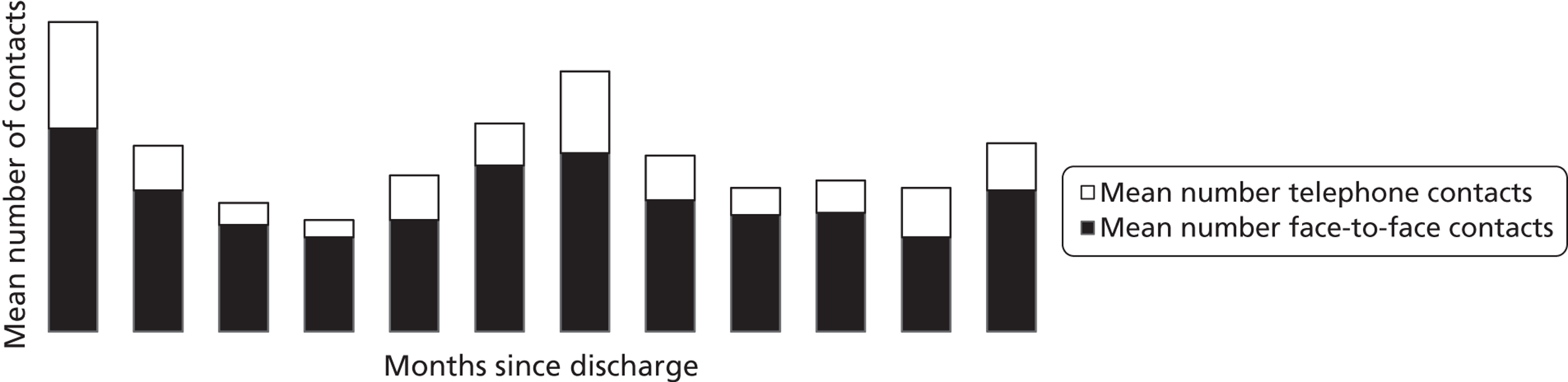
Information from the qualitative interviews (see below) provides evidence on whether the participants felt that the intervention added anything to the perceived level of support provided by community mental health services.
During the course of the study, the mental health trust in one of the areas in which the pilot took place instituted a policy of two home visits to patients in the first week following hospital discharge.
Qualitative interviews
All people who received one or more letters were invited to participate in a qualitative interview to obtain their views about the intervention and assess its acceptability. Thirteen (12.7%) agreed to be interviewed. Table 45 shows the characteristics of these patients. The sample comprised primarily long-term service users who were aware of the services and numbers to ring in a crisis situation. This then influenced how they perceived an intervention aimed at providing post-discharge support.
| Characteristic | Summary data |
|---|---|
| No. of patients recruited | 13 |
| Age (years), mean (median, range) | 40.8 (41.0, 31–56) |
| Sex, n (%) | |
| Male | 8 (61.5) |
| Female | 5 (38.5) |
| Ethnicity,a n (%) | |
| White | 9 (75.0) |
| Black | 2 (16.7) |
| Mixed | 1 (8.3) |
| Diagnosis,b n (%) | |
| Affective disorders | 6 (54.5) |
| Schizophrenia and other psychoses | 2 (18.2) |
| Personality disorders | 2 (18.2) |
| Substance-related disorders | 0 (0.0) |
| Other | 1 (9.1) |
Five respondents had received four intervention letters at the time of the interview, six had received five to seven letters and one had received all eight letters. The findings of the qualitative interviews of particular relevance to the intervention are reported here.
The interviewer field notes and the audio recordings of the interviews indicate that some participants were difficult to engage during the interview. The interview findings must be interpreted with this in mind. The sample size was also small as not all eligible patients were willing to take part, resulting in a sample that does not include a wide range of characteristics. Those who were interviewed had particular experiences of mental health services, including of post-discharge support, and these experiences appeared to influence their views on the intervention. In general, these participants appeared well supported by community mental health services following discharge and recalled instances of the ward telephoning to check on their welfare. The intervention was seen as less or not useful among those who were well supported, as they felt that it did not offer anything new. Therefore, it was felt to be of better use for those new to the system and those with less support:
I think I’m quite lucky that the support I was getting from [team name], and I am still getting pretty much meets all of my needs. So I can imagine for somebody else, if they weren’t happy with what was going on, it might have been more helpful.
P12
To the first timers, yeah, they come out and they’ve got nowhere to turn, and obviously the information could be vital for them.
P13
Because if you do get into trouble, because you’ve already been in the ward, you know the people to ring up (. . .) once you’re admitted in, you work with the crisis team and also your CPN [community psychiatric nurse], they give you all the numbers and things anyway.
P8
Nevertheless, the psychological benefits of receiving the letters, the feelings of reassurance, of not being forgotten, an acknowledgement of hospitalisation and that ‘somebody cares’, were highlighted by several participants. One felt this way despite thinking that the letters were computer generated, and strongly felt that the benefits of sending the letters outweighed any risks. Some also viewed the intervention positively because it appeared to be the only link to the ward/hospital and because it facilitated having all of the numbers in one place so that they were handy in a crisis.
One person (who had been asked to leave the ward) had found the letters upsetting and another explained that the salutation (use of their forename and surname) on the letters had triggered their psychotic symptoms. The salutation was subsequently personalised on letters by the members of ward staff who signed the letters. The intervention did not, however, cause harm to most participants.
Although some found the initial letters positive and reassuring, a recurring theme was that after a while the letters felt repetitive in content, and too frequent, and thereby a reminder of their hospitalisation:
I thought it was quite reassuring (. . .) if I needed contact with anybody then you know the services were available. (. . .) [laughs] And after the first couple, I thought, ‘oh! not another one!’
P10
When I first got the letters they were kind of a reassurance as such that there was (. . .) fall-back service after the crisis team (. . .) But what I found it was a repetition, it was the same letter, same numbers (. . .) it was a reminder that I'd been into hospital.
P9
The similarity of the information provided also influenced whether the letters/leaflets were retained or thrown away and contributed somewhat to the feelings of some that the letters were too frequent and impersonal:
The letters were impersonal, like round robins. To me they suggested that you’d written a draft, it was printed off on the computer, and sent to everyone. (. . .) If you’re looking for a way of reducing self-harm or suicide after a hospital admission you need to have a sense of love (. . .) this sense of actual human compassion instead of this computerised letter and a round robin of telephone numbers.
P5
Participants' use of the numbers/information provided in the letters/leaflets was minimal. Reactions to the letters being sent from the ward were mixed, with some viewing them as positive and others not finding them helpful. There was some confusion and questioning over not being able to contact the ward, despite the letters coming from the ward:
I think the strange thing was though, getting a letter from the hospital kind of telling me about support but nothing of it was to do with them and that felt a little bit strange. (. . .) it was like reminding me that they were there, but they weren’t going to do anything and they can’t help, they’re just giving me information.
P12
Although the opt-out slip was not seen to be important by most participants, some acknowledged that it might have been important for others. Not obtaining consent before sending the letters did not appear to be a particularly problematic issue.
These findings emphasise the different ways that such an intervention can be perceived by mental health service users. For some users a letter reminded them of their illness and hence dependency on the services, whereas for others it may have been a crucial link to the services. It seems unlikely that a single intervention could be developed that will benefit all users.
Questionnaire survey
Individuals who had received letters up to October 2010 (n = 77) were sent a brief questionnaire (see Appendix 15) asking for their views about the letters and information leaflets. Ten (13%) of the questionnaires were completed, resulting in a self-selected sample. Four of the 10 had either already participated in a qualitative interview or agreed to take part in an interview following completion of the questionnaire. The questionnaires therefore provided information only on the views of six respondents in addition to those interviewed.
Although three questionnaire respondents had opted out of the intervention, only one of these was consistently negative in his responses. One described receiving the letters as ‘reassuring’. The other seven respondents were all positive about receiving the letters, one describing them as reminding him of the ‘positive help’ that he had received on the ward. When asked to comment on the letters, two of the seven respondents who had not opted out of the intervention pointed out how useful the support and advice leaflet could be (although neither had used it). Six of the seven respondents who had not opted out of the intervention and two of those who had found the number of letters ‘about right’.
Time taken to establish and deliver the intervention on study wards
The intervention was administered on the wards by two MHRN clinical studies officers and by a ward administrator/health-care assistant. The maximum time taken for mailing the letters in a single week was 7 hours for ward A, 4 hours for ward B and 5 hours for ward C. This gives an indication of the resource required to maintain the intervention at ‘steady state’.
Our assessment of the amount of researcher time required for site recruitment and set-up and maintenance of the intervention was based on our experience on ward C (Gloucester), as by the time that we recruited this ward the development problems with running the intervention and the study database had been resolved at the other two pilot sites. To recruit a centre and set up the intervention on the ward took approximately 20 hours of researcher time, including preparation for meetings, attendance at staff meetings, travel and subsequent contacts. Liaison with trust research and development and tailoring the intervention documents for local use (including details of local organisations for the support and advice leaflet) took approximately 11 hours, and liaison with and training of the person administering the intervention took approximately 17 hours. Thus, a total of 48 hours of research team input was required to establish the intervention on a ward. Once established, approximately 30–60 minutes of researcher time per week was required to respond to issues related to administration of the letters.
Discussion
We set out to develop and pilot a contact-based intervention aimed at reducing the incidence of post-discharge self-harm with the eventual ambition of seeking funding for a full trial of the intervention. Using quantitative and qualitative approaches and involving service users and mental health staff, we successfully designed a letter-based intervention and a process for administering these letters within mainstream psychiatric services. The aims of our pilot were to determine:
-
whether or not the intervention was seen as useful by service users
-
whether or not it would be feasible to run the intervention as a national study and ultimately as a service within the NHS
-
the feasibility of collecting data to identify the costs of the intervention (an economic evaluation) and outcome data.
In this section we discuss each of these issues in turn.
Service users’ views of the intervention
Our qualitative interviews with 13 service users who received the letter, as well as the responses to the questionnaire survey, indicated that, although most patients could see the potential benefits of the letters and were positive about receiving them, they generally felt that they would be of more benefit to people who were new to the mental health system. Some patients did use the information in the leaflet, but this was unusual.
There was concern about the repetitive nature of the letters and that they might appear impersonal. Issues such as how the salutation on the letter was worded, for example first name only or first name and family name (as standard practice in the trusts), could make a difference, but it was clear that different approaches would appeal to different people. The sense of impersonality may have been compounded by the need for us to send an opt-out sheet and reply envelope with each letter. There is clearly a tension between the need for some degree of automation and the inevitable loss of personalisation.
Another indication of the (limited) acceptability of the intervention was the level of opt-out: 23.5% of patients opted out over the intervention period, some after just one or two letters.
Feasibility of a national study of the letter-based intervention
We were able to run the intervention on three different psychiatric inpatient wards across two different mental health trusts. We estimated that it took approximately 48 hours to establish the intervention on a ward, a maximum of 7 hours per week of NHS staff time to deliver the intervention and up to 1 hour of research assistant time per week to respond to issues arising from a ward.
No adverse events arising as a result of us sending the letters were reported, although, as reported in the qualitative interviews, one patient was upset by what he perceived to be the impersonal nature of the salutation used in the letters.
A key issue that became clear to us during the piloting was the high level of readmission (25.5%) in the 12 months following discharge – a figure in keeping with national data indicating that, between April 2004 and March 2005, 24.7% of people discharged from an inpatient psychiatric unit in England were readmitted within 12 months. 164 This raises issues concerning the potential repetitiveness of the cycle of letters in this patient group – if the letters were restarted after the second, third or any subsequent discharge, they may seem less personal. Furthermore, when we compared the overall readmission rates of two of the intervention wards with those for other non-intervention wards in the same hospital we saw no evidence of an intervention-related reduction. In keeping with this, the recent pilot study of a similar letter-/e-mail-based intervention in US military hospitals indicated that those in receipt of the intervention had higher levels of readmission than non-participants (13.6% vs. 7.4%). 166
Eight (10.0%, 95% CI 3.0% to 17.0%) of the participants discharged from the Bristol wards who attended an emergency department following an episode of self-harm after discharge were admitted to a hospital bed. These figures are in keeping with national data: between 1 April 2004 and 31 March 2005, 6.5% of people were admitted to a general hospital bed following a self-harm episode during the 12 months following inpatient psychiatric discharge. 164
The high levels of readmission (25.5%) and opt out (23.5%) meant that only half of those patients who received the first letter received them all. A further 24.7% of discharges were not eligible to receive the letters, mainly because they lived outside the wards' catchment areas. This means that the intervention might be acceptable and deliverable to less than half of all ward discharges.
