Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/156/20. The contractual start date was in December 2015. The final report began editorial review in December 2018 and was accepted for publication in September 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Scott Weich was a member of the Health Technology Assessment (HTA) Mental, Psychological and Occupational Health Panel (2009–15), the HTA Prioritisation Group (2009–15) and the HTA Clinical Evaluation and Trials Committee (2015–19). Sophie Staniszewska was an associate member of the Health Services and Delivery Research (HSDR) Commissioning Board (researcher led) (2009–18). Carole Mockford was an associate member of the HSDR Commissioning Board (researcher led) (2009–18). Frances Griffiths reports receiving grants from the National Institute for Health Research during the conduct of the study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Weich et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction to the final EURIPIDES report
Patient experience and the link to quality improvement
All NHS providers are required to collect feedback routinely on patients’ experiences of care. This data collection takes place within an increasingly constrained wider organisational context in which the NHS is under pressure to deliver effective, timely and affordable care. The manifold pressures exerted on the wider system, and a series of high-profile incidents,1–5 have given rise to concerns about quality and the standards of care.
As a result of a national inquiry and concerns being raised, the National Institute for Health and Care Excellence (NICE), the NHS National Quality Board and others have called for a stronger patient voice and have reiterated core principles of patient-centred care including compassion, dignity, autonomy and choice. 1–3,6,7 Despite this emphasis, there remains little evidence about what to measure, how best to collect this information and how to use the data collected to improve service quality. 8,9
We do not know if reporting patients’ experiences is associated with improved clinical or functional outcomes, improved quality of life, reduced carer burden or reduced costs of care. 10,11 In addition, we do not understand how any such effects may be mediated, for example by better treatment adherence, nor do we know which types of patient experience data are used or useful in improving quality of care and driving service change. 8,10,12–15
Despite trusts routinely collecting patient experience data,16,17 these data are often felt to be of limited value8,18 because of methodological problems (including poor or unknown psychometric properties or missing data) or because the measures used lack the granular detail necessary to produce meaningful action plans to address the concerns raised. 19 The most commonly adopted measure in inpatient settings is the Friends and Family Test (FFT), the results of which are reported to NHS England monthly. 20 Despite aspects of care being captured in satisfaction surveys, it has been recognised that these tests do not capture information that is sufficiently detailed to inform service change. 18
The Evaluating the Use of Patient Experience Data to Improve the Quality of Inpatient Mental Health Care (EURIPIDES) study was commissioned in response to a National Institute for Health Research (NIHR) call to address the dearth of evidence about these issues. The call invited applications for studies examining known concerns with timely and informative data collection, on the alignment of national and/or local needs and on the level at which data should be shared to be most effective and to lead to change. The call recognised the further issue of data being collected but not used and raised concerns about organisational capacity to respond to information gleaned from data. The call expressly asked how these data should be used alongside other data to produce reliable quality indicators.
The EURIPIDES study was unique in responding to this call through a focus on mental health inpatient settings. Thus, it represents the first study of patient experience in acute adult mental health settings and offers a unique contribution to knowledge through providing an evidence base on the approach to collecting and using patient experience data to improve service outcomes.
We hypothesised that we would be able to discern differences between service providers in their commitment to and capacity for using patient experience data to improve services. 2 We further hypothesised that these differences would be apparent in the ways that NHS mental health trusts went about collecting experience data from users of inpatient services, the analysis of these data, the embeddedness of patient experience work in trusts’ core business and the involvement of service users and carers in these processes. 21–23
Based on evidence from other studies, we predicted that differences between providers might include commitment to service improvement among senior leaders, decentralised decision-making, role clarity within the organisation, and support for risk-taking. 21,22 We hypothesised that organisations that use patient experience data most effectively would also have robust data collection strategies. Finally, we hypothesised that organisations that are more patient centred will demonstrate the adoption of co-produced or co-designed approaches to service improvement and will involve service users and carers. 24,25 These hypotheses were central to the programme theory-building (see Chapter 2 and Appendix 17).
The context of inpatient settings
The EURIPIDES study examined inpatient mental health services on the grounds that these are important but costly services that remain unpopular with service users23 and are the settings in which many serious incidents, such as suicide, continue to occur. We knew little about the processes required or used to collect, analyse, interpret and translate meaningful patient experience data into better outcomes for patients and more efficient and cost-effective care. 8,9 We did not know what kinds of feedback were most important or what management processes were needed to translate this into effective action plans and we did not know if this made any difference to patients themselves.
We identified three initiatives that attempt to raise the standards of inpatient mental health care, including the Productive Ward programme,26 led by the NHS Institute for Improvement and Innovation, which focuses on the adoption and spread of a model of ‘lean working’; Star Wards,27 a third-sector initiative that uses patient experience information to develop and share best practice; and the Royal College of Psychiatrists’ Accreditation for Inpatient Mental Health Services scheme, which is based on evaluation against a quality standard and broadly focuses on raising general standards of care, timely and purposeful admission, safety, the environment and facilities, and therapies and activities. 28 In addition, there is a NICE quality standard that applies to inpatient care that identifies four domains of focus, namely shared decision-making, contact with staff, meaningful activity and the use of compulsion. 5,6
Reports about inpatient settings highlight adverse experiences such as fear of assault, overcrowding, noise, lack or privacy and dignity, lack of therapeutic activities, limited individual recovery-focused support and an emphasis on coercion, control and restraint. 24,29 In addition, inpatient mental health services remain the locus of the most pronounced ethnic inequalities in mental health service experience. 25 Patients of black ethnicity (including both African Caribbean and black African groups) remain over-represented in inpatient settings;30 they receive higher doses of medication and experience higher rates of seclusion, physical restraint and injury31 and they have higher rates of suicide. 32 Likewise, many patients are detained under the Mental Health Act33 and, therefore, have no choice about admission. 29 This raises questions about how and when to ascertain information about their experiences.
Inpatient settings therefore represent one of the more challenging areas within the NHS in which to obtain patient experiences, but one in which there are, hypothetically, significant gains possible if quality improvement could be driven by this feedback. The EURIPIDES study represents the first attempt both to provide an overview of the ways in which individual NHS providers of inpatient adult mental health services in England are collecting, managing and using patient experience data, and to interrogate how these processes operate in more granular detail.
Aims and objectives
We set out to understand how, and under what conditions, patient experience feedback processes could be used to support the improvement of health care in NHS adult inpatient mental health settings in England. We addressed this lacuna in knowledge by using a realist research design across five work packages (WPs) to develop a set of recommendations informed by both theory and evidence. Our results were intended to be relevant to front-line staff; service managers; those responsible for the design, implementation or management of patient experience or quality processes; and policy-makers.
The central research question asked was as follows: which approaches to collecting and using patient experience data are the most useful for supporting improvements in inpatient mental health care?
The specific objectives of the EURIPIDES study were to:
-
complete a systematic review to identify evidence-based patient experience themes relevant to mental health care (aim 1)
-
identify, describe and classify approaches to collecting and using patient experience data to improve inpatient mental health services across England by conducting a national survey of patient experience leads (PELs) (aim 2)
-
use the information from the national survey to populate a sampling frame to select diverse sites for six in-depth case studies, in which we would interview those who deliver and receive these services to conduct a realist evaluation of what works, for whom, in what circumstances and why (aim 3)
-
identify which types of patient experience measures and organisational processes facilitate effective translation of these data into service improvement actions, and present these findings to a consensus conference of experts (including service users and carers) at which recommendations about implementing best practice would be agreed (aim 4)
-
model variation in resources (costs) associated with adopting new ways of collecting and using patient experience data and associated service improvements, the obstacles to this and the value (i.e. cost) of evidence required to convince NHS commissioners and providers to substantially alter the way in which they deliver inpatient mental health care (aim 5).
Outputs from the EURIPIDES study include evidence-based recommendations on the most effective existing ways to collect and use patient experience data to improve the quality of inpatient mental health services. Our recommendations cover data collection methods, optimal organisational processes for translating data into action plans, and evidence of (potential) impact. Results are grounded in robust consensus about what is happening presently in an NHS context and on the feasibility, acceptability and sustainability of proposed changes.
Project overview and reporting structure
The overarching research design is set out in Chapter 2 and full details of the methods used at each stage of the study are reported in the corresponding chapters that relate to the five study aims set out above. In essence, the study comprised five interlinked WPs:
-
a systematic review (WP1, aim 1)
-
a survey of NHS providers of inpatient mental health care in England to populate a sampling frame for WP3 (WP2, aim 2)
-
a realist evaluation of six in-depth case studies selected using the WP2 findings (WP3, aim 3)
-
a consensus conference to agree recommendations about best practice and understand challenges to and opportunities for implementation in real-world NHS settings (WP4, aim 4)
-
health economic modelling to estimate the resource required for and barriers to the adoption of best practice (WP5, aim 5).
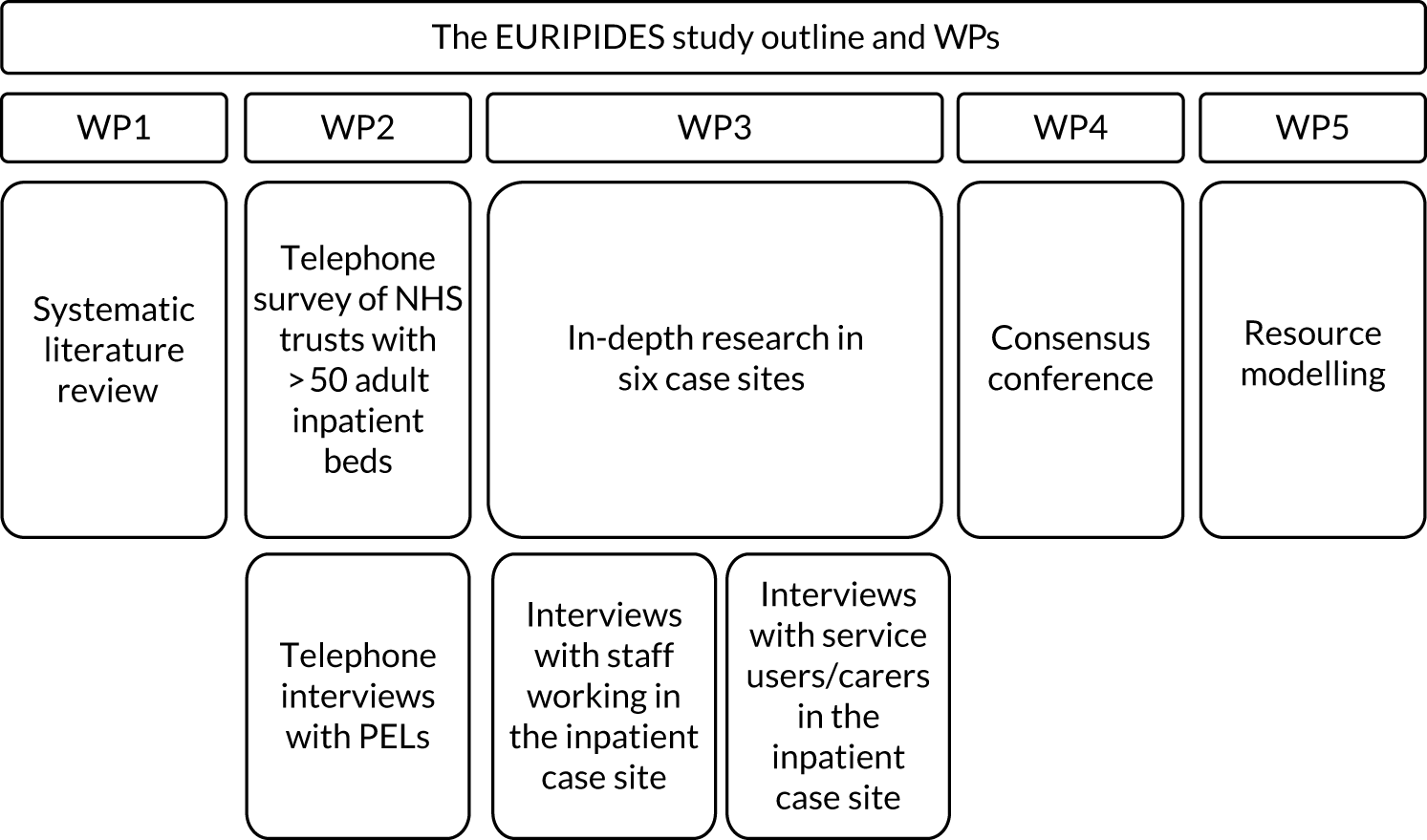
These WPs are represented in Figure 1.
FIGURE 1.
Study outline indicating the content of the different WPs.
Throughout the 3-year study, the multidisciplinary project team met frequently to discuss emerging findings to ensure that each WP informed and complemented the others. The project team benefited from the expertise of those with lived experience who worked alongside academic colleagues drawn from the fields of psychiatry, nursing, psychology, clinical psychology, general practice, health economics and social policy. The work reported under the separate chapter headings, although distinct in focus, is therefore interlinked and the study outcomes are knitted together in a summative integrated findings chapter.
The research was underpinned by a robust two-strand approach to patient and public involvement (PPI). A lay service user and carer reference group is referred to throughout the report as the patient and public involvement team (PPIT). The PPIT comprised people with lived experience of adult inpatient settings and two survivor researchers who supported the study from its design, through data collection, to analysis and writing.
In compiling this report, we have sought to produce a synthesis that embraces the complexity of integrating a realist approach across different research activities to understand the processes of collecting and using patient experience data in adult inpatient mental health settings. We aimed, in particular, to understand how these are currently linked to improvements in service, and under what conditions this might be optimised.
Chapter 2 Realist framework and research design for the study
Introduction
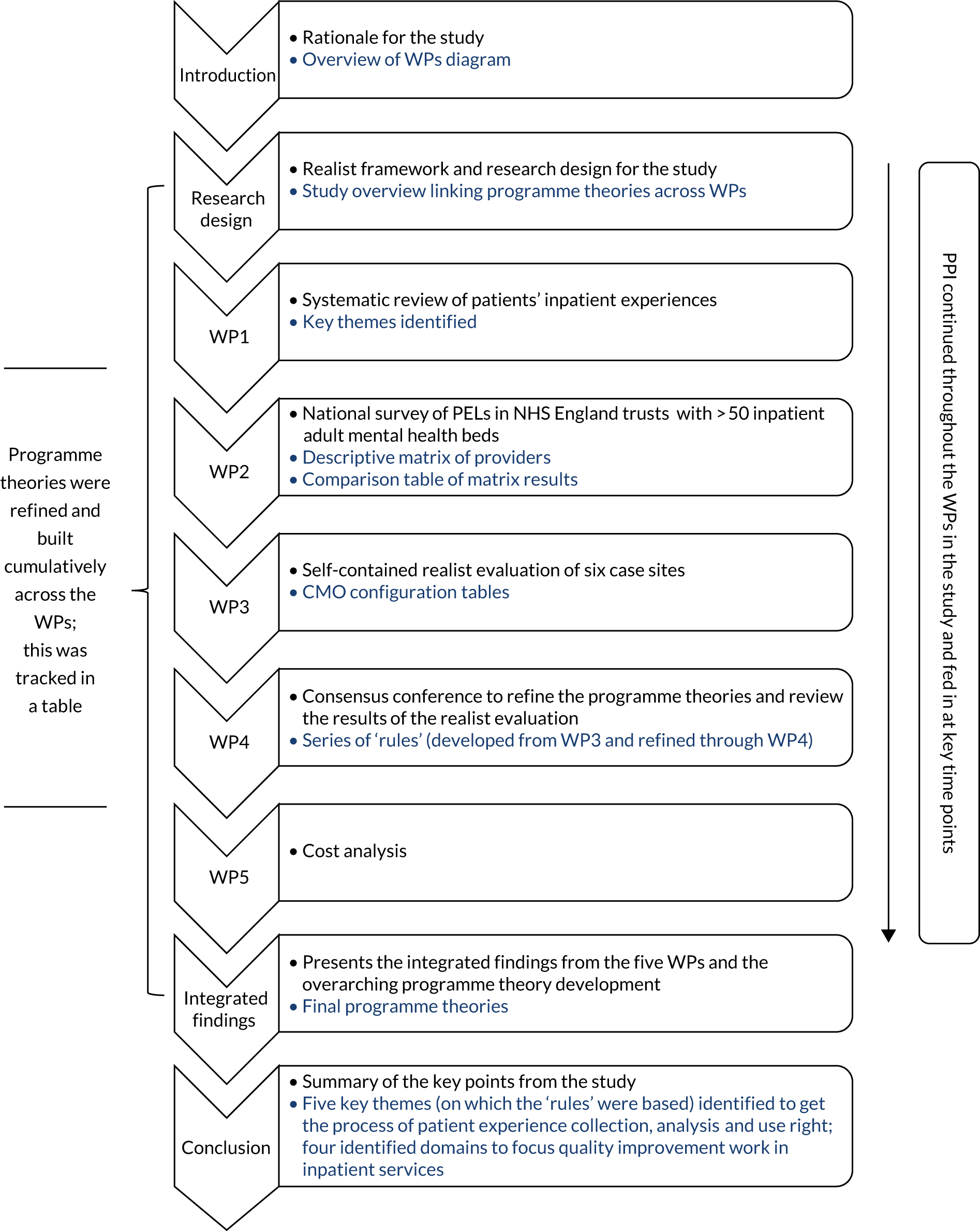
The EURIPIDES study was underpinned throughout the five WPs by a realist research design. Although the five WPs were discrete and self-contained, each was designed to feed successively into the understanding of the others. Nested within the research design was a self-contained realist evaluation (WP3). In this way, there is an underpinning realist philosophy and thread running through all of the WPs contained in this study (Figure 2).
FIGURE 2.
Overview of the chapters contained in this report to show how programme theories are linked across the WPs (in blue are the data that were used to develop and refine the programme theories). CMO, context–mechanism–outcome.
How does the realist research design underpin the work packages?
The ambition of realist research is to understand and analyse the ‘mechanisms and structures behind phenomena’. 34 It builds on the work of critical realists such as Bhaskar and Danermark. 35 In the field of health and social policy, Pawson and Tilley36 developed the realist evaluation approach to move from successionist models of causation in evaluation (which ask does this intervention or programme work?) to consider generative causation in evaluation, instead asking what works, for whom, in what circumstances and why?
Realist evaluation is a way of evaluating a particular programme in context, which, in our case, was the use of patient experience data in adult inpatient mental health settings in NHS England. The purpose of the method is to refine the understanding of how a programme or intervention works in a particular setting. Realist evaluation is theory driven, starting and ending with programme theory.
What do we mean by programme theory?
Programme theories explain how a programme or intervention works. They embody what the problem is, what the solution might be and how this is hypothesised to bring about change, and so encapsulate ideas about causation. Programme theory should not be so specific that it explains things only at the individual level and should not be so abstract that it is generally applicable.
Programme theory is a ‘middle-range theory’ that helps to explain in what ways and how a programme or intervention may or may not be operating successfully in particular circumstances for particular types of actors. Initial programme theory can be developed in a range of ways. In our study, the initial programme theories were based on previously published research, practice knowledge and lived experience. These explanations about how the programme or intervention works were drawn from published literature, practitioners, people with lived experience of mental illness and distress, and the NIHR funding call. We used these initial programme theories to develop the research proposal. These were then refined throughout the study, based on the outcomes of each WP.
What do we mean by generative mechanisms?
Programmes or interventions work or do not work as a result of different individuals responding (or not responding) to that programme or intervention. These responses result in different patterns of outcomes. The biological, psychological or social drivers underpinning each individual’s response are referred to as generative mechanisms. 37,38
Mechanisms are likely to operate at different levels of a system, over different time scales, and to involve interactions that may not be observable. If we define mechanisms in relation to the response of individuals to a programme or intervention, there are only a finite number of ways in which they can respond (e.g. in respect of the experience of inpatient mental health care, trusting staff or feeling disempowered). These responses are commonly recognised as (observable) aspects of human behaviour; however, what is not clear is how these responses are triggered by particular aspects of programmes or interventions in specific contexts. It is not just high-level mechanisms such as trust that we need to understand, but we also need to understand how the programme/intervention works in triggering individual responses that are characterised as the experience of trust.
Realist evaluation and context–mechanism–outcome configurations
Realist evaluation is operationalised through developing context–mechanism–outcome (CMO) configurations. In realist evaluation, outcomes are understood as the product of the context and mechanism. For example, trust may be an obvious mechanism in relation to patient experience; however, how that trust becomes activated (or not) in the inpatient setting is less clear. Understanding this is the work of realist evaluation. 39,40
The ‘context’ of realist evaluation is significant, as it can influence reasoning and behaviour, and it is the context that ‘activates’ (through the circumstances being right) mechanisms and that influences if, and if so which, mechanisms operate. 36,37 Outcomes are contingent, therefore, on both context (which may provide alternative explanations of different observed patterns of outcomes) and mechanism (based on the reasoning and resources38 of actors).
The development of CMO configurations helps to understand both proximal outcomes (which are more immediate and the result of generative mechanisms being activated in relation to the reasoning and resources of actors) and distal outcomes (which are more slowly developing patterns that are observed and built, often from the accumulation of proximal outcomes).
In this study, the outcome being examined was the collection, analysis and use of patient experience data in order to change services, and linked to quality improvement strategies in adult inpatient mental health settings in NHS England.
Evolution of the method: our approach to realist evaluation – laminations and the inverted case study
Realist evaluation has developed since its inception over 20 years ago and is increasingly being adopted to study complex health-care systems. As a result of the diverse approaches to realist research, reporting standards for realist evaluation were developed. 41 This study has paid close attention to those standards.
However, to conduct a study with multiple WPs and an overarching realist research design (including a nested realist evaluation), the programme theory was developed and refined iteratively across the WPs as the study progressed. Two key additions also were made to evolve the realist evaluation approach:
-
taking a laminated (multilayered) approach to understanding cases
-
undertaking analysis using temporal sequencing.
What do we mean by laminations in case study design?
In a classic case study design, a case would be clearly bounded as a unit of analysis and viewed as embedded within a wider system,42 and extraneous factors are viewed in relation to their impact on that case. If utilising a classic multiple case study research design, one would compare distinct and bounded cases. 43 Each case would be discrete and the comparison would take place between cases (Figure 3).
FIGURE 3.
Classic case study research design comparing between cases (adapted with permission from Fenton44).

We adopted a different type of case study research design using the idea of a laminated system43,44 with defined, distinct levels of agency. We operationalised the idea of laminations in our research with the individual- or biographical-level experience understood as patients or carers, the micro- and small-group-level understood as staff working on the wards, the meso-level understood as corporate staff including PELs and senior managers in trusts, and the macro-level understood as policy-makers and organisations responsible for collecting nationally mandated patient experience feedback (Figure 4). Research interviews were conducted across these laminated levels (WP2 and WP3).
FIGURE 4.
Inverted case study research design comparing across and within the laminated structure (adapted with permission from Fenton44).
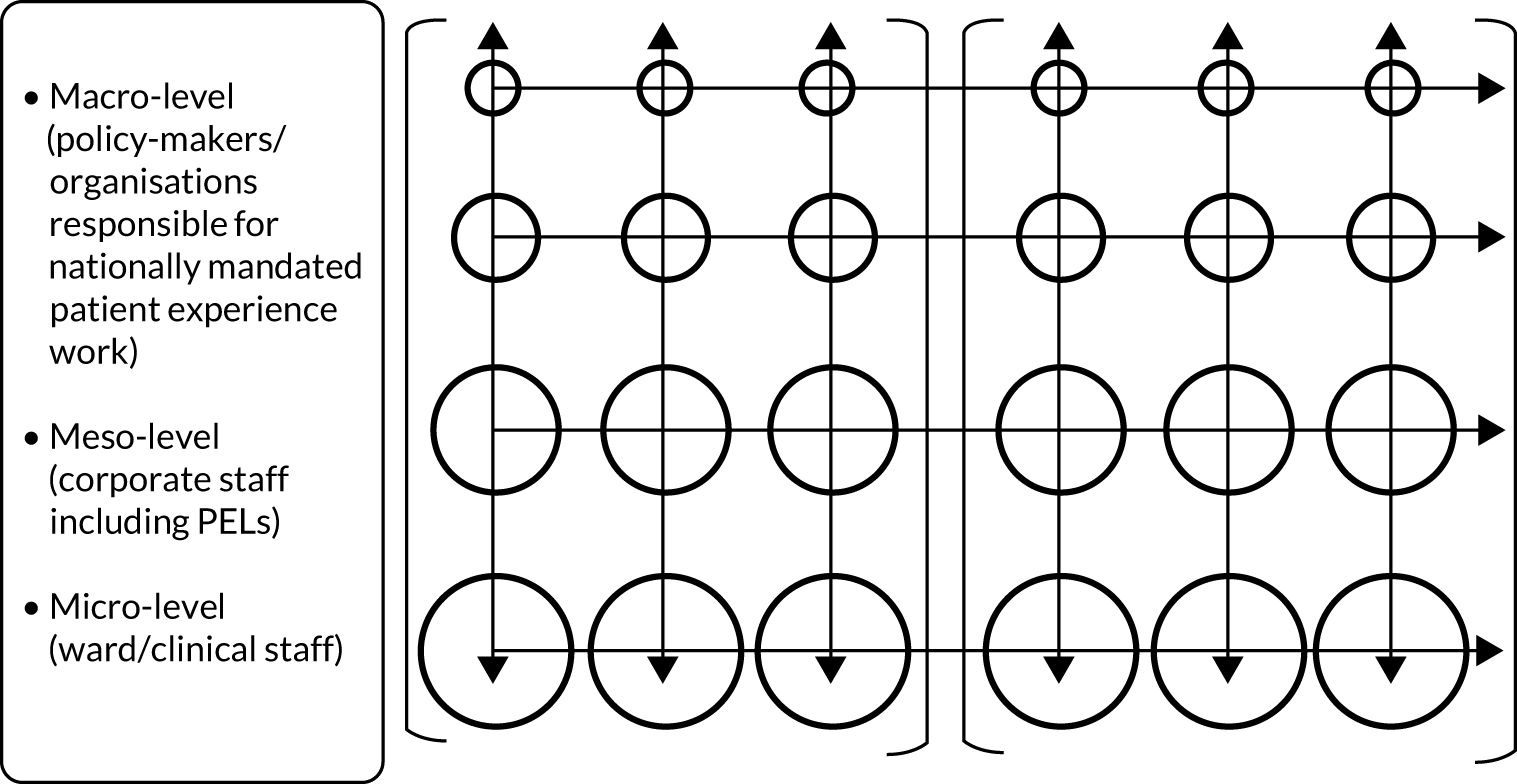
To utilise the concept of laminations within a realist evaluation framework, we undertook research in these sites (WP3) to explore and understand the generative mechanisms operating within and between laminations in each of the case sites. 44 This approach enabled us to read down and through those laminations to understand the generative mechanisms being activated (or not) at different levels in case sites, and facilitated reading across the case sites at the level of each lamination to understand the reach and impact of extraneous factors.
The rationale for using this particular research design was twofold:
-
Rather than use a lamina (or level; interviews with inpatients, for example) as a window into those patients as the object of study, we used those interviews as windows out onto the wider system. While we used context to inform our understanding of generative mechanisms, we privileged narratives at the different levels identified. This makes it is easier to determine what contributes to middle-range theory and to determine those generative mechanisms that are particularly context driven and so relevant to specific case contexts.
-
Case studies traditionally have strong internal validity but suffer from weak external validity and generalisability from the case to the wider population. 42 In our approach, although cases were identified and bounded, we were able to read within levels across case sites to explore what features of a programme or intervention are common to everyone at that laminate level and what features are contextually driven and unique to the case. 44 This strengthened our external validity, without compromising or weakening our internal validity.
How was temporal sequencing introduced to realist evaluation?
Using inpatient experience feedback to improve the quality of care has an embedded temporal sequence, which forms part of the context for our realist evaluation. We brought this into our realist analysis through using a temporal coding framework: collecting, receiving, analysing, implementation and change (see Report Supplementary Material 10).
We adapted and developed these laminated and temporal additions to our realist analysis to ensure generative mechanisms were not identified at too superficial a level to be useful and to understand how combinations of different actors’ reasoning and different contexts interacted to produce different patterns of outcomes.
Ethics approvals for the study
Ethics approval was obtained for this study from the West Midlands (South Birmingham) NHS Research Ethics Committee [reference number 16/WM/0223, Integrated Research Application System (IRAS) project identifier 181897]. The systematic review (WP1) was registered as PROSPERO CRD42016033556.
The research posed ethics issues primarily through the research activity of WP2 (the national survey) and WP3 (the realist evaluation of case study sites). There were ethics issues identified in relation to ensuring anonymity and that adequate consent has been obtained, working with participants who may be identified as being a vulnerable group owing to their mental health issues and minimising possible distress of participants when interviewing.
To address these issues, participants’ details were anonymised and interviews were anonymised prior to transcription and given a unique identifier. Participants were initially approached by a member of clinical staff for permission to share contact details with the study team. Written consent was obtained from all individuals participating in the study and we did not interview individuals who lacked capacity. Taking part had no impact on clinical care and there were no repercussions for not taking part; participation was entirely voluntary. If it had been required, the use of qualified and trained interpreters would have been offered and provided during the interview. A procedure was put in place for managing whistleblowing and disclosure.
In addition, we recognised that, when discussing the experience of being asked about inpatient mental health services, this could have triggered an emotional response from participants during WP3. Although these interviews were not intended to elicit detailed accounts of individual service user inpatient experience, it was likely that sensitive issues such as perceived coercion, a lack of privacy and difficult discharge procedures would be touched on. We therefore provided participants with information about sources of support. A senior member of the project team supervised the research fellow (RF) and research associates (RAs). The survivor researchers had an identified supervisor to access for support through the Mental Health Foundation (MHF) and were supported in the case sites by the RF.
To train, manage and support the research staff, a comprehensive lone-working, disclosure and whistleblowing policy was devised. The RF trained both the RAs and the survivor researchers in these protocols and offered supervision and support to them while they were interviewing. Any disclosures were immediately reported to the RF, the chief investigator and, if appropriate, the NHS trust. Staff were given time out after difficult interviews if they needed it, and a daily debriefing or check-in with the RF took place to provide emotional support and to keep a log of any lone working. To ensure that the RF and whole research team were supported, weekly supervision meetings were held with the WP3 lead, the chief investigator and the RF when undertaking the case site research. In addition, group meetings to review case site data and to discuss issues and emergent themes took place between the WP3 lead, the RF and the RAs.
Chapter 3 Patient and public involvement in the EURIPIDES study
Introduction
The aim of the EURIPIDES study was to understand which of the many different approaches to collecting and using patient experience data are the most useful for supporting improvements in inpatient mental health-care settings. To ensure that the patient voice is heard, NHS trusts are required to collect feedback from patients and, in some cases, they have spent years setting up local systems for this. The project aimed to identify the kinds of feedback that are most important, the management processes needed to translate feedback into effective action plans and if this makes any difference to patients themselves. The study was developed in partnership with the MHF, which led the PPI aspect of the work. Our PPI strategy aimed to ensure that mental health service users (and carers) were genuinely and meaningfully involved at all stages and levels of the research process using for the ‘4Pi’ national standards service user involvement in research45 (Box 1).
In this chapter, we describe and report on the effectiveness of PPI in the EURIPIDES study. We followed the Guidance for Reporting Involvement of Patients and the Public 2 (GRIPP2) long- and short-form guidance checklists for reporting on involvement46 (Box 2 and see Appendices 19–22) to structure this report.
This chapter was written by David Crepaz-Keay (MHF) who co-ordinated PPI in the study, Michael Larkin (EURIPIDES Project Oversight Group) and Emma Ormerod and Stephen Jeffreys (survivor researchers). We are grateful to Sarah-Jane Fenton (RF), Lizz Kimber and Nicole De Valliere (Master of Research students, University of Birmingham) for their contributions.
-
Principles: how do we relate to each other? Meaningful and inclusive involvement starts with a commitment to shared principles and values.
-
Purpose: why are we involving people? Why are we becoming involved?
-
Presence: who is involved? Are the right people involved in the right places?
-
Process: how are people involved? How do people feel about the involvement process?
-
Impact: what difference does involvement make? How can we tell that we have made a difference?
-
Aim: report the aim of PPI in the study.
-
Methods: provide a clear description of the methods used for PPI in the study.
-
Study results: outcomes – report the results of PPI in the study, including both positive and negative outcomes.
-
Discussion and conclusions: outcomes – comment on the extent to which PPI influenced the study overall. Describe positive and negative effects.
-
Reflections/critical perspective: comment critically on the study, reflecting on the things that went well and those that did not, so others can learn from this experience.
Involving service users and carers
The EURIPIDES study was designed with two forms of PPI at its core: first, by employing survivor researchers as co-researchers alongside the RF and RAs during the data collection phases of the project and, second, through the recruitment of a PPIT. The group was referred to as the Service User and Carer Reference Group for the duration of the project. However, the group told us that they felt uncomfortable with the term ‘service user’, as they felt that it implied ‘drug user’. They asked to be referred to as the PPIT in publications and this is how we refer to them in this document.
During the development of the original grant application, the MHF hosted a development meeting of three survivor researchers, the proposed PPI lead and the principal investigator. This group set out the initial approach to PPI across the study. The original plan proposed three layers of PPI: a co-investigator as a member of the project leadership team who was a survivor researcher with overall responsibility for PPI across the study; a team of four survivor researchers who would contribute to data collection and analysis; and a PPIT, comprising people with personal experience of inpatient care or of informal caring.
Patient and public involvement team
The PPIT comprised people who were unlikely to have prior experience of, or involvement with, research, but were experts by experience, having had historical or recent experience of adult mental health inpatient admission or of informal care for someone who had been an inpatient.
We aimed to recruit 8–10 PPIT members through the MHF’s extensive network, ensuring that the group included a degree of diversity with respect to age, gender, ethnicity and geographical location.
Our initial meeting was poorly attended, for a variety of reasons. Only two of the eight people recruited attended, with four sending apologies in advance and two failing to arrive owing to transport issues. After consultation with a number of the project team members and discussions with a service user and carer group, which met regularly close to the MHF’s London office (at a club known as the Dragon Café), we agreed to strengthen the PPIT with members from the Dragon Café. We also increased the payment offered to PPIT members and provided additional support to ensure that people were able to attend.
This led to a much stronger attendance at subsequent meetings and, because the new members knew each other, the PPIT immediately gelled as an entire group. There were a number of consequences of this approach. We sacrificed some geographical diversity (the vast majority of the PPIT were from London, with one regular attendee from the West Midlands and one from the south coast), but we increased ethnic and age diversity. We also increased the number of people involved who had current or very recent experience of inpatient care. Only a small proportion of the group had any experience of PPI in academic research.
We therefore increased support to ensure that the PPIT meetings were accessible for the participants. Initially, we proposed that there would be four PPIT meetings during the lifespan of the study. It became apparent after the first meeting that there were ways in which we might be able to do things differently and more meaningfully. PPIT members gave feedback after the first meeting and it was clear that, to make the most of their expertise, we would need to take more time to get know each other and we would need to plan our meetings more creatively (and with much less paper). As a consequence, we held seven PPIT meetings over 2 years. The format of these meetings was innovative and the benefits were significant. Adaptation enabled more equitable and honest engagement that allowed the PPIT to challenge the research team about the data and ways of working.
Some members of the PPIT found it difficult to maintain concentration, some were less confident with literacy and technical language, and some were voice hearing. There were periods over the 2 years of the study in which people were re-admitted to inpatient units or suffered significant life events. We worked to ensure that nobody felt left out or left behind. We adapted our approach to ensure that everyone was able to participate at the level they felt was appropriate. We used role play and small group discussions and we built in time for plenty of breaks and sandwiches. We visited the group in locations familiar to them outside the formal meetings to ensure that they had space for reflection and to ask for changes or updates ahead of the next meetings. This enabled us to engage people with no prior research experience.
A link worker at MHF (Jo Ackerman) supported the group outside the meeting times to ensure that there were opportunities for everyone to articulate their own opinions, both during and outside meetings. We ensured that travel arrangements were as simple as possible and that no one was left out of pocket on the days of the meeting. Together, we thought carefully about how to support the group in the context of their EURIPIDES study meetings. Working in this way has allowed us to be sensitive to disclosures and helped us to manage risk when it presented.
We began each meeting by demonstrating how the research had been shaped by the PPIT’s involvement (i.e. from changing the ways we interviewed and the tools we used, to implementing a coding structure that they helped us co-design). We also adapted our techniques of working with the PPIT to meaningfully include everybody and let them lead on the approach taken (i.e. through the workshop-style activities that included dramatisation and role play as opposed to reviewing textual materials). It was particularly important to be responsive to fluctuations in the group dynamics if people were unwell and to keep striving to engage people in a supportive way that was accepting of their individual situations. We co-designed (by asking how, in what ways and when they felt the next meetings should take place) the approach, not just the study, and we recognised their role as integral to steering the project.
The members of the PPIT played a critical role in the design of the research tools, in designing coding frameworks and in reflecting on the data throughout analysis. For example, they commented on the systematic review and they refined programme theories (the hypotheses we were testing), and their comments relating to the systematic review findings about what patients said about their experience were built into the interview tools for patients through a process of co-designing flash cards to support realist interviewing (WP3).
In addition, the PPIT chose the priorities for the ongoing research questions in their meeting forum and this shaped the entire data collection process. The PPIT also developed and refined our programme theories (the core work of realist analysis). This work refined our research questions and shaped the conduct of the fieldwork. The PPIT analysis workshop provided us with categories crucial to our data-coding. The impact of this involvement has been significant and it has led each planning and development phase of the primary data collection. Members of the PPIT attended the consensus conference and, to mark the end of the study, we hosted a celebration event to thank participants and recognise the enormous contribution they made to the EURIPIDES study.
Survivor researchers
The survivor researchers (who were people with lived experience of mental illness and its treatment who also held professional roles and had experience conducting research) were people who either had previously worked with the MHF or were recommended by the MHF. We adopted the term ‘survivor’ (rather than ‘patient’ or ‘service user’), as this was preferred by the individuals concerned.
The intention was for survivor researchers to be involved in the study by (1) advising on the questionnaire, topic guide and recruitment materials and on selection of case study sites, (2) advising on all aspects of the conduct of WP3, including planning and undertaking interviews with service users and (3) recruiting service user and carer participants and acting as facilitators at the consensus conference (WP4).
Four survivor researchers were initially recruited to the EURIPIDES study team through the National Survivor User Network and MHF networks and were actively involved in the early stages of the research: advising on recruitment materials, topic guides and approaches to realist interviewing. However, we had a difficult start to the fieldwork, as gaining access to case study sites was complex and time-consuming, as was the bureaucracy around research passports. This contributed to communication issues with the survivor researchers and impeded involvement. In addition, two of the survivor researchers made the decision to withdraw from the study prior to the fieldwork. Once research passport administration issues had been resolved, the two remaining survivor researchers were involved in data collection at only two of the six case study sites.
As the project progressed, we were able to integrate the survivor researchers into the project. Survivor researchers were able to exchange ideas and perspectives during the last two site visits with other members of the research team and were also involved in two meetings to design and refine coding frameworks at the analysis stage. One of the survivor researchers (Emma Ormerod) also participated in role plays of some sections of the interviews for discussion at the PPIT meetings. Both survivor researchers were involved in the final stages of the research process and co-authored this chapter.
What was different about patient and public involvement in the EURIPIDES study?
Often, PPI is poorly understood and conceptualised. 47,48 At best, effective PPI can reduce the chances of health research being ‘wasted’ or disregarded,49 it can improve the outcomes and increase the success of a study,50 and it can also be an empowering experience for the people involved. 51 However, very little is known about the power dynamics, impact and influence of PPI48 and we were also aware that there can often be a significant difference between the rhetoric of involvement and the tokenistic reality. 52
The plans for PPI have to be acceptable to many audiences, including funders, researchers, user groups and NHS trusts. Throughout this study, we have tried to engage all levels and to follow principles of ‘co-production’ with regard to our PPI, whereby power and responsibility are shared at all stages of a project53 (Box 3).
-
Sharing of power: the research is jointly owned and people work together to achieve a joint understanding.
-
Including all perspectives and skills: make sure the research team includes all those who can make a contribution.
-
Respecting and valuing the knowledge of all those working together on the research: everyone is of equal importance.
-
Reciprocity: everybody benefits from working together.
-
Building and maintaining relationships: an emphasis on relationships is key to sharing power. There needs to be joint understanding and consensus and clarity over roles and responsibilities. It is also important to value people and unlock their potential.
Reproduced with permission from INVOLVE. 53
We believe that we have succeeded in some areas and that, as the study progressed, all members of the team began to communicate more effectively with each other and integrate the perspectives and skills of everyone involved. But we are also aware that there are areas for improvement that require further reflection and there are areas of learning that we can take forward for future studies.
We offer the following first-hand reflections from a survivor researcher and from the EURIPIDES study RF (on behalf of the study team):
Survivor researcher reflections (Emma Ormerod):
As a ‘survivor researcher’ it is often easy to feel that you have a curious hybrid identity that reflects the ongoing epistemological tensions between the place of ‘expert/professional’ knowledge and that of the experiential knowledge that is gained through lived experience of mental and emotional distress. At a personal level, it can lead to feelings of uncertainty and confusion about one’s role within and possible contribution to a research study. Other survivor researchers have also written about their ‘double identity’54 and the feeling that they sometimes ‘fall between the two stools: being too professional to be a ‘real’ service user and insufficiently academic to be a ‘real’ researcher’. 55
It is now widely recognised that the involvement of patients/service users, carers and other members of the public in research is vital. By including a diverse range of perspectives and experiences the intention is to shape and positively influence the research process and subsequent outcomes. However, as survivor researchers we know that sometimes this involvement continues to be tokenistic, that our contributions can often be limited to advisory roles, and that many people continue to be marginalised within processes of involvement in research.
As survivor researchers in the EURIPIDES project team, we brought our skills and experiences as researchers, our lived experiences of mental distress and secondary mental health community services (including day services), together with our own experiences of user involvement and feedback-gathering initiatives as both service users and researchers. We were increasingly involved in the research process as the project progressed. But rather than attempting to define our role as survivor researchers in isolation, it might be more helpful to reflect on this as one of the perspectives within a collaborative knowledge-making process, so that understanding the contribution of researchers with lived experience of mental distress becomes ‘not just a question of “what difference do they make?” but an interrogation of how who we all are, as academics, clinicians and service users, shapes the knowledge we produce’. 56 During the course of the research process we began as a team, however informally, to reflect on our own identities, to recognise their multiple and complex nature, and move towards a more equal place of collaborative knowledge-making. It is our hope that future studies will foreground this approach.
The research passport process took longer than anticipated and we spent some time waiting to hear when the data collection would commence. On enquiring, we discovered that because of the administration issues, fieldwork had already commenced without the involvement of the survivor researchers. It was disappointing and concerning to feel ‘out of the loop’. Once research passports had been approved, there was very little time to work with the team (who were already working at case study sites) in order to prepare for interviews or explore issues regarding how the service user/survivor experience could be brought to the interviewer role (e.g. how and when to foreground this in interviews and what the anticipated effect might be).
Due to the knock-on effect of the administration and communication issues, one of us considered withdrawing from the project, but decided to attend the next meeting at the case study site to see how things progressed. Once we met with the other members of the research team and started building relationships with them, these fears around communication were allayed. Despite the initial difficulties, we appreciated the close working relationship with the other members of the research team once on site and their commitment and willingness to share their experiences from earlier sites. We were able to talk informally with them which allayed concerns and enabled us to ‘hit the ground running’.
The two of us only worked on one case study site each (both ‘green’ sites scoring most highly in the survey of mental health inpatient providers). This meant that it was not possible to make effective comparisons at the analysis stage. Both of us conducted interviews with members of the research team, but only one of us moved on to solo interviewing due to a practice of mentoring researchers on their initial interviews and a shortage of recorders.
We noted that there were contrasting areas of worry/concern between the research team and survivor researchers as we began the fieldwork. The research team were extremely careful not to impose themselves on or get in the way of ward staff, but as survivor researchers we noted that this approach was sometimes at odds with how we wanted to position ourselves on the wards (i.e. less deferentially) which may have arisen from our own service user experiences. The research team were also keen to provide us with as much support as we needed and were understandably concerned that we might be affected by the emotionally demanding nature of the fieldwork including possible disclosures from interviewees. However, we were more concerned about practical matters such as travel arrangements, getting up early, etc. As we began to build relationships with the team it felt easier to explain that, for example, for one of us, travelling to and from the case study site was a much greater cause of anxiety than the interviews themselves. Once this had been explained, other members of the research team were very supportive and practical arrangements were put in place to assist with this.
Reflections on behalf of the EURIPIDES study team (Sarah-Jane Fenton):
There were two core components to the PPI work undertaken within the EURIPIDES study, both of which strengthened the overall quality of the study. There was a reference group of people with lived experience of adult inpatient environments who did not have research backgrounds and most of whom had no prior experience of research, which was complemented by survivor researchers who had specific expertise in relation to research activity. It would not have been possible to conduct or complete the study in the way that we did, nor to such a high standard, without this dual strand involvement.
As the RF on the study, I was responsible for being the link person between the two groups alongside colleagues from the MHF. For the PPIT reference group, having a link contact person (Jo Ackerman) to manage the relationships outside the formal meetings based in the MHF really helped to offer an easily accessible point of contact for individuals in between meetings.
Reflecting on what else worked well within the reference group, I felt it was the establishment of clear boundaries at the start and end of each meeting, particularly around signposting people safely to supports and both recognising and not diminishing distress (for example, addressing suicidality when it was presented in meetings), which created a supportive and safe space enabling everyone to contribute. In addition, it was extremely important to be responsive to the different literacy levels and sensitive to both an individual’s reported physical and mental health needs and the wider group dynamics.
It would be easy to create a long list of things that seem obvious in relation to facilitating group work: good communication, clear boundaries, establishing a clear purpose for each meeting, listening, responding to the needs of the group, etc. However, really what has stuck with me over the course of working with the group was the need to allow them to lead and manage as much of the process as possible. Whilst I was clear what the tasks were we needed to achieve in relation to the research at each time point that we met, letting the group determine how we would work on those tasks, letting the group dictate the pace and flow of the meetings, and letting the group challenge and hold us accountable for how their hard work was shaping the study was the real strength in the work.
It was this power-sharing (for a group who had experienced a great deal of disempowering practice), underpinned by all the other good group work practice, that generated or activated underlying mechanisms of trust that led to outcomes of authentic engagement and enjoyment of the co-research process. Being a genuine member of the wider research team, and everyone recognising that each person has a different role to play, was integral to the success of the PPI work.
This underpinning philosophy of mutual respect and shared goal-setting was equally important with the survivor researchers. We did not start off the piece of work together here so well, and there is learning to be drawn out of those earlier less helpful interactions. Despite that, the contribution made by both the research team and the survivor researchers when we did get up and running was unique and powerful. Survivor researcher involvement should not be limited to ‘interviewing the patients’ – but actually their expertise should be woven throughout the study meaningfully as researchers in their own right. The survivor researchers in the field were treated no differently to the research associates – we debriefed together, ate together, travelled together, talked and discussed ideas together. Whilst each of us knew our role and there were clear lines of accountability, it was a team effort and we knew we could trust and rely on the other. This reflexive way of working meant that if people needed to step back or had a particularly difficult experience on the wards, another of us would step in. It was just a more humane way of working with what at times can be a difficult and distressing subject matter.
We adopted this inclusive, supportive approach across the PPI work – departing from the model set or agreed with the funder, and trying out new ways of working. I am grateful to the chief investigator and the wider Project Oversight Group for agreeing this new flexible, innovative way of working, because it genuinely opened up the space for real collaboration and appreciation for everyone’s involvement. It resulted in there being no involvement that was tokenistic or wasted – everything discussed or done together was built consciously back into the study, changing and shaping the way it developed.
Limitations
There were also limitations to the PPI work undertaken in the course of this research. During the early stages of the project, it may have helped with communication and mutual trust to have spent additional time getting to know each other by sharing different perspectives and experiences. It may also have helped for the whole team to have met together (PPIT, survivor researchers and other members of the research team), as this did not happen until the later stages of the research process. For example, when some members of the PPIT met one of the survivor researchers at a later stage in the project, they expressed surprise at realising that service users can also work as researchers (i.e. that some use their own experiences as part of their work as ‘survivor researchers’ and others work as researchers but choose not to integrate their experiences into their research work). Discussions of this nature may have been encouraging for some members of the PPIT, in addition to acknowledging that research skills can be obtained through various means – not just postgraduate and doctoral routes.
Time constraints and limited involvement in fieldwork prevented the survivor researchers from developing their approaches to realist interviewing informed by their own lived experiences of mental distress. The two WP3 case study sites where the survivor researchers were involved were ‘green-rated’ sites that had scored most highly in the WP2 survey of inpatient providers. As some interviews were conducted jointly (with other study researchers) as well as independently, we were unable to fully assess the extent to which specific interview dynamics between interviewee and researcher with lived experience might have shaped the study findings. This is something that could be reflected on as part of a collaborative research process in future projects.
Evaluation summary
Michael Larkin and Elizabeth Newton (EURIPIDES Project Oversight Group members) and Lizz Kimber and Nicole De Valliere (postgraduate research students) conducted a subsidiary research project to evaluate the acceptability and development of the PPI component. This evaluation focused on the engagement and role of the PPIT and it aimed to identify barriers to and facilitators of involvement in the EURIPIDES study, and to provide us with a basis from which to reflect on what we had learned by working together. A full report will be published subsequently, but the following represents a brief overview.
Full ethics review was sought, and approval was received, from the Life and Health Sciences Ethics Committee at Aston University, Birmingham, where Michael Larkin is registered as principal investigator for this subproject.
Sampling
We invited members of the PPIT, members of the research team most involved in working with the PPIT, colleagues from the MHF and the survivor researchers to take part in these research interviews. Potential participants were given the option of taking part in a one-to-one interview or a group interview.
Data collection
At a pre-evaluation meeting with the PPIT, we co-designed a timeline for the project, which captured memorable milestones. We subsequently developed an interview guide around this timeline. The interview guide explored people’s experiences of being involved with the EURIPIDES study and also asked about key barriers to and facilitators of people’s involvement, drawing on a structure commonly used in critical incident technique interviewing.
Interviews with PPIT members were conducted by Michael Larkin and Elizabeth Newton. The remaining participant groups were interviewed by Lizz Kimber. Twelve interviews were conducted; two of these were group interviews. A total of 18 people took part, with representation from each of the four stakeholder groups. All interviews were audio-recorded, transcribed in full and then anonymised.
Data analysis
We used template analysis to code and organise the data. A template in this sense is a set of categories or headings for organising the content of the data. In template analysis, preliminary templates can be developed using an existing framework or they can be developed from exploratory coding of the data. We took the latter approach and we had the luxury of independent coders to help us with this. Nicole De Valliere began coding the interviews conducted with PPIT members (six transcripts) and Lizz Kimber began coding the remainder (six transcripts). When each coder had completed three transcripts, they shared their developing template structures with Michael Larkin, who produced a merged template structure. The remaining interviews were coded according to the structure of this preliminary template. The template was further refined and developed during this stage. The final template structure is detailed and complex, and can be used as the basis for identifying cross-cutting themes. In subsequent reporting, we will take this approach. For the purposes of this document, what follows is a more ‘concrete’ focus on barriers and facilitators.
Analysis
Getting involved gradually
Participants from the PPIT reflected on the gradient of their involvement. To begin with, it was ‘a bit hard to take in, it was a bit complicated’. They described getting to grips with their role, getting to know the study team and coming to an understanding of what the study was about. They described how the study became ‘a constant’ for them. This was positive: a reliable break from other routines and an enjoyable experience. It soon entailed a commitment: ‘[i]t’s a commitment, and it means “yes” all the time. I’ve got my (other regular group activity). I should’ve gone. We told them we couldn’t go today. This has become more important than that.’
Different kinds of contributing
The participants also described ways in which they had contributed, emphasising particularly their role in helping the researchers to understand the problem they were studying: ‘I’ve made them feel informed’. When they did this, they grounded their claims in the value of their experiential insights: ‘I think we’ve all got that experience . . . We could share what we knew about it.’
In addition, PPIT members reflected on other contributions, such as group facilitation (‘I hope that, from time to time, I’ve put forward an idea that might get people moving together to get a consensus’), problem-solving (‘[i]t’s [trying to reconcile the range of views within the group] sort of quite infuriating sometimes, but it’s also very interesting’) and data analysis (‘[w]e went through the interviews . . . we picked out themes that were important’).
One issue that merits some reflection is that some PPIT members seemed to be unclear about the connection between research and practice. There was a tendency to overestimate the speed and directness with which their input might change practices. There is a difficult balance to strike between presenting PPI as a genuine opportunity to make a difference (which it can be) and the frustratingly slow process of translating research insights into practical or political change.
Challenges to contributing
Some of the things that made contributing more difficult were simple practical issues, which research teams can easily resolve if they are prepared to adapt: confusing or complicated concepts, being presented with too much information and a lack of clarity about the PPI role or the research process. Others issues were relational. There was a lot of material about the atmosphere and environment on the first (unsuccessful) meeting, for example. One participant described a ‘quite daunting’ atmosphere, with the group spaced out around a ‘massive table’, listening to strange people talk ‘in quite lengthy terms’, and then said: ‘[a]nd I was sort of sweating and shaking. I’m like “What have I let myself in for?”.’
Some of the relational issues were about getting to know the group. Several participants reflected on the challenges of speaking in large groups. It helped that many PPIT members knew each other, either from the Dragon Café or other activities, but not everybody did, and they also had to get to know the research team and MHF workers. In addition, they were mindful of treading on toes: ‘I think carers have to be very, very careful not to speak for service users’.
Personal factors could also be a barrier at times. A generic issue was the background phenomenon of stigma and personal history. One participant reflected on having to get used to the novelty of being asked for their opinion, for example: ‘[be]cause, by and large, having lived experience of mental health that has you down, and makes you cowed’. Others talked about more specific or intermittent difficulties (such as getting worked up by a particular issue or getting side-tracked) and life events (such as getting sectioned and missing a meeting).
Facilitators of contributing
Factors that helped with involvement were often driven by the motivation to make a difference. Participants described wanting ‘to break down the taboo’, ‘to put across the real’, ‘to help people’ and ‘to improve mental health’. Many people reported very upsetting inpatient experiences (‘[y]ou had to fight to protect yourself’), so the topic was very salient for them. This went hand-in-hand with the appraisal of the research as worthwhile or important: ‘[i]t can change things’.
Practical details such as travel arrangements, appropriate payment and appropriate refreshments were still important (‘[t]hat sort of thing has helped’ but ‘[w]e don’t come here just for the money’). The research team and the MHF participants reflected on the considerable amount of planning and communication that went on to build the right team to support these activities, to get all of the practical details right and to maintain a positive experience for the PPIT.
Some of the above-mentioned relational and personal barriers were overcome because the research team created an environment that felt comfortable (‘welcoming, friendly’, ‘easy going and relaxed’, ‘they’re all calm’, ‘we’ve been treated with respect’, ‘very caring’) but sustained a clear focus and purpose (‘it’s a general discussion’, ‘it’s a structured environment’). In part, this was achieved by stepping outside the routine day-to-day world and coming to the university: ‘[i]f we was in London, and we was talking about this, I don’t think we could be so relaxed. It’s a different environment and we can speak about what we speak about.’ In part, it was achieved by academics offering a different form of professional interest (‘[w]e know that what we said can be trusted. Some places you can’t be trusted – on the wards, cause they say they’re assessing you.’). The participants from the research team described how they had tried to promote equality and offer engaging ways of working. PPIT members were positive about the range of ways to contribute (‘[w]e talked all about it, everybody, and then we changed, swapped and went round over to other people and it was a different experience. It was brilliant.’).
The sense of the group as a group of friends, with a shared purpose, began to cut through worries about group dynamics: ‘[h]aving my friends around me, who also have been going through the same things I’ve been going through, it kind of makes you feel it’s a family’. Positive feedback from the research team about how the PPIT contributions were being taken forward was appreciated (‘[t]his is what you did last time – that’s been important and useful’). Efforts by the team to make sure that everyone had a chance to contribute were also noticed and valued. Honest feedback was appreciated in all quarters and all participant groups described times when it had been provided in a helpful way.
Summary
A more detailed analysis is required, but our initial evaluation highlights the importance of research teams being flexible and for this to be understood and supported by funders and other partners. The PPI component has made an invaluable contribution to the conduct of the EURIPIDES study and it would appear that this has largely been a positive experience for the people involved. These are both excellent outcomes, but they are a consequence of effective adaptation more than a consequence of our initial plans.
Issues with the employment of the survivor researchers (outlined in the previous section) were relatively difficult to resolve, because it proved difficult for partner organisations (and particularly NHS partners) to adapt quickly. By contrast, the problems at the beginning of our PPI programme were resolved quite quickly, because we were supported in responding flexibly to the feedback we received.
What did we learn and what would we recommend?
The EURIPIDES study afforded many opportunities for us to learn what is needed for effective PPI. We would summarise our learning as follows.
Commitment to principles
To ensure that involvement is genuine and meaningful rather than tokenistic, it needs to be taken seriously, both in principle and in practice. It is important to have a clear understanding of and commitment to shared principles of involvement from the outset. We aimed to do this by using resources such as the 4Pi national involvement standards,45 which is a framework for good practice developed by service users and carers themselves. However, we could have spent further time exploring the purpose of involving people with lived experience, particularly with the survivor researchers in relation to issues such as disclosure of service use and the extent to which interview dynamics between interviewee and researcher with lived experience might be present or potentially contributing to the kinds of knowledge produced.
Appropriate resources need to be allocated to PPI work for it to be effective. We realised that, to support the work of the PPIT, we needed to hold more meetings than were originally planned. We also needed to develop ways of supporting the group outside meetings and the PPI work itself (e.g. by arranging visits by team members to the Dragon Café in London and ongoing support from the link worker at the MHF). Although there are often many competing priorities, when making resource allocation decisions it is important to prioritise these principles of involvement when negotiating funding and spending.
Diversity of experience
Although our initial aim was to ensure that PPIT members included a degree of diversity with respect to age, gender, ethnicity and geographical location, issues with recruitment meant that, ultimately, the majority of PPIT were members from the Dragon Café in London. The benefits were substantial in that there was already a degree of mutual trust and understanding between members, which meant that it may have been easier for them to be open during discussions and to disclose experiences. The Dragon Café was also a place to meet the group members where they felt comfortable. However, it may also have meant that a narrower range of perspectives were represented in the PPIT (e.g. this was a very urban/London-centric group) and collective views may already have been consolidated around some issues.
Curiosity and flexibility
It is important to be curious and to listen to the feedback of everyone involved. What do people need or want to make involvement work for them? We discovered that these do not necessarily need to be ‘big things’, for example ensuring that information was presented in an accessible way without the need for paperwork, finding ways to ensure that people felt less anxious about travelling and accommodating preferences in relation to food and refreshments.
As the project progressed, we learned the importance of flexibility and the need to be responsive to other members of the team, even if this meant making changes to original plans. This meant that initial problems were swiftly resolved and it helped to build trust and relationships between the research team and the PPIT.
Communication
For people to be fully involved, communication needs to be open and transparent throughout the research process. This encompasses discussion of shared principles and values at the start of the project, establishing clear lines of communication and support, discussing boundaries and issues around disclosure, negotiating and clarifying roles for different parties, encouraging feedback from team members, etc.
We have acknowledged some of the initial difficulties with regard to communication with the survivor researchers and recognise that improved communication at the research passport and administration stage of the process would have helped to build trust and relationships. However, as the project progressed, all members of the team began to communicate more effectively with each other and integrate the skills and perspectives of everyone involved in the EURIPIDES study.
Sharing of power
The NIHR INVOLVE principles53 state that research needs to be jointly owned. People with a range of prior experiences need to be involved at all levels and stages of the research process. During the course of the study, we acknowledged the importance of sharing power and letting the PPIT lead and manage as much of the process as possible (e.g. with regard to how we worked on tasks and the pace of meetings). Involving and including everyone required a degree of flexibility and creativity and the methods we used were different at each stage in the research process (e.g. role playing sections of interviews for PPIT members to discuss emerging themes, which fed into coding frameworks).
Power-sharing also involves an explicit recognition that, although members of the team occupy specific roles on account of their research experience or their experience of mental/emotional distress, the reality is, of course, that people bring a variety of different overlapping experiences. Challenging hierarchies within research teams is vital for effective PPI and our learning outcomes for future projects would include the need for us to reflect together on our own identities and experiences to create knowledge in more collaborative ways.
Chapter 4 Work package 1: systematic review of patient experiences of mental health inpatient care
Background
Patient experience evidence is increasingly used to enhance the quality of health-care services and to ensure that such services are effective and acceptable to patients. Collecting, synthesising and using experiential data can provide a key way to enhance practice over time, drawing on evidence about what needs to change, for whom, why and in what way, to provide the highest-quality patient experience. 23,25
Mental health inpatients have reported both positive and negative experiences. 6,24,29,31,57,58 A review of mental health services in England by the Care Quality Commission (CQC) in 201759 highlighted a range of concerns about inpatient care, including poor design of buildings that did not meet patient needs, unsafe staffing levels and care provided some distance from patients’ homes. Such negative experiences contrast with the strong policy focus on strengthening the patient voice through care that is compassionate, provides choice and ensures that patients have autonomy and dignity. 1–3,6,7,60 With greater understanding of the key role of patient experience data in service development, NHS trusts routinely collect and use such data, with varying degrees of success. 59,61–63
Despite the focus on data collection, the difference such information makes to the quality of care is not always clear. 8 The quality of data collection methods has varied19 and there is no agreement about which dimensions of patient experiences are most important to users of inpatient mental health care. These and other challenges represent significant barriers to the collection and use of patient experience data in these settings. 8,9 This highlighted the need to identify the most important dimensions of the mental health inpatient experience, to inform our study of current practice in the collection and use of patient experience data to improve services.
Aims and objectives
Aim
The aim was to identify and synthesise evidence-based patient experience themes relevant to mental health inpatient care.
Objectives
The objectives were to systematically:
-
review studies reporting patient experiences of mental health inpatient services
-
identify patient experience themes and subthemes that are relevant to delivering high-quality inpatient mental health care.
Methods
Work package 1 was divided into two parts: a scoping study and a main systematic review. The scoping study was designed to inform the main systematic review by ascertaining the nature and size of the evidence base.
Protocol and registration
The systematic review was registered as PROSPERO 2016 CRD42016033556.
Scoping review
A scoping review was first conducted to ascertain the extent, range and nature of studies, to map emerging key themes without describing the findings in full or performing a quality check64 and to inform the main review. Six key authors known to be experts in mental health patient experience were contacted for new or unpublished reports and studies.
Patient and public involvement team
Draft themes from the scoping review were presented to the PPIT to ensure face and content validity and to discuss gaps in the research (21 September 2016). The PPIT comprised 10 people with experience of inpatient care or caring for someone who had been an inpatient and who had been recruited by the MHF. Members of the PPIT were invited to two consultation meetings for the purpose of the review. The first meeting was to discuss the research team’s early familiarisation with the literature exploring the themes identified in the scoping review, to obtain their views on these and to add further concepts that PPIT members felt were important but that had not been identified from papers. The second meeting was to discuss the themes identified from the systematic review, to obtain PPIT members’ opinions on these and to identify perceived gaps in the literature. Both discussions were important for assuring content and face validity of the subthemes and themes. Public involvement in this WP is reported in Appendix 19 using GRIPP2.
Identification of studies for the systematic review
The themes that emerged from the scoping review guided the development of search terms and the search strategy for the systematic review. These were applied to MEDLINE, the Cumulative Index to Nursing and Allied Health Literature (CINAHL) and PsycINFO. An example of search terms and results are reported in Appendix 14. Reference lists of included papers were scanned. The search deviated from the protocol in that only three of five databases were searched owing to the large numbers of abstracts retrieved.
Inclusion and exclusion criteria
All study designs were considered if papers included experiences of current or former inpatients of mental health institutions. No restrictions were applied based on country. Articles were included if they reported primary research, were peer reviewed and were published in English between January 2000 and January 2016. Papers were excluded if they were not primary studies, were based on pre-2000 data, included children and adolescents (aged < 18 years) or were not in English. When study participants included both inpatients and outpatients, only data regarding inpatient experiences were extracted. Reviews (see Report Supplementary Material 1) were noted and reference lists were scanned, but these were excluded from the review to avoid bias.
Study selection
Titles and abstracts were screened (by Carole Mockford and Greg Chadburn), of which 20% were independently cross-checked for agreement prior to obtaining full-text articles (Sophie Staniszewska and Carole Mockford). Full texts were obtained when the abstract was unclear. Any disagreements could be resolved by consensus (Carole Mockford, Greg Chadburn and Sophie Staniszewska), but no disagreements occurred.
Data extraction
The data were extracted to Microsoft Excel® (version 2013; Microsoft Corporation, Redmond, WA, USA), and included citation details, sample recruitment and research methods and findings related to key concepts; any other emerging concepts were added (Carole Mockford).
Quality and risk of bias in individual studies
The quality of included studies was evaluated using the Critical Appraisal Skills Programme (CASP) qualitative checklist;65 the evaluations were undertaken by Carole Mockford. Owing to the heterogeneity of the studies included, many of which were descriptive in their approach, this checklist provided an appropriate basis for comparison between studies. The only slight question change in the CASP checklist was as follows: ‘is the qualitative methodology appropriate for this study?’ was changed to ‘is the methodology appropriate for this study?’. This was to ensure that the quality check did not discriminate against the few relevant quantitative studies that had measured experiences.
Data analysis
The scoping review shaped the content of the thematic framework in the main review, when a detailed narrative synthesis of identified themes was undertaken. 23 The researcher read each study and undertook an initial preliminary synthesis to identify emerging subthemes and compared themes and subthemes within and across studies to develop the main themes. Themes were summarised in a descriptive form, allowing the findings of all studies included, regardless of design, to be aggregated and summarised. The concept of data saturation was used to form a judgement about the point at which no new themes were identified. 66 This approach was considered appropriate for a large review in which the addition of further papers was unlikely to change key findings.
Systematic review
A total of 4979 abstracts were screened and 116 papers fulfilled the inclusion criteria [Figure 5 shows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)67 flow diagram]. Two consecutive sifts were conducted owing to an error in the first search of the PsycINFO database omitting 2980 hits, which was identified after the first sift was completed. The first sift of 1999 hits resulted in 72 relevant papers for the review. Eleven papers were from the same studies. 68–78 Following this, the second sift of 2980 abstracts resulted in an additional 44 studies fitting the criteria (n = 116). Drawing on the principles of data saturation,30 additional studies that repeated themes already identified were excluded from the main review. In total, eight studies added new themes and were included at this stage. Sixteen systematic reviews (see Appendix 14) that investigated inpatient experience were identified.
FIGURE 5.
The PRISMA flow diagram for the EURIPIDES systematic review (WP1).
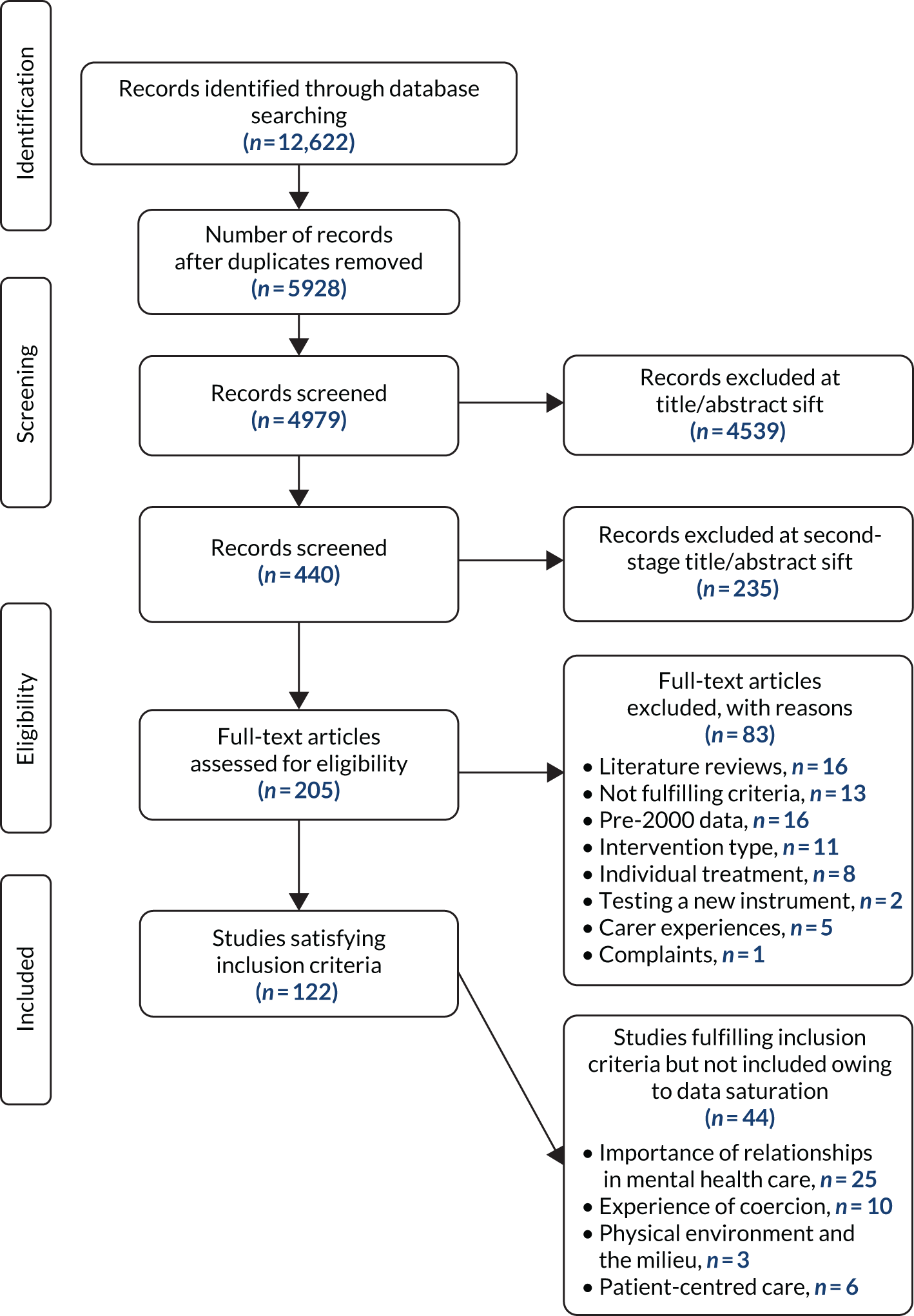
In total, 72 studies were included in the review, of which one-third were from the UK73–95 (n = 24)68,70,74,76,80–97 (see Appendix 14). Studies using qualitative methods were most common (see Appendix 14), but studies using patient experience questionnaires and patient record data were also included. The CASP checklist identified many of the papers as being of medium to poor quality (see Appendix 14).
