Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/24/17. The contractual start date was in July 2016. The final report began editorial review in January 2020 and was accepted for publication in October 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2021 Osborn et al. This work was produced by Osborn et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Osborn et al.
Chapter 1 Ethics
Ethics approvals were gained for all parts of the study from London Bloomsbury Research Ethics Committee (reference 16/LO/2160). In addition, enhanced ethics approvals were gained for work package (WP) 3 from the Confidentiality Advisory Group (reference 17/CAG/0101). Confidentiality Advisory Group approvals were required to use routine clinical data for which service users had not individually given consent to be used in research.
Chapter 2 Introduction
Parts of this chapter have been reproduced with permission from Lamb et al. 1 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
There are well-established challenges facing acute mental health care for people experiencing crises. These include poor experience of services, lack of provision of recommended interventions, delays in accessing care, poor continuity of care, over-reliance on restriction orders, use of police for conveyance, overcrowding in emergency departments and continuing issues with reduced bed capacity. 2,3 A range of reports have highlighted the need for better mental health crisis care in the UK, including the recent Care Quality Commission report about mental health services,4 the Chief Medical Officer’s report in 2013,5 the Crisis Care Concordat6 and the final report by the Commission on Acute Adult Psychiatric Care. 7
Crisis care is typically provided by inpatient wards in hospitals and by crisis resolution teams (CRTs), which are multidisciplinary teams who visit service users at home to provide medication and interventions to prevent admission to inpatient wards. These existing services can be augmented by acute day units (ADUs), which have the potential to address some of the challenges mentioned above. These units offer intensive, short-term community responses to mental health crises, and aim to reduce costly and unpopular admissions, either by avoiding them or by facilitating early discharge. ADUs may be particularly helpful for people who are socially isolated or have poor social support, lack activities or would benefit from peer support or group interventions. Previous research reported that around one in five NHS mental health CRTs in England had access to ADUs within their catchment area. 8
Non-residential day services, previously known as ‘day hospitals’, have been a component of adult mental health services for decades, particularly across Europe. 9 The interventions that ‘day hospitals’ offered were varied, but typically involved longer periods of care than those offered by more recent versions of these. The model for ADUs in the NHS has moved towards providing a shorter period of care, avoiding or shortening inpatient admission by supporting people in the acute phase of their illness. In addition to NHS services, the UK has many non-residential crisis services provided by voluntary sector organisations, which typically offer social interventions and support rather than medical or psychological treatment, for example drop-in ‘crisis cafes’, although research on such services is lacking. 10
Cochrane systematic reviews11,12 have compared acute day hospitals with both outpatient and inpatient psychiatric care. The limited available evidence is not only rather dated, but also heterogeneous in terms of study participants, design and outcomes, making conclusions difficult. The most recent meta-analysis12 involved 10 randomised controlled trials conducted in the USA and Europe. It concluded that mental health day units were as effective as inpatient care in terms of re-admission rates after discharge, employment, quality of life and treatment satisfaction, but that more research was needed to establish the cost-effectiveness of such units.
The most recent British randomised controlled trial,13 involving one London ADU and three inpatient wards, was also promising, reporting that symptom improvement and satisfaction were greater at discharge in the ADU group. This trial found that costs for ADU patients overall were higher than for inpatients, but this was largely a result of mean ADU admissions being nearly twice as long as inpatient admissions (55.7 ADU days vs. 30.5 inpatient days), with the cost per day of ADU treatment being only 70% that of inpatient care.
There is lack of more recent research about ADUs. 12 In the UK, this is likely to be because, although CRTs became mandatory with the 2000 NHS Plan,14 other acute community services such as crisis houses and ADUs were not established nationwide. A recent survey of CRTs8 found that just 22% (40/185) had access to an ADU, and we know from this research that implementation of acute services in practice is often highly variable and suboptimal.
The Crisis Care Concordat6 includes crisis care and acute day care in its suggested domains, and ADUs address many of the ambitions in the NHS Five Year Forward View,14 including making improvements to acute care, personalised care, empowerment and efficiency. ADUs have the potential to be an important part of a well-developed crisis care system, offering user choice and greater possibilities for tailoring response to needs, but we currently lack clear evidence about how best to integrate them into contemporary systems.
Chapter 3 Patient and public involvement
Our service user involvement was planned from the outset both to provide advisory input into the project from a lived experience perspective and to become more involved in the qualitative research component that was peer led, using a range of expertise from experience. This was achieved in the following ways:
-
We worked with two service users to review the original proposal (prior to submission), and one reviewer joined the patient and public involvement (PPI) team as an advisor. They were involved throughout the study.
-
We recruited two additional PPI advisors, both of whom have experience of using acute day units as mental health service users. This provided a small PPI advisory team of three people and a PPI co-applicant lead (VP). We had planned for this group to comprise five people but did not receive that many applications to join the study advisory group, and over time it worked well as a group of three.
-
We recruited a sessional peer researcher to work alongside a University College London (UCL) peer researcher employed on the project full-time for part of the study. The sessional peer researcher ensured that we could deliver as a team the qualitative component with interviews, observation work and analysis shared under the direction of an experienced qualitative specialist (NM).
Advice work
We made some changes to our ways of working in the project early on:
-
First, we decided that, to understand the acute day units that were the focus of the study, to the best of our ability, we wanted to visit them. Thus, we held some of our PPI meetings at acute day units selected for the case study work. In total, we visited three out of the four units.
-
Second, to stay up to date with progress in the study, we were invited to all project team meetings. PPI members attended in person or by telephone. These were held with co-applicants and project staff regularly throughout the study. This was made possible by the PPI group being small.
After each meeting we wrote up reflection notes, including perspectives on how our expertise by experience had been used in a session and changes that the team could make to be more inclusive. Reflection notes were sent to the PPI lead. Extracts from some of the reflection notes are provided in the following sections. The first focuses on the value of involving people ‘from the start’.
Reflection 1: my involvement in the AD-CARE research project
After I was appointed, I was immediately included in the very first meeting at the university to discuss the study. This was both exciting for me and formative for the study because I was able to add my penny’s worth to the perception of ADUs by service users. It was clear to me that the service user voice was very much part of the study. From the outset I felt included at every stage of the process and David Osborn, the team lead, ensured service users understood the jargon and the issues. We were also asked after every point made by other team members what our views were on the matter. Clearly the fact that ADUs were part of the treatment on offer for service users was a key reason for the study.
As part of our active involvement we wrote reflections after each session. After the first meeting I reflected that community day centres and OT-run [occupational therapy-run] day care at the hospitals were part of my recovery, but had been closed. There had been an overall reduction in recovery possibilities and clinical support for the most vulnerable. Service users generally did not have a voice in changes or initiatives. Thus, studying ADUs in the midst of these closures and austerity took on an additional and more important role of preserving records whilst the service was still in place.
It was suggested by our McPin PPI lead, Vanessa Pinfold, that we all go to visit an ADU. The team met up by arrangement at [XXXX] in [XXXX] and we spent several hours discussing with staff what was on offer. This vibrant centre gave us a positive feel for ADUs. Ironically, before the study was completed this ADU was closed. However, the insights we gained there showed what an important role ADUs could play in mental health treatment and we could use it as a benchmark to the others we visited and studied.
Key tasks
The key tasks of the PPI group in terms of advisory input were as follows:
-
In project management meetings, scrutinising progress, being curious about emerging findings and helping with problem-solving.
-
Lived experience advisory group meetings – small sessions with only the lived experience advisory group present alongside programme manager. One session included training in coding qualitative data. In lived experience advisory group meetings, we helped develop interview guides, kept up to date with study progress and planned dissemination activities.
-
Visiting acute day units, observing the environment and the activities provided and reflecting on these personally. We recommended that photographs were taken of the units to help get a sense of the space and environment.
One of the challenges for any research study is keeping the PPI group informed and engaged over several years. Some members are not able to attend all arranged meetings, and when the meetings are infrequent this can lead members to feel disconnected and lost.
Reflection 2: the challenges of being involved in the AD-CARE research project from a distance
I am a former mental health service user, and in the past I have used an acute day care hospital in one of the trusts that AD-CARE has been doing its research. I have been to most of the meetings; two I attended via telephone. One was a meeting where the team were visiting the acute day care hospital in the trust that covers the area that I live in. However, I do not have access to my own transport and I had already committed myself to other work each morning. It would have been quite stressful and pressured to get there, so the decision was taken that I could ring in after the group had their tour. I was grateful that there was the option to be part of this meeting via teleconference. However, I would have to say that the experience was quite stressful and difficult. It left me quite frustrated.
Towards the end of the project, logistics meant that a face-to-face PPI meeting took place in London a week after I had had a major operation. I had at first been upset at the timing of this as I live over 100 miles away from London. However, I was told that the team could ring me and I could contribute that way, which was a great relief. The documents were e-mailed to me the day before and I was able to prepare for the meeting as I usually would have. This experience was so much better than the previous one. I was able to hear what was being said and a big effort was being made to involve me.
Over the last few years the lived experience advisory panel have been invited to the research team meetings for an hour. Myself and another member have telephoned into these. It has been good to be part of them but there have been issues with hearing what was going on, not really knowing some of the people there, not being able to hear very well, making it contributing hard and frustrating; quite a difficult experience. On one occasion I rang off quite upset. I was later offered support by the PPI lead but these calls are examples of where technology has been a mixed blessing.
Inclusivity
Overall, we sought to employ strategies that were inclusive but also tailored to individual needs. We recognised that the involvement of all PPI members in project update meetings was useful but, as these meetings were short and fast-paced and included often quite technical language, support was required for some members to feel able to contribute. An important innovation in this study was PPI meetings at ADU sites, which helped all of the team more fully contextualise the ‘topic’ of study. We also recommended the photographs were taken of the sites, and this provided an important record to share with other team members.
Reflection 3: visiting units
It was interesting to visit an ADU. In all, I visited three units and it brought the study alive: meeting staff, seeing the activities on offer, meeting a few service users, looking at the physical environment of the unit including artwork and positive recovery messages.