During the course of the piloting in Bristol, the local mental health trust introduced a policy of visiting patients discharged from inpatient care twice in the week after discharge, thereby potentially diluting any effect of the letter-based intervention.
Based on our analysis of HES data164 indicating that 6% of patients are admitted to hospital after self-harm in the year after discharge from psychiatric inpatient care and an estimated 12% (n = 10,000) present to emergency departments with self-harm, the sample size required to detect a 15% reduction in episodes of non-fatal self-harm in the year after discharge would be about 9800 patients. The sample size would need to be larger (n = 20,800) if only inpatient admissions for self-harm were used as the outcome measure. With MHRN support, a UK trial of this intervention might be feasible, although challenging, to mount.
Feasibility of collecting data to identify the costs of the intervention (an economic evaluation) and outcome data
Collection of data relevant to an economic evaluation of the intervention and outcome data (readmissions/emergency department attendance for self-harm) was straightforward using routine sources.
Conclusions
The study steering group carefully reviewed the findings from all aspects of the pilot study. Although recognising the heightened risk of self-harm in the early weeks after discharge, the group considered that there were insufficient grounds for pursuing the intervention to a full trial. This decision was particularly informed by three findings. First, service changes within mental health trusts (e.g. the increase in number of post-discharge visits in Bristol) and national policy initiatives to reduce post-discharge suicides mean that any impact of the letters is likely to be diluted. Second, less than half of all patients received the full intervention. In particular, about one-quarter of participants opted out of the intervention and qualitative interviews highlighted the potential for people to be upset by various aspects of it, indicating incomplete buy-in amongst the target population. Third, high levels of readmission mean that the intervention may seem repetitive and, together with high levels of opt-out, only half of patients might complete the intervention. Although alterations to the wording of the letters and other approaches to make them more personalised might reduce levels of opt-out and increase their impact, the other concerns outlined above are likely to outweigh any beneficial impact of such changes.
Chapter 9 Discussion
We have successfully completed a programme of research to inform priority areas identified in the National Suicide Prevention Strategy for England. 3 Some of our findings have already been incorporated within drafts of the revised strategy, Preventing Suicide in England – a Cross-Government Outcomes Strategy to Save Lives. 167 Other findings have informed European and UK medicine regulatory activity in relation to co-proxamol and an ONS asessment of the impact of the increasing use of narrative verdicts by coroners on the reliability of national suicide statistics29,168.
Our work on the relative toxicity of different antidepressants has provided important information regarding safe prescribing. We have developed and piloted two interventions aimed at reducing the risk of suicide in high-risk groups: people who have recently self-harmed and people who have recently been discharged from psychiatric units.
We have disseminated our research findings through publications22,37,79,85,169–183 (submitted paper: Hawton K, Simkin S, Yu L-M, Omar O, Gichuru P, Kapur N, et al. Did UK legislation restricting pack sizes of analgesics result in increased gastro-intestinal disorders due to greater use of NSAIDs?), our programme website (www.bris.ac.uk/social-community-medicine/projects/suicide-prevention/) and conference presentations. When relevant, we have passed on our findings to appropriate government organisations including the ONS, the MHRA, the Department of Health and the All-Party Parliamentary Group on Suicide and Self Harm Prevention.
Synergies
There were a number of synergies between various research streams in this programme. We have not explicitly commented on these in the report, as our focus was on presenting key findings in relation to the main research questions. Nevertheless, the synergies between the various elements informed a number of strands of our research, for example:
-
the inclusion of accidental deaths from paracetamol and co-proxamol poisoning within our analysis of mortality was justified by our findings from the study of coroners' records; specifically, that a high proportion of these are likely to be considered suicides by clinicians (see Chapter 2)
-
when we searched coroners' records we investigated whether or not inquests concerning suicides occurring soon after presentation to hospital for self-harm shed light on common service deficiencies; we did not find any novel/generalisable lessons concerning self-harm management within the records
-
likewise, we did not find any useful information in coroners' records concerning sources of paracetamol used in cases of self-poisoning.
Public and patient involvement
The programme benefited from strong public and patient involvement. Appendix 16 lists specific highlights of such involvement. Public and patient involvement can be challenging with regard to some aspects of suicide research, particularly those concerning methods of suicide and the relative lethality of those different methods, as such information may inform later suicide attempts in vulnerable individuals.
Limitations
Although this research programme makes an important contribution to the evidence base relating to the National Suicide Prevention Strategy for England,3 we also recognise that there are a number of priority areas that were beyond the scope of this programme. Alcohol is commonly a factor in suicide and self-harm,184 but was not addressed as an objective of our research. Future research in this area should investigate the aetiology of alcohol use as a risk factor for suicide and self-harm, as well as how services might best deal with the overlap between alcohol misuse and self-harm behaviour. Similarly, although our research involved samples from within the UK, it did not examine suicide or self-harm within minority ethnic groups who have been shown to be at higher risk. Such groups include young South Asian184,185 and black186 women, who are also less likely to seek psychiatric care. 186,187 Research in this area should investigate the components of cuturally appropriate and effective prevention and treatment programmes for these groups.
In this final chapter we discuss each of the key elements of our programme in turn in relation to their implications for health care and suicide prevention and conclude by making recommendations for future research priorities.
National suicide statistics
Objective 6.1 of the National Suicide Prevention Strategy3 was to monitor suicide statistics relevant to the goals and objectives of the strategy. Accurate suicide statistics, recorded in a consistent manner over time, are vital both to inform priority areas for suicide prevention activity and to monitor the success or failure of such suicide prevention initiatives at a local and a national level. Problems with the accuracy of suicide statistics have long been the subject of debate, nationally and internationally, and recent changes to coroners' certification practices in England and Wales have added to these concerns.
We investigated the validity of national suicide mortality statistics through an in-depth analysis of the inquest records of 12 coroners from 1990–1, 1998 and 2005. We used data collected in this investigation, supplemented by a review of coroners' records for 2006 and 2007, to assess the possible underestimation of numbers of suicides from co-proxamol, paracetamol and TCA poisoning. As a result of new information emerging during the course of the programme, we also carried out an analysis of small-area variations in suicide statistics in relation to the use of narrative verdicts by the local coroners.
We found that suicide rates in recent years are likely to have been underestimated because of a growth in the use of narrative verdicts by coroners since 2000. We also found evidence of a small increase in the use of accidental death verdicts for deaths that our researchers deemed as likely suicides, which will also lead to an underestimation of suicide rates. If these trends continue, so too will the underestimation of suicide rates, and trends in suicide rates will be distorted. Coroners differ in their use of narrative and accidental death verdicts for probable (researcher-defined) suicides. Such variation means that differences in suicide trends in different areas of England must be treated with extreme caution. We also found that an assessment of the overall burden of suicide from co-proxamol, paracetamol and TCA poisoning is best achieved by combining deaths from these medicines receiving suicide, open and accidental verdicts.
We have presented our findings to the ONS and the Ministry of Justice and discussed them at the National Suicide Prevention Advisory Group. We have provided the ONS with a document summarising our findings and have ensured that it has received regular updates of our findings and copies of all of our manuscripts. We have presented our findings to a government minister and the All-Party Parliamentary Group on Suicide and Self Harm Prevention. The ONS is reviewing its practices regarding the coding of narrative verdicts and is working with the Coroners' Society of England and Wales to develop an approach to improve the current situation. The importance of this issue has been highlighted in the revised national suicide prevention strategy167 and we propose further monitoring of this issue over the coming years (see Recommendations for future research).
In the course of our work on coroners' statistics, we also became aware of two issues of emerging importance in relation to suicide prevention. First, we found a number of cases of suicide by charcoal burning. This method is highly lethal and has become a major public health concern in East Asia. 188 We have recently published a brief report describing the characteristics of these early cases183 and have obtained funding to develop a surveillance system to help identify (and respond to) the emergence of a similar epidemic in the UK. Second, we have been able to quantify the proportion of cases of suicide in which the internet may have played a role in facilitating the death. 170 We found that there was evidence of a direct internet contribution in nine (1.5%, 95% CI 0.7% to 2.9%) of the 593 suicides in 2005. In seven (77.8%) of the cases, the individuals had used the internet to research the method of suicide that they used. These findings are likely to underestimate the size of the problem and we recommend that this issue is kept under careful review.
The influence of prescribing and availability of analgesics and antidepressants on suicide
Goal 3 of the National Suicide Prevention Strategy for England3 was focused on reducing the availability and lethality of methods used for suicide. Objective 3.2 targeted self-poisoning suicide cases. Drugs commonly used for fatal self-poisoning include paracetamol, co-proxamol and antidepressants.
Paracetamol
The 1998 UK legislation57 to restrict pack sizes of paracetamol appears to have had significant beneficial effects on both deaths and registrations for liver transplantation. In spite of these apparent benefits, there continues to be a considerable number of deaths each year from paracetamol poisoning, averaging 121 per year (for suicide, open and accidental verdicts) between 2000 and 2009 for paracetamol alone with or without alcohol, excluding compounds. The benefits should therefore not lead to complacency. Further measures may be required to limit this death toll. These might include stronger enforcement of the legislation, although we found few breaches of the sales guidance. Another possibility is for pack sizes to be reduced further. Lower pack sizes have been introduced in some other countries (e.g. Ireland77 and Germany44). Although the findings from our Anglo-Irish study did not suggest that smaller pack sizes of paracetamol in Ireland have resulted in smaller overdoses than in England, there may be several reasons for this. For example, in Ireland, more often than in England, it appears that the numbers of tablets taken are equivalent to multiples of packs. This raises the question of whether or not this practice reflects differences in patients' characteristics and access to care and greater ease of purchasing of multiple packs in Ireland than in England. The findings therefore do not provide definitive information on whether or not a further reduction in the maximum pack sizes for paracetamol sold over the counter in the UK would have further beneficial effects on overdose size (and hence on deaths from paracetamol overdose). The current pharmacy upper limit pack size of 32 tablets includes sufficient paracetamol that if all of it is ingested in an overdose the risk of hepatotoxicity is rather high. 54
Our patient interview study identified media influences (including the internet) in some cases. Media producers should be encouraged to comply with guidelines concerning detailed descriptions of suicide methods. 90 Internet influences on self-harm and suicide are increasingly recognised, including proliferation of sites giving details of drugs that may be used for fatal self-poisoning. 189,190 This requires careful monitoring and, when feasible, possible restriction of those that are considered dangerous.
Another possible measure to limit the dangers of paracetamol overdose would be to reduce the amount of paracetamol in each tablet (e.g. to 325 mg, as has recently been instigated by the US FDA for paracetamol in compound preparations191), especially as lower-dose and 500-mg tablet preparations have been shown to have equivalent pain-relieving efficacy. 192
Fortunately, although we have shown that prescribing of analgesics has risen since the 1998 legislation, increased prescribing of NSAIDs does not appear to have had deleterious effects in terms of GI disturbances, although greater prescribing of antiulcerants could have offset any negative effects on GI function. This study, however, illustrates the importance of widening the evaluation of measures aimed at limiting the availability of specific medications so that any deleterious effects that result from changes in the availability of alternative medications can be detected.
Co-proxamol
In 2003, a report highlighted that co-proxamol was used in 20% of poisoning suicides in England and Wales and that co-proxamol was far more toxic than TCAs in overdose. 101 Consequently, the MHRA reviewed its relative benefit/safety profile and in January 2005 recommended to the CSM that co-proxamol be withdrawn, with a 3-year initial partial withdrawal period. 106 We have shown that during both this period and the subsequent 3 years, as prescribing of co-proxamol declined and there was an increase in prescribing of some other analgesics, there was a net reduction in analgesic poisoning deaths. 79,175 By the end of the 6-year period following the withdrawal of co-proxamol, there had been an estimated 500 fewer suicides involving co-proxamol alone, and 600 when accidental deaths were included, with no evidence of significant substitution by death involving other analgesics. 175
Our findings were communicated to the MHRA both after the evaluation of the first 3 years following its decision and at the end of the 6 years following withdrawal of co-proxamol. They were also presented to the European Medicines Agency and influenced its decision to recommend to the European Union that prescribing of dextropropoxyphene (the more dangerous component of co-proxamol) cease. 114 Prescribing of dextropropoxyphene has now been banned in the USA and Canada.
The UK initiative appears to have been a very successful suicide prevention measure. Our findings are consistent with other evidence which indicates that reducing the availability of a common and particularly dangerous method of suicide can reduce the number of suicides by that method and does not necessarily lead to substitution by an increase in numbers of suicides by similar methods. 11 However, such initiatives require careful long-term evaluation, especially as new methods of suicide become more popular and available.