Identification of key themes
Patient experience themes were categorised into four overarching themes or dimensions of experience: the importance of high-quality relationships; averting negative experiences of coercion; a healthy, safe and enabling physical environment and ward milieu; and authentic experiences of patient-centred care. These key themes, accompanied by subthemes, are described in detail below.
The importance of high-quality relationships
One of the most important themes to emerge from the review was the importance of high-quality relationships. A range of factors influenced the development of high-quality relationships with staff, including being treated with respect, feelings of stability, empathy and high-quality communication68,72,73,76,78,83,84,86,87,98–105 with staff whom patients perceived to be trustworthy, reliable83,102,106 or helpful. 76,98,107,108 These high-quality staff–patient relationships enabled the inpatient care pathway in mental health institutions78,83,87,88,98 and reduced the need for staff to use coercive measures. 83,93,103 A key setting for staff–patient interaction was ward rounds, with patients noting that these were helpful and informative. 92
Studies identified a range of barriers to high-quality relationships, which included gender-specific problems, such as male nursing staff who were not welcome if the patient had a history of abuse by male perpetrators84,103 or when gender-specific cultural barriers existed (e.g. a Muslim woman supervised by a male nurse);88 a lack of meaningful communication when communication was compromised owing to differences in culture, language or religion,82,87,109,110 through the use of coercive measures81,100 or when technical language used by staff was not easily understood;68 the absence of regular ward staff, that is when patients were upset by the absence of regular ward staff owing to office duties, shift working or reliance on temporary staff72,73,76,78,83–85,87,93,94,98,99,102,106,107 and when they had extended waits to speak to staff,73,84,94,107,111–113 particularly at ward rounds;91 poor staff attitude, that is when patients complained that staff ignored them104,109,114,115 or displayed indifference73 or insufficient understanding of patients;103 inconsistent staff behaviour, with reports of staff interpreting ward rules inconsistently, causing confusion;68,72,76,79,81,84,94,97,113,115 and staff abuse, with some patients reporting abuse by staff, including provocation, bullying, shouting or belittling of patients. 68,72,76,78,81,87,103,104,108,114,116,117
Relationships with other patients and relatives
Relationships with others, including other patients and relatives, were important. Patients relied on other patients for information about ward activities and rules, to share experiences and when debriefing after group sessions. 71,93,111,113,117 However, arguments and violence between patients84,87,118 generated fear and isolation for some, causing them to retreat to their rooms to feel safe or to abscond. 72,85,87,97,112,119
Feeling isolated from family caused patients to feel distressed and some patients reported that having a friend or family member with them would have helped with orientation120 or they could have acted as informants to help staff with assessments and treatment plans. 71,86,121 However, family members often felt left out of decision-making about care. 122
Averting negative experiences of coercion
The second main theme was concerned with averting negative experiences of coercion. The coercive measures discussed in studies included experiences of sedation, seclusion and restraint. All patients expected to be treated as ‘normal human beings’73,78,111 and to be addressed professionally, including during restraint. 104 Having the reasons for coercive measures explained to patients was important to help them understand why this occurred and helped some patients to trust staff and feel safe. 94,104,120,123,124 Patients preferred persuasion over threats of force100 and coercion,103 which sometimes brought back memories of past violence and/or neglect. 81,114,125
Two studies examined the commonly held perception that black and minority ethnic patients experienced more coercion on admission than other patients. 70,126 Findings were not conclusive: although hospitals in the UK with higher proportions of minority ethnicity patients employed more coercive practices, this was independent of individual patient ethnicity. 70,126
Some patients recognised that medication was important for their care69,87,89 and some trusted staff to decide on appropriate sedation,80,127 whereas others felt (more) empowered to decide on timing and dose of medication when this was administered on an ‘as needed’ basis. 80 However, some patients were concerned about the lack of communication about consent, information about medication and advanced wishes. 87,127 There were also reports of a lack of confidentiality regarding medication,80,90 perceived overmedication80,87,89,94,95,106,127 (including ignored reports of side effects)78,89 and fear of harm during forced medication,69,80,87,100,103,107 for example a fear of being raped by staff or dying. 69,89,103,114
Some patients reported seclusion as helpful or necessary,73,109,114,120 and reported feeling safe, as staff were nearby. 73,105,109,114 Patient concerns included having insufficient information about the reasons for seclusion72,73,94,109,125 before or after the event. 73,109 Seclusion was perceived as a punishment120 and associated with limited contact,109,114 a lack of concern by staff,125 degradation and humiliation (e.g. lack of facilities73,109,125 or being stripped of clothing in front of staff members),101,115,120,125 and violation of rights114 and dignity. 101
Restraint, typically involving several staff members, mostly nurses72,100,103,114,122 but occasionally security staff,103,122 was described negatively74,81,103 and fear of restraint prevented patients from seeking help earlier. 81 A risk of harm was noted when mechanical restraints were used,104 although these were not used in all countries. Patients thought that it was helpful to talk with staff or to be allowed to examine records of the event following restraint. 81
In addition to the use of coercive measures, patients also described perceived punishment by staff68,83,89,112,115 in the form of the removal of leave entitlements,83 the removal of furniture and personal items89,115 and not being able to stay up in the evening. 68,112 Patients described this as a violation of their rights. 72,109,110,114
A healthy, safe and enabling physical environment and ward milieu
The third main theme focused on a healthy, safe and enabling environment and ward milieu. This was important to how relatives felt when visiting,122 how patients felt about themselves87 and how they reacted. 84,87,90 Johansson and Eklund102 argued that the physical environment was as important to patients as receiving satisfactory care. A number of studies reported that patients viewed the hospital setting as a ‘sanctuary’112 or a ‘safe space’108 where they could have time to reflect away from day-to-day stressors,86,98 be kept safe69,87,107,118 and experience a caring, therapeutic environment. 112
Patients felt that their inpatient care pathway was aided by a connection to the ‘real world’101 and that being made to feel ‘normal’73,78,98,111 was important. This included being allowed to walk around hospital grounds. 87,112 Older establishments often had extensive grounds and patients reported that access to these spaces resulted in less need for medication. 80 Access to a place of worship was comforting,52,66 as was freedom to make small decisions79,89 such as making snacks108 or hot drinks. 84 Private bedrooms were important112 and being near windows enabled ward-bound patients to enjoy the outside and fresh air,117 and appropriate use of colour was described as conducive to recovery. 112 An environment in which staff and patients mixed together reduced feelings of stigma98 and encouraged favourable interactions. 102
Patients reported some environmental features that were not conducive to recovery-focused care. Some of these were associated with the potential for arguments and violence between patients. 84,87,118 Environmental problems included noise from door bells, alarms and telephones. 113 Poor positioning of the nurses’ stations often created physical divisions between patients and staff, and reduced interaction. 101,112,122 Communal spaces sometimes lacked privacy for visiting relatives or opportunities for physical activity,89 especially for those under close observation. 122
In several studies, patients described hospital as a place of confinement rather than therapy. 69,78,84,85,87,90,112 There were analogies with prison78,84,87,90,112 and punishment. 85,87 This was particularly so in secure units with a lack of outside space87 and where more patients were admitted compulsorily. 78
Ward milieu
Experience of ward milieu was often shaped by the conduct of staff. Staff were perceived to provide structure, order and safety113 and were responsible for creating a congenial atmosphere. 107 Feeling safe was a key concern for patients,118,127 who sensed wards were safe when staff were viewed as trustworthy,83 caring and supportive. 83,86 Wards were sometimes criticised for being too busy84,97,107 and staff were criticised for being too reactive to events such as restraint,116,120,122 seclusion115 or violence. 72,110,112 Patients felt vulnerable to violence,72,85,87 fearful of other patients50,77 and worried about the security of their belongings. 84,112,127 Fear contributed to withdrawing from the ward97,128 or leaving hospital. 85,112
Ward routines were important for shaping patients’ experiences. The day98 was often structured to include individual and group therapies and other activities (e.g. puzzles, conversation or listening to music),122 whereas evenings were often less structured. 98 Some patients relished the leisure time24,39,51,55 and took this as a time for personal reflection. 86,98,109 However, others were uneasy86,98 and reported insufficient97,116 activity. 72,73,87,88,118 The hospital being close to family was important to patients75 and they appreciated the inclusion of, and support from, families. 71,86,121
Boredom
‘Boredom’ or having too little to do was mentioned in several studies. 71,72,76,88,89,98,107,112,113,115,117,129 Patients suggested that inactivity slowed the inpatient care pathway,129 reduced self-efficacy,89 exacerbated symptoms112 and was related to aggression and violence on the ward. 71 Some patients reported that inactivity encouraged poor health outcomes (e.g. saying that they would eat, sleep or smoke but not exercise). 73,112,117,129
Authentic experiences of patient-centred care
The final theme brought together a collection of subthemes focused on authentic experiences of patient-centred care, which included shared decision-making, sensitivity to gender and culture, and information provision.
Two studies reported that patients’ involvement in treatment decisions was associated with positive experiences of care. 98,127 Patients wanted to be understood and seen as individuals, and this was often framed in respect of their gender, ethnicity and religion. 81,82,88,103 Some described cultural differences in how they perceived privacy, and reported concerns that staff had not recognised or responded to their discomfort in accepting care from differently gendered staff,88 for example during restraint and sedation81 or for women with a history of sexual abuse by male perpetrators. 103 More positively, female patients tended to prefer single-sex wards, where they felt safer. 84 When this was not available, female patients were satisfied on mixed wards if they had access to a quiet room, if their privacy was respected and if they had access to personal hygiene products. 73,74,77,78,80,82,87,88,90,91,99–101,107,109,110,116,128,129 Faith also mattered: prayer and rituals (e.g. hand-washing) offered comfort to some patients,88 but were not always understood or accommodated by staff. 82
In several studies, patients reported that they felt that they had not received sufficient information about their diagnosis,72,104,106,127 treatment,69 treatment plan,72,80,100,104–106,109,114,115,121,127 choices or rights. 69,94,121,130,131 The timing of giving information was also important, as patients found it difficult to understand or remember this when unwell. 93,106
Discussion
To the best of our knowledge, this was the largest comprehensive international review of mental health inpatient experiences. The systematic review was divided into two phases. The first phase mapped the field of mental health inpatient experience studies and helped shape the search strategy to ensure that it was specific and sensitive. The field of inpatient experience is very large and we used theoretical saturation (previously used to develop the Warwick Patient Experiences Framework7 to inform the NICE guidance on patient experiences60) to help manage the number of papers. This strategy proved effective and a total of 72 papers were included in the final review, ensuring appropriate coverage of themes.
The PPIT played a key role in the systematic review. Members reviewed the themes that emerged from the scoping study for face and content validity. This was particularly important, as the review drew on international studies, and emerging themes had to be tested for applicability in a UK context. The role of the PPIT was also important because the presence of the service user voice in this field of research was often unclear, as studies did not always describe how patients had been involved or how they had influenced study findings. This is not unusual in health research, in which poor reporting about PPI is common, and does not necessarily mean that there was an absence of activity. Future studies should consider the role that involvement can have in research, particularly in the field of mental health, in which the synthesis and interpretation of experience data may differ between professionals and patients.
The review makes a key contribution to the field of mental health inpatient experiences through the identification of four key, interlinked, themes: the importance of high-quality relationships; averting negative experiences of coercion; a healthy, safe and enabling physical environment and ward milieu; and authentic experiences of patient-centred care. These themes and their subthemes represent the ‘active ingredients’ of a high-quality mental health inpatient experience. They also highlight the common causes of poor experiences, which could have detrimental impacts on patients, carers and families. We summarise each theme in the following paragraphs.
The importance of high-quality relationships, particularly with staff, was the most commonly reported theme. Good experiences were reported when staff were compassionate, caring and respectful, engaging patients in ways that helped them feel valued and understood. This had an important role in recovery-focused care and in reducing the use of coercive measures.
The second theme focused on averting negative experiences of coercion. Experiences of coercion included sedation, seclusion and restraint. Some patients reported distressing experiences, particularly if they did not understand the reason why it was happening. Patients sometimes recognised a need for coercion, but still expected to feel that they were valued and understood, and also treated professionally, with their rights protected. This also raises the possibility that the intense distress (and fear) caused by coercion might bias patient experience data itself, for instance through a fear of reprisal or further coercive treatment. A solution may lie in the co-production of data collection systems that facilitate feedback in contexts in which there are power imbalances.
The third main theme was a healthy, safe and enabling physical environment and ward milieu, which included the atmosphere, the culture, staff attitudes and the wider patient community. This provided a vital context for patient experience. The milieu could be vital for nurturing a patient and could provide a sense of safety and sanctuary, almost a therapeutic intervention in itself. Staff played a key role in creating this milieu, with structure, order and safety producing a congenial atmosphere, which made wards feel safe. The physical environment complemented the milieu by contributing to a greater sense of well-being.
The fourth and final substantive theme was authentic experiences of patient-centred care, which recognised the importance of treating patients as individuals and accounting for their perspectives, previous experiences, preferences, gender, ethnicity and religion. Key components of patient-centred care included sufficiently timely information about diagnosis, treatment, plans and choices. Again, relationships were the conduit of patient-centred care, which started at admission and continued until, and sometimes past, discharge.
Limitations
A limitation of this review, common to all secondary research, is that it was reliant on the conduct and content of primary studies, which may have included biases that we could not account for. Relatively few studies mentioned the involvement of service users in data collection and research, so it is unclear to what extent a study finding reflected the user voice. Ensuring greater clarity about whose voice is represented, as a means of minimising bias, represents an important methodological challenge for future research.
Although we utilised data saturation as a means of deciding when to stop data extraction (at the point when we judged no new themes were emerging), it is possible that other papers contained nuances in themes that were unintentionally omitted. The risk of bias in this review may have been mitigated by our scoping review, which identified key authors, a citation search of the papers included and other literature reviews. In addition, the involvement of the PPIT provided important assurance of face and content validity.
The review relied on secondary analysis of qualitative data. The findings we have presented are drawn from the reports of participants in primary studies. Many of these claims (e.g. the perceived role of good relationships in reducing a range of unwanted outcomes or the role of boredom in exacerbating those outcomes) are reported across multiple primary sources. An important limitation of secondary research is the gaps that exist in studies. A key limitation in this review was the experiences of minority ethnic groups, which appear to be under-researched.
Conclusions
This systematic review is the largest review of its type, identifying key aspects of patient experience. The key role of staff in delivering a high-quality experience was the common thread running through many studies and so should represent a key focus for future service developments. Collectively, the four key themes represent the heart of the mental health inpatient experience. By paying attention to them, services can provide the highest-quality patient experience at a time of often great vulnerability and need.
Chapter 5 Work package 2: national survey of patient experience leads in mental health trusts in England with more than 50 inpatient beds
Introduction
There is no existing evidence about the different ways in which providers of NHS inpatient mental health care currently collect, analyse and use patient experience data to improve inpatient mental health services across England.
Aims and objectives
We set out to describe approaches to collecting and using inpatient experience feedback to inform service delivery in mental health trusts, and to create a sampling frame for WP3 case study sites. We also aimed to test, iterate and further develop our initial programme theories (see Appendix 17).
Our objective was to undertake an interview-based survey of PELs in mental health trusts with an estate including > 50 inpatient beds. The survey was designed to collect information about the organisational context for this work, including the extent of patient involvement in processes for collecting and using inpatient experience data.
Methods
The EURIPIDES study was underpinned by realist evaluation methodology. Realist evaluation is explicitly theory driven and theory focused (see Chapter 2). WP2 built on the programme theory development that took place following the systematic review of inpatient experiences in WP1, which identified four key themes (see Chapter 4): relationships, particularly with staff; coercion; the physical environment and ward milieu; and patient-centred care. We compared these themes with the content of questions asked by trusts when collecting inpatient experience feedback.
A three-part, cross-sectional survey was designed that incorporated a semistructured telephone interview, a short questionnaire and the collection of examples of what trusts considered best practice in relation to collecting and using patient experience feedback.
Setting and participants
This survey was conducted with PELs in NHS mental health trusts in England with > 50 adult mental health beds. At the time of undertaking WP2, there were 71 providers of NHS inpatient mental health services in England. Bed availability and occupancy statistics (the KH03) were used to determine eligibility. 132
Ethics approvals
Study materials were approved by the West Midlands (South Birmingham) NHS Research Ethics Committee. These were sent out to NHS trusts and included an invitation letter outlining the study (see Report Supplementary Material 2), a consent form and a participant information sheet; trusts were also issued with a full copy of the research protocol. 133
Data collection
The data collection comprised three elements:
-
telephone interviews with PELs
-
completion of a short questionnaire by PELs
-
documents showcasing patient experience work in the trust.
Telephone interview
A topic guide for the telephone interview was developed covering five key areas:
-
the PEL, their role and the trust in which they worked
-
the patient experience data journey, including methods and content of patient experience data collection, and what happens to the data thereafter
-
patient experience data analysis and management
-
patient experience data feedback mechanisms, and how (or if) these data result in service change
-
reflection on how patient experience data are linked and operationalised within the wider organisation and what this contributes, including other ways that the patient voice is heard in the trust.
Interview schedules were realist in design and built on themes identified in WP1 and developed to test initial programme theories (see Appendix 17). Using a realist interview technique, participants were encouraged to reflect and comment on these developing theories. Field notes were made by the RF to support understanding and analysis. Interviews were audio-recorded with participants’ consent and anonymised.
Questionnaire
A short questionnaire (Table 1) was sent to participants to augment collection of descriptive information about each trust, including ward and bed numbers, and sizes of populations served.
| Number | Item |
|---|---|
| 1.1 | Trust name |
| 1.2 | What is the estimated population that your organisation serves? |
| 1.3 | What is the estimated number of adults with mental health problems that your organisation serves? |
| 1.4 | How many different inpatient wards or units does your trust have for adult mental health inpatients (excluding learning disability services)? |
| 1.5 | What is the annual turnover or budget for your trust? |
| 1.6 | What is the annual turnover or budget for mental health services delivered by your trust? |
| 1.7 | How many staff in your trust work in adult mental health services? |
| 1.8 | How many inpatient adult mental health beds does your trust have (excluding learning disability services)? |
| 1.9 | What is the average length of stay for adult inpatient mental health services (excluding learning disability services)? |
| 1.10 | Does your trust provide forensic mental health services? |
| 1.11 | Does the trust serve a rural or urban community, or a mixed area? |
Participants were allowed to provide this information at interview if they preferred. If data were missing, we used publicly available information provided on the trusts’ websites.
Supporting documents
Interviewees were asked to provide a ‘best practice’ document or to provide their patient experience strategy (sometimes referred to as an involvement or engagement strategy). If participants did not provide these documents, we used public information from the trust’s website to access copies, when possible. If trusts were undertaking surveys on inpatient wards, survey materials were collated to profile the information being collected to aid programme theory development.
Analysis
Telephone interview
Audio files were fully transcribed, reanonymised for any information that may be considered identifying, and analysed using MAXQDA12 (VERBI Software, Berlin, Germany). Transcripts were coded using a thematic analysis framework. Information gleaned from coded transcripts was then summarised into an overarching matrix (see Report Supplementary Material 3). In addition, any programme theories that trusts had identified (even if they were partially developed) were extracted from the interview data and recorded in a programme theory log created to collate these.
Questionnaire
Questionnaire data were summarised using a matrix to facilitate WP3 case site selection (see Report Supplementary Material 3). These data were used with the other summarised information to ensure a balanced selection of case sites in terms of size and scale.
Supporting documents
Documents were entered into MAXQDA12 and reviewed to assist with programme theory development by augmenting data in questionnaires and interview transcripts.
Analysis
We initially identified a descriptive framework developed by The Health Foundation134 for classifying patient experience data collection methods reported by participating trusts. This framework is based on the two dimensions of ‘descriptiveness’ and ‘generalisability’ and classifies tools such as surveys or online ratings as less descriptive than in-depth interviews, complaints and compliments. Using this framework, tools were additionally categorised by their generalisability. Surveys or in-depth interviews were seen as more generalisable, whereas patient stories with a specific individual narrative, anonymous complaints or online ratings were viewed as less generalisable. 134
Although this framework offered a simple means of classifying how feedback was sought from inpatients, it did not provide sufficient detail to enable selection of WP3 case study sites. Our methods therefore evolved to include a more nuanced understanding of the timing and sequence of approaches to patient experience data collection and use. This enabled us to ask more realist questions about how, when, for whom and why particular tools were adopted.
This broader approach was drawn from implementation research related to the heuristic ‘stages’ of the policy cycle. We based our final design on the rationale, objectives, appraisal, monitoring, evaluation and feedback (ROAMEF) cycle, as used to evaluate policy by Her Majesty’s Treasury and the Department of Health and Social Care. 135,136 The ROAMEF cycle phases were adapted to help in understanding the ‘journey’ of patient experience data as it moves through a trust, which we conceptualised in four stages: (1) data collection, (2) data analysis, (3) change informed by the results of analysis and (4) feedback within the patient experience process (i.e. patients and/or carers told about how their feedback had changed service delivery).
We used this four-step cycle to frame our programme theories to try and understand at what points patient experience data were collected, analysed and used. We used this cycle in the semistructured interview schedule to determine what happened in each of these phases, to get a more nuanced understanding of how the patient experience processes operated in participating trusts, and to compare these.
Once we had completed PEL interviews, an iterative process took place (through re-reviewing and triangulating the three sources of information) to ascertain which of our programme theories needed refining and what generative mechanisms could be observed underlying the patient experience work taking place in each trust that might inform the realist evaluation in WP3. The main purpose of the survey, however, was to populate a sampling frame to select case sites.
Collated survey data (transcribed interviews, field notes, best-practice documents and questionnaire data) were coded by study researchers using MAXQDA12. Coding was thematic and purposive in order to pull information into descriptive summary categories. For example, information was extracted on the size, composition and organisational location of patient experience teams. This extracted information was summarised and inserted into a matrix (see Report Supplementary Material 3).
The initial organising principle for these data was the four-step process described above and we initially sought to establish how ‘far around’ the cycle trusts were in relation to collecting and using patient experience data. We then expanded this to reflect information provided by PELs about wider patient experience work (and associated governance and patient engagement processes) in participating trusts. These categories were based on our initial and refined programme theories about what might lead to successful collection, analysis and use of patient experience data in relation to quality improvement and, thus, the sampling frame was strongly influenced by our programme theory development (see Appendix 17).
Developing the appraisal system
We created a system for appraising the data to support the selection of case study sites and minimise bias. Our approach was iterative. The initial matrix spreadsheet document and extracted data were reviewed and analysed in the light of the emergent programme theories (see Appendix 17). We developed a weighted appraisal system based on key themes identified as potentially important in this process. For example, one of the programme theories expressed in the original bid was133 (see Appendix 17):
. . . there will be discernible differences between organisations that demonstrate genuine commitment to, and capacity for, using patient experience data to improve services, and that these differences will be most clearly manifest through the existence of processes that support innovation and quality improvement, including commitment to service improvement among senior leaders, decentralised decision-making (through identifiable champions for change), role clarity within the organisation, and support for risk-taking.
To test this theory (including the level of commitment among senior leaders), we used organisational proximity of the PEL role to trust boards as a proxy. One of the scored items developed, therefore, concerned where the PEL post sat within the trust and how far removed this post was from the trust board in terms of reporting structures.
Based on our initial programme theories, the first iteration of the appraisal system included items about:
-
the completeness of the cycle of data collection, analysis, implementation and feedback
-
the variety of methods used to collect patient experience data
-
the nature and extent of service user and carer or PPI work within the trust
-
if the trust had a separate budget for patient experience work
-
where the PEL post sat organisationally and how far removed this was from the trust board in terms of reporting structures
-
if there were any quality initiatives or any quality data explicitly linked to or triangulated with patient experience data
-
if Patient Advice and Liaison Services (PALSs) or complaints were linked to the patient experience work being undertaken in the trust
-
whether the PEL was a temporary or a permanent post, and if they were supported by a wider team
-
if patient safety data were linked to or triangulated with patient experience data.
The majority of trusts focused on the earlier part of the data collection cycle. Therefore, to differentiate trusts for the purposes of selecting WP3 case study sites, we refined our approach to include evidence to support or refute the following key programme theories133 (see Appendix 17):
-
Organisations that innovate also value information, and ‘we anticipate that organisations that use patient experience data most effectively will also have robust data-collection strategies.’. 133
-
There is a dearth of evidence about the processes required to analyse, interpret and translate these data into tangible actions, better outcomes for patients, and more efficient and cost-effective care. 133
-
Organisations that are genuinely patient-centred will also demonstrate investment in and adoption of codesign approaches to service improvement, and will involve service users and carers meaningfully, as partners. Feedback from patients can be perceived as critical or threatening by professionals, and may be avoided or denigrated. Codesign is a partnership approach that neutralises perceived threats through collaborative working to find mutually agreeable solutions to problems or difficulties experienced by patients when receiving care.
The final matrix was structured to reflect these three key domains (the variety of methods for collecting patient experience data, service user and carer engagement, and the extent of completion of the patient experience cycle from data collection, to analysis, to implementation and feedback; Figure 6).
FIGURE 6.
Weighted appraisal system for WP2.
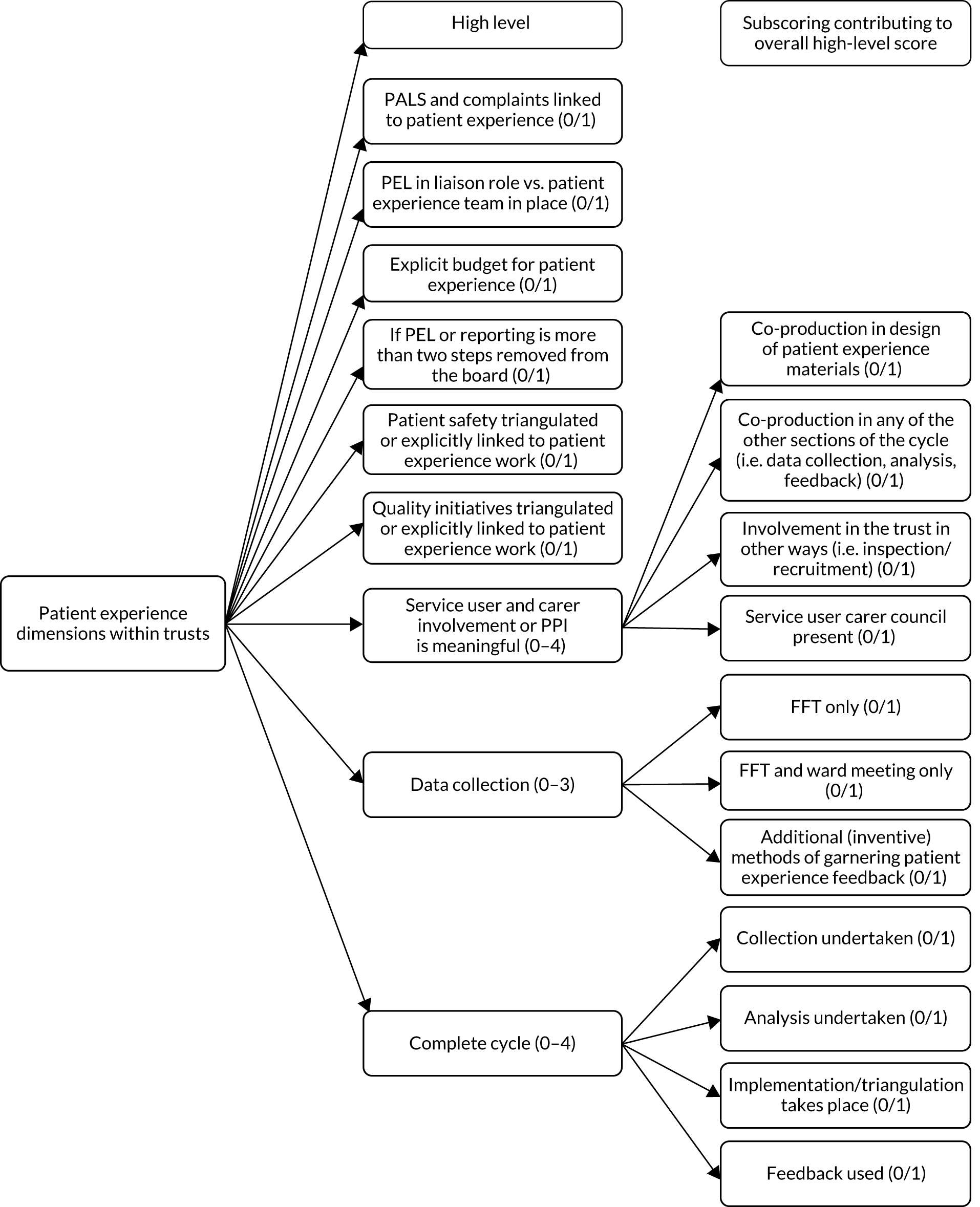
Data from each trust were scored independently by three researchers. Scores were then discussed to reach consensus if they differed.
Development of typologies of NHS mental health trusts
After rating each trust, we sought to red, amber, green (RAG) rate trusts into three bands of low, medium and high scores (Table 2). We used these three bands to form typologies of trust based on ‘levels of embeddedness’ of patient experience work. This term emerged from our programme theories and is used here to refer to the breadth of patient experience work in relation to the whole feedback cycle from data collection to its use in service improvement. ‘Embeddedness’ includes service user and carer involvement in collecting and using patient experience data, and triangulation of patient experience data with quality and safety data.
| Level of embeddedness | Anonymous case site identification | PALS or complaints linked to patient experience (0/1) | PEL in liaison role vs. patient experience team in place (0/1) | Explicit budget (other than staffing) for patient experience (0/1) | PEL or reporting more than two steps removed from the board (0/1) | Patient safety triangulated or explicitly linked to patient experience work (0/1) | Quality initiatives triangulated or explicitly linked to patient experience work (0/1) | Service user and carer involvement or PPI is meaningful (0–4) | Data collection (0–3) | Complete cycle (0–4) | Totals |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Low level of patient experience work embedded in trust | NHSProvA01 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 1 | 5 |
| NHSProvA02 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 5 | |
| NHSProvA03 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 6 | |
| NHSProvA04 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 3 | 1 | 6 | |
| NHSProvA05 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 6 | |
| NHSProvA06 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 2 | 2 | 6 | |
| NHSProvA07 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 7 | |
| NHSProvA08 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 | 1 | 7 | |
| Medium level of patient experience work embedded in trust | NHSProvA09 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 3 | 2 | 8 |
| NHSProvA10 | 0 | 1 | 0 | 1 | 0 | 0 | 2 | 3 | 2 | 9 | |
| NHSProvA11 | 0 | 1 | 0 | 1 | 0 | 0 | 2 | 2 | 3 | 9 | |
| NHSProvA12 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 3 | 3 | 9 | |
| NHSProvA13 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 2 | 2 | 9 | |
| NHSProvA14 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 3 | 2 | 10 | |
| NHSProvA15 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 3 | 3 | 10 | |
| NHSProvA16 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 2 | 3 | 10 | |
| NHSProvA17 | 0 | 0 | 0 | 0 | 1 | 1 | 3 | 3 | 2 | 10 | |
| NHSProvA18 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 3 | 1 | 10 | |
| NHSProvA19 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 3 | 2 | 11 | |
| NHSProvA20 | 0 | 1 | 0 | 1 | 1 | 1 | 2 | 3 | 2 | 11 | |
| NHSProvA21 | 0 | 1 | 0 | 1 | 1 | 1 | 2 | 3 | 2 | 11 | |
| NHSProvA22 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 3 | 3 | 11 | |
| NHSProvA23 | 0 | 1 | 0 | 1 | 0 | 1 | 3 | 3 | 3 | 12 | |
| NHSProvA24 | 0 | 1 | 0 | 0 | 1 | 1 | 2 | 3 | 4 | 12 | |
| NHSProvA25 | 1 | 1 | 0 | 1 | 0 | 1 | 3 | 3 | 2 | 12 | |
| NHSProvA26 | 0 | 1 | 0 | 1 | 0 | 0 | 4 | 3 | 3 | 12 | |
| NHSProvA27 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 3 | 4 | 12 | |
| High level of patient experience work embedded in trust | NHSProvA28 | 0 | 1 | 1 | 1 | 1 | 1 | 2 | 3 | 3 | 13 |
| NHSProvA29 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 3 | 4 | 13 | |
| NHSProvA30 | 1 | 1 | 0 | 1 | 1 | 1 | 2 | 3 | 3 | 13 | |
| NHSProvA31 | 1 | 1 | 0 | 1 | 0 | 1 | 4 | 3 | 2 | 13 | |
| NHSProvA32 | 1 | 1 | 0 | 1 | 1 | 1 | 3 | 2 | 3 | 13 | |
| NHSProvA33 | 0 | 1 | 0 | 1 | 0 | 1 | 4 | 3 | 4 | 14 | |
| NHSProvA34 | 1 | 1 | 0 | 0 | 1 | 1 | 4 | 3 | 3 | 14 | |
| NHSProvA35 | 1 | 1 | 0 | 1 | 1 | 1 | 3 | 3 | 4 | 15 | |
| NHSProvA36 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 3 | 3 | 15 | |
| NHSProvA37 | 0 | 1 | 1 | 1 | 1 | 1 | 3 | 3 | 4 | 15 |
Thus, we were interested in what kinds and how much service user and carer involvement and engagement was taking place in each trust, and the quality of this involvement and engagement; how patient experience linked to quality improvement or other processes through organisational structures; and how seriously it was taken by trust boards. These ideas were explicitly linked to programme theory drawn from the original bid and the findings from WP1 (see Appendix 17).
At the end of the rating process, we had three categories of trust to select case sites from: those with low levels, those with medium levels and those with high levels of embeddedness of patient experience work.
Selection of trusts as potential case sites
The sampling process for WP3 involved a purposive realist approach. 137 Emmel137 suggests that the ‘trick in choosing [realist] cases is to assemble the optimal configuration of ingredients to refine a theory’. 137 Realist sampling strategies are theory driven, with theory being applied to investigate a particular context in the social world. The selection of comparative case sites was purposive in relation to our embeddedness typology. Purposive realist selection took place to refine our understanding of the programme theories and the generative mechanisms operating to create different outcomes between and within trusts. The final selection of case study sites was undertaken by the Project Oversight Group, supported by two service user researchers (Emma Ormerod and Stephen Jeffreys). All data were anonymised (and the initial numbers given to trusts were reanonymised during the analysis phase).
Case sites were chosen based on patterns of outcomes that emerged during the appraisal process. We chose sites with ratings that were similar in their overall totals but different in patterning, to allow for testing and refinement of our programme theories. Therefore, we decided that trusts would be recruited from sites rated in the medium- and high-scoring categories. Case sites with low levels of embeddedness of patient experience work were excluded, as we judged that programme theories would not be testable if little patient experience activity was being carried out. It was also felt that visiting trusts where limited patient experience work was taking place would not be fruitful and would risk upsetting staff.
A longlist of potential sites was established using anonymous data. At this stage, additional information was considered to ensure the sites accounted for the urban or rural setting, size of the trust (e.g. number of wards and beds) and location, to ensure geographical diversity in the sites selected (Table 3).
| Anonymous case site identification | Number of inpatient beds | Number of inpatient wards | Forensic: yes or no | Rural, urban or both |
|---|---|---|---|---|
| NHSProvA01 | Small | Small | Yes | Urban |
| NHSProvA02 | Large | Small | Yes | Urban |
| NHSProvA03 | Large | Medium | Yes | Rural |
| NHSProvA04 | Small | Small | Yes | Rural |
| NHSProvA05 | Medium | Medium | Yes | Rural |
| NHSProvA06 | Large | Large | Yes | Both |
| NHSProvA07 | Large | Large | Yes | Urban |
| NHSProvA08 | Small | Medium | Yes | Both |
| NHSProvA09 | Medium | Medium | No | Urban |
| NHSProvA10 | Medium | Small | No | Both |
| NHSProvA11 | Small | Small | Yes | Rural |
| NHSProvA12 | Small | Small | Yes | Urban |
| NHSProvA13 | Medium | Medium | Yes | Rural |
| NHSProvA14 | Medium | Small | No | Both |
| NHSProvA15 | Small | Small | Yes | Urban |
| NHSProvA16 | Small | Small | Yes | Rural |
| NHSProvA17 | Small | Small | No | Rural |
| NHSProvA18 | Large | Small | Yes | Urban |
| NHSProvA19 | Medium | Small | Yes | Rural |
| NHSProvA20 | Large | Large | Yes | Urban |
| NHSProvA21 | Medium | Medium | Yes | Both |
| NHSProvA22 | Large | Small | No | Both |
| NHSProvA23 | Medium | Medium | Yes | Urban |
| NHSProvA24 | Medium | Medium | Yes | Both |
| NHSProvA25 | Large | Medium | Yes | Rural |
| NHSProvA26 | Medium | Medium | Yes | Both |
| NHSProvA27 | Small | Large | Yes | Rural |
| NHSProvA28 | Small | Small | Yes | Rural |
| NHSProvA29 | Large | Large | Yes | Rural |
| NHSProvA30 | Large | Large | Yes | Urban |
| NHSProvA31 | Small | Small | Yes | Urban |
| NHSProvA32 | Small | Small | No | Rural |
| NHSProvA33 | Medium | Medium | Yes | Rural |
| NHSProvA34 | Small | Small | Yes | Both |
| NHSProvA35 | Large | Large | Yes | Urban |
| NHSProvA36 | Medium | Large | Yes | Urban |
| NHSProvA37 | Small | Medium | Yes | Urban |
Results
When the study commenced in December 2015, there were 57 identified providers of inpatient services for adults of a working age in England with > 50 inpatient beds. Mergers took place between trusts during the study, reducing this number to 54, of which 42 (78%) trusts took part in telephone interviews.
A total of 49 interviews (three trusts required interviews with more than one person owing to the nature of the PEL role) were conducted across 42 trusts between 22 July 2016 and 6 March 2017. Interviews were 49 minutes in duration, on average. In addition, 20,943 words of accompanying field notes were taken during this part of the study.
Five trusts were excluded as ineligible for selection in WP3, as they had been subject to recent mergers and remained in a state of flux, meaning that selection based on the WP2 data would be invalid in relation to the phenomenon that we wanted to observe (patient experience feedback processes). This reduced the number of eligible trusts included in the selection process for WP3 to 37.
Six WP3 case study sites were selected, along with six matched reserve sites. The six trusts selected for inclusion in WP3 were distributed across England, in both rural and urban settings, and varied in size and number of inpatient beds. More descriptive details about these trusts are given in Chapter 6.
Three trusts were selected from the high level of embeddedness (green) typology, as determined by trust scores, and three sites were selected from the medium level of embeddedness (amber) groups (Table 4). Trusts with high levels of embeddedness displayed a fuller completion of the patient experience cycle, yet often scored differently in relation to how their patient experience activities were structured. This offered the opportunity to test programme theories relating to the importance of structural support of patient experience work. Sites were selected from the bottom, middle and top of the appraisal matrix in both the medium- and high-embeddedness groups, which therefore included sites that varied in their completion of the patient experience cycle. Particular anomalies (i.e. one trust was assessed as doing less well for service user and carer involvement yet still ranking highly) were seen as opportunities to test programme theories (e.g. about the importance of service user and carer involvement). 137
| Level of embeddedness | Anonymous case site identification | PALS or complaints linked to patient experience (0/1) | PEL in liaison role vs. patient experience team in place (0/1) | Explicit budget (other than staffing) for patient experience (0/1) | PEL or reporting more than two steps removed from the board (0/1) | Patient safety triangulated or explicitly linked to patient experience work (0/1) | Quality initiatives triangulated or explicitly linked to patient experience work (0/1) | Service user and carer involvement or PPI is meaningful (0–4) | Data collection (0–3) | Complete cycle (0–4) | Totals |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Medium level of patient experience work embedded in trust | NHSProvA09 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 3 | 2 | 8 |
| NHSProvA13 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 2 | 2 | 9 | |
| NHSProvA27 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 3 | 4 | 12 | |
| High level of patient experience work embedded in trust | NHSProvA29 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 3 | 4 | 13 |
| NHSProvA33 | 0 | 1 | 0 | 1 | 0 | 1 | 4 | 3 | 4 | 14 | |
| NHSProvA37 | 0 | 1 | 1 | 1 | 1 | 1 | 3 | 3 | 4 | 15 |
Five of the six trusts agreed to take part. One trust withdrew from the study, as it had defunded its patient experience work between WP2 and WP3 to meet cost improvement targets. This trust was replaced with a trust that had been matched during the selection process.
Turnover of patient experience leads
There was a high turnover rate among PELs in participating trusts. Between April 2016 and March 2017, 16 PELs left their posts or were replaced, and a further three leads were covering short-term or were in interim posts. This meant that a total of 19 PELs across the 42 trusts left their post in the first year of the study.
This staff churn reflected the state of the NHS at the time and offers an insight into the precarious nature of many PEL roles. Patient experience work seemed to be viewed in some trusts as a secondary function. This was relevant when considering some of our original programme theories, in particular those that related to trusts’ commitment to meaningful patient experience work linked to quality improvement, for example: ‘[w]e expect that organisations that set out to improve care quality will be able to evidence of methodologies for achieving this, including clear cycles of planning, implementation and reflection as opposed to small, piecemeal initiatives’ (see Appendix 17).
It became clear from our survey that the PEL role was vulnerable in many places and that, in at least one trust, it had been eliminated. This information was significant for refining programme theories and for site selection.
Completeness of the patient experience cycle
Trusts’ completion of the patient experience cycle from data collection to implementation and change was variable. Some trusts had seemingly long-established and well-developed systems for collecting feedback, whereas others were at an embryonic stage of patient experience work. Although this was unsurprising, what was of note was how few trusts reported using the data collected and explicitly linking this to evidence of service change.
The majority of trusts were collecting patient experience data but reported that these data were not used to drive change (51%). Some trusts were still struggling with collecting patient experience feedback at all (22%), with a similar number reporting using feedback data to support service improvement (27%). However, no trust achieved the potential maximum score (17 points) in relation to completing the patient experience feedback cycle (the highest score awarded was 15). In reality, few trusts were able to articulate how patient experience data were analysed and then used to drive service improvements or change. Some trusts are still in their infancy in relation to developing approaches to collecting patient experience feedback in adult inpatient settings, whereas others are more mature and able to use this feedback.
The extent of completion of the feedback cycle was influenced by multiple factors (resourcing, senior management buy-in, competing system pressures, etc.). It was clear that data analysis was the weakest point in the cycle. Although most trusts placed significant emphasis on data collection, little more than a basic description of the data took place. PELs could often not tell us when and how patient experience data were collected and by whom. This was partly because they did not know and because there was significant variation between wards within trusts. We developed a greater understanding of patient experience in inpatient settings as these interviews progressed. These two findings (relating to the completeness of the cycle and the weakness of analysis) led to programme theories being expanded ahead of WP3.
Comparing patient experience data collection in inpatient mental health services
The range of tools used in adult inpatient settings to capture patient experience data was not dissimilar to that identified by The Health Foundation134 in acute and general health-care settings. The most commonly reported tool used for collecting patient experience information was the FFT; however, trusts varied in how this was used. This varied from administering this test at discharge to monthly, or sometimes just ad hoc, administration. This variation occurred both between wards and between trusts.
Other common sources of patient experience feedback included complaints and compliments, patient stories (often presented to executive boards), community meetings on wards and electronic feedback through Patient Opinion (an independent feedback service) and the NHS Choices website (which is now known simply as the NHS website). Some trusts reported piloting different techniques, ranging from active use of peer support workers or volunteer-led listening clinics to recovery colleges with a patient experience function and more creative and innovative approaches, such as the example of a community-touring feedback camper van.
We identified three dimensions that characterised (and differentiated) approaches to data collection. First (as identified by The Health Foundation134), there was a distinction between approaches that were more descriptive and less generalisable (such as complaints or patient stories) and surveys that were more generalisable but not descriptive (such as the FFT).
The second dimension was the distinction between tools that were ‘formally’ implemented (in as much as they were reported on and used in any form of analysis) and those that were implemented ‘informally’. Exploring formal versus informal patient experience data was identified as important for WP3, to understand how both types of data linked to quality improvement (or not). This also had implications for WP5 (the economic evaluation; see Chapter 8).
The third dimension was the difference between trusts that collected patient experience data using just one formal method and those that employed a broader portfolio of approaches. Trusts that used a more layered (multiple) approach to collecting data appeared to be better at using the findings (i.e. some evidence of implementation following analysis). We were not able to identify outcomes from WP2 data alone, nor could we identify which combination of data collection methods was most effective in which particular settings and why. Again, this finding contributed to the refinement of programme theory and the development of the interview questions for WP3 (see Appendix 17).
The national imperative to report on patient experience was a key driver for routine collection of patient experience data. Although there were explicit criticisms made by PELs of the FFT, many acknowledged the usefulness of a national benchmarking measure and the systems change brought about by mandatory reporting. Nevertheless, FFT data were seen as insufficiently informative for the purposes of action-planning at the ward level. In addition (or perhaps consequently), FFT data were rarely fed back to staff. Analysis was often automated, outsourced or superficial, and there was limited analysis of the free-text data.
Concerns were raised in relation to inpatient mental health, and more so in forensic inpatient mental health settings, about the emotive and inappropriate nature of asking ‘would you recommend this service to your friends and family?’, particularly when admission was involuntary. This was cited as a reason for resistance among staff in administering FFT surveys to inpatients on adult wards.
Analysis and use of patient experience feedback to inform change
Patient experience work in NHS mental health trusts in England among adults of working age in inpatient settings was highly variable. Analysis of patient experience data was the weakest reported area of activity across all trusts. Variation in approaches to data collection was associated with differences in the ways in which these data were analysed and used. Some trusts had developed in-house data collection and reporting systems and ‘dashboards’ for reporting information; one trust had developed a bespoke patient experience dashboard. For many trusts, however, the management of patient experience data was not as robust and, in many places, FFT returns or other information was entered into local systems manually. Some trusts had procured external services and outsourced the analysis of patient experience data, which was received back in summary form and cascaded to staff. Even in trusts in which data collection and management processes were more sophisticated, many still reported that data were held in siloes; triangulation between patient experience data, PALS compliments and complaints, patient safety and other data sources was poor and typically relied on senior individuals taking the time to pull this together.
Often, data were collated and held centrally (even if some data entry was done locally). The initial descriptive analysis of collected feedback took place either through outsourcing or at a corporate level. Following this, information was cascaded through management lines back to wards.
When patient experience feedback led to changes, these were more often ‘environmental’ than ‘cultural’. ‘Environmental’ change was used to refer to changes that related to the physical environment or milieu, which resonated with WP1 findings (see Chapter 4). Examples cited often related to diet, seating areas in wards, temperature control and the physical environment of the ward.
‘Cultural’ change involved responding to patient feedback about relationships (i.e. feedback about staff attitudes). There were only two instances cited by PELs of patient experience leading to staff training. It was acknowledged that these kinds of changes were more difficult to make, particularly as they required additional resources. This resulted in a focus on short-term ‘quick wins’ rather than more complex and further-reaching quality improvement initiatives.
The issue of how difficult it was to know how to weight feedback was also raised by PELs. For example, they mentioned how one very powerful patient story may affect and change a service when it reached board level, whereas a single response to a survey rarely had the same effect. There was discussion in interviews about the ‘critical mass’ of feedback needed to drive change.
How feedback directly translated into quality improvement or the relationship of patient experience to ongoing quality improvement initiatives was often unclear. Triangulation of data across systems proved difficult in all settings. Many PELs highlighted the need for further progress:
After putting systems in place and changing culture around collection of patient experience, the next stage should be to identify what happens to data; the role may naturally evolve into quality improvement.
WP2Lead31
Patient experience may ‘promote’ FFT as they report on it for commissioning; they may also review Patient Opinion and NHS Choices, but these do not drive patient experience or any service improvement culture.
WP2Lead08
There was also awareness among PELs that change is difficult to facilitate and that there were many reasons for this:
Change doesn’t happen because of money, time, lack of support for change and the culture within the organisation; there are a lot of things stopping change.
WP2Lead06
Finite resources are a reason for lack of implementation of patient experience feedback; however, we need to think about what levels patient experience feedback can be used, e.g. in planning for change.
WP2Lead33
There was pervasive concern among WP2 interviewees about finite resources and resource pressure (particularly in a culture in which cost improvement decisions were increasingly difficult). There was also acknowledgement that the reason for not effecting cultural change in response to patient experience feedback was not solely because of a lack of resources. This provided useful programme theory refinement for the case study research (see Chapter 6 and Appendix 17).
Refinement of the EURIPIDES study programme theories
The WP2 survey provided an overview of the range of ways in which patient experience data were being collected in inpatient mental health settings in England. The first refinement of the programme theories related to developing a better understanding of the processes in place and methods that trusts were using to obtain patient experience feedback. One of the initial programme theories from the original bid was that organisations that use patient experience data most effectively will be those with the most robust data collection strategies (see Appendix 17). This theory necessarily evolved, as many trusts had similar data collection strategies, yet this did not, in and of itself, result in high levels of embeddedness of patient experience work being detected through the survey.
Although trusts used a broadly similar range of methods (and instruments) to collect data, these were being used differently within and between trusts. However, it was not clear that it was just the way in which the instruments were being used that influenced what happened next in relation to their success in obtaining genuine patient experience feedback or not. We could not tell from this survey which methods were most effective or why different patterns of outcomes (including uptake) were reported despite similar instruments (i.e. why patients engaged differently with the same instruments to give experience feedback). The implementation of similar tools that were generating different responses offered useful framing for the evolving programme theories that informed WP3. Realist evaluation tries to unearth the unseen mechanisms that generate different patterns of outcomes (see Chapter 2).
We also noted strongly contrasting, and contradictory, views about the approaches needed to obtain meaningful feedback from patients on inpatient units. An example occurred when PELs discussed the successful uptake of their survey or other measures for obtaining patient experience feedback, or tried to explain their FFT return rates. When talking about response rates from adult inpatient services, PELs offered logics including ‘getting their best data from inpatient services because they had a “captive audience”’, which was contradicted by another PEL who explained that they get their worst response rates from inpatient services because ‘patients are too unwell’. Both of these statements hold a potential truth. As the settings and clinical conditions of patients are broadly similar, something different must be operating; in realist terms, this suggests that different mechanisms are being ‘fired’ to warrant such different claims.
Summary of key findings from work package 2
-
Trusts use broadly similar methods for ‘formal’ collection of patient experience data in adult mental health inpatient settings. These are similar to those used in other parts of the NHS.
-
Around one-quarter of trusts were not just collecting patient experience data, but were analysing and using it to implement change at the ward or organisation level. Around half of trusts were collecting patient experience data but not using it to drive change, and around one-quarter were still struggling with the collection of patient experience feedback and did not have systems in place to capture this routinely. No trust achieved the maximum possible score (17 points) in relation to completing the patient experience feedback cycle (the maximum score achieved was 15). When trusts were using multiple approaches to collect and review data, they appeared to be better at using the findings.
-
The most commonly reported tool used for collecting patient experience information was the FFT. However, trusts reported variation in how this was administered and responded to. Some trusts incorporated FFT questions into a wider discharge survey or other questionnaire. The next most commonly used sources of patient experience feedback were complaints and compliments, patient stories (often presented to executive boards), ward rounds and community meetings on wards, and electronic feedback through Patient Opinion and the NHS Choices website.
-
Collection of FFT and other feedback data from adult inpatients varied between and within trusts. This ranged from collecting it on discharge for each individual, to monthly or sometimes ad hoc collection.
-
Allocation of resources for patient experience work was highly variable. Trusts had small corporate staff teams, one PEL (full or part time), delegated ‘champions’ at ward level or no formal roles.
-
When patient feedback led to changes, these were often environmental rather than cultural changes (e.g. food, seating areas in wards, temperature control and the physical environment of the ward). PELs were less likely to cite examples of cultural change (e.g. responding to feedback about poor staff attitudes) than they were to cite environmental changes to ward environments.
-
It was unclear how feedback led to quality improvement. Triangulation of data across patient experience, complaints and compliments, and patient safety or other data systems was limited. PELs acknowledged that quality improvement may be part of the same cycle as data collection and implementation, but many felt that their trusts were ‘not quite there yet’.
Strengths and limitations
This was the first survey of its kind in England. The high rate of participation (42 out of the 54 eligible trusts were represented) was likely to reflect the use of telephone interviews to collect data. Other strengths were the realist approach and in-depth data collection, informed by WP1 and the emergent programme theories that informed our data analysis. Broadening the focus to the embeddedness of patient experience work in trusts, rather than simply the ways in which patient experience data were collected, was a particular strength. This approach ensured that we were able to test and refine programme theories in a way that informed the conduct of WP3 interviews.
The development of the matrix for collating data, and an appraisal system to help summarise the latter, assisted greatly in WP3 case site selection. The main limitation was the absence of robust evidence of reliability or validity for item scoring or for the collation of results into three categories of ‘embeddedness’. The fact that the (blindly) chosen sites met the selection criteria (for diversity, against which to test and refine programme theories) provides a measure of validity for these approaches.
Chapter 6 Work package 3: realist evaluation of the collection and use of patient experience data to improve the quality of inpatient mental health care in six case sites in England
Introduction
The realist evaluation within the overall project
This chapter reports on the comparative realist evaluation of the collection, analysis and use of patient experience data to improve the quality of care in six case study sites in NHS England. This theory-based evaluation builds on the findings of earlier WPs. WP1 used programme theories from the original research bid to interrogate the literature about inpatient experiences of mental health settings (see Chapter 4). The themes identified in WP1 informed the interview schedules for the national telephone survey (WP2) and were used to refine the programme theories (see Appendix 17). These refined programme theories were then used to shape WP3.
The sites selected for the evaluation were identified from the survey of PELs in mental health trusts in England, as described in WP2. The survey provided an overview of the types of data that were being collected and the range of ways in which they were being collected. In WP3, we examined how, why, in what circumstances and for whom the process of patient experience data collection and analysis was being used to improve the quality of care. Our aim was to understand the contradictory statements noted in WP2 interviews, such as ‘[w]e get our best’ versus ‘[w]e get our worst’ patient experience data in inpatient settings through examining the programme theories behind these statements, in an effort to explain the divergence of practices observed (see Appendix 17).
Aim and purpose
Our aim was to undertake an in-depth comparative realist evaluation of the collection, analysis and use of patient experience data to improve the quality of care in adult inpatient mental health settings using six case study sites. Our purpose was to refine programme theories operating at the middle range to ensure that, while respectful of individual trust contexts, generalisable findings could be extracted from across the case study sites (see Appendix 17). From this, we aimed to develop a series of recommendations to take to our consensus conference (WP4) for discussion with key stakeholders.
Methods
Research design
We evaluated the collection, analysis and use of patient experience data in adult inpatient settings. To understand how, why and in what context this process was (or was not) successful, a laminated qualitative research design44 using semistructured interviews was developed that involved interviewing patients, carers, clinical staff working on the wards and corporate staff (see Chapter 2).
Selection and recruitment of case study sites
We considered a case to be an NHS mental health trust in England that manages at least 50 adult mental health inpatient beds. The sampling process involved adopting a purposive realist approach. 137 Emmel137 suggests that the ‘trick in choosing [realist] cases is to assemble the optimal configuration of ingredients to refine a theory’. The selection and recruitment of the six case study sites is reported in Chapter 5.
Setting for the realist evaluation
The six case study sites recruited were geographically dispersed across England and included trusts serving predominantly rural, predominantly urban and mixed rural and urban populations (Box 4).
NHS provider A09 was an urban trust with two hospital sites. There were five wards with 15–20 beds per ward. This provider had no forensic wards but did have a PICU. Staff on each ward included a clinical psychologist, a ward manager, two or three charge nurses, 10 or 11 nurses, two occupational therapists and 8–11 support workers. Wards were single sex with an adjoining nurses’ station and admitted adults aged 18–65 years. Safer staffing levels data found that the highest rate of registered nurses on shift against planned hours was 99% on one ward and that the lowest rate was 81% on another ward during the time of data collection.
There was one PEL for this trust, who worked alongside the PALS team. The PEL was responsible for all patient experience work including FFT and survey data collection. During the data collection period, FFT scores suggested that 100% of the people sampled who used mental health services would recommend the service to their family and friends. Data are reported to the board and are available to ward managers to access and further analyse. 138 The PEL was developing a survey for patients but was unable to explain how data would be analysed. The only visible patient experience work on wards was the PALS postcards available in the waiting area of most wards.
The lack of patient experience structure in this provider meant that patient experience was equated by staff and patients with complaints. Understaffing reduced informal patient experience practices such as community meetings.
NSHProvA13: medium level of patient experience work embedded in trustNHS provider A13 was in a rural area with four geographical sites. There were 10 wards across the trust providing adult mental health inpatient services, with between 16 and 20 beds per ward. This trust also provided a range of inpatient services in addition to acute care, including rehabilitation and recovery wards, forensic wards and PICU wards. Each unit (cluster of wards) had single-sex and mixed-sex wards, with admissions for adults aged between 18 and 65 years. However, one ward accepted younger women if no child or adolescent bed was available. Safer staffing levels data found rates of between 86% and 105% of registered nurses on shift against planned hours during the time of data collection.
The provider has a small patient experience team of one full-time member of staff and one part-time member. The PEL role is separate from the PALS and complaints; however, the roles support one another when possible. The main patient experience activity is a discharge survey and the FFT collected manually on paper. Data input is by members of a central corporate team outside the patient experience team. During the data collection period, FFT scores suggested that 89% (56 responses) of people using mental health services would recommend the service to their family and friends. 138 Results are reported to the trust board and uploaded to the dashboard for clinical teams to access and analyse.
Although limited analysis is conducted of patient experience data, the culture of this provider meant that buy-in to using data and displaying it on boards in the ward was high, and ward staff were aware of quality improvement changes that were happening on wards.
NHSProvA27: medium level of patient experience work embedded in trustNHS provider A27 was a rural trust that provided care on six acute adult inpatient mental health wards with between 16 and 20 beds each. Step-down care to low-security, locked or open rehabilitation wards was available in this trust, along with forensic, learning disability and older adult wards and a PICU. Wards were located across three geographical locations. All acute wards were mixed-sex wards and the admission criteria were considered ageless. Each ward had a doctor, a ward manager, a nursing team and health-care assistants. One lead psychologist oversaw the psychology provision for wards in this trust. Safer staffing levels data found rates of between 74% and 100% of registered nurses on shift against planned hours during the time of data collection.
Patient experience work was integrated into the role of the PALS in this trust. Paper surveys including the FFT questions were the main form of data collection handled by the patient experience/PALS team. All analysis and reporting for patient experience work was completed by this team using basic Microsoft Excel spreadsheets. In addition, this trust had an involvement lead who worked alongside service users and carers on PPI. During the time of data collection, FFT results show that 89% (nine responses) of people using mental health services would recommend the service to their family and friends. Data are reported to the board and to ward managers when requested.
Although the resources to engage with patient experience are minimal for this trust, there was considerable buy-in for the role of patient experience and the involvement of patients in decision-making across wards, with visible patient experience boards and information on a number of wards.
NHSProvA29: high level of patient experience work embedded in trustNHS provider A29 covered a large rural area with a large number of beds and wards split over three geographical sites. There were six wards for adult mental health inpatient services eligible for inclusion in the study, with between 16 and 20 beds per ward. The trust had one specialist PICU and a rehabilitation step-down ward in addition to the six wards. Each ward was single sex, with admissions for adults aged between 18 and 65 years. The wards all had a similar staffing structure: one modern matron, a ward manager, an occupational therapy lead, an activities co-ordinator, a mental health nursing staff, health-care assistants, an administrator and a psychiatry and other allied professional mental health or medical staff member. Safer staffing levels data demonstrated variability across the trust in the rates of registered nurses on shift against planned hours on one ward, namely of between 56% and 91%, during the time of data collection. This provider reported agency staffing levels at 40% on some of these wards and levels of unfilled shifts at 20% for two wards.
This trust was unique in its approach to patient experience work, as each directorate had a dedicated lead who oversaw and supported patient experience work on wards. In addition, each ward was assigned a patient experience champion to help engage ward staff with patient experience work and data collection. All surveys and the FFT were outsourced to an external company that analysed and reported on the data, which was fed back to PELs who worked alongside the modern matrons and ward managers to provide ward-level detail when needed. During the time of data collection, FFT scores suggested that 85% (59 responses) of people using mental health services would recommend the service to their family and friends. 138 Patient experience data were reported to the board and were also broken down and displayed on ward display boards.
NHSProvA33: high level of patient experience work embedded in trustNHS provider A33 was in a rural area with a large number of beds across three geographical sites. There were seven wards across the trust providing adult mental health inpatient services with between 16 and 20 beds per ward. This provider had a range of mental health inpatient services in addition to acute care including step-down care, rehabilitation and recovery wards, forensic and PICU wards, learning disabilities wards, older adult services, specialist personality disorder wards and mental health perinatal services. This provider had mixed-sex and single-sex wards, with admissions for adults aged between 18 and 65 years. Safer staffing levels data found rates of between 72% and 91% of registered nurses on shift against planned hours during the time of data collection.
Twelve full- and part-time staff made up the patient experience team and these staff were supported on wards by employed peer support workers. Patient experience and the PALS sat under the same umbrella, with the patient experience manager overseeing complaints, feedback, survey responses and carer opinions. Ward staff gave out surveys with the support of peer volunteers and returned these to the patient experience team to input into the system. During the time of data collection, FFT scores suggested that 78% (36 responses) of people using mental health services would recommend the service to their family and friends. 138 Data are reported to the board and sent to ward managers who can disseminate them to staff and use them for boards on the wards. A patient-focused report is created annually that is presented to the board for quality improvement goal-setting for the following year. This provider had a high level of PPI in designing and carrying out patient experience work.
NHSProvA37: high level of patient experience work embedded in trustNHS provider A37 was an urban trust providing five acute adult inpatient mental health wards with 20 beds each. All wards were located in the same geographical location. In addition, the trust had a forensic ward, a PICU and inpatient mental health wards for older adults, children and young people. Each ward was single sex and admitted patients aged between 18 and 65 years (unless diagnosis of early-onset dementia or a learning disability existed, in which case specialist ward admission was required). Each ward was staffed by a consultant psychiatrist, a junior doctor, a psychologist, an assistant psychologist, a ward manager, three deputy nurses, 15–20 nurses and 10 health-care assistants. Safer staffing levels data found rates of between 77% and 99% of registered nurses on shift against planned hours during the time of data collection.
A single patient experience team consisting of three members of staff was responsible for patient experience work across the trust. The PALS and complaints were separate from patient experience work. The patient experience team was responsible for the FFT and a patient experience survey that was collected by staff nurses using paper questionnaires, which was then input into the system by the patient experience team manually using specialist software. This was used to generate reports for ward managers to access. Additional analysis for FFT benchmarking was conducted by the business intelligence team. During our time of data collection, FFT scores suggested that 77% (57 responses) of people using mental health services would recommend the service to their family and friends. Data are reported to the board and are available to ward managers to access and further analyse.
This provider scored highly in the WP2 appraisal for its patient experience work, which had a number of strong elements. In practice, however, patient experience work on the acute wards was difficult owing to the high demand for beds (during the data collection period, one ward had 26 people admitted to a 20-bed ward) and the short lengths of stay (estimated at 23 days on average). The psychology team took the lead for patient experience work on the wards, with a (newly appointed) assistant psychologist on each ward being responsible for the community meetings alongside occupational therapists on some wards. Nursing staff appeared removed from the patient experience process. This was reflected in the minimal patient experience information or boards for patients’ feedback on the wards.
PICU, psychiatric intensive care unit.
Sampling and recruitment of participants in the case sites
The EURIPIDES study principal investigator at each case site worked alongside the research team and the local research and development (R&D) teams to identify and recruit participants (staff, patients and carers) for interview. Researchers visited and spoke to key staff on all acute adult mental health wards at each site to understand the context of patient experience activities. We excluded wards that were outside the project scope: children and adolescent mental health service wards, forensic wards, rehabilitation or step-down services.
All adults of working age (18–64 years) who were admitted to inpatient services in the case study sites were eligible to take part, providing they had the capacity to consent. Clinical staff, supported by local R&D teams, identified patients who were well enough to participate and who had the capacity to consent, and made the initial approach. The EURIPIDES study research team arranged to meet with participants in a confidential room (often a relatives’ meeting space) on the wards at a time that was convenient to the participant. The study team would then complete any outstanding consent paperwork, ensure that the participant had a chance to ask any questions and ensure that the participant understood what they were participating in; they would then conduct an interview. Immediately prior to each patient interview, the research team checked with the ward staff that the patient was still well enough to be interviewed, as the initial approach may have been made a few days earlier. If the patient had become unwell, the interview was rescheduled.
Carers were recruited based on their having a friend or family member (for whom they had some caring responsibility) on an adult inpatient ward for adults of working age in the case study sites. Carers were excluded if their experience was historical (> 6 months since supporting a friend or family member who had been an inpatient in mental health services). Clinical staff and the local R&D team made the first approach to carers coming on to the wards or those identified through carer forums, where these existed. There was not necessarily any link between carer and patient participants.
In conjunction with the local principal investigator, key corporate staff were identified who had a role in relation to patient experience data (collection, analysis, management or use of these data from the corporate organisational perspective). Clinical staff were recruited from a range of professions and specialties and a range of bandings: nurses, occupational therapists, psychologists, psychiatrists and health-care assistants. The principal investigator sent an e-mail to relevant staff inviting them to participate and spoke to ward teams asking for volunteers.
Through purposive sampling, we sought to recruit 30 participants per case site, based on research practice relating to minimum participant numbers and saturation of themes. 139 Attention was paid to the balance between recruiting an optimum number of participants for the study and the disruption caused to service delivery. The research team reviewed and discussed their interview experience and reflective field notes daily. Once they perceived that thematic saturation had been reached at a case site, recruitment ceased.
Data on how many potential participants were approached and on how many of these agreed to participate were not recorded. Recruitment was often undertaken opportunistically, for example because a patient’s mental state improved or a carer arrived on the ward. Recording recruitment approaches was felt to be too great an additional burden on overstretched ward staff.
Study materials
Realist interviewing is described as a process whereby ‘I’ll show you my theory if you show me yours’. 36 In a realist interview, theories are placed before the interviewee for them to comment on, with a view to providing refinement. The realist approach assumes that participants’ accounts have a direct relationship with the real experiences of (in this case) the inpatient setting. The subject matter of the interview is the research team’s theory and the subject (participant) is there to confirm, falsify and refine that theory. 140 Separate semistructured interview guides for each participant group were created.
Patient and carer interview schedules were developed in conjunction with the PPIT. The PPIT reviewed WP1 results and, through discussion, added factors that might influence whether or not patients engage in feedback processes. Three key themes were then identified: ways of giving feedback, relationships between staff and patients, and communication and trust. Flash cards were created with the theme label on one side and illustrative quotations from the PPIT discussion on the other (Box 5; see Appendices 9, 11 and 13). Patient and carer quotations differed from each other, reflecting their different perspectives.
I am more likely to be happy to give feedback just before I left and just after I left.
