Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 14/21/45. The contractual start date was in December 2015. The final report began editorial review in September 2019 and was accepted for publication in December 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research, or similar, and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2022. This work was produced by Oulton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health and Care Research, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2022 Queen’s Printer and Controller of HMSO
Easy-read summary
Structure of the report
This report of the findings from the Pay More Attention study has four sections.
Section 1
The introduction comprises three chapters, focusing on the background to the study (see Chapter 1), the study aims and theoretical framework (see Chapter 2) and the literature review (see Chapter 3).
Section 2
Research design and methods of data collection and analysis for each phase (see Chapter 4).
Section 3
The results section comprises five chapters (see Chapters 5–10). The first three of these chapters focus on findings from staff, with data from the survey being used to identify whether or not staff perceive that inequality exists between children with and children without learning disability (LD) and their families (see Chapter 5). Findings from the organisational mapping exercise (see Chapter 6) and staff interviews (see Chapter 7) highlight the cross-organisational, organisational and individual staff factors in NHS hospitals that facilitate and prevent such inequality. Chapters 8–10 focus on parents’ experiences of being in hospital with their child. The narrative of parents of children with LD is the focus of these chapters, but important comparisons will be drawn from the views and experiences of parents of children without LD. Chapter 11 focuses on findings from the parent and child survey about satisfaction with different aspects of the hospital experience. At the end of each chapter the barriers to and facilitators of inequality for children with LD and their families will be presented in a series of diagrams related to each research question. Our aim is to incrementally build a comprehensive picture of what factors are key to ensuring equality.
Section 4
In the synthesis and discussion chapter (see Chapter 10), we bring the data together and generate a single diagram of barriers and facilitators for each research question (RQ), showing where staff and families overlap or differ in their thinking. Chapter 11 concludes with implications for practice and research.
Section 1 Introduction
Chapter 1 Background to the study
Parts of this chapter have been reproduced with permission from Oulton et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/.
Despite comprehensive evidence of health inequalities for adults with LD, including poor practice, discrimination and abuse in hospitals,2–5 to our knowledge there has yet to be a comprehensive review of how well hospital services meet the needs of children and young people (hereafter referred to as children) with LD and their families. A major uncertainty is when the inequalities known to exist for adults with LD start to emerge. Limited qualitative evidence of parental dissatisfaction with the quality, safety and accessibility of hospital care for children with LD exists (see Chapter 3). However, the extent to which these parents’ experiences differ from those of parents of children without LD is not known. Moreover, reports of the views and experiences of children with LD are almost non-existent in the literature.
This study set out to compare how services are delivered to, and experienced by, children with long-term conditions, with and without LD, and their families, to see what inequalities exist, for whom, why and under what circumstances. The cross-organisational, organisational and individual factors in NHS hospitals that facilitate or prevent children with LD and their families receiving equal access to high-quality care and services were explored. Our aim was to generate examples of effective, replicable good practice.
Definition and prevalence
A long-term condition is defined as a health condition that requires ongoing management over a period of years. 6 About one in seven young people (15%) aged 11–15 years in the UK reports that they have been diagnosed with a long-term medical condition. The more common conditions that affect children and young people include diabetes, asthma, epilepsy, severe allergies and anaphylaxis. Among those with a long-term condition, approximately 28% require medical follow-up, of whom approximately 6% have a disability. A proportion of these children will also have a LD, which is a neurodevelopment condition that covers a wide spectrum of impairments; various definitions are applied in the UK and internationally. In the White Paper Valuing People,7 the Department of Health and Social Care states that LD includes the presence of:
-
a significantly reduced ability to understand new or complex information or to learn new skills [impaired intelligence; intelligence quotient (IQ) of < 70], with
-
a reduced ability to cope independently (impaired social functioning).
These impairments start before adulthood and have a lasting effect on development.
Although IQ has historically been the defining measurement of LD, it is now recognised that a low IQ is not, in itself, a sufficient reason for deciding that an individual should be provided with additional health and support. This message was echoed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5),8 in which the term ‘intellectual disability’ (commonly used to describe LD internationally) replaced ‘mental retardation’ and IQ test scores were removed from the diagnostic criteria to prevent these being overemphasised in terms of a person’s overall ability.
The definition includes children with autism who also have LD, but it does not include those who have specific learning difficulties that may impair educational attainment, such as dyspraxia or dyslexia, but who are within the average range of intelligence or those with developmental delay who are late in reaching some or all of their developmental milestones. It is also important to distinguish children with LD from those with neurodiversity, who are of average or above-average intelligence.
Causes of LD can be genetic, or due to prenatal, perinatal and postnatal environmental factors. 9 There is no definitive record of the number of people with LD in England, but the estimated prevalence of LD in children and young people is 2.5%. 10 It is widely acknowledged that the numbers of those with severe intellectual impairment and multiple/complex long-term problems will continue to rise by 1% each year. 11
Health needs, inequality and inequity
In terms of their health, it is widely reported that disabled children are a vulnerable population12 whose care needs are significantly greater than those of other children. 13 However, accurate information about the prevalence of some impairments and health conditions in children with LD is limited, possibly because the population is heterogeneous, the terminology used varies and the main focus of recent efforts to reduce health inequalities related to LD has been adult care.
Much of the available evidence related to children comes from work carried out by Emerson et al. , including a review of the UK literature on the health inequalities experienced by children and young people with intellectual disabilities. 14 Emerson and Hatton15,16 reported that ‘the risk of children being reported by their main carer (usually their mother) to have fair/poor general health is 2.5–4.5 times as great for children with learning disabilities as for other children’, a finding only partially accounted for by differences in socioeconomic status. 17 In addition, children with LD are almost twice as likely to report three or more health problems as children without LD. 16 More recently, a ‘disabilities terminology set’ was developed and used to quantify the multifaceted needs of disabled children and their families in a district disability clinic population. 13 Compared with children without LD, children with LD were found to have significantly more needs overall, including more health conditions, health technology dependencies and family-reported issues, and were more likely to need round-the-clock care.
As well as having intellectual impairment, a large proportion of children with LD will have sensory impairments, such as vision or hearing impairment,18 and/or communication difficulties. 19 They also have higher rates of all types of incontinence, sleep disorders, obesity and epilepsy14 than children without LD. The prevalence of epilepsy among people with LD is at least 20 times higher than among people without LD, and the seizures they experience are commonly resistant to treatment. 20–23
In terms of mental health, children with LD are at significantly increased risk of certain types of psychiatric disorder (prevalence of 39%) compared with children without LD (prevalence of 8%). 24 Some children with LD also have autism spectrum disorders, although estimates of prevalence of these vary considerably. 14 There has also been a reported threefold increase in the risk of behaviours that challenge in children with LD compared with typically developing children,25 a major contributing factor being the existence of a communication impairment that may limit the child’s ability to express frustrations or explain any underlying emotional/physical distress or other external factors.
Children with disabilities experience more frequent and lengthier hospital admissions than children without disabilities,26 which has an impact on school attendance. 17 The ability for children with LD of all ages to understand information about hospital care and treatment may be limited; they may not be able to communicate their needs verbally and may need additional support with all aspects of hospital life. Although many children will find it hard to cope emotionally when they are in an unfamiliar hospital environment, those with LD who display behaviours that challenge27 may find it particularly difficult.
Policy
The publication of Death by Indifference,2 about six people with LD who were seen to have died in hospital unnecessarily, triggered an independent inquiry into access to health care for adults with LD, which revealed significant system failures and less favourable treatment of these patients than those without LD, resulting in prolonged suffering and inappropriate care. The report of this inquiry, Healthcare for All,3 identified the invisibility of people with LD within health services, with a lack of priority given to identifying their particular health needs. A lack of training, combined with ignorance and fear, were recognised as compounding negative attitudes and values held about people with LD and their carers. Furthermore, these were notable factors in failing to deliver equal treatment and to people being treated respectfully and with dignity. 3 A need to strengthen the systems for assuring the equity and quality of health services for people with LD at all levels was identified. The limited direct reference to children with LD in the report presents a mixed picture. Services were praised for ‘providing all-round care’, yet access to general health care for children with LD was reported as being ‘as problematic as it appears to be for adults’.
The resulting Confidential Inquiry into Premature Deaths of People with Learning Disabilities (CIPOLD)4 found that people with LD die, on average, 16 years earlier than people in the general population. Furthermore, it emerged that ‘more people with LD died from causes that were potentially amenable to change by good quality healthcare’. 4 All aspects of care provision, planning, co-ordination and documentation were found to be significantly poorer for people with LD.
NHS England subsequently commissioned the continuing Learning Disabilities Mortality Review (LeDeR)5 programme to monitor deaths among people with LD.
In 2014, the Care Quality Commission introduced a new regulation and inspection process for health and social care services in England, which assesses whether or not services are safe, effective, caring, responsive and well led. Care Quality Commission best-practice guidelines now advocate that ‘all children’s units to have access to a senior learning disability nurse who can provide information, advice and support to health care staff involved in the care of such children and who can help manage difficult situations’. 28
Little evidence exists of the extent of LD nurse provision in children’s hospitals or the nature and impact of this role. A recent NHS benchmarking exercise29 aimed at providing a ‘broad assessment of the state of NHS learning disability services’ failed to include data concerning children’s inpatient LD service provision. As stated in the Royal College of Nursing30 position statement on the role of the LD nurse, ‘National work needs to be undertaken by each UK country as a matter of priority to profile the existing learning disability nursing workforce and identify future requirements’ (reproduced with permission from the Royal College of Nursing). 30 A Department of Health and Social Care-commissioned review by the National Council for Disabled Children31 revealed a number of staffing issues related to the care of children and young people with complex needs and behaviour that challenges involving mental health problems and LD and/or autism. A key finding was the lack of recognition and value placed on the specific skills needed to work with these children, with no professional group identifying themselves as being wholly trained in one or more of their needs. Furthermore, specific issues surrounding the recruitment of nurses with LD education and training were identified, including the possibility that ‘it was only when they were on shift that care plans for this group were implemented’. A need to understand the gaps in staff skills in caring for these children and take necessary action was highlighted.
A key strength of our study is that is has been designed to generate evidence of the issues that affect all children with long-term conditions and those that are particular to children with LD. This evidence is needed to understand the context for making reasonable adjustments for children on the basis of their specific intellectual, emotional, social and physical needs, helping to ensure that resources and interventions that promote equality are better targeted to those who need them, when they need them.
Chapter 2 Study aims and theoretical framework
Parts of this chapter have been reproduced with permission from Oulton et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/.
Study aims
Primary aim
To identify the cross-organisational, organisational and individual factors in NHS hospitals that facilitate or prevent children with LD and their families receiving equal access to high-quality care and services.
Secondary aim
To develop guidance for NHS trusts about the implementation of successful and effective measures to promote equal access for children with LD and their families.
Research questions
From the perspectives of families and clinical staff
-
Do children with and children without LD and their families have equal access to high-quality hospital care that meets their particular needs?
-
Do children with and children without LD, assisted by their families, have equal access to hospital appointments, investigations and treatments?
-
Are children with and children without LD and their families equally involved as active partners in their treatment, care and services?
-
Are children with and children without LD and their families equally satisfied with their hospital experience?
-
Are safety concerns for children with and children without LD the same?
-
What are the examples of effective, replicable good practice for facilitating equal access to high-quality care and services for children with LD and their families at the study sites?
-
What indicators from the data and the literature suggest that the findings may be generalisable to other children with long-term conditions in the hospital setting?
Theoretical framework
We took a systematic approach to an empirical identification of the factors that affect access to high-quality hospital care for children with LD and their families. Building on the work of Tuffrey-Wijne et al. ,32 we devised a provisional theoretical framework for understanding the range of factors at the cross-organisational, organisational and individual levels that might have an impact on the delivery of hospital care to children with LD and their families (Figure 1). This framework was informed by a synthesis of existing policy and literature (see Report Supplementary Material 1) and the wide-ranging expertise and experience of the multidisciplinary research team. Organisational and individual domains of the theoretical framework are indicated in boxes A, B, C and D (see Figure 1). Each box contains a number of factors within each domain that might function as barriers to, or facilitators of, promoting equal access to high-quality hospital care for children with LD and their families in NHS hospitals. Included are outcomes that might be associated with effective measures for promoting equal access. Having tested and refined the theoretical framework throughout the study, it is re-presented in Chapter 12 as an empirical framework for promoting equal access to high-quality hospital care for children with LD and their families.
FIGURE 1.
Theoretical framework. LDLN, learning disabilities liaison nurse.

Chapter 3 Learning from the literature
The number of children with long-term conditions, with and without LD, who require complex care is growing, resulting in the increased use of health-care resources as these children spend prolonged periods of time in hospital for both acute and planned admissions and for both medical and surgical care. The quality of the hospital stay and the extent to which hospital services meet the needs of all children have been studied for some time; the body of literature is expansive. Inequalities have been highlighted but not examined in any detail, particularly in relation to children with LD. The impact of a hospital environment on these populations has rarely been considered in the context of a shared narrative. Rather, studies tend to concentrate on the views of particular stakeholders, such as children, parents or staff, and not on how services are delivered within and across particular hospital settings. For the purposes of this report, we present relevant learning from the literature, focusing predominantly on a number of recently published systematic and narrative reviews.
Adults with learning disability
The majority of studies that do focus on the hospital care of patients with LD relate to the care of adults. Although it is not within the remit of this report to present a review of this literature, three major pieces of work are of particular relevance: a systematic review of hospital experiences of people with LD in general acute hospitals,33 a narrative review of acute care nurses’ experiences of nursing patients with LD,34 and a national mixed-methods study35 of the factors preventing the implementation of strategies to promote a safer environment for patients with LD in English hospitals.
The systematic review of 16 studies of the hospital experiences of people with LD32 revealed seven overarching themes ‘related largely to failures of hospitals and staff to meet patient needs’. The key factors contributing to such failures were staff attitudes and their limited knowledge and skills concerning LD, and a failure at the systems level to make necessary adjustments, resulting in carers being relied on both for care and to advocate for appropriate treatment. Facilitators of care were exceptions rather than common experiences. The narrative review of the experiences of acute care nurses34 similarly found that nurses felt underprepared when caring for adult patients with LD, experienced challenges communicating with them and had ambiguous expectations of paid and unpaid caregivers.
There was also an overlap in findings from the large national study,35 which revealed the main barriers to better and safer hospital care for people with LD to be (1) the invisibility of patients with LD in hospitals, (2) poor staff understanding, (3) a lack of consistent and effective carer involvement and staff misunderstanding of the carer role, and (4) a lack of clear lines of responsibility and accountability. The provision of a learning disability liaison nurse with authority to change practice and the support of senior management were found to be the main enablers of safe care, along with ward managers who facilitated a positive ward culture and ensured the consistent implementation of reasonable adjustments.
Children with learning disability
Few studies focus specifically on the care of ‘children with LD’ in hospital. More often than not, researchers instead focus on particular impairments, such as communication, or specific diagnoses, such as cerebral palsy, without drawing out findings applicable to those with LD. Furthermore, studies related to disabled children or to those with special needs, complex or chronic health needs or who are medically fragile or technological-dependent can include mixed samples of children with and children without LD, or an unspecified sample, which makes it difficult to determine the findings that are relevant to those with LD.
Among those studies that are focused on the care of children with LD in hospital, very few directly include children with LD as participants. A structured review and synthesis of qualitative studies reporting on the experience of disabled children as inpatients36 concluded that their experience was ‘variable and not always optimal’. The main issue was related to communication, which emerged as a key factor in whether the child and family had a positive or a negative experience. Of particular relevance to children with LD was the finding that during outpatient appointments health professionals often talked to parents instead of the child, resulting in feelings of disempowerment,37 and that although parents valued the inclusion of their disabled child, they were worried that children with communication disorders would be misunderstood. 38 Importantly, only two of the eight studies included in this review focused specifically on the care of children with LD and, in these, only two individual children were interviewed. Of significance is that these two children, despite talking positively about nursing staff, were reported to be ‘less positive in general about their hospital stay than their parents’. 39 A recent ethnographic study, one of the few to include observation and interviews with hospitalised children with LD,40 revealed the importance of staff not making assumptions about the capabilities and wishes of these patients. Examples were provided of too much and too little information and involvement, with associated feelings of uncertainty or fear and worry. Observations of practice revealed how important the ‘little things’ are to these patients, such as particular objects or activities, and the anxiety that they can experience when these are not available. Maintaining their routine, keeping them occupied and avoiding waiting were also found to be central to these patients’ well-being in hospital.
Relationship between parents of children with learning disability and staff
The small body of evidence relating to the care of children with LD in hospital mostly focuses on parents’ views and relationships with staff. The importance of parents and professionals working in partnership during any child’s hospital admission is well documented in the context of family-centred care,41 but parents’ central connection to their child in a health-care system relationship is also essential. Family-centred care has been positioned as an approach that encompasses the whole family as the ‘unit of care’; however, recent work has suggested that some parents regard themselves as the ‘care recipient’,42 supporting other work that, in this ‘unit of care’, the child is lost. 43 We do not know what children think about this approach to care, but we do know that having parents nearby is central to their experience,44,45 reinforcing the need for a positive and trusting relationship between parents and hospital staff.
What do parents say?
Much of the existing evidence about the relationship that parents of children with LD have with hospital staff has been captured in a recent systematic review12 specifically about patient safety vulnerabilities in this population and a meta-narrative46 of the experiences of parents of children with LD in hospital. A key theme of the systematic review was the reliance staff had on parents being present to ‘supervise, protect and advocate for the care of their child’. 12 Furthermore, it was reported that the understanding of the individual needs of children with LD could be compromised by assumptions staff make about their behaviour, cognitive ability or experience of pain. It was concluded that ‘when healthcare workers understand and are responsive to children’s individual needs and their intellectual disability, they are better placed to adjust care delivery processes to improve care quality and safety’12 during children’s hospitalisation. The meta-narrative of parents’ experiences of children with LD in hospital46 revealed their sense of being ‘more than a parent’ during this time as a result of their monitoring, protecting and advocating role and feeling expected to take responsibility. They also experienced uncertainty in relation to staff roles and responsibilities, and whether staff had the capacity and knowledge to provide safe, high-quality care to their child. The importance of staff knowing the child and working in partnership with parents also emerged. Adding to these two reviews is a more recent paper reporting on the views of parents of hospitalised children with LD,47 which adds to our understanding of what working in partnerships with professionals means to them. A genuine partnership was characterised by seven key elements: preparation, accessibility, reliability, trust, negotiation, expertise and respect.
The findings from these reviews support the theory of devoted protection put forward by Oulton and Heyman48 in their exploratory study about parenting children with severe LD. They found that parents adopted a risk-averse approach to care across all settings, including in hospital, which meant that they felt complete, unbounded responsibility for their child’s health and well-being. This included never leaving the child alone with someone they did not trust completely; when parents did leave their child, the occurrence of any problems could destroy their trust and prevent them from doing this in the future. They expressed apprehension that the specialist knowledge they held about their child was lacking in others, anger at not being listened to, and concern that their dedicated commitment was unequalled. A feeling that professionals devalued both them and their child with LD was also reported. Wider descriptions of parenting roles and responsibilities for disabled children, not specific to hospital, are also relevant to understanding what it might mean for them to accompany their child into hospital, with parents feeling that asking for support is a sign of failure and inability to cope,49,50 being so overwhelmed that they neglect their own needs,51 wanting to relinquish their responsibility because they feel that they are being taken advantage of52 or becoming increasingly expert so that their sense of responsibility becomes self-perpetuating and invisible to others. 48,53,54
What do staff say?
Although staff views about the care of patients with LD are captured almost entirely in relation to adults, some recently published small-scale studies offer some understanding of what it is like for hospital staff to care for children with LD. One ethnographic study55 included interviews with 23 staff members across a range of professional groups working in a specialist children’s hospital and revealed the need for children with LD to receive individualised care based on staff gaining appropriate experience and training, identifying the population, focusing on the ‘little things’, creating a safe, familiar environment, and accessing and using appropriate resources. Parents were seen to play a central role. It emerged that a lack of staff experience, knowledge, confidence and communication about LD can mean that they rely on parents’ input rather than forming a true partnership with parents. The compartmentalisation of nurse training and the movement of medical staff from specialty to specialty were identified as barriers to these professional groups gaining a ‘true understanding’ of the holistic needs of children with LD. A lack of content on developmental disability in the undergraduate curriculum for both doctors and nurses56,57 has been expressed elsewhere. More recently, Lewis et al. 58 interviewed eight nurses working on an acute admission paediatric ward in a general hospital in Australia, who described that caring for children with LD was in some ways similar to caring for children without LD, in that the goals of keeping them happy and getting them well and back home to normality were the same. Medical diagnosis and treatment were reported to guide care irrespective of other factors. However, further evidence emerged of the need for increased vigilance and additional time to meet the needs of these patients and to keep them safe, as well as the importance of routine, familiarity and working in partnership with parents to negotiate care responsibilities.
Children and young people without learning disability and their parents
There has been an increase in research conducted with children without LD, including those with long-term conditions, to understand the hospital experience from their perspective. This large body of evidence has shifted in focus from a predominantly parental to a child perspective, with an emphasis on the use of qualitative research. Children and their parents may often disagree on what the child’s experience in the hospital is really like,59 describing differing perceptions on issues such as safety, decision-making and lack of privacy. 60–62 Children’s descriptions can be captured using themes from Coyne and Conlon:61 fears about the ward environment and hospital, investigations and treatments, being alone, and what might happen. 63 What helps are people: their characteristics, activities, environment and outcome. 60
Parents describing their experiences of care have prioritised important hospital processes, such as effective clinical care, efficiency, safety and security, timeliness, and patient- and family-centred care. 64,65 Open communication and a willingness to share information are priorities for parents. ‘Respect and valuing of individual expertise by health professionals and an environment conducive to negotiation, allow both parent caregivers and the child input in deciding the type and extent of involvement and participation with which they feel most comfortable’. 66
What we learnt from the literature comes predominately from small-scale, single-site studies highlighting the need to examine how hospital care is delivered to, and experienced by, children with LD and their parents at a national level. Furthermore, no studies have directly compared the views of parents of hospitalised children with and children without LD, which means that we currently lack evidence of what things affect all families and what things are unique to the learning disabled population. The central focus of research about the care of children with LD in hospital has been staff and parents, rather than the experiences of children themselves. Children with LD were at the centre of our study and, wherever possible, their views and experiences were captured first hand. Children’s experiences of hospitalisation are, in the main, mediated by adults, parents/family members and health-care staff; it was important in our study to capture all of these views.
Section 2 Research design, methods and analysis
Chapter 4 Research methods
The aim of this section is to provide an overview of the study design and the methods of data collection. Each of the four phases is described in turn, followed by a section on data analysis for all phases and our patient and public involvement (PPI) activities. The original study protocol has been published1 and parts of this chapter have been reproduced from that publication [published by the BMJ Publishing Group Limited. For permission to use (where not already granted under a licence) please go to http://www.bmj.com/company/products-services/rights-and-licensing/. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text].
A list of protocol amendments is provided in Report Supplementary Material 2.
Research design
A transformative, mixed-methods case study design67 was used, integrating quantitative and qualitative methods across four phases over 3 years (Figure 2). Acknowledged for giving ‘a voice to the powerless and voiceless’,68 the case study approach enabled the views of children with LD and their parents to be prioritised and explored ‘in depth and within its real-life context’. 69 In this study, a single hospital site represented each case, and seven cases (phase 2) were included: four specialist children’s hospitals and three non-specialist hospitals. For every two children with LD recruited one child without LD was also recruited, allowing the experiences of the two groups of patients to be compared. Data from diverse sources were synthesised to enable an understanding of whether or not children with LD and their families receive equal access to high-quality hospital care and services. The production of thick, rich descriptions of the phenomena, using in-depth interviews and creative research methods, meant that the complexities of the situation and the factors that can contribute to those complexities emerged. 70
FIGURE 2.
Four-phase transformative mixed-methods study design. The numbers included in the figure are recruitment targets and not the actual recruitment numbers.

Phase 1 involved mapping the organisational context for the delivery of hospital care to children with LD, as well as comparing hospital staff members’ perceptions of their ability to identify the needs of children with and children without LD and their families and to provide high-quality care to effectively meet those needs.
Phase 2 compared how hospital care and services are experienced by children with and children without LD and their families, and staff members’ views of caring for them. A sample of staff from NHS community trusts were also surveyed.
Phase 3 used child and parent questionnaires to compare levels of satisfaction with inpatient hospital care.
Phase 4 synthesised the study findings to develop the outline content for a staff training DVD (digital versatile disc).
Approvals
Full ethics and health research authority approval for this study was obtained prior to the study commencing (London–Stanmore Research Ethics Committee: reference 16/LO/0645). Local research and development approval was also obtained from each of the 24 participating hospital sites.
Phase 1 research methods and analysis
Sample and setting
Children in England are treated either in specialist (tertiary) children’s hospitals (which may stand alone or be part of a wider NHS trust) or in general hospital settings (secondary care) that have one or more paediatric wards. All 15 specialist children’s hospitals in England agreed to participate following an invitation e-mail sent to the trust’s chief nurse through the Association of Chief Children’s Nurses (ACCN). 71 A sampling strategy informed the recruitment of a selection of non-children’s hospitals, based on their proximity and referral patterns to the specialist children’s hospitals and their throughput of children with LD. Senior clinical or managerial staff with a specific responsibility for LD or those working in a dedicated LD role were eligible to participate in the interviews. All clinical and non-clinical hospital staff who had contact with children were eligible to complete the survey. A local collaborator for each participating site was identified.
Recruitment and consent
Staff who were eligible for interview were identified and approached by the local collaborator and given an information sheet and a consent form. With the staff member’s permission, their contact details were given to the research team, who telephoned the staff member to answer any questions and agree a date for the face-to-face or telephone interview. Staff who were eligible to be surveyed were e-mailed a link to an online survey by the local collaborator, with paper copies also available. The return of a completed survey was taken as consent to participate.
Data collection
Staff interviews
Interviews were semistructured, followed an interview guide (see Report Supplementary Material 3), and focused on the delivery of services to children with LD at the organisational level, including policies, systems and practices. Interviews lasted 30–45 minutes and were audio-recorded and transcribed verbatim. A minimum of two interviews per site were planned to ensure completeness of data.
Staff survey
A review of the literature informed the survey development in consultation with experts in the field and parent members of the Study Steering Committee (SSC). The survey, which was anonymous, had two parts; the first focused on children with LD and long-term conditions and the second focused on children without LD with long-term conditions. The survey focused on five elements of care (capability, capacity, confidence, safety and values) for those with and those without LD, with additional questions regarding access to care and processes used to identify and track those with LD. Likert scales were used for each question, with the majority of questions rated on a five-point scale of ‘strongly agree’ to ‘strongly disagree’. Definitions of LD and long-term conditions were provided for clarification (see Report Supplementary Material 4).
Hospital policies
Sites were asked to provide policies related to the following areas of practice: (1) LD policy (or equivalent), (2) patient (children and young people) experience, (3) child protection, (4) complaints, (5) safeguarding, (6) communication and (7) restraint and holding.
Phase 2 research methods
Phase 2 compared how hospital care and services are experienced by children with and children without LD and their families, and staff’s views of caring for them. A sample of staff from NHS community trusts were also surveyed.
Setting and sample (hospital sites)
A subset of phase 1 hospitals participated in phase 2 data collection, based on the:
-
strength of the organisational context for delivery of care to children with LD
-
staff’s perceived ability to identify and meet the needs of children with LD
-
appointment of a learning disability liaison nurse who had the remit to improve care for children with LD.
To enable an objective selection of sites, scoring criteria were developed by the SSC, which was provided with anonymised information relating to four domains: (1) phase 1 recruitment, (2) hospital facilities and geography, (3) model of care and (4) phase 1 survey results. The executive team applied the scoring criteria, a shortlist was compiled and seven hospitals were included: four specialist children’s hospitals and three non-specialist hospitals (see Appendix 1, Figure 34). All sites had a principal investigator who was responsible for the study and a research nurse or equivalent who screened and approached eligible patients and provided day-to-day contact for the research team.
Sampling (participants)
Phase 2 involved data collection with a range of parents and children and staff working in both the hospital and the community (Table 1). A range of inclusion and exclusion criteria were applied (see Appendix 2).
| Participants | Sampling strategy | Sample size |
|---|---|---|
| Children and parents | A purposive sampling strategy using a sampling matrix to ensure diversity according to severity of LD, age, admission type, length of stay | 56–64 families |
| Hospital staff | A purposive sampling strategy using a sampling matrix to ensure diversity in terms of professional role. Includes subset of staff identified by families as potential participants | 112–28 |
| Ward managers | One from each study ward | 12 |
| Community staff | A convenience sample of staff from NHS community trusts providing health-care services to children in geographical proximity to the phase 2 hospital sites | 280–320 |
We did not recruit children aged ≥ 16 years because we anticipated that they would be in the process of transitioning to adult services, which would make it challenging to draw out similarities and differences in care and for children to be able to accurately reflect on only children’s services, and also because of the increasing body of work related to transition generally.
Operational definition of learning disability
The theoretical definition of LD is not always easily operationalised in practice. Among very young children, only severe LD is likely to be apparent,72 and some children never receive a formal diagnosis of LD, with medical records often stating ‘global developmental delay’ or a ‘syndrome without a name’. For the purposes of the study, a child was classified as having LD if any one of the following was documented in their medical notes:
-
a diagnosis of LD
-
a condition always accompanied by a degree of LD (e.g. Down syndrome)
-
global developmental delay
-
attendance at a special needs school accompanied by the parent verbally confirming that the child had LD.
Matching children and young people without learning disability
Children without LD were screened using four matching criteria: (1) age (5–7 years, 8–11 years or 12–15 years and 364 days), (2) expected length of stay (short, 1–2 nights; medium, 3–7 nights; long, ≥ 8 nights) and (3) reason for admission (surgical, medical or investigations/tests).
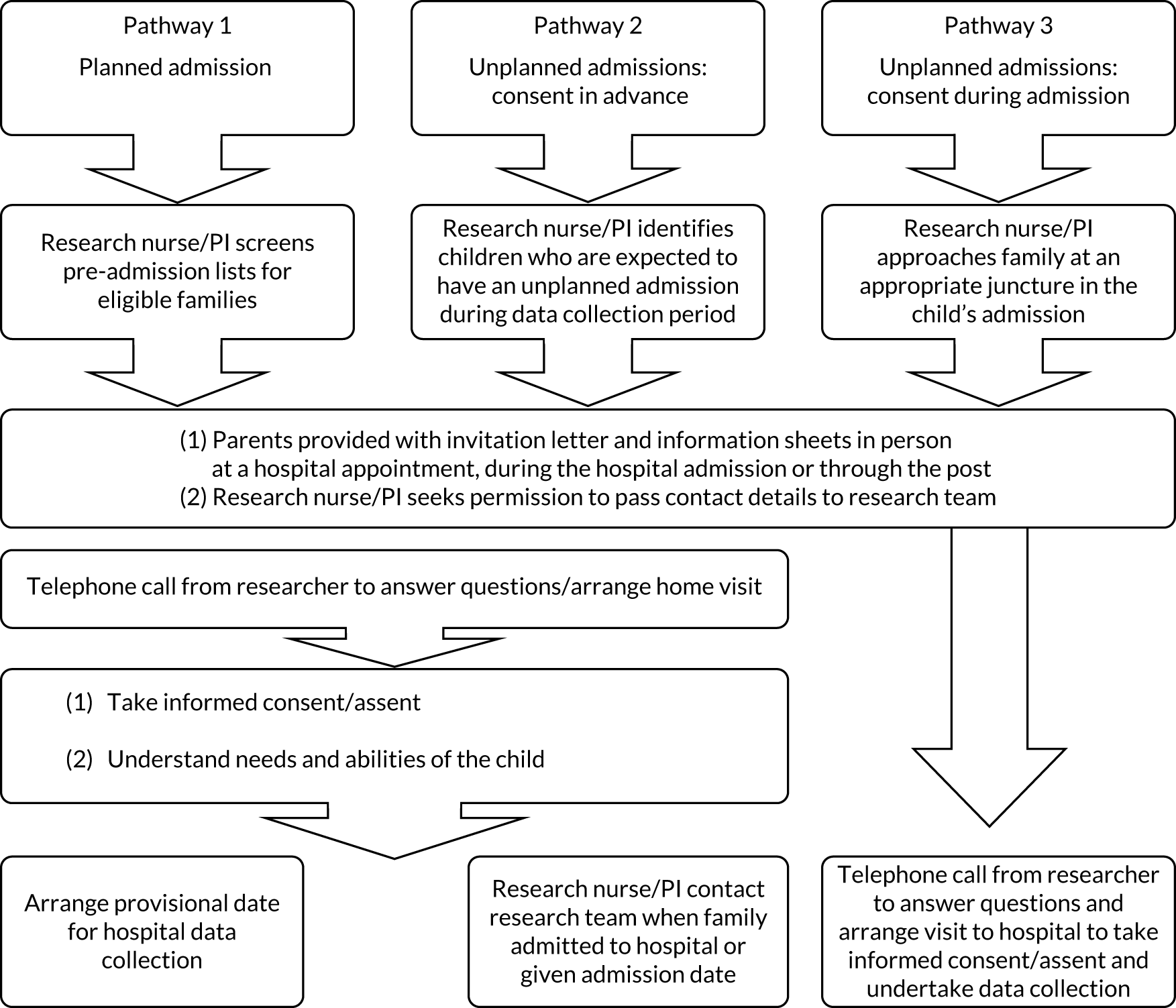
Recruitment and consent
Families
There were three pathways to recruiting and consenting children and their families (Figure 3). All children were invited to participate irrespective of their abilities. The researchers ensured that all participants understood what was being asked of them and that they could have a break or withdraw from the study at any time. Four versions of patient information leaflets were available so that children of different ages and abilities could be included: two were symbol based (see Report Supplementary Material 5) and two were word based (see Report Supplementary Material 6). Children who took part provided verbal or written assent, and their agreement was confirmed just prior to data collection. When possible, the consent/assent process took place in the family home to enable researchers to build rapport with families, ascertain the child’s abilities and interests to tailor data collection activities and ensure that the study questions were relevant and sensitive.
FIGURE 3.
Pathway to recruitment: families. PI, principal investigator.
Hospital staff
During the parent interview, participants were asked to identify hospital staff involved in the care of their child whom they were happy to be invited for interview. These staff names were given to the research nurse, who established the willingness of these staff members to participate. The research nurse also identified and approached additional staff, and provided them with an information sheet and a consent form. With permission, the contact details of staff interested in participating were given to the research team, who contacted them to answer any questions and arrange a mutually convenient time for data collection.
Community staff
Each local collaborator distributed the online survey by e-mail. The front page of the survey provided a synopsis of the study, guidance for completing the survey and study contact details. Submission of the survey was taken as consent to participate.
Methods of data collection with parents
Parents were invited to share their experiences through four data collection methods: hospital diary, photographs, safety review form and an interview following the child’s discharge. The diary offered flexibility in how parents shared their experiences and could be completed at any time of the day/night. Completing parent interviews post discharge enabled researchers to prioritise data collection with children during the hospital admission.
Hospital diary
Paper diaries and a pen were provided in an envelope, and parents were asked to leave these on the ward prior to discharge so that the research nurse could collect them. Guidance on completing the diary was provided, including prompts about who they had interacted with, what information they had been given, decisions that had been made and how they felt about what had happened. Space was provided for further reflections.
Safety review form
The SHINE tool73 was adapted for parents to document positive and negative aspects of their child’s care in relation to six areas of safety: medication, communication and information, equipment, unexpected complications of care, hygiene/cleanliness and ‘other’ (see Report Supplementary Material 7). Parents could also indicate whether they had seen something that was unsafe, and whether or not this had been dealt with. The form was completed just prior to the child’s discharge, or, if it was not, the researcher completed the form with parents during their home interview.
Photography
Parents were asked to capture images of three things that they thought worked well and three things that could be improved about their hospital experience using a camera provided.
Semistructured interview
Interviews were planned for as soon after the child’s discharge as possible. Flexibility was offered in terms of location and timing and also the format (either face to face or over the telephone). Interviews focused on the child’s recent hospital admission, and how the experience differed or not from previous admissions to the same or different hospitals. The semistructured interview guide (see Report Supplementary Material 8) included questions about the child’s needs and whether or not these were identified and met, and the role parents played. Interviews were audio-recorded and transcribed verbatim. All families were given a short study evaluation form to complete (see Report Supplementary Material 9).
Methods of data collection with children
A multimodal approach was used based on the premise that children are experts about their own lives and should be enabled to share their experience in accordance with their abilities and preferences. Researchers spoke to parents on the telephone in advance of data collection to ascertain how the data collection activities needed to be tailored for the child. Three activities were available to elicit data: Modified Talking MatsTM (Talking Mats Centre, Stirling, UK),74 a sticker exercise and a hospital tour. For children unable to participate themselves, parents were invited to participate as a proxy, providing answers from the perspective of their child. Data collection primarily took place at the bedside. With permission, data collection sessions were recorded and transcribed verbatim. A retrospective review of children’s medical notes was also undertaken.
Modified Talking Mats
Talking Mats74 is a communication symbol tool designed by speech and language therapists that uses picture symbols to assist people with a range of communication difficulties in expressing themselves. It has been used with people with LD. A professional artist was commissioned to produce the additional symbols needed for data collection (see Appendix 3), which were then checked with children with and children without LD to ensure that each illustration was a clear and accurate representation of the person/place/object/concept we were wanting to portray. Talking Mats has a ‘top line’ showing a character with a thumbs-up, a thumbs-down or a shrug of the shoulders, which were used in the study to denote ‘like’, ‘don’t like’ and ‘not sure’. For children who required concrete ‘like’ or ‘dislike’, the middle option of ‘not sure’ was removed. Children were presented with a range of symbol cards relevant to their inpatient experience, and they were asked, depending on their ability, to indicate or to physically place these under the appropriate top line card. Depending on the ability, engagement and concentration of the child and their specific hospital experience, the number and type (abstract vs. concrete) of symbol cards varied. Children were encouraged to elaborate, where possible, their feelings about the placement of each card. Children could indicate their preferences verbally, with eye gaze, using communication software or with their parents as communication partners.
Sticker exercise
Children were given a short survey about their interactions with hospital staff and a set of red (frown) and green (smiley) face stickers to indicate a yes or no response to each question. Three versions of the questionnaire were produced: a shorter and longer version using symbols and words (see Report Supplementary Material 10) and a word-only version (see Report Supplementary Material 11), with the addition of frequency responses to indicate how often something did or did not happen. This tended to be used with children who had higher cognition. The researcher read each question aloud, where necessary, and supported those with physical impairments to place their sticker.
Hospital tour with photography
To help children think about their hospital experience, we invited them to take the researcher on a hospital ‘tour’, identifying areas they had accessed during their admission and taking photographs using a digital camera. In practice, tours led by the child focused on the ward or bed space. If a child could not physically take a photograph, their parent or the researcher would take it on their behalf, from the child’s perspective. With the agreement of the child, the ‘tour’ was audio-recorded to capture data relating to what was being photographed. Children were free to take photographs of anything they chose, with the exception of other patients, visitors or identifiable information. Photographs of a member of hospital staff required the approval and written consent of that person. Immediately following the tour, the photographs were printed or viewed on the researcher’s laptop, depending on the child’s preference, and discussed. All children (or their parents) were offered copies of the photographs to keep.
Retrospective mapping of hospital appointments
A retrospective mapping of all inpatient stays and outpatient appointments for the preceding 2 years at the participating hospital was conducted using paper and electronic hospital records for each child and the electronic appointment system. Data from inpatient (e.g. age, diagnosis, treating team, date of discharge, hospital passport, reasonable adjustments) and outpatient (e.g. date and time of appointment, if they did not attend) records were collated in a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet.
Methods of data collection with staff
Hospital staff interviews
Interviews were conducted over the telephone or in person in a quiet room in the hospital, depending on the participant’s preference, using a semistructured interview guide (see Report Supplementary Material 12). Interviews lasted 30–60 minutes and were audio-recorded and transcribed verbatim.
Community staff survey
The phase 1 staff survey was modified, with questions added relating to access to secondary and tertiary care for children with and children without LD (see Report Supplementary Material 13). This was administered as per the phase 1 survey and stayed open for 3–5 weeks.
Phase 3 research methods
The aim of phase 3 was to compare the levels of satisfaction with hospital care between (1) children with and children without LD, and (2) parents of children with and parents of children without LD.
Recruitment and sampling
All seven phase 2 hospitals participated in phase 3, with data collection taking place on up to four wards identified by the principal investigator. All children and their parents who were admitted during the data collection period were eligible to participate. To facilitate the distribution and collection of surveys, no exclusion criteria were applied, and parents were asked to indicate if their child had a long-term condition, LD, neither or both. Participants were advised that returning a completed survey was taken as their consent to participate.
Data collection
An ‘easy-read’ survey (see Report Supplementary Material 14), based on a patient-reported experience measure developed by children and young people for children and young people,75 was developed for all children, irrespective of their age or perceived ability. An artist was commissioned to develop images to sit alongside each question, with a corresponding ‘thumbs-up’ or ‘thumbs-down’ and ‘smiley’ or ‘sad face’ tick box that children could use to indicate their response. The survey, available in English only, was piloted with inpatients at Great Ormond Street Hospital (GOSH) school, with and without LD, and minor revisions were made. Children could complete the survey independently or assisted by their parent, or the parent could complete it on the child’s behalf if the child was unable to. The parent survey (see Report Supplementary Material 15) contained a range of questions, the majority using a five-point Likert scale response. Non-English versions were available in seven languages. Wards were supplied with postboxes for completed surveys, which were collected by the research nurse and couriered to the research team.
Phase 2 and 3 data analysis
Qualitative and quantitative data were analysed in each phase before being merged and connected using data synthesis; congruence and incongruence between data sets was sought. Each data set was analysed by at least two members of the research team. Barriers to and facilitators of high-quality hospital care were identified for each data set, and these were then brought together, allowing a comparison of the factors identified by staff, parents and children. Specific examples of successful and effective measures that promote equal access were also identified. The analytical framework was compared with our initial theoretical framework in order to generate a final empirical framework of factors that affect the promoting of equal access to high-quality hospital care for children with and children without LD and their families.
Qualitative data analysis
The approach to analysis was relevant to each method of data collection; this is detailed in Table 2.
| Phase | Data | Method of analysis | Summary of analysis |
|---|---|---|---|
| 1 | Staff interviews | Framework analysis52,53 | Staff interviews were entered into NVivo 11; analysis was within and between data, applying the stages of framework analysis76 |
| 2 | Hospital documents | Summative content analysis77 | Predefined terminology (LD, special needs, intellectual disability, developmental delay, reasonable adjustments) was used to ascertain references to children with LD, creating a thematic framework based on content. The first set of documents was examined in detail and a coding frame was developed for use with subsequent documents |
| 2 | Parent interviews | Thematic analysis78 | Parent interviews were entered into NVivo 11 and read by at least two members of the research team; schematic maps were produced, checked and discussed further at team analysis meetings |
| 2 | Parent diaries | Thematic analysis78 | A subset of 20 diaries was read independently by two members of the research team, who then met to discuss the content and broad themes identified. An initial framework was developed and used when coding the diary content in NVivo 11, broadly identifying positive and negative experiences |
| 2 | Safety review form | Conventional content analysis77 | Data were extracted from the forms and summarised in a Microsoft Excel spreadsheet using the six domains. Cells were colour coded, and highlighted by one researcher as green indicating a positive issue, red indicating a negative issue and orange indicating in between. The spreadsheet was checked by a second researcher and minor revisions were made. Content analysis aided the counting and reporting of themes |
| 2 | Children’s interviews |
Counting to produce visual maps Thematic analysis78 |
Completed Talking Mats interviews and sticker charts were analysed for the frequency of responses, VILD charts produced to present data, interview data were analysed thematically |
Quantitative data analysis
Staff survey data (phases 1 and 2)
Descriptive statistics were used to characterise the sample. Composite variables were computed to represent capability, capacity, confidence, safety and values separately for questions related to LD and no LD (see Appendix 4, Table 15). All composite variables had acceptable internal reliability, with Cronbach’s alpha values of > 0.7. Composite variables and individual questions about involvement in service delivery and planning services, safety, values and meeting needs were analysed using Wilcoxon signed-rank tests, comparing responses about children with LD with those about children without LD for the total sample and, for hospital staff (phase 1), separately for respondents from children’s and non-children’s hospitals. Responses from community staff were also compared about admission and discharge (phase 2) for children with and children without LD using Wilcoxon signed-rank tests. Differences between children’s and non-children’s hospitals or between hospitals with and hospitals without LD nurse provision were compared using Mann–Whitney tests.
Parent and child satisfaction data (phase 3)
For the purposes of this report we focused on responses from parents and/or children with a long-term condition, with and without LD. Descriptive statistics were used to characterise the sample. Composite variables representing key domains related to satisfaction with care to meet their child’s needs, staff interaction and communication (parent survey) and environment, people, and care and treatment (child survey) were calculated (see Chapter 11). All composite variables on the parent survey had satisfactory internal reliability (Cronbach’s alpha > 0.8); all Cronbach’s alpha values for the composite variables in the children’s survey were > 0.6. Responses were compared separately for children with and children without LD and parents of children with and children without LD using Mann–Whitney, chi-squared or Fisher’s exact tests, as appropriate. For all surveys in each phase, a Bonferroni correction for multicomparisons was made, resulting in an alpha level of 0.005. All data were analysed using IBM SPSS Statistics version 22 (IBM Corporation, Armonk, NY, USA).
Phase 4
Findings from phases 1–3 were synthesised and shared with hospital staff at the phase 2 hospitals, and an open dissemination event was held at GOSH on 18 June 2019. The aim of this was to generate discussion to inform the development of a LD training package for staff. The views of families were also sought through discussion with individual patients on the ward and consultation with members of the Parent Advisory Group (see Parent Advisory Group).
Patient and public involvement
Aim
Patient and public involvement has been central to our work from the outset, with our primary aim being to ensure that the study was carried out in an appropriate, accessible and sensitive manner.
Preparation of proposal for grant funding
This study evolved from four pieces of work involving the chief investigator (KO) and/or other members of the research team (FG, JW, ITW). Key to each of these was our commitment to hearing what matters most to participants. The chief investigator consulted widely with parents, staff and LD experts about the RQs, design, data collection methods and dissemination to ensure that these were acceptable, feasible and of importance. One parent said: ‘Very important – LD are overlooked. My local trust only appointed a LD nurse advisor following a death, which was far too late’. Our parent co-applicant (SK) provided valuable insights and expert PPI throughout the study.
Involvement since grant funding
Parent Advisory Group
A group of 8–10 parents of children with and children without LD who had used hospital services was established to advise on all phases of the study. The Parent Advisory Group met twice per year during the study, with contact between meetings taking place by e-mail for specific requests and study updates. Representatives of the Parent Advisory Group attended three of the four of SSC meetings and fed back to other Parent Advisory Group members.
Phase 1
The Parent Advisory Group gave feedback on the preliminary results from the interviews in a sense-checking exercise to ascertain if the findings resonated with their experiences; this resulted in changes to the phase 2 parent interview topic guide.
Phase 2
The Parent Advisory Group gave feedback on data collection with children, parents and hospital staff. This was either during face-to-face meetings (Table 3) or at the Study Steering Committee meeting, where the group was involved in the ranking exercise for the selection of phase 2 sites and the challenges associated with phase 2. Additional feedback was elicited between meetings by e-mail on aspects such as the layout and instructions of the parent diary, the appropriateness of the parent safety review tool, and the content and layout of the information sheets and consent forms.
| Area of feedback | PPI | |
|---|---|---|
| Staff | Hospital staff recruitment | Recruitment procedure |
| Community staff survey | Suggested content | |
| Parent | Recruitment | Acceptability of procedure |
| Diary | Acceptability/feasibility of method and process | |
| Safety review form | Acceptability/feasibility of method and process | |
| Interview process | Acceptability/feasibility of method and process | |
| Interview topic guide | Suggested content | |
| Children | Use of cameras | Acceptability/feasibility of activity |
| Talking Mats | Acceptability/feasibility of activity | |
| Arts and crafts activities | Acceptability/feasibility of activity |
Phase 3
Feedback was provided on the style, format and administration of the survey to parents, as well as the clarity of questions and completion time. Parents’ knowledge of being in hospital, receiving care and navigating the system was hugely informative, resulting in timely changes to the survey. For the children’s survey, revisions were made to the wording of some questions, ideas were provided for pictures to accompany questions and some questions were moved to the parent survey.
Study Partnership Schools
Two local special educational needs schools, Richard Cloudesley School and The Bridge School, agreed to be Study Partnership Schools. One member of staff was pleased that the students had been asked to help, as it was felt that they were often overlooked for similar opportunities.
Discussions about the methods for collecting data from children were held, and school staff chose to trial the activities that they felt would benefit their students the most. In one school, a class trialled the photograph elicitation activity by taking photographs of their school and documenting what they liked and disliked. These photographs were subsequently used to produce an ‘about my school’ book to help familiarise new students with the school. In the other school, students trialled Talking Mats using photographs and picture symbols to share what they liked and disliked about their curriculum and school environment. A summary of each child’s participation was produced for the class teachers. Both schools were offered a presentation of the phase 1 study results. The opportunity to trial the methods was invaluable for assessing feasibility, strategies for delivery and the extent of student interest and engagement. Staff also gave helpful advice on elicitation techniques used in classroom settings for children with LD.
Students in the GOSH school provided feedback on proposed designs for picture–symbol cards for use with Talking Mats and the children’s survey. Students were asked to describe each picture and what changes could be made to improve clarity. They indicated their preferences for thumbs-up/thumbs-down, smiley faces/sad faces or ticks/crosses for the response options.