Antidepressants
Another way of restricting access to dangerous means of self-poisoning is through prescribing less toxic drugs to people at risk. Depression is the most common psychiatric disorder in people dying by suicide, with approximately 60% of those who die suffering from affective disorder. 118 Affective disorders are also common in patients who engage in non-fatal self-harm, with 72% having such disorders in one UK study. 193 People with depression who engage in suicidal acts often take antidepressants in overdose and therefore considerable attention has been paid to their toxicity, especially that of the TCAs. 45 It is well known that people often take their prescribed medication in overdose. 194 Choice of antidepressant in someone at risk should be determined by effectiveness, side effects and toxicity.
The usual approach to assessing fatal toxicity of a prescribed drug is to compare number of deaths involving that drug with the extent to which it is prescribed. 146 We have employed both this and another less used measure, case fatality, in which the death rate is compared with the rate of non-fatal overdoses,45,159 to assess the relative toxicity of all of the antidepressants in common current use. Importantly, we showed that the results obtained with the relative toxicity and case fatality approaches were practically identical.
Although we have confirmed the well-known higher toxicity of TCAs relative to SSRIs, we have highlighted important differences within these categories. Thus, among the TCAs, both dosulepin and doxepin were found to be considerably more toxic than amitriptyline. The elevated toxicity of dosulepin has previously been recognised,143 but our results, which we communicated to the MHRA, highlight the need for stronger advice to be given to clinicians, especially as dosulepin is still prescribed widely in some parts of the UK. 159 Although doxepin is less often prescribed than dosulepin, clinicians should be aware of its relatively high level of toxicity.
Selective serotonin reuptake inhibitors are well recognised as being safer than the TCAs, but we have shown that citalopram is approximately three times more toxic than the other SSRIs. It is important that clinicians are also aware of this finding, which is supported by other research,129,130 as it is again relevant to prescribing decisions, especially in patients at risk of self-poisoning.
Lastly, although our finding that the toxicity of venlafaxine is intermediate between that of the TCAs and that of the SSRIs has been recognised before and resulted in advice from the MHRA about restricting pack sizes and initial supplies for patients,128 the similar toxicity of mirtazapine is a new finding. This result has also been communicated to the MHRA.
Self-harm services and suicide prevention
Objective 1.2 of the National Suicide Prevention Strategy for England3 was to reduce the number of suicides in the year following self-harm. Despite the strong association between self-harm and suicide, service provision for self-harm in the UK has been extremely variable.
We carried out interviews with key staff and 3-month audit projects in 32 centres in England to investigate this variability, but also to examine how management in hospital was related to outcome. We found that the variability of services was as wide as ever (with a 3.5-fold difference between hospitals in the proportion of individuals who received a specialist assessment and a fivefold difference in the proportion of individuals receiving specialist follow-up). Overall, 4 out of 10 individuals left hospital without having had an assessment with a mental health specialist. There was little evidence that aspects of management were associated with outcome in an ecological analysis, but an individual-level analysis suggested that specialist psychosocial assessment might be associated with a reduced risk of repetition of self-harm. Comparing our data with that from approximately 10 years earlier, we disappointingly found that the levels of specialist assessment had remained static. However, scores on a self-reported service quality scale increased by 26%, suggesting that at least some aspects of care may have improved.
Our findings suggest that national guidelines and policy initiatives have had a limited impact on the variability of self-harm service provision, although service quality may have improved. The effect of this on outcomes is unclear. New guidelines have included an additional focus on implementation,139 which may have a positive effect on the quality of services and patient outcomes in the future.
Preventing suicide in high-risk groups
Goal 1 of the National Suicide Prevention Strategy for England3 was to reduce suicide risk in key high-risk groups. Two groups highlighted were people who have recently self-harmed and those currently or recently in contact with mental health services.
For individuals who have self-harmed, the findings of trials assessing the effect of telephone or postal contact have been equivocal. We developed an intervention for this group of patients, again using qualitative methods. The final intervention consisted of an information leaflet listing local sources of help, two telephone calls soon after presentation to an emergency department and a series of letters expressing concern, sent over a 12-month period. We then carried out a pilot randomised controlled trial of the intervention compared with usual treatment to assess feasibility and to carry out a preliminary investigation of efficacy for reducing repeat self-harm. This pilot trial proved challenging to carry out (with a proportion of individuals being uncontactable and others refusing to participate) but suggested that the methodology was feasible. Paradoxically, the incidence of repetition was higher in the intervention group than in the usual treatment group (34% vs. 12.5%), which may have partly reflected an unequal distribution of baseline risk factors between groups, our selected sample, the study setting or better engagement with services by those receiving the intervention. However, we cannot rule out the possibility that the intervention was associated with a true increase in the risk of repetition. Future studies of these apparently simple contact interventions need to be alert to this possibility.
Our findings with respect to repeat self-harm are interesting and should be used to inform further research rather than as a basis for a decision not to proceed to definitive trials. However, it is our view that moving immediately to a large multicentre trial of the current intervention before undertaking further development work is premature. Equally, further work is clearly needed before contact interventions more generally can be considered for incorporation into routine clinical services.
For people in contact with mental health services, we developed and piloted a contact-based intervention (a series of supportive letters and information leaflets) based on Jerome Motto's intervention trialled successfully in the USA in the 1960s and 1970s. 23 After a questionnaire survey and exploratory interviews with service users and consultation with mental health service staff, we modified Motto's intervention to suit present-day UK clinical practice. We also developed an approach to automate the implementation of the intervention to facilitate its roll-out into mainstream practice if trial evidence supported this move.
We found that the intervention was relatively straightforward to operationalise, taking at most 7 hours per week on the three wards on which it was piloted. However, mainly because of patient opt-out and readmission, only 45 (44.1%) of the 102 patients recruited received the full series of letters. In the context of policy changes in the UK since we developed our original proposal – with more intensive post-discharge follow-up – qualitative interviews with service users showed that most already felt adequately supported and the intervention added little to this. Those interviewed felt that it was possible that the intervention might benefit people new to, or with little follow-up from, mental health services but that fewer letters should be mailed. For these reasons we did not feel that there was sufficient evidence to proceed to a full trial of this intervention.
In a parallel analysis of HES data and data collected by the National Confidential Inquiry, we have found some evidence that recent policy changes (enhanced post-discharge follow-up of people discharged from psychiatric wards) have reduced the risk of non-fatal self-harm in this period. 172 A longer-term analysis of this issue might help to clarify the impact of policy changes on suicide.
Implications and recommendations
This programme of research has a number of findings that have important implications for public health and clinical practice as well as for future research relevant to suicide prevention.
Implications for practice and research
-
Small-area (primary care trusts/LAs) suicide rates and changes in these rates over time since 2000 should be interpreted with caution in those areas where coroners make high use of narrative verdicts.
-
Further increases in the use of narrative verdicts will compromise the quality of national suicide statistics.
-
Coroners could be required to provide both the short-form verdict and a longer narrative account of the death (when appropriate).
-
The ONS might consider including in its suicide statistics deaths from medicine poisoning given a verdict of accident/misadventure by coroners.
-
The Department of Health might consider carrying out surveillance to enable the early identification of increases in the use of high-lethality, easily accessible suicide methods, to enable a timely response.
-
Estimates of the numbers of suicides by co-proxamol, paracetamol and TCA poisoning would be more reliable if they included accidental poisonings from these drugs as well as deaths given suicide and open verdicts by coroners.
-
There should be an in-depth analysis of the proportion of suicides in which the internet may have played a contributory role, assessed alongside evidence of the beneficial effects on mental health and suicide risk.
Implications for clinical practice
-
Services should ensure optimal treatment for those who self-harm, in particular, prioritising the provision of psychosocial assessment as emphasised in national guidelines.
-
When prescribing antidepressants, clinicians should take account of the risk of overdose, especially in patients at risk of self-poisoning, as well as their relative efficacy, acceptability and possible interactions with other medication and alcohol, and patients' concurrent physical morbidity.
-
To prevent ongoing deaths involving paracetamol, further measures might be aimed at reducing breaches of sales guidelines and at encouraging media and internet site producers to follow guidelines on the reporting of suicide.
-
National, multicentre research would benefit from a simplified system of centralised approval for local research governance permissions.
-
Despite their low cost and apparent simplicity, contact-type interventions following psychiatric hospital discharge or self-harm cannot be recommended for widespread introduction.
Recommendations for future research
-
Variability in self-harm services should continue to be monitored to gain a greater understanding of aspects of treatment that are beneficial for preventing repeat self-harm.
-
Further work is needed to elucidate the active components of therapeutic contact following self-harm and to understand in which groups treatments might have the most impact.
-
Trends in the use of narrative verdicts and their impact on national and small-area suicide rates should be reassessed following recent ONS-led interventions to improve the accuracy of suicide reporting.
-
An assessment should be carried out of the feasibility and costs of developing a surveillance system to identify as quickly as possible rises in the use of novel methods of suicide to enable rapid interventions to restrict ease of availability to at-risk individuals.
-
The relative toxicity of other drugs commonly used for intentional self-poisoning should be evaluated to assist clinicians in making prescribing decisions and for informing regulatory agencies.
-
Future changes in availability of medications that are used for self-poisoning should be evaluated in terms of both impacts on self-harm and suicide and indirect consequences because of altered availability of other drugs.
-
The effect on the quality of services and patient outcomes of new guidance and future policies on management of self-harm (such as the November 2011 NICE guidelines139 on the longer-term management of self-harm) requires careful evaluation.
-
Assessment of the relative toxicity of antidepressants should continue as new antidepressants are marketed, and international comparisons are warranted in view of the differences in prescribing practices between countries.
Acknowledgements
The views and opinions expressed in this paper are those of the authors and do not necessarily reflect those of the National Institute for Health Research (NIHR), the NHS or the Department of Health. The NIHR and Department of Health had no role in study design, the collection, analysis and interpretation of data, the writing of the report and the decision to submit the paper for publication.
Avon and Wiltshire Mental Health Partnership NHS Trust hosted the research programme.
Keith Hawton, David Gunnell and Jenny Donovan are NIHR Senior Investigators. Keith Hawton is also supported by Oxford Health NHS Foundation Trust and Nav Kapur by the Manchester Mental Health and Social Care Trust.
We would like to thank the following people for their invaluable help with undertaking components of this programme of work.
Study to investigate the influence of changes in coroners' practices on the validity of national suicide rates in England
We thank the coroners who allowed us access to their files, their staff and Record Office staff who assisted us, and the following researchers: Robert Carroll, Dr Emily Klineberg, Cathryn Rodway, Sarah Steeg and Lesley Sutton.
Oxford-based study of toxicity of antidepressants
Dr Helen Bergen and Keith Waters.
Oxford-based evaluation of co-proxamol withdrawal
Dr Helen Bergen, Anita Brock, Clare Griffiths, Ester Romeri, Claudia Wells, Karen Smith of the Centre for Statistics in Medicine, Oxford, for statistical advice, the Contact Centre Team at the NHS Health and Social Care Information Centre (England) and Sandra Hennefer at the Prescribing Services Partneriaeth Cydwasanaethau GIG Cymru (Wales) for supplying the prescription data.
Oxford-based evaluation of the 1998 UK legislation restricting pack sizes of analgesics
Long-term evaluation
Dr Helen Bergen, Dr Sue Dodd, Dr Phil Pocock, Dr William Bernal and Claudia Wells.
Interview study
Fiona Brand, Sheryl Denman Taylor, Karen Lascelles, Jacklyn Patzsanda, John Ryall, Dr Kate Saunders and Linda Whitehead for their help in identifying patients for the study and conducting some of the interviews; Dorothy Rutherford for assistance in extracting data from the Oxford Monitoring System for Attempted Suicide; and Dr Helen Bergen and Deborah Casey for support and advice on analyses.
Anglo-Irish comparison
Dr Helen Bergen, Dr Ella Arensman, Dr Paul Corcoran and Keith Waters.
Non-steroidal anti-inflammatory drug prescribing and gastrointestinal consequences
Ly-Mee Yu, Omar Omar, Phillip Gichuru, Peter Stephens of IMS Health for organising the provision of prescription data and Dr Ben Wheeler for providing data on trends in hospital admissions for gastrointestinal haemorrhage in England.
Variation in self-harm services study
Dr Matthew Lowe, Iain Donaldson, Rita Jordan, Kelly Wild and clinical studies officers and research staff from the Mental Health Research Network and Comprehensive Local Research Networks.
Manchester-based self-harm intervention study
Dr Sarmad Nadeem, Dr Samer Khalil, Dr Cheryl Hunter, Dr Amanda Owen-Smith, Iain Donaldson, Victoria Matthews, Sarah Steeg, Rita Jordan and Clive Turpin (Self-harm Assessment, Follow-up, Engagement; SAFE team), and Professor Kevin Mackway-Jones.