The reason I got involved in the ADU study is because I wanted to see how ADUs provided alternative crisis support for people. I felt strongly uncomfortable with some units being attached to acute inpatient hospital. This can create a feeling of being associated with being sectioned, as some patients were probably compulsory sectioned on the ward. I found that the locations did vary – stand-alone units, co-location on hospital site, some in cities with good transport links, others where clients have to rely on hospital transport to attend. Inside, these units also varied. One had a joint staff service user communal area; in another the staff office space was separate. There were units with clear disability access, including wide corridors, and others were in old repurposed buildings, sharing rooms with other services. I found a strong sense of the creative in the units, maybe too much emphasis on artwork for my liking in one [see Figure 1 ]. I found it was really important part of our work, visiting the units. I had strong reactions and it helped me reflect on my current views. I had last seen one in 2008 – I needed to update my knowledge, and I feel I have.
FIGURE 1.
Photographs of artwork displayed in one of the participating ADUs.
Peer research sessional input
The PPI model in this project included the appointment of a sessional researcher. Their role was to support the UCL-based peer researcher in completing the qualitative component of the study that explored service user, carer and staff views of ADUs. This model had advantages, including peer input until the end of the qualitative study (as the main post ended early), both male and female perspectives within the peer research team, team support and different lived experiences to draw on. However, there were also challenges.
Overall, the peer-led research in the study provided a significant research component for the PPI group to shape. Much of the other WPs was limited by data availability in existing data sets. It also led to the development of significantly new skills.
Reflection 4: challenge of working within academic environment
Whilst overall my experience has been a positive one, an area of unforeseen difficulty has been where I belong within the teams. I am employed by the McPin Foundation as a sessional peer researcher but have worked predominantly within the UCL research team. My experience has shifted in this time; at the start of the project I worked closely with the full-time peer researcher and whilst we were doing interviews it was easy to maintain good contact. When we shifted to the analysis this was not so easy as I worked remotely. Then the full-time peer researcher left to do other work and I also joined other projects – maintaining contact and ‘in’ the research became more difficult. I also felt a bit cut adrift because I wasn’t quite sure which team I should identify with. The impact of this was that I did not have a sense of belonging to any specific team. This may have been mitigated by having more clarity around my role in the beginning. This was a new way of working and was an unintended consequence; with reflection, an overview of the team structure, demarcation of roles and more regular meetings, perhaps by Zoom or Skype if this was not practical, would be helpful adjustments to make.
Reflection 5: peer researcher significant moments
Right from the moment of interview I have felt that my skills as a researcher as well as my lived experience have been equally valued. I was very excited to be able to put both sets of skills to good use and I have not been disappointed. At no point have I felt like the proverbial ‘token presence’. When I compare my experience of using my lived experience of mental health difficulties within care settings with my experience within a research setting – I would suggest that research teams are way ahead of the game. I wonder if this is because the ethos of social science is to value the individual’s experience as important data for research and the stringent ethical considerations that go alongside this. Perhaps an area for future research? I have felt privileged to be interviewing my peers and the opportunity (and responsibility) of attempting to represent their voice accurately in this research. There is something unique about the relationship a peer researcher can offer an interviewee, which can enhance the data that is gathered; the knowing nod of a shared understanding really does go a long way. As I have visited ADUs, and hearing the vast array of positive experiences from my peers, I am struck once again by (1) the need for an approach to mental health care that has ‘relationships’ at its centre; and (2) the need for those with lived experience of mental health illness to be the ones asking the questions. This has been a valuable experience and one where I have been able to develop my skills as a researcher, and to have such an investment in the whole process has been a great opportunity.
Recommendations from the patient and public involvement team
This study was challenging in terms of PPI in several respects. First, there were several periods when the focus was data collection or analysis of the Mental Health Minimum Data Set (MHMDS) and there was less work for the PPI group to do. Keeping people involved and up to date on progress was important, and we recommend the inclusion of members in project team meetings. Although large telephone conference calls can be difficult, with support this is a workable solution. Second, the PPI team experience of ADUs was not recent, and to address this we decided to update our knowledge through site visits. We recommend this approach to other teams, as taking research team meetings into places that are the subject of the study is very valuable. This would also benefit wider team members, including statisticians and economists, who might not be familiar with the environment that forms the focus of a study. Third, it can be tricky to involve sessional peer researchers working ad hoc, but this can add important expertise and capacity to the study team. In our case, it ensured that a small team of peer researchers was formed, and we had input throughout the study, including write-up. The danger is that they can become excluded from certain tasks, such as analysis and write-up, because of lack of time on the study or because of projects taking longer than original contracted periods. We recommend studies plan these roles carefully, including support arrangements, and ensure sufficient funding for involvement so that meaningful roles can be shaped.
Chapter 4 Work package 1: national mapping and survey of acute day units for mental health care in England
Parts of this chapter have been reproduced with permission from Lamb et al. 1 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
Methods: mapping and survey
Design
This was a mapping exercise to identify existing ADUs for mental health in England, followed by a questionnaire survey of ADU managers.
Objectives
-
To produce a mapping of existing ADUs for mental health in England.
-
To collect data via a cross-sectional questionnaire on the characteristics and service functioning of ADUs.
-
To ascertain whether or not there are distinct ADU models, and, if so, to characterise them.
Setting and participants
All NHS mental health trusts in England were contacted to ascertain whether or not they provided an ADU service. In addition, voluntary sector non-residential crisis day services were sought. NHS trusts that provided at least one ADU, and any relevant voluntary sector services, were included in the study.
ADUs were defined for this survey as non-residential services offering daytime treatment and care to adults experiencing a mental health crisis who would otherwise be considered for acute psychiatric hospital admission, or other alternatives to admission (including crisis resolution services). Services were excluded that:
-
provide rehabilitation, rather than acute care
-
work only with groups of service users who would not be considered for acute psychiatric hospital admission
-
work primarily with populations other than people with mental illness, such as older adults or people with dementia, learning difficulties or primary drug or alcohol dependence disorders
-
do not accept referrals for service users currently living at home (i.e. exclusively provide ‘step-down’ care from hospital)
-
routinely work with service users for longer than 3 months (i.e. longer-term support rather than acute care)
-
do not accept referrals from the local CRTs.
Non-NHS services that met the above criteria were included in the survey. Day services providing dedicated acute care meeting the above criteria within a broader service were also included.
Measures
We used a survey developed for the AD-CARE study (the full survey is available in Report Supplementary Material 1). The survey was provided online via the secure UCL Opinio website, and could be completed over the telephone with a researcher. The survey included questions covering the following areas: location and access, throughput and service user characteristics, integration with other services, service organisation and staffing, interventions provided, service user experience, service development, and outcomes data.
Procedure
All 58 NHS mental health trusts in England were contacted (August 2016) to enable ADUs to be located. The following methods of contact were used:
-
All England NHS mental health trust websites were screened.
-
Local communications teams, patient advice and liaison service teams, research and development teams, trust headquarters, local acute care leads or other appropriate clinical staff were contacted by telephone and e-mail.
-
Relevant professional organisations and networks (e.g. the Royal College of Psychiatrists’ Acute Care Network and Mind’s Acute Care Campaign) were contacted on Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) and by e-mail and telephone.
-
The CRT managers of all teams that had been identified as having an ADU in the 2012 CRT Optimisation and Relapse Prevention (CORE) study survey8 were contacted.
-
Online searches were conducted for any voluntary sector services that met the inclusion criteria.
Where ADUs were identified, study researchers contacted the service managers by telephone to explain the survey, answer any questions and obtain e-mail/postal addresses to enable them to send out information sheets.
Managers (or alternative ADU clinicians with appropriate knowledge and experience) were asked to complete a questionnaire either online or over the telephone with a researcher. Participants were assigned a unique, anonymised study ID. All data were entered into the questionnaire in Opinio and then extracted into Microsoft Excel® version 16 (Microsoft Corporation, Redmond, WA, USA) and SPSS version 24 (IBM Corporation, Armonk, NY, USA) for data analysis. Data collection was carried out from September to November 2016.
Those who did not respond were followed up by study researchers by telephone and e-mail. Any service that declined to complete the survey was not contacted further.
A brief follow-up survey was conducted 1 year after initial data collection (October 2017) to ascertain whether any ADUs had opened or closed. Services identified in the original mapping exercise were contacted by telephone and e-mail to check that they were still operating and to identify any changes to services.
Analysis
As outlined above, the survey had two main aims: (1) to establish a typology of ADU models and (2) to describe current practice in ADUs.
A cluster analysis was carried out to address aim 1. A cluster analysis is a way of grouping units so that those units more similar to each other appear in the same cluster. The process aims to minimise variability within clusters and maximise variability between clusters. There were four stages in this process:
-
Potential grouping variables were identified. These were collated from the questions in the survey, with some grouping variables obtained by the amalgamation of multiple survey questions covering the same topic.
-
The expert working group ranked the list of potential grouping variables, ordering them by most to least important in distinguishing different types of ADUs.
-
The five highest-ranked grouping variables were included in a cluster analysis (where a grouping variable was considered to have poor-quality data available from the survey, it was discarded, and the next highest-ranking variable was used instead). Five is considered an appropriate number of grouping variables to include in this type of analysis.
-
The cluster analysis was refined, with different models run to establish the most appropriate number and composition of groups.
The resulting variables were used in a cluster analysis using SPSS software.
To address aim 2, descriptive data were collated for each survey question, including range, mean and median scores.
Results: mapping and survey
Cluster analysis
Eight members of a multidisciplinary expert working group ranked 14 variables in the survey identified as relevant to ADU type (Table 1). Variables were ranked by participants, using 1 to indicate the most important and 14 to indicate the least important, meaning that those variables with the lowest total scores were considered (by consensus) to be the most important in distinguishing services from each other.
| Variable | ADU service characteristic | Expert working group raters (anonymised) | Total | SD | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| a | b | c | d | e | f | g | h | ||||
| 1 | Interventions provided | 2 | 3 | 8 | 2 | 7 | 10 | 1 | 1 | 24 | 2.88 |
| 2 | Service provider (statutory/voluntary/joint) | 3 | 1 | 2 | 1 | 5 | 5 | 11 | 6 | 29 | 3.58 |
| 3 | Client group served | 1 | 4 | 9 | 4 | 12 | 14 | 2 | 2 | 34 | 4.10 |
| 4 | Length of ‘stay’ | 7 | 8 | 3 | 3 | 2 | 11 | 6 | 5 | 34 | 2.27 |
| 5 | Staffing (types of staff) | 4 | 9 | 7 | 6 | 3 | 9 | 5 | 4 | 38 | 2.07 |
| 6 | Referral sources | 5 | 13 | 1 | 13 | 6 | 13 | 7 | 3 | 48 | 4.63 |
| 7 | Opening hours | 8 | 6 | 5 | 5 | 14 | 4 | 4 | 9 | 51 | 3.45 |
| 8 | Service user/carer involvement | 14 | 5 | 6 | 8 | 10 | 1 | 10 | 7 | 60 | 3.05 |
| 9 | Gatekeeping | 11 | 12 | 12 | 7 | 8 | 12 | 3 | 8 | 61 | 3.25 |
| 10 | Co-location of services | 13 | 2 | 13 | 10 | 1 | 2 | 12 | 14 | 65 | 5.47 |
| 11 | Size/usage of service | 6 | 7 | 11 | 9 | 9 | 8 | 13 | 10 | 65 | 2.36 |
| 12 | Staffing levels (staff FTE : daily attendance) | 10 | 10 | 4 | 12 | 11 | 7 | 9 | 12 | 68 | 2.75 |
| 13 | Joint management of services | 12 | 11 | 14 | 11 | 4 | 3 | 14 | 13 | 79 | 3.45 |
| 14 | Discharge destinations | 9 | 14 | 10 | 14 | 13 | 6 | 8 | 11 | 79 | 2.43 |
Two-step cluster analysis was used to enable the inclusion of categorical and continuous variables, and for the automatic determination of the optimal number of clusters.