Young People’s Advisory Group and Young People’s Forum
Great Ormond Street Hospital runs two groups to provide researchers and clinicians with feedback on research and clinical services. The GOSH Young People’s Advisory Group, comprising 8- to 19-year-olds, is part of a national network of Young People’s Advisory Groups that meets regularly with the remit to be involved in the design and delivery of clinical research to ensure that it is relevant to children, young people and families. The Young People’s Forum, comprising children and young people aged 10–21 years, aims to improve the experiences of teenage patients. Both groups gave feedback on the proposed phase 2 research methods for children, including trialling aspects of the ‘hospital tour’ photograph elicitation activity by taking photographs of public access areas at GOSH and discussing these based on their experience of their own hospital admission. This process informed the practical set-up and delivery of this method of data collection.
We successfully integrated PPI into our research, underpinned by the research team’s belief that PPI is a worthwhile pursuit. Our Parent Advisory Group was pivotal; the members have provided input throughout, and we would highly recommend having a dedicated PPI co-ordinator, supported by other members of the research team. We extend our thanks to all of our PPI partners who have contributed to our study.
Section 3 Results
The results section comprises five chapters. The first three focus on findings from staff, with data from the survey used to identify whether or not staff perceive that inequality exists between children with and children without LD and their families (see Chapter 5). Findings from the organisational mapping exercise (see Chapter 6) and staff interviews (see Chapter 7) subsequently highlight the cross-organisational, organisational and individual staff factors in NHS hospitals that facilitate and prevent such inequality.
Chapters 8–10 focus on parents’ experience of being in hospital with their child with LD. These draw primarily on data from home interviews, supplemented by findings from the parent diaries and safety review form. Parents’ views on how well their child’s needs are met in hospital are reported, as are perceptions of their own role and the impact of hospitalisation on their health and well-being. Comparisons are made with data collected from parents of children without LD. The barriers to and facilitators of children with LD receiving equal access to high-quality hospital care that meets their particular needs are drawn out. Chapter 11 focuses on the findings from the parent and child survey about satisfaction with different aspects of the hospital experience. Findings from children are presented alongside data from the Talking Mats and sticker exercise.
The findings presented should be considered in the context of the Equality Act 2010,79 which sets out the legal duty health-care services have to consider the needs of all people with disabilities, including children, in the way that they organise their buildings, policies and services. This does not mean treating everyone the same but rather it means taking reasonable steps to avoid disadvantage arising from any provision, criterion, practice, physical feature or lack of auxiliary aid that puts any child at a substantial disadvantage. 79 These ‘reasonable adjustments’ reflect the fact that some people with disabilities may have particular needs that standard services do not adequately meet80 but are entitled to expect equality in the outcomes of their hospital stays. It is recognised that people, including those with disabilities, can experience discrimination not just from individuals but from entire organisations such as hospitals, albeit unintentionally. 79 Discrimination includes a child being treated unfavourably because of something arising as a consequence of their disability or if it cannot be shown that their treatment is a proportionate means of achieving a legitimate aim. The only exception is if it can be shown that the person/provider did not know, and could not reasonably have been expected to know, that the child was disabled.
The findings must also be considered in the context of discussions about equal access, equality and equity. Equal means ensuring that everyone has equal opportunities, with no one being treated less favourably because of who they are or what makes them different from other people. 81 Both equality and equity promote fairness, but via different means: the former through ‘treating everyone the same regardless of need’ and the latter through ‘treating people differently dependent on need’. 82 As highlighted by Social Change UK, ‘If equality is the end goal, equity is the means to get there’ (reproduced with permission from Social Change). 82 An essential point is that treating people the same does not necessarily result in equity of outcome. Distinguishing between equality and equity is not necessarily straightforward, especially because the two terms are inextricably linked and sometimes used interchangeably. 83,84 As Northway83 suggests, ‘a failure to make the necessary adjustments to promote equality of access to healthcare results in inequity’ (© 2022 University of Hertfordshire). 83 In this study, we have been able to generate a large body of evidence about the way in which hospital inpatient care is delivered to and experienced by children with LD and their parents, from the perspective of multiple stakeholders, as well as drawing comparisons with children without LD and their families. Although we did not formally measure whether or not children and young people with LD experience equitable outcomes, our focus on equality revealed a lack of individualised hospital care for those with LD based on their particular needs, as well as a lack of policies, systems and processes to facilitate this. Our findings support the principle that ‘working towards equity and not just equality requires . . . seeing another person and their situation clearly enough to understand that what works for one does not work for all’. 85 Thinking equitably may help those providing care to think more pro-actively about the need for reasonable adjustments83 and is an important factor in changing clinical practice going forward.
Chapter 5 Staff survey
Parts of this chapter have been reproduced with permission from Oulton et al. 86 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Parts of this chapter have been reproduced with permission from Kenten et al. 87 © 2019 The Authors. Journal of Applied Research in Intellectual Disabilities published by John Wiley & Sons Ltd. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
The aim of this chapter is to present the results from an anonymised online survey of 2261 hospital staff working across 24 NHS hospitals across England (phase 1) and 429 community staff associated with a subset of seven of these hospitals (phase 2) (Table 4). Our target sample size for the hospital survey was 1800, which we exceeded, but our method of approaching eligible staff for survey completion (via local collaborators in the hospitals and community) precluded being able to determine response rates.
| Method | Number of hospital sites | Number of participants | Staff group (n) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Doctor | Nurse | Allied health professional | Health-care assistant | Other | |||||
| Hospital | |||||||||
| Survey | 24 | Children’s hospital (n = 15) | 2261 | Children’s hospital (n = 1681) | 272 | 762 | 308 | 79 | 260 |
| Range per site (38–202) | |||||||||
| Non-children’s hospital (n = 9) | Non-children’s hospital (n = 580) | 105 | 222 | 67 | 50 | 136 | |||
| Range per site (7–131) | |||||||||
| Community | |||||||||
| Survey | 7 | Children’s hospital (n = 4) | 429 | Children’s hospital (n = 285) | 21 | 57 | 100 | 22 | 85 |
| Range per site (12–202) | |||||||||
| Non-children’s hospital (n = 3) | Non-children’s hospital (n = 144) | 11 | 32 | 32 | 19 | 50 | |||
| Range per site (31–70) | |||||||||
The results are used to help answer four of our five RQs (RQ1, RQ2, RQ3 and RQ5) related to inequality between children with and children without LD and their families. We also provide evidence of whether or not our related phase 1 hypotheses, developed a priori, are supported. The survey questions used for each domain are shown in Appendix 5.
Inequality between children with and children without learning disability, from the perspective of clinical staff
Comparing staff’s views about the hospital care and treatment of children with and children without LD and their families indicates the areas of practice in which staff perceive inequality (Table 5). The results showed significant differences in staff’s views in relation to children with LD (1) having access to high-quality hospital care that meets their particular needs (RQ1); (2) having access to hospital appointments, investigations and treatments (RQ2); (3) being involved as active partners in their treatment, care and services (RQ3); and (4) being safe (RQ4), indicating perceived inequality for children with LD in response to each of our RQs. The only exception was staff perceptions about staff relying on parents too much, which showed no difference between the two groups. However, community staff did perceive there to be a difference, feeling that parents of children with LD were relied on too much by staff, compared with parents of children without LD.
| RQ | Individual questions | Children with LD (%) | Children without LD (%) | Statistics | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (SA) | 2 | 3 | 4 | 5 (SD) | 1 (SA) | 2 | 3 | 4 | 5 (SD) | |||
| 1. Do children with and children without LD and their families have equal access to high-quality hospital care that meets their particular needs? | Necessary knowledge and skills to meet needs | 21 | 45 | 26 | 6 | 3 | 55 | 36 | 6 | 2 | 1 | z = 22.24; p < 0.001 |
| Necessary training to meet needs | 16 | 36 | 29 | 13 | 6 | 50 | 37 | 9 | 3 | 2 | z = 24.66; p < 0.001 | |
| Routinely have access to necessary resources to meet needs | 7 | 25 | 26 | 22 | 10 | 34 | 46 | 14 | 4 | 2 | z = 27.26; p < 0.001 | |
| Routinely have access to additional specialist support to meet needs | 19 | 34 | 23 | 15 | 9 | 33 | 38 | 17 | 7 | 5 | z = 15.36; p < 0.001 | |
| Routinely have access to additional LD specialist staff to meet needs | 10 | 20 | 26 | 27 | 18 | NA | NA | NA | NA | NA | NA | |
| Feel confident to communicate effectively with them | 19 | 39 | 30 | 10 | 2 | 62 | 31 | 5 | 1 | 1 | z = 26.56; p < 0.001 | |
| Feel confident to assess and manage pain | 12 | 34 | 27 | 24 | 12 | 43 | 33 | 11 | 5 | 8 | z = 24.75; p < 0.001 | |
| Work in an environment that is designed to take into account their individual needs | 14 | 33 | 31 | 16 | 6 | 35 | 44 | 16 | 4 | 2 | z = 23.85; p < 0.001 | |
| 2. Do children with and children without LD, assisted by their families, have equal access to hospital appointments, investigations and treatments? | Appropriate access to medical care and equipment | 34 | 44 | 19 | 3 | 1 | 47 | 41 | 10 | 1 | 1 | z = 13.40; p < 0.001 |
| Appropriate access to education | 24 | 36 | 28 | 8 | 3 | 39 | 39 | 15 | 4 | 2 | z = 16.94; p < 0.001 | |
| Appropriate access to play | 30 | 39 | 21 | 7 | 3 | 39 | 40 | 15 | 4 | 2 | z = 11.63; p < 0.001 | |
| Appropriate access to appointments | 33 | 43 | 20 | 3 | 1 | 37 | 42 | 18 | 3 | 1 | z = 3.93; p < 0.001 | |
| Appropriate access to double appointments | 16 | 24 | 38 | 14 | 7 | 20 | 24 | 38 | 13 | 6 | z = 4.66; p < 0.001 | |
| Appropriate access to first or last appointments | 15 | 24 | 38 | 15 | 7 | 19 | 25 | 37 | 13 | 6 | z = 5.10; p < 0.001 | |
| Appropriate access to flexible appointments | 16 | 23 | 38 | 16 | 8 | 20 | 25 | 35 | 14 | 6 | z = 6.96; p < 0.001 | |
| 3. Are children with and without LD and their families equally involved as active partners in their treatment, care and services? | Routinely involve children when making decisions about treatment | 29 | 39 | 20 | 6 | 5 | 49 | 36 | 9 | 2 | 3 | z = 18.23; p < 0.001 |
| Routinely involve parents/carers in making decisions about care and treatment | 61 | 25 | 6 | 3 | 5 | 65 | 25 | 6 | 2 | 2 | z = 4.33; p < 0.001 | |
| Children are routinely involved in the planning of services | 16 | 32 | 33 | 12 | 6 | 29 | 44 | 20 | 5 | 1 | z = 16.21; p < 0.001 | |
| Parents/carers are routinely involved in the planning of services | 32 | 35 | 22 | 8 | 3 | 39 | 38 | 17 | 5 | 1 | z = 8.85; p < 0.001 | |
| Parents/carers are relied on too much by staff | 19 | 30 | 29 | 15 | 7 | 18 | 31 | 28 | 14 | 9 | z = 1.18; p = 0.237 | |
| 5. Are safety concerns for children with and children without LD the same? | Feel confident to safely manage challenging behaviour | 10 | 33 | 32 | 19 | 6 | 26 | 44 | 20 | 7 | 2 | z = 23.31; p < 0.001 |
| Work in an environment that is safe for meeting needs | 14 | 42 | 29 | 11 | 4 | 43 | 43 | 10 | 3 | 1 | z = 24.02; p < 0.001 | |
| Always able to deliver safe care | 16 | 42 | 30 | 8 | 3 | 39 | 45 | 11 | 3 | 2 | z = 21.89; p < 0.001 | |
The z-scores and p-values are shown for the results of Wilcoxon tests for paired data, comparing staff’s responses about caring for children with and children without LD. The areas of practice that showed the greatest difference in hospital staff views were staff knowledge, skills and training to meet the needs of children with LD. This included their confidence in communicating effectively, managing pain and safely managing ‘challenging behaviour’; having access to necessary resources and an environment that is safe and appropriately designed to meet their needs; and being able to deliver safe care (see Table 5).
Hypotheses
The following phase 1 hypotheses were developed to address our RQs:
-
Staff will perceive that they are less able to meet the needs of children with LD, in terms of their confidence, capability and capacity, than the needs of children without LD.
-
Staff will perceive that children with LD and their parents have less involvement in decisions and planning services than children without LD and their parents.
-
Staff will perceive that children with LD are less safe in hospital than children without LD.
-
Staff will perceive that children with LD are valued less and treated with less dignity and respect than children without LD.
With the exception of one aspect, each of our hypotheses was supported by the data (see Appendix 4, Table 15, and Table 5):
-
Hospital staff reported less capacity and lower levels of capability and confidence in meeting the needs of children with LD compared with those without LD, and this was true for respondents from both children’s and non-children’s hospitals. This was also true for community staff with respect to confidence (see Appendix 4, Table 15).
-
Hospital staff perceived that children with LD were significantly less involved than children without LD in decisions about their care (see Table 5) and in planning services, and this was the case for respondents from both children’s and non-children’s hospitals and for community staff. Hospital staff from children’s and non-children’s hospitals also thought that parents of children with LD were significantly less involved than parents of children without LD in planning services, but this was not the case for community staff. However, although staff from children’s hospitals thought that parents of children with LD were significantly less involved than parents of children without LD in making decisions about care, those in non-children’s hospitals did not report any differences and neither did community staff.
-
Staff perceived that children with LD were less safe in hospital than children without LD. This finding was true for respondents from both children’s and non-children’s hospitals, but not for community staff, who did not report any difference in their perceptions of the safety of children with and children without LD (see Appendix 4, Table 15).
-
Staff perceived that children with LD were valued less and treated with less dignity and respect than children without LD, and this was true for respondents from both children’s and non-children’s hospitals.
Chapter 6 Organisational context
Having established that children with LD and their families experience inequality (from the perspective of clinical staff) in relation to numerous areas of hospital care, our aim in this chapter is to explore the organisational factors in NHS hospitals that facilitate or prevent this inequality. The results of the organisational mapping exercise conducted in phase 1 are presented, pertaining to the policies, systems and practices related to the care of children with LD and their families that are in place in NHS hospitals. Also included are findings from the staff survey, related to whether having a flagging system or dedicated LD nurse provision has an impact on staff’s perceptions about the care of these patients.
Sixty-five staff members across 22 hospitals (Table 6) were interviewed, with at least two interviews conducted per hospital. Included was a subset of nine nurses and one allied health professional employed in a dedicated LD nurse role, or similar, the results of which are also reported.
| Method | Number of hospital sites | Number of interviews | Staff group (n) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Doctor | Nurse | Allied health professional | LD nurse | Senior manager | Other | |||||
| Interview | 22 | Children’s n = 15 | 65 | Children’s n = 48 | 6 | 15 | 2 | 8 | 13 | 4 |
| Non-children’s n = 7 | Non-children’s n = 17 | 4 | 11 | 0 | 2 | 1 | 0 | |||
The findings presented in this chapter show that, nationally, there is considerable variation among hospitals in terms of the policies, systems and practices in place specifically for children with LD. Some appear to have little, if anything, in place, some have partial systems, policies or practices and some have a cohesive and comprehensive level of provision (Table 7). These groupings were decided based on what was described as being in place, as well as how well the senior managers in hospitals articulated their responses and the level of clarity and certainty with which they talked about LD provision.
| Type of hospital | LD nurse | Flag and alert | Hospital passport | Stand-alone LD policy or alternative | Planning services involving parents | Planning services involving children | Planning services involving children with LD | Feedback from parents | Feedback from children | Feedback from children with LD | LD identified complaint | LD identified clinical incident | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohesive | C | ||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| N | |||||||||||||
| N | |||||||||||||
| Partial | C | ||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| Little or none | C | ||||||||||||
| C | |||||||||||||
| C | |||||||||||||
| N | |||||||||||||
| N | |||||||||||||
| N | |||||||||||||
| N | |||||||||||||
| N |
Policies
Across organisations, none of the interviewees reported that their trust had a stand-alone LD policy for children. More commonly, issues related to the care of children with LD were integrated into a range of policies (three hospitals) and/or other documents (five hospitals), such as a LD care pathway, a protocol, the Mencap Charter88 or standards. The LD care pathway was reported to offer a way of prompting staff to ‘think about what they need to do’ (nurse, specialist children’s hospital B) to make necessary reasonable adjustments for children with LD, for example in relation to the length and timing of outpatient appointments. A LD protocol was described as more prescriptive than, and different from, a pathway, in that it was for ‘staff to follow’ and was about ‘making sure that they make reasonable adjustments and giving them the tools to do so’ (nurse, non-children’s hospital J). One children’s hospital used standards rather than a LD policy so that it ‘could audit against it . . . because sometimes policies were there to refer to but the standard was trying to make it happen’ (play specialist, children’s hospital K).
The decision in one hospital to integrate aspects of LD into existing policies rather than have a stand-alone policy was intended to encourage staff to be ‘less reliant’ on LD nurses. In nine hospitals there was either a lack of knowledge at a senior level about what policies existed or a lack of consensus among participants from the same organisation.
Systems
System for identifying and flagging children with learning disability
Looking across organisations, fewer than half of the 22 hospitals (45%; eight children’s/two non-children’s) had an electronic flagging and/or alerting system in place for identifying children with LD. It was clear that no consistent formal or informal approach to identification existed, with various external sources of information being utilised in practice, including a general practitioner (GP) referral letter or liaison with a school. If a diagnosis of LD was made in a community setting, this might not be known in the hospital. Internally, information about a child’s LD was ascertained through various means such as hospital records, pre-assessment clinics or another hospital service/department or through discussions with parents during the admission or clinic visits. In four sites, staff felt that parents might not support the identification of children with LD because it felt wrong to ‘label’; emphasis instead was placed on children as ‘individuals’ who should be treated ‘the same’, with equality being favoured over equity. In one children’s hospital, staff actively sought permission from parents before a flag was applied, providing an opportunity for a ‘valuable conversation about the benefits of flagging’, and in another a personalised approach was taken, with the distinct needs of all children being ‘assessed and catered for’ (nurse, specialist children’s hospital F).
Once a flag was applied, the system for alerting staff varied. Most commonly, an e-mail was sent to the LD nurse team in the hospital, which could trigger a telephone call from the LD nurse to the ward to ask about making reasonable adjustments and/or providing a hospital passport. In one site, a children’s hospital, the e-mail notification went to multiple staff, including the ‘music therapist’ and the ‘disability teacher’. The only site that had a flagging system in place without LD nurse provision was a children’s hospital that relied on an ad hoc system of sharing information:
We will put a flag so that when they’re admitted it’s flagged up prior to their admission that they’ve got a LD . . . quite often that information is given to the wards . . . put in the diary about what they need. If I’ve got children with specific needs, such as they need a special bed with high sides . . . the consultant would flag that, quite often as part of the pre-assessment.
Nurse, specialist children’s hospital L
In some hospitals a flagging system was in place, but this was not accompanied by an automatic process of letting staff in relevant roles know that the flag existed.
In relation to the staff survey, one-quarter of respondents, including 19% of nurses and 28% of doctors, reported not knowing what systems their hospital had in place for identifying patients with LD. In some hospitals there was a lack of agreement about the systems that were in place. For example, in one children’s hospital, 62% staff reported that there was no electronic flagging system, whereas 38% staff reported the opposite.
Whether or not children with LD are identified was viewed as depending on staff receiving initial and ongoing training, gaining experience over time, having sufficient time with the patient and their family and having access to appropriate resources. Senior and more experienced ward staff were more likely to identify these patients and to implement reasonable adjustments to meet these patients’ needs. It was expected that staff involved in a child’s care would ask about any LD and/or would have read a patient’s notes. However, it was also recognised that insufficient knowledge about LD could mean that this would be omitted during admission.
Despite just under half (n = 998, 48%) of all survey respondents agreeing that they were routinely informed of a child’s LD, three-quarters felt extremely confident or confident in identifying that a child in their care or who they met had LD. Those from children’s hospitals reported feeling more confident (76%) than respondents from non-specialist hospitals (70%) and senior nursing and allied health staff (bands 7 and 8) felt more able to identify children with LD than their junior colleagues (bands 1–4, 5 and 6) (79% vs. 71%). Staff in both children’s and non-children’s hospitals were more confident when their trust gave them information about how to define LD. Furthermore, staff working in hospitals that had a dedicated LD nurse (see Learning disability nurse provision) were more likely to have been given information about how to define LD than staff working in hospitals that did not have a dedicated LD nurse (46% vs. 41%).
There appeared to be a correlation between the flagging of LD and staff’s views about reasonable adjustments and safety. Staff from hospitals that flagged felt more able to identify reasonable adjustments that are needed for children with LD than did those from hospitals that did not flag; they also felt more confident that any reasonable adjustments would be accommodated in a timely way. Furthermore, staff from hospitals that flagged were more likely to report working in an environment that was deemed safe for meeting the needs of children with LD, always being able to deliver safe care and feeling more confident to safely manage challenging behaviour. Despite feeling more able to identify children with LD, senior nursing and allied health staff (bands 7 and 8) were no more likely to implement reasonable adjustments than their junior colleagues (bands 1–4, 5 and 6).
System for recording complaints and clinical incidents
Interviewees from only two sites (a children’s and a non-children’s hospital) reported a specific mechanism being in place for identifying that a child at the centre of a complaint or clinical incident had LD, such as a tick box or a specific section on the complaints form, highlighting a lack of recognition of the importance of this nationally. A range of practices within and across sites was described that could result in a child’s LD becoming apparent:
Well you should be able to . . . hopefully someone will have documented within the incident that that had been the case, and also if you looked up that child, or that patient . . . then a flag should come up saying they have a learning disability.
Nurse, specialist children’s hospital 5
Other factors that depended on an individual’s response to the incident or complaint included the staff knowing the child or identifying LD based on knowledge of the services the child used. Participants from two hospitals, children’s and non-children’s, said that complaints relating to children with LD were sent to LD staff, although no specific mechanism was described for identifying that the child had LD.
When asked about safety, staff from 12 sites (nine children’s and three non-children’s hospitals) felt that there were no differences in their concerns and/or the way safety is managed between children with and children without LD, with some suggesting that children with LD had the same safety issues as children without LD. Those who reported differences between the two groups identified six areas of risk specific to the care of children with LD (Table 8), most of which were associated with the characteristics of the individual child.
| Theme | Subthemes |
|---|---|
| Child | Challenging behaviour |
| Difficulties maintaining personal safety and/or reporting abuse | |
| Communication impairment | |
| Physical impairment – risks with moving and handling | |
| Feeding – risk of choking | |
| Need for routine/familiarity | |
| Complexity of care/comorbidities/medication regimes | |
| Lack of understanding | |
| Equipment | Lack of appropriate equipment |
| Staff | Reliance on parents |
| Lack of familiarity with moving and handling | |
| Lack of time | |
| Environment | Inappropriate space |
| Other people | May pose a risk to physical safety of children with LD |
| Information | Lack of hospital passport |
| Lack of information-sharing | |
| Insufficient risk assessment |
Practices
Learning disability nurse provision
The interviews revealed that LD nurse provision was in place in eight (53%) children’s hospitals and one (14%) non-children’s hospital. Provision ranged from one to four staff per site, working full- or part-time in various roles, including lead nurse, liaison nurse, nurse specialty, disability assistant and nurse consultant. Some worked across multiple hospitals, some worked across hospital and community settings and some worked in child and adolescent mental health services only.
Interviews with those working in a dedicated LD nurse role revealed elements of the role’s operationalisation in practice, as well as valuable insights into workforce and organisational culture. A key finding was the varying breadth and depth of provision across children’s hospitals; some worked in particular clinical areas, whereas others had trust-wide responsibility; some worked with all children with LD; and others worked with particular groups of children only, such as those with autism and LD. In addition, some LD nurses had been employed to work on particular projects for a defined period only. Nurses’ understanding about what was in place at the organisational level invariably differed, with some being knowledgeable only about their specific area of practice. One nurse was critical of the lack of LD nurses employed nationally at a senior level, indicating that this was seen as typical of the lack of value placed on the lives of patients with LD. Many nurses highlighted the value of LD champions or link leads, although one felt that most in their organisation were not actively engaged with the role.
Some staff talked about the culture of the organisation regarding the care of children with LD. There was a strong feeling that there was a lot of work to do and that things were far from perfect, with one nurse describing their trust as ‘tokenistic’ and risk averse towards LD care. However, some sensed a growing willingness and commitment within their organisation to get it right for this population, with the belief that ‘if we get it right for children with LD or additional needs, we’ll get it right for everybody hopefully’ (LD nurse, specialist children’s hospital A). As one nurse said:
We have very good support from people quite high up . . . we need to be doing more, we need to be reasonably adjusting. We want to listen, we want to improve things. We want children, their parents or carers to want to come to this trust . . . not be frightened to come back.
LD nurse, specialist children’s hospital B
Each of the LD nurses interviewed talked about varying components of their role, and these were mapped onto previously developed role descriptors89 (see Appendix 6, Figure 35). A key focus was on their role as facilitators through contact with either families or supporting staff, especially in relation to supporting reasonable adjustments. The importance of individualised care for patients was described, for example in relation to hospital appointments, the physical and sensory environment, waiting and safety. Having accessible information was seen as key, including using symbols and photographs to make visual journeys of the hospital available to patients in advance of their admission, creating visual timetables and improving hospital signage. Hospitals varied, however, in terms of what they used, particularly in relation to knowledge and use of easy-read materials.
Although nearly three-quarters of sites were reported to have a hospital passport or equivalent available for documenting information about the needs of children with LD, particular issues were described by LD nurses with the use of these in practice. As one said, ‘we get complaints from parents that even when a passport has been pushed through to somebody’s hand, that they feel it hasn’t been read’ (LD nurse, specialist children’s hospital C). This nurse explained that families often do not come in with passports or they do not have the time to access and complete them, and that there are barriers for parents whose first language is not English, or who have LD or low literacy levels. Similar challenges were described in relation to staff utilising hospital passports:
We’ve rolled out the health passport but that’s in relation to the individual practitioner . . . it links to staff knowledge, time and accessibility of the document and the willingness of the practitioner to read or take information from it . . . trying to make sure that’s standard practice at the moment.
LD nurse, specialist children’s hospital A
In another hospital, a lack of ‘organisational commitment’ was felt to have prevented the hospital passport from being implemented:
We were working with a group which included parents . . . to try and develop a passport for children with complex needs. It went quite well but really hasn’t, kind of, been used very much . . . I don’t think, real, kind of, organisational commitment to it.
LD nurse, non-children’s hospital D
A related challenge reported by one LD nurse was acquiring the relevant information to plan and make reasonable adjustments in advance, rather than having to adopt a reactive approach:
If a family can give us plenty of notice once they get their letter then we can start making adjustments but what we are not good at is picking up from the moment . . . to be proactive and to say ‘Hi, what do you need us to do?’ because children are varied and they change so quickly, so we tend to rely on families getting in touch with that.
LD nurse, specialist children’s hospital C
Educating staff and students appeared to be another large component of the LD nurses’ role, and this was seen as fundamental to getting it right for families, alongside staff having opportunities to put their learning into practice. The link between training and confidence was highlighted, as was the need to empower and upskill professionals. A positive initiative in one specialist children’s hospital was training volunteers and staff across accident and emergency and reception areas in positive behaviour support to help children with behaviours that challenge.
Some LD nurses spoke about the strategic element of their role, and of trying to influence the culture and practices at the organisational level through the creation of systems, pathways and policies. These nurses tended to be employed at a more senior role with a trust-wide remit, rather than working in a particular department or with a specific group of children.
Comparing the views of staff working in the eight children’s hospitals with dedicated LD nurse provision (n = 752) with those of staff working in the seven children’s hospitals without dedicated LD nurse provision (n = 929), no significant differences were seen in relation to (1) staff being routinely informed that a child has a LD; (2) staff’s confidence, capability or capacity to meet the needs of children with LD; (3) perceptions of the hospital valuing children with LD; or (4) staff’s perceptions of safety. Furthermore, staff’s perceptions about the access that children with LD have to hospital-based education, medical care, play facilities and first/last or flexible appointments did not differ significantly.
Access to investigations, procedures and treatments
Staff were asked to identify barriers to and facilitators of children with LD accessing investigations, procedures and treatments (Table 9). Six areas were perceived to have an impact on access, of which two were family related (children and parents) and four were hospital related (staff, services, environment and resources/equipment). The over-riding message from these data is that children with LD need access to (1) staff with LD knowledge and training, who in turn can access specialist staff when needed; (2) appropriate equipment and resources; and (3) appropriate spaces. In addition, the ability of parents to advocate for their child should be considered.
| Barriers | Facilitators | |
|---|---|---|
| Staff | Lack of knowledge about needs of children, how to identify them | Knowledge of specific needs of children with LD |
| Lack of access to specialist staff | Access to LD nurses, named paediatricians, play specialists | |
| Lack of time – plan, meet needs | Preparation and planning | |
| Lack of training | Access to LD-specific training and information | |
| Lack of power | ||
| Negative attitudes – not wanting to care for LD patients, believing it is parents’ responsibility to provide care, children with LD will disrupt other patients | Trust recognition of need to focus on LD and staff ‘champions’ | |
| Reliance on parents | ||
| Environment | Lack of appropriate space/cubicles, too cramped | Access to appropriate space: cubicles, wet room, sensory room |
| Lack of quiet space | Access to quiet space | |
| Lack of wheelchair access | ||
| Service related | Lack of co-ordination between hospital services and between hospital and community | Streamlining/co-ordinating appointments and providing flexible services |
| Lack of specialist treatments and/or procedures | ||
| Lack of staff capacity | ||
| Cost – staffing | ||
| Waiting times | ||
| Disparity of care/services within/across hospitals | ||
| Children | Unable to cope with delays/disruption to routine | |
| Anxiety | ||
| Feeling stigmatised | ||
| Parents | Lack of knowledge of what is available | |
| Lack of ability to articulate child’s needs | ||
| Too embarrassed to ask for what they need | ||
| Having a LD themselves | ||
| Language barrier | ||
| Feeling overwhelmed/negative about what can be done | ||
| Do not bring in hospital passport | ||
| Listening to parents | ||
| Working in partnership with parents | ||
| Resources and equipment | Lack of communication tools | Access to communication tools and hospital passport |
| Lack of hoists | Access to hoists | |
| Lack of beds | Access to specialists beds | |
| Lack of bespoke equipment | Access to adapted eating equipment, developmentally appropriate toys |
Practice of involving children and parents as partners in care
When staff were asked about their trust’s policy for involving children and parents as effective partners in care, it was apparent that there was a lack of policies or formal practices. Rather, staff implied that there was an implicit inclusion of children and their parents as partners in care.
Providing information
There was variability in knowledge about what information was available for parents and children, with or without LD, to be partners in care. Most commonly reported was parents being provided with written information leaflets related to their child’s health condition. A guideline for parents of children with LD was reported in one site. Examples of information for children were leaflets, books, easy-read materials and photographs.
Six children’s hospitals and two non-specialist hospitals reported at least one adapted method for providing children with LD information about their condition or inpatient stay, such as easy-read materials, widget symbols or photographs. One hospital had clear guidelines for producing information, including a process to check the accuracy, readability and accessibility of this information, and the LD team worked with departments to produce easy-read materials. There were selected examples of inclusive practices, for example a young person with Down syndrome featuring in a video about a day procedure. Despite these positive examples, only one-third of hospitals in our study had any specific method of providing information to children with LD, with one interviewee acknowledging that engagement was better with children without LD.
Eliciting feedback
Trusts primarily used the NHS Friends and Family test90 to measure satisfaction with their services, alongside other local surveys, feedback sheets or patient narratives. Some reported their intention to collect feedback from all children using child-friendly methods, for example a visual method using a washing line with ‘vests’ and ‘pants’ to help children describe aspects of their care that were positive and negative, which may be a more inclusive way of gathering feedback. Another hospital encouraged children to make films about their hospital experience. Photography, texting, and sing and sign were also mentioned.
The majority of sites did not report having made a specific effort to collect satisfaction data from children with LD. Instead, sites appeared to offer children with LD (regardless of their communication methods or abilities) methods that were used for younger children, such as pictures or using a drawing on the Friends and Family Test. Alongside this, it was suggested that parents or ward staff could assist children with LD to complete any feedback. One site reported having a range of methods for engaging children with LD, including drawing, writing, recording a DVD, putting Post-It notes on a wall or using photographs.
Involving in planning services
Two-thirds of staff from children’s hospitals and one-third of staff from non-children’s hospitals described mechanisms for involving parents in planning specific services, such as parent groups/forums, staff interview panels, family days and listening events. The participation of children in a range of groups or forums was reported, for example, through the ‘15-step programme’, which is based on taking 15 steps into a clinical area and children providing their feedback. A further initiative is ‘a spoonful of sugar scheme’, whereby the nurse meets the child before a consultation to help the child prepare questions they may want to ask. Interviewees were less certain about the specific involvement of children with LD either to inform specific services or, more widely, though a Young People’s Advisory Group or similar. Three hospitals reported active inclusion and engagement with children with LD through children’s forums or the adaptation of, for example, surveys and interviews for those with LD.
Conclusions
The findings presented from both the mapping exercise and the staff survey reveal a range of cross-organisational, organisational, staff and family-related factors in NHS hospitals deemed to facilitate or prevent children with LD having equal access to high-quality hospital care. The diagrams that follow (Figures 4–8) highlight these factors in relation to our RQs, with barriers grouped in the red boxes on the right and facilitators grouped in the green boxes on the left. Using results from subsequent chapters in relation to hospital and community staff (see Chapter 7) and families (see Chapters 8–11), we will incrementally build a comprehensive picture of the factors that are key to ensuring equality, drawing out overarching themes.
FIGURE 4.
Perceived barriers to and facilitators of identifying children with LD in hospital (survey data and mapping exercise) (RQ1). LDLN, learning disability liaison nurse.
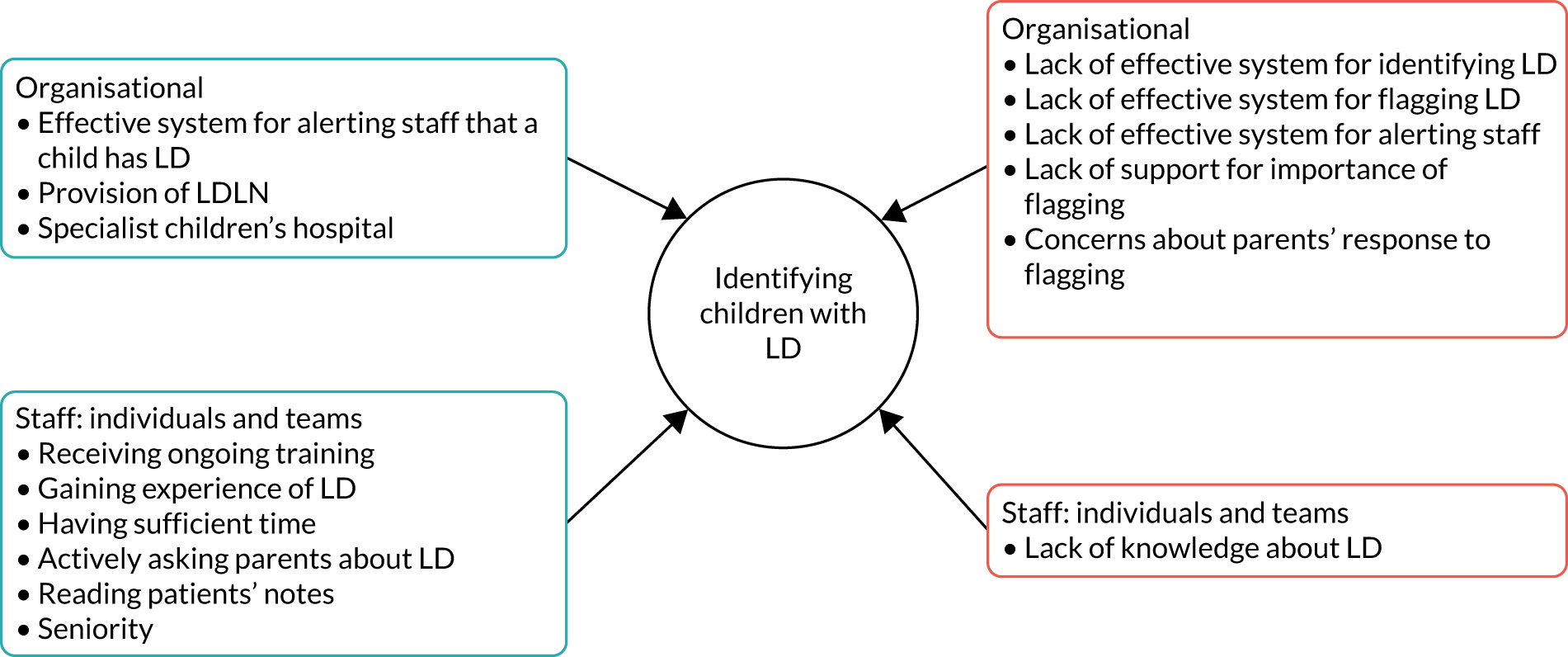
FIGURE 5.
Perceived barriers to and facilitators of meeting the needs of children with LD in hospital (survey data and mapping exercise) (RQ1).
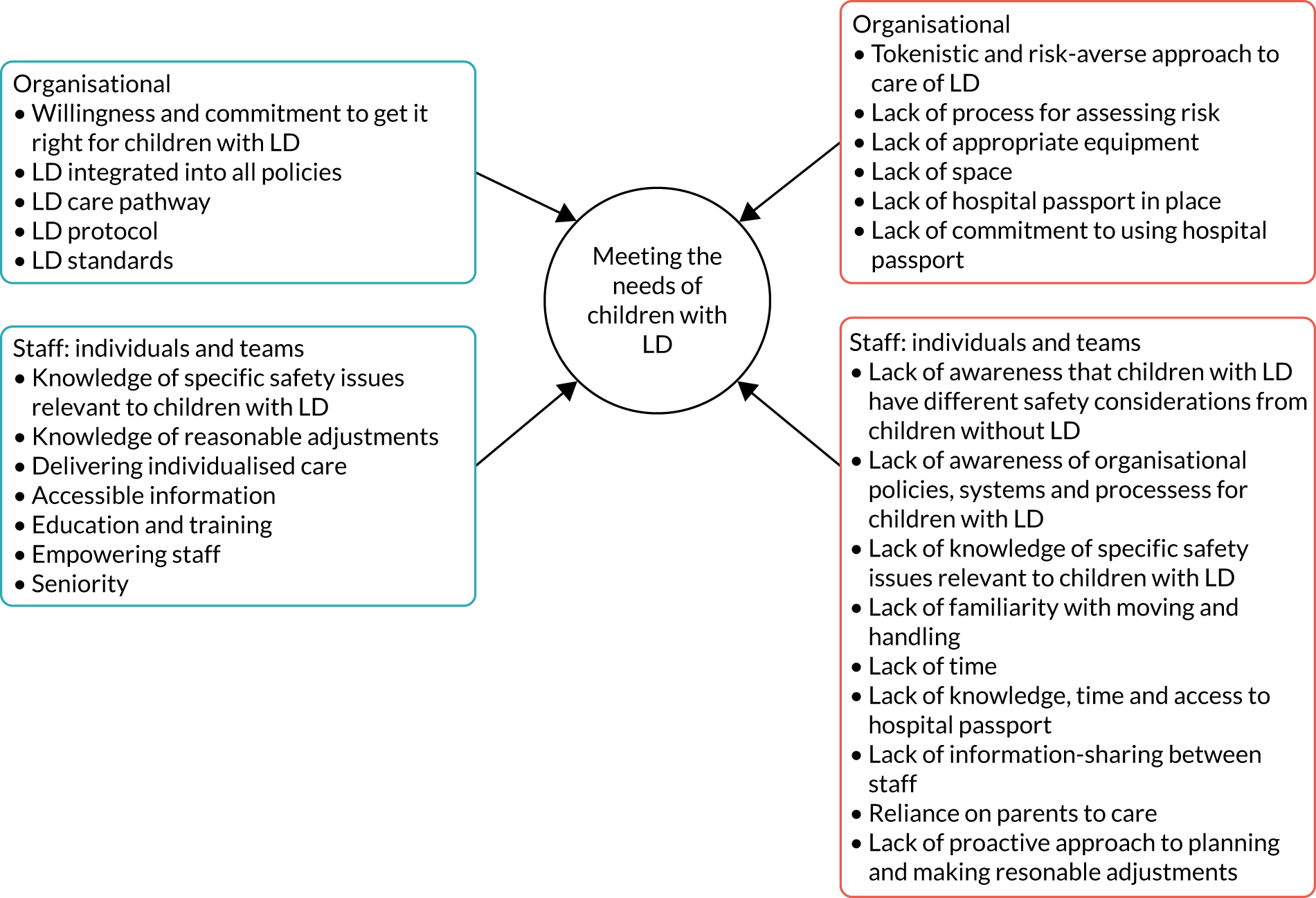
FIGURE 6.
Perceived barriers to and facilitators of children with LD gaining access to investigations, procedures and treatments in hospital (survey data and mapping exercise) (RQ2).

FIGURE 7.
Perceived barriers to and facilitators of involving children with LD and their parents as partners in care (survey data and mapping exercise) (RQ3). LDLN, learning disability liaison nurse.
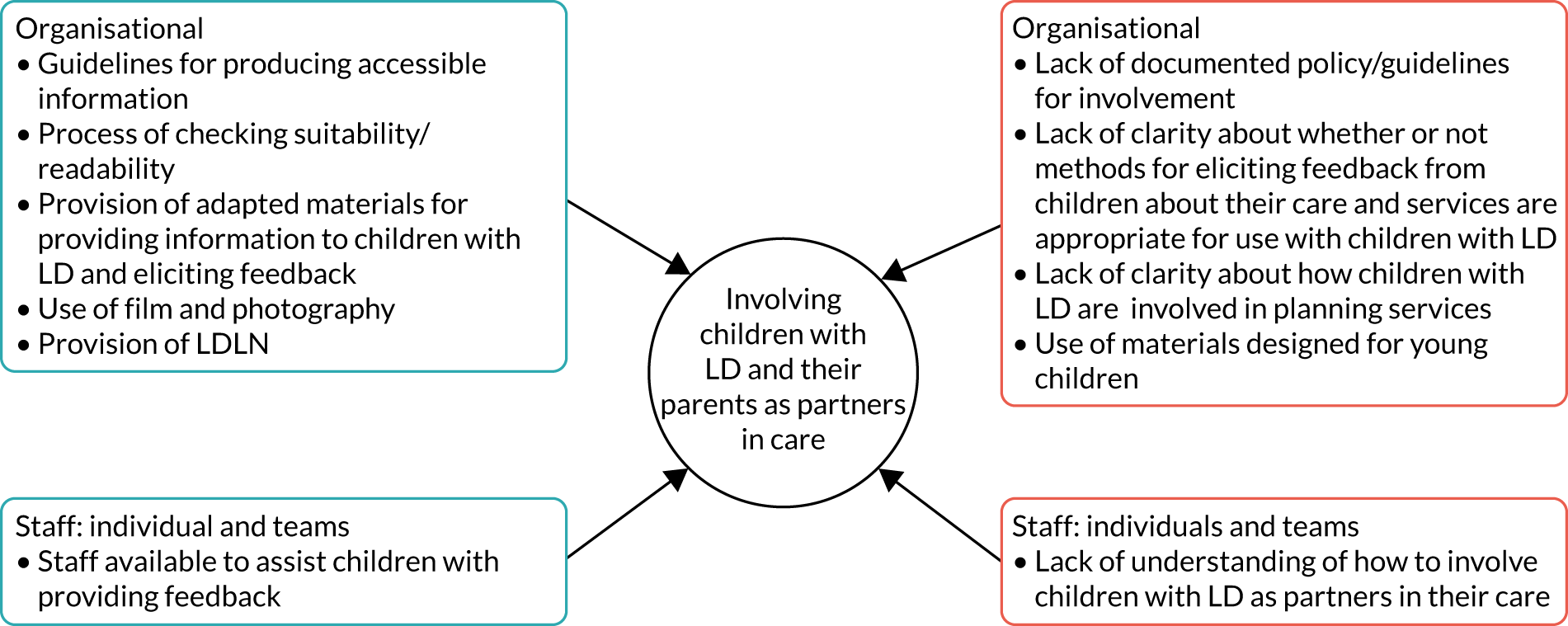
FIGURE 8.
Perceived barriers to and facilitators of children with LD being safe in hospitals (survey data and mapping exercise) (RQ5).
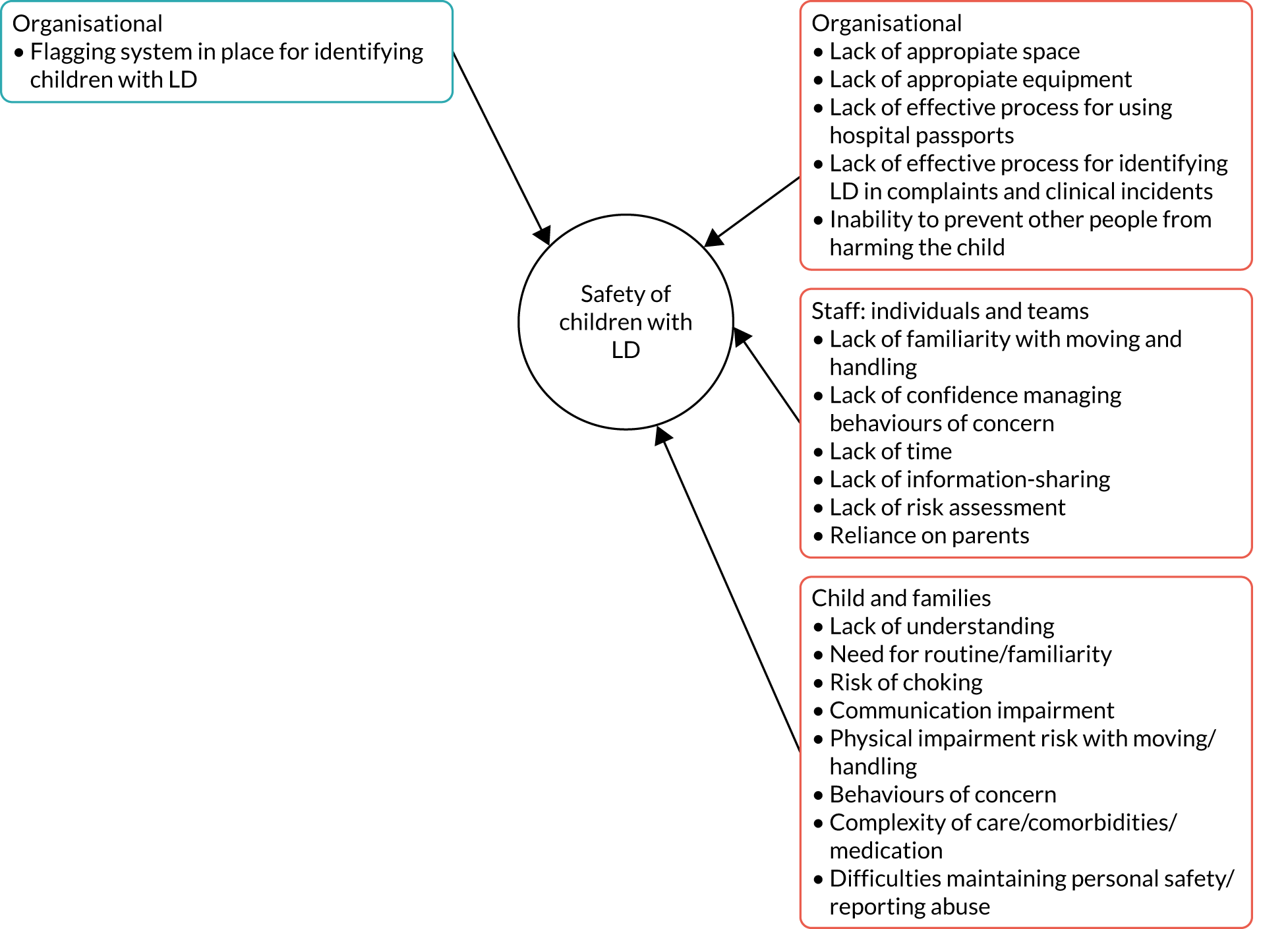
Chapter 7 Experiences of hospital staff
Parts of this chapter have been reproduced with permission from Oulton et al. 91 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
Parts have also been reproduced with permission from Kenten et al. 87 This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. The text below includes minor additions and formatting changes to the original text.
The preceding chapters have highlighted national variation in policies, systems and practices to support the care of children with LD in hospital, as well as considerable uncertainty among senior staff about what is in place in their organisation. We have also provided evidence of perceived inequality for children with LD, from the perspective of staff, in relation to multiple aspects of hospital care, including safety. Interviews with senior managers in 22 hospitals across the country have revealed organisational, staff and family factors that facilitate or prevent such inequality. This chapter focuses on staff views and experiences at the individual level, from interviews with 98 staff working in six of these hospitals, including nine ward managers (phase 2). A clear theme running through this chapter is the often complex relationship that staff have with parents, who can be viewed as being massively helpful but also a hindrance.
