Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 06/85/11. The contractual start date was in November 2010. The draft report began editorial review in May 2016 and was accepted for publication in September 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Peymane Adab reports grants from the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme, the NIHR Public Health Research (PHR) programme, the Wellcome Trust, the National Prevention Research Initiative, the China Medical Board and Yong Ning Pharmaceuticals Ltd, during the conduct of the study; she is a topic expert committee member for the National Institute for Health and Care Excellence (NICE)’s Public Health Advisory Committee ‘Maintaining a healthy weight and preventing excess weight gain among children and adults’, an expert member on the NICE Programme Development group on ‘Lifestyle weight management services for overweight and obese children and young people’ and a member of the PHR Research Funding Board. Janet E Cade reports grants from the development of (1) other dietary assessment tools and (2) a website to support improved dietary assessment, outside the submitted work. In addition, she has a patent on other dietary assessment tools (not the one used here) licensed, and the University of Leeds is planning a spin-out company based on other work supporting dietary assessment tools (myfood24) – this was not used in the study reported here. Paramjit Gill reports grants from the NIHR HTA programme, the NIHR Programme Grants for Applied Research (PGfAR) programme, the NIHR Efficacy and Mechanism Evaluation programme and the Medical Research Council during the conduct of the study; he is a trustee of the charity South Asian Health Foundation and a director of the NICE National Collaborating Centre for Indicator Development, which develops and pilots quality indicators, including lifestyle, which may be implemented through the UK Quality and Outcomes Framework. Emma R Lancashire reports grants from the NIHR HTA programme during the conduct of the study. Eleanor McGee reports grants from the University of Birmingham outside the submitted work during the conduct of the study. Miranda J Pallan reports grants from the NIHR HTA programme and Yong Ning Pharmaceuticals Ltd outside the submitted work. Jayne Parry reports personal fees from the NIHR PGfAR programme outside the submitted work. Sandra Passmore received funding from the Mondelez International Foundation for Health for Life in primary school programme to develop healthy lifestyles among children and their families and is a consultant with Birmingham City Council Public Health on childhood obesity. Jonathan Deeks is a member of the HTA Commissioning Strategy Group and the HTA Commissioning Board and is chairperson of the HTA Efficient Study Designs-2 Board; he is also an investigator on several NIHR HTA programme grants.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Adab et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Epidemiology of childhood obesity
Childhood obesity has been classed as one of the most serious public health challenges of the 21st century,1 affecting around 41 million children aged < 5 years, with a projected increase to 70 million by 2025. 2 Children who are overweight are at a higher risk of adverse physical health,3 emotional4 and social5 consequences during childhood. Furthermore, children who are obese, even from the age of 7 years, and irrespective of their adult weight status, are at higher risk of premature mortality in adulthood than their normal-weight counterparts. 6,7 There is evidence of tracking of lifestyle health behaviours from an early age, such that more than half of very overweight children become obese adults,8 with a consequent increased risk of cardiometabolic and respiratory disease, as well as a higher risk of some cancers and musculoskeletal complications in adulthood. 9,10 This high risk of morbidity has resulted in obesity being designated a ‘disease’ in the USA. 9 The estimated cost of overweight and obesity to the UK economy was £20B (£4.2B to the UK NHS and £15.8B indirect costs) in 2007. 11
In England, data from the most recent population survey showed that around one-third of children aged 2–15 years had excess weight (overweight or obese). 12 Annual surveillance data are also available from the National Child Measurement Programme, which undertakes measurements of height and weight in all primary school children at school entry (aged 4–5 years) and during their last year at school (aged 10–11 years). These data show that during the primary school years the proportion of children with excess weight increases from one-quarter to around one-third, and the proportion who are very overweight doubles (from 9% to 19%). 13 More detailed examination of these data show that certain subgroups are at higher risk. Although there is relatively little inequality in the prevalence of childhood obesity at the age of 4–5 years, during the primary school period an increasing gap in prevalence develops, with a higher increase among boys than among girls, among children of South Asian and African Caribbean ethnicity than among children of white ethnicity and among children from more deprived households than among children from less deprived households. 14 Longitudinal studies suggest that persistent obesity is established by the age of 11 years. 15
All of the above evidence highlights the primary school age period as a critical window for preventative intervention.
Causes of childhood obesity
A large number of observational studies have examined the causes of childhood obesity. A recent evidence review by the National Institute for Health and Care Excellence (NICE) summarised the modifiable behaviours that are likely to affect healthy weight maintenance and prevent weight gain in adults and children. 16 Although, essentially, this can be achieved by adopting healthy eating habits and increasing levels of physical activity (PA), there is no single dietary component or particular type of PA that will solely contribute to weight maintenance; rather, a combination of approaches is always needed.
Reviews of interventional studies suggest that, for weight maintenance, children should be encouraged to aim to undertake at least 60 minutes of moderate to vigorous physical activity (MVPA) over the course of each day. 17 In terms of the dietary components and patterns that are associated with obesity, the evidence is less consistent. Nevertheless, there is good evidence that the moderate consumption of ‘Mediterranean’-style diets (higher fruit and vegetable and fibre content) and a limit on the intake of energy-dense or high-fat foods, as well as high-sugar foods and drinks, are associated with weight maintenance. 16 However, translating this knowledge into behaviour change is complex, as are factors influencing children’s diet and PA levels. 11
Existing research on childhood obesity prevention
Numerous systematic reviews have summarised the evidence on interventions aimed at preventing childhood obesity, the main two of which18,19 [both published after the West Midlands ActiVe lifestyle and healthy Eating in School children (WAVES) trial had started] are reported in detail below.
A Cochrane review,18 first published in 2001 and updated in 2005 and 2011, reviewed 55 prevention trials. These included studies in school, community, health and family settings that targeted a range of ages. Interventions were aimed at improving diet, increasing PA or a combination of the two. Studies with both short- and longer-term follow-up were included. Of the included trials, 50 were from high-income settings, including six from the UK. The majority of trials were aimed at children aged 6–12 years and were delivered in school settings. Data from a subset of 37 of the studies were combined in a meta-analysis (n = 27,946 children) and showed that, overall, these interventions were effective with a small clinical effect, reducing the body mass index z-score (BMI-z) by –0.15 units relative to the control group.
However, there was much heterogeneity in study design, types of intervention and outcome measurements, which limited the ability to draw any firm conclusions. The positive impact of interventions also varied, with some, but not all, improving diet, PA or other outcomes, and impacts being sometimes limited to just boys or just girls. Many of the included studies were of low quality, did not include sufficient sample size to assess effects on weight status and did not sufficiently report on implementation factors to allow wider adoption, and none reported on cost-effectiveness. Longer-term follow-up was also lacking. Equity of intervention, in terms of sex and ethnicity, and any adverse effects were not always assessed.
Although the review concluded that there was strong evidence of school-based interventions – particularly those targeting children aged 6–12 years – having a positive impact on weight status, there was insufficient evidence of the particular components that should be recommended or how such programmes should be implemented in a variety of settings. Commonly included intervention components that seemed to be associated with positive results included school curricula that included healthy eating and PA, increased sessions for PA in the school week, an improvement in the nutritional quality of the school food supply, supportive environments and cultures, support for teachers and parental support to encourage home activities. In terms of research needs, the review concluded that future trials need strong evaluation designs that capture process implementation, longer-term outcomes and equity of effects, and that consider potential harms and cost-effectiveness.
The second comprehensive review was undertaken by the US Agency for Healthcare Research and Quality, which included the findings of studies published up to April 2013. 19,20 This review included data from 147 studies, of which 115 were mainly school based, and the majority of which had been conducted in the USA within the previous 10 years. At least half of the studies reviewed demonstrated a positive effect of school-based interventions on some measure of adiposity, particularly when there was also a home component. Diet-only interventions were generally more successful than PA-only programmes. The review concluded that the evidence for an effect of school-based interventions on weight status was moderate (lower strength of evidence than the conclusions from the Cochrane review)18 and that interventions were more likely to be successful if they were more intense and of longer duration, promoted environmental change as well as providing education, and targeted multiple settings (school, home and community).
Other reviews generally have similar conclusions, suggesting that interventions that target single behaviours are generally less successful,21,22 whereas multicomponent interventions have more chance of having a positive impact. 23,24 However, conclusions are inconsistent about the duration of interventions and those intervention components that are likely to have most effect. 25
In summary, although multifaceted school-based interventions have the potential to prevent weight gain and obesity in children, the results of previous studies are inconsistent and the combination of components most likely to be effective is not clear. Previous studies were not always adequately powered, the basis for interventions was sometimes unclear, process implementation was inadequately reported and long-term outcomes were rarely assessed. A major gap is the reporting of the cost-effectiveness of interventions.
Aims and objectives
In this trial, we sought to address the main methodological weaknesses identified in previous studies. The aim was to assess the clinical effectiveness and cost-effectiveness of a multifaceted, 12-month, school-based intervention aimed at preventing overweight and obesity in primary school children. The intervention was developed and refined using the framework recommended by the Medical Research Council (MRC) for complex interventions. 26 We included a sample size that was large enough to detect clinically significant differences in adiposity, used a range of measures of adiposity and psychosocial effects, included objective measures of PA and diet intake and incorporated a cost-effectiveness evaluation (see Chapter 7), a comprehensive process evaluation (see Chapter 4) and an assessment of longer-term effects (up to 27 months post intervention completion). As the intervention was delivered through schools, the school (cluster) was the main unit of analysis and appropriate cluster-level adjustments were made (see Chapter 2 for a more detailed description).
The research questions were:
-
How effective is the theory-based WAVES study intervention package, delivered at school level, in reducing adiposity in primary school-aged children, compared with usual practice?
-
For how long do any observed effects persist after active intervention has ceased?
-
What is the incremental cost-effectiveness ratio (ICER) of supplying the WAVES study obesity prevention intervention?
-
How effective is the intervention package at improving diet and increasing PA, compared with usual practice?
-
What is the effect of the intervention on quality of life and body image dissatisfaction?
-
Does the intervention work differently by sex, ethnicity, level of deprivation or baseline weight status?
Chapter 2 Methods
Trial design
The WAVES study was a cluster randomised controlled trial evaluating the clinical effectiveness and cost-effectiveness of an obesity prevention intervention programme delivered to primary school children in year 2 (aged 6–7 years). The unit of randomisation was the school. A 1 : 1 (intervention-to-control) allocation ratio was applied using a blocked balancing algorithm for the randomisation procedure.
Participants
Clusters (schools)
All state-maintained primary schools in the West Midlands region of the UK located within a 50-km radius of the study co-ordinating centre and including school years 1–5 (school years in which measurements were scheduled to take place) were eligible for inclusion. Schools were excluded that, at the point of recruitment, were in special measures (a status applied by the Office for Standards of Education in England to schools failing to give their pupils an acceptable standard of education, and the persons responsible for leading, managing or governing the school not demonstrating the capacity to secure the necessary improvement in the school) and schools with < 17 pupils (minimum cluster size) in the relevant school year group. The sampling frame included schools from the following local education authorities: Birmingham Central, Birmingham North, Birmingham South, Coventry, Dudley, Sandwell, Shropshire, Solihull, Staffordshire, Stoke-on-Trent, Telford and Wrekin, Walsall, Warwickshire and Wolverhampton.
Participants (school pupils)
Within each participating school, all children in year 1 (aged 5–6 years), the school year when baseline measurements were undertaken, were eligible for inclusion.
Outcomes
Schools participating in the WAVES study became involved in two groups [group 1 (G1) and group 2 (G2)], with initial involvement of each group being 12 months apart. The WAVES study had four individual participant-level data collection points split across eight measurement periods: baseline (G1 schools May–July 2011 and G2 schools April–July 2012), follow-up 1 (FU1: 3 months post intervention, G1 schools September–December 2012 and G2 schools September–December 2013), follow-up 2 (FU2: 18 months post intervention, G1 schools January to March 2014 and G2 schools January to March 2015) and follow-up 3 (FU3: 27 months post intervention, G1 schools only September–December 2015). Subject to individual verbal assent, participating individuals took part in a variety of assessments undertaken by trained researchers following standardised operating procedures. Outcome measures included in the data collection were the same at each time point, with the exception of FU3, when Actiheart® monitors (CamNtech Ltd, Papworth, UK), used to objectively measure levels of PA, were not fitted. Weighing scales were serviced and calibrated biannually, and skinfold callipers and blood pressure monitors were serviced and calibrated annually. Children were asked to wear light clothing for all of the physical measurements and to remove their shoes and socks for the measurement of their height and weight.
Individual participant-level outcomes
Primary outcomes
The primary outcome is the difference in BMI-zs between control and intervention arms at first and second follow-up. (UK 1990 reference curves were used to allocate BMI-zs at all time points. 27) Data required for BMI-zs were height, weight, sex and age. Height was measured in duplicate to the nearest 0.1 cm using a portable stadiometer (Leicester Height Measure, Invicta Plastics Ltd, Leicester, UK). When the readings differed by > 0.4 cm, an additional reading was taken (see Appendix 1). Provided that there were two height measurements within 0.4 cm of each other, a definitive height was calculated as the average of the two closest readings or, in instances of no two closest readings, the average of all three readings. Weight (see Appendix 2) was measured to the nearest 0.1 kg using a Tanita bioimpedance monitor (Tanita BC-420MA Class III, Tanita Corporation, Tokyo, Japan). Age was calculated in days from date of birth (obtained either directly from the parent or from school records) and date of measurement (recorded on each measurement sheet; see Appendix 3). Sex was obtained either directly from the parent or from school records and was verified at the point of measurement. A body mass index (BMI) value was then calculated by dividing weight in kilograms by height in metres squared. UK 1990 growth reference charts were then used to produce an age- and sex-specific BMI-z for each child from their calculated BMI value. 27,28
Secondary outcomes
Waist z-score
Waist circumference was measured in duplicate to the nearest 0.1 cm using a flexible, non-stretch, cloth tape measure. When the readings differed by > 0.4 cm, an additional reading was taken (see Appendix 4). Provided that there were two waist circumference measurements within 0.4 cm of each other, a definitive measurement value was calculated as the average of two closest readings or, in instances of no two closest readings, the average of all three readings. UK 1990 growth reference curves were then used to produce an age- and sex-specific waist z-score from the definitive waist circumference measurement value.
Skinfold measurement
Skinfold thickness was measured in duplicate to the nearest 0.1 cm at five sites: biceps, suprailiac, subscapular, thigh and triceps. When the readings differed by > 0.4 cm, an additional reading was taken (see Appendix 5). All of the measurements were undertaken on the non-dominant side (the side of the child’s non-writing hand) using Holtain Tanner/Whitehouse skinfold callipers (Holtain Ltd, Crymych, UK). Provided that there were two site-specific skinfold measurements within 0.4 cm of each other, a definitive site-specific measurement value was calculated as the average of two closest readings or, in instances of no two closest readings, the average of all three readings. The ‘sum of four skinfolds’ outcome is the sum of the definitive skinfold measurement values for biceps, subscapular, suprailiac and triceps.
Bioimpedance and body fat percentage
In addition to measuring weight, the Tanita monitor uses bioelectrical impedance analysis technology to calculate body fat percentage. Age, height and sex are entered into the monitor and this information is used together with the weight measured and bioelectrical impedance (assessed through a low, safe signal, which is sent through the body from two electrodes that are built into the foot sensor pads) to calculate body fat percentage. In addition, a bioimpedance value in ohms is provided and this is also reported.
Dietary intake
An instrument developed by the University of Leeds for use in children aged 3–7 years, the Child And Diet Evaluation Tool (CADET), was used to asses dietary intake. The version used was slightly modified from that initially described;29 details of all of the modifications are provided below. CADET provides a 24-hour record of consumption using a 115-item prospective tick list with no necessity to record quantity or weight of the food/drink item. CADET is designed for completion on a school day and, for ease of completion, intake is split into a school diary and a home diary, with seven distinct time periods in total: morning break, lunchtime, afternoon break on the school diary; and before tea/after school, evening meal/tea, after tea/during night and the following day breakfast/before school on the home diary. In the original CADET, breakfast data were routinely collected at school.
For the WAVES study, trained researchers recorded all of the items of food and drink consumed at school by participating children during one school day. On that same day, before the end of school, children were given a home food diary for completion by a parent/carer. Detailed written instructions for completion with illustrative examples were provided in addition to an instructional digital versatile disc (DVD) that could be watched by parents/carers. The following day, a researcher visited the school to collect and evaluate the returned home food diaries. If a child had an incomplete home food diary, or when it was clear that the diary had not been completed correctly, a one-to-one dietary recall was undertaken with the child when possible. Data collected in this way were then processed through the CADET nutrient analysis programme by the Nutrition Epidemiology Group at the University of Leeds. This programme converts the tick list data for each child into macronutrient and micronutrient intakes for the 24-hour data collection period using age- and sex-specific portion sizes. Only participants with both school and home food diary data were included. In addition, it was agreed in advance that CADET records with > 50 ticks for the 24-hour time period were unlikely to have been completed correctly and, therefore, such individuals are excluded from all analyses using dietary intake outcome data.
Updated macronutrient and micronutrient information from the latest UK nutrient databank30 published in 2015 [McCance and Widdowson’s The Composition of Foods: Seventh Summary Edition (MW7)] was used in the CADET nutrient analysis programme for the WAVES study. In addition, to take account of new and deleted food categories in MW7, the weighting of databank food items that make up each CADET-listed food was updated in the CADET nutrient analysis programme in 2015 by the University of Leeds Nutritional Epidemiology Group via the following process.
-
Average food consumption frequencies for 3- to 11-year-olds for food items were extracted from the food level dietary data set of the National Diet and Nutrition Survey Rolling Programme (NDNS-RP) (years 1–4: 2008–9 to 2011–12). 31
-
These frequencies were grouped into MW7 food categories, an example of which is shown in Table 1. There were five MW7 milk categories that were included in the CADET listed food ‘Milk, milky drink, lassi’ (CADET code a1).
-
Consumption frequency proportions were calculated to determine the overall weighting as a percentage for each MW7 category within each CADET listed food [e.g. the percentage of whole-milk of the total milk drunk by children aged 3–11 was calculated to be 35% (see Table 1)].
-
When MW7 food categories had very small frequencies of consumption, professional judgement and food industry knowledge were employed to amalgamate categories to simplify the list of MW7 foods used.
-
Such judgements were cross-checked by another member of the team.
| CADET code | CADET description | MW7 food category description | NDNS updated weightings (%) |
|---|---|---|---|
| a1 | Milk, milky drink, lassi | Milk, soya, non-dairy alternative to milk, unsweetened, fortified | 5 |
| Milk shake, powder, made up with semi-skimmed milk | 2 | ||
| Milk, whole, pasteurised, average | 35 | ||
| Milk, semi-skimmed, pasteurised, average | 56 | ||
| Milk, skimmed, pasteurised, average | 2 |
The age- and sex-specific average food portion sizes used in the CADET nutrient analysis programme are based on mean food intakes from the 1997 National Diet and Nutrition Survey (NDNS),32 which collected weighed food intake data from large nationally representative samples of children and young people. The more recent NDNSs did not collect weighed data and it was therefore felt that portion size estimates from these may be less accurate than using the 1997 data. Age- and sex-specific portions of individual foods using 1997 NDNS data had been provided to the Leeds Nutritional Epidemiology Group, together with suggested weightings to group these further into CADET listed foods by Wendy Wrieden and Karen Barton when they worked for the University of Dundee. (The same data were used to produce aggregated portion data for their 2008 publication. 33) These data were used in earlier calculations of age- and sex-specific portion sizes for items included in the CADET tick list. For the WAVES study, in 2015, the Leeds Nutritional Epidemiology Group determined portion sizes for use in the CADET nutrient analysis programme as follows.
-
All age- and sex-specific portion sizes for items included in the CADET tick list were recalculated using the original 1997 NDNS data provided by the University of Dundee.
-
Despite the relatively large NDNS sample size, some age/sex groups were small, meaning that for some foods the original age- and sex-specific portion size could have been based on data from as few as one individual, which, in some instances, resulted in large portion size fluctuations across the age groups. Portion sizes were manually smoothed using portion sizes from adjacent age groups when it was felt necessary. Table 2 shows boys’ portion sizes for chicken curry before and after smoothing: the smoothed portion size for boys aged 4 years (80) was calculated from the average of the portion size for boys aged 3 and 5 years (70 and 90) because the original value appeared to be too low.
-
In some cases of missing data, portion sizes from similar foods were used; for example, portion sizes that had been determined for ‘nuts’ (CADET code b8) were also used for ‘seeds’ (CADET code k22).
-
For a small number of occurrences of missing data (when one or more age- and sex-specific portion size for a particular item could not be estimated from the 1997 NDNS data), recent non-weighed data from the NDNS-RP (2008–9 to 2011–12)31 were used to estimate portion size. For example, age- and sex-specific portion sizes for ‘beans and pulses’ from the recent NDNS-RP data were used as estimated portion sizes for the CADET listed foods ‘Lentils, dahl’ and ‘Other beans and pulses’ (CADET codes k20 and k21).
| Portion sizes | Male age (years) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Original | 70 | 23 | 90 | 180 | 163 | 140 | 158 | 195 | 196 |
| Smoothed | 70 | 80 | 90 | 180 | 163 | 140 | 158 | 195 | 196 |
Such judgements were cross-checked by another member of the team.
The food and nutrient intake data were used to calculate mean energy intake in kilojoules (kJ) and mean intake in grams of fruit and vegetables, fat and fibre (based on the Englyst method). 34 From the individual data for 24-hour combined fruit and vegetable intake in grams, a binary variable was created to identify children who met the current government recommendation for daily fruit and vegetable consumption of at least five portions. The ‘5 A Day’ campaign in England35 accurately defines fruit and vegetable portion sizes for adults. However, for children, although the consumption of at least five portions of a variety of fruit and vegetables is recommended, as requirements vary with age, body size and levels of PA, only a rough guide – ‘the amount they can fit in the palm of their hand’ – is provided in terms of the amount that constitutes a portion. More quantifiable portion size information is provided, however, by the Northern Ireland Public Health Agency,36 which states that a child portion is ‘roughly half an adult portion’. The number of portions consumed was, therefore, determined based on the definitions from England’s ‘5 A Day’ campaign but halving the number of grams for fresh, frozen or tinned varieties of fruit and vegetables as well as for dried fruit. Therefore, children were assigned one portion per 40 g of fresh, frozen or tinned fruit and vegetables or 15 g of dried fruit consumed. An additional portion was also assigned for the reporting of both fruit juice/smoothie consumption and beans/pulses consumption: multiple servings of these items still contributed only one portion to their total portion intake. Individuals for whom the number of portions determined in this way was five or more were classified as meeting the current government recommendation for children’s consumption of fruit and vegetables.
Free sugar, often referred to as ‘added sugar’ or ‘non-milk extrinsic sugar (NMES)’, is not listed in the latest nutrient databank and is therefore not part of the standard output from CADET. To split the total grams of sugar provided by CADET into free and intrinsic sugar, the food items from CADET were mapped to the nearest available food in the 1997 NDNS. The total, free and intrinsic sugar amounts for the mapped NDNS foods were used to calculate free and intrinsic sugar proportions. The free sugar proportion was then applied to the total sugar amount in the recent UK nutrient bank to obtain a value in grams for free sugar. For example, if a MW7 food had a total sugar amount of 10 g per 100 g and the mapped NDNS equivalent food had a free sugar proportion of 40%, the amount of free sugar allocated within CADET to the MW7 food would be 4 g per 100 g. This was completed for all foods in the CADET nutrient analysis programme (used for the processing of the WAVES study dietary data) and a weighted average was calculated for each of the 115 food categories included in CADET. These data were used to obtain a mean non-milk extrinsic sugar intake in grams during the 24-hour period.
Physical activity
Children wore a combined heart rate and movement sensor (Actiheart)37 attached to the chest with two standard ECG electrodes initialised to record in 30-second epochs. The children were asked to wear the monitor continuously (including during sleep and any water-based activities) for 5 days (including a weekend) and to continue with their usual behaviour (see Appendix 6).
Free-living heart rate data were preprocessed38 and combined with trunk acceleration to derive activity intensity (J/minute/kg) time series using a branched equation framework. 38 Heart rate data were individually calibrated using a group equation based on age, sex and sleeping heart rate derived from submaximal response to a bicycle ergometry exercise in a similarly aged population of Finnish children39 using a previously described modelling methodology. 40
Periods of non-wear were inferred from the combination of non-physiological heart rate and prolonged periods of zero acceleration, which were taken into account to minimise potential diurnal bias when summarising time series data into participant-level summary measures.
Total PA energy expenditure (kJ/day/kg) was summarised, along with its underlying intensity distribution in 0.25 metabolic equivalent (MET) increments (1 MET defined as 118 J/minute/kg ≈5.8 ml O2/minute/kg).
Total movement volume was summarised as average acceleration along with its underlying movement intensity distribution using only the acceleration signal (including for the definition of non-wear). Time spent at specific movement intensities includes MVPA, defined as time spent above the acceleration threshold of 1.75 m/second2 and expressed in minutes per 24 hours; sedentary time is defined as time when acceleration is ≤ 0.075 m/second2 (includes time when sleeping) and is expressed as hours per 24 hours. From the former (time spent in at least moderate activity), a binary variable was created to classify children as either achieving or not achieving the current government minimum PA recommendation for children aged 5–18 years41 of engaging in MVPA for at least 60 minutes every day.
Only children who had at least 24 hours of valid data, distributed as at least 6 hours in each quadrant of the day (morning 03.00 to 09.00, noon 09.00 to 15.00, afternoon 15.00 to 21.00, and midnight 21.00 to 03.00), were included to ensure representation of the whole 24-hour period42 and to further minimise potential diurnal bias.
Health-related quality of life
The child (aged 5–7 years) self-report version of the Paediatric Quality of Life inventory (PedsQL),43 the social acceptance domain of KIDSCREEN-5244 and the Child Health Utility 9D (CHU9D) were used to assess health-related quality of life (HRQL). PedsQL is a validated questionnaire that considers physical, emotional, social and school functioning. These aspects of quality of life are considered separately; emotional, social and school functioning are combined to consider psychosocial functioning, and all four are combined to assess overall quality of life. The social acceptance domain of KIDSCREEN-52 was used to assess bullying. Although the KIDSCREEN-52 domain is validated for use only in slightly older children (aged 8 years), no alternative instrument was available that had been validated for use in children aged 5–6 years. All PedsQL scores have a minimum value of 0 and a maximum value of 100. The KIDSCREEN-52 domain has a score range of 3–15. For both instruments, higher scores indicate a better quality of life. CHU9D45,46 was also administered for use in the health-economic analysis. It is a paediatric, generic, preference-based measure of HRQL. It consists of a descriptive system and a set of preference weights, giving utility values for each health state that is described by the descriptive system, thus allowing the calculation of quality-adjusted life-years (QALYs) for use in cost–utility analyses (CUAs). A description of the HRQL dimensions it assesses, and the scoring mechanism used, is provided in Chapter 7 (see Outcomes/Measuring quality-adjusted life-years). All three instruments were interviewer administered at all time points (see Appendix 7).
Weight status categories
The age- and sex-specific BMI-zs (previously described) were used to classify individuals into four weight status categories, based on the UK 1990 centile cut-off points for population monitoring of weight status: ≤ 2nd centile = underweight; > 2nd centile to < 85th centile = healthy weight; ≥ 85th centile to < 95th centile = overweight; and ≥ 95th centile = obese. Two binary weight status variables were then created: (1) ‘obese’ compared with ‘not obese’ and (2) ‘obese/overweight’ compared with ‘not obese/overweight’.
Blood pressure
Blood pressure was measured in duplicate using a clinically validated, automated oscillometric blood pressure monitor (BpTRU BPM-100, BPTRU Medical Devices, Conquitlam, BC, Canada) with the correct cuff size for each child. All measurements were taken on the right arm, with the child in a seated position, and children were asked to remain still and silent throughout. The first measurement was taken after a 3-minute seated rest. A second measurement was then taken after a 3-minute minimum rest interval. If an error reading occurred, or one of the first two values was outside the normal range, a third reading was taken, again after a 3-minute minimum rest interval (see Appendix 8). A definitive systolic and diastolic value was then calculated. Initially, all of the readings in which either the systolic or the diastolic value was > 20 mmHg above the 99.6th centile of the UK age- and sex-specific blood pressure reference data were excluded as implausible. 47 Unpaired readings, owing to an error reading being returned by the monitor for either the systolic or the diastolic blood pressure value, were then excluded. The remaining systolic and diastolic blood pressure values were then treated independently. When a value was available from only one reading, this was taken as the definitive value. When values from two readings were available, then the definitive value was taken as the average of these two values. When values were available from three readings, then the definitive value was taken as the average of the two closest values or, in instances of no two closest values, the average of all three values.
Body image satisfaction
Body image was assessed using the Child’s Body Image Scale. This is a body image assessment tool for children and consists of seven sex-specific photo images of children who ranged from very thin to obese. 48,49 The instrument was interviewer administered. Each child was shown the appropriate sex-specific range of photo images. Initially, they were asked to select the image that looked most like them (underweight = 1 to obese = 7) and then the image that showed the way that they would like to look. A body image satisfaction score was then calculated by subtracting the second score (the way that they would like to look) from the first score (looked most like them). A score of ‘0’ indicated body image satisfaction (as the child looked like they would like to look). A negative value indicated that the child would like to be fatter; a positive value indicated that the child would like to be thinner, with greater body dissatisfaction the higher the magnitude of the value. To enable dissatisfaction to be considered irrespective of whether the direction was towards wanting to be fatter or wanting to be thinner, the negative values were converted into positive values for use in the body image satisfaction analyses.
Additional variables used in the analysis
Socioeconomic status
The postcode of each participant was requested at baseline and obtained either from school records or directly from the child’s parent/carer. This was used to obtain the Index of Multiple Deprivation (IMD) 2010 score for the area in which each child was living at baseline, as a measure of socioeconomic status. In addition, participants were split into five deprivation groups using quintile cut-off points for England, such that group 1 comprised all of the individuals living in an area classified as being among the 20% most deprived in England and group 5 comprised those living in an area classified as being among the 20% most affluent.
Ethnicity
Ethnic group data, using the classification recommended for use in England by the Office for National Statistics and used in the England and Wales 2011 Census,50 were obtained either from school records or directly from the parent/carer of participating children. These data were then split into four ethnic groups: (1) white (including English, Welsh, Scottish, Northern Irish and British); (2) South Asian (including Bangladeshi, Indian and Pakistani); (3) black (including African and Caribbean); and (4) other ethnic group (including Irish, Gypsy or Irish Traveller, any other white background, white and black Caribbean, white and black African, white and Asian, any other mixed/multiple ethnic background, Chinese, any other Asian background, any other black/African/Caribbean background, Arab, and any other ethnic group).
Intervention implementation level
Schools were classified into three groups (low, medium and high) based on the level of overall implementation fidelity achieved. A detailed description of the methods used is provided in Chapter 4 (see Methods, Assimilation of process evaluation data). The two schools allocated to the intervention arm of the trial that did not implement any components of the intervention programme were universally allocated a score of ‘0’ and were included in the low-implementation fidelity group for the subgroup analyses.
Cluster-level outcomes
In order to inform the sampling procedure and to be of use in the fully adjusted models, school-level data were obtained from all local education authorities in the West Midlands, UK. The latest data available at the time of request were for the 2009–10 school year. The school characteristics requested included school size (number of pupils on roll), the percentage of the school population who were white, the percentage of the school population who were South Asian (including Bangladeshi, Indian and Pakistani), the percentage of the school population who were black (including African and Caribbean) and the percentage of the school population eligible for a free school meal (as an indicator of the socioeconomic make-up of the school population). These are subsequently referred to as baseline school characteristics. In addition, at baseline, head teachers of both control and intervention schools were requested to complete a school questionnaire. The questionnaire aimed to gather information on activities already being undertaken, facilities that were available and the general environment in relation to healthy eating and PA at each participating school (see Appendix 9).
Sample size
As the planned analysis of the WAVES study included adjustment for baseline measurements, power calculations were based on repeated-measures methods using estimates of correlation between before and after measurements. Sample sizes were then inflated and compared with those required for individual randomisation, using the design effect, to account for the randomisation being at the cluster level and making allowance for the variation in cluster sizes. 51
The important summary statistics used to inform the sample size calculations were based on estimates from an analysis of data from a previous study52 involving eight schools and for which baseline and follow-up measurements by control and intervention arms were available. From these data we estimated the intracluster correlation coefficients (ICCs) and the correlation between the before and after measurements. Two outcomes were considered: (1) BMI-z (ICC = 0.01, 95% CI 0 to 0.04, estimated correlation between before and after measurements = 0.9) and (2) percentage of children overweight or obese (ICC = 0, 95% CI 0 to 0.02, estimated difference between before and after measurements = 0.7).
At the protocol stage, previous experience indicated that for schools agreeing to take part, an average number of 43 pupils would be recruited, and the planned sample size and estimation of power it would provide was based on this but also allowed for variation in cluster size [standard deviation (SD) = 23]. However, experience during the initial phase of pupil recruitment for the WAVES study suggested that the average number of pupils recruited per school would be only about 25. Funding for the trial meant that a maximum of a little over 50 schools could be recruited, and it was estimated that there would be a pupil dropout rate of 20% during the course of the study. Revised power calculations were therefore undertaken, based on a final sample size of 1000 children split among 50 clusters.
In relation to the primary outcome of BMI-z, such a sample size provides > 90% power to detect a change of 0.25 z-scores under all probable estimates for the ICC (0, 0.01 or 0.04). A change of 0.25 z-scores is equivalent to approximately 0.5 kg of body weight for a 7-year-old child and has been shown to be associated with clinically detectable benefits in obese adolescents. 53 It also provides > 80% power to detect a change of 0.125 z-scores under more conservative estimates of the ICC (95% CI 0 to 0.009). This sample size also provides > 80% power to detect a difference (between control and intervention schools) in the percentage of children being overweight or obese of about 7% (exact value dependent on baseline values).
All power calculations were carried out in Stata 13 (StataCorp, College Station, TX, USA) using the ‘sampsi’ function with the analysis of covariance method (for repeated measures) and then inflated by the appropriate design effect.
Sequence generation
The unit of randomisation was the school. Schools that had agreed to participate in the study were randomised to either the intervention or the control arm using a blocked balancing algorithm. 54,55 Essentially, this algorithm randomly selected one of a number of allocation designs that minimised the imbalance between a set of prespecified covariate means. The covariates included within this algorithm were percentage of pupils eligible for free school meals, percentage of South Asian pupils within the school, percentage of black African Caribbean pupils within the school, percentage of white pupils within the school, percentage of other ethnic group pupils within the school and number of pupils within the school. The first 27 schools (G1 schools) were randomised in the first block, and 1 year later the second 27 schools (G2 schools) were randomised in the second block, conditioning the balancing algorithm for the first block allocations. For G1 schools, the balance algorithm was implemented to balance on means. In G2 schools, some covariates exhibited a significant departure from normality and a transformation was used to improve the normality assumptions of the balance algorithm. This transformation was selected using the ‘ladder of powers’ function in Stata, and the transformation with the lowest chi-squared value. Covariates transformed were percentage white pupils (log), percentage other ethnic group pupils (square root) and percentage black African Caribbean pupils (square root). In this way, balance was achieved across all allocations.
Allocation concealment mechanism
Allocation to either the control or the intervention arm of the trial was at the cluster (school) level. Randomisation for each group of participating schools took place after completion of baseline measurements, such that both schools and their participating year 1 pupils were not informed of arm allocation (to ensure concealment of allocation) until after consent to participate had been obtained.
Implementation
The trial co-ordinator undertook the school enrolment procedure from a weighted random sample of all eligible schools. The sampling procedure and subsequent randomisation of participating schools were undertaken by the trial statistician.
A weighted random sample of schools was used to try to ensure sufficient representation among participating schools to enable subgroup analysis by minority ethnic group. School populations were stratified by ethnic mix: white, South Asian (comprising Bangladeshi, Indian and Pakistani), black (comprising African and Caribbean) and other ethnicity (comprising all other ethnic groups). Schools were dichotomised as either being or not being in the top 80th percentile in terms of black or South Asian pupil representation in their overall school population. Schools with a higher minority ethnic population (in the top 80th percentile for black or South Asian representation) were given an increased chance of selection with a ratio of 3 : 1 to create a weighted random sample of 200 schools. Schools in this sample were ordered using a random number generator, and seven were excluded as they did not meet the eligibility criteria.
Study invitation letters (followed by telephone calls starting approximately 2 weeks later) were then sent sequentially to the head teachers of the remaining schools. It was anticipated that the relatively large number of clusters being recruited (> 50) should ensure balance across three other important factors [urban/rural location, school size and proportion of children eligible for a free school meal (as an indicator of the socioeconomic make-up of pupils in the school)], such that a range of these school characteristics would be represented. However, regular checks for response bias in terms of these factors as well as ethnic mix were undertaken by the trial statistician, as a precaution, during the school enrolment period.
In schools that had agreed to take part, all of their pupils in year 1 (aged 5–6 years) were eligible for inclusion in the study. Invitation letters, together with a detailed information leaflet about the study and a parental consent form, were sent to schools for distribution. Members of the research team visited schools to explain the study to the eligible children and to provide them and their parents with an opportunity to ask any questions that they might have. Consent for participation in the study by both schools and eligible pupils was completed before the trial statistician randomised schools to either the control or the intervention arm of the trial. Parental consent for the full set of measures (measurements and questionnaires) was gained through an opt-in consent process for both G1 and G2 schools. However, following lower than anticipated pupil recruitment for G1 schools, an additional opt-out consent was introduced for G2 schools. The opt-out consent covered a more limited set of measures (height, weight, blood pressure and all child questionnaires). It was implemented, when possible, in schools in which pupil recruitment was falling short of the anticipated mean cluster size of 25. As would be expected, this occurred more frequently in one class entry schools with only one Year 1 class in which a much higher proportion of consents was required to achieve the anticipated mean cluster size of 25 consented pupils.
Blinding
Owing to the nature of the intervention, blinding of schools or participating pupils was not possible. Although all of the data collection staff were blind to arm allocation at baseline, for logistical reasons it was not possible to blind members of the core research team for follow-up data collection periods. However, the majority of data collection was undertaken by teams of sessional staff, with only supervision by a member of the core research team. The main responsibility in terms of measurements for the core research team staff was the set-up and fitting of monitors to objectively measure PA, although, on occasion, involvement of these staff in other measurements was required. The sessional staff, responsible for the majority of data collection, were not advised of arm allocation, but it is possible that the trial arm could have been revealed to them by a comment from either a member of school staff or one of the pupils from whom data were being collected. To try to assess the frequency of sessional staff becoming unblinded to arm allocation, these staff were asked to complete a questionnaire on termination of employment (for a visual representation of blinding through the progress of the study, see Figure 7).
Chapter 3 Interventions
Control schools
Schools had to agree to take part in the trial knowing that they had an equal chance of being randomised to either the control or the intervention arm. To encourage school agreement to participate, it was considered important (based on findings from the feasibility study) that all schools, irrespective of trial arm allocation, should receive something in addition to the experience of being involved in the trial. During the recruitment process, invited schools were advised that if allocated to the control arm of the trial, the school would be provided with some resources suitable for year 2 personal, social and health education lessons. Resources that had already been developed and did not cover the topic area of health or healthy lifestyle behaviours were identified. These were sent to all control schools at the start of the autumn term of the intervention year. The resources provided were:
-
‘Your World, My World’ resource from Oxfam (Oxford, UK), exploring the lives of four children from around the world (www.oxfam.org.uk/education/resources/your-world-my-world)
-
‘Climate Cops’ resource from Npower (Npower Ltd, Swindon, UK) – a teaching toolkit on electricity and energy.
In addition, schools local to Birmingham received information about the ‘Teddy Bear Hospital’, a service provided by medical students at the University of Birmingham. The service involves medical students visiting schools free to provide a children’s teddy bear clinic with the aim of dispelling any fears about health-care professionals and promoting relevant health and safety issues in a fun, educational manner.
The educational resources were provided to all of the control schools, but how and whether or not the materials were used was the choice of each individual school.
Intervention schools
Schools that were allocated to the intervention arm of the trial were asked to deliver each component of the WAVES study multifaceted intervention programme to all children in year 2 (aged 6–7 years), irrespective of whether or not the child’s parent had consented for them to be involved with the study measurements and, therefore, participate in the trial.
The WAVES study intervention was developed by combining the available research evidence with theory that was informed through qualitative research with relevant stakeholders56 and guided by the MRC framework for complex interventions. 57 We first identified the most promising intervention strategies from systematic reviews of childhood obesity prevention studies. Among 70 included studies within eight systematic reviews, we summarised the intervention components, target behaviour and type of activity. We then conducted focus groups with a range of stakeholders (including parents and school staff) to explore those that were perceived to be the most important and feasible to implement. We considered intervention techniques (e.g. reward behaviours, role model, exposure to PA opportunities), activities (e.g. education materials, parenting classes, cooking workshops) and particular settings (e.g. school curriculum, community setting). Prioritised ideas were checked against available local resources and, with input from an expert group, the intervention package was formed. There were two broad intervention aims: (1) increasing children’s PA levels through school and (2) supporting health behaviour skill development in families through activity-based learning. 56
The intervention was further refined following a feasibility study among children from eight primary schools. 52 The aim of the finalised intervention was to target both the home and school environment, using a variety of behaviour change strategies to increase the level of PA and improve the quality of the children’s diet. Based on findings from earlier qualitative studies, the intervention was introduced to participants as a healthy lifestyle programme. The programme, delivered through school over a 12-month period, had four main components: signposting, additional daily PA programmes to be run in school, cooking workshops and Villa Vitality. A summary is provided below, followed by a more detailed description of each component.
WAVES study intervention programme summary
Signposting
Aim: to increase children’s PA levels outside school with their family.
Method: information sheets were provided for the children to take home, highlighting facilities in the local area and simple ways to increase activity levels. Motivational messages were also included.
Intervention techniques: to provide information on when and where to perform behaviour.
Delivered by: delivered to the school by the WAVES study research team; handed out to the children by class teachers.
Timescale: G1 schools, July 2011 and September–October 2011; G2 schools, July 2012 and September–October 2012.
Physical activity programmes to be run in school
Aim: to encourage children to be physically active and more specifically to increase children’s PA levels by 30 minutes per day during school time.
Method: teachers were asked to select the two most suitable PA programmes for their school, from four offered, to assist them in increasing their children’s PA during school time.
Intervention techniques: environmental restructuring, prompt practice.
Delivered by: class teachers, teaching assistants (TAs) or lunchtime supervisors (depending on school).
Timescale: G1 schools, September 2011–July 2012; G2 schools, September 2012–July 2013.
Cooking workshops
Aim: to improve nutrition knowledge, cooking skills and dietary habits of children and their families (specifically, to encourage the consumption of more fruits, vegetables and high-fibre foods and reduce the consumption of high-sugar and high-fat foods).
Method: the WAVES study research team provided training and materials for school staff to enable them to deliver short lessons on healthy eating and cooking workshops for children and parents – one workshop per school term.
Intervention techniques: to provide information on the consequences of behaviour in general, model/demonstrate behaviour, prompt practice and prompt generalisation of behaviour.
Delivered by: school staff (nominated by the school).
Timescale: one session per term, three in total throughout the school year – G1 schools, 2011–12 academic year; G2 schools, 2012–13 academic year.
Staff training: a 1-day training course run at the University of Birmingham – G1 schools, October 2011; G2 schools October 2012 (two dates offered per year). Attended by school staff who were involved in delivering the cooking workshops at each school.
Villa Vitality
Aim: to use role models to motivate children to adopt healthy lifestyles, with a focus on nutrition and PA.
Method: children were invited to take part in a programme encouraging healthy lifestyle behaviours run by Aston Villa Football Club (AVFC), but also involving weekly challenges and a class project delivered by class teachers.
Intervention techniques: to provide information on the consequences of behaviour in general, model/demonstrate behaviour, prompt practice and prompt generalisation of behaviour.
Delivered by: AVFC and school teachers for challenges and class projects.
Timescale: run during the spring and summer terms: G1 schools, 2011–12 academic year; G2 schools, 2012–13 academic year.
Detailed description of each WAVES study intervention component
Signposting
The signposting component aimed to encourage families to be active over the summer and guide them to local PA opportunities. Prior to the summer holidays, the year 1 class teachers gave an information sheet to all of the children in their classes and asked them to take it home to their parents. This sheet highlighted simple ways to increase levels of PA, such as walking, cycling or visiting the park, and setting weekly achievement goals as a family (see Appendix 10).
During the summer holidays, members of the research team developed school-specific signposting sheets. These outlined activities available within the local area that were suitable for year 2 children, including local play areas, recreational grounds and leisure centres, as well as sports and activity clubs. Prior to printing and distribution, at the start of the autumn term (G1 schools, September 2011; G2 schools, September 2012), the signposting sheets were sent to head teachers to give them the opportunity to suggest extra items for inclusion and check that they felt that all of the items included were appropriate. Once approval of a final version had been obtained, the sheets were distributed at each school to all children [who had now moved into year 2 (aged 6–7 years)] as early as possible in the autumn term. For an example of one of the signposting sheets, with the school name and logo removed, see Appendix 11.
Physical activity programmes to be run in school
The aim of this component was to increase children’s PA in school. The target was to achieve an additional 30 minutes of PA per day, over and above what they were already doing. Four different activity programmes were offered to schools, from which they were asked to select the two that they felt would most suit their school. To avoid additional time required for changing into physical education (PE) kit and, therefore, to make it easier for the activities to be slotted into the timetable, all programmes offered could be undertaken with children wearing their school uniform. All programmes also allowed for a degree of flexibility, enabling teachers to tailor delivery to suit their individual class. It was anticipated that there might be concern from teachers that the time taken out of the school day for the activity component might have a negative impact on academic education. To try to dispel this concern, teachers were advised that feedback from schools with previous experience of the programmes indicated that teaching time lost from the addition of the PA programmes into the timetable is regained through greater concentration and improved behaviour and attitudes towards schooling. All programme materials were delivered to class teachers by a member of the research team, who spent time introducing teachers to the resource and also took the opportunity to remind them that the aim was to increase children’s activity levels by 30 minutes every day during school time. Class teachers were encouraged, if possible, to participate in the activities with their class pupils, acting as role models.
Programmes offered
The Wake Up Shake Up programme58 (Figure 1) involves children following aerobic-type activity routines (5–10 minutes) to music (shown on a self-explanatory DVD). There are different routines for children to work through gradually and, in addition, they can design their own routines as they become more competent. The routines can be fitted into any part of the school day and no extra equipment is required; all of the activities are focused on different movements. The Wake Up Shake Up DVD resource is sufficiently comprehensive for teachers to get started straight away. The aerobic type routines are reasonably energetic, so it was recommended for Wake Up Shake Up to be completed either in classrooms that have a sufficiently large area for activity or in an area such as the school hall. For further information about Wake Up Shake Up, see www.wakeupshakeup.com/.
FIGURE 1.
Wake Up Shake Up. Reproduced with permission from Wake Up Shake Up Productions (Wadebridge, UK).

Activate59 (Figure 2) involves progressive repeated patterns of movement to music. The programme is designed for use in the morning and just after lunch, but the activities can be used spontaneously at any time of day. Activate programmes are repeated for 2 weeks at a time and become progressively more difficult over a developmental 36-week structure. In addition, extra activity extensions can be introduced at a speed to suit the class. No extra equipment is needed; all of the activities are focused around different movements. The Activate pack was sufficiently comprehensive to allow teachers to start implementing the programme as soon as the research team delivered the materials to the school. An information pack was provided as well as a DVD and music compact disc (CD) to guide teachers through the programme. For further information about Activate, see www.valsabinpublications.com/publications/activate/.
FIGURE 2.
Activate. Reproduced with permission from Val Sabin Publications and Training (Northampton, UK).

Positive Play60 (Figure 3) is a resource designed to be used during school playtimes. It provides staff with a wide range of games and activities, for both outdoor and indoor use, as well as guidance and recommendations for organisation. Some (but not all) activities included required equipment such as cones, bean bags, balls and hoops. It was recommended that delivery of this programme took place when possible in the school playground/playing fields or an inside space in the case of bad weather. Teachers were advised that this programme could be used to deliver only half of the 30-minute target of additional daily activity when used during school breaks or lunchtime. For further information about Positive Play, see www.positiveplay.co.uk/.
FIGURE 3.
Positive Play. Reproduced with permission from Val Sabin Publications and Training.
Take 10: Fit to Succeed61 (Figure 4) is a resource that provides ideas with easy-to-follow guidance on how to incorporate 10- to 15-minute bursts of PA into a child’s school day. The activities are grouped into six categories: (1) action rhymes, (2) co-ordination and manipulation challenges, (3) running and chasing games, (4) activities for small spaces, (5) aerobics and (6) skipping. The activities require minimum preparation, as clear instructions are provided in the manual (and, for some activities, a DVD). Some (but not all) of the activities required equipment such as bean bags, balls and skipping ropes. Many of these activities are suitable for use in the classroom. Bursts of activity can be formally scheduled into the timetable, for example first thing in the morning and after lunch, but they can also be used more spontaneously. They can be incorporated into different areas of the curriculum to support learning, for example during personal, social and health education, numeracy, literacy and science. The games are easy to link with, or adapt to, any topic being taught. A number of activities, such as those found in the running and chasing games and skipping section, are designed to be used in the playground or gym to encourage PA during break times. These can also be used by schools to encourage PA during lunch breaks. Teachers were advised that this programme could be used to deliver only half of the 30-minute target of additional daily activity when used during school breaks or lunchtime. As four categories of the programme include a mixture of both physically active and sedentary activities, teachers were provided with a chart for these categories (see Appendix 12), indicating those activities that were suitable for contributing towards the 30-minute daily activity target of the WAVES study PA component. There is no detailed website for Take 10: Fit to Succeed, but to access the materials for the programme see www.take10.org.uk/ (owned and published by Babcock LDP).
FIGURE 4.
Take 10: Fit to Succeed. Reproduced with permission from Babcock LDP (Exeter, UK).

Cooking workshops
The aim of the cooking workshop component of the WAVES study intervention was to improve the dietary behaviours of children and their families through increased nutrition knowledge, food preparation skills and confidence in preparing healthy meals. The workshops and associated resources were developed by research nutritionists who were part of the WAVES study research team, but content and materials were sent to the relevant study co-investigator for approval. The workshops were designed to be delivered by school staff following attendance at a training day run by the WAVES study research team. It was recommended that at least two members of staff per year 2 class attended the workshop training (see Appendix 13). Each workshop was preceded by three or four short lessons delivered to the children in the classroom 1–2 weeks before each workshop. The aim of these lessons was to encourage children to start thinking about the key nutrition messages that would be covered in the workshop. Intervention schools received a payment of £380 to cover the cost of teacher cover for the cooking workshop training and the purchasing of perishable items for the actual cooking workshops. Schools were asked to invite all parents of year 2 children to attend each cooking workshop.
For each workshop, teachers were provided with the following:
-
an invitation letter to parents (see Appendix 14)
-
a workshop advertising poster (see Appendices 15–17)
-
lesson presentation slides and notes (see Appendices 18–27)
-
a workshop session plan (see Appendices 28–30)
-
workshop presentation slides and notes (see Appendices 31–33)
-
parent workshop information sheets (see Appendices 34–36)
-
resources required for the activities and interactive games (see Appendices 37–47).
There were three cooking workshops during the intervention year, one per term, of 60–90 minutes’ duration each. Each workshop covered a different eating occasion: breakfast, lunch and snacks and simple evening meals. The same key simple nutrition messages ran across all workshops to try to reinforce the lifestyle behaviours being encouraged:
-
to increase intake of fruit, vegetables and fibre
-
to reduce intake of sugar and fat.
To help both children and parents follow the workshop presentations and understand the key messages covered, a 6-year-old character called Bert was created. Throughout the workshops Bert was presented to participants in a variety of different scenarios. All workshops involved an element of food preparation, but cooking facilities required were kept intentionally very minimal owing to a general lack of facilities available within UK primary schools at the time of the study. Chopping boards and knives, together with preparation equipment and serving bowls/plates, were provided by the research team, and the only equipment required for delivery was a kettle or another means of boiling water for the third, simple evening meals workshop. In addition to practising food preparation skills, the workshops also included education messages to try to improve nutrition knowledge of both children and parents and a variety of interactive games that aimed to reinforce the information being delivered. All of the workshops could be delivered in the classroom if a school did not have a more suitable location available (such as a school hall).
Breakfast cooking workshop and classroom lessons
Breakfast classroom lesson content
Breakfast classroom lesson 1 covered (1) the importance of eating breakfast every day to help children concentrate at school and be physically active both during PE and during break time and lunchtime, and (2) the fact that cereals are a healthy breakfast option and that high-fibre cereals are healthier because they keep you fuller for longer, are lower in sugar, help blood sugar levels to rise steadily, help to prevent constipation and can prevent some diseases, such as heart disease and diabetes mellitus, as children get older. This was followed by an activity during which children were shown slides containing pictures of different cereals and asked whether they thought it was a cereal that it would be good to eat every day or if it was a cereal best eaten only as a treat and not every day.
Breakfast classroom lesson 2 was about bread and toast. Children were asked to think of different types of bread and which types were healthier, with a prompt to consider bread from different countries. Children were then told that brown and seeded breads are healthier because they are higher in fibre, which means that they help to keep us fuller for longer, keep blood sugar levels steady and prevent constipation. Children were then separated into groups to play ‘bread snap’. Each group was given a set of cards on which there were different types of bread and these were dealt out evenly to each member of the group; each player put down one card at the same time and if two of the same card were put down, the first player to put their hand on the pile and shout ‘bread!’ got to keep all of the cards in the pile. The game then started again. The player who had the most cards at the end was the winner.
Breakfast classroom lesson 3 dealt with spreads and toppings that might be consumed at breakfast time. Children were first asked about the type of milk that is healthiest and then, as a reminder to reinforce messages from the previous two lessons, to think of some healthy cereals and types of bread.
Breakfast workshop content
This started with a reminder of the key nutritional messages that ran through all of the workshops: to increase the intake of fruit, vegetables and fibre and decrease the intake of fat and sugar. As an icebreaker, participants were asked to think about what they usually have for breakfast and why it is important to have breakfast every day. The participants were then introduced to the first Bert scenario: that he goes to school without having breakfast and, as a result, cannot do his lessons, has no energy to play with his friends and is very hungry. This was to show participants the consequences that may result from not eating breakfast and to emphasise the importance of eating breakfast. Bert then decides to have a healthy breakfast in the morning, which is balanced and contains items from several of the food groups. This means that Bert has more energy to enjoy his day, is better able to do his lessons and is no longer hungry. Children were then asked if they could remember from the lessons on cereals and bread the types that would keep them fuller for longer. Participants were then advised that for Bert to stay fuller for longer and, therefore, to prevent snacking, he should eat some starchy food, such as a high-fibre cereal or wholemeal toast, and have a portion of fruit for his breakfast. Teachers were then asked to make sure that participants were aware that eating whole fruit is recommended and is much better than fruit juice, which contains less fibre and is higher in sugar. Fruit juice drinks should be limited to one glass per day as they contain very little fruit and do not therefore contribute to fruit portion consumption.
The next few slides of the workshop presentation showed pictures and/or a description of different types of breakfast and participants were asked which of these they thought would keep Bert fuller for longer.
Following the game, participants were reminded that high-fibre cereals (such as wholewheat cereal biscuits, shredded wholegrain wheat biscuits, wholegrain wheat flakes with wheat bran and wholewheat malted grain squares) and bread (such as wholemeal and seeded) are good for having every day, and foods such as white bread and sugary cereals (such as sugar-frosted flakes of corn or chocolate-flavoured coated rice) are better as a treat, as they will not keep us full for very long. The workshop then moved on to sugar, and participants were asked to think about how many teaspoons of sugar they could have in a day. They were then told that the maximum recommended daily intake for children is eight heaped teaspoons.
Bert was keen to know the amount of sugar in the food and drink that he had. The participants were split into groups and given two sets of cards: one with pictures and descriptions of different types of food and drinks and the other with pictures and descriptions of various numbers of heaped teaspoons of sugar. As a group they were asked to match each food or drink card with the correct teaspoons of sugar card.
Bert was then told that he should aim to cut down on the amount of fat in his breakfast and that he could do this by boiling or poaching eggs rather than frying them, grilling rather than frying treat foods, such as sausages, and cutting excess fat off meats.
Participants were split into groups. They were given a set of cards with pictures of different food and drink items that might be consumed at breakfast and another set of cards that said either ‘treat’ or ‘every day’. They were asked to put the cards into two groups: items that would be OK for Bert to have every day and items that would be better to have only as a treat.
The participants were then given the opportunity to create and taste a healthy breakfast. Schools had been provided with a selection of high-fibre breakfast cereals, tins of fruit in fruit juice, and raisins, and were asked to purchase skimmed milk, low-fat yoghurt and a variety of fresh fruit. Participants were split into pairs and each pair was provided with a chopping board and a plastic knife that was sufficiently strong and sharp to cut fresh fruit. Each participant was also given a disposable bowl and spoon. Participants created and then ate their own healthy breakfast from the items available and all were encouraged to include some chopped fresh fruit as part of their breakfast.
Lunch and snacks cooking workshop and classroom lessons
Lunch and snacks classroom lesson content
At the start of the ‘Lunch and snacks lesson 1’, children were provided with a simple explanation of what is meant by a snack (a small amount of food eaten between meals). They were then told about the advantages of healthy snacks: that they would keep them fuller until their next meal, help them to concentrate on school activities and lessons and give them energy to play with friends. Children were then taught that the best eating pattern for every day was to have three healthy meals and two healthy snacks, before they were asked to think about what snacks it would be good to have at school. The lesson finished with a ‘guess the snack’ activity, in which children were provided with clues for five different snacks and asked to guess the snack that was being described and draw a picture of it on an activity sheet.
‘Lunch and snacks lesson 2’ was about snacks after school. It reinforced the difference between a snack (a small amount of food eaten between meals) and a meal [food eaten at a regular time (breakfast, lunch and dinner) to fill you up] and the fact that three healthy meals and two healthy snacks were best for everyday consumption. Children were reminded that in the previous lunch and snack lesson they had thought about the types of fruit and vegetables that would be good to have at school and were then asked to think of some slightly bigger snacks that they could have after school to keep them full until their next meal. A slide with photographs of such snacks was then shown to the children before they had the opportunity to complete a word search puzzle containing the names of various possible healthy snacks.
The final lunch and snack lesson tried to teach children about healthy packed lunches. First, it covered the types of food/drink that a healthy packed lunch should contain: fruit and vegetables; protein, such as meat, fish or beans; a starchy food; dairy food or drinks; and a drink. Two example healthy packed lunches were then illustrated, with explanations of what each included item was providing. Having been reminded that they had already been taught that some foods were for everyday consumption and that others were best only as a treat, the children were asked to think of some lunchtime foods that they thought would be best to have as a treat. They were then shown photographs of some examples of foods best to have as a treat. The activity for this lesson was to design their own healthy packed lunch for a school trip.
Lunch and snack workshop content
Initially, the aims of the workshop were summarised: to think about the number of snacks children should have in a day; everyday snacks and those to have only as a treat; and packed lunches for school or trips out. As part of this, teachers were asked to make sure that children and parents were aware of the key nutrition messages running through all of the lessons and workshops: to increase fruit and vegetable and fibre intake and to decrease sugar, salt and fat intake. Participants were then asked about the number of healthy meals and healthy snacks that they thought was best for everyday consumption before being advised that the answer was three meals and two snacks. It was suggested that, although snacks could be had at any time, break time in the school day might be a good opportunity to have a healthy snack to delay children’s hunger, help keep their sugar levels constant and maintain their levels of concentration until lunchtime. Depending on the timing of children’s evening meal, the other suggested opportunity for a snack was either after school for families who eat a bit later or, for families whose children eat a bit earlier, between their evening meal and bedtime.
Participants were then asked if they remembered Bert and were given the scenario of Bert not having a snack at break time and its consequences (being unable to do his lessons, having no energy to play and being hungry). The opposite scenario of Bert deciding to have a healthy snack at break time was then presented before participants were asked to think of some healthy snacks. Teachers were asked to reinforce the message of variation and balance, and that no food/drink was being banned but that some were more suitable for everyday consumption and others were best kept to have only as a treat. Participants were then told some of the features of a healthy snack: being low in sugar, fat and salt and providing some vitamins and minerals. Examples of both healthy snacks (dried or fresh fruit, vegetables, low-fat yoghurts, unsalted nuts) and those best consumed only as a treat (cakes, chocolates, crisps, candies, juice) were then provided. Parents were also encouraged to think about portion sizes in relation to snacks best eaten as a treat, with a piece of chocolate rather than a whole bar given as an example. Small healthy home-made sandwiches were suggested as an option for an occasion requiring a slightly bigger snack, and participants were advised that this option would be covered in more detail later in the session. The benefits of healthy snacks were then discussed, namely the fact that they are lower in sugar and fat, thus helping to keep our insides, such as our teeth and heart, healthy; that they can help us feel fuller for longer; and that the vitamins and minerals they contain help to keep us healthy; for example, the calcium in a drink of milk helps to build strong bones and teeth.
The next element of this workshop involved another scenario for Bert: that he was going on a school trip and needed to take a packed lunch with him. The teacher then covered items that could be included in a healthy packed lunch, also providing simple information on the functions of different food types: fruit and vegetables that contain vitamins and minerals that help keep our bodies healthy; protein foods, such as meat, fish, eggs and beans, which help our bodies to grow strong; starchy foods, such as rice, pasta, bread and potatoes, which provide energy and help keep us fuller for longer; dairy foods and drinks, such as low-fat cheese, milk and yoghurt, which contain calcium and help our teeth and bones to grow and stay strong; and a drink to stop you getting thirsty, such as water, milk or juice. In relation to the last item – a drink – teachers asked the children if they could remember the rule about fruit juice: that consumption should be limited to only one glass or small carton a day. Participants were then given some picture cards of different foods and asked to split the cards into treat or everyday packed lunch items.
There was then a quick recap of the session before the final food preparation activity. Participants were encouraged to have healthy snacks. They were reminded of the items that a healthy packed lunch should include and that eating healthily helps keep us fuller for longer, gives us more energy for playing and means that we can concentrate better. Participants were then provided with a wholemeal (if possible) bread tortilla, a variety of different protein and vegetable filling options and visual instructions on how to assemble a wrap. Knives and chopping boards were available for the chopping of vegetable items when required. Participants then made up a healthy wrap using the ingredients provided.
Simple evening meal cooking workshop and classroom lessons
Evening meal classroom lesson content
‘Evening meal lesson 1’ began with the children being shown a picture of the Eatwell plate (Public Health England, in association with the Welsh Government, Food Standards Scotland and the Food Standards Agency in Northern Ireland) and asked to name some foods from each food group. Teachers were asked to highlight to the children that there are lots of different ingredients that can make up a healthy dinner, but that for a dinner to be healthy it was important for it to contain fruit and vegetables and be low in salt and sugar and lower in fat. The lessons and workshop refer to the evening meal as dinner. We are aware that people use different names to refer to their evening meal, so, to avoid confusion, it was explained that dinner is usually the last meal of the day and was the term that would be used to talk about the evening meal. Children were then given the opportunity to say what they called their evening meal. To reinforce the message of what constitutes a healthy meal, which the children had already received in relation to a packed lunch, children were reminded again in relation to dinner, namely that a healthy dinner should contain vegetables and/or fruit, some form of protein, a starchy food, some sort of dairy food or drink and a drink. This was followed by the activity for this lesson in which children were shown slides of different meals/snacks, which also included times, and were asked to select whether the food was for breakfast, lunch, dinner or evening meal and also whether it was for everyday consumption or for a treat.
The second lesson in preparation for the evening meal workshop was all about healthy lifestyle behaviours in general. Children were asked to think of healthy habits that they do every day before being taken through some healthy habits that broadly reinforced the messages of the WAVES study intervention programme. The healthy habits covered were having three healthy meals and two healthy snacks a day, with a reminder to make sure that, in general, they comprised everyday rather than treat foods; eating breakfast every day; consuming five portions of fruit and vegetables every day; water being the best drink, but that they could also have milk, fruit juice (but a maximum of one glass per day) or diluted squash; making sure they had ‘me-sized’ meals; and doing a minimum of 60 minutes of PA every day. The children were then read a story about Bert having a healthy habits day. Some bits of text were deliberately missing and the children were asked to make suggestions for words or phrases that could be used to fill in the blanks. The children were then asked to draw a picture of themselves performing one of their healthy habits.
Lesson three, in preparation for the evening meal workshop, started with teaching children some basic hygiene rules for food preparation and cooking. Children were asked to think of things that they thought it might be important for them to do before starting to cook, before being told about four rules that should be followed: (1) make sure that the cooking area is clean and tidy, (2) tie back long hair, (3) remove any jewellery and, most importantly, (4) wash their hands. The class was then asked what they would do if (1) they felt like they wanted to sneeze and (2) they wanted to go to the toilet while cooking. After some class discussion, the teachers told the children that if they felt like they wanted to sneeze they should put down any food or equipment, move away from the cooking area to sneeze and then blow their nose, wash their hands with soap and warm water and dry them before returning to the cooking area. With regard to leaving the cooking area to go to the toilet, they were told that they should remove their apron and leave it in the kitchen, go to the toilet and, again, wash their hands with soap and warm water and dry them before returning to the kitchen to put on their apron. The lesson then moved on to a discussion on food preparation. Children were given a few examples of techniques and skills that might be needed (chopped/washed/grated/chilled/peeled) and asked, first, if they could think of some more and, second, if they could think of a time when they have used any of the skills or techniques. The activity for this lesson involved the children matching pictures of people doing different cooking actions with the name of the skill being used. Each child was given a sheet with five pictures and skills (washing/mixing/peeling/grating/chopping) on one side and a picture of a blank apron on the other for them to design their own WAVES study apron.
Evening meal workshop content
As for the lunch and snack workshop, this started with an introduction to the aims of the session, namely to think about portion sizes, aiming for five a day (portions of fruit and vegetables) and to plan and prepare a tasty meal. The message introduced in the lunch and snack workshop of three healthy meals and two healthy snacks being best for everyday consumption, with suggestions for the best timing for snacks, was then reinforced before moving on to the concept of ‘me-sized meals’. Teachers introduced participants to the importance of having the right meal for their size and reminded them that children needed only portions that matched their age, stressing that a 5-year-old child requires smaller portions than a 10-year-old child, who requires smaller portions than an adult. Children were asked to compare the size of their fist with that of an adult’s and told that a smaller fist means a smaller tummy that requires smaller portion sizes. Parents present were told that serving more food would not make their child grow any faster, but would be likely to lead to extra fat storing up in their bodies. Some healthy eating habits were then suggested: to wash your hands before eating, to eat together at the table and to turn off the television and computer games while eating. Participants were then reminded of the main food groups (fruit and vegetables/protein foods/starchy foods/dairy foods, and also a treat foods group). They were asked to think of foods they usually have at dinner and the food groups they were from. Participants then played a game of ‘food group bingo’, whereby participants were grouped and each group was given a bingo card with the five food groups – about which they had just been reminded – running horizontally across the card, and the pictures of five food items from each food group running vertically below each of the food group headings. Slides with different foods were then shown for the participant groups to match them to the pictures on their bingo card and cross them off. The first group with a completed row across the page was asked to shout ‘bingo!’ and was the winner.
Next, participants were reintroduced to Bert. They were reminded that he was 6 years old and asked how many portions of fruit and vegetables he should be trying to eat every day, before being told that he should be aiming to eat five child-sized portions every day. Participants were then asked to think whether or not they have their five a day, and suggested ways to achieve this were having fruit and vegetables as snacks and making sure that breakfast, lunch and dinner always include at least one portion. Then another Bert scenario was presented, in which he wanted to try a healthy dinner. To avoid confusion, participants were advised that ‘dinner’ was being used to refer to the last meal of the day; this was followed by a discussion of different names that can be given to the evening meal. Participants were then asked to think about what Bert might mean by a healthy dinner. They were then told that Bert needs a dinner that contains fruit and/or vegetables, is based on healthy carbohydrate foods and includes some protein. The advantages of having a healthy meal were then reiterated (helps Bert to have more energy to play, be fuller for longer and grow strong). In anticipation of the food preparation part of the workshop, participants were asked to think of things that they should do before starting to prepare food or cook. The suggestions provided were the same as for the last classroom lesson (make sure the cooking area is clean and tidy/tie back long hair/remove jewellery/wash your hands). The food skills and preparation for this session was to create a healthy couscous meal including a mix of fresh vegetables and some protein. The couscous was prepared following the instructions on the packet but using a low-salt stock cube, and participants were provided with a variety of vegetable and protein items to chop and add to their bowl of couscous.
Villa Vitality
The aim of the Villa Vitality component was the promotion of healthy lifestyle messages through an iconic sports institution and its staff. Villa Vitality is a programme run by AVFC, an English Premier League football club at the time of the study, that promotes healthy lifestyles and, in particular, increased PA and healthy eating. It aims to motivate children to lead healthy lifestyles by taking the teaching out of a classroom environment and into the engaging setting of a football club. The programme is run over 6 weeks, with a full-day visit to the AVFC ground (Villa Park) in weeks 1 and 6. In between these days, children are involved with weekly healthy lifestyle challenges, work on a class project and are visited at school by a member of AVFC staff. An overview of the programme format is provided in Figure 5. The activities undertaken during the programme focus on developing children’s understanding of the importance of eating a healthy balanced diet and being physically active.