Where there is an opportunity for a face-to-face conversation, I am more likely to be honest.
Relationships between staff and patients
I would be more likely to be honest to people who are genuine.
If the ward staff understand me, I would give them feedback.
Communication and trust
If the person tells me how/explains how my feedback is used and I trust who it goes to, I will be more honest and engaging.
It doesn’t matter which kind of professional asks me, just as long as they are not on my ward.
The clinical and corporate staff interview schedules drew on the findings of WP2. Flash cards for clinical and corporate staff had six themes: changes in service in response to patient feedback, ways of communicating patient experience, resources for patient experience feedback, understanding patient experience data, collecting and using patient experience feedback, and service user and carer involvement (see Chapter 5 and see Appendices 9, 11 and 13). Illustrative quotations were taken from WP2 interviews.
Participant information sheets, consent forms for each participant group and an easy-to-digest recruitment flyer for service users and carers were developed with advice from the MHF (see Report Supplementary Material 2).
Conduct of the interviews
Realist interviewing is often described as a process that ‘involves a highly specific and carefully planned route march which goes between the qualitative and quantitative traditions’. 36 This is because of the way in which the semistructured interviews are constructed and conducted, namely because they contain material about the programme theories, which is then presented to participants and discussed in a very purposeful way. In realist interviewing, the participants are likely to be sensitised to mechanisms and understand contextual constraints on outcomes; the interviewers are likely to bring theoretical knowledge to the understanding of patient experience feedback processes. 140
Realist interviews proceed iteratively. They employ a strategy of curiosity, whereby you see if the kernel of knowledge you uncovered in one interview holds true in a different context or if it is, in fact, being moderated by mechanisms that were perhaps not present in the other setting, resulting in different patterns of outcomes.
At the start of each interview, consent was obtained or, if it had been obtained by the R&D team, consent was checked with the participant. Interviews were audio-recorded. Reflective field notes were written after each interview about the interview process and content, how it was experienced and the ward environment.
Patients and carers were initially asked to describe their experience of giving feedback about their experience in their inpatient settings. This set the context and served to give the participant a chance to become more comfortable in talking about themselves. Once a participant had settled into the interview, the flash cards (see Appendices 9, 11 and 13) were introduced for discussion. Patients and carers were asked to select whichever card they felt was most important to discuss first and asked to explain their reasons for the selection. The theme labels were usually presented first to see if they agreed with them before the cards were turned over, uncovering the quotations, to aid further probing of their ideas. If participants had difficulty with literacy or reflection, the ideas on the cards were raised without necessarily presenting the cards. The researchers undertaking patient interviews also adapted their interview style based on how unwell the patient was at the time of the interview.
Interviews with staff followed a similar format using the staff flash cards (see Appendices 9, 11 and 13). A few staff interviews took place in pairs if this was the only way to engage the staff members (e.g. over a tea break).
Interviews with patients and staff all took place in a confidential room in clinical settings. Carers were mostly interviewed by telephone, with some being interviewed in person in a confidential room on the ward.
If participants became distressed during their interview, they were offered the opportunity to take a break or to terminate the interview. All participants were informed that the study would not affect their clinical care/work and they were given 2 weeks to withdraw their consent to the use of their data following the interview.
After each day of fieldwork, the three researchers collecting data discussed and reflected on the challenges they had faced. The senior researcher in the team provided in-the-field training, particularly on how to manage interviews in the busy, understaffed and often disrupted setting of the ward and how to manage interviews with the more unwell patients.
Data management
Interviews were fully transcribed, anonymised and checked against the audio-recording. Each interview and the accompanying field notes were given a unique identifier. All data were imported into data analysis software (MAXQDA12) for coding. Coded data were exported to Microsoft Excel for identifying CMO configurations. All data were stored securely. Audio-recordings were destroyed at the end of the project.
It was expected that, during these interviews, disclosures might be made that might require action to be taken outside the project. A detailed disclosure log was maintained and the chief investigator reviewed each disclosure as it was logged and ensured that appropriate action was taken.
Data analysis
Analysis took place in two phases. Initially, the research team explored the raw data with the PPIT and together they developed key themes for the thematic coding framework. Thematic coding was then undertaken to provide a platform for the second analysis phase. The latter phase involved refining the analysed data into CMO configurations. Retroduction was used in both analysis phases, as follows.
Retroduction as a form of reasoning in realist evaluation
There are two classic forms of reasoning and logic: deductive (when you start with a theory or observation and see if what you find matches what was expected) and inductive (when you arrive at conclusions based on observations from your data). 141 Realist research uses a third logic of reasoning known as retroduction. This is based on observation and what are sometimes called hunches or associations, meaning that it involves moving backwards and forwards between what is observed and a priori theories or hypotheses, to try and uncover what is producing the observable outcomes while accepting that the things that are causing these may not be visible. In this way, retroduction ‘uses both inductive and deductive logic, as well as insights or hunches’. 141 This logic in realist evaluation is used to theorise programmes and formulate CMOs.
The analysis took account of what was said in interviews, any observations recorded in field notes and any feelings recorded in field notes and coding memos. This uses what we called the ‘three ears of listening’ to make sense of the data. We accounted for what was said (explicit statements; ear 1), what was implied (ear 2) and what was unsaid (that which did not appear and was conspicuous by absence or was present in the felt observation rather than directly expressed; ear 3). To understand data in these three different ways required a robust analytical framework and iterative discussion among the research team members about meaning. It would have been easier to code thematically using ear 1, but it was the use of all three ears that yielded some of the deeper understandings in relation to generative mechanisms.
Analysis phase 1: development of the thematic coding framework for analysis
A draft coding framework was developed with the PPIT. At the outset, PPIT members said that they did not want to receive or review written material or presentations. They wanted material presented in conversations for discussion.
Research team members identified portions of transcripts that they thought contained CMO configurations and acted them out (anonymously) at PPIT meetings. They asked PPIT members to identify key themes and points of significance. PPIT members worked in small groups with a facilitator who made mind maps or lists of these ideas, dependent on group preference. From this, key superordinate themes were developed and imported into MAXQDA12.
Members of the full research team each read transcripts from different types of participants and discussed the superordinate themes identified by PPIT members. The superordinate themes then formed the basis of the coding framework for the staff data. The coding framework was further developed during further coding and research team discussion and emergent themes were added during analysis (see Report Supplementary Material 4). The thematic coding of all the data was done by the three researchers on the research team and included independent coding by two researchers of 100% of the data, followed by comparison and discussion to ensure consistency of coding.
During the process of coding, it became clear that we could not view time as a flat concept. We needed to break down the process of collection and the use of patient experience data to understand in what ways, when and where decisions were being taken and actors’ reasoning was shifting in relation to the resources available to them. 38
To capture this notion of a process, we superimposed the time dimension onto the developing themes by laminating the coding framework (in keeping with the patient experience data cycle) according to the following process sequence: collecting/giving feedback, receiving/listening to feedback, acting (analysis and response to feedback), and quality improvement and change, including feeding back to patients/carers [collecting and giving, receiving and listening, analysing, and quality improvement and change (CRAICh); Figure 7].
FIGURE 7.
The CRAICh coding architecture. QI, quality improvement.
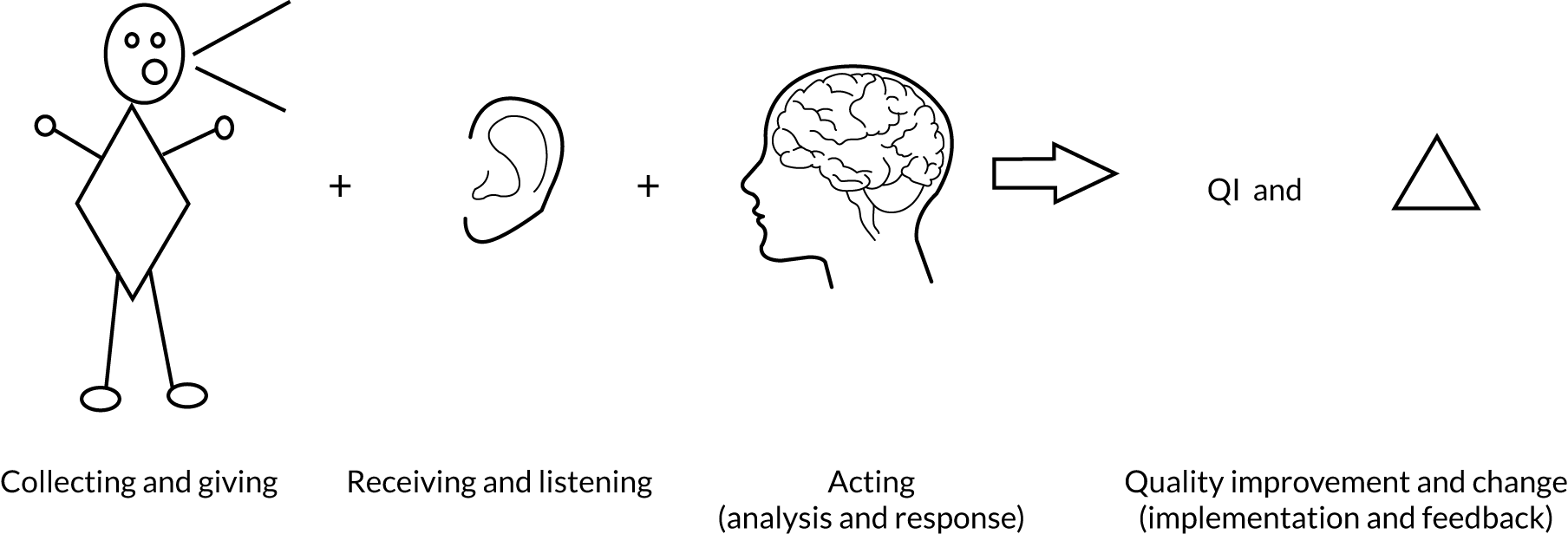
A further lamination within the coding structure was the different participant perspectives (patients, carers and staff). Therefore, the coding framework consisted of the CRAICh framework providing the time dimension, themes identifying content relevant to the development of CMOs and the participant perspective (staff, patients and carers).
A note was made during the coding process of any potential CMO configurations. In addition, there were codes relating to the data needed for the economic analysis (see Chapter 8). During data coding, further themes not directly related to CRAICh but of relevance to the collection and use of patient feedback emerged. These were added to the coding framework.
Analysis phase 2: development of the context–mechanism–outcome configurations
The first step was to export all coded text chunks into Microsoft Excel following the laminated structure of the coding framework. The data coded for the economic analysis and for themes not directly related to CRAICh were not exported.
Each section of CRAICh was exported into a different Excel sheet. In each Excel sheet, the text chunks were grouped first by theme and then by participant perspective. Starting with the CMO configurations noted during thematic coding, Sarah-Jane Fenton compared the relevant text with all the other text in the same lamina. Through this process, data from different field sites were compared. By moving back and forth across the data in the same lamina, the original CMO was refined and further CMOs were identified and refined.
This iterative process allowed us to understand how context interacted with mechanism (reasoning and resources) to produce an outcome. Outcomes from the same mechanism might be different in different contexts. The process was then repeated for all CMO configurations noted during thematic coding and then for all remaining lamina in the coding framework. Frances Griffiths read approximately 30% of the data and reviewed all CMOs with Sarah-Jane Fenton as they were developed. We found many factors interacted, even when we had refined our CMO configurations. To ensure that we produced CMO configurations of use to the NHS and other health provider organisations, we avoided reducing the CMO configurations to every possible combination of C, M and O, as this can make the results unreadable.
This analysis allowed us to understand how, why, in what circumstances and for whom the process of patient experience data collection and analysis was being used to improve the quality of care. Each CMO provides understanding of how and why a mechanism was activated or not and the context for this. The CRAICh framework for the CMO configurations helped to indicate where in the patient experience feedback process and for whom mechanisms were activated in relation to the different reasons and resources of actors.
These findings were then used to further iterate our mid-range programme theories. The initial theories are shown along with the results of WP3 in Appendix 17.
Results
Study participants and data
Care was taken with the theoretical sampling of all three recruitment groups. At least one participant was recruited from each ward providing care for adults with mental illness in each trust (see Appendix 15). Across the six sites, 182 interviews were completed, 62 with patients, 19 with carers and 101 with staff (Table 5). The average interview durations were as follows: staff, 43 minutes; carers, 32 minutes; and patients, 32 minutes. There were 40,000 words of field notes generated.
| Site | Patients (n) | Carers (n) | Staff (n) | Total (n) |
|---|---|---|---|---|
| NHSProvA09 | 11 | 4 | 16 | 31 |
| NHSProvA13 | 11 | 4 | 18 | 33 |
| NHSProvA27 | 10 | 3 | 16 | 29 |
| NHSProvA29 | 10 | 2 | 18 | 30 |
| NHSProvA33 | 10 | 4 | 16 | 30 |
| NHSProvA37 | 10 | 2 | 17 | 29 |
| Total | 62 | 19 | 101 | 182 |
The staff who were interviewed were drawn from a range of professional backgrounds including psychiatry, nursing, occupational health, health-care assistance and health-care management. Staff were sampled at all levels, including those who worked in business support or on information technology (IT) operational functions to ensure that complexity in relation to the case was uncovered. We had representation from all relevant staff groups in the interview data for each of the six case sites and no professional groups were overlooked.
One patient who had agreed to be interviewed became unwell and did not recover sufficiently for interview before fieldwork was completed at that field site. Although some participants became distressed during interviews, no participant chose to terminate the interview. Sixteen disclosures including one whistleblowing incident were made during the course of fieldwork.
The recruitment of carers proved difficult. There were several reasons for this: carers were generally poorly engaged with wards, and many patients were often isolated and did not have carers or people they were close to. Such patients reported either becoming isolated as a result of their illness or isolation being a contributing factor to their illness. Some family members did not want to identify themselves as being in a role related to the care of the patient and some were resentful of being seen in this role. A number of carers also reported struggling financially themselves, so finding time (and fares) to visit relatives or friends was increasingly difficult.
Findings from analysis phase 1: key themes
The PPIT identified five superordinate themes that were retained throughout coding and analysis discussions. The five themes identified were as follows: (1) wellness, (2) the importance of feedback, (3) relationships and communication, (4) resources and (5) power. Each of these operates in different ways within different laminations of the framework, namely at different stages of CRAICh (the patient experience feedback cycle) and in relation to different types of participant.
The thematic analysis relevant to CRAICh was based on 10,812 of a total of 12,026 coded excerpts. The other coded extracts related to the economic analysis or to emergent themes not directly related to CRAICh: professional caring capacity, the experience of delusions and the experience of the Mental Health Act. 33 The analysis reported here will focus on the themes related to CRAICh and to the emergent themes.
Data from some participant perspectives were more dominant than data from other participant perspectives within different parts of CRAICh. For example, the majority of coded excerpts from patients and carers were in ‘collecting and giving’, with relatively few patient- and carer-coded excerpts in the remaining CRAICh lamina (Table 6). For staff, coded excerpts were more evenly distributed, although the majority were located in the first two CRAICh lamina. This, in part, reflects the attention that all trusts pay to collecting feedback, but also that more staff time is invested in obtaining feedback than in making sense of it, implementing changes or feeding back to staff, patients and carers.
| Participants | Collecting and giving | Receiving and listening | Acting (analysis and response) | Quality improvement | Change and feedback | Total coded excerpts |
|---|---|---|---|---|---|---|
| Carers | 248 | 46 | 11 | 8 | 18 | 747 |
| Patients | 3146 | 96 | 25 | 2 | 19 | 4040 |
| Staff | 1769 | 1405 | 813 | 260 | 770 | 6025 |
| Total other | 1214 | |||||
| Overall total coded excerpts | 12,026 | |||||
The full coding framework can be found in Report Supplementary Material 4.
We report each of the superordinate themes using data from across the six field sites along with supporting quotations. We indicate links between themes and links between themes and the second phase of analysis.
In bold we summarise what our data indicate to be the key issues for health-care organisations regarding how to collect, analyse and use patient experience feedback to improve the quality of inpatient services. These summaries formed the basis for what we termed ‘rules’ developed for presentation to the consensus conference (see Chapter 7).
Theme 1: wellness
The wellness of adults in inpatient settings influenced both when people felt able to give meaningful feedback on their experience and how that feedback was received.
Patients reported that they would like to be asked about their experience at the start of their admission. Patients acknowledged that on admission, however, they were often extremely unwell and struggling to make sense of their experiences:
I was very poorly when I came . . .
Do you not think you would have given your feedback then?
Well I could have done . . . If I’d been asked, yes, I would have done.
I wouldn’t have, I was, you know, the first few days I was, I don’t really, I wasn’t, like, really sort of aware of my surroundings.
Despite this, patients expressed very clearly that they could tell staff if they were having a positive or negative experience irrespective of the acuity of their illness.
When asked about more formal feedback (e.g. ward meetings and surveys), patients reported that, from around halfway through their admission (i.e. when they were beginning to feel slightly better), they would be able to offer feedback on their experience of the ward, the staff, their care and their treatment, and be able to offer reflections about changes, for example what was working well and what could be working better.
Despite this, patients felt that offering feedback at the end of their admission on both the environment (physical milieu) and the culture (of care) would be preferable. At this time, the patient not only felt better but the balance of power between the patient and staff/organisation was also less asymmetrical, as the patient was about to leave the ward. This was particularly so for involuntary admissions (see Theme 5: power).
Patients wanted their experience feedback gathered at different points during their stay:
-
feedback on their individual day-to-day experience needed gathering day to day and irrespective of wellness
-
reflective feedback on the inpatient unit was best gathered mid-stay and at the end of their admission.
In contrast, the staff maintained that patients on the ward were often too unwell for them to obtain feedback. Some staff felt that inpatient settings were an inappropriate place to obtain feedback or that the feedback would be unhelpful. This was, in part, because they felt too stretched in terms of staffing levels to have the time to sit with patients who were very unwell and make sense of their feedback. It was also because they felt that they lacked the agency to do anything with the patient feedback.
Everybody on the ward is incredibly unwell . . . as soon as there’s any sign of improvement you’re discharged . . . So it’s a very difficult group to get a clear view of what their experience has been. Because it is clouded by potentially a lot of mental health issues as well. And once people leave, they don’t necessarily want to talk about it anymore . . . You get this view that patients aren’t happy. And some of that is then dismissed, ‘Oh that’s just their illness’ . . . or you don’t get anything out of them.
PTA37.Staff13
Our analysis suggests that patients are not too unwell to explain how they are feeling in relation to their care at any point during admission. Patients may, however, need time to feel better in themselves and make sense of their environment before they can offer reflective feedback on the quality of their care and make suggestions about improvements or commend what is good practice. The collection of patient feedback by staff is difficult when wards are under-resourced.
Theme 2: the importance of feedback and seeing changes
Patients, carers and staff said that feedback was valuable and important in relation to trying to improve services. Experiences from patients, carers and staff were valued. However, our data suggest that positive feedback was not used constructively in inpatient mental health services. Although there were concerns cited by some participants about the standard of clinical care and services being delivered in the case study sites, an equal amount of praise was offered. Patients articulated how they spent time thinking about the way to frame and phrase praise, about how to say thank you or demonstrate this, and about why they were thankful. Some staff described examples of their experience of this:
I’ve got some chocolates; a patient brought some chocolates onto the ward just to say thank you for just even talking to her for half an hour. And it’s just, for us it’s the, it’s not, it’s something part of our role, but obviously it means something to them . . . and then we had another patient who was so unwell, and he came back and it was a really warm day and he brought a big massive bottle of water for each and every staff member on shift. And you know when somebody, I think that was the biggest gesture that I’d ever sort of really appreciate, ‘cause he didn’t have very much money. To go out and actually buy six, sort of, staff members a full, just to think about us at work, it just, that meant, and he was obviously very unwell, but did that. And I think those things just make a massive difference.
PTA33.Staff02
However, positive feedback was often treated in an (unintentionally) dismissive way by staff. Positive feedback really existed only in the informal sphere and was not fed into formal processes for patient experience data collection or analysis. In some cases, positive comments were recorded in patient records. Change was driven across the six sites largely by complaints or crisis, rather than by experiences of competent care:
For compliments we normally get, when people leave we normally get cards and they’ll write like a nice little message in. And they usually get kept in the office or in the airlock . . . I know there was a time we used to keep them out on the front where you signed in. Sometimes you’ll see families and friends pick it up and have a little read of it. Complaints, there’s a procedure that we can go through, if somebody wants to make a complaint and there’s like forms and stuff.
PTA13.Staff08
Patients were aware that complaints were the type of feedback most likely to elicit a response by the health-care organisation and they wanted to compensate for that:
‘Cause I give them a big box of chocolates last time . . . and a big ‘thank you’ card . . . I think it’s really important . . . staff know they’ve done a good job . . . ‘cause I guess there’s the complaints side of things.
PTA09.ServiceUser05
Patients also identified the importance of thanking staff in order to keep them motivated to care. Staff also reported patient appreciation as a source of motivation. Our data suggest that this is also about the demonstration of power in the relationship between patients and staff. Providing positive feedback to staff empowered patients:
I don’t know, a box of chocolates or a card or something with people . . . the more important is leaving the card to say thank you. Because . . . those staff would keep the card . . . and that’s important. Even if it’s just put away in their drawer or a cupboard somewhere, they’d keep a card, they wouldn’t log it . . . it keeps them caring about what they do. That’s, that’s the most important thing, they all care about what they do. Just ‘cause they’re too busy to give me cigarette break, if I went up to them for anything else, they immediately . . . earlier I said, ‘is there any way you could get me a toothbrush and some toothpaste?’, ‘yes, of course’ and immediately I was given toothbrush, toothpaste, soap, comb and sachets of shower gel.
PTA37.ServiceUser07
Our analysis suggests that positive feedback was seen by both patients and staff as having equal value to negative feedback in maintaining or improving the quality of inaptient mental health care.
Our thematic analsyis uncovered the importance of carers, patients and staff seeing changes and staff being able to make changes in response to feedback:
I’ve been here for 2 months now . . . when you give feedback, if they have the ‘Have Your Say’ meeting . . . it’s not always actioned . . . It’s almost to placate the patients rather than to actually action things.
PTA29.ServiceUser05
When change was not observed, it disincentivised patients and carers from giving feedback and staff from collecting it, as they felt that there was nothing they could do about actioning it:
There’s no point in having all this information if you’re not gonna do anything with it at the end of the day . . . we churn out these reports and the services go, ‘that’s absolutely fantastic. We can use that. Let’s go do this, this and this’, but we as a team don’t, don’t necessarily get that feedback back [about] what [the service has] done with all that information.
PTA27.Staff02
However, meaningful change is often hard to achieve, requiring experienced and motivated staff working together:
My patients often talk about never seeing their named nurse, so . . . we talked about which of these broader patterns will actually give a more consistent named nurse to the patient . . . once that we get some of those people together then that’ll drive the change through the culture . . . it is also about sustaining that change . . . that’s where it probably gets the most tiring . . . you are faced with resistance . . . cultural change where it has happened has been done by the people who are . . . more experienced, taking a lead and actually making that their focus. And then coming together and having a common vision sometimes is very helpful.
PTA13.Staff01
Relationships and communication (theme 3) and resources (theme 4) have an impact on staff motivation as discussed in these themes below. Seeing changes from feedback is important if there is to be further collection of feedback. This is explored in greater detail in the second phase of analysis (see Findings from analysis phase 2).
Theme 3: relationships and communication
Relationships between staff and patients and between staff and carers, and the quality of communication around care, was a theme that intersected all of the other themes. It activated generative mechanisms that we explore in the second phase of analysis. This theme is particularly important for understanding other themes, particularly theme 5 (power) and how it operates in adult inpatient settings.
Patients and carers expressed mixed views about whether they would talk only to certain staff members or if they would be happy to approach anyone on the ward. This largely seemed to reflect their personality type and confidence in communicating:
So you don’t mind who you talk to, as long as you get the chance to share your opinion as the person’s carer?
Oh, no, I like to talk to certain people . . . Because I trust them.
However, relationships moderated both if and how patients or carers gave honest feedback to staff. Without an existing relationship, patients or carers would offer feedback only selectively and only about particular issues. Understanding in more detail how these relationships were built and how they functioned in certain conditions was a critical part of the second phase of analysis (see Findings from analysis phase 2).
Across case study sites, it was evident from both staff and patient narratives that opportunities for staff to get to know patients had reduced as wards dealt with more severely ill patients, over shorter lengths of stay. It was difficult to establish therapeutic relationships, as staff were unavailable to talk to patients because the ward was short staffed or there were high levels of agency staff. Patients described finding it hard to approach staff with feedback when they were very unwell. When staff took the time to talk to them in their distress and listen to them, and to try and establish a rapport, patients reported that they found it much easier to communicate about their individual experience and experience of the ward. Our analysis suggests patients were likely to provide honest feedback only to staff whom they felt that they knew and trusted.
The impact of lack of staff on communication was particularly felt by carers. Relationships with carers were particularly fraught in two case study sites. Communication depended on how busy the ward was and, therefore, on how available staff were. In some of the sites identified as ‘green’ in the WP2 typologies, there were bespoke support services for carers and more involvement of carers in care-planning. However, on many of the wards visited in the study, there was no demonstrable culture of including carers in care-planning other than in a tokensitic way. The result was that carers often felt excluded or thought of themselves as annoying the staff:
You’re in a state of high emotion when they first have to go into a mental hospital . . . we didn’t know what the system was . . . and nothing really was explained to us. In fact, we were sidelined, really, we felt. And our daughter was taken away, and she was talked to by the team that . . . had sectioned her, ‘we’re going to put her into hospital’ . . . which is fair enough, ‘cause that’s their first priority. But we didn’t even know there was a social worker, no social workers, if there’d been one, had come out and said ‘these are your rights’ . . . so we need some information. Not everybody can take it in at that time.
PTA29.Carer02
I’ve obviously had a lot of communications with . . . with quite a few of them, and you do get the sense that you’re being a little bit annoying sometimes . . . But I mean, it’s because . . . you haven’t got that information . . . so you have to keep asking. And you do feel a bit of a nuisance . . . you see the look on their faces . . . that they’ve had enough of the X family, that sort of thing, that particular day perhaps. But I mean, that’s understandable, because we do ask a lot of questions. Because obviously, when you’re not in control of your husband’s care . . . you’re going to worry all the time, aren’t you, so, yeah.
PTA29. Carer01
Carers reported being particularly aggreived when they felt that staff did not prioritise listening to them, particularly when the feedback about the patient they were close to could have helped inform the staff in caring for them better:
I did have to complain to the head of the hospital, a chap called X I think his name is. Because, because of the way I was treated in a review by the consultant, a temporary consultant whose attitude was totally inappropriate, downright rude. So when I came out of the review, I told him as well, I told him in the review his attitude was totally unacceptable. As soon as I came out, I contacted X who’s the deputy director of the hospital and, you know, he took it on board . . . but, you know, not much was done.
PTA33.Carer02
I find it’s generally the nurses . . . or the managers in the ward. They are up against it in terms of time . . . they’ve got lots of people to look after with very little staff . . . My daughter’s last admission at one point, spoke to a nurse and said that I need to talk to you and she said, ‘give me a minute’, and she didn’t come back for 10. And I’d more or less forgotten then what it was I wanted to tell her . . . But so they’re so busy that sometimes I think they, they might treat us with a bit of disdain.
PTA29.Carer02
Carers often witness poor care but struggle to report this, as they are concerned about the potential impact on their friend or family member. This is explored further in Theme 5: power.
Our analysis suggests that when staff proactively engage with carers, they can provide intelligence about how best to provide care for the person they care for and about the quality of the care being provided.
Much of the data from staff related to the relationship between corporate and clinical staff and who owned and was empowered to use patient experience data. There was a lack of connection between data collected on wards and their use by wards in the majority of the case sites. The analysis of the data collected was not received by wards in a timely way; it was often redundant by the time it was returned. This reduced staff motivation to collect patient experience data. Staff felt that, in many cases, patient experience data were more about accountability than quality improvement, and that corporate staff engaged with patient experience only when prompted by external agencies or in response to patient safety incidents. When corporate staff were in tune with the wards, or had experience of working at the ward level, they were aware of this perception. This corporate–clinical divide existed to a greater or lesser degree in all case sites:
Collecting and using patient experience feedback . . . it is true, it is staff and patients’ willingness to be involved. You can’t keep flogging a dead horse and trying push people to, to do things if they don’t want to . . . I think they are getting feedback, but they don’t see it as patient experience . . . and the last thing that I want to do centrally is to pile more work onto the clinicians who are run ragged anyway . . . and I often think when you work in corporate, they all think, ‘oh, corporate only come in when it’s bad news, oh’ [laughs]. So I want to try and change that a bit . . . and be seen as a team that’s supportive . . . to the frontline staff, rather than someone that turns up when something’s gone badly wrong on the ward, you know.
PTA27.Staff08
Our analysis suggests that the collection of patient experience data was perceived by ward staff as serving corporate goals, rather than driving local quality improvement.
Theme 4: resources
The theme of resources related to staff having both physical resources (time, supportive line management structures, data collection systems, etc.) and emotional resources (being willing and able, staff burnout, supervision and the culture of the organisation) to receive feedback from patients about their experience.
Staff reported that the bureaucratisation of care meant that they had less time to spend with patients and that this affected their ability to receive patient experience feedback. Similarly, patients found that staff not having sufficient time to spend talking to them affected their ability to give feedback:
I find that . . . a lot of my job is sat at a computer ticking boxes . . . to say that we’ve met kind of patient experience, but I feel, sometimes a patient experience is things like one-to-ones with patients . . . a lot of the time we don’t even get time to do that . . . ‘cause I’m too busy at the computer doing . . . risk assessments.
PTA03.Staff13
They’ve got too much paperwork to do. There’s way too much paperwork and there’s not enough staff. There’s not, there’s not enough staff on the ward, because they’re all in the office . . . most of them are writing . . . there’s only about four staff on a shift, so if you think about it, that’s three, two writing, one doing meds [medications] and one doing the obs [abservations]. Who’s supposed to come round and actually settle and calm, there’s nobody to talk to ‘cause there’s nobody free.
PTA09.ServiceUser10
Staff, patients and carers all commented on the negative effect on the collection of patient experience feedback of having agency staff on wards. They acknowledged that some individuals were good but there was no opportunity for agency staff and patients to build rapport, nor for these staff to work alongside and communicate well with their colleagues. The lack of resource negatively effects relationships and communication (see Theme 2: the importance of feedback and seeing changes):
Some of the other staff are very good. But 9 times out of 10 they’re only there on a temporary basis, ‘cause they’re filling in as bank [agency]. I find it difficult, I’ve had to form a relationship with him, so I can imagine what my daughter’s like, she sees a different face every day . . . But at least there were the consistencies of the two senior nursing staff there that she could go and speak to which is an improvement . . . ‘cause you don’t know who you’re gonna see from one day to the next.
PTA09.Carer03
Our analysis suggests that staff need the resources, both emotional and physical, to enable them to spend time with patients, understanding their experiences of inpatient settings. This can be seen as augmenting and illuminating the theme of relationships and communication, and highlights the centrality of the latter to the giving and receiving of honest feedback.
The ways in which generative mechanisms become activated and lead to staff feeling disempowered and not seeking patient experience feedback are explored in greater detail in the second phase analysis (see Findings from analysis phase 2).
Theme 5: power
Power was a theme that the PPIT felt very strongly about, as it connected to the team members’ own experiences. The theme of power emerged across the laminations of our data and was acknowledged as an issue for patients, carers and staff alike.
Staff discussed their power (or lack of it) to effect change and their power in relation to the corporate and clinical functions of services. However, most of the staff data related to power was about the different power dynamic between staff, patients and carers for involuntarily admissions compared with voluntary admissions. For patients and carers, the deprivation of liberty involved in an involuntary admission magnified the effect of the power asymmetry between patient and clinical staff that exists in any patient–clinician relationship. For patients and carers, their relatively powerless position in relationships with staff damaged individuals’ ability to give honest feedback.
Carers, in particular, cited needing to be strong in order to give feedback when this was met with resistance or hostility or when they were ignored. Other carers talked about the importance of maintaining good relationships with the staff and not being too pushy, which was felt to be counterproductive.
A fear of reprisals, fear of impact on clinical care and fear of sometimes petty and sometimes more serious retaliation from staff members were cited by both patients and carers as some of the main reasons why feedback would not be shared outside a trusting relationship with staff and only under certain conditions. Staff reported something similar, in the sense of being anxious about being the subject of complaints:
The first one that I went to, that was where I made my complaint . . . and it wasn’t like I even felt like the staff disliked me. There were a few that, that rooted for me [laughs]. But they really did dislike me and it was really difficult being there . . . I don’t know whether it was because, like, it definitely wasn’t because I made the complaint, because, like, I did the complaint after some really horrible comments . . . and, I don’t know, I don’t think that helped but . . . I didn’t have any trust in that ward really.
PTA29.ServiceUser03
In the past when I’ve had handovers and said, you know, ‘be very careful with this family ‘cause they’ve put a big complaint in about such and such . . . and it’s still under investigation, or it got sorted and they weren’t happy, so you have to be very careful with these people, you have to be very careful with the patient in case you rock the boat and set things off again’ . . . I think there was a stigma . . . some of them do tend to take it out on the patient, even though it’s not the patient’s fault.
PTA13.Carer04
When it was difficult to establish trusting relationships, such as when there was a shortage of permanent staff or when the quality of care was poor, patients and carers were less likely to give honest feedback about their experience.
Power differences in relationships made the establishment of trusting relationships difficult. This was mostly perceived by patients and carers, but staff were also aware of the effect of power differences. Patients and carers reported a fear of retaliation from staff if they provided feedback, suggesting a lack of recognition by staff of the impact of power differences on patients and carers and a lack of accountability of staff for their actions. When poor cultures of care exist, it is less likely that honest feedback from patients or carers will be obtained.
Our analysis suggests that authentic feedback can be given and received only when there is a transparent and accountable culture.
In the analysis of CMO configurations, the contexts in which patients and carers felt able to give (and receive) honest accounts of care (or not) and the generative mechanisms that facilitate this are identified.
Findings from analysis phase 2: context–mechanism–outcome configurations
Although the thematic analysis was rich in detail, on its own, it did not provide sufficient evidence to help us understand how, for whom, in what circumstances and why underlying generative mechanisms were being activated. This was the purpose of the realist analysis in which CMO configurations were developed.
From the 12,026 coded excerpts related to CRAICh, 154 CMO configurations (see Appendix 16 and Report Supplementary Material 5–9) were developed. Not all coded excerpts from the thematic analysis were used in building CMO configurations, as not all excerpts helped to uncover generative mechanisms or to inform the wider context or outcomes (Table 7).
| Theme | Number of CMO configurations for each stage of CRAICh | |||||
|---|---|---|---|---|---|---|
| Collecting and giving | Receiving and listening | Acting (analysis and response) | Quality improvement | Change and feedback | Total | |
| Wellness | 10 | 3 | 2 | 0 | 2 | |
| Importance of feedback | 10 | 7 | 4 | 6 | 10 | |
| Relationships and communication | 20 | 10 | 1 | 4 | 4 | |
| Resources | 7 | 6 | 3 | 2 | 6 | |
| Power | 15 | 10 | 2 | 4 | 6 | |
| Total | 62 | 36 | 12 | 16 | 28 | 154 |
| Number of excerpts used to generate CMOs | 1449 | 292 | 166 | 141 | 295 | 2343 |
| Total excerpts in original data set | 5163 | 1547 | 849 | 270 | 807 | 8636 |
As expected, the relevance of each theme varied across CRAICh. For example, the themes of wellness and of relationships and communication were important in relation to the collection and receiving of patient experience feedback but not at other stages of CRAICh. The importance of feedback (which includes ‘seeing change’) is predominant at the implementation, quality improvement and change stages in CRAICh (see Table 7).
The majority of CMO configurations based on patient and carer data relate to collecting patient experience feedback, whereas the CMO configurations based on staff data mostly relate to receiving that feedback, although there are CMO configurations across the CRAICh cycle reflecting different staff roles within the process (Table 8).
| CMO | Number of CMOs for each stage of CRAICh | ||||
|---|---|---|---|---|---|
| Collecting and giving | Receiving and listening | Acting (analysis and response) | Quality improvement | Change and feedback | |
| Patient CMOs | 38 | 3 | 1 | 0 | 3 |
| Carer CMOs | 7 | 1 | 0 | 1 | 4 |
| Staff CMOs | 17 | 32 | 11 | 15 | 21 |
| Total CMOs by CRAICh | 62 | 36 | 12 | 16 | 28 |
| Total CMOs | 154 | ||||
All 154 CMO configurations are available in Appendix 16 (see also Report Supplementary Material 5). The results presented in the following sections draw on all 154 CMO configurations that we developed within CRAICh. We present here only examples of CMO configurations, which were chosen as they had the greatest number of underpinning data.
Collecting patient experience feedback
In Table 9 we present a set of patient and staff CMO configurations related to collecting patient experience feedback.
| Collecting patient experience feedback | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Reasoning | Resources | |||
| Patient CMO: relationships and communication | Patients are unwell (often with hallucinations), feel insecure and vulnerable, are struggling to make sense of what is happening to them and are often confused about ward systems and staffing |
Patients find it difficult to talk to staff members who they do not know and with whom they have not had the opportunity to build a trusting relationship Staff taking time to understand patients individually builds rapport and trust. This establishes feelings for the patient of safety and of being accepted A consistency in the approach across the staff team functions to contain patients’ anxieties and establish rapport When patients are trying to make sense of their experience, particularly if they have been confused or experiencing hallucinations, the familiarity of seeing the same people regularly is important to them while they continue to process and are reality-testing Some patients reported trust issues related to historical trauma or abuse that were exacerbated by inconsistent care when they were on the ward |
Consistent ward staffing, with staff having time to spend getting to know patients and willing to make an effort to get to know patients individually and hear what the patients are trying to tell them A consistency in the approach across the staff team |
Patients give feedback; feedback is likely to be honest when a patient has developed a trusting relationship with a staff member and/or the wider team |
| High levels of staff turnover/agency staffing with an inconsistency in the approach across the team, and staff not having time to spend getting to know patients and/or unwilling to get to know patients individually and hear what patients are trying to tell them | Patients do not give feedback or give feedback that is not true to their experience | |||
| Staff CMO: relationships and communication |
Staff understand that making time to sit with patients one-to-one is the most effective way of getting honest patient experience feedback Staff are aware that they can also get patient experience feedback informally through building relationships with carers |
Staff build relationships with patients to build trust and so patients feel safe, which makes them more likely to share their experiences Staff often perceive that their presence on the ward is sufficient to signal their availability for conversation, and that patients and carers can ‘always’ approach them Some staff feel that patients should take responsibility for expressing themselves/giving feedback, rather than staff having make the initial approach Some staff report being anxious or not confident in starting conversations about individuals’ experience, as they do not know ‘what’s gonna come back the other way’ |
Staff are not proactive in seeking feedback but are able, willing and confident to make time for one-to-one conversations if asked. Their availability is moderated by resource pressure Patients are proactive in seeking engagement with staff |
Patient experience feedback is obtained |
|
Staff are not proactive in seeking feedback but are able, willing and confident to make time for one-to-one conversations if asked. Their availability is moderated by resource pressure Patients are NOT proactive in seeking engagement with staff |
Patient experience feedback is obtained | |||
| High staff turnover on inpatient wards | Building relationships with patients is difficult, but, conversely, patients are not always being asked the same questions so do not get impatient with giving feedback as readily | Different staff ask different questions | Patients do not get impatient with giving feedback as the questions asked vary | |
| Patients are frequently returning to the same ward | There is an opportunity to build a relationship over time and so to be able to obtain feedback, although when patients are discharged too early because of bed pressures, patients can be cross. Staff then have to build the relationship back up. Other staff report that these patients have no interest in giving feedback | There is sufficient bed capacity for frequently returning patients to stay until they consider themselves well | Some frequently returning patients provide patient experience feedback | |
| There is NOT sufficient bed capacity for frequently returning patients to stay until they consider themselves well | Patients unlikely to provide patient experience feedback | |||
These inter-related CMO configurations reflect the complexity of building an understanding of relationships and communication in an adult inpatient setting. The patient CMO configurations focus on the importance of consistency and rapport-building with staff, which allows them to trust the staff, feel understood and give honest feedback. When there is a lack of opportunity to spend time with staff, patients can feel anxious, mistrustful, fearful and confused and this can result in patients not giving feedback that is true to their experience. Our analysis suggests that patients building rapport with staff leads to trust developing and, without this trust, patients are unlikely to give feedback that is true to their experience.
The staff are aware that one-to-one time is the most effective way of eliciting patients’ experiences and feedback, but they do not always approach patients. Instead, they consider that their presence on the ward indicates their availability for engaging with patients and expect patients to approach them. Staff availability for patients is often limited when there is understaffing or high staff turnover.
Our CMO analysis regarding wellness suggests that, when patients are unwell, they find it difficult to be proactive in approaching staff and that staff need to show concern and spend time with them exploring their experiences (see Appendix 16 and Report Supplementary Material 5). Our analysis suggests that all staff members need to be proactive in approaching patients for feedback and have time to spend building relationships and gathering patient experience feedback in inpatient settings.
Receiving and listening for patient experience feedback
In Table 10 we present a set of staff CMO configurations about receiving and listening for patient experience feedback.
| Receiving and listening | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Reasoning | Resources | |||
| Staff CMO: resources |
Adequate/inadequate staffing levels Requirement to complete extensive documentation, particularly for risk management |
Less time to spend with patients reduces engagement that enables patients to give and staff to receive feedback Staff do not feel confident about engaging with patients and put boundaries in place with patients, as they lack supportive colleagues If patients see that there is no change as a result of their feedback or that there is an inadequate staffing level to respond to patients’ concerns, staff are worried about escalation and resulting risk and safety issues |
Staff have time to engage with and support patients Staff have supportive colleagues |
The number of incidents on wards is related to risk and safety issues being kept to a minimum |
|
Staff DO NOT have time to engage with and support patients Staff DO NOT have supportive colleagues |
Increased numbers of incidents on wards are related to risk and safety issues | |||
| Adequate/inadequate staffing levels |
Staff are aware that quality of care deteriorates when they are under extreme pressure Lack of staff time in a high-pressure ward setting results in them ‘firefighting’ rather than leading quality improvement in the light of limited resources Staff feel disempowered and demotivated when they feel unable to provide quality care |
Staff have the emotional resource to receive and act on patient experience feedback | Staff engage with patients to capture patient experience feedback | |
| Staff have reduced emotional resources to receive and act on patient experience feedback | Staff DO NOT engage with patients to capture patient experience feedback | |||
From our CMO analysis, we identified the main mediators of staff shortages and their impact on the collection of patient experience feedback. With staff shortages, staff have less time for patients and are less likely to have supportive colleagues. The lack of support reduces their confidence in engaging with patients. They feel disempowered, as they feel unable to provide quality care. Aware of the lower than ideal quality of care that they are able to provide, they become demotivated. If they feel unable to make changes as a result of patient feedback or do not see change, they feel disempowered and unwilling to collect patient feedback. They also feel unsafe. Our analysis suggests that resource pressures in inpatient settings can mean that staff feel uncertain about seeking honest feedback from patients, as they may feel unable to make changes in response to this feedback.
There were other barriers to the collection and receipt of honest feedback. Patient feedback was often overlooked or ignored because of staff hierarchy and power relationships. For example, health-care assistants who were more available to patients on wards were not always linked into formal recording or reporting structures and so the informal feedback that they received from patients was lost.
Informal feedback (typically gleaned through one-to-one conversations) may yield the most honest and, therefore, useful accounts of patients’ experiences. However, because special systems exist to collect formal feedback, specifically to inform quality improvement, formal feedback is more likely to be used to inform change than informal feedback.
The availability of resources was the key driver for the collection of any feedback, as illustrated in the CMO configuration tables (Tables 9–13) and the thematic analysis. Our further CMO analysis suggests that gathering patient experience feedback was seen often by both corporate and clinical staff as an activity that was seen more as ‘nice to have’ than as an integrated functional component for driving quality improvement.
Acting on patient experience feedback (analysis and response)
Table 11 presents a staff CMO configuration related to acting on patient experience feedback.
| Acting on patient experience feedback | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Reasoning | Resources | |||
| Staff CMO: the importance of seeing changes/feedback |
Formal and informal, qualitative and quantitative patient experience feedback is collected In some trusts, patient feedback is collected electronically, and so is available immediately on an electronic dashboard |
If they are given timely formal feedback and access to informal (qualitative and quantitative) feedback, ward staff can perceive the patterns in feedback, relate them to how the ward operates, work out what changes are needed and implement change Ward staff need access to patient feedback soon after it is collected. They can then make changes quickly (it is difficult to respond to something that happened on the ward some time ago) It is difficult for staff to work out whether to respond to one complaint or change services in response to the majority of concerns. Patient experience feedback can feel like a ‘numbers game’ if they cannot see the feedback or how it has been analysed There is a perception that the qualitative feedback ‘never goes anywhere’, whereas the quantitative data are responded to. The qualitative data can enable staff to construct meaning from the data and make sense of them If corporate staff undertake detailed analysis of both informal and formal (qualitative and quantitative) feedback, they will identify patterns to which they can respond in a sustained way rather than having knee-jerk reactions |
Corporate and ward staff receive formal patient feedback soon after it is collected Corporate and ward staff have access to informally collected patient feedback Qualitative and quantitative data are available Corporate and ward staff are able make sense of qualitative and quantitative patient feedback and triangulate them |
Ward staff are able to make changes Corporate staff avoid reactive, knee-jerk responses Corporate staff are able to identify and understand deterioration in the quality of ward care or safety |
Acting often happened independently of the analysis of formal patient experience feedback data. It was sometimes easier to implement changes based on this feedback at a local level and on a small scale than it was to change services based on formal feedback. However, these local, small-scale changes were not always sustained (see Quality improvement and implementing change based on patient experience feedback).
Ratings-based patient experience feedback (such as the FFT) offers little useful information to trusts on why or what elements of service are working or not. This means that wards cannot plan actions or improve quality based on these data alone. When qualitative patient feedback (collected in a more ad hoc way) was analysed, it allowed staff to construct meaning from ratings-based feedback.
Data were often viewed as serving a central purpose and access to patient feedback other than in summary form was often limited. Data that were fed back to wards were often not timely or provided in sufficient detail for planning change. Staff found quantitative indicators were not useful in isolation but qualitative data did not help staff detect trends. In the two case sites that had electronic systems, patient feedback moved much more quickly between corporate and clinical services and was more readily available. However, staff also needed the time and ability to analyse it and make sense of it. When staff were able to do this, they were willing and able to implement change.
Our analysis suggests that some analysis of patient experience feedback needs to be undertaken either at ward level or in conjunction with ward staff, and that feedback loops between formally collected feedback and staff working at the ward level need to be shortened.
Quality improvement and implementing change based on patient experience feedback
Table 12 presents a staff CMO configuration related to implementing change on patient experience feedback.
| Implementing change based on patient experience feedback | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Reasoning | Resources | |||
| Staff CMO: the importance of seeing changes/feedback |
Corporate emphasis on patient feedback collection and curation External requirements for quality assurance from the CQC and commissioners Quantitative patient feedback used to respond to external requirements for quality assurance |
If what is valued is patient feedback collection, the staff focus shifts from understanding the patient experience to recording it Benchmarking statistics within and between trusts are useful, but staff develop a deeper understanding of what is going on only based on qualitative data Fear of the CQC is often a primary driver for implementing changes Collecting and analysing patient feedback is seen as a monitoring exercise |
Corporate provision of analysed patient feedback | Staff disengage from meaningful patient-experience-led quality improvement |
|
Formal complaints procedure Incident reporting process |
Staff investigate, analyse and ‘rationalise’ why an incident has been recorded or a complaint has been made then decide on action(s) to take or changes to implement Fear of complaints, the perceived need to be compliant, risk aversion and pressure from external bodies or corporate services motivates staff to use complaints as the primary source of patient experience feedback that they respond to |
Staff are required to respond to complaints or incidents | Change is driven by complaints and incidents | |
| Staff CMO: relationships and communication |
Patient experience feedback is available Patient safety data are available Other performance data on the provision of care are available (e.g. staffing levels) Data are kept in silos/shared Data are/are not triangulated |
Triangulating different sources of data available in the trust provides corporate and ward staff with contextual evidence and information to understand why things are happening This helps them identify where and what changes need to be implemented The triangulation of data at the ward level allows ward staff to understand why things are happening on their ward and develop a sense of ownership of the changes that are made |
Willingness to collaborate across quality improvement themes (e.g. patient safety, patient experience feedback) Ability to triangulate data from different sources |
Quality improvement takes place based on an understanding developed from a range of sources of feedback/data and is owned and sustained by ward staff |
| Staff CMO: power | Violence and aggression occur on wards |
Reductions in violence and aggression are seen as primary motivators in responding to patient feedback Some ward staff are motivated to enhance patient experience so that patients are more compliant, recover more quickly and do not present in difficult or risky ways on the ward Corporate staff indicate that, when things are ‘so worrying’, they are motivated to implement change and improvement to ensure that incidents are not repeated |
Patient and staff safety is a priority for hospital trusts | Creating a positive experience for patients can ensure that patients are ‘compliant’ and this minimises safety risk |
The implementation of change in response to patient experience feedback was poor across the case sites. This was hampered by resources for both collecting and analysing patient experience feedback and for implementing change in response to the feedback. Even in the case site that scored best during WP2 and had processes in place to collect and synthesise patient experience data, the patient experience data were not sufficient to prompt change. This was a case site in which explicit examples of racism were cited by patients as not being responded to or addressed and in which the culture of care was heavily enmeshed with power relationships.
We found that meaningful and sustained change occurred only when patient experience feedback was analysed alongside other performance data. In almost all case sites, different types of data were being held in silos. The triangulation of patient experience feedback with other data such as patient safety data, clinical outcomes data and complaints helped staff to spot trends or ‘hotspots’. Cause-and-effect relationships as regards serious incidents were much easier to link, and staff were more engaged in using data to understand and innovate within their services. Patient experience feedback often provided the explanation for why trends may be observed at local ward level, which could then inform quality improvement strategies and local action plans.
Without the triangulation of data, quality improvement risks were being driven by targets alone. If a trust centralises its patient experience recording and reporting system and allows its quality improvement to be driven by external drivers, such as the CQC, complaints and serious incidents, staff disengage from collecting feedback and develop a siege mentality motivated by fear (see Appendix 16 and Report Supplementary Material 5).
Our analysis suggests that patient experience feedback alone is not sufficient to drive quality improvement. Instead, it must be the ‘third pillar’ of service planning alongside outcomes and safety data.
Change and quality improvement based on patient experience feedback
In Table 13 we present CMO configurations related to change and quality improvement that, in turn, affect if change occurs, the type of change and the likelihood of sustaining a cycle of change based on patient experience feedback.
| Change and quality improvement based on patient experience feedback | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Reasoning | Resources | |||
| Staff CMO: the importance of seeing changes/feedback |
There is no formal recognition of positive feedback Often, staff seek feedback about the ward environment, as they feel that this is what is relevant for ensuring that patients have a good inpatient care experience Nursing staff are uncomfortable challenging doctors over clinical decision-making or challenging cultures of care Staff are aware that they need to be open to receiving negative feedback rather than resistant to it, as otherwise this impedes change from happening because they deflect the feedback |
Staff do not value positive feedback, as it is not perceived as valued by the organisation and they are trained to be open to negative feedback Staff find that they cannot plan change based on positive feedback because they do not find it specific enough. Negative feedback is often specific Concerns about the patient environment are easier to pinpoint than other aspects of the patient experience, so change feels easier to make Challenging clinical decision-making and challenging cultures of care are difficult, so these aspects of patient experience are not prioritised Positive feedback boosts staff morale, which incentivises them to work in difficult conditions and to care for their patients well, but it is not used to engender change |
Staff ability to plan change based on feedback Staff courage to challenge clinical decision-making and cultures of care |
Change is more likely in response to complaints or criticisms than in response to positive feedback Changes are more likely to be environmental than related to clinical decision-making or cultures of care |
| Carer CMO: the importance of seeing changes/feedback | Carers are interested in quality improvement |
Carers are motivated to offer feedback on their friend’s or family member’s experiences either to change their care or to change services for the future Carers become frustrated when their suggestions are not attended to, if change is not implemented in response to feedback or if they discover that what they are recommending was meant to be happening as standard practice. This motivates carers to complain and generates ill feeling and mistrust |
Time and willingness to listen to carers |
Carers identify areas for quality improvement Maintenance of good relationships with carers Reduction in complaints |
| Patient CMO: the importance of seeing changes/feedback |
Patients notice their experience and any change in their experience Many patients are on wards for relatively short periods of time Patients think change is either not possible or not going to happen |
When feedback is given and nothing happens, patients can feel patronised or as though they are being placated rather than listened to A lack of seeing change decreases motivation and creates apathy about giving experience feedback Giving experience feedback is experienced as disempowering and pointless Patients need to understand how feedback is going to be used to make a difference (for themselves or others) as a motivation for giving honest feedback If patients do not feel that they are going to be in hospital for long, and are therefore not going to be around to see any changes being made, they are less motivated to give their patient experience feedback |
Patients are ignored | Patients stop giving feedback when they see no change in response to their feedback |
| Staff CMO: power |
Staff would like feedback so that they can use it to make changes and understand how the care they are delivering is received Feedback gets sent to corporate services but feedback does not come back to ward staff directly Staff do not understand where feedback goes or how it is used Corporate staff often cite feedback being sent to wards; however, very few staff see or describe using this feedback to create change When positive practice is observed, this is not collected, collated and circulated so learning is not shared across wards Corporate staff often use this patient experience feedback for quality assurance rather than for quality improvement Often, staff describe information cascading down or being sent up, suggesting a power hierarchy in the way that this information and the responsibility for it is perceived |
Staff do not get a response when patient feedback is sent to central management so they do not know how to enact change based on that feedback With no communication from corporate services, staff feel disempowered held back/trapped/inadequate in their responses to patients Staff engage more with patient experience feedback when they can take some ownership for responding to it Quality improvement needs to be driven and happen at all levels of the organisation. Feedback loops enable people to do this |
A dedicated patient experience resource person who liaises directly with ward staff A staff member responsible for shared learning Opportunities to share patient experience feedback across wards |
Feedback is given to ward staff who are then motivated to bring about quality improvement Good practice can be translated across wards |
| Quality improvement is driven from the top down rather than from the bottom up | ||||
Providing evidence of change related to quality improvement was difficult in all case sites. Changes tended to be environmental and measurable rather than cultural, superficial and not sustainable. Positive feedback is seen as superficial and not useful and so staff tend to deflect it, which is disempowering for the patients and carers giving the feedback and a missed opportunity to identify what is working.
Corporate services that fail to share patient feedback in a meaningful way disempower ward staff. When feedback does reach ward staff, the staff can act on it. Ward staff are open to learning from other wards but this needs to be facilitated. Our analysis suggests that services need more systematic ways of using learning from patient experience data to translate this intelligence into effective action plans and that feedback cycles involving telling patients, carers and staff about changes made in response to feedback need to be completed.
What it is important to get right in all patient settings
During our analysis, we identified issues talked about by subgroups of patients. We know from our analysis that it is difficult to get honest feedback from patients on issues other than the ward environment. As these deeper issues were often sensitive for patients, we think they are significant, even though they were raised by only a few patients.
Although there were specific examples of poor care in some sites, we studied each of the following themes, as each was important to get right in all inpatient settings. The four themes were:
-
tackling racism in inpatient settings
-
supporting patients with auditory and visual hallucinations or delusions to communicate about their experiences of care
-
supporting patients to understand their medication
-
supporting patients to understand their care pathways and experience of the Mental Health Act. 33
These four themes were central to a patient’s experiences of services and interacted with all of the other mechanisms we have discussed related to patients, carers and provision of care.
Tackling racism in inpatient settings
A number of patients reported experiencing racism on the wards. This experience was both explicit (e.g. patients cited that they had been racially abused by other patients) and implicit (e.g. patients cited that racist incidents between patients had not been addressed by staff). The experience of racism led to patients feeling completely disempowered. This led to patients disengaging from communicating with staff about their discomfort or distress, remaining silent or not being honest about their experiences when asked:
And so, when you first arrived, and you felt that people were racist and the other patients weren’t being nice to you . . .
They were calling me fake . . . and evil and . . .
And so who did you get to talk to about that here?
Well there weren’t, to be honest, every time someone attacked me, it was like, ‘oh,*name*, you go’ or, you know, ‘move out the way, you’re provoking her’ and ‘you’re preaching’. And I wasn’t really preaching my religion.
Some patients from black, Asian and minority ethnic (BAME) backgrounds felt marginalised by their experience on the ward and were then unwilling or unable to provide honest patient experience feedback. In one case site, even when the patient experience structures were good, the perception of institutional racism changed the engagement in those processes and structures in reality. Our analysis suggests that both explicit and implicit racism on wards, as experienced by patients, needs to be addressed by staff.
Supporting patients with psychotic symptoms to communicate their experiences of care
Both staff and patients reported that patients who were experiencing psychotic symptoms (e.g. auditory and visual hallucinations or delusions and/or impaired reality-testing) were often discouraged from discussing their experiences of care and, in some cases, from discussing their symptoms (e.g. voices commanding them to do things) and their responses to these. Patients described how attempts to communicate about these were dismissed or actively discouraged. Learned behaviours developed around hiding these thoughts to avoid behavioural sanctions or gain rewards such as being granted leave from the ward:
Like the other day when, ‘cause I’ve had to move things in this ward, no one will understand it, but because I know about poltergeists and things I’ve had to go and clean things and move things and stop people doing certain things. And the staff think I’m stealing, they don’t know what I’m doing, they don’t understand what I’m doing.
They don’t understand you.
And they think that I’m crazy ‘cause of what I’m doing. So they talk about me in the staff room and think it’s funny.
That’s me. It’s, it’s, there’s, there’s two sides. You know, there’s a nice side, intellectual side or, what’s it, threatening side. And then there’s the, the violent side, or potentially violent side. And it’s a constant battle between, between the two sides.
Do you feel like there’s anyone you can talk to about those things and that you get the support here for those things?
No, they haven’t got time. And they, they, they just dismiss you with, ‘oh, you know, don’t, try not to worry about it’.
Patients were often not asked for feedback at all if staff perceived that they would need to engage with delusions or hallucinations during the communication. The experience of care by these patients is therefore often unknown to the care providers. Our analysis suggests that, to gain feedback on the care experience of patients experiencing auditory and visual hallucinations, staff need to engage with these patients.
Supporting patients to understand their medication
Medication was an issue, in inpatient settings that distressed both patients and carers, but for different reasons. Patients reported wanting to understand their medication and why it was being administered; they reported not being able to access psychiatrists to talk about their medication. They also reported concerns about medications, particularly focused on side effects and not having the opportunities to communicate about these, which left them feeling isolated and distressed. Medication administered by force was also talked about as distressing:
The nurse comes and hands you medication. I look at her and say, ‘what am I taking this for?’. They say, ‘you asked for it’. I didn’t ask for it. And then they tell the doctor I’m asking for medication. I’m not asking for medication, they’re giving it me. Now they’re telling me the doctor said I’ve got to have it. So I’m . . . confused.
PTA09.ServiceUser10
Carers discussed incidents of when they felt that the person whom they were close to had been administered incorrect medication. Carers reported that they were not included in discussions about medications, which at times was counterproductive, as they had, in some cases, been supporting the patient for years and would have known about what had previously worked or not. The lack of carer involvement in care and treatment-planning was a pervasive theme, but, in relation to medication, carers became particularly distressed, as they felt that their voice was not being heard and that this was affecting the treatment and clinical outcomes of the patient:
They found out about the one medicine, his mood, goes high. Fluoxetine. But I understand they do give him sometimes, but which I’m not happy with that . . . they should read in the notes what is good for him and what’s not, but they still sometime they give him.
And have you been able to talk to anyone about that?
We complain every time.
Our analysis suggests that, for good patient experience, staff need to help patients understand the effects of medication, enable patients to ask questions about medication and its side effects, and listen to patients and carers when they offer feedback on medication.
Supporting patients to understand their care pathways and experience of the Mental Health Act33
Patients reported that they did not understand the sectioning process or their rights and, in some instances, they did not understand how or why they had been detained. This meant that they found it difficult to make sense of their care journey and, consequently, to feed back about their experiences. Feelings of being confused, disempowered and dehumanised led to mistrust and led to them not engaging honestly with ward staff about their care, treatment or experience:
You mentioned that maybe 6 days in you would have liked someone to ask you how you’re feeling . . . what you would have liked.
The hardest thing was I didn’t know what was happening, I didn’t know whether I was . . . I still to this day don’t know if I was sectioned or . . . I know the police got involved but I won’t tell you about that, ‘cause it’s not irrelevant, it’s not relevant to this. But I think the way that you’re treated is awful . . . you have to have really caring staff . . . and understanding staff to work with mental health . . . I just think the whole lack of respect and understanding of each individual’s needs is zero.
Our analysis suggests that staff need to support patients to understand their care and treatment, in particular decisions that have been made about their care without their consent.
Discussion
Work package 3 was informed by and contributes to the overarching realist research design (see Chapter 2). It also forms a self-contained realist evaluation of the collection, analysis and use of adult mental health inpatient experience data to inform and improve the quality of services in six case sites. The thematic and CMO analysis was used to refine the programme theories of the overall study (see Chapter 7).
In undertaking this realist evaluation, we aimed to produce a middle-range theory that can be deployed by health-care provider organisations without further interpretation. We completed this in WP4. Staying with a middle-range theory runs the risk of missing other broader issues. In the final section of the results in this chapter, we identified the following issues: tackling racism in inpatient settings, supporting patients with auditory and visual hallucinations or delusions to communicate about their experiences of care, supporting patients to understand their medication, and supporting patients to understand their care pathways and experience of the Mental Health Act. 33
The analysis as a whole gives an indication of the complexity of providing care for adults with mental illness and collecting and responding to feedback on patients’ experiences of care. Our analysis demonstrates many of the interactions that contribute to this complexity. Each stage of CRAICh is itself complex and interacts with other stages. However, our analysis suggests very specific actions that can be taken that are likely to make a difference. With so many interactions, actions that are relevant to all stages of CRAICh and to all levels of the organisation need to be taken concurrently, at least to some degree, otherwise actions will meet resistance.
Our analysis has demonstrated that patients can give feedback on their experience however unwell they are, although giving honest feedback depends on there being a trusting relationship in place with a member of staff. A lack of resources resulting in overstretched ward teams can make it difficult for patients and staff to develop these trusting relationships. However, such relationships underpin both the treatment of the patient and the collection of patient experience feedback. Staff are listening for a patient’s account of both how they are in terms of their mental health and how they experience their care including experiences that might suggest areas in which improvements are needed in how their care is provided. The difficult task of discerning between these two aspects of the patient experience is the task of staff and not necessarily of the patient.
Carers witness poor care and find it hard to report, as they worry about the impact that this will have on the person they care for. Patients do not give honest feedback when they feel disempowered and when care is of poor quality. Staff are aware that they do not always get authentic feedback. This all makes it difficult to understand the meaning of informal feedback. However, it cannot be ignored. In our data, we identified issues similar to those in the Francis report:4 patients not being heard, patient experience feedback not being valued, a lack of effective action in response to negative feedback, an acceptance of poor standards and a failure to put the patient first. Informal patient experience feedback data need to be taken seriously but interpreted through triangulation with patient experience data from other sources and triangulation with other measures of quality of care.
Strengths and limitations of work package 3
We successfully recruited staff and patients across all sites. For staff, we recruited a range of relevant staff. For patients, we are unable to determine if certain types of patients who were well enough to participate were not invited to participate by recruiting staff. However, we interviewed patients and carers who had both positive and negative things to say about their experiences of care and of giving feedback and some who were willing to talk about sensitive issues such as racism.
Our realist evaluation included lamination to explicitly differentiate between actors in CMO configurations, to differentiate between different points in time and to differentiate between stages in the cycle of patient feedback and change. This has allowed us to manage, in one analysis, a large data set about a very complex process.
We have presented our CMO tables in Appendix 16 (see also Report Supplementary Material 5), along with lists of the data sources for each CMO configuration. Our results are as auditable as a more traditional thematic analysis.
Our evaluation focused on UK NHS adult mental health wards. The purpose of the research was to inform how patient experience feedback is collected, analysed and used in this setting. Our findings are likely to be transferable to settings that are somewhat similar, for example adult mental health wards in other UK NHS provider organisations. However, from our data, we are not able to suggest what determines the transferability of our data to settings beyond this.
Chapter 7 Work package 4: stakeholder conference
Introduction
The realist evaluation (WP3) led to the development of an understanding about what worked, for whom, in what circumstances and why in relation to the collection, analysis and use of patient experience data to improve the quality of care in adult mental health settings. Next, we wanted to know how this understanding could be applied in real-world NHS settings and what might prevent or support this. We undertook the following:
-
We developed what we termed the ‘rules’. These rules were based on our programme theories as developed through the project, including the results of the realist evaluation (WP3) (see the final column in tables in Appendix 17). The rules set out how to collect, analysis and use of patient experience data to improve the quality of care in adult mental health settings.
-
We organised a conference of key stakeholders to discuss the rules and to consider how the rules could be applied within a real-world patient experience feedback process.
-
We refined the rules (see Appendix 17).
The rules operate at the level of middle-range theory. They are developed from the details of specific contexts. They can be deployed in other, somewhat similar, contexts (e.g. other metal health inpatient wards) without further interpretation. They describe actions that, if taken, would form the basis of a good process for the collection, analysis and use of patient experience data to improve the quality of care in adult mental health settings. The rules are the output of the whole study process, rooted in the findings from the realist evaluation.
Aim and purpose of work package 4
The aim of WP4 was to present the findings of our project to stakeholders, including patients and carers, for discussion and, based on the discussion, to refine our project output, particularly the programme theories (see Appendix 17).
Methods
Development of the rules for presentation to the stakeholder conference
The rules were developed from the overarching programme theories and the thematic analysis and CMO configurations reported in WP3 that relate to the collection, analysis and use of patient experience data in adult inpatient settings. They were developed from our in-depth knowledge of the data and through research team discussion and discussion with the PPIT. Research team and PPIT experiences were not used as data; instead, the research team and PPIT worked to co-produce the rules from the primary data (see Appendix 17).
Stakeholder conference
Ethics considerations and consent
All participants who were invited to the conference consented to be in attendance and attended voluntarily. At the conference, all participants were asked if they would like to be formally recognised in the EURIPIDES report as having attended and contributed to WP4. All attendees verbally consented to having their job title recorded for publication in the EURIPIDES report (this list can be found in Appendix 18).
Recruitment of conference participants
The conference was specifically aimed at those who have a role to play in the patient experience cycle. Participation in the EURIPIDES conference was by (e-mail) invitation only. We invited the following:
-
everyone who was invited to participate in WP2
-
key members of staff from the six case sites
-
policy-makers
-
the PPIT.
Conference process
The conference was held on 15 March 2018 at Warwick University, UK. Conference participants were provided in advance with a summary of the results of the prior work of the study, including the systematic review, the national survey of the patient experience landscape for acute adult mental health services in England and the case study findings.
For each of the four stages [with quality improvement, implementation and change (ICh) combined into one stage] of the patient experience data cycle (CRAICh), two facilitated group discussions were run separately with different participants (9–12 participants per group). Participants were allocated to mixed groups including policy leads, NHS trust staff, service users and carers. Participants were assigned to each take part in up to two group exercises.
Four questions were asked in each group discussion:
-
How could the rule currently be applied in the inpatient context with which you are familiar?
-
Why apply it in that way?
-
What are the facilitators of and barriers to the application of the rule?
-
Who is in a position to take responsibility for the application of the rule?
Notes were taken by scribes on the group discussions. Notes from all of the groups were then collated by the research team and presented to the whole audience for final discussion in a plenary session.
During the stakeholder conference, the rules themselves were not explicitly up for debate, as they were derived from our prior work. However, if there was concern about a rule, we reviewed the rule in the light of the original data, refined our analysis and adapted the rule.
Results
The original rules
The rules presented to the stakeholder conference are presented in the final column of the EURIPIDES programme theory development table (see Appendix 17). Prior to the conference, the PPIT raised a concern about rule C2; the wording of this rule was as follows: ‘Make sure you collect positive patient experience feedback.’ They felt that it was important to highlight that all feedback (not just positive feedback) needed to be listened to. It was not the reasoning of the rule that they called into question, rather its phrasing. The rule was changed to the following: ‘Make sure you get both positive and negative patient experience feedback.’
The stakeholder conference
The conference was attended by 44 delegates from across England, including individuals with lived experience of acute inpatient care from our service user and carer reference group and survivor researchers, policy-makers, and both clinical (staff members from inpatient wards) and corporate (corporate patient experience roles) staff (see Appendix 18).
In the EURIPIDES programme theory development table (see Appendix 17), we present the details of the discussion group data and how these were used to refine and add to the original rules.