Identifying children with learning disability
Staff from different professional groups referred to the terminology used around LD and the resulting lack of clarity, especially given that ‘special needs is a huge range’ (ward manager, specialist children’s hospital E) and the lack of education about definitions (staff quotation 1; see Appendix 7). The use of terms such as ‘learning disorder’ or ‘learning difficulty’, ‘developmental delay’ and ‘special needs’, as well as specific diagnoses such as dyslexia or dyscalculia, or the complete lack of any information about LD, was not uncommon. As one allied health professional said:
They say ‘LD’ and that could mean autism. It could mean intellectual disability. It could mean that the child has behaviour needs or mental health needs. You never know what it actually means.
Occupational therapist, specialist children’s hospital H
Furthermore, there appeared to be a conflation between LD (or equivalent) and physical disability.
Different staff talked about various methods by which they could identify that a child in their care had LD. These included both formal methods, including the referral letter, pre-admission clinic, patient notes, admission history, hospital passports or equivalent, flagging or alerts, and informal methods, including huddles/handover, indications from diagnosis, intuition, knowing the child and asking parents. An issue raised was that referral letters might or might not have information about a child’s LD.
At one site with ‘strong links with the community paediatricians’ (nurse, specialist children’s hospital), staff said that this helped hugely with communicating about patients in advance of their child’s admission. Pre-assessment clinics were viewed as an opportunity for staff to ‘gain real insight as to how they’re behaving’ (ward manager, specialist children’s hospital F), and to identify specific needs and plan reasonable adjustments. However, it was also recognised that it may be left to the doctor’s secretary to inform the ward about a patients’ needs, or that the information doctors passed to ward nurses did not always contain the detail needed. There was variability in staff views about the usefulness of patient notes, with some seeing them as a good source of information and others highlighting that it ‘depends whether the nursing staff have written it’ (nurse, non-children’s hospital G). It was also noted that it might be easier to find relevant information about those with more complex needs or patient issues, such as safeguarding, than about those with mild LD, as well as other patient issues such as safeguarding. The value of being given information about what a diagnosis of LD meant for an individual child was highlighted, as was having a dedicated section at the front of the child’s notes to highlight any special needs that they may have (staff quotation 2; see Appendix 7).
Many staff, including several ward managers, highlighted that it was not uncommon that they would not know that they would be admitting a child with LD until the child arrived on the ward, and it might not be until a history was taken that a diagnosis of LD was likely to become apparent. For example, one play specialist working in a specialist children’s hospital described inadvertently offering a child who was blind some books to read, while a paediatrician said, ‘actually do we as nurses and doctors always know when a child in front of us has a visual impairment or hearing impairment, I wonder?’ (non-children’s hospital G). There was variation in whether or not parents were asked directly about LD, with a staff member from one non-children’s hospital saying that it was not asked at all during admission, another saying that it was not done routinely, and another saying that they always talked through the child’s activities of daily living with parents, including behaviour and development. Learning on the job by simply asking the child questions, such as their date of birth, and observing their behaviour was another tactic used in practice. Time was seen as a barrier to acquiring the relevant information. The challenges of unplanned admissions, especially those through accident and emergency, were highlighted.
Across all sites there was an awareness of hospital passports and ‘all about me’ documents, but there was uncertainty about the extent to which these were used by staff or families. Ensuring that the passport was easily accessible and available in advance of the child’s admission was a suggestion to improve practice. Broadly, staff felt that it would benefit their practice and the child’s experience if a flag or alert existed for a patient with LD, but the way in which this would be applied and what it could mean was questioned:
Those alerts come from non-formal assessment . . . I don’t feel like it’s a fair way of communicating about a child’s needs.
Occupational therapist, specialist children’s hospital H
A ward manager working in a different children’s hospital also recognised that parents may not want their child to be labelled, although this view was based on a single previous experience.
A few staff commented that some diagnoses would suggest that a child might be more likely to have LD, for example ‘severe cerebral palsy’ or ‘maybe Down’s syndrome’, but they did not necessarily clarify this with the parent, which meant that it might not be until later in the admission that a particular LD-related need was identified. In addition to the clues from a diagnosis, several staff said that they used their ‘intuition’ (physiotherapist, non-children’s hospital D; nurse, non-children’s hospital G) to identify whether or not a child had LD. They talked about ‘just being able to tell’ (nurse, non-children’s hospital G) or ‘having a little inkling’ (nurse, specialist children’s hospital G) or the child looking ‘a bit slow’ (nurse, non-children’s hospital G). Some, but not all, did go on to say that they would check their suspicions by asking the family or reading the child’s notes.
Several staff talked about ward huddles and handovers as other potential sources of information about a child’s LD and the need for reasonable adjustments. However, other staff felt that the extent of a child’s disability or specific needs might not be shared during huddles and, therefore, this was ‘hit and miss’ (doctor, specialist children’s hospital F).
Interviewees also reported ‘knowing’ some of the children from previous admissions, which meant that they were aware of the child’s background and could draw on this information when caring for the child or sharing their knowledge with other members of staff. About half of staff cited parents as a reliable source of information about their child’s LD:
It’s all about not relying on one system to give you all the information. It’s about using all the ones available to you. Again, we come back to why family are so useful in those situations because they, at the end of the day, will have the most up-to-date information about the patient and how to manage them best, rather than what might have been written days, weeks or months ago.
Doctor, non-children’s hospital G
Parents were largely reported to be forthcoming with information, particularly if they experienced regular hospital admissions. However, as a few staff noted, parents might also have LD, speak English as a second language or be really tired or disengaged, all of which could have an impact on whether or not information about their child’s LD was shared. Moreover, as the ward manager of a surgical ward said:
It must be easier for parents if they’ve not got to explain everything every time they come in . . . if you go in with that little bit of knowledge and probably a little bit of sensitivity and make sure you’re prepared.
Ward manager, specialist children’s hospital E
The value of identifying LD in advance of an admission was recognised by a number of ward managers, who talked about the challenges of trying at the last minute to, for example, prepare bed areas or source specialist beds/equipment, which could take days to arrange.
Confidence, knowledge and skills
The degree to which staff felt confident, knowledgeable and skilled in caring for children with LD varied, as did their views on how this compared with caring for children without LD. What was apparent was that their understanding about children without LD was often the ‘yardstick’ with which staff measured their knowledge. They recognised that, for children with LD, there was no blueprint to follow, and a standard patient pathway for a particular condition or admission type did not necessarily fit with the needs of these children:
We’re used to dealing with them [children without LD] . . . to how that disease displays itself . . . We have our set protocols, we have our practice nurses to do education with them, to help lead practice. But with children with LD you can have one condition that can manifest itself in very different ways . . . we aren’t always as prepared . . . it’s responding to the individual child’s needs, whereas your chronic condition we’re more looking at the condition itself.
Ward manager, specialist children’s hospital F
Many staff recognised that when it came to skills and expertise in relation to children with LD, and particularly those with multiple and complex conditions, there was always room for improvement. However, a lack of training was seen as a particular barrier (see Training), with many describing gaining their knowledge, skills and confidence through experience instead (staff quotation 3; see Appendix 7). Central to this knowledge by experience was being ‘regularly and repeatedly exposed to children with disabilities and the people that care for them in their normal environment’ (nurse, specialist children’s hospital F). Experience was also seen as valuable in terms of building staff’s confidence in being open about the limitations of their own abilities:
The more you look after children with special needs, the easier it becomes. You lose that fear of the unknown and you get to learn how to communicate appropriately . . . watching other people look after children with special needs you can learn quite a lot but it’s also about having the confidence to ask the parents what they expect from you as well . . . not be afraid to say, ‘Look, I don’t know what I’m doing. What do you want me to do?’.
Nurse, specialist children’s hospital F
The presence or absence of parents could have an impact on staff. If parents were present, then staff could work with them to find out specific information about the child and combine this with their own knowledge and skills to provide individualised care (staff quotation 4, staff quotation 5; see Appendix 7). If parents were not present, then providing tailored care was more difficult and could have implications for the time spent with the child, the time set aside to complete a task or the timing of care. This was the case even for staff who had a lot of experience, because ‘there’s often a finely tuned balance where if you don’t quite get something right it can throw other things off’ (nurse, specialist children’s hospital F), whereas for children without LD ‘it’s usually pretty clear-cut’ (nurse, specialist children’s hospital F). It was generally recognised that knowing the individual child helped to develop staff’s confidence, which in turn could have an impact on how much time they spent with the child:
If you know a family well, then you would feel more confident to go and talk to that family but if you didn’t really know how a child communicated or how to communicate back . . . it’s the not knowing. You’re maybe not going to go and put yourself in that unfamiliar environment . . . in that uncomfortable situation.
Ward manager, specialist children’s hospital F
It was recognised that newly qualified staff, who could be scared of the unexpected, may find it particularly challenging to develop their knowledge through experience (staff quotation 6; see Appendix 7).
Training
The amount of undergraduate training that nurses and allied health professionals received in LD varied considerably, with paediatricians reporting more variability than other staff, based on their specialist training. Within the context of a packed curriculum, chronic or long-term conditions appeared to be covered, but only a limited focus was given to LD. Experience of LD largely came from placements, most often in special educational needs schools or other non-hospital settings. Specific LD training, when offered, was highly valued:
I found it brilliant. We had service users coming in, giving us talks and personal accounts and telling us what they would like from nursing staff. We would have parents coming in . . . telling us their experiences . . . and what they would like for the future.
Nurse, non-children’s hospital D
When asked about continued professional development, most staff were not aware of any specific LD training in their hospital, referring instead to mandatory training, such as manual handing and safeguarding, and condition- or treatment-specific training. Skills in and knowledge about LD came from ‘learning on the job’ from patients, parents and colleagues, the success of which varied:
It’s more of the mentorship that I’ve learned . . . I’ve worked with consultants, whose communication with these LD were absolutely fantastic, and you think, ‘Wow, I want be like that’. On the other hand, unfortunately, there are people who haven’t been that brilliant with dealing with children with LD.
Doctor, non-children’s hospital D
A small proportion of staff felt that they had received enough training to care for both children with and children without LD, whereas others reported gaps in their training in relation to LD, autism, Down syndrome and cerebral palsy, communication methods, managing behaviour, and distraction and positioning:
There’s still things that we’re failing to meet . . . it’s more the LD-specific factors that we struggle with.
Ward manager, specialist children’s hospital F
This staff member went on to say that a big weakness in their service was not having enough staff trained in Makaton and other communication methods, highlighting disparity in staff confidence between communicating with a teenager with cystic fibrosis and communicating with a teenager with cerebral palsy (ward manager, specialist children’s hospital F). That parents could subsequently be relied on by staff who might ‘unravel’ without the parents’ support was a factor that a ward manager from another specialist children’s hospital also raised.
Making reasonable adjustments
It is a legal requirement for public services to ensure that their services are accessible to people with disabilities. The 1995 Disability Discrimination Act92 lays out the legal duties of service providers to make adjustments. A range of factors have an impact on whether or not an adjustment is deemed ‘reasonable’, including whether or not it can actually be done, the cost, and the organisation’s resources and size. The guidance documents from the Equality and Human Rights Commission point out that ‘just because something is difficult does not mean it cannot also be reasonable’. 93 Furthermore, the legal requirement is for services to proactively anticipate the need for reasonable adjustments, rather than wait until these adjustments are required.
When staff were asked to explain what the term ‘reasonable adjustments’ meant, about one-third did not have any understanding of the term, with some talking about reasonable adjustments but in another context, such as education or employment. The remaining staff provided some form of description, but with varying degrees of clarity and confidence about what this meant in practice, as shown by the following definitions provided by four ward managers working in two different specialist children’s hospitals:
How we can adjust the environment or how we work, reasonably. So, meeting the needs of the patient, but also not putting needs, or the needs of the services, at risk.
Specialist children’s hospital F
You can alter things that aren’t going to affect us too much.
Specialist children’s hospital F
Putting things in place that are reasonable, so if a patient wants a certain thing and you can give them that without too much trouble, that you’d try your best to do it.
Specialist children’s hospital E
You can do the very best you can for your patient within your own policies, procedures, and health and safety that you could do it for more than one patient. You can’t go above and beyond for the one patient if you weren’t prepared to do it for another patient.
Specialist children’s hospital E
Few staff talked about reasonable adjustments being anticipatory.
The majority of staff felt that they could make (reasonable) adjustments when these were needed, with some less experienced staff feeling that they needed assistance from colleagues or more senior colleagues to put some adjustments in place, something also highlighted by ward managers. Overall, staff believed that they did the best they could to make adjustments to meet the needs of a child whether or not they had LD, but at times an adjustment was more of a ‘best fit’ rather than a ‘perfect fit’.
The majority of (reasonable) adjustments described (see Appendix 8) related to some form of flexible practice, an alternative approach or prioritisation. However, these were not always seen as ‘changing the way things are done for children with LD’. 35 Rather, it was implied that these adjustments were sometimes part of standard practice and that in some cases these were made ‘probably without even realising you’re doing it’. Others were more considered; one service at a specialist children’s hospital had the capacity and flexibility to offer assessment at home rather than distressing the child by having them come to hospital. Staff also noted that parents and children sometimes made specific requests for adjustments that were highly individualised, not all of which were met.
The use of resources to assist in the provision of (reasonable) adjustments was described, and these included a range of equipment such as specific mattresses, beds or seating options. However, the availability and accessibility of these in the hospital varied:
We had a child who needed to be in a pit bed on the floor because they’re not safe to be in our normal beds . . . Ringing round for that pit bed at 3:00 in the morning, who has got the pit bed? No one knows where it is, oh it’s in a room where it’s behind a lock code and nobody knows what the code is. In the end we contacted the adult services and they had a pit bed that we used instead. There’s always a solution but sometimes it can be slightly more longwinded than it needs to be.
Nurse, specialist children’s hospital F
Some staff reflected on the difficulty of knowing that a patient may need a specific adjustment and not having the resources to implement this or the permission to do so (staff quotation 7; see Appendix 7). Some staff felt that it was not their responsibility or within their power to make reasonable adjustments (staff quotation 8; see Appendix 7), including a band 5 staff nurse at a specialist children’s hospital who felt that a reasonable adjustment she had identified for a patient had been implemented only when a more senior member of staff requested it. Conversely, however, some junior nurses felt that being newly qualified had a positive impact on the implementation of reasonable adjustments because they had received recent training in individualised family-centred care. They said that some senior nurses could have rigid approaches to following rules/policies that prevented reasonable adjustments being made. Certainly, the degree to which staff ‘turned a blind eye’ to these rules differed.
Barriers to the implementation of reasonable adjustments were also described in relation to space, ward staff, bed status, the availability of side rooms and unplanned admissions, as well as information about adjustments not being handed over or recorded in a patient’s notes and an adjustment being needed outside regular working hours. Furthermore, it was recognised that information that was available for children about being in hospital or specific medical conditions was in written form and not adjusted to make it accessible for those with LD.
Safety
Overall, the majority of staff indicated that they believed that they were able to provide safe care to children. However, this depended on staffing levels, which could change day to day, and the ward layout, with one children’s hospital having recently increased the number of side rooms and removed the nurses’ station, which compromised the visibility and observation of children. Similar to that already described in relation to communication, parents were viewed as having a pivotal role in the provision of safe care for their children, which often could not be replicated by ward staff when parents needed to leave the bedside:
[Parent says] ‘I’m just popping for a cup of tea, can you sit with them? I’ve left the door open, will you keep an ear out?’ ‘No.’ [Staff member] . . . You do, you try your best and you say, ‘Yes, we’ll pass him by all the time, but I can’t physically sit in there for the duration it takes for you to go and have a cigarette and a cup of tea and a chat with your mum on the phone’. So, that parent might need to actually, you know, forfeit their cup of tea and their fag, and stay with them, because they wouldn’t be safe, but you can’t force parents to stay there. So, that’s when it becomes unsafe, if you’re taking a staff member off the ward to sit with them, but that half hour is vital, isn’t it? Some time for parents to go and have a breather.
Nurse, specialist children’s hospital E
This example highlights particularly well the conflicting views staff can have about supporting parents to have a break in hospital and there appearing to be no choice between that and maintaining the child’s safety. Managing behaviours of concern, in children with and children without LD, was raised as a particular issue that could compromise the safety of children and also staff, who might be hit, punched or kicked as a result (staff quotation 9; see Appendix 7). Staff would try to work with parents when children displayed such behaviours or draw on specialist support, such as the play team, but may not have the resources or strategies in place on the ward, which ‘could be a dangerous place for somebody if they suddenly decide to have this mega blow-out’ (teacher, non-children’s hospital I). As one staff member said:
I’ve looked after children who have been climbing on the lockers and jumping around on the bed, and I suppose that’s not ideal, but I don’t know how you could solve that.
Nurse, non-children’s hospital G
Another example was provided of a child aged 12 years with the intellectual capacity of a 3-year-old who required regular life-saving blood transfusions. The following quotation from a nurse highlights the complexity of managing this situation:
We do have situations where it can become unsafe . . . the child hits you and does quite a lot of damage to staff around him. Managing that is difficult because the cubicle is too small, and he’s at risk of damaging himself. He stands up with the wheelchair on his back and walks around with it. He tries to grab the machine that’s delivering the blood . . . so you need about two to one with him . . . we can’t put him in the playroom because he’s a danger to other children . . . there’s no real space for him . . . he ends up in the corridor, in a very boring end of the unit . . . we can’t sedate him because ethically that’s not right.
Nurse, non-children’s hospital G
Staff across different hospitals recognised that some children need additional support or staff to spend time with them as a result of behaviours of concern or self-harm, but that this may not be provided. However, others did not see that aspects of a child’s safety in hospital were within their remit.
Involving parents
Approximately half of the staff members interviewed talked about parents of children with LD as a reliable source of information and about the importance of working in partnership with parents and listening to their views. Ward managers talked specifically about negotiating roles and responsibilities with parents and that it was important ‘not to jump in and take everything over’ (ward manager, specialist children’s hospital F), as well as recognising that because every family is different ‘you just assess it as they come in’ (ward manager, specialist children’s hospital E). Some staff reflected on the difference between parents of children with LD and parents of children without LD in terms of (1) their willingness to be involved, (2) their expectations and (3) their attitude:
We find that with children with LD, they [parents] are generally more happy to be involved . . . they like to be involved in personal aspects of care, they like to ask questions . . . I think with some of those parents [of children without LD] they tend to take more of a step back.
Support worker, specialist children’s hospital F
The parents with children with LD tend to just make do and manage, to the extent that we go, ‘You really shouldn’t be lifting that child. They’re 15, why are you carrying them up the stairs?’. It’s often that the parents of children . . . suddenly in plaster, where they’ve been a normal child up until then, that have higher expectations of what equipment we can provide, what adaptations we can provide.
Physiotherapist, specialist children’s hospital E
You tend to find the parents of the children who have got LD are not as nervous for the majority of the procedure, unless they’re having something major. They tend to be more aware of the process, they know the staff. They’re a bit more institutionalised, really . . . so they have more patience . . . Your parents that have got children without disabilities and they’ve never been in before, they’re, kind of, expecting an instant service, they come in, they go to theatre, they’re out, they’re home, then that’s it. That’s just not how it works and there’s 100% a difference between those parents.
Nurse, specialist children’s hospital
What was apparent was that the relationship that parents of children with LD had with staff was often complex, and it was evident that, as well as being viewed as a massive help, parents could be seen as a hindrance:
If the parents feel they need it [one-to-one care], but we don’t think they need it, . . . staff can feel quite anxious . . . because they’re such an expert in their child and they want things done precisely . . . they don’t want to be in a position where they think they’re going to be complained about.
Ward manager, specialist children’s hospital E
Parents can be brilliant, but they can also be very difficult to deal with, understandably if their child is in a distressing situation . . . that can manifest itself in them either being very helpful and understanding towards the health-care professionals who are trying to help the child, but it can also lead some parents to being difficult to discuss with. They can sometimes be verbally abusive. They can be sometimes aggressive. They can be just sometimes a bit difficult to deal with.
Physiotherapist, non-children’s hospital G
Examples were also provided of parents potentially compromising the safety of their child or other children on the ward by, for example, carrying hot drinks on the ward, continuing practices from home when the hospital wanted to manage things differently or lifting their child manually rather than hoisting them.
Environment
Although the ward environment was seen to create challenges for both children with and children without LD, it was generally perceived to be less conducive to the needs of those with LD. Lack of space was a particular issue, especially for those who used wheelchairs and required the use of hoists. The number of belongings that parents needed to bring into hospital compounded the situation, particularly in bays where the space between the beds was minimal (staff quotation 10; see Appendix 7). At three sites it was also noted that the bathrooms for children with physical impairment or complex needs were inappropriate or lacked appropriate equipment. In one non-children’s hospital, the bathroom for disabled people was used as a storage cupboard, and in one of the children’s hospitals the ceiling tracking hoists in the side rooms reached the toilet but did not reach the shower.
Many staff recognised the benefit to children on the ward of having access to a playroom, sensory room or activity space, but it was felt that these spaces were primarily suitable for children without LD, who also had a greater choice of toys and activities appropriate to their needs. As one staff member pointed out, ‘there isn’t a massive amount for them [children with disabilities] to do’ [nurse, specialist children’s hospital E]. At one children’s hospital, a redesign of the wards had also resulted in a loss of the sensory room, with the other spaces not perceived as suitable for children with LD or spaces they would use:
We’ve got a teen room for teenagers. We’ve got a playroom for kids. We should probably have a Snoezelen somewhere, because we have a lot of children with multiple LD.
Support worker, specialist children’s hospital E
The age range of children on the ward created difficulties, not just in relation to accommodating children with and children without LD, but also babies and teenagers and boys and girls, with specific provision varying between sites:
We’ve got lots of things for babies; we’ve got youngish children, nothing for that older child range. Not everybody just wants to go home and play on a DVD or an Xbox [Microsoft Corporation, Redmond, WA, USA]. Whether you’ve got LD or not, there’s nothing in between.
Housekeeper, specialist children’s hospital E
We do have good facilities for teenagers who are in hospital more long term . . . so I think they probably would have better access to facilities that what we would offer our children with LD.
Ward manager, specialist children’s hospital F
From a sensory perspective, staff recognised that wards could be noisy, with areas near the nurses’ station noted as particularly noisy and busy during the day, and at night noise could come from patients, machines or admissions to the ward. It was recognised that children with LD could be more sensitive to noise than those without LD and that finding access to a quiet space could be difficult. Staff from a number of sites also felt that the wards were often too hot, making the environment uncomfortable for staff and children. Not all sites and/or wards had reliable air conditioning units. Fans might be available, but there might not be enough for everyone wanting one or they might be removed from the ward. By contrast, the wards could be very cold during the winter months.
In terms of equipment, there were variations in what things were available for which patients. A ward manager compared having direct access to most of the equipment needed for the care of children with long-term conditions on the ward with having to source equipment for children with LD through specialist services in the hospital (e.g. occupational therapy and physiotherapy) or from outside the hospital (e.g. in relation to specialist beds). The challenges of accessing such equipment out of hours, ‘which could be a nightmare’, as well as knowing how to use such equipment, were identified as risks that needed to be addressed. Access to sensory equipment was also variable, with some sites feeling that this was largely lacking and others describing having a fibre-optics trolley with music, a LD box containing objects with different textures and noise, a soft-play area in the play room, a disco ball and bubble tubing.
Inequalities
Staff views about perceived inequality in hospital care between children with and children without LD differed. A considerable number of staff members reported that that they did not believe that any inequalities existed, that they had not seen any inequality or discrimination or that nursing staff treated both groups of children equally. Other staff members felt that inequalities did exist, but interestingly that these were in favour of children with LD. There was no acknowledgement that any adjustments in care, such as some form of prioritisation, increased observation or spending more time with the child, were necessary means of achieving equity. On the other hand, some staff felt that children with LD may be less likely to access schooling, playrooms and sensory equipment, and less likely to be communicated with and engaged with by staff, including nurses and play specialists, who may avoid spending time with them. It was also felt that staff may regard children with LD as a lower priority because of their complexity and the time required to care for them, and one staff member perceived it more likely that the parents of children with LD would complain if problems had occurred. As one nurse summed up:
I’m just trying to think whether more parents of children with a LD have talked about problems they’ve had than if they didn’t have a LD I think it would be unfair to say equal. I think there are parents and children that have had complaints when they haven’t had a LD, and those when they have had the LD. Possibly maybe more so when they’ve got a LD.
Nurse, non-children’s hospital D
When asked about inequality, one staff nurse made an interesting observation about the lack of choice that children with LD have about what is going on around them:
I think children with LD are more likely to comply. It’s children without that are more aware of what’s going on, and they don’t want to be sitting still, and sometimes a person’s who’s got LD doesn’t have a choice but to sit still because they can’t move.
Nurse, specialist children’s hospital E
There was an overall sense that families who advocate and make requests on behalf of their children are often those who get extra support, whereas those who do not speak up may not, the implication being that some families are getting what they need and others are not.
We have presented a wealth of information about the views of hospital staff with experience of caring for children with and children without LD, including factors seen as preventing and facilitating their receipt of high-quality hospital care (Figures 9–12). The challenges associated with identifying children with LD were highlighted, as was the lack of training in issues related to LD both at an undergraduate level and in clinical practice, which could leave staff lacking the necessary skills and confidence to meet the needs of these children. Particular challenges were described in relation to communicating with those who do not use verbal communication and those who present with behaviours that challenge. Although parents were sometimes seen as a hindrance, on the whole staff valued parents’ input and saw them as integral to maintaining the safety of the child. The environment was a particular challenge for meeting the needs of those with LD, who often required more space and more specialist equipment and resources, which were not always available or accessible. Issues related to the care of teenagers without LD was also seen as area that required significant improvement.
FIGURE 9.
Perceived barriers to and facilitators of identifying children with LD in hospital (staff interviews) (RQ1). LDLN, learning disabilities liaison nurse.
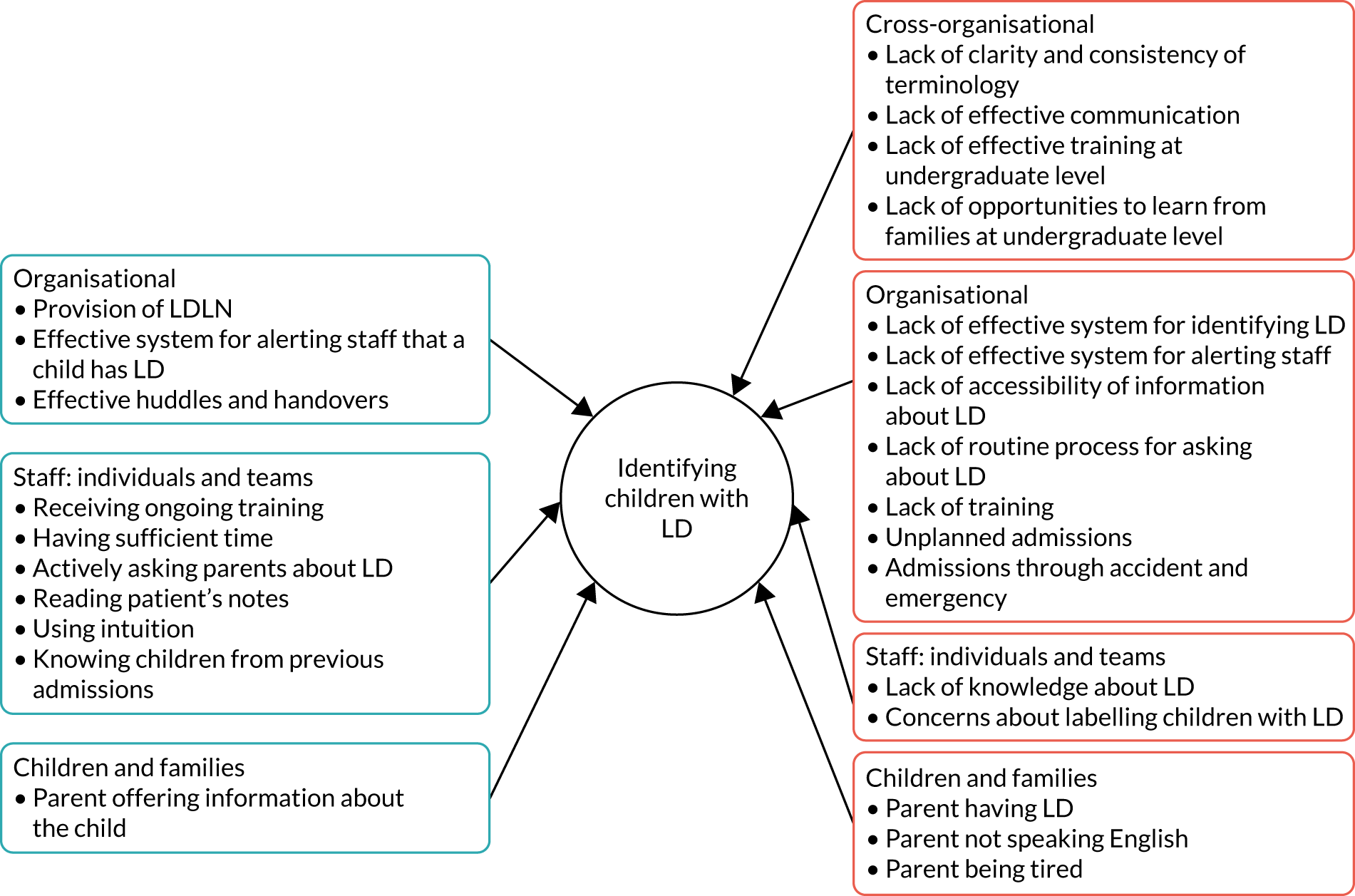
FIGURE 10.
Perceived barriers to and facilitators of meeting the needs of children with LD in hospital (staff interviews) (RQ1).
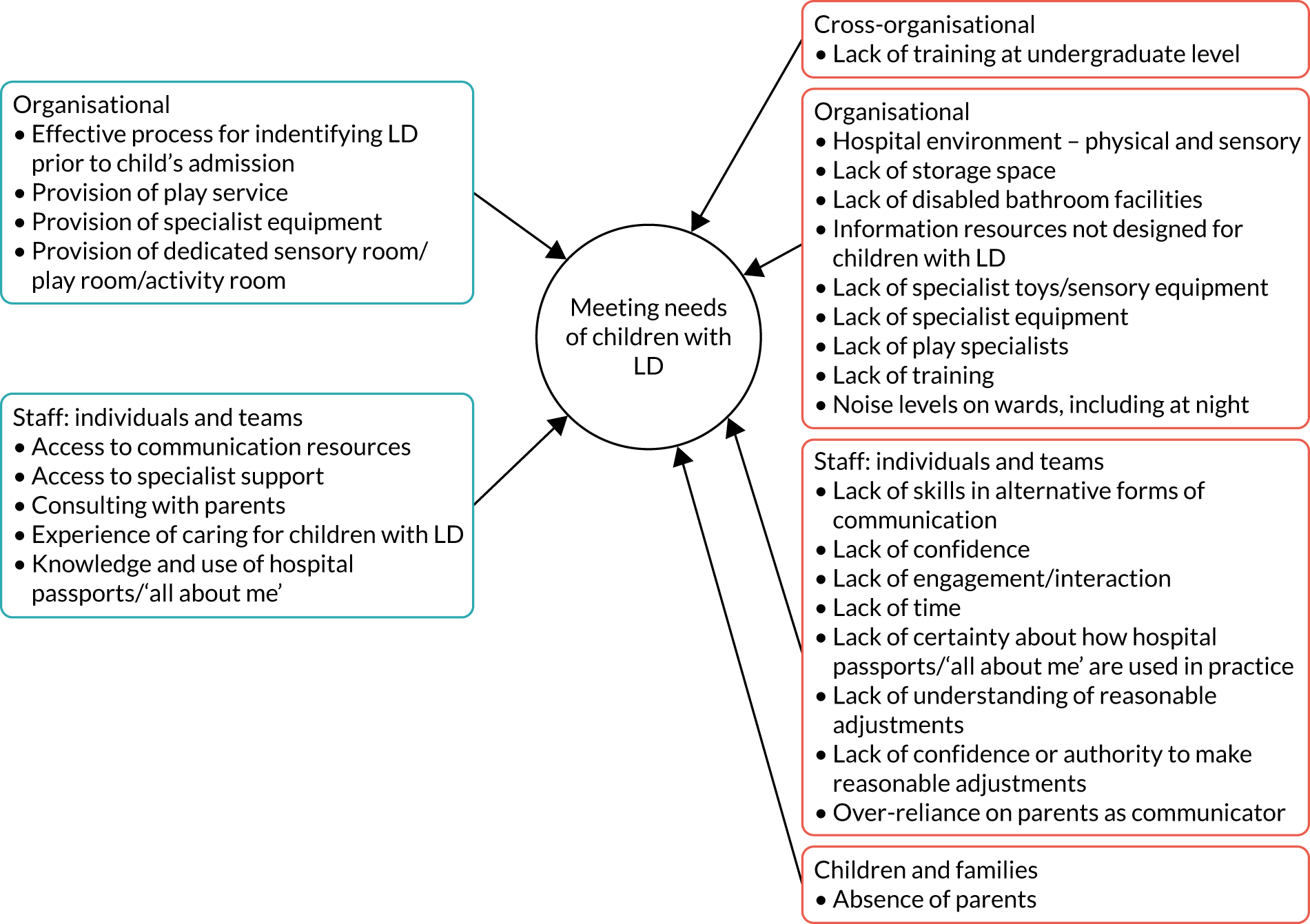
FIGURE 11.
Perceived barriers to and facilitators of involving families as partners in their care (staff interviews) (RQ3).
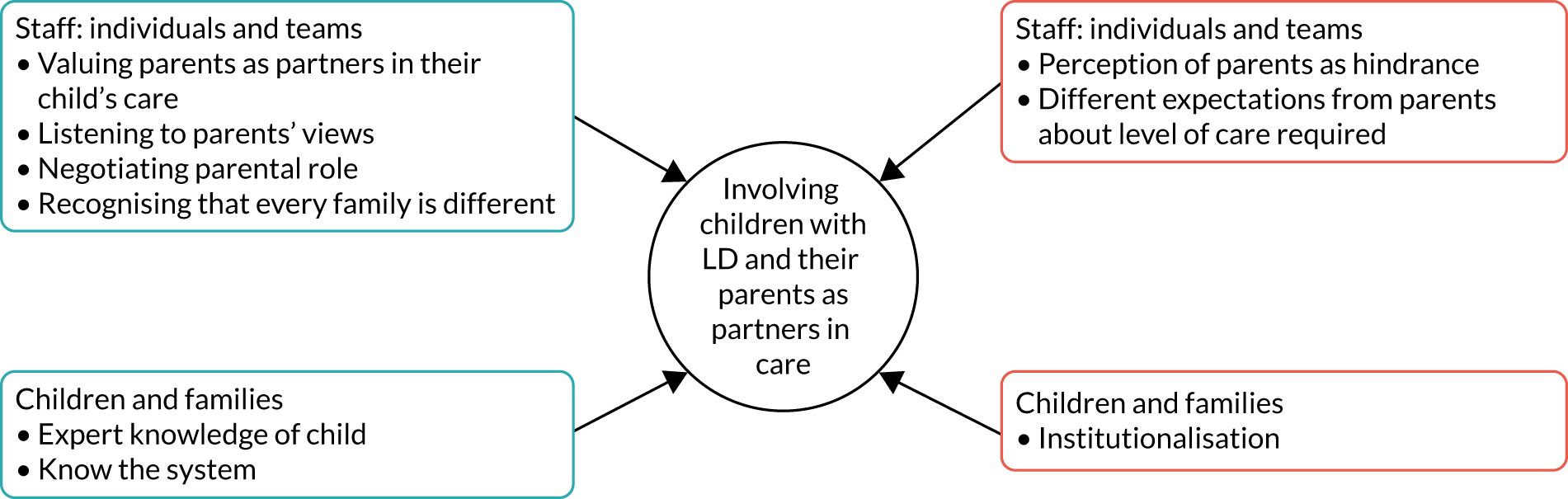
FIGURE 12.
Perceived barriers to and facilitators of children with LD being safe in hospital (staff interviews) (RQ5).
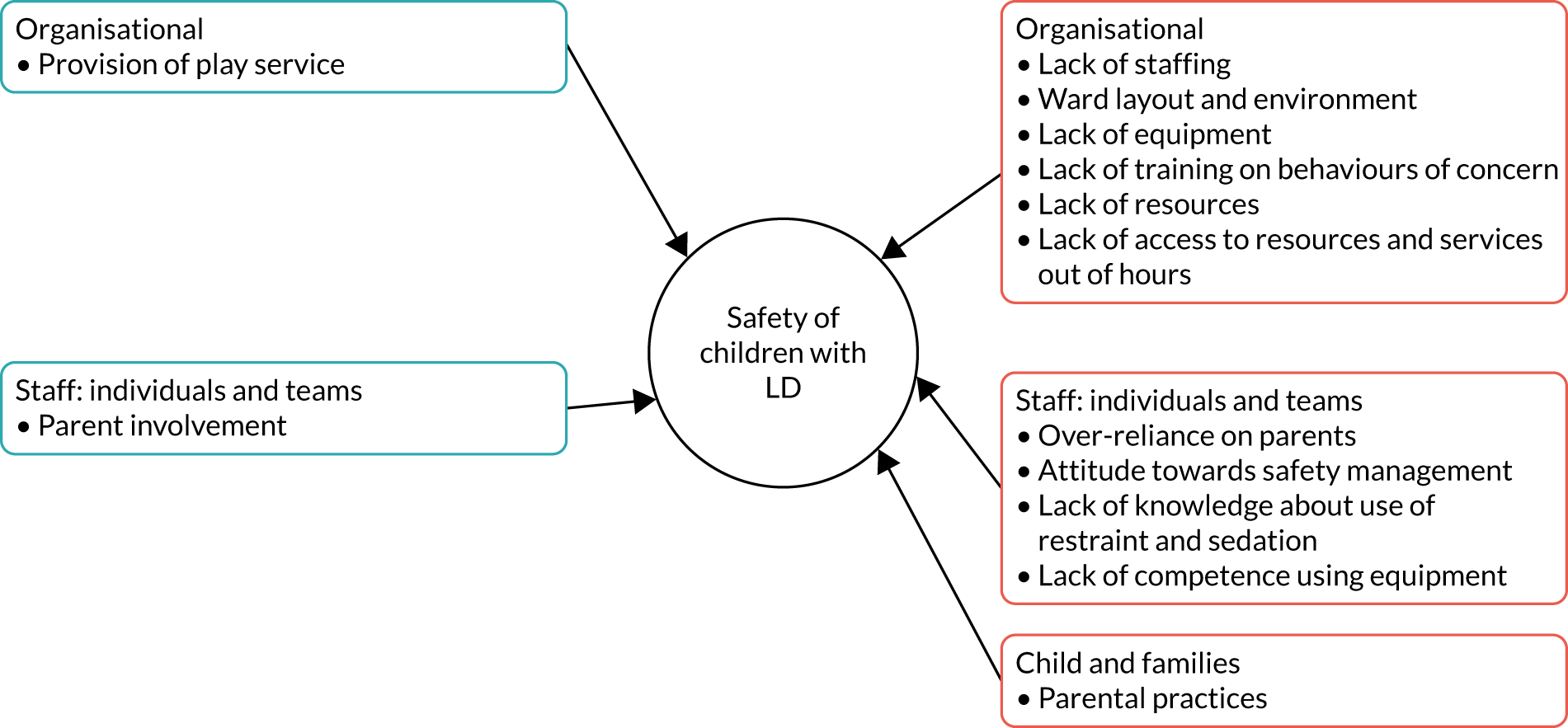
Chapter 8 The experiences of parents
The aim of this chapter is to present the findings of data collected from 63 parents (42 with a child with LD and 21 with a child without LD) during phase 2 (Table 10). To facilitate inclusion and account for the challenges of collecting data in the hospital environment, multiple methods were utilised. Every parent completed a home interview, 38 chose to complete a hospital diary, 48 chose to complete a safety review form and 11 took photographs. Interviews were conducted within 1 week of the child’s discharge from hospital. This time period varied owing to the child’s needs as they recovered at home and other demands on parents’ time (e.g. other children, work or their own health needs). The vast majority of interviews were conducted in the family home. Interviews lasted an average of 90 minutes.
| Characteristic | LD population (n = 52 parents of 42 children), n (%) | Non-LD population (n = 25 parents of 21 children), n (%) |
|---|---|---|
| Participants | ||
| Mother | 26 (50) | 13 (52) |
| Father | 3 (6) | 3 (12) |
| Mother and Father | 20 (38) | 8 (32) |
| Grandmother | 1 (2) | 1 (4) |
| Adopted Mother | 1 (2) | 0 (0) |
| Foster Mother | 1 (2) | 0 (0) |
| Age (years) | ||
| 20–25 | 2 (4) | 0 (0) |
| 26–30 | 0 (0) | 0 (0) |
| 31-35 | 14 (27) | 0 (0) |
| 36–40 | 10 (19) | 7 (28) |
| 41–45 | 13 (25) | 10 (40) |
| 46–50 | 6 (12) | 6 (24) |
| 50+ | 6 (12) | 2 (8) |
| Missing | 1 (2) | 0 (0) |
| Ethnicity | ||
| White British | 40 (77) | 16 (64) |
| White European | 4 (8) | 5 (20) |
| Asian | 6 (12) | 1 (4) |
| African | 1 (2) | 1 (4) |
| West Indian | 0 (0) | 1 (4) |
| Other | 1 (2) | 0 (0) |
| Missing | 0 (0) | 1 (4) |
| Education | ||
| Secondary | 32 (62) | 15 (60) |
| Graduate | 15 (29) | 7 (28) |
| Post graduate | 4 (8) | 3 (12) |
| Employment | ||
| Full-time carer | 29 (56) | 7 (28) |
| Full-time employment | 13 (25) | 6 (24) |
| Part-time employment | 8 (15) | 11 (44) |
| Unemployed | 1 (2) | 0 (0) |
| Retired | 1 (2) | 0 (0) |
| Child’s age (years) | ||
| 5–7 | 16 (38) | 5 (24) |
| 8–11 | 13 (31) | 7 (33) |
| 12–15 | 13 (31) | 9 (43) |
The chapter is constructed primarily around the interviews of parents whose children had LD and is supplemented by findings from the parent diaries, safety review form and photographs. Each RQ is addressed as we present parents’ views on how well the needs of their child with LD are identified and met in hospital, as well as perceptions of their own role and the impact hospitalisation had on their health and well-being. Comparisons are made with data collected from parents of children without LD. The barriers to and facilitators of children with LD receiving equal access to high-quality hospital care that meets their particular needs are summarised at the end of each section. Keeping with the tradition of qualitative research, a balance of quotations and strength of comments are reported in preference to numerical reporting. Where it was felt relevant, to place emphasis on a certain pattern, then reference to ‘number of’ has been included.
For children with LD to be able to receive high-quality hospital care that meets their particular needs, the full breadth of these needs, medical and non-medical, first has to be understood by hospital staff. We provide evidence to show that, in the main, insufficient attention is paid to identifying and meeting the particular needs of children with LD. We first describe parents’ views of their child with LD as having unique needs related to LD that distinguish them from other children, and which require staff to adopt a highly individualised approach to their care. In the second section, we describe parent experiences of what happens in practice, either before or during the hospital admission, that prevents or facilitates staff developing an understanding of the unique needs of each child. We provide evidence of three different approaches taken by staff – proactive, reactive and passive – and the implications of each. The third section focuses on parents’ perceptions of whether or not their child’s particular needs were met in hospital, including barriers and facilitators in relation to their physical care needs and the psychological, social and environmental aspects of their health and well-being.
Children with learning disability are not like other children
Many parents drew distinctions between their child with LD and children without LD in terms of their reaction to being in hospital and their needs during that time, which has important implications when considering the barriers to and facilitators of hospital staff identifying and meeting these needs. One parent reported a conversation that she had had with one staff member:
We have plenty of special needs children come through our doors. Yes, you do, and like every other child, every child is different. Special needs is different again . . . [Child’s] got special needs but the other children in her class don’t have the same needs as what she has, do you know? It’s all completely different.
Many parents described the limitations of the ability of their child with LD to understand what is happening to and around them, and how these made it difficult for parents to reassure them, reason with them, and leave them alone, and unattended, for even short periods. This begins before hospital admission, when the build-up to coming into hospital for a child with LD can be particularly challenging, especially if the child is in pain:
She was desperate. I mean, she was crying and begging us. ‘Hospital now. Take me.’ . . . The build-up to it was horrendous . . . It’s difficult, the way that you’ve got to treat her and talk to her. If it was one of my [other children] I could explain quite happily, even my 7-year-old, but when it’s on [child’s] mind, she’s so repetitive . . . it is constant 12 hours of, ‘My back, my back done. Go now’. It’s constant. She doesn’t stop . . . at 2 o’clock in the morning, she’ll be shouting up, ‘My back. Doctor’.
This parent went on to highlight the emotional impact on her child of her admission being cancelled at the last minute, on the fourth attempt:
That was just horrendous. She screamed all the way home . . . It’s the psychological, with a child like her, with the special needs, and the autism and the repetitiveness, you can’t just say, ‘Oh, it’s been cancelled’ . . . they couldn’t help it either. It was just frustrating.
Another parent described the multiple challenges associated with her child having to wait hours for his operation without being able to eat:
. . . when you’re trying to manage a child with high anxiety and who’s on repeat mode for nearly 5 hours, it’s distressing to see him constantly try and reassure himself and not understanding why he’s not being allowed to have anything to eat. He’s pleading with you, ‘I’m starving, please, can I have some food?’ I mean, you feel terrible, you just feel like the worst person.
In addition to the emotional aspect of hospitalisation, parents identified added concerns associated with their children not being able to ask for help, either through a lack of understanding of how to do so, limited verbal or non-verbal communication skills, or restricted physical ability, for example to use a call button. Equally, the child’s ability to follow instructions or answer questions could be compromised if appropriate adjustments were not made: ‘Because everything goes slowly in the world of Down syndrome and [child] just needs that extra time.’ Concerns were also expressed about a lack of safety awareness in some children with LD, with one parent saying that she was not able ‘to let her guard down’. The inability of children with LD to ‘walk in and fight their own corner’ was also highlighted.
Adding to these issues was the challenging medical symptoms that children with LD can experience, which could mean that no one knows how best to care for and treat them:
I think when children are as complicated as him everybody struggles . . . there’s just no answers. . . . So, I just feel that, he needs to be treated as any other child should be treated, and sometimes that is a battle, which it shouldn’t be, should it?
Some parents reflected on the difference of being in hospital with their child with LD and being there with their other children. One mother described this in terms of having ‘a different level of worry’ that ‘filled her with dread’, and another said:
Children that haven’t got special needs . . . they get on with it. Like, I could take [child’s] older sibling on surgical ward and he’d go in and he could be quite clinical. You could speak to him on that level, on a more adult level, and tell him and get on with it, and he’ll come out, and yes, I had that done, there’s nothing special about it, you know?
The key message was that there are often multiple and compounding layers of complexity surrounding the care of children with LD in hospital and that even those with the same diagnosis as another child with or without LD have unique needs that require staff to take an individualised approach to their care. As discussed in later chapters, it was this individualised approach that appeared to define parents’ understanding of quality care. Parents of children without LD tended not to draw on the concept of difference when thinking about the quality of their child’s care. However, those who had additional learning or behavioural needs associated with attention-deficit hyperactivity disorder (ADHD), autism or dyslexia had an inpatient experience that showed similarities to that of children with LD:
Because she’s got ADHD, she has all this energy. If the nurse was OK, she would talk to them. So, it was all about their personality. How their personality came over to her. If she felt, ‘no’, she wouldn’t talk to them. She wouldn’t let them examine her, wouldn’t let them touch her, but there were just the certain ones. ‘You know, I don’t mind him doing it. I don’t mind her doing it.’ Yes. She had to have that feeling of safeness.
In particular, parents of children with LD pointed to the challenge of their child being in an unfamiliar environment, with unfamiliar people, with times when very little was happening and without their normal routine. There was a perception that some staff see all children with LD as having the same needs, a form of inequity, or underestimate the impact that small things can have on their emotional well-being. In addition, staff caseloads may limit the time that they have for each child. In the following chapters, we show that, although these factors could apply to all children in hospital, the magnitude of effect was usually more significant for children with LD.
Identifying the particular needs associated with a child’s learning disability
For children with LD to receive high-quality hospital care that meets their particular needs, the full breadth of their medical and non-medical needs must be understood by hospital staff. In the majority of cases, parents reported staff taking a passive approach to this, developing their knowledge more by luck than by judgement, through what they happened to observe (or not) during the child’s admission and what the parent happened (or not) to tell them (parent quotation 1; see Appendix 9). As one parent described, staff showed a complete lack of awareness about what having a LD diagnosis meant in terms of her child’s cognitive and communicative abilities:
No nurses came to even talk to her. Yes, they were loving my daughter a lot, they were giving her love, but they did not ask any questions of what she’s capable of doing and what not.
Clearly, a lack of enquiry about the abilities of children with LD does not preclude staff being kind to them (parent quotation 2; see Appendix 9) and will not necessarily have an impact on the quality of care provided. However, as one parent explained, assumptions about her child’s level of understanding were often based on their physical impairment and a label in the notes rather than knowledge of them as an individual. This might have an impact on their expectations of the child, with examples of staff not explaining things before doing them or of the child being excluded from discussions. In more than one example, there was a lack of realisation from staff about a child with LD having a visual impairment, including one young girl who was blind being asked to point out items in a picture.
Many parents talked about the admission process being focused on medical-related needs, such as whether or not the child had any allergies and their medication regime, at the expense of needs regarding particular equipment, food preferences, moving and handling, positioning and sensory needs. Parents cited a number of reasons why staff may not pay attention to a child’s learning and/or communication needs, including them being dismissive, lacking time or understanding of the need to do so, or feeling uncomfortable about asking:
They just saw, ‘[child] 5, PEG [percutaneous endoscopic gastrostomy] fitted’. It’s like no-one actually sat there and went, ‘[child], 5, PEG fitted, has severe cerebral palsy’, and it was like the cerebral palsy thing just didn’t exist . . . I’d like to think it’s not ignorance but whether it’s just the unknown . . . whether it was sheer nerves . . . or are they going to offend the parents?