FIGURE 5.
The Villa Vitality programme.
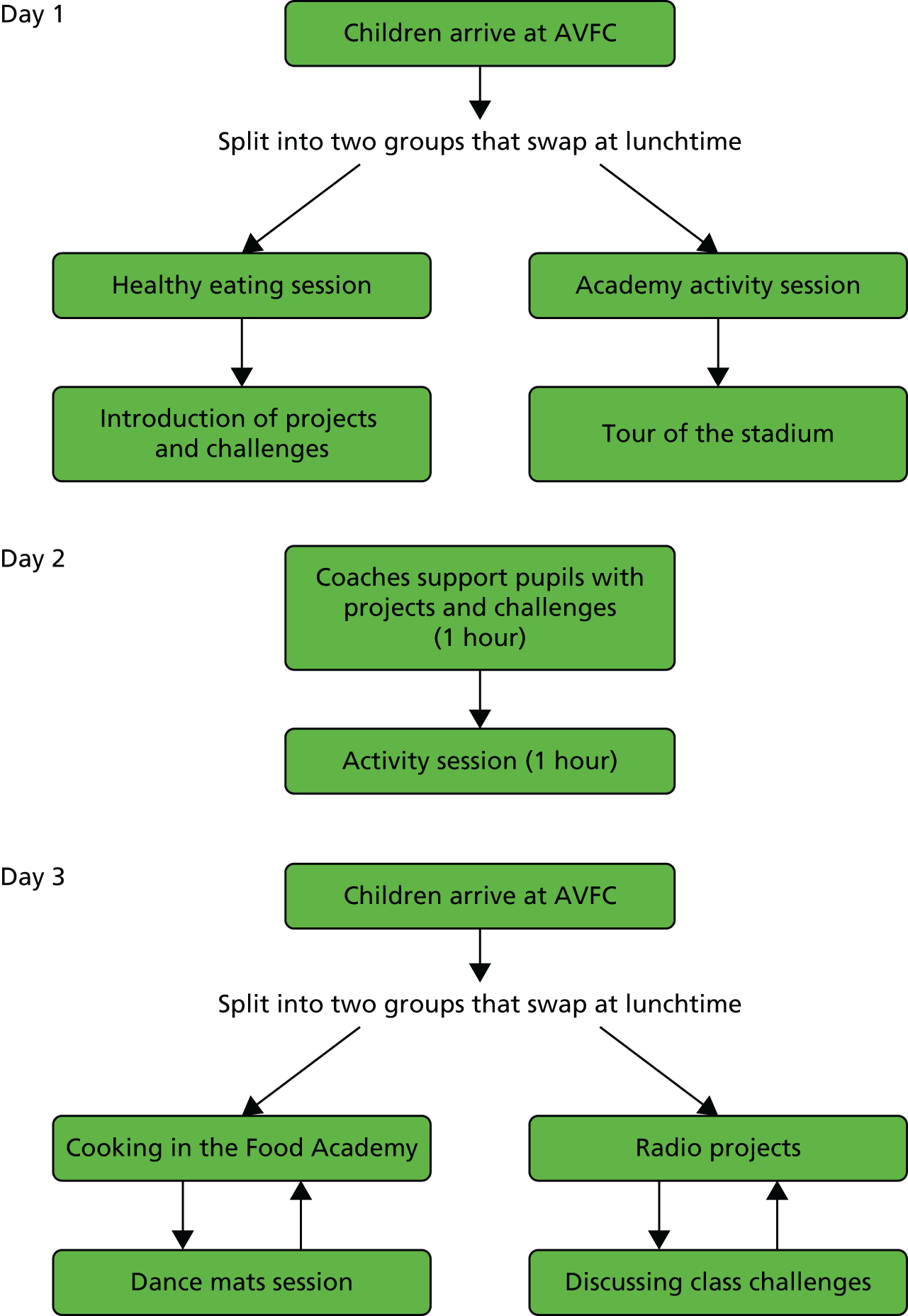
Day 1, the 2-hour session on day 2 and day 3 are run by AFVC staff, who also organise return transport between the school and the AVFC ground. During the 6-week period of the programme, teachers are asked to run weekly healthy lifestyle challenges with their class and also to undertake a class project. A teacher’s pack (see Appendix 48) is provided to all teachers in advance of day 1. In addition to information on the overall programme, the teacher’s pack provides details of the class project and weekly challenges, including suggestions of how these could be delivered.
Day 1
The first day of the programme is divided into three sections: PA, healthy eating and the launch of class projects and challenges.
The PA session is run in the AVFC Academy and involves exercise activities led by AVFC’s community coaches, teaching children the importance of being physically active and highlighting ways to include PA into their daily lives. The session is not dependent on sporting ability. The first part, ‘run around questions’, is intended as a warm-up, but also incorporates an educational element. With the children gathered in a group, the coaches ask them a healthy lifestyle question, provide four possible answers and allocate the answers to different zones marked out on the Academy’s indoor playing field. The children are then asked to run to the zone that they think has the correct answer. The children then regroup; the coach gives them the correct answer, explains why it is correct and then asks another healthy lifestyle question. The next part of the session is about ball skills. The coaches run a variety of different exercises in which children learn skills such as dribbling, turning and passing. For the final part of the session, the children are split into two teams for a football match that allows them to practise the skills they have been taught.
The healthy eating session is delivered by a nutritionist and aims to teach children the importance of eating a healthy balanced diet, how different types of food contribute to this and the concept of portion size and eating ‘me-sized’ meals. For a detailed session plan, see Appendix 49.
The class project and challenges session introduces children and teachers to these elements of the programme, designed for delivery by class teachers at school over the period between the 2 days spent at AVFC. For the project, prepared either together as a class or in smaller groups, children develop a song, rap lyrics, a poem or rhyme incorporating key messages from day 1 of the Villa Vitality programme. The challenges focus on healthy lifestyle behaviours; parents are encouraged to become involved by means of an introductory letter about the challenges, which is followed by a parent information sheet relating to each challenge. There are six challenges, one for each week of the programme, and a sticker reward system is used to incentivise children to complete each challenge. All of the materials, such as introductory letters, parent information sheets and child activity sheets, are included in the teacher’s pack (see Appendix 48). The individual challenges are:
-
60 minutes of activity each day (children and parents are given information on the government recommendation for children to be active for a minimum of 60 minutes every day, the health benefits of being active and some ideas on how to achieve the 60-minute minimum target, and children are asked to keep an activity diary)
-
swap a snack each day (children and parents are asked to think about daily snack consumption, in terms of both quantity and types of snack consumed; they are provided with possible strategies for reducing the number of snacks consumed and given examples of healthier and less healthy snacks; and children are encouraged to swap a high-fat and/or high-salt and/or high-sugar snack for a healthier alternative and to keep a record of all substitutions made)
-
drink more water each day [children and parents are told that over half of the added sugar in children’s diets is from the consumption of sugary drinks and told about the importance of staying hydrated throughout the day for both health and concentration; they are advised that a child needs six to eight glasses of fluid (1.2 l) every day to stay properly hydrated; children are encouraged to replace sugary drinks with water and to keep a record of the drinks consumed each day; parents are provided with tips and ideas on how to get their child to drink more water]
-
eat a healthy breakfast each day (the importance of eating breakfast every day for concentration is highlighted to both children and parents; they are informed that a healthy breakfast is based on a form of starchy carbohydrate, such as bread and cereals, and that wholegrain versions, which are higher in fibre, are better; breakfast is suggested as an opportunity for fruit and vegetable consumption and examples are given of ways in which this could be achieved; and children are asked to draw a picture of what they have for breakfast every day and are encouraged to make sure that it is healthy)
-
eat five portions of fruit and vegetables a day (parents and children are told that at least five portions is the recommended intake for fruit and vegetables and that a handful constitutes a portion; consumption of a range of different coloured fruit and vegetables is encouraged to ensure intake of a full range of vitamins and minerals; parents are provided with suggestions on how a portion can be achieved; and children are encouraged to eat at least five portions and are asked to keep a daily record of all of the fruit and vegetables that they eat)
-
plan, cook and eat a healthy balanced meal with your family (families are encouraged to plan a meal in advance, using the Eatwell plate (Public Health England, London, UK; http://webarchive.nationalarchives.gov.uk/20120206100416/http://nhs.uk/Livewell/Goodfood/Documents/Eatwellplate.pdf) to help them think of the different foods types to include and the proportion that each should contribute to the meal to help achieve a balanced diet; it is suggested to parents that this might be a good opportunity to allow their child to help out in the kitchen).
Children are also provided with a booklet of fun activities to take home and complete, which focuses on the key healthy lifestyle messages taught throughout the day (see Appendix 50).
Day 2
This involves a 2-hour school visit by a member of the AVFC coaching staff. This is scheduled approximately 4 weeks after the children’s first visit to AVFC. During the first hour the coach runs a PA session involving a series of fun team games that are designed to practise the ball skills that the children were taught in the activity session of day 1. The second hour is used to support the pupils and teachers with their Villa Vitality school project and class challenges.
Day 3
Day 3 is divided into three sections: PA, cooking and recording the group project on a CD.
The PA session involves children participating in 1 hour of PA, involving dance mats and aerobic routines supervised by qualified instructors.
The cooking session gives children the opportunity to prepare their own healthy lunch and snacks with an AVFC chef in the Villa Vitality programme Food Academy. In the morning, the lunch preparation is split between the two groups, with one preparing the main course (a pasta bake) and the other preparing the dessert (a fresh fruit salad). In the afternoon, each group is involved in the preparation of a healthy snack to take home (rice and vegetable salad or tuna and salad wrap). Before the start of the first cooking session, the children in both groups are taught food hygiene, including the use of aprons and hats, hand washing and the cleaning of surfaces. Once all of the children are wearing their aprons and hats, and have washed their hands, they learn how to use a knife safely for chopping, as this is a skill that they will use for the preparation of vegetables or fruit later in the session.
The recording of the group project takes place in the AVFC radio studio. Children have the opportunity to record the outcome of the group work that they have been undertaking at school to develop a song, rap lyrics, a poem or rhyme with a healthy lifestyle theme. A member of AVFC staff also undertakes a short interview with each group of children, asking them about the healthy lifestyle messages they have included. The radio studio session with each group is recorded. The recordings for each school are then made into a CD and a copy for each child is sent to the school for distribution.
Patient and public involvement
This trial started before there was a formal requirement to involve patients and the public. Nevertheless, we involved parents, teachers and children at several levels in an informal way. One of our co-investigators is a health education consultant working with Services for Education and so advised the team on how best to engage with schools and how to ensure that the intervention and study procedures would be acceptable within a school environment. We also consulted a head teacher who advised on the wording of information letters for schools and how to encourage participation. A panel of seven parents and children advised on the cooking workshop material and lessons. A class of children from a non-participating school tried out the revised Villa Vitality programme and provided comments on how it could be improved.
Chapter 4 Process evaluation of intervention implementation
Introduction
Process evaluation has become increasingly recognised as an essential component of public health intervention research; it is of particular importance for research evaluating complex interventions that have multiple components delivered externally, as implementation may vary across study sites.
The development and evaluation of the WAVES study intervention programme were guided by the framework published by the MRC in 2008. 62 At the point of development of the WAVES study process evaluation methods, there were a number of resources highlighting important elements for consideration, but a single agreed comprehensive framework for such evaluation was not available, reflected by the heterogeneity of process evaluation methods presented in the literature. In developing our methods we drew together key aspects of process evaluation presented in previous health promotion intervention literature63,64 to produce a comprehensive approach to the process evaluation for the WAVES study, an evaluation of a complex and multifaceted intervention programme delivered by teachers and external facilitators. Although the process evaluation methods for the WAVES study were developed and undertaken prior to the publication of the more recent MRC guidance on process evaluation of complex interventions,65 many of the concepts recommended by the recent framework were included.
Methods
The first stage of development was to define the process evaluation dimensions to be included. This was achieved through the identification of specific research questions that needed to be addressed and the subsequent mapping of these questions on to different evaluation dimensions drawn from existing literature. 63,64 The most appropriate data collection methods to assess the defined dimensions were then identified. Methods and tools that could be used were assimilated through advice provided by experienced researchers in the field and relevant literature. 66–70 Multiple methods of data collection were used for each dimension to allow triangulation of the data and to provide a broad picture of intervention implementation. It was also anticipated that it would help to ensure comprehensive data availability across all of the process evaluation dimensions, even when some data sources for an intervention component were incomplete or missing. This approach also allowed for cross-checking of reporting accuracy, for example comparing a researcher observation with a teacher logbook entry for the same activity. The research questions identified, together with the mapped process evaluation dimensions and the assessment tools used, are presented in Table 3.
| Research question | Process evaluation dimensions | Data source |
|---|---|---|
| Is the intervention being delivered in the way in which it was intended? | Fidelitya/adherenceb | Observations |
| Logbooks | ||
| Qualitative evaluation | ||
| Questionnaires | ||
| How much exposure are children and families getting to each intervention component? | Reacha/dose delivereda/dose receiveda/exposureb | Observations |
| Logbooks | ||
| Qualitative evaluation | ||
| Questionnaires | ||
| What methods are used for encouraging participation in intervention activities? | Recruitmenta | Observation |
| Qualitative evaluation | ||
| What quality of intervention is being received? | Qualityb | Observations |
| Logbooks | ||
| How well are children and families responding to, and engaging with, the intervention? | Dose receiveda/participant responsivenessb | Observations |
| Logbooks | ||
| Qualitative evaluation | ||
| Are there intervention components that are more essential than others? | Programme differentiationb | Observations |
| Logbooks | ||
| Qualitative evaluation | ||
| Questionnaires | ||
| Are there contextual and environmental factors that have the potential to influence delivery? | Contexta | Observations |
| Qualitative evaluation | ||
| Questionnaires | ||
| Research team reflection |
Information sources utilised
Researcher observations
Observations were used to collect data on the following process evaluation dimensions: adherence, exposure, participant responsiveness, quality (of delivery) and using checklists developed for each of the relevant intervention components. The observations were also used for the identification of school-specific contextual factors that may influence intervention component delivery. During the early stages of the implementation phase of the intervention (September–October 2011), the observation checklists were piloted and inter-rater reliability was tested through independent completion by two researchers having observed the same session. Any differences were discussed for clarification of what was expected for different ratings to be selected and explanatory text was added to the checklist with the aim of improving future consistency. This process was continued until high inter-rater reliability was achieved and was intermittently repeated throughout the intervention period to ensure that consistency was maintained. The details of the information collected and dimensions assessed by the observation checklists are provided in Table 4 (see Appendices 51–53 for example observation checklists relating to the Activate PA package, the breakfast cooking workshop and Villa Vitality session 1).
| Researcher observation checklist item | Fidelity/adherence | Reach/dose/exposure | Recruitment | Quality | Participant responsiveness | Programme differentiation | Context |
|---|---|---|---|---|---|---|---|
| Activity observeda,b,c | ✓ | ||||||
| Duration of activitya,b,c | ✓ | ✓ | |||||
| Method of deliveryb | ✓ | ||||||
| Number of childrena,b,c | ✓ | ✓ | |||||
| Number of parentsa | ✓ | ✓ | |||||
| Number of staff present, number joining in, and if not whya,b,c | ✓ | ||||||
| Number of children present but not participating and whya,b,c | ✓ | ✓ | |||||
| Does the leader remind the children of the benefits of the activity?b | ✓ | ✓ | |||||
| Does the leader encourage the children to move energetically?b | ✓ | ✓ | |||||
| Does the leader encourage the children to participate?c | ✓ | ✓ | |||||
| How enthusiastic is the teacher?a,b,c | ✓ | ||||||
| Do the children have sufficient space?b | ✓ | ||||||
| Overall quality of deliverya,b,c | ✓ | ||||||
| Proportion of children achieving MVPAb | ✓ | ||||||
| Proportion of children enthusiastic about/enjoying sessiona,b,c | ✓ | ||||||
| Proportion of children getting actively involved in sessiona | ✓ | ||||||
| Proportion of parents enthusiastic about/enjoying sessiona | ✓ | ||||||
| Proportion of parents getting actively involved in sessiona | ✓ | ||||||
| Was all of the recommended session content delivered?a,c | ✓ | ✓ | |||||
| Children with special educational needs included?a,b,c | ✓ | ✓ | |||||
| Number of children being disruptivea,b,c | ✓ | ||||||
| Are most children able to follow the instructions given?c | ✓ | ||||||
| Did language appear to be a barrier for parents?a | ✓ | ✓ | ✓ |
A trained member of the WAVES study research team undertook observations in all of the schools that delivered the intervention. To try to minimise impact of observer presence during school visits, the research team members were required to be familiar with the checklist content such that they could simply observe or, if appropriate, join in the activity at the time and then complete the checklist as soon as possible after leaving the session. For both activity packages selected by each school (to assist delivery of the PA component), termly observations (per class) of delivery were undertaken. For the cooking workshop component the delivery of at least one of the three workshops was observed at each school, and for the Villa Vitality component one of the three sessions was observed for all of the schools.
Completed observation checklists were not reviewed prior to subsequent school visits to ensure that the researchers were not biased by previous observations. Feedback was not provided to teachers following the observation owing to the study being a Phase IV trial, that is, endeavouring to evaluate the intervention in a real-life setting and aiming to ensure that intervention guidance from the research team was standardised across schools.
Evaluation questionnaires and researcher experiences
Evaluation questionnaires were used for obtaining both parent and staff feedback on different elements of the intervention. A cooking workshop parent feedback questionnaire was distributed for those in attendance at the workshops (see Appendix 54 for an example questionnaire relating to the breakfast cooking workshop). School staff were asked to complete an evaluation for Villa Vitality session 1 (see Appendix 55) as well as for the overall programme (see Appendix 56). The school questionnaire, completed by the head teacher or deputy head teacher in both intervention and control schools (see Chapter 2, Cluster-level outcomes, for further details), was important for the gathering of data on the wider contextual influences of the school on intervention delivery. This information, together with that from observations, was supplemented through a reflective diary for each school. After a researcher school visit, their impressions of the ethos of the school and their overall experience of the school during the visit, together with any particular factors that could be relevant to the WAVES study intervention delivery, were recorded in a school-specific diary of experiences.
School staff logbooks
School staff were asked to complete logbooks to report on the delivery of the PA, cooking workshop and Villa Vitality components of the intervention. The logbooks collected information on the process evaluation dimensions of adherence, exposure, participant responsiveness, quality of delivery and, to some degree, programme differentiation. A separate logbook was sent to schools, ready for the start of each term in the intervention year, for the PA and cooking workshop components, and shortly before session 1 for the Villa Vitality component. The logbooks were designed to be concise and as simple to complete as possible (see Appendices 57–59). Completed logbooks were returned at the end of each term, with two reminder letters sent the following term to schools that had failed to return them. No feedback was given to teachers on the quality of delivery of the various intervention components, but logbooks were inspected on return to check for incomplete or incorrect completion, and any such errors were fed back to staff with the aim of improving subsequent completion. Table 5 summarises the data collected for each logbook, together with the process evaluation dimensions assessed.
| Teacher logbook item | Fidelity/adherence | Reach/dose/exposure | Recruitment | Quality | Participant responsiveness | Programme differentiation | Context |
|---|---|---|---|---|---|---|---|
| PA logbook (completed daily) | |||||||
| Time of activity | ✓ | ✓ | |||||
| Duration of activity | ✓ | ✓ | ✓ | ✓ | |||
| Reason for non-completion | ✓ | ||||||
| Number of children who did not participate | ✓ | ||||||
| Additional comments | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Cooking workshop logbook (one per workshop) | |||||||
| Cooking workshop lessons | |||||||
| Number of lessons delivered prior to the workshop | ✓ | ✓ | ✓ | ✓ | |||
| Time spent delivering the lessons | ✓ | ✓ | |||||
| Additional comments | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Cooking workshop | |||||||
| Time spent and delivering the workshop | ✓ | ✓ | |||||
| Number of children who did not participate and reasons | ✓ | ✓ | |||||
| Number of children with at least one parent/carer present | ✓ | ✓ | ✓ | ||||
| Number of helpers present | ✓ | ||||||
| Additional comments | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Villa Vitality logbook | |||||||
| Villa Vitality days 1–3 | |||||||
| Number of children attending the day | ✓ | ||||||
| Reasons for non-attendance | ✓ | ✓ | |||||
| Villa Vitality project and weekly challenges | |||||||
| Time spent delivering the project/challenges | ✓ | ✓ | |||||
| Number of children who completed each challenge | ✓ | ||||||
| Additional comments | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
Qualitative evaluation
Intervention programme experiences of school staff were explored through interviews, and focus groups were run for parents and children (separately). This qualitative approach was used to collect information relating to the adherence, participation, programme differentiation and responsiveness domains of process evaluation. The parent focus groups were also useful in determining school adherence to the programme, as they provided an indication of whether or not the school had tried to engage parents at the level requested for the relevant components of the intervention programme. The focus group method of data collection was selected for parents and children, as it was thought that such group discussion would encourage open expressions of attitudes and experiences. 72 It was also felt that the children would be more comfortable with a focus group environment, in which their peer group would provide support and promote confidence. 73 Interviews were used for school staff to ensure that school-specific teacher experiences were elicited but also for practical reasons.
Schools were purposively sampled for invitation to participate in the qualitative evaluation such that a range of primary schools varying in terms of pupil ethnic mix, size, geographic location, deprivation (assessed by the percentage of the school population eligible for a free school meal) and level of implementation fidelity achieved for intervention delivery (assessed by members of the research team involved with observations) were involved. Separate topic guides were developed for each participant group, which initially focused on the overall intervention programme before exploring the individual components separately. The topic guide for the teacher interviews and the parent and child focus group topic guides are provided in Box 1.
Question 1: can you tell me about your overall experience of being involved in the WAVES study intervention programme?
Question 2: can you explain your overall experience of the PA programmes?
Question 3: what did you think about the signposting sheets?
Question 4: what were your experiences of the cooking workshops?
Question 5: what were your experiences of the Villa Vitality programme?
Question 6: overall, what impact (if any) do you think the WAVES study intervention programme had on your year 2 children?
Question 7: do you think that there were components of the WAVES programme which were more beneficial than others?
Question 8: do you think that the WAVES study intervention programme could be adopted by primary schools in general?
Topic guide: parent focus groupsQuestion 1: can you tell me what you know about the WAVES study and the activities it involved?
Question 2: can you tell me about you and your child’s overall experience of being involved in the WAVES study?
Question 3: as part of the WAVES study programme, schools were asked to fit in an extra 30 minutes of activity into the school day. Did you know this was happening in your child’s school? How do you feel about it?
Question 4: what did you think about the signposting sheets?
Question 5: what did you think of the cooking workshops? Do you think the workshops had any impact on your family?
Question 6: your child’s class also attended AVFC for the Villa Vitality programme. What do you think your child’s experience of the Villa Vitality programme was?
Question 7: do you think there were components of the WAVES study programme that were more beneficial than others?
Question 8: do you think the WAVES study programme of activities had any effect on your child’s behaviours and attitudes towards healthy lifestyle behaviours?
Question 9: what effect (if any) do you think the WAVES study programme has had on your family’s lifestyle habits?
Question 10: what role (if any) do you think schools play in obesity prevention?
Topic guide: child focus groupsQuestion 1: can you tell us what you know about the WAVES study? What did you do as part of the WAVES study?
Question 2: what did you think of the cooking workshops in school? Did you learn anything new?
Question 3: can you tell me what you think about the WAVES study physical activities? How do they make you feel?
Question 4: what did you think about the Villa Vitality programme? What did you do at Villa Vitality?
Question 5: did you take part in the Villa Vitality challenges? What did you think of the challenges?
Assimilation of process evaluation data
The use of multiple data collection methods for the process evaluation of each of the intervention components resulted in a large number of data. For each of the three main intervention components (cooking workshops, PA and Villa Vitality), key information to be used from each data source to inform the individual process evaluation dimensions was identified and tabulated. This table was then populated by school as illustrated for PA in Figure 6. During this process, if data were available from multiple sources for a particular session, then consistency reporting checks were undertaken. This picked up a few researcher/school staff reporting discrepancies and, in these instances, researcher reported data were used. This data collation process did not include the signposting sheets because of the uniformity of delivery of this component across schools: confirmation of signposting sheet distribution to children was confirmed for all schools.
FIGURE 6.
A worked example of the tabulation of data from multiple sources by process evaluation dimension.

An iterative process of score allocation (to maximise interschool consistency) was then undertaken separately for each of the three main intervention programme components. For the process evaluation dimensions of fidelity/adherence, participant responsiveness, reach/dose/exposure, recruitment and quality, two researchers independently allocated school-specific scores on a scale ranging from one (very low) to five (very high). Programme differentiation and context information contributed through its consideration during the allocation of scores to the other dimensions. Score allocation was undertaken in repeated groups of four randomly selected schools, with inter-researcher discussion between each group to reach a consensus in instances when allocated scores varied. School-specific summary scores for each intervention component and process evaluation dimension, together with an overall score, were then generated, as summarised in Table 6, for a school universally allocated maximum scores. As a general check for possible inconsistencies, the overall score was then used to rank schools in terms of implementation fidelity achieved, considering all dimensions, for separate review by both researchers.
| Process evaluation dimension | Intervention component | Process evaluation dimension score | ||
|---|---|---|---|---|
| PA | Cooking workshop | Villa Vitality | ||
| Fidelity/adherence | 5 | 5 | 5 | 15 |
| Reach/dose/exposure | 5 | 5 | 5 | 15 |
| Recruitment | 5 | 5 | 5 | 15 |
| Quality | 5 | 5 | 5 | 15 |
| Participant responsiveness | 5 | 5 | 5 | 15 |
| Intervention component score | 25 | 25 | 25 | 75 a |
This independent score allocation process was followed by a consultation with the wider WAVES study team. Five researchers familiar with the WAVES study intervention delivery were asked to use the same process of score allocation to independently score six schools. As a further consistency check, these scores were compared with those already allocated. Low levels of variation were observed, with all wider research team allocations being within one point of those allocated by the two researchers. The staff then revisited the scores with specific consideration of those for which there were minor score allocation differences. A consensus was given to reached after this discussion and the wider research team were then asked to undertake another review of the proposed final scores.
At this point, it was agreed that school-specific definitive scores had been determined and a consensus had been reached on the implementation fidelity rating of schools. Three levels of intervention implementation were defined through the ranking of schools by definitive overall score and their subsequent division into tertiles. Schools with scores ranging from 0 to 51 were classified as low, those scoring between 52 and 58 were classified as medium and those scoring between 59 and 75 were classified as high implementation. Scores by intervention component were then calculated proportionately, such that 0–17 represented low fidelity, 18–19 represented medium fidelity and 20–25 represented high fidelity.
Results
Twenty-six schools were randomised to receive the intervention, but unforeseen circumstances in two meant that 24 (classes = 38) implemented the WAVES study intervention and were therefore involved in the process evaluation. With the exception of researcher observations (on account of all data collection targets being met), process evaluation data availability is summarised in Table 7.
| Process evaluation data source | Returned/expected (%) |
|---|---|
| PA logbooks | |
| Term 1 | 19/37a (51) |
| Term 2 | 24/37a (65) |
| Term 3 | 12/37a (32) |
| Cooking workshop logbooks | |
| Breakfast | 28/38 (74) |
| Lunch and snacks | 27/38 (71) |
| Evening meals | 21/38 (55) |
| Villa Vitality logbook | 25/38 (66) |
| Questionnaires/evaluations | |
| School questionnaire | 23/24b (96) |
| Teacher questionnaire | 23/38 (61) |
| Cooking workshop parent evaluations | |
| Breakfast | 23/38 (61) |
| Lunch and snacks | 23/38 (61) |
| Evening meals | 17/38 (45) |
| Villa Vitality teacher evaluations | 51/76c (67) |
| Qualitative data | Total number of participants |
| Teacher interviews | 16 |
| Parent focus groups (n = 8) | 30 |
| Children focus groups (n = 13) | 61 |
Data cross-checking
Overall, there was general agreement between data sources when data were available from more than one source. There was some variation in PA and cooking workshop session duration reporting between logbooks and observation checklists, with the logbook reported values tending to be higher than the researcher observations. From 61 matched data points across 16 schools, a mean difference (MD) for PA of 1.3 minutes (SD 5 minutes) was observed, and from data across 19 schools there was an average cooking workshop duration of 85 minutes compared with 60 minutes. However, after the exclusion of PA logbook data for one school where large discrepancies from matched observation data were identified, with recognition of marginal reporting errors, other data cross-checks between these two sources suggested that, in general, logbooks gave a reasonable estimate of school activity.
Allocated intervention implementation scores and associated levels of fidelity
Across the schools that implemented the intervention, the minimum overall intervention implementation score was 35 and the maximum score was 68 [median score 56, interquartile range (IQR) 51.0–60.8]. As previously described, schools were classified into three levels of intervention implementation fidelity (low, medium and high) by overall score, intervention component score and process evaluation dimension score. This distribution by school is illustrated in Table 8. There were no significant differences when implementation fidelity levels were considered across several school characteristics (outcomes are presented in Table 9).
| School | Intervention component | Process evaluation dimension (average level across all intervention components) | Total scorea | ||||||
|---|---|---|---|---|---|---|---|---|---|
| PA | Cooking workshops | Villa Vitality | Adherence | Exposure | Recruitment | Quality | Response and engagement | ||
| 1 | 68 | ||||||||
| 2 | 68 | ||||||||
| 3 | 67 | ||||||||
| 4 | 64 | ||||||||
| 5 | 62 | ||||||||
| 6 | 61 | ||||||||
| 7 | 60 | ||||||||
| 8 | 60 | ||||||||
| 9 | 58 | ||||||||
| 10 | 58 | ||||||||
| 11 | 57 | ||||||||
| 12 | 57 | ||||||||
| 13 | 55 | ||||||||
| 14 | 54 | ||||||||
| 15 | 53 | ||||||||
| 16 | 52 | ||||||||
| 17 | 51 | ||||||||
| 18 | 51 | ||||||||
| 19 | 51 | ||||||||
| 20 | 51 | ||||||||
| 21 | 49 | ||||||||
| 22 | 42 | ||||||||
| 23 | 39 | ||||||||
| 24 | 35 | ||||||||
| School characteristic | Overall implementation fidelity level achieved | p-valuea | ||
|---|---|---|---|---|
| Low (n = 8), median (IQR) | Medium (n = 8), median (IQR) | High (n = 8), median (IQR) | ||
| School size (number of pupils on roll) | 319 (241–473) | 233 (171–351) | 279 (187–417) | 0.31 |
| Free school meals eligibility (%) | 25.3 (17.2–33.1) | 32.9 (11.3–42.3) | 29.2 (12.1–39.7) | 0.91 |
| Ethnicity (% white) | 40.2 (1.6–84.0) | 75.6 (65.8–82.3) | 17.4 (11.1–94.0) | 0.29 |
| Ethnicity (% Asian) | 32.5 (2.0–79.5) | 13.0 (2.0–21.7) | 37.3 (2.4–63.5) | 0.40 |
| Ethnicity (% black) | 5.2 (1.1–27.8) | 3.4 (1.5–6.5) | 2.1 (0.2–19.6) | 0.62 |
| Ethnicity (% other ethnic group) | 5.9 (3.7–14.3) | 9.5 (5.3–11.4) | 5.6 (2.5–18.4) | 0.91 |
Intervention component-specific scores
This section considers implementation fidelity separately for each of the intervention components and, to add context, integrates the outcomes with some qualitative findings from the process evaluation. Discussed findings are illustrated through direct quotations extracted from the verbatim transcriptions and are presented in Table 10.
| Quotation number | Quotation |
|---|---|
| 1 | For the dinner I tried the beans and I like them.Child |
| 2a | You can’t have loads of sugar.Child |
| 2b | Fibre gives you an energy boost and it gives you energy for longer not like sugars, the sugars just give you energy for 1 minute.Child |
| 3 | The cooking workshops are great and it’s really lovely to come in and work with your child.Parent |
| 4 | It’s been difficult for me cause I think most times that you’ve done the studies my wife’s came in ‘cause I’m at work so I’m a bit sort of in the dark.Parent |
| 5 | So well resourced, you know, you could just literally just pick up the box, I didn’t even have to, you know, the lessons beforehand you didn’t have to photocopy them, everything was just there for you.Female teacher |
| 6 | Well this is going to sound terrible but I’ve only really done the first one and we did that in spring term. The other two we are going to do this term. The reason why well autumn term we do a major production towards Christmas time which I was organising and liaising with four classes, so that took up a lot of our time and hall time as well, and then we’ve just recently had SATS and that took priority.Female teacher |
| 7 | I can’t say we always did 30 minutes, I think we always did possible 20, you know, it’s difficult as you appreciate, you’ve got assessment weeks, you’ve got different activities going on and so . . . we did our best, yeah. I think probably 20 was more realistic.Female teacher |
| 8 | You try and have your routine but then you might have an assembly that goes over or it just doesn’t fit in with the children the way they are, so you know, sometimes we can’t do it now but we have to do it later.Female teacher |
| 9 | They know what they’re expected to do, it starts off the day and the afternoon in a calm way.Female teacher |
| 10 | I had a really, really lots of fun there [Villa Vitality programme at AVFC].Child |
| 11 | I think the Villa Vitality was definitely a highlight for me, and we’re doing reports at the moment and a lot of the children . . . they’re writing about their favourite thing from year 2 and a lot of them have actually mentioned that.Female teacher |
| 12 | It was fantastic and combining the sport and the nutrition was brilliant.Female teacher |
| 13 | Yeah I remember looking at this and thinking we’re all on a tight budget and it’s all about cost.Parent |
| 14 | Signposting I can’t even remember having these.Parent |
| 15a | I haven’t had any children come to me and tell me that they’ve gone to any of these groups.Female teacher |
| 15b | I’m not sure how much of an impact they had.Parent |
Cooking workshops
For the cooking workshops, 15 schools (63%) were classified as achieving either high (n = 11) or medium (n = 4) implementation fidelity. However, it should be noted that in four of these the external staff trained by the WAVES study research team were responsible for their delivery. For two schools this was for all three workshops, as the head teacher informed the research team that the school did not have sufficient staff capacity to run the sessions. In the other two schools the WAVES study team intervened following unsatisfactory delivery of the first cooking workshop (it was considered that children were being given misleading nutrition information).
Although a comparison of matched cooking workshop logbook and observation records (n = 39) identified a shorter duration reported in the latter, the average session length taken from this source was still at the lower limit of planned duration (60–90 minutes). Apart from this difference, there was minimal variation in reporting between these two sources.
Most schools (n = 15) delivered all three workshops. Six schools ran two workshops, but one of these delivered material from all three sessions, as they combined the lunch and dinner workshops into one session. The remaining five schools managed to deliver only one of the workshops. As requested, most schools invited parents to attend the cooking workshops but researcher observations indicate wide variation in the proportion who attended. The proportion of children for whom a parent was present ranged from 2% to 67%, with a mean attendance of 41% (SD 15%). During the qualitative element of the process evaluation, the cooking workshops were recalled well and an analysis of the data showed appreciation from parents, children and teachers (see Table 10, quotations 1–6).
Physical activity
Over half of the schools (54%, n = 13) that undertook intervention implementation were included in the low implementation fidelity group for the PA component, with only four (17%) obtaining high implementation fidelity scores. Among schools (n = 19) for which data on weekly frequency of delivery were available (taken from logbooks and teacher questionnaires), only just over half (53%, n = 10) reported achieving the daily delivery target. A further 21% (n = 4) and 16% (n = 3) reported an overall delivery frequency of three and four times per week, respectively, with the remaining two schools managing to deliver this component on only one or fewer days in an average week. If only days on which delivery of the PA component took place are included, then the daily average duration of additional activity is 17.5 minutes, falling to 12 minutes when days on which delivery did not happen are included, representing 58% and 40%, respectively, of the target duration of 30 minutes.
Fitting in the PA component was identified as a challenge during the teacher interviews, especially achieving the target duration of 30 minutes (see Table 10, quotation 7). Teachers who opted for the ‘as and when’ approach to delivery of the PA component struggled more (see Table 10, quotation 8) than those who tried to embed it into the daily timetable (see Table 10, quotation 9). This was supported by researcher observations in which higher levels of child ability and activity familiarity, together with an easier return from the activity session to classroom work, were reported for classes with regular timetabled slots for the additional PA. The diary of experiences also showed a greater tendency for a generally less structured school day and more challenging child behaviour issues among classes when a ‘casual’ approach to delivery was adopted by the teacher.
Villa Vitality
The Villa Vitality component was completed by all schools that delivered the intervention programme. As might be expected from a component for which delivery was mainly the responsibility of external staff, a high level of implementation fidelity was attained by a large proportion of the schools (71%, n = 17). There was, however, still variation in the fidelity of implementation (through differences in the teachers’ approach to delivery of the weekly challenges and class project, their involvement with the sessions held at the AVFC grounds and the general level of encouragement that they provided). Five schools (21%) were classed as having low implementation fidelity, despite the limited requirement for teacher input. Positive feedback was evident from both the children’s focus groups (see Table 10, quotation 10) and the teacher interviews (see Table 10, quotation 11) in relation to the Villa Vitality component. It was also seen as important by some teachers for the integration of the PA and nutrition messages of the intervention programme (see Table 10, quotation 12).
Signposting
In general, recollections by parents were vague or non-existent (see Table 10, quotation 14) and no changes to behaviours based on this component were reported. Barriers to implementing the advice provided by the signposting sheets were sometimes discussed by parents (see Table 10, quotation 13). The qualitative analysis of the teacher interviews revealed uncertainty about the impact of this component (see Table 10, quotations 15a and b).
Other influences over intervention delivery
The qualitative work and researcher experiences/observations identified that the degree of intervention delivery staff interest in the WAVES’ study overall objective had a strong influence on the level of implementation fidelity. Higher quality of implementation – resulting from greater delivery staff engagement with the research and more effort in intervention implementation across all components – was evident when there was already a belief among staff who were responsible for delivery that healthy lifestyle behaviours form a key element of school life. Perceptions of having sufficient staff capacity to undertake the supplementary activities – and the difficulties with fitting them into an already busy class timetable – were an additional critical factor that had an impact on delivery of all main intervention components. Time available for the intervention was further negatively affected by the pressure under which teachers feel to maximise academic performance. Finally, the level of support for the intervention activities by the school as a whole but, in particular, by the head teacher, was also identified as important, with achievement of generally better implementation fidelity in more supportive schools.
Chapter 5 Statistical analysis methods
In this chapter we outline the main statistical analysis methods, along with a range of sensitivity analyses that were carried out.
Main analysis
Flow chart
A chart summarising the eligibility, trial arm allocation and subsequent progress of schools (cluster level) and consented pupils (participant level) is provided in Chapter 6 (see Figure 7). It provides the numbers of participating schools and consented pupils, and cluster size is summarised by the median and IQR.
Timeline cluster diagram to assess the risk of biases
A lack of clear reporting of the recruitment process and other aspects of blinding means that it can be difficult to establish whether a cluster randomised trial suffers from recruitment or other biases. One potential tool that has been proposed to improve the reporting of these items and allow the identification of potential biases is a timeline cluster tool. 74 We have used this tool to demonstrate the potential risks for bias in the WAVES trial. Within this tool each of the stages of the trial is represented, in chronological order, in the diagram. An accompanying table describes these aspects of the study in more detail.
Baseline characteristics summaries
We first summarised and compared the characteristics of those who consented to the trial and those who did not. We did this for a limited number of routinely collected pupil-level baseline characteristics. To enable this, sex, ethnicity and home postcode were requested from participating schools for all eligible pupils. Home postcode was requested to enable an IMD 2010 score (as an indicator of deprivation) to be obtained for each pupil for the lower-layer super output area in which they lived. These pupil-level baseline characteristics are summarised by consented and non-consented pupils (see Table 12). Sex, ethnicity and IMD quintile are summarised by numbers and percentages; IMD score is summarised by its median and IQR.
The baseline characteristics of consented pupils (see Tables 13 and 14) and participating schools (see Table 15) are summarised by control and intervention arms. These baseline characteristics are summarised by numbers and percentages, by means and SDs or by medians and IQR ranges. Medians and IQRs were used for variables that exhibited non-normality. Further details are given below (see Transformations).
Analyses of outcomes
Analyses of all outcomes are by intention to treat. As randomisation is at the school (cluster) level, appropriate statistical methods to account for the clustering within schools (see Model choice) were used in the analysis. An analysis of outcomes is presented for the first, second and third follow-up stages at 3, 18 and 27 months post intervention completion, respectively. We report unadjusted, partially adjusted and fully adjusted results. Full details are explained below.
Model choice
The primary aim of the study is to evaluate whether or not the BMI-z differs between arms. In statistical terms, this null hypothesis (no difference) can be tested using a mixed linear regression model, with follow-up BMI-z as the dependent variable, baseline BMI-z and treatment arm as the independent variables and school as a random effect.
Null hypotheses for secondary outcomes take a similar form to those for the primary outcome. For example, for the binary outcome of being overweight, the null hypothesis is that the proportion of children who are overweight is the same the between arms. An analysis of the secondary outcomes will, therefore, take a similar form to that described for the primary outcome. Secondary outcomes are either binary (e.g. normal weight vs. overweight) or continuous (e.g. energy expenditure). For binary outcomes we have used Poisson mixed regression; this has been shown to be a reliable way of estimating risk differences (RDs) for binary outcomes when covariate adjustment is needed. 75,76 For continuous outcomes we have used linear mixed regression, with an appropriate transformation to accommodate any non-normality when necessary.
Transformations
To accommodate any non-normality of the outcomes, data were transformed when necessary. To identify which outcome variables required a transformation, a three-step method was used. First, means and medians were calculated and compared for each outcome variable to highlight any clear skew in the data. Second, potential transformations were considered using a ladder of powers plot. 77 This gave a clear indication of whether a variable could be better approximated via a normal distribution before or after transformation. The transformation that visually seemed to represent the best fit via the ladder of powers was then tested to see if it improved goodness of fit. To this end, two models were fitted: one with the data in their raw form and a second with the data in their transformed form. From each model, the residual errors were calculated and plotted. The normality of the residuals was compared between the two models. From this, it was decided whether or not the transformation improved the model. If there was some ambiguity about whether or not the transformed variable improved the model, the preference was to use the untransformed variable, as it aided in the interpretation of the results. Outcomes that needed to be transformed are identified in the relevant results tables. All outcomes requiring transformation were back transformed so that the MDs and confidence intervals (CIs) are presented on the natural scale and comparable for all outcomes. To ensure consistency, outcomes were transformed for all follow-ups using the same transformation, so that if an outcome was transformed at FU1 then the same transformation was used at FU2.
Covariate adjustment
All of the analysis models include a random effect for school. We report a totally unadjusted for covariates result, a partially adjusted result, which is our primary analysis, and a fully adjusted result. The primary partially adjusted analysis will be adjusted for baseline value of the outcome. For binary outcomes, our partially adjusted result adjusts for an appropriate continuous variable that is used when calculating the dichotomous outcome. For example, for obese/overweight, we adjusted for baseline BMI-z; for achieving 60 minutes of at least moderate PA per 24 hours, we adjusted for the baseline minutes of activity per 24 hours that is used to calculate the dichotomous outcome; and for meeting the recommended portions of fruit and vegetables per day, we adjusted for the baseline value of the total grams of fruit and vegetables eaten.
The secondary fully adjusted analysis adjusts for both baseline school- and baseline child-level covariates. Both the baseline child- and baseline school-level covariates to be included in the adjustment were prespecified and included school-level factors that were used in the randomisation. These included school size (number of children attending the school), percentage of pupils eligible for full school meals and ethnic mix of pupils (percentage of school population white, percentage of school population black African Caribbean, percentage of school population South Asian). Pupil-level factors include sex (male/female); baseline BMI-z, ethnicity (white, South Asian, black African Caribbean; and other); deprivation, calculated from home postcode (IMD 2010 score); baseline total energy intake (kJ/day); and baseline total PA expenditure (kJ/kg/day). Age has not been adjusted for, as at each measurement time point there was very limited variation in the children’s ages. We adjust for school- and pupil-level factors for both ethnicity and deprivation, as the school population was expected to differ from the consented study population.
Planned subgroup analyses
We examined whether or not any difference in outcomes between control and intervention arms varies by ethnicity, sex, intervention implementation fidelity, socioeconomic status and obesity levels. For ethnicity we stratified the analysis into white, South Asian and black African Caribbean groups. This stratification was based on the ethnicity of the individual children. For socioeconomic status we stratified the analysis into two groups based on the IMD quintile allocation previously described: children allocated to quintiles 1 and 2 (more deprived) were compared with those allocated to IMD quintiles 3–5 (less deprived). For fidelity, schools that delivered the intervention were allocated implementation fidelity scores for each of the three main intervention programme components, which were then summed to create an overall score for each school. Schools were then ranked by this overall score and divided into tertiles to generate three groups (lower, medium and higher) relating to the level of intervention implementation fidelity achieved. The two intervention schools that did fail to deliver any components of the intervention programme were allocated an overall implementation score of zero and included in the lower implementation fidelity group for this subgroup analysis. Finally, for obesity, we stratified the analysis into two groups and compared those children defined as obese (BMI-z ≥ 95th centile value for relevant age and sex using UK 1990 growth reference charts27) with those defined as not obese.
The significance of subgroup effects is assessed by tests of interactions of these covariates and the treatment effect. The study had low power to detect all but the largest differences.
Exploratory subgroup analyses
A more detailed explanation of why we undertook this exploratory analysis is provided in Chapter 6. A subgroup analysis was conducted on study randomisation ‘groups’. G1 schools received the intervention in the 2011–12 school year, and G2 schools received the intervention in the 2012–13 school year. The significance of the subgroup effect was assessed by a test of interaction between group and treatment arm. In addition, we report the parameter estimate, 95% CI and p-value that correspond to group.
Missing data
The primary analysis is a complete-case analysis. We report the number included in each analysis by arm, so as to allow full consideration of missing data for every result.
In a sensitivity analysis we used multiple imputation.
Reporting of treatment effects
When reporting results, for each continuous outcome we report mean and SD (or median and IQR when appropriate) for baseline and follow-up, along with MD, CI [95% (prespecified key variables) CI or 99% (additional secondary outcomes) CI] and p-value. For binary outcomes we report the number and percentage, again for baseline and follow-up, along with RD, CI and p-value. To obtain the RD from the Poisson model we use a marginal approach whereby we average over the risk in the control group and use the relative risk estimate from the Poisson model [along with its standard error (SE)] to construct a RD and 95% CI. All three of the follow-ups are reported in independent tables.
Statistical significance
The outcomes classified as key anthropometric, diet, PA and psychological variables, and subgroup comparisons at both time points, will be considered significant at the 5% level (and so 95% CIs are reported), whereas other secondary outcomes will be deemed significant at the 1% level (and so 99% CIs are reported). This difference in levels of significance gives more weight to the primary outcomes. Outcomes considered as key anthropometric, diet, PA and psychological variables were prespecified; for continuous variables these are BMI-z, height/waist z-score, sum of four skinfolds, body fat percentage, PA energy expenditure, PedsQL total score, CHU9D utility score and energy intake, and for binary outcomes these are obese, obese/overweight, eating five or more portions of fruit and vegetables and achieving 60 minutes of at least moderate PA per day.
Reporting of intracluster correlations
We report ICCs for all primary and secondary main analyses (unadjusted, partially adjusted and fully adjusted) at all follow-ups. We additionally report ICCs that were estimated with the absence of treatment arm in the model. For continuous outcomes we report the conventional ICC directly from the fitted model. For binary outcomes we report what is known as the conventional ICC on the natural scale, obtained from fitting a linear model to the binary outcome. We report 95% CIs for all ICCs. For all models we were able to report the CI for the ICC using the ‘estat’ function in Stata.
Implementation
All of the analyses were carried out in Stata except the multiple imputation procedures, for which we used REALCOM-IMPUTE (Centre for Multilevel Modelling, Bristol, UK) in conjunction with MLwiN 2.35 (Centre for Multilevel Modelling, Bristol, UK). 78 For the analysis of continuous and binary outcomes, we used the ‘meglm’ command with robust SEs. We used the default estimation method used by the function that involves a mean variance adaptive Gauss–Hermite quadrature, for which the default starting values and default number of integration points in Stata were used.
Changes to analysis methods since protocol stage
Population-averaged models, as opposed to random-effects models (also known as marginal models), were initially specified as the method to allow for clustering. At the protocol stage we had followed guidance in which it was stated that random-effects models lack appropriate interpretation and might be biased. 79 However, before the analysis began, we opted to use the more conventional random-effects approach, as our perception is that this approach is much more commonly used in the analysis of cluster trials. 80
We had also anticipated fitting logistic regression models to binary outcomes and reporting odds ratios. We changed this so that we could report RDs to be consistent with CONSORT (Consolidated Standards of Reporting Trials) guidelines,81 and used a log link to allow the reporting of a RD.
Assessment of the baseline characteristics of randomisation groups 1 and 2 showed an imbalance in the characteristics between the arms within each group and between groups. As such, a post hoc exploratory subgroup analysis of the randomisation groups was conducted (see Chapter 6 for more details).
Sensitivity analyses
In addition to the general methodology, numerous extensions to the standard methods were examined. Each method was chosen to allow the full robustness of results to be methodologically verified. For all of the sensitivity analyses, we restricted the analysis to outcomes classified as key anthropometric, diet, PA and psychological variables. These are the outcomes for which we used a 95% CI in the main results (see Statistical significance). We report the sensitivity analyses for FU1 and FU2, unless stated otherwise.
Multiple imputation
Imputation was conducted for one outcome at a time. For each outcome, the following items were included in the imputation process: outcome of interest, baseline value of outcome, related outcomes (BMI-z at follow-up, height at follow-up, weight at follow-up, waist z-score at follow-up, sum of four skinfolds at follow-up, PedsQL total score at follow-up and PA expenditure at follow-up), treatment arm, ethnicity of individual (white, South Asian, black African Caribbean and other), deprivation quintile of individual (IMD 2010 quintiles), sex, percentage of school population white, percentage of school population black African Caribbean, percentage of school population South Asian, percentage of school population other ethnic group and percentage of school population eligible for free school meals.
To ensure that our inferences are valid, we allow for clustering in the multiple imputation procedure. 82,83 The multiple imputation procedure involves fitting a conditional model for each variable with missing data in which the variable is linearly regressed on all other variables (those with and without missing data). It then uses a Gibbs sampling approach (100 iterations), updating each set of parameters, in turn, conditional on the others. A mixed-effects linear regression model was used to analyse the imputed data. We report the analyses for three models: unadjusted, partially adjusted and fully adjusted. Rubin’s rule84 is used to pool the effect estimates of 10 sets of imputed data. Transformations used in the imputation process were consistent with the main analysis. In the imputation model for binary outcomes, the variable was linear regression on all other variables. A logistic model was then fitted to the data and an odds ratio was estimated. This was then converted to a RD.
Different levels of clustering
Our primary analysis was to allow for clustering at the school level, but we explored sensitivity to models in which clustering at both the class and the school level are included. For this, we added an additional nested random-effects structure into our models, allowing class to be nested within school. We report the treatment effect from these models in addition to the ICCs attributable to the correlation at school and class level for each outcome.
Alternative methods for baseline adjustment
In this repeated cross-sectional cluster trial, we had information on baseline values and follow-up-values. Adjustment for baseline values allows mitigation against any imbalances and also improves the precision of the treatment effect. However, when adjusting for baseline values in our complete-case analysis, we could include only those observations for which both baseline and follow-up-values were available. This resulted in considerable exclusion of data. We therefore explored several methods that have been proposed in the literature85,86 as alternative ways of adjusting for baseline values that might lead to fewer observations being excluded.
First, instead of adjusting for individual baseline values, adjustment using cluster-level means was undertaken. This resulted in only observations without a follow-up value being excluded. Second, we treated each observation in the data set, both baseline and follow-up, as an outcome and included an indicator to denote which observations were exposed and which were unexposed to the intervention, and another variable to indicate which were baseline and which were follow-up-values. We then fitted a mixed model with a random effect for cluster, a random effect for individual (to allow dependence between the repeated measures on the same person) and an interaction between treatment and period, which is the intervention effect.
Treatment by cluster variation in heterogeneity
Our main analyses assumed that the ICC was the same in both arms. An intervention might induce heterogeneity or even homogeneity. To allow for this, we additionally fitted models in which two random effects were included. One random effect was included for schools in the control arm, and a second random effect was included for schools in the intervention arm.
Chapter 6 Results
Participant flow
A chart summarising the eligibility, trial arm allocation and subsequent progress of schools (cluster level) and consented pupils (participant level) is provided in Figure 7.
FIGURE 7.
The CONSORT flow diagram for the WAVES study randomised controlled trial. Reproduced from Adab et al. ,87 with permission.
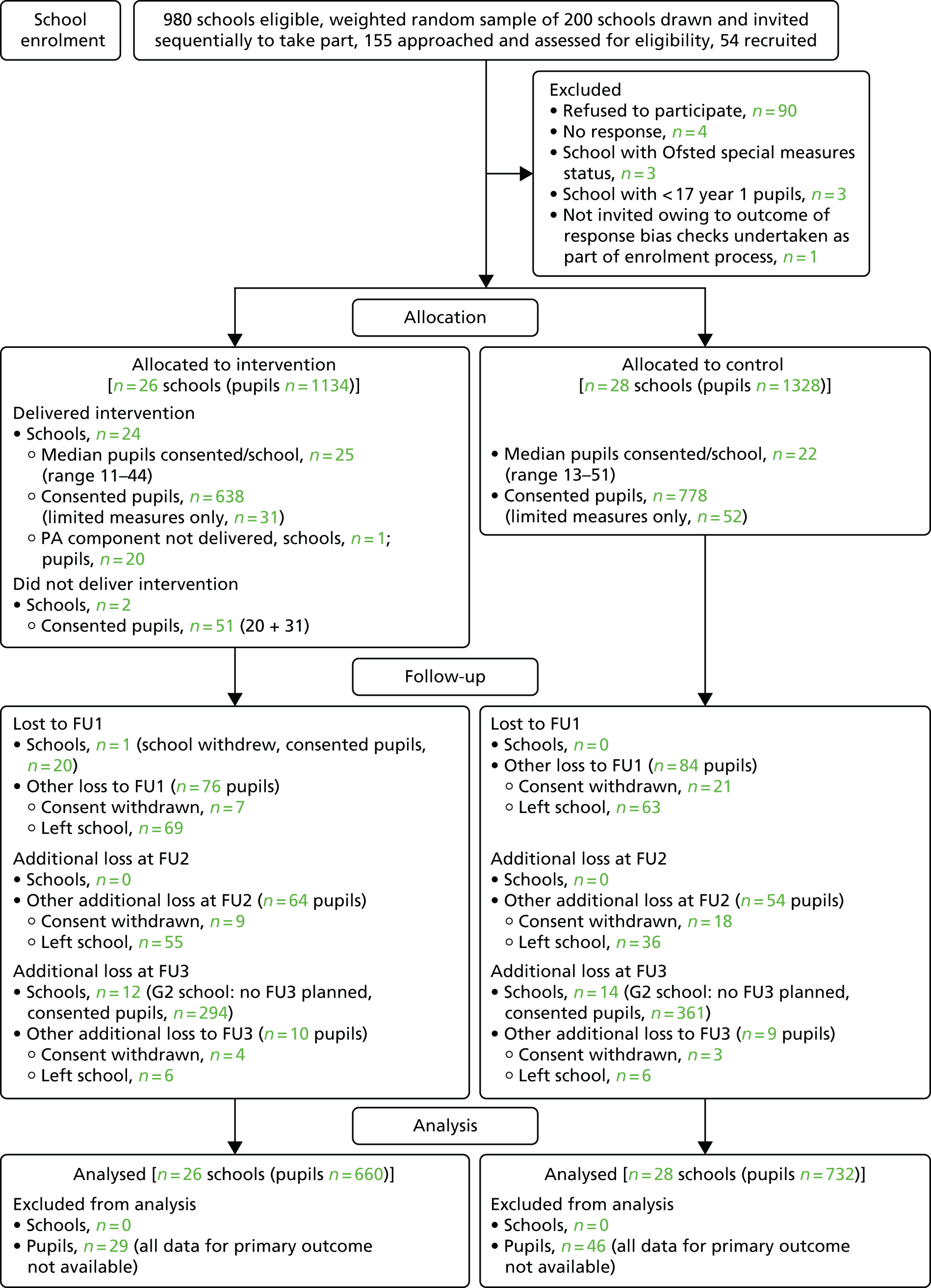
Assessing the risk of bias in the WAVES study
A timeline cluster tool for the WAVES study is provided in Figure 8 and Table 11. Schools were identified and recruited using a weighted random sampling process to guarantee a mix of ethnicities within the study. Following this, letters and accompanying documentation were sent to each school for distribution to the parents of their year 1 pupils. Following the recruitment of schools and pupils, baseline pupil measures were undertaken. During baseline assessment and recruitment, there was no allocation to the intervention, so it was completely blinded. The randomisation process was conducted after baseline assessment. A blocked balancing algorithm was used to randomise schools to the treatment arms. Participating schools were then informed of their allocation.
FIGURE 8.
A timeline cluster diagram to assess the risk of bias. The rings and stick figures refer to the stages that involve schools (cluster) and pupils (individuals), respectively. A stage involving school-level only is represented by a ring only, whereas a stage involving pupils only is represented by a stick figure only. Stages involving pupils and schools are represented by both rings and stick figure (e.g. baseline observations). The shading of the background of the boxes refers to the level of blinding present. Boxes with dark green shading refer to stages with complete blinding, boxes with light green shading refer to partial blinding, and no shading indicates no blinding. Points that are separated by distinct boxes for intervention and control arms represent stages that differ between the trial arms. Reproduced from Adab et al. ,87 with permission.

| Stage number | Stage description |
|---|---|
| 1 | Cluster identification All state-maintained schools in the West Midlands that included school years 1–5 and that were within a 35-mile radius of the University of Birmingham were eligible for inclusion. Two hundred schools were then sampled using a weighted random sampling process to ensure a sufficient mix of ethnicities. The 200 schools were ordered using a random number generator and sequentially invited to take part in the study until the required sample size was met. The sampling process and random ordering of the sample were carried out by the trial statistician |
| 2 | Cluster recruitment Schools were initially approached by letter, before follow-up telephone communication and face-to-face visits to interested schools. This process was carried out by the trial co-ordinator |
| 3 | Patient identification All year 1 pupils (aged 5–6 years) were eligible to take part in the study. Participating schools were advised that the research team would provide a letter and accompanying documentation for each eligible pupil for distribution by the school to their parent/carer |
| 4 | Patient recruitment An invitation letter, an information leaflet and a consent form for each eligible pupil were sent to schools for distribution to their parent/carer. Opt-in parental consent was used for the full set of measures in both G1 and G2 schools. In addition, for G2 schools with low recruitment numbers for the opt-in consent, an opt-out consent was used for a limited set of the measures. Pupils for whom consent was withdrawn or dropped owing to them leaving the school were excluded from the time point at which this happened. Pupils who joined the school at a later date (i.e. year 2 onwards) were not included |
| 5 | Participant and cluster baseline assessment Baseline measurements were taken when participating pupils were in year 1 (aged 5–6 years). Pupils’ date of birth, sex, ethnicity and postcode (used as a proxy for deprivation) were obtained from a parent questionnaire or from school records. Assessment of outcomes was carried out by trained research staff using standardised procedures and validated instruments. Collection of dietary information was undertaken using a validated method, completed by researchers (in school) and a parent/carer (out of school). Psychosocial measures were assessed through validated questionnaires administered to the pupils by trained researchers. PA was measured objectively over 5 days, including at a weekend, using Actiheart monitors. School-level data were collected from local education authorities or from a questionnaire completed by the head teacher or a nominated representative |
| 6 | Randomisation A blocked balancing algorithm was used to randomise schools to the control and intervention arms. The algorithm randomly selected one of a number of allocation designs, which minimised the imbalance between a set of prespecified covariate means. The covariates included were percentage of pupils within the school eligible for free school meals, percentage of South Asian pupils within the school, percentage of black African Caribbean pupils within the school, percentage of white pupils within the school and the number of pupils within the school. Participating schools were then informed of their allocation |
| 7a | Intervention delivery No blinding for pupils, parents or teachers. Implementation fidelity was assessed throughout the intervention year using a range of methods, including direct observation, logbooks, parent and school staff questionnaires, research staff experiences and qualitative evaluation |
| 7b | Usual care No blinding for pupils, parents or teachers |
| 8 | Outcome assessment: FU1 FU1 measurements were taken when participating pupils were in year 3 (aged 7–8 years). Assessment of outcomes was carried out by trained research staff using standardised procedures and validated instruments. Collection of dietary information was undertaken using a validated method, completed by researchers (in school) and a parent/carer (out of school). Psychosocial measures were assessed through validated questionnaires administered to the pupils by trained researchers. PA was measured objectively over 5 days, including at a weekend, using Actiheart monitors |
| 9 | Outcome assessment: FU2 FU2 measurements were taken when participating pupils were in year 4 (aged 8–9 years). Assessment of outcomes was carried out by trained research staff using standardised procedures and validated instruments. Collection of dietary information was undertaken using a validated method, completed by researchers (in school) and a parent/carer (out of school). Psychosocial measures were assessed through validated questionnaires administered to the pupils by trained researchers. PA was measured objectively over 5 days, including at a weekend, using Actiheart monitors |
| 10 | Outcome assessment: FU3 FU3 measurements were taken when participating pupils were in year 5 (aged 9–10 years). Assessment of outcomes was carried out by trained research staff using standardised procedures and validated instruments. Collection of dietary information was undertaken using a validated method, completed by researchers (in school) and a parent/carer (out of school). Psychosocial measures were assessed through validated questionnaires administered to the pupils by trained researchers |
Owing to the nature of the intervention, it was impossible to blind pupils, parents or teachers to their allocation. Efforts were made to keep research staff responsible for pupil assessment blind to allocation, but complete blinding was not possible. The majority of the assessments were undertaken by sessional staff who were not advised of allocation, but trial arm could have been revealed to them by a comment from a school pupil or member of school staff. A questionnaire was used to try to assess awareness of allocation among these staff, and, from the 17 completed, only one staff member indicated that he/she had ever been aware of arm allocation, suggesting that, in general, blinding of the sessional staff was maintained. In addition, it was not possible to blind core research team staff to allocation, as they were involved in the process evaluation observations of the intervention. The main role of these staff members was to supervise the sessional measurement staff and the fitting of the activity monitors; however, the involvement of core research staff in assessments was sometimes necessary.
Recruitment
Group 1 schools and pupils were recruited between April and May 2011. G2 schools were recruited between January and April 2012, with pupil recruitment from January to May 2012. In total, 149 eligible schools were approached to obtain the target number of 54 recruited schools. From the 2462 eligible pupils within the participating schools, parental consent for study measurements was obtained for 1467 children (59.6%). The consent was ‘opt in’ for the full set of measures for 1384 pupils (94% of consents) and ‘opt out’ for the limited measures for 83 pupils (6% of consents). [For dates defining the measurement periods (baseline and FU1–3), see Chapter 2.]