Bristol-based pilot study of an intervention to prevent post-discharge suicide
Jerome Motto for information on the content of the letters sent to participants in his contact-based study that contributed to the development of our study; staff on the intervention wards and from the Mental Health Research Network for their assistance in administering the mailing of the letters, in particular Davina Chauhan, Nicola Cook and Genevieve Riley who collected data on patient participation and retention and outcome data on community contacts; staff in the Avon and Wiltshire Partnership NHS Trust Information Department for providing anonymised outcome data on admissions and readmissions; and steering group members and researchers Rosie Davies, Dr Sarah Greef, Keith Hall, Davidson Ho, Stephen Hoddell (Samaritans), Dr Will Hollingworth, Dr Amanda Owen-Smith and Dr Sangeetha Paramasivan.
Contribution of authors
Professor David Gunnell (Professor of Epidemiology) was co-principal investigator on the programme grant, led the Bristol-based components of the research (coroner study and Bristol-based intervention pilot study) and contributed methodological and practical advice to all other components of the research programme and publications arising from the research.
Professor Keith Hawton (Professor of Psychiatry) was co-principal investigator on the Programme Grant, led the Oxford-based components of the research (pharmacoepidemiological studies) and contributed methodological and practical advice to all other components of the research programme and publications arising from the research.
Professor Nav Kapur (Professor of Psychiatry and Population Health) was co-principal investigator on the Programme Grant, led the Manchester-based components of the research (the self-harm intervention study and variations in self-harm services) and contributed methodological and practical advice to all other components of the research programme and publications arising from the research.
Olive Bennewith (Research Associate) was the lead Bristol-based researcher. She convened research meetings and developed and implemented research protocols for the Bristol-based intervention pilot study of an intervention to reduce self-harm following hospital discharge and the study of coroners' records. She analysed quantitative data arising from these projects and wrote first drafts of the reports of these studies. She also assisted with data collection from a number of centres in the Manchester-led study of self-harm services.
Dr Jayne Cooper (Senior Research Fellow) was the lead Manchester-based researcher and had key roles in the design, writing and implementation of research protocols for the Manchester-based contact intervention for self-harm and the multisite national observational study of self-harm services. She analysed qualitative and quantitative data arising from these projects and contributed to writing the reports of these studies. She also assisted with the study of coroners' records and supervision of junior staff.
Sue Simkin (Research Associate) was the lead Oxford-based researcher. She contributed to the design of the interview study of patients who took large paracetamol overdoses, conducted most of the interviews, analysed the data and wrote the first draft of the paper. She contributed to all of the other Oxford-led studies, including to their design, data collection and writing of papers for publication. She also assisted with data collection for the Bristol-led coroner study and wrote the first draft of an editorial on use of coroners' records for research.
Dr Damien Longson (Consultant in Psychiatry) was a co-applicant on the research programme and provided clinical and self-harm research expertise to the Manchester-based self-harm intervention study, as well as helping to oversee and facilitate recruitment and data collection by clinical teams.
Jenny Donovan (Professor of Social Medicine) was a co-applicant on the research programme and contributed qualitative research expertise and expertise in clinical trial design to the self-harm intervention pilot studies in Bristol and Manchester and supervised qualitative researchers working on these studies.
Jonathan Evans (Senior Lecturer in Psychiatry) was a co-applicant on the research programme and provided clinical and self-harm research expertise to the steering group of the Bristol-based intervention pilot study of an intervention to reduce self-harm following hospital discharge.
Susan O'Connor (Consultant Psychiatrist and former Medical Director of the Avon and Wiltshire Partnership NHS Trust) was a co-applicant on the research programme, provided clinical and self-harm research expertise to the steering group of the Bristol-based intervention pilot study of an intervention to reduce self-harm following hospital discharge and helped engage local wards in participating in the research pilot.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health.
Peer-reviewed publications arising from the research programme
Chen YY, Bennewith O, Hawton K, Simkin S, Cooper J, kapur N, et al. Suicide by burning barbecue charcoal in England. J Public Health 2013;35:223–7.
Gunnell D, Hawton K, Ho D, Evans J, O'Connor S, Potokar J, et al. Hospital admissions for self-harm following psychiatric hospital discharge: cohort study. BMJ 2008;337:1331–4.
Hawton K, Bergen H, Simkin S, Cooper J, Waters K, Gunnell D, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry 2010;196:354–8.
Kapur N, Clements C, Bateman N, Foëx B, Mackway-Jones K, Huxtable R, et al. Advance directives and suicidal behaviour. BMJ 2010;341:590–1.
Kapur N, Cooper J, Bennewith O, Gunnell D, Hawton K. Postcards, green cards, and telephone calls: therapeutic contact with individuals following self-harm. Br J Psychiatry 2010;197:5–7.
Carroll R, Hawton K, Kapur N, Bennewith O, Gunnell D. Impact of the growing use of narrative verdicts by coroners on geographic variations in suicide: analysis of coroners' inquest data [published online ahead of print 15 November 2011]. J Public Health 2011. http://dx.doi.org/10.1093/pubmed/fdr091.
Cooper J, Hunter C, Owen-Smith A, Gunnell D, Donovan J, Hawton K, et al. ‘Well it’s like someone at the other end cares about you'. A qualitative study exploring the views of users and providers of care of contact-based interventions following self-harm. Gen Hosp Psychiatry 2011;33:166–76.
Hawton K, Bergen H, Simkin S, Arensman E, Corcoran P, Cooper J, et al. Impact of different pack sizes of paracetamol in the United Kingdom and Ireland on intentional overdoses: a comparative study. BMC Public Health 2011;11:460.
Hawton K, Bergen H, Waters K, Murphy E, Cooper J, Kapur N. Impact of withdrawal of the analgesic co-proxamol in the UK on non-fatal self-poisoning. Crisis 2011;32:81–7.
Gunnell D, Bennewith O, Kapur N, Simkin S, Cooper J, Hawton K. The use of the Internet by people who die by suicide in England: a cross sectional study. J Affect Disord 2012;141:480–3.
Gunnell D, Metcalfe C, While D, Hawton K, Ho D, Appleby L, et al. Impact of national policy initiatives on fatal and non-fatal self-harm after psychiatric hospital discharge: a time series analysis. Br J Psychiatry 2012;201:233–8.
Hawton K, Bergen H, Simkin S, Wells C, Kapur N, Gunnell D. Six-year follow-up of impact of co-proxamol withdrawal in England and Wales on prescribing and deaths: time-series study. PLoS Med 2012;9:e1001213.
Simkin S, Bennewith O, Cooper J. Investigating official records of suicides for research purposes: challenges and coping strategies. Crisis 2012;33:123–6.
Simkin S, Hawton K, Kapur N, Gunnell D. What can be done to reduce mortality from paracetamol overdoses? A patient interview study. Q J Med 2012;105:41–51.
Hawton K, Bergen H, Simkin S, Dodd S, Pocock P, Bernal W, et al. Reduced pack sizes of paracetamol: long-term evaluation of impacts on poisoning deaths and liver transplant activity in England and Wales. BMJ 2013;346:f403.
Bennewith O, Evans J, Donovan J, Paramasivan S, Owen-Smith A, Hollingworth W, et al. A contact-based intervention for people recently discharged from inpatient psychiatric care: a pilot study. 2013; in press.
Owen-Smith A, Bennewith O, Donovan J, Evans J, Hawton K, Kapur N, et al. ‘When you’re in the hospital, you're in a sort of bubble'. Understanding the high risk of self-harm and suicide following psychiatric discharge: qualitative study. Crisis 2013; in press.
Hawton K, Bergen H, Simkin S, Brock A, Griffiths C, Romeri E, et al. Effect of withdrawal of co-proxamol on prescribing and deaths from drug poisoning in England and Wales: time series analysis. BMJ 2009;338:b2270. http://dx.doi.org/10.1136/bmj.b2270
Kapur N, Gunnell D, Hawton K, Nadeem S, Khalil S, Longson D, J, et al. Messages from Manchester: pilot randomised controlled trial following self-harm. Br J Psychiatry 2013;203:73–4. doi: 10.1192/bjp.bp.113.126425.
References
- Hawton K, Bergen H, Casey D, Simkin S, Palmer B, Cooper J, et al. Self-harm in England: a tale of three cities. Multicentre study of self-harm. Soc Psychiatry Psychiatr Epidemiol 2007;42:513-21. http://dx.doi.org/10.1007/s00127-007-0199-7.
- Gunnell D. The epidemiology of suicide. Int Rev Psychiatry 2000;12:21-6. http://dx.doi.org/10.1080/09540260074076.
- National suicide prevention strategy for England. London: Department of Health; 2002.
- Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, et al. Suicide prevention strategies. A systematic review. JAMA 2005;294:2064-74. http://dx.doi.org/10.1001/jama.294.16.2064.
- Gunnell D, Frankel S. Prevention of suicide: aspirations and evidence. BMJ 1994;308:1227-33.
- Hawton K, Van Heeringen K. Suicide. Lancet 2009;373:1372-81. http://dx.doi.org/10.1136/bmj.308.6938.1227.
- Gunnell D, Lewis G. Studying suicide from the life course perspective: implications for prevention. Br J Psychiatry 2005;187:206-8. http://dx.doi.org/10.1192/bjp.187.3.206.
- Taylor SJ, Kingdon D, Jenkins R. How are the nations trying to prevent suicide? An analysis of national suicide prevention strategies. Acta Psychiatr Scand 1997;95:457-63. http://dx.doi.org/10.1111/j.1600-0447.1997.tb10132.x.
- Office for National Statistics . Deaths related to drug poisoning in England and Wales, 2002–06. Health Stat Q 2007;36:66-72.
- Gunnell D, Hawton K, Kapur N. Coroners' verdicts and suicide statistics: increasing use of narrative verdicts raises serious concerns. BMJ 2011;343.
- Hawton K, Hawton K. Prevention and treatment of suicidal behaviour: from science to practice. Oxford: Oxford University Press; 2005.
- Hawton K, Simkin S, Deeks J, Cooper J, Johnston A, Waters K, et al. UK legislation on analgesic packs: before and after study of long term effect on poisonings. BMJ 2004;329:1076-9. http://dx.doi.org/10.1136/bmj.38253.572581.7C.
- Self-harm: the short-term physical and psychological management and secondary prevention of self-harm in primary and secondary care. London: National Institute for Clinical Excellence; 2004.
- Kapur N, House A, Creed F, Feldman E, Friedman T, Guthrie E. Management of deliberate self poisoning in adults in four teaching hospitals: descriptive study. BMJ 1998;316:831-2. http://dx.doi.org/10.1136/bmj.316.7134.831.
- Bennewith O, Gunnell D, Peters TJ, Hawton K, House A. Variations in the hospital management of self-harm in adults in England: observational study. BMJ 2004;328:1108-9. http://dx.doi.org/10.1136/bmj.328.7448.1108.
- Crawford MJ, Wessely S. Does initial management affect the rate of repetition of deliberate self harm? Cohort study. BMJ 1998;317:985-90. http://dx.doi.org/10.1136/bmj.317.7164.985.
- Hickey L, Hawton K, Fagg J, Weitzel H. Deliberate self-harm patients who leave the accident and emergency department without a psychiatric assessment. A neglected population at risk of suicide. J Psychosom Res 2001;50:87-93.
- Kapur N, House A, May C, Creed F. Service provision and outcome for deliberate self-poisoning in adults – results from a six centre descriptive study. Soc Psychiatry Psychiatr Epidemiol 2003;38:390-5.
- Pirkis J, Burgess P. Suicide and recency of health care contacts. A systematic review. Br J Psychiatry 1998;173:462-74. http://dx.doi.org/10.1192/bjp.173.6.462.
- Appleby L, Shaw J, Kapur N, Windfuhr K, Ashton A, Swinson N, et al. Avoidable deaths: five year report of the national confidential inquiry into suicide and homicide by people with mental illness. Manchester: University of Manchester; 2006.
- Hawton K, Arensman E, Townsend E, Bremner S, Feldman E, Goldney R, et al. Deliberate self-harm: systematic review of efficacy of psychosocial and pharmacological treatments in preventing repetition. BMJ 1998;317:441-7. http://dx.doi.org/10.1136/bmj.317.7156.441.
- Kapur N, Cooper J, Bennewith O, Gunnell D, Hawton K. Postcards, green cards, and telephone calls: therapeutic contact with individuals following self-harm. Br J Psychiatry 2010;197:5-7. http://dx.doi.org/10.1192/bjp.bp.109.072496.