Parents would not automatically offer relevant information about their child. Rather, parents often assumed that staff knew more than they did, which was based on parents knowing their child’s diagnosis, such as cerebral palsy, or forgetting that other people did not know their child the way they did. A common issue nearly all parents faced was the repeated request from staff for the same information about their child. This still tended to be for medical information relating to a diagnosis or the reason for their admission rather than related to LD: ‘When you do eventually see a doctor, or anybody else, they all ask you the same questions over and over again’. This request for information might be made in front of the child, with little or no thought given to the child’s level of cognition or the distress that this may (unintentionally) cause, which could be avoided:
I just had to keep explaining and going through it. I feel sometimes when I’m explaining then it makes him worse, because he knows he has it. He struggles and you can tell he does. People pick up on it, but, obviously, because it was different people coming in and out constantly, I had to keep repeating it.
It’s like interrogation but it does wear you down . . . It’s like War and Peace every time.
Even when armed with specific information about the uniqueness of each child’s diagnosis and comorbidities, staff often relied on parents to provide a greater depth of information, which over time proved to be a source of frustration for some parents:
Well, half of them don’t have a clue. They’ll look on her record and they’ll known what she’s got wrong with her but they all come in and say, ‘What’s this? What’s she got wrong with her?’ I don’t know how many times I have to explain to people what she’s got wrong with her, and I just think, ‘If you don’t know just look it up’ . . . It does get you mad sometimes.
Staff were sometimes seen to actively seek information about the child’s non-medical needs, but this often occurred during the admission, ‘learning on the job’ when something became apparent, rather than in the initial assessment, for example how the child communicates, what they understand and how they express pain. More often, there was a reactive request for information about a child, when the need arose, rather than a proactive request, in order to be able to plan. There was still a reliance on parents to offer information:
Nobody actually asked if we had any specific requirements for her . . . nobody said, ‘Do you need hoisting equipment? Do you need changing tables? Do you need to be able to her hoist her from a chair to a bed?’ . . . One or two of the nurses, just through chit-chat, told them that, ‘This is her “yes” hand, this is her “no” hand’. One of them asked her a couple of questions, but no-one really actually specifically asked us, ‘Does she understand? How much does she understand?’ We tend to have to volunteer the information.
However, it was apparent that staff did not always pay sufficient attention to adapting their practice for the child’s benefit:
We told them about his signs . . . they kind of just went, ‘That’s nice, that’s good’. Nobody asked to see what the signs were or if we could show them . . . I think they’re quite happy for you to get on and use it.
Identifying individual needs was also reflected in relation to children without LD who had additional learning needs. For example, the parent of a child who was receiving therapy input prior to discharge noted in the parent diary:
. . . returned and advised that I should register [child] as autistic!??? and advise the local authority education etc. I had to correct them to say that [child] is not autistic he is dyslexic! Told them that he already is registered as dyslexic and he had a Psychologist Educational Report. I feel that sometimes you are not listened to very well.
This parent also reflected on this experience in her interview:
‘Oh he’s dyslexic, we never knew that.’ That’s where it stopped. There wasn’t any sort of change of learning or nursing or anything with him . . . if they had known and had they had the resources and things, and [known] what to do, things would have definitely been better.
Although this parent had given specific examples of how to adjust the delivery of information and practical solutions, staff failed to act on these and, as a result, the child had experienced an admission three times longer than expected. This mother went on to explain the difference between staff acquiring and not acquiring the relevant information about her child beforehand:
So many hospitals you go to–, she can be in a wheelchair and they’ll speak to her ‘What’s your name? What’s your age? What’s your date of birth?’. You’re like . . . ‘Well, if you’d read the notes, you’d know she can’t speak’ . . . You get that so many times, but they didn’t do that. They went at her speed and her level. If she said something, they listened, and they said, ‘Right, OK, we can work with this, and we’ll do this and that’.
The amount of attention staff pay to identifying the non-medical needs of children with LD clearly has implications for the implementation of reasonable adjustments. Not having the necessary information until the child is admitted to hospital, which in some cases occurs many days later, clearly reduces the opportunities for adjustments to be made (parent quotation 3; see Appendix 9). As one parent suggested, putting things in place for children with LD is not necessarily difficult, but it does require some thought and planning:
All we’re thinking about is 10 children, 10 operations but they’re all individuals . . . could that not be done before you get there? If you know it’s a child with special needs, and you know they’re blind, then it doesn’t take a rocket scientist if you’re a play specialist, to say, ‘Right, I know what type of toys this child’s going to need’. So, in that room, in those cupboards, could be the play set.
Rarely did parents provide examples of staff seeming to pay complete attention to identifying their child’s non-medical needs by consistently and proactively consulting with them prior to admission and discussing the need for any reasonable adjustments. Even at preoperative assessment clinics, the opportunity for staff to identify the child’s individualised needs was often missed; a tendency remained for staff to focus on the reason for the child’s admission and relevant medical issues:
She took details of his condition and the syndrome, the autism . . . but that nurse that did the pre-op check it wasn’t like she asked me about whether there were any good things to be doing with him or things to avoid . . . I made a point of saying keep blood pressure machines away from him because they do totally freak him out but she didn’t probe or ask any questions around how best to deal with him.
One parent reflected on the positive interaction that their child had had with the consultant prior to her operation:
He did speak to her very, very kindly and on her level. He did understand she had special needs. I didn’t have to tell him. Whether he read notes or what, I don’t know, but he did speak to her on her level, and spoke to her in her terms . . . He was absolutely brilliant.
When asked, parents largely reported wanting staff to ask about their child’s specific learning needs, ‘out of decency’ (parent quotation 4; see Appendix 9), rather than not, and this was also the case for parents who had children without LD. However, as one parent explained, being asked in a letter to call the ward prior to admission if her child had LD was not particularly helpful ‘when you’ve already got a million phone calls to do’.
The importance of staff taking a proactive approach to understanding the non-medical needs of a child with LD, as well as the whole team being involved, is exemplified in the following quotation from a parent:
He [doctor] always asks personally if [child] understands and even when they book appointments and they call me . . . When I say, ‘He’s delayed’ they ask me, ‘How can we communicate with him? How can we understand?’ . . . I’m shocked every time how ready they are . . . they would do handover and then they would ask me more questions . . . I feel like that’s a dream . . . They’re not here to judge you. They’re here to support you . . . All staff knew what they needed to do, everyone.
Being proactive meant making information about the child’s LD easily accessible to all staff, for example by having ‘a dedicated page on the outside of the notes’, or ‘stickers up on the wall, just as they have “nil by mouth” stickers’. This may be a function of the hospital passport, but the majority of parents had never heard of it, although they felt that they would have valued being offered one. A couple of parents specifically described making ‘All About Me’ posters to put above their child’s bed, which shows staff the child as the person they are when not unwell. A hospital passport had been provided to a couple of families a few weeks into their children’s admission, by which time the parents could not see the benefit of completing it, with one describing it as a tick-box exercise. One parent whose child became critically ill just after she had been given the passport said that had been the last time she saw it, and another felt that the entire process was futile because ‘nobody asks to see them’. This mother went on to say how traumatic she found having to repeatedly answer doctors’ questions about her child’s birth, explaining that she had had post-traumatic stress disorder at the time and she felt as if she was reliving that each time she came to the hospital. This example highlights the importance of staff paying specific attention to what they need to know from parents for that particular admission, as well as being sensitive to the impact that sharing the information might have on them, something they will be able to do only if they have the right information beforehand.
There was a notable difference in cases when staff already knew the child from their multiple admissions to hospital. This experiential knowledge was felt to give staff valuable insight into what to expect and also what the child was like normally, providing a useful barometer of how unwell he or she was during the admission and what they were capable of:
They’ve got knowledge of [child] now, when we were last in we had a new nurse and they were brilliant I can’t fault them, but you’re having to, point out what other nurses already know. So, other nurses on the ward, why aren’t they allocated to us knowing that?’ It does give us a bit of confidence when you see familiar faces.
It was apparent that maintaining consistency of staff during the admission was essential for them to get used to the child’s ‘isms’, and this was something parents valued highly. When this was not in place, the impact was significant, and this was the case for all children in our study. However, this experiential knowledge was not always enough. One parent said that although staff knew about her child’s rare condition, it was still important for them to ask questions about her own child specifically, because ‘children with the condition are still different in what they can do’. It was also recognised that there was sometimes a limit to what staff might realistically be able to understand within the short time frame the child was in hospital, which meant that working in partnership with parents was vital:
Knowing how to communicate with him is important for people who don’t know him, but it is really difficult because I am always speaking for him . . . it takes months and months to get to know him. So, I don’t expect people, even if they are with him every day for a short period of time to understand, and I expect to have to speak for him.
The degree to which hospital staff paid attention to understanding the non-medical needs of children with LD appeared to depend on the individual staff member who was looking after the child on any given day. Parents reported variability in the approaches of staff working on the same ward at the same time and during different admissions, between staff working on different wards and in different hospitals, and between staff from different professional groups. Nurses were perceived to be on the ward and to have more time than doctors, but consultants modelled good practice, for example by talking directly to the child. The barriers to and facilitators of identifying children with LD in hospital, from the perspectives of parents, are illustrated in Figure 13.
FIGURE 13.
Perceived barriers to and facilitators of identifying children with LD in hospital (parent interviews) (RQ1).
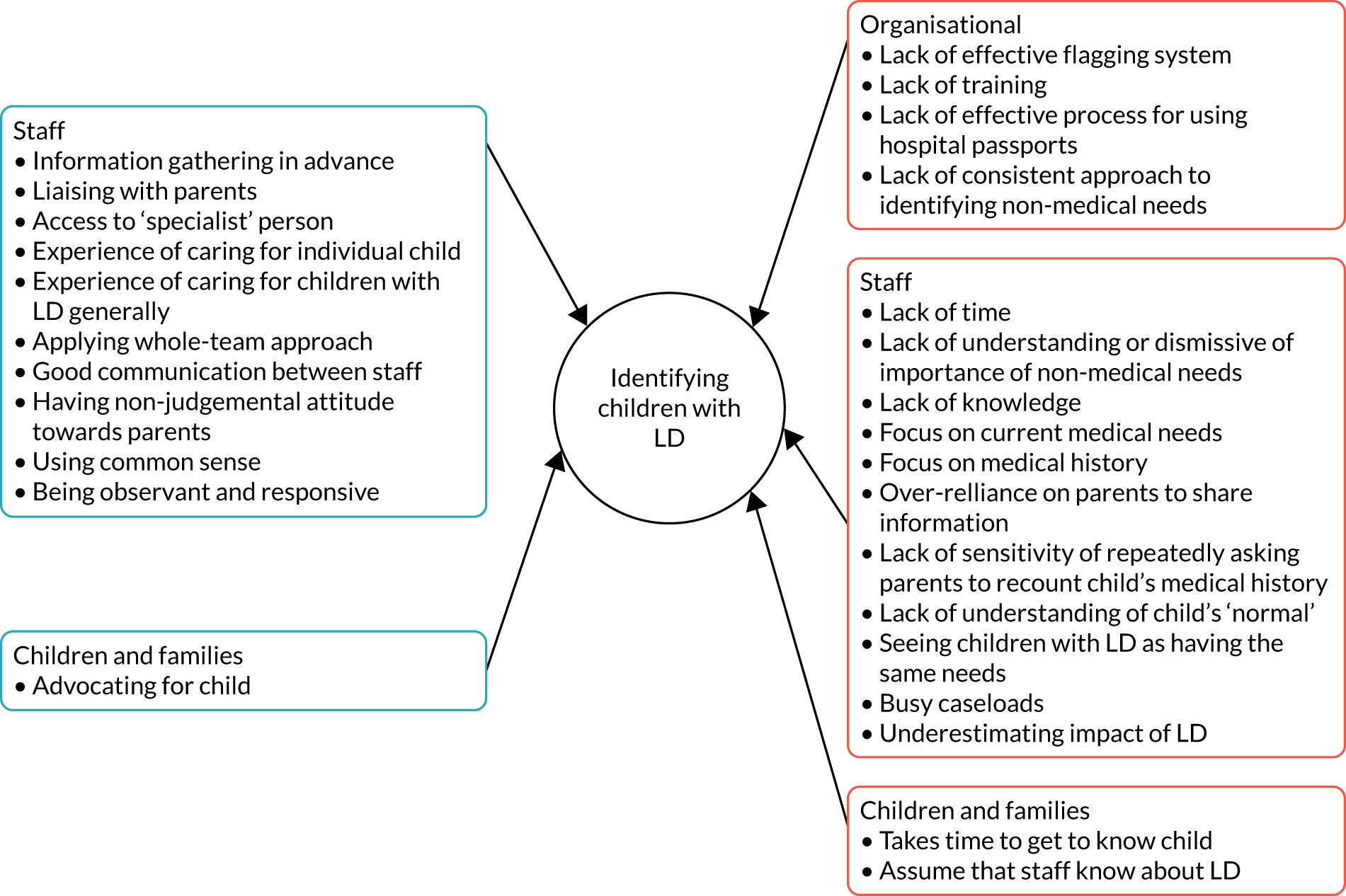
Do children with and children without learning disability have equal access to high-quality hospital care that meets their particular needs (research question 1)?
The aim of this section is to describe parents’ perceptions about whether or not their child’s particular needs were met in hospital, including the barriers and facilitators in relation to the physical care needs and psychological, social and environmental aspects of their health and well-being. In each section, we present data from parents of children with LD first, except in situations in which there is greater benefit from reflecting on both groups of children in the same sentence. In Chapter 9, we explain the strategies that parents used to keep their child safe in the context of the care they received.
Starting with physical care needs, parents tended to focus most on staff confidence and competence in meeting these. Approximately one-third of parents of children with LD positively described their child’s care in general terms, for example ‘cannot fault the ward’, ‘care being excellent’, ‘needs being met’ and ‘surgery going well’. As one parent stated, ‘The staff were brilliant, they really were . . . his care, I thought, was excellent’. More specific examples, mentioned already, included the importance of staff having knowledge of the child and of the complexities surrounding the child’s condition, being an expert and being experienced:
I’d definitely recommend, as a hospital, I think they’re fab . . . you can tell when you’re speaking to consultants, that they really are good at what they do, so from that perspective we couldn’t fault, the expertise . . . we always felt we were in good hands.
Being prepared and adaptable were also mentioned, as was being responsive to the child’s needs, for example using accessible pain ‘tools’ to assess and manage pain, and having things ready in anticipation of seizures. A few parents also talked positively about their child being closely monitored, including the parent of a child with LD in a high-dependency unit who said that ‘every 10 minutes they [nurses] were coming in, writing things down’.
In addition to positive experiences, about half of parents reported concerns about the ability of staff to meet their child’s medical needs, pointing to a lack of knowledge, skills and training, confidence, planning and documentation, with generalised comments such as ‘child’s needs not at all met’, ‘they haven’t got a clue’ and ‘need wider understanding of the basics’.
Particular examples were described in relation to feeding, pain management, moving and handling, and managing seizures and dystonia, including some perceived care errors or near misses, medical incompetence, inequalities in care and diagnostic overshadowing. As one parent said:
We feel very negative about that particular admission . . . I do strongly believe that taking [child] into a hospital is worse for her than staying at home . . . You need efficient people, effective people and you need to know that the quality and professionalism of the provision is well measured . . . They haven’t got the understanding of the level of care that [child] requires . . . It’s almost laughable how pants it was.
Parents reported instances of medication being forgotten, being given via the wrong method or at the wrong dosage, being made up incorrectly or not being given according to the child’s usual regime or in a timely manner. One parent compared her experiences of medicine management at two different hospitals:
He had a load of seizures one day because they didn’t bring his medication on time. They said, ‘Oh, well, the shift change can bring them’. That’s not good enough, he needs them now . . . I think [name of current hospital] were a bit more understanding of the fact that when you’re in hospital, just because the drugs chart has 8 o’clock . . . that’s not in reality what happens at home.
Another mother talked at length about the challenges of managing her child’s dystonia in hospital, despite the fact that there was a ‘robust escalation plan in place’:
Really basic simple things but could be disastrous for [child]. It could set the scene for the entire day if you suddenly trigger a storm . . . they misinterpret that as a seizure . . . then they would probably give her Epistatus or it might be they give her chloral . . . they would likely knock her out for the entire day . . . that’s not a life for [child] just because somebody’s not understood her needs.
She perceived some of the nurses as anxious and worried about how to manage her child’s symptoms, but suggested that care would have been safer and easier for them if they had liaised with her and had taken time to get to know her child from the start rather than ‘trying to second-guess’. What often happened was that this mother was called on to make decisions about treatment, even during the night. Although she wanted to be involved in her child’s care, she reported feeling anxious when staff expressed uncertainty about the best course of treatment. This was reported by several parents, with one describing being left ‘battling between what’s right and what’s wrong’ when two of her child’s consultants disagreed about her epilepsy treatment. Concerns were not necessarily about complex issues but might require an understanding of the child’s individualised needs:
It’s just simple things like his feed. Someone could do it so it’s red-hot and barely tolerable to eat, but another nurse could do it where it’s straight from the fridge, freezing cold, and equally just intolerable. So, to get that, ‘I like my feed warm’, is, actually, these are child’s needs, not what his parents want.
One parent who was highly critical of the quality of food in hospital also highlighted that incorrect assumptions were made about her son’s inability to eat orally because he was also tube fed:
We have to fetch our own food in because they can’t cater for his diet. All that they feed children is chicken nuggets and pizza . . . so they get them in hospital then they ram them full of shit. That’s the politest way I could’ve put it. It’s Jeremy Kyle, sit them down in front of the telly. ‘Here’s your food, I’m watching the telly’ type of mentality.
Several care errors or near-misses in relation to tube feeds were also reported by parents of children with and children without LD.
Staffing levels were also perceived to be a key factor in the delivery of high-quality physical care, with examples provided of nurses ‘having enough time to care’, ‘responding to the buzzer’ and ‘not being rushed’, as well as of nurses being too busy to appropriately manage pain, monitor symptoms, provide necessary treatments or sit and watch the child. Having a higher staff ratio was felt by one parent to lead to more motivated staff and a better ward atmosphere. Several parents, however, described feeling ‘left’ to get on with things, with the child ‘going a long time without having needs met if parents not present’. A small number of participants had care packages that meant their carers continued to provide one-to-one care for the child during their hospital admission. However, one parent felt that this meant ward staff took less time with their child:
The nurse poked her head around and went, ‘Are you all right? Oh dear, she’s not having a very good night, is she?’ . . . She didn’t offer to help . . . There was one time where I think one of our carers had said, ‘Can you sit with her and support her while I draw up the meds?’ . . . She did it for maybe 5 minutes, she went, ‘Oh, she’s ever so strong. I can’t do this any more’, and went.
This parent went on to say that a lack of documentation by hospital staff was a major issue, highlighting that they were still responsible and accountable for her child’s care (parent quotation 5; see Appendix 9).
A small number of parents described situations, either previously or during the current admission, when they had felt that physical symptoms had been attributed to their child’s LD (i.e. diagnostic overshadowing):94
A lot of times, we’re just left or with things like her hypoglycaemia and they just thought, ‘It’s just down to her Down’s syndrome’. There was never any real investigation to find out or try to get to the bottom of it. So, I suppose if you compared that with a typical child, obviously, they wouldn’t, kind of, have that get-out clause, would they?
This parent reported having the same problem in relation to her child’s sleeping issues, constipation and hip problems, with the symptoms just being treated and not followed up because the child was never really seen as an individual. Another parent of a child with Down syndrome reported a similar experience in relation to her child’s sudden onset of pain and difficulty walking:
We went through to orthopaedics and I saw a junior doctor . . . and he blamed the Down syndrome, said, ‘There’s nothing wrong with the knee’ . . . he missed the opportunity to look at the hip . . . he said it was a low muscle tone . . . ‘she’s walked for 11 years, why all of a sudden is she not walking and it’s getting worse?’. He was very arrogant and he sent me away . . . all this time was marching on and she was getting progressively worse.
Not knowing a child was seen as a risk factor for diagnostic overshadowing.
Parents rarely expressed a wholly positive or wholly negative experience when talking about the physical care needs of their child with LD in hospital. Differences in knowledge, expertise and attitudes were described between individuals, for example some nurses ‘going the extra mile’ and others being ‘not good’, as well as between different professional groups, between staff working in different clinical areas such as surgical and medical wards, and between staff working in different hospitals (parent quotation 6, parent quotation 7; see Appendix 9). A paradox appeared to exist, however, between the high levels of medical skills and expertise staff had, often in relation to highly technical procedures, and their lack of knowledge and skills in meeting a child’s basic needs specific to having a LD. One parent described three levels of awareness, highlighting the difference between conscious and unconscious competence:
The difference is palpable to be honest with you. You can feel the difference between those that know and are comfortable with it, those that don’t know that are completely oblivious to it, or those that know but who are not comfortable with it at all. So that could be down to skill set and experience and training.
Although there were no examples in our data of parents of children without LD who needed to bring other carers into the hospital setting, or of diagnostic overshadowing, our data would suggest that many of the issues faced by children with LD in relation to their physical care needs being met are mirrored in the non-LD population. For example, the impact of staffing levels, particularly at night, resulted in periods of increased vigilance. Parents reflected in the main on experiences that ‘ticked all the boxes’ in terms of care needs, being able to ‘stay in the same routine’ in terms of administering medicines, and ‘faultless’ in relation to a high-dependency care unit. An example first from a parent diary (child with LD) and then from an interview quotation (child without LD) show these similarities between child populations:
I wanted to double check the drugs chart before we left to make sure ours says the same thing. There are NO notes on cares after 11 pm. None of her SATS [saturations] drops have been recorded, nor her seizures. Only the obs. on the iPod [Apple Inc., Cupertino, CA, USA] thing.
It really was you have to be 24/7 [24 hours a day, 7 days a week] to make sure everything she needs happens. You know down to taking over the management of her oxygen, all the issues to do with the bed, etc.
The majority of parents talked about the impact that being in hospital had on their child’s psychological well-being. Although again there were pockets of excellent practice, with staff adjusting their care accordingly, parents mostly described barriers to their child’s psychological needs being adequately met. Waiting was a particular challenge for a number of children with LD, who could become ‘restless’, ‘distressed’, ‘scared’ and ‘bored’ as a result. One mother described the impact of having to spend hours in the outpatient department with her son during an inpatient stay:
It was crazy . . . he was still getting over the sleep deprivation; it was just like torture for him to the point that he was hitting and kicking me and I was trying to keep him up. To do that to him, like a 3-hour appointment and it was sweltering down there and they had drinks down there but he couldn’t drink any of that because he only drinks specific things.
Another parent described the impact of her son waiting all day to go to theatre:
We didn’t get told he was last . . . it was half past five before he went down, after we’d been there all day . . . on Polycal which is like pure sugar being pumped into him . . . it made him hyper . . . when he came round from his anaesthetic there was five of them trying to hold him down, so I found it amusing, because I said, ‘Well, we’ve had that all day, and you’ve left us here all day, and left us until the last one . . . he didn’t go to sleep all night.’
In neither of these examples were any reasonable adjustments made to accommodate the child’s needs, and nor were parents informed of how long the wait was likely to be, the impact of which is captured in the two quotations.
More than one-third of parents talked about the psychological impact of their child with LD undergoing tests and procedures, which the child could find ‘overwhelming’, and the potential for staff to ameliorate or exacerbate this. The use of distraction for blood tests was praised, as was the support given to some children when they were going into theatre:
They were really on the ball with the fact that he’s going to need a bit more support. When they came to administer the pre-med . . . the play worker was chatting to him, one nurse was holding his hand then the other one was going to do the administering . . . accommodating of the fact that you couldn’t rush him.
This parent went on to describe the anaesthetic team’s responsiveness to her child’s needs by not using the mask to ‘put him to sleep’ and preventing him becoming hysterical, as had occurred during a previous admission. Similarly, another parent explained that having a ‘pre-med’ on this admission had been helpful, whereas ‘last time he went down fighting and came back fighting’. A number of parents talked specifically about theatre staff and their willingness and ability to adjust their practice to suit the needs of their child (parent quotation 8; see Appendix 9). In the example below, a nurse who knew the child well pretended to be taking her stiches out when in fact the surgeon behind her was doing it:
She let her take stitches–, heavens, for us, you don’t realise how massive that is. This surgeon was with sweat dripping to him . . . Yes, I know [child’s] face and I trust her, she’s been going every week to see her and whatnot so she’s become, like, a real friend. Yes. Then the surgeon took a step back and said, ‘I’ve got them all’, the nurse went ‘Yes, I’m done, [child].’ She was like, ‘OK’.
The challenge of children with LD undergoing procedures was highlighted clearly by a parent whose child had been admitted to a specialist children’s hospital for planned telemetry electroencephalogram (EEG):
He ripped his cannula out . . . it took four nurses and me and my wife to get the cannula back in. They [nurses] were worried about how he was feeling and how stressed he was . . . they went and got the extra nurses and held him down and he was hysterical . . . I think that was probably the hardest human thing to be honest. They got it in eventually and he calmed down after about an hour.
Another parent talked about the challenge of cannulating her child. She described staff instead getting blood by ‘stab[bing] his fingers or his toes and get[ting] blood that way which is quite cruel and it’s not just a little stab’. The laboratories repeatedly reported that the sample was inappropriate, which the consultant later (i.e. post discharge) agreed was probably a result of the method used. A lack of preparation and involvement of parents regarding tests and procedures was seen as a barrier to these being carried out in the best interests of the child. Another mother whose child was admitted to the same hospital for the same procedure predicted that it would be very challenging to put the EEG sensors onto her son’s head:
Another child might understand what’s going on but just not like it . . . but obviously chucking in autism and ADHD and a lack of understanding and communication, that’s just asking for trouble [laughter]. Yes, you’re asking for a disaster there.
Parents would often offer guidance about their child to enable staff to achieve their aims, but they were not always listened to or regarded as an active partner in their child’s care. For the child receiving the EEG, this was the main focus, and the parent was happy for regular observations (e.g. blood pressure and temperature) to be carried out later. It appeared that some children were ‘already at the point of no return’ before staff involved the parent. This had emotional and physical implications for the child:
Obviously, with an autistic child, once they’ve got distressed, then the calming down time is quite time-consuming. You know, he hurt himself. He had bruises all over his legs from chucking himself on the floor . . . he took ages to go to sleep and he was crying, which isn’t normal at all for him. So, I think the distress was obviously probably playing on his mind still.
This parent explained that she had asked for her child to be sedated beforehand and that staff needed to just ‘stop’ and consult with parents in advance about what would be involved and any adaptations that they thought were necessary.
Similarly, parents of children without LD also had both positive and negative experiences. Several parents recounted previously distressing experiences in relation to receiving a general anaesthetic or specific procedures, which had had a negative impact on their child’s ability to manage subsequent events in hospital. One parent described a loss of trust as a result of their child being misinformed about a procedure and being told ‘it’s not going to hurt’ when clearly having blood taken was going to hurt. They went on to talk about their own distress, and their child’s, when he was held during these procedures. This parent, and others, provided several examples of staff working hard to improve these experiences subsequently by paying specific attention to the child’s anxieties, and listening to the parent and/or the child, effectively mitigating these. These efforts of individualised care and attention to a child’s specific needs were praised very highly by parents: ‘Please can you take my cannula out before I wake up? . . . so, she was really good and had taken it out.’ When asked specifically about whether emotional needs were met, a number of parents of children without LD said ‘no, not by the staff’. This was often followed by a statement expressing surprise, and in these cases parents saw this very much as their role: ‘I took care of her emotions’. They were overall less concerned about emotional care, because they could deal with that, either in hospital or when at home, as long as the focus of the admission was not compromised. As with physical care needs, children without LD but with additional learning or behavioural needs had similar experiences to children with LD, highlighting again the significance of knowing a child and individualising their care:
I think, when she goes in that they are told what she’s in for, but don’t necessarily know her background, and take other things into consideration . . . we don’t ever have the same nurse . . . well you know if there’s a change could you please let us know a few hours before so we can prepare? Things like that.
Related to emotional well-being, an additional theme about dehumanisation emerged from the data that came only from interviews with parents of children with LD. For example, the unique diagnoses of some children with LD meant that they might receive greater attention from staff because they were a ‘novelty’ rather than for the child’s benefit:
It did feel like he was a bit of novelty, because the doctors seemed quite excited that he was there . . . that they could show people . . . they weren’t insensitive, but sometimes you did feel a bit he’s not a-, I don’t know a freak show sounds too harsh . . . but he’s not something to be gawked at . . . There’s a balance between showing that and wanting to teach . . . he is aware that people are oohing and ahhing, and ‘oh my gosh’ . . . so there’s a balance, he’s still a human.
This sentiment was echoed by another parent, who felt that staff at her local hospital who did not have the skill set to manage her child’s condition might ‘come and have a look’ and ‘have a nosy’ as if (s)he was ‘one of the seven wonders’. Isolated examples were also provided of staff ‘switching off’ while being told about a child’s needs and displaying an attitude of ‘he just doesn’t understand anything’. As well as staff lacking sensitivity, it was felt that some were simply rude:
We have had some experiences as well where we’ve had consultants be really rude . . . we had a consultant walk up to us and he was just so rude and looked at me and [child’s] dad and said, ‘Have you two been tested so this doesn’t happen again?’ [Down syndrome] and, kind of, referenced at [child] with his hand.
This parent had previously been asked by a consultant whether she had been given the option to abort her child and that, a lot of the time, ‘they [clinical staff] can be really rude and quite condescending about her child and her needs’. She also felt that there was ignorance from staff in hospitals generally in the terminology they use and said how ‘hurtful’ it could be grouping her child into just ‘those with Down syndrome’ and referring to her ‘as if she’s just this different race, like a their’.
One parent described a particularly negative interaction with a consultant, who had been asked by her son’s own consultant to come and review her son ‘as a favour’:
He’s ignorant . . . those posters that are up around bus stops where you’ve got a girl with Down’s syndrome and everything that’s saying, ‘I’m not just a disability’, someone needs to get one and stick it in his locker or his office . . . to say that people in [child’s] condition can’t communicate, so we [parents] jump to assumptions, that is disgusting, and that is also painting all disabilities as one line, and they’re not.
As a result of this exchange, the parent said, ‘I made a vow. No-one treats my child like he’s a cabbage. No-one makes it out my child’s a cabbage’. At times parents felt that staff’s attitudes or assumptions about disability had the potential to have an impact on their child’s access to particular aspects of care or treatment. Examples from previous and current admissions were provided of staff seeming to exclude the child from singing in the playroom with other children, overly focusing on what the child could not do and focusing on palliative care rather than treatment. One child was refused a general anaesthetic for an endoscope, despite the fact he would not tolerate the procedure without one, whereas another parent felt that the lack of value her child’s consultant placed on his life would prevent her wishes about palliative care being honoured. A challenge accessing appropriate pain relief was also described:
Because [child] can’t communicate what he’s feeling or what his needs are it’s taken for granted. So, pain management’s always been an issue because he can’t tell us that he’s in pain . . . let’s be on top of that pain, not react to it. So, we had a mutual disagreement with the pain nurse last time. ‘Oh, often paracetamol is normally fine’. Well, [child’s] not normal and we’re not willing to take the gamble because he’s just been through so much.
One parent described at length the barriers she had faced before obtaining surgery for her child, who had experienced 3 years of extreme pain, after a fourth opinion:
He made the assumption, he said, ‘I’m not going to do the operation’ . . . it was because of the Down syndrome . . . ‘Does that mean a life in a wheelchair full of pain?’ and he said yes. He said, ‘These children,’ by which he meant children with Down syndrome, ‘I can do the operation and they will choose not to get up out of the wheelchair.’ I said to him, ‘You haven’t taken into account [child’s] tenacity or my tenacity in making her do the exercise’ . . . He made an assumption, based on cases he’d done in the past, without really knowing [child] at all or asking me about how we would rehabilitate, it was all his attitude and he didn’t engage with [child] at all.
Not all examples parents shared were in relation to the child’s current admission. However, it was apparent that these incidents could ‘stay’ with them forever, and this is important when thinking about equality of care. The mother quoted above, for example, described having learnt to ‘play the game’ needed to get the treatment her child needed, suggesting that there was ‘no equality whatsoever’ because children without LD were not faced with the same issues. It took a fourth opinion before a consultant agreed to operate on her child, and she said that her experience ‘colours every other appointment that I go to’.
The importance of positive social and environmental aspects of care was also highlighted. The loss of routine and lack of familiarity while in hospital were further issues faced by children with LD, which could have an impact on their sleep, cause confusion and irritability, and raise anxiety. As many parents explained, their children relied on certain things (e.g. smells, objects or activities) happening at certain times to provide them with a sense of security or guide them about what would be happening next, for example in relation to a bedtime routine:
You cannot use it [disabled bathroom] at all . . . It does, it punctuates his day as well. It’s his cue to go to sleep. It relaxes his muscles . . . just little things like that, and being able to do his massage after his bath. The whole thing is a really important part of his routine . . . he hasn’t got the familiar smells and things when he’s in hospital, and he relies on those.
One mother explained how keeping to a routine, such as school, made a ‘massive difference’ to her son, whose teacher visited him in hospital:
His face lit up as soon as he recognised the voices of the staff that he knows. They did hand massage and stuff with him. The day seems to go quicker because it’s really hard trying to entertain a child who’s irritable in a room where you haven’t got your own things and he hasn’t got his own things.
Even trying to establish a routine while being in hospital could be a challenge and, at times, staff ‘just didn’t really take it on board’. Other examples of factors that made this difficult included being moved five times during an 8-week inpatient stay and a lack of resources, such as symbols and social stories, being available.
Most parents spoke very highly about play staff, with the main criticism from both groups of parents being that there was a shortage of provision. Nearly half of parents of children with LD said that during their child’s admission they had been seen at least once by a member of the play team and/or a hospital teacher, who often tried to source appropriate toys and sensory equipment. Some positive examples were given of these individuals making adaptations specifically to meet a child’s individual needs:
The play team were fabulous. They’d come up and they’d say to [child], ‘What do you like playing with? What do you like doing?’ . . . They’d go off and they’d bring her level . . . all these big trays of stuff and nothing was too much trouble. So, yes, they kind of catered individually, for everybody, but never left you alone.
The amount of contact children had with the play team varied considerably, from seeing someone once on admission to seeing them every day. One parent said that the play specialist ‘couldn’t do more for her child’, while another described how they tried 100% to meet her child’s needs, even if they were not always able to. The importance of play specialists paying attention to the child’s chronological age as well as developmental age was highlighted:
Another thing I struggle with [child] is, he’s 15, he’s got 15-year-old hormones raging through his body, he thinks like a 15-year-old, but because of his condition, people talk to him like he’s a baby a lot of the time . . . but the play team spoke to us before they approached him because they didn’t want to offer him baby toys if he wanted something more grown up. I was very impressed with them . . . one sent us off for a cup of tea and sat and read to him, because he loves listening to people read.
The involvement of the hospital school was also highly valued:
The SEN [special educational needs] teacher was just amazing and just having their involvement from very early on actually . . . he adored their sessions . . . they liaised with his normal school and they even learnt one of his favourite songs . . . and the teacher actually sent a video of her doing the song for them, which they showed [child] as well. So it just, kind of, shows the level of liaison really.
However, some parents reported less than positive experiences, rarely, if ever, seeing anyone from the play team during their child’s admission:
I didn’t even know who they were until near the end. I think maybe there might be assumptions, no, maybe not. I don’t know whether they thought there’s not much they could do with him, I don’t know, but for whatever reason, he didn’t have access to that, and I didn’t really know about that.
The feeling that play staff were either not willing or not capable to support their child was also expressed:
I think they spend more time with children who can communicate . . . I don’t think they know what they’re doing with disabled children. I don’t think they have that skill. They are play specialists, so they’re great at thinking about distraction, and managing operations . . . but not one of those play team seem to have a disability hat on.
The perception of some parents was that children with LD did not seem to matter as much to staff or get as much attention, either because they could not speak or because other children were noisier or interacted more, which left children with LD feeling left out and hence bored. The issue of availability of play resources was raised by some parents, who described the need for a greater range of specialist and age-related toys and sensory equipment, whereas others said they had no idea what or who was available, or that toys were locked away outside regular hours and play specialists did not work at the weekends. One mother responded by buying sensory equipment for the ward to keep, although this was said to have been out of action for 8 months. This child’s parents went on to say that offering a slightly personalised play service would enable her child to be distracted, helping to aid her child’s recovery and allow her to go home more quickly, ultimately saving money.
Parents of children without LD also highlighted school and play as some of the positive aspects of care in hospital. They saw significant benefits for their child from these interventions when they occurred. However, similar to accounts from parents of children with LD, access was variable. Admissions over a weekend often meant that play staff were not available, and what was available on the ward was often not ‘age-appropriate’. For many of the parents, both of children with LD and of children without, the lack of activities for older children was consistently highlighted. Access to a television and/or Wi-Fi for iPad or tablet use was clearly important. Although a few parents talked positively about what was available, many raised issues about availability, working order and/or financial cost to parents. It was also noted that links between hospitals and local schools were not always made.
An account from a parent diary (child with LD) and a quotation from a parent interview (child without LD) highlight again that, in both groups, inequalities exists:
Disappointed that the play team did not visit earlier in his stay as we never knew about the play cupboard with jigsaw’s/games. He was introduced to the Teen room to play on Xbox [Microsoft Corporation] on the last 2 days. If told earlier then maybe mood/behaviour would have changed.
The play therapist tried very hard . . . but they just have criteria to fill . . . you were there for one reason and one reason only and they couldn’t consider anything else because they were under pressure . . . they tried. . .
A summary of the barriers to and facilitators of the particular needs of children with LD being met are shown in Figure 14.
FIGURE 14.
Perceived barriers to and facilitators of meeting the needs of children with LD in hospital (parent interviews) (RQ1).

The physical and sensory environment had a significant impact on the delivery of care for children with LD, as well as the equipment and resources available to staff (Figure 15). Many parents described challenges with the space within hospitals for utilising and storing the myriad of equipment their child often required, in particular wheelchairs and hoists. Some described the space as too small or inaccessible. Examples were provided of children being unable to access a special needs bathroom because it was being used as a storage cupboard, of wheelchairs being stored in a ‘filthy’ toilet and of children in wheelchairs being unable to access the sensory room or the facilities in the playroom:
The table wasn’t the right height for the wheelchair to get underneath, and there were no, kind of, lap trays to put anything on. We had to improvise for weeks.
FIGURE 15.
Perceived barriers to and facilitators of children with LD being cared for in the right environment, with the right equipment and resources (parent interviews) (RQ1).
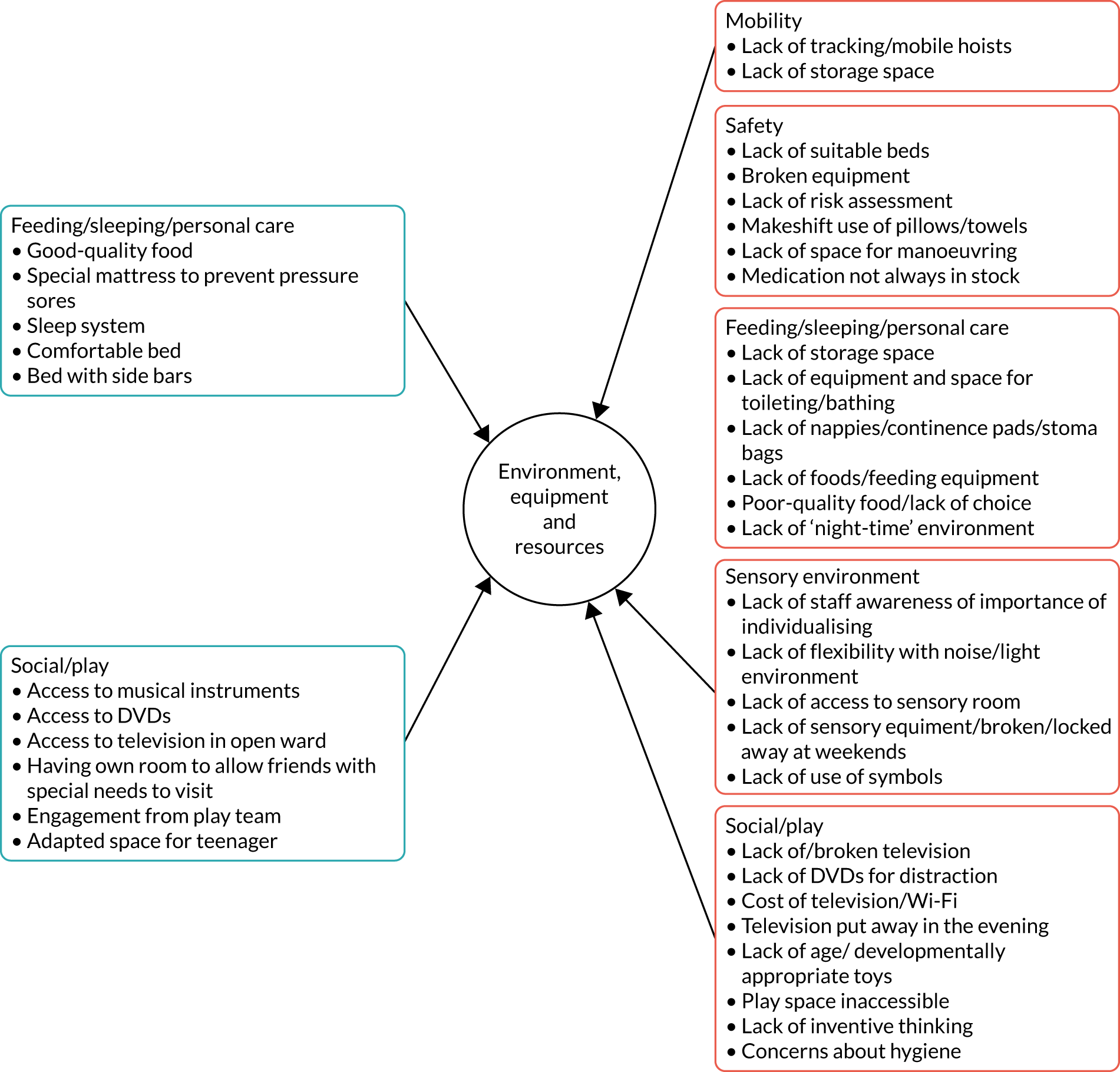
Numerous parents felt that consideration should be given to the bed space allocated to children with LD, with one mother describing the challenges of manoeuvring her daughter’s hoist and wheelchair in an open ward without causing disruption to other patients. In some cases lack of space clearly presented a safety concern, with one parent tripping over a mobile hoist on more than one occasion and another describing therapists ‘having to weave in and out’ [of the equipment], which was ‘almost a laugh but not really funny and not safe’. One parent highlighted how poorly designed hospital waiting areas could be for patients with wheelchairs because the corridor seating was fixed. She explained that every time another patient came down the hospital corridor she had to push her son in his wheelchair to the end of the corridor and back to let them through. Another parent, whose son’s wheelchair had to be stored in the disabled bathroom, described the anxiety he experienced from not being able to actually see it.
Similar to staff, many parents reported a lack of available equipment for lifting or mobilising their child, mostly in relation to ceiling track or mobile hoists. As a result, one mother who had an existing injury felt that she had no option but to manually lift her child. In a number of cases, a lack of hoists was felt to compromise the child’s dignity and/or privacy, for example because they had to have lots of bed baths instead of a shower. Many parents mentioned challenges associated with bathing or showering their child with LD: one parent described how they had to use a bathroom on a different ward because the bath on their ward was inaccessible. The importance of maintaining privacy and dignity was also raised in relation to the provision of personal care to children with LD, especially teenagers, with some parents feeling strongly that they should be offered a cubicle as a result:
Nobody else can walk in, watching them get changed . . . other kids can go to the toilet . . . and can walk round to their showers. Whereas I couldn’t shower her and just wrap a towel around her in the bath seat and then run her round to her room . . . they should have put a hoist in their own room . . . if my brother’s here and he’s sat in there changing her, she doesn’t like it, she’ll whinge.
Related issues that parents raised included their child with LD not being able to be hoisted up to look out of the window and other parents in an open bay complaining about the noise their child made or continuing to look in at them. One parent talked positively about being given a cubicle so that she did not have to deal with her son/daughter’s behaviours of concern in front of other people. In the main, cubicles were valued when they were offered, including to facilitate a child’s disabled school friends visiting. Despite cubicles being favoured, a number of parents did highlight the downside that this usually meant that their child was not visible to nursing staff, which made it even harder for the parent to leave the child for even a short time, an issue also raised by some nursing staff.
As well as having an impact on dignity, a lack of equipment had the potential to compromise the parent’s physical well-being and the child’s safety:
I said, ‘Oh, can we have the hoist? [Child’s] not very happy. I think she’s soiled her pad.’ They said, ‘Oh, it’s in use at the minute.’ I said, ‘Roughly how long is it likely to be?’ She said, ‘Oh, I don’t know, 20, 30 minutes’ . . . [Child] was absolutely apoplectic . . . In the end, with my injury I just had to lift her and move her onto the bed. I mean that’s not safe at all.
Nearly one-quarter of parents reported safety issues associated with hospital beds, primarily the risk of their child becoming trapped in the sidebars, as well as hurting themselves (see Chapter 9). Strategies were sometimes used to minimise risk, but these tended to be ‘makeshift’ and improvised based on what was available, rather than planned to use purposefully designed resources (parent quotation 9; see Appendix 9).
Another parent noted in her diary: ‘They always don’t have enough padding . . . on Wednesday there was only padding on one side. I have to cover the sides with blankets.’ One mother went as far as to sleep in the hospital bed with her child to prevent him from becoming stuck. Reference was also made to the makeshift use of pillows for positioning, as well as to the lack of suitable chairs for children with LD, which resulted in them spending excess time in bed. A small number of parents spoke positively about the provision of specialist air beds/mattresses. However, these could deflate and proved challenging when changing incontinence pads. In terms of tailor-made beds, one parent highlighted the lack of access these allowed for feeding tubes and intravenous lines, rendering them impractical and unsafe for her child after an operation.
Feeding equipment was discussed by several parents, and examples were given of them taking in their own feeding pumps, drinking cups and spoons, or improvising with what was available. Feeding sets were also reported to be incompatible with the available backpacks, and mobile feeding packs were provided only just prior to the child’s discharge. A small number of parents also described making up their child’s feeds at home and bringing them into hospital, which could be difficult for them to manage, including severely compromising their sleep. A reliance on parents to bring supplies into hospital for their child with LD was particularly evident in relation to nappies/incontinence pads. One parent described the challenges her husband faced when bringing in multiple supplies on public transport:
Taking a sibling on the train that’s ASD [autistic spectrum disorder], noise sensitive . . . clean clothes for [child] and me, [child] was going through 10 nappies a day when he was in, plus bringing a week’s supply of milk at three cartons a day.
One of the biggest issues with the hospital ward environment was noise and light, which were particular issues for children with epilepsy, whose seizures could be triggered by such factors:
There was one HCA [health-care assistant] who came to do his obs [observations] in the night. I know she didn’t turn the lights on, but what she did do is shine her torch right in his eyes, you know, but she hadn’t turned the lights on, so that was all right? It’s all light, not the light. So, it’s those misinterpretations.
The lack of attention seemingly paid to the sensory environment was highlighted by many parents, who talked about the noise of bins closing, taps running, doors banging, staff talking and babies crying.
Some parents of children without LD also identified situations in which the hospital environment was unconducive to their children’s emotional well-being. Teenagers, for example, could find it difficult being in a bay with babies, which kept them awake at night. One child found it particularly distressing being nil by mouth on a ward when they were surrounded by children with different issues around food such as anorexia and diabetes; they constantly had to hear discussions about food plans and smell food as it was brought to the ward. Similar to parents of children with LD, cubicles were largely valued, and some children were reported to be ‘over the moon’ at being moved to one. However, as another parent pointed out, the use of cubicles could also lead to children feeling isolated. In some cases, parents could manage situations of psychological distress by advocating for earlier discharge home: ‘In the end [child] said, “I’ve got to go home. You have to get me out of here today because I can’t stay another night”’.
For children without LD whose mobility was impacted, toileting provision and help with moving were also highlighted as poor, and ambulant children experienced equipment and resource shortages that had a negative impact on their hospital stay. This is highlighted particularly well by the example of a child with ADHD and a bowel condition whose dignity and privacy were compromised by not having access to her own toilet. She was further debilitated by a broken drip stand. The noise, lighting and clinical interventions on a ward could also be problematic, particularly at night, with one parent citing the difficulties of being constantly aware of and alert to how much noise they were making and thinking of others on the ward. However, for those with LD whose emotional and physical health was particularly fragile, these issues had a greater impact, as related in the following quotation from a parent diary:
He also due to his disabilities has sound sensitives and struggles/gets stressed with unpredictable noises. So, gets stressed unhappy with infusion pump alarms, monitor alarms, and other children crying . . . much more awareness is needed by staff as to the difficulties that children with special needs and autism have with changes of environments.
Are children with and children without learning disability and their families equally involved as active partners in their treatment, care and services (research question 3)?
There is widespread commitment to family-centred care as the most appropriate model for the care of hospitalised children. 95,96 However, health-care professionals take family-centred care to mean different things or are unclear about what it implies and requires,97,98 which means that putting it into practice can be variable. At its core, however, is ‘involvement’, and we sought to look at this in relation to all children and parents.