The view was expressed during several group discussions that more emphasis was needed on the importance of seeing change that resulted from giving feedback. In the original rules, this formed part of the evidence for several rules. We re-interrogated the WP3 data and developed rule C5 (see Rule C5: seeing changes based on both positive and negative feedback is important for patients, carers and staff). The discussion groups highlighted the absence of carers from the rules. Again we re-interrogated the WP3 data and developed a further rule, C6 (see Rule C6: trusts must engage carers proactively in the inpatient care of the person they care for and staff must communicate to obtain feedback from carers). The final rules are given in the final column of the EURIPIDES programme theory development table (see Appendix 17) and are presented in the following section.
The discussion groups highlighted the need for patient experience processes to be aligned with strategic priorities set by NHS England, to be formally recognised in the inspection criteria of the CQC and to be aligned with explicit priorities for commissioning bodies. The need for a more consistent approach to implementing thoughtful change in response to high-quality feedback and communicating those changes was emphasised, rather than a reactive underfunded superficial approach to quality improvement. There was recognition that change costs money. Discussion groups suggested piloting what was termed ‘engaged ward’ programmes, in which the CRAICh rules are implemented using existing resources from which further quality improvement can be built. Any such initiative needs to take into consideration staff retention, staff well-being and compassion fatigue.
The final rules: the programme theory – how to collect, analyse and use patient experience data to improve the quality of care in adult inpatient mental health settings
Theme 1: collecting and giving
Rule C1: always ask about a patient’s experience
Evidence: patients can tell us about their experiences no matter how unwell they are. However, if feeling very unwell, they can only share experiences such as ‘I’ve had a bad/good day’.
Rule C2: make sure you get both positive and negative patient experience feedback
Evidence: patients being asked for feedback, feeling listened to and heard, and knowing that feedback is being used are essential to improving the quality of services. Feedback from patients is often both negative and positive. Taking note of positives helps strengthen good practice and avoid bad practice. Not understanding positive feedback is a lost opportunity and is disempowering for patients.
Rule C3: ask for feedback in varied ways at different times
Evidence: different sorts of feedback need to be collected at different intervals during admission. During admission (particularly involuntary admission), patients can give feedback on their individual experiences of care, despite being unwell. To provide meaningful feedback about the ward environment, patients need to have reached a degree of recovery, which varies by person, but typically occurs part-way through their admission. Patients want to give honest feedback about the staff, the culture and their overall experience only at the end of their admission, as they are being discharged. Many patients fear that giving feedback will influence their clinical care and, therefore, may be anxious about doing so prior to discharge. People do not always wish to be contacted to give feedback once they have left inpatient services.
Rule C4: personalised care is valued and the same applies to obtaining feedback
Evidence: patients often report feeling dehumanised by the process of admission. They wish to be treated as individuals. Feedback opportunities need to be personalised. Patients need to feel valued and listened to. Relationships with staff are important. Patients report that they are more likely to give honest feedback to people who they perceive as kind and caring. Staff need to have time to get to know and communicate with patients about their experience.
Rule C5: seeing changes based on both positive and negative feedback is important for patients, carers and staff
Evidence: both positive and negative patient experience feedback need to be obtained. Patients being asked for feedback and feeling listened to and heard needs to be accompanied by feedback-driven change. Patients, carers and staff knowing that feedback is being used of is essential to improving the quality of services.
Rule C6: trusts must engage carers proactively in the inpatient care of the person they care for and staff must communicate to obtain feedback from carers
Evidence: carers’ feedback can be a fruitful way of gathering intelligence about the quality of the care being provided. Carers will give honest feedback only if they trust that it will not have an impact on the clinical care of the person they care for.
Theme 2: receiving and listening
Rule R1: staff need protected time to obtain feedback
Evidence: all ward staff should have protected time to spend with patients. Spending time with patients builds rapport and trust to enable more honest feedback. Staff want to do this but often report being too busy. People give authentic feedback only if they feel comfortable and confident to do so. Staff availability, both emotionally and physically, is integral to getting honest feedback.
Rule R2: all staff have a role in receiving, listening to and responding to feedback
Evidence: the collection of patient experience information can be seen as ‘not my role’. There are particular situations in which this is more likely, for example in the case of agency staff. Those who are in lower-band roles are often the ones who receive the most informal patient feedback and distribute formal patient experience tools. They are the least likely to receive the results of feedback or to be involved in acting on it. When patient experience information is escalated to management without local ownership of the feedback or its resolution, ward staff can feel disengaged from the process.
Rule R3: staff should be supported to receive feedback
Evidence: the inpatient mental health setting is emotive and challenging. Staff need to be supervised and well supported so that they have the capacity to listen to and receive patients’ experiences. Supportive cultures motivate and retain staff and there is greater engagement in patient experience work. Staff are less likely to seek honest feedback if they perceive that they are operating in a blame culture or that they cannot do anything to support those who are offering feedback. Staff need to be encouraged to receive positive and negative feedback. Priority is given to negative feedback, so staff are often unable to see the value of positive feedback. Complaints and compliments need to be viewed as equally valuable sources of data.
Rule R4: staff need to be able to respond to the feedback that is received
Evidence: there must be clear guidelines for the use of all types of patient experience feedback. Staff should know what to do with informal and formal feedback, as well as where to report it. Staff become demotivated when they receive feedback but have no clear pathway to escalate concerns.
Theme 3: analysis, acting and response
Rule A1: appraisal should include both qualitative and quantitative evidence
Evidence: the FFT alone is insufficient as patient experience data, but it can provide a useful benchmark. The evaluation of patient experience data should consider both qualitative and quantitative information to provide the granular detail that helps to identify why something is happening, not just that it is happening. Analysis should triangulate all types of patient experience data for a richer picture (e.g. the FFT, complaints, compliments and patient safety data).
Rule A2: informal patient experience feedback must be responded to and used
Evidence: although formal measures are useful and provide metrics, listening and responding to patients when they informally give feedback about their experience is not just about good-quality care provision, it can be used to improve the quality of care. The informal patient experience data held locally on wards should be harnessed at a local level to drive local quality improvement. If patient experience teams exist, they need to support and understand how the informal feedback processes are working. Changes that are made as a result of this informal feedback should be captured in the corporate structure to inform wider quality improvement initiatives in trusts.
Rule A3: both positive and negative feedback should be acted on
Evidence: positive and negative feedback are both valuable and should be included in data collection, analysis and action-planning. Organisations (e.g. trusts) usually respond only to complaints and negative feedback, so staff are not conditioned to respond to positive feedback.
Rule A4: gathering, analysis and using patient feedback is everyone’s business
Evidence: there needs to be buy-in at every level. Devolving the responsibility to the ward level for acting on and responding to patient experience data ensures that ward staff feel engaged in the whole process. Ward staff can make changes if given the permission to do so. Staff can act on patient experience data only if it is made available and is shared. Currently, data are held centrally in many organisations. Often, feedback does not reach ward staff or patients. The weakest area of work is the analysis of patient experience data. Certain types of feedback (e.g. patient stories presented to boards or serious complaints) may be privileged. Although such feedback provides valuable learning opportunities, focusing only on this feedback risks driving change only in response to individual negative feedback.
Theme 4: implementation, change and quality improvement
Rule ICh1: organisations must have a means of contextualising patient experience and feedback alongside other information gathered
Evidence: patient experience data are most effective when not held in a silo and when they are triangulated with other data, such as compliments and complaints and patient safety data. This triangulation enables patterns to be seen that can help change services to improve quality both at the corporate and at the ward levels. The triangulation of data needs to happen at all levels, not just at the corporate level.
Rule ICh2: service improvement should not be led by negative feedback alone
Evidence: staff believe that complaints are the most common driver for change. There is a pervasive sense that quality improvement is sometimes driven by negative feedback or ‘external’ forces. How data gets prioritised within organisations varies. Examples commonly given are of quality improvement initiatives started as a response to serious incidents or complaints, to CQC or external inspection or to deterioration and noticing things are wrong. Although these are all valid reasons, quality improvement cannot solely be led by negative feedback, as this risks losing the knowledge about what works well and is demotivating for staff and disempowering for patients.
Rule ICh3: staff need to be engaged in quality improvement
Evidence: it is unclear to staff how patient experience feedback links to quality improvement work. Understanding where the data came from that inform quality improvement is crucial to engaging staff in that work. Change happens and is sustained when staff and wards take responsibility and ownership for the change. Individual wards cannot lead cultural systemic change, as this needs central and local alignment. If staff are not engaged, there is a risk that, instead of quality improvement, tokenistic or short-term changes are made (e.g. to the ward environment). These changes are usually not sustained in the face of other pressures.
Rule ICh4: quality improvement requires leadership
Evidence: organisations tend to respond more rapidly to feedback about environmental issues. Changes to the environment are implemented at the ward level. Cultural change is more difficult and requires corporate leadership.
Discussion
We have presented our final programme theory developed over WPs 1–4 of this study. The programme theory is expressed as rules on how to collect, analyse and use patient experience data to improve the quality of care in adult mental health settings. These rules can be operationalised into adult mental health wards of UK NHS care providers. The rules are similar to the realities of care provision, so staff are likely to recognise the relevance of these rules to their own care context. This does not mean that putting them into practice is easy. Staff face a complex and sometimes difficult task in collecting, analysing and using patient experience data. They do this in a challenging setting with often very ill patients and a lack of resources. Our stakeholders suggest that the process of change be started by applying the rules in one ward, in what they termed an ‘engaged ward’, with support from the organisation’s management at all levels.
External drivers such as strategic priorities set by NHS England, inspection criteria of the CQC and commissioners’ priorities are a strong influence on care providers. To enable providers to pay attention to the rules that we propose here, these external drivers and the rules need to be aligned. To gain traction on problems of poor quality of care, multiple sources of data (of which patient experience data are only one) need to inform change. A consistency of the approach and sufficient resources are needed to allow complex processes to change.
Strengths and limitations of work package 4
The process by which the EURIPIDES programme theories were developed and refined throughout WPs 1–4 is available in Appendix 17. We have made our process as transparent as possible. The programme theories – expressed as rules – are limited to CRAICh, following the original purpose of the study. Other issues identified in WP3 that were of relevance to quality improvement, although important, were not included in our final rules.
All stakeholders were well represented at the stakeholder conference. Different types of stakeholders engaged with each other in the facilitated discussion groups. Stakeholders were respectful of the rules presented to them, given the number of data and the detailed analysis that underpinned them. This allowed the stakeholders to focus on the use of these rules.
Chapter 8 Work package 5: the costs and consequences of patient experience data collection in practice
This chapter outlines the health economic implications of the collection, processing and analysis of patient experience data.
Background
NHS trusts are required to collect experience data from patients. 142 Currently, there is little understanding of what data are most important, what processes are in place to collect them and whether such data make any difference to the quality of patient experience. There are no widely established principles of data collection and analysis, and there is variability in how such data are used to inform and improve services. 8 A wide range of strategies exists for collecting and implementing patient experience data. Collecting and feeding back data requires resources that could be spent elsewhere within the NHS. We refer to this as ‘opportunity cost’. 143 Therefore, given limited budgets, there is an opportunity cost in capturing and using these data. The role of the health economics component of this study was to examine the resource use and costs associated with different models of experience data collection and feedback, and the benefits that resulted from acting on these data.
Purpose of the health economic component of the EURIPIDES study
Our aims were to (1) examine the resources used in the patient experience data collection and use processes, (2) estimate the incremental costs associated with adopting improved methods for collecting and using patient experience data and (3) consider how the cost-effectiveness of enhanced patient experience processes might be assessed. This involved estimating the costs and benefits associated with different approaches to collecting and using patient experience data.
Design and analysis
As mentioned previously, six sites were recruited to the study. Details of site selection and staff recruitment can be found in Chapter 5. As well as ensuring variation in approaches to and the extent of completeness of the patient experience data cycle, sites were chosen to ensure diversity in size, location, geographical spread, urbanicity and ethnic diversity. Data collection methods are described in Chapter 6. Data were collected using in-depth interviews with ward staff, PELs, trust managers and service users. Consequently, the data collected are cross-sectional in nature and thus preclude the possibility of capturing evidence on the impacts of service change (in terms of both cost and benefits) associated with different models of patient experience processes. The overall approach, therefore, was to identify and cost patient experience processes and produce two packages of patient experience activities, each representing a different level of implementation: low intensity and high intensity. Logic models were then used to examine and extrapolate the implications of different implementations of patient experience processes on cost-effectiveness.
Methods for identifying and attributing cost
A bottom-up costing approach144 was used to examine resource use at each of the case study sites. The analysis comprised six main steps:
-
identify and specify the activities related to patient experience data collection, analysis and feedback
-
identify and quantify resource inputs for activities
-
define ‘low-intensity’ and ‘high-intensity’ models for patient experience processes
-
identify unit costs for resource use
-
combine unit costs and resource unit data to calculate costs for patient experience activities
-
create conceptual models of cost-effectiveness.
Step 1: identifying and specifying patient experience processes
To be able to cost patient experience activities, it was first necessary to identify what patient experience activities take place. Given that sites were selected for their differing approaches to collecting and using patient experience data, the activities representing patient experience data collection and analysis were expected to differ between sites.
The first stage of the microcosting exercise was, therefore, to map the patient experience activities at each site. The exact processes and activities involved in the patient experience data pathway for each site were identified via in-depth interviews with trust staff. Thus, the analysis of cost data relied on granular resource use data extracted from in-depth interviews at each site in relation to the key steps on the patient experience data pathway: data collection, data management, data analysis and presentation/dissemination. For each site, patient experience data processes were mapped to identify how data collection, analysis and use were broadly conducted at each site.
Step 2: identifying and quantifying all resource inputs
For each enumerated activity, resource inputs were identified and quantified using data from the in-depth interviews. Resources can be broadly separated into labour costs and capital costs. Labour refers to the time burden associated with any patient experience activities; for example, 1 hour spent collecting patient experience data. Capital refers to any equipment that is utilised; for example, this could be electronic gadgets for collecting data on the wards or the cost of the software used for analysing the data.
This bottom-up costing approach aimed to identify every item of resource use associated with the patient experience pathway. Whenever patient experience activities were discussed, the interviewer was tasked with eliciting ‘who’ was involved, ‘how long’ they spent conducting such activities, ‘how often’ they occurred and ‘what’ equipment was used. Owing to the number of staff operating at each site, it was not feasible to interview every member of staff; consequently, exemplars were used. Exemplars at each site were to be used to estimate and extrapolate across each ward. Labour resource inputs were quantified in terms of time (hours), whereas capital resources were recorded in their natural units.
Step 3: defining ‘low-intensity’ and ‘high-intensity’ patient experience packages
A goal of the previous WPs was to identify what components of the patient experience data cycle work well and where the shortcomings in patient experience processes lie.
Two simplified, hypothetical packages (or vignettes) of patient experience data collection and use were created, one representing ‘low-intensity’ and the other representing ‘high-intensity’ processes. Low intensity can be thought of as the minimum requirements for collecting and using inpatient mental health-care patient experience feedback within existing regulatory and policy structures. High-intensity processes, on the other hand, comprised activities that were found at sites with more extensive and embedded patient experience data collection and use (and which were rated as such in WP2).
Patient experience activities were enumerated and included in (i.e. allocated to) either the low-intensity or the high-intensity package (or, in some cases, both). These two packages were then used to examine the burden related to low-intensity and high-intensity patient experience data processes. This allowed us to assess the expected cost of adopting best practice in the collection and use of patient experience data in inpatient settings (as identified in WP3 and WP4) across all mental health trusts in England.
Step 4: identifying unit costs for all inputs
Unit costs refer to the cost of one unit of input. For labour, this could be the salary costs (including pensions, overheads and other on-costs) per hour, whereas for software it may be the ongoing cost of a licence. For inputs identified in step 2, a unit cost was attached. For labour, the costs of the Personal Social Services Research Unit145 were used as the primary source for costing. For capital costs, methods were dependent on what capital was being used. When appropriate, for example in the case of software for analysing patient experience data, the key PEL was asked how much was spent on the specified software licences.
Step 5: combining resource input and unit cost data
To calculate the cost for each individual activity in the two packages, we combined resource input data (identified in step 3) with the unit cost data (identified in step 4), that is we multiplied resource use data by unit cost data. This provided us with activity-specific costing for the packages. Thus, we calculated a cost associated with each activity identified in step 1. We then allocated these activities to the ‘low-intensity’ and/or ‘high-intensity’ packages to examine the resource use associated with different levels of implementation of patient experience processes.
Step 6: creating conceptual models of cost-effectiveness
One of our aims was to assess the benefits resulting from the implementation of best practice in patient experience processes across all mental health trusts in England. Acute mental health inpatient stays are expensive, typically costing £404 per bed-day. 145 Consequently, if patient experience data and analysis can lead to change that improves patient experience and earlier discharge, or a lower risk of relapse and re-admission, there is potential for cost savings. Likewise, if patient experience is improved, then there are benefits in terms of improved health-related quality of life and broader well-being.
However, as reported in Chapter 6, a theme across all sites was that data analysis was often limited, thus restricting the potential for benefits arising from data collection. Consequently, to examine the cost-effectiveness implications of collecting and using patient experience data and adopting best practice, three logic models were created. Two logic models representing low- and high-intensity patient experience data processes (as identified in WP3) were developed. A third model was created to illustrate how implementing patient experience feedback could improve cost-effectiveness in the delivery of inpatient care, using the example of alleviating boredom on the ward.
Modelling the change from low- to high-intensity patient experience implementation
The first package represents ‘low-intensity’ patient experience data collection and use and reflects current practice in a constrained form. The activities included in the low-intensity package of patient experience data include:
-
the FFT on discharge, which includes the burden to nurses of distributing it to patients on discharge – the results from the FFT are used by the patient experience staff to aggregate site-level data for routine reporting
-
posters, ‘You said, We did’ boards and ‘safe trees’
-
general patient experience activities conducted by minimal staff – tasks include processing the FFT, the creation of posters and reporting to the board (including ‘patient stories’)
-
one-to-one patient contact for 15 minutes per day, considered to be typical in inpatient care packages
-
weekly community meetings on inpatient wards, which occurred routinely across all but one case study site.
The second package represents ‘high-intensity’ patient experience data processes and incorporates the best aspects of patient experience processes seen at study sites. The additional elements of the high-intensity package can be seen in column five of Table 15. The high-intensity package was developed through an iterative process whereby patient experience activities at each site were enumerated and agreed in discussion with the research associates (Una Foye and Aimee Cairns) and WP3 field notes. This was further informed by WP3 findings.
For example, we found that, although data were being collected, in many sites data were not being analysed fully. Often, when data were analysed, this was used for benchmarking. The high-intensity model therefore incorporated analysis of data through improved patient experience data management systems and more time allocated to data analysis. To enable this, in addition to usual patient notes software, the high-intensity package was costed on the basis of patient experience software and appropriate hardware and licences,146 as used by one of the most highly rated sites for patient experience in this study. This software facilitated the collection of high-quality data, which could then easily be extracted and analysed by the PEL and was capable of creating reports that include ‘free-text’ comments, which are often wasted in the current patient experience climate. Reports were also available at the ward level. The high-intensity package was also costed on the basis of sufficient staff time for patient experience analysis, to allow for meaningful analysis and triangulation of data.
In addition, as used at one of the sites, the high-intensity package allowed for a weekly drop-in session for patients and carers to feed back on their experiences on the wards to staff. Weekly drop-in surgeries allowed minor issues to be discussed and fed back to staff. This allowed for quick resolution of smaller local-level concerns and provided a conduit for escalation to the PALS for more serious issues. This required 1 hour per week per ward of patient experience staff time.
Almost all sites had some sort of display for patient experience feedback (e.g. ‘You said, We did’ boards or posters). These were frequently suboptimally implemented (e.g. placed in inaccessible locations or not updated) and served little use. The high-intensity package model costs included time for patient experience staff to maintain and update these on a regular basis.
A key finding in earlier WPs related to the role that informal patient experience data can play. Nurses play a key role in capturing patient experience data in an informal manner. However, wards are often understaffed and resources are limited, thus reducing the capabilities of nurses to make use of informal feedback. As a result, the high-intensity package includes additional staffing costs to capture informal feedback, thus attributing a further 15 minutes per patient per day to seek out feedback, by assistant psychologists or those on a similar level. Importantly, this gives staff time to upload notes to patient records and escalate issues when necessary. It is important to note that this is in addition to the 15 minutes of one-to-one time included in the ‘low-intensity’ package.
Community meetings were one aspect of informal patient experience that were conducted across almost every site. The community meetings in the ‘high-intensity’ package remain unchanged from those in the ‘low-intensity’ package.
Using WP3 interview data, we combined resource use and cost data to examine the cost and resource burden associated with each package and to identify key cost drivers. The two packages were based on the assumptions that each trust patient experience team was responsible for 20 wards and that there were an average of 18 patients per wards with 11.3 discharges per month (in line with the sites in this study). Results are presented on a per-ward basis to facilitate site-specific interpretation.
Costing patient experience activities
As can be seen in Tables 14 and 15, for both intensity packages, the greatest costs were associated with the informal data collection (> 90% of costs in both scenarios). That is, the opportunity cost for a band nurse to spend 15 minutes per patient per day (£6160.05 per ward per month) quickly surmounts the formal cost of dedicated patient experience staff (£466.97 per ward per month) in the low-intensity scenario. Even the cost of one weekly community meeting per ward (£682.20 per month) surpasses the formal costs in the low-intensity setting. Thus, for the low-intensity package, which consists of a PEL with administrative support, the burden of the formal patient experience staff is low relative to informal costs. There were many instances in which the data were not consistently granular enough to allocate specific time to certain activities. This was particularly the case for smaller activities that the patient experience team members were responsible for (e.g. updating ‘You said, We did’ boards). Consequently, for these activities, the time associated with them is included in the larger ‘patient experience team activities’ time cost.
| Low intensity (typical activities currently conducted) | Resource use per ward | Cost (£) per ward per month (includes on-costs) | Assumptions |
|---|---|---|---|
| Formal: FFT | |||
| Distributed by band-6 nurses (5–10 minutes per patient at discharge) | 7.5 minutes per patient discharged per month | 63.56 |
11.3 discharges per month Band-6 nurse (£45/hour) |
| Informs and is included in reports to the board | Results included in routine reporting by the patient experience team | Unquantifiable: included in ‘patient experience team activities’ | N/A |
| ‘You said, We did’ boards, posters and safe trees | |||
| Updated by patient experience team | Ongoing task as part of the patient experience team role (see two rows below) | Ongoing task as part of the patient experience team role (see two rows below) | N/A |
| Patient experience team activities – monitor notes, conduct analyses at directorate level and report | |||
| Minimal staffing to meet bare requirements | Band-6 full-time PEL | 299.81 |
|
| Band-4 part-time support | 103.59 | ||
| Total formal costs (£) | £466.97 per ward per month | ||
| One-to-one informal feedback: 15 minutes per patient per day | |||
| Conducted by staff nurse | 15 minutes per patient per day | 6160.05 | Band-6 nurse (£45/hour): 18 patients per ward |
| Community meetings | |||
| Conducted once per week per ward |
Assistant psychologist/occupational therapist 4.25 hours/week (band 4) Nurse 0.5 hours/week (band 5) Health-care assistant 0.5 hours/week (band 2) |
682.20 | Community meeting details taken from one site |
| Total informal costs (£) | 6842.25 per ward per month | ||
| Total cost (£) | 7309.21 per ward per month | ||
| High intensity (activities needed for change) | Resource use per ward | Cost (£) per month per ward (includes on-costs) | Enhancement over ‘low intensity’ | Assumptions (unit costs for time taken from PSSRU 2017143) |
|---|---|---|---|---|
| Advanced data package (in this case, the patient experience software package including FFT data collection software and a ward iPad (Apple Inc., Cupertino, CA, USA) to support data collection) | ||||
| Conducted by external company and used by patient experience team | £20,000 licence (per year) | 83.33 | Patient experience software facilitates the extraction and analysis of detailed ward-level data for the patient experience team with increased granularity. The results can then be fed back to specific wards | Used across 20 wards |
| Equipment | ||||
| iPads for collecting patient experience data | One per ward | 8.31 | Technology is used to reduce paperwork and improve the accuracy of data | 3-year useful life |
| Patient and carer drop in session for minor feedback/issues/suggestions | ||||
| 1 hour per week per ward (band-6 patient experience team) | 1 hour per week per adult mental health ward | 195.54a | Additional service | Band-6 patient experience team member (£45/hour) |
| ‘You said, We did’ boards, posters and safe trees | ||||
| Updated by patient experience team members | Ongoing task as part of the patient experience team role (see row below) | Ongoing task as part of the patient experience team role (see two rows below) | Meaningful implementation: regularly updated and should be placed on wards (an example of suboptimal implementation was a board placed in an airlock) | N/A |
| Patient experience team that oversees the above activities, monitors and analyses at the ward level, and reports to ward managers | ||||
| Patient experience team | One band 8 full-time staff | 433.06 | Extra patient experience team set aside to facilitate ward-level analysis and feedback | Band 8 (£62/hour) |
| Two band 6 full-time staff | 599.63 | Band 6 (£45/hour) | ||
| One band 4 part-time support | 103.59 | Band 4 (£31/hour) | ||
| Assumes that they are working across 20 wards | ||||
| Total formal costs (£) | 1227.92 | |||
| Community meetings | ||||
| Conducted once per week per ward |
|
682.20 | No change | Community meeting details taken from one site |
| One-to-one informal feedback: 15 minutes per patient per day | ||||
| Conducted by nurse (band 6) and notes uploaded to patient notes software | 15 minutes per patient per day | 6023.16 | No change | Band-6 nurse: 18 patients per ward |
| One-to-one informal feedback: 15 minutes per patient per day (time to upload and act on notes) | ||||
| Conducted by assistant psychologists/occupational therapists and notes uploaded to patient notes software | 15 minutes per patient per day | 4243.59 | Additional time to process, upload and escalate patient experience data | Band-4 staff: 18 patients per ward |
| Total informal costs | 11,085.84 | |||
| Total cost per ward per month | 12,313.76 | |||
The additional activities included in the high-intensity package resulted in a congruent increase in associated costs. Again, the informal costs dwarf those of formal costs, with an additional 15 minutes of face-to-face time per day per patient far surpassing the increase in costs associated with more dedicated patient experience staff, patient experience software, equipment and a weekly drop-in session. Even if the high-intensity formal staff time was increased by a factor of five, it would still be far less than the informal burden of patient experience care. In terms of formal care costs, the most significant cost is staff time, closely followed by the cost of new software.
Pathway to cost-effectiveness: implications of enhanced patient experience practices
As reported in earlier chapters, a common theme across sites was that there was very little analysis of patient experience data. Consequently, there were few benefits (in terms of meaningful service improvement) identified as arising from patient experience processes (see Chapter 6). Of the few benefits reported, most were local and environmental (e.g. the introduction of a safer storage system to stop patients’ belongings from getting lost).
Conceptual models were therefore constructed to consider possible causal pathways to cost-effectiveness. Figure 8 presents the current state of implementation of patient experience processes commonly seen across sites and described in the low-intensity package. In this instance, only minimal activities are taking place. However, there are still formal and informal costs associated with patient experience data processes. In terms of output, beyond those arising from benchmarking and reports to the CQC, owing to a lack of formal analysis, there is little evidence of meaningful change, with benefits typically being localised environmental change. Consequently, it is unlikely that patient experience data processes beyond mandatory reporting in this model are likely to represent a cost-effective use of resources. That is, there is no clear pathway to cost-effectiveness for non-mandatory patient experience activities when data are not analysed.
FIGURE 8.
Patient experience data collection and analysis: current implementation (low intensity).

Through this study, lessons have been learned about how patient experience processes could be enhanced to lead to meaningful change. To demonstrate how enhanced patient experience data processes could be a cost-effective use of resources, a conceptual model (Figure 9) was created based on best practice in patient experience data showing the causal pathway from increased activities to improved outcomes. This model highlights how, although an increase in activities leads to increased levels of inputs (costs), it also leads to increased outputs that can create meaningful outcomes. This includes reduced rates of violent incidents, improved quality of life and faster discharge, in addition to other perceived benefits such as improved staff morale, which could feed back into improved care. Ensuring cost-effectiveness is not simply a case of minimising costs, but also involves assessing whether or not the benefits are worth the costs. If the benefits are sufficient, there is scope for this to be a cost-effective use of resources. Thus, for patient experience processes to be cost-effective, it is necessary to implement processes sufficiently to facilitate meaningful change. The logic model also highlights the data requirements that would need to be captured to inform a formal cost-effectiveness evaluation.
FIGURE 9.
Patient experience data collection and analysis: pathway to cost-effectiveness analysis (high intensity).
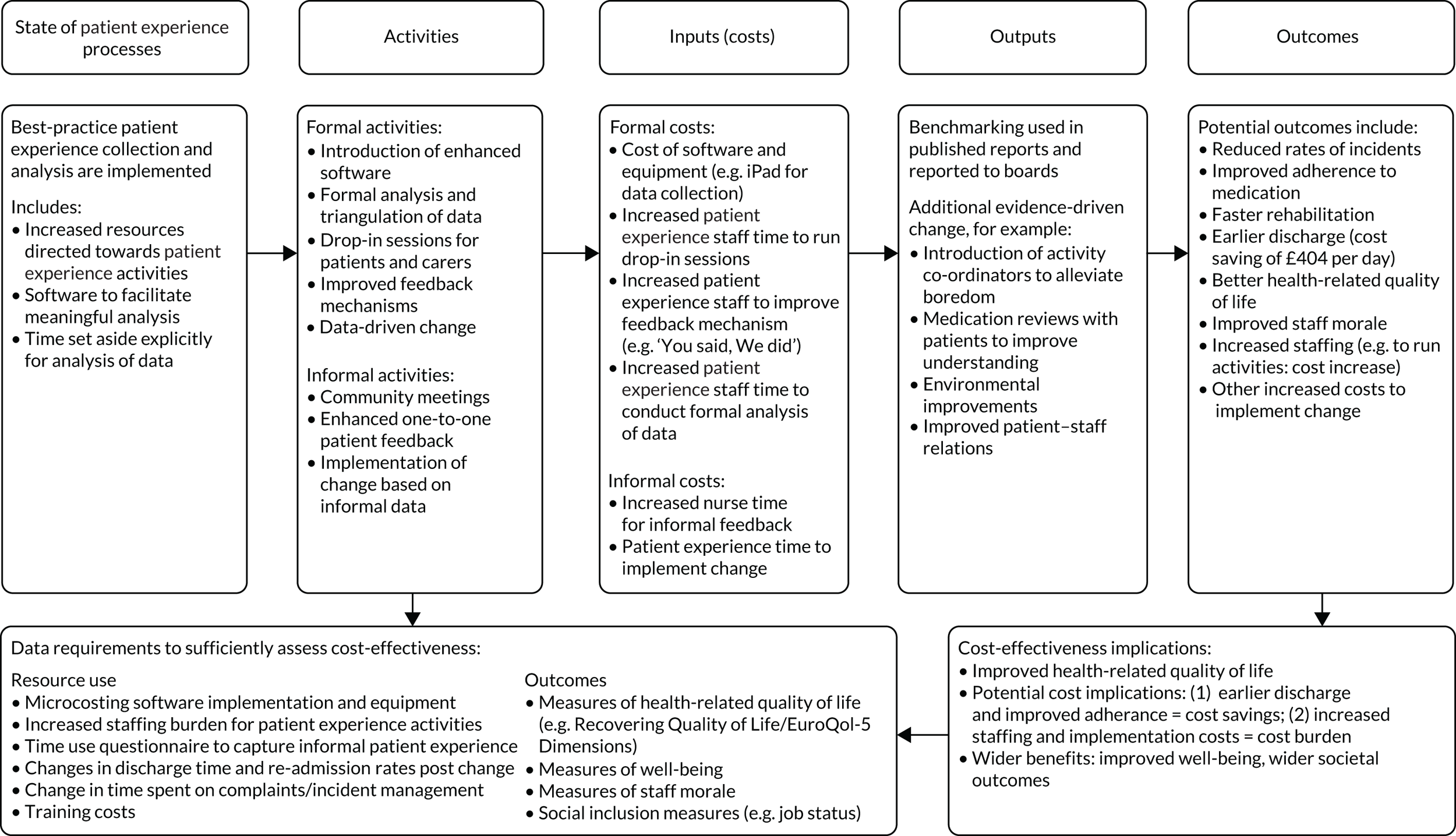
To highlight how such processes could potentially be cost-effective, a further conceptual model is presented using one of the few instances in which a clear link between patient experience data analysis led to meaningful change (see Figure 10). This example relates to the introduction of activities co-ordinators in response to the finding that there was an increase in incidents during the morning when nurses were occupied. It was hypothesised that this was due to the boredom of patients, as nursing staff are typically busy with other duties during the morning shift.
As demonstrated in the logic model in Figure 10, although there would be an increase in resources used, there is reason to believe that such a change could feasibly lead to benefits as follows. By supporting occupation in the mornings, activity co-ordinators reduce boredom; this then results in reduced rates of disturbance on wards. Although there are increased costs, there are likely to be tangible benefits that may, in turn, improve patients’ experiences. This could lead to improved quality of life, earlier discharge and wider on-ward benefits. We did not have sufficient data to establish if this would be cost-effective. Outlined in the model are the data requirements and tools that could be used in a prospective study to evaluate the cost-effectiveness of this intervention.
FIGURE 10.
Pathway to cost-effectiveness analysis: morning boredom – an illustrative example.
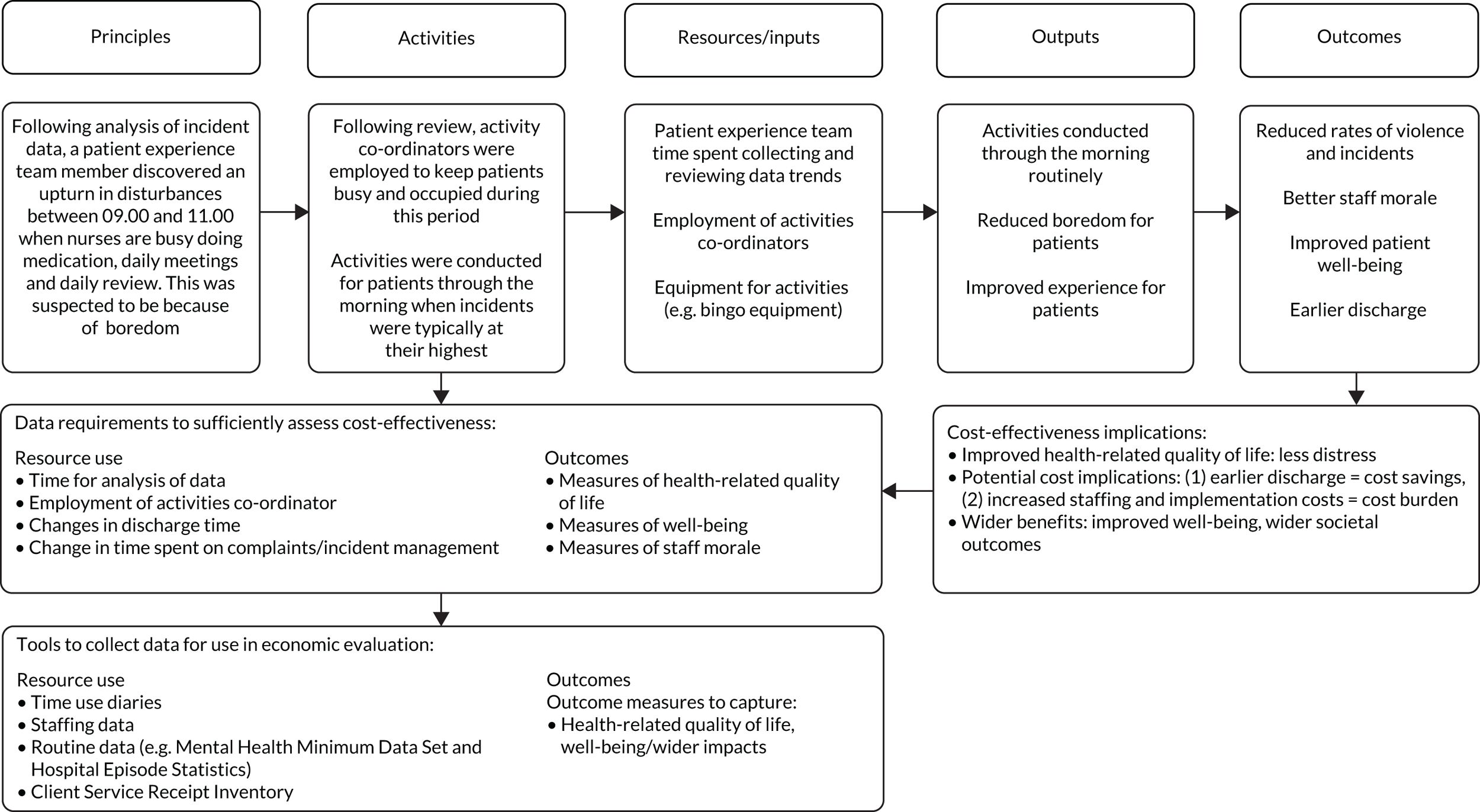
Discussion
In the context of limited resources and increasing constraints on health-care budgets,147 it important to consider the opportunity cost of patient experience activities. This chapter sought to examine the costs and benefits associated with patient experience data processes. Given data limitations (as further discussed below) a pragmatic approach was adopted. At each site, activities relating to patient experience processes were mapped, when possible. Given the lack of consistently granular information, two hypothetical patient experience activity packages (vignettes) were created using data from across sites to illustrate the costs associated with different levels of patient experience data collection and use.
Contextualising the health economic results: opportunity cost
Within current frameworks, the formal costs associated with patient experience data are relatively low. For example, in the low-intensity package, the estimated formal costs amounted to just £466.97 per ward per month. In the high-intensity setting, these increase to £1227.92 per ward per month. How these costs are perceived is subjective and related to the size of budgets that departments are operating on and potential economies of scale. With a bed-day costing the NHS approximately £404 per day, the formal patient experience costs in the high-intensity scenario equate to three bed-days per ward per month. Whether or not that cost can be justified can be determined only through a formal analysis of the benefits that such a use of money would bring.
Contextualising the health economic results: formal versus informal patient experience data
Formal costs were far outweighed by the costs associated with collecting informal patient experience data. Earlier chapters (Chapters 5 and 6) highlight the importance of informal patient experience to improve care. Given this, there is tension between the costs of informal patient experience data processes and their benefits.
The results from the two vignettes demonstrate that, when the opportunity cost of staff time is considered, informal patient experience costs can be substantial. If, as in the low-intensity scenario, these data are not used, the implication is that these data are not cost-effective and should be discontinued. However, there is a degree of nuance that needs to be considered in relation to defining informal patient experience data. Some of the costs presented in the vignettes relating to informal data experience processes can be very clearly defined as a patient experience mechanism, for example community meetings. These discrete and well-defined activities can be clearly tied to patient experience processes and quantified. The biggest cost driver in both vignettes was related to informal one-to-one patient experience time. However, activities that we classified as informal patient experience activity, for example 15 minutes of one-to-one contact time, could just as easily be classified as normal therapeutic care. This should be borne in mind when comparing the costs and benefits of informal patient experience data with those of formal processes.
Cost-effectiveness
As reported in Chapter 6, there was limited evidence of analysis of patient experience data across study sites. Trusts were not recording or measuring the benefits of patient experience data analysis or the implementation of change. As a result, there was a dearth of evidence for use in a cost-effectiveness framework. Instead, conceptual models were created to show the mechanisms by which patient experience data could possibly be cost-effective. These models highlight the data and tools that would be required to evaluate cost-effectiveness in future trials of patient experience implementation. This includes the prospective measurement of resource use and patient-reported outcome measures alongside the implementation of patient experience processes. Likewise, large national databases could be harnessed to examine whether or not the implementation of new patient experience policies improve patient outcomes over time.
Challenges in assessing costs and benefits
There were many issues that limited the scope of the economic analysis. These issues arose for the following reasons: (1) inconsistent data quality/granularity, (2) comparability issues (including between wards at the same site) and (3) ambiguity throughout in terms of the interpretation of ‘patient experience’ data.
Data issues
The work reported in this chapter was based on secondary data, collected across six qualitative case studies and whose primary aim was a realist evaluation of approaches to the collection and use of patient experience data. It was not possible, therefore, to determine statistically which aspects of formal data collection at each stage caused the greatest resource burden.
Patient experience teams are responsible for numerous tasks within the patient experience cycle. For example, they may be responsible for collecting and processing FFT data; for collecting, responding to and feeding back complaints data; and for writing reports and reporting to board meetings. In terms of the time dedicated to each of these tasks, the data were not granular enough to identify what proportion of time was spent on each of these tasks and, therefore, did not allow the measurement of which of these tasks created the greatest burden. Thus, we could not ascribe units of time for patient experience staff to individual activities at all sites. Instead, all formal activities could be expressed only as part of the patient experience/PALS team time.
There are several knock-on impacts of this. First, it means that we could not say with any certainty what stages of the patient experience process cause the greatest burden. This feeds into the inability to accurately assess cost drivers. Although we can make general statements about the cost of staff and certain informal activities, we cannot identify which activities create the largest burden and, thus, drive formal costs. This is compounded by the fact that patient experience staff typically did not distinguish between the time they spent working on patient experience activities on adult mental health wards and time spent working in the rest of the trust; patient experience staff often worked across the trust on multiple ward types but typically did not specify the time allocated to adult mental health wards.
Comparability issues and the need for vignettes
In terms of aggregation and comparisons across sites, there were limits to what could be concluded because of extensive heterogeneity. Even within typologies, sites often undertook different patient experience activities at the ward level. Likewise, given the heterogeneity between the six sites, it was not possible to extrapolate easily to other sites in England. Likewise, the distinction between the PALS and patient experience teams was often opaque, with some sites classing the PALS as part of the patient experience team (or vice versa), whereas others did not. This further hindered comparability, as it did not allow like-for-like comparisons. Given this, in addition to the aforementioned data granularity issues, illustrative vignettes to represent the frameworks of patient experience processes were created to examine cost drivers.
Defining patient experience data processes: issues with ‘informal’ data
We intended to assess the differences in cost between formal and informal patient experience data processes. Despite limitations, for formal data collection, it is possible to harness the time and resources used by the formal patient experience teams to calculate cost. However, costs related to informal patient experience processes should be interpreted with caution.
Information on informal processes relied on qualitative data provided through interviews. For certain informal activities, costing was relatively straight forward (e.g. community meetings), as the activity was discrete and well defined. For other informal activities, it was much more challenging and, in some cases, not possible. This largely relates to the nebulous nature of ‘patient experience’ and how people respond to questions relating to patient experience data. One-to-one patient interaction was an example. At one site, nurses were allocated a specific patient to check on through the day and nurses specified that they spent approximately 20 minutes doing this. At another site, however, there were no specifically allotted patients; given this, nurses considered asking patients how they were feeling to be a central part of their job. This hindered the utility of our data to address these issues.
The result was that explicit comparisons between the costs of formal and informal patient experience processes should be treated with caution. Although we can give some examples of the various informal patient experience activities, the true costs of these activities may vary depending on other aspects of ward practices. For example, if we were to consider nurses simply talking to patients as patient experience data collection, then it would be likely that patient experience data collection care costs would be vast; however, the opposite approach, whereby patient interaction is not patient experience work but simply ‘part of the job’, may lead to an underestimate of costs.
Defining patient experience processes: issues with interpretation of ‘patient experience data’
The lack of clarity surrounding ‘patient experience data activity’ and its somewhat nebulous nature caused further issues in the data collection process. Various informants were unable to quantify the time they spent on patient experience data. For example, a deputy director of nursing argued that their overarching goal is to improve patient experience and suggested, as a result, that 100% of their time is spent on patient experience activities. Although this may be the case from a theoretical standpoint, it does not, however, relate to the view of patient experience data in this project. In essence, they were confusing patient experience data processes with quality of care. That is, they were not spending all of their time collecting, processing, analysing and feeding back patient experience data. They were instead doing their job, which they consider to be all about improving patients’ experiences and outcomes of care.
Likewise, the lack of operational definition of patient experience data activity led to estimates that included components that were not necessarily related to formal patient experience data collection and analysis. For example, in the following quotation, the respondent conflates activities that are related to patient experience data (e.g. ‘feedback’) with those that are not (e.g. ‘incidents’) when estimating the time they spend on patient experience data processes:
. . . one way of estimating would be like me spending definitely one afternoon sitting where there’s a regular discussion about incidents, complaints, feedback, service development. And I think those things are quite closely, all them, it’s about patient experience. So I would say that is 4 hours in 40.
Other staff also struggled to articulate the amount of time spent on patient experience data, with many simply resorting to terms such as: ‘a lot’, ‘varies hugely’, ‘informally throughout the day’, ‘a massive part’, ‘hard to quantify – once per week’, ‘not much’, ‘every day’, ‘limited’ and ‘smallest amount of time’. These terms did not permit the costing of time spent on collecting, analysing and feeding back patient experience data. This was further hindered in instances in which it was not clear what type of patient experience work they were referring to.
For example, one nurse stated that they spend 50% of their time on patient experience activities, which, when extrapolated across all adult mental health nurses at the site, resulted in huge and unbelievable cost estimates (£223,750.80 per month across 10 adult mental health wards) for patient experience activities. We have tried to provide realistic and pragmatic estimates of costs, with the above caveats in mind.
Quantifying benefits
We did not aim to undertake a formal cost-effectiveness analysis. Instead, data were used to conceptualise how patient experience data might theoretically be cost-effective.
Economic evaluation has two components: costs and benefits. This study was not designed to collect such data in a way that would be amenable to economic evaluation. On the benefits side, there were few quantifiable benefits. More explicit benefits, for example concerning how a patient experience policy change might lead to increased discharge rates, would have provided a quantifiable benefit. The majority of the benefits, however, were diffuse and environmental (e.g. improved food or locker facilities). It is challenging to model such intangible benefits and, thus, the benefits side of the cost-effectiveness equation was limited. Consequently, we chose to develop theoretical logic models, informed by interview data, to explore how best practice in the collection and use of patient experience data might lead to cost-effective service improvements. These models highlighted the data that would be required to evaluate cost-effectiveness in future.
It is important to note that, although few benefits across sites were reported, there was no evidence to indicate what would happen in the absence of (even low-intensity) formal patient experience processes. That is, although there were few perceived benefits, we do not know what would have happened had there been no patient experience work at all.
Lessons for future health economic studies on patient experience processes
The present study was designed for the primary purpose of identifying and understanding best practice in the collection and use of patient experience data, using a realist approach. Given this, the data collected were not particularly well suited to traditional health economic analyses. We therefore designed the economic WP to reflect this and to develop more conceptual models of potential cost-effectiveness, including modelling key parameters and potential pathways to cost-effectiveness.
Formal evaluation of cost-effectiveness in any future study (e.g. of interventions to disseminate the present study findings) will require a different design. Patient experience data activities will need to be operationalised and defined, and distinguished from (broader) activities designed to enhance experiences of care. Approaches to capturing the former activities (in both nature and duration) will need to be developed and tested, for instance through resource use diaries or time use surveys. 148 This would involve, for each site, giving an exemplar for each role a resource use diary to complete daily. This would seek to get participants to allocate the time they spent each day on various tasks including patient experience activities. This, however, could be very burdensome on the exemplar and alternative strategies could be employed, for example having a researcher shadow exemplars and complete these tasks on behalf of the patient experience staff.
To fully appraise the impact of new patient experience procedures, a prospective trial design could be implemented to rigorously assess not only the costs of patient experience data processes, but also the benefits that this type of systems change could bring.
Chapter 9 Discussion, integrated findings and conclusions
We set out to describe the ways in which feedback from people who receive inpatient mental health care, and those who care for and support them, in NHS settings in England may be most effectively collected and used to improve the quality of those services. We adopted a realist research design across five WPs for developing a theoretically and evidence-informed set of recommendations.
Our results are intended to be of direct relevance and utility to those who commission and deliver, as well as those who use, inpatient mental health services. We structured the study, and this report, around the ‘patient experience data journey’, from data collection (both the giving and the receiving of feedback) to data analysis and service improvement (including changes visible to the givers and collectors of feedback). In undertaking a realist evaluation, we developed and refined programme theories that are concerned with the critical processes and mechanisms at each stage of the pathway from data collection to service improvement.
This report begins with a detailed examination of the most salient inpatient experiences and hence the optimal data content (WP1), by means of a systematic review of studies that explored the experiences of people who have used inpatient mental health services. As well as identifying the key themes that emerged from the data, we identified the mechanisms by which particular experiences were linked to key outcomes. We also identified the circumstances under which positive and negative experiences were more likely to occur. The results from WP1 informed our initial programme theories.
This was followed by the first-ever survey (using individual telephone interviews) of patient experience leads in NHS mental health trusts (WP2). The data that emerged from these in-depth interviews enabled us not only to create a sampling frame for later studies, but also to understand the current state of patient experience work in NHS mental health trusts and the variation that exists between services. We were also able to further develop our programme theories about the circumstances under which the cycle of patient feedback, from collection to visible service improvement, was most likely to be completed.
The most complex and important part of this research was WP3. Through in-depth interviews with patients, carers and staff at six purposively chosen, contrasting sites (trusts), we were able to examine the processes and current practice at each stage of the patient experience data cycle. This provided rich data through which to understand when, where and under what conditions salient, meaningful feedback can be elicited from patients and translated into service improvements. These data generated more than 150 CMO configurations, namely the building blocks by which we understand the way in which different processes operate, or are activated, in different settings.
We summarised these findings and sought confirmation and clarification of our central programme theories in a consensus conference, attended by 44 participants (WP4). We framed these central programme theories as a series of 18 ‘rules’ about the conditions that need to be met for the effective transmission and translation of patient experience feedback into tangible service improvements. Finally, we undertook exploratory health economic modelling (WP5) to reflect on the relative costs and potential benefits of applying the rules agreed in WP4 to the collection, analysis and use of patient experience data in real-world NHS settings.
Main findings
This section describes the final iteration of the programme theories and seeks to synthesise and summarise the key study findings across all five WPs.
Systematic review of inpatient experiences (work package 1)
The systematic review of the most salient aspects of the experiences in inpatient mental health settings (WP1) identified four themes: (1) the importance of high-quality relationships, (2) averting negative experiences of coercion, (3) healthy, safe and enabling physical environment and ward milieu and (4) authentic experiences of patient-centred care.
Survey of patient experience leads (work package 2)
In the survey of PELs (WP2), we found that patient experience work was universally regarded as a positive influence but was rarely embedded in the core business of mental health trusts. More worryingly, PEL posts were subject to high rates of turnover and many were insecurely funded and hence acutely vulnerable to cost improvement pressures. We found that most trusts collect patient experience data (albeit in varying ways and at different intervals across wards), but few analyse or use it; therefore, the feedback cycle is rarely completed. Consequently, we found few examples of service change that had occurred as a result of patient feedback and, when this did happen, it was more likely to take the form of environmental rather than cultural change. This was reflected in the overwhelming predominance of our data in WP3 that concerned the conditions necessary for patients to be able to give, and staff to elicit and receive, meaningful feedback. When we observed best practice, the staff saw the collection of patient experience feedback as integral to caring for the patient, prioritised spending time with patients (which is difficult when reporting demands are high so staff have to spend a lot of time in the office) and were able to discern from patients’ accounts of their experience what was due to illness and what related to the experience of the ward. When staff were over stretched, demoralised because they felt that they did not have the agency or resource to provide good-quality care, and frustrated at the lack of change that resulted from patient experience feedback, they stopped attempting to collect the feedback. This negative cycle was exacerbated by aggression on wards, which required investigation, and by patient complaints (both of which were more likely when quality of care was poor). Staff became fearful of engaging with patients about their experience and, in extreme cases, blamed patients for problems with care.
We found much less evidence of a nuance in approaches to analysing these data or indeed to using these data to bring about service improvements. This was in contrast to the importance that many senior staff placed on patient-centred care and improving the patient experience of care in their organisation.
Case studies (work package 3)
Our analysis of WP3 (case studies) data was undertaken in two stages. First, a thematic analysis was undertaken that spanned all four stages of the patient experience data cycle, for which we coined the acronym CRAICh (collecting and giving, receiving and listening, analysing, and quality improvement and change). In the second part of our analyses, we developed 154 CMO configurations to understand how, for whom, in what circumstances and why underlying generative mechanisms were activated. The generative mechanisms were reported using the CRAICh framework. The five themes identified in the first phase of analysis were wellness, the importance of feedback, relationships and communication, resources, and power.
The wellness theme revealed that patients who are acutely psychotic, or particularly unwell, can describe their experiences, and many such patients do wish to communicate these. However, many such patients feel that staff may discourage this, a view that has some basis in fact, particularly when staff feel that it may be countertherapeutic to encourage patients to discuss delusional beliefs or distressing, internally driven experiences. Consequently, patients may come to view certain topics as ‘off limits’ (i.e. implicitly and explicitly discouraged), which may, in turn, inhibit them from sharing their experiences of care as they approach discharge. We also found that power imbalances (highlighted in another of the five themes) shape patients’ willingness to share certain aspects of their experiences of care for fear that this might interfere with their care, leave or discharge plan. This means that there may be only a small window of opportunity to ask about certain types of care experience, at the point of discharge.
We found that, no matter how unwell a person was, they were able to say if they were having a good or bad experience of care. When they are feeling slightly better, they can offer more nuanced reflective feedback on the episode of care or the setting. Patients should be encouraged to speak freely and authentically (including about their delusions), by suitably skilled and trained staff, to support them in making sense of their experiences. If this is discouraged, it inhibits the development of trust and reduces patients’ ability and willingness to give meaningful feedback about their care and treatment.
Collecting meaningful feedback from patients takes time and emotional resources (another of the five themes), both of which were in short supply in a system that was evidently under pressure. There were identifiable impacts (i.e. the availability of staff to talk to patients about their inpatient experiences) of resource pressure in inpatient settings; however, the realist evaluation uncovered that, although resource pressure and the wider climate of austerity may exacerbate the problems of collecting authentic patient experience feedback, this alone did not determine the culture of the inpatient setting. Instead, it was a collection of activated mechanisms that generated an environment in which patients felt safe and supported, which, in turn, enabled them to trust staff in order to engage in giving honest feedback. Conversely, what was most detrimental to quality of care was when poor culture developed that hampered authentic patient experience work.
We found that patients will give feedback only to staff whom they trust, a finding that resonates with the results of WP1, which highlights the importance of trusting, available, consistent therapeutic relationships (the fourth of the themes) with ward staff as the most important determinant of patient experience. What realist evaluation has offered, to both support and enhance this finding, is the mechanisms by which the loss of trust takes place and how, why and for whom that happens. This is particularly relevant when thinking about institutional racism (i.e. staff not tackling racist abuse between patients) as damaging particular populations’ abilities to trust within inpatient settings. The culture of the ward or organisation is a powerful contextual moderator of the outcomes of obtaining meaningful inpatient experience data.
Linked to this point, the realist evaluation demonstrated that, although the conditions in which trust may be activated vary, establishing trust was a critical ingredient for patient experience work. Our results support the view that meaningful patient experience data are available only in places where the quality of care is good and where patients feel able to trust staff. Paradoxically, therefore, it may be impossible to obtain meaningful (and vitally important) feedback when the care quality is poor. This is even truer for carers, who often feel excluded and that their views are unwelcome. Moreover, they fear for the safety of their friend or family member and worry about giving honest feedback because they do not want to negatively influence their care.
One consequence of this was that ward staff (who rarely see the results of feedback, let alone actions that might arise from its use) often perceived patient experience data as serving corporate purposes (e.g. the obligation to report these data outside the organisation) rather than as leading to service improvement. Because service users do not see changes occurring as a result of their feedback (the final theme), they may be loath to give it. By contrast, ward staff, who were closest to the patient experience data and, therefore, best placed to effect meaningful change as a result, often did not get sight of the formal patient experience data and were therefore denied the opportunity to act on it. At the same time, they were not empowered to act on the informal patient experience feedback that was given to them or their colleagues directly.
Another key finding was that positive feedback is important for patients to give (from their perspective), but is often dismissed. Negative feedback (in the form of complaints) was often considered to carry far more weight and is subject to formal processes. Positive feedback, which was often dismissed (and, therefore, lost) is a rich source of data for planning and service improvement. However, some staff perceive feedback as threatening and avoid asking for it. This was particularly evident in trusts in which the corporate function (i.e. service management) was visible at ward level only in response to criticism, complaints or serious incidents, rather than in response to feedback in the round.
Health economic modelling (work package 5)
To examine the cost-effectiveness implications of collecting and using patient experience data and of adopting best practice, three logic models were created. Two logic models, representing low- and high-intensity patient experience data processes (as identified in WP3), were developed. A third model was created to illustrate how implementing patient experience feedback could improve cost-effectiveness in the delivery of inpatient care, using the example of alleviating boredom on the ward. In the absence of prospective data, we sought to compare the costs (obtained using standard unit costs for activities characterised from our WP3 case study data) and potential benefits of these two archetypes.
A key conclusion of our economic modelling (WP5) was that the costs of collecting informal patient feedback (i.e. staff time) far outweighed all other aspects of the patient experience data cycle. Although it might be argued that some of this time is part of routine patient care, it highlights a dilemma: investment in collecting patient experience data this way carries substantial risk given the dearth of evidence showing that these data lead to substantive improvements in patient care.
Further findings
There were a number of findings that, although less common in our data set, require comment. The first of these is experiences of racism. This took the form of patients complaining that they had been subject to racist remarks by other patients and that staff had not responded to or addressed these adequately. We are unable to comment on whether or not this represents instances of institutional racism, but these experiences had a profound effect on the patients concerned. In terms of the aims of our research, our conclusion is that this created a divide between patients and staff, prevented the formation of trusting therapeutic relationships and deterred patients from BAME communities from giving honest feedback. One reason why this is so important is because patients of black ethnicity, in particular, continue to be over-represented in inpatient mental health settings. Unless experiences of racism are addressed effectively, it will continue to prove difficult for patients from BAME groups to give honest patient experience feedback. As long as this continues, services will be unable to improve in response to poor episodes of care, further marginalising and disadvantaging particular populations.
We also found that many (if not the majority of) patients that we interviewed reported that they did not understand their medication, had questions they wished to ask about their medication or were concerned about the side effects of medication. Likewise, many patients told us that they did not understand their care pathway, the implications of being detained under the Mental Health Act33 or their rights in relation to their health and care. Explaining medication and other aspects of treatment, and offering patients more opportunity to consult about their medication, was linked to the likelihood of obtaining patient experience feedback. Giving people time to talk needs to be a priority in inpatient settings, because, without having their questions answered and their concerns (e.g. about side effects) addressed, patients remain mistrustful of professionals. This resonates with the ‘patient-centred’ theme from the WP1 systematic review and reminds us that the processes that underlie good-quality care also increase the chances that patients will be motivated (and feel sufficiently secure) to provide meaningful feedback.
Strengths and limitations
The strengths and limitations of each of the five WPs are described in previous chapters. We wish to draw attention here to the way in which each of these informed the WPs that followed and supported the realist methodology. Without WP1 and WP2, we would not have been able to create the interview schedules in WP3 or to engage participants in the WP4 consensus conference. We would also like to highlight the extensive involvement of service users and carers throughout, including the contribution of two survivor researchers and the highly engaged PPIT.
To our knowledge, the systematic review of inpatient experiences (WP1) was the largest review of its kind and WP2 was the first-ever national survey of PELs in NHS mental health trusts in England. These interviews provided considerable insights into the nature of patient experience work, its methods and organisational embeddedness, and its often insecure status. Following these interviews, we secured the participation of six case study sites, the diversity of which, in respect of patient experience practice, reflected well on the data-gathering and site selection methodologies in WP2. We achieved all recruitment targets in WP3 and interviewed at least one patient on all adult inpatient wards in each participating trust. We were able to secure the enthusiastic participation of staff and patients at each site, without inferring that any one place was superior to the other in terms of its patient experience practices.
We elicited a large number of rich data during the course of WP3, which generated over 12,000 coded excerpts and more than 150 CMO configurations. The rules that were based on these findings were well received by participants at the WP4 consensus conference. The use of a realist approach to evaluation meant that we treated context as both informative and central to the activation of the mechanisms we elucidated at each stage of the patient experience data cycle. Therefore, we believe that our findings will be more readily actionable in other settings than if we had adopted a more traditional evaluation of effectiveness.
There were a number of limitations of this research. As a qualitative study, based on a subsample of all eligible trusts, our case study sites were not intended to be representative. They were selected to enable us to develop, test and refine our programme theories, rather than for benchmarking practice in participating trusts. Likewise, rather than identifying examples of ‘best practice’ (which were context dependent and, therefore, difficult to transpose to different settings), we have generated an understanding of the ways in which context and process interact to generate desired outcomes.
We were limited by the relatively brief time frame of our research. Ours was essentially a cross-sectional study in which we asked participants about recent experiences (or current practices) in respect of giving, receiving, analysing or using patient experience data to drive service change. We were reliant on participants to identify examples of service change, rather than being able to observe these ourselves. This had implications for our health economic models (in WP5), which were limited in the estimation and costing of tangible benefits associated with the collection and use of patient experience data. The health economic WP was, however, primarily limited by different understandings of what ‘patient experience’ data collection, analysis and use comprised, and particularly whether time spent talking to patients about their experiences was patient experience work or a routine care activity. This made costing the different elements of patient experience work difficult.
We deliberately avoided approaching this work by means of comparative analysis across trusts. We were sensitive from the outset to the risk of (even unwittingly) labelling trusts as good, bad or indifferent at collecting and using patient experience data to improve services. We recognise that this type of approach is prevalent in the NHS, in which inspection and benchmarking are commonplace. We studiously avoided this for several reasons.
First, our assessment tools (especially the WP2 semistructured interview schedule) were designed to elicit information for sampling case study sites and not to score and rank trusts. Any attempt to do this would lack validity. Second, rating and ranking trusts would almost certainly have undermined participation in our research. It is highly unlikely that trusts assigned low or poor ratings would have taken part. Finally, our realist approach was designed to develop, test and iterate programme theories about the optimal ways to collect and use patient experience data based on interviews from across all of the case study sites. This is very different from a comparative approach in which we might have sought to identify trusts that were doing things well and concluded that all trusts should replicate or emulate this.
Service managers were represented at the consensus conference, although we acknowledge that the consultation about potential barriers to adopting optimal (best) practice might have been more extensive had time permitted. This is something we will need to address in developing the proposed interventional study.
Conclusions and implications for research and practice
We achieved our stated aims of identifying the most effective ways of collecting and using patient experience data to improve the quality of inpatient mental health care. We did so by means of realist evaluation and in a way that derived a nuanced understanding of the processes involved, rather than by picking out and highlighting trusts that were doing this particularly well. In truth, practice was highly variable and some trusts did some things well in some of their wards. Our learning was weighted in favour of insights into the contexts and mechanisms that condition the collection of patient feedback, because there were so few tangible examples of patient experience data being analysed and used to change the ways that care is delivered. We framed our final programme theories as 18 rules that might guide trusts in their efforts to collect and use patient experience in inpatient settings more effectively. We believe that this is far more useful, and practical, than concluding that trust X is a beacon to be emulated.
Patient experience work is insufficiently embedded in most mental health trusts that we surveyed and visited. There was, however, a great deal of enthusiasm for this work among the very dedicated PELs we spoke to. However, to have an impact on services and those who use them, this work needs to be informed by the ‘rules’ we have elucidated in the course of this project. Collecting and acting on patient experience feedback needs to be seen as everyone’s business and as essential to the delivery of care. Positive and informal feedback needs to be valued far more highly than at present, and it is incumbent on those who collect these data to recognise that those who give such feedback will do so only if they trust the recipient and if they have confidence that the information they provide will be acted on.
This leads us to the further reflection that the willingness of patients to provide meaningful (as opposed to superficial) feedback is influenced by the same factors that determine positive experiences of inpatient care, namely trusting and compassionate therapeutic relationships. This finding raises the very serious concern that the most important forms of feedback may not be forthcoming in places where care is poor. Furthermore, patients and staff need to view feedback as a quality improvement activity rather than as a bureaucratic or regulatory exercise. This might be achieved in two ways: by improving feedback about feedback and by shortening the loop between feedback and improvement actions by empowering those nearest to patients to act on the feedback they receive.
Perhaps the most important finding is that patient experience data alone are not sufficient to inform service improvement actions in the absence of data on safety and outcomes. Instead, patient experience data need to be triangulated with safety and outcomes indicators to support and drive quality improvement in inpatient mental health services. When this is done, there are gains to be made. However, we found that patient experience data were often either treated as necessary only for regulatory compliance (in the form of the minimally informative results from the FFT) or viewed as ‘nice to have’ rather than as essential to the delivery of trusts’ core objectives.
Our findings suggest that, when safety and outcomes data indicate a service ‘hot spot’, patient experience data can be crucial in providing evidence of the ways in which services need to change. Whereas outcomes and safety data can show what is happening (as well as trends), patient experience data often hold explanatory power and help explain the reasons why something is happening. Consideration of data held in silos is unhelpful and counterproductive; instead, our results support the role of targeted, intelligence-led, co-ordinated patient experience enquiry.
We suggest that further research is needed to test if our findings can be put into practice and if they lead to improvements in patient experience and clinical and service outcomes. The 18 rules identified by the end of WP4, representing a codified version of our final programme theories, will form the basis of an intervention that is to be tailored according to local needs and preferences. This work will not be without challenge, including operationalising an intervention that will inevitably vary in exact content between places. Moreover, any such research will need to consider carefully how best to distinguish between (and attach relevant costs to) items of service that are specific to patient experience activities rather and those that are routine clinical care, given that these are inextricably interwoven. This will require further reflection on how best to capture more informal ways of giving and receiving feedback. This will inevitably require significant work to demonstrate both the feasibility of delivering the intervention and the conditions necessary for robust evaluation. Such a study might, for example, lend itself to a stepped-wedge design.
Acknowledgements
This work uses data provided by the patients, carers and NHS staff who took part in the interviews described in this report and would not have been possible without their involvement.
We acknowledge the assistance, support and guidance of the R&D staff at each of the six case study sites who played a substantial role in enabling the study.
We would like to acknowledge research assistants Nicole De Valliere and Lizz Kimber for the data collection relating to the evaluation of PPIT involvement and the PPI chapter (Chapter 3).
Contributions of authors
Scott Weich (https://orcid.org/0000-0002-7552-7697) (Professor, mental health service research) was the chief investigator and guarantor of the research. He had overall responsibility for the design, delivery, interpretation and dissemination of the study findings, as well as research governance and data security. He chaired the Project Oversight Group and attended the Study Steering Committee. He was responsible for the final version of this report.
Sarah-Jane Fenton (https://orcid.org/0000-0001-9751-6262) (Research Fellow, health services research) was the senior project researcher responsible for the day-to-day running of the study, including undertaking WP2 interviews and leading WP3 fieldwork. She led all aspects of the data analysis, prepared interim reports and drafted several chapters of the final report. She was a member of the Project Oversight Group and the Study Steering Committee. She co-designed and co-led the PPI work with David Crepaz-Keay. She contributed to the PPI chapter (Chapter 3).
Sophie Staniszewska (https://orcid.org/0000-0002-7723-9074) (Professor, user involvement) led WP1 and was responsible for its design, conduct and reporting, and supervised one of the researchers (Carole Mockford). She drafted Chapter 4 based on this review. She was a member of the Project Oversight Group.
Alastair Canaway (https://orcid.org/0000-0002-4270-6808) (Research Fellow, health economics) undertook the study analyses in relation to WP5 and drafted the relevant chapter in this report (Chapter 8). He was a member of the Project Oversight Group.
David Crepaz-Keay (https://orcid.org/0000-0003-3845-4721) (expert by experience, PPI) was responsible for co-ordinating and leading the mental health service user and carer consultation throughout the project. He drafted a report of the service user and carer involvement work, which was drawn on in drafting Chapter 3, and he contributed to the interpretation and reporting of the study findings. He co-authored the PPI chapter (Chapter 3). He was a member of the Project Oversight Group.
Michael Larkin (https://orcid.org/0000-0003-3304-7000) (Professor, psychology) contributed to the study design and conduct, particularly WP1 and WP3. He contributed to the work on service user and carer involvement and led the evaluation of this. He contributed to the interpretation of study findings and to the drafting of the final report. He co-authored the PPI chapter (Chapter 3). He was a member of the Project Oversight Group.
Jason Madan (https://orcid.org/0000-0003-4316-1480) (Professor, health economics) led WP5, provided health economics expertise, supervised Alastair Canaway on the WP5 data analysis and contributed to the drafting of the final report. He was a member of the Project Oversight Group.
Carole Mockford (https://orcid.org/0000-0002-4288-9229) (Senior Research Fellow, health services research) undertook the WP1 systematic review and contributed to the drafting of the relevant chapter in the final report (Chapter 4).
Kamaldeep Bhui (https://orcid.org/0000-0002-9205-2144) (Professor, mental health service research) contributed to the design of the study, commented on and contributed to the interpretation of the results throughout the project, commented in detail on study reports and attended project team meetings. He was a member of the Project Oversight Group.