- Motto JA. Suicide prevention for high-risk persons who refuse treatment. Suicide Life Threat Behav 1976;6:223-30.
- Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv 2001;52:828-33. http://dx.doi.org/10.1176/appi.ps.52.6.828.
- Hawton K, Harriss L, Hall S, Simkin S, Bale E, Bond A. Deliberate self-harm in Oxford, 1990–2000: a time of change in patient characteristics. Psychol Med 2003;33:987-96.
- Cooper P, Milroy C. The coroners' system and under-reporting of suicide. Med Sci Law 1995;35:319-26.
- O’Donnell I, Farmer R. The limitations of official suicide statistics. Br J Psychiatry 1995;166:458-61. http://dx.doi.org/10.1192/bjp.166.4.458.
- Linsley KR, Schapira K, Kelly TP. Open verdict v. suicide – importance to research. Br J Psychiatry 2001;178:465-8. http://dx.doi.org/10.1192/bjp.178.5.465.
- Hill C, Cook L. Narrative verdicts and their impact on mortality statistics in England and Wales. Health Stat Q 2011;49:81-100. http://dx.doi.org/10.1057/hsq.2011.4.
- Bennewith O, Gunnell D, Nowers M. The effect of the barriers on the Clifton Suspension Bridge, England on local patterns of suicide. Br J Psychiatry 2007;190:266-7. http://dx.doi.org/10.1192/bjp.bp.106.027136.
- Holding T, Barraclough B. Undetermined deaths – suicide or accident?. Br J Psychiatry 1978;133:542-9. http://dx.doi.org/10.1192/bjp.133.6.542.
- Adelstein A, Mardon C. Suicides 1961–74. Popul Trends 1975;2:13-8.
- De Leo D, Dudley MJ, Aebersold CJ, Mendoza JA, Barnes MA, Harrison JE, et al. Achieving standardised reporting of suicide in Australia: rationale and program for change. Med J Aust 2010;192:452-6.
- Page A, Taylor R, Martin G. Recent declines in Australian male suicide are real, not artefactual. Aust N Z J Psychiatry 2010;44:358-63. http://dx.doi.org/10.3109/00048670903489874.
- Nicholson S. Suicide in North Devon: epidemic or problem of classification?. Health Trends 1992;24:95-6.
- Saunderson T, Haynes R, Langford IH. Urban–rural variations in suicides and undetermined deaths in England and Wales. J Public Health Med 1998;20:261-7. http://dx.doi.org/10.1093/oxfordjournals.pubmed.a024767.
- Carroll R, Hawton K, Kapur N, Bennewith O, Gunnell D. Impact of the growing use of narrative verdicts by coroners on geographic variations in suicide: analysis of coroners' inquest data. J Public Health 2011. http://dx.doi.org/10.1093/pubmed/fdr091.
- Ministry of Justice . Coroners Statistics – England and Wales, 2006 n.d. www.dca.gov.uk/statistics/cb2006full2.pdf (accessed December 2010).
- Platt S, Backett S, Kreitman N. Social construction or causal ascription: distinguishing suicide from undetermined deaths. Soc Psychiatry Psychiatr Epidemiol 1988;23:217-21. http://dx.doi.org/10.1007/BF01787820.
- Ministry of Justice . Coroners Statistics – England and Wales, 2009 n.d. www.justice.gov.uk/statistics/coroners-and-burials/deaths (accessed December 2010).
- The Information Centre . National Compendium of Clinical and Health Indicators n.d. www.nchod.nhs.uk (accessed June 2011).
- Thomas K, Gunnell D. Suicide in England and Wales 1861 to 2007: a time-trends analysis. Int J Epidemiol 2010;39:1464-75. http://dx.doi.org/10.1093/ije/dyq094.
- Pounder D. Classifying suicide. BMJ 1992;305. http://dx.doi.org/10.1136/bmj.305.6851.472.
- Kapusta N, Tran U, Rockett I, De Leo D, Naylor C, Niederkrotenthaler T, et al. Declining autopsy rates and suicide misclassification: a cross-national analysis of 35 countries. Arch Gen Psychiatry 2011;68:1050-7. http://dx.doi.org/10.1001/archgenpsychiatry.2011.66.
- Tollefsen I, Hem E, Ekeberg O. The reliability of suicide statistics: a systematic review. BMC Psychiatry 2012;12. http://dx.doi.org/10.1186/1471-244X-12-9.
- Prescott K, Stratton R, Freyer A, Hall I, Le Jeune I. Detailed analyses of self-poisoning episodes presenting to a large regional teaching hospital in the UK. Br J Clin Pharmacol 2009;68:260-8. http://dx.doi.org/10.1111/j.1365-2125.2009.03458.x.
- Gunnell D, Murray V, Hawton K. Use of paracetamol (acetaminophen) for suicide and non-fatal poisoning: world-wide patterns of use and misuse. Suicide Life Threat Behav 2000;30:313-20.
- Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, et al. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology 2005;42:1364-72. http://dx.doi.org/10.1002/hep.20948.
- Nourjah P, Ahmad SR, Karwoski C, Willy M. Estimates of acetaminophen (paracetamol)-associated overdoses in the United States. Pharmacoepidemiol Drug Saf 2006;15:398-405.
- Daly FFS, Fountain JS, Murray L, Graudins A, Buckley NA. Guidelines for the management of paracetamol poisoning in Australia and New Zealand – explanation and elaboration. Med J Aust 2008;188:296-301.
- Wei G, Bergquist A, Broomé U, Lindgren S, Wallerstedt S, Almer S, et al. Acute liver failure in Sweden: etiology and outcome. J Intern Med 2007;262:393-401. http://dx.doi.org/10.1111/j.1365-2796.2007.01818.x.
- Canbay A, Jochum C, Bechmann LP, Festag S, Gieseler RK, Yüksel Z, et al. Acute liver failure in a metropolitan area in Germany: a retrospective study (2002–2008). Z Gastroenterol 2009;47:807-13. http://dx.doi.org/10.1055/s-0028-1109058.
- National registry of deliberate self harm annual report 2009. Cork, Ireland: National Suicide Research Foundation; 2010.
- Prescott LF. Paracetamol overdosage: pharmacological considerations and clinical management. Drugs 1983;25:290-314. http://dx.doi.org/10.2165/00003495-198325030-00002.
- British national formulary. London: BMA and RPS; 2010.
- Committee on Safety of Medicines . Paracetamol and aspirin. Curr Prob Pharmacovigilance 1997;23.
- The Medicines (Sales or Supply) (Miscellaneous Provisions) Amendment (No 2) Regulations 1997. London: The Stationery Office; 1997.
- Medicines and Healthcare products Regulatory Agency . Best Practice on the Sale of Medicines for Pain Relief n.d. www.mhra.gov.uk/home/idcplg?IdcService=GET_FILE&dDocName=CON065560&RevisionSelectionMethod=Latest (accessed December 2009).
- Bialas MC, Reid PG, Beck P, Lazarus JH, Smith PM, Scorer RC, et al. Changing patterns of self-poisoning in a UK health district. QJM 1996;89:893-901. http://dx.doi.org/10.1093/qjmed/89.12.893.
- Hawton K, Fagg J, Simkin S, Bale E, Bond A. Trends in deliberate self-harm in Oxford, 1985–1995. Implications for clinical services and the prevention of suicide. Br J Psychiatry 1997;171:556-60. http://dx.doi.org/10.1192/bjp.171.6.556.
- Gunnell D, Hawton K, Murray V, Garnier R, Bismuth C, Fagg J, et al. Use of paracetamol for suicide and non-fatal poisoning in the UK and France: are restrictions on availability justified?. J Epidemiol Community Health 1997;51:175-9. http://dx.doi.org/10.1136/jech.51.2.175.
- Bray GP. Liver failure induced by paracetamol: avoidable deaths still occur. BMJ 1993;306:157-8.
- Bernal W. Changing patterns of causation and the use of transplantation in the United Kingdom. Semin Liver Dis 2003;23:227-37.
- Hawton K, Ware C, Mistry H, Hewitt J, Kingsbury S, Roberts D, et al. Why patients choose paracetamol for self poisoning and their knowledge of its dangers. BMJ 1995;310. http://dx.doi.org/10.1136/bmj.310.6973.164.
- Hawton K, Ware C, Mistry H, Hewitt J, Kingsbury S, Roberts D, et al. Paracetamol self-poisoning. Characteristics, prevention and harm reduction. Br J Psychiatry 1996;168:43-8. http://dx.doi.org/10.1192/bjp.168.1.43.
- Hawton K, Townsend E, Deeks JJ, Appleby L, Gunnell D, Bennewith O, et al. Effects of legislation restricting pack sizes of paracetamol and salicylates on self poisoning in the United Kingdom: before and after study. BMJ 2001;322:1203-7. http://dx.doi.org/10.1136/bmj.322.7296.1203.
- Prince MI, Thomas SHL, James OFW, Hudson M. Reduction in incidence of severe paracetamol poisoning. Lancet 2000;355:2047-8. http://dx.doi.org/10.1016/S0140-6736(00)02354-0.
- Hawkins LC, Edwards JN, Dargan PI. Impact of restricting paracetamol pack sizes on paracetamol poisoning in the United Kingdom: a review of the literature. Drug Saf 2007;30:465-79. http://dx.doi.org/10.2165/00002018-200730060-00002.
- Bateman DN. Limiting paracetamol pack size: has it worked in the UK?. Clin Toxicol 2009;47:536-41. http://dx.doi.org/10.1080/15563650903093192.
- Morgan O, Griffiths C, Majeed A. Impact of paracetamol pack size restrictions on poisoning from paracetamol in England and Wales: an observational study. J Public Health 2005;27:19-24. http://dx.doi.org/10.1093/pubmed/fdh216.
- Bateman DN, Gorman DR, Bain M, Inglis JHC, House FR, Murphy D. Legislation restricting paracetamol sales and patterns of self-harm and death from paracetamol-containing preparations in Scotland. Br J Clin Pharmacol 2006;62:573-81. http://dx.doi.org/10.1111/j.1365-2125.2006.02668.x.
- Sheen CL, Dillon JF, Bateman DN, Simpson KJ, MacDonald TM. Paracetamol pack size restriction: the impact on paracetamol poisoning and over-the-counter supply of paracetamol, aspirin and ibuprofen. Pharmacoepidemiol Drug Saf 2002;11:329-31. http://dx.doi.org/10.1002/pds.701.
- Norman E, Dhairiwan R, Dargan PI, Wallace C, Jones AL. Paracetamol poisoning: can it be prevented?. Proc R Coll Physicians Edinb 2001;31:62-5.
- Greene SL, Dargan PI, Leman P, Jones AL. Paracetamol availability and recent changes in paracetamol poisoning: is the 1998 legislation limiting availability of paracetamol being followed?. Postgrad Med J 2006;82:520-3. http://dx.doi.org/10.1136/pgmj.2005.042036.
- Medicines and Healthcare products Regulatory Agency . Advertising Complaint – Home Bargains Stores, Multiple Sales of Paracetamol – August 2009 n.d. www.mhra.gov.uk/Howweregulate/Medicines/Advertisingofmedicines/Advertisinginvestigations/CON065609 (accessed December 2009).
- Mills J. Student, 17, Sold Lethal Paracetamol Dose by Tesco. Daily Mail 2006. www.dailymail.co.uk/news/article-387953/Student-17-sold-lethal-paracetamol-dose-Tesco.html# (accessed February 2011).
- S.I. No. 150/2001 – Medicinal Products (Control of Paracetamol) Regulations, 2001. Dublin: Stationery Office; 2001.
- NHS Evidence . Nonsteroidal Anti-Inflammatory Drugs (standard or Coxibs) – Prescribing Issues – Management 2012. www.cks.nhs.uk/nsaids_prescribing_issues/management/detailed_answers/gastrointestinal_adverse_effects/preventing_gi_adverse_effects (accessed February 2012).
- Hawton K, Bergen H, Simkin S, Brock A, Griffiths C, Romeri E, et al. Effect of withdrawal of co-proxamol on prescribing and deaths from drug poisoning in England and Wales: time series analysis. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b2270.
- Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299-30. http://dx.doi.org/10.1046/j.1365-2710.2002.00430.x.
- Ramsay CR, Matowe L, Grilli R, Grimshaw JM, Thomas RE. Interrupted time series designs in health technology assessment: lessons from two systematic reviews of behavior change strategies. Int J Technol Assess Health Care 2003;19:613-23. http://dx.doi.org/10.1017/S0266462303000576.
- Zhang F, Wagner A, Soumerai SB, Ross-Degnan D. Estimating confidence intervals around relative changes in outcomes in segmented regression analyses of time series data. Buffalo, NY: NorthEast SAS Users Group Inc.; 2002.