Baseline data
A comparison of baseline demographic characteristics between pupils with and pupils without parental consent to participate in the WAVES study measures is provided in Table 12. These data were requested from schools for all of the pupils who were eligible to take part in the WAVES study. However, some schools were prepared to provide the information for consented pupils only. From individuals for whom the data were available, compared with those without consent, pupils with consent were less likely to be of South Asian (30.5% vs. 40.8%) or black African Caribbean (7.9% vs. 9.1%) ethnicity, or to be living in an area classified as being one of the 20% most deprived in England (54.9% vs. 64.2%).
| Characteristic: N (number with consent) | Pupils | Total | |
|---|---|---|---|
| With parental consent | Without parental consent | ||
| Sex: N = 2218 (1467), n (%) | |||
| Male | 749 (51.1) | 396 (52.7) | 1145 (51.6) |
| Female | 718 (48.9) | 355 (47.3) | 1073 (48.4) |
| Not knowna | 0a | 244a | 244a |
| Ethnicity: N = 2165 (1451), n (%) | |||
| White British | 658 (45.3) | 222 (31.1) | 880 (40.6) |
| South Asian | 443 (30.5) | 291 (40.8) | 734 (33.9) |
| Black African Caribbean | 115 (7.9) | 65 (9.1) | 180 (8.3) |
| Other | 235 (16.2) | 136 (19.0) | 371 (17.1) |
| Not knowna | 16a | 281a | 297a |
| IMD quintile: N = 2093 (1439), n (%) | |||
| 1 (most deprived) | 790 (54.9) | 433 (66.2) | 1223 (58.4) |
| 2 | 274 (19.0) | 85 (13.0) | 359 (17.2) |
| 3 | 146 (10.1) | 58 (8.9) | 204 (9.7) |
| 4 | 119 (8.3) | 36 (5.5) | 155 (7.4) |
| 5 (least deprived) | 110 (7.6) | 42 (6.4) | 152 (7.3) |
| Not knowna | 28a | 341a | 369a |
| IMD score: N = 2093 (1439), median (IQR) | 38.9 (20.1–49.5) | 44.6 (26.9–54.4) | 40.2 (21.7–51.4) |
Baseline pupil-level demographic characteristics and key anthropometric, diet, PA and psychological data are presented in Table 13, both overall and by trial arm, with the data by trial arm showing some imbalance at baseline between the groups. A comparison of intervention with control participants’ demographic characteristics shows that they were less likely to be male (49.2% vs. 52.7%), more likely to be of South Asian (32.7% vs. 28.6%) or black African Caribbean (9.2% vs. 6.8%) ethnicity, and more likely to be from more deprived households (mean IMD 2010 score 39.8 vs. 37.6). In terms of the prespecified key anthropometric, diet, PA and psychological variables, intervention arm participants had higher mean BMI and waist z-scores (0.23 vs. 0.15 and 0.77 vs. 0.66, respectively) and body fat percentage (21.30 vs. 20.95), and are less likely to meet the current government healthy lifestyle recommendations for children (46.4% vs. 49.6% meeting the 60-minute minimum target for being at least moderately physically active and 59.8% vs. 64.8% consuming five or more portions of fruit and vegetables a day) than those in the control arm.
| Characteristic: N (number in intervention arm) | Arm | Total | |
|---|---|---|---|
| Intervention | Control | ||
| Demographic | |||
| Age (years): N = 1397 (662), mean (SD) – not known: intervention = 27, control = 43 | 6.31 (0.30) | 6.27 (0.31) | 6.29 (0.31) |
| Sex: N = 1467 (689), n (%) | |||
| Male | 339 (49.2) | 410 (52.7) | 749 (51.1) |
| Female | 350 (50.8) | 368 (47.3) | 718 (48.9) |
| Ethnicity: N = 1451 (676), n (%) | |||
| White British | 297 (43.9) | 361 (46.6) | 658 (45.3) |
| South Asian | 221 (32.7) | 222 (28.6) | 443 (30.5) |
| Black African Caribbean | 62 (9.2) | 53 (6.8) | 115 (7.9) |
| Other | 96 (14.2) | 139 (17.9) | 235 (16.2) |
| Not known | 13a | 3a | 16a |
| IMD quintile: N = 1439 (670), n (%) | |||
| 1 (most deprived) | 392 (58.5) | 398 (51.8) | 790 (54.9) |
| 2 | 120 (17.9) | 154 (20.0) | 274 (19.0) |
| 3 | 72 (10.7) | 74 (9.6) | 146 (10.1) |
| 4 | 65 (9.7) | 54 (7.0) | 119 (8.3) |
| 5 (least deprived) | 21 (3.1) | 89 (11.6) | 110 (7.6) |
| Not known | 19a | 9a | 28a |
| IMD score: N = 1439 (670), median (IQR) – not known: intervention = 19, control = 9 | 39.80 (21.86–52.68) | 37.60 (17.89–48.79) | 38.93 (20.14–49.49) |
| Anthropometric | |||
| BMI-z: N = 1392 (660), mean (SD) – not known: intervention = 29, control = 46 | 0.23 (1.24) | 0.15 (1.20) | 0.19 (1.22) |
| Height (cm): N = 1396 (664), mean (SD) – not known: intervention = 25, control = 46 | 118.63 (5.60) | 118.18 (5.38) | 118.39 (5.49) |
| Waist circumference z-score: N = 1259 (589), mean (SD) – not known: intervention = 100, control = 108 | 0.77 (1.24) | 0.66 (1.25) | 0.71 (1.25) |
| Sum of four skinfoldsb (mm): N = 1137 (540), median (IQR) – not known: intervention = 149, control = 181 | 28.55 (23.30–35.43) | 28.10 (23.00–36.60) | 28.35 (23.10–36.05) |
| Body fat %: N = 1376 (660), mean (SD) – not known: intervention = 29, control = 62 | 21.30 (5.35) | 20.95 (5.22) | 21.12 (5.28) |
| Weight status:c N = 1392 (660), n (%) | |||
| Underweight (≤ 2nd centile) | 20 (3.0) | 20 (2.7) | 40 (2.9) |
| Healthy weight (> 2nd and < 85th centiles) | 495 (75.0) | 562 (76.8) | 1057 (75.9) |
| Overweight (≥ 85th and < 95th centiles) | 61 (9.2) | 63 (8.6) | 124 (8.9) |
| Obese (≥ 95th centile) | 84 (12.7) | 87 (11.9) | 171 (12.3) |
| Not known | 29a | 46a | 75a |
| 24-hour dietary intake | |||
| Energy (kJ in 24 hours): N = 1187 (562), median (IQR) – not known: intervention = 127, control = 153 | 6904 (5865–8054) | 6911 (5804–7964) | 6907 (5829–8002) |
| Five or more portions of fruit and vegetables: N = 1187 (562), n (%) | |||
| Yes | 336 (59.8) | 405 (64.8) | 741 (62.4) |
| No | 226 (40.2) | 220 (35.2) | 446 (37.6) |
| Not known | 127a | 153a | 280a |
| PA | |||
| PA energy expenditure (kJ/kg/day): N = 1052 (492), mean (SD) – not known: intervention = 197, control = 218 | 96.43 (23.16) | 94.08 (24.38) | 95.18 (23.83) |
| ≥ 60 minutes’ MVPA/24 hours: N = 1048 (491), n (%) | |||
| Yes | 228 (46.4) | 276 (49.6) | 504 (48.1) |
| No | 263 (53.6) | 281 (50.4) | 544 (51.9) |
| Not known | 198a | 221a | 419a |
| Psychological | |||
| PedsQL total score: N = 1384 (663), median (IQR) – not known: intervention = 26, control = 57 | 71.74 (60.87–82.61) | 73.91 (60.87–82.61) | 71.74 (60.87–82.61) |
| CHU9D utility score: N = 1350 (643), mean (SD) – not known: intervention = 46, control = 71 | 0.84 (0.13) | 0.82 (0.14) | 0.83 (0.14) |
For the additional anthropometric, diet, PA and psychological variables considered, there was a reasonably good balance between the control and intervention arms (Table 14). This was also generally true for the school-level characteristics, as shown in Table 15.
| Characteristic: N (number in intervention arm) | Arm | Total | |
|---|---|---|---|
| Intervention | Control | ||
| Anthropometric | |||
| Subscapular skinfold (mm): N = 1187 (558), median (IQR) – not known: intervention = 131, control = 149 | 5.98 (5.05–7.30) | 5.80 (4.95–7.20) | 5.85 (5.00–7.25) |
| Suprailiac skinfold (mm): N = 1184 (565), median (IQR) – not known: intervention = 124, control = 159 | 6.50 (4.75–9.45) | 6.10 (4.55–9.30) | 6.30 (4.70–9.33) |
| Biceps skinfold (mm): N = 1220 (580), median (IQR) – not known: intervention = 109, control = 138 | 6.15 (4.80–7.80) | 6.15 (4.70–8.40) | 6.15 (4.70–8.10) |
| Triceps skinfold (mm): N = 1213 (574), median (IQR) – not known: intervention = 115, control = 139 | 9.80 (7.90–12.30) | 10.00 (7.95–12.60) | 9.90 (7.90–12.45) |
| Thigh skinfold (mm): N = 1031 (494), median (IQR) – not known: intervention = 195, control = 241 | 13.43 (11.10–16.75) | 13.30 (10.90–17.20) | 13.35 (10.93–17.00) |
| Bioimpedance (Ω): N = 1373 (657), mean (SD) – not known: intervention = 32, control = 62 | 656.13 (81.30) | 654.00 (82.33) | 655.02 (81.82) |
| PA | |||
| Sedentary hours/24 hours: N = 1048 (491), mean (SD) – not known: intervention = 198, control = 221 | 14.42 (1.88) | 14.57 (1.78) | 14.50 (1.83) |
| MVPA minutes/24 hours: N = 1048 (491), median (IQR) – not known: intervention = 198, control = 221 | 57.91 (42.52–85.90) | 59.47 (42.80–81.53) | 58.68 (42.59–82.84) |
| Blood pressure | |||
| Systolic (mmHg): N = 1332 (634), mean (SD) – not known: intervention = 55, control = 80 | 95.67 (9.04) | 98.10 (10.06) | 96.94 (9.66) |
| Diastolic (mmHg): N = 1332 (634), mean (SD) – not known: intervention = 55, control = 80 | 62.18 (7.99) | 64.21 (8.59) | 63.24 (8.37) |
| 24-hour dietary intake | |||
| Fat (grams in 24 hours): N = 1187 (562), median (IQR) – not known: intervention = 127, control = 153 | 56.08 (45.39–69.28) | 54.74 (44.75–67.58) | 55.55 (45.06–68.13) |
| Free sugar (grams in 24 hours): N = 1187 (562), mean (SD) – not known: intervention = 127, control = 153 | 76.63 (31.01) | 76.13 (30.88) | 76.37 (30.93) |
| Fibre (grams in 24 hours): N = 1187 (562), median (IQR) – not known: intervention = 127, control = 153 | 11.00 (8.80–13.68) | 11.35 (8.99–13.95) | 11.20 (8.91–13.80) |
| Fruit and vegetables (grams in 24 hours): N = 1187 (562), median (IQR) – not known: intervention = 127, control = 153 | 226.92 (132.00–330.09) | 247.58 (157.25–341.40) | 233.08 (143.62–334.36) |
| Psychological | |||
| PedsQL physical functioning score: N = 1384 (663), mean (SD) – not known: intervention = 26, control = 57 | 73.06 (18.07) | 74.87 (17.26) | 74.00 (17.67) |
| PedsQL psychosocial functioning score: N = 1384 (663), mean (SD) – not known: intervention = 26, control = 57 | 69.47 (17.95) | 69.28 (18.19) | 69.37 (18.07) |
| PedsQL emotional functioning score: N = 1384 (663), mean (SD) – not known: intervention = 26, control = 57 | 73.36 (22.20) | 71.68 (23.05) | 72.49 (22.65) |
| PedsQL social functioning score: N = 1383 (662), mean (SD) – not known: intervention = 27, control = 57 | 67.72 (22.34) | 68.60 (21.71) | 68.18 (22.01) |
| PedsQL school functioning score: N = 1382 (663), mean (SD) – not known: intervention = 26, control = 59 | 67.35 (21.72) | 67.54 (21.56) | 67.45 (21.63) |
| KIDSCREEN-52 bullying: N = 1374 (661), mean (SD) – not known: intervention = 28, control = 65 | 11.74 (3.20) | 12.05 (2.97) | 11.91 (3.08) |
| Body image satisfaction score: N = 1374 (663), mean (SD) – not known: intervention = 26, control = 67 | 0.17 (2.07) | 0.43 (2.05) | 0.31 (2.06) |
| Characteristic | Intervention arm, median (IQR) (n = 26) | Control arm, median (IQR) (n = 28) | Total arm, median (IQR) (N = 54) |
|---|---|---|---|
| % black African or Caribbean pupils on roll | 3.70 (1.40–8.30) | 6.06 (0.88–12.70) | 5.10 (1.01–11.90) |
| % South Asian pupils on roll | 22.70 (1.39–51.90) | 21.80 (2.30–48.30) | 21.80 (2.30–48.30) |
| % of pupils eligible for a free school meal | 29.60 (19.31–41.60) | 23.59 (14.50–34.80) | 27.00 (19.31–37.80) |
| Total number of pupils on roll | 300 (216–394) | 327 (202–478) | 327 (206–429) |
Numbers analysed
All of the analyses undertaken were by intention to treat. At baseline, one or more of the variables needed to calculate the primary outcome was not available for 75 pupils. This was mainly due to consented children being absent from school on measurement days, although six had left the school and a handful did not assent to some measurements: two children did not agree to either height or weight measurement and an additional child did not agree to height measurement only. One intervention arm school (pupils = 20) was excluded from all of the analyses involving follow-up data because of its withdrawal from the study after baseline measurement completion. Fifty-three schools (control arm, n = 28; intervention arm, n = 25) were therefore included in the FU1 and FU2 analyses. In addition to the 20 pupils from the withdrawn school, a further 160 were lost to FU1: 28 owing to the parent withdrawing consent and 132 owing to the pupil changing school. The maximum number of pupils available for analysis at FU1 was therefore 1287, with primary outcome data available for 1249 pupils (the gap being due to pupil absence on measurement days).
Between FU1 and FU2, an additional 118 pupils were excluded: 27 owing to the parent withdrawing consent and 91 owing to the pupil no longer attending the school, resulting in a maximum number of 1169 pupils available for analysis at FU2 (1145 with primary outcome data). Analyses at FU3 were for G1 schools (n = 27: control, n = 14; intervention, n = 13; maximum number of pupils available for analysis n = 509, primary outcome data available n = 488). The number of participants included for each outcome (overall and by trial arm) is provided for all of the models in the first column of each results table. Numbers vary between outcomes because of either lack of assent from a few children for some measures or exclusion of data as previously described (see Chapter 2). For the primary analysis of the secondary outcomes, data availability was lowest in relation to the PA and thigh skinfold thickness variables (n = 720 and n = 571, n = 826 and n = 610, at FU1 and FU2, respectively). For the remaining outcomes, valid data were available for between 902 and 1200 children at FU1, 724 and 1096 children at FU2, and 330 and 468 children at FU3 (G1 schools only for prespecified key variables).
Outcomes and estimation
The results for the prespecified key anthropometric, diet, PA and psychological variables are presented for both continuous and binary outcomes at FU1 in Table 16 (corresponding ICCs are reported in Table 17), at FU2 in Table 18 (corresponding ICCs are reported in Table 19) and at FU3 in Table 20 (corresponding ICCs are reported in Table 21). Results are reported below for the partially adjusted primary analysis (which adjusts for the baseline value of the outcome only) and also for the fully adjusted model (which additionally adjusts for the prespecified pupil and school-level baseline characteristics). When values are reported without value model specification, the values are for the partially adjusted analyses. With the exception of height, included for BMI interpretation, the outcomes are reported for each time point in the same order as the variables are presented in the results tables.
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value |
| BMI-z | ||||||||||
| N = 1249 (n = 574, unadjusted) | 0.23 (1.24) | 0.34 (1.34) | 0.15 (1.20) | 0.23 (1.27) | 0.101 (–0.073 to 0.275) | 0.255 | –0.075 (–0.183 to 0.033) | 0.175 | –0.077 (–0.191 to 0.037) | 0.186 |
| N = 1197 (n = 556, partially adjusted) | ||||||||||
| N = 837 (n = 393, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 1251 (n = 575, unadjusted) | 118.63 (5.60) | 127.37 (6.09) | 118.18 (5.38) | 127.03 (5.75) | 0.346 (–0.255 to 0.947) | 0.259 | –0.073 (–0.652 to 0.505) | 0.804 | –0.198 (–0.798 to 0.402) | 0.517 |
| N = 1200 (n = 558, partially adjusted) | ||||||||||
| N = 837 (n = 392, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 1151 (n = 528, unadjusted) | 0.77 (1.24) | 1.05 (1.36) | 0.66 (1.25) | 0.87 (1.32) | 0.177 (0.005 to 0.348) | 0.043 | 0.026 (–0.168 to 0.220) | 0.794 | 0.019 (–0.122 to 0.161) | 0.789 |
| N = 1069 (n = 490, partially adjusted) | ||||||||||
| N = 796 (n = 368, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 1048 (n = 488, unadjusted) | 28.55 (23.30–35.43) | 31.48 (24.57–43.65) | 28.10 (23.00–36.60) | 29.40 (23.63–41.67) | 1.317 (–0.231 to 2.864) | 0.095 | 0.366 (–0.157 to 0.890) | 0.170 | 0.417 (–0.193 to 1.027) | 0.180 |
| N = 902 (n = 421, partially adjusted) | ||||||||||
| N = 683 (n = 323, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 1236 (n = 574, unadjusted) | 21.30 (5.35) | 21.79 (6.73) | 20.95 (5.22) | 20.87 (6.30) | 0.841 (–0.040 to 1.722) | 0.061 | 0.040 (–0.707 to 0.786) | 0.917 | 0.048 (–0.749 to 0.845) | 0.906 |
| N = 1169 (n = 553, partially adjusted) | ||||||||||
| N = 822 (n = 391, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 1112 (n = 507, unadjusted) | 6904 (5865–8054) | 7152 (6107–8376) | 6911 (5804–7964) | 7074 (5963–8233) | 122.611 (–213.680 to 458.902) | 0.475 | 61.531 (–217.772 to 340.834) | 0.666 | 30.988 (–257.865 to 319.840) | 0.833 |
| N = 978 (n = 449, partially adjusted) | ||||||||||
| N = 803 (n = 369, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 868 (n = 395, unadjusted) | 96.43 (23.16) | 91.70 (23.71) | 94.08 (24.38) | 91.27 (25.42) | –0.207 (–4.552 to 4.137) | 0.926 | –0.866 (–5.389 to 3.658) | 0.708 | –1.762 (–5.753 to 2.228) | 0.387 |
| N = 724 (n = 335, partially adjusted) | ||||||||||
| N = 658 (n = 310, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 1231 (n = 554, unadjusted) | 71.74 (60.87–82.61) | 76.09 (65.22–84.78) | 73.91 (60.87–82.61) | 76.09 (65.22–84.78) | –0.662 (–2.805 to 1.481) | 0.545 | –0.630 (–3.487 to 2.227) | 0.665 | –0.437 (–3.354 to 2.481) | 0.769 |
| N = 1171 (n = 538, partially adjusted) | ||||||||||
| N = 817 (n = 375, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 1215 (n = 550, unadjusted) | 0.84 (0.13) | 0.87 (0.11) | 0.82 (0.14) | 0.86 (0.10) | 0.012 (–0.007 to 0.030) | 0.230 | 0.010 (–0.009 to 0.029) | 0.300 | 0.015 (–0.007 to 0.037) | 0.185 |
| N = 1130 (n = 519, partially adjusted) | ||||||||||
| N = 786 (n = 358, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value |
| Obeseh | ||||||||||
| N = 1249 (n = 574, unadjusted) | 84 (12.73) | 93 (16.20) | 87 (11.89) | 100 (14.81) | 0.014 (–0.018 to 0.053) | 0.381 | –0.036 (–0.066 to 0.004) | 0.074 | –0.007 (–0.038 to 0.031) | 0.676 |
| N = 1197 (n = 556, partially adjusted) | ||||||||||
| N = 837 (n = 393, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 1249 (n = 574, unadjusted) | 145 (21.97) | 165 (28.75) | 150 (20.49) | 167 (24.74) | 0.040 (–0.006 to 0.095) | 0.093 | –0.013 (–0.061 to 0.048) | 0.655 | 0.000 (–0.050 to 0.064) | 0.994 |
| N = 1197 (n = 556, partially adjusted) | ||||||||||
| N = 837 (n = 393, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 1112 (n = 507, unadjusted) | 336 (59.79) | 244 (48.13) | 405 (64.80) | 297 (49.09) | –0.010 (–0.085 to 0.080) | 0.820 | –0.014 (–0.090 to 0.077) | 0.753 | 0.004 (–0.057 to 0.074) | 0.900 |
| N = 978 (n = 449, partially adjusted) | ||||||||||
| N = 803 (n = 369, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 866 (n = 396, unadjusted) | 228 (46.44) | 207 (52.27) | 276 (49.55) | 234 (49.79) | 0.015 (–0.076 to 0.126) | 0.762 | 0.041 (–0.058–0.163) | 0.446 | 0.005 (–0.078 to 0.105) | 0.911 |
| N = 720 (n = 334, partially adjusted) | ||||||||||
| N = 654 (n = 310, fully adjusted) | ||||||||||
| Outcome | Unadjusted ICC | ICC adjusted for treatment arm | Partially adjusted ICCa | Fully adjusted ICCb |
|---|---|---|---|---|
| Continuous outcomes | ||||
| BMI-z | 0.0211 (0.0074 to 0.0590) | 0.0193 (0.0063 to 0.0577) | 0.0858 (0.0501 to 0.1432) | 0.0805 (0.0441 to 0.1423) |
| Height (cm) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.2913 (0.2096 to 0.3893) | 0.3750 (0.2813 to 0.4790) |
| Waist z-score | 0.0136 (0.0027 to 0.0650) | 0.0089 (0.0010 to 0.0772) | 0.1538 (0.0950 to 0.2394) | 0.1094 (0.0619 to 0.1860) |
| Sum of four skinfolds (mm) | 0.0051 (0.0001 to 0.1808) | 0.0029 (0.0000 to 0.5966) | 0.1466 (0.0906 to 0.2286) | 0.1215 (0.0710 to 0.2002) |
| Body fat % | 0.0252 (0.0101 to 0.0616) | 0.0208 (0.0074 to 0.0572) | 0.1032 (0.0620 to 0.1669) | 0.1059 (0.0620 to 0.1752) |
| Energy intake (kJ in 24 hours) | 0.0534 (0.0275 to 0.1012) | 0.0525 (0.0269 to 0.1000) | 0.0418 (0.0184 to 0.0921) | 0.0363 (0.0148 to 0.0865) |
| PA energy expenditure (kJ/kg/day) | 0.0493 (0.0220 to 0.1068) | 0.0493 (0.0220 to 0.1068) | 0.0819 (0.0410 to 0.1570) | 0.0556 (0.0222 to 0.1329) |
| PedsQL total score | 0.0403 (0.0189 to 0.0839) | 0.0395 (0.0184 to 0.0829) | 0.0394 (0.0181 to 0.0839) | 0.0176 (0.0037 to 0.0799) |
| CHU9D utility score | 0.0577 (0.0297 to 0.1094) | 0.0559 (0.0286 to 0.1066) | 0.0587 (0.0296 to 0.1134) | 0.0604 (0.0293 to 0.1203) |
| Binary outcomes | ||||
| Obesec | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) |
| Obese/overweightc | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0192 (0.0052 to 0.0684) | 0.0040 (0.0000 to 0.6448) |
| Five or more portions of fruit and vegetablesd | 0.0390 (0.0171 to 0.0864) | 0.0390 (0.0171 to 0.0865) | 0.0313 (0.0118 to 0.0806) | 0.0000 (0.0000 to 0.0000) |
| Achieving ≥ 60 minutes of PAe | 0.0641 (0.0326 to 0.1222) | 0.0642 (0.0327 to 0.1225) | 0.0770 (0.0382 to 0.1488) | 0.0568 (0.0241 to 0.1282) |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)a | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI)a | p-valuec |
| BMI-z | ||||||||||
| N = 1145 (n = 524, unadjusted) | 0.23 (1.24) | 0.42 (1.34) | 0.15 (1.20) | 0.31 (1.32) | 0.103 (–0.053 to 0.258) | 0.197 | –0.027 (–0.137 to 0.083) | 0.627 | –0.042 (–0.163 to 0.080) | 0.500 |
| N = 1094 (n = 505, partially adjusted) | ||||||||||
| N = 772 (n = 359, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 1146 (n = 524, unadjusted) | 118.63 (5.60) | 134.73 (6.68) | 118.18 (5.38) | 134.86 (6.43) | –0.135 (–0.945 to 0.675) | 0.744 | –0.483 (–1.120 to 0.154) | 0.137 | –0.639 (–1.235 to –0.044) | 0.035 |
| N = 1096 (n = 506, partially adjusted) | ||||||||||
| N = 773 (n = 359, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 990 (n = 446, unadjusted) | 0.77 (1.24) | 1.15 (1.25) | 0.66 (1.25) | 0.90 (1.35) | 0.240 (0.041 to 0.440) | 0.018 | 0.103 (–0.042 to 0.248) | 0.163 | 0.068 (–0.085 to 0.221) | 0.383 |
| N = 923 (n = 414, partially adjusted) | ||||||||||
| N = 703 (n = 320, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 845 (n = 381, unadjusted) | 28.55 (23.30–35.43) | 34.70 (25.50–49.95) | 28.10 (23.00–36.60) | 31.93 (24.00–48.90) | 1.927 (–0.402 to 4.256) | 0.105 | 0.644 (0.103 to 1.186) | 0.020 | 0.532 (–0.077 to 1.141) | 0.087 |
| N = 724 (n = 334, partially adjusted) | ||||||||||
| N = 560 (n = 262, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 1115 (n = 516, unadjusted) | 21.30 (5.35) | 22.52 (7.48) | 20.95 (5.22) | 21.58 (7.26) | 0.921 (–0.020 to 1.863) | 0.055 | 0.344 (–0.396 to 1.085) | 0.362 | 0.166 (–0.715 to 1.047) | 0.712 |
| N = 1051 (n = 495, partially adjusted) | ||||||||||
| N = 747 (n = 354, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 1015 (n = 453, unadjusted) | 6904 (5865–8054) | 7656 (6436–9118) | 6911 (5804–7964) | 7817 (6748–9212) | –214.643 (–561.717 to 132.430) | 0.225 | –139.552 (–467.690 to 188.585) | 0.405 | –273.658 (–616.542 to 69.225) | 0.118 |
| N = 895 (n = 401, partially adjusted) | ||||||||||
| N = 729 (n = 331, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 690 (n = 305, unadjusted) | 96.43 (23.16) | 79.66 (22.26) | 94.08 (24.38) | 78.60 (22.43) | 1.184 (–3.254 to 5.623) | 0.601 | 0.001 (–4.371 to 4.373) | 0.999 | –0.224 (–4.120 to 3.672) | 0.910 |
| N = 571 (n = 253, partially adjusted) | ||||||||||
| N = 520 (n = 237, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 1116 (n = 495, unadjusted) | 71.74 (60.87–82.61) | 82.61 (71.74–89.13) | 73.91 (60.87–82.61) | 80.43 (71.74–89.13) | 0.997 (–1.301 to 3.295) | 0.395 | 1.248 (–1.453 to 3.948) | 0.365 | 1.246 (–1.083 to 3.575) | 0.294 |
| N = 1055 (n = 477, partially adjusted) | ||||||||||
| N = 755 (n = 346, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 1131 (n = 517, unadjusted) | 0.84 (0.13) | 0.89 (0.09) | 0.82 (0.14) | 0.90 (0.09) | –0.004 (–0.018 to 0.011) | 0.617 | –0.006 (–0.021 to 0.010) | 0.481 | –0.007 (–0.023 to 0.009) | 0.405 |
| N = 1049 (n = 486, partially adjusted) | ||||||||||
| N = 741 (n = 344, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 1145 (n = 524, unadjusted) | 84 (12.73) | 108 (20.61) | 87 (11.89) | 112 (18.04) | 0.026 (–0.014 to 0.076) | 0.227 | –0.004 (–0.040 to 0.041) | 0.837 | 0.020 (–0.019 to 0.069) | 0.336 |
| N = 1094 (n = 505, partially adjusted) | ||||||||||
| N = 772 (n = 359, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 1145 (n = 524, unadjusted) | 145 (21.97) | 176 (33.59) | 150 (20.49) | 187 (30.11) | 0.035 (–0.017 to 0.096) | 0.201 | 0.002 (–0.053 to 0.069) | 0.948 | 0.004 (–0.047 to 0.065) | 0.892 |
| N = 1094 (n = 505, partially adjusted) | ||||||||||
| N = 772 (n = 359, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 1015 (n = 453, unadjusted) | 336 (59.79) | 253 (55.85) | 405 (64.80) | 317 (56.41) | –0.006 (–0.079 to 0.079) | 0.891 | 0.012 (–0.068 to 0.103) | 0.789 | 0.002 (–0.074 to 0.091) | 0.954 |
| N = 895 (n = 401, partially adjusted) | ||||||||||
| N = 729 (n = 331, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 700 (n = 307, unadjusted) | 228 (46.44) | 70 (22.80) | 276 (49.55) | 120 (30.53) | –0.077 (–0.149 to 0.026) | 0.127 | –0.068 (–0.147 to 0.048) | 0.215 | –0.067 (–0.146 to 0.049) | 0.219 |
| N = 575 (n = 254, partially adjusted) | ||||||||||
| N = 524 (n = 239, fully adjusted) | ||||||||||
| Outcome | Unadjusted ICC | ICC adjusted for treatment arm | Partially adjusted ICCa | Fully adjusted ICCb |
|---|---|---|---|---|
| Continuous outcomes | ||||
| BMI-z | 0.0051 (0.0001 to 0.1774) | 0.0025 (0.0000 to 0.7649) | 0.0331 (0.0126 to 0.0838) | 0.0219 (0.0048 to 0.0933) |
| Height (cm) | 0.0066 (0.0004 to 0.0971) | 0.0066 (0.0004 to 0.0972) | 0.1591 (0.1020 to 0.2396) | 0.1260 (0.0752 to 0.2034) |
| Waist z-score | 0.0360 (0.0144 to 0.0871) | 0.0258 (0.0081 to 0.0793) | 0.0648 (0.0322 to 0.1262) | 0.0557 (0.0248 to 0.1205) |
| Sum of four skinfolds (mm) | 0.0393 (0.0148 to 0.0998) | 0.0369 (0.0135 to 0.0970) | 0.0436 (0.0151 to 0.1193) | 0.0469 (0.0155 to 0.1334) |
| Body fat % | 0.0131 (0.0024 to 0.0678) | 0.0086 (0.0008 to 0.0864) | 0.0468 (0.0207 to 0.1020) | 0.0476 (0.0192 to 0.1133) |
| Energy intake (kJ in 24 hours) | 0.0499 (0.0238 to 0.1019) | 0.0480 (0.0225 to 0.0995) | 0.0521 (0.0243 to 0.1081) | 0.0380 (0.0145 to 0.0959) |
| PA energy expenditure (kJ/kg/day) | 0.0570 (0.0225 to 0.1369) | 0.0565 (0.0222 to 0.1364) | 0.0753 (0.0329 to 0.1634) | 0.0527 (0.0173 to 0.1495) |
| PedsQL total score | 0.0717 (0.0387 to 0.1292) | 0.0712 (0.0384 to 0.1281) | 0.0674 (0.0355 to 0.1240) | 0.0458 (0.0186 to 0.1084) |
| CHU9D utility score | 0.0459 (0.0215 to 0.0954) | 0.0450 (0.0208 to 0.0947) | 0.0540 (0.0259 to 0.1092) | 0.0526 (0.0226 to 0.1174) |
| Binary outcomes | ||||
| Obesec | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0033 (0.0000 to 0.6713) | 0.0000 (0.0000 to 0.0000) |
| Obese/overweightc | 0.0007 (0.0000 to 1.0000) | 0.0000 (0.0000 to 0.0000) | 0.0321 (0.0121 to 0.0822) | 0.0143 (0.0020 to 0.0967) |
| Five or more portions of fruit and vegetablesd | 0.0442 (0.0180 to 0.1043) | 0.0443 (0.0181 to 0.1044) | 0.0491 (0.0201 to 0.1150) | 0.0173 (0.0027 to 0.1039) |
| Achieving ≥ 60 minutes of PAe | 0.0870 (0.0427 to 0.1692) | 0.0793 (0.0372 to 0.1611) | 0.0872 (0.0406 to 0.1776) | 0.0797 (0.0343 to 0.1742) |
| Follow-up outcome variable: N = total participants (n = number of in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU3 | Baseline | FU3 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value |
| BMI-z | ||||||||||
| N = 488 (n = 242, unadjusted) | 0.29 (1.24) | 0.49 (1.37) | 0.28 (1.12) | 0.63 (1.22) | –0.143 (–0.352 to 0.067) | 0.182 | –0.204 (–0.396 to –0.013) | 0.037 | –0.177 (–0.336 to –0.017) | 0.030 |
| N = 467 (n = 232, partially adjusted) | ||||||||||
| N = 345 (n = 173, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 489 (n = 242, unadjusted) | 118.95 (5.74) | 138.70 (6.84) | 118.75 (5.60) | 138.89 (6.69) | –0.188 (–1.368 to 0.993) | 0.755 | –0.035 (–0.781 to 0.711) | 0.927 | –0.003 (–0.735 to 0.729) | 0.993 |
| N = 468 (n = 232, partially adjusted) | ||||||||||
| N = 346 (n = 173, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 471 (n = 234, unadjusted) | 0.86 (1.17) | 1.07 (1.30) | 0.92 (1.14) | 1.17 (1.28) | –0.134 (–0.459 to 0.190) | 0.418 | –0.114 (–0.423 to 0.194) | 0.467 | –0.089 (–0.365 to 0.188) | 0.529 |
| N = 439 (n = 211, partially adjusted) | ||||||||||
| N = 331 (n = 160, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 404 (n = 199, unadjusted) | 29.02 (24.48–35.65) | 37.70 (26.60–52.20) | 30.55 (24.45 – 40.10) | 36.10 (26.40–55.75) | –0.479 (–4.205 to 3.247) | 0.801 | 0.398 (–0.771 to 1.567) | 0.504 | 0.657 (–1.066 to 2.381) | 0.455 |
| N = 330 (n = 166, partially adjusted) | ||||||||||
| N = 250 (n = 123, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 487 (n = 241, unadjusted) | 21.33 (5.19) | 22.51 (8.15) | 21.18 (5.21) | 22.60 (8.03) | –0.106 (–1.752 to 1.540) | 0.900 | –0.765 (–2.004 to 0.474) | 0.226 | –0.876 (–2.146 to 0.393) | 0.176 |
| N = 463 (n = 230, partially adjusted) | ||||||||||
| N = 344 (n = 172, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 466 (n = 224, unadjusted) | 6907 (5858–7964) | 8100 (6902–9626) | 7071 (5948–8038) | 7993 (6887–9260) | 89.663 (–444.253 to 623.578) | 0.742 | 135.524 (–326.225 to 597.273) | 0.565 | 16.932 (–415.049 to 448.914) | 0.939 |
| N = 395 (n = 197, partially adjusted) | ||||||||||
| N = 330 (n = 161, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 486 (n = 240, unadjusted) | 72.83 (63.04–84.78) | 82.61 (73.91–91.30) | 73.91 (63.04–82.61) | 82.61 (73.91–91.30) | 0.180 (–2.930 to 3.291) | 0.910 | –0.073 (–3.628 to 3.481) | 0.968 | 0.123 (–3.272 to 3.519) | 0.943 |
| N = 463 (n = 230, partially adjusted) | ||||||||||
| N = 344 (n = 172, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 486 (n = 241, unadjusted) | 0.84 (0.13) | 0.91 (0.09) | 0.82 (0.14) | 0.90 (0.09) | 0.012 (–0.004 to 0.029) | 0.151 | 0.008 (–0.010 to 0.026) | 0.389 | 0.013 (–0.007 to 0.034) | 0.207 |
| N = 453 (n = 223, partially adjusted) | ||||||||||
| N = 333 (n = 164, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 488 (n = 242, unadjusted) | 39 (13.36) | 55 (22.73) | 43 (13.15) | 54 (21.95) | 0.008 (–0.043 to 0.073) | 0.788 | –0.031 (–0.079 to 0.033) | 0.306 | –0.024 (–0.075 to 0.044) | 0.449 |
| N = 467 (n = 232, partially adjusted) | ||||||||||
| N = 345 (n = 173, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 488 (n = 242, unadjusted) | 67 (22.95) | 87 (35.95) | 67 (20.49) | 89 (36.18) | –0.002 (–0.078 to 0.093) | 0.958 | –0.026 (–0.097 to 0.065) | 0.543 | –0.028 (–0.091 to 0.051) | 0.460 |
| N = 467 (n = 232, partially adjusted) | ||||||||||
| N = 345 (n = 173, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 466 (n = 224, unadjusted) | 160 (60.61) | 135 (60.27) | 207 (72.13) | 138 (57.02) | 0.032 (–0.084 to 0.177) | 0.614 | 0.013 (–0.107 to 0.164) | 0.845 | –0.007 (–0.103 to 0.110) | 0.901 |
| N = 395 (n = 197, partially adjusted) | ||||||||||
| N = 330 (n = 161, fully adjusted) | ||||||||||
| Outcome | Unadjusted ICC | ICC adjusted for treatment arm | Partially adjusted ICCa | Fully adjusted ICCb |
|---|---|---|---|---|
| Continuous outcomes | ||||
| BMI-z | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0423 (0.0112 to 0.1475) | 0.0025 (0.0000 to 0.9999) |
| Height (cm) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0839 (0.0376 to 0.1770) | 0.0701 (0.0253 to 0.1797) |
| Waist z-score | 0.0363 (0.0088 to 0.1371) | 0.0355 (0.0087 to 0.1338) | 0.1314 (0.0637 to 0.2516) | 0.0943 (0.0375 to 0.2178) |
| Sum of four skinfolds (mm) | 0.0200 (0.0023 to 0.1520) | 0.0201 (0.0023 to 0.1533) | 0.0945 (0.0326 to 0.2442) | 0.1097 (0.0386 to 0.2745) |
| Body fat % | 0.0143 (0.0013 to 0.1422) | 0.0143 (0.0013 to 0.1422) | 0.0502 (0.0161 to 0.1457) | 0.0477 (0.0127 to 0.1633) |
| Energy intake (kJ in 24 hours) | 0.0541 (0.0186 to 0.1471) | 0.0542 (0.0188 to 0.1465) | 0.0483 (0.0142 to 0.1517) | 0.0156 (0.0009 to 0.2139) |
| PedsQL total score | 0.0408 (0.0107 to 0.1434) | 0.0411 (0.0108 to 0.1437) | 0.0314 (0.0058 to 0.1519) | 0.0179 (0.0011 to 0.2281) |
| CHU9D utility score | 0.0048 (0.0000 to 0.7046) | 0.0020 (0.0000 to 0.9995) | 0.0102 (0.0003 to 0.2426) | 0.0043 (0.0000 to 0.9778) |
| Binary outcomes | ||||
| Obesec | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0123 (0.0005 to 0.2214) | 0.0000 (0.0000 to 0.0000) |
| Obese/overweightc | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0204 (0.0023 to 0.1575) | 0.0102 (0.0002 to 0.3697) |
| Five or more portions of fruit and vegetablesd | 0.0593 (0.0193 to 0.1678) | 0.0581 (0.0189 to 0.1649) | 0.0541 (0.0160 to 0.1669) | 0.0000 (0.0000 to 0.0000) |
Primary outcomes
Body mass index z-score (at follow-ups 1 and 2)
At FU1, in the partially adjusted primary analysis, the mean BMI-z was lower in the intervention arm than in the control arm, with a MD of –0.075. However, this was not statistically significant (95% CI –0.183 to 0.033; p = 0.175). This estimate was robust to covariate adjustment, as the fully adjusted estimate (MD –0.077, 95% CI –0.191 to 0.037; p = 0.186) does not differ much from that of the partially adjusted model.
At FU2, the difference in mean BMI-z between the trial arms is smaller, but remains lower in the intervention arm than in the control arm, with a MD of –0.027. However, this difference is also not statistically significant (95% CI –0.137 to 0.083). There is a slight increase in the MD (MD –0.042) after covariate adjustment but the outcome remains insignificant.
Secondary outcomes
Body mass index z-score (at follow-up 3)
At FU3, both the partially and the fully adjusted models show a statistically significant (and similar) difference in mean BMI-z between arms. The same direction of effect as at previous follow-ups was observed, with a lower mean BMI-z in the intervention arm than in the control arm, and a MD of –0.204 (95% CI –0.396 to –0.013; p = 0.037) and –0.177 (95% CI –0.336 to –0.017; p = 0.030) in the partially and fully adjusted models, respectively.
Waist z-score
At FU1 and FU2, the mean waist z-score was slightly higher in the intervention arm than in the control arm (MD of 0.103 and 0.026, respectively), whereas at FU3 it was slightly lower (MD –0.114). However, observed differences were not significant in either of the adjusted models at any time point.
Sum of four skinfolds
At FU1, FU2 and FU3, the sum of skinfolds was slightly higher in the intervention arm than in the control arm (MD 0.366, 0.644 and 0.398, respectively). These differences were not statistically significant in any model at any time point.
Body fat percentage
At FU1 and FU2, body fat percentage was very slightly higher in the intervention arm participants than in the control arm participants (MD 0.040 and 0.344, respectively), but lower at FU3 (MD –0.765). None of these differences was statistically significant.
Energy intake
The median number of kilojoules of energy consumed over the 24-hour period assessed, in participants in the intervention arm compared with those in the control arm, was a little higher at FU1 and FU3 (MD of 61.5 kJ and 135.5 kJ, respectively), but slightly lower at FU2 (MD –139.6 kJ). The differences observed, however, were not statistically significant in either the partially (values reported here) or the fully adjusted models.
Physical activity energy expenditure
This was measured in only the first two follow-up periods and the differences observed were extremely small [MD (intervention vs. control) –0.866 kJ/kg/day and 0.001 kJ/kg/day at FU1 and FU2, respectively] and not significant.
Quality of life (Paediatric Quality of Life Inventory total score and Child Health Utility 9D utility score)
In both the partially (values presented) and the fully adjusted models, only very minor and non-significant differences in overall quality of life were observed between intervention and control arm participants at all time points. Using the PedsQL total score, MDs of –0.630, 1.248 and –0.073 were observed at FU1, FU2 and FU3, respectively, with the equivalent values of 0.010, –0.006 and 0.008 for the CHU9D utility score.
Proportion obese
At FU1, 16.2% of those in the intervention arm and 14.8% of those in the control arm were classified as obese. The partially adjusted RD of –0.036 (95% CI –0.066 to 0.004; p = 0.074) indicates that the risk of being obese at FU1 after adjusting for baseline BMI-z is 3.6% lower in the intervention arm than in the control arm. Although the difference in risk approaches significance in the partially adjusted model, after the additional covariate adjustment the association becomes weaker (RD –0.007, 95% CI –0.050 to 0.064; p = 0.676).
At FU2, the proportion of those classified as obese increases in both arms but remains higher in the intervention arm (20.61%) than in the control arm (18.04%). After adjustment for baseline BMI-z, there is a very small negative difference in risk between the intervention and control arms (RD –0.004), but this is not significant (p = 0.837), and in the fully adjusted model the effect is reversed (RD 0.020) and is, again, not significant (p = 0.336).
Further increases in the proportion who were obese are observed at FU3 but the difference between the arms is lower than at the previous follow-ups (intervention, 22.73% obese; control, 21.95% obese). The RD in both the partially (RD –0.031) and the fully adjusted (RD –0.024) models show a reduced risk of obesity in the intervention arm compared with the control arm, but the observed differences in risk are not statistically significant (p = 0.306 and p = 0.449, respectively).
Proportion obese/overweight
A similar pattern was seen for the percentage of participants who were classified as being overweight (including obese). This proportion increased over time in both the intervention and control groups [baseline to FU3: intervention arm, 21.97%, 28.75%, 33.59% and 35.95%; and control arm, 20.49%, 24.74%, 30.11% and 36.18%)]. The proportions overweight/obese were higher in the intervention arm than inthe control arm at baseline, and FU1 and FU2, and although the proportions were more similar between arms at FU3, in contrast with the previous time points, the proportion was slightly higher in the control arm. After adjusting for baseline BMI-z, at FU1 and FU3 the risk of being overweight was lower in the intervention arm than in the control arm (RD –0.013 and –0.026, respectively). The estimate was robust to covariate adjustment at third follow-up (RD –0.028), but not at first follow-up (RD 0.000). At second follow-up there was very little difference in the risk of being at least overweight between the arms (RD 0.002). None of these observed differences was statistically significant.
Proportion meeting government recommendation for fruit and vegetable consumption
The proportion of children eating at least five portions of fruit and vegetables at FU1 was 48.13% in the intervention arm and 49.09% in the control arm. After adjustment for baseline grams of fruit and vegetable consumption, the RD of the intervention arm compared with the control arm showed that participants in the intervention arm were 1.4% less likely than those in the control arm to meet the government fruit and vegetable consumption recommendation. However, the difference between arms was not significant (p = 0.753). The fully adjusted model showed a small difference in the opposite direction (RD 0.004), but again this was not statistically significant (p = 0.900).
At FU2, compared with at FU1, a greater proportion of children met the government fruit and vegetable consumption recommendation in both arms, with the proportion remaining slightly lower in the intervention arm (55.85%) than in the control arm (56.41%). There were small positive RDs between intervention and control arms in both the partially (RD 0.01) and the fully (RD 0.002) adjusted models, but neither difference was statistically significant (p = 0.789 and p = 0.954, respectively).
The proportion of children eating at least five portions of fruit and vegetables increased again between FU2 and FU3, but the increase was greater in the intervention arm such that, in contrast with the previous time points, the proportion was greater in the intervention arm (60.27%) than in the control (57.02%) arm. The RD in the partially adjusted model showed that participants in the intervention arm were 1.3% more likely than those in the control arm to meet the government recommendation, but the difference was not statistically significant (p = 0.845). The RD was small but reversed after covariate adjustment (–0.007) and was also not significant (p = 0.901).
Proportion meeting government recommendation for physical activity in children
The proportion of children doing at least 60 minutes of at least moderate PA per day increased between baseline and FU1 in the intervention arm by 5.8%, whereas there was no real change in the control arm (difference = 0.24%). There was, however, a big reduction in both arms between FU1 and FU2, with the change being greater in the intervention arm than in the control arm (intervention, 52.27% to 22.8%; control, 49.79% to 30.53%). After adjustment for baseline minutes of at least moderate PA, the RD at FU1 (RD 0.041) shows that, compared with those in the control arm, participants in the intervention arm were 4.1% more likely to achieve the minimum 60-minute PA government target. The RD at second follow-up (RD –0.068) suggests that this is reversed at that time point, with participants in the intervention arm being 6.8% less likely than those in the control arm to meet the recommendation. None of the observed differences was statistically significant. PA data were not collected at third follow-up.
Additional anthropometric, diet, physical activity and psychological outcomes
The results for the prespecified additional anthropometric, diet, PA and psychological variables are presented for both continuous and binary outcomes at first follow-up in Table 22 (corresponding ICCs are reported in Table 23) and at second follow-up in Table 24 (corresponding ICCs are reported in Table 25). Although a few significant differences between the intervention and control arms were observed for the additional outcomes, there was no consistent message and, apart from one outcome (subscapular skinfold at FU2), the differences observed were not significant in either the partially or the fully adjusted model. Significant differences, however, are reported below.
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (99% CI) | p-value | MD (99% CI) | p-value | MD (99% CI) | p-value | ||
| Subscapular skinfold (mm)d | ||||||||||
| N = 1097 (n = 509, unadjusted) | 5.98 (5.05–7.30) | 6.55 (5.20–9.00) | 5.80 (4.95–7.20) | 6.20 (5.15–8.40) | 0.188 (–0.243 to 0.619) | 0.260 | 0.005 (–0.167 to 0.177) | 0.940 | 0.006 (–0.184 to 0.196) | 0.935 |
| N = 973 (n = 453, partially adjusted) | ||||||||||
| N = 733 (n = 346, fully adjusted) | ||||||||||
| Suprailiac (mm)d | ||||||||||
| N = 1100 (n = 511, unadjusted) | 6.50 (4.75–9.45) | 6.75 (4.80–11.80) | 6.10 (4.55–9.30) | 6.10 (4.50–10.40) | 0.413 (–0.215 to 1.042) | 0.090 | 0.178 (–0.136 to 0.493) | 0.144 | 0.226 (–0.189 to 0.642) | 0.161 |
| N = 977 (n = 460, partially adjusted) | ||||||||||
| N = 745 (n = 356, fully adjusted) | ||||||||||
| Biceps (mm)e | ||||||||||
| N = 1118 (n = 520, unadjusted) | 6.15 (4.80–7.80) | 6.88 (5.30–9.85) | 6.15 (4.70–8.40) | 6.60 (5.00–9.25) | 0.340 (–0.313 to 0.992) | 0.180 | 0.181 (–0.093 to 0.456) | 0.089 | 0.153 (–0.175 to 0.480) | 0.230 |
| N = 1018 (n = 480, partially adjusted) | ||||||||||
| N = 772 (n = 369, fully adjusted) | ||||||||||
| Triceps skinfold (mm)e | ||||||||||
| N = 1122 (n = 517, unadjusted) | 9.80 (7.90–12.30) | 11.30 (8.35–15.05) | 10.00 (7.95–12.60) | 10.60 (8.50–14.70) | 0.320 (–0.420 to 1.060) | 0.265 | 0.073 (–0.211 to 0.357) | 0.508 | 0.061 (–0.252 to 0.374) | 0.617 |
| N = 1018 (n = 474, partially adjusted) | ||||||||||
| N = 772 (n = 365, fully adjusted) | ||||||||||
| Thigh skinfold (mm)f | ||||||||||
| N = 1045 (n = 486, unadjusted) | 13.43 (11.10–16.75) | 15.90 (12.00–20.70) | 13.30 (10.90–17.20) | 15.05 (11.80–20.40) | 0.357 (–0.768 to 1.482) | 0.414 | –0.038 (–0.468 to 0.391) | 0.819 | –0.124 (–0.630 to 0.382) | 0.527 |
| N = 826 (n = 391, partially adjusted) | ||||||||||
| N = 640 (n = 304, fully adjusted) | ||||||||||
| Bioimpedance (Ω) | ||||||||||
| N = 1229 (n = 569, unadjusted) | 656.13 (81.30) | 660.28 (87.46) | 654.00 (82.33) | 655.07 (86.82) | 5.030 (–15.061 to 25.120) | 0.519 | 6.884 (–5.419 to 19.187) | 0.150 | 6.679 (–4.804 to 18.163) | 0.134 |
| N = 1160 (n = 546, partially adjusted) | ||||||||||
| N = 815 (n = 385, fully adjusted) | ||||||||||
| Sedentary time (hours/24 hours) | ||||||||||
| N = 866 (n = 396, unadjusted) | 14.42 (1.88) | 14.01 (2.12) | 14.57 (1.78) | 14.08 (2.20) | 0.016 (–0.511 to 0.543) | 0.938 | –0.045 (–0.610 to 0.521) | 0.839 | 0.156 (–0.384 to 0.697) | 0.456 |
| N = 720 (n = 334, partially adjusted) | ||||||||||
| N = 654 (n = 310, fully adjusted) | ||||||||||
| MVPA time (minutes/24 hours)f | ||||||||||
| N = 866 (n = 396, unadjusted) | 57.91 (42.52–85.90) | 62.07 (38.80–102.97) | 59.47 (42.80–81.53) | 59.80 (40.91–96.95) | –2.092 (–13.957 to 9.774) | 0.650 | –1.310 (–11.843 to 9.224) | 0.749 | –3.939 (–16.561 to 8.682) | 0.421 |
| N = 720 (n = 334, partially adjusted) | ||||||||||
| N = 654 (n = 310, fully adjusted) | ||||||||||
| Systolic blood pressure (mmHg) | ||||||||||
| N = 1197 (n = 552, unadjusted) | 95.67 (9.04) | 95.35 (8.78) | 98.10 (10.06) | 95.29 (8.22) | 0.003 (–1.980 to 1.986) | 0.997 | 0.624 (–1.725 to 2.973) | 0.494 | 0.931 (–1.307 to 3.169) | 0.284 |
| N = 1100 (n = 513, partially adjusted) | ||||||||||
| N = 778 (n = 369, fully adjusted) | ||||||||||
| Diastolic blood pressure (mmHg) | ||||||||||
| N = 1197 (n = 552, unadjusted) | 62.18 (7.99) | 62.08 (7.81) | 64.21 (8.59) | 62.19 (7.43) | –0.158 (–1.905 to 1.589) | 0.816 | 0.335 (–1.721 to 2.392) | 0.675 | 0.945 (–1.247 to 3.137) | 0.267 |
| N = 1100 (n = 513, partially adjusted) | ||||||||||
| N = 778 (n = 369, fully adjusted) | ||||||||||
| Fat intake (grams in 24 hours)d | ||||||||||
| N = 1112 (n = 507, unadjusted) | 56.08 (45.39–69.28) | 60.95 (47.32–71.98) | 54.74 (44.75–67.58) | 57.36 (46.87–70.15) | 2.157 (–2.233 to 6.546) | 0.206 | 1.426 (–2.291 to 5.143) | 0.323 | 1.260 (–2.336 to 4.857) | 0.367 |
| N = 978 (n = 449, partially adjusted) | ||||||||||
| N = 803 (n = 369, fully adjusted) | ||||||||||
| Free sugars in 24 hours intake (grams in 24 hours) | ||||||||||
| N = 1112 (n = 507, unadjusted) | 76.63 (31.01) | 72.05 (33.03) | 76.13 (30.88) | 75.31 (32.88) | –3.242 (–13.239 to 6.755) | 0.404 | –4.329 (–12.781 to 4.124) | 0.187 | –5.636 (–12.285 to 1.014) | 0.029 |
| N = 978 (n = 449, partially adjusted) | ||||||||||
| N = 803 (n = 369, fully adjusted) | ||||||||||
| Fibre intake (grams in 24 hours)f | ||||||||||
| N = 1112 (n = 507, unadjusted) | 11.00 (8.80–13.68) | 11.76 (9.41–14.62) | 11.35 (8.99–13.95) | 11.77 (9.18–14.46) | –0.010 (–0.954 to 0.934) | 0.977 | 0.013 (–0.767 to 0.793) | 0.965 | 0.008 (–0.914 to 0.930) | 0.982 |
| N = 978 (n = 449, partially adjusted) | ||||||||||
| N = 803 (n = 369, fully adjusted) | ||||||||||
| Fruit and vegetables intake (grams in 24 hours)g | ||||||||||
| N = 1112 (n = 507, unadjusted) | 226.92 (132.00–330.09) | 200.23 (91.79–315.28) | 247.58 (157.25–341.40) | 201.84 (116.16–316.56) | –5.387 (–44.140 to 33.367) | 0.720 | –2.875 (–33.148 to 27.399) | 0.807 | –5.652 (–41.150 to 29.847) | 0.682 |
| N = 978 (n = 449, partially adjusted) | ||||||||||
| N = 803 (n = 369, fully adjusted) | ||||||||||
| PedsQL physical functioning score | ||||||||||
| N = 1231 (n = 554, unadjusted) | 73.06 (18.07) | 77.79 (16.28) | 74.87 (17.26) | 78.86 (15.14) | –1.020 (–4.367 to 2.327) | 0.433 | –0.649 (–4.006 to 2.708) | 0.618 | –0.191 (–3.498 to 3.116) | 0.882 |
| N = 1171 (n = 538, partially adjusted) | ||||||||||
| N = 817 (n = 375, fully adjusted) | ||||||||||
| PedsQL psychosocial functioning score | ||||||||||
| N = 1230 (n = 554, unadjusted) | 69.47 (17.95) | 71.27 (16.58) | 69.28 (18.19) | 72.10 (15.81) | –0.797 (–4.033 to 2.440) | 0.526 | –0.661 (–3.798 to 2.475) | 0.587 | –0.679 (–3.352 to 1.993) | 0.513 |
| N = 1170 (n = 538, partially adjusted) | ||||||||||
| N = 817 (n = 375, fully adjusted) | ||||||||||
| PedsQL emotional functioning score | ||||||||||
| N = 1231 (n = 554, unadjusted) | 73.36 (22.20) | 75.88 (21.02) | 71.68 (23.05) | 75.75 (20.67) | –0.068 (–4.223 to 4.087) | 0.966 | –0.045 (–4.236 to 4.147) | 0.978 | 0.115 (–3.954 to 4.184) | 0.942 |
| N = 1171 (n = 538, partially adjusted) | ||||||||||
| N = 817 (n = 375, fully adjusted) | ||||||||||
| PedsQL social functioning score | ||||||||||
| N = 1230 (n = 554, unadjusted) | 67.72 (22.34) | 70.89 (20.52) | 68.60 (21.71) | 72.39 (19.39) | –1.397 (–4.903 to 2.109) | 0.305 | –1.134 (–4.634 to 2.366) | 0.404 | –1.137 (–4.193 to 1.918) | 0.338 |
| N = 1169 (n = 537, partially adjusted) | ||||||||||
| N = 816 (n = 374, fully adjusted) | ||||||||||
| PedsQL school functioning score | ||||||||||
| N = 1229 (n = 554, unadjusted) | 67.35 (21.72) | 67.04 (20.03) | 67.54 (21.56) | 68.07 (18.72) | –0.847 (–4.730 to 3.036) | 0.574 | –0.810 (–4.533 to 2.912) | 0.575 | –0.876 (–4.331 to 2.579) | 0.514 |
| N = 1167 (n = 538, partially adjusted) | ||||||||||
| N = 814 (n = 375, fully adjusted) | ||||||||||
| KIDSCREEN-52 bullying score | ||||||||||
| N = 1227 (n = 552, unadjusted) | 11.74 (3.20) | 13.21 (6.95) | 12.05 (2.97) | 14.22 (10.14) | –1.006 (–2.431 to 0.420) | 0.069 | –1.101 (–2.655 to 0.453) | 0.068 | –0.544 (–1.930 to 0.842) | 0.312 |
| N = 1156 (n = 533, partially adjusted) | ||||||||||
| N = 806 (n = 370, fully adjusted) | ||||||||||
| Body image satisfaction score | ||||||||||
| N = 1218 (n = 550, unadjusted) | 1.54 (1.39) | 1.37 (1.17) | 1.56 (1.40) | 1.27 (1.11) | 0.080 (–0.136 to 0.296) | 0.341 | 0.041 (–0.168 to 0.251) | 0.611 | 0.015 (–0.168 to 0.216) | 0.847 |
| N = 1149 (n = 533, partially adjusted) | ||||||||||
| N = 805 (n = 372, fully adjusted) | ||||||||||
| Outcome | Unadjusted ICC | ICC adjusted for treatment arm | Partially adjusted ICCa | Fully adjusted ICCb |
|---|---|---|---|---|
| Suprascapular skinfold (mm) | 0.0051 (0.0001 to 0.1860) | 0.0041 (0.0000 to 0.2871) | 0.0716 (0.0389 to 0.1282) | 0.0747 (0.0400 to 0.1351) |
| Suprailiac skinfold (mm) | 0.0258 (0.0094 to 0.0692) | 0.0246 (0.0087 to 0.0676) | 0.2433 (0.1655 to 0.3427) | 0.2260 (0.1500 to 0.3257) |
| Biceps skinfold (mm) | 0.0444 (0.0209 to 0.0920) | 0.0427 (0.0198 to 0.0898) | 0.1416 (0.0861 to 0.2242) | 0.1313 (0.0777 to 0.2133) |
| Triceps skinfold (mm) | 0.0166 (0.0042 to 0.0636) | 0.0150 (0.0034 to 0.0637) | 0.1720 (0.1113 to 0.2562) | 0.1441 (0.0897 to 0.2234) |
| Thigh skinfold (mm) | 0.0131 (0.0025 to 0.0651) | 0.0126 (0.0023 to 0.0654) | 0.1047 (0.0590 to 0.1789) | 0.0985 (0.0535 to 0.1745) |
| Bioimpedance (Ω) | 0.0623 (0.0342 to 0.1108) | 0.0616 (0.0337 to 0.1099) | 0.0510 (0.0253 to 0.1002) | 0.0241 (0.0070 to 0.0795) |
| Sedentary time (hours/24 hours) | 0.0551 (0.0259 to 0.1134) | 0.0552 (0.0259 to 0.1135) | 0.0634 (0.0292 to 0.1321) | 0.0554 (0.0229 to 0.1281) |
| MVPA time (minutes/24 hours) | 0.0799 (0.0422 to 0.1463) | 0.0800 (0.0422 to 0.1464) | 0.0954 (0.0501 to 0.1742) | 0.0688 (0.0308 to 0.1466) |
| Systolic blood pressure (mmHg) | 0.0608 (0.0315 to 0.1141) | 0.0608 (0.0315 to 0.1142) | 0.1130 (0.0671 to 0.1839) | 0.0979 (0.0546 to 0.1695) |
| Diastolic blood pressure (mmHg) | 0.0570 (0.0290 to 0.1091) | 0.0570 (0.0289 to 0.1090) | 0.1064 (0.0627 to 0.1750) | 0.1049 (0.0595 to 0.1784) |
| Fat intake (grams in 24 hours) | 0.0436 (0.0206 to 0.0900) | 0.0422 (0.0198 to 0.0878) | 0.0317 (0.0120 to 0.0812) | 0.0269 (0.0092 to 0.0764) |
| Free sugars in 24 hours intake (grams in 24 hours) | 0.1421 (0.0903 to 0.2167) | 0.1400 (0.0886 to 0.2141) | 0.0954 (0.0539 to 0.1634) | 0.0556 (0.0259 to 0.1154) |
| Fibre intake (grams in 24 hours) | 0.0530 (0.0268 to 0.1021) | 0.0530 (0.0268 to 0.1021) | 0.0452 (0.0202 to 0.0977) | 0.0338 (0.0130 to 0.0852) |
| Fruit and vegetables intake (grams in 24 hours) | 0.0395 (0.0172 to 0.0879) | 0.0392 (0.0170 to 0.0876) | 0.0420 (0.0179 to 0.0956) | 0.0136 (0.0020 to 0.0870) |
| PedsQL physical functioning score | 0.0450 (0.0217 to 0.0910) | 0.0438 (0.0209 to 0.0896) | 0.0459 (0.0217 to 0.0945) | 0.0356 (0.0135 to 0.0908) |
| PedsQL psychosocial functioning score | 0.0327 (0.0140 to 0.0744) | 0.0321 (0.0137 to 0.0738) | 0.0292 (0.0117 to 0.0709) | 0.0018 (0.0000 to 0.9956) |
| PedsQL emotional functioning score | 0.0295 (0.0116 to 0.0732) | 0.0296 (0.0116 to 0.0732) | 0.0317 (0.0127 to 0.0770) | 0.0062 (0.0001 to 0.2537) |
| PedsQL social functioning score | 0.0158 (0.0041 to 0.0589) | 0.0142 (0.0033 to 0.0592) | 0.0144 (0.0032 to 0.0614) | 0.0000 (0.0000 to 0.0000) |
| PedsQL school functioning score | 0.0368 (0.0165 to 0.0801) | 0.0361 (0.0160 to 0.0794) | 0.0293 (0.0117 to 0.0715) | 0.0077 (0.0005 to 0.1145) |
| KIDSCREEN-52 bullying | 0.0143 (0.0031 to 0.0646) | 0.0111 (0.0017 to 0.0680) | 0.0107 (0.0015 to 0.0738) | 0.0000 (0.0000 to 0.0000) |
| Body image satisfaction score | 0.0256 (0.0090 to 0.0702) | 0.0232 (0.0075 to 0.0696) | 0.0176 (0.0043 to 0.0689) | 0.0000 (0.0000 to 0.0000) |
| Follow-up outcome variable: N = total participants (n =number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (99% CI) | p-value | MD (99% CI) | p-value | MD (99% CI) | p-value | ||
| Subscapular skinfold (mm)d | ||||||||||
| N = 913 (n = 405, unadjusted) | 5.97 (5.05–7.30) | 6.90 (5.40–11.10) | 5.80 (4.95–7.20) | 6.38 (5.05–9.72) | 0.502 (–0.184 to 1.188) | 0.059 | 0.198 (–0.028 to 0.423) | 0.024 | 0.199 (–0.016 to 0.414) | 0.017 |
| N = 811 (n = 362, partially adjusted) | ||||||||||
| N = 620 (n = 285, fully adjusted) | ||||||||||
| Suprailiac (mm)d | ||||||||||
| N = 931 (n = 413, unadjusted) | 6.50 (4.75–9.45) | 7.90 (5.05–13.55) | 6.10 (4.55–9.30) | 7.13 (4.60–13.35) | 0.441 (–0.306 to 1.189) | 0.128 | 0.241 (–0.088 to 0.571) | 0.059 | 0.161 (–0.200 to 0.523) | 0.251 |
| N = 824 (n = 373, partially adjusted) | ||||||||||
| N = 639 (n = 293, fully adjusted) | ||||||||||
| Biceps (mm)e | ||||||||||
| N = 980 (n = 435, unadjusted) | 6.15 (4.80–7.80) | 7.50 (5.40–11.05) | 6.15 (4.70–8.40) | 7.30 (5.15–10.90) | 0.278 (–0.713 to 1.268) | 0.470 | 0.198 (–0.178 to 0.575) | 0.175 | 0.166 (–0.189 to 0.521) | 0.229 |
| N = 887 (n = 400, partially adjusted) | ||||||||||
| N = 681 (n = 312, fully adjusted) | ||||||||||
| Triceps skinfold (mm)e | ||||||||||
| N = 980 (n = 436, unadjusted) | 9.80 (7.90–12.30) | 12.80 (9.10–16.90) | 10.00 (7.95–12.60) | 11.90 (9.00–16.95) | 0.318 (–0.787 to 1.423) | 0.459 | 0.087 (–0.231 to 0.405) | 0.483 | 0.088 (–0.237 to 0.414) | 0.484 |
| N = 881 (n = 394, partially adjusted) | ||||||||||
| N = 672 (n = 306, fully adjusted) | ||||||||||
| Thigh skinfold (mm)f | ||||||||||
| N = 789 (n = 354, unadjusted) | 13.43 (11.10 to 16.75) | 17.60 (12.85–22.65) | 13.30 (10.90–17.20) | 16.75 (12.40–22.95) | 0.263 (–1.132 to 1.658) | 0.628 | 0.111 (–0.398 to 0.620) | 0.574 | 0.016 (–0.495 to 0.528) | 0.935 |
| N = 610 (n = 280, partially adjusted) | ||||||||||
| N = 480 (n = 222, fully adjusted) | ||||||||||
| Bioimpedance (Ω) | ||||||||||
| N = 1118 (n = 513, unadjusted) | 656.13 (81.30) | 659.80 (85.22) | 654.00 (82.33) | 655.40 (83.73) | 6.302 (–13.573 to 26.178) | 0.414 | 9.099 (–4.237 to 22.435) | 0.079 | 12.160 (0.523 to 23.797) | 0.007 |
| N = 1051 (n = 490, partially adjusted) | ||||||||||
| N = 744 (n = 348, fully adjusted) | ||||||||||
| Sedentary time (hours/24 hours) | ||||||||||
| N = 700 (n = 307, unadjusted) | 14.42 (1.88) | 15.86 (1.86) | 14.57 (1.78) | 15.73 (1.94) | 0.112 (–0.496 to 0.720) | 0.635 | 0.186 (–0.443 to 0.814) | 0.447 | 0.287 (–0.368 to 0.941) | 0.260 |
| N = 575 (n = 254, partially adjusted) | ||||||||||
| N = 524 (n = 239, fully adjusted) | ||||||||||
| MVPA time (minutes/24 hours)f | ||||||||||
| N = 866 (n = 396, unadjusted) | 57.91 (42.52–85.90) | 40.79 (31.47–57.19) | 59.47 (42.80–81.53) | 44.36 (32.85–67.94) | –4.162 (–12.856 to 4.532) | 0.218 | –3.332 (–10.706 to 4.042) | 0.245 | –4.314 (–12.697 to 4.070) | 0.185 |
| N = 720 (n = 334, partially adjusted) | ||||||||||
| N = 651 (n = 308, fully adjusted) | ||||||||||
| Systolic blood pressure (mmHg) | ||||||||||
| N = 1083 (n = 483, unadjusted) | 95.67 (9.04) | 96.98 (8.30) | 98.10 (10.06) | 97.75 (8.21) | –0.728 (–2.429 to 0.974) | 0.271 | 0.310 (–1.528 to 2.148) | 0.664 | 0.577 (–1.431 to 2.584) | 0.459 |
| N = 996 (n = 447, partially adjusted) | ||||||||||
| N = 711 (n = 325, fully adjusted) | ||||||||||
| Diastolic blood pressure (mmHg) | ||||||||||
| N = 1083 (n = 483, unadjusted) | 62.18 (7.99) | 63.29 (7.46) | 64.21 (8.59) | 63.50 (7.34) | –0.020 (–1.892 to 1.851) | 0.978 | 0.482 (–1.570 to 2.533) | 0.545 | 0.517 (–1.605 to 2.639) | 0.530 |
| N = 996 (n = 447, partially adjusted) | ||||||||||
| N = 711 (n = 325, fully adjusted) | ||||||||||
| Fat intake (grams in 24 hours)f | ||||||||||
| N = 1015 (n = 453, unadjusted) | 56.08 (45.39–69.28) | 65.66 (51.81 to 79.88) | 54.74 (44.75–67.58) | 67.41 (54.59–81.08) | –2.605 (–7.519 to 2.310) | 0.172 | –1.943 (–6.629 to 2.742) | 0.285 | –2.740 (–7.652 to 2.171) | 0.151 |
| N = 895 (n = 401, partially adjusted) | ||||||||||
| N = 729 (n = 331, fully adjusted) | ||||||||||
| Free sugars in 24 hours intake (grams in 24 hours) | ||||||||||
| N = 1015 (n = 453, unadjusted) | 76.63 (31.01) | 74.50 (32.18) | 76.13 (30.88) | 81.21 (35.16) | –7.778 (–18.815 to 3.259) | 0.069 | –7.886 (–18.488 to 2.716) | 0.055 | –9.220 (–19.032 to 0.592) | 0.015 |
| N = 895 (n = 401, partially adjusted) | ||||||||||
| N = 729 (n = 331, fully adjusted) | ||||||||||
| Fibre intake (grams in 24 hours)f | ||||||||||
| N = 1015 (n = 453, unadjusted) | 11.00 (8.80–13.68) | 12.44 (10.01–15.47) | 11.35 (8.99–13.95) | 12.77 (10.44–15.66) | –0.391 (–1.419 to 0.636) | 0.327 | –0.163 (–1.162 to 0.837) | 0.675 | –0.461 (–1.499 to 0.577) | 0.253 |
| N = 895 (n = 401, partially adjusted) | ||||||||||
| N = 729 (n = 331, fully adjusted) | ||||||||||
| Fruit and vegetables intake (grams in 24 hours)g | ||||||||||
| N = 1015 (n = 453, unadjusted) | 226.92 (132.00–330.09) | 218.06 (115.60–348.41) | 247.58 (157.25–341.40) | 219.28 (116.54–341.33) | 8.155 (–39.775 to 56.085) | 0.661 | 14.195 (–29.969 to 58.360) | 0.408 | 14.598 (–34.821 to 64.018) | 0.447 |
| N = 895 (n = 401, partially adjusted) | ||||||||||
| N = 729 (n = 331, fully adjusted) | ||||||||||
| PedsQL physical functioning score | ||||||||||
| N = 1115 (n = 493, unadjusted) | 73.06 (18.07) | 83.71 (13.86) | 74.87 (17.26) | 84.18 (12.85) | –0.089 (–3.684 to 3.507) | 0.949 | 0.118 (–3.411 to 3.646) | 0.932 | 0.704 (–2.557 to 3.965) | 0.578 |
| N = 1054 (n = 475, partially adjusted) | ||||||||||
| N = 752 (n = 344, fully adjusted) | ||||||||||
| PedsQL psychosocial functioning score | ||||||||||
| N = 1113 (n = 492, unadjusted) | 69.47 (17.95) | 77.52 (14.40) | 69.28 (18.19) | 76.27 (14.96) | 1.607 (–1.667 to 4.881) | 0.206 | 1.593 (–1.598 to 4.784) | 0.198 | 1.468 (–1.480 to 4.415) | 0.200 |
| N = 1052 (n = 474, partially adjusted) | ||||||||||
| N = 751 (n = 343, fully adjusted) | ||||||||||
| PedsQL emotional functioning score | ||||||||||
| N = 1114 (n = 493, unadjusted) | 73.36 (22.20) | 83.42 (18.11) | 71.68 (23.05) | 81.57 (18.86) | 2.151 (–1.499 to 5.802) | 0.129 | 1.972 (–1.766 to 5.710) | 0.174 | 2.021 (–1.745 to 5.787) | 0.167 |
| N = 1053 (n = 475, partially adjusted) | ||||||||||
| N = 752 (n = 344, fully adjusted) | ||||||||||
| PedsQL social functioning score | ||||||||||
| N = 1113 (n = 492, unadjusted) | 67.72 (22.34) | 76.72 (18.31) | 68.60 (21.71) | 75.81 (18.91) | 1.061 (–2.523 to 4.646) | 0.446 | 0.993 (–2.517 to 4.503) | 0.466 | 1.089 (–2.305 to 4.483) | 0.409 |
| N = 1051 (n = 473, partially adjusted) | ||||||||||
| N = 751 (n = 343, fully adjusted) | ||||||||||
| PedsQL school functioning score | ||||||||||
| N = 1113 (n = 492, unadjusted) | 67.35 (21.72) | 72.40 (17.50) | 67.54 (21.56) | 71.42 (18.21) | 1.344 (–2.631 to 5.318) | 0.384 | 1.698 (–2.181 to 5.577) | 0.260 | 1.447 (–2.077 to 4.971) | 0.290 |
| N = 1050 (n = 474, partially adjusted) | ||||||||||
| N = 749 (n = 343, fully adjusted) | ||||||||||
| KIDSCREEN-52 bullying | ||||||||||
| N = 1116 (n = 496, unadjusted) | 11.74 (3.20) | 14.30 (7.92) | 12.05 (2.97) | 14.05 (6.28) | 0.249 (–0.907 to 1.406) | 0.579 | 0.594 (–0.482 to 1.671) | 0.155 | 0.359 (–0.799 to 1.516) | 0.425 |
| N = 1046 (n = 475, partially adjusted) | ||||||||||
| N = 746 (n = 342, fully adjusted) | ||||||||||
| Body image satisfaction score | ||||||||||
| N = 1110 (n = 494, unadjusted) | 1.54 (1.39) | 1.19 (1.04) | 1.56 (1.40) | 1.11 (0.96) | 0.081 (–0.091 to 0.253) | 0.226 | 0.049 (–0.132 to 0.229) | 0.487 | –0.024 (–0.185 to 0.137) | 0.700 |
| N = 1044 (n = 476, partially adjusted) | ||||||||||
| N = 748 (n = 344, fully adjusted) | ||||||||||
| Outcome | Unadjusted ICC | ICC adjusted for treatment arm | Partially adjusted ICCa | Fully adjusted ICCb |
|---|---|---|---|---|
| Suprascapular skinfold (mm) | 0.0668 (0.0330 to 0.1305) | 0.0627 (0.0301 to 0.1262) | 0.0766 (0.0398 to 0.1423) | 0.0463 (0.0192 to 0.1074) |
| Suprailiac skinfold (mm) | 0.0205 (0.0049 to 0.0821) | 0.0200 (0.0047 to 0.0820) | 0.1432 (0.0827 to 0.2364) | 0.1361 (0.0754 to 0.2333) |
| Biceps skinfold (mm) | 0.0893 (0.0487 to 0.1580) | 0.0886 (0.0482 to 0.1574) | 0.1461 (0.0878 to 0.2331) | 0.1276 (0.0728 to 0.2142) |
| Triceps skinfold (mm) | 0.0413 (0.0176 to 0.0940) | 0.0400 (0.0167 to 0.0930) | 0.1061 (0.0596 to 0.1819) | 0.1074 (0.0590 to 0.1877) |
| Thigh skinfold (mm) | 0.0128 (0.0011 to 0.1301) | 0.0122 (0.0009 to 0.1393) | 0.0356 (0.0083 to 0.1400) | 0.0140 (0.0004 to 0.3311) |
| Bioimpedance (Ω) | 0.0620 (0.0322 to 0.1159) | 0.0614 (0.0320 to 0.1149) | 0.0805 (0.0443 to 0.1419) | 0.0394 (0.0149 to 0.1002) |
| Sedentary time (hours/24 hours) | 0.1238 (0.0710 to 0.2070) | 0.1229 (0.0703 to 0.2060) | 0.1236 (0.0679 to 0.2146) | 0.1261 (0.0676 to 0.2232) |
| MVPA time (minutes/24 hours) | 0.1406 (0.0815 to 0.2318) | 0.1354 (0.0775 to 0.2259) | 0.1491 (0.0847 to 0.2493) | 0.1591 (0.0904 to 0.2647) |
| Systolic blood pressure (mmHg) | 0.0329 (0.0126 to 0.0834) | 0.0304 (0.0110 to 0.0813) | 0.0550 (0.0263 to 0.1111) | 0.0561 (0.0253 to 0.1198) |
| Diastolic blood pressure (mmHg) | 0.0740 (0.0407 to 0.1310) | 0.0740 (0.0406 to 0.1311) | 0.1027 (0.0604 to 0.1691) | 0.1020 (0.0574 to 0.1748) |
| Fat intake (grams in 24 hours) | 0.0542 (0.0267 to 0.1071) | 0.0517 (0.0250 to 0.1040) | 0.0558 (0.0269 to 0.1122) | 0.0485 (0.0213 to 0.1066) |
| Free sugars in 24 hours intake (grams in 24 hours) | 0.1356 (0.0797 to 0.2214) | 0.1242 (0.0714 to 0.2073) | 0.1000 (0.0516 to 0.1848) | 0.0818 (0.0386 to 0.1651) |
| Fibre intake (grams in 24 hours) | 0.0572 (0.0283 to 0.1121) | 0.0560 (0.0275 to 0.1108) | 0.0579 (0.0278 to 0.1166) | 0.0234 (0.0062 to 0.0843) |
| Fruit and vegetables intake (grams in 24 hours) | 0.0625 (0.0311 to 0.1217) | 0.0624 (0.0310 to 0.1214) | 0.0668 (0.0332 to 0.1301) | 0.0438 (0.0179 to 0.1035) |
| PedsQL physical functioning score | 0.0877 (0.0503 to 0.1485) | 0.0876 (0.0502 to 0.1485) | 0.0844 (0.0472 to 0.1465) | 0.0749 (0.0378 to 0.1427) |
| PedsQL psychosocial functioning score | 0.0518 (0.0249 to 0.1044) | 0.0503 (0.0241 to 0.1019) | 0.0485 (0.0228 to 0.0999) | 0.0203 (0.0042 to 0.0913) |
| PedsQL emotional functioning score | 0.0304 (0.0114 to 0.0786) | 0.0287 (0.0106 to 0.0758) | 0.0308 (0.0116 to 0.0791) | 0.0008 (0.0000 to 1.0000) |
| PedsQL social functioning score | 0.0235 (0.0071 to 0.0753) | 0.0233 (0.0070 to 0.0749) | 0.0208 (0.0056 to 0.0739) | 0.0046 (0.0000 to 0.5299) |
| PedsQL school functioning score | 0.0512 (0.0252 to 0.1011) | 0.0505 (0.0249 to 0.0999) | 0.0457 (0.0213 to 0.0950) | 0.0213 (0.0049 to 0.0877) |
| KIDSCREEN-52 bullying | 0.0042 (0.0001 to 0.2254) | 0.0040 (0.0001 to 0.2460) | 0.0008 (0.0000 to 1.0000) | 0.0077 (0.0003 to 0.1939) |
| Body image satisfaction score | 0.0109 (0.0013 to 0.0835) | 0.0087 (0.0007 to 0.1026) | 0.0122 (0.0016 to 0.0884) | 0.0000 (0.0000 to 0.0000) |
In the primary analysis (adjusted only for baseline outcome), there were no significant differences observed at FU1. However, there was a statistically significant difference at FU1 in the fully adjusted model in relation to free sugar intake (MD –5.636 g, 95% CI –12.285 to 1.014 g; p = 0.029) and body image satisfaction (MD 0.251, 95% CI –0.026 to 0.528; p = 0.020). With regard to the former, there was also a difference approaching significance at FU2 in the partially adjusted model (MD –7.886 g, 95% CI –18.488 to 2.716 g; p = 0.055) that was strengthened and became significant after the additional covariate adjustment in the fully adjusted model (MD –9.22 g, 95% CI –19.032 to 0.592 g; p = 0.015). The direction of effect was consistent across both follow-up time points, with greater mean free sugar consumption in the 24-hour period assessed in the control arm than in the intervention arm.