Elizabeth Newton (https://orcid.org/0000-0002-1113-8801) (Lecturer, psychology) contributed to the study design and conduct, particularly WP3. She contributed to the service user and carer involvement work and undertook the evaluation of this. She contributed to the interpretation of study findings and to the drafting of the final report. She co-authored the PPI chapter (Chapter 3). She was a member of the Project Oversight Group.
Charlotte Croft (https://orcid.org/0000-0002-9672-7567) (Associate Professor, organisational research) contributed to the study design and conduct (particularly in WP3) and to the analysis and interpretation of the study data and to the drafting of the final report. She was a member of the Project Oversight Group.
Una Foye (https://orcid.org/0000-0002-3414-2854) (Research Associate, health services research) and Aimee Cairns (https://orcid.org/0000-0002-6090-3602) (Research Associate, health services research) undertook WP3 data collection and assisted in the analysis of WP2 and WP3 data. They supported the service user and carer involvement work and the survivor researchers. They contributed to the interpretation of the study findings and to the drafting of the final report. They contributed to the PPI chapter (Chapter 3).
Emma Ormerod (https://orcid.org/0000-0001-6939-8473) (survivor researcher) and Stephen Jeffreys (https://orcid.org/0000-0002-5088-9309) (survivor researcher) undertook WP3 data collection and contributed to the analysis of these data. She supported the service user and carer involvement work and contributed to the interpretation of WP2 data and to the selection of WP3 case study sites. She co-authored the PPI chapter (Chapter 3).
Frances Griffiths (https://orcid.org/0000-0002-4173-1438) (Professor, health services research) contributed to all aspects of the study design and conduct, including dissemination and report writing. She led WP3 and WP4. She supervised Sarah-Jane Fenton in the analysis of WP3 data. She was a member of the Project Oversight Group.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Staniszewska S, Bullock I. Can we help patients have a better experience? Implementing NICE guidance on patient experience. Evid Based Nurs 2012;15. https://doi.org/10.1136/eb-2012-100988.
- NHS Confederation . Feeling Better? Improving Patient Experience in Hospital 2010.
- Department of Health and Social Care . NHS Patient Experience Framework 2012.
- Francis RQ. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary 2013.
- National Institute for Health and Care Excellence . Patient Experience in Adult NHS Services. Evidence Update February 2014: Evidence Update 52 2014.
- National Institute for Health and Care Excellence . Service User Experience in Adult Mental Health: Improving the Experience of Care for People Using Adult NHS Mental Health Services 2011.
- Staniszewska S, Boardman F, Gunn L, Roberts J, Clay D, Seers K, et al. The Warwick Patient Experiences Framework: patient-based evidence in clinical guidelines. Int J Qual Health Care 2014;26:151-7. https://doi.org/10.1093/intqhc/mzu003.
- Coulter A, Locock L, Ziebland S, Calabrese J. Collecting data on patient experience is not enough: they must be used to improve care. BMJ 2014;348. https://doi.org/10.1136/bmj.g2225.
- Boiko O, Campbell JL, Elmore N, Davey AF, Roland M, Burt J. The role of patient experience surveys in quality assurance and improvement: a focus group study in English general practice. Health Expect 2015;18:1982-94. https://doi.org/10.1111/hex.12298.
- Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-001570.
- Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care 2011;17:41-8.
- Black NVM, Hutchings A. Relationships between patient reported experience (PREMs) and patient reported outcomes (PROMs) in elective surgery. BMJ Qual Saf 2014;23:534-42. https://doi.org/10.1136/bmjqs-2013-002707.
- Fenton JJ, Jerant AF, Bertakis KD, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med 2012;172:405-11. https://doi.org/10.1001/archinternmed.2011.1662.
- Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med 2013;368:201-3. https://doi.org/10.1056/NEJMp1211775.
- Rose G, Beale I, Malone J, Kinkead S, Higgin J. Validity of a scale for consumer evaluation of mental health service delivery. Int J Pers Centered Med 2011;1:733-40.
- Care Quality Commission . Community Mental Health Survey 2015 n.d. www.cqc.org.uk/content/community-mental-health-survey-2015 (accessed 23 August 2016).
- NHS England . Friends and Family Test n.d. www.england.nhs.uk/ourwork/pe/fft/ (accessed 19 May 2017).
- Robert G, Cornwell J, Black N. Friends and Family Test should no longer be mandatory. BMJ 2018;360. https://doi.org/10.1136/bmj.k367.
- NHS England . The Friends and Family Test Review 2014 n.d. www.england.nhs.uk/fft/fft-test-review/ (accessed 28 January 2020).
- NHS . NHS England and NHS Improvement Guidance. Using the Friends and Family Test to Improve Patient Experience n.d. www.england.nhs.uk/wp-content/uploads/2019/09/using-the-fft-to-improve-patient-experience-guidance-v2.pdf (accessed 28 January 2020).
- Keown OP, Parston G, Patel H, Rennie F, Saoud F, Al Kuwari H, et al. Lessons from eight countries on diffusing innovation in health care. Health Aff 2014;33:1516-22. https://doi.org/10.1377/hlthaff.2014.0382.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Faulkner A, Williams K. Future Perfect: Mental Health Service Users Set Out a Vision for the 21st Century 2005. www.rethink.org/media/2689/future-perfect-report.pdf (accessed 28 January 2020).
- Mind . Listening to Experience: An Independent Inquiry into Acute and Crisis Mental Healthcare 2011.
- Royal College of Psychiatrists . Improving In-Patient Mental Health Services for Black and Minority Ethnic Patients: Recommendations to Inform Accreditation Standards 2010.
- Morrow E, Robert G, Maben J, Griffiths P. Improving healthcare quality at scale and pace: lessons from The Productive Ward: Releasing Time to CareTM. Int J Qual Health Care 2011;25:237-53. https://doi.org/10.1108/09526861211221464.
- Star Wards . Star Wards n.d. www.starwards.org.uk/ (accessed 1 December 2017).
- Cresswell J, Beavon M. Accreditation for Inpatient Mental Health Services (AIMS): Standards For Inpatient Wards – Working-age Adults. London: Royal College of Psychiatrists’ Centre for Quality Improvement; 2010.
- Commission for Healthcare Audit and Inspection . The Pathway to Recovery: A Review of NHS Acute Inpatient Mental Health Services 2008.
- Bhui K, Stansfeld S, Hull S, Priebe S, Mole F, Feder G. Ethnic variations in pathways to and use of specialist mental health services in the UK. Systematic review. Br J Psychiatry 2003;182:105-16. https://doi.org/10.1192/bjp.182.2.105.
- Commission for Healthcare Audit and Inspection . Count Me In 2008: Results of the 2008 National Census of Inpatients in Mental Health and Learning Disability Services in England and Wales 2008.
- Bhui KS, Dinos S, McKenzie K. Ethnicity and its influence on suicide rates and risk. Ethn Health 2012;17:141-8. https://doi.org/10.1080/13557858.2011.645151.
- Great Britain . Mental Health Act 2007 2007.
- Alvesson M, Skoldberg K. Reflexive Methodology: New Vistas for Qualitative Research. London: SAGE Publications Ltd; 2009.
- Bhaskar R, Danermark B. Metatheory, interdisciplinarity and disability research: a critical realist perspective. Scand J Disabil Res 2006;8:278-97.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 1997.
- Westhorp G. Realist Impact Evaluation: An Introduction 2014. www.odi.org/publications/8716-realist-impact-evaluation-introduction (accessed 28 January 2020).
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Jagosh J. Introduction to Realist Evaluation and Synthesis n.d.
- Jagosh J, Bush PL, Salsberg J, Macaulay AC, Greenhalgh T, Wong G, et al. A realist evaluation of community-based participatory research: partnership synergy, trust building and related ripple effects. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1949-1.
- Wong G, Westhorp G, Greenhalgh J, Manzano A, Jagosh J, Greenhalgh T. Quality and reporting standards, resources, training materials and information for realist evaluation: the RAMESES II project. Health Serv Deliv Res 2017;5:1-108. https://doi.org/10.3310/hsdr05280.
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: SAGE Publications, Inc.; 2014.
- Harvey DL, Byrne DS, Ragin CC. The SAGE Handbook of Case-Based Methods. London: SAGE Publications Ltd; 2009.
- Fenton S-J. Mental Health Service Delivery for Adolescents and Young People: A Comparative Study Between Australia and the UK 2016.
- National Survivor User Network . Involvement for Influence: 4PI Involvement Standards 2015. www.nationalvoices.org.uk/sites/default/files/public/4pinationalinvolvementstandardsfullreport20152.pdf (accessed 28 January 2020).
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- Madden M, Speed E. Beware zombies and unicorns: toward critical patient and public involvement in health research in a neoliberal context. Front Sociol 2017;2. https://doi.org/10.3389/fsoc.2017.00007.
- Rose D, Carr S, Beresford P. ‘Widening cross-disciplinary research for mental health’: what is missing from the Research Councils UK mental health agenda?. Disabil Soc 2018;33:476-81. https://doi.org/10.1080/09687599.2018.1423907.
- Minogue V, Cooke M, Donskoy AL, Vicary P, Wells B. Patient and public involvement in reducing health and care research waste. Res Involv Engagem 2018;4. https://doi.org/10.1186/s40900-018-0087-1.
- Ennis L, Wykes T. Impact of patient involvement in mental health research: longitudinal study. Br J Psychiatry 2013;203:381-6. https://doi.org/10.1192/bjp.bp.112.119818.
- Wolstenholme D, Grindell C, Dearden A. A co-design approach to service improvement resulted in teams exhibiting characteristics that support innovation. Des Health 2017;1:42-58. https://doi.org/10.1080/24735132.2017.1295531.
- Ormerod E, Beresford P, Carr S, Gould D, Jeffreys S, Machin K, et al. Survivor Researcher Network Manifesto: Mental Health Knowledge Built by Service Users and Survivors 2018.
- INVOLVE . Guidance on Co-Producing a Research Project 2018.
- Rose D, Sweeney A, Beresford P, Faulkner A, Sweeney A, Rose D, et al. This is Survivor Research. Ross-on-Wye: PCCS Books; 2009.
- Faulkner A, Sweeney A, Beresford P, Faulkner A, Sweeney A, Rose D, et al. This is Survivor Research. Ross-on-Wye: PCCS Books; 2009.
- Gillard S, Turner K, Neffgen M, Staddon P. Mental Health Service Users in Research: Critical Sociological Perspective. New York, NY: Policy Press; 2015.
- Care Quality Commission . Monitoring the Mental Health Act in 2012 13 2014.
- National Institute for Health and Care Excellence (NICE) . Service User Experience in Adult Mental Health Services 2011.
- Care Quality Commission . The State of Care in Mental Health Services 2014 to 2017: Findings from CQC’s Programme of Comprehensive Inspections of Specialist Mental Health Services 2017.
- National Institute for Health and Care Excellence . Patient Experience in Adult NHS Services: Improving the Experience of Care for People Using Adult NHS Services 2012.
- Curtis S, Gesler W, Priebe S, Francis S. New spaces of inpatient care for people with mental illness: a complex ‘rebirth’ of the clinic?. Health Place 2009;15:340-8. https://doi.org/10.1016/j.healthplace.2008.06.007.
- Barbato A, Bajoni A, Rapisarda F, D’Anza V, De Luca LF, Inglese C, et al. Quality assessment of mental health care by people with severe mental disorders: a participatory research project. Community Ment Health J 2014;50:402-8. https://doi.org/10.1007/s10597-013-9667-6.
- Bramesfeld A, Klippel U, Seidel G, Schwartz FW, Dierks ML. How do patients expect the mental health service system to act? Testing the WHO responsiveness concept for its appropriateness in mental health care. Soc Sci Med 2007;65:880-9. https://doi.org/10.1016/j.socscimed.2007.03.056.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- CASP . Critical Skills Appraisal Programme 2007. https://casp-uk.net/ (accessed 18 December 2018).
- Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018;52:1893-907. https://doi.org/10.1007/s11135-017-0574-8.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Katsakou C, Marougka S, Garabette J, Rost F, Yeeles K, Priebe S. Why do some voluntary patients feel coerced into hospitalisation? A mixed-methods study. Psychiatry Res 2011;187:275-82. https://doi.org/10.1016/j.psychres.2011.01.001.
- Katsakou C, Rose D, Amos T, Bowers L, McCabe R, Oliver D, et al. Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol 2012;47:1169-79. https://doi.org/10.1007/s00127-011-0427-z.
- Bennewith O, Amos T, Lewis G, Katsakou C, Wykes T, Morriss R, et al. Ethnicity and coercion among involuntarily detained psychiatric in-patients. Br J Psychiatry 2010;196:75-6. https://doi.org/10.1192/bjp.bp.109.068890.
- Kauppi K, Hätönen H, Adams CE, Välimäki M. Perceptions of treatment adherence among people with mental health problems and health care professionals. J Adv Nurs 2015;71:777-88. https://doi.org/10.1111/jan.12567.
- Kontio R, Anttila M, Lantta T, Kauppi K, Joffe G, Välimäki M. Toward a safer working environment on psychiatric wards: service users’ delayed perspectives of aggression and violence-related situations and development ideas. Perspect Psychiatr Care 2014;50:271-9. https://doi.org/10.1111/ppc.12054.
- Kontio R, Joffe G, Putkonen H, Kuosmanen L, Hane K, Holi M, et al. Seclusion and restraint in psychiatry: patients’ experiences and practical suggestions on how to improve practices and use alternatives. Perspect Psychiatr Care 2012;48:16-24. https://doi.org/10.1111/j.1744-6163.2010.00301.x.
- Whittington R, Bowers L, Nolan P, Simpson A, Neil L. Approval ratings of inpatient coercive interventions in a national sample of mental health service users and staff in England. Psychiatr Serv 2009;60:792-8. https://doi.org/10.1176/ps.2009.60.6.792.
- Bowers L, Haglund K, Muir-Cochrane E, Nijman H, Simpson A, Van Der Merwe M. Locked doors: a survey of patients, staff and visitors. J Psychiatr Ment Health Nurs 2010;17:873-80. https://doi.org/10.1111/j.1365-2850.2010.01614.x.
- Stewart D, Burrow H, Duckworth A, Dhillon J, Fife S, Kelly S, et al. Thematic analysis of psychiatric patients’ perceptions of nursing staff. Int J Ment Health Nurs 2015;24:82-90. https://doi.org/10.1111/inm.12107.
- Wyder M, Bland R, Herriot A, Crompton D. The experiences of the legal processes of involuntary treatment orders: tension between the legal and medical frameworks. Int J Law Psychiatry 2015;38:44-50. https://doi.org/10.1016/j.ijlp.2015.01.006.
- Wyder M, Bland R, Blythe A, Matarasso B, Crompton D. Therapeutic relationships and involuntary treatment orders: service users’ interactions with health-care professionals on the ward. Int J Ment Health Nurs 2015;24:181-9. https://doi.org/10.1111/inm.12121.
- Alexander J. Patients’ feelings about ward nursing regimes and involvement in rule construction. J Psychiatr Ment Health Nurs 2006;13:543-53. https://doi.org/10.1111/j.1365-2850.2006.00977.x.
- Baker JA, Lovell K, Easton K, Harris N. Service users’ experiences of ‘as needed’ psychotropic medications in acute mental healthcare settings. J Adv Nurs 2006;56:354-62. https://doi.org/10.1111/j.1365-2648.2006.04016.x.
- Bonner G, Lowe T, Rawcliffe D, Wellman N. Trauma for all: a pilot study of the subjective experience of physical restraint for mental health inpatients and staff in the UK. J Psychiatr Ment Health Nurs 2002;9:465-73. https://doi.org/10.1046/j.1365-2850.2002.00504.x.
- Bowl R. The need for change in UK mental health services: South Asian service users’ views. Ethn Health 2007;12:1-19. https://doi.org/10.1080/13557850601002239.
- Chorlton E, Smith I, Jones SA. Understanding how people who use illicit drugs and alcohol experience relationships with psychiatric inpatient staff. Soc Psychiatry Psychiatr Epidemiol 2015;50:51-8. https://doi.org/10.1007/s00127-014-0920-2.
- Cutting P, Henderson C. Women’s experiences of hospital admission. J Psychiatr Ment Health Nurs 2002;9:705-12. https://doi.org/10.1046/j.1365-2850.2002.00516.x.
- Duggins R, Shaw I. Examining the concept of patient satisfaction in patients with a diagnosis of schizophrenia: a qualitative study. Psychiatr Bull 2006;30:142-5. https://doi.org/10.1192/pb.30.4.142.
- Fenton K, Larkin M, Boden ZV, Thompson J, Hickman G, Newton E. The experiential impact of hospitalisation in early psychosis: service-user accounts of inpatient environments. Health Place 2014;30:234-41. https://doi.org/10.1016/j.healthplace.2014.09.013.
- Gilburt H, Rose D, Slade M. The importance of relationships in mental health care: a qualitative study of service users’ experiences of psychiatric hospital admission in the UK. BMC Health Serv Res 2008;8. https://doi.org/10.1186/1472-6963-8-92.
- Greenwood N, Hussain F, Burns T, Raphael F. Asian in-patient and carer views of mental health care. Asian views of mental health care. J Ment Health 2000;9:397-408. https://doi.org/10.1080/713680255.
- Hughes R, Hayward M, Finlay WML. Patients’ perceptions of the impact of involuntary inpatient care on self, relationships and recovery. J Ment Health 2009;18:152-60. https://doi.org/10.1080/09638230802053326.
- Jones A, Crossley D. In the mind of another shame and acute psychiatric inpatient care: an exploratory study. A report on phase one: service users. J Psychiatr Ment Health Nurs 2008;15:749-57. https://doi.org/10.1111/j.1365-2850.2008.01316.x.
- Labib PLZ, Brownell L. Factors affecting patient satisfaction with the psychiatric ward round: retrospective cross-sectional study. Psychiatr Bull 2009;33:295-8. https://doi.org/10.1192/pb.bp.108.020529.
- Milner G, Jankovic J, Hoosen I, Marrie D. Patients and staff understanding of general adult psychiatry ward rounds. J Ment Health 2008;17:492-7. https://doi.org/10.1080/09638230701529673.
- Nolan P, Bradley E, Brimblecombe N. Disengaging from acute inpatient psychiatric care: a description of service users’ experiences and views. J Psychiatr Ment Health Nurs 2011;18:359-67. https://doi.org/10.1111/j.1365-2850.2010.01675.x.
- Ridley J, Hunter S. Subjective experiences of compulsory treatment from a qualitative study of early implementation of the Mental Health (Care . Treatment) (Scotland) Act 2003. Health Soc Care Community 2013;21:509-18. https://doi.org/10.1111/hsc.12041.
- Russo J, Rose D. ‘But what if nobody’s going to sit down and have a real conversation with you?’ Service user/survivor perspectives on human rights. J Public Ment Health 2013;12:184-92. https://doi.org/10.1108/JPMH-05-2013-0030.
- Stenhouse RC. ‘They all said you could come and speak to us’: patients’ expectations and experiences of help on an acute psychiatric inpatient ward. J Psychiatr Ment Health Nurs 2011;18:74-80. https://doi.org/10.1111/j.1365-2850.2010.01645.x.
- Kennedy J, Fortune T. Women’s experiences of being in an acute psychiatric unit: an occupational perspective. Br J Occup Ther 2014;77:296-303. https://doi.org/10.4276/030802214X14018723138048.
- Borge L, Fagermoen MS. Patients’ core experiences of hospital treatment: wholeness and self-worth in time and space. J Ment Health 2008;17:193-205. https://doi.org/10.1080/09638230701505996.
- Gunasekara I, Pentland T, Rodgers T, Patterson S. What makes an excellent mental health nurse? A pragmatic inquiry initiated and conducted by people with lived experience of service use. Int J Ment Health Nurs 2014;23:101-9. https://doi.org/10.1111/inm.12027.
- Sibitz I, Scheutz A, Lakeman R, Schrank B, Schaffer M, Amering M. Impact of coercive measures on life stories: qualitative study. Br J Psychiatry 2011;199:239-44. https://doi.org/10.1192/bjp.bp.110.087841.
- Thibeault CA, Trudeau K, d’Entremont M, Brown T. Understanding the milieu experiences of patients on an acute inpatient psychiatric unit. Arch Psychiatr Nurs 2010;24:216-26. https://doi.org/10.1016/j.apnu.2009.07.002.
- Johansson H, Eklund M. Patients’ opinion on what constitutes good psychiatric care. Scand J Caring Sci 2003;17:339-46. https://doi.org/10.1046/j.0283-9318.2003.00233.x.
- Ejneborn Looi GM, Engström Å, Sävenstedt S. A self-destructive care: self-reports of people who experienced coercive measures and their suggestions for alternatives. Issues Ment Health Nurs 2015;36:96-103. https://doi.org/10.3109/01612840.2014.951134.
- Chien WT, Chan CW, Lam LW, Kam CW. Psychiatric inpatients’ perceptions of positive and negative aspects of physical restraint. Patient Educ Couns 2005;59:80-6. https://doi.org/10.1016/j.pec.2004.10.003.
- Iversen VC, Sallaup T, Vaaler AE, Helvik A-S, Morken G, Linaker O. Patients’ perceptions of their stay in a psychiatric seclusion area. J Psychiatr Intensive Care 2011;7:1-10. https://doi.org/10.1017/S1742646410000075.
- McGuinness D, Dowling M, Trimble T. Experiences of involuntary admission in an approved mental health centre. J Psychiatr Ment Health Nurs 2013;20:726-34. https://doi.org/10.1111/jpm.12007.
- Donald F, Duff C, Lee S, Kroschel J, Kulkarni J. Consumer perspectives on the therapeutic value of a psychiatric environment. J Ment Health 2015;24:63-7. https://doi.org/10.3109/09638237.2014.954692.
- Thomas SP, Shattell M, Martin T. What’s therapeutic about the therapeutic milieu?. Arch Psychiatr Nurs 2002;16:99-107. https://doi.org/10.1053/apnu.2002.32945.
- Ntsaba GM, Havenga Y. Psychiatric in-patients’ experience of being secluded in a specific hospital in Lesotho. Health SA Gesondheid 2007;12:3-12. https://doi.org/10.4102/hsag.v12i4.267.
- Robins CS, Sauvageot JA, Cusack KJ, Suffoletta-Maierle S, Frueh BC. Consumers’ perceptions of negative experiences and ‘sanctuary harm’ in psychiatric settings. Psychiatr Serv 2005;56:1134-8. https://doi.org/10.1176/appi.ps.56.9.1134.
- Lilja L, Hellzén O. Former patients’ experience of psychiatric care: a qualitative investigation. Int J Ment Health Nurs 2008;17:279-86. https://doi.org/10.1111/j.1447-0349.2008.00544.x.
- Muir-Cochrane E, Oster C, Grotto J, Gerace A, Jones J. The inpatient psychiatric unit as both a safe and unsafe place: implications for absconding. Int J Ment Health Nurs 2013;22:304-12. https://doi.org/10.1111/j.1447-0349.2012.00873.x.
- Lindgren BM, Aminoff C, Hällgren Graneheim U. Features of everyday life in psychiatric inpatient care for self-harming: an observational study of six women. Issues Ment Health Nurs 2015;36:82-8. https://doi.org/10.3109/01612840.2014.941077.
- Ezeobele IE, Malecha AT, Mock A, Mackey-Godine A, Hughes M. Patients’ lived seclusion experience in acute psychiatric hospital in the United States: a qualitative study. J Psychiatr Ment Health Nurs 2014;21:303-12. https://doi.org/10.1111/jpm.12097.
- Meehan T, Vermeer C, Windsor C. Patients’ perceptions of seclusion: a qualitative investigation. J Adv Nurs 2000;31:370-7. https://doi.org/10.1046/j.1365-2648.2000.01289.x.
- Lucas M, Stevenson D. Violence and abuse in psychiatric in-patient institutions: a South African perspective. Int J Law Psychiatry 2006;29:195-203. https://doi.org/10.1016/j.ijlp.2005.08.010.
- Shattell M, Bartlett R, Beres K, Southard K, Bell C, Judge CA, et al. How patients and nurses experience an open versus an enclosed nursing station on an inpatient psychiatric unit. J Am Psychiatr Nurses Assoc 2015;21:398-405. https://doi.org/10.1177/1078390315617038.
- Stenhouse RC. ‘Safe enough in here?’: patients’ expectations and experiences of feeling safe in an acute psychiatric inpatient ward. J Clin Nurs 2013;22:3109-19. https://doi.org/10.1111/jocn.12111.
- Eytan A, Bovet L, Gex-Fabry M, Alberque C, Ferrero F. Patients’ satisfaction with hospitalization in a mixed psychiatric and somatic care unit. Eur Psychiatry 2004;19:499-501. https://doi.org/10.1016/j.eurpsy.2004.09.004.
- Mayers P, Keet N, Winkler G, Flisher AJ. Mental health service users’ perceptions and experiences of sedation, seclusion and restraint. Int J Soc Psychiatry 2010;56:60-73. https://doi.org/10.1177/0020764008098293.
- Cleary M, Hunt GE, Escott P, Walter G. Receiving difficult news. Views of patients in an inpatient setting. J Psychosoc Nurs Ment Health Serv 2010;48:40-8. https://doi.org/10.3928/02793695-20100504-01.
- O’Brien L, Cole R. Mental health nursing practice in acute psychiatric close-observation areas. Int J Ment Health Nurs 2004;13:89-9. https://doi.org/10.1111/j.1440-0979.2004.00324.x.
- Georgieva I, Mulder CL, Wierdsma A. Patients’ preference and experiences of forced medication and seclusion. Psychiatr Q 2012;83:1-13. https://doi.org/10.1007/s11126-011-9178-y.
- Steinert T, Birk M, Flammer E, Bergk J. Subjective distress after seclusion or mechanical restraint: one-year follow-up of a randomized controlled study. Psychiatr Serv 2013;64:1012-17. https://doi.org/10.1176/appi.ps.201200315.
- Holmes D, Kennedy SL, Perron A. The mentally ill and social exclusion: a critical examination of the use of seclusion from the patient’s perspective. Issues Ment Health Nurs 2004;25:559-78. https://doi.org/10.1080/01612840490472101.
- Anders RL, Olson T, Bader J. Assessment of acutely mentally ill patients’ satisfaction of care: there is a difference among ethnic groups. Issues Ment Health Nurs 2007;28:297-308. https://doi.org/10.1080/01612840601174094.
- Cleary M, Horsfall J, Jackson D, O’Hara-Aarons M, Hunt GE. Patients’ views and experiences of pro re nata medication in acute mental health settings. Int J Ment Health Nurs 2012;21:533-9. https://doi.org/10.1111/j.1447-0349.2012.00814.x.
- Kulkarni J, Gavrilidis E, Lee S, Van Rheenen TE, Grigg J, Hayes E, et al. Establishing female-only areas in psychiatry wards to improve safety and quality of care for women. Australas Psychiatry 2014;22:551-6. https://doi.org/10.1177/1039856214556322.
- Roe D, Ronen Y. Hospitalization as experienced by the psychiatric patient: a therapeutic jurisprudence perspective. Int J Law Psychiatry 2003;26:317-32. https://doi.org/10.1016/S0160-2527(03)00041-4.
- Brunero S, Lamont S, Fairbrother G. Using and understanding consumer satisfaction to effect an improvement in mental health service delivery. J Psychiatr Ment Health Nurs 2009;16:272-8. https://doi.org/10.1111/j.1365-2850.2008.01371.x.
- Thapinta D, Anders RL, Wiwatkunupakan S, Kitsumban V, Vadtanapong S. Assessment of patient satisfaction of mentally ill patients hospitalized in Thailand. Nurs Health Sci 2004;6:271-7. https://doi.org/10.1111/j.1442-2018.2004.00203.x.
- NHS England . Bed Availability and Occupancy Statistics 2016. www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/ (accessed 14 February 2018).
- Weich S, Fenton S-JH, Bhui K, Staniszewska S, Madan J, Larkin M, et al. Realist evaluation of the use of patient experience data to improve the quality of inpatient mental health care (EURIPIDES) in England: study protocol. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021013.
- De Silva D. Measuring Patient Experience. London: The Health Foundation; 2013.
- Her Majesty’s Treasury . The Green Book: Central Government Guidance on Appraisal and Evaluation 2011. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/685903/The_Green_Book.pdf (accessed 28 January 2020).
- Department of Health and Social Care . Policy Appraisal and Health n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/191503/policy_appraisal_and_health.pdf (accessed 28 January 2020).
- Emmel N. Sampling and Choosing Cases in Qualitative Research: A Realist Approach. Thousand Oaks, CA: SAGE Publications, Inc.; 2013.
- NHS England . Friends and Family Test Data – October 2017 2017. www.england.nhs.uk/publication/friends-and-family-test-data-october-2017/ (accessed 30 August 2018).
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006;18:59-82. https://doi.org/10.1177/1525822X05279903.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60. https://doi.org/10.1177/1356389016638615.
- Greenhalgh T, Pawson R, Wong G, Westhorp G, Greenhalgh J, Manzano A, et al. Retroduction in Realist Evaluation: The RAMESES II Project 2017. www.ramesesproject.org/media/RAMESES_II_Retroduction.pdf (accessed 12 July 2018).
- Care Quality Commission . Community Mental Health Survey 2017 2017. www.cqc.org.uk/publications/surveys/community-mental-health-survey-2017 (accessed 20 August 2018).
- Buchanan JM. The New Palgrave Dictionary of Economics. London: Palgrave Macmillan UK; 2017.
- Chapko MK, Liu CF, Perkins M, Li YF, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ 2009;18:1188-201. https://doi.org/10.1002/hec.1422.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- iWantGreatCare . IWantGreatCare 2018. www.iwgc.org/ (accessed 6 November 2018).
- The King’s Fund . Mental Health Under Pressure 2015. www.kingsfund.org.uk/publications/mental-health-under-pressure (accessed 6 November 2018).
- Marques E, Johnson EC, Gooberman-Hill R, Blom AW, Noble S. Using resource use logs to reduce the amount of missing data in economic evaluations alongside trials. Value Health 2013;16:195-201. https://doi.org/10.1016/j.jval.2012.09.008.
- Binnema D. Interrelations of psychiatric patient experiences of boredom and mental health. Issues Ment Health Nurs 2004;25:833-42. https://doi.org/10.1080/01612840490506400.
- Cutliffe J, Santos J, Kozel B, Taylor P, Lees D. Raiders of the Lost Art: a review of published evaluations of inpatient mental health care experiences emanating from the United Kingdom, Portugal, Canada, Switzerland, Germany and Australia. Int J Ment Health Nurs 2015;24:375-85. https://doi.org/10.1111/inm.12159.
- Duncan E, Best C, Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database Syst Rev 2010;1. https://doi.org/10.1002/14651858.CD007297.pub2.
- Ford SB, Bowyer T, Morgan P. The experience of compulsory treatment: the implications for recovery-orientated practice?. Ment Health Soc Inclusion 2015;19:126-32. https://doi.org/10.1108/MHSI-05-2015-0017.
- Gerolamo AM. State of the science: outcomes of acute inpatient psychiatric care. Arch Psychiatr Nurs 2004;18:203-14. https://doi.org/10.1016/j.apnu.2004.09.003.
- Hopkins JE, Loeb SJ, Fick DM. Beyond satisfaction, what service users expect of inpatient mental health care: a literature review. J Psychiatr Ment Health Nurs 2009;16:927-37. https://doi.org/10.1111/j.1365-2850.2009.01501.x.
- Katsakou C, Priebe S. Patient’s experiences of involuntary hospital admission and treatment: a review of qualitative studies. Epidemiol Psichiatr Soc 2007;16:172-8. https://doi.org/10.1017/S1121189X00004802.
- McHale J, Felton A. Self-harm: what’s the problem? A literature review of the factors affecting attitudes towards self-harm. J Psychiatr Ment Health Nurs 2010;17:732-40. https://doi.org/10.1111/j.1365-2850.2010.01600.x.
- Maatta S. Exploring male and female patients’ experiences of psychiatric hospital care: a critical analysis of the literature. Issues Ment Health Nurs 2009;30:174-80. https://doi.org/10.1080/01612840802694445.
- Newman D, O’Reilly P, Lee SH, Kennedy C. Mental health service users’ experiences of mental health care: an integrative literature review. J Psychiatr Ment Health Nurs 2015;22:171-82. https://doi.org/10.1111/jpm.12202.
- Omer S, Priebe S. Continuity across inpatient and outpatient mental health care or specialisation of teams? A systematic review. Eur Psychiatry 2015;30:258-7. https://doi.org/10.1016/j.eurpsy.2014.08.002.
- Sequeira H, Halstead S. Restraint and seclusion: service user views. J Adult Protection 2002;4:15-24. https://doi.org/10.1108/14668203200200003.
- Strout TD. Perspectives on the experience of being physically restrained: an integrative review of the qualitative literature. Int J Ment Health Nurs 2010;19:416-27. https://doi.org/10.1111/j.1447-0349.2010.00694.x.
- Sturrock A. Restraint in inpatient areas: the experiences of service users. Ment Health Pract 2010;14:22-6. https://doi.org/10.7748/mhp2010.11.14.3.22.c8071.
- Van der Merwe M, Bowers L, Jones J, Simpson A, Haglund K. Locked doors in acute inpatient psychiatry: a literature review. J Psychiatr Ment Health Nurs 2009;16:293-9. https://doi.org/10.1111/j.1365-2850.2008.01378.x.
- Van Der Merwe M, Muir-Cochrane E, Jones J, Tziggili M, Bowers L. Improving seclusion practice: implications of a review of staff and patient views. J Psychiatr Ment Health Nurs 2013;20:203-15. https://doi.org/10.1111/j.1365-2850.2012.01903.x.
- Borge L, Hummelvoll JK. Patients’ experience of learning and gaining personal knowledge during a stay at a mental hospital. J Psychiatr Ment Health Nurs 2008;15:365-73. https://doi.org/10.1111/j.1365-2850.2007.01237.x.
- Cleary M, Horsfall J, Hunt GE. Consumer feedback on nursing care and discharge planning. J Adv Nurs 2003;42:269-77. https://doi.org/10.1046/j.1365-2648.2003.02616.x.
- Giacco D, Fiorillo A, Del Vecchio V, Kallert T, Onchev G, Raboch J, et al. Caregivers’ appraisals of patients’ involuntary hospital treatment: European multicentre study. Br J Psychiatry 2012;201:486-91. https://doi.org/10.1192/bjp.bp.112.112813.
- Olusina AK, Ohaeri JU, Olatawura MO. Patient and staff satisfaction with the quality of in-patient psychiatric care in a Nigerian general hospital. Soc Psychiatry Psychiatr Epidemiol 2002;37:283-8. https://doi.org/10.1007/s00127-002-0548-5.
- Shattell M, Melanie Andes M, Thomas S. How patients and nurses experience the acute care psychiatric environment. Nurs Inq 2008;15:242-50. https://doi.org/10.1111/j.1440-1800.2008.00397.x.
- Smith D, Roche E, O’Loughlin K, Brennan D, Madigan K, Lyne J, et al. Satisfaction with services following voluntary and involuntary admission. J Ment Health 2014;23:38-45. https://doi.org/10.3109/09638237.2013.841864.
- Sorgaard KW. Satisfaction and coercion among voluntary, persuaded/pressured and committed patients in acute psychiatric treatment. Scand J Caring Sci 2007;21:214-9. https://doi.org/10.1111/j.1471-6712.2007.00458.x.
- Strauss JL, Zervakis JB, Stechuchak KM, Olsen MK, Swanson J, Swartz MS, et al. Adverse impact of coercive treatments on psychiatric inpatients’ satisfaction with care. Community Ment Health J 2013;49:457-65. https://doi.org/10.1007/s10597-012-9539-5.
- Svindseth MF, Dahl AA, Hatling T. Patients’ experience of humiliation in the admission process to acute psychiatric wards. Nord J Psychiatry 2007;61:47-53. https://doi.org/10.1080/08039480601129382.
- Great Britain . Freedom of Information Act 2000 2000.
Appendix 1 Research instruments: work package 2 topic guide for NHS staff
Appendix 2 Research instruments: work package 2 questionnaire for NHS staff
Appendix 3 Research instruments: work package 3 topic guide for NHS staff
Appendix 4 Research instruments: work package 3 topic guide for patients/service users
Appendix 5 Research instruments: work package 3 topic guide for carers
Appendix 6 Research instruments: work package 3 interview schedule for NHS ward staff
Appendix 7 Research instruments: work package 3 flash cards for NHS ward staff using direct quotations from interviews for work package 2
Appendix 8 Research instruments: work package 3 interview schedule for NHS corporate staff
Appendix 9 Research instruments: work package 3 flash cards for NHS corporate staff using direct quotations from interviews for work package 2
Appendix 10 Research instruments: work package 3 interview schedule for patients/service users
Appendix 11 Research instruments: work package 3 realist flash cards for patients/service users using direct quotations from work of the patient and public involvement team
Appendix 12 Research instruments: work package 3 interview schedule for carers
Appendix 13 Research instruments: work package 3 realist flash cards for carers using direct quotations from work of the patient and public involvement team
Appendix 14 Analysis: work package 1 supplementary tables and figures
| Results | Search type | Number of hits |
|---|---|---|
| 1 | exp Inpatients/or inpatient*.mp. | 73,820 |
| 2 | service user*.mp. | 2556 |
| 3 | patient/ | 17,869 |
| 4 | exp ‘Commitment of Mentally Ill’/ | 6286 |
| 5 | involuntary.mp. | 10,996 |
| 6 | 1 or 2 or 3 or 4 or 5 | 108,766 |
| 7 | exp Hospitals, Psychiatric/or psychiatric.mp. | 218,311 |
| 8 | psychiatry.mp. or Psychiatry/ | 74,187 |
| 9 | Mental Disorders/ | 139,896 |
| 10 | 7 or 8 or 9 | 341,433 |
| 11 | exp Patient Satisfaction/ | 67,505 |
| 12 | (satisf* or experience*).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] | 930,899 |
| 13 | 11 or 12 | 933,891 |
| 14 | 6 and 10 and 13 | 3204 |
| 15 | limit 14 to yr = ‘2000 -Current’ | 2181 |
| 16 | limit 15 to english language | 1943 |
| Author(s) and date | Focus of review | Number of studies | Years searched | Key findings: headings or themes from findings |
|---|---|---|---|---|
| Binnema (2004)149 | Psychiatric patients and boredom | Not stated, but c.18 | Appears to be 1994–2003 | Boredom is a lack of experience of meaning; many psychiatric patients experience boredom and lack opportunities to experience meaning. This indicates a lack in the therapeutic potential of the hospital environment and a need for change |
| Cutliffe et al. (2015)150 | Evaluations of inpatient mental health-care experiences in six countries | Not stated | Not stated | Convergence and congruence in service user experience evaluations, overall disturbing picture of inpatient mental health care, major disconnect between policy and practice, problems caused by a multitude of variables, can learn from therapeutic relationships |
| Duncan et al. (2010)151 | Cochrane review: shared decision-making interventions for people with mental health conditions | 2 | Up to 2008 | Effects of interventions – clinical outcomes; health service-related outcome: rate of re-admission to hospital. Secondary outcomes – level of consumer involvement in decision-making process; consumer satisfaction with information provided; provider satisfaction; consumer concordance with treatment plan; consultation time |
| Ford et al. (2015)152 | Experience of compulsory treatment and implications for recovery-orientated practice | 5 | 2000 onwards | Views of the justification of compulsory detention; power imbalance; lack of information or choice |
| Gerolamo (2004)153 | Patient outcomes after treatment in acute care psychiatric hospitals and wards | 47 | 1991–2004 | Re-admission, rehospitalisation, recidivism; symptom and function improvement, client satisfaction; suicide and self-injury |
| Hopkins et al. (2009)154 | Responsiveness as the context to understanding patient perceptions of and expectations for inpatient mental health care | 10 | 1998–2008 | Respect for dignity; confidentiality; autonomy; prompt attention; amenities; access to social networks; choice of provider |
| Katsakou and Priebe (2007)155 | Patient experiences of involuntary hospital admission and treatment | 5 | Selected papers are from 2001–3 | Lack of autonomy and not included in decision-making; quality of care and not being cared for; emotional impact of involuntary treatment and feeling devalued; respect and autonomy; being cared for and treatment benefits; being a human being like other people |
| McHale and Felton (2010)156 | Factors affecting attitudes towards self-harm | 19 | Papers from 1998–2009 | Lacking education/training; role expectations and clinical culture; perception of health needs; knowledge of self-harm; education and training use; dissatisfaction with care |
| Maatta (2009)157 (only abstract available) | Exploring male and female patients’ experiences of psychiatric hospital care: a critical analysis of the literature | 5 | Not in abstract | Treatment specifically related to women; to keep a façade; and single-sex or mixed ward |
| Newman et al. (2015)158 | Mental health service users’ experience of mental health care | 34 | 2008–12 | Acknowledging a mental health problem and seeking help; building relationships through participation in care; working towards continuity of care |
| Omer and Priebe (2015)159 | Continuity of care vs. specialist systems | 21 | 1985–2013 | Hospitalisation, length of stay, transition of care, and staff and patient views: with regard to patient views, there were more positive reports for continuity of care |
| Sequeira and Halstead (2002)160 | Restraint and seclusion | 23 | 1975–2001 | Client’s experience of seclusion; restraint |
| Strout (2010)161 | Experience of being physically restrained | 12 | 1966–2009 | Negative psychological impact; retraumatisation; perceptions of unethical practices; broken spirit |
| Sturrock (2010)162 | Experiences of restraint in inpatient areas | 5 | 2000 to March 2009 | Distressing; should be debriefed; can lead to potentially abusive situations; engendered fear, anxiety and rage; incidents could be prevented |
| Van Der Merwe et al. (2009)163 | Views on locked doors | 11 | Up to 2008 | Advantages of locked doors; disadvantages of locked doors by patients, by staff; aggressive incidents and the door status; patients’ satisfaction with treatment and the door status; patients’ symptoms and the door status |
| Van Der Merwe et al. (2013)164 | Improving seclusion practice: staff and patient views | 39 | 1960–2006 | Patient and staff perception of seclusion; improvement suggestions |
| Author and date | Country | CASP | Value |
|---|---|---|---|
| Alexander (2006)79 | UK | No relationship described between researcher and participants; limited value |
Quantitative: staff–patient comparisons on WAS and HHPP showed minimal significant differences Qualitative: six patient themes, all negative; no real description of the differences between Lemon and Orange wards; only two wards studied; patients self-selected |
| Anders (2007)126 | HI, USA | Unclear aim; no understanding of the findings; limited value | No data on place of birth or how long patients had lived in Hawaii; substantial differences in those recruited within 48 hours of admission and those not recruited (to do with their state of health at admission); the authors could not define the reasons for the differences in satisfaction of care; part of a larger study |
| Baker (2006)80 | UK | No relationship described between researcher and participants; limited value | Sample is self-selected and from one area of the UK |
| Bennewith (2010)70 | UK | Recruitment strategy and ethics considerations not described; no relationship described between researcher and participants; limited value | Description given to participants of what was meant by coercion, for data collection, was blunt |
| Bonner (2002)81 | UK | Recruitment strategy not described; no relationship described between researcher and participants; limited value | Pilot study; much of the methodological description was missing and only six patients/staff members were interviewed |
| Borge (2008)98 | Norway | No relationship described between researcher and participants; limited value | One institution in Norway |
| Borge and Hummelvoll (2008)165 | Norway | Limited value | One clinic in Norway |
| Bowers (2010)75 | The Netherlands | No relationship described between researcher and participants; limited value | Large study in three UK centres |
| Bramesfeld (2007)63 | Germany | No relationship described between researcher and participants; limited value | Only about patients with complex needs but findings can indicate areas for service development |
| Brunero (2009)130 | Australia | No relationship described between researcher and participants; data not rigorously analysed; limited value | Two wards in one institution in Australia |
| Bowl (2007)82 | UK | Unclear aims and findings; no relationship described between researcher and participants; data not rigorously analysed; limited value | Limited, as it was difficult to find focus group participants and because inpatients were interviewed individually; small groups from one small metropolitan area; interviews not recorded |
| Chien (2005)104 | China | No relationship described between researcher and participants; limited value | Large qualitative sample (n = 38) of a difficult patient population, in one establishment in China (physical restraint not used in all countries) |
| Chorlton (2015)83 | UK | Ethics considerations not described; limited value | IPA; therefore, small sample. Limited value although does raise some issues (e.g. importance of compassion to counteract rejection) |
| Cleary (2003)166 | Australia | No relationship described between researcher and participants; data not rigorously analysed; limited value | Limited, as it was conducted in one hospital in New South Wales and at only one given time. The lowest mean rating in this satisfaction survey was 2.74 and the highest was 3.83 (1 = poor, 5 = excellent) |
| Cleary (2012)127 | Australia | No relationship described between researcher and participants; limited value | One hospital |
| Cleary (2010)121 | Australia | Unclear aims; no relationship described between researcher and participants; data not rigorously analysed; limited value | One hospital but 100 people were surveyed |
| Cutting (2002)84 | UK | Unclear aims and findings; unclear methodology; unclear design; unclear data collection; no relationship described between researcher and participants; data not rigorously analysed; limited value | As it stands, very little robust information about what underpinned the findings |
| Donald (2015)107 | Australia | No relationship described between researcher and participants; limited value | One hospital site |
| Duggins (2006)85 | UK | Recruitment strategy not described; no relationship described between researcher and participants; limited value | One hospital site and little information given on participants; small sample |
| Ejneborn (2015)103 | Sweden | Unclear aims; unclear methodology; unclear study design; unclear recruitment strategy; unclear data collection; no relationship described between researcher and participants; unclear data analysis; uncertain about validity of findings; limited value | Too much uncertainty with data |
| Eytan (2004)119 | Switzerland | Unclear aims; recruitment strategy not described; no relationship described between researcher and participants; limited value | Use of non-validated questionnaire and one hospital site in Switzerland |
| Ezeobele (2014)114 | TX, USA | Limited value | One US hospital site |
| Fenton (2014)86 | UK | Unclear aims; ethics considerations not described; limited value | One UK hospital |
| Georgieva (2012)123 | The Netherlands | No relationship described between researcher and participants; limited value | One Dutch hospital |
| Giacco (2012)167 | Sweden | No relationship described between researcher and participants; ethics considerations not described; large study; limited value | Over eight countries; few patients had caregivers; only 48% of eligible patients participated and 36.9% had a caregiver; relationship was not considered (e.g. how many times visited) |
| Gilburt (2008)87 | UK | Unclear aims; no relationship described between researcher and participants; ethics considerations not described; limited value | Small sample (n = 19) and covered only 10 hospitals so findings are of limited value, as hospitals differ and there is no way of knowing what underpinned the experiences |
| Greenwood (2009)88 | UK | No relationship described between researcher and participants; ethics considerations not described; limited value | Small sample (n = 24) in one psychiatric hospital; use of interpreters |
| Gunasekara (2014)99 | Australia | No relationship described between researcher and participants; ethics considerations not described; data not rigorously analysed; vague findings; limited value | A service evaluation from one psychiatric hospital and limited value owing to small sample and few data |
| Holmes (2004)125 | Canada | Unclear aims; recruitment strategy unclear; ethics considerations not described; limited value | Small sample (n = 6) and a lack of description of aim, recruitment and questions asked |
| Hughes (2009)89 | UK | Recruitment strategy not described; no relationship described between researcher and participants; ethics considerations not described; limited value | Little information on aims, recruitment and analysis |
| Iversen (2011)105 | Norway | Relationship described between researcher and participants unclear; limited value | One hospital and 57 respondents |
| Jones (2008)90 | Wales, UK | Recruitment strategy unclear; relationship described between researcher and participants unclear; limited value | One study site |
| Johansson (2003)102 | Sweden | – | Across a large medical district in southern Sweden |
| Katsakou (2011)68 | UK | No relationship described between researcher and participants; limited value | Sample size for estimating and predicting levels of coercion during hospital treatment was small (58 patients), with limited statistical power to detect significant associations, so negative findings should be interpreted cautiously; limited to two hospitals, but large samples for quantitative and qualitative data |
| Katsakou (2011)69 | UK | – | Large sample of involuntary patients across 22 hospital sites |
| Kauppi (2015)71 | Finland | Limited value | Retrospectively collected data |
| Kennedy (2014)97 | UK | No relationship described between researcher and participants; limited value | One ward in one UK hospital |
| Kontio (2014)72 | Finland | Limited value | Retrospective data; one country (unsure if one hospital) |
| Kontio (2012)73 | Finland | Relationship described between researcher and participants unclear; limited value | Two study sites |
| Kulkarni (2014)128 | Australia | No relationship described between researcher and participants; limited value | One site with new ward for women; statistics very simple means and percentages |
| Labib (2009)91 | UK | No relationship described between researcher and participants; ethics considerations not described; data not rigorously analysed; vague findings; limited value | One hospital |
| Lilja (2008)111 | Norway | Unclear aims; limited value | Small sample from those attending three support groups in the community; retrospective data |
| Lindgren (2015)113 | Sweden | Unclear aims; unclear methodology; unclear data collection; relationship described between researcher and participants unclear; limited value | Ad hoc interviewing; one site |
| Lucas (2006)116 | South Africa | Unclear aims; no description of data analysis; limited value | One hospital |
| Mayers (2010)120 | South Africa | Unclear aims; unclear methodology; unclear recruitment strategy; unclear data collection; no relationship described between researcher and participants; unclear data analysis; limited value | 43 participants; retrospective data; few methodological details given |
| McGuiness (2013)106 | Republic of Ireland | No relationship described between researcher and participants; limited value | |
| Meehan (2000)115 | Australia | Unclear aims; unclear recruitment strategy; ethics considerations not described; limited value | Two hospital sites |
| Milner (2008)92 | UK | Unclear aims; unclear methodology; no relationship described between researcher and participants; unclear data analysis; limited value | Non-validated questionnaires; results based on 39 responses |
| Muir-Cochrane (2013)112 | Australia | Unclear aims; unclear recruitment strategy; no relationship described between researcher and participants; limited value | Background to responders unknown; no demographic information collected; retrospective data |
| Nolan (2011)93 | UK | No relationship described between researcher and participants; no description of data analysis; limited value | One hospital site; lack of analysis details, although did have follow-up interview; 44 interviewees |
| Ntsaba (2007)109 | South Africa | Little description of recruitment strategy; no relationship described between researcher and participants; limited value | One hospital in one country |
| O’Brien (2004)122 | Australia | Little description of recruitment strategy; no relationship described between researcher and participants; little description of data analysis; limited value | Methodology unclear; numbers of patients (and other groups) interviewed not given; one site |
| Olusina (2002)168 | Nigeria | No relationship described between researcher and participants; little description of data analysis; unclear findings; limited value | Limited; one site and cross-sectional, although this is the first teaching hospital in Nigeria and a model of medical practice in the country |
| Ridley (2013)94 | UK | Unclear aims; little description of recruitment strategy; little relationship described between researcher and participants; limited value | Large study in Scotland; four areas and 49 people interviewed |
| Robins (2005)110 | SC, USA | Unclear aims; no relationship described between researcher and participants; little description of data analysis; limited value | Very limited, as small sample (n = 27); retrospective; serious mental illness; female only; one area; methodology not well described |
| Roe (2003)129 | USA | Unclear aims; no relationship described between researcher and participants; ethics considerations not described; little description of data analysis; limited value | Limited, as only one US area, although four hospitals; 43 interviewed; lack of description of methodology |
| Russo (2013)95 | UK | Unclear aims; little description of recruitment strategy; ethics considerations not described; little description of data analysis; limited value | Large sample; many countries; few quotations in view of the large sample so difficult to see how valuable it is |
| Shattel (2008)169 | South-eastern USA | Recruitment strategy not described; no relationship described between researcher and participants; limited value | Limited; 10 patients and one unit |
| Sibitz (2011)100 | Austria | Little description of data analysis; limited value | Limited value as only one hospital site; 15 interviewees; retrospective data |
| Smith (2014)170 | Republic of Ireland | Limited value | Limited to one hospital; large sample |
| Sorgaard (2007)171 | Norway | Little description of recruitment strategy; little description of data collection; no relationship described between researcher and participants; no clear statement of findings; limited value | Limited, as only one hospital; methodology not clearly described |
| Steinert (2013)124 | Germany | Little description of recruitment strategy; ethics considerations not described; limited value | Limited, as only one hospital; retrospective but a follow-up; n = 60 |
| Stenhouse (2013)118 | Scotland, UK | No relationship described between researcher and participants; limited value | Limited; small sample (n = 13); one hospital; retrospective |
| Stewart (2015)76 | UK | Limited value | Of some value; large sample (n = 119) in one hospital |
| Strauss (2013)172 | USA | Little description of data collection; no relationship described between researcher and participants; limited value | Limited; one hospital in the USA; large sample |
| Svindseth (2007)173 | Norway | No relationship described between researcher and participants; limited value | Limited by the low proportions of patients exposed to physical force (14%) and threats (7%), which gave low statistical power to findings and a considerable risk for type II statistical errors; but large sample (n = 102) |
| Thapinta (2004)131 | Thailand | Unclear aims; little description of recruitment strategy; data analysis not described; unclear findings; limited value | Unknown if, had the patients completed the questions independently, the outcomes would have been different. Given the public facility is the only hospital available to most patients, these patients may not be accurately reporting their experiences; limited, as methodology was unclear |
| Thibeault (2010)101 | Canada | Limited value | Limited, as only six participants in one hospital |
| Thomas (2002)108 | USA | Unclear aims; little description of recruitment strategy; no relationship described between researcher and participants; limited value | Limited: unsure of data, as four patients were recruited to a different study and a further four were recruited to this study – seems data were aggregated but no description |
| Whittington (2009)74 | UK | No relationship described between researcher and participants; limited value | 136 wards surveyed across UK; results limited by the questionnaire, as it did not allow for descriptions of preferences or experiences because it was simply numerical |
| Wyder (2015)78 | Australia | No aims; no relationship described between researcher and participants; limited value | ‘[W]e did not check with health-care professionals or their files if these events really happened. Thus, it is possible that some events did not occur in the way they were described’; limited value, as no clear aims; 25 interviewed but one hospital in Australia |
| Wyder (2015)77 | Australia | Unclear aims; no relationship described between researcher and participants; ethics considerations not described; limited value | Limited for same reason as given in row above: same data, different perspective |
Appendix 15 Work package 3 total wards in case study trusts: overview diagram
Figure 11 displays the recruitment across eligible wards in the NHS case sites selected; at least one participant was drawn from each eligible ward in the trust to ensure that the whole case site was explored for variance in practice to inform the realist evaluation (WP3).
FIGURE 11.
Overview diagram of the total wards in case study trusts in WP3. a, Patients and staff were recruited from every eligible ward. In addition, at three sites, staff involved in patient experience work in other units were also interviewed. We did this to gain a fuller understand of the complexity of the setting, including variation in processes relating to collection and use of patient experience data between wards.
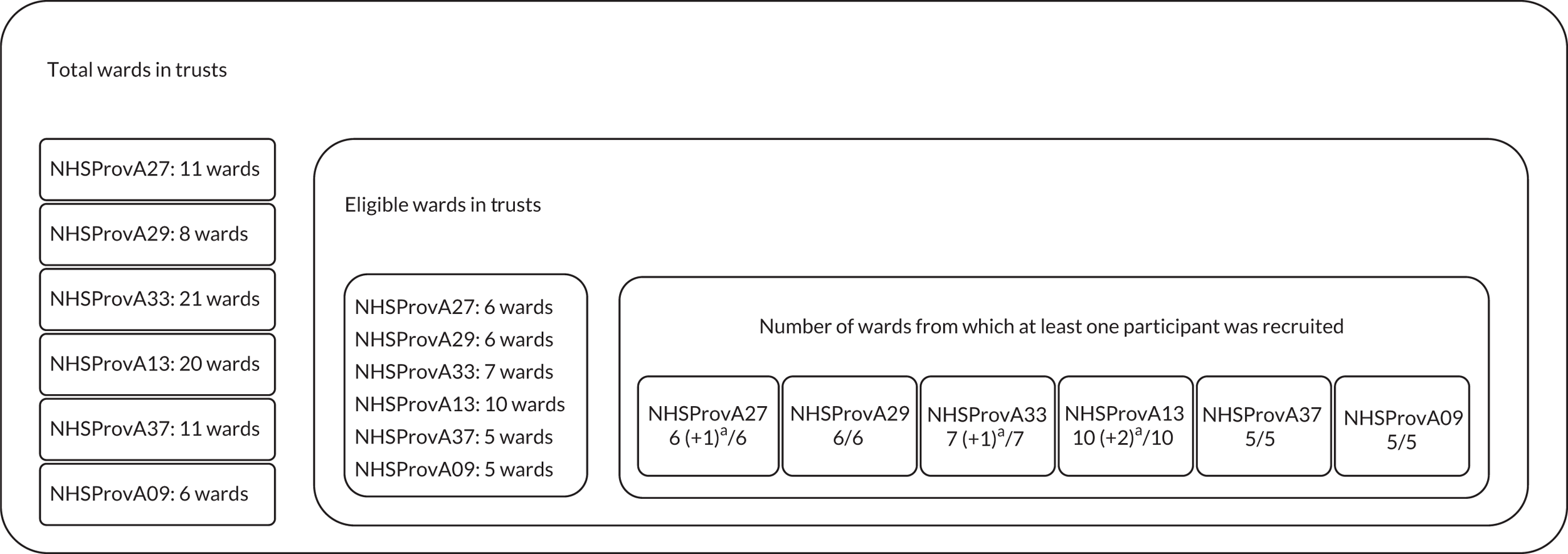
Appendix 16 Analysis: work package 3 supplementary context–mechanism–outcome configuration tables for each stage in the patient experience feedback process
The CMOs presented in this appendix are based on the CRAICh analysis that can be seen in the Excel CMO tables available as an additional online resource, in which the data on which each CMO is based can be seen. From the Excel spreadsheet (see Report Supplementary Materials 5–9), the text of each CMO has been edited for clarity and based on the further analysis undertaken as regard to what is considered context, what is considered a mechanism and what is considered an outcome. The CMOs presented as examples in the report have been further refined.