- Neuberger J, Gimson A, Davies M, Akyol M, O’Grady J, Burroughs A, et al. Selection of patients for liver transplantation and allocation of donated livers in the UK. Gut 2008;57:252-7. http://dx.doi.org/10.1136/gut.2007.131730.
- Bernal W, Auzinger G, Sizer E, Wendon J. Intensive care management of acute liver failure. Semin Liver Dis 2008;28:188-200. http://dx.doi.org/10.1055/s-2008-1073118.
- Simkin S, Hawton K, Kapur N, Gunnell D. What can be done to reduce mortality from paracetamol overdoses? A patient interview study. Q J Med 2012;105:41-5. http://dx.doi.org/10.1093/qjmed/hcr135.
- Bancroft J, Hawton K, Simkin S, Kingston B, Cumming C, Whitwell D. The reasons people give for taking overdoses: a further inquiry. Br J Med Psychol 1979;52:353-65. http://dx.doi.org/10.1111/j.2044-8341.1979.tb02536.x.
- Beck A, Schuyler D, Herman J, Beck A, Resnik H, Lettieri DJ. The prediction of suicide. Bowie, MD: Charles Press; 1974.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Hawton K, Simkin S, Deeks JJ, O’Connor S, Keen A, Altman DG, et al. Effects of a drug overdose in a television drama on presentations to hospital for self poisoning: time series and questionnaire study. BMJ 1999;318:972-7. http://dx.doi.org/10.1136/bmj.318.7189.972.
- Beales I. The editors' codebook: the handbook to the editors' code of practice (major revision for 2011). London: Newspaper Publishers Association, Newspaper Society, Periodical Publishers Association, Scottish Daily Newspaper Society, Scottish Newspaper Publishers Association; 2011.
- Media guidelines for reporting suicide and self-harm. Ewell, Surrey: Samaritans; 2008.
- Pohjola-Sintonen S, Kivistö KT, Vuori E, Lapatto-Reiniluoto O, Tiula E, Neuvonen PJ. Identification of drugs ingested in acute poisoning: correlation of patient history with drug analyses. Ther Drug Monit 2000;22:749-52. http://dx.doi.org/10.1097/00007691-200012000-00016.
- Bergen H, Hawton K, Waters K, Cooper J, Kapur N. Epidemiology and trends in non-fatal self-harm in three centres in England, 2000 to 2007. Br J Psychiatry 2010;197:493-8. http://dx.doi.org/10.1192/bjp.bp.110.077651.
- Laffoy M, Scallan E, Byrne G. Paracetamol availability and overdose in Ireland. Ir Med J 2001;94:212-14.
- NíMhaoláin ÁM, Davoren M, Kelly BD, Breen E, Casey P. Paracetamol availability in pharmacy and non-pharmacy outlets in Dublin, Ireland. Ir J Med Sci 2009;178:79-82.
- Donohue E, Walsh N, Tracey JA. Pack-size legislation reduces severity of paracetamol overdoses in Ireland. Ir J Med Sci 2006;175:40-2.
- Wheeler BW, Metcalfe C, Gunnell D, Stephens P, Martin RM. Population impacts of regulatory activity to restrict prescribing of selective COX-2 inhibitors (‘coxibs’) on gastrointestinal haemorrhage and acute myocardial infarction: ecological study. Br J Clin Pharmacol 2009;68:752-64.
- Hospital episode statistics database. London: Department of Health; 2007.
- Office for National Statistics . Population Estimates for UK, England and Wales, Scotland and Northern Ireland 2007. www.statistics.gov.uk/StatBase/Product.asp?vlnk=601 (accessed June 2009).
- Simkin S, Hawton K, Sutton L, Gunnell D, Bennewith O, Kapur N. Co-proxamol and suicide: a review to inform initiatives to prevent the continuing toll of overdose deaths. Q J Med 2005;98:159-70.
- Hawton K, Simkin S, Deeks JJ. Co-proxamol and suicide: a study of national mortality statistics and local non-fatal self-poisonings. BMJ 2003;326:1006-8. http://dx.doi.org/10.1136/bmj.326.7397.1006.
- Distalgesic and its equivalents: time for action . Drug Ther Bull 1983;21:17-9.
- Bateman DN, Afshari R. Licence needs to be changed. BMJ 2003;327. http://dx.doi.org/10.1136/bmj.327.7409.287.
- Hawton K, Simkin S, Gunnell D, Sutton L, Bennewith O, Turnbull P, et al. A multicentre study of co-proxamol poisoning suicides based on coroners' records in England. Br J Clin Pharmacol 2005;59:207-12.
- Office for National Statistics . Deaths related to drug poisoning: England and Wales, 1993–2005. Health Stat Q 2007;33:82-8.
- Medicines and Healthcare products Regulatory Agency . Withdrawal of Co-Proxamol Products and Interim Updated Prescribing Information. n.d. www.mhra.gov.uk/home/groups/pl-a/documents/websiteresources/con019461.pdf (accessed March 2005).
- Committee on Safety of Medicines . Withdrawal of co-proxamol (Distalgesic, Cosalgesic, Dolgesic). Curr Prob Pharmacovigilance 2006;31.
- Daigle MS. Suicide prevention through means restriction: assessing the risk of substitution: a critical review and synthesis. Accid Anal Prev 2005;37:625-32.
- Brock A, Baker A, Griffiths C, Jackson G, Fegan G, Marshall D. Suicide trends and geographical variations in the United Kingdom, 1991–2004. Health Stat Q 2006;31:6-22.
- Office for National Statistics . Deaths Related to Drug Poisoning in England and Wales, 2010. Statistical Bulletin 2011. www.ons.gov.uk/ons/rel/subnational-health3/deaths-related-to-drug-poisoning/2010/pdf-download.pdf (accessed September 2011).
- Gottlieb S. Warnings issued over COX 2 inhibitors in US and UK. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.330.7481.9-c.
- Gunnell D, Platt S, Hawton K. The economic crisis and suicide. Consequences may be serious and warrant early attention. BMJ 2009;338:1456-7.
- Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. Effects of the 2008 recession on health: a first look at European data. Lancet 2011;378:124-5. http://dx.doi.org/10.1016/S0140-6736(11)61079-9.
- European Medicines Agency recommends withdrawal of dextropropoxyphene-containing medicines. London: EMEA; 2009.
- US Food and Drug Administration . FDA Takes Action on Darvon, Other Pain Medications Containing Propoxyphene 2009. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm170769.htm (accessed February 2009).
- US Food and Drug Administration . Xanodyne Agrees to Withdraw Propoxyphene from the U.S. Market 2010. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm234350.htm (accessed May 2011).
- Health Canada . Darvon-N (dextropropoxyphene) – Recall and Withdrawal in Canada – for the Public 2010. www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/public/_2010/darvon-n_pc-cp-eng.php (accessed May 2011).
- Cavanagh JTO, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003;33:395-40. http://dx.doi.org/10.1017/S0033291702006943.
- Tournier M, Grolleau A, Cougnard A, Molimard M, Verdoux H. Factors associated with choice of psychotropic drugs used for intentional drug overdose. Eur Arch Psychiatry Clin Neurosci 2009;259:86-91. http://dx.doi.org/10.1007/s00406-008-0839-2.
- Buckley N, McManus P. Fatal toxicity of serotonergic and other antidepressant drugs: analysis of United Kingdom mortality data. BMJ 2002;325:1332-3.
- White N, Litovitz T, Clancy C. Suicidal antidepressant overdoses: a comparative analysis by antidepressant type. J Med Toxicol 2008;4:238-50. http://dx.doi.org/10.1007/BF03161207.
- Henry J. A fatal toxicity index for antidepressant poisoning. Acta Psychiatr Scand 1989;80:37-45. http://dx.doi.org/10.1111/j.1600-0447.1989.tb03045.x.
- Rose J, Unis A. A mortality index for postmarketing surveillance of new medications. Am J Emerg Med 2000;18:176-9. http://dx.doi.org/10.1016/S0735-6757(00)90013-5.
- Lawrenson RA, Tyrer F, Newson RB, Farmer RDT. The treatment of depression in UK general practice: selective serotonin reuptake inhibitors and tricyclic antidepressants compared. J Affect Disord 2000;59:149-57.
- IMS Health . Intercontinental Medical Statistics n.d. www.imshealth.com (accessed October 2008).
- Office for National Statistics . Population Estimates for UK, England and Wales, Scotland and Northern Ireland – Current Datasets 2008. www.statistics.gov.uk/statbase/Product.asp?vlnk=15106 (accessed June 2009).
- Medicines and Healthcare products Regulatory Agency . Dosulepin: measures to reduce risk of fatal overdose. Drug Saf Update 2007;1:7-8.
- Medicines and Healthcare products Regulatory Agency . Venlafaxine (Efexor) Summary of Basis for Regulatory Position 2006. www.mhra.gov.uk/Safetyinformation/Safetywarningsalertsandrecalls/Safetywarningsandmessagesformedicines/CON2023846 (accessed March 2009).
- Flanagan R. Fatal toxicity of drugs used in psychiatry. Hum Psychopharmacol 2008;23:43-51. http://dx.doi.org/10.1002/hup.916.
- Kelly CA, Dhaun N, Laing WJ, Strachan FE, Good AM, Bateman DN. Comparative toxicity of citalopram and the newer antidepressants after overdose. Clin Toxicol 2005;42:67-71. http://dx.doi.org/10.1081/CLT-120028747.
- Kapur N. Management of self-harm in adults: which way now?. Br J Psychiatry 2005;187:497-9. http://dx.doi.org/10.1192/bjp.187.6.497.
- Assessment following self-harm in adults. London: Royal College of Psychiatrists; 2005.
- Better Services for People who Self-harm project. London: Royal College of Psychiatrists; 2005.
- Gunnell D, Bennewith O, Peters TJ, House A, Hawton K. The epidemiology and management of self-harm amongst adults in England. J Public Health 2005;27:67-73. http://dx.doi.org/10.1093/pubmed/fdh192.
- Dickson S, Steeg S, Gordon M, Donaldson I, Matthews V, Kapur N, et al. Manchester: Centre for Suicide Prevention, University of Manchester; 2011.
- Kapur N, Murphy E, Cooper J, Bergen H, Hawton K, Simkin S, et al. Psychosocial assessment following self-harm: results from the Multi-Centre Monitoring of Self-Harm Project. J Affect Disord 2008;106:285-93. http://dx.doi.org/10.1016/j.jad.2007.07.010.
- Department of Health . Total Time Spent in A&Amp;E 2011. www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/AccidentandEmergency/DH_079085 (accessed July 2012).
- While D, Bickley H, Roscoe A, Windfuhr K, Rahman S, Shaw J, et al. Implementation of mental health service recommendations in England and Wales and suicide rates, 1997–2006: a cross-sectional and before-and-after observational study. Lancet 2012;379:1005-12. http://dx.doi.org/10.1016/S0140-6736(11)61712-1.
- Self-harm: longer-term management. London: British Psychological Society and Royal College of Psychiatrists; 2012.
- Carter GL, Clover K, Whyte IM, Dawson AH, D’Este C. Postcards from the EDge project: randomised controlled trial of an intervention using postcards to reduce repetition of hospital treated deliberate self poisoning. BMJ 2005;331:805-9. http://dx.doi.org/10.1136/bmj.38579.455266.E0.
- Carter GL, Clover K, Whyte IM, Dawson AH, D’Este C. Postcards from the EDge: 24-month outcomes of a randomised controlled trial for hospital-treated self-poisoning. Br J Psychiatry 2007;191:548-53. http://dx.doi.org/10.1192/bjp.bp.107.038406.
- Beautrais A, Gibb S, Faulkner A, Fergusson D, Mulder R. Postcard intervention for repeat self-harm: randomised controlled trial. Br J Psychiatry 2010;197:55-60. http://dx.doi.org/10.1192/bjp.bp.109.075754.
- Hassanian-Moghaddam H, Sarjami S, Kolahi AA, Carter GL. Postcards in Persia: randomised controlled trial to reduce suicidal behaviours 12 months after hospital-treated self-poisoning. Br J Psychiatry 2011;198:309-16. http://dx.doi.org/10.1192/bjp.bp.109.067199.
- Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry 2002;181:193-9. http://dx.doi.org/10.1192/bjp.181.3.193.
- Evans MO, Morgan HG, Hayward A, Gunnell DJ. Crisis telephone consultation for deliberate self-harm patients: effects on repetition. Br J Psychiatry 1999;175:23-7. http://dx.doi.org/10.1192/bjp.175.1.23.