Cluster model 1 for acute day unit types
The first model used variables 1, 2, 3, 4 and 5 (see Table 1), and it identified two clusters. Cluster 1 included services that offered a larger number of interventions, a longer average length of ‘stay’ and a more multidisciplinary staff team; the services were more likely to be provided by the NHS and to have restrictions on the types of clients they took on. Services in cluster 2 offered a smaller variety of interventions, a shorter ‘stay’ and a less varied multidisciplinary team; they were more likely to be provided by voluntary organisations and to have fewer restrictions on the client groups taken on. The most important distinguishing variable was whether services were provided by statutory bodies (NHS) or by voluntary organisations (including joint voluntary/NHS services). The results are shown in Table 2 (numeric variables), Table 3 (categorical variable) and Table 4 (binary variable).
| Cluster | Number of interventions offered from defined list, mean (SD) | Typical length of ‘stay’ in the team, as reported by the manager, mean (SD) | Number of different staff types in the service, mean (SD) |
|---|---|---|---|
| 1 | 18.31 (4.936) | 36.81 (18.552) | 7.19 (2.689) |
| 2 | 9.27 (5.781) | 7.18 (3.995) | 2.27 (0.647) |
| Combined | 14.63 (6.884) | 24.74 (20.611) | 5.19 (3.223) |
| Cluster | Services, frequency (%) | ||
|---|---|---|---|
| Statutory | Voluntary | Joint statutory/voluntary | |
| 1 | 16 (100.0) | 0 (0.0) | 0 (0.0) |
| 2 | 0 (0.0) | 3 (100.0) | 8 (100.0) |
| Combined | 16 (100.0) | 3 (100.0) | 8 (100.0) |
| Cluster | Services, frequency (%) | |
|---|---|---|
| Exclusion criteria | No exclusion criteria | |
| 1 | 8 (80.0) | 8 (47.1) |
| 2 | 2 (20.0) | 9 (52.9) |
| Combined | 10 (100.0) | 17 (100.0) |
Model 2
The service provider variable (variable 2) could be considered a ‘swamping’ variable (one that has large differences between categories within it, which may overpower weaker, but substantively interesting, differences in other variables). Therefore, a model was run excluding this variable and including the sixth ranked variable, ‘number of referral sources’.
Services in cluster 1 offered a larger number of different interventions, a longer average length of ‘stay’ and a more varied multidisciplinary staff team; they accepted referrals from fewer sources and were more likely to have restrictions on the types of clients taken on. Services in cluster 2 offered fewer different types of interventions, a shorter ‘stay’ and a less multidisciplinary team; they accepted referrals from more sources and had fewer restrictions about client groups taken on.
Once again, even without including the ‘service provider’ variable, the model produced two distinct clusters, with the most important distinguishing variable being whether services were provided by statutory bodies (NHS) or voluntary organisations (including joint voluntary/NHS services). The results are shown in Table 5 (numeric variables) and Table 6 (binary variable).
| Cluster | Number of interventions offered from defined list | Typical length of ‘stay’ in the team, as reported by the manager | Number of different staff types in the service | Number of referral sources | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| 1 | 16.67 | 6.721 | 33.11 | 20.522 | 6.67 | 2.951 | 2.44 | 1.688 |
| 2 | 10.56 | 5.480 | 8.00 | 3.571 | 2.22 | 0.667 | 12.11 | 4.567 |
| Combined | 14.63 | 6.884 | 24.74 | 20.611 | 5.19 | 3.223 | 5.67 | 5.463 |
| Cluster | Services, frequency (%) | |
|---|---|---|
| Exclusions criteria | No exclusions criteria | |
| 1 | 10 (100.0) | 8 (47.1) |
| 2 | 0 (0.0) | 9 (52.9) |
| Combined | 10 (100.0) | 17 (100.0) |
The two resulting typologies aligned with whether or not the ADU was provided by the NHS, and no further typologies were identified in the analysis. Therefore, the descriptive results characterising ADUs are reported separately for NHS-ADUs and for voluntary sector ADUs.
Prevalence of acute day unit services
Forty-five individual ADU services meeting our criteria were identified across England. Of these 45 ADUs, 27 (60%) were provided solely by NHS trusts (17 trusts, 29% of the 58 mental health trusts in England), eight were jointly provided NHS and voluntary sector services (17%) and 10 were voluntary sector services (23%).
The geographical locations of the services identified are shown in Figure 2.
FIGURE 2.
Map of UK ADU services. Map data © 2019 Google (Google Inc., Mountain View, CA, USA).

In total, 37 of the 45 identified ADU services completed the initial 2016 survey (two declined and six did not respond to multiple requests for information), representing a response rate of 82%. The two ADUs that declined were from the same trust, but the six that did not respond were from different trusts and voluntary organisations. Twenty-two NHS services and 15 joint or voluntary services responded to the survey.
Results are reported separately for NHS services (referred to as ‘NHS-ADUs’) and for joint and voluntary services (referred to as joint/voluntary). As not every survey respondent answered every question, the denominator is given when reporting each result.
Location and access
Most NHS-ADUs (n = 17/22, 77%) were co-located with other mental health services, with the remaining ones on independent premises. Most commonly, NHS-ADUs were co-located with CRTs (n = 11/17), acute inpatient wards (n = 10/17) and community mental health teams (n = 9/17). Several NHS-ADUs were jointly managed with other acute mental health services (n = 13/17). Most NHS-ADUs reported making their own decisions about accepting referrals to their service (‘gatekeeping’) (n = 15/22); in other cases, gatekeeping was either joint with a local CRT (n = 3), or carried out entirely by another team (n = 4).
Very few joint/voluntary services were co-located with CRTs (n = 2/15) (both were joint services), with none being jointly managed, and all gatekeeping their own services.
Purpose of service
In a free-text response to a question asking what the purpose of the service was, 18 of the 22 NHS-ADUs (82%) stated explicitly that their purpose was to provide an alternative to inpatient admission and/or to facilitate early admission from inpatient wards.
All 15 of the joint/voluntary services expressed their purpose as providing support and/or a safe place for those in mental health crisis. In addition, 11 of these 15 (73%) aimed to provide an alternative to admission to inpatient wards and/or accident and emergency (A&E).
Referrals and discharges
The majority of NHS-ADUs accepted referrals from secondary mental health services, CRTs and inpatient wards, with some accepting referrals directly from A&E. NHS-ADUs that accepted referrals from other sources (e.g. primary care) or self-referrals were less common. Nine NHS-ADUs accepted referrals from secondary mental health services only. One NHS-ADU accepted self-referrals from service users or carers. No NHS-ADUs had a completely open access referrals policy. Joint/voluntary services accepted referrals from a wider range of sources, with 6 out of 15 having a completely open access referral policy.
Two NHS-ADUs reported that they rarely referred service users on to other services because typically service users were already using other services as well as the ADU. Two joint/voluntary services also did not refer people on to other services. The remaining services reported a variety of services to which they discharged or referred people, with the majority of both NHS and joint/voluntary services referring on to secondary mental health services (Table 7).
| Referral source | Discharge destination | |||
|---|---|---|---|---|
| NHS-ADU, n/22 (%) | Joint/voluntary, n/15 (%) | NHS-ADU, n/20 (%) | Joint/voluntary, n/13 (%) | |
| Self/carer | 1 (5) | 12 (80) | N/A | N/A |
| CRTs | 15 (68) | 11 (73) | 15 (75) | 10 (77) |
| Crisis houses | 3 (14) | 9 (60) | 6 (30) | 5 (38) |
| Inpatient wards | 18 (82) | 8 (53) | 17 (85) | 6 (46) |
| Other secondary mental health services | 16 (73) | 12 (80) | 17 (85) | 12 (92) |
| GPs | 2 (9) | 12 (80) | 12 (60) | 11 (85) |
| IAPT | 3 (14) | 10 (67) | N/A | N/A |
| Other primary care | 2 (9) | 11 (73) | 4 (20) | 6 (46) |
| A&E | 9 (41) | 13 (87) | N/A | N/A |
| Police | 1 (5) | 11 (73) | N/A | N/A |
| Counselling | N/A | N/A | 7 (35) | 12 (92) |
| Welfare advice services | N/A | N/A | 7 (35) | 8 (62) |
| Housing services | N/A | N/A | 6 (30) | 4 (46) |
Client group served by acute day units
Ten of the 22 NHS-ADUs (45%) reported that they had no exclusion criteria. Of the 12 that had exclusion criteria, seven (67%) would not accept people with a diagnosis of dementia. Other explicit exclusion criteria included having a diagnosis of personality disorder (1/12, 8%), brain injury (1/12, 8%), primary alcohol and substance misuse problems (4/12, 33%) and learning disability (3/12, 25%), and being unable to engage with the programme offered (1/12, 8%). Only one NHS-ADU (8%) reported that it excluded those who were actively psychotic or unable to keep themselves or others safe.
Among the joint/voluntary services, the only exclusion criteria were being too intoxicated to engage with the service (4/15, 27%) and being ‘too high risk’ (e.g. having active psychosis) (1/15, 6%). Three services out of the 15 (20%) also excluded those with very severe learning disabilities that would prevent them from engaging.