At FU2, the primary analysis showed a significant difference between the intervention and control arms for subscapular skinfold (MD 0.198, 95% CI –0.028 to 0.423; p = 0.024), with the estimate being robust to covariate adjustment (MD 0.199, 95% CI –0.016 to 0.414; p = 0.017). Although the MD shows that the mean subscapular skinfold thickness was higher in the intervention arm than in the control arm, the difference is in fact very small (< 0.2 mm). For the same time point, a difference [again very small (MD 0.241)] in the same direction approaching statistical significance (p = 0.059) is also observed for suprailiac skinfold in the partially adjusted analysis, but the difference reduces and is no longer significant after covariate adjustment.
Ancillary analyses
Prespecified subgroup analyses
For tables presenting the results of the prespecified subgroup analyses at FU1 and FU2, see Appendix 60. For each characteristic considered in the subgroup analysis (ethnicity, fidelity, sex, deprivation and weight status), the results are presented in a separate table (first for FU1 and then for FU2), followed by a further table presenting the outcomes of the interaction tests undertaken to determine whether or not there is a statistically significant difference in treatment effect between the subgroups considered for each characteristic.
Although the CIs and p-values for a few outcomes in some of the subgroups were suggestive of a statistically significant intervention effect, there were no consistent patterns in general, and the difference in intervention effect between the subgroups was not accompanied by a significant interaction term.
The subgroup analysis including only participants of black African Caribbean ethnicity was the only one with some consistent patterns that were worth considering. At FU1, the MD in the intervention arm compared with the control arm favoured the intervention for all measures of adiposity. The differences were statistically significant in the fully adjusted models for BMI-z (MD –0.372, 95% CI –0.652 to –0.091; p = 0.009), waist z-score (MD –0.689, 95% CI –1.044 to –0.333; p < 0.001) and body fat percentage (MD –2.198, 95% CI –4.278 to –0.118; p = 0.038). The negative values for the MDs show that the value of the mean for these outcomes is higher in the control arm than in the intervention arm after adjustment for baseline outcome and the prespecified covariates.
In addition, there was a significant positive RD between the arms in terms of achieving 60 minutes of at least moderate PA (RD 0.446, 95% CI 0.010 to 1.255; p = 0.043). This means that in the black African Caribbean subgroup, after baseline and covariate adjustment, the participants in the intervention arm were 44.6% more likely than those in the control arm to meet the government guideline for PA in children and young adults. The interaction terms were not significant for any of these observed differences.
At FU2, a similar pattern was seen in terms of adiposity. In the fully adjusted analyses BMI-z (MD –0.613, 95% CI –1.053 to –0.173; p = 0.006), waist z-score (MD –1.029, 95% CI –1.417 to –0.641; p = < 0.001), sum of four skinfolds (MD –3.485, 95% CI –5.497 to –1.473; p = 0.001) and body fat percentage (MD –3.437, 95% CI –6.289 to –0.585; p = 0.018) were all significantly lower among children in the intervention arm than among those in the control arm. The proportion of children with excess weight was also lower in the intervention arm than in the control arm (partially adjusted model RD –0.193, 95% CI –0.282 to –0.038; p = 0.021; fully adjusted model RD –0.349, 95% CI –0.391 to –0.123; p = 0.017), indicating a lower prevalence of 19.3% and 34.9% in the partially and fully adjusted models, respectively. The proportion who were obese (RD –0.131, 95% CI –0.201 to –0.002; p = 0.047) was also lower, but only in the partially adjusted model, indicating that after baseline value adjustment the intervention arm participants are 13.1% less likely to be obese than participants in the control arm.
In terms of behavioural outcomes, however, PA energy expenditure (partially adjusted model MD –14.565, 95% CI –27.44 to –1.689; p = 0.027; fully adjusted model MD –15.80, 95% CI –29.817 to –1.782; p = 0.027), likelihood of achieving 60 minutes of at least moderate PA (RD –0.282, 95% CI –0.293 to –0.130; p = 0.016) and consumption of at least five portions of fruit and vegetables (partially adjusted model RD –0.283, –0.429 to –0.030; p = 0.033; fully adjusted model RD –0.502, 95% CI –0.593 to –0.204; p = 0.009) were all significantly lower among intervention children than among control children.
At FU2, the interaction tests showed significant intervention effect for sum of four skinfolds (partial and fully adjusted models, interaction terms of 0.036 and 0.005, respectively), physical activity energy expenditure (partial and fully adjusted models, interaction terms of 0.006 and < 0.001, respectively) and proportion at least overweight (partial and fully adjusted models, interaction terms of 0.003 and 0.028, respectively).
Exploratory subgroup analyses (by school group)
This analysis was prompted by the observed difference in magnitude of effect size for BMI-z between arms at FU2 compared with at FU3 (see Appendix 60). We found a statistically and clinically significant difference between trial arms in the G1 school participants at 27 months in favour of the intervention. However, at both FU1 and FU2 (where we had combined data for participants in G1 and G2 schools), the difference between arms was small and not statistically significant. To interpret this finding we needed to know whether or not this could be a late intervention effect, or whether or not there were differences between G1 and G2 schools. As part of this exploration, we considered differences in baseline characteristics, contextual differences (within schools or at a wider policy level, given that intervention delivery between groups was 1 year apart) or differences in the way in which the intervention was delivered. As we were not aware of any major contextual differences, and the process evaluation provided no evidence of differences in terms of intervention delivery, we undertook this exploratory analysis.
Baseline characteristics in G1 (Table 26) and G2 (Table 27) schools are presented separately below. In G1 schools the mean BMI-z in intervention and control arms was similar (0.29 and 0.28, respectively). However, in G2 schools, there was an imbalance, with higher mean BMI-z in the intervention arm (0.19) than in the control arm (0.04). Overall, BMI-z was also higher in G1 schools than in G2 schools. Owing to these baseline differences, an exploratory analysis of primary and secondary outcomes between trial arms at FU1 and FU2 was undertaken. The findings are described below, and tables presenting these results are shown in Appendix 61.
| Characteristic N (number in intervention arm) | Arm | Total | |
|---|---|---|---|
| Intervention | Control | ||
| Demographic | |||
| Age (years): N = 621 (293), mean (SD) – not known: intervention = 9, control = 20 | 6.34 (0.30) | 6.32 (0.30) | 6.33 (0.30) |
| Sex | |||
| N = 650 (302), n (%) | |||
| Male | 137 (45.4) | 180 (51.7) | 317 (48.8) |
| Female | 165 (54.6) | 168 (48.3) | 333 (51.2) |
| Ethnicity | |||
| N = 645 (298), n (%) | |||
| White British | 154 (51.7) | 181 (52.2) | 335 (51.9) |
| South Asian | 82 (27.5) | 83 (23.9) | 165 (25.6) |
| Black African Caribbean | 25 (8.4) | 23 (6.6) | 48 (7.4) |
| Other | 37 (12.4) | 60 (17.3) | 97 (15.0) |
| Not known | 4a | 1a | 5a |
| IMD quintile | |||
| N = 636 (291), n (%) | |||
| 1 (most deprived) | 128 (44.0) | 179 (51.9) | 307 (48.3) |
| 2 | 67 (23.0) | 73 (21.2) | 140 (22.0) |
| 3 | 48 (16.5) | 35 (10.1) | 83 (13.1) |
| 4 | 44 (15.1) | 25 (7.2) | 69 (10.8) |
| 5 (least deprived) | 4 (1.4) | 33 (9.6) | 37 (5.8) |
| Not known | 1a | 3a | 14a |
| IMD score | |||
| N = 636 (291), median (IQR) – not known: intervention = 11, control = 3 | 30.25 (17.14–44.36) | 37.55 (19.84–46.29) | 32.87 (17.59–46.09) |
| Anthropometric | |||
| BMI-z | |||
| N = 619 (292), mean (SD) – not known: intervention = 10, control = 21 | 0.29 (1.24) | 0.28 (1.12) | 0.29 (1.18) |
| Height (cm) | |||
| N = 619 (292), mean (SD) – not known: intervention = 10, control = 21 | 118.95 (5.74) | 118.75 (5.60) | 118.84 (5.66) |
| Waist circumference z-score | |||
| N = 600 (273), mean (SD) – not known: intervention = 29, control = 21 | 0.86 (1.17) | 0.92 (1.14) | 0.89 (1.16) |
| Sum of four skinfoldsb (mm) | |||
| N = 512 (240), median (IQR) – not known: intervention = 62, control = 76 | 29.03 (24.48–35.65) | 30.55 (24.45–40.10) | 29.68 (24.48–37.93) |
| Body fat % | |||
| N = 616 (291), mean (SD) – not known: intervention = 11, control = 23 | 21.33 (5.19) | 21.18 (5.21) | 21.25 (5.20) |
| Weight statusc | |||
| N = 619 (292), n (%) | |||
| Underweight (≤ 2nd centile) | 8 (2.7) | 2 (0.6) | 10 (1.6) |
| Healthy weight (> 2nd and < 85th centiles) | 217 (74.3) | 258 (78.9) | 475 (76.7) |
| Overweight (≥ 85th and < 95th centiles) | 28 (9.6) | 24 (7.3) | 52 (8.4) |
| Obese (≥ 95th centile) | 39 (13.4) | 43 (13.1) | 82 (13.2) |
| Not known | 10≈ | 21≈ | 31≈ |
| 24-hour dietary intake | |||
| Energy (kJ in 24 hours) | |||
| N = 551 (264), median (IQR) – not known: intervention = 38, control = 61 | 6907 (5858–7964) | 7071 (5960–8030) | 7015 (5900–8009) |
| Five or more portions of fruit and vegetables | |||
| N = 551 (264), n (%) | |||
| Yes | 160 (60.6) | 207 (72.1) | 367 (66.6) |
| No | 104 (39.4) | 80 (27.9) | 184 (33.4) |
| Not known | 38a | 61a | 99a |
| PA | |||
| PA energy expenditure (kJ/kg/day) | |||
| N = 528 (244), mean (SD) – not known: intervention = 58, control = 64 | 93.07 (21.69) | 91.82 (22.42) | 92.39 (22.07) |
| ≥ 60 minutes’ MVPA/24 hours | |||
| N = 525 (242), n (%) | |||
| Yes | 88 (36.4) | 133 (47.0) | 221 (42.1) |
| No | 154 (63.6) | 150 (53.0) | 304 (57.9) |
| Not known | 60a | 65a | 125a |
| Psychological | |||
| PedsQL total score | |||
| N = 617 (292), median (IQR) – not known: intervention = 10, control = 23 | 72.83 (63.04–84.78) | 73.91 (63.04–82.61) | 73.91 (63.04–82.61) |
| CHU9D utility score | |||
| N = 594 (277), mean (SD) – not known: intervention = 25, control = 31 | 0.84 (0.13) | 0.82 (0.14) | 0.83 (0.14) |
| Characteristic N (number in intervention arm) | Arm | Total | |
|---|---|---|---|
| Intervention | Control | ||
| Demographic | |||
| Age (years) | |||
| N = 776 (369), mean (SD) – not known: intervention = 18, control = 23 | 6.28 (0.30) | 6.22 (0.31) | 6.25 (0.31) |
| Sex | |||
| N = 817 (387), n (%) | |||
| Male | 202 (52.2) | 230 (53.5) | 432 (52.9) |
| Female | 185 (47.8) | 200 (46.5) | 385 (47.1) |
| Ethnicity | |||
| N = 806 (378), n (%) | |||
| White British | 143 (37.8) | 180 (42.1) | 323 (40.1) |
| South Asian | 139 (36.8) | 139 (32.5) | 278 (34.5) |
| Black African Caribbean | 37 (9.8) | 30 (7.0) | 67 (8.3) |
| Other | 59 (15.6) | 79 (18.5) | 138 (17.1) |
| Not known | 9a | 2a | 11a |
| IMD quintile | |||
| N = 803 (379), n (%) | |||
| 1 (most deprived) | 264 (69.7) | 219 (51.7) | 483 (60.1) |
| 2 | 53 (14.0) | 81 (19.1) | 134 (16.7) |
| 3 | 24 (6.3) | 39 (9.2) | 63 (7.8) |
| 4 | 21 (5.5) | 29 (6.8) | 50 (6.2) |
| 5 (least deprived) | 17 (4.5) | 56 (13.2) | 73 (9.1) |
| Not known | 8a | 6a | 14a |
| IMD score | |||
| N = 803 (379), median (IQR) – not known: intervention = 8, control = 6 | 42.75 (30.92–55.24) | 37.88 (16.42–50.46) | 41.63 (22.69–51.65) |
| Anthropometric | |||
| BMI-z | |||
| N = 773 (368), mean (SD) – not known: intervention = 19, control = 25 | 0.19 (1.24) | 0.04 (1.26) | 0.11 (1.25) |
| Height (cm) | |||
| N = 777 (372), mean (SD) – not known: intervention = 15, control = 25 | 118.37 (5.48) | 117.73 (5.15) | 118.04 (5.32) |
| Waist circumference z-score | |||
| N = 659 (316), mean (SD) – not known: intervention = 71, control = 87 | 0.69 (1.30) | 0.41 (1.29) | 0.54 (1.30) |
| Sum of four skinfoldsb | |||
| (mm) N = 625 (300), median (IQR) – not known: intervention = 87, control = 105 | 27.55 (22.13– 35.30) | 26.75 (22.15– 34.05) | 27.20 (22.15–34.85) |
| Body fat % | |||
| N = 760 (369), mean (SD) – not known: intervention = 18, control = 39 | 21.27 (5.49) | 20.76 (5.22) | 21.01 (5.35) |
| Weight statusc | |||
| N = 773 (368), n (%) | |||
| Underweight (≤ 2nd centile) | 12 (3.3) | 18 (4.4) | 30 (3.9) |
| Healthy weight (> 2nd and < 85th centiles) | 278 (75.5) | 304 (75.1) | 582 (75.3) |
| Overweight (≥ 85th and < 95th centiles) | 33 (9.0) | 39 (9.6) | 72 (9.3) |
| Obese (≥ 95th centile) | 45 (12.2) | 44 (10.9) | 89 (11.5) |
| Not known | 19a | 25a | 44a |
| 24-hour dietary intake | |||
| Energy (kJ in 24 hours) | |||
| N = 636 (298), median (IQR) – not known: intervention = 89, control = 92 | 6894 (5871–8098) | 6739 (5700–7830) | 6833 (5779–7988) |
| Five or more portions of fruit and vegetables | |||
| N = 636 (298), n (%) | |||
| Yes | 176 (59.1) | 198 (58.6) | 374 (58.8) |
| No | 122 (40.9) | 140 (41.4) | 262 (41.2) |
| Not known | 89a | 92a | 181a |
| PA | |||
| PA energy expenditure (kJ/kg/day) | |||
| N = 524 (248), mean (SD) – not known: intervention = 139, control = 154 | 99.73 (24.11) | 91.81 (22.42) | 97.98 (25.20) |
| ≥ 60 minutes’ MVPA/24 hours | |||
| N = 523 (249), n (%) | |||
| Yes | 140 (56.2) | 143 (52.2) | 283 (54.1) |
| No | 109 (43.8) | 131 (47.8) | 240 (45.9) |
| Not known | 138a | 156a | 294a |
| Psychological | |||
| PedsQL total score | |||
| N = 767 (371), median (IQR) – not known: intervention = 16, control = 34 | 69.57 (56.52–80.43) | 71.74 (60.87–82.61) | 71.74 (58.70–80.43) |
| CHU9D utility score | |||
| N = 756 (366), mean (SD) – not known: intervention = 21, control = 40 | 0.83 (0.14) | 0.81 (0.15) | 0.82 (0.14) |
Continuous outcome: body mass index z-score
At FU1, the mean BMI-z in G1 was 0.35 (SD 1.32) in the intervention arm and 0.53 (SD 1.16) in the control arm. This corresponds to an unadjusted MD in BMI-z between intervention and control arms in G1 of –0.176 (95% CI –0.375 to 0.024; p = 0.084). This indicates that the average BMI-z was smaller in the intervention arm than in the control arm in G1. After adjusting for baseline BMI-z, the MD in BMI-z in G1 was –0.233 (95% CI –0.345 to –0.122; p < 0.001). This estimate is robust to covariate adjustment, as the fully adjusted estimate does not differ much (MD –0.258, 95% CI –0.355 to –0.160; p < 0.001).
For G2, at FU1, the mean BMI-z was 0.33 (SD 1.35) in the intervention arm and –0.00 (SD 1.31) in the control arm. This corresponds to an unadjusted MD in BMI-z between intervention and control arms in G2 of 0.331 (95% CI 0.128 to 0.534; p = 0.001). This indicates that the average BMI-z was greater in the intervention arm than in the control arm in G2. After adjusting for baseline BMI-z, the MD in BMI-z in G2 was 0.079 (95% CI –0.088 to 0.246; p = 0.353). The fully adjusted estimate of the MD in BMI-z was 0.136 (95% CI –0.025 to 0.297; p = 0.097).
At FU1, the mean BMI-z was greater in G1 than in G2. This corresponds to the group effect of 0.529 (95% CI 0.302 to 0.756; p = < 0.001) in the unadjusted analyses. This represents the average difference in BMI-z between G1 and G2, and indicates that the average BMI-z was 0.529 higher in G1 than in G2. After adjusting for all covariates, the group effect was 0.294 (95% CI 0.148 to 0.440; p < 0.001). In all of the three models, there was a statistically significant difference at the 5% level between the mean BMI-z of G1 and G2.
At first follow-up there is evidence to suggest that the intervention behaved differently across randomised G1 and G2 on BMI-z. In the unadjusted model, the p-value for the interaction between group and arm (< 0.001) indicates that there is a statistically significant difference at the 5% level between the intervention effect on BMI-z. This difference is statically significant in the partially adjusted model (p = 0.001) and in the fully adjusted model (p < 0.001).
Other continuous outcomes for group 1 schools
For waist z-score and body fat percentage, there was a similar pattern of effects to that observed for BMI-z, with effects favouring the intervention in G1 schools at FU1, although the differences were of borderline statistical significance. The MD in sum of skinfolds at both follow-up points, and for waist z-score at FU2, were higher in the intervention arm than in the control arm, although the differences were not statistically significant.
The CHU9D utility score was higher in the intervention arm than in the control arm in G1 schools at FU1 (partially adjusted model 0.026, 95% CI –0.001 to 0.053; p = 0.056; fully adjusted model 0.031, 95% CI 0.000 to 0.062; p = 0.050). At FU2, the difference between groups was much smaller and not statistically significant (partially adjusted model 0.006, 95% CI –0.010 to 0.022; p = 0.44; fully adjusted model 0.013, 95% CI –0.004 to 0.029; p = 0.127).
Binary outcome: obesity
In G1 at FU1, 16.85% of those in the intervention arm and 17.75% of those in the control arm were classified as obese. The unadjusted RD of –0.009 (95% CI –0.045 to 0.037; p = 0.674) indicates that the risk of being obese is 0.9% lower in the intervention arm than in the control arm. After adjusting for baseline BMI-z, the RD of being obese is –0.056 (95% CI –0.092 to –0.005; p = 0.035). When adjusting for all of the covariates, the association becomes slightly weaker (RD –0.037, 95% CI –0.069 to 0.004; p = 0.076).
At FU1, 15.64% of those in the intervention arm in G2 were classified as obese, compared with 12.57% of those in the control arm. The risk of being obese is 3.1% higher in the intervention arm than in the control arm. This corresponds to the unadjusted RD of 0.031 (95% CI –0.014 to 0.093; p = 0.202). The RD of being obese in G2 after adjusting for baseline BMI-z is –0.022 (95% CI –0.063 to 0.042; p = 0.428). After adjusting for all of the covariates, the RD of being obese in G2 is 0.016 (95% CI –0.039 to 0.104).
At first follow-up, there is not a statistically significant difference between the intervention effect on the risk of being obese between G1 and G2 (p = 0.196). This indicates that there is insufficient evidence to suggest that the intervention behaved differently in G1 compared with G2 with respect to lowering the risk of obesity. There is not a statistically significant difference in the risk of obesity between G1 and G2 when adjusting for baseline BMI-z (p = 0.200) or in the fully adjusted model (p = 0.658).
Sensitivity analyses
For tables presenting the results of the sensitivity analyses at FU1 and FU2, see Appendix 62. Results are presented for the key anthropometric, diet, PA and psychological variables in the same order as described in Chapter 5 (see Sensitivity analyses): multiple imputation (FU1 then FU2), different levels of clustering (FU1 then FU2), alternative methods for baseline adjustment (FU1 then FU2) and treatment by cluster variation in heterogeneity (FU1 then FU2). There were no important changes in any conclusions as a result of undertaking any of these sensitivity analyses.
Harm
Potential harm from the intervention was objectively assessed by the wider psychosocial outcomes. Quality of life (assessed using the PedsQL), as total score or subdomains, did not differ significantly between arms at either FU1 or FU2. Similarly, there were no significant differences between the arms at any follow-up point in terms of social acceptance (KIDSCREEN-52) or body image dissatisfaction. Therefore, we found no evidence of harm from the intervention.
Chapter 7 Cost-effectiveness of an obesity-prevention intervention programme in primary school-aged children
Summary
In this chapter, the economic evaluation conducted alongside the WAVES trial is reported. Obesity costs the NHS millions of pounds every year, increasing to billions of pounds if wider societal costs are also included. Obese children are at an increased risk of health problems and also more likely to become obese adults, so it is vital that robust evidence is produced on the cost-effectiveness of interventions to prevent obesity in children. The overall aim in this chapter is to estimate the cost-effectiveness of the WAVES obesity prevention intervention programme in primary school-aged children. To achieve this, an analysis comparing the cost-effectiveness of the intervention with that of no intervention was undertaken. The primary analysis was based on the outcome measure QALYs. A secondary analysis based the evaluation on cost per obesity case prevented. Given the school-based multifaceted nature of the intervention, the analysis was from the public sector perspective and therefore included costs falling on the schools. All of the costs are expressed in the year 2014. Missing data were addressed using multiple imputation methods, and the uncertainty surrounding the cost-effectiveness estimates was examined through the use of the net benefit regression (NBR) framework and presented using cost-effectiveness acceptability curves (CEACs). The analysis of cost-effectiveness was carried out in accordance with current best-practice methods for conducting economic evaluation alongside cluster randomised controlled trials. 88
Aim
The aim was to estimate the cost-effectiveness of an obesity prevention intervention programme in primary school-aged children.
Methods
Data collection
In order to conduct the economic evaluation, information on both the costs and the QALYs was required. 89 As with standard practice, the base-case analysis assumed that the intervention was ‘up and running’, that is, it excluded sunk costs. These costs were included, however, within the sensitivity analyses. To calculate the costs of the intervention, resource use was collected throughout the intervention period to which unit costs were applied. To calculate QALYs, health-utility data were collected using the CHU9D) instrument46 at baseline (start of the intervention), at FU1, which was 3 months post intervention (15 months since baseline), and at FU2, which was 18 months post intervention (30 months since baseline). Outcomes were collected at the individual level and costs were collected at the cluster level (e.g. a teacher preparing for a nutrition lesson); these cluster-level costs were then averaged across the children within the cluster to derive individual-level costs for the intervention.
Costs
Cluster-level resource use was combined with unit costs to calculate the total cluster-level cost. The costs associated with the intervention were split into three phases:
-
development/set-up costs
-
implementation costs
-
delivery/running costs.
For the base-case cost-effectiveness analysis, only the costs involved with delivering the intervention were included. However, all of the costs are described in this section.
Table 28 outlines the cost items that were associated with each phase of the intervention. The first phase comprised costs associated with the development and set-up of the intervention. These costs included staff time for the development of materials for the intervention and its delivery. Implementation costs were costs associated with the printing of intervention materials and staff training. Phase 3 costs were focused on the delivery of the intervention. These were the costs associated with the intervention once it was ‘up and running’ and included all of the aspects that were associated with delivering the intervention on an ongoing basis. The base-case analysis assumed that the intervention was in a steady state and thus included only phase 3 costs. Set-up and implementation costs were considered, however, within the sensitivity analyses.
| Phase 1: intervention development and trial set-up costs | Phase 2: intervention implementation costs | Phase 3: intervention delivery/running costs |
|---|---|---|
|
|
|
There were four main components to the intervention, each of which contained subcomponents:
-
cooking workshops (including short healthy eating class lessons)
-
signposting of PA opportunities
-
increased levels of PA
-
the use of role models (Villa Vitality component).
Study-specific resource use collection instruments were developed for these four components of the intervention.
The cooking component
The resource use associated with the cooking component of the intervention was measured using school staff-completed logbooks. School staff recorded how much time was spent on both the preparation and the delivery of the workshops and classroom sessions. On most occasions it was the teacher who was involved, and sometimes TAs were used. When ‘other staff’ members were listed but their roles were not described, a TA-level role was assumed. The materials used in the workshops were purchased and delivered by the research team in person. Parents were also invited, and their time and travel costs were acquired from a resource use questionnaire. Receipts for the materials used in the cooking workshops were logged and costed to estimate the average material cost per class. The costs associated with delivering the materials to the schools were calculated from the mileage and time it took for the research assistant to travel to each school.
The physical activity component
Each school within the intervention arm was asked to pick two of the offered PA packages. The costs associated with these packages were recorded as implementation costs and are detailed in Table 29. The PA component was delivered either during class time or at lunchtime. All resource use associated with the preparation and delivery of the packages was recorded using school staff-completed logbooks.
| Type | Resource use item | Unit cost, £ (two dp) | Assumptions | Source |
|---|---|---|---|---|
| School costs | Hour of teacher time | 20.09/hour | Based on standard contracted 1265 hour/year | Department of Health and Department for Education (2013–14) salary scales – M3 |
| Hour of TA time | 9.04/hour | ONS 2014 New Earnings Survey90 | ||
| Lunchtime assistant lady | 7.75/hour | ONS 2014 New Earnings survey90 | ||
| Supply cover | 200/day, 100/half-day | Specified by attendee at training workshop | ||
| University staff time | Hour of administrative support time | 11.67 | Adjusted per hour on the assumption of 7.5 hours per day, 104 days’ weekend, 15 closed days’ and 25 days’ annual leave | Official university pay scales (2013–14); spine point 35 |
| Hour of research assistant/associate time | 16.48 | As above | Official university pay scales (2013–14); grade 6 Spine point 26 | |
| Hour of research fellow time | 18.54 | As above | Official university pay scales (2013–14); grade 7 spine point 30 | |
| Hour of senior research fellow time | 32.44 | As above | Official university pay scales (2013–14); grade 9 spine point 49 | |
| Hour of professorial time | 44.37 | As above | Official university pay scales (2013–14); professorial band 2, spine point 11 | |
| One-off intervention costs | Villa Vitality package | 1979.66/class | One-off payment, which included the day and printing. Unit cost adjusted to 2014 prices and divided across classes | Trial team finance records |
| Cooking workshop materials: breakfast | ||||
| Raisins | 0.36 | Resource use was captured from the shopping lists for G2 schools in the trial. An implicit assumption is that the resource use was the same for G1 schools in the trial | Tesco (Tesco PLC, Welwyn Garden City, UK) | |
| Tinned fruit | 0.34 | Asda (Asda, Leeds, UK) | ||
| Cereals | 2.33 | Asda | ||
| Weetabix (Weetabix Food Company, Kettering, UK) | 1.80 | Asda | ||
| Bran flakes (Kellogg Company, Manchester, UK) | 0.68 | Asda | ||
| Chopping boards | 0.7 | IKEA (IKEA, Leiden, the Netherlands) | ||
| Knives | 0.02 | Asda | ||
| Spoons | 0.02 | Asda | ||
| Bowls | 0.10 | Asda | ||
| Kitchen towels | 0.34 | Asda | ||
| Archive boxes | 1.29 | Asda | ||
| Perishables | 6.34 | Trial estimate | ||
| Cooking workshop materials: lunch | ||||
| Tuna | 0.70 | Items were bought in bulk; the unit cost represents the per-unit cost | Asda | |
| Sweetcorn | 0.49 | |||
| LF salad cream | 0.95 | |||
| Bowls | 0.10 | |||
| Spoons | 0.02 | |||
| Kitchen rolls | 0.34 | |||
| Cooking workshop materials: dinner | ||||
| Couscous | 0.68 | Prices adjusted to 2014 prices | Asda | |
| Tinned beans | 0.29 | |||
| Sweetcorn | 0.49 | |||
| Vegetable stock | 0.98 | |||
| Kitchen rolls | 0.34 | |||
| Spoons | 0.02 | |||
| Bowls | 0.10 | |||
| PA materials | ||||
| Wake Up Shake Up | 26.11 | Prices adjusted to 2014 prices | Unit costs identified from purchase order receipts collected by the trial team | |
| Activate | 277.59 | |||
| Positive Play | 87.08 | |||
| Take 10 | 51.81 | |||
| Travel costs | Mileage | 0.45 per mile | HMRC/gov.uk guidance91 | |
Villa Vitality programme
This part of the intervention was split into the following subcomponents:
-
two Villa Vitality days
-
one Villa Vitality school-based session (run by football club staff)
-
classroom challenges and class project.
The Villa Vitality days were purchased at a fixed cost, which was then averaged across all of the classes to derive a cost per class. When school staff had supervised the children during the Villa Vitality days, the costs that were associated with their time were included. Parents were also welcome to attend the Villa Vitality days and, when this happened, their time and resource use were recorded in travel cost questionnaires and included within the sensitivity analysis, for which a wider perspective was adopted.
Teaching staff completed logbooks to record the resource use that was associated with the delivery of the classroom sessions.
Signposting
The resource use associated with the signposting included printing and the delivery of materials to the schools. All of the purchase orders and receipts for printing were recorded and the cost of delivery was estimated based on the number of sheets posted. This item of expenditure was treated as an ongoing cost, as it required either updating (generic signposting sheet) or complete revision (school-specific signposting sheet) at the start of each intervention year and was therefore included as part of the intervention cost within the base-case analysis.
Unit costs and assumptions
This section outlines the justification of, and source for, the unit costs applied to each component of the intervention, as outlined in Table 29.
School unit costs
Unit costs for an hour of a teacher’s time were calculated using the mid-scale point on the standardised Department for Education salary scales. 92 Resource use was measured on a per-hour basis. The annual salary scales were based on a contracted 1265 hours per year. Thus, to estimate the cost per hour, the annual salary was divided by 1265 hours. Annual salary scales were not available for TAs, LTAs or dinner ladies, and so to calculate the hourly unit costs for these roles the estimates were based on unit costs published by the Office for National Statistics in its 2014 New Earnings Survey. 90
University unit costs
Included within the sensitivity analyses were the costs associated with the set-up and implementation of the intervention. Many of these costs were incurred by the research institute at the University of Birmingham. These costs included administration and research staff time. To calculate the unit costs for each of these roles, the 2014 University of Birmingham academic/support staff salary scales were used. Appropriate mid-points of the salary scale were selected for each staff position. These salaries were then converted to an hourly rate assuming that staff worked 7.5 hours per day excluding weekends, university ‘closed days’ and public holidays.
Other unit costs
For the cooking workshops, the unit costs for the cooking materials used were based on the purchase price of each item. For the PA elements of the intervention, the fixed costs associated with the activity packages chosen were recorded by the trial team and the receipts were retained.
All of the costs were adjusted to 2014 prices. Finally, for various aspects of the intervention, there were associated travel costs. When travel by car was recorded, the Her Majesty’s Revenue & Customs guidance was used and a £0.45-per-mile cost was applied in line with standard practice.
Outcomes
Measuring quality-adjusted life-years
After initial pilot research on the acceptability, reliability and validity of competing preference-based measures for children,93 the CHU9D instrument was used to collect quality-of-life information for the children. The CHU9D46 features nine dimensions of child HRQL: worried, sad, pain, tired, annoyed, schoolwork/homework, sleep, daily routine and ability to join in activities. Each dimension contains five severity levels, resulting in 1,953,125 unique health states that are associated with the measure. Responses from the CHU9D questionnaires were transformed into quality-of-life (utility) weights derived from a UK general population sample using an algorithm developed by Stevens et al. 46 This gives a possible utility value set of between 0.33 (worst health state) and 1 (best health state). The QALYs were then calculated for each individual child using the area under the curve method,94 which uses the trapezium rule.
Assessing quality-adjusted life-year differences
To control for differences in baseline utility between the intervention and control arms,94 prespecified covariates were adjusted for based on a statistical analysis plan. These were cluster-level variables, which were used in the randomisation (size of school, proportion of pupils eligible for free school meals, ethnic mix of pupils), and pupil-level factors (sex, baseline CHU9D score, ethnicity, deprivation, baseline total energy consumption and baseline PA energy expenditure). 95
Thus, three models are reported within the analysis:
-
a linear regression model
-
a multilevel regression model controlling for baseline utility
-
a multilevel regression model controlling for baseline utility and prespecified covariates.
The first model is an unadjusted model, that is, a linear regression of costs (or QALYs) on the independent intervention dummy variable. The data, however, were clustered, and, to account for this, the second model adopts a hierarchical approach to account for clustering while also controlling for baseline utility to address baseline differences. The third and final model, and the one used for the primary analysis, adds the prespecified covariates to model 2. This model, therefore, adjusts for clustering and baseline utility, as well as the covariates specified within the analysis plan. All of the multilevel models were implemented using Stata’s ‘mi estimate: mixed’ command, using maximum likelihood estimation to fit a multilevel mixed-effect linear regression including a random effect for the level 2 school variable using multiply imputed data.
Multiple imputation
Resource use data were collected at the cluster-level, whereas health outcome data were collected at the individual level; consequently, any reason for missing data (the missingness mechanism) varied for these two different types of data. The cost and QALY data were therefore imputed separately to include the relevant covariates within the imputation model and then combined to form a complete data set. During the imputation process, to account for the hierarchical nature of the data, all of the individual-level data were imputed using multilevel multiple imputation. This was implemented through REALCOM-IMPUTE software in conjunction with Stata 13. Thirty imputations were conducted, resulting in 30 complete data sets. Rubin’s rule,84 which incorporates uncertainty around the predicted values, was used to calculate pooled estimates of the mean costs and QALYs, as well as CIs. Given the number of missing data, the base-case analysis uses the imputed data.
Analyses
Our primary analysis was a CUA examining the cost per QALY gained for all of the children. In this trial context, the control group was no intervention, and, therefore, no costs were associated with this arm. To calculate the ICER between the intervention and control arms, the differences in costs and QALYs were analysed jointly, and to account for both the correlation between costs and outcomes96 and the clustered nature of the trial, the NBR framework97,98 was applied. This facilitates the calculation of the ICER and the analysis of uncertainty via a CEAC while controlling for any baseline differences and clustering effects. 97 As the economic evaluation was carried out alongside the trial, only costs and outcome data collected from the trial were included. All costs and outcomes were discounted at 3.5%.
Sensitivity analysis methods
A series of sensitivity analyses were conducted.
Sensitivity analysis 1: different multiple imputation methods
To test the sensitivity of the results to the multiple imputation model used for the base-case analysis (random-effects imputation model), a fixed-effects imputation model was applied.
Sensitivity analysis 2: including set-up and implementation costs
The base-case analysis assumed that the intervention was in a ‘running state’ and thus included only costs that were associated with the ongoing delivery of the intervention. Within the trial, however, there were a number of set-up and implementation costs that were also captured, and, to test how sensitive the results were to these costs, the costs were included in the second sensitivity analysis.
Sensitivity analysis 3: including wider costs
For two components of the intervention (Villa Vitality and the cooking workshops), some parents attended. As requested, schools invited all of the parents of the children in the intervention year (year 2) to attend the cooking workshops, with levels of actual parental attendance varying between schools. Some schools also invited parents to attend the Villa Vitality days as helpers. The third sensitivity analysis tested the sensitivity of the results to the inclusion of these costs. Parents’ time and travel costs were collected using time and travel cost questionnaires, but, unfortunately, there was a low response rate. To estimate the opportunity cost of time, occupation details were used to assume income levels using the New Earnings Survey 2014. 90 When no occupation was listed, the national minimum wage was assumed as a valid cost of leisure time. As data were collected for only a small number of schools, these costs were averaged and applied to other schools for which data were missing.
Sensitivity analysis 4: best-case scenario
Within the trial, not all of the children in each class were included in the study. This was due to parents not consenting their children to be part of the measurement element of the study. As a result, there were children in the class who received the intervention but were not part of the study. On average, there were 17 children with parental consent to undertake measurements in each class. To examine the best-case scenario, sensitivity analysis 4 assumed that all of the children received the intervention and that all classes comprised 30 children. The average cost was, therefore, reduced per child.
Secondary analysis
Cost per ‘case of obesity prevented’
A secondary analysis was conducted to assess the cost-effectiveness of the intervention in terms of cost per ‘case of obesity prevented’. Cases of interest were defined as children who were not obese at baseline but became obese by FU2. That is, if the intervention was effective, fewer children should be transitioning from a non-obese state to an obese state in the intervention arm than in the control arm. To examine this, a transition dummy variable was created to represent whether or not the child had transitioned from a non-obese state to an obese state throughout the duration of the trial. A multilevel logit model including a dummy variable for the intervention was used to assess the impact of the intervention on the likelihood of transitioning to an obese state while controlling for clustering and other relevant covariates. This was implemented within Stata 13 using the ‘melogit’ command, with the school variable being the level 2 identifier.
Results
Impact of intervention on health-related quality of life
Table 30 outlines the response rate for the CHU9D instrument.
| Time point | CHU9D completed, n (%) | Missing (%) | |
|---|---|---|---|
| Control arm | Intervention arm | ||
| Baseline | 1350 (92) | 7 | 9 |
| FU1 | 1215 (83) | 20 | 15 |
| FU2 | 1131 (77) | 25 | 21 |
Table 31 describes the mean utility values at each time point for the whole sample, the control arm and the intervention arm. The mean utility at baseline for all of the children was 0.826. At baseline, the mean utility for the control arm was 0.816 compared with 0.836 for the intervention arm; this difference was adjusted for within the main CUAs. 94
| Measurement time point | All participants: mean (95% CI) | Control arm: mean (95% CI) | Intervention arm: mean (95% CI) |
|---|---|---|---|
| Baseline (n = 1350) | 0.826 (0.818 to 0.833) | 0.816 (0.805 to 0.827) | 0.836 (0.826 to 0.846) |
| FU1 (n = 1215) | 0.863 (0.857 to 0.869) | 0.858 (0.850 to 0.866) | 0.868 (0.858 to 0.877) |
| FU2 (n = 1128) | 0.896 (0.890 to 0.901) | 0.898 (0.891 to 0.905) | 0.893 (0.884 to 0.901) |
Figure 9 shows the CHU9D utility scores only for complete cases (n = 991), for which there was measurement at all three points. The mean utility value for the control arm was statistically significantly (p < 0.05) lower (indicating a poorer quality of life) at baseline than for the intervention arm. By FU2, however, the mean utility value associated with the control arm had increased and slightly superseded the intervention arm.
FIGURE 9.
Mean CHU9D score at each time point (complete cases only).

Examining the impact on quality-adjusted life-years
Table 32 describes the unadjusted mean QALYs for each arm of the trial. At FU2, the intervention group accrued 2.17 QALYs, compared with 2.14 QALYs for the control group. This difference was not significant at the 0.05 significance level, given the way that QALYs are calculated using the ‘area under the curve’ method, and as highlighted in Figure 9, the extra QALYs within the intervention arm are probably due to the large imbalance at baseline.
| Measurement time point | All participants, mean (95% CI) | Control arm, mean (95% CI) | Intervention arm, mean (95% CI) |
|---|---|---|---|
| FU1 (n = 1130) | 1.053 (1.046 to 1.060) | 1.045 (1.036 to 1.055) | 1.063 (1.052 to 1.073) |
| FU2 (n = 995) | 2.154 (2.142 to 2.167) | 2.141 (2.124 to 2.157) | 2.171 (2.152 to 2.189) |
After conducting multiple imputation, the unadjusted QALY estimates remain similar to those pre imputation (Table 33).
| Measurement time point | All participants, mean (95% CI) | Control arm, mean (95% CI) | Intervention arm, mean (95% CI) |
|---|---|---|---|
| FU1 | 1.055 (1.048 to 1.062) | 1.046 (1.038 to 1.055) | 1.064 (1.055 to 1.074) |
| FU2 | 2.153 (2.141 to 2.164) | 2.144 (2.130 to 2.159) | 2.163 (2.145 to 2.180) |
Incremental analysis: effectiveness
Table 34 describes the incremental difference in mean QALYs between the intervention and control group for the data with no adjustment, with adjustment for clustering and baseline differences, and with adjustments for clustering, baseline differences and the prespecified covariates using multilevel multivariate regression.
When controlling for baseline utility, clustering and the covariates, the mean QALY difference for FU1 and FU2 was negligible and insignificant.
| Measurement time point | No adjustment | Adjusted for clustering and baseline utility | Adjusted for clustering, baseline utility and covariates | |||
|---|---|---|---|---|---|---|
| MD (95% CI) | p-value | MD (95% CI) | p-value | Mean (95% CI) | p-value | |
| FU1 | 0.018 (0.005 to 0.031) | 0.006 | 0.005 (–0.008 to 0.017) | 0.461 | 0.005 (–0.008 to 0.018) | 0.429 |
| FU2 | 0.019 (–0.003 to 0.041) | 0.097 | 0.005 (–0.025 to 0.034) | 0.791 | 0.006 (–0.024 to 0.036) | 0.701 |
Of interest, we explored the differences in mean QALYs between the intervention and control groups by trial intervention year. Table 35 outlines the results. The coefficient for incremental QALYs in G1 schools at all follow-up points is positive, indicating that more QALYs were attained in the intervention group than in the control group. In contrast, however, the corresponding coefficient for G2 schools is negative, indicating the opposite effect, namely that fewer QALYs were attained in the intervention group than in the control group.
| Incremental QALYs for the intervention group by group (adjusted for clustering, baseline utility and covariates) | ||||
|---|---|---|---|---|
| Measurement time point | G1 | G2 | ||
| MD (95% CI) | p-value | MD (95% CI) | p-value | |
| FU1 | 0.016 (0.000 to 0.034) | 0.65 | –0.006 (–0.022 to 0.010) | 0.463 |
| FU2 | 0.039 (–0.002 to 0.079) | 0.06 | –0.026 (–0.063 to 0.010) | 0.164 |
Resource use and costs
Details of all resource use and costs for the intervention group are displayed in Tables 36–38. Compared with the running costs, the set-up and development costs of the intervention were relatively low. In terms of the set-up costs, the largest component of cost was the time attributed to research staff developing materials for the intervention, in particular the development of the cooking workshop and classroom materials. The largest cost driver for implementing the intervention related to the time of the teaching staff and the cost of staff cover for attending the training sessions. Other significant costs related to the creation of the signposting materials and the purchasing of the PA packages. The ongoing running/delivery costs had the biggest impact on the overall costs of the intervention. Of the main components of the intervention, in terms of delivery, the cheapest by far was the signposting. The most expensive component of the trial was the Villa Vitality sessions, which accounted for over half of the running costs.
Set-up/development costs
| Component | Resource type | Resource use per class (SD)a | Mean cost per class, £ (SE) |
|---|---|---|---|
| Intervention handbook development | Staff time (hours) | ||
| Professor | 0.025 | 1.11 | |
| Senior research fellow | 0.025 | 0.81 | |
| Research fellow | 0.15 | 2.78 | |
| Printing handbooks | |||
| Number of handbooks | 2.5 | 11.47 | |
| Intervention set-up meeting (researcher visit to school) | Staff time (hours) | ||
| Research fellow travel/meeting time | 1.014 (0.647) | 18.79 (1.896) | |
| Teacher meeting time | 0.324 (0.133) | 6.53 (0.423) | |
| Travel costs (miles) | |||
| Mileage | 18.6 (19.39) | 8.37 (1.38) | |
| Development of cooking workshop/classroom materials | Staff time | ||
| Research associate | 6.5 | 107.12 | |
| Research fellow | 1.75 | 32.45 | |
| Preparing trainers for central training session | Staff time (hours) | ||
| Research associate | 0.325 | 5.36 | |
| Research fellow | 0.2 | 3.71 | |
| Adapting Villa Vitality for children aged 6–7 years | Staff time (hours) | ||
| Senior research fellow | 0.125 | 4.06 | |
| Research fellow | 0.25 | 4.64 | |
| Research associate | 0.25 | 4.12 | |
| Preparing Villa Vitality teacher packs and liaising with schools | Staff time (hours) | ||
| Research associate | 1.5 | 24.72 | |
| Total mean set-up/development cost per school (£) | 363.14 | ||
| Total mean set-up/development cost per class (£) | 236.04 | ||
| Total mean set-up/development cost per consented child (£) | 13.70 | ||
| Total mean set-up/development cost per intervention child, assuming a class size of 30 pupils (£) | 7.87 | ||
Implementation costs
| Component | Resource type | Resource use per class (SD)a | Mean cost per class, £ (SE) |
|---|---|---|---|
| Cooking workshop central training costs (teacher training to deliver cooking workshops) | University costs | ||
| Staff time (hours) | |||
| Research associate | 1.2 | 19.78 | |
| Research fellow | 0.6 | 11.12 | |
| Materials | |||
| Two sessions, each estimated as the cost of one breakfast, lunch and dinner workshop (£40.95); thus, £81.90 for both, then divided back through the number of classes attended to get cost per class | n/a | 2.04 | |
| School/participant costs | |||
| Staff time (hours) | |||
| Teacher attendance time | 3.8 (3.3) | 76.36 (12.13) | |
| TA attendance time | 3.2 (3.14) | 28.93 (5.19) | |
| Travel costs | |||
| Travel costs (£) | 12.49 (2.47) | ||
| TA travel time (hours) | 1.15 (1.45) | 10.42 (2.39) | |
| Teacher travel time (hours) | 1.26 (1.31) | 25.37 (4.79) | |
| Teacher cover costs | |||
| Cost of cover | n/a | 116 (18.79) | |
| Special dependant arrangements (£) | n/a | 1.44 (1.27) | |
| PA packages | PA packages | ||
| Activate | 0.51 (19 packs total) | 142.55 | |
| Take 10 | 0.46 (17 packs total) | 23.80 | |
| Wake Up Shake Up | 0.32 (12 packs total) | 8.47 | |
| Positive Play | 0.43 (16 packs total) | 37.66 | |
| Total mean implementation cost per school (£) | 794.49 | ||
| Total mean implementation cost per class (£) | 516.42 | ||
| Total mean implementation per consented child (£) | 29.98 | ||
| Total mean implementation cost per child assuming a class of 30 pupils (£) | 17.21 | ||
Ongoing/intervention delivery costs
| Component | Resource type | Annual resource use per class (SD)a | Mean cost per class, £ (SE) |
|---|---|---|---|
| Development/updating of generic signposting for schools | Staff time (hours) | ||
| Research associate | 1.525 | 25.13 | |
| Development/updating of school specific signposting | Staff time (hours) | ||
| Study administrator | 0.938 | 10.94 | |
| Research associate | 4.8 | 70.86 | |
| Signposting (delivery) | Generic printing | ||
| Printing | 38.75 | 8.88 | |
| School-specific printing | |||
| Printing | 38.81 (17.71) | 14.38 (1.39) | |
| Delivery | |||
| Cost of delivery | n/a | 2.94 | |
| Villa Vitality | Package | ||
| Villa Vitality package | 1 | 1979.66 | |
| Villa Vitality day 1 | |||
| Teacher time | 8.88 (4.33) | 178.48 (17.75) | |
| TA time | 11.65 (5.06) | 105.28 (9.34) | |
| Villa Vitality school visit | |||
| Teacher time | 6.77 (2.12) | 135.94 (9.1) | |
| TA time | 5.61 (4.72) | 50.75 (9.10) | |
| Villa Vitality day 2 | |||
| Teacher time | 7.79 (3.12) | 156.57 (12.80) | |
| TA time | 11.58 (5.14) | 104.71 (9.48) | |
| Villa Vitality class project and challenges | |||
| Teacher time | 8.17 (6.61) | 164.11 (132.81) | |
| Cooking workshop | Cooking workshop classes: breakfast | ||
| Teacher time | 1.53 (1.05) | 30.72 (4.71) | |
| TA time | 0.40 (0.22) | 3.61 (1.98) | |
| Cooking workshop classes: lunch | |||
| Teacher time | 1.43 (0.83) | 28.76 (4.05) | |
| TA time | 0.25 (0.58) | 2.26 (1.28) | |
| Cooking workshop classes: dinner | |||
| Teacher time | 1.22 (1.31) | 24.44 (6.81) | |
| TA time | 0.2 (0.527) | 2.26 (1.51) | |
| Cooking workshop: breakfast | |||
| Teacher time | 2.13 (0.94) | 42.79 (4.21) | |
| TA time | 0.31 (1.00) | 2.83 (2.03) | |
| Staff helpers | 2.84 (1.91) | 25.69 (3.86) | |
| Cooking workshop: lunch | |||
| Teacher time | 2.08 (1.07) | 41.86 (5.22) | |
| TA time | 0.18 (0.50) | 1.60 (1.09) | |
| Staff helpers | 2.06 (1.02) | 18.66 (2.24) | |
| Cooking workshop: dinner | |||
| Teacher time | 1.73 (1.13) | 34.66 (7.20) | |
| TA time | 0.25 (0.53) | 2.26 (1.51) | |
| Staff helpers | 1.43 (1.65) | 12.96 (4.71) | |
| Cooking workshop packing/purchasing | |||
| Research fellow | 0.3 | 5.56 | |
| Research associate | 0.9 | 14.83 | |
| Study administration | 0.1 | 1.17 | |
| Cooking workshop printing materials | |||
| Printing | n/a | 100.09 | |
| Cooking workshop delivering materials | |||
| Research associate time breakfast | 0.79 (0.61) | 12.95 (2.26) | |
| Breakfast travel costs | n/a | 10.29 (2.36) | |
| Research associate time lunch | 0.80 (0.67) | 13.16 (2.68) | |
| Lunch travel costs | n/a | 10.39 (2.65) | |
| Research associate time dinner | 0.95 (0.72) | 15.71 (3.76) | |
| Dinner travel costs | n/a | 12.98 (4.19) | |
| Cooking workshop materials: breakfast | |||
| Raisins | 7.25 | 2.58 | |
| Tinned pineapple | 4 | 1.37 | |
| Weetabix | 1 | 2.33 | |
| Bran flakes | 1 | 1.80 | |
| Chopping boards | 7.25 | 4.96 | |
| Knives | 28.5 | 0.46 | |
| Spoons | 35 | 0.57 | |
| Bowls | 35 | 3.42 | |
| Kitchen towels | 1 | 0.34 | |
| Archive box | 1 | 1.29 | |
| Perishables | 1 | 6.35 | |
| Cooking workshop materials: lunch | |||
| Tuna | 5 | 3.52 | |
| Sweetcorn | 3 | 1.46 | |
| LF salad cream | 0.6 | 0.57 | |
| Bowls | 20 | 1.95 | |
| Spoons | 20 | 0.33 | |
| Kitchen rolls | 2 | 0.67 | |
| Cooking workshop materials: dinner | |||
| Couscous | 1 | 0.68 | |
| Tinned beans | 2 | 0.59 | |
| Sweetcorn | 2 | 0.98 | |
| Vegetable stock | 1 | 0.98 | |
| Kitchen rolls | 1 | 0.34 | |
| Spoons | 30 | 0.49 | |
| Bowls | 30 | 2.93 | |
| PA | PA term 1 | ||
| Teacher time | 11.12 (6.70) | 223.44 (31.72) | |
| TA time | 1.35 (3.40) | 12.25 (7.26) | |
| LTS time | 2.16 (4.15) | 16.74 (7.59) | |
| PA term 2 | |||
| Teacher time | 17.35 (10.99) | 348.60 (47.09) | |
| TA time | 0.48 (0.98) | 4.38 (1.89) | |
| LTS time | 4.21 (7.57) | 27.14 (11.85) | |
| PA term 3 | |||
| Teacher time | 18.90 (12.63) | 379.88 (73.27) | |
| TA time | 0.32 (0.64) | 2.93 (1.66) | |
| LTS time | 6.50 (12.40) | 50.38 (27.74) | |
| Total mean running cost per school (£) | 7058.19 | ||
| Total mean running cost per class (£) | 4587.82 | ||
| Total mean running cost per consented child (£) | 266.35 | ||
| Total mean running cost per child assuming a class of 30 pupils (£) | 152.93 | ||
Missing cost data
For all of the components of the intervention for which the resource use data were collected by the research team, there were no missing data. For much of the intervention, however, the cost data were collected from logbooks and there were extensive missing data. Some teachers failed to complete the logbooks, citing time constraints; other logbooks were returned, but without completion of the requested cost data; some logbooks were completed but lost by the school; and other logbooks were reported to have been returned but were never received. Given the multifaceted nature of the intervention, there were large numbers of missing data (Table 39).
| Intervention cost subcomponent | Missing data (%) |
|---|---|
| Intervention handbook development and set-up | 0 (collected by trial team) |
| Development and preparation for cooking workshop central training | 0 (collected by trial team) |
| Adapting Villa Vitality materials and developing Villa Vitality packs | 0 (collected by trial team) |
| Cooking workshop central training | 26 |
| Development of signposting materials | 0 (collected by trial team) |
| Signposting printing and postage | 0 (collected by trial team) |
| PA and Villa Vitality package costs | 0 (collected by trial team) |
| PA term 1 | 55 |
| PA term 2 | 45 |
| PA term 3 | 70 |
| Cooking workshop and classes: breakfast | 52.5 |
| Cooking workshop and classes: lunch | 57.5 |
| Cooking workshop and classes: dinner | 75 |
| Villa Vitality day 1 | 40 |
| Villa Vitality class project and challenges | 47.5 |
| Villa Vitality: school visit | 45 |
| Villa Vitality day 2 | 40 |
The high levels of missing data for both costs and QALYs provide a strong case for using multiple imputation.
Incremental analysis of cost
Multiple imputations (30 imputations) were run for each subcomponent of cost, and these were then combined to calculate the total costs of the intervention. Therefore, the analysis of cost was conducted on 30 data sets.
Table 40 outlines the incremental costs of the intervention arm compared with the control arm after adjusting for clustering, baseline utility and the covariates. Unsurprisingly, given the assumed ‘no costs’ associated with the control arm, the intervention arm was statistically significantly more expensive than the control arm.
| No adjustment | Adjusted for clustering | Adjusted for clustering, baseline utility and covariates | |||
|---|---|---|---|---|---|
| MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value |
| 262.57 (254.98 to 270.16) | 0.000** | 267.24 (240.22 to 294.25) | 0.000** | 267.39 (240.64 to 294.14) | 0.000** |
Cost–utility analysis
The CUA combines the incremental costs with the incremental QALYs to produce an ICER. The ICER associated with the base case is £46,083 per QALY and, thus, the intervention is not cost-effective. Through the net benefit framework it is possible to assess the uncertainty around the ICER, while also considering clustering and the correlation between costs and outcomes. Given the very small effect size, and the uncertainty around the effect size, it is unsurprising to find extremely large levels of uncertainty around the ICER. At the NICE-recommended willingness-to-pay (WTP) threshold of £20,000–30,000 per QALY, the control arm is more likely to be cost-effective than the intervention arm. At the lower threshold of £20,000 per QALY, there is just a 30% chance that the intervention is more cost-effective than usual practice. Even at a WTP threshold of £100,000 per QALY, the intervention arm has only a 59% chance of being the more cost-effective option. The reason underlying this uncertainty can be attributed to the lack of effect of the intervention. As the effect size approaches zero, the CIs around the net benefit widen.
Figure 10 shows the net benefits associated with the intervention at different levels of WTP. As the WTP threshold increases, the CIs widen, showing the increasing levels of uncertainty.
FIGURE 10.
Net benefit of intervention at differing WTP levels.

This is reflected in the CEAC (Figure 11), which shows the probability of the intervention being cost-effective at different levels of WTP for a QALY. Owing to the negligible treatment effect, even at high levels of WTP per QALY there is only a slightly better than 50 : 50 chance that the intervention is the more cost-effective option.
FIGURE 11.
Cost-effectiveness acceptability curve.
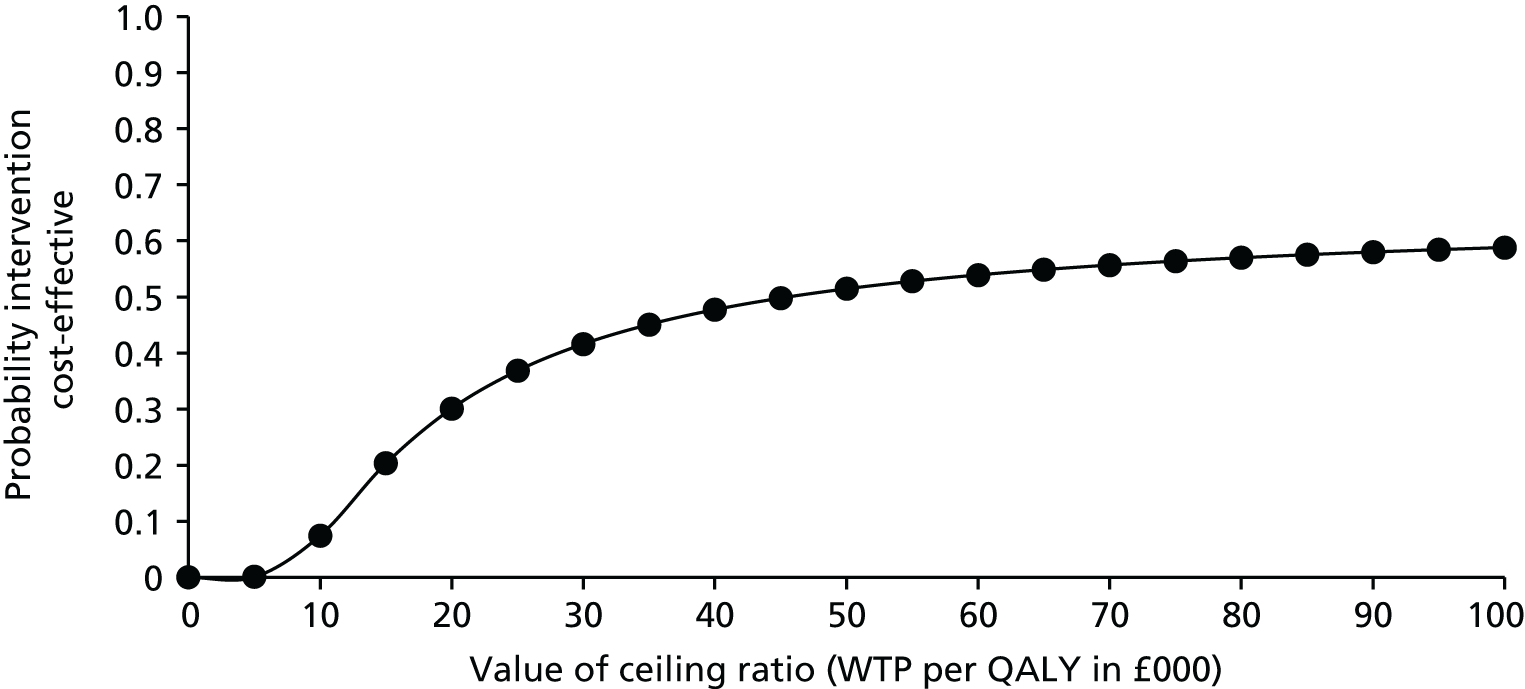
Sensitivity analysis
Sensitivity analysis 1: different multiple imputation method
When an alternative imputation strategy that utilised a fixed effect for clusters was applied, there was little impact on the results (Table 41). The overall ICER reduced to just under £42,000 per QALY; however, the estimates remained extremely uncertain, given the small and inconsistent effect size. This is reflected in the CEAC shown in Figure 12.
| Mean (95% CI) | p-value |
|---|---|
| 0.006 (–0.024 to 0.037) | 0.683 |
FIGURE 12.
Cost-effectiveness acceptability curve with alternative fixed-effect imputation strategy.
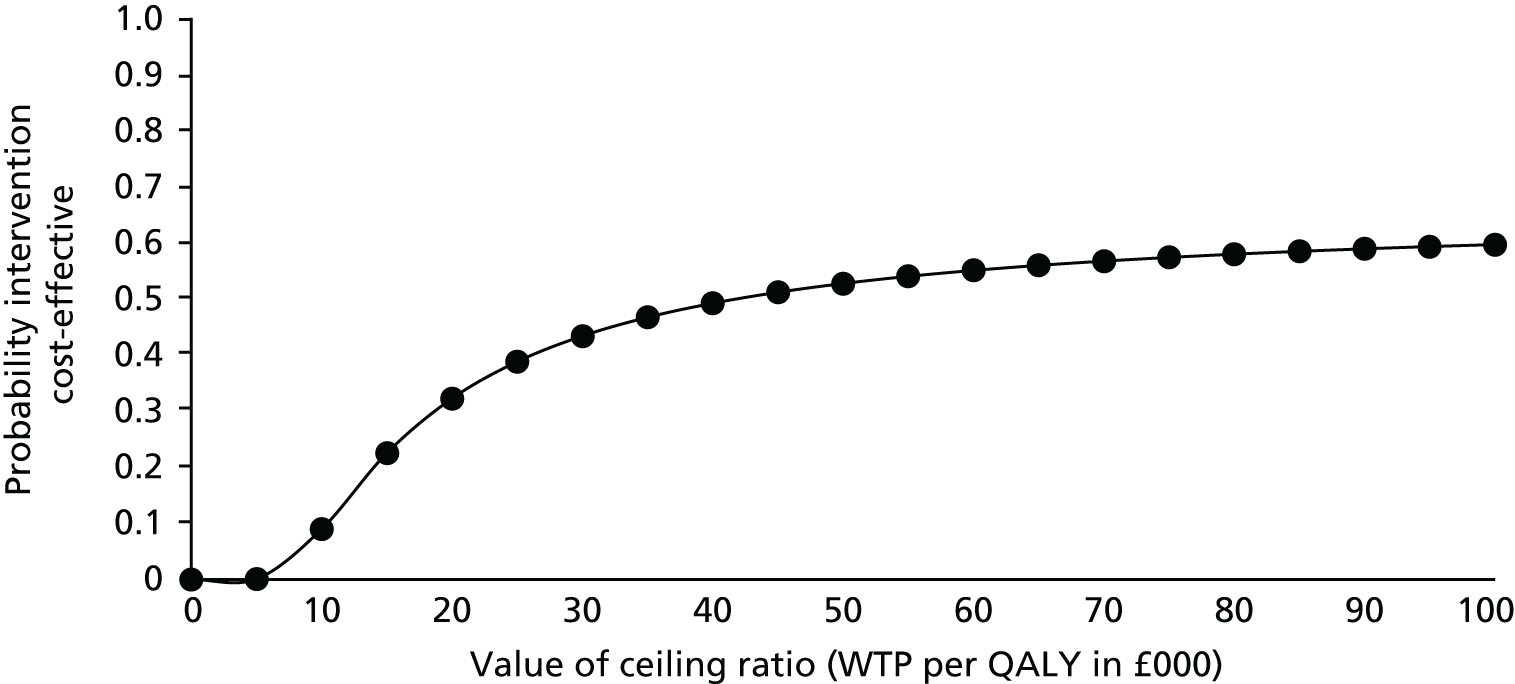
Sensitivity analysis 2: including set-up and implementation costs
As expected, the inclusion of set-up and implementation costs led to an increase in the ICER associated with the intervention and an even less favourable CEAC. The addition of the set-up and implementation costs increased the mean costs by £43.66, increasing costs to £311.07 per child. This increase in cost had a notable impact on the ICER, increasing the ICER to £53,610 per QALY.