- Vaiva G, Ducrocq F, Meyer P, Mathieu D, Philippe A, Libersa C, et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. BMJ 2006;332:1241-5. http://dx.doi.org/10.1136/bmj.332.7552.1241.
- Fleischmann A, Bertolote JM, Wasserman D, De Leo D, Bolhari J, Botega NJ, et al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bull World Health Organ 2008;86:703-9. http://dx.doi.org/10.2471/BLT.07.046995.
- Bertolote JM, Fleischmann A, De Leo D, Phillips MR, Botega NJ, Vijayakumar L, et al. Repetition of suicide attempts: data from emergency care settings in five culturally different low- and middle-income countries participating in the WHO SUPRE-MISS Study. Crisis 2010;31:194-201. http://dx.doi.org/10.1027/0227-5910/a000052.
- Patton M. Qualitative evaluation and research methods. Newbury Park, CA: Sage; 1990.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-100. http://dx.doi.org/10.1191/1478088706qp063oa.
- Sandelowski M. Sample size in qualitative research. Res Nurs Health 1995;18:179-83. http://dx.doi.org/10.1002/nur.4770180211.
- Clarke AR, Schnieden V, Hamilton BA, Dudley AM, Beard J, Einfeld SL, et al. Factors associated with treatment compliance in young people following an emergency department presentation for deliberate self-harm. Arch Suicide Res 2004;8:147-52. http://dx.doi.org/10.1080/13811110490270994.
- Hawton K, Sinclair J. The challenge of evaluating the effectiveness of treatments for deliberate self-harm. Psychol Med 2003;33:955-8. http://dx.doi.org/10.1017/S0033291703008304.
- Schulz K, Altman D, Moher D. CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c332.
- Sinclair J, Gray A, Rivero-Arias O, Saunders K, Hawton K. Healthcare and social services resource use and costs of self-harm patients. Soc Psychiatry Psychiatr Epidemiol 2011;46:263-71. http://dx.doi.org/10.1007/s00127-010-0183-5.
- Owens C. Interventions for self-harm: are we measuring outcomes in the most appropriate way?. Br J Psychiatry 2010;197:502-3. http://dx.doi.org/10.1192/bjp.197.6.502a.
- Hatcher S, Owens D. Do get in touch. BMJ 2005;331:78-9. http://dx.doi.org/10.1136/bmj.331.7520.788.
- Vaiva G, Walter M, Al Arab AS, Courtet P, Bellivier F, Demarty AL, et al. ALGOS: the development of a randomized controlled trial testing a case management algorithm designed to reduce suicide risk among suicide attempters. BMC Psychiatry 2011;11. http://dx.doi.org/10.1186/1471-244X-11-1.
- Geddes J, Juszczak E. Period trends in rate of suicide in first 28 days after discharge from psychiatric hospital in Scotland, 1968–92. BMJ 1995;311:357-60. http://dx.doi.org/10.1136/bmj.311.7001.357.
- Goldacre M, Seagroatt V, Hawton K. Suicide after discharge from psychiatric inpatient care. Lancet 1993;342:283-6. http://dx.doi.org/10.1016/0140-6736(93)91822-4.
- Meehan J, Kapur N, Hunt IM, Turnbull P, Robinson J, Bickley H, et al. Suicide in mental health in-patients and within 3 months of discharge. National clinical survey. Br J Psychiatry 2006;188:129-34. http://dx.doi.org/10.1192/bjp.188.2.129.
- Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry 2005;62:427-32. http://dx.doi.org/10.1001/archpsyc.62.4.427.
- Thong JY, Su AH, Chan YH, Chia BH. Suicide in psychiatric patients: case–control study in Singapore. Aust N Z J Psychiatry 2008;42:509-19.
- Gunnell D, Hawton K, Ho D, Evans J, O’Connor S, Potakar J, et al. Hospital admissions for self harm after discharge from psychiatric inpatient care: cohort study. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a2278.
- Preventing suicide: a toolkit for mental health services. Leeds: NIMHE; 2003.
- Luxton DD, Kinn JT, June JD, Pierre LW, Reger MA, Gahm GA. Caring letters project: a military suicide-prevention pilot program. Crisis 2012;33:5-12. http://dx.doi.org/10.1027/0227-5910/a000093.
- Preventing suicide in England – a cross-government outcomes strategy to save lives. London: Department of Health; 2011.
- Office for National Statistics . Suicides in the United Kingdom 2011. Statistical Bulletin 2013. www.ons.gov.uk/ons/rel/subnational-health4/suicides-in-the-united-kingdom/2011/stb-suicide-bulletin.html (accessed August 2013).
- Cooper J, Hunter C, Owen-Smith A, Gunnell D, Donovan J, Hawton K, et al. ‘Well it’s like someone at the other end cares about you'. A qualitative study exploring the views of users and providers of care of contact-based interventions following self-harm. Gen Hosp Psychiatry 2011;33:166-76. http://dx.doi.org/10.1016/j.genhosppsych.2011.01.009.
- Gunnell D, Bennewith O, Kapur N, Simkin S, Cooper J, Hawton K. The use of the Internet by people who die by suicide in England: a cross sectional study. J Affect Disord 2012;141:480-3. http://dx.doi.org/10.1016/j.jad.2012.04.015.
- Gunnell D, Hawton K, Ho D, Evans J, O’Connor S, Potokar J, et al. Hospital admissions for self-harm following psychiatric hospital discharge: cohort study. BMJ 2008;337:1331-4.
- Gunnell D, Metcalfe C, While D, Hawton K, Ho D, Appleby L, et al. Impact of national policy initiatives on fatal and non-fatal self-harm after psychiatric hospital discharge: a time series analysis. Br J Psychiatry 2012;201:233-8. http://dx.doi.org/10.1192/bjp.bp.111.104422.
- Hawton K, Bergen H, Simkin S, Arensman E, Corcoran P, Cooper J, et al. Impact of different pack sizes of paracetamol in the United Kingdom and Ireland on intentional overdoses: a comparative study. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-460.
- Hawton K, Bergen H, Simkin S, Cooper J, Waters K, Gunnell D, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry 2010;196:354-8. http://dx.doi.org/10.1192/bjp.bp.109.070219.
- Hawton K, Bergen H, Simkin S, Wells C, Kapur N, Gunnell D. Six-year follow-up of impact of co-proxamol withdrawal in England and Wales on prescribing and deaths: time-series study. PLoS Med 2012;9. http://dx.doi.org/10.1371/journal.pmed.1001213.
- Hawton K, Bergen H, Waters K, Murphy E, Cooper J, Kapur N. Impact of withdrawal of the analgesic co-proxamol in the UK on non-fatal self-poisoning. Crisis 2011;32:81-7.
- Kapur N, Clements C, Bateman N, Foëx B, Mackway-Jones K, Huxtable R, et al. Advance directives and suicidal behaviour. BMJ 2010;341:590-1. http://dx.doi.org/10.1136/bmj.c4557.
- Simkin S, Bennewith O, Cooper J. Investigating official records of suicides for research purposes: challenges and coping strategies. Crisis 2012;33:123-6. http://dx.doi.org/10.1027/0227-5910/a000167.
- Hawton K, Bergen H, Simkin S, Dodd S, Pocock P, Bernal W, et al. Reduced pack sizes of paracetamol: long-term evaluation of impacts on poisoning deaths and liver transplant activity in England and Wales. BMJ 2013;346.
- Bennewith O, Evans J, Donovan J, Paramasivan S, Owen-Smith A, hollingworth W, et al. A contact-based intervention for people recently discharged from inpatient psychiatric care: a pilot study n.d.
- Owen-Smith A, Bennewith O, Donovan J, Evans J, Hawton K, Kapur N, et al. ‘When you’re in the hospital, you're in a sort of bubble'. Understanding the high risk of self-harm and suicide following psychiatric discharge: qualitative study. Crisis 2013.
- Kapur N, Gunnell D, Hawton K, Nadeem S, Khalil S, Longson DJ, et al. Messages from Manchester pilot randomised controlled trial following self-harm. Br J Psychiatry 2013;203:73-4.
- Chen Y, Bennewith O, Hawton K, Simkin S, Cooper J, Kapur N, et al. Suicide by burning barbecue charcoal in England. J Public Health 2013;203:73-4. http://dx.doi.org/10.1093/pubmed/fds095.
- Haw C, Hawton K, Casey D, Bale E, Shepherd A. Alcohol dependence, excessive drinking and deliberate self-harm. Soc Psychiatry Psychiatr Epidemiol 2005;40:964-71. http://dx.doi.org/10.1007/s00127-005-0981-3.
- Bhui K, McKenzie K, Rasul F. Rates, risk factors and methods of self harm among minority ethnic groups in the UK: a systematic review. BMC Public Health 2007;7. http://dx.doi.org/10.1186/1471-2458-7-336.
- Cooper J, Murphy E, Webb R, Hawton K, Bergen H, Waters K, et al. Ethnic differences in self-harm rates, characteristics and service provision: three-city cohort study. Br J Psychiatry 2010;197:212-18. http://dx.doi.org/10.1192/bjp.bp.109.072637.
- Husain M, Waheed W, Husain N. Self-harm in British South Asian women: psychosocial correlates and strategies for prevention. Ann Gen Psychiatry 2006;5.
- Liu KY, Beautrais A, Caine E, Chan K, Chao A, Conwell Y, et al. Charcoal burning suicides in Hong Kong and urban Taiwan – an illustration of the impact of a novel method of suicide on overall regional rates. J Epidemiol Community Health 2007;61:248-53. http://dx.doi.org/10.1136/jech.2006.048553.
- Biddle L, Donovan J, Hawton K, Kapur N, Gunnell D. Suicide and the Internet. BMJ 2008;336:800-2. http://dx.doi.org/10.1136/bmj.39525.442674.AD.
- Collings SC, Macdonald C, Kemp C, Fortune S, Hawton K. In the balance. Pro-suicide and support material located by New Zealand-based web searches. Auckland: Te Pou; 2010.
- US Food and Drug Administration . FDA Limits Acetaminophen in Prescription Combination Products; Requires Liver Toxicity Warnings 2011. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm239894.htm (accessed January 2011).
- Toms L, McQuay HJ, Derry S, Moore RA. Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.CD004602.pub2.
- Haw C, Hawton K, Houston K, Townsend E. Psychiatric and personality disorders in deliberate self-harm patients. Br J Psychiatry 2001;178:48-54. http://dx.doi.org/10.1192/bjp.178.1.48.
- Gjelsvik B, Heyerdahl F, Hawton K. Prescribed medication availability and deliberate self-poisoning: a longitudinal study. J Clin Psychiatry 2012;73:e548-54. http://dx.doi.org/10.4088/JCP.11m07209.
Appendix 1 Form used to extract data on coroners' verdicts
Appendix 2 Protocol for coding vignettes
We define suicide as ‘any act of self-damage which on the balance of evidence was considered to be deliberately initiated and which resulted in the individual's death’.
All vignettes will be independently coded by DG, KH and NK blind to the year of death. Based on the available information each investigator will rate the probability that a particular death was suicide as:
-
1 = high
-
2 = moderate
-
3 = low
-
9 = not clear.
For deaths coded as ‘low’ or ‘not clear’ likelihood of suicide, the most likely alternative cause of death will be coded as one of the following:
-
accident
-
homicide
-
misadventure (the unintended outcome of an intended action)
-
other – please specify.
The following indicators will contribute to decision-making (based in part on those used by Cooper and Milroy26):
-
a suicide note (likely high probability)
-
prima facie evidence of intent (e.g. statement to others that person intended to take his or her life) (high probability)
-
the method used – hanging/firearm/carbon monoxide poisoning from car/barbecue charcoal (high probability of deliberate act) [although exceptions are possible, for example autoerotic hanging (as indicated by presence of pornography/cross-dressing)]
-
previous acts of non-fatal self-harm (increased probability)
-
a history of previous psychiatric illness with associated suicide risk, for example schizophrenia/major depression was seen as increasing the possibility that an act was suicide
-
circumstantial evidence as to the most reasonable and probable explanation for the death
-
if there are clear psychosocial stressors around the time of the act that might plausibly have prompted some to kill themselves (e.g. bankruptcy/impending criminal conviction/marriage breakdown), these were taken to increase the likelihood of suicide
-
if there is evidence of a high level of alcohol or illicit drug ingestion prior to the act, this may introduce some degree of uncertainty (unless other indicators such as a note are present – moderate)
-
if there is insufficient information (e.g. someone has been dead for several weeks and post-mortem blood levels are unreliable), code as not clear
-
if other people involved with the case (medical staff/family) felt that suicide was likely
-
if the blood level of a drug is considerably above the therapeutic dose this is a pointer to deliberate overdose rather than accidental overdosing, for example to relieve pain in someone who has high blood alcohol levels.