Nineteen of the 22 NHS-ADUs provided data about the age ranges of the people they worked with. All of these NHS-ADUs worked with service users aged 18–65 years, apart from five older-age NHS-ADU teams that worked only with adults aged ≥ 60 years (23%) and one team that worked only with service users aged 24–65 years (5%). Some teams (6/19, 32%) had no upper age limit; two teams (11%) additionally worked with people aged ≥ 17 years.
Two of the 15 joint/voluntary services worked with people aged ≥ 16 years (13%), with the remaining 13 working with those aged ≥ 18 years (87%). Only one service (5%) had an upper age limit, which was 67 years.
Not all teams responded to questions about service user demographics (which asked for averages over the previous month), but Table 8 shows that, among those that did, the average age of people using NHS-ADUs was higher than that of those using joint/voluntary services. Only three of the joint/voluntary services responded to the question about ethnicity, and two responded to the question about sexual orientation. Among the services that responded, Table 8 shows that the average percentage of service users of different ethnicities and sexual orientations is similar across type of service, with client groups being majority white and heterosexual. These demographics were calculated on the basis of data from the month before the survey was completed.
| Characteristic | NHS-ADU | Joint/voluntary | ||
|---|---|---|---|---|
| n/22 teams responding | Median (range) or % | n/15 teams responding | Median (range) or % | |
| Average age (years) | 11 | 48 (28–79) | 12 | 34 (30–46) |
| Female | 16 | 55% | 14 | 68% |
| White | 13 | 77% | 3 | 82% |
| Asian | 13 | 9% | 3 | 8% |
| Black | 13 | 5% | 3 | 1% |
| Mixed | 13 | 4% | 3 | 1% |
| Other | 13 | 4% | 3 | 8% |
| Heterosexual | 10 | 93% | 2 | 79% |
Length of stay
Six of the 22 NHS-ADUs (27%) had no limit on the maximum length of time a service user could use the service. Those that did (73%) had a limit ranging from 10 days to 6 months, with most (12/16, 75%) being between 6 and 12 weeks. The typical length of time with the service ranged from 15 to 84 days, with the median being 30 days (IQR 25–48 days) (18/22 NHS-ADUs responded).
Only three of the 15 joint/voluntary services (20%) put limits on the length of time someone can use the service. One service limited use of the service to 2 hours per visit (but no restriction on the number of visits), one limited users to three visits per referral (but no restriction on the number of referrals) and one service limited use of the service to 10 days. People using these 15 services typically did so for between 1 and 12 days in a month, with a median of 7 days per month (IQR 4–10 days per month) (12/15 services responded).
Caseload
Among the 18 out of 22 NHS-ADUs responding, the total number of places on the caseload available ranged from 6 to 55 (median 25 places, IQR 18–30 places), with between 3 and 45 service users typically visiting the ADU per day (median 15 service users, IQR 11–22 service users).
The annual usage also varied substantially among the 17 out of 22 NHS-ADUs that responded. The median number of service users treated in the previous 12 months was 186 (IQR 138–342 service users, range 114–2000 service users). The median number of distinct treatment episodes provided was 170 (IQR 159–253 episodes, range 120–5544 episodes).
As the joint/voluntary services do not typically keep a ‘caseload’ in the sense that NHS services do, this survey question was not relevant to them. The median number of people using these services per day was 7 (IQR 3–15 people, range 2–20 people), and per year the median was 200 (IQR 100–300 people, range 54–400 people). The median number of periods of care provided by these services was 1874 (IQR 700–4000 periods of care, range 100–6000 periods of care).
Opening hours
Most of the 19 out of 21 NHS-ADUs responding reported opening during the working week, in office hours only, with just two running 24-hour services. The joint/voluntary services were more varied in their opening hours, with two opening during office hours, 10 opening for some period between 12 p.m. and 2 a.m., and three opening from 8 p.m. to 6 a.m. None was a 24-hour service.
Workforce
Table 9 shows the average number of staff members employed by services in various roles (as well as the range of values given and the number of teams that employed staff in each type of role). NHS-ADUs typically employed more nurses, occupational therapists and support workers than any other type of staff, and more qualified clinical staff in general; joint/voluntary services employed more peer support workers and ‘other’ workers, such as staff employed to provide general support to people dropping in to such services. In addition to the roles below, four NHS-ADUs reported having a few hours per week from an arts therapist, and one of those also had time from a music therapist and a dance and movement therapist.
| Type of staff | NHS-ADU | Joint/voluntary service | ||
|---|---|---|---|---|
| Total number of staff, median (range) | Teams employing staff in role (n/22) | Total number of staff, median (range) | Teams employing staff in role (n/15) | |
| Nurses | 3 (1–10) | 18 | 2 (1–3) | 6 |
| Consultant psychiatrists | 1 (1–2) | 13 | 0 | 0 |
| Other medical staff | 2 (1–6) | 9 | 0 | 0 |
| Social workers | 1 (1) | 2 | 2 (1–2) | 2 |
| Occupational therapists | 2 (1–6) | 16 | 0 | 0 |
| Psychologists | 1 (1–2) | 11 | 0 | 0 |
| Graduate mental health workers | 1 | 1 | 0 | 0 |
| Pharmacists | 1 (1) | 6 | 0 | 0 |
| Support workers | 3 (1–10) | 17 | 3 (2–4) | 10 |
| Mental health project workers | 0 | 0 | 10 | 1 |
| Crisis recovery workers | 0 | 0 | 12 | 1 |
| Administrative staff | 1 (1–2) | 12 | 0 | 0 |
| Peer support workers | 1 (1–16) | 3 | 3 (1–13) | 6 |
| Counsellors | 0 | 0 | 2 (1–2) | 2 |
| Students | 1 (1–7) | 8 | 1 | 1 |
| Volunteers | 1 (1–8) | 7 | 6 | 1 |
Interventions provided
A wide range of interventions were provided by services, but no interventions were universally provided. A large majority of NHS-ADUs provided support with medication, physical health, relapse prevention, psychological therapies, daily living activities and one-to-one support. Joint/voluntary services tended not to provide physical or psychological interventions, but all provided one-to-one support, and a large majority provided relapse prevention support. This is shown in Table 10.
| Intervention | NHS-ADU, n/22 (%) | Joint/voluntary service, n/15 (%) |
|---|---|---|
| Medication review, prescription and dispensing | 19 (86) | 0 |
| Medication support and monitoring | 19 (86) | 6 (40) |
| Physical health monitoring/investigation | 18 (82) | 1 (7) |
| Self-management/relapse prevention | 18 (82) | 12 (80) |
| Advance directives | 8 (36) | 1 (7) |
| Psychological therapies | 18 (82) | 5 (33) |
| Family work/therapy | 7 (32) | 1 (7) |
| Peer-run groups | 6 (27) | 7 (47) |
| Carer support groups | 9 (41) | 3 (20) |
| Art/drama/music therapy/groups | 7 (32) | 0 |
| Sports groups | 10 (45) | 0 |
| Daily living activities | 19 (86) | 2 (13) |
| Work experience | 2 (9) | 5 (33) |
| Alcohol/substance misuse groups | 11 (50) | 6 (40) |
| One-to-one support | 20 (91) | 15 (100) |
| Debt/benefits/housing help | 15 (68) | 8 (53) |
Service user and carer involvement
Table 11 summarises findings from NHS-ADU and joint/voluntary service respondents on service user and carer involvement in various aspects of the services. A majority of NHS-ADUs involved service users in staff recruitment and had service user forums, and a large majority sought feedback from service users and, to a lesser extent, from carers. Joint/voluntary services had more service user involvement in general, with the majority involving service users and/or carers in management, advisory groups, staff recruitment, collecting feedback (including service users collecting feedback from others) and addressing feedback. A majority also held service user forums and community meetings, and employed peer support workers.
| Activity | NHS-ADU (n/19), n (%) | Joint/voluntary service (n/15), n (%) | ||
|---|---|---|---|---|
| Service users | Carers | Service users | Carers | |
| Service management | 2 (10.5) | 1 (5.3) | 11 (73.3) | 6 (40) |
| Advisory groups | 6 (31.6) | 4 (21.1) | 13 (86.7) | 10 (66.7) |
| Staff recruitment | 12 (63.2) | 5 (26.3) | 12 (80) | 6 (40) |
| Staff training | 5 (26.3) | 2 (10.5) | 7 (46.7) | 6 (40) |
| Delivering interventions | 3 (15.8) | 0 (0) | 7 (46.7) | 6 (40) |
| Facilitating groups | 4 (21.1) | 1 (5.3) | 5 (33.3) | 4 (26.7) |
| Feedback about service | 17 (89.5) | 13 (68.4) | 14 (93.3) | 11 (73.3) |
| Collecting feedback | 8 (42.1) | 6 (31.6) | 10 (66.7) | 6 (40) |
| Addressing feedback | 3 (15.8) | 1 (5.3) | 11 (73.3) | 6 (40) |
| Paid positions | 2 (10.5) | 0 (0) | 6 (40) | 0 (0) |
| Peer support workers | 4 (21.1) | 7 (36.8) | 9 (60) | 6 (40) |
| Service user/carer forums | 12 (63.2) | 4 (21.1) | 10 (66.7) | 6 (40) |
| Community meetings | 9 (47.4) | 3 (15.8) | 8 (53.3) | 3 (20) |
Follow-up survey
The follow-up survey in October 2017 identified that five of the NHS-ADU services had closed down (three in one NHS trust and the others in two different trusts), and one had been redesigned to provide a reduced model of ADU care (this was reported to have been done to reduce costs). One new NHS trust had plans to open a pilot ADU, which was to be co-located and managed with an existing CRT. The pilot ADU was due to be opened in early 2018, and, if the pilot site performed well, an additional six ADUs (also alongside existing CRTs) were planned to open later in 2018. At the time of checking, this meant that 23 NHS-ADUs were available, covering 14 NHS mental health trusts (of 58 trusts in total). All of the joint/voluntary services we had identified in the original survey were still operating at this time.
Discussion: mapping and survey
Main findings
The mapping exercise, which identified 45 ADUs in England, demonstrates that ADUs are not an established part of mental health service provision in most areas. The cluster analysis found evidence of two types of service model: (1) NHS services (n = 27) and (2) voluntary sector services (including jointly run NHS and voluntary sector services) (n = 17). Considering the geographical distribution of services (see Figure 2), it is clear that large parts of the population have no access to any kind of acute day service as defined by this survey. Although the evidence base for ADUs is small, there have been positive findings in previous studies (i.e. greater symptom improvement and service user satisfaction than for inpatient wards13), so it is surprising that ADUs are not more widespread.