| Theme | Participants | Context | Mechanism | Outcome | CMO reference codes | |
|---|---|---|---|---|---|---|
| Reasoning | Resources | |||||
| Wellness | Service user | Community meetings held on wards | In some trusts, patients are reluctant or not allowed to raise personal issues in the community meetings. This discouragement to share leads to patients feeling uncomfortable and disempowered and feeling comfortable to share only those experiences related to the ward environment. It leaves them with no space to talk about their experience. Community meetings are often poorly attended; however, some patients value collective meeting forums so that they are ‘not the one that’s moaning’. The need for patients to appear collectively engaged links to the CMO relating to the ‘us vs. them’ culture that develops on some wards. Community meetings often stop happening if wards are unsettled or if there are staff/resourcing issues. This means that patients cannot rely on them as a place to give feedback. The inconsistent approach to community meetings means that patients become ambivalent about attending them, so they cease to be a safe space to raise even environmental concerns. Community meetings are often highly controlled by staff. Potentially contentious or difficult issues are avoided. Patients do not understand the point of them other than to discuss the environmental features of the ward or to praise the staff | Staff skill in managing community meetings. When this is lacking, the meetings can be highly controlled or manipulated by staff | In community meetings, patients do not talk about their experience unless it is not personal or unless it relates to the ward environment. When patient experience staff are controlling or manipulating community meetings, patients may disengage from giving feedback on their experiences in other situations [see CMO on genuine feedback (see Table 20) and CMO on listening (Table 20)] | CMOC1, CMOC2, CMOC111, CMOC112, CMOC116, CMOC140, CMOC141, CMOC386, CMOC498, CMOC499, CMOC513, CMOC546, CMOC547, CMOC593, CMOC600, CMOC631, CMOC638, CMOC656, CMOC676, CMOC677, CMOC690, CMOC710, CMOC722, CMOC737, CMOC764, CMOC780 |
| Ward/review meetings, at which multiple professionals gather around the patient, can be intimidating and confusing when patients are unwell | When a patient is unwell, the pace of information delivered can be confusing and so patients often report either not feeling able to or forgetting to raise the important questions or give the feedback that they wanted to at the ward/review meeting. This is because they feel confused, intimidated, patronised or not listened to. Often, after the meetings, patients will have questions or want to try and make sense of things but they will be either told or feel that their opportunity has passed, leaving them with unresolved anxieties about their care. If the ward is very busy, short staffed or unsettled, it can be difficult to get staff to attend the ward/review meeting, so patients feel that their needs are not being met/they are not valued, which disinclines them to use ward/review meetings to give patient experience feedback | Staff need time for one-to-one conversations and to attend ward/review meetings | Patients do not feel that they give adequate or honest feedback inward/review meetings | CMOC122, CMOC124, CMOC177, CMOC199, CMOC236, CMOC354, CMOC434, CMOC473, CMOC474, CMOC476, CMOC582, CMOC595, CMOC610, CMOC613, CMOC640 | ||
| Patients who are admitted voluntarily often find being admitted less stressful than those who are involuntarily detained | Experiencing involuntary admission is such a disempowering experience that patients find it difficult to share honest feedback about their patient experience. This is in part due to their wellness on admission, but trust is damaged during the admission process, making it more difficult for patients to open up to give feedback. Patients who have been voluntarily admitted but whose only other choice was to be involuntarily admitted (so they lacked a real choice) respond in similar ways to those who have been involuntarily admitted | Patients are admitted involuntarily | Patients who are involuntarily admitted do not find it easy to give honest feedback about their inpatient experience. They might comment on the ward environment | CMOC11, CMOC182, CMOC375, CMOC566,CMOC668 | ||
| When they are unwell, patients do not understand the formal pathways to feedback; in particular, they do not understand the complaints or other legal processes related to their care | Patients can feel confused and isolated when admitted and often associate giving feedback with complaints and other formal processes. This means that they are initially less likely to give feedback. The processes are experienced as intimidating and seem difficult for individuals to understand and follow when they are feeling unwell. Information is often not presented in helpful ways to patients or relies on them knowing that a way of giving feedback exists, where to look or how to access the method of giving feedback (e.g. a form). Patients do not find it easy to give feedback if they are unwell |
Lack of understanding of how confusing formal feedback processes can be Insufficient resource for or attention paid to obtaining patients’ experiences |
Patients do not engage in feeding their experience back through formal processes when they are feeling unwell | CMOC6, CMOC38, CMOC58, CMOC122, CMOC161, CMOC198, CMOC205, CMCO264, CMOC282, CMOC283, CMOC284, CMOC289, CMOC338, CMOC340, CMOC341, CMOC342 CMOC351, CMOC385, CMOC418, CMOC426, CMOC430, CMOC476, CMOC477, CMOC491, CMOC517 | ||
| Patients who are unwell can find it difficult to independently approach staff members to communicate with them about their experiences. This is particularly the case when patients are first admitted to the ward | Patients can feel confused and unsure about who to approach and do not have the confidence to speak to people. They may be experiencing feelings of paranoia or have difficulty trusting people. Patients want people to take the time to speak to them individually and build a rapport with them to facilitate them opening up and feeling comfortable to share their experience. Some patients felt that they needed this to be ‘structured’. Patients wanted consistent or reliable communication experiences, as they considered this more caring than being asked if they were OK in passing. They needed to feel that the staff had taken the time to get to know them and cared about the answers they were giving. No matter how well they feel, patients can offer feedback on their experience. Obtaining their views is important, as, by making time to speak to them when they are feeling very unwell, staff can stop them ruminating and prevent escalation of small issues that could have been resolved earlier. Patients report that an environment in which there is lots of unoccupied time is one in which smaller things become magnified. Quieter patients feel that their need for communication and to give feedback gets overlooked compared with that of others who may be more aggressive, demanding or vocal | Staff making time to build a rapport through speaking to patients individually | Patients are less likely to independently approach staff to give feedback when they are not feeling well | CMOC13, CMO14, CMO15, CMO18, CMOC19, CMOC23, CMOC24, CMOC32, CMOC43, CMOC64, CMOC120, CMOC133, CMOC134, CMOC154, CMOC203, CMOC239, CMOC240, CMOC248, CMOC265, CMOC266, CMOC272, CMOC273, CMOC74, CMOC299, CMOC320, CMOC322, CMOC323, CMOC350, CMOC358, CMOC361, CMOC390, CMOC392, CMOC393, CMOC413, CMOC438, CMOC450, CMOC460, CMOC461, CMOC465, CMOC479, CMOC480, CMOC487, CMOC509, CMOC510, CMOC517, CMOC526, CMOC527, CMOC544, CMOC604, CMOC609, CMOC624, CMOC629, CMOC630, CMOC648, CMOC721, CMOC752, CMOC756, CMOC759 | ||
| When patients are experiencing difficulties with visual or auditory hallucinations or are unwell with other symptoms, communicating their experience in a way that they feel that staff respond and listen to in order to explain what it is that is bothering them can be difficult | Patients feel that staff discount or do not listen to what they are saying if they try and communicate their experience while experiencing auditory or visual hallucinations. Patients also report being discouraged from sharing what their experience is owing to these symptoms, which means that they do not or are not able to communicate their experiences or concerns to staff (i.e. about their medication). This lack of engagement makes patients feel isolated and unsupported and it makes them conform to a normalised pattern of behaviour in order to comply with the informal rules of the ward so that they may be discharged, rather than necessarily making them feel better or well. Patients are then likely to be dishonest when giving feedback as a result of this conditioned behaviour around communicating certain types of experience or distress. Often, patients will have concerns about leaving the unit or things will be worrying them from outside the unit and these concerns (as they are now in and of the unit) are also things that they do not feel that they can share or they are discouraged from talking about. This leaves patients who are quite confused negotiating a complex set of informal rules about what is able to be discussed and about what staff are receptive to and what they are not receptive to. This creates further anxiety and ultimately results in patients sharing less about their experience or limiting the information they share with staff. They develop placatory behaviours, giving staff only feedback that they feel is acceptable to staff | Staff do not encourage patients to share experiences. They actively discourage them if patients are communicating their concerns while also discussing their auditory or visual hallucinations. Staff do shut down these conversations | Patients do not feel that they can explain or raise their concerns about their experiences and so do not engage in giving honest feedback | CMOC45, CMOC46, CMOC47, CMOC48, CMOC49, CMOC52, CMOC53, CMOC60, CMOC67, CMOC107, CMOC108, CMOC110, CMOC232, CMOC233, CMOC234, CMOC338, CMOC339, CMOC343, CMOC348, CMOC358, CMOC368, CMOC369, CMOC407, CMOC413, CMOC429, CMOC450, CMOC517, CMOC525, CMOC526, CMOC567, CMOC568, CMOC569, CMOC740, CMOC779, CMOC781 | ||
| Complaints or concerns are dismissed because patients are ‘unwell’. Patients feel that they are deliberately not asked for feedback because they are unwell | When patients have experience of complaining or raising concerns and these are refuted, dismissed or not accepted, and the reason given for this is the patient’s wellness, this is disempowering and disincentivises patients from engaging in giving honest feedback about their experience to staff in future | Patients who feel disempowered in the inpatient setting can be supported to make sense of and to feed back their own experience independently. Having their views listened to is empowering | Patients disengage from giving feedback to staff | CMOC149, CMOC348, CMOC548, CMOC549, CMOC603, CMOC744 | ||
| When patients are unwell, they sometimes need carers or family members to advocate for them, as they are confused and unable to make decisions. They need carers or family members to help plan their care with staff | Patients felt disempowered, as they were not capable of independence within the inpatient setting, despite also feeling grateful for the support from carers or family members. Patients being able to independently make sense of and give feedback on their own experience and to have their views listened to is important, as it is empowering. Among the patients interviewed for this study, these were often younger patients or patients who have long-term carers, for example patients with learning disabilities | Patients who feel disempowered but are supported to provide feedback on their experience of care are able to do so and find the process empowering | Providing feedback on experience of care can be empowering | CMOC235, CMOC382, CMOC492, CMOC598, CMOC663, CMOC704, CMOC787 | ||
| Formal feedback is very seldom invited from inpatients. Patients have to be proactive to make an opportunity to give feedback. People’s experience of the inpatient setting changes over the time that they are in the ward and so their experience of the ward and their reflections on it are likely to change during the admission | On their first-ever admission, patients can find it a daunting experience and take a while to adjust to being in an inpatient setting. Patients, when first admitted, may not trust the environment or the staff; therefore, giving honest feedback may not be possible until rapport has been established. Patients who have had prior admissions adjust more quickly. When patients are admitted to the ward initially (irrespective of prior admission), they report that they are confused and unlikely to be able to give feedback about the ward or the process of admission at that point. Patients note being able to talk about themselves all of the time, but not feeling well enough when first admitted to be able to offer reflections on the ward environment. Getting early feedback allows staff to identify issues such as bullying so they can be addressed. Around the mid-point of their admission, patients have some experience of the environment and are well enough to offer some reflections on this. At the point of discharge, patients may be more likely to raise concerns without fearing that it will have an impact on their ongoing care |
Recognition that obtaining patient feedback is difficult Staff can be proactive in seeking patient feedback Staff can reassure patients that any feedback they give will not have an impact on their discharge or care quality Collect feedback from patients at different times during their ward stay. A ‘good time’ for collecting feedback might vary between patients depending on how ill they are and how they feel about their admission Staff can establish trusting relationships in order to collect feedback from patients Management need to demonstrate to patients that they take notice of and act on feedback |
On their first-ever admission, patients may give less feedback than those who have had prior admissions. Early in an admission, patients can talk about their current experience. At around the mid-point of admission, patients can give reflective feedback about their patient experience. Feedback from patients near the time of discharge is likely to be more honest than feedback given at other times. Patients ready for discharge may tick boxes quickly without reflection | CMOC100, CMOC102, CMOC157, CMOC173, CMOC186, CMOC187, CMOC210, CMOC213, CMOC217, CMOC218, CMOC219, CMOC220, CMOC224, CMOC227, CMOC229, CMOC230, CMOC231, CMOC232, CMOC249, CMCO256, CMOC257, CMOC258, CMOC266, CMOC276, CMOC279, CMOC280, CMOC281, CMOC282, CMOC288, CMOC292, CMOC294, CMOC316, CMOC353, CMOC358, CMOC370, CMOC371, CMOC372, CMOC374, CMOC375, CMOC376, CMOC395, CMCO397, CMOC398, CMOC399, CMOC430, CMOC432, CMOC433, CMOC435, CMOC439, CMOC441, CMOC445, CMOC463, CMOC464, CMOC483, CMOC484, CMOC508, CMOC514, CMOC515, CMOC528, CMOC529, CMOC530, CMOC531, CMOC536, CMOC538, CMOC542, CMOC543, CMOC552, CMOC560, CMOC561, CMOC574, CMOC605, CMOC625, CMOC653, CMOC661, CMOC675, CMOC679, CMOC680, CMOC688, CMOC698, CMOC699, CMOC700, CMOC702, CMOC703, CMOC712, CMOC715, CMOC716, CMOC717, CMOC718, CMOC740, CMOC753, CMOC762, CMOC763, CMOC771, CMOC772, CMOC773, CMOC777, CMOC785 | ||
| Clinical staff | Staff perceive that it is more difficult to get feedback in inpatient settings than in other care settings owing to the patients being unwell. Staff do not believe you can get patient experience feedback from individuals when they are unwell, as patients are confused, experiencing auditory or visual hallucinations, or struggling to make sense of their surroundings. Staff report increasing numbers of very unwell patients. Staff feel that they are discharging patients much earlier than they used to because of the bed pressures. Some patients are discharged before they are ready to leave | Staff, at times, feel that patients may exaggerate or be confused, as they are unwell. It makes listening to concerns difficult, as they need to determine proportionate responses. When patients do not have a good experience but do not explain why, staff can attribute this to their being unwell. With increasing numbers of very unwell patients, staff have to make more effort to obtain patient experience feedback. Staff may feel that patients are not well enough to give feedback during their stay, almost right up to discharge. At discharge, the staff member may not want to ask for feedback from a patient who does not feel that they are ready to leave. Staff view much of the feedback received from patients as arising from tick-box surveys on discharge. They do not value this as they do not feel that it is truthful. Staff are aware that patients are not always honest with them when offering feedback. This is particularly the case when they may wish to appear better so that they will be granted leave from the ward or because they want to go home | Staff can assess a patient’s wellness while also hearing their feedback | Staff do not always take on board feedback if they think that the patient is being dishonest with them. Staff do not seek feedback from patients when they think that patients are too unwell | CMOC918, CMOC920, CMOC944, CMOC963, CMOC968, CMOC969, CMOC975, CMOC991, CMOC993, CMOC1002, CMOC1005, CMOC1010, CMOC1014, CMOC1015, CMOC1021, CMOC1022, CMOC1024, CMOC1030, CMOC1036, CMOC1043, CMCO1044, CMOC1045, CMOC1054, CMOC1066, CMOC1067, CMOC1069, CMOC1071, CMOC1085, CMOC1087, CMOC1111, CMOC1113, CMOC1138, CMOC1143, CMOC1154, CMCO1161, CMOC1171, CMOC1182, CMOC1185, CMOC1189, CMOC1190, CMOC1211, CMOC1216, CMOC1231, CMOC1240, CMOC1244, CMOC1245, CMOC1248, CMOC1250, CMCO1254, CMCO1255, CMOC1273, CMOC1279, CMOC1280, CMOC1283, CMOC1284, CMOC1291, CMOC1292, CMOC1293, CMOC1294, CMOC1296, CMOC1300, CMOC1303, CMOC1307, CMOC1308, CMOC1310, CMOC1311, CMOC1321, CMOC1330, CMOC1331, CMOC1337, CMOC1338, CMOC1341, CMOC1345, CMOC1347, CMOC1350, CMOC1353, CMOC1354, CMOC1355, CMOC1356, CMOC1365, CMOC1396, CMOC1397, CMOC1399, CMOC1401, CMCO1405, CMOC1407, CMOC1425, CMOC1442, CMOC1447, CMOC1448 | |
| Importance of feedback/seeing changes | Service user | Patients do/do not feel listened to. Patients are/are not given explanations or reasons for change not happening. Patients do/do not see staff making changes or patients see that staff are unable to make changes in response to patient experience feedback | Patients detect apathy from the staff about making changes. This is experienced as frustrating and disincentivises patients from giving patient experience feedback. Patients do not feel that staff listen to their requests and lose trust in staff members. Trust enables patients to give honest patient experience feedback (see rapport CMO). Being ‘allowed to talk’ – which involves someone being open and receptive to whatever a patient is trying to communicate – is an important part of listening that then leads to patients feeling heard and supported. Staff being approachable and friendly is an important aspect of whether or not patients feel that they are likely to be listened to. If patients feel listened to, they are more likely to give their feedback. When patients do not see changes being made in response to feedback, it can be difficult for them to raise the issues again. Patients want to know that their feedback is going to be used. This relates to feelings of being disempowered. Although some patients reported that they could give feedback, many believe that their feedback will be ignored or ‘put in the bin’. This disincentivises them from giving feedback through formal routes or at all. When patients see change being made in response to their feedback, they are more likely to talk to staff and give feedback |
Staff being/not being approachable and friendly and listening/not listening to patients Staff able to/not able to make changes in response to patient experience feedback |
Patients are more likely to give feedback if they are listened to and can see changes being made in response to that feedback. Patients are less likely to give feedback if they are not listened to and cannot see changes being made in response to that feedback | CMOC26, CMOC32, CMOC33, CMOC34, CMOC47, CMOC83, CMOC84, CMOC98, CMOC99, CMOC112, CMOC113, CMOC114, CMOC115, CMOC140, CMOC141, CMOC142, CMOC148, CMOC170, CMOC172, CMOC183, CMOC216, CMOC277, CMOC285, CMOC287, CMOC299, CMOC317, CMOC318, CMOC327, CMOC328, CMOC332, CMOC334, CMOC336, CMOC352, CMOC354, CMOC360, CMOC377, CMOC378, CMOC384, CMOC396, CMOC420, CMOC440, CMOC441, CMOC457, CMOC512, CMOC617, CMOC618, CMOC619, CMOC620, CMOC623, CMOC632, CMOC641, CMOC673, CMOC674, CMOC677, CMOC746 |
| Shorter admission period for patients | When patients experience multiple short admissions or the admission time is shortened, they sometimes cannot see the point of giving feedback on the inpatient setting, as they do not believe that they are going to be in the setting long enough to see any changes; therefore, they lack the motivation to give feedback. Patients are more likely to tolerate discomfort or unhappiness if they feel that they are going to be an inpatient for only a short time. Shorter lengths of stay lead to mechanisms that affect patients’ motivation to give feedback |
Patients being on shortened admissions Staff not collecting feedback explicitly |
Patients on shorter admissions are less likely to give feedback, as they do not feel that they will see any changes from their feedback | CMOC88, CMOC562 | ||
| Patients are often motivated to give feedback to support changes being made to NHS mental health services both for other people and to improve services for any potential future admissions. Some patients want to give feedback to thank staff for their care. Giving positive feedback is important to patients | Patients are hopeful that the quality of services will improve and they want to be part of this process. There is a reciprocity in giving positive feedback related to receiving care when they are unwell. It is empowering for patients to be able to give feedback and to feel that this has been received and will be responded to | Staff receive and respond to patient experience feedback | Patients give feedback that is received and responded to by staff and used to improve the quality of inpatient mental health provision | CMOC150, CMOC304, CMOC388, CMOC402, CMOC448, CMOC519, CMOC540, CMOC572, CMOC628, CMOC701, CMOC723, CMOC789 | ||
| Feedback forms ask for overall rankings of patient experience. Patients do not see changes made in response to formal feedback mechanisms (i.e. surveys or forms). Patients do see changes being made in response to informal feedback given at the ward level | Patients report that formal feedback mechanisms are difficult to understand and use – they are ‘clunky’ or ‘cumbersome’. Patients find formal feedback forms difficult to complete, particularly when they are unwell. Formal feedback routes do not give patients the opportunity to express themselves in the level of detail that they want. Being asked to give an overall ranking, as opposed to being able to disaggregate between staff members, upsets some patients who then struggle to fill out the form. Being asked to give an overall grade for experience when there may have been one very bad incident but overall they were happy with their care is confusing. Patients see changes made at the ward level that are related to feedback that is given during ward meetings (see changes are made CMO in Table 20) rather than through formal mechanisms of patient experience data collection (e.g. surveys). Patients are motivated to give feedback to improve services, but they are less motivated to engage with formal feedback, as they do not see how it links to improvements. Patients are motivated to give feedback to improve services (see motivation CMO in Table 23). Formal anonymous feedback is seen as driving larger-scale changes, whereas locally given feedback is seen as being responded to more immediately | Staff and patients do not get feedback on the results of formally collected patient experience data | Patients do not see the point in completing formal feedback (e.g. forms), as they do not know what happens to it and change does not follow as a result of its being collected | CMOC148, CMOC151, CMCO152, CMOC153, CMOC162, CMOC220, CMOC400, CMOC401, CMOC406, CMOC462, CMOC486, CMOC490, CMOC500, CMOC501, CMOC503, CMOC520, CMOC524, CMOC528, CMOC571, CMOC608 | ||
| Carer | Carers raise issues with staff about patient experience | Carers feel better about the safety of the person they care for and feel less anxious if they receive a response to or see changes as a result of the issues they raise with ward staff. This also helps them to feel more engaged in their friend or family member’s care | Staff give carers feedback about changes made in response to carers raising concerns | Carers engage in giving feedback and feel more included in the care of the patient they care for | CMOC856, CMOC886, CMOC902 | |
| Clinical staff | Positive feedback is mostly given verbally, in person. Staff do not recognise this as formal feedback. Negative feedback is formal and responded to in a timely manner | Staff note that they do not receive positive feedback as often as negative feedback. Positive feedback is rarely used or acted on and is often disregarded. The only purpose of positive feedback recognised by staff is that it boosts individual staff members’ morale. The volume of negative feedback and the serious way in which the organisation responds to it means that staff respond and internalise negative feedback far more than positive feedback and they use this to shape and change their practice. Staff can be fearful of negative feedback because of the way in which it is managed or handled in the organisation at an individual level. Consequently, staff will avoid getting negative feedback wherever possible. This can lead to staff not seeking feedback. Staff perceive that negative feedback is more likely to be responded to than any other feedback. Staff believe that negative feedback is more useful. Staff perceive that negative feedback needs to be acted on quickly and responded to in order to avoid complaints. Staff feel that this creates a culture whereby the patients who ‘shout loudest’ get more attention. Complaints and serious incidents take up the majority of time in relation to patient experience work for corporate/ward management staff. One of the important functions of informal feedback is that there may be more honest feedback given in this way, as people may fear that formal feedback will affect their clinical care. Feedback that is given directly to staff tends to be more critical than the positive feedback recorded formally. Some trusts find that negative feedback is left online |
Staff do not receive positive feedback often and, when they do, this is often perceived as informal and disregarded Staff perceive that the organisation cares only about negative feedback and complaints |
Positive feedback is rarely received by individual staff members and is not passed on or formalised in order to make or sustain changes in services. Staff respond to negative feedback swiftly | CMOC921, CMOC923, CMOC924, CMOC925, CMOC926, CMOC929, CMOC941, CMOC946, CMOC947, CMOC957, CMOC958, CMOC965, CMOC984, CMOC985, CMOC996, CMOC1000, CMOC1001, CMOC1008, CMCO1009, CMOC1016, CMOC1017, CMOC1018, CMOC1050, CMOC1060, CMOC1061, CMOC1062, CMOC1068, CMOC1092, CMOC1093, CMOC1094, CMOC1100, CMOC1110, CMOC1112, CMOC1139, CMOC1140, CMOC1142, CMOC1145, CMOC1150, CMOC1151, CMOC1152, CMOC1153, CMOC1162, CMOC1172, CMOC1174, CMOC1179, CMOC1180, CMOC1187, CMOC1188, CMOC1197, CMOC1198, CMOC1207, CMOC1208, CMOC1209, CMOC1210, CMOC1213, CMOC1220, CMOC1221, CMOC1226, CMOC1228, CMOC1237, CMOC1242, CMOC1246, CMOC1247, CMOC1252, CMOC1266, CMOC1272, CMOC1278, CMOC1282, CMOC1297, CMOC1298, CMOC1309, CMOC1323, CMOC1348, CMOC1349, CMOC1351, CMOC1352, CMOC1360, CMOC1363, CMOC1364, CMOC1370, CMOC1371, CMOC1372, CMOC1373, CMOC1374, CMOC1376, CMOC1418, CMOC1422, CMOC1427 | |
| The use of feedback forms or other formal data collection tools is not sustained and happens sporadically in line with organisational pressure or at a single time point (i.e. on discharge). Collecting patient experience feedback is not always an everyday part of business | Formal feedback forms go through phases of being introduced and used in line with corporate pressure; however, the use of these is not sustained. The collection of formal feedback is often poorly implemented without support or resources in place to help people make time to collect the data. Collection is slightly easier when there are electronic data systems in place, as feedback can be received by wards in a more timely manner. Staff are motivated to get patients well and to get them home and, in cases in which feedback is not available, they use this as a proxy measure of how well the ward is doing or assume that this feedback is sufficient. The lack of visibility of the results of formal patient feedback demotivates staff in relation to regularly collecting feedback. This results in forms or feedback mechanisms being abandoned or staff being of the opinion that they ‘collect it because we have to’. When there is staff buy-in through staff being able to see the results and use them, staff are more likely to collect patient feedback. Staff often rely on patients completing feedback forms themselves and do not see it as part of their role to collect this feedback. When it becomes a routine but meaningless part of target-driven core business with limited useful analysis reaching ward staff, the collection of patient experience feedback loses its purpose for the staff. This disincentivises staff from collecting the feedback, other than to meet seemingly arbitrary targets. Staff feel that patient experience measures do not capture ‘compassion and treatment’ but instead capture ‘risk assessments and discharge, and medication’. They feel that the emphasis/values are wrong | Staff do not keep up the use of formal feedback tools if they do not receive any feedback on the results from these tools. When feedback on results is received, there is staff buy-in, so patient feedback is collected | Feedback is not routinely collected from patients in environments in which staff cannot see the results of the data | CMOC888, CMOC931, CMOC932, CMOC934, CMOC936. CMOC937, CMOC945, CMOC953, CMOC960, CMOC961, CMOC962, CMOC964, CMOC966, CMOC982, CMOC997, CMOC999, CMOC1000, CMOC1004, CMOC1025, CMOC1026, CMOC1027, CMOC1028, CMOC1029, CMOC1048, CMOC1063, CMOC1070, CMOC1072, CMOC1080, CMOC1082, CMOC1083, CMOC1099, CMOC1107, CMOC1108, CMOC1118, CMOC1119, CMOC1120, CMOC1133, CMOC1146, CMOC1147, CMOC1148, CMOC1149, CMOC1159, CMOC1160, CMOC1163, CMOC1165, CMOC1167, CMOC1169, CMOC1183, CMOC1195, CMOC1196, CMOC1199, CMOC1205, CMOC1214, CMOC1217, CMOC1230, CMOC1233, CMOC1235, CMOC1258, CMOC1262, CMOC1265, CMOC1289, CMOC1302, CMOC1306, CMOC1316, CMOC1317, CMOC1318, CMOC1319, CMOC1359, CMOC1387, CMOC1395, CMCO1412, CMOC1421, CMOC1423 | ||
| It is difficult to get changes made to how care is delivered and, when change is made, it occurs slowly. Patients may see little or no change, as they come and go more quickly than the time it takes for substantial change to be made. Staff turnover is high so staff may not experience change | Staff at the ward level are sometimes not able to make changes in response to feedback. This means that staff begin to resist collecting or asking for feedback because it is frustrating for both themselves and patients to see no changes. Staff feel that patients being happier is a proxy for the service running well, but are also aware that, for patients who may have to return to the service at a later stage, seeing changes or feeling listened to through feedback being used is important, as it makes them less fearful about returning to the ward. Community meetings are an example of cases in which staff feel that patients become disengaged from giving feedback, because things do not change as a result of feedback. Staff and patients ‘lose heart’ when they see the same comments coming back meeting after meeting and no change being made. Consequently, patients stop attending community meetings. Staff become disengaged from or stop attending community meetings for the same reason. When community meetings work well, informal patient experience feedback can be gleaned; however, this does not form part of patient experience work and so staff often cannot/do not use this to make changes. Staff feel that ‘information flows upwards and outwards’ and that they do not see the feedback or use it | Staff cannot make changes based on patient experience feedback | Patients stop giving feedback and staff stop seeking it | CMOC884, CMOC948, CMOC956, CMOC1031, CMOC1048, CMOC1065, CMOC1073, CMOC1074, CMOC1084, CMOC1105, CMOC1141, CMOC1177, CMOC1215, CMOC1227, CMOC1241, CMOC1246, CMOC1277, CMOC1288, CMOC1322, CMOC1337, CMOC1358, CMOC1361, CMOC1385, CMOC1387, CMOC1394, CMOC1434, CMOC1436, CMOC1449, CMOC1450 | ||
| Environmental factors (e.g. heating and food) are much easier to change than ward culture | Staff are aware that not only are they more likely to collect feedback on environmental factors (see CMO from staff and patients about not obtaining feedback on individual care in community meetings), but also environmental factors are easier to address than cultural factors (i.e. staff vs. patients or bullying on wards). These therefore receive the majority of attention. Using the formal patient experience feedback mechanisms that exist, staff can collect feedback on the ward environment and are able to make changes to the environment. Collecting feedback in this way can feel quite ‘rigid’ to staff. It is usually cultural factors that are the cause of serious incidents or complaints, however (i.e. staff attitudes). Staff feel that they do not have the tools and sometimes avoid collecting other types of feedback. When cultural factors within the organisation make it difficult to change anything other than environmental factors, staff are more likely to talk about barriers to collecting feedback | Staff do not actively collect individual patient experience feedback. Staff ask about and, therefore, receive feedback on ward environment | Changes made on wards based on patient experience feedback are predominantly related to environmental factors | CMOC949, CMOC955, CMOC995, CM1005, CMOC1011, CMOC1178, CMOC1226, CMOC1253, CMOC1357 | ||
| The FFT is often incorporated into ‘tick box’ exit questionnaires. Staff dislike asking patients to complete the FFT, as the questions can be emotive. They do not feel that the FFT is appropriate and they get resistance to it as a measure from patients. Staff do not see it as useful for themselves or the patients. Staff are aware that they are monitored based on FFT feedback | Staff are reluctant to ask patients to complete the FFT, as they cannot defend the rationale for its use. Staff also do not find the ratings system as useful as explanatory feedback, so ward staff find it difficult to explain the point of completing the form to patients. Some patients report to staff that they do not wish to give feedback on their experience after an admission, as they prefer not to think about it again. Faced with the difficult nature of the FFT questions and some patients refusing to answer the questions, staff become reluctant to approach patients for feedback. Staff struggle to advise patients who want to use the form to complain about an individual aspect of care rather than rating their entire stay. How the patient completes the form depends on how its function is perceived. Staff feel that the FFT is not a ‘true reflection’ of patients’ experiences | Staff are reluctant to ask patients to complete the FFT | Patient experience data using the FFT are collected sporadically or when there is a corporate-led push on data collection | CMOC997, CMOC998, CMOC999, CMOC1000, CMOC1115, CMOC1154, CMOC1191, CMOC1212, CMOC1229, CMOC1268, CMOC1269, CMOC1270, CMOC1271, CMOC1274, CMOC1301, CMOC1302, CMOC1316, CMOC1317, CMOC1318, CMOC1320, CMOC1321, CMOC1327, CMOC1339, CMOC1340, CMOC1344, CMOC1359, CMOC1361, CMOC1377, CMOC1378, CMOC1379, CMOC1383, CMOC1388, CMOC1389, CMOC1390, CMOC1391, CMOC1393, CMOC1404, CMOC1406, CMOC1412, CMOC1413, CMOC1415, CMOC1416, CMOC1421, CMOC1431, CMOC1440, CMOC1441, CMOC1444 | ||
| Relationships and communication | Service user | Patients can struggle with communication and with approaching staff when they are not feeling well. People with lived experience of mental illness (including other patients) and non-clinical staff can sometimes communicate in ways that are more accessible to patients | Access to people with lived experience and non-clinical staff enables patients to communicate about their experience more easily. They feel that their communication is better understood. When patients struggle to communicate their thoughts and wishes, they can feel isolated on the ward and they lack agency in relation to their care plan, particularly communicating that their care and treatment plan is not going in a direction that they want | Having people with lived experience/non-clinical staff available to communicate with patients in a language that is accessible to the patients | Patients are more likely to engage in giving patient experience feedback | CMOC8, CMOC9, CMOC10, CMO15, CMOC77, CMOC145, CMOC176, CMOC178, CMOC179, CMOC180, CMOC181, CMOC335, CMOC553 |
| Staff adopt more restrictive practices or the ward is stripped bare of things (i.e. homely, communal items such as board games) as a response to serious incidents on the ward | Restrictive practices or the ward being stripped bare has an impact on the physical day-to-day experience of the patients and on the way patients interact with staff. Patients withdraw from communicating about their needs. There is often little recognition of other patients’ needs for communication about these incidents to help patients move on from them. Practice could change in respect of particular individuals on the ward having high levels of need, which results in other patients feeling that there is nobody available for them to talk to | Staff change their practices to be more restrictive in response to a serious incident on the ward but do not communicate with patients about the incident | Restrictive practices have an impact on patients’ ability or willingness to give feedback. Patients can end up feeling guilty or responsible for incidents and internalise these feelings in ways that affect both their experience and their ability or willingness to give feedback | CMOC16, CMOC17, CMOC25, CMOC56, CMOC57, CMO59, CMOC385, CMOC467, CMOC482, CMOC511, CMOC512, CMOC637 | ||
| Violence, racism, bullying or aggression from other patients on the ward affects the ways in which communication develops. Serious incidents on the ward and the ways in which these are responded to have an impact on patients’ ability to give feedback | When patients are violent on the wards or if they are bullying or aggressive towards staff or other patients, this affects other patients’ experience and changes the way in which they communicate on the wards. If patients feel less safe, they are less able to engage in giving honest feedback and withdraw from doing so. Even long after a violent/racist/bullying or other serious incident has occurred, patients remain wary in the inpatient environment and so additional effort will need to be made by staff to encourage them to talk about their experience. How violent incidents are responded to by staff is important in relation to how comfortable patients feel about talking or sharing information. Patients will not give feedback and fear being ‘snitches’ if the wards are not perceived as safe and there are high levels of violence, bullying or aggression. In the worst cases, doctors or nurses have acknowledged patients’ feelings of safety and risk on the ward and agreed that they may not be able to keep them safe | Staff and patients can struggle to respond when patients are violent on the wards | Patients are more fearful of their environment so their experience is directly affected. Fear of the other patients will make them withdraw and less likely to speak to staff for fear of reprisals from other patients | CMOC50, CMOC51, CMOC130, CMOC131, CMOC132, CMOC191, CMOC192, CMOC193, CMOC197, CMOC237, CMOC258, CMOC259, CMOC260, CMOC261, CMOC262, CMCO266, CMOC281, CMOC329, CMOC347, CMOC348, CMOC364, CMOC365, CMOC366, CMOC367, CMOC385, CMOC409, CMOC410, CMOC422, CMOC423, CMOC428, CMOC457, CMOC458, CMOC459, CMOC466, CMOC467, CMOC494, CMOC495, CMOC554, CMOC564, CMOC565, CMOC590, CMOC633, CMOC634, CMOC635, CMOC648, CMOC659, CMOC681, CMOC682, CMOC685, CMOC686, CMOC692, CMOC693, CMOC729, CMOC730, CMOC731, CMOC761, CMOC764, CMOC765, CMOC775, CMOC776, CMOC790, CMOC792 | ||
| When a patient’s behaviour is disruptive or aggressive or they shout, the patient does not feel that this feedback is tolerated or accepted on the ward | Patients report being ignored if their behaviour is challenging or they shout and, consequently, they learn that this is not a way in which feedback is accepted or will be received by staff. This requires a level of wellness, understanding and an ability to process to then make the decision to adapt their behaviour. Being ignored is internalised quite negatively, with one patient describing how ‘the psychosis I went through is a result of people making me feel like I was a bit, like I was grotesque. And the staff did make me feel like I was slightly more grotesque by being scared of me, by treating me as if I was something that needed to be controlled’. | Staff do not respond to or engage with feedback if it is shouted or aggressively communicated | Patients can experience staff as punitive and, therefore, learn or adapt their behaviour to give feedback in ways that the staff are receptive to | CMOC206, CMOC207, CMOC238, CMOC306, CMOC307 | ||
| When patients trust ward staff and feel safe, they are better able to communicate with them about their experiences. Conversely, when patients do not feel safe, they will not share experiences | When patients develop trust in staff, feel that they will be listened to and feel safe on the ward, they will approach staff to share concerns (i.e. about abuse from other patients) or share their experiences. When wards are violent or there is bullying and aggression, patients will not share their experiences, as they feel intimidated | Staff are trusted by patients and are approachable and open to receiving feedback – this is linked to ward safety and cannot operate independently of the culture/safety on the ward | Patients will communicate their personal or individual experiences or raise concerns with staff when they feel safe. If wards are unsafe, they may raise concerns about others but are less likely to share their feedback of their experience with staff, as they do not feel the ward is a safe place to do so | CMOC97, CMOC105, CMOC106, CMOC129, CMOC130, CMOC131, CMOC132, CMOC144, CMOC159, CMOC160, CMOC168, CMOC171, CMOC183, CMOC184, CMOC358, CMOC380, CMOC387, CMOC388, CMOC393, CMOC411, CMOC412, CMOC459, CMOC570, CMOC778 | ||
| Patients may have had a previous admission or experience of an inpatient mental health setting in which they felt disempowered or not listened to | Some patients have had prior admissions to wards or other units, which has an impact on their experience in the current unit and diminishes their desire or ability to give honest feedback in the new admission. Patients who have previously felt disempowered and, in particular, not listened to regarding former complaints can be hostile to the idea of giving feedback or see it as pointless, as nothing was done in response to their previous complaint or feedback. If staff take the time to address concerns that are raised in relation to previous admissions, patients are more likely to feel motivated to engage in giving honest patient experience feedback about their current admission | Staff listen to issues and concerns raised regarding previous admissions | Patients respond better and engage in giving honest feedback about their current admission | CMOC308, CMOC383, CMOC406, CMOC626 | ||
| Patients are unwell (often with hallucinations), feel insecure and vulnerable, are struggling to make sense of what is happening to them and are often confused about ward systems and staffing | Patients find it difficult to talk to staff members who they do not know and with whom they have not had the opportunity to build a trusting relationship. Staff taking time to understand patients individually builds rapport and trust. This establishes feelings of safety and of being accepted for the patient. A consistency in approach across the staff team allows patients’ anxieties to be contained and establishes rapport. When patients are trying to make sense of their experience, particularly if they have been confused or experienced hallucinations, the familiarity of seeing the same people regularly is important to them, while they continue to process and are reality-testing. Some patients reported trust issues related to historical trauma or abuse that were exacerbated by inconsistent care when they were on the ward | Consistent ward staffing with staff having time to spend getting to know patients and willing to make an effort to get to know patients individually and hear what the patients are trying to tell them. Consistency of approach across the staff team | Patients give feedback; feedback is likely to be honest when a patient has developed a trusting relationship with a staff member and/or the wider team | CMOC20, CMOC42, CMOC47, CMOC54, CMOC55, CMOC61, CMOC62, CMOC64, CMOC65, CMOC81, CMOC83, CMOC89, CMOC90, CMOC91, CMOC95, CMOC96, CMOC101, CMOC119, CMOC126, CMOC127, CMOC128, CMOC129, CMOC143, CMOC160, CMOC169, CMOC175, CMOC200, CMOC202, CMOC212, CMOC214, CMOC221, CMOC222, CMOC223, CMOC225, CMOC226, CMOC239, CMOC241, CMOC242, CMOC243, CMOC244, CMOC252, CMOC253, CMOC255, CMOC258, CMCO259, CMOC270, CMOC271, CMOC273, CMOC274, CMOC275, CMOC278, CMOC305, CMOC309, CMOC310, CMOC314, CMOC325, CMOC392, CMOC393, CMOC394, CMOC419, CMOC439, CMOC446, CMOC447, CMOC451, CMOC468, CMOC479, CMOC480, CMOC481, CMOC492, CMOC502, CMOC545, CMOC550, CMOC558, CMOC579, CMOC600, CMOC615, CMOC621, CMOC636, CMOC642, CMOC649, CMOC650, CMOC652, CMOC660, CMOC669, CMOC694, CMOC695, CMOC699, CMOC707 | ||
| High levels of staff turnover/agency staffing with inconsistency in approach across the team, and staff not having time to spend getting to know patients and/or are unwilling to get to know patients individually and hear what patients are trying to tell them | Patients do not give feedback or give feedback that is not true to their experience | |||||
| Patients are worried about being dismissed or rejected by staff when they approach them to share their experience | When staff have been dismissive or unavailable, or if staff ask patients to wait when they approach them to talk to them, patients can internalise this in a persecutory way and feel rejected. Sometimes they feel that they are dismissed because of their level of wellness. At other times they feel that staff are not taking them seriously or do not have time for them. When patients see or witness staff behaving impatiently, rudely or abruptly with either themselves or other patients, then patients may develop anxiety and may fear staff members. This makes them less likely to approach staff or give feedback, as they avoid interactions that may be experienced as painful. Taking the time to complain or raise a concern the first time takes courage from the patients, and they report that if their concern or complaint is initially dismissed or poorly handled, either they will not raise it again or it makes it very difficult for them to do so | Staff being dismissive or unavailable, or just asking patients to wait because they are busy | Patients become less likely to approach staff or give feedback when they experience staff as dismissive or too busy | CMOC28, CMOC34, CMOC35, CMOC41, CMOC79, CMOC189, CMOC215, CMOC420, CMOC488, CMOC521, CMOC549, CMOC611, CMOC669 | ||
| Patients are more likely to give feedback if they feel that they are going to be listened to | Building rapport between staff and patients helps patients feel that staff are listening to them. They feel valued and that the staff care about their opinion. If patients find staff approachable, they feel they are going to be listened to. When patients do not feel that their concern has been addressed or listened to or if it is dismissed without staff taking time to go through why it may not be possible to address their concern (e.g. side effects of medication, concerns about the environment on the ward or a desire to take leave), patients can become apathetic about giving feedback and perceive that staff do not care about their concerns. Not being listened to is disempowering, which, in a setting where patients already feel disempowered, exacerbates the patient’s feeling of disempowerment. When patients do not feel listened to, they can get extremely frustrated and desperate to attract attention to get their communication needs met | Staff making time to listen to patients | If patients feel listened to, they are more likely to give their feedback | CMOC32, CMOC34, CMOC35, CMOC41, CMOC53, CMOC68, CMOC69, CMOC70, CMOC83, CMOC189, CMCOC211, CMOC275, CMOC303, CMOC344, CMOC475, CMOC478, CMOC516, CMOC521, CMOC555, CMOC556, CMOC576, CMOC626, CMOC627, CMOC670, CMOC687, CMOC691, CMOC705, CMOC706, CMOC714 | ||
| Although there may be formal structures (forms and meetings) for capturing feedback on wards, patients perceive that the staff are not genuinely interested in the feedback | The feeling of staff members being ‘genuine’ is linked to feeling cared about or cared for by individual staff members. Sometimes, the lack of interest in feedback is observable at the ward level through lack of resources (i.e. no pen to complete forms on the ward). However, it is when this lack of interest is observed in staff attitudes (i.e. they are too busy to listen) that patients make very little effort to give feedback. Patients find that they relate better to staff whom they perceive as more genuine and genuinely interested in their care. This feeling that the staff are ‘genuine’ is important, as this can break down the power differential between staff and patients ‘because they become real people then, not some just authoritative figure’ | Lack of interest in patients and their experience expressed by staff or staff expressing genuine concern for the patient | Patients are more or less likely to give honest patient experience feedback depending on the degree of interest in patients shown by staff | CMOC29, CMOC30, CMOC31, CMOC65, CMOC66, CMOC69, CMOC190, CMOC226, CMOC301, CMOC302, CMOC311, CMOC312, CMOC313, CMOC337, CMOC421, CMOC436, CMOC437, CMOC481, CMOC484, CMCO485, CMOC505, CMOC539, CMOC576, CMOC578, CMOC628, CMOC689 | ||
| Some patients find it difficult to criticise or complain when they are receiving care from staff. They would prefer to speak to someone independent of the ward | Some patients find it difficult to offer feedback that might be critical or a complaint, as they recognise that the staff are trying to care for them. Partly this is linked to a fear of retaliation, but it is also related to wanting to not make the feedback personal to individual staff members and instead make it about the organisation or their care in general | Patients do not have the opportunity to give feedback independent of the ward or anonymously | The lack of opportunity to give independent or anonymous feedback may mean that patients do not share their experience honestly | CMOC228, CMOC229, CMOC400, CMCO401, CMOC602 | ||
| Carer | The most commonly cited concern of carers is that they are not sufficiently involved in the care of the person they care for and that the communication from staff is poor. When trusts do get communication and involvement right, the relationship is much more useful and reciprocal between staff and carers | Staff attitudes to carers are important. When carers feel that they are not listened to or that they are dismissed when they do try and have input or offer feedback, they feel disconnected from the one they care for. Carers want more feedback from staff on the treatment plan and support being given to the one they care for. Because relationships with staff are not built through regular communication, carers are more reluctant to give feedback on the care experience. Not being involved in the care nor being invited to meetings about the person they care for is experienced by carers as anxiety-provoking and disempowering. It is particularly anxiety-provoking if there are concerns about the care within the inpatient setting that they do not feel are being addressed (these include concerns about physical health, medication and a risk of abuse in the setting). Some carers perceive their exclusion from meetings as deliberate, whereas others feel that it is pressure on services or the culture of service that leads to their being left out. Not being involved is particularly anxiety-provoking when discharge plans are being made and carers are expecting the person they care for to return to either living with them or living in the community. Carers are often particularly apprehensive about their caring role in relation to discharge. They need to plan for their caring role and to have their caring role acknowledged, including their own limitations and the impact of caring on their lives. Assumptions on the part of the ward about their ability to cope with caring is particularly distressing when carers feel that they are struggling. In the worst cases, an adversarial relationship between carers and staff develops and carers actively avoid feeding any information back to staff | When staff do not communicate with or give feedback to carers, this creates barriers. When carers are involved and the communication is good with staff, this leads to better engagement with feedback processes | When carers are involved by ward staff, they find it much easier to support the care plan in place for the person they care for and are generally less likely to be anxious or upset by staff. When feedback is given and received by both staff and carers, a mutually reinforcing reciprocal relationship can develop to support the inpatient. When carers are not involved by ward staff, they are less likely to give feedback and want more feedback from the ward, which gives rise to complaints and poor satisfaction with services | CMOC793, CMOC794, CMOC795, CMOC812, CMOC813, CMOC814, CMOC815, CMOC822, CMOC823, CMOC824, CMOC825, CMOC826, CMOC827, CMOC828, CMOC829, CMOC830, CMOC857, CMOC858, CMOC862, CMOC863, CMOC864, CMOC865, CMOC869, CMOC870, CMOC871, CMOC872, CMOC873, CMOC875, CMOC876, CMOC879, CMOC882, CMOC883, CMOC885, CMOC887, CMOC889, CMOC892, CMOC893, CMOC894, CMOC895, CMOC896, CMOC897, CMOC898, CMOC903, CMOC904, CMOC905, CMOC906, CMOC907, CMOC908, CMOC909, CMOC910, CMOC911, CMOC913, CMOC914, CMOC915 | |
| Carers are not routinely asked for their feedback. When they are asked, they do not know what happens to their feedback or may be reluctant to give honest feedback to ward staff | When carers are not routinely asked for their feedback, they can feel left out. They may also feel that their feedback is unwelcome or unnecessary. Some carers do not know how to give feedback and would not do this independently of being asked. When staff do not ask for feedback in meetings from the carers, it can be disempowering and make them feel redundant (in the meetings, not in relation to their experience of being a carer for the inpatient). Often, this leads to their perceiving the staff as dismissive or rude. The need to preserve patient confidentiality makes it difficult for staff and carers, and communication is often obstructed. Carers feel that they have the ability to offer useful insights into ward functioning or would like the opportunity to make suggestions to improve the quality of care, but they are frustrated when the opportunity to provide feedback is not offered. When they are asked for their feedback, carers have no idea what happens to their feedback, why it is collected or what it is used for. They have to trust that it will not affect their friend or family member’s clinical care, and that it will be used to make change. Carers report that they are very unlikely to complain about staff because they ‘do not want anyone to lose their job’ or because they feel grateful that their friend or family member is being looked after. Staff need to actively seek feedback, as carers often sit with uncomfortable situations or downplay their concerns for these reasons | Staff do not ask for carers’ feedback; confidentiality makes this difficult but there is also a lack of opportunity for carers to give feedback | Carers do not engage in giving honest feedback | CMOC796, CMOC797, CMOC799, CMOC811, CMOC821, CMOC834, CMOC835, CMOC836, CMOC837, CMOC838, CMOC839, CMOC840, CMOC842, CMOC843, CMOC844, CMOC845, CMOC846, CMOC847, CMOC848, CMOC849, CMOC850, CMOC851, CMOC860, CMOC861, CMOC864, CMOC866, CMOC875, CMOC877, CMOC878, CMOC886, CMOC891, CMOC899, CMOC900, CMOC901, CMOC902, CMOC912 | ||
| First admission is often very difficult for carers | First admission is the most difficult and traumatic time for carers. They require additional communication at this time to make sense of and understand what is happening; however, there is often very little communication from services. Carers reported being overwhelmed and needing support to process any information they were given because the experience of having the person they care for admitted to an inpatient unit was very shocking | Staff do not communicate sufficiently with carers during the first admission of their friend or family member | Carers are overwhelmed and have lots of unanswered questions and support needs in relation to understanding the first admission. They are not engaged in giving feedback that could be useful to their friend’s or family member’s care or useful to support quality improvements in the admissions process or in the experience for carers | CMOC798, CMOC817, CMOC841 | ||
| Carers being able to establish a relationship with a member of staff is important | When carers have been able to establish a relationship with and build rapport with a staff member, they feel more engaged in the care of the person they care for and they feel that the feedback is easier to both give and obtain. Building rapport helps carers to trust the staff. Staff members giving carers the time to talk and checking in with them to see that they are happy helps to build this rapport. This makes them feel included and helps them to provide support during the admission, including feeling being able to advocate for the person they care for or communicate concerns. When such relationships do not exist, carers are less likely to communicate concerns for fear of this affecting the care received | Staff members being able to take time to get to know a carer | Carers engage better in giving feedback and feel more included in their friend’s or family member’s care and receive feedback more easily | CMOC803, CMOC806, CMOC808, CMOC818, CMOC831, CMOC832, CMOC833, CMOC840, CMOC851, CMOC852, CMOC853, CMOC854, CMOC855, CMOC858, CMOC859, CMOC867, CMOC868, CMOC874, CMOC886, CMOC890 | ||
| Clinical staff | Staff are aware that patients rarely complete formal feedback (surveys or forms). Staff feel that feedback on experience should be continuous, rather than patients waiting to complete a form at the end of their stay when they are being discharged | Staff are aware that patients rarely complete formal feedback (surveys or forms). They believe this is, in part, because these are not offered or patients are not encouraged to complete these forms or because the forms are inaccessible owing to language/literacy issues. Staff do not see the point in the forms, as they rarely see any feedback from these and so are disinclined (unless they are asked to or pushed to by management) to encourage patients to complete the forms. Staff feel that this type of feedback is ‘forced’. Staff do not routinely collect patient experience data using these tools and instead rely on patients completing them on their own if they want to. Staff do not find the discharge survey or collecting feedback at the end of an admission the most useful way of obtaining patient experience feedback, as it does not give them a sufficient overview of the patient’s experience on the ward. This relates to understanding that they get better engagement and more honest feedback from one-to-one interactions. They feel that they are more likely to get ‘lip service stuff’ in the final formal forms. Being able to extract meaning from informal conversations and help patients to give feedback more formally (e.g. linking to advocacy services) if needed is part of the staff role in collecting patient experience feedback. This soft intelligence or informal feedback is where some of the most useful information about how patients are experiencing the ward comes from for staff. Most of the informal feedback gets stored in patient notes and never makes it into formal patient experience monitoring, as the two systems operate entirely separately. Ward staff rarely see feedback from formal routes. They get most of their patient experience feedback from the informal route | Staff often do not ask patients to complete formal feedback forms. Staff do not find the survey at discharge the most effective way of getting patient experience feedback | Formal feedback is rarely obtained from patients and so change or improvement based on this will be limited. Formal feedback is not the most useful to staff at the ward level in terms of making changes | CMOC917, CMOC922, CMOC927, CMOC945, CMOC970, CMOC971, CMOC972, CMOC974, CMOC979, CMOC981, CMOC982, CMOC994, CMOC1007, CMOC1012, CMOC1015, CMOC1020, CMOC1024, CMOC1033, CMOC1034, CMOC1042, CMOC1048, CMOC1064, CMOC1083, CMOC1084, CMOC1136, CMOC1137, CMOC1147, CMOC1160, CMOC1163, CMOC1164, CMOC1173, CMOC1181, CMOC1194, CMOC1195, CMOC1202, CMOC1203, CMOC1204, CMOC1217, CMOC1218, CMOC1219, CMCO1220, CMCO1224, CMOC1235, CMOC1239, CMOC1249, CMOC1259, CMOC1260, CMOC1281, CMOC1285, CMOC1295, CMOC1306, CMOC1326, CMOC1362, CMOC1367, CMOC1382, CMOC1386, CMOC1406, CMOC1407, CMOC1408, CMOC1409, CMOC1421, CMOC1436 | |
| Staff understand that making time to sit with patients one-on-one is the most effective way of getting honest patient experience feedback. Staff are aware they can also get patient experience feedback informally through building relationships with carers. There is high staff turnover on inpatient wards and patients are frequently returning to the same ward | Staff build relationships with patients to build trust and so patients feel safe, which makes them more likely to share their experiences. Staff often perceive that their presence on the ward is sufficient to signal their availability for conversation and that patients and carers can ‘always’ approach them. Some staff feel that patients should take responsibility for expressing themselves/giving feedback, rather than staff having to make the initial approach. Some staff report being anxious or under confident to start conversations about individuals’ experience, as they do not know ‘what’s gonna come back the other way’ | Staff are not proactive in seeking feedback but are able, willing and confident to make time for one-to-one conversations if asked. Their availability is moderated by resource pressure. Patients are proactive in seeking engagement with staff | Patient experience feedback is obtained | CMOC919, CMOC943, CMOC954, CMOC967, CMOC974, CMOC992, CMOC1004, CMOC1013, CMOC1019, CMOC1027, CMOC1032, CMOC1033, CMOC1051, CMOC1052, CMCOC1059, CMOC1066, CMOC1084, CMOC1106, CMOC1114, CMCO1136, CMOC1147, CMOC1160, CMOC1163, CMOC1164, CMOC1168, CMOC1175, CMOC1218, CMOC1219, CMOC1234, CMOC1236, CMOC1237, CMOC1239, CMOC1243, CMOC1250, CMOC1251, CMOC1261, CMOC1280, CMOC1281, CMOC1290, CMOC1292, CMOC1324, CMOC1325, CMOC1366, CMOC1380, CMOC1381, CMOC1382, CMOC1384, CMOC1409 | ||
| Staff are not proactive in seeking feedback but are able, willing and confident to make time for one-to-one conversations if asked. Their availability is moderated by resource pressure. Patients are not proactive in seeking engagement with staff | Patient experience feedback is obtained | |||||
| Building relationships with patients is difficult but, conversely, patients are not always being asked the same questions so do not get impatient with giving feedback as readily | Different staff ask different questions | Patients do not get impatient with giving feedback as the questions they are asked vary | ||||
| There is an opportunity to build a relationship over time and so staff are able to obtain feedback, although, when patients are discharged too early because of bed pressures, patients can be cross. Staff then have to build the relationship back up. Other staff report that these patients have no interest in giving feedback | There is sufficient bed capacity for frequently returning patients to stay until they consider themselves well | Some frequently returning patients provide patient experience feedback | ||||
| There is not sufficient bed capacity for frequently returning patients to stay until they consider themselves well | Patients are unlikely to provide patient experience feedback | |||||
| Staff discourage patients from raising personal issues in communal settings or meetings | Staff actively discourage patients from sharing personal concerns or talking about themselves in meetings. Staff see those meetings as a space to discuss feedback on the running of the ward or on the environment of the ward, not to get feedback at an individual level. There is tension between staff wanting a collective level overview to try and build changes into ward practice and individuals needing to give feedback about their unique experience | Staff do not discuss individual experiences in community or communal meetings | Staff do not obtain individual patient experience feedback from meetings | CMOC942, CMOC983, CMOC1057, CMOC1079 | ||
| Staff are aware that anonymity and knowing how feedback will affect their clinical care is important to patients | Some staff demonstrated awareness that patients may be anxious about giving honest feedback in case it affects their clinical care, and felt, therefore, that feedback should be anonymised. Staff are aware that patients may feel extremely vulnerable and disempowered in the inpatient setting. However, staff also acknowledge that the feedback processes are often not anonymous. When complaints need to be investigated they cannot be anonymous. In some trusts, asking for feedback from patients while they are still on the ward can feel coercive (see CMO relating to involuntary admission and power relationship). When there are confidential electronic systems, this is less of a concern for staff. Anonymous online feedback has been seen to be more negative in some trusts than other formally collected feedback data | Staff are aware of the power relationships in inpatient settings and how these affect patients’ ability to give honest feedback | Patients may be reluctant to give honest feedback | CMOC980, CMOC1006, CMOC1040, CMOC1047, CMOC1089, CMOC1090, CMOC1091, CMOC1095, CMOC1096, CMOC1097, CMOC1098, CMOC1099, CMOC1163, CMOC1170, CMOC1192, CMOC1200, CMOC1228, CMOC1230, CMOC1263, CMOC1346 | ||
| Corporate staff | The majority of the formal survey feedback received is positive | Corporate staff have a different perception of patient feedback from ward staff, as the majority of formal feedback that is returned is positive. This feedback is not used; only a minority of complaints feedback is attended to and acted on | Corporate staff respond to complaints feedback | Complaints drive changes in service | CMOC1035, CMOC1041 | |
| Resources | Service user | When staff do not have the resources to make change, their frustration with the organisational situation can get transferred to or is communicated to patients | Patients feel that staff frustrations are personal and become fearful in response to staff members’ annoyance that they are being asked for things or to change things but they cannot take action on these requests. Patients sense hostility and so stop engaging in giving feedback | Staff do not have the resources (emotional or physical) to make changes in inpatient settings | Patients stop asking for support or sharing their experiences/giving honest feedback | CMOC5, CMOC363 |
| Wards are understaffed | Patients are aware that wards are understaffed. They hear staff talking to each other and they witness understaffing: a lack of staff available on the wards to talk to and few staff members for the number of patients. This means that they become less likely to approach staff, as either there is nobody available to talk to or they empathise with overstretched staff and do not want to add to their work. If patients understand that staff are busy, they know that they cannot talk to them. Patients attribute increased violence or numbers of incidents on wards to understaffing: staff do not respond to patients and so patients ‘kick off’. When the ward is unsettled, patients report not being able to share their experience, as the majority of the staff are involved in dealing with an individual | Either staff are too busy or there are not enough staff to receive patient experience feedback | Patients do not approach staff to share their experience, as they perceive that staff are too busy or that there are physically not enough staff to approach | CMOC27, CMOC135, CMOC164, CMOC201, CMOC208, CMOC209, CMOC246, CMOC268, CMOC293, CMOC296, CMOC297, CMOC300, CMOC319, CMOC324, CMOC333, CMOC349, CMOC377, CMOC378, CMOC466, CMOC469, CMOC470, CMOC489, CMOC490, CMOC497, CMOC576, CMOC591, CMOC597, CMOC599, CMOC601, CMOC607, CMOC622, CMOC643, CMOC647, CMOC648, CMOC654, CMOC655, CMOC658, CMOC661, CMOC664, CMOC665, CMOC666, CMOC741, CMOC768 | ||
| Patients are aware of pressures nationally on resources for health care, particularly for mental health, in part because of the media but also because staff give this as the reason why they are unable to respond to feedback | Patients diminish their needs or do not give feedback honestly about what they are unhappy about or their experience of the ward if they perceive that the staff are busy because the ward is understaffed. Staff often explain that the reason changes cannot be made is because of NHS cuts, staff shortages or other resourcing issues. Patients feel that they must try not to have needs that place further strain on the NHS/staff. This can lead to them not explaining when they are uncomfortable or unhappy, as they feel guilty for being in need. When there are high levels of agency or short-term staff, this affects patients being able to build rapport and share their experience with staff, as patients report that they are not as genuine as permanent staff (see CMO on rapport-building and being genuine) | The media and staff discuss the national staffing/resource crisis in the NHS and mental health specifically with patients. This is often supplied as a reason for not being able to enact change in inpatient settings | Patients are less likely to approach staff, as they perceive that there is either no point (because there are not sufficient resources or staff do not have the time to listen) or they do not wish to place further burden or strain on the staff who are responsible for delivering their care | CMOC65, CMOC119, CMOC121, CMOC208, CMOC225, CMOC226, CMOC324, CMOC472, CMOC490, CMOC522, CMOC556, CMOC559, CMOC601, CMOC636, CMOC642, CMOC665 | ||
| Carer | Carers find understaffing or resource pressure one of the main difficulties in getting feedback or being able to give feedback about the care of the person they care for | Understaffing with staff being too busy means that carers are unable to find available staff to either get feedback from or give feedback to about the person they care for. They perceive that staff do not have the time to communicate with them. Although carers recognise that they are ‘not the number one priority’, they can find this lack of availability frustrating and it exacerbates feelings that the staff are dismissive or disdainful of them and their involvement. The bad manners of staff when they are busy was often commented on. Carers additionally find communicating with the bank or agency staff, who may not have much knowledge of the patient or the ward, frustrating | Understaffing means that staff are unavailable to carers | Carers have no opportunity to communicate with staff to either give or receive feedback | CMOC800, CMOC801, CMOC802, CMOC804, CMOC805, CMOC806, CMOC808, CMOC809, CMOC810, CMOC811, CMOC816, CMOC819, CMOC820, CMOC824, CMOC834, CMOC880, CMOC881, CMOC889, CMOC916 | |
| Clinical staff | Understaffing means that staff are often unable to collect feedback | Getting patient experience feedback requires staff to sit with patients and complete forms or to prompt patients to complete them. This takes staff time. When staff do not have time to do this, it can compromise the quality of the answers. Staff do not have sufficient resources in terms of numbers of staff available on wards to administer formal feedback instruments. Sometimes they do not have time to spend one to one listening to patients to get feedback. A lack of time results in staff not recording feedback from patients in notes. Understaffing results in community patient meetings being cancelled. These meetings are not seen as a priority, whereas multidisciplinary team meetings are held without fail. When there are high numbers of agency or temporary staff on wards, the wards struggle to collect patient experience feedback regularly. Managers struggle if there is not a stable enough staff base to have a reliable enough workforce to collect patient experience data or champion improvement work. Ward staff are burdened with paperwork and other administration. Collecting patient experience feedback is seen as another administrative or paperwork-driven task. Health-care assistants and lower-band staff have more contact one to one with patients, as they have less paperwork or administration to do; however, they are not linked to formal patient experience data collection processes. They have to pass reported experiences on to nursing staff. Staff cannot respond to there not being enough staff, which frustrates them. This further disincentivises them to ask patients for feedback | Staff do not have time to collect feedback from patients | Patient experience feedback is not collected | CMOC928, CMOC930, CMOC932, CMOC934, CMOC938, CMOC939, CMOC940, CMOC951, CMOC952, CMOC959, CMOC1004, CMOC1039, CMOC1055, CMOC1056, CMOC1058, CMOC1075, CMOC1077, CMOC1078, CMOC1090, CMOC1104, CMOC1105, CMOC1109, CMOC1121, CMOC1128, CMOC1134, CMOC1135, CMOC1136, CMOC1149, CMOC1156, CMOC1157, CMOC1158, CMOC1171, CMOC1176, CMOC1186, CMCO1229, CMOC1234, CMOC1236, CMOC1237, CMOC1275, CMOC1276, CMOC1277, CMOC1286, CMOC1287, CMOC1290, CMOC1333, CMOC1334, CMOC1335, CMOC1336, CMOC1380, CMOC1381, CMOC1429 | |
| Staff are aware that once feedback is obtained it needs to be reflected on and analysed, but this takes resources | Staff are aware that the feedback needs to be analysed in relation to the workings of the ward for meaning and sense to be made of it, and to enable suggested changes to practice to happen. Staff are aware that they need to consider what weight to give to patient feedback. If 100 people raise something, it does not mean it is more important than one person raising a concern, as it can be difficult for people to complain. Corporate staff and ward staff need to be able to engage with the patient experience feedback and make meaning from it or else it becomes redundant | Staff need to have the resources to analyse any feedback collected | Feedback is not collected when staff do not feel that it will be analysed and used. Patient experience feedback, when it is collected, is not used to inform change | CMOC985, CMOC976, CMOC977, CMOC1076, CMOC1078, CMOC1103, CMOC1106, CMOC1119, CMOC1166, CMOC1193 | ||
| Corporate staff | Corporate patient experience teams are often small with limited resource. These teams investigate patient complaints | Corporate patient experience teams that centrally collate data but do not have easy systems of feeding back to staff at the ward level often struggle to get ward managers to respond to and implement suggestions based on feedback. These teams tend to be small and feel that they have little agency to change practice at the ward level. When patient experience work is not well embedded in core ward business, corporate staff can struggle to get patient experience feedback from wards. There is tension about what feedback is for – reporting for management and/or the CQC or being used at the ward level. The patient response numbers are not useful in themselves at the ward level; however, these are reported to NHS England. This means motivations to collect patient experience feedback can vary between ward and corporate staff. This can create tensions and lead to breakdowns in communication. Corporate staff are aware that, when punitive cultures develop, staff can feel frightened of being involved in the collection of patient experience feedback so they do not do it. Staff often feel that complaints or other top-down feedback that comes from corporate or management staff are an individual ‘slap on the wrist’ rather than a process of learning and change. Staff report being fearful of complaints and this drives practices such as ‘covering your own back’. Involvement by the corporate team in patient complaints can sometimes create barriers for working with ward-level staff | Corporate staff struggle to get feedback on centrally collated data back to the ward level; ward staff may not engage with corporate staff readily within organisational cultures where corporate staff mainly interact with them regarding serious incidents or complaints | Changes at the ward level are not made in response to feedback because of difficulties in the relationship between ward and corporate staff | CMOC989, CMOC987, CMOC988, CMOC989, CMOC990, CMOC1000, CMOC1001, CMOC1002, CMOC1003, CMOC1004, CMOC1037, CMOC1039, CMOC1061, CMOC1062, CMOC1065, CMOC1082, CMOC1086, CMOC1101, CMOC1102, CMOC1117, CMOC1118, CMOC1119, CMOC1122, CMOC1149, CMOC1150, CMOC1151, CMOC1152, CMOC1153, CMOC1193, CMOC1199, CMOC1233, CMOC1246, CMOC1247, CMOC1256, CMOC1316, CMOC1319, CMOC1320, CMOC1323, CMOC1342, CMOC1349, CMOC1369, CMOC1410, CMOC1411, CMOC1412, CMOC1418, CMOC1420, CMOC1426, CMOC1431, CMOC1432, CMOC1449 | |
| Power | Service user | Patients experience inpatient settings as disempowering and as depriving them of liberty (through their being detained against their will) or as depriving them of access to the resources that they are accustomed to (e.g. hairdresser) | Disempowerment has a negative effect on the patient’s experience. Patients find it difficult to communicate the subtle ways in which this disempowerment is experienced, for example not being able to participate in their usual activities or routines. Disempowerment can be experienced through the deals struck with staff in which privileges are allowed in return for conforming to certain ways of behaving: if you do X, I will give you Y. Disempowerment can be experienced as being denied things (e.g. access to washing or toilet facilities without being made to wait a long time for these to be unlocked). Patients worry that if they are honest when giving feedback, privileges will be revoked (e.g. not being allowed out on leave). Being made to wait while staff finish a conversation, paperwork or chatting can reinforce existing feelings of disempowerment, humiliation and vulnerability, and increases resentment. This leads to patients disengaging from feedback processes. Being bored and a lack of intellectual stimulation leads to patients feeling patronised. They find the setting dehumanising. Patients are more likely to respond to staff who they feel treat them with respect and give these staff honest feedback about their experience | Patients cannot participate in their normal activities/maintain their normal routines | Patients feel disempowered, which affects their ability to provide feedback, as the power relationship is such that they are already uncomfortable. Getting honest patient experience feedback about their experience is therefore difficult | CMOC3, CMOC4, CMOC12, CMOC138, CMOC146, CMOC165, CMOC289, CMOC326, CMOC327, CMOC330, CMOC331, CMOC343, CMOC346, CMOC355, CMOC356, CMOC357, CMOC360, CMOC362, CMOC378, CMOC379, CMOC387, CMOC388, CMOC389, CMOC391, CMOC413, CMOC414, CMOC437, CMOC449, CMOC452, CMOC454, CMOC455, CMOC494, CMOC495, CMOC504, CMOC518, CMOC521, CMOC523, CMOC526, CMOC527, CMOC534, CMOC535, CMOC537, CMOC568, CMOC573, CMOC583, CMOC584, CMOC585, CMOC586, CMOC591, CMOC592, CMOC606, CMOC618, CMOC619, CMOC620, CMOC657, CMOC662, CMOC711, CMOC720, CMOC727, CMOC728, CMOC732, CMOC733, CMOC734, CMOC735, CMOC736, CMOC738, CMOC739, CMOC742, CMOC743, CMOC744, CMOC747, CMOC748, CMOC749, CMOC750, CMOC751, CMOC754, CMOC755, CMOC757, CMOC760, CMOC761, CMOC766, CMOC767, CMOC769, CMOC779,CMOC782, CMOC783, CMOC784, CMOC785, CMOC786, CMOC788 |
| There is a ward hierarchy and, in particular, a power dynamic has been observed by patients in relation to nursing staff and consultants | The ward hierarchy and power of consultants on the wards means that the patients will often wait to speak to the ward manager or consultants to share their feedback, as they see the disempowerment of other staff and internalise this by understanding that the nursing or other staff cannot help them, as they do not have the agency to do so. Psychiatrists are often seen to hold the most power, as their decisions dictate if a person can have leave or go home from the ward. They also make decisions about medications. Patients can become resentful or mistrusting, as the psychiatrists do not deliver the majority of their care and they do not see them often unless they are afforded the opportunity to build some rapport with their clinician. Interactions with psychiatrists can become pressurised and a source of anxiety or upset for patients. Medical staff are not as visible on the ward as nursing staff and do not build rapport with patients in the same way. This means that patients can find it difficult to trust their decisions (see CMO on rapport-building). When patients feel very disempowered, they will often look to the most empowered or powerful individual at the ward level to support them with what they need. Previous history of trauma and abuse (particularly when this is gendered) can also lead to a feeling of disempowerment (e.g. in relation to a male psychiatrist) | Pronounced power hierarchies on wards in relation to medical and other professional staff | Patients do not believe that feeding back to anyone other than the consultant will achieve change and so they stop communicating about their experience. This means that their opportunities to provide feedback are limited, as their access to consultants is limited | CMOC7, CMOC85, CMOC86, CMOC93, CMOC94, CMOC98, CMOC104, CMOC104, CMOC109, CMOC123, CMOC156, CMOC165, CMOC166, CMOC167, CMOC168, CMOC174, CMOC188, CMOC194, CMOC195, CMOC196, CMOC200, CMOC204, CMOC211, CMOC247, CMOC255, CMOC263, CMOC286, CMOC290, CMO291, CMOC295, CMOC298, CMOC299, CMOC300, CMOC315, CMOC321, CMOC359, CMOC387, CMOC388, CMOC405, CMOC408, CMOC444, CMOC453, CMOC471, CMOC490, CMOC522, CMOC538, CMOC551, CMOC556, CMOC557, CMOC558, CMOC563, CMOC575, CMOC577, CMOC580, CMOC581, CMOC585, CMOC586, CMOC587, CMOC588, CMOC589, CMOC596, CMOC639, CMOC640, CMOC644, CMOC645, CMOC646, CMOC647, CMOC651, CMOC667, CMOC671, CMOC672, CMOC683, CMOC684, CMOC691, CMOC696, CMOC758, CMOC791 | ||
| In certain ward environments, feedback is not sought by staff and, therefore, requires patients to be proactive to communicate about their wishes and needs | Patients felt that, unless they proactively gave feedback, opinions on their care were not sought. Staff waited for patients to approach them, which is possible only if a person is feeling well enough or confident enough to do so. Patients feel that they could just be left to ‘sit and fester’ if they are left with the responsibility for seeking out one-to-one chats and seeking out things to do. Patients describe feeling bewildered and experiencing the staff as uncaring because their opinion was not sought and effort was not made to engage them. One patient reflected that not being approached by staff was something particular to inpatient mental health rather than to physical health wards. Many patients talked about the need to acclimatise or learn the rules of how inpatient settings work | Staff do not approach patients to ask for feedback | When staff do not seek patients’ views and wait to be approached, certain patient types will be disadvantaged in having care adapted to meet their needs, as this relies on individuals being well or confident enough to give feedback | CMOC13, CMO14, CMO15, CMO18, CMOC19 | ||
| Patients want to know who does what role before they approach them, as they want to make sure the person they are sharing their experience with can do something about it. Often, patients are confused about who is who. They understand that some people (e.g. volunteers) cannot change or affect their care | Patients wait to identify staff members who they feel have the power to effect change in relation to their care – they do not like to approach people who they do not perceive as having any power in the ward environment. Patients internalise ward hierarchies and power relationships on the ward, which conditions how they deliberately choose to speak to particular individuals about their experience instead of others | Ward hierarchies related to decision-making about patient care mean patients will not approach just anyone; they identify the person they feel has the power to effect change in relation to their experience | Patients do not share their experience if they do not know who to approach | CMOC22, CMOC58 | ||
| Patients can fear that giving honest feedback will affect their inpatient experience and that there will be repercussions, retaliation or reprisals or that they will get into trouble (some fear staff, some fear other patients and some fear both). Patients may also feel that giving any feedback could delay their discharge from the inpatient unit | Patients can be fearful that giving open and honest feedback about their experience will have an impact on their clinical care and on their day-to-day experience of the ward. Patients may not to give honest feedback because they worry that privileges will be revoked (e.g. leave). Patients describe retaliatory behaviour and repercussions for complaining or raising concerns from both staff and other patients during current or previous admissions. This makes them less likely to give honest feedback because they are fearful. Patients are managing their relationship with professionals who have the power to deprive them of their liberty. If they think being honest about their experience could delay their discharge from the unit, patients will be reluctant to be honest about their care or give any feedback to staff. Instead, they will focus on giving feedback that is compliant (e.g. not discussing their auditory or visual hallucinations). The opportunity to give anonymised feedback (e.g. not to put it in a box outside the nurses’ office where they can see you putting it into the box) and knowing what will happen to them as a result of feedback is important to some patients. Patients can develop an understanding that they are to blame or at fault for their illness and consequent behaviours, which can be quite shaming and makes them unwilling to give feedback. This is linked to fear of being dismissed | Staff exhibit retaliatory behaviour in response to complaints or concerns raised in ward environments. Staff do not reassure patients or have processes in place to support patients to give feedback honestly without it affecting their clinical care. Patients become fearful about other patients and do not trust staff to intervene or protect them if they raise concerns | Patients do not engage in feeding back their experience honestly | CMOC37, CMOC39, CMOC44, CMOC78, CMOC106, CMOC117, CMOC118, CMOC125, CMOC157, CMOC158, CMOC161, CMOC210, CMOC345, CMOC380, CMOC383, CMOC395, CMOC400, CMOC404, CMOC418, CMOC425, CMOC443, CMOC444, CMOC456, CMOC457, CMOC459, CMOC491, CMOC495, CMOC496, CMOC504, CMOC506, CMOC507, CMOC541, CMOC551, CMOC565, CMOC571, CMOC611, CMOC612, CMOC653, CMOC697, CMOC708, CMOC709, CMOC712, CMOC713, CMOC719, CMOC724, CMOC725, CMOC726, CMOC745 | ||
| Patients feel that staff do not genuinely care about their experience and are recording experience information only to ‘cover our backs’ or patients feel that they are ignored. Some patients feel that staff laugh at or mock them. Staff presence on the ward is minimal. Staff are seen spending time talking to one another in the office and not communicating with patients | A ‘staff vs. patients’ culture is felt or experienced by the patients and anxiety about the nature of the staff–patient relationship is higher when staff are less present on the ward or do not express genuine care. Patients do not feel that the experience information they give to staff is responded to genuinely or used to make changes | Patients hear or observe staff discussing recording experience or feedback information to ‘cover our backs’ or do not experience staff as genuine or caring in relation to their feedback | Patients lose trust in staff and are less likely to share feedback about their experience | CMOC76, CMOC80, CMOC81, CMOC87, CMOC91, CMOC92, CMOC94, CMOC149, CMOC155, CMOC163, CMOC164, CMOC383, CMOC386, CMOC403, CMOC415, CMOC416, CMOC417, CMOC418, CMOC420, CMOC431, CMOC616, CMOC709, CMOC712 | ||