Appendix 3 Interrupted time-series segmented regression analysis
The following is an explanation of the method of Wagner et al. ,80 applied to our particular analysis. Segmented regression analysis is a method of estimating changes in levels and trends in an outcome (deaths, in our case) associated with an intervention (the legislation in the third quarter of 1998 to reduce pack size of paracetamol). The time-series regression equation for this model is:
where Ŷt is the outcome (mean number of deaths per quarter); time indicates the number of quarters from the start of the series (1–68); intervention is a dummy variable taking the values 0 in the pre-intervention segment and 1 in the post-intervention segment; time_after_intervention is 0 in the pre-intervention segment and counts the quarters in the post-intervention segment at time t (1–45); the coefficient β0 estimates the base level of the outcome (number of deaths) at the beginning of the series; β1 estimates the base trend, that is, the change in outcome per quarter in the pre-intervention segment; β2 estimates the change in level of deaths in the post-intervention segment; β3 estimates the change in trend in deaths in the post-intervention segment; and et estimates the error.
Absolute effect of the intervention
The model was used to estimate the absolute effect of the intervention in two ways, both of which we used:
-
(a) First, we calculated the difference between the estimated outcome at a certain time after the intervention and the outcome at that time if the intervention had not taken place. For example, to estimate the effect of the intervention at the mid-point of the post-intervention period (when time = 46 and time_after_intervention = 23), we have:
Thus, the absolute effect of the intervention is:
-
(b) Second, when there is an increasing trend in the pre-intervention period, a more conservative estimate of the absolute effect of the intervention may be calculated. Here the outcome without the intervention was taken at the earlier time (not assuming any increase in the post-intervention period). Thus, we have:
and the outcome with the intervention remains unchanged:
Thus, the conservative estimate of absolute effect of the intervention was:
Coefficients and errors from full models including all terms in Equation 1 are given in Table 46. Non-significant terms were included as there may be correlation between slope and level terms, which should be accounted for.
| Cause of death | Segmented regression modelsa | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Base-level coefficient (β0) | Robust SE | p-value | Base-trend coefficient (β1) | Robust SE | p-value | Step-change coefficientb (β2) | Robust SE | p-value | Trend-change coefficientb (β3) | Robust SE | p-value | |
| With September 1998 as the point of intervention | ||||||||||||
| Deaths: suicide, open | ||||||||||||
| Paracetamol | 30.103 | 1.901 | < 0.001 | 0.188 | 0.116 | 0.111 | − 6.023 | 2.430 | 0.016 | − 0.463 | 0.132 | 0.001 |
| Paracetamol (adjusted)c | 21.085 | 7.208 | 0.005 | 0.149 | 0.113 | 0.194 | − 6.473 | 2.397 | 0.009 | − 0.328 | 0.164 | 0.049 |
| Paracetamol (adjusted)d | 11.005 | 10.018 | 0.276 | 0.206 | 0.117 | 0.082 | − 6.535 | 2.540 | 0.012 | − 0.424 | 0.140 | 0.004 |
| Paracetamol compounds | 4.801 | 1.081 | < 0.001 | 0.007 | 0.087 | 0.933 | 1.249 | 1.534 | 0.419 | 0.013 | 0.095 | 0.892 |
| All drug poisoning except paracetamol | 291.078 | 12.757 | < 0.001 | 1.290 | 0.886 | 0.150 | 12.928 | 12.150 | 0.291 | − 4.347 | 0.925 | < 0.001 |
| All drug poisoning | 321.373 | 14.007 | < 0.001 | 1.462 | 0.966 | 0.135 | 7.142 | 13.067 | 0.587 | − 4.795 | 1.011 | < 0.001 |
| All causes | 1277.176 | 28.050 | < 0.001 | − 1.075 | 2.365 | 0.651 | 36.928 | 41.443 | 0.376 | − 2.893 | 2.574 | 0.265 |
| Deaths: suicide, open, accidental | ||||||||||||
| Paracetamol | 39.344 | 2.460 | < 0.001 | 0.309 | 0.158 | 0.055 | − 10.300 | 3.111 | 0.002 | − 0.521 | 0.0176 | 0.004 |
| Paracetamol (adjusted)c | 30.171 | 7.099 | < 0.001 | 0.236 | 0.170 | 0.170 | − 9.959 | 3.085 | 0.002 | − 0.426 | 0.191 | 0.029 |
| Paracetamol compounds | 5.777 | 1.172 | < 0.001 | 0.017 | 0.087 | 0.842 | 0.358 | 1.489 | 0.811 | 0.081 | 0.094 | 0.392 |
| All drug poisoning except paracetamol | 445.966 | 27.361 | < 0.001 | 2.919 | 1.885 | 0.126 | − 10.246 | 29.152 | 0.726 | − 3.931 | 2.042 | 0.059 |
| All drug poisoning | 468.263 | 29.352 | < 0.001 | 3.122 | 1.989 | 0.121 | − 18.461 | 31.001 | 0.554 | − 4.361 | 2.140 | 0.046 |
| With January 1998 as the point of intervention | ||||||||||||
| Deaths: suicide, open | ||||||||||||
| Paracetamol | 29.803 | 2.117 | < 0.001 | 0.216 | 0.181 | 0.239 | − 3.567 | 2.984 | 0.236 | − 0.531 | 0.190 | 0.007 |
Appendix 4 Questionnaire and topic guide for interview study with patients who had taken an overdose of paracetamol
Appendix 5 Hospital interview questionnaire
Appendix 6 Audit form
Appendix 7 Topic guide: service user interviews
Appendix 8 Topic guide: staff focus group
Appendix 9 Leaflet provided to patients in the intervention group
Appendix 10 Example letter for contact intervention
Appendix 11 Topic guide: post-intervention participant interviews
Appendix 12 Emergent themes from post-intervention participant interviews
Appendix 13 Letters used for contact intervention
Week 1 letter to service users discharged to a community mental health team
Week 2 letter to service users discharged to a community mental health team
Appendix 14 Intervention leaflet
Appendix 15 Post-intervention participant questionnaire
Appendix 16 Public and patient involvement in the research programme
-
Two to three service user collaborators on the programme attended annual programme grant meetings and were active contributors to discussions.
-
There were two service users and a Samaritans' representative on the steering group for the strand of the programme in which we developed and piloted a contact-based intervention aimed at reducing the incidence of fatal and non-fatal self-harm in the period after psychiatric hospital discharge (see Chapter 8). One is a co-author on the paper arising from this strand of the research.
-
The contact letters and protocols for patient contact following psychiatric hospital discharge (see Chapter 8) were co-produced with the service user member of the research group and had input from a number of patients who had recently been discharged from a psychiatric inpatient unit.
-
Using qualitative methodologies to investigate the views of service users and staff regarding contact-based interventions, we developed a three-stage intervention for people presenting to hospital with self-harm (the process is described in Chapter 7 and in a paper published in General Hospital Psychiatry170). We interviewed self-harm patients recently discharged from an emergency department, and clinical and voluntary staff from relevant service areas (including a local branch of the Samaritans) took part in a focus group and individual interviews.
-
For the study of contact following self-harm (see Chapter 7), a service user and a representative from MIND commented on the design of the study and provided comments and suggestions that were incorporated into the final letters to patients and the telephone interview guide.
-
Service users are members of the advisory groups for the self-harm data collection centres involved in assembling data on non-fatal poisoning. These data were used in the studies of relative toxicity of antidepressants and of the sizes of overdoses of paracetamol in England and Ireland. Service user representatives were able to comment on the studies.
-
Towards the end of the programme, we sought wide public and patient involvement in planning the next phase of the research and our application for further NIHR funding. A 1-day meeting was convened and members of the planning group included service users from several centres (one of whom was a co-applicant on our application for renewed funding), a representative of the Samaritans (Chief Executive), Madeleine Moon MP (chairperson of the All-Party Parliamentary Group on Suicide and Self Harm Prevention), representatives of the ONS (Myer Glickman, Head of Health Analysis; Claudia Wells, Head of Mortality Analysis) and a representative of the MHRA (June Raine, Director of Post Licensing).
-
Throughout the programme, members of the research team engaged with the print and broadcast media and undertook presentations to lay and user groups including national meetings of the Samaritans and Papyrus.
Glossary
- Accidental death
- A death resulting from actions by an individual or others that have unintended consequences.
- Case fatality index
- The rate of mortality from self-poisoning relative to the non-fatal self-poisoning rate for a specific drug (mortality rate/non-fatal self-poisoning rate). Note: case fatality would typically be defined as the proportion of cases of self-poisoning that are fatal; however, the nature of our data (national mortality/multicentre register incidence, that is, data from three centres) has led us to operationalise the definition slightly differently.
- Co-proxamol
- A prescribed medicine combining paracetamol and dextropropoxyphene used for pain relief. It was withdrawn from use in the UK on 31 December 2007.
- Cyclo-oxygenase-2 (COX-2) inhibitor
- A type of non-steroidal anti-inflammatory drug that works by directly targeting COX-2, an enzyme that is involved in causing inflammation and pain.
- Dosulepin
- One of a group of similar antidepressants known as tricyclic antidepressants.
- Fatal toxicity index
- The rate of mortality from overdose of a specific drug relative to its rate of prescription (mortality rate/prescription rate).
- Misadventure, death by
- The terms ‘accident’ and ‘misadventure’ are often used interchangeably by coroners. Some suggest that the distinction is that a death by misadventure occurs when the action was deliberate but the outcome unintended, whereas with accidents both the action and the outcome were unintended.
- Narrative verdict
- This form of verdict records, in several sentences, how, and in what circumstances, the death occurred, rather than giving a single ‘short-form’ verdict such as suicide, open or accidental death.
- Non-steroidal anti-inflammatory drug
- Non-steroidal anti-inflammatory drugs such as aspirin and ibuprofen work to reduce both pain and inflammation and are used very commonly to treat conditions such as headache and arthritis. However, the chemical action of non-steroidal anti-inflammatory drugs that makes them effective in treating pain and inflammation can also cause gastrointestinal problems, particularly in long-term users.
- Noradrenergic and specific serotonergic antidepressant
- A type of antidepressant that works by increasing neurotransmission of noradrenaline and serotonin.
- Open verdict
- A verdict given by a coroner following an inquest when there is insufficient evidence to determine the deceased's intent or if it is unclear whether the death was self-inflicted or accidental.
- Paracetamol-induced hepatotoxicity
- Injury to the liver caused by overdose or excessive use of paracetamol, which can lead to liver failure.
- Potential years of life lost
- A measure of premature mortality calculated by comparing the age of premature death (e.g. by suicide) with the expected age of death had the person not died prematurely from that cause (e.g. 75 years).
- Selective serotonin reuptake inhibitor
- A type of antidepressant that works by increasing the amount of serotonin in the brain.
- Self-harm
- A deliberate non-fatal act, whether physical, drug overdose or poisoning, carried out in the knowledge that it was potentially harmful and, in the case of drug overdose, that the amount taken was excessive.
- Serotonin–noradrenaline reuptake inhibitor
- A type of antidepressant that works by increasing the amount of serotonin and noradrenaline in the brain.
- Suicide
- An act of self-harm that results in death.
- Tricyclic antidepressants
- An older style of antidepressant named for its chemical structure that forms three rings; these act by increasing the level of noradrenaline and serotonin in the brain.
List of abbreviations
- CDMS
- Clinical Decision Management System
- CI
- confidence interval
- CSM
- Committee on Safety of Medicines
- df
- degrees of freedom
- FDA
- US Food and Drug Administration
- GI
- gastrointestinal
- HADS
- Hospital Anxiety and Depression Scale
- HES
- Hospital Episode Statistics
- HR
- hazard ratio
- ICD-9
- International Classification of Diseases, Ninth Edition
- ICD-10
- International Classification of Diseases, Tenth Edition
- IQR
- interquartile range
- IRR
- incidence risk ratio
- LA
- local authority
- MHRA
- Medicines and Healthcare products Regulatory Agency
- MHRN
- Mental Health Research Network
- NaSSA
- noradrenergic and specific serotonergic antidepressant
- NICE
- National Institute for Health and Care Excellence
- NSAID
- non-steroidal anti-inflammatory drug
- ONS
- Office for National Statistics
- OR
- odds ratio
- OTC
- over-the-counter
- PYLL
- potential years of life lost
- SD
- standard deviation
- SIS
- Suicidal Intent Scale
- SNRI
- serotonin–noradrenaline reuptake inhibitor
- SSRI
- selective serotonin reuptake inhibitor
- TCA
- tricyclic antidepressant
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.