The difference between the NHS and joint/voluntary services is quite marked. NHS-ADUs are typically available 10 a.m.–4 p.m. on weekdays, with a wide range of interventions (including medication review/prescription/support, physical health, psychological therapies, and help with daily living activities), a multidisciplinary team including clinically qualified professionals, and service users attending for an average of 5 weeks. By contrast, joint/voluntary services tend to consist of supportive staff working in non-clinical capacities, who provide brief, one-off listening and signposting support to those in immediate crisis, often in the evening and the early hours of the morning. NHS-ADUs have less service user/carer involvement in paid roles, management, recruitment and training than the joint/voluntary services. In this regard, NHS-ADUs appear to involve service users and carers at similar levels to CRTs. 8 Although the practical offerings of the two types of service are quite different, the explicitly stated purpose of a large majority of both types is an alternative to inpatient admission. The joint/voluntary services are more often intended as an alternative to A&E, which may explain the difference in daily support offered. There are certainly opportunities for cross-sectoral learning here, and in particular the joint NHS/voluntary sector services could lead on sharing best practice between these different types of service.
It is notable that there are currently no national (or international) standards for how ADUs should be set up or function, and this perhaps explains the variation evident, for example, in the wide range of interventions offered. Unlike for CRTs, early intervention services and assertive outreach teams, no guidance was given in The Mental Health Policy Implementation Guide15 about the composition of NHS-ADUs, resulting in a certain amount of heterogeneity, and no standards or criteria are given by which to assess service functioning. Guidance on the place of ADUs within the acute care pathway is similarly lacking.
The findings of this study are in line with previous research about ADUs, both in England and internationally. For example, a previous survey of psychiatric day hospitals in England found heterogeneity of service provision,16 as did a survey of day hospitals for general psychiatric patients in Germany, England, Poland, Slovakia and Czechia,9 although both studies found that the majority of services aimed to provide an alternative to inpatient admission, similar to the current survey. One aspect we investigated in this survey, namely the involvement of service users and carers in the management and running of ADUs, is lacking in previous research, and there is little indication from international studies that this issue has been addressed elsewhere. It is also unclear from international research whether or not ADUs are provided by the voluntary sector in other countries, as this survey demonstrates they are in England.
NHS-ADUs and CRTs are similar in that both offer a range of interventions, delivered by multidisciplinary teams, as an alternative to admission. The key differences between the services are the location and the timing of contact. Because service users attend a single location during office hours, ADUs are able to offer a wider range of interventions, consistency in terms of the staff service users see, more contact time, and peer support. In comparison, by providing home visits and working shifts, CRT contact time is brief, there is little consistency in which staff member sees which service user, and there is no opportunity for peer support (all of which are well-documented complaints of CRT users17). Although CRTs offer more flexibility in timing and location of care, and the opportunity for the clinical team to observe a service user’s home environment (for people for whom loneliness, isolation and lack of activity are a problem, or whose home environment is problematic), ADU care potentially has added benefits than CRT-only care.
In addition to the differences between NHS-ADUs and CRTs, the two ADU models identified by this survey (NHS and joint/voluntary services) indicate further complexity in the acute care pathway. The different offerings of NHS and joint/voluntary services may explain the geographical overlap evident in Figure 2, with joint/voluntary services ‘filling the gaps’ that NHS-ADUs and CRTs do not cover by providing drop-in services out of office hours. Research into how NHS and voluntary sector services complement each other and work together is currently lacking, although a programme of work is under way to gain insight into this important area. 10
The follow-up survey suggests that NHS-ADU services occupy a precarious position. The closure of five NHS-ADUs in a relatively short time is striking. It implies an unstable environment in which non-mandated services may be seen as easily disposable when there is pressure on resources, despite research evidence suggesting that they can be effective. 12,13 At the same time, the piloting and planned opening of seven new NHS-ADUs in one trust suggests that the value of such units is recognised by some commissioners, which reflects the importance of providing choices for people in crisis. 14
Strengths and limitations
There are two main strengths of this survey. The first is the high response rate (81%), meaning that we can take the results to be broadly representative of existing ADUs in England. The second is the inclusion of all services, whether provided by NHS or by voluntary sector services, which gives a comprehensive picture of what is available, and where.
There are three key limitations. The first is that because ADUs are not mandated services, lacking a definitive name or model, identifying such services was challenging. Although we used a clear and specific definition of the type of team we were interested in, it was frequently the case that one part of a trust would identify no such teams, and then another source within the trust would identify a service that clearly met our inclusion criteria. For this reason, and despite the multiple avenues we used to identify teams, it is possible that there are more ADUs in the country than were identified by this survey.
A second limitation was that, because we found that teams close and open relatively quickly, accurately identifying the number of these services in the country at any one time is challenging.
The third limitation regards the quality of the data obtained in the survey. Many teams did not answer all of the survey questions. In the case of joint/voluntary services this was often because the questions were not relevant, or, as with questions about ethnicity and sexual orientation, because they did not keep records of these variables, but even among the NHS-ADUs some data were missing. The aim was for the survey to be as comprehensive as possible while remaining feasible for busy clinicians to complete, but perhaps a shorter survey would have encouraged a higher completion rate. There is the possibility of social desirability bias from this self-report survey, and that respondents interpreted questions in different ways.
Research implications
The results of this survey demonstrate the need for further research into these services. Although some previous research has compared outcomes for people using ADUs with those for people using inpatient wards,12 there is little evidence comparing ADUs with other non-residential services. The finding12 that ADUs are as effective as inpatient wards is promising, but it would be helpful to investigate the place and effectiveness of ADUs in the wider acute care context. Understanding how the ADU complements other crisis and community provision by increasing the support options available is vital. There is a lack of research considering the acute crisis care system as a whole, and how the range of services available can work together to meet the needs of different people. Investigation of the service user and carer experience of ADUs is also, as far as we can find, entirely lacking, and this is particularly important to rectify. Although this survey was focused on ADUs in England, this is an issue of international relevance, and so comparison with services in other countries would be helpful.
Given that CRTs are widely available as the standard service for non-residential crisis care, it is important to know whether or not ADU provision enhances outcomes for people using acute services. However, the lack of model specification for ADUs and the resulting heterogeneity of services means that in any such research, similar types of service should be considered. Research into the different models of ADU care available, and their relative merits in terms of service user outcomes and experiences, would be beneficial, as would a thorough economic evaluation of the costs and benefits of ADUs in comparison with other acute services. The current Acute Day Units as Crisis Alternatives to Residential Care (AD-CARE) study aims to address these issues.
Implications for policy and practice
A detailed health economic analysis of ADUs would be highly useful for policy-makers and service planners, particularly given the current economic and political climate in the UK. Such an analysis would provide vital information about the best ways to configure services, given the economic pressures that NHS trusts and wider communities find themselves under.
This survey suggests that, on average, around 1215 people use NHS-ADUs or voluntary/joint services per day in England. Putting this in context, as of 2017 there were 18,730 mental health inpatient beds in England. Taking the conservative Marshall12 estimate of the proportion of inpatients suitable for ADUs [23.2%, 95% confidence interval (CI) 21.2% to 25.2%], this suggests that, potentially, approximately 3130 additional service users per day could benefit from ADU care. Given the known pressures on beds, frequent out-of-area placements, and the inherent desirability of offering choice regarding acute care, commissioners and policy-makers should consider the place of ADUs in the acute care pathway. The development of a national policy and the implementation of a standard ADU model would mean that these services would be less vulnerable to closure during economically challenging periods.
For existing NHS-ADUs, it may be worth considering further how former and current service users and carers can contribute to services, and the ways in which voluntary sector ADUs manage this could be of interest to NHS-ADUs. Greater sharing of best practice between services would certainly be desirable, as the heterogeneity of services suggests that this is currently not a regular occurrence.
Chapter 5 Work package 2: case studies
Work package 2 consisted of two parts: WP 2.1, a cohort study of ADU and CRT participants; and WP 2.2, a qualitative study investigating the experiences of ADU staff, service users and carers. Five case study sites were recruited for this part of the project, but one site closed its ADUs within a month of beginning participant recruitment, meaning that this site withdrew from the study. The remaining four sites are included in this report, and each participating ADU is described briefly below.
ADU 1
ADU 1 was located near the centre of a large city with a relatively affluent population (one of the least deprived English core cities according to the 2015 Index of Multiple Deprivation (IMD). 18 The ADU opened for a 6-month pilot as we started study recruitment, which was intended to establish the feasibility of rolling out several larger ADUs across the local trust. It was, consequently, a much smaller unit than the others in the study in terms of both caseload (maximum of 10 service users compared with ≈ 30 at the other sites) and physical size.
ADU 1 differed from the other sites in other significant ways. It was jointly run with the local crisis team; it accepted referrals only from the crisis team or inpatient wards, rather than from community teams; it had a group programme constituted of fewer arts-based therapy groups and more psychological groups based on coping strategies and symptom management; and it was the only study ADU to employ peer support workers in a voluntary capacity (each worked at the unit for half a day each week).
The unit was based in an expansive site in a large modern building that also contained mental health wards. The unit itself was tiny – all based off one central corridor – and comprised three communal areas and a garden, without dedicated space for one-to-one work. However, this was a temporary space for use in the pilot, which, if successful, was to lead to a larger caseload and premises. Ultimately, after 12 months of operation, ADU 1 was closed because of trust funding pressures.
ADU 2
ADU 2 was located in an inner-city area, and its catchment area included some of the most socially deprived areas in the country as well as some of the wealthiest. It occupied a freestanding building in the centre of a much larger psychiatric hospital site. There was a crisis house in the same site, users of which were also able to attend the ADU.
The WP 1 survey indicated that people using the service at this site were more likely than those at the other study sites to be from minority ethnic backgrounds, to have problems with practical issues such as housing and debt, and to have diagnoses of severe and enduring psychosis. ADU 2 accepted more referrals directly from the ward than from CRT or community services.
ADU 2 had the most diverse programme of groups among the study sites; auricular acupuncture and aromatherapy were among the available group sessions. It was also the only site to employ dedicated arts therapists, music therapists and dance and movement therapists on a part-time basis.