Involvement of children with learning disability
Discussion about engaging directly with children, and involving them, revealed a number of barriers. Lack of time was seen as a particular barrier to staff fully engaging with children with LD, as was a lack of awareness of some of the issues related to communication, as in the following quotation:
In front of [child], nurse told children didn’t have to go to school on discharge – therefore [child] didn’t want to go to school!
The need for greater attention to be paid to the communication needs of children with LD was often mentioned:
If they wanted to accommodate special needs children, they could easily have picture symbols. [Child] can’t read, so, obviously I was telling him all his choices and then he was picking. For a special needs child, that is an area I guess that they’re not accommodating.
However, some parents of children with profound and multiple LD reported that the nature of their child’s LD was such that the involvement of their child in any aspect of their care and treatment was always going to be limited.
One mother went as far as to suggest that because her child ‘has special needs and cannot speak’ sometimes ‘decisions were forced on her’. Other parents explicitly felt that staff treated their child differently from children without LD, in the sense that ‘staff just look and see disabled and think he wouldn’t know, when he does’.
Parents had various perceptions of the way that staff interacted with their child and the extent to which staff involved their child. Some positively described staff talking directly to their child, informing them who they were and explaining beforehand the things they were going to do. They talked about the tone some staff adopted, for example sounding gentle or calming, using laughter and ‘banter’, or speaking like a friend, which one mother said helped to make her child feel at home. Staff being kind and friendly was also described. Some parents also commented positively on nurses being patient with their child, taking the time to answer their questions. The benefit of the same staff being allocated to care for their child during the same admission or across admissions was highlighted once again; one parent explained how interactions and explanations improved as staff became more familiar with her child and another indicated that staff who knew her child were more relaxed with him. Another parent described at length the different experiences she had with individual staff on different admissions, from some ignoring her son to others being fully engaged:
She spoke to him, not just me. She spoke with him. When she was checking his obs and everything she was explaining to him . . . she was saying, ‘You’re a smiler, you are’ . . . it was like she’s getting the job done but at the same point she treated him like he was a typical little boy. We both made comments, how he smiles with his eyes and everything.
Despite positive examples of staff being kind and friendly in their interactions with children with LD, when involvement occurred it tended to be limited to giving simple explanations and answering questions, rather than involving children actively in making any decisions (where they had the capacity for this). One clear example was a child of 12 years who had been involved in whether or not to have surgery on the basis that she was ‘of sound mind’, but her parent did not feel that this had been handled well. The parent explained that the anaesthetist had revisited this decision on the morning of the surgery, which was particularly unhelpful because as soon as her daughter had been given the choice of going home she was never going to want to stay, irrespective of what she had agreed to beforehand. Approximately equal numbers of parents reflected negatively on the way that some staff interacted with their child, with many describing their child being ignored or talked over, even in situations when they ‘like being spoken to’ or ‘could answer’ for themselves. One parent subsequently described their child being petrified, and another said that talking inappropriately in front of her daughter with severe cerebral palsy makes her daughter ‘feel like she is taken on a rollercoaster ride’. She went on to explain further:
The doctors certainly talk to the grown-ups and don’t really address the children, and I think because of child’s physicality, a lot of people don’t know how much she understands. We have had other appointments with doctors who’ve said some quite inappropriate things about, you know, potential operations, things that will need to be further down the line, that she really didn’t need to go into graphic detail.
This parent shared what her daughter had requested in her annual review:
One of the things that she’d like grown-ups, in general, to do more of is tell her what they’re going to do before they do it. I think there is that assumption with her that they come in and go, ‘Right, we’ll just put you on the pump,’ or, ‘We’ll just do this with your dressing,’ and no-one actually says, ‘All right [child], what we’re going to have to do is-,’ and explain it as they’re going along . . . explain how it might make her feel, explain, you know, how long it might take before they do it.
There were further examples in the context of care provision of staff ‘doing things’ to children with LD, including taking blood and removing a nasogastric tube, without any discussion or preparation and without recognising the child as an agent:
To start with, when they were taking his temperature and his blood pressure and that, they weren’t saying, ‘Hi, I’m going to put this to your ear, but this will be taking your temperature. It’s going to do a bit of a beep,’ . . . It was literally just being done to start with, which is pretty ignorant . . . It’s not how we’d be treated so I don’t think he should have been.
It’s about treating her as a person . . . she’s got a right to that and we expect it for her. You’re not suddenly pulling her, because she’s heard a conversation between me and you . . . that’s going to come as a shock . . . I think they do need to start realising that they are still individuals, no matter what the disability, and start learning the skill set that goes with that, then I think you will get better results.
The variability with which different nurses interacted with their child was highlighted:
It depends on personality of the nurses. Some of them will say, ‘Hello, how are you?’ ‘Fine.’ ‘I’m going to attach you to the machine.’ Very professional. It just stays that. Basically, some nurses see me there, so they’ll see me, and they won’t take him as an individual. They’re doing their job, just telling him, ‘I’m attaching you to the line,’ and ‘It’s finished.’ Talking to mum, what’s happening. You understand? There are other nurses who love him, and they will speak to him as an individual. That’s what I want for him. He is an individual. So, they will talk to him. ‘How are you? What are you doing? What are you drawing?’ That’s very few.
Parents of children without LD highlighted staff who listened and understood their child, rather than imposed a plan. Seeking out the child’s view, listening to the child as part of providing personalised care was highly valued, when it occurred. Parents used their own presence in hospital (sometimes extending the period of time they stayed) to mitigate a lack of effective individualised communication with their child. For children without LD but who had additional learning needs, their involvement in their care was equally compromised when adjustments were not made, and their suggestions were not listened to:
Considering his learning style, I said if you could get a teddy or a doll, and put some cages on it, and show how its going to work, demonstrate with and he could copy his teddy . . . it didn’t happen, I don’t know if they didn’t have the time, or it was something they couldn’t physically do or won’t do, I’m not sure. It didn’t go anywhere.
The involvement of parents of children with learning disability
Three times as many parents described their experience of working in partnership with staff as being entirely negative as those who described their experience as being entirely positive. Most parents described a mix of feelings about their involvement. Facilitators of feeling involved as a partner in their child’s care were being listened to and respected, being kept informed, and being included and involved in decisions about their child’s care, as well as being able to negotiate their role. In terms of their involvement, parents described various aspects of what they did for their child, including practical care. Sometimes this was welcomed by parents, who wanted control over the quality and timing of care, who wanted something to do or who felt that it was simply part of their parenting role:
We administered his medication and did his personal care, as I say, mainly for something to do, because we do it every day anyway. It is very time-consuming. I would have felt slightly embarrassed sitting reading a magazine in [child’s] room while a nurse sat there for an hour slowly giving him his medication, although they were always there to do it if we needed them to. They were happy for us to do whatever level of care for him we wanted to, but they were also happy to take over at any point.
Parents advocating on behalf of their child, and being their voice, especially for those children unable to communicate for themselves, was frequently described. For some parents, however, a sense of responsibility and being relied on by staff reinforced feelings that they were expected to provide care or stay by their child’s bedside, for example implicitly by not realising that leaving ‘was even an option’ or explicitly through signs on the ward informing them they were ‘not allowed to leave’. Another said that she had been given the impression that the nurses would have done more for her child and prioritised his care had she not been present, and another talked about feeling pressure not to be gone for long if she did leave. Sometimes, knowing the family well could lead staff to assume that a parent would adopt certain responsibilities during every admission:
The one I get is, ‘You know what you’re doing because you do it all anyway, don’t you?’ They don’t ask any more. They assume. Most of the time, as I’ve said, I would rather do it myself. When he’s really poorly and really tired, sometimes I do need them to say, ‘I’ll do those meds if you want’ . . . it would be nice, just given the context of where we’re at, for them to observe us both . . . ‘I’ll do that,’ rather than me having to, again, ask and say, ‘I’m really tired. I’m really stressed. I’m worried. I’m upset. Can you do that?’
Again, it was apparent that a single negative incident could have a long-lasting impact on parents’ future decisions about the care of their child:
Our consultant said that we could have a play specialist to sit with him/her . . . the sister in charge made out that we’d asked for a play specialist to be with them 24/7 . . . It was a shame because some of the staff there were fantastic. It was just that one experience that just put us off completely.
In terms of being listened to, one parent reflected positively on how staff had changed their attitude towards her over time, saying ‘In the early days, we had a lot of upsetting experiences . . . with nurses or doctors thinking that they knew it all’. She described her child’s new consultant as fantastic: ‘she’s even written in his education and health-care plan that the parents are to be, kind of, consulted at every stage with child’s care’. The relationship that this parent had with staff from her local non-children’s hospital, compared with the relationship that she had had with those at the specialist children’s hospital further away, was described:
Every ward we’ve been on at [children’s hospital] has been lacking in that . . . that emotional side of being a nurse, showing care and compassion . . . at [local hospital] they put a lot of emphasis on that kind of relationship building with the parents as well.
By contrast, however, another parent spoke highly of staff from a specialist children’s hospital, including her child’s consultant paediatric neurologist, who had said to her, ‘A mother always right. You know the child . . . You’re not paranoid and don’t consider yourself paranoid . . . That gave me a lot of confidence’. The nursing staff were also praised for the way they negotiated aspects of care, for example in relation who would administer her child’s medication:
I wouldn’t like it different. It was just perfect. Neither too much, neither too little.
Honestly, they let you choose . . . and not make you feel guilty.
The following quotation from the mother of a child with profound and multiple LD who had been admitted to a non-children’s hospital highlights particularly well parents’ views on what it means to be a partner in their child’s care:
I feel that we have the respect of the doctors and consultants . . . they listen to us . . . they put trust in our knowledge of [child] . . . They don’t hesitate to ask our opinion . . . and have acted on requests that we’ve made. I definitely feel that we’re right alongside them. I’m also impressed how much the doctors listen to the nurses who have been caring for him. There’s no hierarchy. They are very open to discussion, and never rush us.
However, nearly every parent of children with LD described numerous barriers to feeling involved as partners in their child’s care, many of which exactly mirrored the facilitators described above, such as feeling uninformed, not listened to or respected and not involved in decisions. Not being in control, valued or believed were other descriptions provided. Furthermore, doctors were seen by some parents to be either inaccessible or disengaged, giving the sense that they ‘can’t be bothered’, and nurses were often described as rushed and busy:
Care was like what we have to do at home. The only thing that they did was the obs and the meds. Apart from that, the rest of it is just done by the parents . . . I was quite happy with it because she was a little bit more comfortable with me doing it, rather than someone else . . . most of the time there’s no one to ask . . . you just get on and do it.
Parents described uncertainty, frustration, anxiety, anger, helplessness and invisibility, as well as a lack of trust from staff, with one parent describing feeling like a convict:
Paediatric doctor in the hospital, the way she was speaking to me as if I’m the convicted prisoner, and she’s the jailer officer. I have no say. She really behaved very rudely with me, very badly, as if she’s not my child, I’ve got no right on her.
Additional barriers were a lack of consistency, communication, co-ordination and collaboration between individuals and teams:
It was very confusing because everybody had different ideas about what intervention was needed. The communication between them wasn’t clear . . . we were stuck in the middle, [child] was the one struggling on the bed . . . Myself and my husband were begging them to intubate . . . They just said, ‘I hear what you’re saying, but I’m not going to change my mind.’ . . . He was seizing, he was in a dystonic storm, he was in an awful amount of pain. Just it was the most distressing thing I’ve ever seen.
This mother went on to say that a few hours later the crash team had to be called as her son’s lung had collapsed and he required immediate intubation. Her feeling that the unique knowledge she had about her son was often ignored by staff is highlighted in the following quotation:
That’s it, an expert in my own child . . . I am child’s interpreter. I’m telling them all the time, but they’re not listening . . . you go away thinking about it and playing on it in your mind . . . feeling useless and just feeling exhausted by it all, because I knew what he needed, but it wasn’t being taken on board.
She explained that there were numerous situations that could have been avoided had her opinion been valued, and she later questioned whether or not doctors felt threatened by her. Parents’ perception of the distinction between the individual-level knowledge (idiographic) that parents hold about their children with LD and the group-level knowledge (nomothetic) staff hold about children with LD in general is epitomised in the following quotation:
We know that you guys are the ones that have gone through these years of training, you’ve got years of experience dealing with medical fields, but this is our child and we’ve known her every single day of her life since. We know that something is not right . . . because we’ve seen these similar symptoms before. You’ve seen her for 5 minutes. We would like you to take our advice on board a bit.
Another barrier to parental involvement was not being properly informed, which could be due to the timing or to the way that information is shared (or not shared) with parents:
You’ve just got this big group of consultants coming around and there isn’t anybody that really explains or stops and says, ‘Look, this is what we did’ . . . we’re trying to grasp for that bit more time, you know, they’re walking off and we’re still heckling them for questions and answers.
The extent to which this parent lacked information about her child’s hip surgery is highlighted in the following quotation:
When we took her down for an X-ray, she’s just got this really big piece of metal in her femur and her hip and we didn’t know they were going to be putting the metalwork in.
This parent went on to describe the different sense of involvement she had felt in relation to staff at another hospital and questioned whether the complexity of her child’s surgery accounted for the difference in attitude:
They just could not have been any better. Everything about that service up there, we did feel valued as parents and we did feel as if our opinion mattered, but I suppose, because she’d had such complex surgery maybe they did approach parents differently. I suppose, when we’re looking at [child] having hip dislocations, it’s very different to open-heart surgery, isn’t it?
Parents of children without LD described how they had become highly skilled over time as their knowledge grew and they applied that to how they knew their child usually responded. Parents expected to take the responsibility for meeting their child’s physical care needs in hospital, including those that arose as a result of their child’s clinical condition (e.g. enteral feeding). However, some parents were surprised by this, but when they realised what was required, they took on the role of a carer in hospital. During longer admissions, parents articulated the impact that this role had on their own well-being. Some had not known that this would be expected of them. This expectation of this parental role was not always described in such a positive way, as with this parent of a child without LD in her diary said:
Biggest thing??????? Is the need for parents effectively to act as a surrogate nurse to ensure she gets what she needs. This is OK and understood, but would have been better to have had explained earlier to allow prep.
Parents had a range of views in relation to the staff listening to their concerns and consulting them – in the cases they felt listened to and a responsibility to voice their child’s wishes alongside their own views. There were examples of parents feeling that they were working as a team with some health-care professionals. The barriers to and facilitators of children with LD and their parents feeling involved as partners in their care are shown in Figure 16.
FIGURE 16.
Perceived barriers to and facilitators of involving children with LD and their parents as partners in their care (parent interviews) (RQ3).
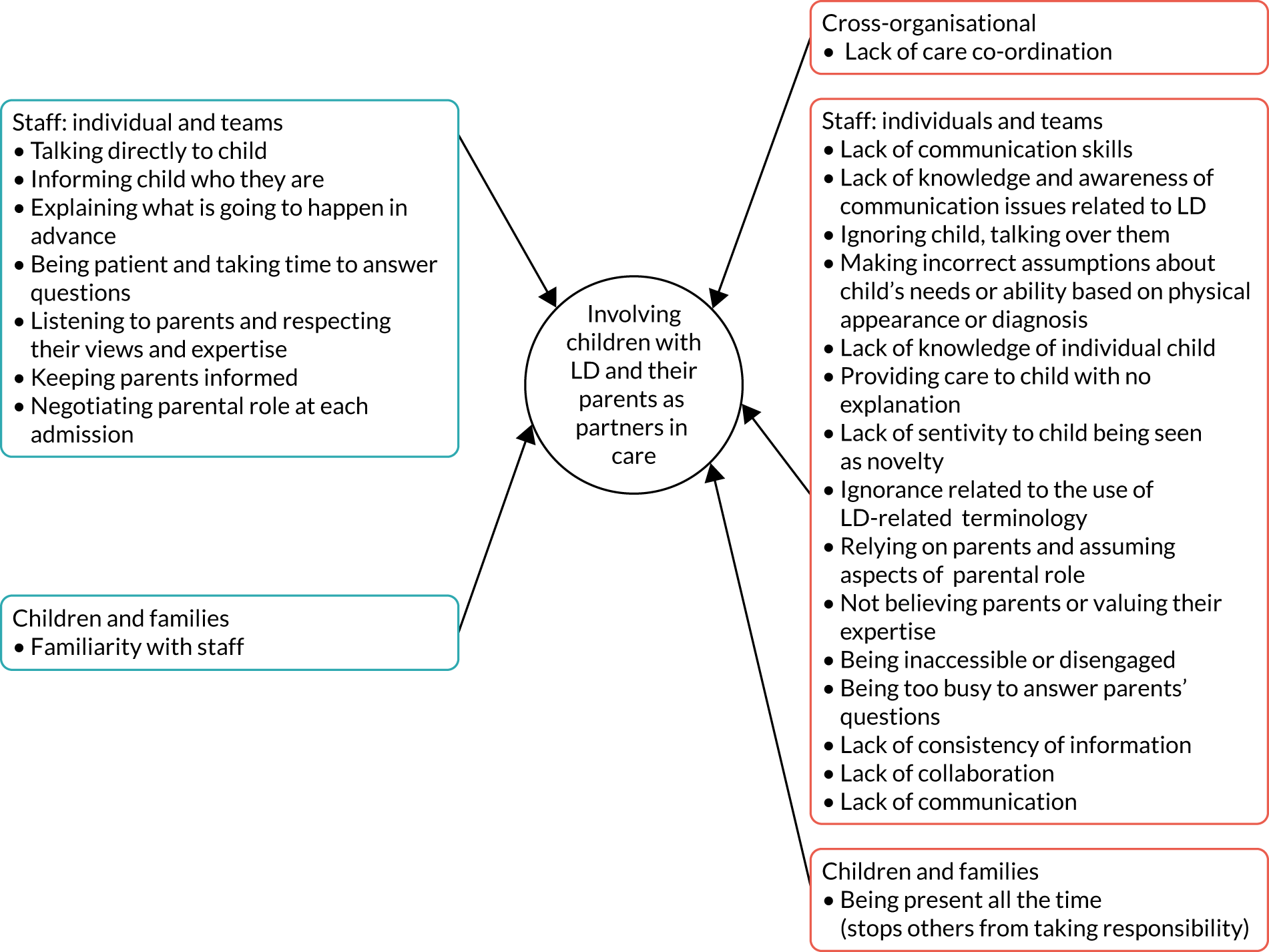
Chapter 9 Parents’ safety concerns
Drawing on data collected from home interviews and the safety review form, this chapter focuses on parents’ safety concerns and the impact that such concerns had on their health and well-being. Also included are parents’ views about the complaints process. In conjunction with the safety issues related to the environment described in Chapter 8, the evidence presented contributes to answering RQ5, concerning whether or not the safety concerns of parents of children with and those of parents of children without LD are the same.
Parent interviews
The majority of parents of children with LD described having concerns about their child’s safety while in hospital, which prevented them from leaving their child’s bedside unless this was absolutely necessary. Sometimes this was limited to when the child was asleep, and sometimes not even then. An understanding of their child’s increased vulnerability resulted in parents feeling that they needed to be constantly vigilant:
I can’t leave her, she’s got a learning disability and she’s too vulnerable for me to leave, I just can’t. I’ve never left her, I can’t do it, it’s not an option.
This was the case even for a child in intensive care who had 24-hour supervision, with the parent leaving the bedside only when the child was asleep and being cared for by a nurse ‘that I knew would call me or knew child well enough to know what she’d need’.
A number of factors facilitated parents feeling that they could leave their child’s bedside even if they did not choose to, including being supported and encouraged to have a break:
I could have gone home and come back again and cooked a pot of food if I wanted. They were really supportive. I think they would encourage you to take a break, to go outside, to have a break, to rest, to have a coffee or just go out, breathe air.
Absolutely key to instilling confidence in parents was feeling able to trust staff to stay with their child while they were gone:
They’d say, ‘Yes, we’ll watch her’. I’d come back and, nine times out of ten, either the play nurse would be with her, just talking because she was quite happy, or the nurses would be stood at the end talking and chatting to her.
The promise nurses frequently gave of ‘keeping an eye’ on their child was often not good enough for parents, who felt that nothing short of constant supervision was needed. If parents did choose to leave, then staff reporting back how their child had been during that time was important, including any care that had been provided. Parents reflected on experiences, from the current or previous admission, of leaving their child briefly and coming back to find that they were unsupervised or in potentially dangerous situations, reinforcing concerns about trusting staff to keep their child safe:
He was literally hanging out the bed and there were three nurses stood about 3 m away from him, all stood there chatting . . . I am scared of that happening again because next time, it could be more serious. He could get his neck trapped . . .
Keeping the child safe meant knowing what to do in the context of each child:
We left him with three nurses while we went to make a cup of coffee, he came back and he’d stripped off all his clothes and his nappy, and he’s stood there weeing on the floor while there’s three nurses just stood watching.
Parents were concerned about not only physical harm but also emotional well-being; being alone in an unfamiliar environment could cause the child distress:
For him to be in a strange environment is one thing, but to be in an environment that he doesn’t know, with people he doesn’t know, and no-one to soothe him, it can make anything worse . . . Nobody can really take over, that period that you’re there, so, it’s nice that they offer, but the reality is that they can’t do anything.
A delicate balance was described in managing the physical and the emotional well-being of children with LD, whose need for routine and familiarity can be an important feature in an assessment of their risk. Many parents highlighted the increased vulnerability that came from their child being unable to communicate, which precluded the child asking for help but also meant that they were not able to express their needs and wishes or say if anything was wrong. For many, their child’s inability to recognise risk or manage their own safety made them particularly vulnerable to injury and harm (parent quotation 10; see Appendix 9). One mother mentioned her daughter’s inability to recognise when it was and was not appropriate for people to examine her, because ‘she hasn’t got that full understanding . . . she will trust them to do whatever they want’:
When they say, ‘You can leave him,’ but you can’t. I was trying to think how it would be if it was one of my other children. I wouldn’t want to leave them either, but at least if I had to leave them, I’d know that they can ask for what they need. If they want to talk to somebody, they can make a phone call. They can communicate, so it just isn’t an option to leave him somewhere where he doesn’t know anybody.
The numbers of nursing staff on shift and perceived level of ‘busyness’ was another factor in parents’ decision about whether or not to leave their child’s bedside. The level of monitoring some children received in hospital could be less than they had at home, with one-to-one care and the use of cameras described. As one parent, whose child was blind and had severe epilepsy, pointed out, ‘why would we risk walking off, no camera on her, when the nurse is too busy?’. A suggestion was to have trained volunteers available to sit with children with LD, helping instil confidence in parents to leave. This parent went on to say that having a break for an hour would ‘mean the world’.
Parents’ sense of trust was influenced by the care of other children they witnessed on the ward:
He [other patient] had his tube in but he was still being fed. His mum had to take a call and she had asked the nurse to keep an eye on him . . . the nurse had to attend to something quickly, and while she was on the phone, he was climbing out of his bed, and trying to walk away.
This was not reported as something that happened frequently during admissions or indeed during every admission, but one incident of poor care or a near miss could have an impact on parental trust for all future admissions. In some cases, parents reported that this impact was felt even years later.
Trust and the need for vigilance were also described by parents of children without LD; they described their responsibility as a continuum of vigilance, which differed in nature and intensity to the constant sense of heightened vigilance described by parents of children with LD. Their confidence in leaving their child for any period of time was influenced by their trust in hospital staff to both provide adequate care and ensure parental involvement in decision-making. Their decision was not always associated with safety, as was primarily the case for parents of children with LD, but leaving a child who was anxious: ‘I don’t think I would ever do that’. Trust was sometimes about the whole hospital or unit or, as with parents of children with LD, limited to specific staff members’ presence and an overall sense of the quality of the care being provided to their child:
It depends who’s taking care of [child] that day because they are people doing the job by the book . . . sometimes I know from the first point in the morning that on that day I will have to be watching like a meerkat to go and get the medication at 2 o’clock, to ring the buzzer or something to make kind of waves like, ‘we are here’.
For example, a mother of a 13-year-old said, ‘If I had to fly to Australia I would leave her at the [non-children’s hospital] all day long . . . I wouldn’t trust them [children’s hospital] as far as I could throw them’. Presence meant that parents often chose to stay overnight with their children and also at particular times of the day, such as meal times. This was either because their child would be reluctant to ask for assistance or related to the stability of their condition. On the whole, parents were more confident about leaving older children, with a mobile phone providing a sense of security and a safety net for communication. This increasing confidence had evolved over the time of the child’s illness trajectory. Many children had been diagnosed with their long-term condition at an early age, and, over time, their parents’ confidence had grown, reflected in parents’ willingness to leave their child for long periods of the day and night. Other factors that facilitated parents’ decisions to leave their child were being in a hospital that was relatively close to their home, the health status of their child improving, and trusting staff to contact them if there were any changes and/or providing updates on their return.
As previously mentioned, in a small number of examples a lack of attention to the child’s view had had a highly significant impact on the child’s hospital admission, including on their treatment success, length of stay and emotional well-being. As with parents of children with LD, previous experiences of poor care led to parents choosing to be present during the majority of their child’s hospitalisation. This presence provided a further safety check, or if there was a trusted member of staff to either prevent errors or their recurrence then they would feel confident to leave their child, knowing their child would be safe. Trust in staff was crucial to all parents. The perceived barriers to and facilitators of the safety of children with LD in hospital are shown in Figure 17.
FIGURE 17.
Perceived barriers to and facilitators of children with LD being safe in hospital (parent interviews) (RQ5).
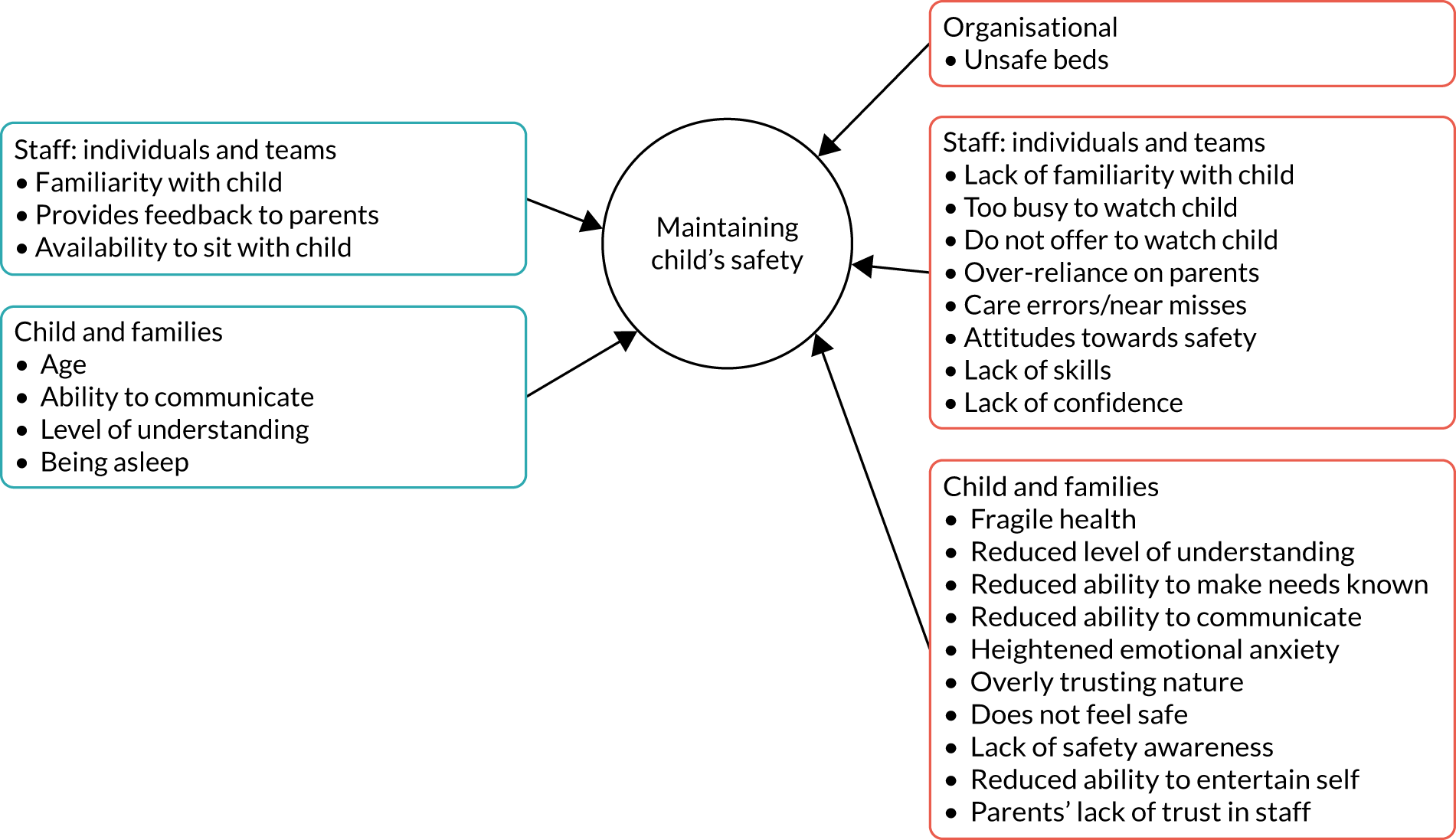
Safety review form
Thirty-two of the parents of children with LD (78%) and 14 of the parents of children without LD (67%) completed the safety review form, highlighting safety concerns or good practice in relation to six domains, including ‘other’. Their responses are captured in a visual individualised Likert display (VILD) (Figure 18) that enables comparisons to be drawn between parents of children with LD and parents of children without LD and between children’s hospitals and non-children’s hospitals.
FIGURE 18.
Visual representation of parents’ views about safety and good practice in relation to six safety domains.
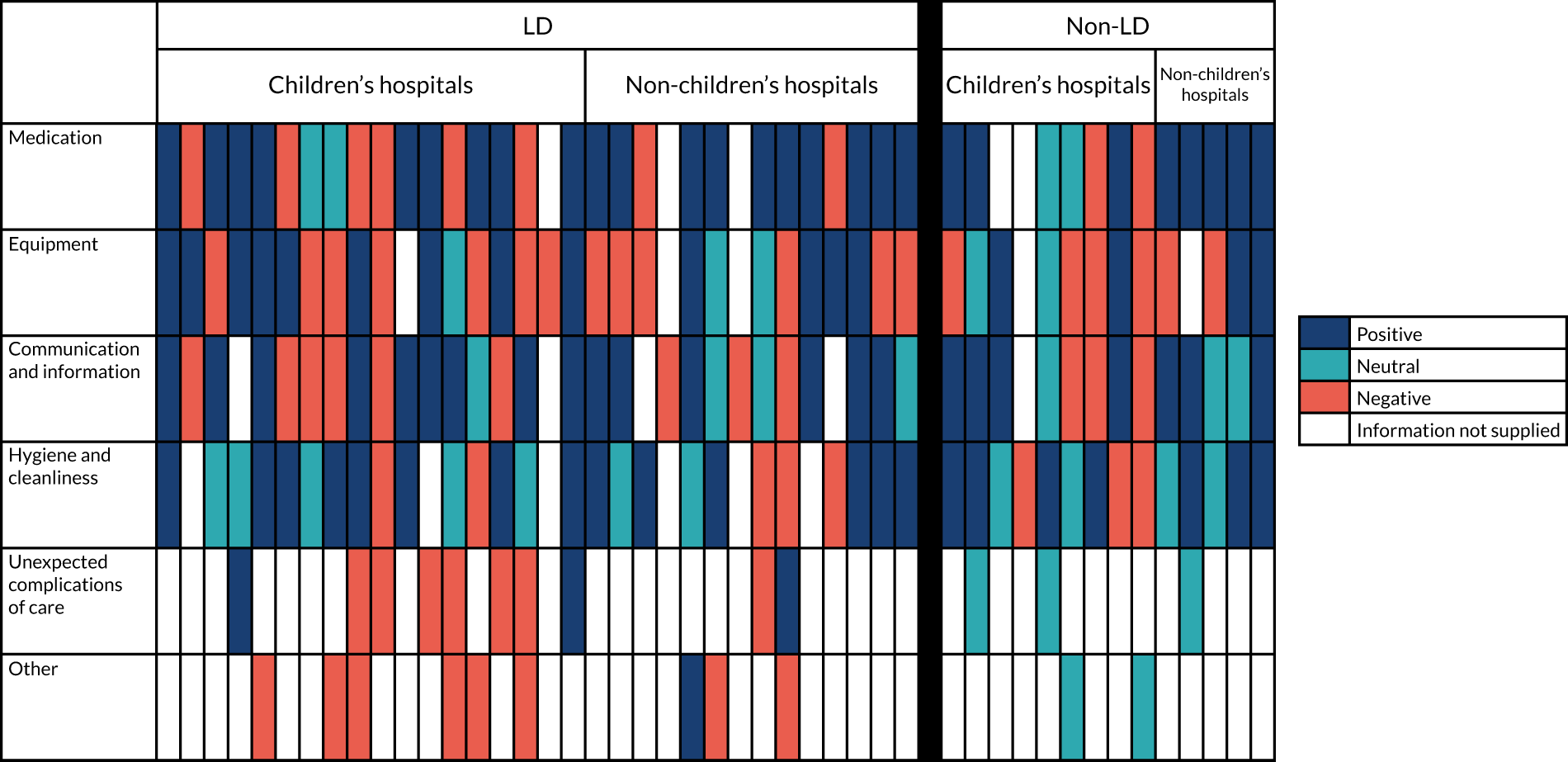
Starting with medication, the majority of comments from both parents of children with and parents of children without LD were positive. Parents valued being given control over the administration of their child’s medication, and, in cases where staff were in control, they were mostly vigilant in terms of checking the patient’s details, ensuring that the drug chart was signed and keeping medication locked away. Parents of children without LD referred to poor symptom management in relation to pain and vomiting; there was one incident of a child’s medication not being put back in the fridge when it was no longer needed. Parents of children with LD appeared to have more concerns with greater implications. There were two issues related to delayed epilepsy medication, which had the potential to have an impact on the control of seizures, as well as two near misses requiring parents to intervene to prevent an incorrect dosage and incorrect route of administration. Insufficient overnight feed was also described, as well as issues with the documentation of medication prior to discharge, hygiene and storage of medication on the ward. Parents in non-children’s hospitals expressed fewer concerns (11%) than parents in children’s hospitals (50%).
Equipment was a concern for both groups of parents, irrespective of whether they were in a children’s or non-children’s hospital. Space was generally a problem, and, in addition, some equipment/supplies were not available and staff lacked the confidence and capability to use the equipment. A number of comments were made about resources such as televisions, toys and games, and sockets being broken. Several concerns were expressed specifically about equipment not being suitable for children with LD, as well as a lack of staff awareness of this equipment, which support the findings reported in Chapter 8.
With regard to staff communication and the provision of information, approximately two-thirds of parents were positive, describing staff as friendly, accessible and honest. Several parents of children with and children without LD reported having things explained well, including to their child. Concerns were expressed, however, across a number of areas, including a lack of availability and trust in staff and poor communication between them; inconsistent or incomplete information; lack of privacy; and lack of follow-up. Several parents of children with LD felt that there was a lack of direct communication with their child. They reported that staff lacked understanding of their child’s needs, and this was also the case for the parent of a child who did not have LD but who had dyslexia.
Feedback about hygiene and cleanliness on the ward was mixed, with parents of children with and children without LD reporting both positively and negatively on the frequency, quality and timing of cleaning. There were no comments, positive or negative, that related specifically to a child’s LD or long-term condition, except in the case of one parent of a child with LD who commented on her daughter being left in soiled pads because of a lack of hoisting equipment.
In terms of unexpected complications of care, those reported were nearly all from parents of children with LD and mostly from those staying in children’s hospitals (see Figure 18), possibly reflecting the nature of the admission in those cases. Examples included the occurrence of pressure sores, infection, a lack of care co-ordination leading to repeated finger pricks for blood tests, cannula ‘tissuing’, multiple ward changes causing the child emotional distress and not being able to feed the child.
Nearly all of the ‘other’ issues raised were from parents of children with LD, and all but one of these were safety concerns rather than examples of good care. These included issues related to access to the hospital, staffing levels, vigilance in terms of people entering the ward and not feeling able to leave the child, night-time disturbances, privacy and handling by porters.
Chapter 10 Barriers to and facilitators of a timely, effective discharge
This chapter describes parents’ experience of their child’s discharge, as well as the views of community staff about the admission and discharge process and communication between the community and the hospital. The data presented contribute to answering RQ1 about equality of access to high-quality hospital care that meets the particular needs of children with and children without LD.
Parents’ experiences of discharge
Just under one-third of parents of children with LD described experiencing a timely/early discharge, making reference to medications and/or discharge letters being ready in time for them going home. One parent of a child with extremely complex needs positively described the role of a discharge co-ordinator in improving her experience of discharge. As noted in a parent diary, ‘We were told today that we would be discharged tomorrow . . . All the necessary plans were put in place to ensure that discharge would run smoothly’.
Just over half, however, described challenges that resulted in some form of delay; the main issue was medication, with some waiting as long as 5–6 hours for it and others leaving without the medication prescribed, sometimes with a plan to return for it later. It was apparent that once a child with LD has heard that they can go home, waiting to do so could become a real challenge for them and subsequently their parents. Several examples were described of a more extensive delay to the child’s discharge as a result of staff-related issues, such as doctors not being on the ward to sign the necessary forms, the relevant people being on annual leave or staff shortages during a bank holiday.
Other reasons for a delay included unexpected health-related complications as a result of a lack of preoperative preparation, and issues with community support, including conflict about who was responsible for the child’s package of care and equipment delays:
Had it been managed and planned as everybody would probably have wanted it to be, I think we probably could have been there for 2, maybe 3 weeks tops. Now, I feel like we’ve wasted everybody’s time and everybody’s wasted our time. Eight weeks bed-blocking isn’t right . . . we weren’t willing to go until we were sorted. We were just waiting.
In terms of parents feeling ready to go home, several positively described how they had been actively involved in the decision:
She said, ‘You can go if you feel like you can handle him at home,’ and then she did the, ‘Make sure you do come back up–’ He’s got open access so all I have to do is make a phone call and I can get him back up there.
Nursing staff checking in with parents prior to discharge and input from therapists were seen as helpful. Only one parent, whose child with LD required very complex care, referred to a discharge planning meeting. They spoke positively about having a clear plan of care including the necessary risk assessments.
One-quarter of parents felt that they had not been ready to go home when they did. A lack of warning or preparation was described, for example in relation to feeling equipped to provide the necessary care, having the necessary community support in place or being well informed, with an appropriate plan of care.
One parent reported feeling insecure and anxious about the responsibility she had for her child’s feeding regime at home, which she felt was handed over too quickly, compounded by inconsistent advice from the dietitian and other health-care professionals. Another parent described the discharge process as abrupt and traumatic, feeling that they had been kicked out when neither her nor her child was ready to leave. This was echoed by a parent who questioned the basis for her child being sent home:
I felt like they just turfed us out really, because he wasn’t coping, but I don’t know whether physically it was done for the right reasons. I understand mentally it was, but there needs to be some sort of, like, mix of the two.
Many parents talked about their experience of post-discharge follow-up, with numerous examples provided of things that went well and things that did not. Although some parents talked positively about appointments, equipment/supplies and community support being in place, others described these as absent.
Discharge letters were sometimes missing or lacking correct information; one parent reported that her child was unable to go back to school without this. A number of issues were reported in relation to changing dressings, with parents feeling uncertain about when bandages/stitches had to be removed, feeling left to arrange the dressing changes and not being sent home with any or enough dressings. There was a lot of criticism from parents of children with and parents of children without LD that postoperative community care for children who had undergone scoliosis surgery was non-existent.
Although some parents welcomed having a follow-up call and/or being given the details of someone to contact if they had any concerns, others felt left to get on with things and that they had to arrange their own community/hospital follow-up:
[Child] comes home in spica but we don’t really get any support, so we’re just, kind of, sent home to manage it . . . now I think we just accept it . . . we’ve asked for things such as changing tables because we have to change [child] on the floor . . . we’re just, kind of, left to manage that.
A number of children experienced complications following discharge that required community input or readmission to hospital, primarily as a result of pain, infection or breathing difficulties. Some parents felt well supported, with one doctor saying that perhaps the child had been discharged too early. Other parents, however, struggled to have their concerns realised by the hospital:
I called the ward . . . I said, ‘My daughter is having a high fever. I didn’t want my child to be discharged and now she’s discharged and she’s hardly eating any food,’ as in the hospital she was not eating and I was still discharged . . . He said, ‘We can’t do anything. You are discharged from here’.
Importantly, one parent who wanted reassurance following discharge said that, although she had known she could call the ward, she had not done so. A sense of not wanting to waste doctors’ time was also given.
These challenges were more or less the same for children without LD. Frequent delays were reported in children being discharged. The most likely cause was a delay in medications being ready. In hospitals that were more local to home parents managed this by electing to use their current supplies if there had been no changes or choosing to return to the ward later in the day to collect the medications. Lack of support in the community setting – home adaptations, community therapy and a continuing care package – was a further cause of delay to discharge for some children. Lack of transport to take the child home was also a challenge. On the whole, discharge remained variable, and it depended on staff putting in place processes and parents making sure that it was done in a timely way.
Community staff survey
Community staff were asked eight questions about preparation for admission, communication between the community and the hospital, and meeting needs and discharge in relation to children with and children without LD (Table 11). Overall, community staff reported that preparation of and communication about children with LD was poorer than it was for children without LD. Communication between community services and the hospital was reported to be poorer for children with LD before admission and at discharge (i.e. both from the community to the hospital and the hospital to the community). Communication between primary, secondary and tertiary care was also seen to be less effective and less timely when it was in relation to children with LD than when it was in relation to those without LD. Community staff did not perceive children with LD to be more likely to experience a delay in admission due to factors beyond their control than those without LD, but delays in discharge were seen to be more likely for those with LD. In terms of their own ability to meet the needs of children after hospital discharge, community staff felt less able to meet the needs of those with LD than those without LD.
| Individual questions | Children with LD (%) | Children without LD (%) | Comments | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 (SA) | 2 | 3 | 4 (SD) | 1 (SA) | 2 | 3 | 4 (SD) | ||
| In the community, CYP are always helped to prepare for their hospital admission | 6 | 33 | 48 | 13 | 9 | 40 | 43 | 9 | z = 4.00; p < 0.001 |
| Prior to admission, community services always share information with the hospital about the needs of the CYP | 8 | 32 | 47 | 13 | 8 | 40 | 40 | 12 | z = 3.05; p = 0.002 |
| Prior to discharge the hospital always shares information with community services about the needs of CYP | 5 | 27 | 46 | 23 | 6 | 31 | 49 | 15 | z = 4.17; p < 0.001 |
| I feel able to meet the needs of CYP after their hospital discharge | 9 | 48 | 35 | 8 | 13 | 53 | 29 | 5 | z = 3.63; p < 0.001 |
| Communication between primary care, secondary care and tertiary services about the needs of a CYP is always effective | 1 | 24 | 51 | 24 | 2 | 32 | 51 | 15 | z = 6.15; p < 0.001 |
| Communication between primary care, secondary care and tertiary services about the needs of a CYP is always timely | 1 | 23 | 53 | 23 | 2 | 27 | 53 | 18 | z = 3.60; p < 0.001 |
| VF | F | IF | N | VF | F | IF | N | ||
| Frequency of admission of a CYP to hospital being delayed because of factors beyond the family’s control | 5 | 44 | 50 | 0 | 2 | 48 | 49 | 2 | z = 1.94; p = 0.053 |
| Frequency of discharge of CYP from hospital delayed because of factors beyond the family’s control | 6 | 48 | 45 | 0 | 3 | 45 | 50 | 3 | z = 3.85; p < 0.001 |
This chapter has illustrated the highly variable experiences that parents have of their child’s discharge, with things seeming to go either very well or not at all well in terms of timeliness, feeling ready to go home and receiving follow-up community support. The range of barriers to and facilitators of a good discharge from the perspective of parents is shown in Figure 19. The findings from the community staff survey reveal inequalities in the needs of children with LD being met in the community, the timeliness of their discharge from hospital, and communication between primary, secondary and tertiary services.
FIGURE 19.
Perceived barriers to and facilitators of a good discharge for children with LD (parent interview, community staff survey) (RQ1).
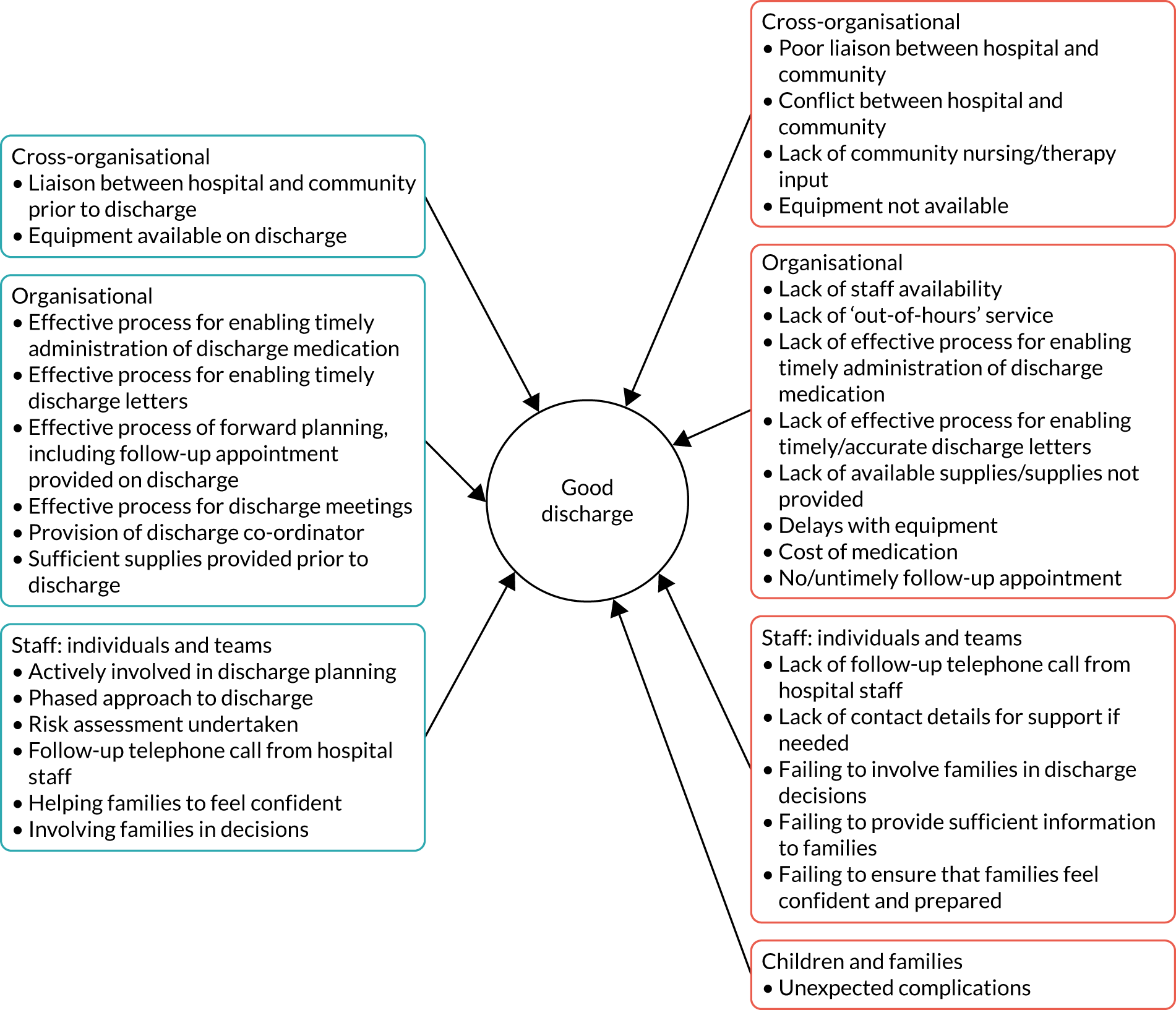
Chapter 11 Feedback from children and parents about their hospital stay
In this chapter we present the results of the anonymous child and parent survey (phase 3) from the seven participating hospitals, combined with qualitative data regarding children’s views of their hospital experience (phase 2, but who did not complete the survey).
We received 1371 completed parent questionnaires and 1180 completed child questionnaires. Just over one-third (n = 543) of children completed the child questionnaires themselves, with an additional 12 in conjunction with a parent, and 587 were completed by parents on behalf of their child. In 38 cases, information about who completed the child questionnaire was missing.
Owing to the nature of how these data were collected, this sample includes questionnaires related to children without LD and without a long-term condition. For completeness and ethics reasons, we provide demographic data about this full data set of children and their parents (see Appendix 10, Table 16, and Appendix 11, Table 17). Given that this report is focused on children and young people with and without LD who do have a long-term condition, we do not report on this data set in this chapter.
Comparisons of the quantitative data below focus on those children with a long-term condition and LD (n = 198) with those with a long-term condition only (n = 355). Demographic data about these participants are shown in Appendix 12, Tables 17 and 18. Children without a long-term condition and their parents are not included in this comparison.
Although the questionnaires were designed primarily to answer RQ4, related to satisfaction with the hospital experience, additional questions were included that contributed to answering the other four RQs. Findings from the parents’ and children’s questionnaire are provided first, followed by qualitative data collected from children using a combination of a sticker exercise, a Talking Mats interview and a ward tour with photography.
Parent questionnaire
Research question 1: do children with and children without learning disability have equal access to high-quality hospital care that meets their particular needs?