The CEAC (Figure 13) shows the impact of the higher levels of cost moving the CEAC downwards, especially at the lower levels of WTP than with the base-case analysis. Again, because of the lack of effect of the intervention, there is a great deal of uncertainty surrounding the results.
FIGURE 13.
Cost-effectiveness acceptability curve: including set-up and implementation costs.
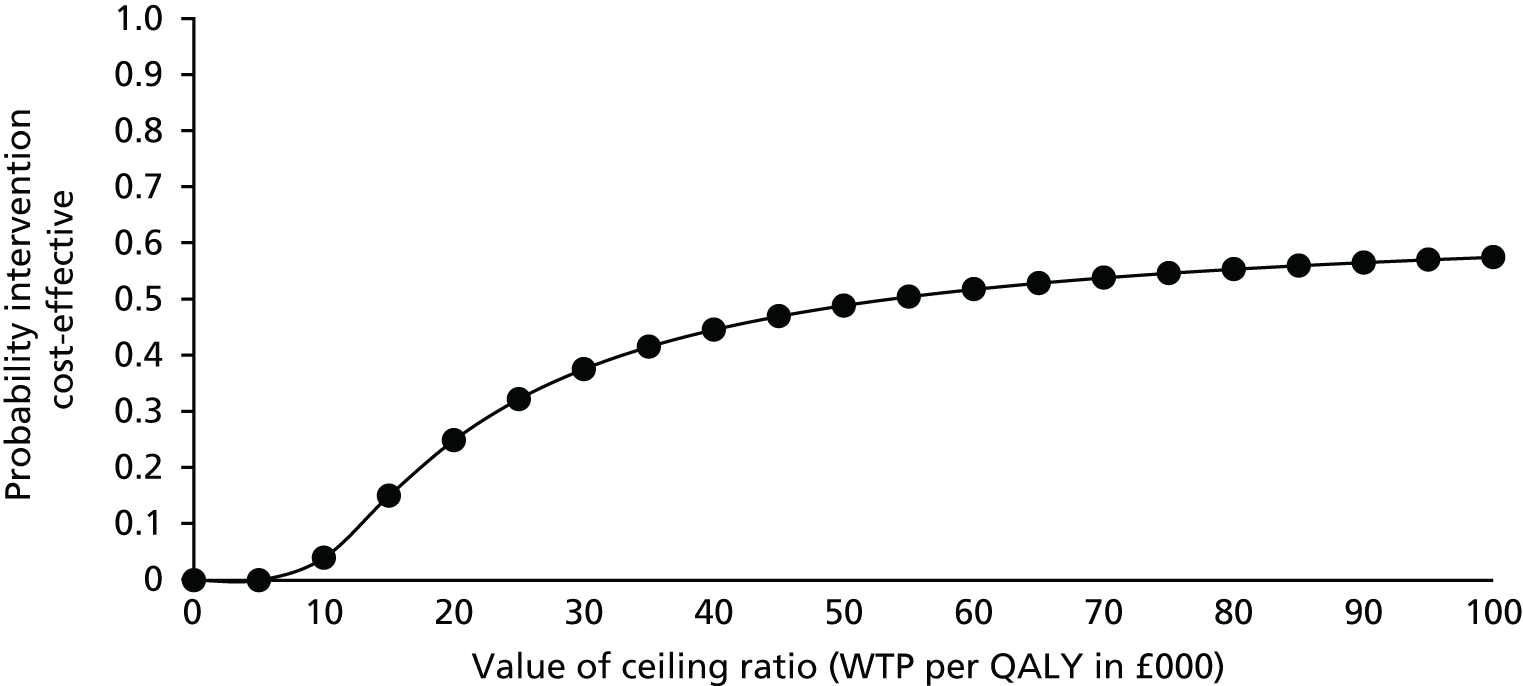
Sensitivity analysis 3: including wider costs
As with sensitivity analysis 2, the inclusion of wider costs results in the ICER rising to just under £52,000 per QALY. As shown by the CEAC in Figure 14, there was little chance that the intervention is cost-effective. At a WTP of £20,000 per QALY, there is just a 26% chance that the intervention is more cost-effective than usual care. When wider costs are considered, the intervention remains not cost-effective.
FIGURE 14.
Cost-effectiveness acceptability curve: including wider costs.

Sensitivity analysis 4: best-case scenario
In this scenario it is assumed that there are 30 children in every class; therefore, the cost has reduced to £155.53 per child. This produced a more favourable cost-effectiveness result, with the ICER falling to approximately £26,804 per QALY. Although this would be borderline cost-effective, it is again important to note the uncertainty around this best-case estimate, as demonstrated in the CEAC in Figure 15. Again, because of the lack of treatment effect within the trial, there is a great deal of uncertainty surrounding all cost-effectiveness results. Even at a WTP of £100,000 per QALY, there would be only a 62% probability that the intervention is more cost-effective than usual care.
FIGURE 15.
Cost-effectiveness acceptability curve: best-case scenario.

Cost per obesity case prevented
The purpose of the intervention is to prevent obesity and it is therefore important to consider the intervention in terms of its success at preventing children transitioning to an obese state. In the control arm, 7% of the children transitioned to an obese health state at FU2, having been in a non-obese state at baseline. In contrast, 10% of those in the intervention arm transitioned into an obese state in the intervention arm. That is, more children in the intervention arm transitioned into an obese state than those in the control arm. This is reflected by the results of the multilevel logit model. To demonstrate the lack of effect of the intervention, the odds ratio associated with children in the intervention arm transitioning into an obese state is 1.17 (95% CI 0.66 to 2.09) when controlling for covariates. This indicates that those in the intervention arm are more likely to transition into an obese state than those in the control arm. It should be noted, however, that this is not a significant difference. This negative finding, however, makes it impossible to assess the cost per obesity case prevented as a result of there being zero cases of obesity prevented by the intervention. These results reflect the primary trial analysis of the health outcomes data, which indicates that there was no notable impact of the intervention on clinical outcomes.
Conclusion
The economic evaluation has summarised the methods and results for capturing both the incremental costs that were associated with the intervention and the incremental effectiveness. The economic evaluation analysed both costs and benefits jointly using the NBR framework. In terms of costs, the intervention costs were largely driven by the Villa Vitality package and school staff time for delivering the intervention. With respect to the analysis of effectiveness and cost-effectiveness, the main result is the lack of intervention effect in terms of QALY gain or in terms of obesity prevention. The economic evaluation suggests that the intervention, despite its relatively low cost on a per-child basis, has negligible benefits, and thus fails to demonstrate cost-effectiveness. When considering the uncertainty surrounding the ICERs, the lack of treatment effect becomes apparent and a great deal of uncertainty underlies the apparent cost-effectiveness. Consequently, even when considering a particularly high WTP threshold for QALYs, and a reduced intervention cost as in sensitivity analysis 4, there is still a vast amount of uncertainty about whether or not the intervention would be deemed cost-effective.
A number of challenges were encountered within the economic evaluation, which included dealing with clustering, and also missing data. Clustering was largely accounted for within the analysis by implementing multilevel imputation and analysis models. The second of these challenges, that is, the missing data, proved to be a significant limitation. In terms of effectiveness data, follow-up rates were good and the level of attrition throughout the follow-up periods was typical for a trial. For the cost data, however, missing data were a much more significant challenge. This largely relates to the methods of resource use collection. Resource use as recommended by best practice was collected alongside the trial. Collection of many of the resource use data was through teacher logbooks, which varied by component. Given the multifaceted nature of the intervention, and the consequently large number of cost components, it is perhaps unsurprising that missing cost data were pervasive throughout. Consequently, a complete-case analysis would have removed nearly every single child from the analysis. Multiple imputation, as recommended in the literature, was therefore necessary to address this and to make best use of the data.
This was a trial-based economic evaluation and, thus, health-care costs were not considered, as any potential health-care usage from being obese would occur well into the future. Had the intervention been effective in preventing obesity, it would have been possible to model future cost savings and health improvements using a decision-analytic modelling approach. A direct result of the lack of effectiveness of the intervention was that this modelling stage was, unfortunately, not required.
Chapter 8 Discussion
Summary of findings
The WAVES study is one of the largest cluster randomised controlled trials of childhood obesity prevention to date, with a sufficient sample size to ascertain the effectiveness of the intervention on BMI-z and incorporating a cost-effectiveness analysis.
In terms of our primary outcomes, we found no evidence of a significant intervention effect on BMI-z at 3 and 18 months after the end of the intervention period (although the direction of effect favoured the intervention). There were also no consistent intervention effects on any of the secondary anthropometric, behavioural, clinical or psychological outcomes. However, in the subgroup of participants who underwent a third follow-up at 27 months (G1 schools), there was a statistically significant and clinically important difference in BMI-z in favour of the intervention (MD –0.204, 95% CI –0.396 to –0.013 in the partially adjusted model and MD –0.177, 95% CI –0.336 to –0.017 in the fully adjusted model). There was no statistically significant intervention effect for the other anthropometric measures, although the direction of effect for some favoured the intervention. There was no significant difference between the trial arms in terms of quality of life, self-perception or body image dissatisfaction, suggesting that there was no evidence of harm from the intervention.
Alongside the trial, an economic evaluation provided evidence on the cost-effectiveness of the intervention compared with no intervention. A trial-based CUA, based on outcome of cost per QALY, was conducted. Using the CHU9D, at 18 months post intervention the incremental cost-effectiveness of the intervention compared with no intervention was £46,083 per QALY (or £26,804 per QALY for the best-case scenario, taking into account all of those who received the intervention, rather than just those who consented to measurements). The intervention is therefore not cost-effective using NICE-recommended WTP threshold of £20,000–30,000 per QALY. This is mainly a result of the lack of intervention effect in terms of QALY gains, which led to a high level of uncertainty around the ICERs.
Subgroup effects
In terms of sociodemographic and clinical subgroups, we found no consistent pattern suggesting heterogeneity of treatment effects by sex, household level of deprivation or baseline weight status. There was a statistically significant effect in favour of the intervention for most anthropometric measures in children from the black African Caribbean ethnic subgroup in the fully adjusted models at FU1 and FU2. There was an inconsistent pattern in relation to behavioural outcomes in this subgroup, but the intervention group had lower levels of PA and consumed fewer portions of fruit and vegetables at FU2 than the control group. Such an effect was not seen in any other ethnic subgroup. We considered the credibility of this finding representing a true subgroup effect, based on recommended criteria (Table 42). 99 Although this was a prespecified subgroup analysis that fulfilled the design criteria, there was no significant interaction effect, and the contextual evidence to support such a finding is mixed. The relatively small size of this subgroup also makes interpretation more complex. Therefore, on balance, it is possible, but uncertain, that the intervention was effective only in this subgroup.
| Credibility criteria considered | Assessment outcome |
|---|---|
| Design | |
| Was the subgroup variable a baseline characteristic? | Yes |
| Was the subgroup variable a stratification factor at randomisation? | Yes |
| Was the subgroup hypothesis specified a priori? | Yes |
| Was the subgroup analysis one of a small number of subgroup hypotheses tested (≤ 5)? | Subgroups: sex, household deprivation (IMD), baseline weight status and ethnicity |
| Analysis | |
| Was the test of interaction significant (interaction p < 0.05)? | No |
| Was the significant interaction effect independent, if there were multiple significant interactions? | No |
| Context | |
| Was the direction of subgroup effect correctly prespecified? | Yes |
| Was the subgroup effect consistent with evidence from previous related studies? | Somewhat |
| Was the subgroup effect consistent across related outcomes? | Yes |
| Was there any indirect evidence to support the apparent subgroup effect, for example biological rationale, laboratory tests, animal studies? | Theoretical evidence of potential heterogeneity by ethnicity. No supportive evidence from process evaluation |
Overall, there was no evidence of the intervention resulting in inequity and it was unlikely that there was a differential effect of the intervention in the black African Caribbean subgroup.
In view of the BMI-z results at FU3, a post hoc exploratory analysis was undertaken to compare intervention effects between G1 and G2 schools. This showed a statistically significant effect in the fully adjusted models for BMI-z in favour of intervention at FU1 (–0.23, 95% CI –0.34 to –0.12) and FU2 (–0.17, 95% CI –0.34 to 0.00) in the G1 schools, which was maintained at FU3 (–0.20, 95% CI –0.40 to –0.01). In G2 schools, there were non-significant differences between arms, with the direction of effect favouring the control (0.08, 95% CI –0.09 to 0.25 at FU1; and 0.09, –0.04 to 0.22 at FU2). This was not a prespecified analysis and should, therefore, be interpreted with caution. Credibility of a genuine subgroup effect is suggested by the following:
-
significant interaction between group and the treatment arm
-
consistency in terms of direction of effect for most anthropometric measures
-
consistency of direction and size of effect at all follow-up periods
-
significant difference in mean BMI-z at baseline between G1 and G2 schools.
Although mean BMI-z was very similar at baseline between the trial arms in G1 schools, there was a large baseline imbalance in G2 schools, with greater BMI-z in the intervention arm than in the control arm. This may be an explanation for the observed difference in effect between the two groups of schools.
However, other factors suggest that this observation may not be a genuine subgroup effect:
-
The analysis was not specified a priori.
-
Taken together with the prespecified subgroup analyses, there were five categories of subgroup hypotheses that have been tested (with a total of 11 variables).
-
There was no consistency of effect in terms of behavioural outcomes.
On balance, there is a possibility of a genuine subgroup effect.
Strengths and limitations
The WAVES study addresses many of the limitations that have been identified in previous childhood obesity prevention trials.
Design
We used a cluster randomised control design to take account of clustering at school level, with a sufficiently large sample to provide sufficient power for assessment of the primary outcomes. The participating schools and children were sampled to represent a wide range of ethnicities and socioeconomic backgrounds. This allowed consideration of subgroup effects in the analysis. Full allocation concealment was achieved by undertaking all of the baseline measurements prior to randomisation.
Intervention
The intervention was developed in a phased and rigorous way, using the MRC framework for complex interventions as a guide,56,57 and following a successful feasibility trial. 52 The final multicomponent intervention package included many of the elements identified as promising in systematic reviews,18,19 and incorporated a range of behaviour change techniques, including four that were most associated with positive outcomes in previous childhood obesity prevention trials (prompt generalisation of behaviour, practice, model behaviour and goal-setting). 100
Outcome assessment
The outcomes were assessed with mainly objective measurements, using validated instruments and standardised protocols. In addition to BMI-z, we undertook a range of anthropometric measurements to account for reported limitations of using BMI in children. Dietary and PA levels were objectively assessed using validated instruments, which is a strength compared with subjective measurements in many previous trials. Loss to follow-up was relatively small, with 79% of pupils retained to the second follow-up, and the loss of one school.
Data analysis
We had a prespecified analysis plan, we took account of clustering in the analysis, and the findings were robust to a range of sensitivity analyses.
Long-term follow-up
This was one of few trials that undertook longer-term follow-up to assess whether or not any intervention effects would be sustained. This longer-term follow-up was important in helping to interpret the findings, as we have shown a consistent magnitude of effect in terms of difference in BMI-z between intervention and control arms in G1 schools.
Process evaluation
A detailed process evaluation was undertaken alongside the trial, and this has helped to contextualise the findings and interpret the results.
Economic analysis
The WAVES study was the first trial of childhood obesity prevention that incorporated an economic analysis alongside the study. Nevertheless, there were also a number of limitations.
The block balancing algorithm to allocate schools to intervention or control arm was based on data at school (cluster) level. However, within clusters, only children from one year group were eligible for the trial, and, among those eligible, just over half consented to study measurements. There was baseline imbalance between the arms in relation to the outcome of interest and, although the primary analysis adjusted for baseline measures, this may have not fully accounted for the imbalance. Such baseline imbalance is a known limitation of cluster trials and can best be overcome with recruitment of larger numbers of clusters. 101–103
The fact that consent for study measurements was obtained for only 60% of eligible pupils means that there is the potential for selection bias. However, the comparison of demographic characteristics between consented and non-consented pupils showed only small differences in relation to ethnicity and deprivation.
Intervention delivery was variable, with two schools failing to deliver any, and some only partially delivering, components. However, a subgroup analysis by implementation fidelity did not show any evidence of subgroup effect. Although follow-up to 18 months was in all groups, longer-term follow-up (to 27 months) was limited to a subset of participating schools, which limits interpretation. At each follow-up time point there was loss to follow-up, with the potential introduction of follow-up bias. The proportion of participants without primary outcome data at follow-up for those included in the measurement time point and with baseline primary outcome data available was 14%, 21% and 25% at FU1, FU2 and FU3, respectively. It is worth noting, however, that the majority of this loss to follow-up was a result of either school dropout (one G2 school, 20 participants with baseline primary outcome data) or participants having changed school between baseline measurements and follow-up. The proportions lost to follow-up for either consent withdrawal or not being available at school on the day of measurement were relatively small (4%, 5% and 7% for FU1, FU2 and FU3, respectively). A comparison has been undertaken of pupil-level demographic and weight status characteristics for those with baseline primary outcome data who also had follow-up data with those who were lost to follow-up at each time point. Although, with the exception of sex, there are some differences between those with and those without follow-up data, in general the differences are relatively small, with inconsistency in characteristics between the three follow-up time points.
In terms of weight status (non-overweight vs. overweight/obese) there was very little difference in proportions at FU1 or FU2 (proportion at least overweight, follow-up data available vs. lost to follow-up: 21% vs. 22.1% and 22.0% vs. 22.2%, at FU1 and FU2, respectively). However, at FU3, those lost to follow-up were less likely than those successfully followed up to be overweight or obese (19% vs. 22.5%).
With regard to ethnicity at both FU1 and FU2, those lost to follow-up were less likely than those retained to be white (FU1 40.6% vs. 45.9, FU2 42.6% vs. 45.9%) or South Asian (FU1 26.2% vs. 30.9%, FU2 24.6% vs. 31.8%) and more likely to be black (FU1 11.2% vs. 7.5%, FU2 12.5% vs. 6.9%) or in the other ethnic group category (FU1 21.9% vs. 15.6%, FU2 20.4% vs. 15.4%). A similar pattern was observed at FU3 for the South Asian (19.7% vs. 27.2%), black (11.6% vs. 6.4%) and other (17% vs. 14.8%) ethnic groups, but there was no difference in the proportion who were white between those with and those without follow-up data.
The final characteristic considered was deprivation. There were no consistent patterns in terms of deprivation among those who were successfully followed up compared with those lost to follow-up at the different time points. The analysis did consider subgroup effects, but the sample size for subgroup analysis was insufficient to detect anything other than larger effects. Furthermore, the prespecified ethnic subgroups were heterogeneous themselves. Smaller subgroup effects, therefore, cannot be dismissed.
Assessment of behavioural outcomes
Dietary intake was assessed objectively and data were collected prospectively using average portion sizes that were specific to the child’s age and sex. This reduced the potential for recall bias and the need for weighing food. The CADET provided a quick, easy to administer tool, requiring minimal training and having a relatively low respondent burden. However, as the dietary intake estimate is based on only one weekday record of consumption, it may not be reflective of habitual intake. As with any dietary assessment tool there also a risk of misreporting104 and there may have been seasonal variation105 between the baseline and follow-up data collection periods. Furthermore, adaptations to the CADET to align it to MW730 and smooth anomalous portion sizes may have undermined the validation of this tool. In addition, there were two important considerations. First, the CADET was a written tool and, therefore, if English literacy was an issue, completing the record correctly may have been problematic. However, in an attempt to reduce the impact of this, participants were provided with an instructional DVD on how to complete the CADET booklet. This information was also available online. Second, the CADET was developed to capture foods that were typically consumed in the UK. Although there was an attempt to represent some foods that may be consumed in other cultures, this was limited and, therefore, it may have been difficult to accurately complete the record if the participant consumed a non-Western diet. Despite these limitations, we achieved useable data from ≈ 89% of children at both follow-up points. This is much higher than the completion rate for dietary assessment in our feasibility study52 and similar to that reported in other studies in children. 106,107
Physical activity assessment was also objective, and we aimed to obtain data over 5 days including a weekend. However, not all of the children were compliant, and usable data were available for 69.4% at FU1 and 61.1% at FU2. This is higher than or similar to the rates achieved in other similar studies. 106,108
Comparison with other studies
Our findings build on the findings of previous reviews by addressing a number of important weaknesses in previous randomised controlled trials of childhood obesity prevention. Two major systematic reviews suggested that there was moderate19 to strong18 evidence of effectiveness of school-based interventions in preventing childhood obesity. Nevertheless, both reviews acknowledged study heterogeneity, the variable quality of included studies and the lack of longer-term follow-up as limiting factors in the interpretation. A meta-analysis included in the Cochrane review18 showed that the summary magnitude of effect in terms of BMI-z from pre to post intervention relative to the change in the control group was –0.15 units. This was smaller than the effect size that was used for estimating sample size for our trial. Nevertheless, the WAVES study was larger than most of the 31 previous obesity prevention trials in primary school children that were included in the meta-analysis (sample size of individuals in included studies = 30–1807) and substantially larger than the 21 studies considered to have a low risk of bias (n = 9–574). Furthermore, many of these previous trials had not taken account of the clustered nature of the data during analysis.
Despite the methodological limitations of many of the previous trials, the summary effect size of 0.15-unit difference in BMI-z between intervention and control groups is relatively small. Previous studies have shown that a reduction in BMI-z of 0.25 units is associated with improved cardiometabolic risk in obese adolescents. 53 Nevertheless, even smaller reductions of 0.15 units,109 or even of 0.1 units (equivalent to 0.5 kg in body weight for an average 10-year-old boy),110 have also been shown to be associated with important measurable health benefits. Given the trend of increasing obesity with increasing age and over time, such small reductions in BMI-z at a population level are, therefore, clinically important.
Since the publication of the reviews, findings have become available from another well-conducted, large, school-based cluster randomised controlled trial in the UK. 106 The Active for Life Year 5 intervention was adapted from a promising programme that had been developed and evaluated in the USA, which included training of teachers, provision of lessons to children in school year 5 (aged 9–10 years) and interactive homework that involved parents. The primary aim was to increase PA levels, reduce sedentary time and improve fruit and vegetable intake in the target group. This large trial, which included > 2000 children from 60 schools, found no evidence of an intervention effect immediately after the end of the 1-year intervention period. There was also no effect on weight-related secondary outcome measures.
Findings from a more ambitious European community- family- and school-based intervention programme aimed at childhood obesity prevention were also recently reported. 111 The 2-year intervention was developed using intervention mapping and included community involvement, media campaigns, school classroom, curricular and homework activities, active playgrounds and other environmental changes at school level, as well as parental education materials. The effects of the intervention were evaluated in a sample of over 16,000 children aged 2–10 years from eight European countries. At the end of the intervention period, there was no evidence of intervention effect on measures of adiposity.
The lack of evidence of any significant effect on adiposity at the end of the intervention period in these two larger trials is similar to the overall findings in our trial and adds to the larger body of evidence showing mixed or weak results from dietary and PA interventions.
Interpretation of study findings
Several factors may have contributed to the absence of evidence of effects on primary outcomes in the WAVES study and other trials.
Target behaviours addressed by intervention
In the WAVES study, as in other similar childhood obesity prevention studies, the multicomponent intervention package addressed dietary and PA behaviours. These target behaviours are generally associated with adiposity levels in observational studies, but there are conflicting views on whether or not all associations are causal. 112 Unless there is a strong causal link between the target behaviour and the desired outcome, interventions will not be effective. 113 Furthermore, within the complex web of causal factors, modifying one behaviour may lead to compensatory action that offsets any positive effects. For example, engaging in additional PA may be accompanied by the consumption of more energy-dense foods as a reward.
Strategies for behaviour change
Although the common behaviour change strategies that have been associated with successful childhood obesity prevention interventions have been summarised,100,114 it is not known which are the most effective.
Intervention delivery
The intervention was delivered by non-researchers, similar to other school-based and community studies. The degree to which the intervention was delivered as intended was variable, and, although the fidelity of implementation was high overall, a few schools failed to implement the intervention fully or at all. Although this reflects more closely the probable effects of the intervention if it is implemented outside a trial setting, the efficacy of the true intervention cannot be fully assessed. Intercomponent differences in fidelity were mainly driven by required teacher workload, enthusiasm and support from senior staff. Although teachers were encouraged to tailor the PA component of the intervention to their particular circumstances, this component was the most challenging for them. The need to deliver this component on a daily basis was burdensome, and, even among schools that had developed a routine, the full ‘dose’ of 30 minutes per day was not achieved.
Duration of intervention and timing of follow-up
Most childhood obesity prevention interventions are of short duration (up to 12 months). It is unlikely that an intervention will have long-term effects unless it is ongoing or unless changes in the environment continue to support behaviour change. Although the aim of the intervention was to facilitate sustainable changes, few teachers intended to continue delivering the intervention after the end of the study. Even if sustained behaviour change is achieved, intervention effects on weight status may take a longer time to manifest. 112
Wider context
There is increasing emphasis on obesity prevention, and a number of local and national initiatives have started over recent years. Although the findings from the feasibility study suggested that the intervention was promising, intervention delivery for the trial and subsequent follow-up measurements took place some years later, during which time wider environmental changes may have diluted any effects. Furthermore, although school is an important setting for influencing children’s health behaviour, wider impacts from the family and community, including socioeconomic circumstances, must also be considered. Food marketing and easy access to less healthy foods, as well as environments that discourage walking and PA, may also affect behaviour. 11 The qualitative data from teachers115 and parents,116 collected as part of our process evaluation, support the possibility that these wider influences have a greater effect than any school-based intervention.
Interpretation from the WAVES process evaluation
The extensive process evaluation suggests that intervention delivery was variable, although the majority of intervention schools delivered most of the components, and teachers reported that the implementation of the programme was relatively easy and manageable. 115 Furthermore, teachers commented on the ease of use of the intervention, their appreciation of the flexibility to adapt resources to their individual circumstances and the inclusive nature of activities, meaning that all children could get involved regardless of academic or motor skill level. The teachers also discussed how the key messages of the intervention supported existing practice and the ethos of school responsibility for the whole child. 115 When exploring the views of parents, all were supportive and appreciative of the programme, but there was some differentiation in terms of the perceived impact. Families from higher socioeconomic areas considered that they gained little additional knowledge and already practised healthy behaviours, whereas positive lifestyle changes were more likely to be reported by families from more disadvantaged communities. 116 However, our subgroup analysis did not support this finding.
The signposting information was resource intensive to produce and not recalled by participants. Therefore, this component is unlikely to have had any impact.
Although in most schools the PA component was not delivered at the intended intensity, overall, the average daily increase in MVPA exposure achieved was around 12 minutes. This is close to the 15 minutes per day of additional activity that is promoted by ‘The Daily Mile’ initiative, which has been reported to be simple and feasible to deliver and has been associated anecdotally with positive changes. Schools that did implement this component often reported positive effects in terms of concentration and mood among children, although a minority of schools reported negative effects. Schools were more likely to deliver the intervention if they planned and timetabled PA into their daily routine.
Most of the cooking workshops were delivered and covered the key content and activities. However, parental attendance at the workshops was just over 40%. Schools that had pre-existing parent engagement relationships were more likely to involve parents. Parents and children reported improved knowledge, skills and diet as a result of these workshops. 116 Teachers also observed increased knowledge and some behavioural changes among the children as a result of this element of the intervention. 115
The Villa Vitality component of the intervention was particularly well received by teachers, as it was seen to draw together the key messages and provide the opportunity for children to practise healthy lifestyle behaviours in an inspirational setting outside the classroom. 115 Children recalled this component vividly and parents commented on the impact of this visit in terms of the role models and the weekly challenges. 116
The process evaluation also highlighted challenges in delivery of the intervention. Competing demands on teachers’ time and pressure for academic achievement meant that intervention delivery could be compromised. In addition, support from parents, the wider school and government was seen as important for facilitating intervention delivery. The sustainability of any intervention effect was also questioned, as parents and teachers considered that a 1-year programme may be insufficient for long-term behaviour change.
Implications of findings
Our overall conclusion is that the WAVES study intervention did not have a significant effect on our prespecified primary outcomes. The post hoc exploratory analysis demonstrated heterogeneity of effects between G1 and G2 schools, which may be explained by differences in the baseline characteristics and more marked adiposity imbalance between the arms in G2. We found no evidence of harm or inequity.
Schools offer an important setting for delivering obesity prevention interventions, as they reach the majority of children, have long-term and in-depth contact with children, and offer a space in which children can observe and practise health behaviours that contribute to obesity prevention. A meta-synthesis of qualitative studies exploring the role of primary schools in preventing childhood obesity highlighted the need for schools, parents and government to work together to promote healthy lifestyles in children and support activities in the school setting. 117 School staff view the provision of healthy lifestyles education as a key school responsibility in relation to children’s holistic development, but they need national and local policies to be in place to support the delivery of a health-promoting environment and curriculum. 118 From September 2014, primary schools in the UK were expected to teach children about food, cooking and nutrition under the national curriculum. Schools are also encouraged to offer 5 hours of PA opportunities per week,119 although this rarely happens in practice.
Although our findings do not support the wider implementation of the WAVES study intervention, the PA and cooking workshop components could be considered by schools to fulfil their mandated responsibilities. These components are relatively low cost, have been shown to be acceptable and feasible to deliver, are appreciated by teachers, children and parents, and are not associated with any harm. Furthermore, the possibility of potential benefit cannot be completely dismissed. The Daily Mile initiative is gaining popularity,120 and, although the WAVES study PA component was not identical, the overall aim was similar. Future interventions could focus on optimising delivery of this component by (1) further training teachers to help them feel more confident with delivery, (2) encouraging teachers’ understanding of the importance of increased PA on wider outcomes, including positive academic achievement and (3) facilitating timetabling of the activity by encouraging teachers to consider competing demands and plan delivery to suit their class needs. The cooking workshops could fulfil the new national curriculum requirements. Future programmes should focus on how to better engage parents in the delivery of such workshops.
In summary, this theory-informed, multicomponent intervention, which was feasible to deliver and was well received by children and parents, was not cost-effective, did not result in a significant reduction in obesity prevalence overall and did not alter diet or PA levels in children. Schools are important settings for accessing children and their families, but are one of several levels of environments that influence behaviour. Delivery of knowledge and skills to support healthy lifestyles is one of the mandatory functions of schools. School staff recognise the importance of encouraging healthy behaviours within the context of children’s wider well-being. Future school-based interventions need to be integrated within a wider societal framework and supported by upstream interventions. This includes having supportive policies to promote social and environmental change. Interventions at multiple levels are needed to tackle the complex set of interacting factors that contribute to childhood obesity. 121 A realist review and synthesis of the literature on childhood obesity prevention studies could further inform future interventions. By considering the variety of contexts in which interventions were delivered, and the different strategies used in relation to the patterns of outcomes, such an approach can be used to build a theory to explain how, why and for which groups intervention components may be effective.
In terms of methodology, future cluster randomised controlled trials need to take appropriate steps to ensure a balanced allocation of intervention and control across key characteristics in order to reduce the risk of chance bias. This could be achieved by increasing the number of clusters.
Acknowledgements
We wish to thank and acknowledge the children, school staff and parents who participated in the trial, and the children, teachers and parents who took part in focus groups as part of the process evaluation. We acknowledge the support of staff at AVFC in delivering the Villa Vitality programme.
We would like to thank the study team, including Dr Behnoush Mohammadpoor Ahranjani and Mrs Emma Parkes, who helped to oversee the study measurements and data collection, as well as the administrative team who facilitated the running of the project. We also express our thanks to the research staff who undertook the study measurements and to Mr Robert Lancashire, who developed the trial database and oversaw data management.
Contributions of authors
Professor Peymane Adab (Professor of Chronic Disease Epidemiology and Public Health, Institute of Applied Health Research) led the trial as principal investigator, prepared the summary, introduction and discussion chapters and assisted with preparation of the results chapter.
Professor Timothy Barrett (Leonard Parsons Professor of Paediatrics, Institute of Cancer and Genomic Sciences) was a co-investigator and advised on the anthropometric measurement tools used and arranged for initial training of research staff to undertake measurements. He also contributed to the trial design, measurement procedures and interpretation of findings.
Professor Raj Bhopal (Bruce and John Usher Chair in Public Health) was a co-investigator and has contributed to the trial design, measurement procedures and interpretation of findings.
Professor Janet E Cade (Professor of Nutritional Epidemiology and Public Health, School of Food Science and Nutrition) was a co-investigator, developed the dietary intake assessment tool used in the study and supervised all of the processing of the dietary intake data collected using the tool. In collaboration with other colleagues at the University of Leeds, she revised the dietary intake part of the outcomes section of the methods chapter.
Dr Alastair Canaway (Research Fellow, Clinical Trials Unit) undertook the cost-effectiveness analysis under the direction of the trial health economist. He also prepared the cost-effectiveness chapter.
Professor Kar Keung Cheng (Professor of Public Health and Primary Care, Institute of Applied Health Research) was a co-investigator and advisor to the trial management team. He has contributed to the trial design, measurement procedures and interpretation of findings.
Dr Joanne Clarke (Research Fellow, Institute of Applied Health Research) assisted in both measurement and process evaluation data collection and was one of the two main researchers responsible for consolidating and analysing the process evaluation data. She assisted in the preparation of the interventions chapter.
Dr Amanda Daley (Reader in Behavioural Medicine, Institute of Applied Health Research) was a co-investigator and has contributed to the trial design and aspects of intervention design, and interpretation of findings.
Professor Jonathan Deeks (Professor of Biostatistics, Institute of Applied Health Research) was a co-investigator and advised on statistical aspects of the trial and in the interpretation of findings.
Professor Joan Duda (Professor of Sport and Exercise Psychology, School of Sport, Exercise and Rehabilitation Sciences) was a co-investigator and contributed to the trial design, psychological measurement instruments and interpretation of findings.
Professor Ulf Ekelund (Professor of Physical Activity and Health, Department of Sport Medicine, Norwegian School of Sport Sciences/ Cambridge MRC Epidemiology Unit) was co-investigator and advised on PA assessment, and oversaw the training of researchers in collecting Actiheart data and the processing of the PA data. He prepared the PA part of the outcomes section of the methods chapter in collaboration with other colleagues at the MRC Epidemiology Unit.
Dr Emma Frew (Reader in Health Economics, Institute of Applied Health Research) was a co-investigator and the trial health economist. She advised on all aspects of the cost-effectiveness component of the study. She assisted in both the preparation and the revision of the cost-effectiveness chapter.
Dr Paramjit Gill (Reader in Primary Care Research, Institute of Applied Health Research) was a co-investigator and contributed to the trial design, measurement procedures and interpretation of findings.
Dr Tania Griffin (Research Fellow, Institute of Applied Health Research) was part of the main study team and was responsible for all of the aspects of the process evaluation component of the study. She assisted in the preparation and revision of the process evaluation of intervention implementation chapter.
Dr Karla Hemming (Senior Lecturer in Biostatistics, Institute of Applied Health Research) was the trial statistician and a member of the Trial Steering Committee and undertook the sampling and random allocation procedures. She advised on all of the aspects of the main study analyses and revised the statistical analysis methods chapter and part of the statistical elements of the methods chapter. She also assisted in the preparation of the results chapter.
Mrs Kiya Hurley (Research Assistant, Institute of Applied Health Research) supervised the measurement teams throughout the study, prepared the dietary intake part of the outcomes section of the methods chapter and revised all of the outcomes section of the methods chapter.
Dr Emma R Lancashire (Senior Research Fellow, Institute of Applied Health Research) was the trial co-ordinator for the study and led the trial management team. She prepared the methods, interventions, process evaluation of intervention implementation and results chapters. She undertook the analysis for, and produced, the CONSORT flow diagram and the pupil- and school-level baseline characteristics tables.
Mr James Martin (Research Assistant, Institute of Applied Health Research) undertook the main study analyses, including sensitivity and ancillary analyses, under the direction of the trial statistician. He produced all of the key and additional variable results tables and prepared the statistical analysis methods chapter. He also assisted in the preparation of the results chapter.
Ms Eleanor McGee (Public Health Nutrition Lead Birmingham Community Healthcare NHS Trust) was a co-investigator and contributed to the trial design, measurement procedures and interpretation of findings.
Dr Miranda J Pallan (Senior Lecturer in Public Health, Institute of Applied Health Research) was a co-investigator and part of the trial management team, working alongside the principal investigator and trial co-ordinator at all stages. She assisted in the preparation and revision of the process evaluation of intervention implementation chapter.
Professor Jayne Parry (Professor of Policy and Public Health, Institute of Applied Health Research) was a co-investigator and advised on process evaluation and contributed to trial design, measurement procedures and interpretation of qualitative data.
Dr Sandra Passmore (Education Advisor, Birmingham Services for Education) was a co-investigator and contributed to liaison with schools, intervention design and interpretation of findings.
All authors have read and approved the final version.
Trial Steering Committee
We would like to thank and acknowledge members of the external trial steering committee for overseeing the trial:
Dr Kelvin Jordan, Keele University: chairperson/statistician.
Professor Peter Whincup, St George’s, University of London: subject expert.
Dr Louise Longworth, Brunel University: health economist.
Mr John Bennett, PHSE advisor: public representative.
Medical Research Council Epidemiology Unit, University of Cambridge
We would like to acknowledge support and assistance from staff at the Institute of Metabolic Science at the MRC Epidemiology Unit, particularly Dr Soren Brage, Miss Kate Westgate and Mrs Stefani Hollidge, for training of staff on the use of Actihearts, providing advice and maintaining the Actiheart monitors and processing the data to allow analysis of the PA data.
Nutrition Epidemiology Group, University of Leeds
We acknowledge support and assistance from staff who are working, or have previously worked, at the Nutrition Epidemiology Group in Leeds, who have supported the trial team in terms of administration of the CADET food tick list, and processing of the data to enable us to undertake dietary intake analysis. In particular, we would like to thank Neil Hancock, Cristina Cleghorn, Meagan Christian, Jayne Hutchinson, Holly Rippin and Catherine Rycroft.
Publications
Canaway AG, Frew EJ. Measuring preference-based quality of life in children aged 6–7 years: a comparison of the performance of the CHU-9D and EQ-5D-Y: the WAVES Pilot Study. Qual Life Res 2013;22:173–83.
Canaway A, Frew E. Is utility-based quality of life in children aged 6–7 years affected by Body Mass Index (BMI)? Int J Obes 2014;38:1146.
Griffin TL, Clarke JL, Lancashire ER, Pallan MJ, Passmore S, Adab P. Teacher experiences of delivering an obesity prevention programme (The WAVES study intervention) in a primary school setting. Health Educ J 2014;74:655–67.
Griffin TL, Pallan MJ, Clarke JL, Lancashire ER, Lyon A, Parry JM, Adab P, on behalf of the WAVES study trial investigators. Process evaluation design in a cluster randomised controlled childhood obesity prevention trial: the WAVES study. IJBNPA 2014;11:112.
Adab P, Pallan MJ, Lancashire ER, Hemming K, Frew E, Griffin T, et al. A cluster-randomised controlled trial to assess the effectiveness and cost-effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6-7 year old children: the WAVES study protocol. BMC Public Health 2015;15:488.
Clarke J, Griffin T, Lancashire E, Adab P, Parry J, Pallan M. Parent and child perceptions of school-based obesity prevention in England: a qualitative study. BMC Public Health 2015;15:1224.
Frew EJ, Pallan M, Lancashire E, Hemming K, Adab P. Is utility-based quality of life associated with overweight in children? Evidence from the UK WAVES randomised controlled study. BMC Pediatric 2015;15:211.
Clarke JL, Pallan MJ, Lancashire ER, Adab P. Obesity prevention in English primary schools: headteacher perspectives. Health Promot Int 2017;32:490–9.
Adab P, Pallan MJ, Lancashire ER, Hemming K, Frew E, Barrett T, et al. Effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6-7 year old children: cluster randomised controlled trial (WAVES) study. BMJ 2018;360:k211.
Data sharing statement
All available data are available from the corresponding author on request.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- World Health Organization (WHO) . Global Strategy on Diet, Physical Activity, and Health: Childhood Overweight and Obesity n.d. www.who.int/dietphysicalactivity/childhood/en/ (accessed 13 July 2016).
- Commission on Ending Childhood Obesity. Report of the Commission on Ending Childhood Obesity. Geneva: WHO; 2016.
- Wijga AH, Scholtens S, Bemelmans WJ, de Jongste JC, Kerkhof M, Schipper M, et al. Comorbidities of obesity in school children: a cross-sectional study in the PIAMA birth cohort. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-184.
- Pizzi MA, Vroman K. Childhood obesity: effects on children’s participation, mental health, and psychosocial development. Occup Ther Health Care 2013;27:99-112. http://dx.doi.org/10.3109/07380577.2013.784839.
- Caird J, Kavanagh J, Oliver K, Oliver S, O’Mara A, Stansfield C, et al. Childhood Obesity and Educational Attainment: A Systematic Review. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2011.
- Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 2007;357:2329-37. http://dx.doi.org/10.1056/NEJMoa072515.
- Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord 1999;23:2-11. https://doi.org/10.1038/sj.ijo.0800852.
- Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med 1993;22:167-77. https://doi.org/10.1006/pmed.1993.1014.
- Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. AHA/ACC/TOS Guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2013;129:S102-38. https://doi.org/10.1161/01.cir.0000437739.71477.ee.
- Litwin SE. Childhood obesity and adulthood cardiovascular disease: quantifying the lifetime cumulative burden of cardiovascular risk factors. J Am Coll Cardiol 2014;64:1588-90. http://dx.doi.org/10.1016/j.jacc.2014.07.962.
- Butland B, Jebb S, Kopelman P. Tackling Obesities: Future Choices – Project Report. London: Foresight Programme of the Government Office for Science; 2007.
- Statistics on Obesity, Physical Activity and Diet, England 2015. Leeds: NHS; 2015.
- National Child Measurement Programme: England, 2014/15, School Year. Leeds: NHS; 2015.
- Pallan MJ, Adab P, Sitch AJ, Aveyard P. Are school physical activity characteristics associated with weight status in primary school children? A multilevel cross-sectional analysis of routine surveillance data. Arch Dis Child 2014;99:135-41. http://dx.doi.org/10.1136/archdischild-2013-303987.
- Wardle J, Brodersen NH, Cole TJ, Jarvis MJ, Boniface DR. Development of adiposity in adolescence: five year longitudinal study of an ethnically and socioeconomically diverse sample of young people in Britain. BMJ 2006;332:1130-5. http://dx.doi.org/10.1136/bmj.38807.594792.AE.
- Johnson L, Sebire S. Maintaining a Healthy Weight and Preventing Excess Weight Gain in Children and Adults – Partial Update of CG43. London: Centre for Public Health at NICE; 2014.
- Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school-age youth. J Pediatr 2005;146:732-7. http://dx.doi.org/10.1016/j.jpeds.2005.01.055.
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12. http://dx.doi.org/10.1002/14651858.CD001871.pub3.
- Wang Y, Cai L, Wu Y, Wilson RF, Weston C, Fawole O, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev 2015;16:547-65. http://dx.doi.org/10.1111/obr.12277.
- Wang Y, Wu Y, Wilson RF, Bleich S, Cheskin L, Weston C. Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-Analysis. Rockville, MD: Agency for Healthcare Research and Quality; 2013.
- Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ 2009;180:719-26. http://dx.doi.org/10.1503/cmaj.080966.
- Demetriou Y, Höner O. Physical activity interventions in the school setting: a systematic review. Psychol Sport Exerc 2012;13:186-96. https://doi.org/10.1016/j.psychsport.2011.11.006.
- Katz DL, O’Connell M, Njike VY, Yeh MC, Nawaz H. Strategies for the prevention and control of obesity in the school setting: systematic review and meta-analysis. Int J Obes 2008;32:1780-9. http://dx.doi.org/10.1038/ijo.2008.158.
- Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes Rev 2012;13:214-33. http://dx.doi.org/10.1111/j.1467-789X.2011.00947.x.
- Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull 2006;132:667-91. http://dx.doi.org/10.1037/0033-2909.132.5.667.
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694-6. https://doi.org/10.1136/bmj.321.7262.694.
- Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995;73:25-9. https://doi.org/10.1136/adc.73.1.25.
- Harlow Healthcare . LMS Growth for UK 1990 Growth Reference Data n.d. www.healthforallchildren.com/shop-base/shop/software/lmsgrowth/ (accessed 13 July 2016).
- Cade JE, Frear L, Greenwood DC. Assessment of diet in young children with an emphasis on fruit and vegetable intake: using CADET – Child and Diet Evaluation Tool. Public Health Nutr 2006;9:501-8. https://doi.org/10.1079/PHN2005871.
- Roe M, Pinchen H, Church S, Finglas P. McCance and Widdowson’s The Composition of Foods: Seventh Summary Edition and updated composition of foods integrated dataset. Nutr Bull 2015;40:36-9. https://doi.org/10.1111/nbu.12124.
- Bates B, Lennox A, Prentice A, Bates C, Page P, Nicholson S, et al. National Diet and Nutrition Survey Results from Years 1, 2, 3 and 4 (combined) of the Rolling Programme (2008/2009–2011/2012). London: Department of Health; 2014.
- Gregory JR, Collins DL, Davies PSW, Hughes JM, Clarke PC. National Diet and Nutrition Survey: Children Aged 1½ to 4½ Years. Volume 1: Report of the Diet and Nutrition Survey. London: Department of Health; 1995.
- Wrieden WL, Longbottom PJ, Adamson AJ, Ogston SA, Payne A, Haleem MA, et al. Estimation of typical food portion sizes for children of different ages in Great Britain. Br J Nutr 2008;99:1344-53. http://dx.doi.org/10.1017/S0007114507868516.
- Englyst HN, Cummings JH. Improved Method for Measurement of Dietary Fiber As Non-Starch Polysaccharides in Plant Foods n.d. http://europepmc.org/abstract/med/2458334 (accessed 13 July 2016).
- 5 A Day Portion Sizes. London: NHS; 2015.
- Public Health Agency . Enjoy Healthy Eating: Fruit and Vegetables 2014. www.enjoyhealthyeating.info/nutrition/children-aged-1-5-years/fruit-and-vegetables (accessed 13 July 2016).
- Brage S, Brage N, Franks P, Ekelund U, Wareham N. Reliability and validity of the combined heart rate and movement sensor Actiheart. Eur J Clin Nutr 2005;59:561-70. https://doi.org/10.1038/sj.ejcn.1602118.
- Stegle O, Fallert SV, MacKay DJ, Brage S. Gaussian process robust regression for noisy heart rate data. IEEE Trans Biomed Eng 2008;55:2143-51. http://dx.doi.org/10.1109/TBME.2008.923118.
- Haapala EA, Väistö J, Lintu N, Tompuri T, Brage S, Westgate K, et al. Adiposity, physical activity and neuromuscular performance in children. J Sports Sci 2016;34:1699-706. http://dx.doi.org/10.1080/02640414.2015.1134805.
- Brage S, Ekelund U, Brage N, Hennings MA, Froberg K, Franks PW, et al. Hierarchy of individual calibration levels for heart rate and accelerometry to measure physical activity. J Appl Physiol 2007;103:682-92. http://dx.doi.org/10.1152/japplphysiol.00092.2006.
- Department of Health . Physical Activity Guidelines for Children and Young People (5–18 Years) 2011. www.gov.uk/government/uploads/system/uploads/attachment_data/file/213739/dh_128144.pdf (accessed 13 July 2016).
- Collings PJ, Wijndaele K, Corder K, Westgate K, Ridgway CL, Sharp SJ, et al. Magnitude and determinants of change in objectively-measured physical activity, sedentary time and sleep duration from ages 15 to 17.5y in UK adolescents: the ROOTS study. Int J Behav Nutr Phys Act 2015;12. http://dx.doi.org/10.1186/s12966-015-0222-4.
- Varni JW. Pediatric Quality of Life Inventory Used to Measure Health Related Quality of Life n.d. www.pedsql.org (accessed 13 July 2016).
- Child Public Health . KIDSCREEN-52 Health-Related Quality of Life Questionnaire for Children and Adolescents Aged from 8 to 18 Years n.d. www.kidscreen.org/english/questionnaires/kidscreen-52-long-version (accessed 13 July 2016).
- Stevens K. University of Sheffield . Child Health Utility 9D n.d. www.shef.ac.uk/scharr/sections/heds/mvh/paediatric/about-chu9d (accessed 13 July 2016).
- Stevens KJ. Working with children to develop dimensions for a preference-based, generic, pediatric, health-related quality-of-life measure. Qual Health Res 2010;20:340-51. http://dx.doi.org/10.1177/1049732309358328.
- Jackson LV, Thalange NK, Cole TJ. Blood pressure centiles for Great Britain. Arch Dis Child 2007;92:298-303. http://dx.doi.org/10.1136/adc.2005.081216.
- Truby H, Paxton SJ. Development of the Children’s Body Image Scale. Br J Clin Psychol 2002;41:185-203. https://doi.org/10.1348/014466502163967.
- Truby H, Paxton SJ. The Children’s Body Image Scale: reliability and use with international standards for body mass index. Br J Clin Psychol 2008;47:119-24. https://doi.org/10.1348/014466507X251261.
- Office for National Statistics . Ethnic Group Classification Guidance and Methodology n.d. http://webarchive.nationalarchives.gov.uk/20160105160709/www.ons.gov.uk/ons/guide-method/measuring-equality/equality/ethnic-nat-identity-religion/ethnic-group/index.html#1 (accessed 13 July 2016).
- Eldridge SM, Ashby D, Kerry S. Sample size for cluster randomized trials: effect of coefficient of variation of cluster size and analysis method. Int J Epidemiol 2006;35:1292-300. http://dx.doi.org/10.1093/ije/dyl129.
- Adab P, Pallan MJ, Cade J, Ekelund U, Barrett T, Daley A, et al. Preventing childhood obesity, phase II feasibility study focusing on South Asians: BEACHeS. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2013-004579.
- Ford AL, Hunt LP, Cooper A, Shield JP. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health?. Arch Dis Child 2010;95:256-61. http://dx.doi.org/10.1136/adc.2009.165340.
- Carter BR, Hood K. Balance algorithm for cluster randomized trials. BMC Med Res Methodol 2008;8. http://dx.doi.org/10.1186/1471-2288-8-65.
- Raab GM, Butcher I. Balance in cluster randomized trials. Stat Med 2001;20:351-65. https://doi.org/10.1002/1097-0258(20010215)20:3<351::AID-SIM797>3.0.CO;2-C.
- Pallan M, Parry J, Cheng KK, Adab P. Development of a childhood obesity prevention programme with a focus on UK South Asian communities. Prev Med 2013;57:948-54. http://dx.doi.org/10.1016/j.ypmed.2013.08.025.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Wake Up Shake Up Productions (Creative Director Ruth Mitchell) . Wake Up Shake Up Physical Activity Package n.d. www.wakeupshakeup.com/ (accessed 13 July 2016).
- Val Sabin Publications and Training . Activate Physical Activity Programme n.d. www.valsabinpublications.com/publications/activate/ (accessed 13 July 2016).
- Val Sabin Publications and Training . Positive Play Physical Activity Package n.d. www.valsabinpublications.com/publications/6-daily-activities-positive-play-activate-skillax/positive-play-ks1-and-ks2/ (accessed 24 January 2017).
- Babcock LDP. Take 10 Physical Activity Package n.d. www.take10.org.uk/ (accessed 13 July 2016).
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- Steckler AB, Linnan L, Israel B. Process Evaluation for Public Health Interventions and Research. San Francisco, CA: Jossey-Bass; 2002.
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control?. Clin Psychol Rev 1998;18:23-45. https://doi.org/10.1016/S0272-7358(97)00043-3.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h1258.
- Dusenbury L, Brannigan R, Falco M, Hansen WB. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Educ Res 2003;18:237-56. https://doi.org/10.1093/her/18.2.237.
- Gibson CA, Smith BK, Dubose KD, Greene JL, Bailey BW, Williams SL, et al. Physical activity across the curriculum: year one process evaluation results. Int J Behav Nutr Phys Act 2008;5. http://dx.doi.org/10.1186/1479-5868-5-36.
- Fagan AA, Hanson K, Hawkins JD, Arthur MW. Bridging science to practice: achieving prevention program implementation fidelity in the community youth development study. Am J Community Psychol 2008;41:235-49. http://dx.doi.org/10.1007/s10464-008-9176-x.
- Goldberg Lillehoj CJ, Griffin KW, Spoth R. Program provider and observer ratings of school-based preventive intervention implementation: agreement and relation to youth outcomes. Health Educ Behav 2004;31:242-57. http://dx.doi.org/10.1177/1090198103260514.
- Saunders RP, Evans MH, Joshi P. Developing a process-evaluation plan for assessing health promotion program implementation: a how-to guide. Health Promot Pract 2005;6:134-47. http://dx.doi.org/10.1177/1524839904273387.
- Baranowski T, Stables G. Process evaluations of the 5-a-day projects. Health Educ Behav 2000;27:157-66. https://doi.org/10.1177/109019810002700202.
- Byers PY, Wilcox JR. Focus groups: a qualitative opportunity for researchers. J Bus Commun 1991;28:63-78. https://doi.org/10.1177/002194369102800105.
- Mauthner M. Methodological aspects of collecting data from children: lessons from three research projects. Child Soc 1997;11:16-28. https://doi.org/10.1111/j.1099-0860.1997.tb00003.x.
- Caille A, Kerry S, Tavernier E, Leyrat C, Eldridge S, Giraudeau B. Timeline cluster: a graphical tool to identify risk of bias in cluster randomised trials. BMJ 2016;354. http://dx.doi.org/10.1136/bmj.i4291.
- Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 2003;3. http://dx.doi.org/10.1186/1471-2288-3-21.
- Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702-6. https://doi.org/10.1093/aje/kwh090.
- Mosteller F, Tukey JW. Data Analysis and Regression: A Second Course in Statistics. Boston, MA: Addison-Wesley; 1977.
- Carpenter JR, Goldstein H, Kenward MG. REALCOM-IMPUTE software for multilevel multiple imputation with mixed response types. J Stat Softw 2011;45:1-14. https://doi.org/10.18637/jss.v045.i05.
- Campbell MJ, Donner A, Klar N. Developments in cluster randomized trials and Statistics in Medicine. Stat Med 2007;26:2-19. https://doi.org/10.1002/sim.2731.
- Fiero M, Huang S, Bell ML. Statistical analysis and handling of missing data in cluster randomised trials: protocol for a systematic review. BMJ Open 2015;5. http://dx.doi.org/10.1136/bmjopen-2014-007378.
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux P, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 2010;63:e1-37. https://doi.org/10.1016/j.jclinepi.2010.03.004.
- Gomes M, Díaz-Ordaz K, Grieve R, Kenward MG. Multiple imputation methods for handling missing data in cost-effectiveness analyses that use data from hierarchical studies: an application to cluster randomized trials. Med Decis Making 2013;33:1051-63. http://dx.doi.org/10.1177/0272989X13492203.
- Díaz-Ordaz K, Kenward MG, Cohen A, Coleman CL, Eldridge S. Are missing data adequately handled in cluster randomised trials? A systematic review and guidelines. Clin Trials 2014;11:590-60. http://dx.doi.org/10.1177/1740774514537136.
- Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b2393.
- Klar N, Darlington G. Methods for modelling change in cluster randomization trials. Stat Med 2004;23:2341-57. http://dx.doi.org/10.1002/sim.1858.
- Heo M, Leon AC. Sample size requirements to detect an intervention by time interaction in longitudinal cluster randomized clinical trials. Stat Med 2009;28:1017-27. http://dx.doi.org/10.1002/sim.3527.
- Adab P, Pallan MJ, Lancashire ER, Hemming K, Frew E, Barrett T, et al. Effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6-7 year old children: cluster randomised controlled trial (WAVES) study. BMJ 2018;360.
- Campbell MK, Piaggio G, Elbourne DR, Altman DG. CONSORT Group . Consort 2010 statement: extension to cluster randomised trials. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e5661.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Office for National Statistics . Annual Survey of Hours and Earnings, 2014, Provisional Results 2014. www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/annualsurveyofhoursandearnings/2014-11-19 (accessed 3 August 2016).
- HM Revenue & Customs . Travel – Mileage and Fuel Rates and Allowances n.d. www.gov.uk/government/publications/rates-and-allowances-travel-mileage-and-fuel-allowances/travel-mileage-and-fuel-rates-and-allowances.
- Department for Education . Teachers’ Pay and Allowances from 1 September 2013 2014. www.education-ni.gov.uk/sites/default/files/publications/de/2014-13-teachers-pay-and-allowances-from-1-september-2013.pdf (accessed 3 August 2016).
- Canaway AG, Frew EJ. Measuring preference-based quality of life in children aged 6–7 years: a comparison of the performance of the CHU-9D and EQ-5D-Y: the WAVES pilot study. Qual Life Res 2013;22:173-83. https://doi.org/10.1007/s11136-012-0119-5.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- Adab P, Pallan MJ, Lancashire ER, Hemming K, Frew E, Griffin T, et al. A cluster-randomised controlled trial to assess the effectiveness and cost-effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6-7 year old children: the WAVES study protocol. BMC Public Health 2015;15. http://dx.doi.org/10.1186/s12889-015-1800-8.
- Gomes M, Ng ES, Grieve R, Nixon R, Carpenter J, Thompson SG. Developing appropriate methods for cost-effectiveness analysis of cluster randomized trials. Med Decis Making 2012;32:350-61. http://dx.doi.org/10.1177/0272989X11418372.
- Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ 2002;11:415-30. http://dx.doi.org/10.1002/hec.678.
- Hoch JS, Dewa CS. Advantages of the net benefit regression framework for economic evaluations of interventions in the workplace: a case study of the cost-effectiveness of a collaborative mental health care program for people receiving short-term disability benefits for psychiatric disorders. J Occup Environ Med 2014;56:441-5. http://dx.doi.org/10.1097/JOM.0000000000000130.
- Sun X, Briel M, Busse JW, You JJ, Akl EA, Mejza F, et al. Credibility of claims of subgroup effects in randomised controlled trials: systematic review. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e1553.
- Martin J, Chater A, Lorencatto F. Effective behaviour change techniques in the prevention and management of childhood obesity. Int J Obes 2013;37:1287-94. http://dx.doi.org/10.1038/ijo.2013.107.
- Roberts C, Torgerson DJ. Understanding controlled trials: baseline imbalance in randomised controlled trials. BMJ 1999;319. https://doi.org/10.1136/bmj.319.7203.185.
- Hahn S, Puffer S, Torgerson DJ, Watson J. Methodological bias in cluster randomised trials. BMC Med Res Methodol 2005;5. http://dx.doi.org/10.1186/1471-2288-5-10.
- Puffer S, Torgerson D, Watson J. Evidence for risk of bias in cluster randomised trials: review of recent trials published in three general medical journals. BMJ 2003;327:785-9. http://dx.doi.org/10.1136/bmj.327.7418.785.
- Macdiarmid J, Blundell J. Assessing dietary intake: who, what and why of under-reporting. Nutr Res Rev 1998;11:231-53. http://dx.doi.org/10.1079/NRR19980017.
- Zaborskis A, Moceviciene R, Iannotti RJ. The influence of chronological period of data collection on differences in reported dietary intake among school-aged children surveyed in 39 countries. J Nutr Educ Behav 2014;46:359-69. http://dx.doi.org/10.1016/j.jneb.2013.11.017.
- Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g3256.
- Donin AS, Nightingale CM, Owen CG, Rudnicka AR, McNamara MC, Prynne CJ, et al. Ethnic differences in blood lipids and dietary intake between UK children of black African, black Caribbean, South Asian, and white European origin: the Child Heart and Health Study in England (CHASE). Am J Clin Nutr 2010;92:776-83. https://doi.org/10.3945/ajcn.2010.29533.
- Owen CG, Nightingale CM, Rudnicka AR, Cook DG, Ekelund U, Whincup PH. Ethnic and gender differences in physical activity levels among 9–10-year-old children of white European, South Asian and African–Caribbean origin: the Child Heart Health Study in England (CHASE Study). Int J Epidemiol 2009;38:1082-93. https://doi.org/10.1093/ije/dyp176.
- Kirk S, Zeller M, Claytor R, Santangelo M, Khoury PR, Daniels SR. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res 2005;13:876-82. https://doi.org/10.1038/oby.2005.101.
- Kolsgaard MLP, Joner G, Brunborg C, Anderssen SA, Tonstad S, Andersen LF. Reduction in BMI z-score and improvement in cardiometabolic risk factors in obese children and adolescents. The Oslo Adiposity Intervention Study: a hospital/public health nurse combined treatment. BMC Pediatr 2011;11. https://doi.org/10.1186/1471-2431-11-47.
- De Henauw S, Huybrechts I, De Bourdeaudhuij I, Bammann K, Barba G, Lissner L, et al. Effects of a community-oriented obesity prevention programme on indicators of body fatness in preschool and primary school children. Main results from the IDEFICS study. Obes Rev 2015;16:16-29. http://dx.doi.org/10.1111/obr.12346.
- Baranowski T, Lytle L. Should the IDEFICS outcomes have been expected?. Obes Rev 2015;16:162-72. http://dx.doi.org/10.1111/obr.12359.
- Baranowski T, Cerin E, Baranowski J. Steps in the design, development and formative evaluation of obesity prevention-related behavior change trials. Int J Behav Nutr Phys Act 2009;6. http://dx.doi.org/10.1186/1479-5868-6-6.
- Hardeman W, Griffin S, Johnston M, Kinmonth AL, Wareham NJ. Interventions to prevent weight gain: a systematic review of psychological models and behaviour change methods. Int J Obes Relat Metab Disord 2000;24:131-43. https://doi.org/10.1038/sj.ijo.0801100.
- Griffin TL, Clarke JL, Lancashire ER, Pallan MJ, Passmore S, Adab P. Teacher experiences of delivering an obesity prevention programme (the WAVES study intervention) in a primary school setting. Health Educ J 2014;74:655-67. https://doi.org/10.1177/0017896914556907.
- Clarke JL, Griffin TL, Lancashire ER, Adab P, Parry JM, Pallan MJ. WAVES study trial investigators . Parent and child perceptions of school-based obesity prevention in England: a qualitative study. BMC Public Health 2015;15. http://dx.doi.org/10.1186/s12889-015-2567-7.
- Clarke J, Fletcher B, Lancashire E, Pallan M, Adab P. The views of stakeholders on the role of the primary school in preventing childhood obesity: a qualitative systematic review. Obes Rev 2013;14:975-88. http://dx.doi.org/10.1111/obr.12058.
- Clarke JL, Pallan MJ, Lancashire ER, Adab P. Obesity prevention in English primary schools: headteacher perspectives. Health Promot Int 2017;32:490-9. https://doi.org/10.1093/heapro/dav113.
- Unlocking Potential: A Manifesto For PE And School Sport. Loughborough: Youth Sport Trust; 2015.
- The Daily Mile Foundation . The Daily Mile 2016 n.d. http://thedailymile.co.uk/ (accessed 13 July 2016).
- Davison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obes Rev 2001;2:159-71. https://doi.org/10.1046/j.1467-789x.2001.00036.x.
Appendix 1 Height measurement standardised operating procedure
Photographs reproduced with the permission of the University of Birmingham.
Appendix 2 Weight measurement standardised operating procedure
Photographs reproduced with the permission of the University of Birmingham.
Appendix 3 Pupil measurement data sheet
Appendix 4 Waist circumference standardised operating procedure
Photographs reproduced with the permission of the University of Birmingham.
Appendix 5 Skinfold measurement standardised operating procedure
Photographs reproduced with the permission of the University of Birmingham.
Appendix 6 Actiheart fitting standardised operation procedure
Photographs reproduced with the permission of the University of Birmingham.
Appendix 7 Child questionnaire administration standardised operating procedure
Appendix 8 Blood pressure measurement standardised operating procedure
Photographs reproduced with the permission of the University of Birmingham.
Appendix 9 Baseline school questionnaire
Appendix 10 Generic signposting sheet
Appendix 11 Anonymised school-specific signposting sheet
Appendix 12 Take 10 suitable activities chart
Appendix 13 Cooking workshop teacher training: presentation slides
Available on request from either Professor Peymane Adab (p.adab@bham.ac.uk) or Dr Emma Lancashire (e.r.lancashire@bham.ac.uk).