ADU 2 was the longest-running of the study sites, having been operating as an acute day unit for 15 years. It evolved directly out of, and occupied the same space as, a day hospital operating under an older, more long-term treatment model, which opened in the early 1990s. Several of the staff members had worked there for over 20 years, had seen the transition from a predominantly psychodynamic approach to a more recovery-focused, short-term one, and carried a strong institutional memory of the previous model.
During the study period, ADU 2 was undergoing a period of significant change. The unit lost a significant amount of space, as community teams moved in and occupied rooms that were formerly for ADU use; and for several months there was a threat of closure, until it was decided that the other ADU in the trust would close instead and be incorporated within ADU 2. All of this had an impact on staff morale.
ADU 2 seemed less well attended than the other study sites. At the other sites, the general expectation, and reality, was that all service users on the caseload would attend the unit every day – unless their days were being reduced as part of a planned tapering period – with few exceptions. In the WP 1 survey, the ADU 2 manager indicated that on an average day they would have a caseload of 25 service users, of whom 11 attended and 14 did not attend.
ADU 3
ADU 3 had been open for 7 years and was located in a commuter town outside a medium-sized city; its catchment was largely rural, and included a few other large and small towns. The decline of local industry in the post-war years had led to many of the areas within the team’s catchment area being relatively deprived (as measured using the Index of Multiple Deprivation), particularly compared with the other rural catchment area in the study, ADU 4.
This disparity appeared to be reflected in the budgets afforded to the two teams, as reported in the WP 1 survey: although the two sites had similar caseloads, the annual budget of ADU 3 was half that of ADU 4. It became clear during the study that the work of the team was significantly constrained by budgetary concerns, but this was counteracted by the dedication of the staff team; to raise sufficient funds to buy, for example, basic art supplies, staff conducted a number of fun runs, bake sales and other charitable events in their spare (unpaid) time.
The hospital where the unit was located was originally a general hospital but now focused on mental health; several other buildings were on the hospital site but the ADU was in the main central building, which was grand, dated from the early 20th century, and was built of red brick.
The interior of the unit, however, contrasted sharply with the exterior. The ADU had moved to these new premises from elsewhere on the trust site shortly after the study started. The unit had been freshly refurbished as we started work with it, and was bright, clean and freshly painted. The ADU had a very creative focus, and works of art by service users were displayed throughout.
In keeping with other study ADUs, there was a mix of large rooms used for groups and smaller rooms used for one-to-one work. The unit included a ‘relaxation room’, which was particularly popular with service users; it featured lilac-painted walls, large leather massage chairs and a sound system.
There was also a fully equipped medical clinic, and all service users were given a full physical examination during their first week of attending the ADU. The clinic was also used as a clozapine titration clinic: once per week, service users not otherwise on the ADU caseload attended for clozapine titration. Organising and carrying out this clozapine titration was the responsibility of ADU staff, but they were not resourced to put on extra staff for the occasion, meaning that clinic days were always hectic and drew resources away from the ADU’s primary function.
ADU 4
ADU 4 had been open for 6 years and was located in the commuter belt. Like ADU 3, it was located in a large town and served a largely rural catchment, including small and large towns; unlike ADU 3, the surrounding area was relatively affluent (as measured using the IMD).
ADU 4 reported the lowest proportion of service users experiencing psychosis and served more people with diagnoses of depression or anxiety than the other teams in the study. It was relatively well funded and well staffed; it was the only team to say in response to the survey that staffing felt sufficient.
The ADU site was set back behind some garages on a quiet residential street; the setting was very discreet, and it was impossible to discern the ADU unless actively looking for it. It was part of a larger community site but occupied its own building, which was single-storey and modern. Inside, it was unremarkable but well presented and functional. There was a large group room, a large art room, a common room with a small kitchen, and two smaller rooms that could be used for one-to-one sessions. There was a dedicated garden area where service users could sit and socialise as well as participate in occasional gardening sessions when weather permitted.
Chapter 6 Work package 2.1: cohort study – a comparison of re-admission rates, satisfaction and mental health outcomes in people using acute day units and people using only crisis resolution teams in four localities in England
Parts of this chapter have been reproduced from Lamb et al. 19 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
Methods: cohort study
Design
The design was a cohort study of ADU users and CRT users, comparing re-admission rates with those of the acute care pathway during a 6-month period, and satisfaction with services. Five sites with ADUs and CRTs were identified and recruited from the national survey carried out in WP 1, although one site dropped out of the study shortly after starting recruitment, leaving us with four study sites. Recruitment began in March 2017 and was completed by the end of March 2019, with follow-up completed by the end of September 2019. We invited people who were consecutively admitted to each ADU to participate in baseline interviews and then in telephone or online follow-up 8–12 weeks after baseline, with electronic health records (EHRs) outcome data collected at 6 months.
We also invited people from the trusts who used CRTs to participate in the parallel non-ADU cohort.
Objectives
-
To describe the clinical and sociodemographic characteristics of people who use each of the ADUs selected for the in-depth case studies.
-
To determine their pathways into the ADU, length of stay, treatments received, experience, empowerment, loneliness and re-admissions.
-
To compare these characteristics with those of a cohort of people who receive acute CRT care in the same locality but without ADU input.
Setting
Data were collected from ADUs and CRTs in four NHS mental health trusts in England. We investigated the possibility of including a voluntary/joint voluntary–NHS ADU service in the study, but no such units were able to provide the data required to enable a comparison with a local CRT service. Therefore, the study focused on NHS ADUs, as identified by the mapping and survey work of WP 1.
Sample size
We calculated the sample size to detect a 12–13% absolute reduction in the main outcome of re-admissions to the acute pathway at 6 months after baseline (using admission figures from previous research). Our CORE programme grant in crisis teams was powered at 80% to detect a 15% difference between trial arms (50% vs. 35%). Data from London crisis services suggest that baseline re-admission rates could be lower, at 40%. We explored various sample size calculations, including different assumptions regarding this baseline re-admission rate. These showed that 310 people in each arm would afford 90% power to detect differences such as 50% compared with 36.8%, 45% compared with 32.0% or 40% compared with 27.4%. Inflating for a design effect by 30% to accommodate the clustered study design required 400 per arm. These numbers also afforded > 90% power to detect an effect size or difference of 0.3 standard deviations in the client experience measure the CSQ-8 [crisis team mean CSQ 25, standard deviation (SD) 6]. Therefore, we required 400 ADU participants and 400 CRT participants (total n = 800).
Participants
Inclusion criteria
Inclusion criteria were as follows:
-
aged ≥ 18 years
-
have used the ADU/CRT service for at least 1 week
-
can read and understand English (or there are translation services in place to enable communication)
-
have the capacity to provide informed consent
-
do not pose too high a risk to others or themselves to participate.
Exclusion criteria
We excluded service users who were too unwell to consent, but otherwise we aimed to be inclusive to gain a fully representative sample, including using local interpretation facilities for people who did not speak sufficient English, when necessary.
Measures
Data were collected from participants using a questionnaire (provided in hard copy or online) at baseline, and another questionnaire 8–12 weeks later, and baseline and 6-month data were collected from EHRs by researchers. The validated measures used in the questionnaire are listed in the next few sections. A full list of the variables included in data collection at each time point is available in Table 12.
| Data source | Time point | ||
|---|---|---|---|
| Baseline | 8- to 12-week follow-up | 6-month follow-up | |
| Questionnaire |
|
|
N/A |
| EHR |
|
N/A |
|
The primary outcome was re-admission for acute treatment during the 6-month study period, which was collected from service use data in the EHRs. After discharge from the service used at baseline, any subsequent use of acute mental health services during the 6-month study period was recorded, along with the duration of each admission to services and any detention under the Mental Health Act (MHA).
The full baseline questionnaire is available in Report Supplementary Material 2, the full follow-up questionnaire is available in Report Supplementary Material 3 and the full EHR data collection schedule is available in Report Supplementary Material 4.
Client Satisfaction Questionnaire – 8-item version
The CSQ-8 was used to collect self-report data on satisfaction with services. The scale has eight items that ask about satisfaction with the mental health service used at baseline, with four response categories indicating low to high satisfaction. Responses are summed to provide a total score, with higher scores indicating greater satisfaction. 20 The scale has evidence of good internal consistency and adequate construct validity. 20
Short Warwick–Edinburgh Mental Well-being Scale
The Short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS)21 was used to collect self-report data from participants about their mental well-being. The scale has seven positively worded items, answered in reference to thoughts and feelings over the past 2 weeks, using five response categories (from ‘none of the time’ to ‘all of the time’), and responses are summed to provide a single score, with higher scores indicating better well-being. The scale shows adequate internal consistency and reliability. 21 Increases in scores of 1–3 points are considered to represent clinically meaningful increases in well-being.
Center for Epidemiologic Studies Depression Scale
The Center for Epidemiologic Studies Depression Scale-10 (CES-D-10) was used to collect self-report data from participants about feelings of depression. The scale has 10 positively and negatively worded items, answered in reference to feelings over the past week, using four response categories (from ‘rarely or none of the time’ to ‘all of the time’), and responses are summed to provide a single score, with higher scores indicating higher levels of depression. The scale showed adequate validity. 22 A cut-off score of ≥ 10 is suggested to indicate the presence of depressive symptoms.
The questionnaire also included the following measures for use by a PhD (Doctor of Philosophy) student associated with the project:
-
University of California, Los Angeles (UCLA) Loneliness Scale (8-item version)23
-
Lubben Social Network Scale (6-item version)24
-
Health and Lifestyles Survey Social Capital Questionnaire25
-
Internalized Stigma of Mental Illness Inventory (10-item version). 26
The data from these measures will be analysed at a later date.
Procedure
At baseline, ADU/CRT staff screened all service users consecutively admitted to their service from the start date. All service users who met the inclusion criteria were approached by ADU/CRT staff/trust-employed clinical studies officers/clinical researchers and asked if they were willing to discuss participation further (except at sites where service users had already given consent to be contacted directly about research projects, in which case researchers contacted service users directly once their eligibility and any risk-related safety requirements had been established). The researchers kept a record of potential participants to be contacted and the date and the name of the clinician with whom this had been agreed. Researchers noted the service user’s agreement to being contacted by a researcher in their EHRs. Those who agreed were contacted by a researcher with an information sheet and offer to answer any questions. Potential participants were given at least 24 hours to consider whether or not they wanted to take part, and if they were still interested their consent was taken by a researcher, who also collected the baseline data. Consent and data collection could occur up to 14 days post discharge.