| Staff have the power to share or manage personal and sensitive patient information | Patients feel vulnerable because they know that staff have what the patient considers sensitive or privileged information about their lives. If this information is shared conversationally or without explicit consent on the ward, patients can perceive this as putting them at risk from other patients. They do not feel supported or respected if this happens. They become fearful of the implications of confidential information being shared. For example, a policeman who was admitted to a ward did not want the other patients to know what he did for a living. This caused the patient anxiety when one of the staff members told other people in the inpatient setting conversationally, not respecting his request not to make this known. Confidentiality is important to patients and they will often share their experiences only if they believe that what they are saying will remain confidential | Staff share information that patients consider to be of some sensitivity or of a confidential nature with others on the ward (including other patients) without explicit consent to share the information | If patients lose trust in staff to maintain professional boundaries or respect confidentiality, they feel anxious and are less likely to share their experiences | CMOC40, CMOC245, CMOC250, CMCO251, CMOC253, CMOC251, CMOC267, CMOC269, CMOC382, CMOC594, CMOC726 | ||
| Being involuntarily detained or forcibly medicated as an inpatient damages patients’ relationship with staff | Patients experience a breakdown in their relationship with staff when staff have to forcibly medicate them. Patients become profoundly mistrustful of the staff and the care that they are receiving. Patients report struggling to make sense of or understand the treatment that they have received. Patients feel unable to give any feedback to staff after an episode of being forcibly medicated. It makes them feel overpowered and, if they have had previous traumatic experiences in which they have been overpowered (e.g. abuse), it can retraumatise them or compound existing trauma. The lack of communication about why medication has been administered and the lack of help given to patients trying to make sense of these experiences are some of the key drivers of ongoing mistrust. Patients remain fearful that they will be overpowered again. Some patients are aware that they may have been aggressive while they were unwell and so do not feel that they have the right to complain about their experience given their difficult behaviours. This makes them reluctant to talk to staff and give honest feedback if things have upset them or are bothering them about their treatment, as they feel humiliated and as though they in some way deserve to be treated poorly | Staff having to forcibly medicate patients | Patients may lose trust in, become suspicious of or refuse to engage honestly with staff after being forcibly medicated | CMOC71, CMOC72, CMOC73, CMOC136, CMOC137, CMOC138, CMOC139, CMOC147, CMOC182, CMOC187, CMOC188, CMOC379, CMOC380, CMOC381 | ||
| Once patients have experienced forcible medication or restraint, they may no longer trust ward staff and so having an independent advocate or someone with lived experience to talk to about their experience is important. Conversely, patients who have not had this experience may still be happy to speak to ward staff once they have built a rapport | Once trust in staff has been lost following a patient being forcibly medicated, having an independent advocate or someone with lived experience to talk to can be important for patients, as they can perceive that nobody is to be trusted on the ward, which leaves them feeling isolated while trying to make sense of their experience. At this point, they are more likely to speak to someone whom they view as independent. However, anyone who is perceived as working within the organisation can be mistrusted and so careful explanation of their role and how confidentiality operates is needed to reassure the patient and help them to feel safe in relation to having conversations about their care | Independent advocate or person with lived experience made available for patients to speak to | Patients are unlikely to engage further with or give honest patient experience feedback to ward staff if they have been forcibly medicated on the ward. It is important that, if this happens, patients are offered an independent person to speak to and are able to talk through and make sense of this experience | CMOC74, CMOC75, CMOC378, CMOC379, CMOC381, CMOC424 | ||
| When complaints cannot be resolved at the ward level, patients feel that they need to go ‘higher’ and so PALS or corporate complaints functions are used | When patients do not trust that their issues will be resolved at the ward level, they/their family members may be supported to or may choose to complain to PALS or corporate complaint functions that are perceived to be ‘higher’ than the ward. Some patients will not trust anyone they do not have a rapport with and perceive PALS or corporate staff to be ‘strangers’ so will not give feedback outside the ward. Provision needs to be made for both feedback mechanisms to coexist | Patients are unable to resolve issues locally at the ward level and so complain to PALS or corporate services | Patients give formal feedback and complain outside the ward environment | CMOC161, CMCO270, CMOC427 | ||
| When the CQC is inspecting, patients report staff behaviour changes in respect of their care | Patients can develop feelings of resentment when the attention and care they receive is improved by an outside inspection such as a CQC visit. This makes them feel that the staff are falsely interested in spending time with them and listening to them as opposed to their normal behaviour of remaining in their office (see CMO on the importance of being genuine in relation to obtaining feedback) | Staff change care or behaviour when being inspected | Patients mistrust staff intentions in spending time with them to get feedback, resent the lack of genuine care and do not engage in giving honest feedback | CMOC678 | ||
| Carer | Carers are made to feel as though they are a nuisance or are annoying staff when they ask for things or try and get information on the inpatient they care for | Carers report feeling as though they are annoying, in the way or a nuisance when they ask for information about the inpatient care or try and approach staff on the wards. In part, they attribute this to staff being busy, but it is disempowering and makes them feel useless in relation to the person they care for and their care experience on the ward. Carers become apprehensive about approaching staff, as they do not wish to irritate them, which puts a strain on communication between carers and the ward. Carers are less likely to give honest feedback to the unit as a result and often temper their unease or do not communicate information for fear of annoying staff. In particular, carers are worried about the impact on the care of the person they care for if they complain or raise concerns | Staff do not involve carers or they see them as an additional burden of work when they are already stretched | Carers do not engage in giving honest feedback to the unit | CMOC807, CMOC862, CMOC864 | |
| Clinical staff | Staff are aware of the disempowering experience of many patients | Staff are aware that being admitted involuntarily under the Mental Health Act33 is a very disempowering experience for patients and they see seeking patient experience feedback in part as a way of redressing that balance. Staff feel that having to forcibly administer medication to keep people safe alters their ability to get honest feedback from patients because the patients feel disempowered. When good practice exists, the staff spend time explaining the reasons for this happening to patients and carers. They report that this transparency is important in keeping the lines of communication open and in relation to being able to obtain honest patient experience feedback. Staff understand that, owing to the hierarchical nature of wards, patients will seek out managers, as they understand that these individuals have more power over and responsibility for their care and treatment. Given the power imbalance and disempowering nature of inpatient care, staff can find asking for feedback difficult or uncomfortable and they are reluctant to do so. In some trusts, the way in which feedback is asked for can be perceived as coercive, as staff ask patients to rate them in front of them. This creates or reinforces staff feeling that they are disempowering patients. Staff see instances in which patients can genuinely be listened to (e.g. in their review meetings) as an opportunity to address the power imbalance so staff make an effort to collect patient experience feedback and patients’ views on their care during review meetings and incorporate patient wishes into care planning | Staff are sensitive to the disempowerment of patients and seek opportunities to redress the power imbalance | Staff maintain their relationship with patients and so patients are able to give honest feedback | CMOC933, CMOC950, CMOC973, CMOC979, CMOC993, CMOC1010, CMOC1014, CMOC1017, CMOC1021, CMOC1022, CMOC1023, CMOC1045, CMOC1053, CMOC1058, CMOC1066, CMOC1068, CMOC1081, CMOC1088, CMOC1090, CMOC1091, CMOC1096, CMOC1097, CMOC1138, CMOC1148, CMOC1163, CMOC1170, CMOC1200, CMOC1201, CMOC1211, CMOC1218, CMCO1220, CMOC1223, CMOC1225, CMOC1248, CMOC1299, CMOC1312, CMOC1313, CMOC1314, CMOC1315, CMOC1321, CMOC1329, CMOC1330, CMOC1331, CMOC1332, CMOC1368, CMOC1375, CMOC1379, CMOC1392, CMOC1397, CMOC1414, CMOC1417, CMOC1424, CMOC1427, CMOC1430, CMOC1443 | |
| Service users and carers are involved in patient experience work | Corporate staff involving service users and carers in all staff training about how to collect feedback is useful, as it gives the staff insight from the patients’ perspective. Corporate staff perceive that this increases the likelihood of feedback being collected, as staff buy in to feedback processes and understand the reasons for collecting feedback. Often, service user involvement exists only at the strategy, recruitment or training level. Some wards have peer support workers; however, many staff do not feel that co-production is taking place on wards or there is no actual evidence of co-production at the ward level. Staff do not see much of the patient experience work as co-produced. Some teams are resistant to having peer support workers – largely, this is to do with concerns about resources and supporting them or managing them within teams, but there are also those that feel that user involvement is difficult in inpatient settings because of the nature of the environment. In cases in which peer support workers have been introduced, staff describe this as having been a process of ‘breaking down barriers’ and, in particular, challenging professional dominance as a way of changing organisational culture. Peer support works well when it is integrated into patient experience work and ward life (e.g. supporting patients in review meetings or to feel less anxious about giving feedback or in following up on feedback). In these circumstances, peer support workers feel valued and as though they are supporting the relationship and communication between staff and patients. Some staff feel that peer supporter workers have a role to play in empowering or facilitating patients to make complaints, which is in part driven by the culture of collecting and responding only to negative feedback. When service users or volunteers are involved in collecting feedback, this is not responded to as seriously by the organisation as complaints or formal feedback scores, and so the collection of feedback and the results from it are not taken seriously by the staff either. This relates to the hierarchical nature of the ward, where the most senior people have the most ‘responsible’ tasks. When the peer support work is tokenistic, staff are aware that some peer support workers’ experience is very dated and they cannot relate to temporary ward life or the pressures of the contemporary ward environment | Service users and carers contribute to staff training and to providing peer support for patients | Feedback is most likely to be collected from patients by ward-level staff | CMOC1038, CMOC1046, CMOC1049, CMOC1116, CMOC1118, CMOC1123, CMOC1124, CMCO1125, CMOC1126, CMOC1129, CMOC1130, CMOC1131, CMOC1132, CMOC1155, CMOC1184, CMOC1206, CMOC1222, CMOC1232, CMOC1257, CMOC1267, CMOC1304, CMOC1305, CMOC1313, CMOC1328, CMOC1343, CMOC1398, CMOC1400, CMOC1402, CMOC1403, CMOC1419, CMOC1420, CMOC1433, CMOC1435, CMOC1444, CMOC1445, CMOC1446 | ||
| There is a perception by some staff that it is easier to obtain feedback from inpatients, as they are a ‘captive audience’ | There is a perception from some staff that it is easier to collect feedback from inpatients, as they are a ‘captive audience’ in that they are unable to leave the ward and it is easier to therefore administer feedback tools such as surveys. Conversely, some trusts do not attempt to obtain feedback in inpatient settings, as they perceive that people are too unwell (see CMO about wellness in Table 20) | Staff find it easier to collect feedback in inpatient settings | More feedback is collected in inpatient settings | CMOC1144 | ||
| Theme | Participants | Context | Mechanism | Outcome | CMO reference code | |
|---|---|---|---|---|---|---|
| Reasoning | Resources | |||||
| Wellness | Clinical staff |
Staff receive feedback/complaints from patients who are very unwell Staff perceive that, at times, patients are too unwell to give feedback |
Staff perceive that people are making complaints based on the situational context, their level of wellness and their understanding of what is happening to them. They reason that their wellness is the thing that is likely to be causing the complaint Staff can sometimes appear defensive, saying that patients ‘exaggerate’, which makes them less likely to be open to receiving feedback Staff discuss how levels of risk and unwellness lead to staff withdrawing from engaging that patient: ‘if you’ve got somebody who’s particularly aggressive or rude or nasty, then staff have a tendency to withdraw from that person’ Staff need to have the emotional availability and time to engage with unwell patients. Without these, they withdraw. This means that opportunities to capture patient experience from people who are very unwell may be missedPathways for feedback need to consider patient experience not as decision based (regarding wanting to go home) but as a way to understand the wider experience Staff need time and the emotional resource to be available to listen to feedback from those who are unwell Staff making assumptions about patients’ capacity to give individual experience feedback based on their assumed capacity or the Mental Health Act33/section is disempowering for patients. It can lead to staff disregarding unwell patients’ opinions |
Staff receiving and managing complaints locally for patients and to resolving them, and discerning the level of complaint and whether or not it needs to be escalated, taking account of patient wellness Staff sometimes dismiss or do not respond to informal feedback, as they attribute it to the patients’ wellness |
Staff are more likely to manage complaints from people they perceive as very unwell at a local level. Staff do not make these complaints formal or pass these on Staff are less likely to receive feedback and act on it from patients who are perceived to be very unwell Communication gaps can occur |
CMOR42, CMOR44, CMOR53, CMOR56, CMOR58, CMOR69, CMOR70, CMOR87, CMOR98, CMOR103, CMOR176, CMOR177, CMOR205, CMOR209, CMOR222, CMOR230, CMOR246, CMOR249, CMOR250 |
| Staff sometimes resist receiving feedback or discussing what the patient wishes to discuss, as they feel that the patient is too unwell to engage in the conversation |
The patient is perceived as too unwell to engage in conversation, so staff change the topic, shut down or terminate the conversation. This creates tension between the staff and the patient Staff perceive the management of risk and safety as their main priorityAnother motivation for engaging in conversation with patients from the staff point of view is to get the patient well enough for discharge Patients want to talk about their experiences and the wider context of their lives |
Staff being emotionally and practically unavailable to patients | Patients and staff do not work collaboratively and patient experience feedback is not received when patients try to communicate | CMOR62, CMOR133, CMOR176, CMOR178 | ||
| Getting feedback from a patient about their experience can happen at any time – getting feedback about the ward environment and what might need to be improved to improve the quality of service or patients’ experience of service is best obtained when staff have built a relationship with the patients and have observed that they are making sense of their environment | Observing the patient through engaging with them to understand how they are doing facilitates knowing when to ask patients for experience to get accurate, honest and helpful feedback. It is also necessary, when patients are not communicating, that staff are able to gauge how patients are experiencing the ward through observation | Staff developing an understanding of the patient over time and knowing when to ask for more detailed feedback about their experience |
Staff observation of patients about the timing of when it would be best to receive feedback helps patients and staff to get a more accurate picture of how they are experiencing the ward, which helps to make feedback meaningful and of use Feedback about how a person is experiencing their stay can be sought at any point, but feedback that is useful for action-planning comes when patients have a better understanding of what has happened to them and why they have been admitted |
CMOR29, CMOR43, CMOR107, CMOR206, CMOR249 | ||
| Importance of feedback/seeing changes | Patients | Patients do not see the point in giving feedback, as they do not see changes happening as a result of their feedback |
When patients give feedback but do not see anything changing as a result of their feedback, they are less likely to give feedback because they feel disempowered and as though there is no point. Without understanding why change is not happening, patients feel ‘fobbed off’ and disengage Patients find that actions being taken as a result of feedback makes them feel valued When patients are told why nothing will change or why something is happening and are given a reason (i.e. as a result of resourcing issues), they are more likely to give feedback about other things relating to their experience. Giving the reason why something cannot change, even if they still wish that it would change, and an explanation is important, as this is empowering |
Staff explaining why things cannot change or making changes | If staff explain why change cannot happen or if changes are made, patients are more likely to give feedback | CMOR267, CMOR268, CMOR269, CMOR270, CMOR274, CMOR275, CMOR277, CMOR278, CMOR279, CMOR280 |
| Clinical staff | Staff do not receive positive feedback and use it in relation to planning, although they may find it boosts morale; they receive and use negative feedback to plan | Positive feedback is seen as ‘nice to receive’ but staff ‘react more’ to negative feedback. Staff dismiss positive feedback and do not use it to plan because it feels more personal, whereas positive comments are deflected. If only negative feedback is received and responded to, staff can find this ‘draining’ and it can desensitise them to feedback, as there is no balance. Staff also feel that corporate staff/managers do not value compliments and that these are often outweighed by complaints | Ward staff being emotionally unavailable to receive positive feedback and taking negative feedback personally | Negative feedback is used to change practice or make changes on the ward, but positive feedback is not received in the same way and is often discarded, meaning potential good practice is lost | CMOR28, CMOR35, CMOR36, CMOR37, CMOR54, CMOR59, CMOR75, CMOR76, CMOR77, CMOR93, CMOR94, CMOR100, CMOR101, CMOR102, CMOR120, CMOR121, CMOR147, CMOR151, CMOR158, CMOR179, CMOR190, CMOR223, CMOR264, CMOR265 | |
| Staff receive complaints and use these to change service; there can be a culture of those who ‘shout loudest’ being most likely to be heard | Analysing complaints helps staff to learn and staff are motivated to change to avoid further complaints. Conversely, because complaints are responded to, if complaints are not received, staff can ‘assume everything is fine’. Staff are more likely to respond to complaints, as these are formally recognised by the organisation and there are sanctions associated with action that takes place as a result of these, which can mean that patients who complain or shout loudest are more likely to be heard | Staff receiving complaints and being able to analyse these to decide on ways to change the service | Staff change the service in response to patient feedback in the form of complaints | CMOR60, CMOR153, CMOR183, CMOR190, CMOR223, CMOR239, CMOR242, CMOR244, CMOR251, CMOR258, CMOR259 | ||
| Staff are mandated to use the FFT or discharge surveys as the primary method of collecting patient experience feedback | Staff are disinclined to receive patient experience feedback, as they cannot utilise or make meaning from a ratings-based system without information about why the rating has been given. They cannot engage with the process, as the outcome is not meaningful for them and they do not see the rating leading to change, so do not value it. In addition, if ranked and scored low in response to feedback, staff feel disinclined to continue to put extra effort into collecting it if the response to the feedback results in lower staff morale. Bad feedback affects morale and staff become disheartened by the ranking process and the power of the system in place (this links to punitive corporate structures and power CMOs) | FFT or discharge survey ratings collection as the primary method of patient experience feedback | Staff getting only the ratings, and not further information about the ratings, does not motivate them to collect patient experience feedback because the rating alone is not meaningful. Staff disengage from receiving patient experience feedback | CMOR63, CMOR84, CMOR86, CMOR95, CMOR133, CMOR147, CMOR138, CMOR167, CMOR168, CMOR179, CMOR198, CMOR354 | ||
| Staff report feedback (i.e. what has changed) to patients on the ward | Patients receiving feedback makes staff feel that they are empowering patients and that this allows them to feel listened to and validated. If staff cannot report change to patients, they find this ‘demoralising’ in relation to obtaining feedback | Staff being able to give feedback to patients on the changes made in response to patient feedback | Staff feel that patients value feedback, as this is empowering for them | CMOR50, CMOR74, CMOR182 | ||
| Staff (and patients) do not see changes in response to feedback/ are not able to make changes | Staff and patients become annoyed and staff lose the incentive and become reluctant to receive feedback when change is not seen in response to feedback. Staff are unaware of how feedback creates change or is used. Sometimes change cannot be enacted owing to resource pressures. However, those decisions are made by corporate services, meaning that staff can feel disempowered and then feel that they are not being ‘open’ and ‘honest’ with patients in response to things that are raised, as they are not informed. Staff do not want to feel that they are ‘fobbing off’ patients. Seeing that changes have been made leads to patient buy-in and builds trust to enable patients to approach staff and ask for changes. Part of that is about transparency or honesty around the receipt of feedback, which also creates staff buy-in and endorses the patient voice and listening as central to practice | The organisation not responding quickly enough to patient experience feedback or poor communication about the outcomes of feedback between wards and corporate services | Staff stop asking for patient experience feedback when things are not responded to or changed, as they do not want to deal with patients’ frustrations or expectations of change. Change does not happen in response to patient experience feedback | CMOR64, CMOR65, CMOR66, CMOR74, CMOR82, CMOR83, CMOR84, CMOR85, CMOR91, CMOR97, CMOR181, CMOR182, CMOR186, CMOR191, CMOR196, CMOR197, CMOR203, CMOR248 | ||
| Staff in lower bands or on the wards do not get patient experience feedback. Experience feedback is used more by corporate staff | The lack of information and the fact that it is not fed back to staff at all levels creates confusion about and inhibits an understanding of patient experience data | Lower-band staff are the most likely to spend time with patients, but they do not get access to the feedback data that usually comes back to ward managers. Sometimes, even senior staff do not receive patient experience feedback, as this is collated centrally and not communicated | Staff are unaware of what patients have said and, therefore, are unable to enact change | CMOR24, CMOR47, CMOR160, CMOR161 | ||
| Relationships and communication | Patients | Relationships with staff and who receives patient experience feedback are important | Relationships are important, as patients feel that who receives their experience feedback links to whether or not actions are taken; patients also feel that this is more likely if they know the person or the person has some responsibility for them (e.g. is their named worker). Patients observe that agency staff are less integrated/cannot use feedback or are less motivated to do so than other staff and so patients are less likely to give experience feedback to these staff | Staff having a relationship and being able to capture or receive experience feedback and then act on it | Patients are more likely to give feedback, and changes as a result of feedback are more likely to be actioned | CMOR271, CMOR276, CMOR281 |
| Patients | Staff are receptive and available emotionally and physically to receive feedback | When patients observe that staff are preoccupied either with other nursing tasks or with their own activities and are not open and available to patients (e.g. are shut in the office), patients are less likely to approach them to give their experience feedback. Patients need to feel that staff are receptive to their information | Staff being available (emotionally/physically) to receive feedback | Patients are less likely to give feedback | CMOR272, CMOR273, CMOR282 | |
| Carers | Carers do not feel listened to or included, or as though action is taken as a result of their feedback | Carers do not feel listened to or included, or as though action is taken as a result of their feedback. They are often wary of being too pushy, but find it difficult to have their feedback received. Carers either complain (as a way to get a response) or cease to offer feedback. They continue to engage with the service on behalf of their friend or family member but from a position that feels increasingly disempowered. When carers do feel listened to and staff take the time to speak to them, they develop more trust in services | Staff do not engage and communicate well with carers | Carer feedback is not taken for analysis or to be used to drive quality improvement | CMOR283, CMOR284, CMOR285, CMOR286, CMOR287, CMOR288, CMOR289, CMOR290, CMOR291 | |
| Clinical staff | A staff member having personal experience (of self or family member) accessing inpatient mental health services/staff members (peer support workers) with lived experience and whom patients can relate to facilitates communication. Peer support workers proactively asking for informal feedback or if patients have requests (i.e. leave requests) before formal meetings with doctors encourages patients to give feedback. The availability of staff members to talk to on the wards when people are very unwell is important in building relationships and helping people engage with services | A staff member having lived experience creates relatability between staff and patients. Staff taking the time to share their personal experience and to respond to patients when they are distressed and in the way that they want, instead of making them wait, puts patients at ease and builds the relationship. If staff had experienced assumptions being made about their own or a friend’s/family member’s care led to the staff having a better understanding of how to communicate and how disempowering assumption-driven behaviours from staff to patients can be. Staff feel that former service users or patient engagement staff with lived experience are more likely to get honest feedback from patients. Receiving honest feedback from patients is difficult and some staff perceive that this is more likely to happen if the person asking about patients’ experiences of the ward have lived experience, as this changes the power relationship and means that the patient may not feel as vulnerable and may be able to speak more freely | Staff availability to speak to people in distress is resource constrained; there may not always be someone with lived experience to talk to. Resources are needed to have practitioners with lived experience on wards | Patients build rapport and engage with staff with lived experience to give feedback. Such staff have an enlightened understanding of how disempowering some ways of caring can feel or be, which has changed their own professional practice. People with lived experience may be able to collect and receive more honest feedback owing to the more equal power relationship | CMOR1, CMOR2, CMOR3, CMOR14, CMOR37, CMOR55, CMOR71, CMOR128, CMOR136, CMOR137, CMOR150, CMOR165, CMOR171, CMOR172, CMOR214, CMOR218, CMOR220, CMOR232, CMOR233 | |
| Having multiple ways of engaging carers and encouraging them to give feedback is important | Getting to know carers in their own right in one-to-one feedback meetings encourages them to give feedback. In particular, informing carers about how to give feedback, having face-to-face contact and offering carers support is important. This helps carers to feel understood and supported in their caring role and helps them to be informed, which facilitates engagement | Having specific or dedicated carer resources and multiple ways of obtaining feedback | Better engagement of carers in the feedback process | CMOR4 | ||
| Staff need time to spend with patients. Receiving feedback in person (particularly informal feedback) yields different information and allows for easier conversations with staff to resolve issues locally. Rich data can be gained from these interactions |
Staff spending time with patients and listening to them builds trust and facilitates getting honest in-person feedback. The building of relationships is important in getting honest feedback The use of feedback forms alone does not provide peace of mind to patients that their voice has been heard, whereas one-to-one interactions show that someone has received the feedback Indirect feedback is more easily captured in person than formally (written or electronic). The conversational nature of garnering feedback in this way makes patients feel ‘more fluent’ in the way they communicate and data can be captured more readily/in a timely way, which means staff can have conversations more immediately about patients’ experiences Making time (even though staff are busy) and being consistent – coming back to speak to patients when they have been told that a staff member will return – is really important to patients Staff feel that sometimes patients just tick the formal feedback forms to comply with completing them, or complete the forms without really engaging with and thinking about them fully. Some of the rich data are then lost because honest feedback is retained by individuals and not reported or recorded. Informal feedback is not often responded to and is just received |
Staff having the time to gather feedback on patients’ experiences in person is important. Staff being able to discuss such feedback among themselves to resolve issues locally is important, as there is rich information in such feedback to support planning and response | Feedback in person (informal) gives a richer (more granular) picture and can be acted on immediately and resolved by staff. However, the disadvantage of informal feedback is that it is often ‘lost’ and not recorded or acted on and is therefore not used to make or sustain change | CMOR5, CMOR31, CMOR34, CMOR41, CMOR66, CMOR72, CMOR79, CMOR87, CMOR106, CMOR108, CMOR111, CMOR184, CMOR194, CMOR201, CMOR202, CMOR204, CMOR206, CMOR215, CMOR221, CMOR234, CMOR235, CMOR236, CMOR237, CMOR238, CMOR241, CMOR247, CMOR253, CMOR266 | ||
| Staff can sometimes be reluctant to receive feedback |
Staff can become reluctant to receive feedback for many reasons (see CMO relating to seeing changes in Table 22) Staff can feel anxious about asking for feedback and are concerned about what feedback they will receive. They may become defensive/fear reprisal from patients/corporate staff Staff may not know what to do with the feedback or may feel disempowered to be able to do anything with the feedback and, therefore, disinclined to collect it |
Staff do not seek feedback and can be reluctant to receive it | Feedback is not obtained | CMOR185, CMOR246, CMOR261 | ||
| Staff discussing the timeliness of addressing a complaint raised by a patient on the ward regarding their diagnosis led to the patient feeling distressed and upset | An understanding is needed of patients’ needs and levels of distress, and a role is needed in which staff must reassure patients in distress | The time taken to communicate the information given by doctors in a way that patients can make sense of – this takes time by ward staff | Addressing complaints at a local level to avoid further distress may elevate risk on the ward. Addressing complaints in a timely manner for the patient is important | CMOR173 | ||
| There is a lack of communication between ward staff and psychiatrists or other staff as regards patients feeding back their experience of medication or concerns |
Poor communication around a patient’s experience can lead to inaction. Ward staff did not receive and then hand over a patient’s experience of the side effects of their medication, meaning that the medication was not reviewed and the patient became increasingly distressed and non-compliant over 4 weeks. The staff not receiving this feedback and then not translating it so that change could be enacted in care was an example linked to the idea of patient wellness and of patients not being believed, which appears in the ‘change’ (Table 22) and ‘receiving’ CMOs. Patient concerns can be minimised, dismissed or, worse, ignored if this more informal conversational patient experience feedback is not responded to at all levels on the ward There can be assumptions made around wellness that can lead to concerns not being addressed and needs not being met Psychiatrists are aware that the reason that they do not receive the informal feedback about the side effects of medication is because the patient perceives that saying anything to them may delay their discharge. This means that most informal feedback is held at the ward level and needs to be drawn out to inform clinical care |
Patient experience feedback not being received and responded to appropriately Concerns not being passed on to staff who can enact change |
There are concerns among ward staff about patient concerns not being filtered to higher levels for action, including delays from the point of view of patients in medication being reviewed. Staff are upset that concerns are not communicated. Patients experience a delay in recovery as a result | CMOR175, CMOR177 | ||
| Corporate staff | Reflective practice and triangulating data to look across different types of patient feedback helps with planning and quality improvement in the face of multiple competing pressures in a service | Being able to observe trends and patterns by reading across data to analyse and understand these trends allows so that staff can develop responses/make changes to service allows knowledge to be built and helps identify both positive practice and where poor practice is taking place | People need to be able to access, then have time to triangulate and make sense of, the different types of patient experience data generated | Being reflective across data and triangulating data are important, as this helps to filter out both what is good practice and what is not working, so, as things change, progress is made and the wheel is not reinvented | CMOR6, CMOR7, CMOR8, CMOR116, CMOR167, CMOR169, CMOR170, CMOR207, CMOR208, CMOR231 | |
| Resources | Clinical staff | Resource pressure means that staff are less available to carers to obtain feedback or to give feedback on their friend’s or family member’s care | Carer engagement is affected and carers’ relationships with and trust in staff are damaged by poor communication | Poor communication between ward staff and carers can be caused by a lack of staff availability | Feedback from carers is not sought and feedback is not given to carers when there are staffing or resource pressures, which means that staff get less information about the patients and cannot form those trusting relationships with carers. This also means that carers do not get involved in decision-making processes about their friend’s or family member’s care | CMOR4, CMOR5, CMOR25, CMOR27, CMOR68 |
|
The bureaucratic nature of care and the lack of time to spend with patients affects staff members’ ability to engage with and collect patient experience feedback. This links to risk management and making sure things are documented in case of incidents Staffing shortages mean that staff find it difficult to put boundaries in place with patients, as they do not have colleagues to support them |
Staff members’ ability to receive information from patients is affected by demands of the job in relation to data management Staff are concerned that paper-driven data collection processes that prioritise risk and documenting concerns means that staff do not have time to build rapport, which detracts from the patients’ experience Spending time with patients facilitates engagement, enabling patients to give and staff to receive feedback. A lack of staff resource means that staff lack confidence in putting boundaries in place with patients, as they lack the support of other colleagues. Staff are worried about risk and safety in relation to escalation if change is not happening and there are not adequate staffing levels to respond to patient concerns Staff feel that, if time is not spent with patients listening to them and receiving feedback because of other (resource) pressures, this can lead to increasing numbers of incidents on the ward |
A lack of staff time as a resource to engage with/support patients | Staff are not available to receive patient experience data, as they are not spending enough time engaging with patients. If there are not sufficient staff resources in place, change does not happen, as staff feel unsupported in making changes. Staff also become wary of obtaining feedback in response to staffing shortages and managing safety and risk | CMOR9, CMOR10, CMOR11, CMOR21 CMOR33, CMOR38, CMOR46, CMOR48, CMOR57, CMOR66, CMOR73, CMOR78, CMOR81, CMOR92, CMOR96, CMOR113, CMOR114, CMOR123, CMOR124, CMOR127, CMOR144, CMOR149, CMOR216, CMOR219, CMOR227, CMO228, CMOR263 | ||
| Having a stable workforce (low turnover of staff and enough staff) helps to build organisational culture and staff cohesion to support or drive quality improvement |
Staff are enabled to receive feedback Staff develop loyalty to the area that promotes motivation for and engagement in obtaining feedback The staff team operates more cohesively Staff are approachable, as they behave in ways that are ‘friendly’ and ‘caring’ A lack of stability for staff, with no supportive team built because of staff churn, means that there is no consistency for patients and staff cannot build relationships and trust on a ward. This contributes to staff feeling as though they are working in isolation. Staff experience burnout, as they lack supportive relationships with colleagues |
Low staff turnover | This enables staff to engage in patient experience processes because they are motivated to do so, and they have the emotional capacity to receive feedback | CMOR20, CMOR37, CMOR40, CMOR45, CMOR92, CMOR125, CMOR190, CMOR225, CMOR262 | ||
| There is a lack of staff on the wards who are able to obtain feedback from or give feedback to patients, or a lack of time to dedicate to such tasks, owing to resource constraints |
High levels of agency staffing on wards or low staff numbers affect staff members’ ability to receive patient experience feedback Staff may not understand why there are issues or the nature of resource issues, which creates frustration and this is expressed when responding to patients’ questions The resource pressure means staff are less available to respond to or receive patient experience feedback Resource pressures are not just affecting ward staff. PALS is unable to meet targets owing to stretched staff and lack of staff A one-size-fits-all template is followed rather than being personalised, without acknowledging resource limits on wards and on how structured the approach to following this is Targets are missed and patients are not having their voice heard |
A lack of staff due to resource constraints | Staff feel disempowered and frustrated by their inability to explain why there are limited resources/staff available and why there is a lack of support from senior management. This affects their ability to receive patient experience feedback or provide patients with explanations | CMO23, CMOR27, CMOR39, CMOR40, CMOR48, CMOR109, CMOR132, CMOR145, CMOR187, CMOR188, CMOR189, CMOR198, CMOR200, CMOR201, CMOR211, CMOR224, CMOR257 | ||
| A lack of beds, resource pressures for services and inadequate resourcing all affect patient experience | Staff feel patients are not having their needs met (i.e. getting timely access to treatment) and that they have no control over improving the quality of care pathway, as it is a wider hospital and health system resourcing issue | Patients are slower to be discharged owing to a lack of community options and so beds are unavailable for people to access when they need them | This has impacts on the care that staff can give and on patients’ experience | CMOR30, CMOR65, CMOR132, CMOR143, CMOR152 | ||
| Staff availability to receive and respond to feedback affects patient experience. When staff spend time with patients on the ward, they get more patient experience feedback |
When there are no resources (i.e. enough staff/time) then staff feel disempowered and demotivated and do not actively prioritise collecting patient experience feedback through spending time with patients. Resource pressure affects staff morale, the emotional resources and the time available to receive and act on patient experience feedback Staff availability and time means that they can engage with and build rapport and relationships with patients to get meaningful feedback. Building the therapeutic relationship is important in getting honest feedback Staff need to be emotionally available to receive feedback. Staff are aware that quality deteriorates when they are under extreme pressure. Lack of staff time in a high-pressure ward setting results in them ‘firefighting’ rather than leading quality improvement in the light of limited resources |
Other priorities such as managing risk, risk assessments and logging these in IT systems, or physical health checks, take precedence over getting patient experience feedback |
Resource issues mean that staff feel disempowered by the bureaucratic nature and volume of tasks and so do not engage with patients to capture patient experience feedback; staff have less time to spend with patients to collect their feedback Conversely, when staff have time to spend building rapport with patients, staff value patients’ feedback Staff disengage from collecting patient experience data if quality of care is low, as they are solely firefighting |
CMOR4, CMOR10, CMOR11, CMOR22, CMOR31, CMOR33, CMOR34, CMOR40, CMOR41, CMOR45, CMOR46, CMOR61, CMOR65, CMOR66, CMOR71, CMOR72, CMOR81, CMOR90, CMOR97, CMOR106, CMOR111, CMOR155, CMOR156, CMOR180, CMOR187, CMOR188, CMOR189, CMOR190, CMOR195, CMOR200, CMOR211, CMOR225, CMOR226, CMOR227, CMOR228, CMOR236, CMOR237, CMOR241, CMOR251, CMOR258, CMOR259, CMOR260 | ||
| Power | Clinical staff | Staff feel listened to and feel that they can have an impact or can actually influence or enact change |
Staff feel empowered when they are listened to and understand why decisions have been taken within the trust (i.e. they are informed) Staff feel that decisions are taken at corporate ‘bigwig’ level and influenced by external (national) priorities Empowerment and feeling valued and listened to creates motivation to support change Conversely, if staff do not feel listened to or that patient experience feedback is responded to, they are disinclined to seek or respond to feedback, as they cannot see the point |
Staff being listened to themselves, and being able to influence or have an impact on services; not just collecting data for assurance purposes |
Staff enact cultural change and engagement in receiving patient experience feedback Staff enact change if they are empowered to do so |
CMOR13, CMOR19, CMOR26, CMOR82, CMOR83, CMOR88, CMOR89, CMOR96, CMOR138, CMOR139, CMOR141, CMOR142, CMOR154, CMOR163, CMOR164, CMOR166, CMOR191, CMRO192, CMOR193, CMOR198 |
| Staff encourage patients to make complaints. Staff use patients to advocate about issues such as resourcing | Staff feel disempowered to make change (feel their voice will not be heard) and so can encourage patients to complain in order to try and prompt action within ward settings | Staff do not feel that they have the agency to effect change without using the patient voice to do so | Staff feel disempowered and encourage patients to put in complaints to try and drive change or improvement in services | CMOR49 | ||
| Staff feel persecuted by the complaints process and as though they are not supported or listened to |
Ward staff feel that patients have a stronger voice in relation to complaints or concerns raised and that they are unsupported during corporate staff investigations. This makes them feel disempowered and resentful. Staff lose the incentive to listen to and receive feedback, and they withdraw from seeking or hearing it, as it may lead to complaints Staff feel disempowered by the system, unheard and not listened to, which leads to them feeling that they have a lack of power within the ward; this results in increased pessimism and upset, compounded by the experience of not seeing things improve (see CMO about seeing changes in Table 22), which can lead to reduced motivation to try (burnout) |
Staff become disengaged or withdraw from patient experience by trying to avoid receiving complaints | Patient experience and complaints feedback is resisted by staff and the opportunity for quality improvement based on this feedback is lost | CMOR212, CMOR223, CMOR261, CMOR264, CMOR265 | ||
| More established ward staff are resistant to change coming from newer members of staff | Staff who are routinised in practices do not want to change, or cannot see the rationale for change, and so either do not engage with or obstruct changes being made | A lack of support for proposed changes or a lack of effort made by colleagues to support change | Efforts to make change are lost because there is no consensus or other staff members resist making changes | CMOR112, CMOR135 | ||
| Lower-band nursing staff or health-care assistants are more available (in terms of time) to listen to patients’ experiences. Nursing staff tend to focus on feedback that relates to clinical care | Spending time with patients and sitting down with them to directly ask about their experience generates engagement and leads to patients giving a richer type of experience feedback. Patient experience may not be seen as a priority by ‘higher-band’ staff. In addition, there are examples in which clinicians are aware that patients are less likely to give honest feedback (e.g. to the psychiatrist who is responsible for their discharge or care plan, because they fear that sharing concerns will delay their release from the ward). This means that the informal feedback held by ward staff is crucial in relation to understanding and managing the patient experience | Roles on wards mean that health-care assistants and lower-band staff collect the majority of informal, honest patient experience feedback on an individual basis from patients | Lower-band staff (who are often not linked with or able to feed in themselves to formal patient experience data collection) collect patient experience feedback; sometimes this creates a communication gap or is a lost opportunity for wards to act on feedback | CMOR22, CMOR32, CMOR33, CMOR51, CMOR52, CMOR57, CMOR80, CMOR96, CMOR104, CMOR105, CMOR110, CMOR115, CMOR118, CMOR119, CMOR159, CMOR176, CMOR177, CMOR199, CMOR213, CMOR252 | ||
| Staff must have the right values in relation to individuals and care, namely to understand that one size does not fit all. Staff must not take a tokenistic approach to collecting feedback, that is there must be meaningful engagement and co-design in services. Staff must not wield power abusively/unhelpfully (i.e. ‘key swingers’). When power hierarchies are unhelpful, working in silos occurs | Values prompt reflection and analysis, which leads to learning that facilitates action-planning for change. Minimising power hierarchies encourages buy-in and participation across the ward. It creates a culture of a ward ecosystem whereby everyone at all levels takes responsibility for the experience and feedback on the ward. Conversely, rigid authoritarian behaviours whereby power is held over patients or more junior members of staff does not create the culture or conditions in which feedback is either given or responded to and both staff and patients become fearful. This also damages collegiality and collaboration and encourages siloed working. Staff are aware that, when there are power hierarchies that are unhelpful and patients are treated as a ‘captive audience’, patients may not give honest feedback and so they do not want to engage in getting patients’ feedback, as they perceive it as coercive | The ‘soft but important elements of actually having a health service that actually is about the individual’ – putting individuals at the centre of what actually happens, rather than building a corporate strategy or organisation without thinking about that individual themselves | This creates the circumstances for staff to be able to receive feedback meaningfully and to act on it | CMOR15, CMOR16, CMOR17, CMOR18, CMOR117, CMOR124, CMOR129, CMOR130, CMOR131, CMOR132, CMOR135, CMOR240 | ||
|
Staff do not have the ability to sustain change There are reactive models of working without senior leadership/corporate buy-in Resources are not in place to make the change happen effectively |
This creates frustration in responding to patient experience feedback and staff either make small tokenistic or easy environmental changes or avoid changing things and instead maintain the status quo |
A lack of strategic priority setting in relation to patient experience feedback and not tying this to quality improvement initiatives more widely Lack of resourcing for change |
There is a lack of sustained change/incremental change and a lack of overall quality improvement | CMOR154, CMOR155 | ||
| Management staff on wards have to make judgements about how to respond to feedback (i.e. escalate it or offer reassurance and support junior colleagues in receiving feedback) | Management staff have to make decisions about if a piece of information or patient experience feedback received informally needs to be raised more formally and escalated or if it is something that is known and the patient requires reassurance about. Making these judgements in a pressured ward environment is difficult and requires experience and a working knowledge of the patients and the ward. Management staff feel that inexperienced or junior staff require more support in understanding patient experience feedback and how to receive and respond to that appropriately | Senior ward staff support junior staff to respond to patient feedback | New concerns are raised or escalated in relation to informal feedback and patients are offered reassurance when concerns are known | CMOR174, CMOR215 | ||
|
There is a lack of corporate staff on wards, except in times of crisis or pressure, or feedback serves corporate staff rather than being returned to and used at the ward level Corporate staff do not work alongside or with ward staff There is a blaming culture |
Senior staff being visible only during or in work related to concerns or incidents creates feelings of being ‘under a microscope’ and of ‘blame’ and ‘fault’, namely a fear culture. Staff are disinclined to receive feedback and engage in patient experience work when there is a perceived ‘blaming’ organisational culture. Blaming cultures can lead to staff becoming risk averse and, therefore, not problem-solving effectively in relation to patient experience. When there is a blaming or target-based culture, there is evidence that feedback is biased, as staff select people purposively to give feedback |
Higher visibility of senior staff, not just in response to incidents Stronger relationship between corporate/senior staff and clinical staff on wards |
A high visibility of and relationships with senior staff means that ward staff and patients are less ‘alarmed’ by the presence of corporate staff on the ward | CM0R12, CMOR16, CMOR67, CMOR95, CMOR97, CMOR99, CMOR102, CMOR122, CMOR126, CMOR140, CMOR141, CMOR146, CMOR157, CMOR162, CMOR217, CMOR243, CMOR245 | ||
| Staff are aware that the inpatient environment can feel coercive, not just because of restricted rights but also through a lack of information for patients regarding processes | Staff are aware that when patients lack information or are unhappy with an aspect of their treatment, or when there is confusion and fear in patients, this may affect their willingness to give honest feedback to staff. Part of receiving feedback is creating the conditions in which staff are willing and able to receive the feedback and patients are willing and able to give it. Staff need to listen to get an understanding of how the patient is experiencing the environment on their initial admission, to try and support them to engage. Staff feel that anonymity is important to patients in some instances to offer them a chance to give feedback when they may otherwise not do so | Staff need to give patients information about their care and the environment to facilitate feedback; patients need to be able to give feedback anonymously | Without patients being given information about their care and the environment, they may become fearful and not give honest feedback to staff. Without ways of anonymously giving feedback, these voices may be lost | CMOR210, CMOR229, CMOR247, CMOR255 | ||
| Theme | Participants | Context | Mechanism | Outcome | CMO reference code | |
|---|---|---|---|---|---|---|
| Reasoning | Resources | |||||
| Wellness | Corporate staff | Patients make large numbers of complaints during a short time in their admission |
Corporate staff investigating complaints from patients who make a large number of complaints during a short space of time in their admission can attribute this to the patient’s level of wellness Staff find it difficult to sustain action with patient turnover. When the patient is discharged, the pressure to act is reduced |
Corporate staff respond to all complaints but can infer that a person is not well from the volume of complaints made during their admission | Corporate staff relate the reason for complaining to patient wellness | CMOA75, CMOA165 |
| Patients | Patients do not see data being analysed or thought about or actions being taken as a result of such data at the ward level |
Patients feel that their feedback is not taken seriously, as they do not see any analysis or processing of the feedback taking place at the ward level Very often they have requests refused but without being given the rationale, which is disempowering, as it makes them feel that the staff are not thinking through their suggestions/concerns |
Staff do not analyse or interpret feedback; instead, it gets sent to corporate or management staff for approval/dismissal | Patients feel that ward staff do not think about their feedback and that decisions are made in a seemingly arbitrary way about their care | CMOA1, CMOA2, CMOA3 | |
| Importance of feedback/seeing changes | Clinical staff | Staff consider that ensuring that the patient has a positive experience and getting positive feedback ‘is taken as part of the job’ |
Staff consider that ensuring that the patient has a positive experience and getting positive feedback ‘is taken as part of the job’. They often dismiss this feedback instead of using it Positive feedback can boost morale but is seen as having little value and is not analysed or scrutinised in the same way as complaints or other methods of informal or formal feedback |
Staff do not analyse or interpret positive feedback to either sustain or learn from good practice | Staff do not use positive feedback to improve the quality of care | CMOA7, CMOA8 |
| Clinical staff |
Staff at the ward level have access to patient experience data in a timely manner (e.g. through an electronic dashboard) Corporate or ward staff are able to triangulate quantitative patient experience data with other types of patient data |
Staff feel that they are able to respond better to individual patient experience feedback (e.g. patient stories) than formal feedback. They are better informed if they can analyse these individual experiences alongside other data collected about patients’ experiences and the operational running of the ward Ward staff need access to patient experience data (not just the result of analysis) and to have a range of data in order to try and understand why particular patterns of outcomes are being generated. These data need to be accessible in a timely manner, otherwise ward staff cannot respond quickly. They find it difficult to take action in relation to something that happened some time ago on the ward There is insufficient analysis at the ward/corporate level to identify themes in relation to which quality improvement is needed. A reactive/knee-jerk approach is often adopted When electronic systems exist, corporate staff often use data to identify ‘hotspots’ or to try and spot deterioration in quality of care or safety on wards through triangulating data |
Staff are able to make sense of data in context (i.e. patient stories in the context of wider feedback and management data) |
It is easier for staff to understand what is happening at the ward level in order to make changes if patient experience data are triangulated with other data collected Being able to triangulate data and analyse it alongside other data facilitates understanding rather than encouraging reactionary improvement practice, which is often not sustained |
CMOA16, CMOA29, CMOA30, CMOA33, CMOA34, CMOA35, CMOA36, CMOA37, CMOA38, CMOA46, CMOA47, CMOA48, CMOA56, CMOA64, CMOA65, CMOA69, CMOA82, CMOA84, CMOA85, CMOA94, CMOA96, CMOA99, CMOA101, CMOA103, CMOA104, CMOA107, CMOA108, CMOA109. CMOA112, CMOA113, CMOA114, CMOA121, CMOA122, CMOA123, CMOA124, CMOA125, CMOA126, CMOA127, CMOA128, CMOA129, CMOA131, CMOA132, CMOA134, CMOA135, CMOA146, CMOA147, CMOA149, CMOA160, CMOA161, CMOA163 | |
| Corporate staff | Having a mixture of qualitative and quantitative feedback (e.g. the FFT and patient opinion or other qualitative feedback) is helpful for corporate staff trying to make changes |
Anonymous quantitative indicators are not useful on their own. The information collected is too generic. Qualitative experience data that give more granular detail at the service level are more helpful for action-planning and are easier to respond to Qualitative experience data are useful in helping to understand what is happening, where it is happening and why in order to drive change or quality improvement It is difficult for staff to work out how to weight data (i.e. should they respond to one complaint or change services in response to the majority of concerns, for example if 20 people raise an issue) Patient experience feedback can begin to feel like a ‘numbers game’ and not feel relevant to staff if they cannot use or do not see the analysis of the data. There is a perception that qualitative feedback ‘never goes anywhere’, whereas quantitative data prompts a response |
Staff need to be able to analyse quantitative indicator data alongside qualitative data | Combined quantitative and qualitative data are the most effective way of seeing quality improvement – quantitative data alone are not sufficiently useful | CMOA24, CMOA31, CMOA33, CMOA39, CMOA41, CMOA45, CMOA46, CMOA52, CMOA56, CMOA60, CMOA66, CMOA68, CMOA80, CMOA83, CMOA86, CMOA87, CMOA88, CMOA97, CMOA105. CMOA111, CMOA115, CMOA117, CMOA122, CMOA123, CMOA125, CMOA136, CMOA137, CMO153, CMOA155, CMOA158, CMOA164 | |
| Clinical staff | Informal verbal feedback is often a really useful source of patient experience information for staff to either adapt practice in relation to individual patients or make changes at the ward level | Verbal feedback given by patients to staff is something that staff often can and will act on immediately. This is better for the patients, as they receive immediate feedback and it helps with the running of the ward in relation to both managing individual patient experience and making changes to the ward | Staff respond to individual (informal) verbal feedback | Staff are able to make more immediate changes in response to patient experience feedback at the ward level | CMOA4, CMOA20, CMOA22, CMOA40, CMOA78, CMOA79, CMOA89, CMOA93, CMOA95, CMOA98, CMOA100, CMOA111, CMAO128, CMOA129, CMOA130, CMOA140 | |
| Relationships and communication | Clinical staff |
Patient experience feedback is often ‘fed upwards’ to corporate staff who report that there are not the resources to make changes or send feedback back down to the ward level to respond to or make changes Staff perceive that instructions are ‘sent down’ from corporate staff |
Staff report that patient experience feedback received informally at the ward level (i.e. in community meetings) is often ‘sent up’ to corporate level and instructions in relation to this are ‘sent down’ Anonymously collected patient experience data are sent to corporate staff, who are responsible for analysing this and feeding back to wards. Ward staff are aware that decisions are often made off the ward (by corporate staff) and most of the feedback or suggested changes cannot be put in place and are not looked into because there are insufficient resources The upwards delegation and lack of ability to respond to patient experience feedback is disempowering for ward staff. They are aware that it affects patients when they do not see their feedback being thought through or changes being made in response to their feedback. There is often a blanket response to patient experience feedback. Decisions can feel reactive to individual cases Staff feel disconnected from corporate decision-making about patient experience and care. Analysis at the corporate level is often to benchmark or analyse trends (i.e. by the CQC) – this is different analysis from what is needed at the ward level |
Ward staff do not analyse patient experience feedback for the feasibility of making relevant change The responsibility for analysis often lies with corporate services Ward staff may be sent the analysed feedback with the expectation that they take action Target-driven change results in poor staff buy-in with staff not engaging with action for change |
Feedback is sent to corporate staff for decisions that ultimately are made based on resource allocations Change seldom comes from patient experience feedback expressed at the ward level |
CMOA9, CMOA10, CMOA21, CMOA25, CMOA26, CMOA28, CMOA91, CAMOA92, CMOA94, CMOA101, CMOA102, CMOA106, CMOA109, CMOA110, CMOA111, CMOA116, CMOA119, CMOA120, CMOA123, CMOA124, CMOA125, CMOA127, CMOA128, CMOA129, CMOA138, CMOA139, CMOA142, CMOA143, CMOA144, CMOA145, CMOA150, CMOA151, CMOA152, CMOA154, CMOA158 |
| Resources | Clinical staff | Resource pressures (busy wards, staff shortages and small patient experience corporate teams) mean that analysis of patient experience feedback rarely takes place or takes a long time. Analysed patient experience or other feedback is not readily available in a useful format to ward managers (unless there is an electronic interface) or to other ward staff | When wards are busy with many patients and there are staff shortages, the patient experience is worse and the opportunity to collect patient experience data is not taken up by staff. In part this is because they are busy, but it is also because they are reluctant to invite feedback when they feel they are not delivering an optimum standard of care. Staff report that they end up ‘firefighting’ during these periods and working additional shifts when there are staffing shortages, which means that patient experience feedback and other data do not get analysed and, therefore, are not used to drive change. Analysis is not prioritised in the face of resource pressure; it is seen as a non-essential priority. If corporate staff in patient experience roles are responsible for the analysis, there can be overwhelming volumes of data for them to ‘weed through’ and there are usually few people in these roles | Staff do not analyse data (at the ward or corporate level) for resourcing reasons but instead only analyse data that are activated differently | Quality improvement does not happen based on patient experience feedback. Analysis of data is the weakest area of the patient experience cycle, as limited resources are allocated to this | CMOA11, CMOA12, CMOA13, CMOA14, CMOA15, CMOA19, CMOA23, CMOA27, CMOA42, CMOA43, CMOA44, CMOA49, CMOA53, CMOA54, CMOA55, CMOA61, CMOA63, CMOA64, CMOA65, CMOA71, CMOA77, CMOA105, CMOA115, CMOA118, CMOA119, CMOA132, CMOA133, CMOA134, CMOA143, CMOA144, CMOA156, CMOA157, CMOA159, CMOA162 |
| Corporate staff | Fiscal constraint means that improvement initiatives are cut | Staff report that fiscal constraints in the NHS mean that posts such as nurse consultants are removed or people are not replaced when they move on, which means that there is less capacity to carry out improvement tasks and staff do not feel that these are a priority | Fewer staff in improvement-related roles/posts are replaced owing to budget cuts | Quality improvement strategies or activities are not taken forward | CMOA72 | |
| Clinical staff | Complaints are analysed in detail by individual staff, ward managers and corporate staff | Staff respond to negative feedback swiftly to try and avoid complaints. When complaints do happen, staff analyse these to see where changes need to be made because they are often formal and monitored by corporate services. There are two common approaches to complaints from staff: they view them either as a learning opportunity or as something that is associated with punitive management intervention that are to be avoided at all costs. Irrespective of the approach to complaints, staff try and avoid patients’ concerns being escalated through not feeling heard. Staff feel as though there are many situations in which they cannot change the things that the patients are complaining about; therefore, they do not find the complaint useful in relation to trying to improve the quality on the ward. Staff feel that quality assurance (based on complaints or incidents) rather than quality improvement (based on patient experience data) takes precedent | Staff respond to negative feedback swiftly to try and avoid complaints. When complaints do happen, staff analyse these to see where changes need to be made | Change is mostly based on the analysis of complaints, and quality improvement does not get prioritised | CMOA5, CMOA6, CMOA8, CMOA32, CMOA50, CMOA51, CMOA52, CMOA62, CMOA70, CMOA73, CMOA74, CMOA76, CMOA148 | |
| Power | Corporate staff | Staff feel that the board or executives are more likely to buy in to change if there is service user and carer involvement | Staff cite many reasons for promoting or supporting service user and carer involvement, but in relation to acting on feedback some staff report that service user and carer involvement is often seen as necessary (as well as desirable) in order to secure management or executive support for change | Staff commit to service user and carer involvement as a way of brokering change with board/senior management staff | Service user and carer involvement is used to improve the quality of care | CMOA17, CMOA18, CMOA58, CMOA59, CMOA90, CMOA116 |
| Staff feel that board-level buy-in is important in driving change | Staff feel more accountable if there is board-level buy-in to patient experience work (including complaints) and oversight of that work. Staff often report analysis and action to the board | Staff report to the board or chief executives on patient experience | Board-level buy-in drives quality improvement or change in services | CMOA67, CMOA70, CMOA81, CMOA85, CMOA141, CMOA148 | ||
| Theme | Participants | Context | Mechanism | Outcome | CMO reference code | |
|---|---|---|---|---|---|---|
| Reasoning | Resources | |||||
| Importance of feedback/seeing changes | Carer | Carers want to know that change has happened as a result of their feedback; trusts that are responsive to carer feedback can demonstrate that change has taken place. Sustaining change is often difficult and carers identify previous change that has not been sustained | Carers find it frustrating not to be able to see change based on their feedback and, if they do not know what happens to their feedback, this affects their trust with the service and leads to further complaints. Carers identify that change is not sustained or that repeated pressure needs to be put on services for their views to be heard, which places them in an adversarial position in relation to the trust and their friend’s or family member’s care. They identify staff being too busy or resourcing issues as being central to why implementation of change in response to feedback does not take place or is not sustained | Sustaining change based on feedback requires trust buy-in, staff buy-in and resources | Carers’ feedback is used to implement changes | CMOI1, CMOI2, CMOI3, CMOI4, CMOI5, CMOI24, CMOI28 |
| Clinical staff | The implementation of change in response to patient experience feedback is mostly linked to complaints or incidents |
Staff are more likely to be able to implement and act on feedback related to environmental concerns than to other concerns Behavioural change is less immediate and, therefore, more difficult to measure than environmental change, making it less likely to be prioritised by staff Changing cultures is often prompted by incidents or inspection and requires staff buy-in at all levels, as well as generation of support for the approach being adopted by the wider staff team |
Systems in place to more easily respond to environmental concerns | Environmental changes are more readily implemented than cultural changes | CMOI6, CMOI25, CMOI39, CMOI45, CMOI49, CMOI50, CMOI61, CMOI76, CMOI89, CMOI92 | |
| No implementation takes place in response to patient experience feedback that is collected. Feedback is collected and stored but not used | This makes staff feel like collecting feedback is a ‘waste of time’ | Feedback is collected but not used | No change is implemented in response to feedback | CMOI13 | ||
| Staff struggle to implement changes based on ratings, in particular with positive feedback, for which no data are gathered on the experience to contextualise it | Staff do not see the point and do not feel that they can use positive feedback or patient experience feedback that lacks detail on where, how and why something happening. Cultures of resistance develop in which patient experience work becomes about targets, without meaning attached | Ratings or scores being given as feedback (i.e. without rationale) is not useful to staff in being able to implement change | Partial feedback information does not lead to change being implemented | CMOI18, CMOI19, CMOI37, CMOI44, CMOI67, CMOI113, CMOI117, CMOI126, CMOI128 | ||
| The implementation of change in response to patient experience feedback is often linked to complaints or incidents | Staff investigate, ‘rationalise’ and analyse why an incident has taken place or a complaint has been made – they evaluate practice in order to decide on the action to take or on the changes to implement. A fear of complaints, a need to be compliant, risk aversion and pressure from external bodies or corporate services all motivate staff to use complaints as the primary source of patient experience feedback that they respond to | Complaints or incidents are responded to | Complaints are more likely to be responded to and to drive the implementation of changes | CMOI20, CMOI26, CMOI32, CMOI36, CMO138, CMOI50, CMOI51, CMOI98, CMOI112, CMOI115, CMOI121 | ||
| Quality improvement becomes quality assurance that is largely target or data driven and linked to auditing or external pressures (i.e. the CQC/commissioners), which affects the type of feedback collected | Staff lose the meaning behind quality improvement if all that is valued is data collection and curation. This means that the focus shifts from patients’ experience to the recording of their experience. Benchmarking statistics is seen to be useful within and between trusts, but staff develop a deeper understanding of what is going on only based on qualitative data. Fear (i.e. of the CQC) is often cited as the primary driver for implementing changes | Quality assurance and quality improvement are data driven, and quality improvement is seen as something that is a step removed from clinical practice | Staff can disengage from meaningful patient experience-led quality improvement if solely driven by targets and collating data – data need to be combined with context and understanding to be useful rather than simply used in a monitoring exercise | CMOI52, CMOI53, CMOI55, CMOI57, CMOI63, CMOI64, CMOI65, CMOI73, CMOI74, CMOI90, CMOI93, CMCOI97, CMOI98, CMOI100, CMOI101, CMOI102, CMOI103, CMOI104, CMOI107, CMOI108, CMOI110, CMOI111, CMOI113, CMOI119, CMOI120, CMOI121, CMOI123, CMOI124, CMOI125, CMOI126, CMOI128, CMOI133, CMOI134 | ||
| Relationships and communication | Clinical staff | Implementing change requires local (ward) level buy-in and working in partnership across corporate and clinical services | When there are knee-jerk reactions to complaints/inspection and change is implemented in response to stimulus rather than in consultation with staff to see how best to address concern, staff feel disempowered and it creates resistance to implementation | Top-down knee-jerk responses to concerns | Staff understand the rationale for decisions and are able to apply the logic or decision to the local context and adapt when needed. This creates more ownership of the implementation process and is more likely to create change | CMOI14, CMOI33, CMOI34, CMOI69 |
| Staff need feedback on patient experience in a timely manner and at the ward level |
Not getting feedback or not getting it quickly reduces staff motivation to change or maintain good practice in response to feedback. It increases frustration with corporate services. If they receive no feedback on patient experiences at all, ward staff are unable to act to improve quality. Staff (particularly in lower bands) rarely receive analysed patient experience feedback. They feel particularly disempowered and disengaged from the patient experience feedback process in relation to trying to achieve service quality improvement Staff like to get feedback and to promptly take action to make changes. This motivates them to receive feedback |
Delays in receiving patient experience feedback/not receiving patient experience feedback at the ward level | Staff lose the incentive to change practice in response to patient experience feedback | CMOI81, CMOI114, CMOI118, CMOI135, CMOI136, CMOI137 | ||
| Feedback numbers are low in inpatient mental health settings |
Staff find it difficult to implement change in response to patient feedback because so few patients give formal feedback Staff lose confidence that the feedback is useful or representative and so are less likely to make changes based on these data Staff find it difficult to weigh up if they should make changes based feedback from one or two individuals |
Little formal feedback in inpatient settings | Staff are reluctant to make changes based on patient experience feedback and lose confidence in the usefulness of the feedback process | CMOI94 | ||
| Corporate staff | Corporate staff triangulate patient experience data with other outcomes or ratings data. When triangulation is done badly, patient experience data exist in a silo or are aligned to only one type of data (i.e. patient safety data). Triangulation and ‘lessons learned’ often happen only at corporate levels and are either not filtered down effectively or slowly disseminated; this means the sense-making process is not owned locally by wards | Triangulation provides staff with contextual evidence and information to understand why things are happening. This leads to a process of sense-making regarding why things are happening on wards. If triangulation does not take place locally, ward staff do not have the ability to take an overview and understand why things are happening. Triangulating data helps to identify where and what changes need to be implemented | Triangulation with patient experience (i.e. patient stories at board meetings) shows how the individual experience relates to the ratings being shown | Implementing triangulation of outcomes and other data with patient experience data gives the rationale or reason for action; this needs to happen both at the local ward level and at the corporate level to be able to drive quality improvement | CMOI8, CMOI12, CMOI27, CMOI29, CMOI31, CMOI42, CMOI43, CMOI54, CMOI57, CMOI58, CMOI62, CMOI63, CMOI67, CMOI68, CMOI86, CMOI87, CMOI88, CMOI95 | |
| Resources | Clinical staff | There is a dedicated resource (i.e. staff member or team) for patient experience work | Having dedicated resource allows those individuals focused on patient experience to be able to analyse data and observe themes or trends to respond to. It also allows those individuals to think about what might be able to be implemented elsewhere in the trust and to share good practice across wards | Dedicated resource for patient experience. When quality improvement and patient experience information are closely linked in services where they can provide evidence for and demonstrate change, there are often resources (i.e. electronic dashboards and people) dedicated to this work | Having dedicated patient experience resource helps to identify good practice across trusts and to engage staff in thinking about quality improvement in response to patient experience feedback | CMOI30, CMOI59, CMOI60, CMOI63, CMOI66, CMOI98 |
| Corporate staff | Resources not put in place to support implementation and change | Staff can perceive that the change is not valued by corporate services or that it is unimportant and, therefore, fail to implement the change if it is not adequately resourced. Finance to support change is associated with the significance of the intention to change something | No resource from organisation/corporate services to change | Implementation of change does not happen | CMOI21 | |
| Power | Clinical staff | Staff implement change based on patient experience involving feedback from service users | Staff are more engaged if implementation involves service users from the start, as they see them as the recipients of service and experts in the experience of inpatient settings, so staff involve them by ‘having them round the table’ so that staff and service users work together and ‘come up with sort of compromise’. Direct feedback from service users can be viewed as a fresh perspective on systems and processes and, when this is received in a supportive culture, change can be implemented swiftly that is positive for both staff and patients |
Partnership with patients Evidence of co-produced action with service users in trusts (forensic setting) ‘Always events’: service users come up with something that should always happen no matter what Implementation in partnership with patients is more effective when trying to improve services |
There is staff buy-in and traction around the implementation of change based on service user feedback. Implementation is more successful for quality improvement initiatives | CMOI7, CMOI9, CMOI10, CMOI40, CMOI41, CMOI56, CMOI130, CMOI131, CMOI132, CMOI136, CMOI137 |
| Implementing change to improve patient experience links to quality and safety |
Some staff reported being motivated to enhance patient experience so that patients are more compliant, recover more quickly and do not present in difficult or risky ways on the ward (e.g. a lack understanding of the role of empathetic care) Corporate staff indicate that, when things are ‘so worrying’, they are motivated to implement change and improvement in order to ensure that incidents are not repeated. Reductions of violence and aggression are seen as primary motivators in responding to patient feedback |
Safety as a motivation to implement change in relation to patient experience feedback | Some staff report that a motivation to implement change and to improve quality to create a positive experience for patients can be to ensure that patients are ‘compliant’ and this minimises safety issues | CMOI15, CMOI22, CMOI63, CMOI75, CMOI77, CMOI78, CMOI79, CMOI80, CMOI81, CMOI83, CMOI87, CMOI91, CMOI96, CMOI98, CMOI99, CMOI100, CMOI101, CMOI102, CMOI103, CMOI109, CMOI113, CMOI125, CMOI129 | ||
| Corporate staff | Corporate staff monitor patient experience | Corporate staff monitor patient experience champions and ‘You said, We did’ outcomes to understand and try and predict where problems may be occurring to intervene early. Changes are less likely to be successfully implemented top down, but management buy-in and corporate support are important. Patient experience teams are able to analyse and respond to patient experience feedback to identify potential problems as they arise, and to focus on areas that may need improvement. Staff on the ground are able to consider the feedback given and implement change in relation to that feedback because the information is accessible to them. There is also a sense of accountability if this is built into corporate monitoring processes – the two need to work in tandem in order to motivate staff to implement change and enhance their understanding of the reasons behind change. If staff feel that change is only in response to external forces (i.e. not ward factors, for example the CQC, inspection or audit), they are more likely to engage only superficially in implementing change or to not engage with implementation at all, as this is experienced as disempowering and patronising. There is no local ownership and the feedback is seen to serve a corporate rather than a collective function | Corporate strategy in relation to patient experience and monitoring/accountable process needs to relate to local-level ward activity |
Patient experience processes at the ward level alongside monitoring and accountability is helpful in relation to implementation and change in response to feedback When organisational strategy and local ward implementation become ‘divorced’ from one another, this obstructs overarching quality improvement |
CMOI16, CMOI17, CMOI22, CMOI23, CMOI27, CMOI29, CMOI33, CMOI34, CMOI35, CMOI46, CMOI47, CMO148, CMOI55, CMOI56, CMOI60, CMOI69, CMOI70, CMOI72, CMOI81, CMOI84, CMOI95, CMOI99, CMOI100, CMOI101, CMOI102, CMOI103, CMOI104, CMOI105, CMOI106, CMOI108, CMOI116, CMOI122, CMOI124, CMOI125, CMOI126, CMOI127, CMOI128 | |
| Corporate staff explain to ward staff their motivation(s) and the audience(s) for patient experience feedback | Staff engage with patient experience work to implement change, in part motivated by fear of when things go wrong. Corporate teams explaining that they are answerable to external audiences engages staff in patient experience work, as they can understand the wider system pressures and why information is being sought, which also means that they engage with patient experience work | Patient experience team communicating with staff and responding to queries | Staff implement change with support from corporate patient experience teams | CMOI11, CMOI71, CMOI124, CMOI126, CMOI127, CMOI128 | ||
| Theme | Participants | Context | Mechanism | Outcome | CMO reference code | |
|---|---|---|---|---|---|---|
| Reasoning | Resources | |||||
| Wellness | Clinical staff | Staff can integrate their understanding of a patient’s wellness and feedback in responding to this feedback or changing their behaviour. If they attribute the complaint or feedback raised to an individual’s wellness, they dismiss the content of it |
Staff are subject to criticism and complaint quite frequently in inpatient units. They develop resistance to this and can retreat into a defensive position, particularly when not supported. They discount or dismiss a patient’s experience as a facet of their illness. They use this to become immune to the complaints process, which can otherwise be distressing. An unintended consequence of this is that they can fail to accept patient experience feedback and change in response to it Staff are often reluctant to ask for feedback when they feel that they may be prompting criticism. In part, a patient’s wellness means that staff feel that they are more likely to give negative comments and so do not hand out the forms to get feedback Staff are aware that the expectation around caring for patients and being an inpatient mental health ward is different from that of physical health wards |
Staff are not supported to understand communication from patients | Staff may dismiss patient experience feedback and fail to change practice in response to this feedback | CMOCh94, CMOCh140, CMOCh148, CMOCh246, CMOCh264, CMOCh275, CMOCh285 |
| Staff acknowledge that getting reliable feedback is difficult. One patient’s story (often linked to a complaint) may be important, but so may multiple survey responses. Weighting feedback to determine action is difficult |
Staff find it difficult to decide what weight to give to collective feedback from multiple people versus one person’s complaint when deciding what should drive change Staff find that the difficulty of deciding what weight to give feedback makes it difficult to ‘rely’ on feedback. When this is done well and patient experience staff are in place to analyse this information, the reasons behind deterioration or improvement in quality on wards become clearer, which enables changes to be enacted. There are times, for example when patients are restrained, when staff find getting feedback on practice particularly difficult |
Making change in response to feedback requires analysis of both individual patient experiences (including complaints) and collective responses to questionnaires | When feedback from different sources is given carefully considered weighting to inform priorities for action for change, patient experience feedback can be used to understand quality on wards that are deteriorating or improving | CMOCh111, CMOCh112, CMOCh151, CMOCh155 | ||
| Importance of feedback/seeing changes | Service user | A lack of visible change in response to patient experience feedback leads to patients not believing that change is possible/will happen | Patients think that change is either not possible or not going to happen. A lack of visible change decreases motivation and creates apathy about giving experience feedback. It is experienced as disempowering and pointless to engage in giving feedback. When the point of feedback is not explained, patients do not engage in giving it (e.g. by attending meetings). Patients need to understand how feedback is going to be used to make a difference (for themselves or others) as a motivation for giving honest feedback. When feedback is given and nothing happens, patients can feel patronised or as though they are being placated rather than listened to. This is also dependent on the length of stay in hospital – if patients do not feel that they are going to be in hospital for a long time, and are therefore not going to be around to see any changes being made, they are less motivated to give their patient experience feedback | No changes made in response to patient experience feedback | When change is not made in response to their feedback, patients stop giving feedback | CMOCh1, CMOCh2, CMOCh3, CMOCh4, CMOCh5, CMOCh6, CMOCh7, CMOCh8, CMOCh10, CMOCh11 |
| Change is made promptly in response to the ‘fear’ of patients | Patients are aware and internalise through experience that particular behaviour (i.e. aggression) gets feedback quicker and so they behave in this way to get things to change | Staff making changes in response to aggressive patients teaches patients that, to make change happen, you need to be aggressive | Patients behave in a logical way in order to get a response (i.e. they are aggressive to get change) | CMOCh13 | ||