The findings showed evidence of inequality (Table 12). Parents were asked eight questions about their satisfaction with care to meet their child’s needs in relation to aspects of staff competence, confidence and capacity. Levels of satisfaction were generally lower among parents of children with LD, particularly in relation to access to resources and confidence in communicating with their child. Only 50% of parents of children with LD were completely satisfied that staff were routinely able to access LD specialist staff to meet their child’s needs. Parents of children with LD also reported lower levels of satisfaction in relation to staff working in an environment that was designed to take into account their child’s individual needs; two-thirds of parents of children with LD were completely satisfied compared with more than three-quarters of parents of children without LD.
| Domain | Question/statement | Children with long-term condition and LD (% scoring in each response category) | Children with long-term condition only (% scoring in each response category) | Statistics (Mann–Whitney tests) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| Satisfaction with care to meet child’s needs (RQ1) | Staff have the knowledge and skills to meet the needs of my childa | 75 | 18 | 5 | 2 | 0 | 81 | 14 | 3 | 2 | 1 | z = 1.48; p = 0.140 |
| Staff have the expertise to meet my child’s needsa | 75 | 18 | 5 | 2 | 0 | 81 | 14 | 3 | 1 | 1 | z = 1.47; p = 0.140 | |
| Staff have access to resources to meet the needs of my child (e.g. communication aids, equipment)a | 65 | 20 | 11 | 3 | 1 | 81 | 11 | 6 | 1 | 1 | z = 4.04; p < 0.001 | |
| Staff have access to support to meet the needs of my child (e.g. play specialist)a | 71 | 17 | 11 | 1 | 1 | 78 | 1 | 7 | 1 | 1 | z = 1.64; p = 0.101 | |
| Staff can routinely access LD specialist staff to meet my child’s needsa | 51 | 16 | 24 | 6 | 3 | 66 | 6 | 25 | 1 | 1 | z = 2.75; p = 0.006 | |
| Staff are confident and adaptable when communicating with my childa | 71 | 18 | 6 | 4 | 1 | 84 | 12 | 3 | 1 | 0 | z = 3.73; p < 0.001 | |
| Staff assessed and managed my child’s pain and discomforta | 73 | 17 | 7 | 2 | 1 | 77 | 16 | 4 | 3 | 0 | z = 1.10; p = 0.273 | |
| Staff managed my child’s behavioura | 65 | 17 | 15 | 3 | 1 | 73 | 13 | 13 | 0 | 1 | z = 1.87; p = 0.062 | |
| Staff work in an environment that takes account of my child’s individual needsb | 68 | 20 | 9 | 4 | 1 | 78 | 15 | 4 | 2 | 1 | z = 2.69; p = 0.007 | |
| Equal access to hospital care (RQ2) | Overall, I felt my child’s care was well co-ordinatedb | 81 | 12 | 4 | 3 | 1 | 82 | 13 | 2 | 2 | 2 | z = 0.23; p = 0.820 |
| Equal involvement in treatment, care and services (RQ3) | I felt actively involved in decisions about the care and treatment of my childb | 79 | 17 | 2 | 2 | 1 | 77 | 16 | 4 | 1 | 2 | z = 0.38; p = 0.702 |
| I felt I had a choice in the care I provided for my childb | 77 | 17 | 4 | 1 | 1 | 76 | 17 | 4 | 2 | 2 | z = 0.38; p = 0.706 | |
| Staff valued my experience as a parentb | 73 | 19 | 5 | 3 | 1 | 72 | 15 | 8 | 3 | 3 | z = 0.50; p = 0.618 | |
| Staff took me and my concerns seriouslyb | 74 | 19 | 5 | 2 | 0 | 78 | 13 | 5 | 2 | 2 | z = 0.68; p = 0.496 | |
| Staff interaction (RQ4) | Staff were responsive to my needsb | 78 | 16 | 4 | 2 | 1 | 78 | 13 | 4 | 2 | 2 | z = 0.21; p = 0.836 |
| Staff were responsive to my child’s needsb | 83 | 15 | 1 | 1 | 1 | 82 | 13 | 2 | 2 | 1 | z = 0.37; p = 0.713 | |
| Staff spent enough time with meb | 72 | 21 | 5 | 2 | 0 | 72 | 18 | 7 | 2 | 2 | z = 0.39; p = 0.697 | |
| Staff spent enough time with my childb | 74 | 20 | 3 | 3 | 1 | 74 | 18 | 6 | 2 | 1 | z = 0.19; p = 0.853 | |
| Staff wanted to help meb | 82 | 14 | 3 | 1 | 0 | 79 | 13 | 5 | 2 | 1 | z = 0.85; p = 0.396 | |
| Staff wanted to help my childb | 91 | 7 | 1 | 1 | 0 | 89 | 8 | 2 | 1 | 1 | z = 0.84; p = 0.401 | |
| Staff asked questions about how I was feelingb | 56 | 24 | 13 | 3 | 5 | 60 | 20 | 10 | 4 | 6 | z = 0.71; p = 0.476 | |
| Staff asked questions about how my child was feelingb | 86 | 11 | 1 | 2 | 1 | 85 | 10 | 2 | 2 | 1 | z = 0.46; p = 0.648 | |
| Communication (RQ4) | Satisfaction with understanding the purpose of the admissiona | 88 | 10 | 1 | 1 | 1 | 89 | 10 | 1 | 0 | 0 | z = 0.46; p = 0.647 |
| Satisfaction with being kept up to date with what is happeninga | 76 | 16 | 5 | 2 | 2 | 68 | 24 | 3 | 4 | 1 | z = 1.90; p = 0.058 | |
| Staff clearly explained any tests or procedures required by my childb | 88 | 10 | 2 | 1 | 1 | 85 | 12 | 2 | 1 | 0 | z = 0.90; p = 0.367 | |
| Staff dealt with my child’s questions appropriatelyb | 83 | 10 | 5 | 3 | 0 | 86 | 10 | 3 | 1 | 0 | z = 0.95; p = 0.341 | |
| Staff dealt with my questions in a timely wayb | 80 | 13 | 5 | 1 | 1 | 78 | 14 | 4 | 3 | 1 | z = 0.68; p = 0.500 | |
| When I had an important question to ask a nurse I got an answer that I could understandb | 85 | 10 | 3 | 1 | 1 | 85 | 10 | 3 | 1 | 1 | z = 0.12; p = 0.903 | |
| When I had an important question to ask a doctor I got an answer that I could understandb | 85 | 12 | 2 | 1 | 1 | 84 | 11 | 3 | 1 | 2 | z = 0.20; p = 0.839 | |
| Safety concerns (RQ5) | For this admission how satisfied are you that staff were always able to deliver safe care to your childa | 77 | 18 | 4 | 2 | 0 | 84 | 13 | 2 | 2 | 0 | z = 1.76; p = 0.078 |
| I had trust and confidence in the nurses caring for my childb | 84 | 13 | 1 | 2 | 1 | 81 | 13 | 3 | 1 | 1 | z = 0.84; p = 0.401 | |
| I had trust and confidence in the doctors caring for my childb | 84 | 10 | 3 | 1 | 2 | 87 | 9 | 2 | 1 | 2 | z = 0.97; p = 0.331 | |
Research question 2: do children with and children without learning disability, assisted by their families, have equal access to hospital appointments, investigations and treatments?
The findings do not show evidence of inequality. We asked parents of children with and parents of children without LD about the co-ordination of their child’s care and found that > 80% in both groups strongly agreed that their child’s care was well co-ordinated.
Research question 3: are children with and children without learning disability and their families equally involved as active partners in their treatment, care and services?
The findings do not show evidence of inequality. Approximately three-quarters of parents in both groups strongly agreed that they were actively involved in decisions about the care and treatment of their child and had a choice in the care provided for their child. Similar proportions also agreed that staff valued their experience as a parent and took them and their concerns seriously.
Research question 4: are children with and children without learning disability and their families equally satisfied with their hospital experience?
The findings showed no evidence of inequality. There was no difference between parents of children with and parents of children without LD regarding the helpfulness of any of the staff groups. Overall ratings were generally positive, with most staff rated as extremely helpful. However, 10 out of 77 parents (13%) of children with LD reported that they had not seen a LD nurse but would have liked to and eight (10%) did not know whether or not they had seen a LD nurse. The fact that some families wanted to see an LD nurse and did not have the opportunity to is a potential source of inequity. Parents of children with and parents of children without LD demonstrated equal levels of agreement about how staff interacted with them in terms of being responsive to their own and their child’s needs, helping them and their child, spending enough time with them and their child and asking them and their child questions about how they were feeling. Parents were also equally satisfied with how staff communicated with them in terms of the purpose of the admission, keeping up to date with what was happening, explaining tests and procedures and answering their questions. Overall levels of satisfaction were high, with > 98% of parents in both groups completely or mostly satisfied with their hospital experience.
Research question 5: are safety concerns for children with and children without learning disability the same?
Although similarly high proportions of parents in both groups had trust and confidence in both doctors and nurses, a higher proportion (84%) of parents of children without LD were completely satisfied that staff were always able to deliver safe care to their child than of parents of children with LD (77%).
Overall levels of satisfaction were high among parents with ward rounds, with activities available for their child and with going home at the right time, with no differences between parents of children with and parents of children without LD. Parents in both groups also showed high levels of agreement about staff introducing themselves [82% strongly agreed, three (2%) parents of children with LD did not agree and 11 (5%) parents of children without LD did not agree]. Similar patterns of responses were seen with regard to whether or not staff explained their role, and only six (1%) parents (all of whom were in the non-LD group) did not agree that staff were polite and approachable.
Children’s questionnaire
For the purposes of reporting data from the child questionnaire, data supplied by the child or by a parent-proxy on behalf of the child are presented together. The questionnaire was designed predominantly to answer RQ4, related to children’s satisfaction with their hospital experience. Questions focused on three aspects – the environment, people, and care and treatment – and we found no differences in ratings of satisfaction between those with and those without LD for any of these (Table 13).
| Domain | Question/statement | Children with long-term condition and LD (% scoring in each response category) | Children with long-term condition only (% scoring in each response category) | Statistics (Fisher’s exact tests) | ||
|---|---|---|---|---|---|---|
| Thumbs up | Thumbs down | Thumbs up | Thumbs down | |||
| Environment | How did you feel about where you stayed on the ward? | 90 | 10 | 91 | 9 | p = 0.349 |
| How did you feel about sleeping on the ward? | 76 | 24 | 78 | 22 | p = 0.332 | |
| How did you feel about noise on the ward? | 65 | 35 | 70 | 30 | p = 0.186 | |
| How did you feel about what the ward looked like? | 95 | 5 | 94 | 6 | p = 0.398 | |
| Were there enough things for young people your age to do on the ward? | 84 | 16 | 80 | 20 | p = 0.187 | |
| How did you feel about waiting for things in hospital? | 63 | 37 | 59 | 41 | p = 0.260 | |
| Did you have enough privacy when staying on the ward? | 89 | 11 | 90 | 10 | p = 0.314 | |
| People | Did the staff help you if you had pain or were not comfortable? | 98 | 2 | 97 | 3 | p = 0.544 |
| Did the staff spend enough time with you? | 90 | 10 | 93 | 7 | p = 0.145 | |
| Were the staff friendly? | 100 | 0 | 100 | 0 | p = 0.635 | |
| Did the staff listen to what you said? | 96 | 4 | 98 | 2 | p = 0.235 | |
| Did the staff do something about what you said? | 94 | 6 | 96 | 4 | p = 0.203 | |
| Care and treatment | How did you feel about having any tests or treatments? | 74 | 26 | 77 | 23 | p = 0.238 |
| Before you had any tests or treatments did you understand what was going to happen? | 80 | 20 | 85 | 15 | p = 0.140 | |
| While you were in hospital did you get enough information? | 94 | 6 | 93 | 7 | p = 0.364 | |
| Was the information easy to understand? | 88 | 12 | 92 | 8 | p = 0.145 | |
Responses to the individual questions were predominantly positive (> 80%) from both groups of children, particularly in relation to their perceptions of how friendly staff were, their feeling of being safe and having trust in the people looking after them, and pain management. Children’s views about waiting, noise, sleeping, tests and treatments and having a say in decisions were less positive in both groups (59–80%).
Research question 3: are children with and children without learning disability and their families equally involved as active partners in their treatment, care and services?
The findings showed no evidence of inequality. When asked whether they had a say in any decisions about their care and treatment, > 80% children in each group responded positively.
Research question 5: are safety concerns for children with and children without learning disability the same?
The findings showed no evidence of inequality, with 98% of children in each group reporting that they trusted the people looking after them and > 96% of children in each group reporting that they felt safe when staying on the ward.
Children were asked whether they had stayed in a cubicle or a bay during their hospital stay. Of those who answered, the majority (n = 188) stayed in a bay, with 141 staying in a cubicle and 18 staying in both. A higher proportion of children who stayed in a cubicle reported a more positive experience in terms of noise, sleeping on the ward and waiting for things than those who stayed in a bay. Perceptions of privacy were high wherever children stayed (cubicle, 97%; bay, 85%; both cubicle and bay, 86%), but 10% across the groups did not feel that they had enough privacy when staying on the ward.
Children’s sticker exercise
Sixty children from phase 2 completed the sticker exercise; examples are shown in Figure 20.
FIGURE 20.
Examples of sticker exercise completed by children (a) with and (b) without LD.


The VILD chart (Figure 21) shows individual children’s (or proxy) responses to all 13 questions, enabling the comparison of responses to individual questions between children with LD and without LD and between children’s and non-children’s hospitals. The data show the variable experiences that children have, including some reporting nearly all positive responses and others nearly all negative responses, including from the same hospital.
FIGURE 21.
Visual representation of children’s responses on the sticker exercise.
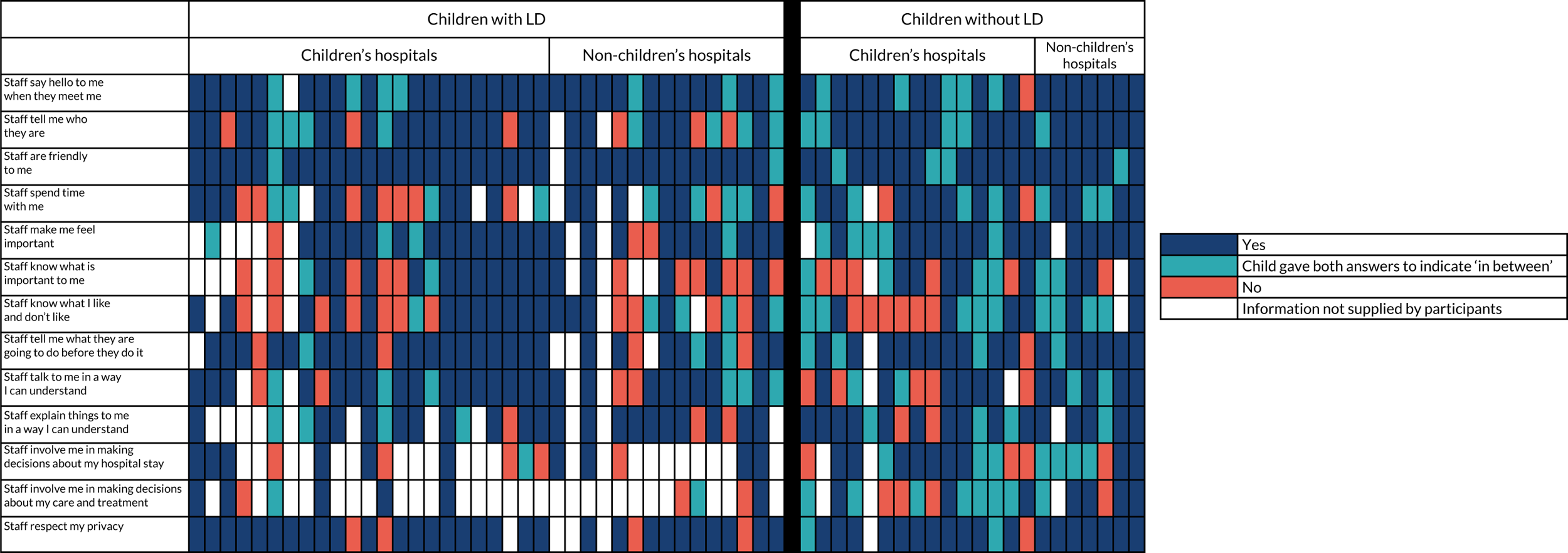
As with the questionnaire, the vast majority of children with LD felt that staff were friendly to them (95%) and most, but not all, said hello to them when they met them (78%):
Staff say hello to me when they meet me?
What do you think?
A smiley face.
Smiley face. Do all the nurses say hello to you?
Yes, they do. They come and do my obs. and they always come to tickle my toes [child was in caste from knee to toes].
That’s good. What about the doctors? Do they say hello to you?
Yes, they always do.
This was also the same for children without LD. However, only just over half (61%) of children with LD reported that staff actually told them who they were when they met them:
Staff tell me who they are? They told me what their name was yesterday, and they told me that I need to have a rest and keep calm and don’t get out of bed and don’t, well anyway, [Surgeon] has come to me and told me who they are.
So, if the nurse comes in, do they say, ‘Hello, my name is [name]’?
Do you think the nurses have all told you who they are this week?
Well, no, they haven’t.
Although proportionally more children without LD (77%) felt that staff did tell them who they were, there were still some who said that this was not always the case. One child, for example, said that she felt ‘a bit offended’ by staff not introducing themselves, going on to explain, ‘I wanted to say something but I didn’t know how to say it because I didn’t know their name’.
Children generally did not think that staff knew them, with only 48% feeling that staff knew what was important to them and 41% feeling that staff knew what they liked and did not like. As one mother acting as parent proxy said:
She’s actually called [nickname]. Nobody asked if she’d like to be called anything else, which I would have thought they’d do that, but no.
LD
It was evident from the positive examples of staff knowing the child ‘inside and out’ how valuable this could be to both children with and children without LD and their parents:
Because they know me they know about all my phobias . . . We have this little sheet with a star on it and it says like my needs and how I do it, so it says talk to my mum for example and not to me and we normally hang it around the door.
Non-LD
We have the purple thing up there [child summary on door], it’s his level of cognition and they read it.
Parent proxy, LD
Right, staff knows what is important to me? That is going to be thumbs up . . . Because they, it’s very important because they always give me important stuff to do and they always listen to the important stuff.
LD
In terms of the two questions about children’s involvement in decisions, those with LD were largely unable to answer them, and, when they did, their responses were variable. One child talked about choosing food from the menu, and another talked positively about choosing the colour of their plaster cast. A mother acting as parent proxy for her child with LD talked positively about the way hospital staff tried to involve her daughter, despite the fact she was non-verbal and did not have an effective communication device:
She can’t be understood by other people. So, yes, they did take heed of [child’s] wishes, and that was very impressive. I haven’t had to confront them. It’s been their initiative. So, that’s really impressive. They feel it as much, and respect-, they put the child first. I don’t have to advocate for her . . . they involve her in terms of informing her, and helping her participate, but she doesn’t really decide.
By contrast, another child with LD explained, with the help of her mother, that hospital staff were not able to communicate with her in the same way as her teachers did in school:
Which DVDs did you bring?
Sing.
Sing. Come on, and? Sign. Sing and sign DVDs.
Sing and sign. Is that a good one?
Yes.
Do you do signing when you’re in school?
Yes, I do.
You do, and do any of the nurses or doctors around here, do they sign as well, or is that just in school?
That’s just in school.
In addition, another child with LD said:
The staff doesn’t give me in a way I can understand . . . Staff don’t tell me what they are going to do for me, they don’t, they never tell me.
Involvement in decisions was suboptimal among both groups of children. This was particularly apparent in relation to decisions about care and treatment, in which only 55% of children felt always or sometimes involved. As two children without LD said:
I’d like to be a bit more involved in being able to say ‘I think I should do this’ and that kind of thing. I wasn’t involved in decisions [last week about care] but in the past sometimes I have.
I get asked what I like but sometimes they make the decisions . . . Because its mum that’s involved because she’s the parent, they don’t really ask the kids.
This child did go on to say, however, that she thought that it was appropriate that her mother was involved in making decisions.
Both children with and children without LD positively rated staff respecting their privacy:
Staff respect my privacy? That’s a thumb’s up because they always let me have a privacy . . . they shut my curtains when they come around and give me some obs. and I talk about my thoughts.
LD
I make my own space bubble . . . They respect your space bubble because you are either talking about something personal or you’re say getting dressed or some other things that humans do not like to know about – so that’s what the curtains are for. People seem to realise that the majority of the time – so they respect that.
Non-LD
However, this child goes on to highlight the issue with hospital curtains and the maintenance of privacy:
Occasionally people bump into the curtain and they move it so there’s a gap and like they walk past they can see in the gap. I don’t like that . . . That’s why I prefer separate rooms, they have doors not curtains.
A greater proportion of children with LD (28%) than children without LD (10%) did not think that staff spent time with them.
Talking Mats
Fifty-nine children (or their parent proxy) completed the Talking Mats exercise, either verbally by talking about each symbol and whether they liked or disliked it or using the mat to indicate their answers. Examples are provided in Figures 22 and 23. More children without LD were able to explain the reasons for their responses.
FIGURE 22.
Examples of Talking Mats responses from children with LD.
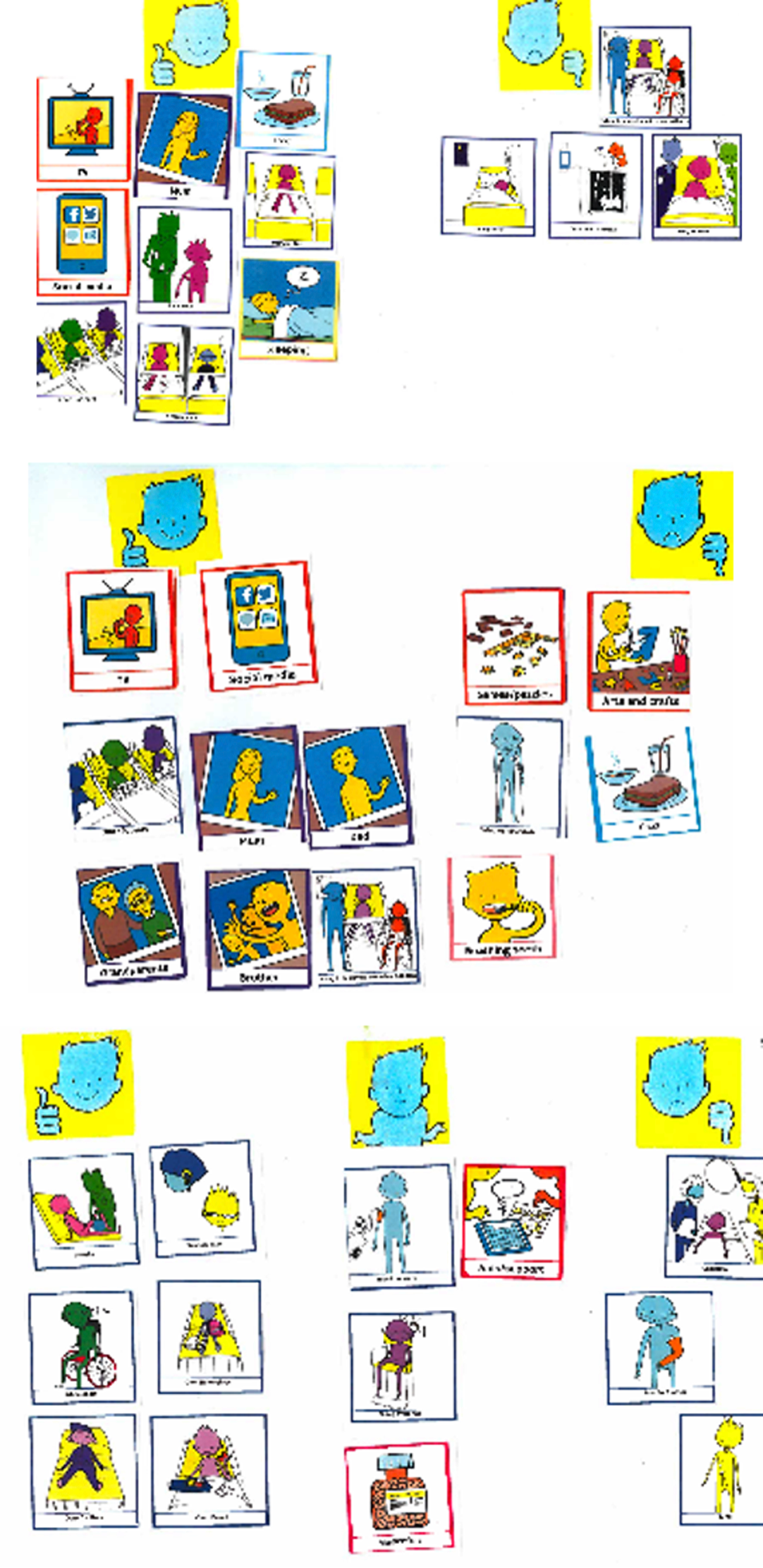
FIGURE 23.
Examples of Talking Mats responses from a child without LD.
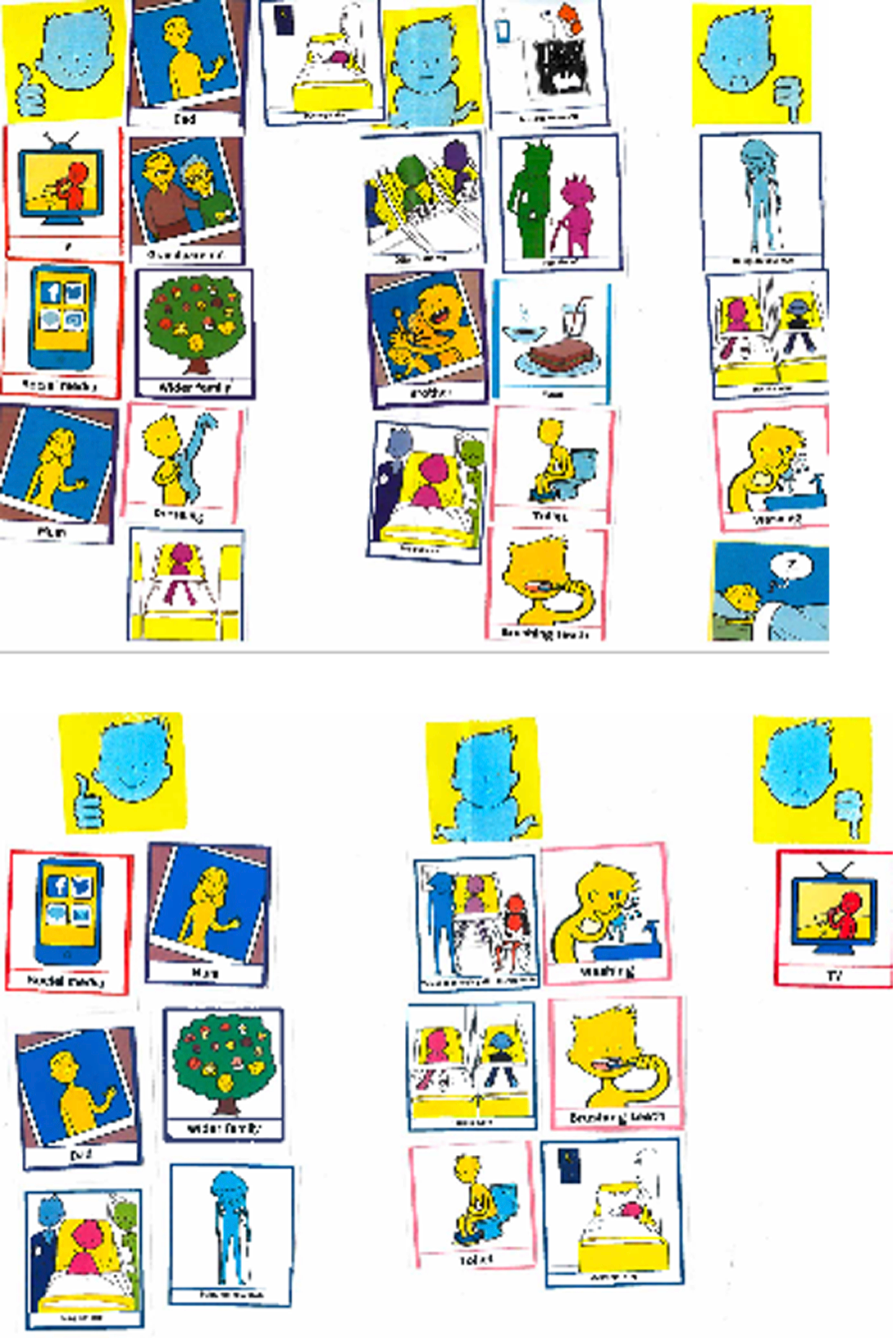
The Talking Mats VILD chart (Figure 24) shows the responses from individual children with LD and without LD to various aspects of their experience of being in either a children’s or a non-children’s hospital.
FIGURE 24.
Visual representation of children’s responses using modified Talking Mats.
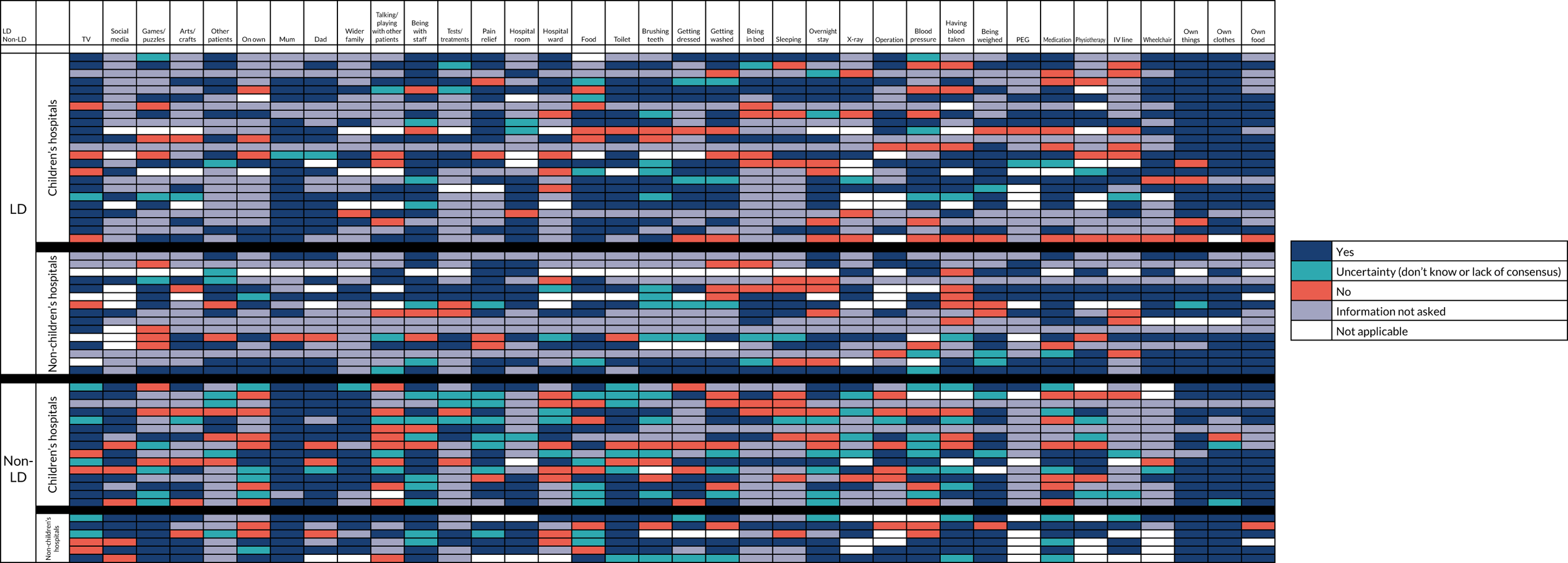
Family was clearly important, with most children reporting ‘liking’ both parents being with them. The television appeared especially important for children with LD, and social media especially important for children without LD.
Children with LD in particular indicated that they liked being with staff in hospital (75%). One child who indicated this also said:
Staff make me feel important. Yes they do. They take the time.
Similar feedback was given by a child without LD, who also liked being with staff:
They say to me like if I’ve done something good then they say to me ‘oh you’ve done really good’ and it makes me feel quite good about myself . . . I’d like it if maybe they could have two nurses per bay instead of one so they could have more time to talk.
Two children without LD who said that they did not like being with staff indicated why that might be:
I think it was the doctor, he just came and said ‘are you OK?’ and I said ‘yes’ and he was like ‘walk’ and then he left really quickly and I was confused . . . Sometimes he walked away in mid-answer.
I didn’t want to speak to him much more – he was dismissive of anything I really said, he was like – he just kept saying ‘oh well we’ll soon be out of the hospital, you’ll soon be discharged’.
Children were also asked if they liked being with other patients in hospital, and a higher proportion of children with LD answered ‘yes’ (75%) to this question than did those without LD (50%). As one child without LD said:
I like other children of my own age and under, and maybe a few years above but I don’t really socialise with [them].
Another child without LD explained why he had answered ‘no’ to liking being with other patients:
I wish I could have been with people my own age then I could have made friends, because I get bored. So if I could have made some friends it would be nice – they could relate to you [me].
One teenager without LD suggested that staff could introduce patients on the same ward to each other to help overcome any awkwardness and help them get to know each other.
There appeared to be a clear difference in children’s perceptions of having medication, with more children with LD saying that they liked it than children without LD. However, this difference may be accounted for by the fact that the majority of those with LD had a percutaneous endoscopic gastrostomy, which may have precluded the need for any medication to be given orally.
Children’s views about food were mixed, with only half saying that they always liked it. Comments were made about the timing and the lack of choice available:
I prefer not to eat anything because I’ve just woken up and I can’t be bothered to eat then, I’d rather wake up before I eat.
Non-LD
This child went on to describe the different feeling he had about food at his school:
I tend to just snack at break time at school – because they have a tuck shop, it’s a happy feeling. So happy.
One child without LD also talked about the challenges of being surrounded by people who were eating when he was not allowed to.
There were lots of comments about the noise from other children, particularly for children being nursed in bays rather than cubicles. Children talked about babies screaming and crying, other children being in pain and nurses being loud. As one child without LD said:
And there was a girl and she screamed all night. She had the most ridiculous cry. It was so pathetically long. It was irritating – I wanted to strangle her.
Tests and treatments were challenging for many children, both with and without LD. Talking about having her blood pressure taken, one child with LD said:
First of all they put a bandage around you, then they do a bear hug, what I don’t like.
She’s scared of having her blood pressure taken. They won’t do it because she’s frightened.
How does it feel having your blood pressure taken?
I didn’t like the bear hug. It feels angry like that [gestures tensing up her arms].
We are confident at this stage that our data from all phases of data collection have been evidenced. The narratives from children, parents and staff have been captured. The synthesis of these data sets is the next important step to describe in this report; without that, the story told so far around inequalities across child populations in hospital would be incomplete.
Section 4 Synthesis, discussion, recommendations for research, limitations and conclusions
Chapter 12 Synthesis and discussion
We set out to identify the cross-organisational, organisational and individual factors in NHS hospitals that facilitate or prevent children with LD and their families receiving equal access to high-quality care and services, as well as to develop guidance for NHS trusts about the implementation of successful and effective measures to promote equal access for children with LD and their families.
To achieve our aim, we needed to answer a number of RQs.
From the perspectives of families and clinical staff:
-
Do children with and children without LD and their families have equal access to high-quality hospital care that meets their particular needs?
-
Do children with and children without LD, assisted by their families, have equal access to hospital appointments, investigations and treatments?
-
Are children with and children without LD and their families equally involved as active partners in their treatment, care and services?
-
Are children with and children without LD and their families equally satisfied with their hospital experience?
-
Are safety concerns for children with and children without LD the same?
-
What are the examples of effective, replicable good practice for facilitating equal access to high-quality care and services for children with LD and their families at the study sites?
-
What indicators from the data and the literature suggest that the findings may be generalisable to other children with long-term conditions in the hospital setting?
We were able to generate a large body of evidence about the way in which hospital inpatient care is delivered to and experienced by children with LD and their parents, from the perspective of multiple stakeholders, as well as drawing comparisons with children without LD and their families. Synthesising these data reveals a range of barriers to and facilitators of children with LD and their families receiving high-quality hospital care in relation to (1) how their particular needs are identified and met in hospital (RQ1); (2) their access to investigations, treatments and procedures (RQ2); (3) their involvement as partners in their care (RQ3); and (4) their safety (RQ5) (Figures 25–29). Quantitative and qualitative data collected at the organisational level (phase 1) and at the individual staff level (phase 2) showed evidence of inequality in each of these areas, as well as how valued children were and whether or not they were treated with dignity and respect. There was no difference in these findings between children’s and non-children’s hospitals.
FIGURE 25.
Synthesis of perceived barriers to and facilitators of identifying children with LD in hospital (RQ1). a, Organisation mapping, staff survey; b, staff interviews; c, parent interviews. LDLN, learning disabilities liaison nurse.

FIGURE 26.
Synthesis of perceived barriers to and facilitators of meeting the needs of children with LD in hospital (RQ1). a, Organisation mapping, staff survey; b, staff interviews; c, parent interviews. LDLN, learning disabilities liaison nurse.
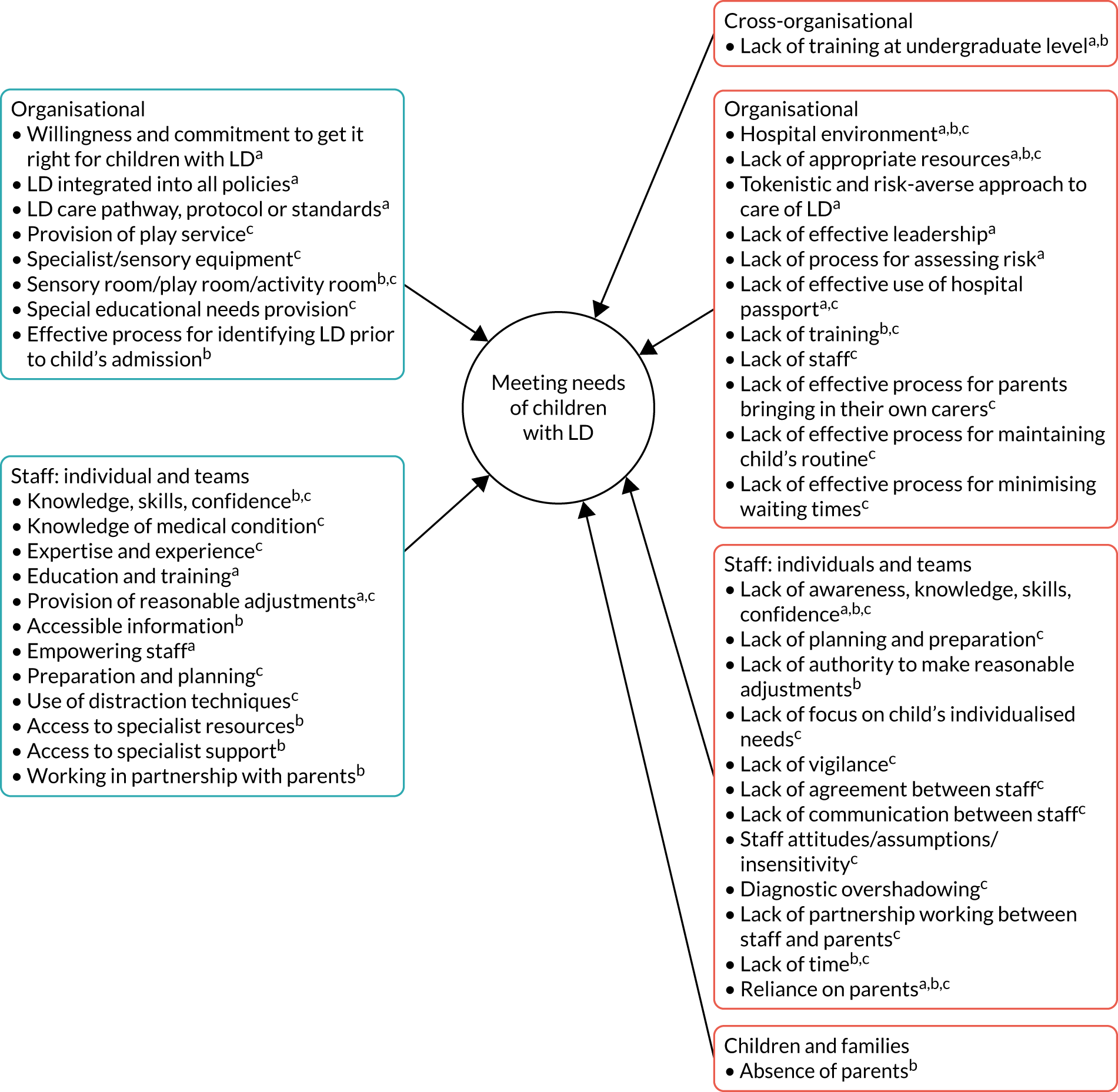
FIGURE 27.
Synthesis of perceived barriers to and facilitators of children with LD gaining access to investigations, procedures and treatments in hospital (RQ2).
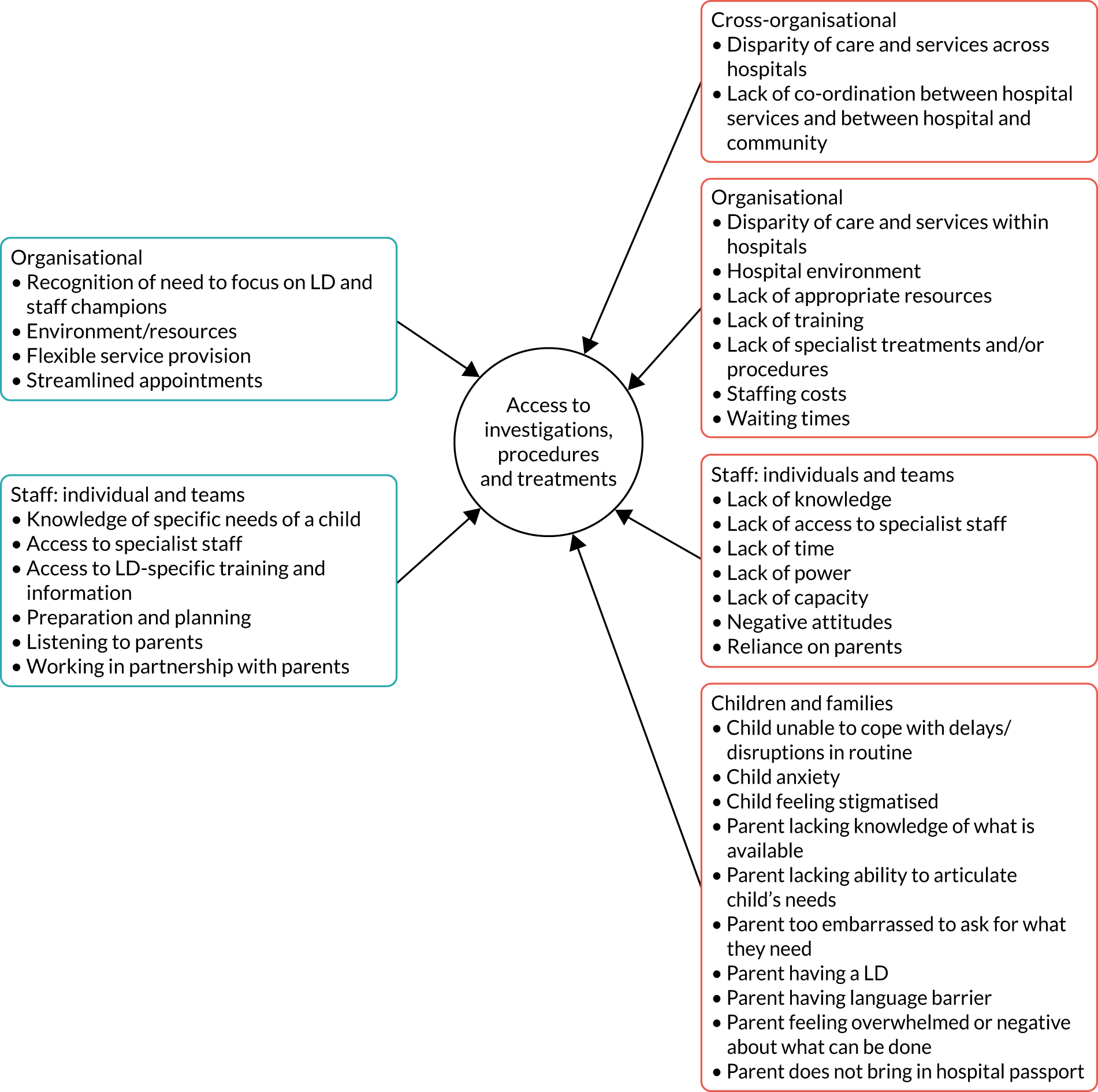
FIGURE 28.
Synthesis of perceived barriers to and facilitators of involving children with LD and their families as partners in care (RQ3). a, Organisation mapping, staff survey; b, staff interviews; c, parent interviews. LDLN, learning disabilities liaison nurse.
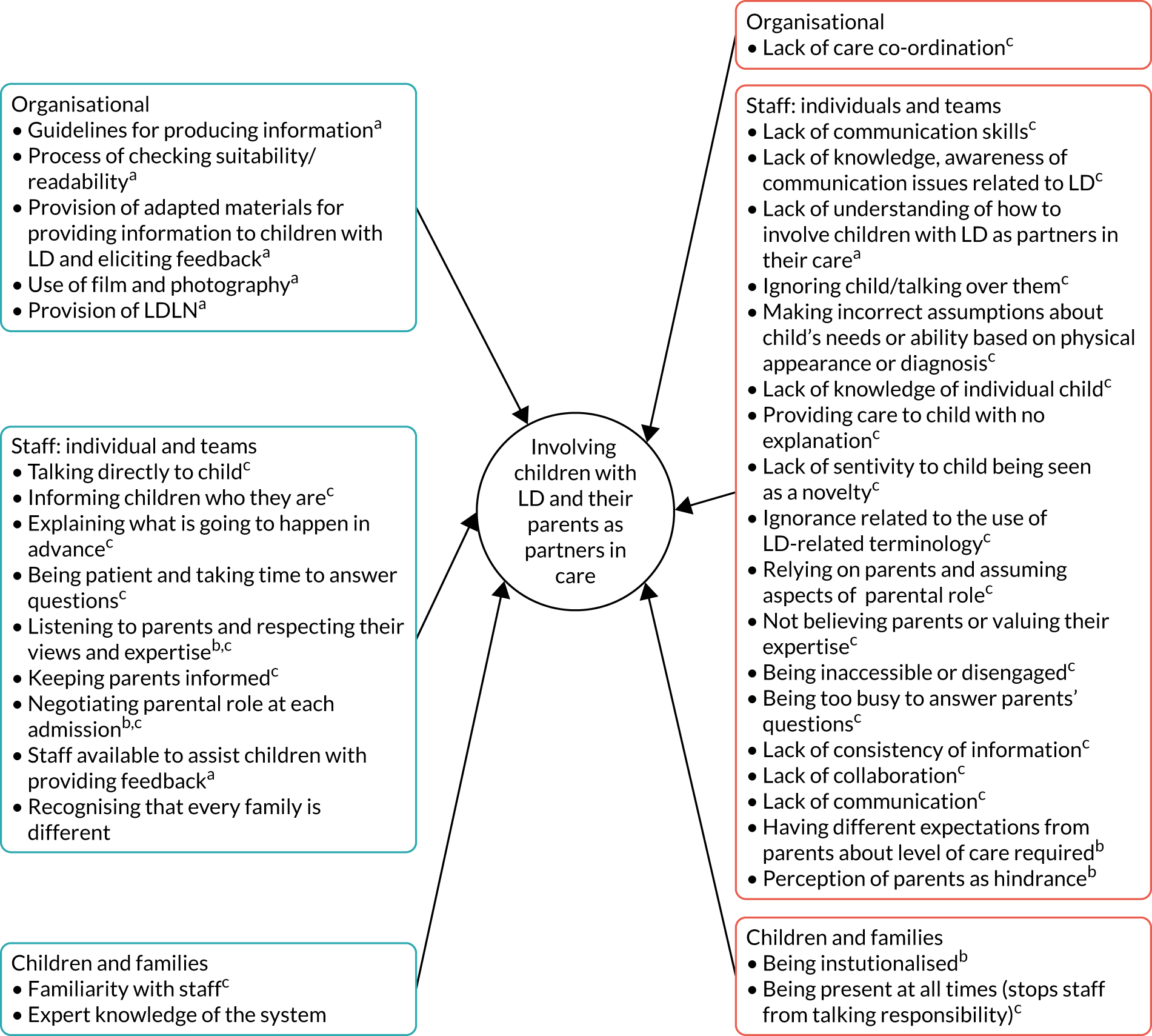
FIGURE 29.
Synthesis of perceived barriers to and facilitators of children with LD being safe in hospital (RQ5). a, Organisation mapping, staff survey; b, staff interviews; c, parent interviews. LDLN, learning disabilities liaison nurse.