Participants were offered reimbursement of £20 (in vouchers) for taking part (£10 for the baseline interview and £10 for the follow-up interview 8–12 weeks after baseline). Participants were telephoned by a researcher 8–12 weeks after baseline for the collection of follow-up data. At 6 months after baseline, participant data were collected from EHRs and clinical notes.
Although many people find talking about their experiences to be helpful, some found that completing the questionnaire brought up issues that caused emotional distress. Where this happened, the researcher provided immediate emotional support to the participant, offered to pause or postpone the interview, and, if the participant asked, contacted a person of the participant’s choice (e.g. current care co-ordinator, carer, friend, family member, colleague) on their behalf.
If service users or carers reported any untoward feedback about the service used, the researcher conducting the interview asked the participant whether or not they wanted the researcher to pass this on to the service or other relevant person. If the untoward feedback was of a nature that led the researcher to be concerned for the safety of others, the participant was informed that the feedback would be passed on to the relevant service or person to be addressed, but that, if desired and if possible, they would remain anonymous.
Analysis
We derived descriptive statistics comparing the baseline characteristics of the CRT cohort and ADU cohort for the sample as a whole, and within sites. We explored baseline differences in demographics, clinical data and content of care using parametric and non-parametric tests, as appropriate.
For the primary outcome (time to acute admission during the 6-month study period) we compared the time to re-admission in the CRT cohort compared with the ADU cohort using Cox regression and adjusting for trust, age, sex, diagnosis [severe mental illness (SMI) or not], employment, Health of the Nation Outcome Scales (HoNOS) score, SWEMWBS score and whether or not the person had previously been an inpatient. Covariates were added using a stepwise procedure, starting with a univariate model with trust as a fixed effect, and then adding age, sex and employment, followed by diagnosis, followed by HoNOS score, followed by SWEMWBS score, followed by previous inpatient. We tested for any interaction between team (ADU/CRT) and trust as a sensitivity analysis.
In addition, we analysed a number of secondary outcomes:
-
We compared satisfaction mean CSQ-8 scores at the 8- to 12-week time point in the two cohorts using linear regression, using trust as a fixed effect, and adjusting for important covariates (as above). We tested for effect modification by individual ADU. We did not make head-to-head comparisons of outcomes between the different ADUs.
-
We compared mean SWEMWBS scores at the 8- to 12-week time point in the two cohorts using linear regression, as above.
-
We compared mean CES-D-10 depression scores at the 8- to 12-week time point in the two cohorts using linear regression, as above.
-
We compared the duration of admissions in the CRT cohort compared with the ADU cohort using Poisson regression, adjusting for the same covariates as above.
Results: cohort study
Five sites were recruited to participate, but, owing to ADU service closures, one site withdrew from the study. Recruitment began in April 2017 and concluded in March 2019. Participants were recruited from ADUs and CRTs in each participating trust.
Figure 3 shows the flow of participants into the study.
FIGURE 3.
The STROBE diagram of the flow of participants into the study. Adapted with permission from Lamb et al. 19 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
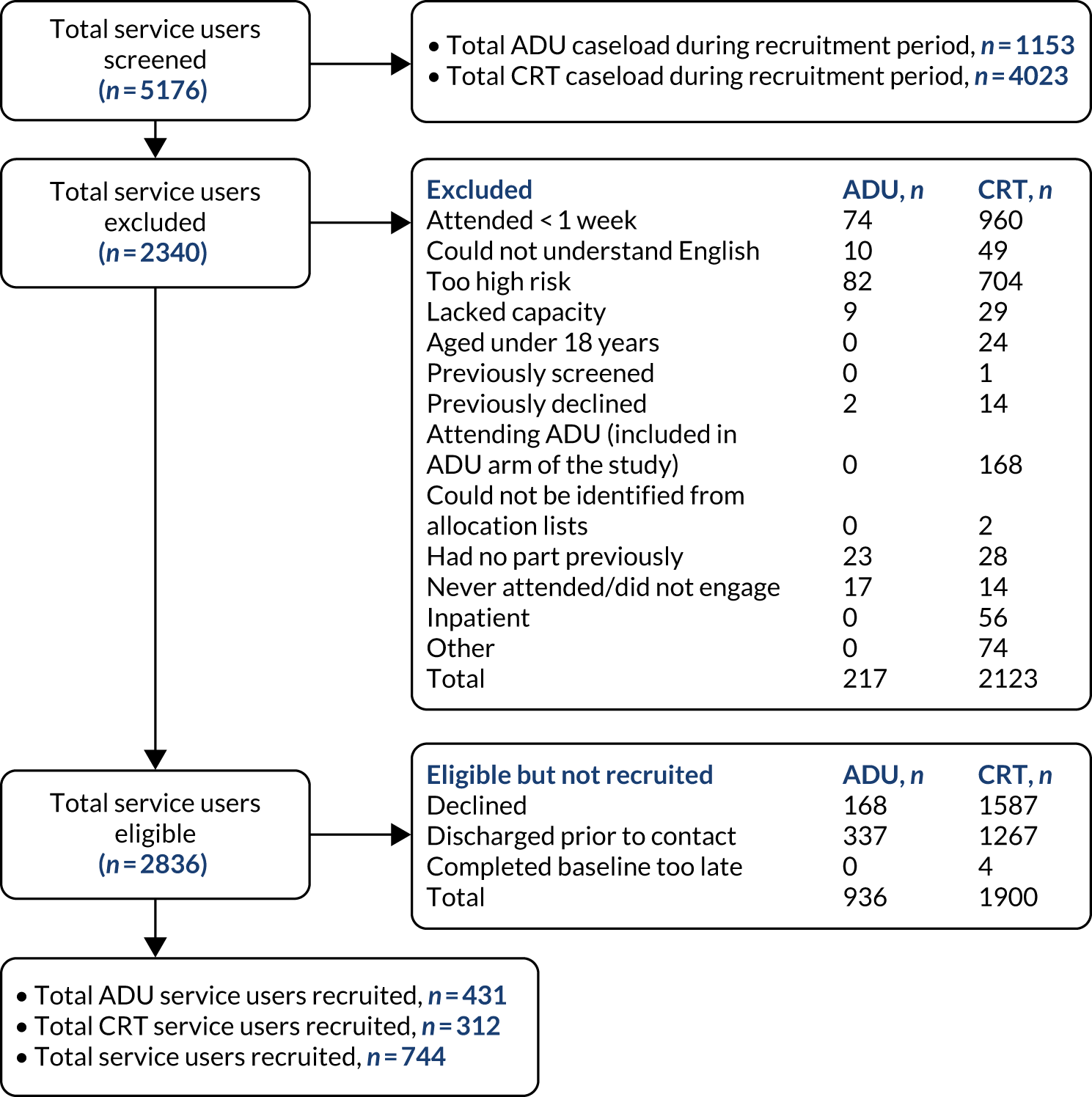
Cohort descriptives
Sociodemographic characteristics, clinical characteristics and baseline measures
A total of 743 participants were recruited: 431 from ADUs and 312 from CRTs. There was a small difference in age between the groups, with a mean ADU age of 42 years (SD 14.01 years) and mean CRT age of 39 years (SD 13.12 years). There was a slightly larger proportion of males using ADUs (51.04%) than CRTs (44.87%). The majority of participants in both groups were white (ADU, 84.58%; CRT, 82.30%). There was a substantial difference in the proportion of participants who were employed, with 29.23% of ADU participants employed compared with 42.63% of CRT participants. The majority of participants in both groups were single (ADU, 62.18%; CRT, 60.58%).
The most frequent International Statistical Classification of Diseases, Tenth Revision (ICD-10), diagnosis was mood disorders, accounting for 50% of each group, with more ADU participants diagnosed with psychosis (19.05%) than CRT participants (14.04%), and more ADU participants diagnosed with personality disorders (15%) than CRT participants (10.53%). Overall, 33.10% of ADU participants were diagnosed with SMI, compared with 28.07% of CRT participants. More ADU participants reported good, very good or excellent physical health (58.47%) than CRT participants (53.53%). More ADU participants were smokers (41.05%) than CRT participants (38.38%), but more CRT participants misused substances (27.60%) than ADU participants (24.29%). A higher proportion of ADU participants had previously been admitted to a psychiatric inpatient ward (57.54%; mean admissions 1.44, SD 2.54 admissions) than CRT participants (37.18%; mean admissions 1.09, SD 3.00 admissions).
The mean CES-D-10 depression scores were lower in ADU participants (16.4, SD 5.3) than in CRT participants (17.5, SD 5.4), whereas mean SWEMWBS scores were higher in ADU participants (18.15, SD 4.25) than in CRT participants (18.02, SD 4.88). The mean HoNOS score for ADU participants was 14 (SD 6.10), compared with 12 (SD 6.17) for CRT participants.
In terms of content of care while using the ADU or CRT at the start of participating in the study, 80.38% of ADU participants received a physical health assessment, compared with 34.19% of CRT participants. Carers were involved for 43.06% of ADU participants (CRT 32.90%), and 58.77% of ADU participants received psychological input during their care (CRT 41.23%).