Appendix 14 Cooking workshop: parent invitation letters
Appendix 15 Breakfast cooking workshop: poster
Appendix 16 Lunch and snacks cooking workshop: poster
Appendix 17 Evening meals cooking workshop: poster
Appendix 18 Breakfast cooking workshop lesson 1: teacher presentation slides
Appendix 19 Breakfast cooking workshop lesson 2: teacher presentation slides
Appendix 20 Breakfast cooking workshop lesson 3: teacher presentation slides
Appendix 21 Breakfast cooking workshop lesson 4: teacher presentation slides
Appendix 22 Lunch and snacks cooking workshop lesson 1: teacher presentation slides
Appendix 23 Lunch and snacks cooking workshop lesson 2: teacher presentation slides
Appendix 24 Lunch and snacks cooking workshop lesson 3: teacher presentation slides
Appendix 25 Evening meals cooking workshop lesson 1: teacher presentation slides
Appendix 26 Evening meals cooking workshop lesson 2: teacher presentation slides
Appendix 27 Evening meals cooking workshop lesson 3: teacher presentation slides
Appendix 28 Breakfast cooking workshop: session plan
Appendix 29 Lunch and snacks cooking workshop: session plan
Appendix 30 Evening meals cooking workshop: session plan
Appendix 31 Breakfast cooking workshop: teacher presentation slides
Appendix 32 Lunch and snacks cooking workshop: teacher presentation slides
Appendix 33 Evening meals cooking workshop: teacher presentation slides
Appendix 34 Breakfast cooking workshop: parent information sheet
Appendix 35 Lunch and snacks cooking workshop: parent information
Appendix 36 Evening meals cooking workshop: parent information
Appendix 37 Breakfast cooking workshop lesson 2 activity: bread snap cards
Appendix 38 Breakfast cooking workshop interactive game 2: sugar cards
Appendix 39 Breakfast cooking workshop interactive game 2: answers
Sugar game answers.
| Item | Sugar teaspoons (1 teaspoon = 6 g of sugar) |
|---|---|
| A can of cola | 6 |
| A carton of orange juice | 3½ |
| A bottle of fruit juice drink | 3½ |
| A carton of juicy water | 2½ |
| A bowl of chocolate-flavour toasted rice | 2 |
| A glass of diluted squash | 1 |
| A bowl of wholewheat cereal biscuits | A tiny bit |
| A glass of water | 0 |
Appendix 40 Breakfast cooking workshop interactive game 3: treat or everyday cards
Appendix 41 Lunch and snacks cooking workshop lesson 1: guess the snack activity
Appendix 42 Lunch and snacks cooking workshop lesson 2: healthy snacks word search puzzle activity
Appendix 43 Lunch and snacks cooking workshop lesson 3: design a healthy school trip packed lunch – activity
Appendix 44 Lunch and snacks cooking workshop interactive game 2: packing a healthy lunch treat or everyday – activity
Appendix 45 Evening meals cooking workshop lesson 2: Bert’s healthy habits day story – activity
Appendix 46 Evening meals cooking workshop lesson 3: matching cooking skill words to pictures – activity
Appendix 47 Evening meals cooking workshop interactive game 1: food group bingo
Appendix 49 Villa Vitality healthy eating session plan
Appendix 50 Villa Vitality children’s activity booklet
Appendix 51 Observation checklist for Activate
Appendix 52 Observation checklist for breakfast cooking workshop
Appendix 53 Observation checklist for Villa Vitality session 1
Appendix 54 Cooking workshop parent evaluation: breakfast
Appendix 55 Villa Vitality teacher evaluation questionnaire: session 1
Appendix 56 Villa Vitality teacher evaluation questionnaire: whole programme
Appendix 57 Physical activity logbook: September to December 2012
Appendix 58 Cooking workshop logbook: breakfast
Appendix 59 Villa Vitality logbook
Appendix 60 Prespecified subgroup analyses
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusted)a | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 571 (n = 262, unadjusted) | 0.24 (1.03) | 0.34 (1.16) | 0.19 (1.07) | 0.30 (1.14) | 0.007 (–0.230 to 0.244) | 0.953 | –0.103 (–0.246 to 0.040) | 0.157 | –0.104 (–0.265 to 0.056) | 0.203 |
| N = 548 (n = 257, partially adjusted) | ||||||||||
| N = 402 (n = 188, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 572 (n = 257, unadjusted) | 118.07 (5.34) | 126.93 (5.75) | 117.50 (5.12) | 126.54 (5.71) | 0.393 (–0.559 to 1.345) | 0.418 | 0.098 (–0.672 to 0.867) | 0.803 | –0.100 (–0.853 to 0.653) | 0.795 |
| N = 549 (n = 257, partially adjusted) | ||||||||||
| N = 403 (n = 188, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 522 (n = 237, unadjusted) | 0.81 (0.97) | 1.00 (1.26) | 0.72 (1.09) | 0.92 (1.25) | 0.076 (–0.141 to 0.292) | 0.494 | 0.010 (–0.269 to 0.288) | 0.945 | –0.042 (–0.231 to 0.147) | 0.666 |
| N = 493 (n = 229, partially adjusted) | ||||||||||
| N = 389 (n = 183, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 475 (n = 216, unadjusted) | 28.45 (23.90–34.20) | 31.48 (24.65–41.35) | 27.95 (22.75–34.15) | 28.45 (23.70–38.00) | 1.688 (–0.397 to 3.772) | 0.113 | 0.555 (–0.174 to 1.283) | 0.136 | 0.972 (–0.119 to 2.063) | 0.081 |
| N = 411 (n = 190, partially adjusted) | ||||||||||
| N = 331 (n = 153, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 568 (n = 262, unadjusted) | 20.61 (4.28) | 20.87 (5.73) | 20.26 (4.63) | 20.06 (5.99) | 0.556 (–0.751 to 1.863) | 0.405 | –0.044 (–0.986 to 0.899) | 0.928 | 0.054 (–0.967 to 1.075) | 0.917 |
| N = 544 (n = 256, partially adjusted) | ||||||||||
| N = 398 (n = 187, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 508 (n = 229, unadjusted) | 6912 (5964–7868) | 7196 (6188–8376) | 7031 (6144–7964) | 7386 (6489–8462) | –192.002 (–454.492 to 70.488) | 0.152 | –150.680 (–373.252 to 71.892) | 0.185 | –113.857 (–346.691 to 118.978) | 0.338 |
| N = 471 (n = 217, partially adjusted) | ||||||||||
| N = 392 (n = 181, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 404 (n = 182, unadjusted) | 96.48 (20.69) | 95.26 (23.68) | 97.64 (24.08) | 96.23 (25.67) | –0.272 (–6.674 to 6.131) | 0.934 | 0.449 (–6.806 to 7.703) | 0.903 | –0.054 (–6.289 to 6.180) | 0.986 |
| N = 338 (n = 160, partially adjusted) | ||||||||||
| N = 320 (n = 151, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 574 (n = 264, unadjusted) | 73.91 (63.04–83.70) | 76.09 (65.22–86.96) | 73.91 (60.87–82.61) | 76.09 (67.39–86.96) | –0.573 (–3.555 to 2.409) | 0.706 | –0.882 (–5.040 to 3.276) | 0.678 | 1.010 (–3.127 to 5.147) | 0.632 |
| N = 550 (n = 259, partially adjusted) | ||||||||||
| N = 406 (n = 190, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 565 (n = 260, unadjusted) | 0.85 (0.12) | 0.88 (0.11) | 0.83 (0.14) | 0.86 (0.09) | 0.020 (–0.003 to 0.043) | 0.089 | 0.021 (–0.003 to 0.045) | 0.081 | 0.026 | 0.074 |
| N = 527 (n = 245, partially adjusted) | (–0.003 to 0.055) | |||||||||
| N = 388 (n = 178, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 571 (n = 262, unadjusted) | 26 (9.00) | 33 (12.60) | 33 (9.85) | 39 (12.62) | –0.000 (–0.040 to 0.057) | 0.992 | –0.012 (–0.058 to 0.063) | 0.707 | –0.009 (–0.046 to 0.046) | 0.717 |
| N = 548 (n = 257, partially adjusted) | ||||||||||
| N = 402 (n = 188, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 571 (n = 262, unadjusted) | 49 (16.96) | 69 (26.34) | 69 (20.60) | 74 (23.95) | 0.023 (–0.053 to 0.131) | 0.596 | 0.012 (–0.061 to 0.115) | 0.774 | 0.037 (–0.048 to 0.161) | 0.441 |
| N = 548 (n = 257, partially adjusted) | ||||||||||
| N = 402 (n = 188, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 508 (n = 229, unadjusted) | 151 (59.22) | 114 (49.78) | 193 (64.33) | 131 (46.95) | 0.028 (–0.077 to 0.161) | 0.628 | 0.035 (–0.072 to 0.170) | 0.553 | 0.105 (0.027 to 0.194) | 0.007 |
| N = 471 (n = 217, partially adjusted) | ||||||||||
| N = 392 (n = 181, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 402 (n = 181, unadjusted) | 87 (39.55) | 97 (53.59) | 133 (51.35) | 120 (54.30) | –0.007 (–0.126 to 0.146) | 0.918 | 0.034 (–0.108 to 0.224) | 0.678 | 0.006 (–0.119 to 0.169) | 0.937 |
| N = 333 (n = 157, partially adjusted) | ||||||||||
| N = 316 (n = 149, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 389 (n = 190, unadjusted) | –0.00 (1.42) | 0.15 (1.52) | –0.03 (1.33) | 0.03 (1.46) | 0.112 (–0.213 to 0.437) | 0.498 | –0.080 (–0.253 to 0.093) | 0.367 | –0.077 (–0.265 to 0.111) | 0.422 |
| N = 369 (n = 179, partially adjusted) | ||||||||||
| N = 259 (n = 127, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 389 (n = 179, unadjusted) | 118.47 (5.79) | 126.94 (6.20) | 118.17 (5.23) | 126.76 (5.58) | 0.175 (–0.778 to 1.128) | 0.719 | –0.002 (–0.734 to 0.730) | 0.995 | 0.104 (–0.653 to 0.862) | 0.788 |
| N = 369 (n = 179, partially adjusted) | ||||||||||
| N = 259 (n = 127, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 365 (n = 180, unadjusted) | 0.50 (1.43) | 1.01 (1.42) | 0.49 (1.47) | 0.76 (1.49) | 0.252 (–0.040 to 0.544) | 0.091 | 0.168 (–0.064 to 0.401) | 0.156 | 0.194 (–0.005 to 0.393) | 0.056 |
| N = 329 (n = 156, partially adjusted) | ||||||||||
| N = 237 (n = 111, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 333 (n = 167, unadjusted) | 29.50 (22.95–37.40) | 31.55 (26.00–50.00) | 28.65 (23.20–38.35) | 31.70 (23.65–47.25) | 0.712 (–2.240 to 3.663) | 0.637 | 0.130 (–0.736 to 0.997) | 0.768 | 0.051 (–0.713 to 0.814) | 0.896 |
| N = 283 (n = 136, partially adjusted) | ||||||||||
| N = 210 (n = 103, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 385 (n = 190, unadjusted) | 21.41 (5.89) | 22.32 (7.60) | 21.75 (5.46) | 21.84 (6.48) | 0.480 (–0.927 to 1.888) | 0.503 | –0.152 (–1.155 to 0.851) | 0.767 | –0.445 (–1.462 to 0.572) | 0.391 |
| N = 359 (n = 177, partially adjusted) | ||||||||||
| N = 254 (n = 126, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 351 (n = 171, unadjusted) | 6384 (5307–8035) | 7137 (6151–8418) | 6644 (5303–7969) | 6564 (5505–7517) | 501.593 (–84.445 to 1087.631) | 0.093 | 339.206 (–192.377 to 870.788) | 0.211 | 232.957 (–303.526 to 769.440) | 0.395 |
| N = 293 (n = 138, partially adjusted) | ||||||||||
| N = 246 (n = 116, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 269 (n = 129, unadjusted) | 96.30 (23.05) | 87.93 (23.53) | 95.10 (25.21) | 89.57 (26.25) | –1.898 (–9.123 to 5.327) | 0.607 | –2.979 (–10.374 to 4.416) | 0.430 | –3.155 (–10.945 to 4.635) | 0.427 |
| N = 223 (n = 106, partially adjusted) | ||||||||||
| N = 198 (n = 98, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 374 (n = 174, unadjusted) | 69.57 (57.61–80.43) | 76.09 (65.22–82.61) | 71.74 (58.70–80.43) | 76.09 (65.22–84.78) | –0.702 (–3.839 to 2.435) | 0.661 | –0.728 (–5.037 to 3.581) | 0.740 | 0.702 (–3.121 to 4.526) | 0.719 |
| N = 349 (n = 164, partially adjusted) | ||||||||||
| N = 242 (n = 113, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 370 (n = 174, unadjusted) | 0.83 (0.14) | 0.86 (0.11) | 0.79 (0.16) | 0.86 (0.11) | –0.003 (–0.036 to 0.030) | 0.856 | –0.011 (–0.040 to 0.019) | 0.478 | –0.010 (–0.045 to 0.024) | 0.560 |
| N = 341 (n = 163, partially adjusted) | ||||||||||
| N = 235 (n = 112, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 389 (n = 190, unadjusted) | 27 (12.98) | 33 (17.37) | 23 (10.95) | 31 (15.58) | 0.018 (–0.038 to 0.101) | 0.584 | –0.050 (–0.093 to 0.018) | 0.129 | 0.013 (–0.049 to 0.108) | 0.728 |
| N = 369 (n = 179, partially adjusted) | ||||||||||
| N = 259 (n = 127, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 389 (n = 190, unadjusted) | 44 (21.15) | 54 (28.42) | 38 (18.10) | 51 (25.63) | 0.028 (–0.045 to 0.126) | 0.495 | –0.041 (–0.100 to 0.039) | 0.281 | –0.044 (–0.112 to 0.055) | 0.339 |
| N = 369 (n = 179, partially adjusted) | ||||||||||
| N = 259 (n = 127, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 351 (n = 171, unadjusted) | 94 (54.65) | 75 (43.86) | 119 (65.75) | 94 (52.22) | –0.084 (–0.183 to 0.045) | 0.184 | –0.096 (–0.204 to 0.046) | 0.167 | –0.096 (–0.208 to 0.055) | 0.189 |
| N = 293 (n = 138, partially adjusted) | ||||||||||
| N = 246 (n = 116, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 272 (n = 131, unadjusted) | 67 (44.08) | 61 (46.56) | 76 (46.06) | 64 (45.39) | 0.007 (–0.138 to 0.220) | 0.933 | –0.003 (–0.148 to 0.210) | 0.975 | 0.009 (–0.136 to 0.220) | 0.916 |
| N = 227 (n = 108, partially adjusted) | ||||||||||
| N = 201 (n = 100, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 94 (n = 48, unadjusted) | 0.72 (1.36) | 0.79 (1.27) | 0.55 (1.05) | 0.58 (1.11) | 0.209 (–0.272 to 0.690) | 0.394 | –0.044 (–0.296 to 0.208) | 0.732 | –0.372 (–0.652 to –0.091) | 0.009 |
| N = 90 (n = 46, partially adjusted) | ||||||||||
| N = 50 (n = 22, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 94 (n = 47, unadjusted) | 121.72 (5.89) | 130.64 (6.79) | 120.76 (5.51) | 129.55 (5.76) | 1.092 (–1.514 to 3.698) | 0.412 | 0.332 (–0.991 to 1.656) | 0.623 | –0.066 (–1.222 to 1.090) | 0.911 |
| N = 91 (n = 47, partially adjusted) | ||||||||||
| N = 50 (n = 22, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 81 (n = 41, unadjusted) | 1.24 (1.52) | 1.32 (1.54) | 0.85 (1.00) | 1.00 (1.03) | 0.326 (–0.227 to 0.880) | 0.248 | –0.047 (–0.426 to 0.332) | 0.808 | –0.689 (–1.044 to –0.333) | < 0.001 |
| N = 76 (n = 38, partially adjusted) | ||||||||||
| N = 47 (n = 20, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 71 (n = 37, unadjusted) | 28.52 (23.75–40.65) | 32.40 (21.05–43.65) | 26.30 (22.50–36.50) | 28.65 (23.55–42.90) | 0.889 (–5.676 to 7.454) | 0.791 | –0.375 (–1.627 to 0.878) | 0.558 | –0.701 (–1.947 to 0.545) | 0.270 |
| N = 61 (n = 32, partially adjusted) | ||||||||||
| N = 37 (n = 18, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 90 (n = 48, unadjusted) | 24.09 (6.53) | 24.01 (7.57) | 22.66 (4.65) | 22.34 (6.57) | 1.909 (–1.711 to 5.530) | 0.301 | –0.535 (–2.789 to 1.719) | 0.642 | –2.198 (–4.278 to –0.118) | 0.038 |
| N = 85 (n = 46, partially adjusted) | ||||||||||
| N = 46 (n = 22, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 81 (n = 41, unadjusted) | 7777 (6522–8511) | 6990 (5717–8066) | 7007 (5173–7964) | 7224 (6262–8949) | –561.581 (–1369.895 to 246.733) | 0.173 | –511.770 (–1151.293 to 127.753) | 0.117 | –417.325 (–1350.508 to 515.858) | 0.381 |
| N = 66 (n = 30, partially adjusted) | ||||||||||
| N = 47 (n = 21, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 57 (n = 26, unadjusted) | 87.88 (27.15) | 82.69 (21.86) | 76.39 (17.45) | 80.68 (20.74) | 2.011 (–7.291 to 11.314) | 0.672 | 0.822 (–11.456 to 13.100) | 0.896 | 1.183 (–8.801 to 11.167) | 0.816 |
| N = 44 (n = 20, partially adjusted) | ||||||||||
| N = 38 (n = 15, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 94 (n = 48, unadjusted) | 69.57 (58.70–80.43) | 73.91 (63.04–85.87) | 73.91 (60.87–84.78) | 71.74 (65.22–78.26) | 0.531 (–7.105 to 8.166) | 0.892 | 0.690 (–7.572 to 8.952) | 0.870 | –5.222 (–23.734 to 13.289) | 0.580 |
| N = 91 (n = 47, partially adjusted) | ||||||||||
| N = 50 (n = 22, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 94 (n = 48, unadjusted) | 0.81 (0.16) | 0.86 (0.12) | 0.83 (0.15) | 0.85 (0.10) | 0.005 (–0.050 to 0.059) | 0.866 | 0.007 (–0.047 to 0.062) | 0.788 | –0.035 (–0.087 to 0.017) | 0.189 |
| N = 89 (n = 45, partially adjusted) | ||||||||||
| N = 48 (n = 20, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 94 (n = 48, unadjusted) | 14 (23.33) | 12 (25.00) | 13 (25.49) | 10 (21.74) | 0.033 (–0.081 to 0.240) | 0.650 | –0.090 (–0.155 to 0.034) | 0.125 | –0.028 (–0.171 to 0.479) | 0.837 |
| N = 90 (n = 46, partially adjusted) | ||||||||||
| N = 50 (n = 22, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 94 (n = 48, unadjusted) | 23 (38.33) | 17 (35.42) | 16 (31.37) | 15 (32.61) | 0.028 (–0.121 to 0.285) | 0.767 | –0.097 (–0.210 to 0.115) | 0.294 | –0.188 (–0.286 to 0.081) | 0.122 |
| N = 90 (n = 46, partially adjusted) | ||||||||||
| N = 50 (n = 22, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 81 (n = 41, unadjusted) | 24 (55.81) | 19 (46.34) | 28 (65.12) | 25 (62.50) | –0.162 (–0.317 to 0.071) | 0.150 | –0.147 (–0.282 to 0.036) | 0.105 | –0.210 (–0.414 to 0.161) | 0.213 |
| N = 66 (n = 30, partially adjusted) | ||||||||||
| N = 47 (n = 21, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 56 (n = 26, unadjusted) | 22 (56.41) | 17 (65.38) | 15 (45.45) | 16 (53.33) | 0.121 (–0.076 to 0.400) | 0.263 | 0.074 (–0.164 to 0.482) | 0.612 | 0.446 (0.010 to 1.255) | 0.043 |
| N = 42 (n = 20, partially adjusted) | ||||||||||
| N = 37 (n = 15, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | |||||
|---|---|---|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjusted modelb | ||||
| South Asian | African Caribbean | South Asian | African Caribbean | South Asian | African Caribbean | |
| Continuous outcomes | ||||||
| BMI-z | 0.567 | 0.389 | 0.961 | 0.667 | 0.819 | 0.678 |
| Height (cm) | 0.734 | 0.606 | 0.959 | 0.621 | 0.906 | 0.692 |
| Waist z-score | 0.280 | 0.340 | 0.779 | 0.583 | 0.344 | 0.758 |
| Sum of four skinfolds (mm)c,d | 0.588 | 0.931 | 0.213 | 0.486 | 0.188 | 0.635 |
| Body fat % | 0.797 | 0.523 | 0.712 | 0.773 | 0.592 | 0.851 |
| Energy intake (kJ in 24 hours)e | 0.044 | 0.360 | 0.141 | 0.380 | 0.193 | 0.339 |
| PA energy expenditure (kJ/kg/day) | 0.916 | 0.816 | 0.645 | 0.701 | 0.433 | 0.616 |
| PedsQL total scoref | 0.745 | 0.642 | 0.769 | 0.543 | 0.949 | 0.907 |
| CHU9D utility score | 0.120 | 0.597 | 0.026 | 0.659 | 0.034 | 0.080 |
| Binary outcomes | ||||||
| Obeseg | 0.693 | 0.698 | 0.632 | 0.185 | 0.847 | 0.438 |
| Obese/overweightg | 0.971 | 0.970 | 0.157 | 0.145 | 0.186 | 0.028 |
| Five or more portions of fruit and vegetablesh | 0.183 | 0.100 | 0.185 | 0.072 | 0.059 | 0.076 |
| Achieving ≥ 60 minutes of PAi | 0.861 | 0.269 | 0.775 | 0.716 | 0.543 | 0.290 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 874 (n = 199, unadjusted) | 0.18 (1.15) | 0.38 (1.24) | 0.15 (1.20) | 0.23 (1.27) | 0.126 (–0.064–0.317) | 0.193 | 0.024 (–0.094–0.142) | 0.691 | 0.007 (–0.108–0.121) | 0.911 |
| N = 832 (n = 191, partially adjusted) | ||||||||||
| N = 587 (n = 143, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 875 (n = 192, unadjusted) | 118.64 (5.87) | 127.30 (6.55) | 118.18 (5.38) | 127.03 (5.75) | 0.276 (–0.421–0.972) | 0.438 | –0.319 (–0.901–0.262) | 0.282 | –0.367 (–0.982–0.248) | 0.242 |
| N = 834 (n = 192, partially adjusted) | ||||||||||
| N = 588 (n = 143, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 809 (n = 186, unadjusted) | 0.75 (1.22) | 1.05 (1.46) | 0.66 (1.25) | 0.87 (1.32) | 0.173 (–0.005–0.350) | 0.057 | –0.031 (–0.388–0.326) | 0.864 | –0.030 (–0.222–0.162) | 0.760 |
| N = 752 (n = 173, partially adjusted) | ||||||||||
| N = 564 (n = 136, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 731 (n = 171, unadjusted) | 26.35 (21.43–32.63) | 31.25 (26.00–42.15) | 28.10 (23.00–36.60) | 29.40 (23.63–41.67) | 1.890 (0.409 to 3.372) | 0.012 | 0.912 (0.240 to 1.585) | 0.008 | 0.807 (0.080 to 1.534) | 0.030 |
| N = 626 (n = 145, partially adjusted) | ||||||||||
| N = 476 (n = 116, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 861 (n = 199, unadjusted) | 20.92 (5.09) | 21.94 (6.43) | 20.95 (5.22) | 20.87 (6.30) | 1.022 (0.104–1.939) | 0.029 | 0.741 (0.011–1.471) | 0.047 | 0.642 (–0.118–1.402) | 0.098 |
| N = 805 (n = 189, partially adjusted) | ||||||||||
| N = 572 (n = 141, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 785 (n = 180, unadjusted) | 6936 (5922–8098) | 6931 (5801–8066) | 6911 (5804–7964) | 7074 (5963–8233) | –214.756 (–611.465 to 181.953) | 0.289 | –193.957 (–559.700 to 171.786) | 0.299 | –308.111 (–607.526 to –8.696) | 0.044 |
| N = 694 (n = 165, partially adjusted) | ||||||||||
| N = 570 (n = 136, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 598 (n = 125, unadjusted) | 96.35 (21.87) | 89.90 | 94.08 (24.38) | 91.27 (25.42) | –2.330 (–7.835 to 3.176) | 0.407 | –2.893 (–8.788 to 3.002) | 0.336 | –3.072 (–9.081–2.937) | 0.316 |
| N = 497 (n = 108, partially adjusted) | (21.07) | |||||||||
| N = 450 (n = 102, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 854 (n = 177, unadjusted) | 71.74 (58.70–80.43) | 76.09 (65.22–84.78) | 73.91 (60.87–82.61) | 76.09 (65.22–84.78) | –0.137 (–3.646 to 3.372) | 0.939 | 0.583 (–3.886 to 5.052) | 0.798 | 1.179 (–2.412 to 4.769) | 0.520 |
| N = 804 (n = 171, partially adjusted) | ||||||||||
| N = 566 (n = 124, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 841 (n = 176, unadjusted) | 0.83 (0.14) | 0.86 (0.11) | 0.82 (0.14) | 0.86 (0.10) | 0.865 (0.834 to 0.896) | < 0.001 | 0.221 (0.014 to 0.427) | 0.036 | 0.317 (0.173 to 0.462) | < 0.001 |
| N = 775 (n = 164, partially adjusted) | ||||||||||
| N = 545 (n = 117, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 874 (n = 199, unadjusted) | 26 (11.40) | 32 (16.08) | 87 (11.89) | 100 (14.81) | 0.013 (–0.023–0.058) | 0.517 | 0.001 (–0.041–0.060) | 0.954 | 0.012 (–0.036–0.081) | 0.664 |
| N = 832 (n = 191, partially adjusted) | ||||||||||
| N = 587 (n = 143, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 874 (n = 199, unadjusted) | 46 (20.18) | 57 (28.64) | 150 (20.49) | 167 (24.74) | 0.039 (–0.020–0.113) | 0.213 | 0.033 (–0.061–0.173) | 0.546 | 0.024 (–0.051–0.128) | 0.569 |
| N = 832 (n = 191, partially adjusted) | ||||||||||
| N = 587 (n = 143, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 785 (n = 180, unadjusted) | 129 (62.62) | 75 (41.67) | 405 (64.80) | 297 (49.09) | –0.073 (–0.184 to 0.077) | 0.303 | –0.067 (–0.188 to 0.102) | 0.392 | –0.030 (–0.121 to 0.084) | 0.576 |
| N = 694 (n = 165, partially adjusted) | ||||||||||
| N = 570 (n = 136, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 596 (n = 126, unadjusted) | 87 (48.88) | 71 (56.35) | 276 (49.55) | 234 (49.79) | 0.051 (–0.055 to 0.182) | 0.377 | 0.075 (–0.059 to 0.252) | 0.303 | 0.037 (–0.077–0.183) | 0.556 |
| N = 495 (n = 109, partially adjusted) | ||||||||||
| N = 447 (n = 103, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 827 (n = 152, unadjusted) | 0.36 (1.21) | 0.39 (1.31) | 0.15 (1.20) | 0.23 (1.27) | 0.135 (–0.071 to 0.341) | 0.200 | –0.170 (–0.332 to –0.009) | 0.039 | –0.178 (–0.359 to 0.004) | 0.055 |
| N = 790 (n = 149, partially adjusted) | ||||||||||
| N = 556 (n = 112, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 828 (n = 149, unadjusted) | 118.36 (5.50) | 127.60 (6.17) | 118.18 (5.38) | 127.03 (5.75) | 0.573 (–0.957 to 2.103) | 0.463 | 0.272 (–0.983 to 1.527) | 0.671 | –0.003 (–1.199 to 1.194) | 0.997 |
| N = 791 (n = 149, partially adjusted) | ||||||||||
| N = 557 (n = 112, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 766 (n = 143, unadjusted) | 0.96 (1.17) | 1.25 (1.25) | 0.66 (1.25) | 0.87 (1.32) | 0.358 (0.040 to 0.676) | 0.027 | 0.094 (–0.161 to 0.350) | 0.468 | 0.098 (–0.089 to 0.285) | 0.303 |
| N = 715 (n = 136, partially adjusted) | ||||||||||
| N = 532 (n = 104, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 693 (n = 133, unadjusted) | 31.55 (25.63–38.55) | 30.80 (24.70–48.60) | 28.10 (23.00–36.60) | 29.40 (23.63–41.67) | 1.835 (–0.489 to 4.158) | 0.122 | –0.012 (–0.816 to 0.793) | 0.977 | 0.277 (–0.574 to 1.127) | 0.523 |
| N = 606 (n = 125, partially adjusted) | ||||||||||
| N = 457 (n = 97, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 814 (n = 152, unadjusted) | 21.35 (5.15) | 21.16 (6.39) | 20.95 (5.22) | 20.87 (6.30) | 0.203 (–0.830 to 1.236) | 0.700 | –0.772 (–1.972 to 0.427) | 0.207 | –0.550 (–1.904 to 0.804) | 0.426 |
| N = 765 (n = 149, partially adjusted) | ||||||||||
| N = 543 (n = 112, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 742 (n = 137, unadjusted) | 6808 (5832–8064) | 7191 (6188–8209) | 6911 (5804–7964) | 7074 (5963–8233) | 141.872 (–244.429 to 528.173) | 0.472 | 78.522 (–230.509 to 387.553) | 0.618 | –157.393 (–484.957 to 170.171) | 0.346 |
| N = 659 (n = 130, partially adjusted) | ||||||||||
| N = 537 (n = 103, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 589 (n = 116, unadjusted) | 97.78 (23.58) | 90.65 (23.30) | 94.08 (24.38) | 91.27 (25.42) | –1.019 (–6.401 to 4.363) | 0.711 | –2.457 (–9.219 to 4.305) | 0.476 | –3.771 (–10.656 to 3.114) | 0.283 |
| N = 487 (n = 98, partially adjusted) | ||||||||||
| N = 440 (n = 92, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 830 (n = 153, unadjusted) | 71.74 (60.87–82.61) | 71.74 (60.87–82.61) | 73.91 (60.87–82.61) | 76.09 (65.22–84.78) | –2.914 (–5.546 to –0.282) | 0.030 | –3.175 (–7.192 to 0.842) | 0.121 | –3.520 (–7.503 to 0.462) | 0.083 |
| N = 783 (n = 150, partially adjusted) | ||||||||||
| N = 555 (n = 113, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 817 (n = 152, unadjusted) | 0.83 (0.13) | 0.86 (0.12) | 0.82 (0.14) | 0.86 (0.10) | 0.857 (0.825 to 0.889) | < 0.001 | 0.237 (0.118 to 0.357) | < 0.001 | 0.254 (0.104 to 0.404) | 0.001 |
| N = 755 (n = 144, partially adjusted) | ||||||||||
| N = 535 (n = 107, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 827 (n = 152, unadjusted) | 25 (14.79) | 26 (17.11) | 87 (11.89) | 100 (14.81) | 0.023 (–0.019 to 0.079) | 0.318 | –0.053 (–0.094 to 0.016) | 0.111 | 0.012 (–0.031 to 0.068) | 0.631 |
| N = 790 (n = 149, partially adjusted) | ||||||||||
| N = 556 (n = 112, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 827 (n = 152, unadjusted) | 41 (24.26) | 44 (28.95) | 150 (20.49) | 167 (24.74) | 0.042 (–0.013 to 0.110) | 0.143 | –0.046 (–0.101 to 0.030) | 0.210 | 0.041 (–0.027 to 0.130) | 0.265 |
| N = 790 (n = 149, partially adjusted) | ||||||||||
| N = 556 (n = 112, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 742 (n = 137, unadjusted) | 96 (61.15) | 72 (52.55) | 405 (64.80) | 297 (49.09) | 0.035 (–0.077 to 0.177) | 0.576 | 0.038 (–0.077 to 0.183) | 0.554 | 0.095 (–0.004 to 0.214) | 0.060 |
| N = 659 (n = 130, partially adjusted) | ||||||||||
| N = 537 (n = 103, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 586 (n = 116, unadjusted) | 57 (43.18) | 53 (45.69) | 276 (49.55) | 234 (49.79) | –0.047 (–0.168 to 0.119) | 0.534 | 0.019 (–0.131 to 0.233) | 0.829 | –0.059 (–0.160 to 0.075) | 0.352 |
| N = 483 (n = 97, partially adjusted) | ||||||||||
| N = 435 (n = 91, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 898 (n = 223, unadjusted) | 0.19 (1.33) | 0.27 (1.44) | 0.15 (1.20) | 0.23 (1.27) | 0.038 (–0.176–0.253) | 0.727 | –0.082 (–0.218–0.054) | 0.238 | –0.058 (–0.177–0.062) | 0.344 |
| N = 857 (n = 216, partially adjusted) | ||||||||||
| N = 582 (n = 138, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 900 (n = 217, unadjusted) | 118.79 (5.44) | 127.28 (5.62) | 118.18 (5.38) | 127.03 (5.75) | 0.255 (–0.471 to 0.982) | 0.491 | –0.165 (–0.735 to 0.404) | 0.569 | –0.294 (–0.970–0.381) | 0.394 |
| N = 859 (n = 217, partially adjusted) | ||||||||||
| N = 583 (n = 138, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 822 (n = 199, unadjusted) | 0.65 (1.30) | 0.92 (1.33) | 0.66 (1.25) | 0.87 (1.32) | 0.045 (–0.155 to 0.245) | 0.662 | 0.016 (–0.229–0.262) | 0.897 | 0.001 (–0.169–0.171) | 0.992 |
| N = 760 (n = 181, partially adjusted) | ||||||||||
| N = 556 (n = 128, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 744 (n = 184, unadjusted) | 28.38 (23.82–35.38) | 31.75 (23.27–42.30) | 28.10 (23.00–36.60) | 29.40 (23.63–41.67) | 0.437 (–1.497 to 2.370) | 0.658 | 0.243 (–0.515 to 1.001) | 0.530 | 0.337 (–0.585 to 1.259) | 0.473 |
| N = 632 (n = 151, partially adjusted) | ||||||||||
| N = 470 (n = 111, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 885 (n = 223, unadjusted) | 21.58 (5.69) | 22.08 (7.19) | 20.95 (5.22) | 20.87 (6.30) | 1.098 (–0.073 to 2.269) | 0.066 | 0.100 (–0.805–1.005) | 0.829 | 0.081 (–0.836–0.999) | 0.862 |
| N = 831 (n = 215, partially adjusted) | ||||||||||
| N = 569 (n = 138, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 795 (n = 190, unadjusted) | 6926 (5805–7971) | 7328 (6258–8785) | 6911 (5804–7964) | 7074 (5963–8233) | 430.562 (–88.214 to 949.337) | 0.104 | 290.758 (–132.734 to 714.250) | 0.178 | 393.089 (–49.579 to 835.758) | 0.082 |
| N = 683 (n = 154, partially adjusted) | ||||||||||
| N = 564 (n = 130, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 627 (n = 154, unadjusted) | 95.52 (24.15) | 93.96 (25.90) | 94.08 (24.38) | 91.27 (25.42) | 2.082 (–2.314 to 6.478) | 0.353 | 2.224 (–2.529 to 6.977) | 0.359 | 0.012 (–4.318–4.341) | 0.996 |
| N = 518 (n = 129, partially adjusted) | ||||||||||
| N = 464 (n = 116, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 901 (n = 224, unadjusted) | 71.74 (60.87–82.61) | 76.09 (65.91–86.96) | 73.91 (60.87–82.61) | 76.09 (65.22–84.78) | 0.642 (–1.903 to 3.187) | 0.621 | 0.373 (–3.001 to 3.747) | 0.828 | 1.662 (–1.986 to 5.310) | 0.372 |
| N = 850 (n = 217, partially adjusted) | ||||||||||
| N = 580 (n = 138, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 887 (n = 222, unadjusted) | 0.84 (0.13) | 0.88 (0.10) | 0.82 (0.14) | 0.86 (0.10) | 0.025 (0.003 to 0.047) | 0.028 | 0.021 (0.000 to 0.043) | 0.050 | 0.029 (0.010 to 0.049) | 0.004 |
| N = 822 (n = 211, partially adjusted) | ||||||||||
| N = 562 (n = 134, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 898 (n = 223, unadjusted) | 33 (12.55) | 35 (15.70) | 87 (11.89) | 100 (14.81) | 0.009 (–0.033 to 0.066) | 0.714 | –0.051 (–0.093 to 0.020) | 0.133 | –0.025 (–0.063 to 0.030) | 0.333 |
| N = 857 (n = 216, partially adjusted) | ||||||||||
| N = 582 (n = 138, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 898 (n = 223, unadjusted) | 58 (22.05) | 64 (28.70) | 150 (20.49) | 167 (24.74) | 0.040 (–0.015 to 0.107) | 0.166 | –0.031 (–0.093 to 0.056) | 0.441 | –0.030 (–0.090 to 0.051) | 0.420 |
| N = 857 (n = 216, partially adjusted) | ||||||||||
| N = 582 (n = 138, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 795 (n = 190, unadjusted) | 111 (55.78) | 97 (51.05) | 405 (64.80) | 297 (49.09) | 0.020 (–0.065 to 0.122) | 0.673 | –0.000 (–0.083 to 0.099) | 0.997 | –0.016 (–0.091 to 0.073) | 0.703 |
| N = 683 (n = 154, partially adjusted) | ||||||||||
| N = 564 (n = 130, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 624 (n = 154, unadjusted) | 84 (46.41) | 83 (53.90) | 276 (49.55) | 234 (49.79) | 0.028 (–0.086 to 0.174) | 0.664 | 0.040 (–0.083 to 0.200) | 0.563 | 0.027 (–0.080 to 0.162) | 0.654 |
| N = 514 (n = 128, partially adjusted) | ||||||||||
| N = 460 (n = 116, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | |||||
|---|---|---|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | ||||
| Low fidelity | Medium fidelity | Low fidelity | Medium fidelity | Low fidelity | Medium fidelity | |
| Continuous outcomes | ||||||
| BMI-z | 0.333 | 0.911 | 0.141 | 0.021 | 0.274 | 0.013 |
| Height (cm) | 0.965 | 0.720 | 0.638 | 0.362 | 0.945 | 0.415 |
| Waist z-score | 0.235 | 0.237 | 0.816 | 0.539 | 0.851 | 0.362 |
| Sum of four skinfolds (mm)c,d | 0.093 | 0.999 | 0.163 | 0.055 | 0.213 | 0.098 |
| Body fat % | 0.865 | 0.088 | 0.154 | 0.014 | 0.165 | 0.026 |
| Energy intake (kJ in 24 hours)e | 0.024 | 0.118 | 0.047 | 0.172 | 0.005 | 0.241 |
| PA energy expenditure (kJ/kg/day) | 0.061 | 0.670 | 0.071 | 0.901 | 0.168 | 0.995 |
| PedsQL total scoref | 0.674 | 0.164 | 0.952 | 0.169 | 0.839 | 0.030 |
| CHU9D utility score | 0.269 | 0.658 | 0.447 | 0.501 | 0.207 | 0.440 |
| Binary outcomes | ||||||
| Obeseg | 0.878 | 0.668 | 0.602 | 0.192 | 0.984 | 0.350 |
| Obese/overweightg | 0.986 | 0.927 | 0.576 | 0.192 | 0.965 | 0.166 |
| Five or more portions of fruit and vegetablesh | 0.231 | 0.214 | 0.200 | 0.140 | 0.367 | 0.028 |
| Achieving ≥ 60 minutes of PAi | 0.754 | 0.221 | 0.862 | 0.684 | 0.999 | 0.343 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 640 (n = 280, unadjusted) | 0.35 (1.36) | 0.50 (1.47) | 0.13 (1.25) | 0.25 (1.29) | 0.253 (0.059 to 0.446) | 0.011 | –0.076 (–0.194 to 0.043) | 0.210 | –0.098 (–0.227 to 0.031) | 0.138 |
| N = 618 (n = 272, partially adjusted) | ||||||||||
| N = 432 (n = 193, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 640 (n = 272, unadjusted) | 119.32 (5.54) | 128.22 (6.08) | 118.86 (5.40) | 127.72 (5.82) | 0.500 (–0.360 to 1.359) | 0.254 | –0.000 (–0.599 to 0.599) | 0.999 | –0.137 (–0.769 to 0.494) | 0.670 |
| N = 618 (n = 272, partially adjusted) | ||||||||||
| N = 432 (n = 193, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 601 (n = 266, unadjusted) | 0.77 (1.27) | 1.15 (1.36) | 0.61 (1.23) | 0.82 (1.32) | 0.329 (0.135 to 0.523) | 0.001 | 0.083 (–0.070 to 0.236) | 0.288 | 0.070 (–0.045 to 0.185) | 0.233 |
| N = 568 (n = 252, partially adjusted) | ||||||||||
| N = 418 (n = 186, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 542 (n = 245, unadjusted) | 25.70 (21.30–32.80) | 28.70 (21.90–40.35) | 25.80 (21.40–32.10) | 25.70 (21.70–34.50) | 1.674 (0.192 to 3.156) | 0.027 | 0.331 (–0.205 to 0.867) | 0.226 | 0.362 (–0.189 to 0.914) | 0.198 |
| N = 476 (n = 219, partially adjusted) | ||||||||||
| N = 353 (n = 167, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 631 (n = 280, unadjusted) | 20.86 (5.19) | 21.24 (7.23) | 20.21 (4.72) | 19.63 (5.89) | 1.607 (0.668 to 2.546) | 0.001 | 0.283 (–0.500 to 1.067) | 0.479 | 0.210 (–0.533 to 0.953) | 0.579 |
| N = 598 (n = 270, partially adjusted) | ||||||||||
| N = 423 (n = 192, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 572 (n = 254, unadjusted) | 7151 (6126–8300) | 7193 (6129–8477) | 7119 (5998–8223) | 7207 (5938–8303) | 77.484 (–355.031 to 509.999) | 0.725 | 36.778 (–339.655 to 413.212) | 0.848 | 18.341 (–395.820 to 432.502) | 0.931 |
| N = 498 (n = 219, partially adjusted) | ||||||||||
| N = 411 (n = 183, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 439 (n = 192, unadjusted) | 103.42 (23.84) | 98.01 (24.10) | 100.36 (25.02) | 97.25 (25.43) | 0.726 (–4.619 to 6.070) | 0.790 | –2.907 (–8.665 to 2.850) | 0.322 | –3.761 (–9.128 to 1.605) | 0.170 |
| N = 367 (n = 165, partially adjusted) | ||||||||||
| N = 328 (n = 150, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 628 (n = 267, unadjusted) | 70.65 (59.98–82.61) | 76.09 (63.04–84.78) | 73.91 (60.87–84.78) | 76.09 (67.39–84.78) | –1.748 (–4.124 to 0.627) | 0.149 | –1.679 (–4.821 to 1.462) | 0.295 | –1.715 (–5.076 to 1.646) | 0.317 |
| N = 601 (n = 260, partially adjusted) | ||||||||||
| N = 420 (n = 182, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 617 (n = 265, unadjusted) | 0.83 (0.14) | 0.86 (0.11) | 0.82 (0.15) | 0.86 (0.11) | 0.006 (–0.017 to 0.028) | 0.633 | 0.005 (–0.018 to 0.028) | 0.662 | 0.008 (–0.016 to 0.033) | 0.506 |
| N = 579 (n = 253, partially adjusted) | ||||||||||
| N = 406 (n = 176, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 640 (n = 280, unadjusted) | 50 (15.20) | 59 (21.07) | 51 (13.04) | 57 (15.83) | 0.049 (0.009 to 0.100) | 0.015 | –0.025 (–0.057 to 0.018) | 0.233 | 0.012 (–0.030 to 0.067) | 0.623 |
| N = 618 (n = 272, partially adjusted) | ||||||||||
| N = 432 (n = 193, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 640 (n = 280, unadjusted) | 90 (27.36) | 99 (35.36) | 78 (19.95) | 87 (24.173) | 0.112 (0.043 to 0.197) | 0.001 | 0.020 (–0.040 to 0.097) | 0.558 | 0.042 (–0.034 to 0.146) | 0.314 |
| N = 618 (n = 272, partially adjusted) | ||||||||||
| N = 432 (n = 193, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 572 (n = 254, unadjusted) | 157 (57.30) | 109 (42.91) | 206 (62.05) | 135 (42.45) | 0.010 (–0.088 to 0.136) | 0.862 | 0.011 (–0.086 to 0.136) | 0.843 | 0.033 (–0.055 to 0.142) | 0.497 |
| N = 498 (n = 219, partially adjusted) | ||||||||||
| N = 411 (n = 183, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 435 (n = 189, unadjusted) | 138 (56.10) | 116 (61.38) | 161 (54.76) | 141 (57.32) | 0.041 (–0.069 to 0.174) | 0.494 | 0.051 (–0.061 to 0.187) | 0.400 | –0.011 (–0.102 to 0.099) | 0.832 |
| N = 362 (n = 162, partially adjusted) | ||||||||||
| N = 323 (n = 148, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 609 (n = 294, unadjusted) | 0.11 (1.10) | 0.18 (1.17) | 0.16 (1.15) | 0.20 (1.25) | –0.038 (–0.281 to 0.206) | 0.762 | –0.041 (–0.170 to 0.089) | 0.539 | –0.054 (–0.200 to 0.093) | 0.472 |
| N = 579 (n = 284, partially adjusted) | ||||||||||
| N = 405 (n = 200, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 611 (n = 286, unadjusted) | 117.95 (5.59) | 126.56 (6.00) | 117.40 (5.25) | 126.23 (5.57) | 0.333 (–0.509 to 1.175) | 0.438 | –0.105 (–0.716 to 0.506) | 0.736 | –0.216 (–0.843 to 0.411) | 0.499 |
| N = 582 (n = 286, partially adjusted) | ||||||||||
| N = 406 (n = 200, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 550 (n = 262, unadjusted) | 0.76 (1.22) | 0.96 (1.36) | 0.71 (1.27) | 0.94 (1.32) | 0.015 (–0.249 to 0.279) | 0.912 | –0.020 (–0.277 to 0.236) | 0.876 | –0.022 (–0.241 to 0.197) | 0.842 |
| N = 501 (n = 238, partially adjusted) | ||||||||||
| N = 378 (n = 182, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 506 (n = 243, unadjusted) | 30.80 (25.70–38.35) | 33.60 (27.75–47.95) | 32.00 (25.45–40.42) | 34.00 (27.65–47.55) | 0.058 (–2.617 to 2.733) | 0.966 | 0.163 (–0.568 to 0.893) | 0.662 | 0.144 (–0.770 to 1.057) | 0.758 |
| N = 426 (n = 202, partially adjusted) | ||||||||||
| N = 330 (n = 156, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 605 (n = 294, unadjusted) | 21.72 (5.49) | 22.31 (6.18) | 21.79 (5.62) | 22.27 (6.47) | –0.102 (–1.381 to 1.178) | 0.876 | –0.215 (–1.098 to 0.669) | 0.634 | –0.074 (–1.108 to 0.959) | 0.888 |
| N = 571 (n = 283, partially adjusted) | ||||||||||
| N = 399 (n = 199, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 540 (n = 253, unadjusted) | 6644 (5596–7772) | 7052 (6100–8207) | 6719 (5591–7639) | 6918 (5971–8170) | 183.372 (–211.505 to 578.248) | 0.363 | 59.870 (–271.652 to 391.392) | 0.723 | 61.088 (–239.035 to 361.212) | 0.690 |
| N = 480 (n = 230, partially adjusted) | ||||||||||
| N = 392 (n = 186, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 429 (n = 203, unadjusted) | 89.38 (20.18) | 85.73 (21.76) | 86.98 (21.57) | 84.73 (23.80) | –0.006 (–5.197 to 5.184) | 0.998 | 2.126 (–3.031 to 7.284) | 0.419 | 0.220 (–4.566 to 5.006) | 0.928 |
| N = 357 (n = 170, partially adjusted) | ||||||||||
| N = 330 (n = 160, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 603 (n = 287, unadjusted) | 71.74 (60.87–82.61) | 76.09 (65.22–84.78) | 71.74 (58.70–80.43) | 73.91 (63.13–84.78) | 0.699 (–2.175 to 3.573) | 0.633 | 1.012 (–3.169 to 5.193) | 0.635 | 1.034 (–4.111 to 6.178) | 0.694 |
| N = 570 (n = 278, partially adjusted) | ||||||||||
| N = 397 (n = 193, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 598 (n = 285, unadjusted) | 0.84 (0.12) | 0.88 (0.11) | 0.81 (0.14) | 0.86 (0.10) | 0.015 (–0.004 to 0.034) | 0.112 | 0.012 (–0.008 to 0.032) | 0.245 | 0.013 (–0.009 to 0.034) | 0.250 |
| N = 551 (n = 266, partially adjusted) | ||||||||||
| N = 380 (n = 182, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 609 (n = 294, unadjusted) | 34 (10.27) | 34 (11.56) | 36 (10.56) | 43 (13.65) | –0.023 (–0.066 to 0.044) | 0.443 | –0.039 (–0.077 to 0.017) | 0.146 | –0.041 (–0.077 to 0.012) | 0.115 |
| N = 579 (n = 284, partially adjusted) | ||||||||||
| N = 405 (n = 200, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 609 (n = 294, unadjusted) | 55 (16.62) | 66 (22.45) | 72 (21.11) | 80 (25.40) | –0.029 (–0.085 to 0.044) | 0.396 | –0.037 (–0.092 to 0.038) | 0.303 | –0.057 (–0.105 to 0.007) | 0.078 |
| N = 579 (n = 284, partially adjusted) | ||||||||||
| N = 405 (n = 200, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 540 (n = 253, unadjusted) | 179 (62.15) | 109 (42.91) | 199 (67.92) | 135 (42.45) | –0.031 (–0.119 to 0.075) | 0.543 | –0.046 (–0.133 to 0.058) | 0.363 | –0.017 (–0.102 to 0.084) | 0.731 |
| N = 480 (n = 230, partially adjusted) | ||||||||||
| N = 392 (n = 186, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 431 (n = 207, unadjusted) | 90 (36.73) | 91 (43.96) | 115 (43.73) | 93 (41.52) | 0.015 (–0.100 to 0.172) | 0.822 | 0.044 (–0.086 to 0.226) | 0.556 | 0.022 (–0.096 to 0.184) | 0.749 |
| N = 358 (n = 172, partially adjusted) | ||||||||||
| N = 331 (n = 162, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | ||
|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | |
| Continuous outcomes | |||
| BMI-z | 0.027 | 0.669 | 0.619 |
| Height (cm) | 0.783 | 0.408 | 0.657 |
| Waist z-score | 0.044 | 0.278 | 0.879 |
| Sum of four skinfolds (mm)c,d | 0.166 | 0.453 | 0.559 |
| Body fat % | 0.023 | 0.163 | 0.651 |
| Energy intake (kJ in 24 hours)e | 0.703 | 0.962 | 0.720 |
| PA energy expenditure (kJ/kg/day) | 0.859 | 0.147 | 0.252 |
| PedsQL total scoref | 0.062 | 0.131 | 0.193 |
| CHU9D utility score | 0.330 | 0.392 | 0.943 |
| Binary outcomes | |||
| Obeseg | 0.069 | 0.038 | 0.084 |
| Obese/overweightg | 0.004 | 0.504 | 0.700 |
| Five or more portions of fruit and vegetablesh | 0.660 | 0.604 | 0.667 |
| Achieving ≥ 60 minutes of PAi | 0.885 | 0.902 | 0.713 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 897 (n = 428, unadjusted) | 0.21 (1.30) | 0.30 (1.39) | 0.20 (1.28) | 0.28 (1.33) | 0.015 (–0.202 to 0.232) | 0.892 | –0.089 (–0.215 to 0.037) | 0.165 | –0.082 (–0.212 to 0.048) | 0.215 |
| N = 865 (n = 415, partially adjusted) | ||||||||||
| N = 590 (n = 290, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 898 (n = 416, unadjusted) | 118.58 (5.56) | 127.42 (6.10) | 118.21 (5.44) | 127.12 (5.82) | 0.300 (–0.483 to 1.082) | 0.453 | –0.128 (–0.736 to 0.481) | 0.681 | –0.206 (–0.839 to 0.427) | 0.524 |
| N = 867 (n = 416, partially adjusted) | ||||||||||
| N = 591 (n = 290, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 824 (n = 400, unadjusted) | 0.71 (1.29) | 1.04 (1.34) | 0.72 (1.31) | 0.92 (1.39) | 0.120 (–0.093 to 0.333) | 0.269 | 0.046 (–0.154 to 0.246) | 0.653 | 0.010 (–0.148 to 0.169) | 0.898 |
| N = 770 (n = 373, partially adjusted) | ||||||||||
| N = 556 (n = 269, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 748 (n = 373, unadjusted) | 28.45 (22.95–35.30) | 30.75 (23.80–42.20) | 29.25 (23.60–37.70) | 29.70 (23.70–44.40) | –0.071 (–1.808 to 1.666) | 0.936 | 0.165 (–0.381 to 0.710) | 0.554 | 0.177 (–0.382 to 0.735) | 0.535 |
| N = 654 (n = 328, partially adjusted) | ||||||||||
| N = 482 (n = 246, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 888 (n = 428, unadjusted) | 21.28 (5.37) | 21.71 (6.96) | 21.42 (5.43) | 21.30 (6.65) | 0.289 (–0.772 to 1.349) | 0.594 | 0.079 (–0.772 to 0.930) | 0.856 | 0.109 (–0.795 to 1.013) | 0.813 |
| N = 843 (n = 414, partially adjusted) | ||||||||||
| N = 580 (n = 290, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 791 (n = 384, unadjusted) | 6978 (5887–8207) | 7116 (6074–8333) | 6895 (5730–7992) | 6959 (5855–8170) | 41.447 (–336.188 to 419.081) | 0.830 | 8.003 (–328.144 to 344.150) | 0.963 | –110.936 (–460.253 to 238.381) | 0.534 |
| N = 683 (n = 332, partially adjusted) | ||||||||||
| N = 559 (n = 269, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 601 (n = 288, unadjusted) | 97.05 (23.72) | 90.79 (23.23) | 93.05 (24.16) | 88.99 (24.66) | 1.519 (–3.338 to 6.375) | 0.540 | –0.008 (–4.672 to 4.657) | 0.997 | –0.627 (–5.052 to 3.798) | 0.781 |
| N = 504 (n = 243, partially adjusted) | ||||||||||
| N = 453 (n = 224, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 875 (n = 406, unadjusted) | 71.74 (58.70–82.61) | 76.09 (63.04–84.78) | 73.91 (60.87–82.61) | 73.91 (65.22–84.78) | –0.311 (–2.997 to 2.375) | 0.820 | –0.121 (–3.818 to 3.576) | 0.949 | –0.809 (–5.039 to 3.421) | 0.708 |
| N = 836 (n = 395, partially adjusted) | ||||||||||
| N = 567 (n = 271, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 864 (n = 406, unadjusted) | 0.83 (0.14) | 0.86 (0.11) | 0.81 (0.15) | 0.86 (0.11) | 0.011 (–0.011 to 0.032) | 0.339 | 0.007 (–0.014 to 0.029) | 0.518 | 0.005 (–0.016 to 0.027) | 0.626 |
| N = 809 (n = 387, partially adjusted) | ||||||||||
| N = 548 (n = 264, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 897 (n = 428, unadjusted) | 65 (13.18) | 73 (17.06) | 73 (13.96) | 80 (17.06) | –0.000 (–0.038 to 0.049) | 0.999 | –0.037 (–0.077 to 0.020) | 0.180 | 0.005 (–0.037 to 0.059) | 0.849 |
| N = 865 (n = 415, partially adjusted) | ||||||||||
| N = 590 (n = 290, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 897 (n = 428, unadjusted) | 114 (23.12) | 122 (28.50) | 116 (22.18) | 123 (26.23) | 0.023 (–0.026 to 0.082) | 0.389 | –0.014 (–0.065 to 0.050) | 0.642 | –0.000 (–0.054 to 0.067) | 0.998 |
| N = 865 (n = 415, partially adjusted) | ||||||||||
| N = 590 (n = 290, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 791 (n = 384, unadjusted) | 260 (61.47) | 175 (45.57) | 274 (63.57) | 185 (45.45) | 0.001 (–0.082 to 0.103) | 0.980 | –0.015 (–0.093 to 0.079) | 0.729 | –0.009 (–0.080 to 0.075) | 0.820 |
| N = 683 (n = 332, partially adjusted) | ||||||||||
| N = 559 (n = 269, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 602 (n = 290, unadjusted) | 184 (50.55) | 152 (52.41) | 189 (48.59) | 153 (49.04) | 0.034 (–0.069 to 0.162) | 0.550 | 0.045 (–0.062 to 0.178) | 0.445 | 0.020 (–0.076 to 0.138) | 0.713 |
| N = 502 (n = 242, partially adjusted) | ||||||||||
| N = 452 (n = 224, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 337 (n = 138, unadjusted) | 0.29 (1.09) | 0.43 (1.16) | –0.00 (1.01) | 0.11 (1.10) | 0.312 (0.023 to 0.601) | 0.035 | –0.007 (–0.169 to 0.156) | 0.933 | –0.032 (–0.302 to 0.238) | 0.816 |
| N = 318 (n = 133, partially adjusted) | ||||||||||
| N = 247 (n = 103, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 337 (n = 133, unadjusted) | 118.84 (5.71) | 127.11 (5.96) | 118.09 (5.24) | 126.86 (5.65) | 0.252 (–0.543 to 1.047) | 0.535 | –0.063 (–0.863 to 0.737) | 0.878 | –0.244 (–1.032 to 0.544) | 0.543 |
| N = 318 (n = 133, partially adjusted) | ||||||||||
| N = 247 (n = 103, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 314 (n = 122, unadjusted) | 0.95 (1.10) | 1.14 (1.15) | 0.52 (1.07) | 0.79 (1.14) | 0.356 (0.143 to 0.569) | 0.001 | 0.002 (–0.230 to 0.235) | 0.985 | 0.004 (–0.183 to 0.190) | 0.970 |
| N = 287 (n = 111, partially adjusted) | ||||||||||
| N = 240 (n = 99, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 288 (n = 109, unadjusted) | 29.13 (23.95–36.38) | 33.60 (26.70–50.50) | 26.90 (22.20–33.63) | 28.70 (23.60–36.80) | 4.878 (2.039 to 7.718) | 0.001 | 1.054 (0.173 to 1.936) | 0.019 | 1.262 (–0.084 to 2.609) | 0.066 |
| N = 239 (n = 89, partially adjusted) | ||||||||||
| N = 201 (n = 77, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 334 (n = 138, unadjusted) | 21.24 (4.97) | 21.95 (6.05) | 19.81 (4.48) | 19.89 (5.37) | 2.060 (0.936 to 3.183) | < 0.001 | 0.283 (–0.917 to 1.482) | 0.644 | 0.413 (–0.980 to 1.806) | 0.561 |
| N = 313 (n = 131, partially adjusted) | ||||||||||
| N = 242 (n = 101, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 310 (n = 118, unadjusted) | 6773 (5706–7748) | 7116 (6074–8333) | 6930 (5955–7946) | 6959 (5855–8170) | 375.273 (–208.371 to 958.916) | 0.208 | 251.091 (–121.287 to 623.469) | 0.186 | 297.274 (–121.874 to 716.422) | 0.165 |
| N = 287 (n = 112, partially adjusted) | ||||||||||
| N = 244 (n = 100, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 256 (n = 102, unadjusted) | 93.70 (21.54) | 93.74 (24.96) | 96.67 (24.93) | 96.18 (26.68) | –2.979 (–9.767 to 3.810) | 0.390 | –0.402 (–9.662 to 8.858) | 0.932 | –5.920 (–14.469 to 2.629) | 0.175 |
| N = 213 (n = 88, partially adjusted) | ||||||||||
| N = 205 (n = 86, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 340 (n = 139, unadjusted) | 73.91 (65.22–84.78) | 78.26 (65.91–84.78) | 73.91 (63.04–82.61) | 76.09 (67.39–86.96) | –1.113 (–4.182 to 1.956) | 0.477 | –1.441 (–5.374 to 2.492) | 0.473 | –0.966 (–5.359 to 3.426) | 0.666 |
| N = 320 (n = 134, partially adjusted) | ||||||||||
| N = 250 (n = 104, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 336 (n = 135, unadjusted) | 0.85 (0.12) | 0.86 (0.11) | 0.84 (0.14) | 0.86 (0.11) | 0.017 (–0.012 to 0.047) | 0.246 | 0.018 (–0.012 to 0.049) | 0.239 | 0.007 (–0.026 to 0.040) | 0.679 |
| N = 307 (n = 123, partially adjusted) | ||||||||||
| N = 238 (n = 94, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 337 (n = 138, unadjusted) | 18 (11.84) | 19 (13.77) | 14 (6.97) | 20 (10.05) | 0.037 (–0.012 to 0.114) | 0.163 | –0.061 (–0.079 to –0.030) | 0.001 | –0.061 (–0.083 to –0.020) | 0.009 |
| N = 318 (n = 133, partially adjusted) | ||||||||||
| N = 247 (n = 103, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 337 (n = 138, unadjusted) | 27 (17.76) | 40 (28.99) | 34 (16.92) | 43 (21.61) | 0.074 (–0.018 to 0.208) | 0.130 | –0.042 (–0.118 to 0.093) | 0.461 | –0.057 (–0.138 to 0.111) | 0.406 |
| N = 318 (n = 133, partially adjusted) | ||||||||||
| N = 247 (n = 103, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 310 (n = 118, unadjusted) | 67 (52.76) | 67 (56.78) | 129 (68.25) | 111 (57.81) | –0.010 (–0.142 to 0.161) | 0.894 | 0.049 (–0.091 to 0.230) | 0.526 | 0.088 (–0.058 to 0.274) | 0.260 |
| N = 287 (n = 112, partially adjusted) | ||||||||||
| N = 244 (n = 100, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 253 (n = 101, unadjusted) | 38 (32.48) | 53 (52.48) | 85 (52.47) | 78 (51.32) | –0.004 (–0.133 to 0.167) | 0.953 | 0.034 (–0.118 to 0.246) | 0.702 | –0.076 (–0.175 to 0.054) | 0.227 |
| N = 210 (n = 88, partially adjusted) | ||||||||||
| N = 202 (n = 86, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | ||
|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjusted modelb | |
| Continuous outcomes | |||
| BMI-z | 0.115 | 0.475 | 0.475 |
| Height (cm) | 0.934 | 0.430 | 0.545 |
| Waist z-score | 0.109 | 0.820 | 0.776 |
| Sum of four skinfolds (mm)c,d | 0.003 | 0.316 | 0.445 |
| Body fat % | 0.012 | 0.797 | 0.630 |
| Energy intake (kJ in 24 hours)e | 0.113 | 0.176 | 0.076 |
| PA energy expenditure (kJ/kg/day) | 0.214 | 0.990 | 0.952 |
| PedsQL total scoref | 0.769 | 0.689 | 0.884 |
| CHU9D utility score | 0.927 | 0.804 | 0.590 |
| Binary outcomes | |||
| Obeseg | 0.254 | 0.706 | 0.390 |
| Obese/overweightg | 0.331 | 0.208 | 0.451 |
| Five or more portions of fruit and vegetablesh | 0.904 | 0.562 | 0.655 |
| Achieving ≥ 60 minutes of PAi | 0.587 | 0.901 | 0.829 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 252 (n = 124, unadjusted) | 1.99 (0.81) | 2.04 (0.82) | 1.94 (0.73) | 2.05 (0.75) | –0.001 (–0.199 to 0.197) | 0.989 | –0.098 (–0.240 to 0.045) | 0.180 | –0.129 (–0.296 to 0.038) | 0.130 |
| N = 252 (n = 124, partially adjusted) | ||||||||||
| N = 169 (n = 89, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 252 (n = 124, unadjusted) | 121.72 (5.55) | 131.07 (5.89) | 120.74 (5.38) | 130.14 (5.83) | 0.924 (–0.424 to 2.272) | 0.179 | –0.025 (–0.792 to 0.742) | 0.950 | –0.654 (–1.441 to 0.134) | 0.104 |
| N = 252 (n = 124, partially adjusted) | ||||||||||
| N = 169 (n = 89, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 233 (n = 116, unadjusted) | 2.33 (0.96) | 2.60 (0.97) | 2.41 (0.89) | 2.62 (0.77) | –0.018 (–0.238 to 0.201) | 0.870 | –0.045 (–0.199 to 0.108) | 0.562 | –0.069 (–0.215 to 0.077) | 0.353 |
| N = 220 (n = 109, partially adjusted) | ||||||||||
| N = 153 (n = 81, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 190 (n = 98, unadjusted) | 43.40 (33.40–55.90) | 55.53 (38.90–73.95) | 44.75 (36.85–62.20) | 55.88 (42.67–72.47) | –3.386 (–8.362 to 1.589) | 0.182 | –0.197 (–1.498 to 1.104) | 0.767 | 0.256 (–1.576 to 2.088) | 0.784 |
| N = 165 (n = 87, partially adjusted) | ||||||||||
| N = 120 (n = 68, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 250 (n = 124, unadjusted) | 27.93 (5.70) | 29.28 (7.38) | 28.06 (5.17) | 29.63 (5.85) | –0.357 (–2.189 to 1.474) | 0.702 | –0.885 (–2.110 to 0.341) | 0.157 | –0.877 (–2.259 to 0.505) | 0.213 |
| N = 248 (n = 123, partially adjusted) | ||||||||||
| N = 167 (n = 89, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 224 (n = 111, unadjusted) | 7386 (6128–8339) | 7147 (5930–8351) | 6851 (5902–7975) | 7139 (5968–8308) | 23.929 (–551.127 to 598.984) | 0.935 | –12.946 (–500.822 to 474.929) | 0.959 | 158.159 (–282.745 to 599.063) | 0.482 |
| N = 203 (n = 102, partially adjusted) | ||||||||||
| N = 161 (n = 83, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 169 (n = 85, unadjusted) | 94.95 (21.50) | 90.41 (22.93) | 89.86 (22.55) | 90.49 (23.46) | –0.546 (–8.398 to 7.307) | 0.892 | –0.282 (–7.968 to 7.404) | 0.943 | –1.383 (–8.609 to 5.842) | 0.707 |
| N = 142 (n = 71, partially adjusted) | ||||||||||
| N = 129 (n = 67, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 246 (n = 118, unadjusted) | 67.39 (58.70–80.43) | 76.09 (65.22–82.61) | 73.91 (60.87–82.61) | 73.91 (63.04–84.78) | 0.803 (–2.278 to 3.884) | 0.609 | 1.674 (–2.357 to 5.706) | 0.416 | 1.570 (–3.942 to 7.082) | 0.577 |
| N = 244 (n = 118, partially adjusted) | ||||||||||
| N = 163 (n = 83, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 241 (n = 116, unadjusted) | 0.82 (0.14) | 0.88 (0.10) | 0.81 (0.13) | 0.85 (0.11) | 0.027 (0.001 to 0.054) | 0.046 | 0.025 (–0.002 to 0.052) | 0.067 | 0.032 (–0.001 to 0.065) | 0.057 |
| N = 232 (n = 112, partially adjusted) | ||||||||||
| N = 154 (n = 78, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 252 (n = 124, unadjusted) | 84 (57.93) | 84 (67.74) | 87 (58.00) | 88 (68.75) | –0.010 (–0.090 to 0.081) | 0.818 | –0.049 (–0.125 to 0.037) | 0.252 | –0.018 (–0.112 to 0.091) | 0.729 |
| N = 252 (n = 124, partially adjusted) | ||||||||||
| N = 169 (n = 89, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 252 (n = 124, unadjusted) | 145 (100) | 105 (84.68) | 150 (100) | 116 (90.63) | –0.059 (–0.148 to 0.040) | 0.230 | –0.074 (–0.167 to 0.030) | 0.154 | –0.099 (–0.194 to 0.009) | 0.071 |
| N = 252 (n = 124, partially adjusted) | ||||||||||
| N = 169 (n = 89, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 224 (n = 111, unadjusted) | 85 (66.93) | 57 (51.35) | 75 (63.03) | 51 (45.13) | 0.062 (–0.074 to 0.248) | 0.412 | 0.021 (–0.109 to 0.198) | 0.782 | 0.094 (–0.041 to 0.273) | 0.191 |
| N = 203 (n = 102, partially adjusted) | ||||||||||
| N = 161 (n = 83, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 171 (n = 86, unadjusted) | 44 (40.74) | 42 (48.84) | 49 (47.12) | 38 (44.71) | 0.041 (–0.120 to 0.282) | 0.666 | 0.125 (–0.055 to 0.396) | 0.203 | 0.077 (–0.080 to 0.309) | 0.385 |
| N = 145 (n = 72, partially adjusted) | ||||||||||