| When changes are made and patients observe change being made, these are often environmental changes | When patients see change, they feel valued. When change is made, patients internalise this as feeling considered and cared for. However, changes are often environmental and the lack of cultural change can leave patients with the perception that they are not being listened to even though the environment is changing in response to patient experience feedback. The feedback mechanisms (e.g. ‘Have Your Say’ meetings) are often seen as there to raise environmental concerns about the running of the ward rather than concerns that are intrinsic to experience | Change made in response to feedback | Environmental change is more likely to take place in response to patient feedback | CMOCh9, CMOCh10, CMOCh11, CMOCh12, CMOCh14 | ||
| Carer | Carers are interested in quality improvement | Carers are motivated to offer feedback on their friend’s or family member’s experiences, either to change their care or to change services for the future. Carers become frustrated when their suggestions are not attended to, if change is not implemented in response to feedback or if they discover that what they are recommending was meant to be happening as standard practice but that something has not been operating as it should. This motivates carers to complain and generates ill feeling and mistrust | If listened to and responded to appropriately, carers can help in identifying areas for quality improvement in trusts | Carers identify areas for quality improvement | CMOCh20, CMOCh21, CMOCh22, CMOCh23 | |
| Carer feedback is used to make changes | Carers feel they have to explicitly ask to give feedback or demand services/push for change | Staff do not seek experience or feedback from carers and use it to implement change proactively | Change happens because carers push for it | CMOCh15 | ||
| Clinical staff | Making changes to service is much more likely based on negative feedback rather than on positive feedback and change is much more likely to be related to environmental rather than cultural factors | Staff find that they cannot plan actions around positive feedback because they do not find it specific enough, whereas negative comments often come with specific concerns attached. There is no formal recognition of positive feedback, which means staff do not value it, as it is not perceived as valued by the organisation. These concerns are often easier to pinpoint (i.e. complaints about environmental factors); therefore, the change feels easier to make. Nursing staff find it easier to change environmental factors and more uncomfortable to challenge doctors over clinical decision-making or cultures of care, making it less likely that non-environmental factors are prioritised. Staff also are aware that they need to be open to receiving negative feedback rather than resistant to it, as otherwise this impedes change from happening because they deflect the feedback. Positive feedback boosts staff morale, which incentives them to work in difficult conditions and to care for their patients well, but action plans are not developed based on positive feedback to engender change or to change other things while maintaining this good practice. Often the ward environment is what the staff explicitly seek feedback about, as they feel that this is the relevant link or factor in relation to the patient having a good inpatient care experience | Staff action-planning and changing service in response to complaints/negative feedback | Change is more likely in response to complaints or criticism and the changes made are likely to be environmental | CMOCh24, CMOCh55, CMOCh65, CMOCh67, CMOCh68, CMOCh73, CMOCh74, CMOCh80, CMOCh81, CMOCh82, CMOCh84, CMOCh87, CMOCh89, CMOCh90, CMOCh91, CMOCh95, CMOCh96, CMOCh99, CMOCh127, CMOCh134, CMOCh137, CMOCh139, CMOCh141, CMOCh143, CMOCh161, CMOCh166, CMOCh181, CMOCh185, CMOCh192, CMOCh193, CMOCh195, CMOCh239, CMOCh240, CMOCh244, CMOCh245, CMOCh248, CMOCh249, CMOCh255, CMOCh259, CMOCh263, CMOCh289 | |
| Staff do not find a ratings metric useful in prompting change. Often a patient story (qualitative narrative) will have more impact in making change than ratings, particularly at the board level | Staff mistrust the reliability of ratings (which they feel are a snapshot in time) as a way of understanding issues in inpatient settings. They feel that they do not carry as much weight with senior (board) management. The relatability of qualitative feedback and the fact that the board is not able to ignore a patient story are important. Staff do not pay attention to summary metric information because they cannot make meaning from it or apply it directly to the care of inpatients. The personalised ‘I want great care’, publicly accessible and individual ratings for clinicians have caused anxiety, particularly in relation to how these will be responded to and managed by the trust and how staff will be supported in response to public criticism of their individual care | Staff cannot use ratings alone to understand how to change services, nor do they provide sufficient impetus (in relation to action at the board level) to create changes in services | Change is more likely in response to a patient story or qualitative account with examples rather than based on a ratings system (e.g. the FFT). Staff do not see the link between quality improvement and feedback | CMOCh35, CMOCh101, CMOCh102, CMOCh104, CMOCh105, CMOCh106, CMOCh110, CMOCh117, CMOCh125, CMOCh131, CMOCh150, CMOCh155, CMOCh157, CMOCh167, CMOCh171, CMOCh182, CMOCh186, CMOCh218, CMOCh224, CMOCh250, CMOCh251, CMOCh252, CMOCh262 | ||
| Formal and informal feedback generates different kinds of change |
Staff perceive that formal feedback is that which can be collected and acted on (measured or demonstrated), for example feedback on food and change to food. Informal feedback or softer feedback about skills and culture (which is rich in experience data) is not readily captured and is more difficult for staff to use to effect change Feedback from patients on the environment is used to inform change in inpatient settings at a local level Staff enjoy being able to respond locally to patient needs and their feedback, and reflect these in service Collecting metrics centrally (at the corporate level) can sometimes drive how staff engage in patient experience work but, ultimately, the collection of metrics does not lead to change in and of itself |
Staff use predominantly measurable or formal feedback to make changes, and these are often about environmental factors | Change that occurs at the ward level is often environmental | CMOCh47, CMOCh56, CMOCh57, CMOCh60, CMOCh109, CMOCh110, CMOCh228, CMOCh229, CMOCh262 | ||
| Staff do not see changes and do not feel that they can enact or make changes in response to patient experience feedback | Not seeing changes or being able to make changes means staff adapt to the ‘status quo’ and lose motivation to change services or improve quality. Feedback loops close to staff are important in encouraging them to respond to and maintain changes | Staff become apathetic in response to a lack of change or agency to change services | Staff become demotivated and no longer engage to create change | CMOCh210, CMOCh211, CMOCh214, CMOCh235, CMOCh236, CMOCh237, CMOCh241, CMOCh267 | ||
| Corporate staff |
Learning is drawn out from patient experience feedback and shared Staff teams meet together to review and analyse feedback data across wards. This allows comparison across wards and the identification of common themes. This requires dedicated resource (staff and time) and triangulation of types of data Patient safety and complaints data are often triangulated but patient experience data are rarely included |
Ward managers and the community team managers meet to review data. Each team has been sent their specific information beforehand and they have the opportunity to think about this and bring information about the points raised to this forum. The managers then work through the patient experience feedback together to draw out learning across teams. This gives them space for reflection and support. It encourages team building. A balance of good practice and poor practice is sought for inclusion in reports that are then created by the group and circulated more widely. In this way, shared ownership of care quality across wards can be developed and feedback is not individualised, so individual health professionals do not feel that the feedback is personal. Invariably, however, at present, this is largely based on complaints or incidents rather than on the whole patient experience Conversely, when data review meetings and the triangulation of data does not take place, change happens locally as a process of constant small, incremental (largely environmental) changes. These changes are not sustained and are tiring for staff and confusing for patients who may be repeatedly admitted and have to learn new rules or ways of working each time. Change feels tokenistic rather than purposeful and sustainable |
Staff meet to review and triangulate data to draw out ‘lessons learned’ | Changes are implemented and ‘lessons learned’ are communicated across the trust. Without triangulating data, you can get either inertia or cyclical patterns of change without really driving forward quality improvement, as there is not the organisational impetus to drive change across wards and only incremental progress is made | CMOCh145, CMOCh196, CMOCh198, CMOCh199, CMOCh201, CMOCh202, CMOCh203, CMOCh204, CMOCh205. CMOCh234, CMOCh277 | |
| Relationships and communication | Clinical staff | Being able to effectively respond to complaints can create positive change and improve relationships with patients and carers | When staff can engage with complaints constructively, while acknowledging that it feels horrible to receive complaints about yourself, there is better chance of changes being made. This happens when there is not a blaming or punitive organisational culture and there is a more enquiring culture around complaints. In these circumstances, complaints can be a useful source of learning for staff that can prompt them to make changes in service to improve the quality of care. Staff can develop better relationships with carers and patients as a result of them feeling listened to and their feedback being used and useful. When complaints are badly handled, staff feel undermined. Staff need to feel supported and that they have ownership of feedback | Staff engaging proactively with learning from complaints feedback and enacting change as a result of that feedback | Change is implemented following complaints and relationships between patients and carers are improved | CMOCh39, CMOCh87, CMOCh88, CMOCh135, CMOCh168, CMOCh215, CMOCh254 |
| Staff recognise that communication is crucial in their relationship building with patients and that relationships are important to patients’ experience of inpatient care | Communicating with patients about their experience in ways that they can understand (language/literacy) builds the relationship and improves the patient experience, as patients feel that staff care and patients are more likely to trust staff and their care |
Staff recognition that communicating about a patient’s experience of care with a patient is crucial to their experience of care Staff recognition that there may be language, literacy or other barriers that mean that communication is difficult, but overcoming those barriers by making time to communicate with patients using a range of media |
Clear communication improves the patient experience | CMOCh54, CMOCh103, CMOCh123, CMOCh155, CMOCh168, CMOCh242, CMOCh262 | ||
| Staff give patients and carers ‘the perception that we are prepared to listen to them’, namely show an understanding of a patient’s need to see changes. This often manifests itself in only particular feedback being sought (i.e. patients being discouraged from sharing ‘personal’ experiences instead of discussing operational recommendations in ‘Have Your Say’ meetings) | Staff select easier things (environmental factors), such as changing food, to tackle so that they can report back to patients. Staff understand that hospitalisation on inpatient units can be very disempowering and so can rationalise that they want to make practical change in response to feedback in order to try and redress some of the balance. Things that are cultural or take longer are not able to be used to demonstrate change (and listening), and so staff can be less inclined to address these more complex issues | Staff go through the motions of getting feedback and reporting back to patients and carers, without actually engaging in the spirit of feedback and change |
Change is not authentic Inertia or incremental change occurs that does not lead to sustained change or quality improvement |
CMOCh48, CMOCh49, CMOCh52, CMOCh117, CMOCh124 | ||
| The way in which change or the lack of change is explained is important for patients’ experiences of care | Staff recognising that being open and approachable, and then honestly responding to patients to let them know that there is not much that they can do in response to their feedback or how they are going to action it, builds trust and improves relationships between staff and patients | Staff being approachable and honest in communicating about change | Staff/patient relationships are improved, which improves patients’ experience of care | CMOCh50, CMOCh241, CMOCh277 | ||
| Resources | Carer | Change in response to carer feedback is not happening in trusts | Carers perceive that, when change does not happen in the service, this is in part due to staff being overstretched and there not being enough resources in place to make changes | No staff time or availability to change and pressure on resources | Change does not happen | CMOCh16, CMOCh17 |
| Carers perceive that, when there are bank or agency staff, change is less likely | Having higher numbers of bank or agency staff means that there is less consistency in the approach to care, and carers do not know who is coming into the inpatient unit/working with their friend or family member. They feel that this has an impact on relationship building, which means that getting feedback and using this to produce change does not happen as readily | Agency or bank staff being used on inpatient wards | Change does not happen | CMOCh18, CMOCh19 | ||
| Clinical staff | A lack of resource is perceived as the main reason for changes not being made. Staff do not want to continually pass on/report that resource issues are the reason for the lack of change in response to patient experience feedback | Staff do not always communicate to patients the reasons why change has not happened or feedback cannot be acted on. Sometimes they have not thought about the need to explain to patients that there are insufficient resources to enact change. Staff become tired of repeatedly reporting that the main issue is resources and that this is the reason why change is not being made. Staff feel bad about their inability to change things (usually environmental) that they know would enhance a patient’s experience. Staff also find that, when there are inconsistencies about resources or they cannot offer justification for why resources are not available, they are ‘caught’ and that they can readily appreciate why patients feel irritated. Frustration develops and this affects willingness to engage in asking for people’s feedback if the staff and patients cannot see action being taken or make changes in response to feedback. Staff at the ward level perceive that getting ‘feedback to managers’ is essential in accessing the resources to enact change | Staff not having the resources to make changes |
Staff stop reporting why change is not happening to patients in response to their feedback Resource is perceived as the main reason that change does not happen |
CMOch31, CMOCh32, CMOCh41, CMOCh42, CMOCh43, CMOCh44, CMOCh51, CMOCh72, CMOCh79, CMOCh123, CMOCh143, CMOCh174, CMOCh176, CMOCh225, CMOCh226, CMOCh227, CMOCh253, CMOCh274 | |
| Staff do not have the resources (time) to learn from feedback in order to create change | When dedicated time is not made for patient experience (collecting, analysing and implementing change in response to feedback) then staff do not prioritise this in their work. Either staff develop resistance to seeking or listening to feedback because they perceive that it takes a lot of time that they cannot afford or do not have, or they develop a resistant culture perceiving that it is not core to their role, while acknowledging that ‘listening’ is important. This results in staff not understanding the importance of using patient experience feedback in relation to their planning and remain in a firefighting mentality. Even when the systems for cascading metrics and collated data are in place, time is needed for staff to be able to digest, understand and make use of those things | Staff are not able to prioritise/the wards or the trust does not prioritise staff taking the time to learn from feedback to be able to change | No resource (time) to analyse and respond to feedback (change) means that changes are not enacted in response to feedback. This is bad for staff morale and creates deterioration in the patient relationship owing to changes not being made and this being perceived as feedback not being listened to. There is an awareness that, to enact cultural change, staff need longer to digest and think about how to change and to invest time in bringing other staff members on board. When resources are not dedicated to feedback, cultural change is less likely to be possible | CMOCh63, CMOCh78, CMOCh115, CMOCh120, CMOCh122, CMOCh125, CMOCh131, CMOCh147, CMOCh156, CMOCh163, CMOCh176, CMOCh251, CMOCh265, CMOCh268, CMOCh274, CMOCh279 | ||
| Responding to feedback to create change requires data to be available in a timely manner at the ward level and this is usually when there is a dashboard/electronic feedback system in place | Staff enjoy being able to see data in a timely manner. They also appreciate detailed data that are broken down, as this helps them to interpret or understand the data in order to support planning and ultimately to make any changes at the ward level. It gives staff more ownership of the information | Patient experience data-capture systems allow staff at the ward level to see data in a timely manner | This supports staff to engage with patient experience data and makes it accessible for planning and change | CMOCh165, CMOCh167, CMOCh169, CMOCh171, CMOCh186, CMOCh198 | ||
| Corporate staff | There are not the tools or resources (staff) available to manage the volume of qualitative feedback received or to feed this back to wards that can review this and implement local change based on this feedback | Staff make decisions about how to filter comments and, in doing so (as opposed to listening to the wider complaint) look for explicit examples of things that can be improved. This is so that they do not become overwhelmed by the volume of data | Staff resource or tools not available to utilise feedback | Change is not made through robust analysis of qualitative feedback | CMOCh118, CMOCh125, CMOCh262 | |
| Power | Clinical staff | Feedback gets sent to corporate services but feedback does not come back to ward staff directly; learning is not shared across wards | Staff find that they do not understand where feedback goes or how it is used, and they do not get a response when it is sent centrally so they do not know how to enact change based on that feedback if there has been no communication from corporate services, which leads to them feeling disempowered and inertia and makes them feel they are held back/trapped/inadequate in their responses to patients. Staff rarely get to see analysed or other data. If they do not understand why they are collecting data, they are more reluctant to do so and disengage from the process. When feedback is given back to ward staff, it is often when there is a dedicated patient experience resource/person who liaises directly with the ward staff such as a matron with patient experience remit. When positive practice is observed, this is not collected, collated and circulated so staff do not know what changes are being enacted on other wards. Staff would like feedback so that they can use it to make changes and understand how the care they are delivering is received. Staff need to feel they have ownership of feedback. There is a fundamental disconnect in the way in which staff understand how patient experience feedback is used to improve quality – corporate staff often cite feedback being sent to wards; however, very few staff see or describe using this feedback to create change. When learning is shared, there is direct resource (staff) in place to try and translate good practice across wards. Staff engage more with patient experience feedback when they can take some ownership for responding to it. Very often, staff describe information cascading down or being sent up – denoting the power hierarchy and way in which this information and responsibility for this information is perceived. Change needs to happen and be driven at all levels; staff across the organisation need to mobilise change. Feedback needs to be a loop to enable people to do this | Staff do not get responses to patient experience feedback that are sent centrally, and positive practice is not shared across wards. Corporate staff often use these data for quality assurance rather than for quality improvement to drive change at the ward level | Action and feedback can be escalated to the corporate level, but staff at the ward level often do not know what happens either to or as a result of that feedback. This demotivates them in relation to collecting the data, and change does not get enacted either. If change is escalated upwards, this delays the process of getting or making changes at the ward level. Positive practice similarly is not disseminated across the trust. This makes change local/siloed/incremental rather than linking to an overall quality improvement strategy. Change is top-down rather than bottom-up driven | CMOCh25, CMOCh26, CMOCh29, CMOCh30, CMOCh58, CMOCh62, CMOCh64, CMOCh65, CMOCh66, CMOCh70, CMOCh71, CMOCh74, CMOCh75, CMOCh76, CMOCh77, CMOCh82, CMOCh83, CMOCh84, CMOCh85, CMOCh86, CMOCh88, CMOCh92, CMOCh99, CMOCh100, CMOCh107, CMOCh108, CMOCh113, CMOCh117, CMOCh119, CMOCh121, CMOCh122, CMOCh128, CMOCh129, CMOCh138, CMOCh139, CMOCh149, CMOCh150, CMOCh154, CMOCh158, CMOCh159, CMOCh160, CMOCh164, CMOCh167, CMOCh170, CMOCh173, CMOCh175, CMOCh176, CMOCh177, CMOCh180, CMOCh184, CMOCh186, CMOCh187, CMOCh191, CMOCh194, CMOCh197, CMOCh198, CMOCh200, CMOCh204, CMOCh209, CMOCh212, CMOCh213, CMOCh216, CMOCh217, CMOCh218, CMOCh219, CMOCh220, CMOCh221, CMOCh222, CMOCh223, CMOCh230, CMOCh231, CMOCh232, CMOCh233, CMOCh238, CMOCh243, CMOCh247, CMOCh250, CMOCh255, CMOCh256, CMOCh266, CMOCh267, CMOCh269, CMOCh270, CMOCh271, CMOCh272, CMOCh273, CMOCh276, CMOCh280, CMOCh281, CMOCh282, CMOCh283, CMOCh287, CMOCh290, CMOCh291 |
| Staff are aware of the importance of demonstrating change in response to patient feedback. Changes made in co-produced ways may lead to better engagement from staff | Staff are aware that patients lose hope or faith in the process if they do not see changes as a result of their feedback. Better engagement in services is as a result of listening, compromise and change. Staff are aware that sometimes it can feel disempowering for patients and coercive when there are blanket rules or when there is not enough flexibility in relation to feedback to allow changes. When changes are made based on patient experience feedback and change is co-produced with patients, staff report better outcomes and cultural changes rather than solely environmental changes. Staff engagement is crucial to getting cultural change | Staff respond to patient experience feedback to make changes | Staff and patients engage better within services | CMOCh27, CMOCh28, CMOCh29, CMOCh98, CMOCh126, CMOCh152, CMOCh153, CMOCh154, CMOCh159, CMOCh206, CMOCh207, CMOCh208, CMOCh241, CMOCh267, CMOCh280, CMOCh284, CMOCh286, CMOCh288, CMOCh291 | ||
| Co-production and codesign of services often remain at the strategy level or advising on documents/recruitment | Co-production is usually experienced as being something that relates more to corporate rather than clinical environments. Co-production is more likely in longer-term forensic/rehabilitation settings. Ward staff do not feel that they engage in co-design or co-production | Staff do not engage in co-production or co-design at the ward level | Staff are rarely involved in authentic co-production/co-design in inpatient settings; this is more likely to happen in relation to strategy or corporate management settings | CMOCh33, CMOCh34, CMOCh36, CMOCh37, CMOCh38, CMOCh40, CMOCh172 | ||
| The main drivers of change are complaints, serious incidents, external audit, targets and inspection (i.e. the CQC) | Staff perceive that change is mandated from the top down (which is disempowering) and is in response to external pressure or risk (i.e. safety issues, the CQC or audit). This can sometimes be ‘knee-jerk’ and feel reactive and top down, which means that staff can sometimes feel resistant and that the changes being made are not necessarily patient led or in the best interest of the ward. Staff sometimes do not agree with or understand the rationale for particular changes and struggle to relate these to their working practice. There is more support for patient- or local ward-led changes. When there is a blaming culture, staff experience fear in relation to patient feedback and complaints, and an ‘us and them’ culture between corporate and clinical staff develops. The experience can be disempowering for staff who want to be able to respond to feedback and make changes locally. Staff develop resistance when they feel ‘hounded’ for patient experience information (data) and then get feedback only in response to serious concerns. Staff are receptive to being held accountable to feedback and are more willing to engage in obtaining and responding to changes in services if they feel that there is a supportive culture centrally in corporate services. If this culture does not exist, staff develop feelings of being persecuted and that their views or operational needs are dismissed, which operates to disincentivise them to collecting or responding to patient experience feedback in the first place other than as a perceived duty or as the right thing to do to listen to patients. This creates an inauthenticity in the way they elicit feedback and subsequently respond | Staff change in response to management pressure – corporate staff and clinical staff have different objectives and understandings of priorities in relation to the use of patient experience data | Change happens top down often in response to external pressure and does not have staff buy-in; it is also not led by patient experience | CMOCh45, CMOCh46, CMOCh58, CMOCh59, CMOCh60, CMOCh61, CMOCh68, CMOCh71, CMOCh95, CMOCh97, CMOCh114, CMOCh116, CMOCh130, CMOCh131, CMOCh132, CMOCh133, CMOCh136, CMOCh137, CMOCh142, CMOCh144, CMOCh147, CMOCh156, CMOCh162, CMOCh175, CMOCh177, CMOCh178, CMOCh179, CMOCh188, CMOCh189, CMOCh190, CMOCh196, CMOCh200, CMOCh202, CMOCh232, CMOCh256, CMOCh257, CMOCh258, CMOCh260, CMOCh261, CMOCh278 | ||
| Staff address the culture of caring by recognising that, to improve this culture, patient voice and partnership are essential |
Staff recognise that a culture of care that is person centred in which patients are listened to makes gathering and collecting patient experience feedback easier and more useful To change the culture, they need to change how they ‘view patients’ and how they ‘manage what’s going on for them’. Staff have engaged in redefining the nursing role through trying to be less restrictive (particularly around medication), instead being more collaborative. This involves staff shifting their thinking about their role and sharing power or the responsibility of care with the patients. This is described as ‘being with’ rather than ‘doing for’. This enhances the patient’s experience of care |
Staff address the culture of care to improve the quality of the patient experience in the inpatient setting | To change or shift the culture, there needs to be some power-sharing with patients | CMOCh53, CMOCh69 | ||
| There are some staff who are resistant to the idea of changing their practice in relation to patient feedback | When staff are resistant to using patient experience feedback to change services, this is perceived as a threat to their professional role and as challenging their professionalism. To get staff to take on board feedback and effect practical change, this needs to be addressed. Feedback is perceived as based on personal preferences in relation to the staff member and not linked to the way in which they deliver care. These attitudes can exist in trusts in which there are processes to encourage patient experience feedback to be shared and used. Changing cultures within staff groups therefore requires addressing these underlying mechanisms | Staff refusal to acknowledge or use patient experience feedback | No change in response to patient experience feedback and no engagement with that feedback | CMOCh87, CMOCh93 | ||
Appendix 17 Analysis: work package 4 supplementary data – programme theory development tables
These tables give an overview of the programme theory development. A full Excel spreadsheet can be found online in the supplementary materials (see Report Supplementary Material 10).
| Original programme theories from the bid | Programme theory refinement for WP1: themes from the literature review | Programme theory refinement for WP2: flash cards developed for WP3 interviews | First refinement (post WP3) | Programme theory refinement for WP3: rules developed based on WP3 and analysis of CMOs | First refinement (post WP4) | Final programme theories (reiterated rules post WP4) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Collecting service user (CSU) data | Collecting staff (CS) data | Collecting system (CST) data | Service user/carer | Staff | System | Data | Facilitators | Barriers | Iterations/changes through discussion at the consensus conference | ||||
| CSU1: we do not know what kinds of feedback are most important (protocol) | CS1: we do not know what management processes are needed to translate this into effective action plans (protocol) | CST1: we do not know if this makes any difference to patients themselves (protocol) | Importance of high-quality relationships: the importance of high-quality relationships was the most commonly reported theme, with staff–patient relationships representing the ‘back bone’ of patient experience, with good experiences reported when staff were compassionate, caring and respectful, engaging the patient in ways that helped them feel valued and understood. High-quality relationships also had an important role in recovery and in reducing the use of coercive measures. Therefore, the role of staff in creating high-quality environments and in enabling patient-centred care was key. In terms of enhancing future care, improving the initiation and the development of meaningful staff–patient relationships, particularly through conversation and listening to the patient, could have an important impact on care. In addition, developing better endings to relationships at the point of discharge could also contribute to a higher-quality experience | Communication and trust: if I can understand my loved one’s condition and the planned treatment and I am informed, I can contribute to their recovery | Patients can tell us about their experiences no matter how ill they are; however, if unwell, they can share experiences only at an individual level (e.g. I’ve had a good or a bad day) | Episodes of poor care that are collected on the wards informally need to be integrated to understand patient experience more broadly in order to support sustainable change/quality improvement | C1: Always ask about a patient’s experience. Patients can tell us about their experiences no matter how unwell they are. However, if feeling very unwell, they can share experiences in only a more limited way (e.g. ‘I’ve had a bad/good day’) | Timing is critical (e.g. when no other distractions, immediate needs are met); all staff be ready to ask but be flexible about who asks whom; multiple opportunities – formal and informal, structured and unstructured; some staff protected time – staffing issues will prevent rule, implication; more money for mental health; Clinical Commissioning Groups should be commissioning patient experience feedback; needs to be opportunity to give feedback after discharge – may be months later; independent advocate (not a volunteer, not funded by trust) might be trusted by a patient who is feeling vulnerable and wants to give feedback; patient experience data being collected by organisations external to the trust – feedback to the trust is anonymous | Funding to implement change/Clinical Commissioning Group does not commission mental health; staff understanding of feedback – informal and formal | Timing is critical; there are multiple opportunities, not just at discharge. But must include options for after discharge; all staff be ready to ask but be flexible about who asks whom; inclusive of formal and informal ways |
Rule C1: always ask about a patient’s experience Evidence: patients can tell us about their experiences no matter how unwell they are. However, if feeling very unwell, they can only share experiences such as ‘I’ve had a bad/good day’ |
||
| Relationships between staff and service users: I do not care who asks for my feedback as long as I get a chance to say/share it | As patients progress (half way into admission/wellness) they can reflect on the environment | Collecting patient experience data needs to happen using a range of media – choice of medium needs to be personalised to the individual | C2: Make sure you get both positive and negative patient experience feedback. Patients being asked for feedback, feeling listened to and heard, and knowing that feedback is being made use of are essential to improving the quality of services. Feedback from patients is often both negative and positive. Taking note of positives helps strengthen good practice and avoids bad practice. Not understanding positive feedback is not just a lost opportunity, it is disempowering for patients | Have a process and training on how to look at data or share data with the team. A mind set to look at positive and negative feedback and put both up on ward; by highlighting positive feedback, staff more are likely to ask for feedback; collect and use neutral feedback too; present positive and negative feedback in meetings; parity of esteem of positive and negative; when asking individuals about feedback, ask if they give positive or negative feedback, or vice versa; work hard to collect and collate positive feedback to counter the obligation to report negatives; err on the side of assuming that the negative comments are not linked to the illness | Clearly identify a process and training; gathering positive feedback may motivate staff to collect feedback | Staff need training; obligation to report negatives; wellness | Need to get a balance and enquire about both (when asking individuals about feedback, ask if they give positive or negative feedback, or vice versa) |
Rule C2: make sure you get both positive and negative patient experience feedback Evidence: patients being asked for feedback, feeling listened to and heard, and knowing that feedback is being made use of are essential to improving the quality of services. Feedback from patients is often both negative and positive. Taking note of positives helps strengthen good practice and avoids bad practice. Not understanding positive feedback is a lost opportunity and is disempowering for patients |
|||||
| The timing of giving feedback and wellness: there is a need to distinguish very clearly whether it is a first admission or a subsequent admission | Just prior to discharge or on discharge, patients can reflect on their experience as a whole | C3: ask for feedback in varied ways at different times. Different sorts of feedback need to be collected at different intervals during admission. During admission (particularly involuntary admission), patients can give feedback on their individual experiences of care despite being unwell. To provide meaningful feedback about the ward environment, patients need to have reached a point of recovery, which varies by person, but typically occurs part-way through their admission. Patients want to give honest feedback about the staff, the culture and their overall experience only at the end of their admission as they are being discharged. Many patients fear that giving feedback will influence their clinical care and hence may be anxious about doing so prior to discharge. People do not always wish to be contacted to give feedback once they have left inpatient services | Carers can be a good source of feedback with a different perspective; put it all together (e.g. CQC reports, staff and patient governors, Healthwatch, carers, independent health, third-sector organisations, advocates) with patient feedback; regular meetings with all the organisations that collect or collate feedback – or bring together reports; look at overall trends but also individual feedback for nuggets that may otherwise be missed; variety of ways of collecting data – verbal, written, anonymous, electronic (i.e. iPad, meetings/individuals) and different timings (at different times?); multiple ways (e.g. meetings, iPad, personalised, surveys, ward-based community groups), also see feedback from other channels, volunteers in wards doing surveys; anonymous process as well as other routes; need resources to bring different sources of feedback together then present it in an understandable way | Resources; systems and ways to collect in multiple ways; trends vs. individual | Inclusive of carers (links carers when they are not included in the rules); to allow for triangulation (links to the whole loop) but this also links to a need for multiple systems and mechanisms – we need to consider in this rule; need to mention the variety of ways of collecting to suit patient needs/preferences and to consider anonymity |
Rule C3: ask for feedback in varied ways at different times Evidence: different sorts of feedback need to be collected at different intervals during admission. During admission (particularly involuntary admission), patients can give feedback on their individual experiences of care despite being unwell. To provide meaningful feedback about the ward environment, patients need to have reached a degree of recovery, which varies by person, but typically occurs part-way through their admission. Patients want to give honest feedback about the staff, the culture and their overall experience only at the end of their admission as they are being discharged. Many patients fear that giving feedback will influence their clinical care and hence may be anxious about doing so prior to discharge. People do not always wish to be contacted to give feedback once they have left inpatient services |
|||||||
| Organisations that innovate also value information, and we anticipate that those that use patient experience data most effectively will also be the ones with the most robust data-collection strategies (protocol) | When asking for feedback, we need to consider how well the person is and if we are giving them a sufficient range of ways to give feedback. If we collect patient experience feedback on wards, we have a ‘captive audience’ | C4: personalised care is valued and the same applies to obtaining feedback. Patients often report feeling ‘dehumanised’ by the process of admission. They wish to be ‘treated as an individual’. Feedback opportunities need to be personalised. Patients need to feel valued and listened to. Relationships with staff are important. Patients report that they are more likely to give honest feedback to people who they perceive as kind and caring. Staff need to have time to get to know and communicate with patients about their experience | Carers can be a good source of feedback with a different perspective; put it all together (e.g. CQC reports, staff and patient governors, Healthwatch, carers, independent health, third-sector organisations, advocates) with patient feedback; regular meetings with all the organisations that collect or collate feedback – or bring together reports; look at overall trends but also individual feedback for nuggets that may otherwise be missed; variety of ways of collecting data – verbal, written, anonymous, electronic (i.e. iPad, meetings/individuals) and different timings (at different times?); multiple ways (e.g. meetings, iPad, personalised, surveys, ward-based community groups), also see feedback from other channels, volunteers in wards doing surveys; anonymous process as well as other routes; need resources to bring different sources of feedback together then present it in an understandable way | Resources; systems and ways to collect in multiple ways; trends vs. individual | Inclusive of carers (links carers when they are not included in the rules); to allow for triangulation (links to the whole loop) but this also links to a need for multiple systems and mechanisms – we need to consider in this rule; need to mention the variety of ways of collecting to suit patient needs/preferences and to consider anonymity |
Rule C4: personalised care is valued and the same applies to obtaining feedback Evidence: patients often report feeling dehumanised by the process of admission. They wish to be treated as an individual. Feedback opportunities need to be personalised. Patients need to feel valued and listened to. Relationships with staff are important. Patients report that they are more likely to give honest feedback to people who they perceive as kind and caring. Staff need to have time to get to know and communicate with patients about their experience |
|||||||
| It is good to look across data and begin developing more sophisticated analysis but initially the priority is getting/collecting the feedback | Patients on their first admission do not understand ward culture or ways to give feedback, making it harder to gather their patient experience data |
Rule C5: seeing changes based on both positive and negative feedback is important for patients, carers and staff Evidence: both positive and negative patient experience feedback needs to be obtained. Patients being asked for feedback and feeling listened to and heard needs to be accompanied by feedback driving change. Patients, carers and staff knowing that feedback is being made use of is essential to improving the quality of services |
|||||||||||
| When ward culture is poor, the patients are reluctant to give feedback (safety) | Agency staff are less likely to collect/receive/act on patient experience feedback. In part, this is because they do not receive anything back | Organisations with disconnect between their organisation- and ward-level patient experience management have poorer levels of embedded patient experience work |
Rule C6: trusts must engage carers proactively in the inpatient care of the person they care for and staff must communicate to obtain feedback from carers Evidence: carers’ feedback can by a fruitful way of gathering intelligence about the quality of the care being provided. Carers will give honest feedback only if they trust that it will not affect the clinical care of the person they care for |
||||||||||
| In organisations in which staff have little patient contact time, this can act as a barrier to both the giving and the receiving of feedback (relationship and trust) | Levels of embeddedness of patient experience work influence quality improvement initiatives and link to patient experience feedback | ||||||||||||
| When staff do not receive feedback from patient experience feedback, they are less likely to collect/receive/listen to patient experience | Organisational/corporate willingness to accept and act on patient experience feedback influences staff members’ willingness to receive it and pass it on (directional) | ||||||||||||
| Staff who fail to see change as a result of passing on feedback are more reluctant to obtain it in future | |||||||||||||
| In unsupportive cultures, staff resist collecting and receiving feedback or are selective of who they choose to receive feedback from. In some cases, feedback is not passed on in a culture that is felt to be punitive by staff | |||||||||||||
| Staff in resource pressured situations (un)consciously communicate these pressures to patients who respond negatively in a series of ways (e.g. escalating risk to elicit attention and communication through risky behaviours) or withdraw (e.g. not wanting to be burdensome) | |||||||||||||
| Understanding and prior experience = reluctance to obtain patient experience? | |||||||||||||
| Directly inverted logic of understanding around key issues (i.e. data being held locally or centrally to facilitate confidentiality or inpatients being a ‘captive audience so this is where the best data comes from’ vs. ‘inpatient facilities are where the worst data comes from because people are too sick to participate’) (first iteration changes) | |||||||||||||
| CSU2: organisations that are genuinely patient-centred will also demonstrate investment in and adoption of co-design approaches to service improvement, and will involve service users and carers meaningfully, as partners. Feedback from patients can be perceived as critical or threatening by professionals, and may be avoided or denigrated. Co-design is a partnership approach that neutralises perceived threats through collaborative working to find mutually agreeable solutions to problems or difficulties experienced by patients when receiving care (protocol) | Authentic experience of patient-centred care: authentic experiences of patient-centred care should recognise the importance of treating patients as individuals, with their perspectives, previous experiences, preferences, gender, ethnicity and religion understood and accounted for. Key components of patient-centred care include sufficient timely information about diagnosis, treatment, treatment plan and choices. Relationships were often the conduit of patient-centred care, which started at admission and continued until (and sometimes past) discharge | Staff who spend most of their time patient facing (i.e. health-care assistants and domestics) are not incorporated into patient experience processes (could be disproved: communication) | |||||||||||
| Solutions are not co-produced and analysis and problem-solving excludes patient input | When there is a close relationship between corporate and ward staff and patient experience is more embedded, quality improvement initiatives are more likely to be successful | The majority of patient experience feedback is resolved locally (informal). Serious incidents/complaints are escalated | |||||||||||
| Poor communication of the results of analysis to staff locally means change/quality improvement does not get back locally throughout the system | Analysis is descriptive/themed, which often leads to responding only to environmental rather than cultural concerns or major/minor themes | ||||||||||||
| Staff time to engage in the analysis and interpretation of results affects the effectiveness of quality improvement driven by patient feedback | Analysis and solutions are not person-centred; some analysis leads to changes that are not conducive to wards improving quality | ||||||||||||
| Theming is not analysis and staff struggle to develop action plans against general statements | |||||||||||||
| Change happens at the ward level | |||||||||||||
| Original programme theories from the bid | Programme theory refinement for WP1: themes from the literature review | Programme theory refinement for WP2: flash cards developed for WP3 interviews | Programme theory refinement for WP3: rules developed based on WP3 and analysis of CMOs | First refinement (post WP4) | Final programme theories (reiterated rules post WP4) | ||
|---|---|---|---|---|---|---|---|
| Data | Facilitators | Barriers | |||||
| RST1: despite a surfeit of routinely collected patient experience data, most are of limited value either because of methodological problems (including poor or unknown psychometric properties or missing data) or because existing measures lack granular detail (protocol) | Averting negative experience of coercion: the second theme focused on coercion and averting negative experiences of coercion. Experiences of coercion included sedation, seclusion and restraint. Some patients reported very distressing experiences that overwhelmed them, particularly if they did not understand the reason why it was happening. Patients sometimes recognised a need for different forms of coercion, but still expected to be valued, understood and treated professionally with their rights protected. The potential for intense distress caused by coercion creates particular challenges for collecting experience data and highlights the need for the co-production of data-collection systems that facilitate feedback in contexts in which patients are inpatients and fear reprisal | The FFT lacks qualitative data, but it is easier and more accessible than other methods. As FFT data are generally positive, the FFT is not as useful as qualitative/complaints data | R1: staff need protected time to obtain feedback. All ward staff should have protected time to spend with patients. Spending time with patients builds rapport and trust to enable more honest feedback. Staff want to do this but often report being too busy. People give authentic feedback only if they feel comfortable and confident to do so. Staff availability (both emotionally and physically) is integral to getting honest and open feedback | Collect via non-clinical workers (e.g. peer support), (+)does not draw clinical staff away from clinical work, (–)not the same opportunity to give feedback in trusting relationship. Use preparation for review meetings to collect feedback, (+)makes use of regular event, (–)this is an anxiety-provoking event. Protected one-on-one time, (+)builds relationship, needs appropriately resourced units. Informal walk-and-talk (e.g. escorted leave, (+)good use of this time), (–)difficult to record these data | Collect via non-clinical workers (e.g. peer support), (+)does not draw clinical staff away from clinical work. Use preparation for review meetings to collect feedback, (+)makes use of regular event | *Collect via non-clinical workers (e.g. peer support) (–) not the same opportunity to give feedback in trusting relationship *Use preparation for review meetings to collect feedback *Resources *Informal walk-and-talk (e.g. escorted leave) difficult to record these data |
Rule R1: Staff need protected time to obtain feedback Evidence: All ward staff should have protected time to spend with patients. Spending time with patients builds rapport and trust to enable more honest feedback. Staff want to do this but often report being too busy. People give authentic feedback only if they feel comfortable and confident to do so. Staff availability, both emotionally and physically, is integral to getting honest feedback |
| R2: all staff have a role in receiving, listening and responding to feedback. All staff have a role in receiving patient experience feedback. Collection of patient experience information can be seen as ‘not my role’. There are particular situations in which this is more likely – agency staff who are not included in patient experience collection activities or for whom the feedback on the wider organisation may not be perceived as meaningful. When patient experience information is escalated to management without local ownership of the feedback or resolution, ward staff can feel disengaged from the process. Those who are in lower-band roles are often the ones who receive the most informal patient feedback and distribute formal patient experience tools. They are the least likely to receive the results of feedback or to be involved in acting on it | Processes and values reflected in: recruitment, training, supervision, appraisal, (+)embeds expectation in culture, (–)needs driver/DHSC/incentive (e.g. FFT). Analogy to risk or FOI,174 can be local variation, but everyone should know local policy and enact, (+)universal, (–)burden, (–)difficult for subcontractors. Have a means for everyone to be heard; tools (e.g. ‘green button’ staff and postcard patient), opportunities (e.g. community meetings, co-production/improvement processes) and dialogue (not debate). Listening and communication skills to know what they are hearing – different targets/types of feedback | Have a means for everyone to be heard; tools (e.g. ‘green button’ staff and postcard patient), opportunities (e.g. community meetings, co-production/improvement processes). Embeds expectation in culture. Analogy to risk or FOI,174 can be local variation, but everyone should know local policy and enact, (+)universal | (–)Needs driver/DHSC/incentive (e.g. FFT). Burden. Difficult for subcontractors. Listening and communication skills to know what they are hearing – different targets/types of feedback. Dialogue (not debate) |
Rule R2: all staff have a role in receiving, listening to and responding to feedback Evidence: collection of patient experience information can be seen as ‘not my role’. There are particular situations in which this is more likely, for example agency staff. Those who are in lower-band roles are often the ones who receive the most informal patient feedback and distribute formal patient experience tools. They are the least likely to receive the results of feedback or to be involved in acting on it. When patient experience information is escalated to management without local ownership of the feedback or its resolution, ward staff can feel disengaged from the process |
|||
| R3: staff should be supported to receive feedback. The inpatient mental health setting is emotive and challenging. Staff need to be supervised and well supported so that they have the capacity to listen to and receive patients’ experiences. Supportive cultures motivate and retain staff and there is greater engagement in patient experience work. Staff are less likely to seek open and honest feedback if they perceive that they are operating in a blaming culture or that they cannot do anything to support those individuals who are offering feedback. Staff need to be encouraged to receive positive and negative feedback. Priority is given to negative feedback so staff are often unable to see the value of positive feedback. Complaints and compliments need to be viewed as equally valuable sources of data | If all staff, all need to be supported to receive and respond to feedback. Clinical supervision. Training in communication and how to receive feedback. Positive and negative are equal in weight and same systems. Whole-system approach – organisation level. Support includes supervision, (–)expensive, (–)subcontractors. Training in communication, (+)universal service, improvement (–)expensive. Understanding, feedback (weight, target, stepping back, avoiding, defensiveness). Mechanisms for showcase at the ward level | Creates a universal approach to patient experience. Clinical supervision. Training in communication and how to receive feedback. Positive and negative are equal in weight and same systems | All staff need to be supportive, requires a whole-system approach and support from the organisation level. Support includes supervision, (–)expensive, (–)subcontractors. Training in communication, (–)expensive. Understanding, feedback (weight, target, stepping back, avoiding, defensiveness) |
Rule R3: staff should be supported to receive feedback Evidence: the inpatient mental health setting is emotive and challenging. Staff need to be supervised and well supported so that they have the capacity to listen to and receive patients’ experiences. Supportive cultures motivate and retain staff and there is greater engagement in patient experience work. Staff are less likely to seek honest feedback if they perceive that they are operating in a blame culture or that they cannot do anything to support those who are offering feedback. Staff need to be encouraged to receive positive and negative feedback. Priority is given to negative feedback so staff are often unable to see the value of positive feedback. Complaints and compliments need to be viewed as equally valuable sources of data |
|||
| R4: staff need to be able to respond to feedback that is received. There must be clear guidelines for the use of all types of patient experience feedback. Staff should know what to do with informal and formal feedback as well as where to report it. Staff become demotivated when they receive feedback but have no clear pathway to escalate concerns | Staff need to be able to respond to feedback. Idea: cultural top down, not penalised, complaints an opportunity to learn, (+)trust induction, top down, (–)formal systems not good for non-complaints or formal feedback. Idea: two levels of feedback – formal and informal – both equally important; informal is bread and butter work, need clear systems for both (–)not always recorded, no clear system, do people realise this is feedback and do something with it? Idea: mechanisms to respond to show it has been dealt with (e.g. ‘You said, We did’, feedback in meetings, intranet/showcase) | Creates culture in which complaints are an opportunity to learn, (+)trust induction | Requires cultural change without penalisation, difficult as top down (–)formal systems not good for non-complaints or formal feedback. Formal and informal – both equally important; informal is bread-and-butter work, need clear systems for both, (–)not always recorded, no clear system, do people realise this is feedback and do something with it? Idea: mechanisms to respond to show it has been dealt with (e.g. ‘You said, We did’, feedback in meetings, intranet/showcase) |
Rule R4: staff need to be able to respond to feedback that is received Evidence: there must be clear guidelines for the use of all types of patient experience feedback. Staff should know what to do with informal and formal feedback, as well as where to report it. Staff become demotivated when they receive feedback but have no clear pathway to escalate concerns |
|||
| Original programme theories from the bid | Programme theory refinement for WP1: themes from the literature review | Programme theory refinement for WP2: flash cards developed for WP3 interviews | First refinement (post WP3) | Programme theory refinement for WP3: rules developed based on WP3 and analysis of CMOs | First refinement (post WP4) | Final programme theories (reiterated rules post WP4) | |||
|---|---|---|---|---|---|---|---|---|---|
| Data | Facilitators | Barriers | |||||||
| ARST1: there is a dearth of evidence about the processes required to analyse, interpret and translate these data into tangible actions, better outcomes for patients and more efficient and cost-effective care (protocol) | A healthy, safe and enabling physical environment and ward milieu: a healthy, safe and enabling physical environment and ward milieu represented the third theme, which included the atmosphere, the culture, staff attitudes and the wider patient community. The milieu could be vital for nurturing a patient and providing a sense of safety and sanctuary, almost a therapeutic intervention in itself. Staff played a key role in creating this milieu, with structure, order and safety producing a congenial atmosphere, which made wards feel safe. Conversely, when the milieu was perceived as unsafe, feared or violent, it would be to the detriment of the patient experience. In a similar way, the physical environment complemented the milieu, with a good environment contributing to a greater sense of well-being. Sometimes, accessing other physical places extended the therapeutic environment, for example access to green spaces or places of worship, or through feeling connected to the outside world. | The FFT lacks qualitative data, but it is easy and more accessible than other methods. As FFT data are generally positive, it is not as useful as qualitative/complaints data | A1: appraisal should include both qualitative and quantitative evidence. The FFT alone provides insufficient patient experience data, but it can provide a useful benchmark. Evaluation of patient experience data should consider both qualitative and quantitative information to provide the granular detail that helps to identify why something is happening, not just that it is happening. Analysis should triangulate all types of patient experience data for a richer picture (e.g. the FFT, complaints, compliments and patient safety data) |
Need to go beyond only qualitative and quantitative data – take environment into the context (e.g. boredom: ‘just want something to say’) Priority setting for change. Need all data to go to one place. Across a long period of time. Qualitative data feed into quantitative data. Barrier = cannot please everyone, must do something. Quantitative data = no incidences, etc., so good trust is shown quantitatively but qualitative data show patients hate the ward – need to combine quantitative and qualitative data. National drivers focus on quantitative data; qualitative data are only driven locally. The FFT changed to equal a compliments system Qualitative data are unpredictable, as are the means for collecting them |
Helps to consider the environment and that the service user wants to ‘just talk’. Local drivers for qualitative data | Priorities set based on external settings/government set the agenda – need to change this to reach this rule = national drivers are for quantitative data, so qualitative data need investment for any engagement. The FFT needs to be recharged so that qualitative and quantitative/positive and negative are equal. Qualitative data are unpredictable. Cannot please everyone, must do something. Systems need changes to address this need. Qualitative and quantitative data show different things so can they be analysed and responded to the same way? |
Rule A1: appraisal should include both qualitative and quantitative evidence Evidence: the FFT alone is insufficient for use as patient experience data, but it can provide a useful benchmark. Evaluation of patient experience data should consider both qualitative and quantitative information to provide the granular detail that helps to identify why something is happening, not just that it is happening. Analysis should triangulate all types of patient experience data for a richer picture (e.g. the FFT, complaints, compliments and patient safety data) |
||
|
Staff need to see the importance of/use in doing something in order to commit to it and get survey responses Information flows upwards and outwards |
A2: informal patient experience feedback must be responded to and used. Although formal measures are useful and provide metrics, listening and responding to patients when they informally give feedback about their experience is not just about good quality care provision, it can be used to improve the quality of care. The informal uncollected patient experience data held locally on wards should be harnessed at the local level to drive local quality improvement. When patient experience teams exist, they need to support and understand how the informal feedback processes are working. Changes that are made as a result of this informal feedback should be captured in the corporate structure to inform wider quality improvement initiatives in trusts | Communication! No buy-in or need to pass on something that is not a complaint. Collect informally in a range of ways (not just in complaints and the FFT). Have independent organisations involved to create buy-in (e.g. the CQC, FFT, NHS, etc.). Empower ward staff to embrace and report. Barrier – ‘if it’s not written down it didn’t happen’ culture, informal needs to be documented!. Barrier – consistency across wards; system is not fit for purpose; informal needs to be made equal to formal. Informal is just as important for patients – ‘soft intelligence’ needs to be shared with all ward staff/corporate staff/patients | Important to service user. Staff training needs to empower staff with this. Independent buy-in would drive this | Buy-in. Understanding of what feedback is. ‘If it’s not written down it didn’t happen’ culture; informal needs to be documented! Barrier – consistency across wards, system is not fit for purpose; informal needs to be made equal to formal. System not in place for informal feedback loop |
Rule A2: informal patient experience feedback must be responded to and used Evidence: although formal measures are useful and provide metrics, listening and responding to patients when they informally give feedback about their experience is not just about good quality care provision, it can be used to improve the quality of care. The informal patient experience data held locally on wards should be harnessed at the local level to drive local quality improvement. When patient experience teams exist, they need to support and understand how the informal feedback processes are working. Changes that are made as a result of this informal feedback should be captured in the corporate structure to inform wider quality improvement initiatives in trusts |
||||
| A3: both positive and negative feedback should be acted on. Positive and negative feedback are both valuable and should be included in data collection, analysis and action-planning. Organisations (e.g. trusts) usually respond only to complaints and negative feedback, so staff are not conditioned to respond to positive feedback | No consensus between group. Positive feedback should not be captured, as it is not part of your role. No buy-in or need to pass on something if it is not a complaint (positive feedback kept by person on ward). Positive feedback boosts morale; use staff awards – awarded by patients. Promote good practice and learn from each other. Positive cycle – share best practice between wards when it works. Positive feedback is discretionary owing to no money, etc. Patient experience is for the benefit of patients; staff benefit is a bonus. Feels intrusive; do not want to over survey or irritate. Environment needs to be right for informal feedback (e.g. ‘relax’ off ward). One-to-one time is hard to have because there is no room/space/area for confidentiality. Staff do not know how to deal with positive feedback (not the culture). Ripple of a compliment does not travel as far as that of a complaint | Positive feedback boosts moral; use staff awards – awarded by patients. Promote good practice and learn from each other. Positive cycle – share best practice between wards when it works. Patient experience is for the benefit of patients; staff benefit is a bonus | Positive feedback should not be captured as it is not part of your role. No buy-in or need to pass on something if it is not a complaint (positive feedback kept by person on ward). Positive feedback is discretionary owing to no money, etc. Feels intrusive; do not want to over survey or irritate. Environment needs to be right for informal feedback (e.g. ‘relax’ off ward). One-to-one time is hard to have owing to no room/space/area for confidentiality. Staff do not know how to deal with positive feedback (not the culture). Ripple of a compliment does not travel as far as that of a complaint |
Rule A3: both positive and negative feedback should be acted on Evidence: positive and negative feedback are both valuable and should be included in data collection, analysis and action-planning. Organisations (e.g. trusts) usually respond only to complaints and negative feedback, so staff are not conditioned to respond to positive feedback |
|||||
| A4: gathering, analysing and using patient feedback is everyone’s business. The responsibility for collecting, analysing and acting on patient experience data should be shared so that there is buy-in at every level. Devolving responsibility for acting on and responding to patient experience data ensures that ward staff feel engaged in the whole process. Ward staff can make changes if given permission to do so. Staff can act on patient experience data only if they are made available and shared. Currently, data are held centrally in many organisations. Often feedback does not reach ward staff or patients. The weakest area of work is the analysis of patient experience data. Certain types of feedback (e.g. patient stories presented to the board or serious complaints) may be privileged. Although these are valuable learning opportunities, this risks driving change in response to individual negative feedback | People who buy in are already doing it; singing to the choir. Need to regenerate new culture. ‘It’s common sense what needs to be done’ but different staff have different procedures to do so. ’Short circuit’ exists – close the gap to allow feedback to be acted on. Staff do not feel they are authorised to ‘act and respond’. Barrier = ward environment is distracting | People who buy in are already doing it; singing to the choir = a need to regenerate new culture beyond the role of one person. ‘It’s common sense what needs to be done’ but different staff have different procedures to do so. ‘Short circuit’ exists (see car park) – close the gap to allow feedback to be acted on. Staff do not feel they are authorised to ‘act and respond’. Barrier = ward environment is distracting |
Rule A4: gathering, analysing and using patient feedback is everyone’s business Evidence: there needs to be buy-in at every level. Devolving responsibility to the ward level for acting on and responding to patient experience data ensures that ward staff feel engaged in the whole process. Ward staff can make changes if given permission to do so. Staff can act on patient experience data only if they are made available and shared. Currently, data are held centrally in many organisations. Often feedback does not reach ward staff or patients. The weakest area of work is the analysis of patient experience data. Certain types of feedback (e.g. patient stories presented to the board or serious complaints) may be privileged. While these are valuable learning opportunities, this risks driving change in response to individual negative feedback |
||||||
| Performance and rankings alone do not drive quality improvement and there can be unintended consequences on staff morale | Quantity over quality | ||||||||
| CQC – power beyond trust; leverage | |||||||||
| Who does quality improvement serve? (Temporal/sustainability) | |||||||||
| Quality improvement is poorly understood and it depends on if the trust applies external models, organisationally driven by internal critiques | |||||||||
| When patient experience is not embedded, trusts do not use patient experience data to drive quality improvement | |||||||||
| Typologies of trust are being developed based on the sophistication of mechanisms and investment in all parts of the feedback and implementation cycle – the typology of trust will influence the programme theory outcome (i.e. when there are less developed IT systems, data access will be worse, which will affect the patient experience system) – to what extent does the typology drive the findings? (First iteration changes) | |||||||||
| ARST2: it is not known if reporting patients’ experiences is associated with improved outcomes (including clinical and functional outcomes and quality of life), reduced carer burden or reduced costs (protocol) | By driving data ‘downwards’ and back to wards for them to take responsibility for such data, things should be resolved locally | ||||||||
| ARST3: we do not know how any effect might be mediated (e.g. via better treatment adherence) or which types of patient experience data are of most use for improving services (protocol) | By driving data ‘downwards’ and back to wards for them to take responsibility for such data, things should be resolved locally | ||||||||
| Feedback should be a loop and not a continuous process; there should be outcomes, end points and information that go somewhere | |||||||||
|
Staff need to see the importance of/use in doing something in order to commit to it and get survey responses Information flows upwards and outwards |
|||||||||
| Original programme theories from the bid | Programme theory refinement for WP2: flash cards developed for WP3 interviews | Programme theory refinement for WP3: rules developed based on WP3 and analysis of CMOs | First refinement (post WP4) | Final programme theories (reiterated rules post WP4) | |||
|---|---|---|---|---|---|---|---|
| Data | Facilitators | Barriers | |||||
| Change | After putting systems in place and changing the culture around the collection of patient experience data, the next stage should be to identify what happens to data; the role may naturally evolve into quality improvement | IC1: organisations must have a means of contextualising patient experience and feedback alongside other information gathered. Patient experience data are most effective when not held in a silo and when they are triangulated with other data such as compliments and complaints and patient safety data. This triangulation enables patterns to be seen that can help change services to improve quality both at the corporate and at the ward levels. Trusts must ensure that analysis includes triangulation of data at all levels, not just at the corporate level |
How? Oversight role: integration of safety/complaints = identity themes from integrated feedback; share information widely; link to patient record = has potential for concerns/patients unlikely to complain; celebrate excellent ward-based practice in meetings; need to create ‘themes’ from feedback to identify quality improvement strategy; staff create/‘own’ action plans from integrated themes; patient stories; trust needs to be embedded for quality improvement to happen (not just at the organisational/corporate level); use triangulated feedback to identify issues/drill down into more specific areas (i.e. create opportunities for more feedback) Why? How else can so much information be collated? Facilitators and barriers: siblings; operations and governance not integrated; overview tends to be of negative not positive feedback; a lot of reports not seen by ward-level staff Who: integrated work role; corporate level |
Operations and governance not integrated. Overview tends to be of negative not positive feedback. A lot of reports not seen by ward-level staff | How? Oversight role: integration of safety/complaints = identity themes from integrated feedback; share information widely; link to patient record = has potential for concerns/patients unlikely to complain; celebrate excellent ward-based practice in meetings; need to create ‘themes’ from feedback to identify quality improvement strategy; staff create/‘own’ action plans from integrated themes; patient stories; trust needs to be embedded for quality improvement to happen (not just at the organisational/corporate level); use triangulated feedback to identify issues/drill down into more specific areas (i.e. create opportunities for more feedback) |
Rule ICh1: organisations must have a means of contextualising patient experience and feedback alongside other information gathered Evidence: patient experience data are most effective when not held in a silo and when they are triangulated with other data such as compliments and complaints and patient safety data. This triangulation enables patterns to be seen that can help change services to improve quality both at the corporate and at the ward levels. Triangulation of data needs to happen at all levels, not just at the corporate level |
|
| By seeing how feedback is used and if it is being used influences both staff and patients’ willingness to engage | IC2: service improvement should not be led by negative feedback alone. Staff believe that complaints are the most common driver for change. There is a pervasive sense that quality improvement is sometimes driven by negative feedback or ‘external’ forces. How data are prioritised within organisations varies. Examples commonly given are of quality improvement initiatives started based on responding to serious incidents or complaints, the CQC or external inspection or deterioration and noticing things are wrong. Although these are all valid reasons, quality improvement cannot solely be led by negative feedback, as this risks losing the knowledge about what works well, is demotivating for staff and is disempowering for patients |
How? Learning from what we do right = staff feedback sessions; learning from excellence = positive incident reporting system; recording personal stories (not shoehorning into standardised systems); contact of contacts vs. complaints; ‘always’ events; feedback gathered in co-designed ways Facilitators and barriers: system set up to respond when things go wrong = bigger focus on negative data; a vision of what good looks like; negative feedback is more of a risk – no learning from positive feedback; stuck in ‘You said, We did’ not ‘You said, We kept/amended’ = too much focus on ‘change’ |
System set up to respond when things go wrong = bigger focus on negative data. A vision of what good looks like. Negative feedback is more of a risk – no learning from positive feedback. Stuck in ‘You said, We did’ not ‘You said, we kept/amended’ = too much focus on ‘change’ | Learning from what we do right = staff feedback sessions; learning from excellence = positive incident reporting system; recording personal stories (not shoehorning into standardised systems); contact of contacts vs. complaints; ‘always’ events; feedback gathered in co-designed ways |
Rule ICh2: service improvement should not be led by negative feedback alone Evidence: staff believe that complaints are the most common driver for change. There is a pervasive sense that quality improvement is sometimes driven by negative feedback or ‘external’ forces. How data gets prioritised within organisations varies. Examples commonly given are of quality improvement initiatives started as a response to serious incidents or complaints, the CQC or external inspection, or deterioration and noticing things are wrong. Although these are all valid reasons, quality improvement cannot solely be led by negative feedback, as this risks losing the knowledge about what works well, is demotivating for staff and is disempowering for patients |
||
| IC3: staff need to be engaged in quality improvement. It is unclear for staff how patient experience feedback links to quality improvement work. Understanding where the data came from that inform quality improvement is crucial to engaging staff in that work. Change happens and is sustained when staff and wards take responsibility and ownership for the change. Individual wards cannot lead cultural systemic change that needs central and local alignment. If staff are not engaged then there is a risk that instead of quality improvement, tokenistic or short-term changes are made (e.g. to the ward environment). These changes are usually not in the face of other pressures |
How? Open access to feedback measures for staff; incentives/posters/promotion; patient and staff working together (continuous feedback and dialogue); regular weekly meetings about quality improvement and how it links with goals; individual link to responsibilities of ward staff; website for trust-wide feedback (with detailed search options); give staff ownership of quality improvement/permission to make change; train staff to be ‘change agents’ Facilitators and barriers; ward staff feel disempowered by large need from corporate staff for information; discretionary ward budget to make small changes |
Ward staff feel disempowered by large need from corporate staff for information. Discretionary ward budget to make small changes | Open access to feedback measures for staff; incentives/posters/promotion; patient and staff working together (continuous feedback and dialogue); regular weekly meetings about quality improvement and how it links with goals; individual link to responsibilities of ward staff; website for trust-wide feedback (with detailed search options); give staff ownership of quality improvement/permission to make change; train staff to be ‘change agents’ |
Rule ICh3: staff need to be engaged in quality improvement Evidence: it is unclear for staff how patient experience feedback links to quality improvement work. Understanding where the data came from that inform quality improvement is crucial to engaging staff in that work. Change happens and is sustained when staff and wards take responsibility and ownership for the change. Individual wards cannot lead cultural systemic change that needs central and local alignment. If staff are not engaged then there is a risk that instead of quality improvement, tokenistic or short-term changes are made (e.g. to the ward environment). These changes are usually not sustained in the face of other pressures |
|||
| IC1: we believe that there are differences between organisations’ use of patient experience data to improve and inform service development and we are curious about the variety of ways in which this is being undertaken (protocol) | If we concentrate on building relationships with service users that work on the ground, we will be able to look at ‘how’ change is produced because service users are invested in and care about the services | IC4: quality improvement requires leadership. Organisations tend to respond more rapidly to feedback about environmental issues. Changes to the environment are implemented at the ward level. Cultural change is more difficult and requires corporate leadership |
How? Wards where staff were felt to work in compassionate ways that supported patient experience could be acknowledged at corporate level; quality improvement owned by whole board, not just director of nursing, etc.; dedicated quality improvement team; prioritise frontline staff perspective and patient views; agreement among leaders about quality improvement; empower leaders on top floor; staff not just vehicles for organisational-level quality improvement; corporate staff need to be visible on wards; getting ‘people around the table’ to hear about quality improvement/corporate states/ward-based initiatives Facilitators and barriers: trusts concerned about external relationship/change/reputation/media backlash; quality improvement can become compartmentalised, not integrated into corporate board; operational leadership can be detached from ward leadership; temporal difference between ward-level and corporate-level priorities; not helped by staff turnover/instability (but can be welcomed by collection leadership) Who? Collective leadership/staggered structures |
Quality improvement owned by whole board, not just director of nursing, etc. Dedicated quality improvement team. Prioritise frontline staff perspective and patient views. Agreement among leaders about quality improvement. Empower leaders on shop floor. Staff not just vehicles for organisational-level quality improvement. Getting ‘people around the table’ to hear about quality improvement/corporate states/ward-based initiatives | Corporate staff need to be visible on wards. Trusts concerned about external relationship/change/reputation/media backlash. Quality improvement can become compartmentalised, not integrated into corporate board. Operational leadership can be detached from ward leadership. Temporal difference between ward-level and corporate-level priorities. Not helped by staff turnover/instability (but can be welcomed by collection leadership) | Collective leadership/staggered structures |
Rule ICh4: quality improvement requires leadership Evidence: organisations tend to respond more rapidly to feedback about environmental issues. Changes to the environment are implemented at the ward level. Cultural change is more difficult and requires corporate leadership |
| Feedback should be a loop and not a continuous process; there should be outcomes, end points and information that goes somewhere | |||||||
| Systemic influences that would encourage services to adopt this approach | CQC – any trust that wants a good CQC rating needs PPI for a good quality improvement rating. Buy-in from the CQC and NHS England – need to push and have buy-in from above/government agencies that have influence. What is the tipping point? The cycle needs to be more nuanced and drivers beyond the FFT = need an incentive for other ways (i.e. for more of the cycle questions: all parts of the cycle need incentives). Need to consider better ways to catch and use positive feedback. Feedback in exchange for feedback – have not thought of how = we need evidence of how to do this. Evidence of leadership all through. Change culture of threat of feedback: trust induction to staff = buy-in and how to train people to do that. Commissioners ≥ value-for-money models to present to these commissioners to ‘save money’. Persuasion to implement = drive for patient experience – need more evidence for these. Showcasing the positive for health competition = showcasing changes/best practice/where feedback has led to change and positive patient experience. Elaboration of the incentives to deeply embed patient experience = corporate interest. ‘Devil is in detail’ = trust-level feedback back down = when is there enough feedback to prompt change? NHS England and CQC – it needs to come down the line. No consistency = improve with training evidence, how to change culture, leadership?; not WM needs to come from higher. How should incentives work and between which organisations? = Persuasion and incentives. Pilot on an engaged ward = evaluation = existing resources = showcase positives = healthy competition ≥ quality improvement and changes. Extend modelling = staff retention and well-being | Systemic influences that would encourage services to adopt this approach:
|
|||||
| IC2: the proliferation of diverse but often unco-ordinated initiatives to collect and use patient experience data means that new and more theoretically coherent approaches must compete for space on operational agendas (protocol) | The FFT lacks qualitative data, but it is easy and more accessible than other methods. As FFT data are generally positive, it is not as useful as qualitative/complaints data | ||||||
| It is good to look across data and begin developing more sophisticated analysis but initially the priority is getting/collecting the feedback | |||||||
| IC3: we believe that there will be discernible differences between organisations that demonstrate genuine commitment to, and capacity for, using patient experience data to improve services, and that these differences will be most clearly manifest through the existence of processes that support innovation and quality improvement, including commitment to service improvement among senior leaders, decentralised decision-making (through identifiable champions for change), role clarity within the organisation and support for risk-taking (protocol) | By seeing how feedback is used and if it is being used influences both staff and patients’ willingness to engage | ||||||
| IC4: we expect that organisations that set out to improve care quality will be able to provide evidence of methodologies for achieving this, including clear cycles of planning, implementation and reflection as opposed to small, piecemeal initiatives (protocol) | The national staffing crisis makes ‘experience’ feedback difficult to fix compared with environmental examples, which are easier to change | ||||||
| By seeing how feedback is used and if it is being used influences both staff and patients’ willingness to engage | |||||||
Appendix 18 Analysis: work package 4 supplementary data – consensus conference attendance list
Attended: 44 (+4 Warwick scribes).
Of the 44, 11 were part of the PPIT, 17 were directly involved with the project and 16 were from NHS trusts.
Job roles
-
Adult Mental Health Project Officer
-
Centre Lead for Psychiatry
-
Patient Experience Officer and Improvement Leads
-
Research Fellow
-
Head of Empowerment and Social Inclusion
-
Assistant Professor
-
Patient Experience Officer
-
Deputy Research Delivery Manager – Dementia, Mental Health and Neurology
-
Research Fellow
-
Research Associate
-
Student
-
Head of Division
-
Head of Recovery, Participation and Partnership
-
Associate Director of Nursing Patient Experience
-
Lead for Service User, Carer and Public Engagement
-
Member of the Survivor Researcher Network working group
-
Healthwatch Steering Group
-
Reader in Psychology
-
Student
-
Patient Experience and Involvement Manager
-
Professor
-
Clinical Lead – Involvement and Experience Team
-
Research Assistant
-
Patient and Carer Involvement Lead (Mental Health Nurse)
-
Clinical Psychologist, Research Fellow
-
Research Nurse
-
Student
-
PALS and Complaints Manager
-
Student
-
Healthwatch Steering Group
-
Research Site Co-ordinator
-
Insight and Feedback Officer in the Insight and Feedback Team
-
Senior Research Fellow
-
Senior Applied Psychologist (Urgent Care)
-
Professor of Mental Health
-
Patient Safety Manager
-
Involvement, Experience and Volunteering Lead for Local Partnerships.
Appendix 19 GRIPP forms: work package 1 GRIPP2 form
Appendix 20 GRIPP forms: work package 2 GRIPP2 form
Appendix 21 GRIPP forms: work package 3 GRIPP2 form
Appendix 22 GRIPP forms: work package 4 GRIPP2 form
List of abbreviations
- BAME
- black, Asian and minority ethnic
- CASP
- Critical Appraisal Skills Programme
- CMO
- context–mechanism–outcome
- CQC
- Care Quality Commission
- CRAICh
- collecting and giving, receiving and listening, acting, and quality improvement and change
- EURIPIDES
- Evaluating the Use of Patient Experience Data to Improve the Quality of Inpatient Mental Health Care
- FFT
- Friends and Family Test
- GRIPP2
- Guidance for Reporting Involvement of Patients and the Public 2
- IT
- information technology
- MHF
- Mental Health Foundation
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PALS
- Patient Advice and Liaison Service
- PEL
- patient experience lead
- PPI
- patient and public involvement
- PPIT
- patient and public involvement team
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- R&D
- research and development
- RA
- research associate
- RAG
- red, amber, green
- RF
- research fellow
- ROAMEF
- rationale, objectives, appraisal, monitoring, evaluation and feedback
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08210).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