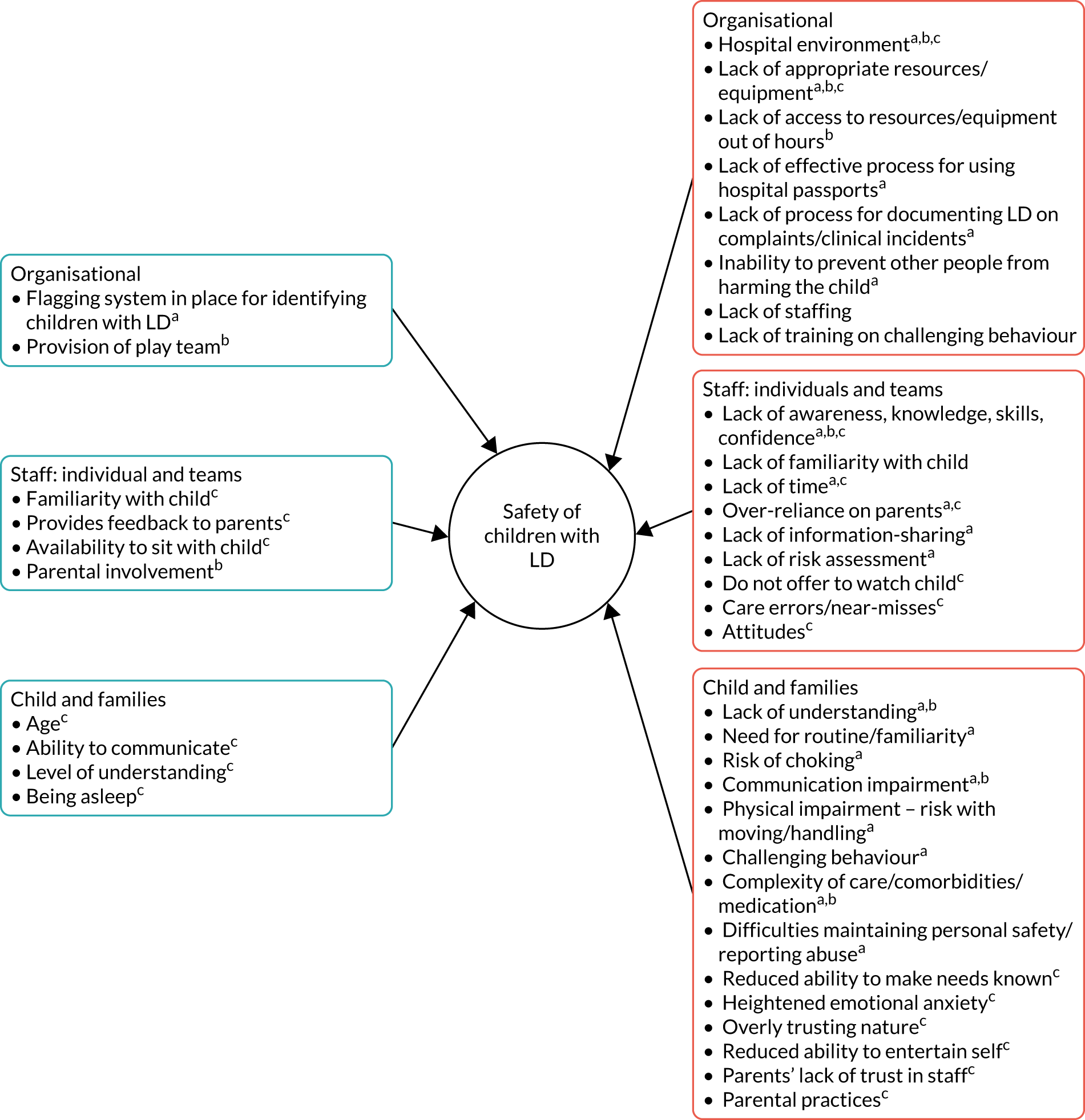
Findings from both quantitative and qualitative data indicated inequality with regard to children’s access to high-quality hospital care that meets their particular needs (RQ1) and children’s safety (RQ5) from the perspective of parents. Although the quantitative data did not show evidence of inequality in relation to parents’ perceptions of their child’s access to investigations, treatment and procedures (RQ2), there were examples in the qualitative data of parents describing their child’s access being affected by the presence of LD, including in terms of particular aspects of provision, such as the hospital play service, suggestive of inequity. Similarly, the quantitative data did not show evidence of inequality in terms of parents’ perception of their involvement as active partners in their child’s treatment, care and services (RQ3), and this was reflected in the qualitative data, with both sets of parents expressing very mixed views. Parents of children with LD expressed particular issues in relation to being listened to and having their expertise respected and their child being included in conversations and interactions. RQ4, related to parents’ satisfaction, was addressed through the inpatient survey only, and there was no evidence of inequality between parents of children with and parents of children without LD. The children’s inpatient survey showed no evidence of inequality in relation to RQ3, RQ4 and RQ5. The qualitative data, however, provided insight into what children with and children without LD like and dislike about being in hospital, with examples of both good and suboptimal experiences across many areas for individuals in both children’s and non-children’s hospitals. Data revealed the importance of all children having access to age and developmentally appropriate play facilities, television and Wi-Fi, as well as good food and sleep. Children generally found staff to be friendly, but did not always feel listened to or involved in their care or that staff knew what was important to them or had enough time to spend with them. Findings from the parents’ and children’s survey supported what families shared in their interviews: that, on the whole, being in a cubicle, which provided privacy, space and a quiet environment, was preferred. This presented a risk, however, of families being ‘out of sight, out of mind’, which was particularly challenging for children with LD, who were unable to ask for help or keep themselves safe.
A key factor to inequality appeared to be the lack of effective policies, systems and processes in place to support the provision of individualised care to children with LD in hospital, which often led to insufficient or, in some cases, a complete lack of attention being paid to their particular needs resulting in potential inequity. This stems from staff usually not knowing that the child has LD in advance of meeting them, and not having sufficient knowledge of the diagnosis or what it then means for that child, which is made more difficult by a lack of consistent terminology. When drawing comparisons between the views of parents of children with and parents of children without LD, a key difference appeared to be the scale of impact when care is not individualised. For example, whereas both groups of children may find it difficult to wait in hospital or have their routine disrupted, this can lead to a complete emotional breakdown for children with LD that can last for hours afterwards, rather than them being upset or fed up at the time. Furthermore, it might be easier for parents of children without LD to rationalise things with their child and find strategies to resolve situations than it is for parents of children with LD. Likewise, children without LD, especially when the admission is short, can often find other resources they can rely on when things are not available. As one mother said, ‘If you’re good enough to be interacted with, it’s time to leave. Which is fine.’ In relation to parents, the difference in scale of impact when care is not individualised is highlighted most clearly with regard to their safety concerns, with parents of children with LD expressing a level of hypervigilance that differed in scale and intensity from the continuum of vigilance described by parents of children without LD; although not sleeping was common to both groups, parents of children with LD might sleep with their child; although maintaining personal care was an issue for both groups, parents of children with LD might take their child with them to the toilet.
What largely appears to happen in practice is that children coming into hospital tend to be treated ‘equally’, rather than ‘equitably’, and are expected to follow the same care pathway, which is determined by their medical needs and the reason for their admission. Any adjustments in care, rather than being considered in advance, are largely made or not made as and when a child falls off the pathway; the multiple and compounding layers of complexity surrounding the care of children with LD places them at greater risk of this falling-off than other children. Getting these children back on the pathway depends on a number of factors, discussed below, but a lack of flexibility within the system is key. For children with learning difficulties, such as dyslexia or autism, but without LD, these same issues in following the pathway were described.
We know from other research99 that this is a common complaint from parents, not just those whose child has LD. One key factor seen to make a positive difference was staff knowing the child as a result of a previous admission, although, as parents highlighted, these staff were not always on shift or, if they were, were not necessarily allocated to them.
Another barrier to the provision of individualised care to children with LD in hospital is the lack of ‘nomothetic’100 knowledge that staff hold about children with LD in general. As reported elsewhere,56,57 with the exception of paediatricians, undergraduate training in LD is extremely limited, and opportunities for training in the clinical setting are almost non-existent. Hence, we found that in the most part, the knowledge staff developed about children with LD came from experience gained over time. This would explain why staff in children’s and non-children’s hospitals reported having less capacity and lower levels of capability and confidence to meet the needs of children with LD than of those without LD, particularly in relation to communicating effectively, assessing and managing pain, and managing behaviours that challenge. The findings closely resemble those reported in relation to adults with LD,32 in which limited staff knowledge and skills concerning LD and a failure at the systems level for required adjustments to be made were key factors in patients’ needs not being met.
Parents described three approaches by which staff appeared to generate ‘idiographic’100 knowledge about the needs of a child with LD: most commonly, the passive ad hoc approach of generating ‘knowledge by chance’ at varying points during the admission, with staff relying predominantly on parents actively sharing information about their child; the reactive approach of generating knowledge through ‘learning on the job’ and seeing what can or cannot be done with that information; and, rarely, paying complete attention through a proactive approach of asking parents in advance of the admission what reasonable adjustments are needed for their child, ‘leaving no stone unturned’ (Figure 30). This represents a lost opportunity for staff to build a complete understanding of the child’s individualised needs in a timely manner and use that knowledge to inform their practice. This lack of knowledge is reflected in the data collected from children with LD, with only 52% feeling sure that staff knew their likes and dislikes, and even fewer (41%) feeling sure that staff knew what was important to them. Compounding this situation is that inpatient documentation and communication about children with LD is overwhelmingly medically focused and, despite senior managers in nearly every participating hospital reporting having a hospital passport in place, few parents had even heard of this; those who had heard of it felt that this were not used well in practice, an issue that was also raised by staff. Good documentation is particularly important for unplanned admissions, where the opportunity to gather information that relates to medical and non-medical needs in advance is limited.
FIGURE 30.
Approaches staff take to identify that a child has LD.
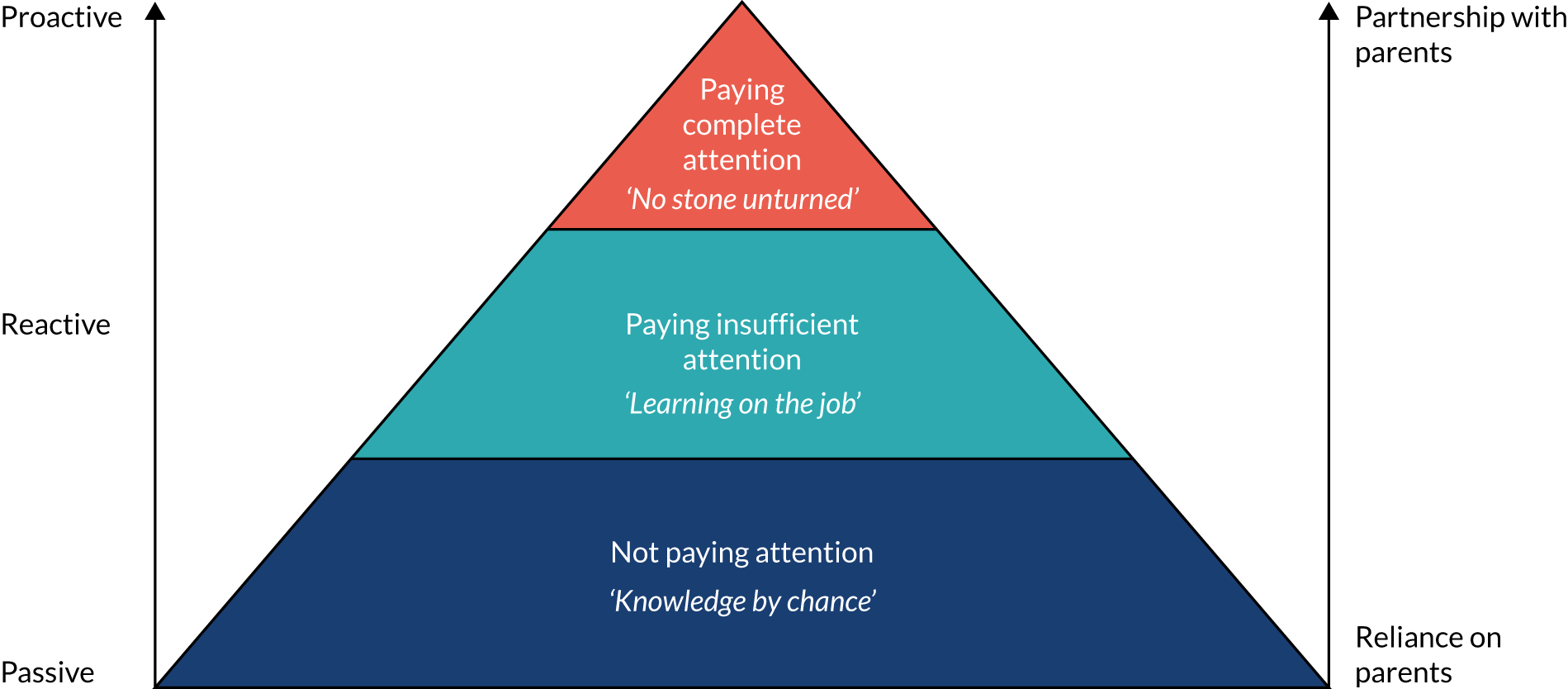
Although some individual staff had concerns about labelling children with LD, parents valued being asked about the additional needs of their child, including any learning requirements, so that necessary adjustments could be made. This was also the case for parents whose children without LD had additional learning or behavioural needs. What parents of children with LD disliked was constantly repeating the same information, especially when it meant repeating their child’s entire medical history for no clear reason. This appeared to be particularly true when there were sensitivities surrounding the LD diagnosis.
Bringing the data from parents and staff together shows a relationship between the type of knowledge staff hold about disability and the skills and confidence of staff to apply that knowledge in practice (Figure 31). It shows the equal importance of staff undertaking training and gaining experience to build their knowledge about children with LD generally, as well as generating knowledge at the individual level for every child through proactively working in partnership with parents prior to the child’s admission to hospital. There were examples in the data that supported each component of this model; what is evident is that the LD nurse is well placed to have both good knowledge of the individual child and the confidence and skills to apply this knowledge in practice. They described numerous aspects to their role, which focuses on supporting individualised care for children with LD, and staff valued their input as well as that of LD champions, where these existed. Furthermore, the few parents in the study who had input from a LD nurse valued this highly, and some indicated on the parent survey that they would have valued input from a LD nurse had this been an option. At present, provision of LD nurses is patchy and there is a lack of consistency in terms of their seniority and remit. What is important is understanding how the LD nurse role is best operationalised in practice to have the greatest impact on families, supporting and empowering all staff to adapt their own practice and providing them with the opportunity to do so.
FIGURE 31.
Relationship between types of knowledge staff hold about disability and the skills and confidence of staff to apply that knowledge in practice.
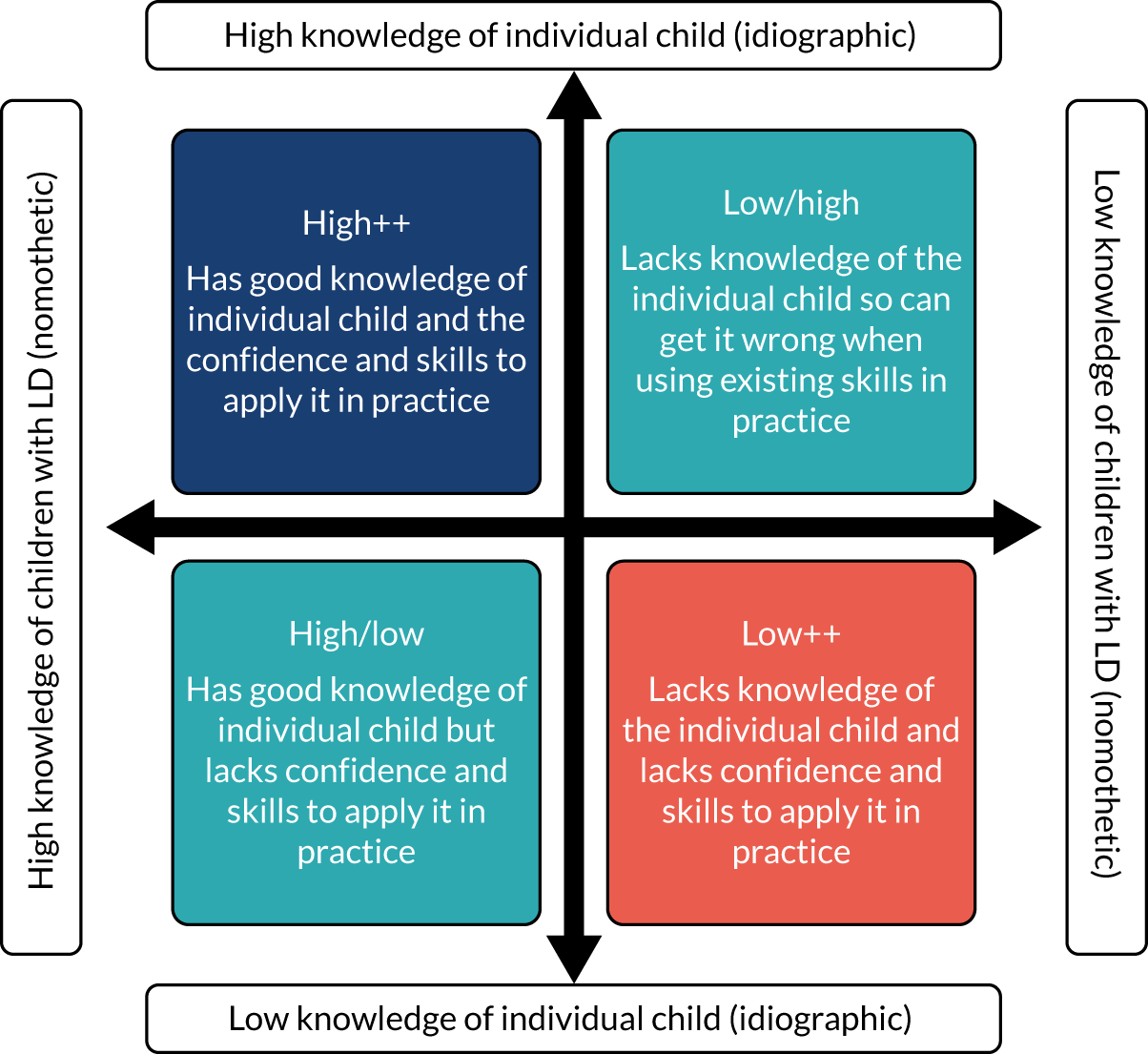
The child and family in hospital exist at the centre of a complex series of interconnected systems within and across organisations. The huge variability in LD-related provision within and across these organisations results from the lack of a coherent, robust approach to the care of these children. The experience of individual children and families in our study, both those with and those without LD, was overwhelmingly affected by the individual health-care professional caring for them at any given time, with a lack of consistency in attitudes, practices, skills and knowledge of staff working on the same ward at the same time and across different wards and hospitals. Furthermore, the suitability of the hospital environment for children with LD and the availability of appropriate resources and equipment differ. This variability leads to uncertainty for parents and children, especially those with LD, about what to expect in terms of their hospital experience and the ‘rules of engagement’, leading to a strong preference for selected staff and creating heightened anxiety when those key people are not around. Similarly, for a multitude of reasons, including a lack of familiarity with the child, a lack of staffing or a lack of skills and confidence, staff can come to rely on parents being present with their child, thereby highlighting the particular strains that the current system inadvertently imposes on parents. The safety of the child underpinned the role that all parents played in hospital, including a general lack of willingness and ability to relinquish aspects of responsibility for their child’s health and well-being to hospital staff in whom they did not have complete trust. Sometimes even complete trust was not enough for parents to leave their child, as happens when children attend school. This is in stark contrast to parents’ willingness to hand over responsibility for their child to teachers at school. The safety concerns of parents of children with LD were heightened as a result of issues with the hospital environment and use of equipment, and their child’s restricted ability to ask for help, to spot danger and to keep themselves safe. Based on perceptions of risk, only in the rare cases that constant vigilance101 was offered by staff would parents of children with LD take a break, with a resulting impact on their own health and well-being that was similar to, but on a different scale from, that reported by parents of children without LD.
Although our phase 1 survey data found that staff perceive that children with LD are valued less and treated with less dignity and respect than children without LD, interviews with LD liaison nurses across children’s hospitals revealed evidence of an improving organisational culture and a commitment to getting it right. However, at present, the relevant policies, systems, and practices are not sufficiently embedded in clinical practice, with, for example, many senior managers not knowing whether or not a specific LD policy exists in their organisation. Only half of children’s hospitals have any form of flagging and alerting system in place, and these vary in terms of their effectiveness in informing staff of a child’s LD and what that means for them. Furthermore, only two hospitals reported having any formal mechanism for recording LD within complaints and clinical incidents, which represents a lost opportunity to compare group-level data.
What is needed is to ensure both equality and equity is a joined-up, cohesive approach to the management and governance of LD health care at all levels that facilitates the development of an ‘institutional memory’ of the specific child rather than relying on the ‘individual memory’ of a particular member of staff.
In Figure 32 we have brought together the factors at the cross-organisational, organisational, staff, team and family levels that are shown to facilitate equity and equality. This, together with our empirical framework (Figure 33), offers a level of detail to guide NHS trusts about service design and delivery. The acronym PROACTIVE is used to illustrate the factors that individual staff and teams need to consider when delivering individualised care to promote equality and equity for children with LD and their families through the provision of reasonable adjustments. It serves as a useful reminder of the importance of staff taking the initiative to identify reasonable adjustments in advance of a child’s visit or admission to hospital, as well as providing a useful way for staff to remember what factors to consider in practice. Being ‘PROACTIVE’ advocates staff working in partnership with parents and other community partners (P), having access to appropriate resources (R), taking the opportunity to understand the individualised needs of the child (O), asking parents and children what matters to them and advocating on their behalf (A), communicating effectively (C), having sufficient time and thinking about the timing of care (T), identifying children with LD within the organisation and having an inclusive approach to developing services to meet their needs (I), valuing every child as an individual (V) and adjusting the environment (E). Table 14 provides examples of good practice taken from our data for each of these factors. By applying these in practice for children with LD, it should be possible to get it right for all children irrespective of their age, cultural background or cognitive ability, including the issues related to teenagers highlighted by staff.
FIGURE 32.
A conceptual model of the individual, organisational and cross-organisational factors relevant to the delivery of individualised care to children with LD and their families in hospital.
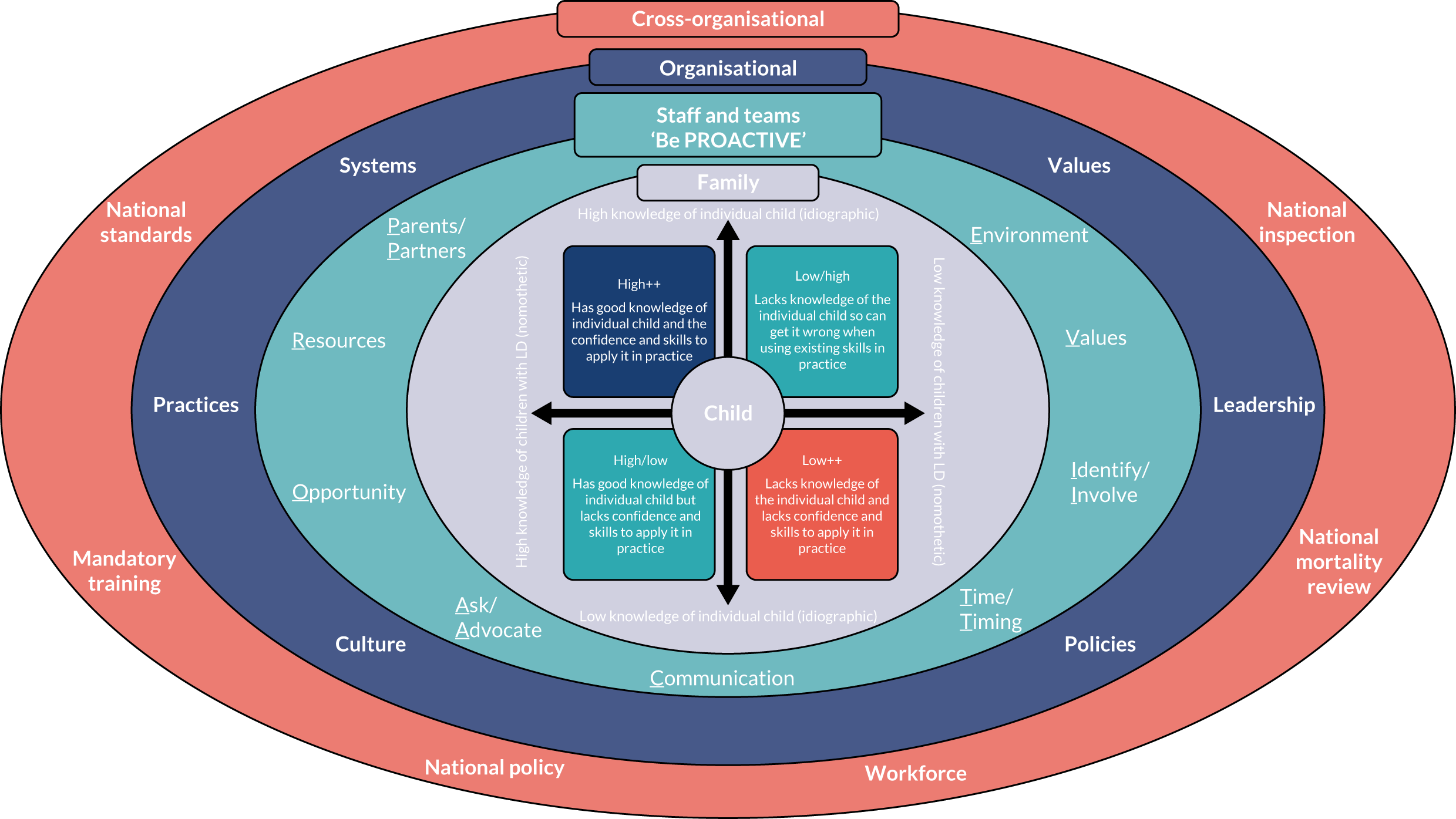
FIGURE 33.
Empirical framework. LDLN, learning disabilities liaison nurse.
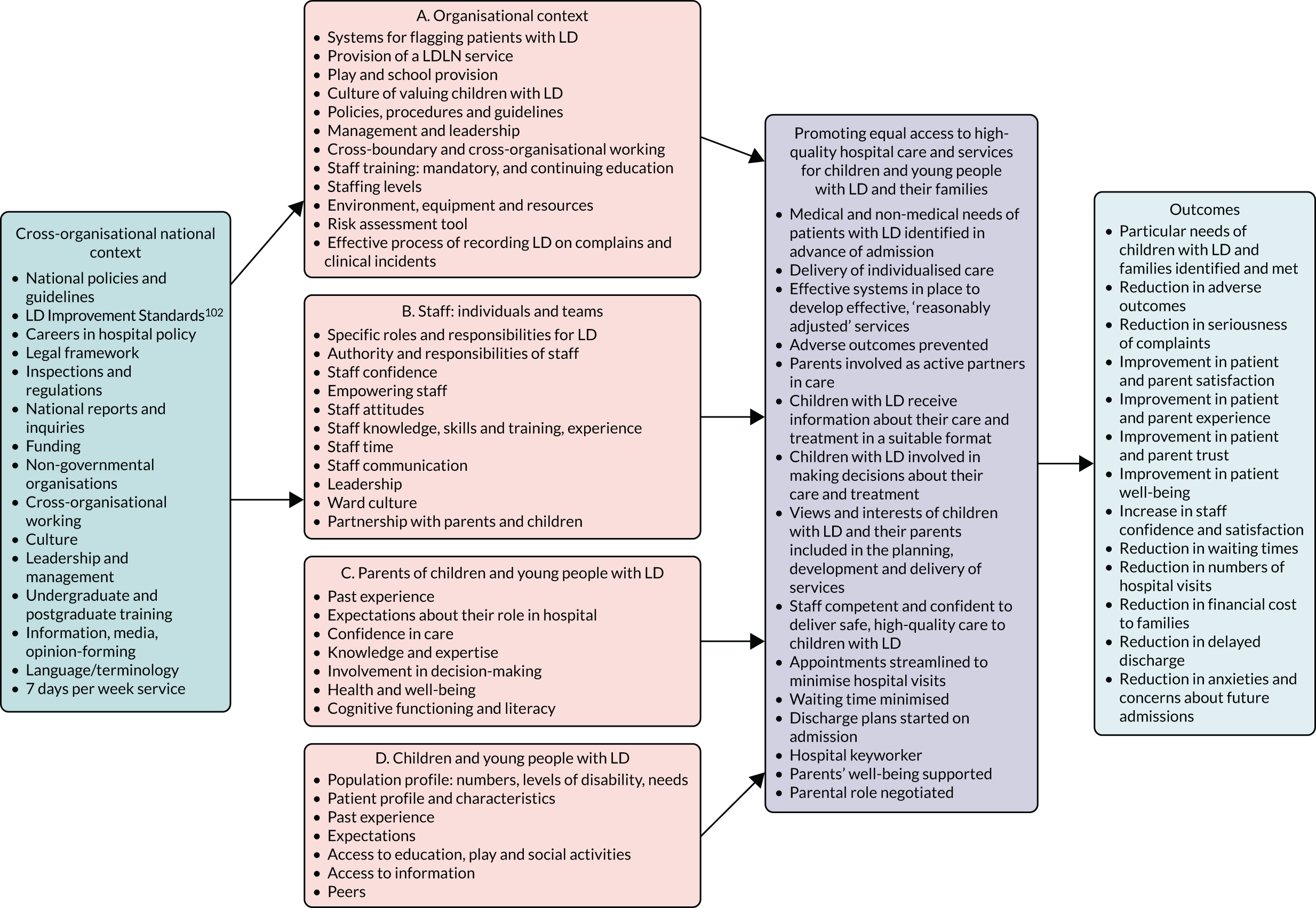
| PROACTIVE | Examples of good practice |
|---|---|
| Partnership and parents |
|
| Resources |
|
| Opportunity |
|
| Ask and advocate |
|
| Communication |
|
| Time and timing |
|
| Identification and Involvement |
|
| Values |
|
| Environment |
|
Although examples of individualised care were largely lacking in this study, this should not take away from the many examples of good practice that parents and children described in the care they received, with many individual staff being praised for going out of their way to give families a good experience. Furthermore, when it was provided, individualised care was highly valued by parents and children, with small gestures appearing to make all the difference. On the whole, the data show that staff are being let down by an inadequate system, and the negative attitudes and assumptions of the minority, which can have a lasting impact on parents and children, need to be addressed.
Cross-organisational
The results of this study are timely, underscoring the relevance that a number of recent developments at the national level have had to the care of children with LD in hospital, as well as adults, who hitherto have been the primary focus. The development of The Learning Disability Improvement Standards for NHS Trusts,102 the ongoing national mortality review programme,5 the increasing focus on LD in Care Quality Commission inspections,103 the Transforming Care agenda104 and recent guidance on issues such as reducing the need for restraint and restrictive interventions105 are important contributions to achieving quality care and provide a sufficient framework to support organisations to respond to the majority of our findings. The Learning Disability Improvement Standards for NHS Trusts, for example, highlight the need for a flagging system to identify patients with LD and for measures to promote antidiscriminatory practices, learning from complaints, services to be co-designed and to develop ‘workforce plans that manage and mitigate the impact of the growing, cross-system shortage of qualified practitioners with a professional specialism in LD’ (contains public sector information licensed under the Open Government Licence v3.0). 102 They also require NHS trusts to demonstrate that they are making reasonable adjustments for patients with LD. All of these relate to issues raised in this study. What is missing from The Learning Disability Improvement Standards for NHS Trusts102 is a focus on the role of parents in hospital and their physical and emotional well-being; an improvement standard related to this is needed.
However, we cannot expect essential improvements to happen without an investment in education and training for all staff and a recognition that increased resources are needed. Undergraduate nursing courses are currently offered across five specialist branches, one of which is LD. A range of post-qualification courses are also available. We found only one that was a combined children’s and LD course. All education to qualify as a children’s nurse will include some content on caring for children with LD, but on the whole this will be a small part of any curriculum, and is known to vary across courses. Nurses can make a huge contribution to reducing inequalities and inequities of care for this patient group. This requires an understanding of the needs of these patients and when to refer them for specialist support, such as that provided by LD nurses. To do this, every nurse requires training that covers a ‘common core curriculum’. 99 Our conceptual model provides a framework for this training that can be tailored accordingly to different professional groups and health-care settings. Trusts across the UK will soon be required to put in place mandated in-house LD/autism education and training, and essentially this must be supported by nurse leadership; a nominated executive LD lead must be in place. A core curriculum that standardises undergraduate training and continuing professional development provided by each trust is an important step forward.
Although the national commitment to providing mandatory disability awareness training for all hospital staff is welcome, this alone will be insufficient to address the issues our research has highlighted. If LD nurses spend years being trained as specialist nurses and hold the knowledge and education to help and understand the daily struggles of people with LD (www.mencap.org.uk/blog/daily-struggleslearning-disability-nurse), these skills should be utilised in all settings to help achieve, promote and drive equal rights in health care.
The data also highlight that a lack of shared language across health, education and social care organisations in relation to LD is a barrier to equality and equity, but more so is a lack of communication and documentation between health-care professionals about what any diagnosis or ‘label’ means for an individual child. Part of any training has to include an understanding of the need to individualise care for patients with LD, and for that we need consistent language, with less focus on diagnostic labels and more focus on asking families what is important to them.
Chapter 13 Conclusions and implications
Recommendations for research
This study has generated considerable evidence about the way in which inpatient hospital care is delivered to, and experienced by, children with LD and their parents. As highlighted by Northway,83 the identification of what inequalities exist, and for whom and in what circumstances, leads us to make the key following recommendations for research.
1. Patient safety: develop and validate an instrument for the assessment and management of risk in children with learning disability in hospital
It is evident that staff and parents feel that the safety needs of children with LD are not fully identified and met in hospital. Key barriers include a lack of appropriately trained staff who have the competence and confidence to deliver safe care, a lack of suitable resources, and issues with space and the environment. Research is required to develop and validate an instrument to assess and manage risk in children with LD in hospital, which can be linked directly to the identification and provision of reasonable adjustments. The instrument would be likely to empower health-care professionals, particularly nurses, in their interactions with families, as a result of enabling more informed discussions about risk and safety, with additional benefits for parents from the increased trust and confidence in staff, enabling the development of a true partnership in care. Alongside the development of the instrument should be a detailed review of the types of reasonable adjustments that children with LD require in hospital, along with the frequency with which these adjustments are required and the barriers to and facilitators of their being accommodated.
2. Learning disability liaison nurse posts: measure the impact of dedicated learning disability nurse provision in specialist and non-specialist children’s hospitals
We have provided evidence of a limited and highly variable LD service for children in hospital, valued by hospital staff and shown to have a positive impact on their perceptions of their capability to care for this group of patients. However, the provision of LD nurses was not shown to increase staff perceptions of capacity or confidence, or to increase how children with LD are valued within hospital, or their safety and their access to appointments. There is no clear guidance on how many LD nurses are needed to deliver safe and effective hospital care to children with LD or about the level at which they should be working. The Learning Disability Improvement Standards for NHS Trusts102 state that:
Trusts must have workforce plans that manage and mitigate the impact of the growing, cross-system shortage of qualified practitioners with a professional specialism in learning disabilities . . . [and] must demonstrate clinical and practice leadership and consideration of the needs of people with learning disabilities, autism or both, within local strategies to ensure safe and sustainable staffing.
To understand how we might begin to address these issues and inform service delivery and workforce planning, research is needed to measure the impact of dedicated LD roles on the care of children with LD in hospitals. Given the diversity of roles described in this report, it is important that this research captures the full range of LD posts in addition to LD nurses, who are embedded within the clinical setting but who are not employed specifically to work with patients with LD. This should include an evaluation of how the LD role is best operationalised in practice to have the greatest impact on children and families, as well as how we monitor and evaluate these roles to ensure that they are utilised effectively and efficiently, including carrying out a cost–benefit analysis.
3. Staff training
The issue of a lack of LD training at both undergraduate and postgraduate level was raised by staff from different professional groups and working in different hospitals. Research is needed to evaluate the impact of the forthcoming mandatory LD awareness training on staff, patients and families. Furthermore, we need to understand how well the new Nursing and Midwifery Council 2018 standards106 are being implemented in relation to LD and what difference, if any, they are making.
4. Patient- and family-centred care: there is a critical need to understand expectations of staff and parents in contemporary practice
Throughout our work we heard from parents about their perceptions and first-hand experience of what is referred to as family-centred care. The clearest voice in our data spoke to poor clarity in terms of roles and responsibilities, revealing a critical need to understand the expectations of staff and parents. There is a body of research that underpins this approach to care, but how that applies to contemporary practice remains unknown. Published work already informs us that interpretations are known to vary considerably, and that there are concerns that the child has been ‘lost’ within this unit of care. Partnership emerges as a concept that requires further clarification, as does the notion of negotiation. Underpinning this approach has always been a clear and agreed plan of care about who does what for the child when they are in hospital. Our data would suggest that this is at the core of variable practices. Good and less good practices were described, but, overall, ‘chance’ plays too big a part in there being a clear understanding of the parent’s role while their child is in hospital.
The term ‘parental participation’ first appeared in the literature in the 1980s. Health-care practices have changed significantly since that time. Recent studies have highlighted the lack of attention to cultural and societal changes in the delivery of care within this framework. 98 We would argue for the need to understand family-centred care as it applies to contemporary practice. Further research examining the effects of family-centred care for children, their families, health-care professionals and health-care organisations, reflecting cultural diversity and norms, must be conducted. Importantly, this expanded understanding, from all of these perspectives, would clarify the role of the parent when their child is in hospital. Thus, a shared understanding that is communicated at the outset, where good practices of working with all parents prevail, would reduce the role of ‘chance’ that we observed. It is important to ensure that families do not feel that they are expected to provide input into the care of their child beyond their expectations or capabilities, or indeed for the full 24 hours of each day in hospital.
5. Use of mixed-methods studies: we need to maximise the potential of mixed methods to provide a comprehensive and meaningful account of hospital care
It is evident that, in our study, had we used only questionnaires as a source of evidence with parents and staff, we would have reported an incomplete story. For some, questionnaires will have been easier and less time-consuming to complete than answering questions in an interview, but the interviews allowed us to reach greater depth, and parents and staff clearly felt comfortable expressing their concerns as well as sharing good practice; inequalities not evident from questionnaires became apparent when talking with parents. Although questionnaires are considered easy to deliver, they may lack questions relevant to those in our care. So, to understand the full range of family experiences while in hospital, we need to maximise the potential of mixed methods to provide a comprehensive and meaningful account.
Limitations
In this four-phase study, both strengths and limitations have been reflected on. As this was a national study, collecting multiple sources of data within an NHS setting presented a number of challenges. Here we report the particular issues from each phase that could have had some impact on our final study findings.
Phase 1
We cannot say with certainty that our organisational mapping is complete or that our description of the LD nurse role is comprehensive. Although we collected over 2000 survey responses, our sampling method meant that we were not able to determine a meaningful response rate in terms of representativeness of different professional groups. Furthermore, participants were self-selecting, which means that the findings cannot be generalised with any degree of precision. In all participating sites, we were reliant on the local collaborator to distribute the survey to staff who had contact with children with and children without LD. It is possible that in non-children’s hospitals not all eligible staff were identified and given the opportunity to participate. Similarly, we depended on the local collaborator to identify senior staff who had the knowledge to answer the interview questions, and it is possible that we did not include those in the organisation who were the most informed, although we tried to address this limitation by holding at least two interviews per site. The NHS staff who participated in interviews were identified locally and encompassed a wide variety of roles (e.g. medical consultants, matrons, clinical nurse specialist and managers), which may have produced a lack of consistency in the data. At two sites (non-specialist hospitals), no staff agreed to be interviewed. The 30-minute interview was designed to encourage participation, but it did limit in-depth discussion around site practices. Although we ensured that more than one interview was conducted per site to ensure that all questions were addressed, this time constraint inevitably placed restrictions on the depth of qualitative data generated. Furthermore, staff interviews were relatively short (30–45 minutes) because of the clinical commitments of these staff. We did not set out to formally evaluate LD nurse provision as this was beyond the scope of our wider project. Hence, interviews did not specifically focus on the role, but rather asked about knowledge of the systems, practices and policies in place in the organisation. Key questions such as the rationale and decision-making behind the delivery of the LD nurse service and how much time dedicated LD nurses spend undertaking different components of their job description remain unanswered.
Phases 2 and 3
We cannot say with certainty that the sites, although selected objectively, are representative of all services caring for these children. Although the aim of the study was not to be proportionally representative of specialist children’s hospitals and non-specialist hospitals, children are more likely to receive treatment in their local hospital, which for many is unlikely to be a specialist hospital for children. If this study were repeated, a sample that better reflects this form of access might be incorporated. We relied heavily on the local principal investigator and their staff to identify and recruit families to our study, and to support the survey in phase 3. In one of our sites no children with LD were identified at all, which was surprising, as this site was a specialist children’s hospital. Pressures on NHS staff that have an impact on their time to deliver and participate in research was a major challenge, even though they received financial reimbursement for taking part in the study. Other limitations were in data collection methods; we were unable to use photography in some trusts, and our use of creative e-technologies in data collection was often challenged by local systems, despite us having ethics approval to use these. Concerns about the use of electronic diaries, for example, centred on data protection and confidentiality issues, and this resulted in a lack of choice for families of using this method. With regard to photography, some research and development departments put restrictions in place with the primary purpose of protecting the organisation’s reputation, and these restrictions were not conducive to giving children with LD and/or autism control over what they saw as important to capture. This was despite our reassurance that for these organisations we would not share any images beyond the research team.
Conclusions
At the start of this journey there were concerns about practice, and the delivery of hospital care to children with LD. There were a number of high-profile cases that demanded a sea-change. We sought to map this context of care and to take learning from the adult disability field and the associated policies to look at practice through a new lens. We have done that within the milieu in which inequalities exist; we needed to understand these inequalities and how they had an impact on the care of children in hospital. We knew at the outset that to understand these inequalities we needed to ask a range of stakeholders, that included children, and use multiple sources of data that would help us to build a picture of what is actually happening.
There are three key messages from our work.
Safety issues and quality of care affect all children in acute hospitals and their parents, but the impact on children with LD and their parents is much greater. Hence, if we address the issues for children with LD, all children will benefit.
Key to this is individualising care through the provision of reasonable adjustments. The key message was that multiple and compounding layers of complexity often surround the care of children with LD in hospital and that even those with the same diagnosis as another child with or without LD have unique needs that require staff to take an individualised approach to their care. It was this individualised approach that appeared to define parents’ understanding of quality care. Parents of children without LD tended not to draw on the concept of difference when thinking about the quality of their child’s care. However, children who also had additional learning or behavioural needs associated with ADHD, autism or dyslexia had an inpatient experience similar to that for children with LD. Staff therefore need to undertake training and gain experience to build their general skills and knowledge about children with LD and/or additional learning or behaviour needs, as well as generating knowledge about the individual child by proactively working in partnership with parents prior to the child’s admission. Training in LD needs to be firmly embedded in the undergraduate curriculum for all professional groups, as well as be consolidated in practice through mandated education that includes face-to-face learning with experts by experience. We believe that our conceptual model provides a framework for this training that can be tailored accordingly to different professional groups and different health-care settings. Parents want to be asked about their child’s needs. The same approach can be adopted for all children and families, asking ‘what do I need to know about you/your child for this admission?’.
We need to address the impact of children’s hospitalisation on parents’ health and well-being; trust is essential to ensuring that parents get a break from caring responsibilities. Key to this is staff working proactively with parents in advance of the child’s admission to identify any safety concerns and plan necessary reasonable adjustments to minimise risk. The development of an evidence-based risk assessment instrument would facilitate this process, as would a robust process for flagging patients with LD that focuses on alerting staff of the need for reasonable adjustments. Parents’ access to healthy and affordable food, comfortable beds and suitable places to unwind should be seen as essential requirements rather than optional extras.
Acknowledgements
We would like to thank the families and staff who took the time to participate in our research. We would also like to thank the Study Steering Committee, our Partnership Schools, our Parent Advisory Group and our local collaborators, principal investigators and research nurses for their contributions. We would also like to acknowledge the contribution of Dr Kate Khair, consultant nurse, for her contributions to the analysis of children’s data.
Study Steering Committee members
Kath Evans (chairperson).
Janet Cobb.
Peter Fleming.
Margaret Fletcher.
Michelle Johnson.
Andrea White.
Lorna Wales.
Partnership schools
Richard Cloudelsey School, Islington, London.
The Bridge School, Islington London.
Contributions of authors
Kate Oulton (https://orcid.org/0000-0002-5778-3849) (Consultant Nurse, Senior Research Fellow – Learning Disabilities) was the chief investigator and led on the design of the study, with contributions from Faith Gibson (https://orcid.org/0000-0002-8125-4584) (Professor of Children’s Cancer Care), Jo Wray (https://orcid.org/0000-0002-4769-1211) (Associate Professor, Health Psychology), Lucinda Carr (https://orcid.org/0000-0001-9238-108X) (Consultant Neurologist), Irene Tuffrey-Wijne (https://orcid.org/0000-0002-7288-9529) (Professor of Intellectual Disability and Palliative Care), Angela Hassiotis (https://orcid.org/0000-0002-9800-3909) (Professor of Psychiatry of Intellectual Disability), Carey Jewitt (https://orcid.org/0000-0002-2971-984X) (Professor of Learning and Technology) and Sam Kerry (Expert Parent).
Charlotte Kenten (https://orcid.org/0000-0001-7012-7347) (Research Fellow) was the project manager and collected data along with Jessica Russell (https://orcid.org/0000-0003-3194-412X) (Research Associate). Both had previous experience of working with people with learning disabilities and of undertaking research, with Charlotte Kenten having completed a PhD (Doctor of Philosophy) and Jessica Russell a master’s degree in anthropology.
Data analysis was undertaken primarily by the core team (Kate Oulton, Charlotte Kenten, Jessica Russell, Jo Wray and Faith Gibson) with contributions from the executive team [Sam Kerry, Lucinda Carr, Angela Hassiotis, Carey Jewitt, Irene Tuffrey-Wijne, Mark Whiting (https://orcid.org/0000-0002-4056-6784) (WellChild Professor of Community Children’s Nursing) and Paula Kelly (https://orcid.org/0000-0002-0581-5474) (Senior Research Fellow, Palliative Care)] as required.
Dr Kate Oulton led on the writing of the report with Jo Wray, Charlotte Kenten and Faith Gibson.
Jessica Russell led on patient and public involvement with Faith Gibson and Mark Whiting.
All authors reviewed and approved the final report.
Publications
Oulton K, Wray J, Carr L, Hassiotis A, Jewitt C, Kerry S, Tuffrey-Wijne I, Gibson F. Pay More Attention: a national mixed methods study to identify the barriers and facilitators to ensuring equal access to high-quality hospital care and services for children and young people with and without learning disabilities and their families. BMJ Open 2016;6:e012333.
Oulton K, Gibson F, Carr L, Hassiotis A, Jewitt C, Kenten C, Russell J, et al. Mapping staff perspectives towards the delivery of hospital care for children and young people with and without learning disabilities in England: a mixed methods national study. BMC Health Serv Res 2018;18:203.
Kenten C, Wray J, Gibson F, Russell J, Tuffrey-Wijne I, Oulton K. To flag or not to flag: identification of children and young people with learning disabilities in English hospitals. J Appl Res Intellectual Dis 2019;32:1176–83.
Oulton K, Wray J, Hassiotis A, Kenten C, Russell J, Tuffrey-Wijne, et al. Learning disability nurse provision in children’s hospitals: hospital staff perceptions of whether it makes a difference. BMC Pediatrics 2019;19:192.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Oulton K, Wray J, Carr L, Hassiotis A, Jewitt C, Kerry S, et al. Pay More Attention: a national mixed methods study to identify the barriers and facilitators to ensuring equal access to high-quality hospital care and services for children and young people with and without learning disabilities and their families. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012333.
- Mencap . Death by Indifference 2007.
- Michael J, Richardson A. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People With Learning Disabilities 2008. https://doi.org/10.1108/13595474200800036.
- Improving Health and Lives Learning Disabilities Observatory . Confidential Inquiry into Premature Deaths of People With Learning Disabilities. 2012.
- University of Bristol . Learning Disabilities Mortality Review (LeDeR) Programme: Annual Report 2015–2016 n.d. www.bristol.ac.uk/media-library/sites/sps/leder/LeDeR%20annual%20report%20October%202016_FINAL%20v8.pdf (accessed 20 October 2020).
- World Health Organization . Innovative Care for Chronic Conditions. Building Blocks for Action 2002.
- Department of Health and Social Care . Valuing People: A New Strategy for Learning Disability for the 21st Century. 2001.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Emerson E, Hatton C, Felce D, . Learning Disabilities: The Fundamental Facts. London: Foundation for People with Learning Disabilities; 2001.
- Public Health England Learning Disabilities Observatory . People With Learning Disabilities in England 2015: Main Report 2016.
- Prime Minister’s Strategy Unit . Improving the Life Chances of Disabled People 2005.
- Mimmo L, Harrison R, Hinchcliff R. Patient safety vulnerabilities for children with intellectual disability in hospital: a systematic review and narrative synthesis. BMJ Paediatr Open 2018;2. https://doi.org/10.1136/bmjpo-2017-000201.
- Horridge KA, Harvey C, McGarry K, Williams J, Whitlingum G, Busk M, et al. Quantifying multifaceted needs captured at the point of care. Development of a Disabilities Terminology Set and Disabilities Complexity Scale. Dev Med Child Neurol 2016;58:570-80. https://doi.org/10.1111/dmcn.13102.
- Allerton LA, Welch V, Emerson E. Health inequalities experienced by children and young people with intellectual disabilities: a review of literature from the United Kingdom. J Intellect Disabil 2011;15:269-78. https://doi.org/10.1177/1744629511430772.
- Emerson E, Hatton C. Contribution of socioeconomic position to health inequalities of British children and adolescents with intellectual disabilities. Am J Ment Retard 2007;112:140-50.
- Emerson E, Hatton C. Poverty, socio-economic position, social capital and the health of children and adolescents with intellectual disabilities in Britain: a replication. J Intellect Dev Disabil 2007;51:866-74. https://doi.org/10.1111/j.1365-2788.2007.00951.x.