| N = 131 (n = 68, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcome | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 945 (n = 432, unadjusted) | –0.26 (0.82) | –0.17 (1.00) | –0.32 (0.80) | –0.20 (0.93) | 0.001 (–0.176 to 0.177) | 0.995 | –0.062 (–0.174 to 0.049) | 0.273 | –0.080 (–0.202 to 0.042) | 0.200 |
| N = 945 (n = 432, partially adjusted) | ||||||||||
| N = 668 (n = 304, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 946 (n = 432, unadjusted) | 117.79 (5.31) | 126.36 (5.80) | 117.51 (5.18) | 126.40 (5.49) | –0.043 (–0.744 to 0.657) | 0.903 | –0.082 (–0.671 to 0.506) | 0.784 | –0.119 (–0.696 to 0.457) | 0.684 |
| N = 946 (n = 432, partially adjusted) | ||||||||||
| N = 669 (n = 304, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 870 (n = 396, unadjusted) | 0.33 (0.92) | 0.59 (1.10) | 0.23 (0.89) | 0.47 (1.05) | 0.117 (–0.064 to 0.298) | 0.205 | 0.041 (–0.165 to 0.248) | 0.693 | 0.023 (–0.127 to 0.173) | 0.764 |
| N = 847 (n = 380, partially adjusted) | ||||||||||
| N = 643 (n = 287, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 815 (n = 373, unadjusted) | 26.75 (21.95–31.60) | 29.05 (22.85–36.75) | 26.45 (22.20–32.00) | 27.70 (22.50–34.40) | 0.851 (–0.690 to 2.392) | 0.279 | 0.268 (–0.183 to 0.720) | 0.244 | 0.282 (–0.219 to 0.783) | 0.270 |
| N = 737 (n = 334, partially adjusted) | ||||||||||
| N = 563 (n = 255, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 936 (n = 432, unadjusted) | 19.39 (3.20) | 19.48 (4.44) | 19.10 (3.28) | 18.77 (4.33) | 0.594 (–0.145 to 1.333) | 0.115 | 0.317 (–0.383 to 1.018) | 0.374 | 0.273 (–0.461 to 1.008) | 0.466 |
| N = 921 (n = 430, partially adjusted) | ||||||||||
| N = 655 (n = 302, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 840 (n = 379, unadjusted) | 6841 (5782–7948) | 7129 (6107–8319) | 6961 (5767–8004) | 7042 (5938–8149) | 110.696 (–215.404 to 436.797) | 0.506 | 65.915 (–219.587 to 351.418) | 0.651 | –52.801 (–351.824 to 246.221) | 0.729 |
| N = 759 (n = 344, partially adjusted) | ||||||||||
| N = 642 (n = 286, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 660 (n = 295, unadjusted) | 96.84 (23.61) | 92.32 (23.90) | 95.03 (24.70) | 91.61 (26.11) | 0.176 (–4.749 to 5.101) | 0.944 | –0.749 (–5.648 to 4.151) | 0.764 | –2.060 (–6.648 to 2.528) | 0.379 |
| N = 582 (n = 264, partially adjusted) | ||||||||||
| N = 529 (n = 243, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 933 (n = 418, unadjusted) | 71.74 (60.87–82.61) | 76.09 (65.22–84.78) | 73.91 (60.87–82.61) | 76.09 (65.22–84.78) | –1.157 (–3.655 to 1.342) | 0.364 | –1.458 (–4.824 to 1.909) | 0.396 | –1.165 (–4.673 to 2.343) | 0.515 |
| N = 924 (n = 418, partially adjusted) | ||||||||||
| N = 654 (n = 292, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 923 (n = 416, unadjusted) | 0.84 (0.13) | 0.86 (0.11) | 0.82 (0.15) | 0.86 (0.10) | 0.007 (–0.013 to 0.028) | 0.477 | 0.004 (–0.016 to 0.024) | 0.686 | 0.006 (–0.016 to 0.028) | 0.595 |
| N = 895 (n = 405, partially adjusted) | ||||||||||
| N = 632 (n = 280, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 945 (n = 432, unadjusted) | 0 (0.00) | 4 (0.93) | 0 (0.00) | 11 (2.14) | –0.012 (–0.018 to 0.004) | 0.109 | –0.013 (–0.018 to 0.003) | 0.081 | –0.014 (–0.019 to 0.003) | 0.078 |
| N = 945 (n = 432, partially adjusted) | ||||||||||
| N = 668 (n = 304, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 945 (n = 432, unadjusted) | 0 (0.00) | 53 (12.27) | 0 (0.00) | 45 (8.77) | 0.033 (–0.011 to 0.100) | 0.163 | 0.026 (–0.010 to 0.080) | 0.182 | 0.012 (–0.025 to 0.071) | 0.575 |
| N = 945 (n = 432, partially adjusted) | ||||||||||
| N = 668 (n = 304, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 840 (n = 379, unadjusted) | 247 (57.44) | 176 (46.44) | 317 (65.09) | 231 (50.11) | –0.037 (–0.120 to 0.064) | 0.449 | –0.031 (–0.114 to 0.071) | 0.528 | –0.015 (–0.078 to 0.059) | 0.682 |
| N = 759 (n = 344, partially adjusted) | ||||||||||
| N = 642 (n = 286, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 656 (n = 295, unadjusted) | 184 (48.04) | 155 (52.54) | 227 (50.11) | 182 (50.42) | 0.018 (–0.087 to 0.149) | 0.760 | 0.027 (–0.083 to 0.165) | 0.661 | –0.022 (–0.113 to 0.089) | 0.673 |
| N = 575 (n = 262, partially adjusted) | ||||||||||
| N = 523 (n = 242, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | ||
|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | |
| Continuous outcomes | |||
| BMI-z | 0.838 | 0.580 | 0.639 |
| Height (cm) | 0.204 | 0.637 | 0.015 |
| Waist z-score | 0.276 | 0.334 | 0.454 |
| Sum of four skinfolds (mm)c,d | 0.094 | 0.752 | 0.958 |
| Body fat % | 0.320 | 0.046 | 0.102 |
| Energy intake (kJ in 24 hours)e | 0.642 | 0.710 | 0.347 |
| PA energy expenditure (kJ/kg/day) | 0.931 | 0.787 | 0.830 |
| PedsQL total scoref | 0.297 | 0.189 | 0.368 |
| CHU9D utility score | 0.114 | 0.090 | 0.099 |
| Binary outcomes | |||
| Obeseg | 0.126 | 0.131 | 0.119 |
| Obese/overweightg | 0.075 | 0.075 | 0.193 |
| Five or more portions of fruit and vegetablesh | 0.247 | 0.634 | 0.382 |
| Achieving ≥ 60 minutes of PAi | 0.782 | 0.339 | 0.408 |
Follow-up 2
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 524 (n = 240, unadjusted) | 0.24 (1.03) | 0.43 (1.17) | 0.19 (1.07) | 0.32 (1.18) | 0.111 (–0.082 to 0.304) | 0.261 | 0.043 (–0.093 to 0.179) | 0.537 | –0.005 (–0.137 to 0.128) | 0.945 |
| N = 501 (n = 235, partially adjusted) | ||||||||||
| N = 378 (n = 177, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 524 (n = 235, unadjusted) | 118.07 (5.34) | 134.63 (6.10) | 117.50 (5.12) | 134.44 (6.19) | 0.209 (–0.984 to 1.402) | 0.732 | 0.008 (–0.730 to 0.746) | 0.983 | –0.117 (–0.752 to 0.519) | 0.719 |
| N = 501 (n = 235, partially adjusted) | ||||||||||
| N = 378 (n = 177, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 470 (n = 213, unadjusted) | 0.81 (0.97) | 1.15 (1.10) | 0.72 (1.09) | 0.88 (1.20) | 0.257 (0.022 to 0.493) | 0.032 | 0.190 (0.005 to 0.374) | 0.044 | 0.108 (–0.077 to 0.293) | 0.252 |
| N = 443 (n = 204, partially adjusted) | ||||||||||
| N = 361 (n = 168, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 404 (n = 182, unadjusted) | 28.45 (23.90–34.20) | 34.50 (26.15–48.75) | 27.95 (22.75–34.15) | 29.50 (23.80–43.00) | 3.480 (0.670 to 6.290) | 0.015 | 1.329 (0.487 to 2.172) | 0.002 | 1.063 (0.061 to 2.066) | 0.038 |
| N = 347 (n = 162, partially adjusted) | ||||||||||
| N = 290 (n = 136, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 512 (n = 238, unadjusted) | 20.61 (4.28) | 21.46 (6.24) | 20.26 (4.63) | 20.42 (6.73) | 1.028 (–0.123 to 2.178) | 0.080 | 0.674 (–0.238 to 1.587) | 0.148 | 0.321 (–0.677 to 1.319) | 0.529 |
| N = 490 (n = 233, partially adjusted) | ||||||||||
| N = 370 (n = 176, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 469 (n = 209, unadjusted) | 6912 (5964–7868) | 7656 (6567–8966) | 7031 (6144–7964) | 7939 (6919–9256) | –398.197 (–789.949 to –6.445) | 0.046 | –246.505 (–612.762 to 119.753) | 0.187 | –224.534 (–671.998 to 222.929) | 0.325 |
| N = 435 (n = 198, partially adjusted) | ||||||||||
| N = 361 (n = 167, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 324 (n = 140, unadjusted) | 96.48 (20.69) | 86.18 (23.15) | 97.64 (24.08) | 82.97 (21.68) | 3.116 (–2.466 to 8.698) | 0.274 | 2.260 (–3.016 to 7.536) | 0.401 | 3.227 (–2.505 to 8.958) | 0.270 |
| N = 276 (n = 125, partially adjusted) | ||||||||||
| N = 262 (n = 119, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 523 (n = 240, unadjusted) | 73.91 (63.04–83.70) | 82.61 (73.91–91.30) | 73.91 (60.87–82.61) | 82.61 (71.74–89.13) | 2.520 (–0.753 to 5.792) | 0.131 | 2.768 (–1.258 to 6.794) | 0.178 | 2.924 (–1.264 to 7.113) | 0.171 |
| N = 499 (n = 235, partially adjusted) | ||||||||||
| N = 378 (n = 177, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 518 (n = 238, unadjusted) | 0.85 (0.12) | 0.89 (0.09) | 0.83 (0.14) | 0.90 (0.09) | –0.002 (–0.026 to 0.021) | 0.847 | –0.004 (–0.029 to 0.022) | 0.771 | –0.006 (–0.033 to 0.021) | 0.666 |
| N = 482 (n = 224, partially adjusted) | ||||||||||
| N = 363 (n = 168, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 524 (n = 240, unadjusted) | 26 (9.00) | 40 (16.67) | 33 (9.85) | 44 (15.49) | 0.012 (–0.040 to 0.088) | 0.703 | 0.030 (–0.023 to 0.102) | 0.302 | 0.023 (–0.027 to 0.091) | 0.408 |
| N = 501 (n = 235, partially adjusted) | ||||||||||
| N = 378 (n = 177, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 524 (n = 240, unadjusted) | 49 (16.96) | 78 (32.50) | 69 (20.60) | 69 (24.30) | 0.082 (0.000 to 0.191) | 0.049 | 0.100 (0.003 to 0.236) | 0.043 | 0.073 (–0.006 to 0.180) | 0.075 |
| N = 501 (n = 235, partially adjusted) | ||||||||||
| N = 378 (n = 177, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 469 (n = 209, unadjusted) | 151 (59.22) | 120 (57.42) | 193 (64.33) | 139 (53.46) | 0.040 (–0.065 to 0.167) | 0.484 | 0.060 (–0.059 to 0.209) | 0.352 | 0.097 (–0.026 to 0.251) | 0.132 |
| N = 435 (n = 198, partially adjusted) | ||||||||||
| N = 361 (n = 167, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 327 (n = 142, unadjusted) | 87 (39.55) | 47 (33.10) | 133 (51.35) | 60 (32.43) | 0.007 (–0.091 to 0.145) | 0.909 | 0.036 (–0.083 to 0.216) | 0.608 | 0.081 (–0.059 to 0.301) | 0.304 |
| N = 277 (n = 126, partially adjusted) | ||||||||||
| N = 264 (n = 121, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 368 (n = 176, unadjusted) | –0.00 (1.42) | 0.32 (1.51) | –0.03 (1.33) | 0.24 (1.48) | 0.082 (–0.209 to 0.373) | 0.581 | –0.052 (–0.273 to 0.168) | 0.641 | –0.007 (–0.239 to 0.226) | 0.956 |
| N = 347 (n = 164, partially adjusted) | ||||||||||
| N = 244 (n = 115, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 369 (n = 164, unadjusted) | 118.47 (5.79) | 133.96 (7.02) | 118.17 (5.23) | 134.39 (6.41) | –0.433 (–1.577 to 0.710) | 0.458 | –0.700 (–1.673 to 0.273) | 0.159 | –0.799 (–1.866 to 0.268) | 0.142 |
| N = 348 (n = 164, partially adjusted) | ||||||||||
| N = 245 (n = 115, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 315 (n = 149, unadjusted) | 0.50 (1.43) | 1.07 (1.42) | 0.49 (1.47) | 0.80 (1.56) | 0.254 (–0.134 to 0.642) | 0.200 | 0.025 (–0.245 to 0.295) | 0.856 | –0.021 (–0.324 to 0.282) | 0.893 |
| N = 287 (n = 132, partially adjusted) | ||||||||||
| N = 212 (n = 98, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 262 (n = 124, unadjusted) | 29.50 (22.95–37.40) | 36.20 (25.32–56.23) | 28.65 (23.20–38.35) | 35.33 (25.45–53.25) | 0.103 (–4.085 to 4.290) | 0.962 | 0.039 (–0.988 to 1.067) | 0.940 | –0.056 (–0.854 to 0.741) | 0.890 |
| N = 220 (n = 102, partially adjusted) | ||||||||||
| N = 167 (n = 80, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 357 (n = 171, unadjusted) | 21.41 (5.89) | 23.68 (8.47) | 21.75 (5.46) | 22.84 (7.44) | 0.842 (–0.693 to 2.376) | 0.282 | 0.395 (–0.725 to 1.515) | 0.489 | 0.063 (–1.347 to 1.474) | 0.930 |
| N = 329 (n = 157, partially adjusted) | ||||||||||
| N = 233 (n = 112, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 334 (n = 158, unadjusted) | 6384 (5307–8035) | 7710 (6282–9181) | 6644 (5303–7969) | 8034 (6592–9511) | –322.904 (–1060.300 to 414.492) | 0.391 | –250.883 (–964.647 to 462.882) | 0.491 | –312.679 (–952.135 to 326.776) | 0.338 |
| N = 278 (n = 126, partially adjusted) | ||||||||||
| N = 231 (n = 107, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 229 (n = 108, unadjusted) | 96.30 (23.05) | 73.47 (18.86) | 95.10 (25.21) | 74.89 (23.41) | –1.414 (–6.707 to 3.879) | 0.601 | –2.520 (–8.923 to 3.883) | 0.441 | –2.723 (–8.718 to 3.272) | 0.373 |
| N = 186 (n = 84, partially adjusted) | ||||||||||
| N = 166 (n = 79, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 361 (n = 168, unadjusted) | 69.57 (57.61–80.43) | 80.43 (68.48–89.13) | 71.74 (58.70–80.43) | 80.43 (71.74–89.13) | –1.373 (–4.056 to 1.310) | 0.316 | –1.279 (–4.392 to 1.835) | 0.421 | –1.100 (–4.525 to 2.325) | 0.529 |
| N = 334 (n = 156, partially adjusted) | ||||||||||
| N = 237 (n = 111, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 364 (n = 175, unadjusted) | 0.83 (0.14) | 0.89 (0.10) | 0.79 (0.16) | 0.91 (0.08) | –0.023 (–0.040 to –0.006) | 0.010 | –0.026 (–0.045 to –0.008) | 0.006 | –0.019 (–0.043 to 0.005) | 0.112 |
| N = 333 (n = 162, partially adjusted) | ||||||||||
| N = 234 (n = 113, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 368 (n = 176, unadjusted) | 27 (12.73) | 40 (22.99) | 23 (10.95) | 39 (20.31) | 0.024 (–0.043 to 0.119) | 0.529 | –0.009 (–0.065 to 0.070) | 0.799 | 0.053 (–0.025 to 0.165) | 0.211 |
| N = 347 (n = 164, partially adjusted) | ||||||||||
| N = 244 (n = 115, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 368 (n = 176, unadjusted) | 44 (21.15) | 60 (34.09) | 38 (18.10) | 64 (33.33) | 0.008 (–0.071 to 0.110) | 0.867 | –0.037 (–0.117 to 0.073) | 0.465 | 0.009 (–0.084 to 0.134) | 0.872 |
| N = 347 (n = 164, partially adjusted) | ||||||||||
| N = 244 (n = 115, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 334 (n = 158, unadjusted) | 94 (54.65) | 89 (56.33) | 119 (65.75) | 103 (58.52) | –0.022 (–0.112 to 0.085) | 0.667 | 0.017 (–0.085 to 0.139) | 0.768 | 0.011 (–0.095 to 0.141) | 0.854 |
| N = 278 (n = 126, partially adjusted) | ||||||||||
| N = 231 (n = 107, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 232 (n = 109, unadjusted) | 67 (44.08) | 9 (8.26) | 76 (46.06) | 32 (26.02) | –0.178 (–0.214 to –0.114) | < 0.001 | –0.191 (–0.233 to –0.116) | < 0.001 | –0.200 (–0.241 to –0.122) | < 0.001 |
| N = 187 (n = 85, partially adjusted) | ||||||||||
| N = 167 (n = 80, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 78 (n = 42, unadjusted) | 0.72 (1.36) | 0.62 (1.28) | 0.55 (1.05) | 0.62 (1.30) | –0.002 (–0.512 to 0.509) | 0.995 | –0.177 (–0.443 to 0.090) | 0.194 | –0.613 (–1.053 to –0.173) | 0.006 |
| N = 75 (n = 40, partially adjusted) | ||||||||||
| N = 37 (n = 15, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 78 (n = 41, unadjusted) | 121.72 (5.89) | 137.78 (7.29) | 120.76 (5.51) | 137.96 (6.17) | –0.205 (–3.371 to 2.960) | 0.899 | –0.038 (–2.008 to 1.933) | 0.970 | –2.759 (–3.803 to –1.716) | 0.000 |
| N = 76 (n = 41, partially adjusted) | ||||||||||
| N = 37 (n = 15, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 57 (n = 27, unadjusted) | 1.24 (1.52) | 1.23 (1.27) | 0.85 (1.00) | 1.22 (1.25) | 0.010 (–0.647 to 0.666) | 0.977 | 0.049 (–0.463 to 0.562) | 0.850 | –1.029 (–1.417 to –0.641) | < 0.001 |
| N = 54 (n = 24, partially adjusted) | ||||||||||
| N = 31 (n = 11, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 55 (n = 25, unadjusted) | 28.52 (23.75–40.65) | 33.80 (22.70–45.45) | 26.30 (22.50–36.50) | 32.48 (22.85–63.80) | –0.946 (–11.454 to 9.562) | 0.860 | –1.761 (–3.590 to 0.068) | 0.059 | –3.485 (–5.497 to –1.473) | 0.001 |
| N = 50 (n = 23, partially adjusted) | ||||||||||
| N = 30 (n = 11, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 76 (n = 42, unadjusted) | 24.09 (6.53) | 23.95 (8.53) | 22.66 (4.65) | 22.72 (7.41) | 1.226 (–2.184 to 4.637) | 0.481 | –1.266 (–3.439 to 0.907) | 0.254 | –3.437 (–6.289 to –0.585) | 0.018 |
| N = 72 (n = 40, partially adjusted) | ||||||||||
| N = 36 (n = 15, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 60 (n = 28, unadjusted) | 7777 (6522–8511) | 7555 (6432–9043) | 7007 (5173–7964) | 7412 (6586–9074) | 115.763 (–530.825 to 762.350) | 0.726 | 21.388 (–502.475 to 545.250) | 0.936 | 751.522 (–933.493 to 2436.536) | 0.382 |
| N = 51 (n = 21, partially adjusted) | ||||||||||
| N = 33 (n = 12, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 39 (n = 16, unadjusted) | 87.88 (27.15) | 64.49 (15.70) | 76.39 (17.45) | 70.55 (18.58) | –6.052 (–14.675 to 2.570) | 0.169 | –14.565 (–27.441 to –1.689) | 0.027 | –15.800 (–29.817 to –1.782) | 0.027 |
| N = 27 (n = 10, partially adjusted) | ||||||||||
| N = 24 (n = 8, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 64 (n = 28, unadjusted) | 69.57 (58.70–80.43) | 80.43 (65.22–86.96) | 73.91 (60.87–84.78) | 78.26 (66.30–84.78) | –0.433 (–5.756 to 4.890) | 0.873 | –0.297 (–7.375 to 6.780) | 0.934 | 4.672 (–3.090 to 12.435) | 0.238 |
| N = 62 (n = 27, partially adjusted) | ||||||||||
| N = 35 (n = 13, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 77 (n = 41, unadjusted) | 0.81 (0.16) | 0.89 (0.10) | 0.83 (0.15) | 0.87 (0.11) | 0.022 (–0.031 to 0.075) | 0.414 | 0.030 (–0.025 to 0.084) | 0.282 | –0.024 (–0.068 to 0.019) | 0.272 |
| N = 74 (n = 39, partially adjusted) | ||||||||||
| N = 36 (n = 14, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 78 (n = 42, unadjusted) | 14 (23.33) | 11 (26.19) | 13 (25.49) | 10 (27.78) | –0.016 (–0.142 to 0.227) | 0.861 | –0.131 (–0.201 to –0.002) | 0.047 | –0.243 (–0.281 to 0.085) | 0.085 |
| N = 75 (n = 40, partially adjusted) | ||||||||||
| N = 37 (n = 15, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 78 (n = 42, unadjusted) | 23 (38.33) | 13 (30.95) | 16 (31.37) | 14 (38.89) | –0.079 (–0.212 to 0.153) | 0.424 | –0.193 (–0.282 to –0.038) | 0.021 | –0.349 (–0.391 to –0.123) | 0.017 |
| N = 75 (n = 40, partially adjusted) | ||||||||||
| N = 37 (n = 15, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 60 (n = 28, unadjusted) | 24 (55.81) | 11 (39.29) | 28 (65.12) | 20 (62.50) | –0.232 (–0.384 to 0.017) | 0.064 | –0.283 (–0.429 to –0.030) | 0.033 | –0.502 (–0.593 to –0.204) | 0.009 |
| N = 51 (n = 21, partially adjusted) | ||||||||||
| N = 33 (n = 12, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 40 (n = 16, unadjusted) | 22 (56.41) | 4 (25.00) | 15 (45.45) | 9 (37.50) | –0.125 (–0.290 to 0.358) | 0.460 | –0.004 (–0.224 to 0.914) | 0.985 | –0.282 (–0.293 to –0.130) | 0.016 |
| N = 27 (n = 10, partially adjusted) | ||||||||||
| N = 24 (n = 8, fully adjusted) | ||||||||||
| Variables | p-value of interaction term | |||||
|---|---|---|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | ||||
| South Asian | African Caribbean | South Asian | African Caribbean | South Asian | African Caribbean | |
| Continuous outcomes | ||||||
| BMI-z | 0.867 | 0.693 | 0.434 | 0.112 | 0.807 | 0.132 |
| Height (cm) | 0.427 | 0.834 | 0.538 | 0.873 | 0.699 | 0.246 |
| Waist z-score | 0.849 | 0.551 | 0.208 | 0.483 | 0.276 | 0.070 |
| Sum of four skinfolds (mm)c,d | 0.118 | 0.578 | 0.024 | 0.036 | 0.099 | 0.005 |
| Body fat % | 0.817 | 0.900 | 0.573 | 0.127 | 0.778 | 0.366 |
| Energy intake (kJ in 24 hours)e | 0.755 | 0.498 | 0.973 | 0.729 | 0.623 | 0.626 |
| PA energy expenditure (kJ/kg/day) | 0.444 | 0.073 | 0.399 | 0.006 | 0.327 | < 0.001 |
| PedsQL total scoref | 0.022 | 0.494 | 0.026 | 0.564 | 0.137 | 0.429 |
| CHU9D utility score | 0.082 | 0.447 | 0.090 | 0.418 | 0.148 | 0.859 |
| Binary outcomes | ||||||
| Obeseg | 0.885 | 0.715 | 0.670 | 0.505 | 0.822 | 0.598 |
| Obese/overweightg | 0.202 | 0.110 | 0.008 | 0.003 | 0.111 | 0.028 |
| Five or more portions of fruit and vegetablesh | 0.388 | 0.044 | 0.664 | 0.029 | 0.406 | 0.152 |
| Achieving ≥ 60 minutes of PAi | 0.001 | 0.445 | 0.002 | 0.839 | 0.001 | 0.267 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 800 (n = 179, unadjusted) | 0.18 (1.15) | 0.37 (1.30) | 0.15 (1.20) | 0.31 (1.32) | 0.045 (–0.103 to 0.193) | 0.554 | –0.036 (–0.147 to 0.075) | 0.528 | –0.064 (–0.168 to 0.040) | 0.231 |
| N = 760 (n = 171, partially adjusted) | ||||||||||
| N = 543 (n = 130, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 801 (n = 172, unadjusted) | 118.64 (5.87) | 135.08 (7.04) | 118.18 (5.38) | 134.86 (6.43) | 0.205 (–0.782 to 1.192) | 0.684 | –0.392 (–1.117 to 0.333) | 0.289 | –0.460 (–1.070 to 0.151) | 0.140 |
| N = 762 (n = 172, partially adjusted) | ||||||||||
| N = 544 (n = 130, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 691 (n = 147, unadjusted) | 0.75 (1.22) | 1.13 (1.21) | 0.66 (1.25) | 0.90 (1.35) | 0.214 (–0.027 to 0.454) | 0.081 | 0.056 (–0.111 to 0.222) | 0.511 | 0.005 (–0.181 to 0.191) | 0.959 |
| N = 644 (n = 135, partially adjusted) | ||||||||||
| N = 494 (n = 111, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 590 (n = 126, unadjusted) | 26.35 (21.43–32.63) | 32.98 (23.55–46.50) | 28.10 (23.00–36.60) | 31.93 (24.00–48.90) | 0.430 (–2.000 to 2.860) | 0.729 | 0.978 (0.475 to 1.480) | < 0.001 | 0.744 (0.053 to 1.436) | 0.035 |
| N = 501 (n = 111, partially adjusted) | ||||||||||
| N = 389 (n = 91, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 775 (n = 176, unadjusted) | 20.92 (5.09) | 22.52 (7.34) | 20.95 (5.22) | 21.58 (7.26) | 0.946 (–0.061 to 1.953) | 0.066 | 0.694 (–0.007 to 1.395) | 0.052 | 0.309 (–0.443 to 1.062) | 0.421 |
| N = 722 (n = 166, partially adjusted) | ||||||||||
| N = 519 (n = 126, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 704 (n = 142, unadjusted) | 6936 (5922–8098) | 7568 (6568–9342) | 6911 (5804–7964) | 7817 (6748–9212) | –72.826 (–590.405 to 444.754) | 0.783 | 22.890 (–431.282 to 477.061) | 0.921 | –121.248 (–564.137 to 321.641) | 0.592 |
| N = 628 (n = 134, partially adjusted) | ||||||||||
| N = 508 (n = 110, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 480 (n = 95, unadjusted) | 96.35 (21.87) | 76.43 (21.20) | 94.08 (24.38) | 78.60 (22.43) | –2.693 (–9.495 to 4.108) | 0.438 | –4.956 (–12.485 to 2.572) | 0.197 | –4.706 (–11.564 to 2.152) | 0.179 |
| N = 397 (n = 79, partially adjusted) | ||||||||||
| N = 360 (n = 77, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 771 (n = 150, unadjusted) | 71.74 (58.70–80.43) | 82.61 (71.74–89.13) | 73.91 (60.87–82.61) | 80.43 (71.74–89.13) | 1.597 (–2.477 to 5.671) | 0.442 | 2.274 (–2.329 to 6.876) | 0.333 | 2.785 (–0.328 to 5.898) | 0.080 |
| N = 721 (n = 143, partially adjusted) | ||||||||||
| N = 526 (n = 117, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 787 (n = 173, unadjusted) | 0.83 (0.14) | 0.90 (0.09) | 0.82 (0.14) | 0.90 (0.09) | 0.899 (0.878 to 0.920) | < 0.001 | 0.219 (0.084 to 0.354) | 0.001 | 0.298 (0.182 to 0.415) | < 0.001 |
| N = 723 (n = 160, partially adjusted) | ||||||||||
| N = 518 (n = 121, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 800 (n = 179, unadjusted) | 26 (11.40) | 32 (17.88) | 87 (11.89) | 112 (18.04) | –0.002 (–0.040 to 0.048) | 0.943 | 0.013 (–0.043 to 0.091) | 0.684 | 0.025 (–0.021 to 0.083) | 0.313 |
| N = 760 (n = 171, partially adjusted) | ||||||||||
| N = 543 (n = 130, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 800 (n = 179, unadjusted) | 46 (20.18) | 57 (31.84) | 150 (20.49) | 187 (30.11) | 0.017 (–0.028 to 0.071) | 0.480 | 0.030 (–0.038 to 0.114) | 0.423 | –0.009 (–0.067 to 0.063) | 0.790 |
| N = 760 (n = 171, partially adjusted) | ||||||||||
| N = 543 (n = 130, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 704 (n = 142, unadjusted) | 129 (62.62) | 76 (53.52) | 405 (64.80) | 317 (56.41) | –0.029 (–0.120 to 0.081) | 0.582 | 0.010 (–0.085 to 0.124) | 0.848 | –0.009 (–0.088 to 0.083) | 0.835 |
| N = 628 (n = 134, partially adjusted) | ||||||||||
| N = 508 (n = 110, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 488 (n = 95, unadjusted) | 87 (48.88) | 17 (17.89) | 276 (49.55) | 120 (30.53) | –0.131 (–0.229 to 0.090) | 0.180 | –0.141 (–0.237 to 0.089) | 0.166 | –0.139 (–0.235 to 0.082) | 0.160 |
| N = 400 (n = 79, partially adjusted) | ||||||||||
| N = 362 (n = 77, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 756 (n = 135, unadjusted) | 0.36 (1.21) | 0.56 (1.33) | 0.15 (1.20) | 0.31 (1.32) | 0.220 (–0.047 to 0.487) | 0.106 | –0.030 (–0.187 to 0.128) | 0.711 | –0.062 (–0.229 to 0.104) | 0.464 |
| N = 721 (n = 132, partially adjusted) | ||||||||||
| N = 513 (n = 100, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 757 (n = 132, unadjusted) | 118.36 (5.50) | 134.61 (6.54) | 118.18 (5.38) | 134.86 (6.43) | –0.242 (–1.249 to 0.766) | 0.638 | –0.163 (–1.074 to 0.748) | 0.726 | –0.566 (–1.412 to 0.280) | 0.190 |
| N = 722 (n = 132, partially adjusted) | ||||||||||
| N = 514 (n = 100, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 667 (n = 123, unadjusted) | 0.96 (1.17) | 1.29 (1.25) | 0.66 (1.25) | 0.90 (1.35) | 0.364 (0.111 to 0.617) | 0.005 | 0.147 (–0.069 to 0.362) | 0.183 | 0.091 (–0.150 to 0.333) | 0.459 |
| N = 624 (n = 115, partially adjusted) | ||||||||||
| N = 474 (n = 91, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 574 (n = 110, unadjusted) | 31.55 (25.63–38.55) | 35.05 (26.40–51.75) | 28.10 (23.00–36.60) | 31.93 (24.00–48.90) | 3.150 (–0.699 to 7.000) | 0.109 | 0.552 (–0.076 to 1.179) | 0.085 | 0.330 (–0.320 to 0.981) | 0.320 |
| N = 494 (n = 104, partially adjusted) | ||||||||||
| N = 381 (n = 83, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 733 (n = 134, unadjusted) | 21.35 (5.15) | 22.72 (7.04) | 20.95 (5.22) | 21.58 (7.26) | 1.084 (–0.378 to 2.546) | 0.146 | 0.434 (–0.782 to 1.650) | 0.484 | 0.400 (–0.968 to 1.769) | 0.566 |
| N = 688 (n = 132, partially adjusted) | ||||||||||
| N = 493 (n = 100, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 689 (n = 127, unadjusted) | 6808 (5832–8064) | 7508 (6244–8835) | 6911 (5804–7964) | 7817 (6748–9212) | –448.925 (–970.684 to 72.835) | 0.092 | –374.165 (–865.445 to 117.116) | 0.136 | –530.508 (–1135.051 to 74.034) | 0.085 |
| N = 613 (n = 119, partially adjusted) | ||||||||||
| N = 493 (n = 95, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 474 (n = 89, unadjusted) | 97.78 (23.58) | 85.65 (23.97) | 94.08 (24.38) | 78.60 (22.43) | 7.261 (1.436 to 13.086) | 0.015 | 4.245 (–0.641 to 9.132) | 0.089 | 3.335 (–3.087 to 9.758) | 0.309 |
| N = 395 (n = 77, partially adjusted) | ||||||||||
| N = 355 (n = 72, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 756 (n = 135, unadjusted) | 71.74 (60.87–82.61) | 80.43 (71.74–89.13) | 73.91 (60.87–82.61) | 80.43 (71.74–89.13) | 0.751 (–2.020 to 3.523) | 0.595 | 1.265 (–1.842 to 4.372) | 0.425 | –0.198 (–3.914 to 3.519) | 0.917 |
| N = 710 (n = 132, partially adjusted) | ||||||||||
| N = 509 (n = 100, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 748 (n = 134, unadjusted) | 0.83 (0.13) | 0.89 (0.09) | 0.82 (0.14) | 0.90 (0.09) | 0.893 (0.870 to 0.917) | < 0.001 | 0.152 (0.058 to 0.246) | 0.002 | 0.179 (0.092 to 0.265) | < 0.001 |
| N = 690 (n = 127, partially adjusted) | ||||||||||
| N = 493 (n = 96, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 756 (n = 135, unadjusted) | 25 (14.79) | 35 (25.93) | 87 (11.89) | 112 (18.04) | 0.079 (0.010 to 0.173) | 0.022 | 0.018 (–0.049 to 0.119) | 0.651 | 0.081 (0.016 to 0.167) | 0.011 |
| N = 721 (n = 132, partially adjusted) | ||||||||||
| N = 513 (n = 100, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 756 (n = 135, unadjusted) | 41 (24.26) | 51 (37.78) | 150 (20.49) | 187 (30.11) | 0.077 (–0.008 to 0.186) | 0.079 | 0.009 (–0.062 to 0.101) | 0.822 | 0.083 (0.007 to 0.178) | 0.030 |
| N = 721 (n = 132, partially adjusted) | ||||||||||
| N = 513 (n = 100, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 689 (n = 127, unadjusted) | 96 (61.15) | 69 (54.33) | 405 (64.80) | 317 (56.41) | –0.021 (–0.148 to 0.146) | 0.783 | –0.000 (–0.150 to 0.205) | 0.997 | 0.081 (–0.068 to 0.275) | 0.320 |
| N = 613 (n = 119, partially adjusted) | ||||||||||
| N = 493 (n = 95, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 483 (n = 90, unadjusted) | 57 (43.18) | 27 (30.00) | 276 (49.55) | 120 (30.53) | –0.005 (–0.093 to 0.120) | 0.923 | 0.058 (–0.053 to 0.216) | 0.351 | 0.077 (–0.048 to 0.262) | 0.266 |
| N = 399 (n = 78, partially adjusted) | ||||||||||
| N = 358 (n = 73, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 831 (n = 210, unadjusted) | 0.19 (1.33) | 0.38 (1.39) | 0.15 (1.20) | 0.31 (1.32) | 0.055 (–0.133 to 0.243) | 0.569 | –0.023 (–0.199 to 0.154) | 0.801 | 0.001 (–0.175 to 0.177) | 0.993 |
| N = 791 (n = 202, partially adjusted) | ||||||||||
| N = 542 (n = 129, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 832 (n = 202, unadjusted) | 118.79 (5.44) | 134.50 (6.48) | 118.18 (5.38) | 134.86 (6.43) | –0.361 (–1.527 to 0.804) | 0.544 | –0.821 (–1.885 to 0.243) | 0.131 | –0.873 (–1.865 to 0.118) | 0.084 |
| N = 792 (n = 202, partially adjusted) | ||||||||||
| N = 543 (n = 129, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 720 (n = 176, unadjusted) | 0.65 (1.30) | 1.08 (1.28) | 0.66 (1.25) | 0.90 (1.35) | 0.156 (–0.116 to 0.428) | 0.260 | 0.097 (–0.111 to 0.304) | 0.361 | 0.099 (–0.066 to 0.264) | 0.239 |
| N = 673 (n = 164, partially adjusted) | ||||||||||
| N = 501 (n = 118, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 609 (n = 145, unadjusted) | 28.38 (23.82–35.38) | 35.60 (25.50–50.70) | 28.10 (23.00–36.60) | 31.93 (24.00–48.90) | 2.261 (–0.561 to 5.084) | 0.116 | 0.550 (–0.430 to 1.530) | 0.271 | 0.766 (–0.432 to 1.964) | 0.210 |
| N = 509 (n = 119, partially adjusted) | ||||||||||
| N = 386 (n = 88, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 805 (n = 206, unadjusted) | 21.58 (5.69) | 22.39 (7.89) | 20.95 (5.22) | 21.58 (7.26) | 0.753 (–0.670 to 2.175) | 0.300 | –0.019 (–1.124 to 1.086) | 0.973 | –0.068 (–1.345 to 1.210) | 0.917 |
| N = 753 (n = 197, partially adjusted) | ||||||||||
| N = 521 (n = 128, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 746 (n = 184, unadjusted) | 6926 (5805–7971) | 7755 (6411–9153) | 6911 (5804–7964) | 7817 (6748–9212) | –135.158 (–590.471 to 320.154) | 0.561 | –57.112 (–488.917 to 374.694) | 0.795 | –164.351 (–589.455 to 260.753) | 0.449 |
| N = 642 (n = 148, partially adjusted) | ||||||||||
| N = 524 (n = 126, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 506 (n = 121, unadjusted) | 95.52 (24.15) | 77.80 (21.06) | 94.08 (24.38) | 78.60 (22.43) | –0.903 (–6.004 to 4.199) | 0.729 | –0.033 (–5.148 to 5.082) | 0.990 | –0.698 (–5.671 to 4.275) | 0.783 |
| N = 415 (n = 97, partially adjusted) | ||||||||||
| N = 371 (n = 88, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 831 (n = 210, unadjusted) | 71.74 (60.87–82.61) | 82.61 (71.74–89.13) | 73.91 (60.87–82.61) | 80.43 (71.74–89.13) | 0.732 (–2.454 to 3.917) | 0.653 | 0.548 (–3.166 to 4.261) | 0.772 | 1.827 (–0.811 to 4.464) | 0.175 |
| N = 780 (n = 202, partially adjusted) | ||||||||||
| N = 538 (n = 129, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 824 (n = 210, unadjusted) | 0.84 (0.13) | 0.89 (0.09) | 0.82 (0.14) | 0.90 (0.09) | 0.888 (0.872 to 0.904) | < 0.001 | 0.199 (0.090 to 0.308) | < 0.001 | 0.174 (0.054 to 0.295) | 0.005 |
| N = 762 (n = 199, partially adjusted) | ||||||||||
| N = 524 (n = 127, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 831 (n = 210, unadjusted) | 33 (12.55) | 41 (19.52) | 87 (11.89) | 112 (18.04) | 0.015 (–0.034 to 0.080) | 0.589 | –0.030 (–0.071 to 0.025) | 0.249 | –0.010 (–0.057 to 0.054) | 0.732 |
| N = 791 (n = 202, partially adjusted) | ||||||||||
| N = 542 (n = 129, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 831 (n = 210, unadjusted) | 58 (22.05) | 68 (32.38) | 150 (20.49) | 187 (30.11) | 0.023 (–0.041 to 0.102) | 0.518 | –0.022 (–0.103 to 0.091) | 0.664 | –0.027 (–0.102 to 0.077) | 0.567 |
| N = 791 (n = 202, partially adjusted) | ||||||||||
| N = 542 (n = 129, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 746 (n = 184, unadjusted) | 111 (55.78) | 108 (58.70) | 405 (64.80) | 317 (56.41) | 0.023 (–0.068 to 0.130) | 0.642 | 0.023 (–0.069 to 0.131) | 0.645 | –0.012 (–0.107 to 0.103) | 0.825 |
| N = 642 (n = 148, partially adjusted) | ||||||||||
| N = 524 (n = 126, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 515 (n = 122, unadjusted) | 84 (46.41) | 26 (21.31) | 276 (49.55) | 120 (30.53) | –0.093 (–0.191 to 0.088) | 0.249 | –0.109 (–0.206 to 0.081) | 0.201 | –0.113 (–0.228 to 0.167) | 0.314 |
| N = 418 (n = 97, partially adjusted) | ||||||||||
| N = 374 (n = 89, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | |||||
|---|---|---|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | ||||
| Low fidelity | Medium fidelity | Low fidelity | Medium fidelity | Low fidelity | Medium fidelity | |
| Continuous outcomes | ||||||
| BMI-z | 0.897 | 0.116 | 0.818 | 0.907 | 0.611 | 0.624 |
| Height (cm) | 0.383 | 0.425 | 0.464 | 0.658 | 0.527 | 0.919 |
| Waist z-score | 0.713 | 0.259 | 0.685 | 0.413 | 0.349 | 0.573 |
| Sum of four skinfolds (mm)c,d | 0.177 | 0.123 | 0.380 | 0.106 | 0.880 | 0.022 |
| Body fat % | 0.815 | 0.837 | 0.205 | 0.687 | 0.439 | 0.614 |
| Energy intake (kJ in 24 hours)e | 0.841 | 0.266 | 0.768 | 0.201 | 0.903 | 0.262 |
| PA energy expenditure (kJ/kg/day) | 0.635 | 0.012 | 0.223 | 0.020 | 0.176 | 0.048 |
| PedsQL total scoref | 0.724 | 0.723 | 0.536 | 0.712 | 0.811 | 0.321 |
| CHU9D utility score | 0.703 | 0.412 | 0.616 | 0.377 | 0.249 | 0.742 |
| Binary outcomes | ||||||
| Obeseg | 0.571 | 0.025 | 0.774 | 0.463 | 0.670 | 0.458 |
| Obese/overweightg | 0.863 | 0.141 | 0.704 | 0.772 | 0.868 | 0.693 |
| Five or more portions of fruit and vegetablesh | 0.384 | 0.920 | 0.555 | 0.905 | 0.756 | 0.166 |
| Achieving ≥ 60 minutes of PAi | 0.689 | 0.193 | 0.752 | 0.082 | 0.735 | 0.080 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 589 (n = 255, unadjusted) | 0.35 (1.36) | 0.61 (1.44) | 0.13 (1.25) | 0.35 (1.35) | 0.263 (0.061 to 0.464) | 0.011 | 0.023 (–0.100 to 0.146) | 0.716 | –0.038 (–0.167 to 0.090) | 0.560 |
| N = 568 (n = 246, partially adjusted) | ||||||||||
| N = 397 (n = 172, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 589 (n = 246, unadjusted) | 119.32 (5.54) | 135.48 (6.51) | 118.86 (5.40) | 135.42 (6.41) | 0.061 (–0.956 to 1.078) | 0.907 | –0.530 (–1.271 to 0.211) | 0.161 | –0.615 (–1.334 to 0.104) | 0.094 |
| N = 568 (n = 246, partially adjusted) | ||||||||||
| N = 397 (n = 172, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 517 (n = 223, unadjusted) | 0.77 (1.27) | 1.12 (1.30) | 0.61 (1.23) | 0.82 (1.33) | 0.300 (0.046 to 0.554) | 0.021 | 0.071 (–0.098 to 0.241) | 0.409 | 0.012 (–0.163 to 0.187) | 0.893 |
| N = 490 (n = 209, partially adjusted) | ||||||||||
| N = 367 (n = 156, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 469 (n = 198, unadjusted) | 25.70 (21.30–32.80) | 30.35 (22.25–45.70) | 25.80 (21.40–32.10) | 27.90 (22.10–42.10) | 1.698 (–0.553 to 3.949) | 0.139 | 0.472 (–0.192 to 1.136) | 0.164 | 0.331 (–0.382 to 1.043) | 0.363 |
| N = 408 (n = 176, partially adjusted) | ||||||||||
| N = 311 (n = 136, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 575 (n = 251, unadjusted) | 20.86 (5.19) | 21.93 (8.41) | 20.21 (4.72) | 20.10 (7.16) | 1.826 (0.572 to 3.080) | 0.004 | 0.623 (–0.224 to 1.471) | 0.150 | 0.400 (–0.486 to 1.286) | 0.376 |
| N = 544 (n = 240, partially adjusted) | ||||||||||
| N = 386 (n = 170, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 527 (n = 226, unadjusted) | 7151 (6126–8300) | 7566 (6255–9016) | 7119 (5998–8223) | 7787 (6728–9244) | –347.761 (–758.689 to 63.167) | 0.097 | –266.416 (–640.120 to 107.289) | 0.162 | –307.410 (–736.999 to 122.178) | 0.161 |
| N = 460 (n = 194, partially adjusted) | ||||||||||
| N = 379 (n = 162, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 363 (n = 160, unadjusted) | 103.42 (23.84) | 84.72 (24.04) | 100.36 (25.02) | 85.28 (23.20) | 0.671 (–5.300 to 6.643) | 0.826 | –1.854 (–7.629 to 3.921) | 0.529 | –2.038 (–8.033 to 3.957) | 0.505 |
| N = 304 (n = 130, partially adjusted) | ||||||||||
| N = 271 (n = 120, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 575 (n = 242, unadjusted) | 70.65 (59.98–82.61) | 81.52 (71.74–89.13) | 73.91 (60.87–84.78) | 81.82 (69.57–89.13) | –0.054 (–2.185 to 2.077) | 0.960 | 0.334 (–2.432 to 3.100) | 0.813 | 0.529 (–2.478 to 3.537) | 0.730 |
| N = 548 (n = 233, partially adjusted) | ||||||||||
| N = 391 (n = 168, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 581 (n = 251, unadjusted) | 0.83 (0.14) | 0.89 (0.09) | 0.82 (0.15) | 0.90 (0.09) | –0.007 (–0.024 to 0.010) | 0.403 | –0.008 (–0.025 to 0.010) | 0.376 | –0.005 (–0.023 to 0.013) | 0.592 |
| N = 546 (n = 238, partially adjusted) | ||||||||||
| N = 384 (n = 166, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 589 (n = 255, unadjusted) | 50 (15.20) | 67 (26.27) | 51 (13.04) | 66 (19.76) | 0.059 (0.009–0.124) | 0.019 | 0.000 (–0.036–0.046) | 0.990 | 0.048 (–0.006 to 0.119) | 0.085 |
| N = 568 (n = 246, partially adjusted) | ||||||||||
| N = 397 (n = 172, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 589 (n = 255, unadjusted) | 90 (27.36) | 109 (42.75) | 78 (19.95) | 104 (31.14) | 0.116 (0.037 to 0.213) | 0.002 | 0.037 (–0.027 to 0.114) | 0.282 | 0.044 (–0.022 to 0.123) | 0.207 |
| N = 568 (n = 246, partially adjusted) | ||||||||||
| N = 397 (n = 172, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 527 (n = 226, unadjusted) | 157 (57.30) | 115 (50.88) | 206 (62.05) | 154 (51.16) | –0.003 (–0.089 to 0.100) | 0.954 | 0.018 (–0.076 to 0.134) | 0.725 | 0.038 (–0.055 to 0.150) | 0.453 |
| N = 460 (n = 194, partially adjusted) | ||||||||||
| N = 379 (n = 162, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 368 (n = 162, unadjusted) | 138 (56.10) | 44 (27.16) | 161 (54.76) | 82 (39.81) | –0.116 (–0.217 to 0.042) | 0.129 | –0.119 (–0.224 to 0.048) | 0.138 | –0.117 (–0.220 to 0.043) | 0.130 |
| N = 305 (n = 131, partially adjusted) | ||||||||||
| N = 272 (n = 122, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 556 (n = 269, unadjusted) | 0.11 (1.10) | 0.24 (1.22) | 0.16 (1.15) | 0.27 (1.29) | –0.043 (–0.266 to 0.180) | 0.706 | –0.023 (–0.157 to 0.110) | 0.731 | –0.012 (–0.173 to 0.149) | 0.883 |
| N = 526 (n = 259, partially adjusted) | ||||||||||
| N = 375 (n = 187, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 557 (n = 260, unadjusted) | 117.95 (5.59) | 134.02 (6.79) | 117.40 (5.25) | 134.20 (6.41) | –0.167 (–1.419 to 1.086) | 0.794 | –0.423 (–1.074 to 0.228) | 0.202 | –0.601 (–1.239 to 0.037) | 0.065 |
| N = 528 (n = 260, partially adjusted) | ||||||||||
| N = 376 (n = 187, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 473 (n = 223, unadjusted) | 0.76 (1.22) | 1.18 (1.19) | 0.71 (1.27) | 0.98 (1.37) | 0.174 (–0.116 to 0.464) | 0.239 | 0.145 (–0.041 to 0.331) | 0.126 | 0.148 (–0.056 to 0.353) | 0.155 |
| N = 433 (n = 205, partially adjusted) | ||||||||||
| N = 336 (n = 164, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 376 (n = 183, unadjusted) | 30.80 (25.70–38.35) | 37.65 (29.50–52.30) | 32.00 (25.45–40.42) | 38.95 (27.65–55.60) | 0.829 (–2.807 to 4.466) | 0.655 | 0.659 (0.005 to 1.314) | 0.048 | 0.687 (0.053 to 1.320) | 0.034 |
| N = 316 (n = 158, partially adjusted) | ||||||||||
| N = 249 (n = 126, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 540 (n = 265, unadjusted) | 21.72 (5.49) | 23.08 (6.44) | 21.79 (5.62) | 23.32 (6.99) | –0.314 (–1.635 to 1.008) | 0.642 | –0.210 (–1.142 to 0.722) | 0.659 | –0.003 (–1.138 to 1.132) | 0.996 |
| N = 507 (n = 255, partially adjusted) | ||||||||||
| N = 361 (n = 184, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 488 (n = 227, unadjusted) | 6644 (5596–7772) | 7814 (6596–9250) | 6719 (5591–7639) | 7856 (6779–9165) | –52.406 (–537.463 to 432.651) | 0.832 | 19.290 (–460.927 to 499.506) | 0.937 | –187.707 (–643.125 to 267.711) | 0.419 |
| N = 435 (n = 207, partially adjusted) | ||||||||||
| N = 350 (n = 169, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 327 (n = 145, unadjusted) | 89.38 (20.18) | 74.09 (18.66) | 86.98 (21.57) | 71.15 (18.99) | 2.900 (–1.969 to 7.769) | 0.243 | 3.939 (–0.653 to 8.530) | 0.093 | 2.931 (–1.366 to 7.229) | 0.181 |
| N = 267 (n = 123, partially adjusted) | ||||||||||
| N = 249 (n = 117, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 541 (n = 253, unadjusted) | 71.74 (60.87–82.61) | 82.61 (71.74–90.91) | 71.74 (58.70–80.43) | 80.22 (71.74–89.13) | 1.498 (–1.702 to 4.698) | 0.359 | 1.724 (–2.009 to 5.457) | 0.365 | 1.553 (–1.567 to 4.672) | 0.329 |
| N = 507 (n = 244, partially adjusted) | ||||||||||
| N = 364 (n = 178, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 550 (n = 266, unadjusted) | 0.84 (0.12) | 0.89 (0.09) | 0.81 (0.14) | 0.90 (0.09) | –0.002 (–0.022 to 0.018) | 0.849 | –0.006 (–0.028 to 0.016) | 0.605 | –0.008 (–0.029 to 0.014) | 0.478 |
| N = 503 (n = 248, partially adjusted) | ||||||||||
| N = 357 (n = 178, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 556 (n = 269, unadjusted) | 34 (10.27) | 41 (15.24) | 36 (10.56) | 46 (16.03) | –0.009 (–0.067 to 0.080) | 0.813 | 0.015 (–0.050 to 0.111) | 0.692 | –0.007 (–0.070 to 0.092) | 0.866 |
| N = 526 (n = 259, partially adjusted) | ||||||||||
| N = 375 (n = 187, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 556 (n = 269, unadjusted) | 55 (16.62) | 67 (24.91) | 72 (21.11) | 83 (28.92) | –0.040 (–0.103 to 0.045) | 0.318 | –0.011 (–0.088 to 0.095) | 0.809 | –0.027 (–0.097 to 0.069) | 0.538 |
| N = 526 (n = 259, partially adjusted) | ||||||||||
| N = 375 (n = 187, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 488 (n = 227, unadjusted) | 179 (62.15) | 138 (60.79) | 199 (67.92) | 163 (62.45) | –0.017 (–0.104 to 0.085) | 0.734 | –0.007 (–0.098 to 0.101) | 0.898 | –0.019 (–0.124 to 0.108) | 0.753 |
| N = 435 (n = 207, partially adjusted) | ||||||||||
| N = 350 (n = 169, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 332 (n = 145, unadjusted) | 90 (36.73) | 26 (17.93) | 115 (43.73) | 38 (20.32) | –0.024 (–0.099 to 0.104) | 0.644 | 0.008 (–0.071 to 0.140) | 0.876 | –0.010 (–0.085 to 0.120) | 0.852 |
| N = 270 (n = 123, partially adjusted) | ||||||||||
| N = 252 (n = 117, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | ||
|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | |
| Continuous outcomes | |||
| BMI-z | 0.033 | 0.475 | 0.968 |
| Height (cm) | 0.759 | 0.523 | 0.244 |
| Waist z-score | 0.447 | 0.721 | 0.265 |
| Sum of four skinfolds (mm)c,d | 0.310 | 0.960 | 0.638 |
| Body fat % | 0.016 | 0.099 | 0.457 |
| Energy intake (kJ in 24 hours)e | 0.261 | 0.311 | 0.592 |
| PA energy expenditure (kJ/kg/day) | 0.440 | 0.095 | 0.161 |
| PedsQL total scoref | 0.298 | 0.395 | 0.743 |
| CHU9D utility score | 0.595 | 0.749 | 0.731 |
| Binary outcomes | |||
| Obeseg | 0.170 | 0.205 | 0.155 |
| Obese/overweightg | 0.009 | 0.414 | 0.774 |
| Five or more portions of fruit and vegetablesh | 0.822 | 0.686 | 0.433 |
| Achieving ≥ 60 minutes of PAi | 0.493 | 0.283 | 0.488 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 816 (n = 384, unadjusted) | 0.21 (1.30) | 0.40 (1.40) | 0.20 (1.28) | 0.38 (1.38) | 0.020 (–0.170 to 0.210) | 0.834 | –0.032 (–0.155 to 0.090) | 0.605 | –0.053 (–0.194 to 0.089) | 0.465 |
| N = 785 (n = 371, partially adjusted) | ||||||||||
| N = 543 (n = 261, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 817 (n = 372, unadjusted) | 118.58 (5.56) | 134.54 (6.74) | 118.21 (5.44) | 134.91 (6.49) | –0.360 (–1.339 to 0.619) | 0.471 | –0.620 (–1.362 to 0.121) | 0.101 | –0.787 (–1.497 to –0.077) | 0.030 |
| N = 787 (n = 372, partially adjusted) | ||||||||||
| N = 544 (n = 261, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 698 (n = 326, unadjusted) | 0.71 (1.29) | 1.13 (1.27) | 0.72 (1.31) | 0.96 (1.43) | 0.154 (–0.092 to 0.400) | 0.219 | 0.086 (–0.090 to 0.262) | 0.337 | 0.056 (–0.139 to 0.250) | 0.575 |
| N = 656 (n = 305, partially adjusted) | ||||||||||
| N = 485 (n = 227, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 583 (n = 273, unadjusted) | 28.45 (22.95–35.30) | 34.10 (25.50–49.95) | 29.25 (23.60–37.70) | 33.70 (24.55–52.00) | 0.316 (–2.547 to 3.179) | 0.829 | 0.446 (–0.188 to 1.080) | 0.168 | 0.319 (–0.389 to 1.027) | 0.377 |
| N = 510 (n = 245, partially adjusted) | ||||||||||
| N = 383 (n = 188, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 792 (n = 376, unadjusted) | 21.28 (5.37) | 22.49 (7.76) | 21.42 (5.43) | 22.13 (7.60) | 0.343 (–0.749 to 1.435) | 0.538 | 0.369 (–0.467 to 1.204) | 0.387 | 0.075 (–0.919 to 1.068) | 0.883 |
| N = 750 (n = 363, partially adjusted) | ||||||||||
| N = 523 (n = 258, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 713 (n = 331, unadjusted) | 6978 (5887–8207) | 7751 (6486–9342) | 6895 (5730–7992) | 7820 (6704–9294) | –83.395 (–518.854 to 352.064) | 0.707 | –11.748 (–425.495 to 401.999) | 0.956 | –120.351 (–552.310 to 311.608) | 0.585 |
| N = 619 (n = 287, partially adjusted) | ||||||||||
| N = 504 (n = 234, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 488 (n = 228, unadjusted) | 97.05 (23.72) | 77.60 (20.98) | 93.05 (24.16) | 77.01 (21.79) | 0.605 (–3.398 to 4.609) | 0.767 | –1.250 (–6.163 to 3.663) | 0.618 | –1.557 (–5.673 to 2.559) | 0.458 |
| N = 401 (n = 185, partially adjusted) | ||||||||||
| N = 363 (n = 174, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 788 (n = 356, unadjusted) | 71.74 (58.70–82.61) | 82.61 (71.74–89.13) | 73.91 (60.87–82.61) | 78.26 (69.57–88.04) | 1.349 (–1.071 to 3.768) | 0.275 | 1.622 (–1.187 to 4.430) | 0.258 | 1.127 (–1.347 to 3.602) | 0.372 |
| N = 748 (n = 344, partially adjusted) | ||||||||||
| N = 526 (n = 248, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 804 (n = 378, unadjusted) | 0.83 (0.14) | 0.90 (0.09) | 0.81 (0.15) | 0.89 (0.09) | 0.005 (–0.009 to 0.019) | 0.505 | 0.002 (–0.014 to 0.017) | 0.815 | 0.001 (–0.014 to 0.016) | 0.895 |
| N = 750 (n = 359, partially adjusted) | ||||||||||
| N = 521 (n = 253, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 816 (n = 384, unadjusted) | 65 (13.18) | 86 (22.40) | 73 (13.96) | 87 (20.14) | 0.023 (–0.023 to 0.080) | 0.365 | 0.010 (–0.039 to 0.074) | 0.721 | 0.029 (–0.021 to 0.093) | 0.276 |
| N = 785 (n = 371, partially adjusted) | ||||||||||
| N = 543 (n = 261, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 816 (n = 384, unadjusted) | 114 (23.12) | 126 (32.81) | 116 (22.18) | 138 (31.94) | 0.009 (–0.046 to 0.074) | 0.773 | 0.004 (–0.057 to 0.078) | 0.918 | 0.003 (–0.052 to 0.070) | 0.913 |
| N = 785 (n = 371, partially adjusted) | ||||||||||
| N = 543 (n = 261, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 713 (n = 331, unadjusted) | 260 (61.47) | 186 (56.19) | 274 (63.57) | 205 (53.66) | 0.025 (–0.061 to 0.127) | 0.588 | 0.049 (–0.039 to 0.152) | 0.292 | 0.048 (–0.039 to 0.150) | 0.297 |
| N = 619 (n = 287, partially adjusted) | ||||||||||
| N = 504 (n = 234, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 497 (n = 229, unadjusted) | 184 (50.55) | 48 (20.96) | 189 (48.59) | 72 (26.87) | –0.057 (–0.132 to 0.061) | 0.294 | –0.049 (–0.135 to 0.092) | 0.429 | –0.043 (–0.132 to 0.101) | 0.488 |
| N = 404 (n = 185, partially adjusted) | ||||||||||
| N = 367 (n = 175, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 316 (n = 134, unadjusted) | 0.29 (1.09) | 0.45 (1.17) | –0.00 (1.01) | 0.15 (1.17) | 0.303 (0.034 to 0.571) | 0.027 | 0.013 (–0.135 to 0.160) | 0.866 | –0.023 (–0.250 to 0.204) | 0.842 |
| N = 297 (n = 128, partially adjusted) | ||||||||||
| N = 229 (n = 98, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 316 (n = 128, unadjusted) | 118.84 (5.71) | 135.18 (6.46) | 118.09 (5.24) | 134.81 (6.34) | 0.373 (–0.836 to 1.582) | 0.545 | 0.075 (–0.760 to 0.910) | 0.860 | 0.146 (–0.491 to 0.783) | 0.653 |
| N = 297 (n = 128, partially adjusted) | ||||||||||
| N = 229 (n = 98, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 281 (n = 115, unadjusted) | 0.95 (1.10) | 1.18 (1.17) | 0.52 (1.07) | 0.75 (1.15) | 0.422 (0.131 to 0.713) | 0.004 | 0.090 (–0.059 to 0.240) | 0.235 | 0.077 (–0.068 to 0.222) | 0.296 |
| N = 257 (n = 104, partially adjusted) | ||||||||||
| N = 218 (n = 93, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 254 (n = 103, unadjusted) | 29.13 (23.95–36.38) | 36.40 (24.95–48.55) | 26.90 (22.20–33.63) | 29.40 (23.40–43.00) | 5.263 (2.468 to 8.058) | 0.000 | 0.973 (0.216 to 1.731) | 0.012 | 1.083 (0.212 to 1.953) | 0.015 |
| N = 208 (n = 85, partially adjusted) | ||||||||||
| N = 177 (n = 74, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 310 (n = 134, unadjusted) | 21.24 (4.97) | 22.51 (6.67) | 19.81 (4.48) | 20.30 (6.32) | 2.203 (1.015 to 3.392) | 0.000 | 0.495 (–0.688 to 1.678) | 0.412 | 0.480 (–1.113 to 2.073) | 0.555 |
| N = 290 (n = 126, partially adjusted) | ||||||||||
| N = 224 (n = 96, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 290 (n = 117, unadjusted) | 6773 (5706–7748) | 7560 (6280–8464) | 6930 (5955–7946) | 7793 (6899–9159) | –525.078 (–966.210 to –83.946) | 0.020 | –402.539 (–764.021 to –41.057) | 0.029 | –334.060 (–696.955 to 28.835) | 0.071 |
| N = 267 (n = 109, partially adjusted) | ||||||||||
| N = 225 (n = 97, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 194 (n = 73, unadjusted) | 93.70 (21.54) | 85.48 (25.38) | 96.67 (24.93) | 82.30 (23.57) | 3.085 (–5.382 to 11.551) | 0.475 | 3.588 (–3.096 to 10.272) | 0.293 | 1.770 (–5.144 to 8.684) | 0.616 |
| N = 165 (n = 65, partially adjusted) | ||||||||||
| N = 157 (n = 63, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 316 (n = 134, unadjusted) | 73.91 (65.22–84.78) | 82.61 (71.74–89.13) | 73.91 (63.04–82.61) | 82.61 (73.91–89.13) | –0.000 (–4.443 to 4.442) | 0.999 | –0.447 (–5.664 to 4.770) | 0.867 | 0.113 (–5.169 to 5.394) | 0.967 |
| N = 296 (n = 128, partially adjusted) | ||||||||||
| N = 229 (n = 98, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 314 (n = 133, unadjusted) | 0.85 (0.12) | 0.88 (0.10) | 0.84 (0.14) | 0.91 (0.08) | –0.029 (–0.059 to 0.001) | 0.059 | –0.031 (–0.063 to 0.000) | 0.050 | –0.031 (–0.061 to 0.000) | 0.051 |
| N = 287 (n = 121, partially adjusted) | ||||||||||
| N = 220 (n = 91, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 316 (n = 134, unadjusted) | 18 (11.84) | 21 (15.67) | 14 (6.97) | 25 (13.74) | 0.019 (–0.028 to 0.087) | 0.470 | –0.062 (–0.093 to –0.012) | 0.021 | –0.056 (–0.100 to 0.036) | 0.178 |
| N = 297 (n = 128, partially adjusted) | ||||||||||
| N = 229 (n = 98, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 316 (n = 134, unadjusted) | 27 (17.76) | 46 (34.33) | 34 (16.92) | 45 (24.73) | 0.096 (0.001 to 0.228) | 0.047 | –0.026 (–0.105 to 0.094) | 0.612 | –0.050 (–0.135 to 0.095) | 0.424 |
| N = 297 (n = 128, partially adjusted) | ||||||||||
| N = 229 (n = 98, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 290 (n = 117, unadjusted) | 67 (52.76) | 64 (54.70) | 129 (68.25) | 109 (63.01) | –0.083 (–0.206 to 0.075) | 0.276 | –0.066 (–0.200 to 0.107) | 0.417 | –0.053 (–0.191 to 0.128) | 0.529 |
| N = 267 (n = 109, partially adjusted) | ||||||||||
| N = 225 (n = 97, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 195 (n = 74, unadjusted) | 38 (32.48) | 20 (27.03) | 85 (52.47) | 46 (38.02) | –0.109 (–0.219 to 0.078) | 0.208 | –0.119 (–0.233 to 0.082) | 0.198 | –0.070 (–0.200 to 0.153) | 0.463 |
| N = 165 (n = 66, partially adjusted) | ||||||||||
| N = 157 (n = 64, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | ||
|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | |
| Continuous outcomes | |||
| BMI-z | 0.094 | 0.680 | 0.874 |
| Height (cm) | 0.407 | 0.218 | 0.321 |
| Waist z-score | 0.182 | 0.892 | 0.672 |
| Sum of four skinfolds (mm)c,d | 0.012 | 0.166 | 0.372 |
| Body fat % | 0.017 | 0.823 | 0.752 |
| Energy intake (kJ in 24 hours)e | 0.158 | 0.084 | 0.066 |
| PA energy expenditure (kJ/kg/day) | 0.575 | 0.121 | 0.076 |
| PedsQL total scoref | 0.453 | 0.420 | 0.693 |
| CHU9D utility score | 0.015 | 0.021 | 0.040 |
| Binary outcomes | |||
| Obeseg | 0.905 | 0.145 | 0.975 |
| Obese/overweightg | 0.102 | 0.151 | 0.346 |
| Five or more portions of fruit and vegetablesh | 0.221 | 0.176 | 0.203 |
| Achieving ≥ 60 minutes of PAi | 0.730 | 0.646 | 0.736 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 229 (n = 108, unadjusted) | 1.99 (0.82) | 1.99 (0.83) | 1.94 (0.73) | 2.06 (0.75) | –0.080 (–0.310 to 0.151) | 0.497 | –0.084 (–0.260 to 0.091) | 0.345 | –0.170 (–0.363 to 0.022) | 0.083 |
| N = 229 (n = 108, partially adjusted) | ||||||||||
| N = 154 (n = 77, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 229 (n = 108, unadjusted) | 121.72 (5.55) | 138.71 (6.63) | 120.74 (5.37) | 138.71 (6.43) | –0.001 (–1.761 to 1.759) | 0.999 | –0.600 (–1.419 to 0.218) | 0.150 | –1.026 (–1.828 to –0.225) | 0.012 |
| N = 229 (n = 108, partially adjusted) | ||||||||||
| N = 154 (n = 77, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 200 (n = 95, unadjusted) | 2.33 (0.96) | 2.46 (0.89) | 2.41 (0.89) | 2.59 (0.77) | –0.147 (–0.419 to 0.125) | 0.289 | –0.135 (–0.365 to 0.095) | 0.249 | –0.207 (–0.457 to 0.042) | 0.104 |
| N = 190 (n = 89, partially adjusted) | ||||||||||
| N = 135 (n = 68, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 156 (n = 75, unadjusted) | 43.40 (33.40–55.90) | 62.95 (40.80–82.35) | 44.75 (36.85–62.20) | 66.50 (48.80–79.60) | –4.940 (–13.134 to 3.255) | 0.237 | 0.183 (–1.545 to 1.912) | 0.835 | –0.010 (–2.311 to 2.292) | 0.993 |
| N = 138 (n = 70, partially adjusted) | ||||||||||
| N = 99 (n = 55, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 223 (n = 107, unadjusted) | 27.93 (5.70) | 30.34 (7.90) | 28.06 (5.17) | 31.25 (6.04) | –0.954 (–2.984 to 1.077) | 0.357 | –0.799 (–2.384 to 0.787) | 0.323 | –1.085 (–2.609 to 0.440) | 0.163 |
| N = 222 (n = 106, partially adjusted) | ||||||||||
| N = 150 (n = 76, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 211 (n = 99, unadjusted) | 7386 (6128–8339) | 7487 (6080–9142) | 6851 (5902–7975) | 7782 (6795–9228) | –467.059 (–1017.963 to 83.844) | 0.097 | –368.871 (–935.829 to 198.086) | 0.202 | –566.272 (–1364.981 to 232.437) | 0.165 |
| N = 191 (n = 91, partially adjusted) | ||||||||||
| N = 150 (n = 73, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 134 (n = 68, unadjusted) | 94.95 (21.50) | 80.40 (21.46) | 89.86 (22.55) | 76.68 (20.36) | 3.719 (–3.334 to 10.773) | 0.301 | 3.575 (–2.861 to 10.012) | 0.276 | 2.182 (–3.338 to 7.701) | 0.439 |
| N = 110 (n = 53, partially adjusted) | ||||||||||
| N = 100 (n = 51, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 222 (n = 102, unadjusted) | 67.39 (58.70–80.43) | 81.52 (71.74–89.13) | 73.91 (60.87–82.61) | 78.26 (67.39–89.13) | 2.385 (–1.394 to 6.164) | 0.216 | 3.121 (–1.482 to 7.724) | 0.184 | 4.021 (–0.682 to 8.724) | 0.094 |
| N = 220 (n = 102, partially adjusted) | ||||||||||
| N = 150 (n = 74, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 227 (n = 107, unadjusted) | 0.82 (0.14) | 0.89 (0.09) | 0.81 (0.13) | 0.89 (0.10) | 0.006 (–0.015 to 0.028) | 0.560 | 0.002 (–0.022 to 0.025) | 0.884 | –0.003 (–0.029 to 0.022) | 0.794 |
| N = 219 (n = 104, partially adjusted) | ||||||||||
| N = 146 (n = 73, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | N (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 229 (n = 108, unadjusted) | 84 (57.93) | 75 (69.44) | 87 (58.00) | 85 (70.25) | –0.008 (–0.115 to 0.118) | 0.893 | –0.011 (–0.107 to 0.100) | 0.838 | –0.025 (–0.134 to 0.104) | 0.682 |
| N = 229 (n = 108, partially adjusted) | ||||||||||
| N = 154 (n = 77, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 229 (n = 108, unadjusted) | 145 (100) | 91 (84.26) | 150 (100) | 110 (90.91) | –0.067 (–0.154 to 0.031) | 0.175 | –0.065 (–0.151 to 0.030) | 0.172 | –0.109 (–0.194 to –0.014) | 0.026 |
| N = 229 (n = 108, partially adjusted) | ||||||||||
| N = 154 (n = 77, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 211 (n = 99, unadjusted) | 85 (66.93) | 50 (50.51) | 75 (63.03) | 67 (59.82) | –0.093 (–0.222 to 0.080) | 0.260 | –0.128 (–0.258 to 0.048) | 0.138 | –0.122 (–0.251 to 0.051) | 0.150 |
| N = 191 (n = 91, partially adjusted) | ||||||||||
| N = 150 (n = 73, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 139 (n = 70, unadjusted) | 44 (40.74) | 16 (22.86) | 49 (47.12) | 17 (24.64) | –0.021 (–0.137 to 0.218) | 0.811 | 0.010 (–0.119 to 0.279) | 0.913 | 0.063 (–0.144 to 0.731) | 0.691 |
| N = 114 (n = 55, partially adjusted) | ||||||||||
| N = 104 (n = 53, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 865 (n = 397, unadjusted) | –0.26 (0.82) | –0.04 (1.10) | –0.32 (0.80) | –0.11 (1.03) | 0.055 (–0.102 to 0.212) | 0.491 | –0.004 (–0.118 to 0.109) | 0.939 | –0.024 (–0.155 to 0.107) | 0.717 |
| N = 865 (n = 397, partially adjusted) | ||||||||||
| N = 618 (n = 282, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 866 (n = 397, unadjusted) | 117.79 (5.31) | 133.68 (6.36) | 117.52 (5.18) | 134.09 (6.10) | –0.417 (–1.306 to 0.472) | 0.358 | –0.444 (–1.110 to 0.222) | 0.192 | –0.585 (–1.244 to 0.075) | 0.082 |
| N = 866 (n = 397, partially adjusted) | ||||||||||
| N = 619 (n = 282, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 748 (n = 335, unadjusted) | 0.33 (0.92) | 0.74 (1.06) | 0.23 (0.89) | 0.50 (1.09) | 0.229 (0.028 to 0.429) | 0.025 | 0.156 (0.005 to 0.308) | 0.043 | 0.146 (–0.018 to 0.311) | 0.081 |
| N = 732 (n = 324, partially adjusted) | ||||||||||
| N = 568 (n = 252, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 652 (n = 292, unadjusted) | 26.75 (21.95–31.60) | 31.52 (23.73–42.75) | 26.45 (22.20–32.00) | 29.05 (23.20–39.88) | 1.350 (–0.720 to 3.420) | 0.201 | 0.447 (0.017 to 0.877) | 0.042 | 0.408 (–0.106 to 0.922) | 0.120 |
| N = 586 (n = 264, partially adjusted) | ||||||||||
| N = 461 (n = 207, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 844 (n = 391, unadjusted) | 19.39 (3.20) | 20.20 (5.57) | 19.10 (3.28) | 19.26 (5.33) | 0.931 (0.140 to 1.722) | 0.021 | 0.617 (–0.106 to 1.341) | 0.094 | 0.576 (–0.336 to 1.488) | 0.216 |
| N = 829 (n = 389, partially adjusted) | ||||||||||
| N = 597 (n = 278, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 757 (n = 337, unadjusted) | 6841 (5782–7948) | 7729 (6538–9117) | 6961 (5767–8004) | 7820 (6716–9303) | –161.071 (–569.019 to 246.878) | 0.439 | –72.351 (–429.873 to 285.171) | 0.692 | –234.859 (–600.153 to 130.435) | 0.208 |
| N = 687 (n = 307, partially adjusted) | ||||||||||
| N = 579 (n = 258, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 524 (n = 225, unadjusted) | 96.84 (23.61) | 80.01 (22.47) | 95.03 (24.70) | 79.59 (22.78) | 0.663 (–4.171 to 5.497) | 0.788 | –0.667 (–5.366 to 4.031) | 0.781 | –1.300 (–5.591 to 2.992) | 0.553 |
| N = 461 (n = 200, partially adjusted) | ||||||||||
| N = 420 (n = 186, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 844 (n = 375, unadjusted) | 71.74 (60.87–82.61) | 82.61 (71.74–89.13) | 73.91 (60.87–82.61) | 80.43 (71.74–89.13) | 0.560 (–1.912 to 3.032) | 0.657 | 0.654 (–2.306 to 3.613) | 0.665 | 0.566 (–2.135 to 3.266) | 0.681 |
| N = 835 (n = 375, partially adjusted) | ||||||||||
| N = 605 (n = 272, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 853 (n = 391, unadjusted) | 0.84 (0.13) | 0.89 (0.09) | 0.82 (0.15) | 0.90 (0.09) | –0.007 (–0.023 to 0.010) | 0.435 | –0.008 (–0.025 to 0.008) | 0.327 | –0.009 (–0.027 to 0.009) | 0.326 |
| N = 829 (n = 381, partially adjusted) | ||||||||||
| N = 595 (n = 271, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 865 (n = 397, unadjusted) | 0 (0.00) | 26 (6.55) | 0 (0.00) | 24 (5.13) | 0.014 (–0.014 to 0.064) | 0.397 | 0.008 (–0.017 to 0.053) | 0.604 | 0.014 (–0.019 to 0.079) | 0.501 |
| N = 865 (n = 397, partially adjusted) | ||||||||||
| N = 618 (n = 282, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 865 (n = 397, unadjusted) | 0 (0.00) | 74 (18.64) | 0 (0.00) | 70 (14.96) | 0.034 (–0.023 to 0.117) | 0.280 | 0.019 (–0.028 to 0.085) | 0.465 | 0.014 (–0.038 to 0.089) | 0.649 |
| N = 865 (n = 397, partially adjusted) | ||||||||||
| N = 618 (n = 282, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 757 (n = 337, unadjusted) | 247 (57.44) | 195 (57.86) | 317 (65.09) | 231 (55.00) | 0.029 (–0.058 to 0.130) | 0.538 | 0.049 (–0.040 to 0.153) | 0.296 | 0.052 (–0.038 to 0.157) | 0.273 |
| N = 687 (n = 307, partially adjusted) | ||||||||||
| N = 579 (n = 258, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 529 (n = 225, unadjusted) | 184 (48.04) | 53 (23.56) | 227 (50.11) | 99 (32.57) | –0.090 (–0.162 to 0.014) | 0.084 | –0.088 (–0.163 to 0.024) | 0.109 | –0.085 (–0.162 to 0.029) | 0.127 |
| N = 461 (n = 199, partially adjusted) | ||||||||||
| N = 420 (n = 186, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | ||
|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | |
| Continuous outcomes | |||
| BMI-z | 0.349 | 0.473 | 0.214 |
| Height (cm) | 0.612 | 0.895 | 0.437 |
| Waist z-score | 0.014 | 0.022 | 0.011 |
| Sum of four skinfolds (mm)c,d | 0.081 | 0.846 | 0.546 |
| Body fat % | 0.066 | 0.167 | 0.118 |
| Energy intake (kJ in 24 hours)e | 0.408 | 0.331 | 0.508 |
| PA energy expenditure (kJ/kg/day) | 0.388 | 0.159 | 0.254 |
| PedsQL total scoref | 0.315 | 0.325 | 0.236 |
| CHU9D utility score | 0.215 | 0.316 | 0.552 |
| Binary outcomes | |||
| Obeseg | 0.386 | 0.426 | 0.338 |
| Obese/overweightg | 0.115 | 0.115 | 0.337 |
| Five or more portions of fruit and vegetablesh | 0.247 | 0.634 | 0.382 |
| Achieving ≥ 60 minutes of PAi | 0.446 | 0.362 | 0.620 |
Appendix 61 Exploratory subgroup analyses
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 560 (n = 267, unadjusted) | 0.29 (1.24) | 0.35 (1.32) | 0.28 (1.12) | 0.53 (1.16) | –0.176 (–0.375 to 0.024) | 0.084 | –0.233 (–0.345 to –0.122) | < 0.001 | –0.258 (–0.355 to –0.160) | < 0.001 |
| N = 536 (n = 258, partially adjusted) | ||||||||||
| N = 407 (n = 195, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 561 (n = 258, unadjusted) | 118.95 (5.74) | 127.33 (6.09) | 118.75 (5.60) | 126.99 (5.95) | 0.338 (–0.489 to 1.166) | 0.423 | 0.460 (–0.063 to 0.984) | 0.085 | 0.501 (0.049 to 0.952) | 0.030 |
| N = 537 (n = 258, partially adjusted) | ||||||||||
| N = 408 (n = 195, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 554 (n = 263, unadjusted) | 0.86 (1.17) | 0.99 (1.39) | 0.92 (1.14) | 1.05 (1.30) | –0.064 (–0.253 to 0.124) | 0.503 | –0.061 (–0.370 to 0.248) | 0.698 | –0.046 (–0.264 to 0.172) | 0.679 |
| N = 513 (n = 237, partially adjusted) | ||||||||||
| N = 389 (n = 180, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 499 (n = 243, unadjusted) | 29.02 (24.48–35.65) | 32.05 (24.70–43.65) | 30.55 (24.45–40.10) | 31.50 (25.23–45.72) | –0.431 (–2.927 to 2.064) | 0.735 | 0.265 (–0.534 to 1.065) | 0.515 | 0.481 (–0.442 to 1.405) | 0.307 |
| N = 409 (n = 198, partially adjusted) | ||||||||||
| N = 316 (n = 152, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 552 (n = 267, unadjusted) | 21.33 (5.19) | 22.00 (6.83) | 21.18 (5.21) | 22.01 (6.70) | –0.076 (–1.394 to 1.241) | 0.910 | –0.807 (–1.621 to 0.006) | 0.052 | –0.869 (–1.648 to –0.090) | 0.029 |
| N = 527 (n = 257, partially adjusted) | ||||||||||
| N = 402 (n = 195, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 535 (n = 249, unadjusted) | 6907 (5858–7964) | 7292 (6258–8491) | 7071 (5948–8038) | 7213 (6306–8520) | 78.698 (–404.798 to 562.194) | 0.750 | 32.129 (–332.899 to 397.157) | 0.863 | 16.142 (–371.590 to 403.874) | 0.935 |
| N = 460 (n = 218, partially adjusted) | ||||||||||
| N = 394 (n = 182, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 453 (n = 214, unadjusted) | 93.07 (21.69) | 93.90 (24.55) | 91.82 (22.42) | 89.68 (26.59) | 2.979 (–3.763 to 9.721) | 0.387 | 3.363 (–3.537 to 10.263) | 0.339 | 1.565 (–4.318 to 7.448) | 0.602 |
| N = 388 (n = 183, partially adjusted) | ||||||||||
| N = 346 (n = 167, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 561 (n = 268, unadjusted) | 72.83 (63.04–84.78) | 78.26 (65.22–85.87) | 73.91 (63.04–82.61) | 76.09 (67.39–84.78) | 0.173 (–3.166 to 3.513) | 0.919 | –0.098 (–4.396 to 4.200) | 0.964 | 0.012 (–6.068 to 6.093) | 0.997 |
| N = 536 (n = 259, partially adjusted) | ||||||||||
| N = 409 (n = 196, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 550 (n = 264, unadjusted) | 0.84 (0.13) | 0.88 (0.10) | 0.82 (0.14) | 0.86 (0.09) | 0.027 (0.001 to 0.054) | 0.039 | 0.026 (–0.001 to 0.053) | 0.056 | 0.031 (0.000 to 0.062) | 0.050 |
| N = 510 (n = 245, partially adjusted) | ||||||||||
| N = 388 (n = 183, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 560 (n = 267, unadjusted) | 39 (13.36) | 45 (16.85) | 43 (13.15) | 52 (17.75) | –0.009 (–0.045 to 0.037) | 0.674 | –0.056 (–0.092 to –0.005) | 0.035 | –0.037 (–0.069 to 0.004) | 0.076 |
| N = 536 (n = 258, partially adjusted) | ||||||||||
| N = 407 (n = 195, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 560 (n = 267, unadjusted) | 67 (22.95) | 72 (26.97) | 67 (20.49) | 82 (27.99) | –0.010 (–0.067 to 0.061) | 0.757 | –0.048 (–0.095 to 0.012) | 0.110 | –0.043 (–0.093 to 0.021) | 0.173 |
| N = 536 (n = 258, partially adjusted) | ||||||||||
| N = 407 (n = 195, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 535 (n = 249, unadjusted) | 160 (60.61) | 132 (53.01) | 207 (72.13) | 150 (52.45) | 0.006 (–0.089 to 0.121) | 0.915 | 0.017 (–0.087 to 0.146) | 0.767 | 0.011 (–0.060 to 0.093) | 0.772 |
| N = 460 (n = 218, partially adjusted) | ||||||||||
| N = 394 (n = 182, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 453 (n = 214, unadjusted) | 88 (36.36) | 124 (57.94) | 133 (47.00) | 122 (51.05) | 0.069 (–0.052 to 0.222) | 0.290 | 0.098 (–0.031 to 0.263) | 0.148 | 0.108 (–0.079 to 0.337) | 0.280 |
| N = 385 (n = 181, partially adjusted) | ||||||||||
| N = 343 (n = 166, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 689 (n = 307, unadjusted) | 0.19 (1.24) | 0.33 (1.35) | 0.04 (1.26) | –0.00 (1.31) | 0.331 (0.128 to 0.534) | 0.001 | 0.079 (–0.088 to 0.246) | 0.353 | 0.136 (–0.025 to 0.297) | 0.097 |
| N = 661 (n = 298, partially adjusted) | ||||||||||
| N = 430 (n = 198, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 690 (n = 300, unadjusted) | 118.37 (5.48) | 127.41 (6.10) | 117.73 (5.15) | 127.06 (5.60) | 0.357 (–0.536 to 1.249) | 0.433 | –0.583 (–1.463 to 0.298) | 0.195 | –0.991 (–1.867 to –0.115) | 0.027 |
| N = 663 (n = 300, partially adjusted) | ||||||||||
| N = 430 (n = 198, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 597 (n = 265, unadjusted) | 0.69 (1.30) | 1.12 (1.33) | 0.41 (1.29) | 0.72 (1.32) | 0.401 (0.151 to 0.650) | 0.002 | 0.118 (–0.077 to 0.313) | 0.235 | 0.074 (–0.062 to 0.210) | 0.285 |
| N = 556 (n = 253, partially adjusted) | ||||||||||
| N = 407 (n = 188, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 549 (n = 245, unadjusted) | 27.55 (22.13–35.30) | 30.90 (24.20–43.65) | 26.75 (22.15–34.05) | 28.00 (22.18–38.38) | 2.563 (1.026 to 4.100) | 0.001 | 0.379 (–0.342 to 1.099) | 0.303 | 0.450 (–0.372 to 1.273) | 0.283 |
| N = 493 (n = 223, partially adjusted) | ||||||||||
| N = 367 (n = 171, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 684 (n = 307, unadjusted) | 21.27 (5.49) | 21.61 (6.65) | 20.76 (5.22) | 20.01 (5.86) | 1.589 (0.622 to 2.556) | 0.001 | 0.900 (–0.230 to 2.029) | 0.118 | 1.280 (0.171 to 2.389) | 0.024 |
| N = 642 (n = 296, partially adjusted) | ||||||||||
| N = 420 (n = 196, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 577 (n = 258, unadjusted) | 6894 (5871–8098) | 6975 (5903–8209) | 6739 (5700–7830) | 6916 (5692–7999) | 142.566 (–281.248 to 566.380) | 0.510 | 79.212 (–306.631 to 465.055) | 0.687 | 62.958 (–307.891 to 433.808) | 0.739 |
| N = 518 (n = 231, partially adjusted) | ||||||||||
| N = 409 (n = 187, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 415 (n = 181, unadjusted) | 99.73 (24.11) | 89.10 (22.46) | 96.40 (26.08) | 92.89 (24.12) | –3.828 (–9.190 to 1.534) | –6.010 (–11.033 to –0.986) | 0.019 | –5.620 (–11.290 to 0.049) | 0.052 | |
| N = 336 (n = 152, partially adjusted) | 0.162 | |||||||||
| N = 312 (n = 143, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 670 (n = 286, unadjusted) | 69.57 (56.52–80.43) | 73.91 (63.04–82.61) | 71.74 (60.87–82.61) | 73.91 (63.04–84.78) | –1.386 (–3.849 to 1.077) | 0.270 | –0.897 (–4.419 to 2.624) | 0.618 | 0.018 (–2.752 to 2.788) | 0.990 |
| N = 635 (n = 279, partially adjusted) | ||||||||||
| N = 408 (n = 179, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 665 (n = 286, unadjusted) | 0.83 (0.14) | 0.85 (0.12) | 0.81 (0.15) | 0.85 (0.11) | –0.004 (–0.028 to 0.021) | 0.757 | –0.005 (–0.030 to 0.020) | 0.702 | –0.006 (–0.035 to 0.022) | 0.664 |
| N = 620 (n = 274, partially adjusted) | ||||||||||
| N = 398 (n = 175, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 689 (n = 307, unadjusted) | 45 (12.23) | 48 (15.64) | 44 (10.86) | 48 (12.57) | 0.031 (–0.014 to 0.093) | 0.202 | –0.022 | 0.428 | 0.016 (–0.039 to 0.104) | 0.635 |
| N = 661 (n = 298, partially adjusted) | (–0.063 to 0.042) | |||||||||
| N = 430 (n = 198, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 689 (n = 307, unadjusted) | 78 (21.20) | 93 (30.29) | 83 (20.49) | 85 (22.25) | 0.080 (0.016 to 0.163) | 0.012 | 0.014 (–0.059 to 0.118) | 0.743 | 0.083 (–0.018 to 0.232) | 0.121 |
| N = 661 (n = 298, partially adjusted) | ||||||||||
| N = 430 (n = 198, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 577 (n = 258, unadjusted) | 176 (59.06) | 112 (43.41) | 198 (58.58) | 147 (46.08) | –0.024 (–0.122 to 0.103) | 0.681 | –0.044 (–0.145 to 0.089) | 0.479 | 0.002 (–0.078 to 0.099) | 0.964 |
| N = 518 (n = 231, partially adjusted) | ||||||||||
| N = 409 (n = 187, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 413 (n = 182, unadjusted) | 140 (56.22) | 83 (45.60) | 143 (52.19) | 112 (48.48) | –0.044 (–0.159 to 0.112) | 0.540 | –0.025 (–0.151 to 0.149) | 0.745 | –0.112 (–0.309 to 0.138) | 0.348 |
| N = 335 (n = 153, partially adjusted) | ||||||||||
| N = 311 (n = 144, fully adjusted) | ||||||||||
| Variable | p-value of interaction term | ||
|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | |
| Continuous outcomes | |||
| BMI-z | < 0.001 | 0.001 | < 0.001 |
| Height (cm) | 0.976 | 0.053 | 0.006 |
| Waist z-score | 0.004 | 0.323 | 0.333 |
| Sum of four skinfolds (mm)c,d | 0.027 | 0.741 | 0.430 |
| Body fat % | 0.050 | 0.014 | 0.003 |
| Energy intake (kJ in 24 hours)e | 0.820 | 0.835 | 0.757 |
| PA energy expenditure (kJ/kg/day) | 0.112 | 0.031 | 0.085 |
| PedsQL total scoref | 0.471 | 0.791 | 0.953 |
| CHU9D utility score | 0.092 | 0.119 | 0.119 |
| Binary outcomes | |||
| Obeseg | 0.196 | 0.200 | 0.658 |
| Obese/overweightg | 0.042 | 0.025 | 0.044 |
| Five or more portions of fruit and vegetablesh | 0.677 | 0.323 | 0.797 |
| Achieving ≥ 60 minutes of PAi | 0.354 | 0.334 | 0.169 |
| Continuous outcome variables | Unadjusted model | Partially adjusted modela | Fully adjusted modelb | |||
|---|---|---|---|---|---|---|
| Group effect (95% CI) | p-value | Group effect (95% CI) | p-value | Group effect (95% CI) | p-value | |
| BMI-z | 0.529 (0.302 to 0.756) | < 0.001 | 0.212 (0.075 to 0.349) | 0.002 | 0.294 (0.148 to 0.440) | < 0.001 |
| Height (cm) | –0.068 (–0.699 to 0.564) | 0.834 | –1.410 (–1.948 to –0.871) | < 0.001 | –1.656 (–2.204 to –1.108) | < 0.001 |
| Waist z-score | 0.334 (0.148 to 0.519) | < 0.001 | –0.126 (–0.365 to 0.114) | 0.304 | 0.003 (–0.202 to 0.207) | 0.980 |
| Sum of four skinfolds (mm)c,d | 3.643 (1.290 to 5.997) | 0.002 | 0.079 (–0.530 to 0.688) | 0.800 | 0.232 (–0.586 to 1.049) | 0.579 |
| Body fat % | 1.968 (0.637 to 3.299) | 0.004 | 1.462 (0.526 to 2.397) | 0.002 | 1.773 (0.818 to 2.728) | 0.000 |
| Energy intake (kJ in 24 hours)e | 465.178 (34.084 to 896.272) | 0.034 | 335.853 (–14.911 to 686.617) | 0.061 | 299.770 (–23.999 to 623.539) | 0.070 |
| PA energy expenditure (kJ/kg/day) | –2.158 (–9.792 to 5.477) | 0.580 | –0.922 (–8.218 to 6.375) | 0.804 | –0.798 (–7.125 to 5.529) | 0.805 |
| PedsQL total scoref | 0.970 (–2.035 to 3.974) | 0.527 | 1.140 (–2.912 to 5.192) | 0.581 | 0.450 (–4.008 to 4.907) | 0.843 |
| CHU9D utility score | 0.003 (–0.020 to 0.027) | 0.783 | 0.003 (–0.020 to 0.027) | 0.784 | –0.001 (–0.026 to 0.024) | 0.957 |
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 524 (n = 252, unadjusted) | 0.29 (1.24) | 0.44 (1.32) | 0.28 (1.12) | 0.54 (1.25) | –0.100 | 0.361 | –0.167 (–0.339 to 0.004) | 0.055 | –0.182 (–0.352 to –0.012) | 0.036 |
| N = 499 (n = 242, partially adjusted) | (–0.315 to 0.115) | |||||||||
| N = 376 (n = 182, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 524 (n = 242, unadjusted) | 118.95 (5.74) | 134.87 (6.83) | 118.75 (5.60) | 135.37 (6.45) | –0.469 (–1.763 to 0.826) | 0.478 | –0.206 (–1.112 to 0.701) | 0.656 | –0.329 (–1.222 to 0.563) | 0.469 |
| N = 499 (n = 242, partially adjusted) | ||||||||||
| N = 376 (n = 182, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 493 (n = 235, unadjusted) | 0.86 (1.17) | 1.28 (1.24) | 0.92 (1.14) | 1.22 (1.30) | 0.064 (–0.151 to 0.279) | 0.558 | 0.066 (–0.153 to 0.286) | 0.553 | 0.040 (–0.131 to 0.210) | 0.649 |
| N = 459 (n = 215, partially adjusted) | ||||||||||
| N = 349 (n = 166, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 458 (n = 214, unadjusted) | 29.02 (24.48–35.65) | 35.65 (25.60–51.00) | 30.55 (24.45–40.10) | 34.60 (25.05–58.83) | –0.079 (–3.059 to 2.901) | 0.959 | 0.677 (–0.126 to 1.480) | 0.099 | 0.690 (–0.186 to 1.566) | 0.123 |
| N = 373 (n = 179, partially adjusted) | ||||||||||
| N = 288 (n = 139, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 511 (n = 249, unadjusted) | 21.33 (5.19) | 22.49 (7.65) | 21.18 (5.21) | 22.34 (7.53) | 0.125 (–1.399 to 1.649) | 0.872 | –0.655 (–1.746 to 0.435) | 0.239 | –0.709 (–1.817 to 0.398) | 0.209 |
| N = 485 (n = 238, partially adjusted) | ||||||||||
| N = 368 (n = 181, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 506 (n = 246, unadjusted) | 6907 (5858–7964) | 7566 (6359–8963) | 7071 (5948–8038) | 7869 (6794–9337) | –341.251 (–739.918 to 57.416) | 0.093 | –248.531 (–622.397 to 125.336) | 0.193 | –327.334 (–707.974 to 53.306) | 0.092 |
| N = 431 (n = 214, partially adjusted) | ||||||||||
| N = 367 (n = 179, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 332 (n = 150, unadjusted) | 93.07 (21.69) | 81.78 (24.16) | 91.82 (22.42) | 78.03 (22.96) | 3.648 (–2.052 to 9.348) | 0.210 | 2.391 (–2.595 to 7.376) | 0.347 | 1.904 (–2.577 to 6.385) | 0.405 |
| N = 282 (n = 124, partially adjusted) | ||||||||||
| N = 250 (n = 113, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 524 (n = 252, unadjusted) | 72.83 (63.04–84.78) | 84.78 (73.91–91.30) | 73.91 (63.04–82.61) | 78.26 (71.74–89.13) | 3.674 (0.848 to 6.500) | 0.011 | 4.142 (0.889 to 7.395) | 0.013 | 3.675 (0.931 to 6.420) | 0.009 |
| N = 497 (n = 242, partially adjusted) | ||||||||||
| N = 376 (n = 182, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 519 (n = 251, unadjusted) | 0.84 (0.13) | 0.90 (0.09) | 0.82 (0.14) | 0.89 (0.09) | 0.010 (–0.003 to 0.024) | 0.142 | 0.006 (–0.010 to 0.022) | 0.443 | 0.013 (–0.004 to 0.029) | 0.127 |
| N = 480 (n = 233, partially adjusted) | ||||||||||
| N = 360 (n = 173, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 524 (n = 252, unadjusted) | 39 (13.36) | 55 (21.83) | 43 (13.15) | 60 (22.06) | –0.002 (–0.058 to 0.072) | 0.943 | –0.037 (–0.086 to 0.031) | 0.253 | –0.011 (–0.060 to 0.054) | 0.719 |
| N = 499 (n = 242, partially adjusted) | ||||||||||
| N = 376 (n = 182, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 524 (n = 252, unadjusted) | 67 (22.95) | 81 (32.14) | 67 (20.49) | 86 (31.62) | 0.005 (–0.068 to 0.101) | 0.901 | –0.030 (–0.097 to 0.057) | 0.461 | –0.029 (–0.088 to 0.046) | 0.423 |
| N = 499 (n = 242, partially adjusted) | ||||||||||
| N = 376 (n = 182, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 506 (n = 246, unadjusted) | 160 (60.61) | 134 (54.47) | 207 (72.13) | 152 (58.46) | –0.040 (–0.141 to 0.085) | 0.501 | –0.034 (–0.143 to 0.103) | 0.599 | –0.062 (–0.151 to 0.045) | 0.236 |
| N = 431 (n = 214, partially adjusted) | ||||||||||
| N = 367 (n = 179, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 337 (n = 151, unadjusted) | 88 (36.36) | 43 (28.48) | 133 (47.00) | 52 (27.96) | 0.004 (–0.095 to 0.156) | 0.945 | 0.009 (–0.097 to 0.174) | 0.897 | –0.024 (–0.260 to 0.363) | 0.875 |
| N = 283 (n = 124, partially adjusted) | ||||||||||
| N = 252 (n = 114, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 621 (n = 272, unadjusted) | 0.19 (1.24) | 0.40 (1.36) | 0.04 (1.26) | 0.14 (1.35) | 0.262 (0.088 to 0.436) | 0.003 | 0.092 (–0.039 to 0.224) | 0.168 | 0.111 (–0.011 to 0.234) | 0.075 |
| N = 595 (n = 263, partially adjusted) | ||||||||||
| N = 396 (n = 177, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 622 (n = 264, unadjusted) | 118.37 (5.48) | 134.60 (6.56) | 117.73 (5.15) | 134.46 (6.40) | 0.141 (–0.855 to 1.137) | 0.781 | –0.787 (–1.722 to 0.148) | 0.099 | –1.060 (–1.782 to –0.339) | 0.004 |
| N = 597 (n = 264, partially adjusted) | ||||||||||
| N = 397 (n = 177, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 497 (n = 211, unadjusted) | 0.69 (1.30) | 1.01 (1.25) | 0.41 (1.29) | 0.61 (1.33) | 0.404 (0.201 to 0.608) | 0.000 | 0.134 (–0.044 to 0.313) | 0.141 | 0.128 (–0.035 to 0.291) | 0.125 |
| N = 464 (n = 199, partially adjusted) | ||||||||||
| N = 354 (n = 154, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 387 (n = 167, unadjusted) | 27.55 (22.13–35.30) | 33.50 (24.45–46.90) | 26.75 (22.15–34.05) | 29.50 (22.68–42.20) | 3.222 (0.773 to 5.672) | 0.010 | 0.463 (–0.268 to 1.194) | 0.215 | 0.569 (–0.273 to 1.411) | 0.185 |
| N = 351 (n = 155, partially adjusted) | ||||||||||
| N = 272 (n = 123, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 604 (n = 267, unadjusted) | 21.27 (5.49) | 22.55 (7.33) | 20.76 (5.22) | 20.99 (6.99) | 1.561 (0.516 to 2.607) | 0.003 | 1.233 (0.352 to 2.113) | 0.006 | 0.989 (0.068 to 1.910) | 0.035 |
| N = 566 (n = 257, partially adjusted) | ||||||||||
| N = 379 (n = 173, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 509 (n = 207, unadjusted) | 6894 (5871–8098) | 7763 (6528–9311) | 6739 (5700–7830) | 7722 (6622–9108) | –82.686 (–645.495 to 480.123) | 0.773 | 0.378 (–518.071 to 518.828) | 0.999 | –226.061 (–833.751 to 381.629) | 0.466 |
| N = 464 (n = 187, partially adjusted) | ||||||||||
| N = 362 (n = 152, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 358 (n = 155, unadjusted) | 99.73 (24.11) | 77.61 (20.12) | 96.40 (26.08) | 79.11 (21.99) | –1.004 (–7.681 to 5.673) | 0.768 | –2.127 (–8.978 to 4.724) | 0.543 | –0.157 (–5.498 to 5.185) | 0.954 |
| N = 289 (n = 129, partially adjusted) | ||||||||||
| N = 270 (n = 124, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 592 (n = 243, unadjusted) | 69.57 (56.52–80.43) | 80.43 (67.39–89.13) | 71.74 (60.87–82.61) | 81.82 (69.57–89.13) | –1.945 (–5.157 to 1.267) | 0.235 | –2.006 (–5.965 to 1.953) | 0.321 | –2.211 (–6.184 to 1.762) | 0.275 |
| N = 558 (n = 235, partially adjusted) | ||||||||||
| N = 379 (n = 164, fully adjusted) | ||||||||||
| CHU9D utility score | ||||||||||
| N = 612 (n = 266, unadjusted) | 0.83 (0.14) | 0.89 (0.10) | 0.81 (0.15) | 0.91 (0.09) | –0.019 (–0.044 to 0.005) | 0.124 | –0.020 (–0.045 to 0.006) | 0.136 | –0.029 (–0.055 to –0.003) | 0.031 |
| N = 569 (n = 253, partially adjusted) | ||||||||||
| N = 381 (n = 171, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 621 (n = 272, unadjusted) | 45 (12.23) | 53 (19.49) | 44 (10.86) | 52 (14.90) | 0.046 (–0.002 to 0.109) | 0.061 | 0.023 (–0.026 to 0.091) | 0.392 | 0.055 (–0.015 to 0.158) | 0.141 |
| N = 595 (n = 263, partially adjusted) | ||||||||||
| N = 396 (n = 177, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 621 (n = 272, unadjusted) | 78 (21.20) | 95 (34.93) | 83 (20.49) | 101 (28.94) | 0.060 (–0.009 to 0.146) | 0.093 | 0.033 (–0.044 to 0.134) | 0.435 | 0.062 (–0.031 to 0.189) | 0.213 |
| N = 595 (n = 263, partially adjusted) | ||||||||||
| N = 396 (n = 177, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 509 (n = 207, unadjusted) | 176 (59.06) | 119 (57.49) | 198 (58.58) | 165 (54.64) | 0.029 (–0.070 to 0.148) | 0.598 | 0.056 (–0.048 to 0.183) | 0.314 | 0.060 (–0.054 to 0.201) | 0.325 |
| N = 464 (n = 187, partially adjusted) | ||||||||||
| N = 362 (n = 152, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 363 (n = 156, unadjusted) | 140 (56.22) | 27 (17.31) | 143 (52.19) | 68 (32.85) | –0.156 (–0.240 to 0.008) | 0.059 | –0.142 (–0.236 to 0.045) | 0.110 | –0.249 (–0.404 to 0.022) | 0.066 |
| N = 292 (n = 130, partially adjusted) | ||||||||||
| N = 272 (n = 125, fully adjusted) | ||||||||||
| Outcomes | p-value of interaction term | ||
|---|---|---|---|
| Unadjusted model | Partially adjusted modela | Fully adjustedb | |
| Continuous outcomes | |||
| BMI-z | 0.010 | 0.020 | 0.016 |
| Height (cm) | 0.448 | 0.380 | 0.365 |
| Waist z-score | 0.023 | 0.678 | 0.505 |
| Sum of four skinfolds (mm)c,d | 0.052 | 0.956 | 0.839 |
| Body fat % | 0.133 | 0.009 | 0.023 |
| Energy intake (kJ in 24 hours)e | 0.465 | 0.433 | 0.623 |
| PA energy expenditure (kJ/kg/day) | 0.297 | 0.268 | 0.272 |
| PedsQL total scoref | 0.009 | 0.015 | 0.009 |
| CHU9D utility score | 0.031 | 0.059 | 0.038 |
| Binary outcomes | |||
| Obeseg | 0.174 | 0.170 | 0.615 |
| Obese/overweightg | 0.319 | 0.110 | 0.132 |
| Five or more portions of fruit and vegetablesh | 0.389 | 0.411 | 0.121 |
| Achieving ≥ 60 minutes of PAi | 0.111 | 0.168 | 0.170 |
| Continuous outcome variables | Unadjusted model | Partially adjusted modela | Fully adjustedb | |||
|---|---|---|---|---|---|---|
| Group effect (95% CI) | p-value | Group effect (95% CI) | p-value | Group effect (95% CI) | p-value | |
| BMI-z | 0.396 (0.188 to 0.605) | < 0.001 | 0.113 (–0.043 to 0.268) | 0.156 | 0.211 (0.057 to 0.366) | 0.007 |
| Height (cm) | 0.886 (–0.302 to 2.074) | 0.144 | –0.553 (–1.353 to 0.247) | 0.176 | –0.634 (–1.451 to 0.182) | 0.128 |
| Waist z-score | 0.612 (0.414 to 0.810) | < 0.001 | 0.165 (–0.053 to 0.383) | 0.137 | 0.245 (0.021 to 0.469) | 0.032 |
| Sum of four skinfolds (mm)c,d | 5.778 (2.877 to 8.679) | < 0.001 | –0.006 (–0.702 to 0.690) | 0.987 | 0.184 (–0.713 to 1.081) | 0.688 |
| Body fat % | 1.348 (0.053 to 2.642) | 0.041 | 1.019 (0.042 to 1.996) | 0.041 | 1.448 (0.517 to 2.379) | 0.002 |
| Energy intake (kJ in 24 hours)e | 9.909 (–441.449 to 461.268) | 0.966 | –91.553 (–501.930 to 318.824) | 0.662 | –106.208 (–557.510 to 345.095) | 0.645 |
| PA energy expenditure (kJ/kg/day) | –0.185 (–6.143 to 5.773) | 0.952 | 0.118 (–5.871 to 6.107) | 0.969 | –0.066 (–6.181 to 6.050) | 0.983 |
| PedsQL total scoref | –1.252 (–4.269 to 1.765) | 0.416 | –1.518 (–5.276 to 2.240) | 0.428 | –1.707 (–5.176 to 1.761) | 0.335 |
| CHU9D utility score | –0.021 (–0.040 to –0.002) | 0.026 | –0.019 (–0.039 to 0.000) | 0.054 | –0.025 (–0.044 to –0.005) | 0.015 |
Appendix 62 Sensitivity analyses
Multiple imputation
| Follow-up outcome variable | Intervention vs. control | |||||
|---|---|---|---|---|---|---|
| Unadjusted | Partially adjusteda | Fully adjustedb | ||||
| Continuous outcomes | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value |
| BMI-z | 0.081 (–0.083 to 0.244) | 0.334 | –0.048 (–0.170 to 0.074) | 0.439 | –0.057 (–0.182 to 0.068) | 0.370 |
| Height (cm) | 0.561 (–0.069 to 1.192) | 0.081 | –0.011 (–0.619 to 0.596) | 0.971 | –0.172 (–0.793 to 0.449) | 0.587 |
| Waist z-score | 0.189 (0.008 to 0.369) | 0.040 | 0.057 (–0.144 to 0.258) | 0.578 | 0.032 (–0.129 to 0.192) | 0.701 |
| Sum of four skinfolds (mm)c,d | 0.944 (–1.308 to 3.196) | 0.409 | 0.486 (–0.266 to 1.237) | 0.202 | 0.460 (–0.375 to 1.294) | 0.276 |
| Body fat % | 0.749 (–0.180 to 1.678) | 0.114 | 0.207 (–0.622 to 1.036) | 0.623 | 0.162 (–0.671 to 0.995) | 0.703 |
| Energy intake (kJ in 24 hours)e | 646.049 (–687.396 to 1979.495) | 0.340 | 571.985 (–630.065 to 1774.036) | 0.348 | 518.404 (–572.128 to 1608.935) | 0.349 |
| PA energy expenditure (kJ/kg/day) | 0.950 (–3.679 to 5.579) | 0.687 | 0.356 (–3.979 to 4.690) | 0.872 | 0.069 (–4.275 to 4.413) | 0.975 |
| PedsQL total scoref | –0.554 (–3.43 to 2.325) | 0.705 | –0.710 (–5.247 to 3.828) | 0.758 | –0.402 (–5.255 to 4.450) | 0.871 |
| CHU9D total score | 0.012 (–0.009 to 0.033) | 0.272 | 0.009 (–0.012 to 0.031) | 0.404 | 0.014 (–0.009 to 0.036) | 0.236 |
| Binary outcomes | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value |
| Obeseg | 0.025 (–0.016 to 0.076) | 0.248 | 0.014 (–0.034 to 0.076) | 0.612 | –0.006 (–0.049 to 0.051) | 0.813 |
| Obese/overweightg | 0.049 (–0.005 to 0.109) | 0.078 | 0.037 (–0.035 to 0.123) | 0.338 | 0.010 (–0.058 to 0.092) | 0.786 |
| Eating five or more portions of fruit and vegetablesh | 0.030 (–0.053 to 0.112) | 0.484 | 0.017 (–0.060 to 0.093) | 0.667 | 0.016 (–0.054 to 0.086) | 0.652 |
| Achieving ≥ 60 minutes of PAi | 0.015 (–0.081 to 0.111) | 0.760 | 0.015 (–0.085 to 0.115) | 0.774 | –0.017 (–0.114 to 0.082) | 0.732 |
| Follow-up outcome variable | Intervention vs. control | |||||
|---|---|---|---|---|---|---|
| Unadjusted | Partially adjusteda | Fully adjustedb | ||||
| Continuous outcomes | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value |
| BMI-z | 0.114 (–0.036 to 0.264) | 0.137 | –0.013 (–0.128 to 0.102) | 0.824 | –0.039 (–0.162 to 0.085) | 0.538 |
| Height (cm) | 0.162 (–0.635 to 0.960) | 0.69 | –0.46 (–1.112 to 0.191) | 0.166 | –0.626 (–1.228 to –0.024) | 0.041 |
| Waist z-score | 0.291 (0.051 to 0.532) | 0.018 | 0.176 (–0.011 to 0.362) | 0.065 | 0.119 (–0.068 to 0.306) | 0.21 |
| Sum of four skinfolds (mm)c,d | 1.808 (–1.020 to 4.636) | 0.208 | 0.785 (–0.043 to 1.614) | 0.063 | 0.635 (–0.121 to 1.391) | 0.099 |
| Body fat % | 1.067 (0.125 to 2.009) | 0.027 | 0.432 (–0.386 to 1.251) | 0.298 | 0.255 (–0.625 to 1.136) | 0.569 |
| Energy intake (kJ in 24 hours)e | 170.2378 (–758.431 to 1098.906) | 0.718 | 158.583 (–711.427 to 1028.593) | 0.720 | 13.69412 (–765.471 to 792.860) | 0.972 |
| PA energy expenditure (kJ/kg/day) | 0.979 (–4.114 to 6.072) | 0.704 | 0.266 (–4.573 to 5.105) | 0.913 | 0.282 (–4.359 to 4.924) | 0.904 |
| PedsQL total scoref | 1.886 (–0.807 to 4.578) | 0.169 | 0.775 (–0.089 to 1.639) | 0.078 | 0.628 (–0.201 to 1.456) | 0.136 |
| CHU9D total score | –0.0042673 (–0.022 to 0.014) | 0.643 | –0.0063602 (–0.025 to 0.012) | 0.501 | –0.006 (–0.025 to 0.012) | 0.499 |
| Binary outcomes | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value |
| Obeseg | 0.036 (–0.012 to 0.094) | 0.153 | 0.026 (–0.031 to 0.096) | 0.402 | 0.019 (–0.038 to 0.089) | 0.551 |
| Obese/overweightg | 0.046 (–0.010 to 0.106) | 0.110 | 0.026 (–0.048 to 0.109) | 0.504 | 0.007 (–0.067 to 0.091) | 0.869 |
| Eating five or more portions of fruit and vegetablesh | 0.034 (–0.055 to 0.118) | 0.449 | 0.052 (–0.039 to 0.141) | 0.264 | 0.042 (–0.052 to 0.129) | 0.377 |
| Achieving ≥ 60 minutes of PAi | 0.015 (–0.081 to 0.111) | 0.760 | 0.014 (–0.080 to 0.115) | 0.774 | –0.017 (–0.114 to 0.082) | 0.732 |
Different levels of clustering
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU1 | Baseline | FU1 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 1249 (n = 574, unadjusted) | 0.23 (1.24) | 0.34 (1.34) | 0.15 (1.20) | 0.23 (1.27) | 0.120 (–0.051 to 0.292) | 0.170 | –0.074 (–0.183 to 0.035) | 0.184 | –0.063 (–0.181 to 0.054) | 0.291 |
| N = 1197 (n = 556, partially adjusted) | ||||||||||
| N = 837 (n = 393, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 1251 (n = 575, unadjusted) | 118.63 (5.60) | 127.37 (6.09) | 118.18 (5.38) | 127.03 (5.75) | 0.346 (–0.255 to 0.947) | 0.259 | –0.064 (–0.641 to 0.514) | 0.829 | –0.194 (–0.795 to 0.408) | 0.528 |
| N = 1200 (n = 558, partially adjusted) | ||||||||||
| N = 837 (n = 392, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 1151 (n = 528, unadjusted) | 0.77 (1.24) | 1.05 (1.36) | 0.66 (1.25) | 0.87 (1.32) | 0.186 (0.010 to 0.361) | 0.038 | 0.067 (–0.108 to 0.243) | 0.453 | 0.028 (–0.115 to 0.172) | 0.697 |
| N = 1069 (n = 490, partially adjusted) | ||||||||||
| N = 796 (n = 368, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 1048 (n = 488, unadjusted) | 28.55 (23.30–35.43) | 31.48 (24.57–43.65) | 28.10 (23.00–36.60) | 29.40 (23.63–41.67) | 1.349 (–0.178 to 2.876) | 0.083 | 0.317 (–0.181 to 0.816) | 0.212 | 0.364 (–0.233 to 0.961) | 0.232 |
| N = 902 (n = 421, partially adjusted) | ||||||||||
| N = 683 (n = 323, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 1236 (n = 574, unadjusted) | 21.30 (5.35) | 21.79 (6.73) | 20.95 (5.22) | 20.87 (6.30) | 0.841 (–0.040 to 1.722) | 0.061 | 0.044 (–0.703 to 0.792) | 0.908 | 0.051 (–0.747 to 0.849) | 0.900 |
| N = 1169 (n = 553, partially adjusted) | ||||||||||
| N = 822 (n = 391, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 1112 (n = 507, unadjusted) | 6904 (5865–8054) | 7152 (6107–8376) | 6911 (5804–7964) | 7074 (5963–8233) | 122.507 (–223.935 to 468.949) | 0.488 | 30.825 (–270.606 to 332.256) | 0.841 | 6.568 (–288.615 to 301.752) | 0.965 |
| N = 978 (n = 449, partially adjusted) | ||||||||||
| N = 803 (n = 369, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 868 (n = 395, unadjusted) | 96.43 (23.16) | 91.70 (23.71) | 94.08 (24.38) | 91.27 (25.42) | –0.207 (–4.552 to 4.137) | 0.926 | –0.866 (–5.389 to 3.658) | 0.708 | –1.691 (–5.821 to 2.440) | 0.422 |
| N = 724 (n = 335, partially adjusted) | ||||||||||
| N = 658 (n = 310, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 1231 (n = 554, unadjusted) | 71.74 (60.87–82.61) | 76.09 (65.22–84.78) | 73.91 (60.87–82.61) | 76.09 (65.22–84.78) | –0.662 (–2.805 to 1.481) | 0.545 | –0.630 (–3.487 to 2.227) | 0.665 | –0.437 (–3.354 to 2.481) | 0.769 |
| N = 1171 (n = 538, partially adjusted) | ||||||||||
| N = 817 (n = 375, fully adjusted) | ||||||||||
| CHU9D total score | ||||||||||
| N = 1215 (n = 550, unadjusted) | 0.84 (0.13) | 0.87 (0.11) | 0.82 (0.14) | 0.86 (0.10) | 0.012 (–0.007 to 0.030) | 0.228 | 0.009 (–0.009 to 0.028) | 0.323 | 0.012 (–0.009 to 0.032) | 0.265 |
| N = 1130 (n = 519, partially adjusted) | ||||||||||
| N = 786 (n = 358, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 1249 (n = 574, unadjusted) | 84 (12.73) | 93 (16.20) | 87 (11.89) | 100 (14.81) | 0.015 (–0.017 to 0.055) | 0.381 | –0.034 (–0.064 to 0.005) | 0.084 | –0.006 (–0.036 to 0.033) | 0.753 |
| N = 1197 (n = 556, partially adjusted) | ||||||||||
| N = 837 (n = 393, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 1249 (n = 574, unadjusted) | 145 (21.97) | 165 (28.75) | 150 (20.49) | 167 (24.74) | 0.043 (–0.004 to 0.099) | 0.076 | –0.010 (–0.059 to 0.051) | 0.720 | 0.002 (–0.050 to 0.066) | 0.958 |
| N = 1197 (n = 556, partially adjusted) | ||||||||||
| N = 837 (n = 393, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 1112 (n = 507, unadjusted) | 336 (59.79) | 244 (48.13) | 405 (64.80) | 297 (49.09) | –0.010 (–0.085 to 0.080) | 0.820 | –0.014 (–0.090 to 0.077) | 0.753 | 0.004 (–0.057 to 0.074) | 0.900 |
| N = 978 (n = 449, partially adjusted) | ||||||||||
| N = 803 (n = 369, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 866 (n = 396, unadjusted) | 228 (46.44) | 207 (52.27) | 276 (49.55) | 234 (49.79) | 0.015 (–0.076 to 0.126) | 0.762 | 0.057 (–0.049 to 0.188) | 0.320 | 0.017 (–0.072 to 0.125) | 0.729 |
| N = 720 (n = 334, partially adjusted) | ||||||||||
| N = 654 (n = 310, fully adjusted) | ||||||||||
| Follow-up outcome variable: N = total participants (n = number in intervention arm) | Arm | Intervention vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Unadjusted | Partially adjusteda | Fully adjustedb | ||||||
| Baseline | FU2 | Baseline | FU2 | |||||||
| Continuous outcomes | Mean (SD) or median (IQR)c | Mean (SD) or median (IQR)c | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| BMI-z | ||||||||||
| N = 1145 (n = 524, unadjusted) | 0.23 (1.24) | 0.42 (1.34) | 0.15 (1.20) | 0.31 (1.32) | 0.107 (–0.048 to 0.262) | 0.175 | –0.002 (–0.105 to 0.101) | 0.973 | –0.028 (–0.152 to 0.097) | 0.660 |
| N = 1094 (n = 505, partially adjusted) | ||||||||||
| N = 772 (n = 359, fully adjusted) | ||||||||||
| Height (cm) | ||||||||||
| N = 1146 (n = 524, unadjusted) | 118.63 (5.60) | 134.73 (6.68) | 118.18 (5.38) | 134.86 (6.43) | –0.135 (–0.945 to 0.675) | 0.744 | –0.427 (–1.079 to 0.224) | 0.198 | –0.642 (–1.273 to 0.011) | 0.046 |
| N = 1096 (n = 506, partially adjusted) | ||||||||||
| N = 773 (n = 359, fully adjusted) | ||||||||||
| Waist z-score | ||||||||||
| N = 990 (n = 446, unadjusted) | 0.77 (1.24) | 1.15 (1.25) | 0.66 (1.25) | 0.90 (1.35) | 0.279 (0.085 to 0.473) | 0.005 | 0.143 (–0.003 to 0.290) | 0.056 | 0.083 (–0.074 to 0.240) | 0.300 |
| N = 923 (n = 414, partially adjusted) | ||||||||||
| N = 703 (n = 320, fully adjusted) | ||||||||||
| Sum of four skinfolds (mm)d,e | ||||||||||
| N = 845 (n = 381, unadjusted) | 28.55 (23.30–35.43) | 34.70 (25.50–49.95) | 28.10 (23.00–36.60) | 31.93 (24.00–48.90) | 2.156 (–0.235 to 4.548) | 0.077 | 0.649 (0.129 to 1.170) | 0.015 | 0.501 (–0.085 to 1.086) | 0.094 |
| N = 724 (n = 334, partially adjusted) | ||||||||||
| N = 560 (n = 262, fully adjusted) | ||||||||||
| Body fat % | ||||||||||
| N = 1115 (n = 516, unadjusted) | 21.30 (5.35) | 22.52 (7.48) | 20.95 (5.22) | 21.58 (7.26) | 0.975 (0.025 to 1.925) | 0.044 | 0.452 (–0.306 to 1.210) | 0.242 | 0.222 (–0.674 to 1.119) | 0.627 |
| N = 1051 (n = 495, partially adjusted) | ||||||||||
| N = 747 (n = 354, fully adjusted) | ||||||||||
| Energy intake (kJ in 24 hours)f | ||||||||||
| N = 1015 (n = 453, unadjusted) | 6904 (5865–8054) | 7656 (6436–9118) | 6911 (5804–7964) | 7817 (6748–9212) | –272.925 (–615.526 to 69.675) | 0.118 | –186.728 (–507.225 to 133.769) | 0.253 | –330.700 (–666.100 to 4.700) | 0.053 |
| N = 895 (n = 401, partially adjusted) | ||||||||||
| N = 729 (n = 331, fully adjusted) | ||||||||||
| PA energy expenditure (kJ/kg/day) | ||||||||||
| N = 690 (n = 305, unadjusted) | 96.43 (23.16) | 79.66 (22.26) | 94.08 (24.38) | 78.60 (22.43) | 1.167 (–3.226–5.560) | 0.603 | 0.001 (–4.371–4.373) | 0.999 | –0.076 (–3.770–3.618) | 0.968 |
| N = 571 (n = 253, partially adjusted) | ||||||||||
| N = 520 (n = 237, fully adjusted) | ||||||||||
| PedsQL total scoreg | ||||||||||
| N = 1116 (n = 495, unadjusted) | 71.74 (60.87–82.61) | 82.61 (71.74–89.13) | 73.91 (60.87–82.61) | 80.43 (71.74–89.13) | 1.002 (–1.283 to 3.286) | 0.390 | 1.248 (–1.453 to 3.948) | 0.365 | 1.263 (–1.062 to 3.588) | 0.287 |
| N = 1055 (n = 477, partially adjusted) | ||||||||||
| N = 755 (n = 346, fully adjusted) | ||||||||||
| CHU9D total score | ||||||||||
| N = 1131 (n = 517, unadjusted) | 0.84 (0.13) | 0.89 (0.09) | 0.82 (0.14) | 0.90 (0.09) | –0.004 (–0.018 to 0.011) | 0.615 | –0.006 (–0.021 to 0.010) | 0.472 | –0.006 (–0.021 to 0.008) | 0.396 |
| N = 1049 (n = 486, partially adjusted) | ||||||||||
| N = 741 (n = 344, fully adjusted) | ||||||||||
| Binary outcomes | n (%) | n (%) | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | ||
| Obeseh | ||||||||||
| N = 1145 (n = 524, unadjusted) | 84 (12.73) | 108 (20.61) | 87 (11.89) | 112 (18.04) | 0.026 (–0.014 to 0.076) | 0.227 | –0.004 (–0.040 to 0.041) | 0.837 | 0.020 (–0.019 to 0.069) | 0.336 |
| N = 1094 (n = 505, partially adjusted) | ||||||||||
| N = 772 (n = 359, fully adjusted) | ||||||||||
| Obese/overweighth | ||||||||||
| N = 1145 (n = 524, unadjusted) | 145 (21.97) | 176 (33.59) | 150 (20.49) | 187 (30.11) | 0.035 (–0.017 to 0.096) | 0.201 | 0.002 (–0.053 to 0.069) | 0.948 | 0.004 (–0.047 to 0.065) | 0.892 |
| N = 1094 (n = 505, partially adjusted) | ||||||||||
| N = 772 (n = 359, fully adjusted) | ||||||||||
| Five or more portions of fruit and vegetablesi | ||||||||||
| N = 1015 (n = 453, unadjusted) | 336 (59.79) | 253 (55.85) | 405 (64.80) | 317 (56.41) | –0.006 (–0.079 to 0.079) | 0.890 | 0.011 (–0.068 to 0.103) | 0.790 | 0.002 (–0.074 to 0.091) | 0.953 |
| N = 895 (n = 401, partially adjusted) | ||||||||||
| N = 729 (n = 331, fully adjusted) | ||||||||||
| Achieving ≥ 60 minutes of PAj | ||||||||||
| N = 700 (n = 307, unadjusted) | 228 (46.44) | 70 (22.80) | 276 (49.55) | 120 (30.53) | –0.077 (–0.149 to 0.026) | 0.127 | –0.068 (–0.147 to 0.048) | 0.215 | –0.067 (–0.146 to 0.049) | 0.219 |
| N = 575 (n = 254, partially adjusted) | ||||||||||
| N = 524 (n = 239, fully adjusted) | ||||||||||
| Outcome | Unadjusted ICC | ICC adjusted for treatment arm | Partially adjusted ICCa | Fully adjusted ICCb | ||||
|---|---|---|---|---|---|---|---|---|
| School-level ICC | Class-level ICC | School-level ICC | Class-level ICC | School-level ICC | Class-level ICC | School-level ICC | Class-level ICC | |
| Continuous outcomes | ||||||||
| BMI-z | 0.0211 (0.0074 to 0.0590) | 0.0211 (0.0074 to 0.0590) | 0.0193 (0.0063 to 0.0577) | 0.0193 (0.0063 to 0.0577) | 0.0840 (0.0449 to 0.1519) | 0.0869 (0.0497 to 0.1475) | 0.0805 (0.0441 to 0.1423) | 0.0805 (0.0441 to 0.1423) |
| Height | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.2700 (0.1840 to 0.3775) | 0.3045 (0.2223 to 0.4013) | 0.3672 (0.2708 to 0.4755) | 0.3795 (0.2857 to 0.4833) |
| Waist z-score | 0.0136 (0.0027 to 0.0650) | 0.0136 (0.0027 to 0.0650) | 0.0089 (0.0010 to 0.0772) | 0.0089 (0.0010 to 0.0772) | 0.1443 (0.0795 to 0.2478) | 0.1552 (0.0963 to 0.2405) | 0.1067 (0.0522 to 0.2058) | 0.1099 (0.0621 to 0.1872) |
| Sum of four skinfolds | 0.0051 (0.0001 to 0.1813) | 0.0051 (0.0001 to 0.1813) | 0.0029 (0.0000 to 0.5995) | 0.0029 (0.0000 to 0.5995) | 0.0879 (0.0312 to 0.2235) | 0.1831 (0.1223 to 0.2648) | 0.0671 (0.0178 to 0.2222) | 0.1596 (0.1018 to 0.2414) |
| Body fat % | 0.0252 (0.0101 to 0.0616) | 0.0252 (0.0101 to 0.0616) | 0.0208 (0.0074 to 0.0572) | 0.0208 (0.0074 to 0.0572) | 0.0984 (0.0541 to 0.1724) | 0.1061 (0.0634 to 0.1720) | 0.1059 (0.0620 to 0.1752) | 0.1059 (0.0620 to 0.1752) |
| Energy intake (kJ in 24 hours) | 0.0443 (0.0177 to 0.1067) | 0.0658 (0.0342 to 0.1231) | 0.0436 (0.0173 to 0.1057) | 0.0649 (0.0336 to 0.1220) | 0.0305 (0.0076 to 0.1144) | 0.0513 (0.0233 to 0.1092) | 0.0212 (0.0024 to 0.1651) | 0.0450 (0.0193 to 0.1010) |
| PA energy expenditure (kJ/kg/day) | 0.0493 (0.0220 to 0.1068) | 0.0493 (0.0220 to 0.1068) | 0.0493 (0.0220 to 0.1068) | 0.0493 (0.0220 to 0.1068) | 0.0819 (0.0410 to 0.1570) | 0.0819 (0.0410 to 0.1570) | 0.0468 (0.0053 to 0.3130) | 0.0572 (0.0226 to 0.1376) |
| PedsQL total score | 0.0403 (0.0189 to 0.0839) | 0.0403 (0.0189 to 0.0839) | 0.0395 (0.0184 to 0.0829) | 0.0395 (0.0184 to 0.0829) | 0.0394 (0.0181 to 0.0839) | 0.0394 (0.0181 to 0.0839) | 0.0176 (0.0037 to 0.0799) | 0.0176 (0.0037 to 0.0799) |
| CHU9D total score | 0.0535 (0.0224 to 0.1226) | 0.0599 (0.0304 to 0.1145) | 0.0513 (0.0208 to 0.1209) | 0.0581 (0.0294 to 0.1118) | 0.0407 (0.0105 to 0.1456) | 0.0654 (0.0343 to 0.1213) | 0.0335 (0.0046 to 0.2064) | 0.0710 (0.0361 to 0.1348) |
| Binary outcomes | ||||||||
| Obesec | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) |
| Obese/overweightc | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0192 (0.0052 to 0.0684) | 0.0192 (0.0052 to 0.0684) | 0.0040 (0.000 to 0.6448) | 0.0040 (0.000 to 0.6448) |
| Five or more portions of fruit and vegetablesd | 0.0371 (0.0110 to 0.1175) | 0.0396 (0.0168 to 0.0906) | 0.0371 (0.0110 to 0.1182) | 0.0396 (0.0168 to 0.0906) | 0.0233 (0.0038 to 0.1310) | 0.0314 (0.0103 to 0.0916) | 0.0000 (0.0000 to 0.0000) | 0.0072 (0.0002 to 0.2466) |
| Outcome | Unadjusted ICC | ICC adjusted for treatment arm | Partially adjusted ICCa | Fully adjusted ICCb | ||||
|---|---|---|---|---|---|---|---|---|
| School-level ICC | Class-level ICC | School-level ICC | Class-level ICC | School-level ICC | Class-level ICC | School-level ICC | Class-level ICC | |
| Continuous outcomes | ||||||||
| BMI-z | 0.0046 (0.0000 to 0.5444) | 0.0056 (0.0001 to 0.2975) | 0.0000 (0.0000 to 0.0000) | 0.0047 (0.0000 to 0.4389) | 0.0000 (0.0000 to 0.0000) | 0.0480 (0.0180 to 0.1215) | 0.0000 (0.0000 to 0.0000) | 0.0375 (0.0122 to 0.1090) |
| Height | 0.0066 (0.0004 to 0.0971) | 0.0066 (0.0004 to 0.0971) | 0.0066 (0.0004 to 0.0972) | 0.0066 (0.0004 to 0.0972) | 0.0962 (0.0375 to 0.2253) | 0.2097 (0.1442 to 0.2946) | 0.0845 (0.0314 to 0.2077) | 0.1607 (0.1005 to 0.2470) |
| Waist z-score | 0.0252 (0.0050 to 0.1174) | 0.0444 (0.0185 to 0.1027) | 0.0075 (0.0000 to 0.6311) | 0.0368 (0.0139 to 0.0936) | 0.0291 (0.0029 to 0.2376) | 0.0796 (0.0428 to 0.1436) | 0.0335 (0.0050 to 0.1929) | 0.0682 (0.0319 to 0.1401) |
| Sum of four skinfolds | 0.0288 (0.0055 to 0.1361) | 0.0467 (0.0184 to 0.1135) | 0.0230 (0.0028 to 0.1655) | 0.0455 (0.0180 to 0.1105) | 0.0000 (0.0000 to 0.0000) | 0.0721 (0.0334 to 0.1488) | 0.0000 (0.0000 to 0.0000) | 0.0806 (0.0372 to 0.1660) |
| Body fat % | 0.0115 (0.0011 to 0.1057) | 0.0149 (0.0022 to 0.0938) | 0.0042 (0.0000 to 0.7345) | 0.0129 (0.0016 to 0.0980) | 0.0040 (0.0000 to 0.9998) | 0.0705 (0.0370 to 0.1301) | 0.0053 (0.0000 to 0.9995) | 0.0667 (0.0313 to 0.1367) |
| Energy intake (kJ in 24 hours) | 0.0045 (0.0000 to 0.9899) | 0.0908 (0.0530 to 0.1512) | 0.0000 (0.0000 to 0.0000) | 0.0889 (0.0518 to 0.1485) | 0.0000 (0.0000 to 0.0000) | 0.1083 (0.0648 to 0.1754) | 0.0000 (0.0000 to 0.0000) | 0.0879 (0.0481 to 0.1551) |
| PA energy expenditure (kJ/kg/day) | 0.0515 (0.0076 to 0.2794) | 0.0573 (0.0227 to 0.1369) | 0.0520 (0.0080 to 0.2723) | 0.0568 (0.0224 to 0.1365) | 0.0753 (0.0329 to 0.1634) | 0.0753 (0.0329 to 0.1634) | 0.0000 (0.0000 to 0.0000) | 0.0601 (0.0225 to 0.1510) |
| PedsQL total score | 0.0708 (0.0326 to 0.1466) | 0.0720 (0.0386 to 0.1304) | 0.0697 (0.0316 to 0.1470) | 0.0715 (0.0383 to 0.1293) | 0.0674 (0.0355 to 0.1240) | 0.0674 (0.0355 to 0.1240) | 0.0428 (0.0114 to 0.1481) | 0.0467 (0.0186 to 0.1124) |
| CHU9D total score | 0.0438 (0.0158 to 0.1153) | 0.0466 (0.0215 to 0.0980) | 0.0428 (0.0151 to 0.1152) | 0.0458 (0.0209 to 0.0973) | 0.0481 (0.0160 to 0.1357) | 0.0554 (0.0268 to 0.1112) | 0.0526 (0.0226 to 0.1174) | 0.0526 (0.0226 to 0.1174) |
| Binary outcomes | ||||||||
| Obesec | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) | 0.0033 (0.0000 to 0.6713) | 0.0033 (0.0000 to 0.6713) | 0.0000 (0.0000 to 0.0000) | 0.0000 (0.0000 to 0.0000) |
| Obese/overweightc | 0.0000 (0.0000 to 0.0000) | 0.0014 (0.0000 to 1.0000) | 0.0000 (0.0000 to 0.0000) | 0.0012 (0.0000 to 1.0000) | 0.0190 (0.0011 to 0.2607) | 0.0358 (0.0140 to 0.0885) | 0.0143 (0.0020 to 0.0967) | 0.0143 (0.0020 to 0.0967) |
| Five or more portions of fruit and vegetablesd | 0.0000 (0.0000 to 0.0000) | 0.0516 (0.0244 to 0.1057) | 0.0000 (0.0000 to 0.0000) | 0.0516 (0.0244 to 0.1055) | 0.0000 (0.0000 to 0.0000) | 0.0589 (0.0271 to 0.1232) | 0.0000 (0.0000 to 0.0000) | 0.0313 (0.0094 to 0.0992) |
| Achieving ≥ 60 minutes of PAe | 0.0459 (0.0043 to 0.3501) | 0.0976 (0.0498 to 0.1823) | 0.0391 (0.0025 to 0.4006) | 0.0901 (0.0442 to 0.1749) | 0.0394 (0.0019 to 0.4739) | 0.0992 (0.0485 to 0.1922) | 0.0457 (0.0031 to 0.4230) | 0.0902 (0.0397 to 0.1917) |
Alternative methods for baseline adjustment
| Follow-up outcome variable | Method 1a | Method 2b | Method 3c | ||||
|---|---|---|---|---|---|---|---|
| Continuous outcomes | MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | |
| BMI-z | –0.075 (–0.183 to 0.033) | 0.175 | 0.026 (–0.098 to 0.151) | 0.680 | –0.069 (–0.175 to 0.037) | 0.201 | |
| Height (cm) | –0.073 (–0.652 to 0.505) | 0.804 | 0.163 (–0.406 to 0.731) | 0.575 | 0.151 (–0.341 to 0.644) | 0.547 | |
| Waist z-score | 0.026 (–0.168 to 0.220) | 0.794 | 0.140 (–0.001 to 0.280) | 0.051 | 0.074 (–0.086 to 0.233) | 0.367 | |
| Sum of four skinfolds (mm)d,e | 0.366 (–0.157 to 0.890) | 0.170 | 0.459 (–0.178 to 1.096) | 0.158 | 1.111 (–0.421 to 2.643) | 0.155 | |
| Body fat % | 0.040 (–0.707 to 0.786) | 0.917 | 0.651 (–0.146 to 1.448) | 0.109 | 0.129 (–0.592 to 0.849) | 0.727 | |
| Energy intake (kJ in 24 hours)f | 61.531 (–217.772 to 340.834) | 0.666 | 59.017 (–263.384 to 381.418) | 0.720 | 59.017 (–263.384 to 381.418) | 0.720 | |
| PA energy expenditure (kJ/kg/day) | –0.866 (–5.389 to 3.658) | 0.708 | –0.547 (–4.665 to 3.570) | 0.794 | –0.764 (–5.223 to 3.696) | 0.737 | |
| PedsQL total scoreg | –0.630 (–3.487 to 2.227) | 0.665 | –0.546 (–2.961 to 1.868) | 0.657 | –0.546 (–2.961 to 1.868) | 0.657 | |
| CHU9D total score | 0.010 (–0.009 to 0.029) | 0.300 | 0.010 (–0.007 to 0.028) | 0.255 | 0.012 (–0.006 to 0.030) | 0.197 | |
| Binary outcomes | RD (95% CI) | p-value | RD (95% CI) | p-value | RD (95% CI) | p-value | |
| Obeseh | –0.036 (–0.066 to 0.004) | 0.074 | –0.057 (–0.106–0.009) | 0.083 | –0.035 (–0.065–0.005) | 0.083 | |
| Obese/overweighth | –0.013 (–0.061 to 0.048) | 0.655 | –0.009 (–0.060–0.055) | 0.748 | –0.009 (–0.060–0.055) | 0.748 | |
| Five or more portions of fruit and vegetablesi | –0.014 (–0.090 to 0.077) | 0.753 | 0.001 (–0.055 to 0.064) | 0.975 | 0.013 (–0.059 to 0.097) | 0.742 | |
| Achieving ≥ 60 minutes of PAj | 0.041 (–0.058 to 0.163) | 0.446 | 0.014 (–0.042 to 0.077) | 0.645 | 0.004 (–0.054 to 0.071) | 0.889 | |
| Follow-up outcome variable | Original model, MD (95% CI)a | Including random effect for individual, MD (95% CI) |
|---|---|---|
| Continuous outcomes | ||
| BMI-z | –0.075 (–0.183 to 0.033) | –0.045 (–0.163 to 0.073) |
| Height | –0.073 (–0.652 to 0.505) | 0.004 (–0.611 to 0.619) |
| Waist z-score | 0.026 (–0.168 to 0.220) | 0.030 (–0.144 to 0.203) |
| Sum of four skinfoldsb,c | 0.366 (–0.157 to 0.890) | 0.539 (–0.975 to 2.054) |
| Body fat % | 0.040 (–0.707 to 0.786) | 0.268 (–0.537 to 1.074) |
| Energy intake (kJ in 24 hours)d | 61.531 (–217.772 to 340.834) | 109.053 (–390.752 to 608.858) |
| PA energy expenditure (kJ/kg/day) | –0.866 (–5.389 to 3.658) | –1.180 (–6.045 to 3.685) |
| PedsQL total scoree | –0.630 (–3.487 to 2.227) | –0.379 (–3.574 to 2.815) |
| CHU9D total score | 0.010 (–0.009 to 0.029) | –0.011 (–0.039 to 0.018) |
| Binary outcomes | RD (95% CI) | RD (95% CI) |
| Obesef | –0.036 (–0.066 to 0.004) | –0.002 (–0.030 to 0.033) |
| Obese/overweightf | –0.013 (–0.061 to 0.048) | 0.019 (–0.029 to 0.078) |
| Five or more portions of fruit and vegetablesg | –0.014 (–0.090 to 0.077) | 0.032 (–0.062 to 0.146) |
| Achieving ≥ 60 minutes of PAh | 0.041 (–0.058 to 0.163) | 0.059 (–0.072 to 0.232) |
Treatment by cluster heterogeneity
| FU1 measurements: outcome | Overall ICCa | Mixed model with separate random effects | |
|---|---|---|---|
| Treatment | Control | ||
| BMI-z | 0.0193 | 0.0000 | 0.0461 |
| Height | 0.0000 | 0.0065 | 0.0000 |
| Waist z-score | 0.0089 | 0.0089 | 0.0089 |
| Sum of four skinfolds | 0.0029 | 0.0000 | 0.0137 |
| Body fat % | 0.0208 | 0.0000 | 0.0415 |
| Energy intake (kJ in 24 hours) | 0.0525 | 0.0619 | 0.0445 |
| PA energy expenditure (kJ/kg/day) | 0.0493 | 0.0000 | 0.0990 |
| PedsQL total score | 0.0395 | 0.0380 | 0.0407 |
| CHU9D total score | 0.0559 | 0.0733 | 0.0399 |
| Obese | 0.0000 | 0.0000 | 0.0000 |
| Obese/overweight | 0.0000 | 0.0000 | 0.0066 |
| Five or more portions of fruit and vegetables | 0.0390 | 0.0456 | 0.0325 |
| Achieving ≥ 60 minutes of PA | 0.0642 | 0.0460 | 0.0776 |
| FU2 measurements: outcome | Overall ICCa | Mixed model with separate random effects | |
|---|---|---|---|
| Treatment | Control | ||
| BMI-z | 0.0025 | 0.0000 | 0.0198 |
| Height | 0.0066 | 0.0000 | 0.0150 |
| Waist z-score | 0.0258 | 0.0031 | 0.0466 |
| Sum of four skinfolds | 0.0369 | 0.0113 | 0.0547 |
| Body fat % | 0.0086 | 0.0032 | 0.0136 |
| Energy intake (kJ in 24 hours) | 0.0480 | 0.0525 | 0.0444 |
| PA energy expenditure (kJ/kg/day) | 0.0565 | 0.0444 | 0.0651 |
| PedsQL total score | 0.0712 | 0.0794 | 0.0644 |
| CHU9D total score | 0.0450 | 0.0451 | 0.0450 |
| Obese | 0.0000 | 0.0000 | 0.0000 |
| Obese/overweight | 0.0000 | 0.0000 | 0.0099 |
| Five or more portions of fruit and vegetables | 0.0443 | 0.0395 | 0.0478 |
| Achieving ≥ 60 minutes of PA | 0.0793 | 0.0891 | 0.0712 |
List of abbreviations
- AVFC
- Aston Villa Football Club
- BMI
- body mass index
- BMI-z
- body mass index z-score
- CADET
- Child And Diet Evaluation Tool
- CD
- compact disc
- CEAC
- cost-effectiveness acceptability curve
- CHU9D
- Child Health Utility 9D
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CUA
- cost–utility analysis
- DVD
- digital versatile disc
- FU1
- follow-up 1
- FU2
- follow-up 2
- FU3
- follow-up 3
- G1
- group 1
- G2
- group 2
- HRQL
- health-related quality of life
- ICC
- intracluster correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- MD
- mean difference
- MRC
- Medical Research Council
- MVPA
- moderate to vigorous physical activity
- MW7
- McCance and Widdowson’s The Composition of Foods: Seventh Summary Edition
- NBR
- net benefit regression
- NDNS
- National Diet and Nutrition Survey
- NDNS-RP
- National Diet and Nutrition Survey Rolling Programme
- NICE
- National Institute for Health and Care Excellence
- PA
- physical activity
- PE
- physical education
- PedsQL
- Paediatric Quality of Life Inventory
- QALY
- quality-adjusted life-year
- RD
- risk difference
- SD
- standard deviation
- SE
- standard error
- TA
- teaching assistant
- WTP
- willingness to pay