- Emerson E, Hatton C, Robertson J, . People with Learning Disabilities in England: Improving Health and Lives. London: Learning Disabilities Observatory, Department of Health and Social Care; 2011.
- Carvill S. Sensory impairments, intellectual disability and psychiatry. J Intellect Dev Disabil 2001;45:467-83. https://doi.org/10.1046/j.1365-2788.2001.00366.x.
- Royal College of Speech and Language Therapists . Five Good Communication Standards. Reasonable Adjustments to Communication That Individuals With Learning Disability and Or Autism Should Expect in Specialist Hospital and Residential Settings. RCSLT 2013. www.rcslt.org/wp-content/uploads/media/Project/RCSLT/good-comm-standards.pdf#:~:text=Communication%20is%20a%20significant%20risk%20factor%20contributing%20to,both%20expressing%20themselves%20and%20understanding%20what%20others%20say.5 (accessed 3 November 2021).
- Amiet C, Gourfinkel-An I, Bouzamondo A, Tordjman S, Baulac M, Lechat P, et al. Epilepsy in autism is associated with intellectual disability and gender: evidence from a meta-analysis. Biol Psychiatry 2008;64:577-82. https://doi.org/10.1016/j.biopsych.2008.04.030.
- Branford D, Bhaumik S, Duncan F. Epilepsy in adults with learning disabilities. Seizure 1998;7:473-7. https://doi.org/10.1016/S1059-1311(98)80005-8.
- Matthews T, Weston N, Baxter H, Felce D, Kerr M. A general practice-based prevalence study of epilepsy among adults with intellectual disabilities and of its association with psychiatric disorder, behaviour disturbance and carer stress. J Intellect Dev Disabil 2008;52:163-73. https://doi.org/10.1111/j.1365-2788.2007.01025.x.
- Emerson E, Baines S. Health inequalities and people with learning disabilities in the UK. Tizard Learning Dis Rev 2011;16:42-8. https://doi.org/10.5042/tldr.2011.0008.
- Emerson E. Prevalence of psychiatric disorders in children and adolescents with and without intellectual disability. J Intellect Dev Disabil 2003;47:51-8. https://doi.org/10.1046/j.1365-2788.2003.00464.x.
- Einfeld SL, Ellis LA, Emerson E. Comorbidity of intellectual disability and mental disorder in children and adolescents: a systematic review. J Intellect Dev Disabil 2011;36:137-43. https://doi.org/10.1080/13668250.2011.572548.
- Mahon M, Kibirige MS. Patterns of admissions for children with special needs to the paediatric assessment unit. Arch Dis Child 2004;89:165-9. https://doi.org/10.1136/adc.2002.019158.
- Emerson E, Kiernan C, Alborz A, Reeves D, Mason H, Swarbrick R, et al. Predicting the persistence of severe self-injurious behavior. Res Dev Disabil 2001;22:67-75. https://doi.org/10.1016/S0891-4222(00)00062-7.
- Glasper EA. Optimising the care of children with intellectual disabilities in hospital. Compr Child Adolesc Nurs 2017;40:63-7. https://doi.org/10.1080/24694193.2017.1309827.
- NHS Benchmarking Network . Benchmarking Learning Disability Services 2018. www.nhsbenchmarking.nhs.uk/nhsi-ld-project-documentation-outputs (accessed 3 November 2021).
- Royal College of Nursing . Connecting for Change: For the Future of Learning Disability Nursing 2017.
- Lenehan C. These Are Our Children. London: Council for Disabled Children; 2017.
- Tuffrey-Wijne I, Goulding L, Giatras N, Abraham E, Gillard S, White S, et al. The barriers to and enablers of providing reasonably adjusted health services to people with intellectual disabilities in acute hospitals: evidence from a mixed-methods study. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-004606.
- Iacono T, Bigby C, Unsworth C, Douglas J, Fitzpatrick P. A systematic review of hospital experiences of people with intellectual disability. BMC Health Serv Res 2014;14. https://doi.org/10.1186/s12913-014-0505-5.
- Lewis P, Gaffney RJ, Wilson NJ. A narrative review of acute care nurses’ experiences nursing patients with intellectual disability: underprepared, communication barriers and ambiguity about the role of caregivers. J Clin Nurs 2017;26:1473-84. https://doi.org/10.1111/jocn.13512.
- Tuffrey-Wijne I, Giatras N, Goulding L, Abraham E, Fenwick L, Edwards C, et al. Identifying the factors affecting the implementation of strategies to promote a safer environment for patients with learning disabilities in NHS hospitals: a mixed-methods study. Health Serv Deliv Res 2013;1.
- Shilling V, Edwards V, Rogers M, Morris C. The experience of disabled children as inpatients: a structured review and synthesis of qualitative studies reporting the views of children, parents and professionals. Child Care Health Dev 2012;38:778-88. https://doi.org/10.1111/j.1365-2214.2012.01372.x.
- Hubner LM, Feldman HM, Huffman LC. Parent communication prompt to increase shared decision-making: a new intervention approach. Front Pediatr 2018;6. https://doi.org/10.3389/fped.2018.00060.
- Wharton S, Hames A, Milner H. The accessibility of general NHS services for children with disabilities. Child Care Health Dev 2005;31:275-82. https://doi.org/10.1111/j.1365-2214.2005.00497.x.
- Brown FJ, Guvenir J. The experiences of children with learning disabilities, their carers and staff during a hospital admission. Br J Learn Disabil 2009;37:110-15. https://doi.org/10.1111/j.1468-3156.2008.00522.x.
- Oulton K, Sell D, Gibson F. ‘LEARN’ing what is important to children and young people with intellectual disabilities when they are in hospital. J Appl Res Intellectual Dis 2018;31:792-803. https://doi.org/10.1111/jar.12433.
- Shields L, Zhou H, Pratt J, Taylor M, Hunter J, Pascoe E. Family-centred care for hospitalised children aged 0–12 years. Cochrane Database Syst Rev 2012;10. https://doi.org/10.1002/14651858.CD004811.pub3.
- Arabiat D, Whitehead L, Foster M, Shields L, Harris L. Parents’ experiences of Family Centred Care practices. J Pediatr Nurs 2018;42:39-44. https://doi.org/10.1016/j.pedn.2018.06.012.
- Uniake S, Browne TK, Shields L. How should we understand family-centred care?. J Child Health Care 2018;22:460-9. https://doi.org/10.1177/1367493517753083.
- Gibson F, Aldiss S, Horstman M, Kumpunen S, Richardson A. Children and young people’s experiences of cancer care: a qualitative research study using participatory methods. Int J Nurs Stud 2010;47:1397-407. https://doi.org/10.1016/j.ijnurstu.2010.03.019.
- Gibson F, Kumpunen S, Bryan G, Forbat L. Insights from parents of a child with leukaemia and healthcare professionals about sharing illness and treatment information: a qualitative research study. Int J Nurs Stud 2018;83:91-102. https://doi.org/10.1016/j.ijnurstu.2018.04.008.
- Mimmo L, Woolfenden S, Travaglia J, Harrison R. Partnerships for safe care: a meta-narrative of the experience for the parent of a child with intellectual disability in hospital. Health Expect 2019;22:1199-212. https://doi.org/10.1111/hex.12968.
- Oulton K, Sell D, Gibson F. Hospitalized children with intellectual disability: parents as partners in their care. J Appl Res Intellect Disabil 2020;33:917-26. https://doi.org/10.1111/jar.12713.
- Oulton K, Heyman R. Devoted protection: how parents of children with severe learning disabilities manage risks. Health Risk Soc 2009;11:303-19. https://doi.org/10.1080/13698570903013631.
- Beresford B. Positively Parents: Caring for a Severely Disabled Child. York: Social Policy Research Unit, University of York; 1994.
- Todd S, Jones S. Looking at the future and seeing the past: the challenge of the middle years of parenting a child with intellectual disabilities. J Intellect Disabil Res 2005;49:389-404. https://doi.org/10.1111/j.1365-2788.2005.00675.x.
- Pelchat D, Levert MJ, Bourgeois-Guerin V. How do mothers and fathers who have a child with a disability describe their adaptation/transformation process?. J Child Health Care 2009;13:239-59. https://doi.org/10.1177/1367493509336684.
- McKeever P. Mothering Chronically Ill, Technology Dependent Children: An Analysis Using Critical Theory 1991.
- Ray LD. Parenting and childhood chronicity: making visible the invisible work. J Pediatr Nurs 2002;17:424-38. https://doi.org/10.1053/jpdn.2002.127172.
- Read J. Disability, The Family and Society: Listening to Mothers. Buckingham: Open University Press; 2000.
- Oulton K, Sell D, Kerry S, Gibson F. Individualizing hospital care for children and young people with learning disabilities: it’s the little things that make the difference. J Pediatr Nurs 2015;30:78-86. https://doi.org/10.1016/j.pedn.2014.10.006.
- Breau LM, Aston M, MacLeod E. Education creates comfort and challenges stigma towards children with intellectual disabilities. J Intellect Disabil 2018;22:18-32. https://doi.org/10.1177/1744629516667892.
- O’Reilly K, Lewis P, Wiese M, Goddard L, Trip H, Conder J, et al. An exploration of the practice, policy and legislative issues of the specialist area of nursing people with intellectual disability: a scoping review. Nurs Inq 2018;25. https://doi.org/10.1111/nin.12258.
- Lewis P, Wilson NJ, Jaques H, O’Reilly K, Wiese M. A qualitative study of nurses’ perspectives of caring for children with intellectual disability and their families in a paediatric acute care setting. J Child Health Care 2019;23:639-51. https://doi.org/10.1177/1367493519867234.
- Hargreaves DS, Sizmur S, Pitchforth J, Tallett A, Toomey SL, Hopwood B, et al. Children and young people’s versus parents’ responses in an English national inpatient survey. Arch Dis Child 2018;103:486-91. https://doi.org/10.1136/archdischild-2017-313801.
- Pelander T, Leino-Kilpi H. Children’s best and worst experiences during hospitalisation. Scand J Caring Sci 2010;24:726-33. https://doi.org/10.1111/j.1471-6712.2010.00770.x.
- Coyne I, Conlon J. Children’s and young people’s views of hospitalization: ‘it’s a scary place’. J Childrens Young Peoples Nurs 2007;1:16-21. https://doi.org/10.12968/jcyn.2007.1.1.23302.
- Rokach A. Psychological, emotional and physical experiences of hospitalized children. Clin Case Rep Rev 2016;2:399-401. https://doi.org/10.15761/CCRR.1000227.
- Wilson ME, Megel ME, Enenbach L, Carlson KL. The voices of children: stories about hospitalization. J Pediatr Health Care 2010;24:95-102. https://doi.org/10.1016/j.pedhc.2009.02.008.
- Coker TR, Rodriguez MA, Flores G. Family-centered care for US children with special health care needs: who gets it and why?. Pediatrics 2010;125:1159-67. https://doi.org/10.1542/peds.2009-1994.
- Leyenaar JK, Rizzo PA, O’Brien ER, Lindenauer PK. Paediatric hospital admission processes and outcomes: a qualitative study of parents’ experiences and priorities. BMJ Qual Saf 2018;27:790-8. https://doi.org/10.1136/bmjqs-2017-007442.
- Balling K, McCubbin M. Hospitalized children with chronic illness: parental caregiving needs and valuing parental expertise. J Pediatr Nurs 2001;16:110-19. https://doi.org/10.1053/jpdn.2001.23157.
- Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. London: SAGE Publications Ltd; 2011.
- Tellis W. Application of a case study methodology. Qual Rep 1997;3. https://doi.org/10.46743/2160-3715/1997.2015.
- Yin RK. Enhancing the quality of case studies in health services research. Health Serv Res 1999;34:1209-24.
- Howard DE, Lothen-Kline C, Boekeloo BO. Using the case-study methodology to teach ethics to public health students. Health Promot Pract 2004;5:151-9. https://doi.org/10.1177/1524839903258223.
- The Association of Chief Children’s Nurses n.d. www.accn.uk (accessed 20 October 2020).
- Community and Mental Health Team, Health and Social Care Information Centre . Learning Disabilities Census Report 2013 n.d. https://files.digital.nhs.uk/publicationimport/pub13xxx/pub13149/ld-census-initial-eng-sep13-rep.pdf (accessed 21 October 2021).
- The Health Foundation . Shine 2012 Final Report: Doctors in Training Leading Quality Improvement: Families Reporting Critical Incidents and Near Misses in a Children’s Hospital n.d. www.health.org.uk/sites/default/files/Shine2012_GreatOrmondStreet_report.pdf (accessed November 2021).
- Talking Mats Limited . Talking Mats n.d. www.talkingmats.com (accessed 20 October 2020).
- Wray J, Hobden S, Knibbs S, Oldham G. Hearing the voices of children and young people to develop and test a patient-reported experience measure in a specialist paediatric setting. Arch Dis Child 2018;103:272-9. https://doi.org/10.1136/archdischild-2017-313032.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277-88. https://doi.org/10.1177/1049732305276687.
- Atkinson P, Coffey A. Making Sense of Qualitative Data: Complementary Research Strategies. London: SAGE Publications Ltd; 1996.
- Great Britain . Equality Act 2010 2010.
- Royal College of Nursing (RCN) . Dignity in Health Care for People With Learning Disabilities 2017.
- National Council for Voluntary Organisations . Get Started With Equity, Diversity and Inclusion 2021. https://knowhow.ncvo.org.uk/organisation/equity-diversity-and-inclusion/get-started-with-equity-diversity-and-inclusion (accessed 8 November 2021).
- Social Change UK . Equality and Equity 2019. https://social-change.co.uk/blog/2019-03-29-equality-and-equity#:~:text=Gender%20Equity%20“If%20equality%20is%20the%20end%20goal%2C,and%20women%20fairly%20based%20on%20their%20respective%20needs (accessed 8 November 2021).
- Northway R. Equality and Equity of Access to Healthcare for People With Intellectual Disabilities 2017. www.intellectualdisability.info/changing-values/articles/equality-and-equity-of-access-to-healthcare-for-people-with-intellectual-disabilities (accessed 8 November 2021).
- Buchholtz N, Stuart A, Frønes TS, Frønes TS, Pettersen A, Radišić J, et al. Equity, Equality and Diversity in the Nordic Model of Education. Springer: Berlin; 2020.
- Belden C. #StayWoke . . . Live Inclusively: Equity Vs. Equality 2017. www.theinclusionsolution.me/staywoke-live-inclusively-equity-vs-equality/ (accessed 8 November 2021).
- Oulton K, Gibson F, Carr L, Hassiotis A, Jewitt C, Kenten C, et al. Mapping staff perspectives towards the delivery of hospital care for children and young people with and without learning disabilities in England: a mixed methods national study. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-2970-8.
- Kenten C, Wray J, Gibson F, Russell J, Tuffrey-Wijne I, Oulton K. To flag or not to flag: identification of children and young people with learning disabilities in English hospitals. J Appl Res Intellect Disabil 2019;32:1176-83. https://doi.org/10.1111/jar.12608.
- Mencap . Getting It Right Charter 2012. www.mencap.org.uk/search/resources?search=charter%26x=0%26y=0 (accessed 1 August 2017).
- Brown M, MacArthur J, McKechanie A, Mack S, Hayes M, Fletcher J. Learning disability liaison nursing services in south-east Scotland: a mixed-methods impact and outcome study. J Intellect Disabil Res 2012;56:1161-74. https://doi.org/10.1111/j.1365-2788.2011.01511.x.
- NHS England . Friends and Family Test n.d. www.england.nhs.uk/fft/ (accessed 24 November 2020).
- Oulton K, Wray J, Hassiotis A, Kenten C, Russell J, Tuffrey-Wijne I, et al. Learning disability nurse provision in children’s hospitals: hospital staff perceptions of whether it makes a difference. BMC Pediatr 2019;19. https://doi.org/10.1186/s12887-019-1547-y.
- Great Britain . Disability Discrimination Act 1995 1995.
- Equality and Human Rights Commission . Your Rights to Equality from Health and Social Care Services. Equality Act 2010 Guidance of Your Rights 2010.
- Mason J, Scior K. ‘Diagnostic overshadowing’ amongst clinicians working with people with intellectual disabilities in the UK. J Appl Res Intellect Dis 2004;17:85-90. https://doi.org/10.1111/j.1360-2322.2004.00184.x.
- Coyne I. Families and health-care professionals’ perspectives and expectations of family-centred care: hidden expectations and unclear roles. Health Expect 2015;18:796-808. https://doi.org/10.1111/hex.12104.
- Kuo DZ, Houtrow AJ, Arango P, Kuhlthau KA, Simmons JM, Neff JM. Family-centered care: current applications and future directions in pediatric health care. Matern Child Health J 2012;16:297-305. https://doi.org/10.1007/s10995-011-0751-7.
- Coyne I, Hallstrom I, Soderback M. Reframing the focus from a family-centred to a child-centred care approach for children’s healthcare. J Child Health Care 2016;20:494-502. https://doi.org/10.1177/1367493516642744.
- O’Connor S, Brenner M, Coyne I. Family-centred care of children and young people in the acute hospital setting: a concept analysis. J Clin Nurs 2019;28:3353-67. https://doi.org/10.1111/jocn.14913.
- Zwaanswijk M, Tates K, van Dulmen S, Hoogerbrugge PM, Kamps WA, Bensing JM. Young patients’, parents’, and survivors’ communication preferences in paediatric oncology: results of online focus groups. BMC Pediatr 2007;7. https://doi.org/10.1186/1471-2431-7-35.
- Somers M. The narrative constitution of identity: a relational and network approach. Theory Soc 2004;23:605-9. https://doi.org/10.1007/BF00992905.
- Sullivan-Bolyai S, Deatrick J, Gruppuso P, Tamborlane W, Grey M. Constant vigilance: mothers’ work parenting young children with type 1 diabetes. J Pediatr Nurs 2003;18:21-9. https://doi.org/10.1053/jpdn.2003.4.
- NHS Improvement . The Learning Disability Improvement Standards for NHS Trusts 2018. www.england.nhs.uk/wp-content/uploads/2020/08/v1.17_Improvement_Standards_added_note.pdf (accessed 21 October 2021).
- Public Health England . Learning Disabilities and CQC Inspection Reports 2018. www.gov.uk/government/publications/learning-disabilities-and-cqc-inspection-reports/learning-disabilities-and-cqc-inspection-reports (accessed 24 November 2020).
- NHS England . Learning Disabilities n.d. www.england.nhs.uk/wp-content/uploads/2017/02/model-service-spec-2017.pdf (accessed 3 November 2021).
- Department for Education and Department of Health and Social Care . Reducing the Need for Restraint and Restrictive Intervention. 2019.
- Nursing & Midwifery Council n.d. www.nmc.org.uk/standards/ (accessed 1 October 2021).
- Great Britain . Mental Capacity Act 2005 2205.
Appendix 1 Selection of phase 2 hospitals
FIGURE 34.
Selection of phase 2 hospitals. LDLN, learning disabilities liaison nurse.
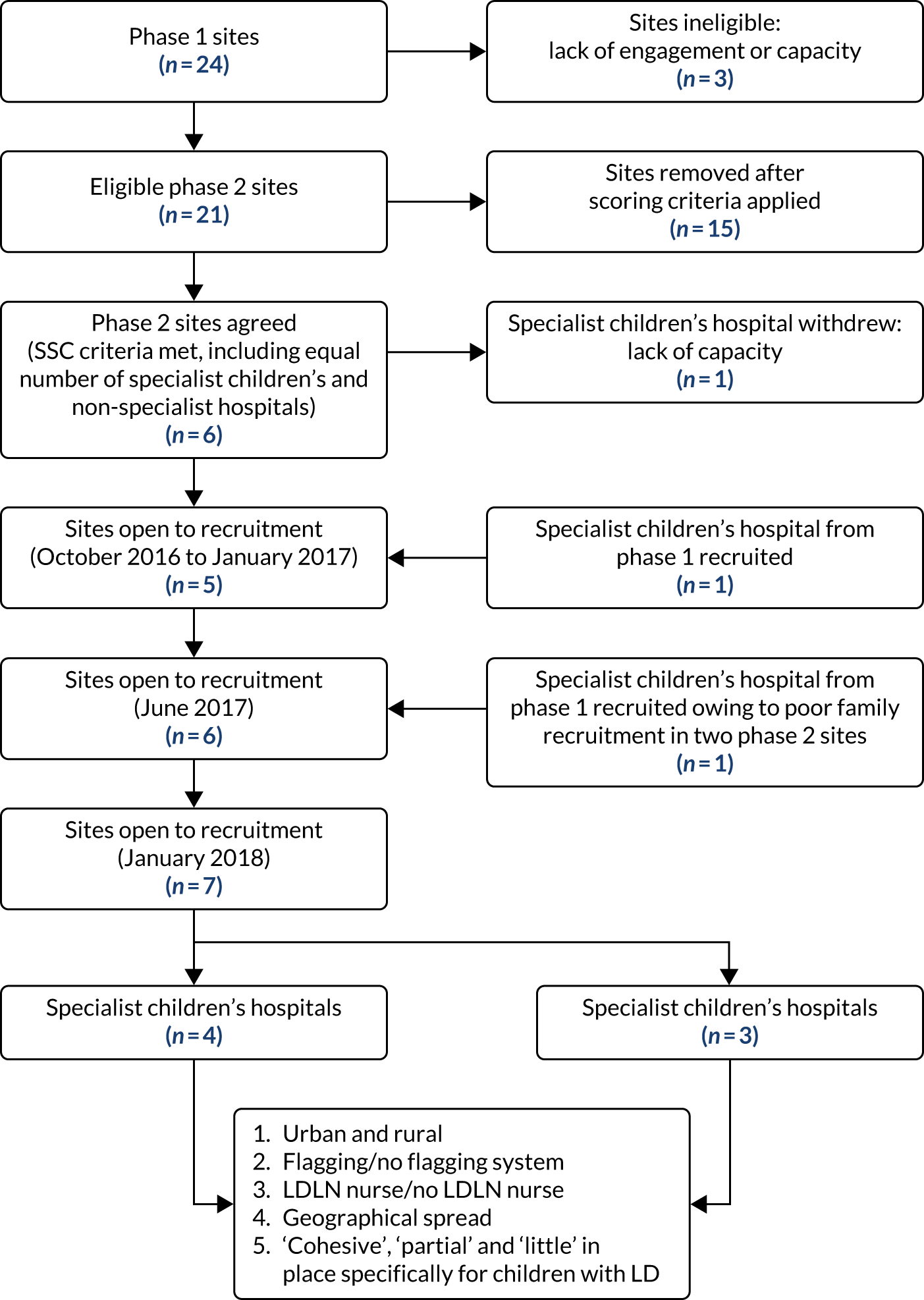
Appendix 2 Inclusion and exclusion criteria
Children
Inclusion criteria
-
Aged ≥ 5 and < 16 years.
-
Known LD or long-term condition.
-
Expected inpatient stay: ≥ 1 night.
-
History of unplanned admissions within previous 2 years (pre-consent LD only).
-
No current formal complaints against the trust or concern for safeguarding.
Exclusion criteria
-
Acute health problem only.
-
No evidence of unplanned admissions in hospital records (pre-consent LD only).
-
Child on the Child Protection Register or researchers at risk of harm by entering the family home.
Parents
Inclusion criteria
-
Able to speak English.
Exclusion criteria
-
None.
Hospital/community staff
Inclusion criteria
-
Has contact with children.
Exclusion criteria
-
No contact with children.
Appendix 3 Selection of additional symbols for data collection with children
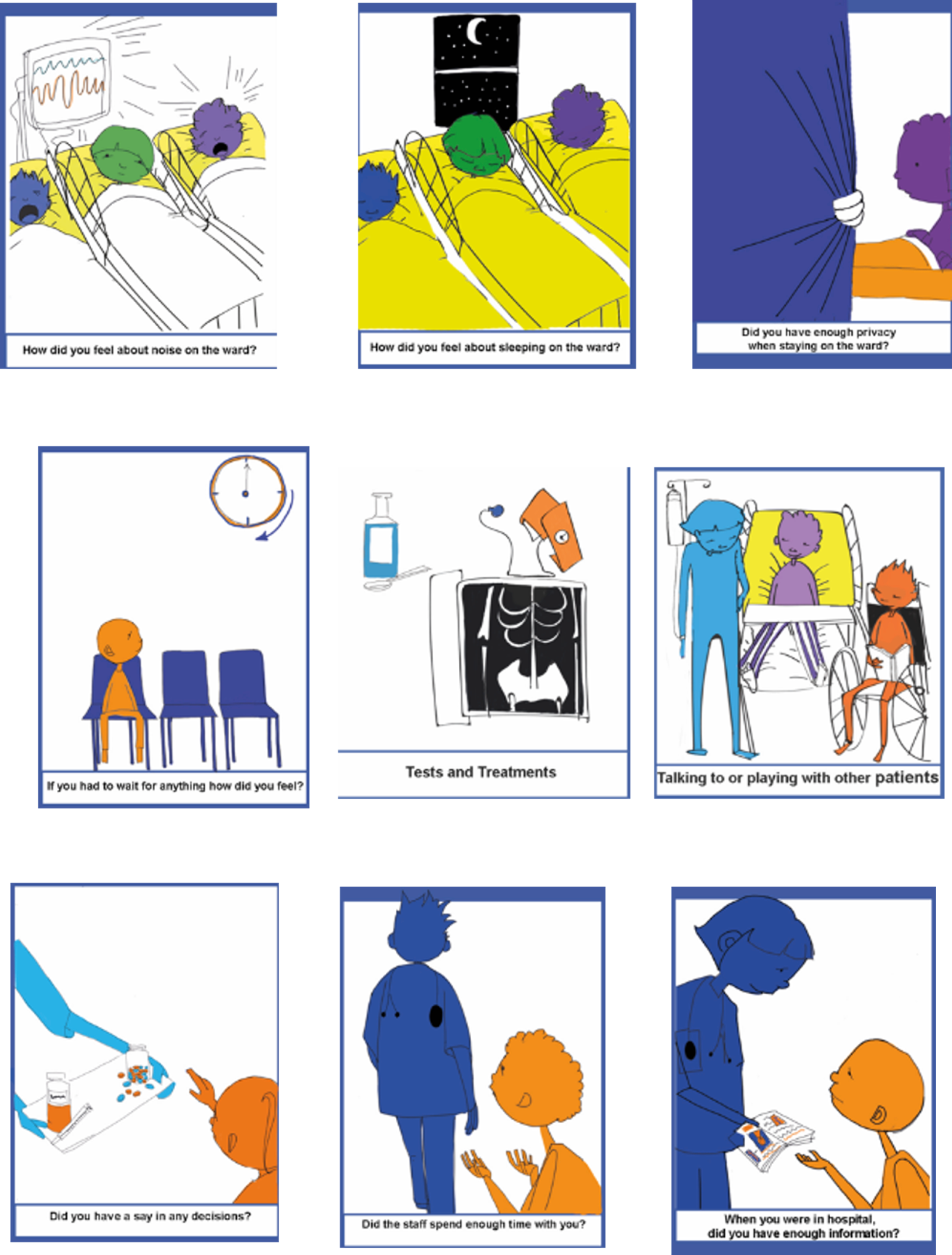
Appendix 4 Composite variables
| Domain | All children’s and non-children’s hospitals | Children’s hospitals | Non-children’s hospitals | Community | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LD, median (IQR) | Non-LD, median (IQR) | Statistics (Wilcoxon test for paired data) | LD, median (IQR) | Non-LD, median (IQR) | Statistics (Wilcoxon test for paired data) | LD Median (IQR) | Non-LD, median (IQR) | Statistics (Wilcoxon test for paired data) | LD, median (IQR) | Non-LD, median (IQR) | Statistics (Wilcoxon test for paired data) | |
| Capacity | 8 (6–10) | 6 (5–8) | z = 27.19; p < 0.001 | 8 (6–10) | 6 (4–7) | z = 23.81; p < 0.001 | 9 (7–11) | 6 (5–8) | z = 13.17; p < 0.001 | Not asked | Not asked | |
| Capability | 7 (6–9) | 5 (3–6) | z = 25.86; p < 0.001 | 7 (6–9) | 4 (3–6) | z = 22.59; p < 0.001 | 7 (6–9) | 6 (4–7) | z = 12.56; p < 0.001 | Not asked | Not asked | |
| Confidence | 8 (6–10) | 5 (4–7) | z = 28.33; p < 0.001 | 8 (6–10) | 5 (4–7) | z = 24.71; p < 0.001 | 8 (6–10) | 6 (4–7) | z = 13.85; p < 0.001 | 8 (6–10) | 7 (6–9) | z = 3.65; p < 0.001 |
| Safety | 7 (6–9) | 6 (4–7) | z = 27.22; p < 0.001 | 7 (6–9) | 6 (4–7) | z = 23.75; p < 0.001 | 8 (6–10) | 6 (4–7) | z = 13.31; p < 0.001 | 7 (5–9) | 7 (5–9) | z = 1.23; p = 0.217 |
| Values | 6 (4–8) | 5 (4–8) | z = 15.58; p < 0.001 | 6 (4–8) | 5 (4–8) | z = 13.92; p < 0.001 | 7 (5–9) | 6 (4–8) | z = 7.14; p < 0.001 | Not asked | Not asked | |
Appendix 5 Hospital staff survey questions for each domain
Capability
-
I have the necessary knowledge and skills to meet their needs.
-
I have the necessary training to meet their needs.
-
I feel able to identify what reasonable adjustments are needed for children and young people with a *long-term condition and learning disabilities.
Capacity
-
I routinely have access to the necessary resources to meet their needs.
-
I routinely have access to additional specialist support to meet their needs.
-
I routinely have access to additional LD specialist staff to meet their needs.
-
I work in an environment that is designed to take into account their individual needs.
-
I feel confident that any reasonable adjustments will be accommodated in a timely way.
Confidence
-
I feel confident to communicate effectively with them.
-
I feel confident to assess and manage pain.
-
I feel confident to safely manage challenging behaviour.
Safety
-
I work in an environment that is safe for meeting their needs.
-
I am always able to deliver safe care.
Values
-
Children and young people with a *long-term condition and learning disabilities are always treated with dignity and respect.
-
Overall I think my trust values children and young people with a *long-term condition and learning disabilities.
*The term learning disabilities was removed from this question when asking staff about children with a long-term condition only.
Appendix 6 Learning disability liaison nurse role descriptors
FIGURE 35.
Learning disability liaison nurse role descriptors.
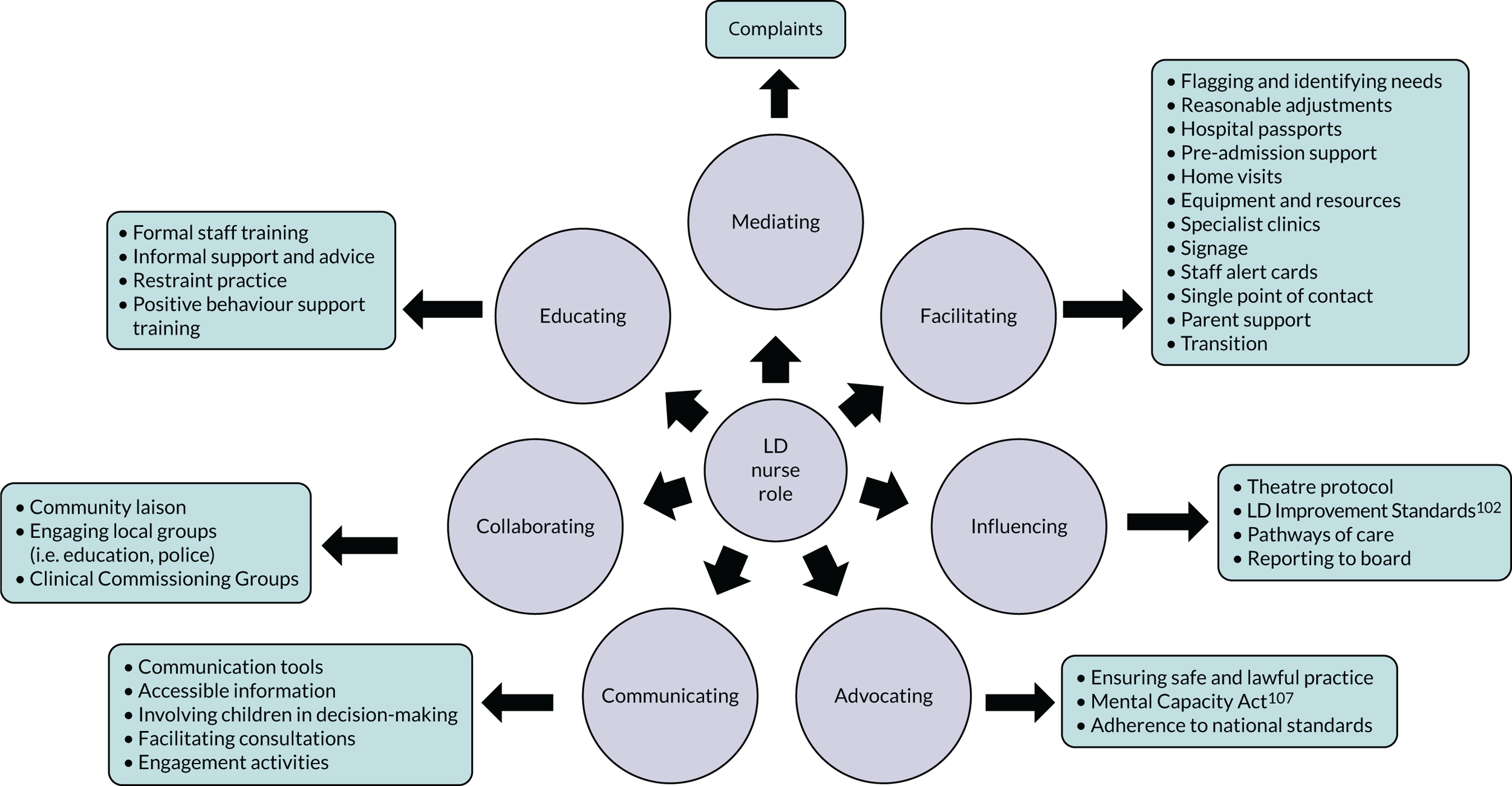
Appendix 7 Staff quotations
I think it’s about not knowing. I don’t think it’s about being lazy . . . People would use the terms ‘learning difficulty’ and ‘learning disability’ interchangeably, and I know there’s a difference, but it wasn’t taught to me at medical school. Well it was taught to me in one lecture . . . I think people are not confident in dealing with those issues, and poorly educated.
Doctor, specialist children’s hospital F
They all have medical care, but not actually that will say what they can and can’t do, what they like or don’t like. I think that something that would be good on the front of a child’s notes was just an all about me type of thing.
Play assistant, non-children’s hospital D
Whether that was dystonia management, pain, tension headaches . . . it was very hard to interpret. I’ve never met a child quite like her. So, you would pull on different resources for her . . . the neurology team, the pain team . . . source out as much information as possible, so there’s always more learning. I wouldn’t be so naive to say, ‘Yes, I know everything.’ I’ll always embrace any learning opportunities from other professionals, yes.
Nurse, specialist children’s hospital F
I have one child with severe LD who doesn’t speak but is very vocal in hand gestures. Communicating to him is really difficult, but because I’ve known him a number of years, I’ve got to know him very well. I think it’s all about building your relationship with the parents. If you can get into how the parents want the child to be spoken to, or treated, and then you can get to a stage where you can understand . . . what the child wants.
Nurse, non-children’s hospital G
I think we rely very heavily on a parent having the ability to relay that child’s need to you . . . I wouldn’t have known tall of this unless the parent then relays it to the nurse in charge and says, ‘look, he’s a bit anxious’.
Nursery nurse, non-children’s hospital I
I now I feel very confident but I’ve been doing it for a long time. I think when I first qualified it was very difficult and I don’t think I did meet the needs of these children because I was always scared to talk to them. Sometimes you’d be scared to go over just because you didn’t know what to expect so you didn’t necessarily give them as much time. I mean, now I’m very confident and I love looking after children with complex needs and disabilities.
Nurse, specialist children’s hospital F
Unfortunately, they see the need and the whole hospital whereas we’re just looking after the children, so I think sometimes we get conflicting situations where what I might think is best for the child is not met because the hospital need is great, if that makes sense.
Nurse, specialist children’s hospital F
A lot of it would be more senior or nursing positions. Where a patient goes, for instance, would not be in my hands. I can do day-to-day management, but decisions that would be beyond the usual scope of reasonable adjustment would be more difficult for me to make.
Doctor, specialist children’s hospital F
We don’t get danger money, get paid to be bit and kicked . . . there was the kid who threw a little brick, I think he was 12. He threw it off my back. I mean that wasn’t assault. I was thinking, ‘What if it gets worse?’ because sometimes they come round and we get these, you can’t say naughty can you, but we get these children with a lot of problems and attitude, on drugs, and they come swaggering on the ward.
Nursery nurse, non-children’s hospital I
Space is limited . . . children with complex needs, who may or may not have a LD, 9 times out of 10 have more things, more belongings with them because they need more equipment, more medicines, more clothes, more changes of things . . . and there’s one locker, bed, chair. You want a clear run to your oxygen suction and you still need to be able to put curtains around and there’s never enough room.
Nurse, specialist children’s hospital F
Appendix 8 Examples of reasonable adjustments made or requested
Providing extra services
-
Giving parents a break.
-
Offering a cubicle.
-
Therapy pet accompanying child to theatre.
-
Agency staff provided to give mum respite.
-
Agency staff provided to give one-to-one care.
-
Provision of learning disability liaison nurse.
-
Use of visual timetables/symbols/photographs.
-
First and double appointments.
-
Access to the play team out of hours.
Changing the way things are done
-
Accommodating siblings overnight.
-
Catering team plating food up in specific way.
-
Child’s dog staying overnight in hospital.
-
Assessment conducted in family home.
-
Learning disability liaison nurse providing training for hospital staff.
-
Decoration of splints or braces with football team badge.*
-
Request for a specific nurse familiar to child.
Providing extra aids
-
Providing specialised beds or mattresses/bed bumpers.
Could not be met.
Appendix 9 Parent quotations
We had, a couple of times, odd doctors come over and say, ‘I’ll just come and go to talk to [child],’ directly, before they’d introduce themselves to either myself and child’s mother. They go to talk to child and of course, he/she doesn’t communicate with strangers anyway. Of course, if they don’t say, ‘Hi, I’m such-and-such. Do you mind if I just talk to him/her a minute?’ We’d then be able to say.
They didn’t really account of the fact of her learning difficulties . . . they were very warm and welcoming to her and spoke to her well . . . didn’t say anything that was too over her head . . . Because it’s a children’s ward they are quite good with how they speak to children, so they do speak to them more like a child, but in her case, that’s quite nice, but jokey and laughing.
The planning wasn’t done appropriately. I’ve done my bit but from their side it should have, you know, been indicated . . . the flashing of the additional needs that should be more visual. . . The important parts should be focused on is the child able to communicate? You know, bits and pieces of that child, so that as a parent I have less to worry about.
I’m more offended by someone not asking than I am someone actually turning round and saying, ‘Not being rude but can [child] speak and communicate? . . . I would rather someone actually have the decency to ask because then they’re showing an interest in child. It makes me feel more relaxed, but then they would actually know their arses from their elbow as to what my son can, can’t achieve or do.
Those notes drive the findings for the likes of the consultants . . . we could have literally stayed at home which was a more appropriate environment for child and called them to let them know . . . It just felt like everybody had just sat back and forgotten about us because it was already been done by somebody else . . . It doesn’t remove your responsibility, you’re still accountable.
You’re always going to have a mixture of nurses that are very good with children with learning difficulties and those that feel quite uncomfortable around them . . . just some general education about autism and learning difficulties and what that means for the child . . . It’s about a lot wider issue and that ignorance isn’t helpful . . . a wider understanding of the basics it was perhaps needed for some members of staff.
I had two different experiences with X-rays. This time that we went in, they were absolutely wonderful and they gave her the time. Last time . . . the guy then had no tolerance . . . there was lots of tutting . . . So, it’s down to individual staff, and that’s at the same hospital, yes, in the same X-ray room.
With child being a special needs child, it’s patience and understanding, and taking things that much slower helps the process for him/her . . . they just seem to have upped their game on all of that, massively . . . It was almost like being in [name of specialist children’s hospital] . . . they must have done some more training.
His arms do go stiff and go straight, and I said, ‘He’ll get his fingers stuck behind there and that’s it’ . . . She [nurse] was an absolute diamond . . . got the foam things. They had tried to change the bed after the op to the padded one . . . but that wasn’t working properly, and then they put him back to the other bed . . . it wasn’t correctly fitted . . . it was a makeshift.
Appendix 10 Demographic data of children in the full data set
| Domain | n (%) |
|---|---|
| Data from children | |
| Boys | 617 (44) |
| Girls | 556 (40) |
| Unknown | 246 (17) |
| Stayed in hospital previously | |
| No | 431 (30) |
| Yes | 736 (52) |
| Unknown | 252 (18) |
| Place where child or young person stayed | |
| Bay | 739 (52) |
| Cubicle | 383 (27) |
| Both bay and cubicle | 36 (3) |
| Unknown | 261 (18) |
| Data from parents | |
| Person completing survey | |
| Mother | 1074 (76) |
| Father | 202 (14) |
| Other carer | 42 (3) |
| Unknown | 101 (7) |
| Child had an operation | |
| Yes | 659 (46) |
| No | 662 (47) |
| Unknown | 98 (7) |
| Age of child (mean, SD); range | 7.03 (5.5) years; 0–18 years |
| Child has a long-term condition only | 355 (25) |
| Child has both LD and a long-term condition | 198 (14) |
| Child has neither LD nor a long-term condition | 814 (57) |
| Unknown | 52 (4) |
| Admission | |
| Planned | 643 (45) |
| Unplanned | 526 (37) |
| Unknown | 250 (18) |
| Day case | 133 (9) |
| Overnight stay | 272 (19) |
| Unknown | 1014 (72) |
| Number of nights, mean (SD; range) | 2.83 (2.34; 0–13) |
| Number of admissions to this hospital in last year | |
| 0 | 631 (44) |
| 1–4 | 613 (43) |
| 5–8 | 64 (5) |
| 9–12 | 17 (1) |
| > 13 | 28 (2) |
| Unknown | 66 (5) |
| Number of admissions to any hospital in last year | |
| 0 | 1025 (72) |
| 1–4 | 253 (18) |
| 5–8 | 32 (2) |
| 9–12 | 10 (1) |
| > 13 | 20 (1) |
| Unknown | 79 (6) |
Appendix 11 Demographic data of the full data set of parents
| Domain | n (%) |
|---|---|
| Age group of parent (years) | |
| < 20 | 66 (4.8) |
| 21–25 | 92 (6.7) |
| 26–30 | 189 (13.8) |
| 31–35 | 268 (19.5) |
| 36–40 | 297 (21.7) |
| 41–45 | 189 (13.8) |
| 46–50 | 118 (8.6) |
| > 50 | 91 (6.6) |
| Not known | 61 (4.4) |
| Main language spoken at home | |
| English | 1193 (87.0) |
| Other European language | 30 (2.2) |
| Asian language | 40 (2.9) |
| African language | 6 (0.4) |
| Other | 18 (1.3) |
| Not known | 84 (6.1) |
| Education level of parent/carer completing questionnaire | |
| Primary | 57 (4.2) |
| Secondary | 454 (33.1) |
| Graduate | 355 (25.9) |
| Postgraduate | 214 (15.6) |
| Not known | 291 (21.2) |
| Employment status of parent/carer completing questionnaire | |
| Unemployed | 191 (13.9) |
| Full-time work | 458 (33.4) |
| Part-time work | 372 (27.1) |
| Full-time carer | 148 (10.8) |
| Part-time carer | 16 (1.2) |
| Not known | 186 (13.6) |
| Impact of having a child with a medical condition on employment | |
| No impact | 808 (58.9) |
| Had to leave work to care for child | 162 (11.8) |
| Not been able to return to work | 59 (4.3) |
| Not progressed as far in job | 30 (2.2) |
| Had to reduce number of hours worked | 129 (9.4) |
| Had to increase number of hours worked | 8 (0.6) |
| Not known | 175 (12.8) |
| Impact of having a child with a medical condition on partner’s employment | |
| No impact | 786 (57.3) |
| Had to leave work to care for child | 66 (4.8) |
| Not been able to return to work | 26 (1.9) |
| Not progressed as far in job | 24 (1.8) |
| Had to reduce number of hours worked | 81 (5.9) |
| Had to increase number of hours worked | 13 (0.9) |
| Not known/not applicable | 375 (27.4) |
Appendix 12 Demographic data of phase 3 participants
| Domain | LD population (N = 198), n (%) | Non-LD population (N = 355), n (%) |
|---|---|---|
| Data from children | ||
| Boys | 97 (49) | 150 (42) |
| Girls | 74 (37) | 152 (43) |
| Unknown | 27 (14) | 53 (15) |
| Stayed in hospital previously | ||
| No | 27 (14) | 37 (10) |
| Yes | 144 (73) | 264 (74) |
| Unknown | 27 (14) | 54 (15) |
| Place where CYP stayed | ||
| Cubicle | 66 (33) | 129 (36) |
| Bay | 95 (48) | 154 (43) |
| Both bay and cubicle | 9 (5) | 14 (4) |
| Unknown | 28 (14) | 58 (16) |
| Data from parents | ||
| Child had an operation | ||
| No | 76 (38) | 187 (53) |
| Yes | 114 (58) | 158 (45) |
| Unknown | 8 (4) | 10 (3) |
| Age of child (years), mean (SD) | 8.67 (4.76) | 8.24 (5.67) |
| Admission | ||
| Planned | 120 (60) | 195 (55) |
| Unplanned | 58 (29) | 117 (33) |
| Unknown | 20 (10) | 43 (12) |
| Number of nights, mean (SD) | 3.38 (2.52) | 3.24 (2.91) |
| Number of admissions to this hospital in last year | ||
| 0 | 72 (36) | 110 (31) |
| 1–4 | 100 (51) | 181 (51) |
| 5–8 | 11 (6) | 35 (10) |
| 9–12 | 4 (2) | 11 (3) |
| ≥ 13 | 8 (4) | 14 (4) |
| Unknown | 3 (2) | 4 (1) |
| Number of admissions to any hospital in last year | ||
| 0 | 124 (63) | 230 (65) |
| 1–4 | 48 (24) | 93 (26) |
| 5–8 | 10 (5) | 13 (4) |
| 9–12 | 3 (2) | 5 (1) |
| ≥ 13 | 7 (4) | 9 (3) |
| Unknown | 6 (3) | 5 (1) |
| Domain | LD population (N = 198), n (%) | Non-LD population (N = 355), n (%) |
|---|---|---|
| Age group of parent (years) | ||
| ≤ 20 | 12 (6) | 11 (3) |
| 21–25 | 6 (3) | 20 (6) |
| 26–30 | 17 (9) | 48 (14) |
| 31–35 | 35 (18) | 70 (20) |
| 36–40 | 47 (24) | 67 (19) |
| 41–45 | 33 (17) | 48 (14) |
| 46–50 | 22 (11) | 37 (10) |
| > 50 | 22 (11) | 39 (11) |
| Not known | 5 (3) | 15 (4) |
| Main language spoken at home | ||
| English | 181 (91) | 315 (89) |
| Other European language | 2 (1) | 3 (< 1) |
| Asian language | 6 (3) | 10 (3) |
| African language | 0 (0) | 3 (< 1) |
| Other | 2 (1) | 4 (1) |
| Not known | 8 (4) | 20 (6) |
| Education level of parent/carer completing questionnaire | ||
| Primary | 11 (6) | 16 (5) |
| Secondary | 80 (4) | 120 (34) |
| Graduate | 37 (19) | 94 (26) |
| Post graduate | 32 (16) | 58 (16) |
| Not known | 39 (20) | 67 (19) |
| Employment status of parent/carer completing questionnaire | ||
| Unemployed | 23 (12) | 44 (12) |
| Full-time work | 42 (21) | 104 (29) |
| Part-time work | 37 (19) | 105 (30) |
| Full-time carer | 65 (33) | 49 (14) |
| Part-time carer | 6 (3) | 5 (1) |
| Not known | 26 (13) | 48 (14) |
| Impact of having a child with a medical condition on employment | ||
| No impact | 74 (37) | 168 (47) |
| Had to leave work to care for child | 54 (27) | 50 (14) |
| Not been able to return to work | 19 (10) | 24 (7) |
| Not progressed as far in job | 8 (4) | 19 (5) |
| Had to reduce number of hours worked | 26 (13) | 62 (17) |
| Had to increase number of hours worked | 1 (1) | 1 (< 1) |
| Not known | 17 (9) | 31 (9) |
| Impact of having a child with a medical condition on partner’s employment | ||
| No impact | 86 (43) | 169 (48) |
| Had to leave work to care for child | 17 (9) | 18 (5) |
| Not been able to return to work | 8 (4) | 12 (3) |
| Not progressed as far in job | 8 (4) | 10 (3) |
| Had to reduce number of hours worked | 22 (11) | 35 (10) |
| Had to increase number of hours worked | 4 (2) | 7 (2) |
| Not known/not applicable | 54 (27) | 104 (29) |
List of abbreviations
- 24/7
- 24 hours a day, 7 days a week
- ACCN
- Association of Chief Children’s Nurses
- ADHD
- attention-deficit hyperactivity disorder
- DVD
- digital versatile disc
- EEG
- electroencephalogram
- GOSH
- Great Ormond Street Hospital
- GP
- general practitioner
- IQ
- intelligence quotient
- LD
- learning disability
- PPI
- patient and public involvement
- RQ
- research question
- SSC
- Study Steering Committee
- VILD
- visual individualised Likert display
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/NWKT5206).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