Table 13 provides more details.
| Characteristic/variable | ADU | CRT | Total |
|---|---|---|---|
| Sociodemographic characteristic | |||
| Age (years), mean (SD) | 41.83 (14.01) | 38.95 (13.12) | 40.62 (13.70) |
| Sex | |||
| Male | 220 (51.04) | 140 (44.87) | 360 (48.45) |
| Female | 211 (48.96) | 172 (55.13) | 383 (51.55) |
| Ethnicity | |||
| White | 362 (84.58) | 251 (82.30) | 613 (83.63) |
| Black | 23 (5.37) | 17 (5.57) | 40 (5.46) |
| Asian | 28 (6.54) | 17 (5.57) | 45 (6.14) |
| Mixed | 15 (3.50) | 20 (6.56) | 35 (4.77) |
| Employed (yes) | 126 (29.23) | 133 (42.63) | 259 (34.86) |
| Marital status | |||
| Single | 268 (62.18) | 189 (60.58) | 457 (61.51) |
| Cohabiting | 41 (9.51) | 37 (11.86) | 78 (10.50) |
| Married | 88 (20.42) | 69 (22.12) | 157 (21.13) |
| Divorced | 31 (7.19) | 15 (4.81) | 46 (6.19) |
| Widowed | 3 (0.70) | 2 (0.64) | 5 (0.67) |
| Clinical characteristic | |||
| ICD-10 diagnosis | |||
| Psychosis | 80 (19.05) | 40 (14.04) | 120 (17.02) |
| Mood disorders | 210 (50.00) | 143 (50.18) | 353 (50.07) |
| Anxiety | 55 (13.10) | 55 (19.30) | 110 (15.60 |
| Personality disorders | 63 (15.00) | 30 (10.53) | 93 (12.19) |
| Other | 12 (2.86) | 17 (5.96) | 29 (4.11) |
| SMI (yes) | 139 (33.10) | 80 (28.07) | 219 (31.06) |
| Physical health | |||
| Excellent | 21 (4.87) | 17 (5.45) | 38 (5.11) |
| Very good | 84 (19.49) | 49 (15.71) | 133 (17.90) |
| Good | 147 (34.11) | 101 (32.37) | 248 (33.38) |
| Fair | 124 (28.77) | 85 (27.24) | 209 (2813) |
| Poor | 55 (12.76) | 60 (19.23) | 115 (15.48) |
| Comorbidity | |||
| Mental health | 100 (23.58) | 74 (23.87) | 174 (23.71) |
| Physical health | 101 (23.81) | 57 (18.39) | 158 (21.53) |
| Both | 58 (13.68) | 38 (12.26) | 96 (13.08) |
| Substance misuse (yes) | 103 (24.29) | 85 (27.60) | 188 (25.68) |
| Smoker (yes) | 172 (41.05) | 114 (38.38) | 286 (39.94) |
| Previous inpatient (yes) | 248 (57.54) | 116 (37.18) | 364 (48.99) |
| Number of previous admissions, mean (SD) | 1.44 (2.54) | 1.09 (3.00) | 1.29 (2.75) |
| Baseline measure | |||
| CES-D-10 depression score | 16.4 (5.3) | 17.5 (5.4) | 28.81 (7.84) |
| SWEMWBS score | 18.15 (4.25) | 18.02 (4.88) | 19.10 (4.52) |
| HoNOS score | 14.10 (6.10) | 12.43 (6.17) | 13.39 (6.18) |
| Content of care | |||
| Physical assessment | 340 (80.38) | 106 (34.19) | 445 (60.85) |
| Carers involved | 183 (43.06) | 102 (32.90) | 285 (38.78) |
| Psychological input | 248 (58.77) | 174 (41.23) | 246 (33.61) |
Outcome measures
Only one participant declined to give consent to access their EHRs at the 6-month time point, meaning that follow-up data were collected for nearly 100% of participants on the primary outcome (i.e. the use of services during the 6-month study period). Follow-up data on the secondary outcomes were collected from 566 participants (76%) at the 8- to 12-week point.
The data collected from EHRs at the 6-month time point on the primary outcome show that 21.35% of ADU participants were re-admitted during the 6-month period, compared with 23.40% of CRT participants (Table 14). When the follow-up time at risk is taken into account, the re-admission rate was 54.87 for ADU participants and 55.33 for CRT participants per 100 person-years.
| Outcome | ADU | CRT | Total |
|---|---|---|---|
| Re-admitted, n (%) | 92 (21.35) | 73 (23.40) | 165 (22.21) |
| Re-admission rate per 100 person-years | 54.87 | 55.33 | 55.08 |
| CSQ score | 26.65 (5.04) | 24.37 (6.57) | 25.67 (5.85) |
| CES-D-10 depression score | 14.4 (6.0) | 16.6 (5.7) | 26.13 (8.46) |
| SWEMWBS score | 20.50 (4.97) | 19.20 (5.03) | 19.95 (5.03) |
The questionnaires completed at the 8- to 12-week follow-up point for the secondary outcomes show that ADU participants had higher CSQ satisfaction scores (mean 26.65, SD 5.04) than CRT participants (mean 24.37, SD 6.57). ADU participants had lower CES-D-10 depression scores (mean 14.4, SD 6.0) than CRT participants (mean 16.6, SD 5.7), and higher SWEMWBS well-being scores (mean 20.50, SD 4.97) than CRT participants (mean 19.20, SD 5.03).
Primary outcome: re-admission
The unadjusted model with trust as a fixed effect produced a hazard ratio (HR) for re-admission in the ADU group of 0.94 (95% CI 0.67 to 1.32). Adjusting for age, sex and employment in model 2 reduced the HR to 0.90 (95% CI 0.64 to 1.28). In model 3 the remaining covariates were added (SMI diagnosis, whether or not participant had previously been an inpatient, baseline HoNOS score and baseline SWEMWBS score). The addition of these covariates reduced the fully adjusted HR in model 3 to 0.78 (95% CI 0.54 to 1.14). None of the models showed statistically significant differences between the ADU and CRT groups.
As only three participants identified as transgender, they were included in the analysis under the sex category indicated by the name they provided. A sensitivity analysis was run excluding these three participants, which showed no significant changes in the model (model 4).
We then tested for any interaction between team (ADU or CRT) and trust in model 5, and found evidence of an interaction between ADU/CRT and trust and the primary outcome of re-admission. Model 5 showed that in trust 1 the risk of re-admission was statistically significantly lower for ADU participants than for CRT participants (0.46, 95% CI 0.25 to 0.83; p < 0.01). In trust 2 there was no statistically significant difference (0.74, 95% CI 0.39 to 1.42). In trust 3 the risk of admission was statistically significantly higher for ADU participants than for CRT participants (9.11, 95% CI 1.22 to 68.09; p = 0.03). In trust 4 there was no statistically significant difference between ADU and CRT participants (0.83, 95% CI 0.27 to 2.54).
Full results are shown in Table 15.
| Variable | Model 1: team, trust | Model 2: age, sex, employment | Model 3: SMI, previous inpatient, HoNOS score, SWEMWBS score | Model 4: sensitivity analysis for sex | Model 5: interaction between team and trust |
|---|---|---|---|---|---|
| CRT | 1 | 1 | 1 | 1 | – |
| ADU | 0.94 (0.67 to 1.32) | 0.90 (0.64 to 1.28) | 0.78 (0.54 to 1.14) | 0.80 (0.55 to 1.16) | – |
| Trust 1 | 1 | 1 | 1 | 1 | 1 |
| Trust 2 | 0.54 (0.37 to 0.81) | 0.52 (0.35 to 0.77) | 0.52 (0.34 to 0.79) | 0.52 (0.34 to 0.79) | 0.41 (0.22 to 0.75) |
| Trust 3 | 0.31 (0.19 to 0.49) | 0.31 (0.19 to 0.49) | 0.46 (0.27 to 0.77) | 0.44 (0.26 to 0.75) | 0.04 (0.01 to 0.32) |
| Trust 4 | 0.15 (0.83 to 0.28) | 0.15 (0.08 to 0.28) | 0.17 (0.09 to 0.32) | 0.17 (0.09 to 0.32) | 0.13 (0.05 to 0.34) |
| Age | – | 0.99 (0.98 to 1.01) | 0.99 (0.98 to 1.01) | 0.99 (0.98 to 1.01) | 0.99 (0.98 to 1.01) |
| Male | – | 1 | 1 | 1 | 1 |
| Female | – | 1.18 (0.84 to 1.66) | 1.41 (0.98 to 2.04) | 1.40 (0.97 to 2.02) | 1.42 (0.99 to 2.04) |
| Not employed | – | 1 | 1 | 1 | 1 |
| Employed | – | 0.78 (0.53 to 1.13) | 0.92 (0.61 to 1.39) | 0.94 (0.62 to 1.42) | 0.88 (0.58 to 1.33) |
| No SMI | – | – | 1 | 1 | 1 |
| SMI | – | – | 1.51 (1.03 to 2.23) | 1.52 (1.03 to 2.25) | 1.45 (0.98 to 2.13) |
| Not previous inpatient | – | – | 1 | 1 | 1 |
| Previous inpatient | – | – | 2.65 (1.72 to 4.07) | 2.68 (1.74 to 4.14) | 2.31 (1.51 to 3.52) |
| HoNOS score | – | – | 1.03 (1.00 to 1.06) | 1.03 (1.00 to 1.06) | 1.02 (0.99 to 1.05) |
| SWEMWBS score | – | – | 0.99 (0.94 to 1.03) | 0.99 (0.94 to 1.03) | 0.99 (0.94 to 1.04) |
| Team × Trust 1 | – | – | – | – | 0.46 (0.25 to 0.84) |
| Team × Trust 2 | – | – | – | – | 0.74 (0.39 to 1.43) |
| Team × Trust 3 | – | – | – | – | 9.11 (1.22 to 68.09) |
| Team × Trust 4 | – | – | – | – | 0.83 (0.27 to 2.54) |
Secondary outcomes
We compared service user satisfaction between CRT and ADU participants, using the CSQ-8 measured during the 8- to 12-week follow-up period, and found statistically significantly higher scores (indicating higher satisfaction) in ADU participants than in CRT participants (Table 16). The unadjusted standardised mean difference in satisfaction on the CSQ was 0.39. On average, and taking account of trust, age, sex, employment, SMI diagnosis and previous inpatient use, the mean CSQ score among ADU participants was 2.27 (95% CI 1.24 to 3.30) points higher than that of CRT participants (p < 0.001).
| Exposure variable | CSQ | SWEMWBS | CES-D-10 |
|---|---|---|---|
| Team (CRT) | |||
| ADU | 2.27 (1.24 to 3.30) | 1.38 (0.58 to 2.17) | –1.7 (–2.6 to –0.7) |
| Trust (trust 1) | |||
| Trust 2 | –0.63 (–2.14 to 0.88) | –1.25 (–2.41 to –0.09) | 1.2 (–0.2 to 2.6) |
| Trust 3 | –0.20 (–1.71 to 1.31) | –0.12 (–1.28 to 1.04) | 1.7 (0.2 to 3.1) |
| Trust 4 | 0.23 (–1.30 to 1.76) | –0.30 (–1.48 to –0.87) | –1.0 (–2.4 to 0.4) |
| Age | 0.71 (0.03 to 0.11) | 0.02 (–0.01 to 0.05) | 0.0 (0.0 to 0.0) |
| Sex (male) | |||
| Female | –0.12 (–1.10 to 0.86) | 0.12 (–0.64 to 0.87) | 0.6 (–0.3 to 1.5) |
| Employment (none) | |||
| Employed | 1.69 (0.63 to 2.76) | 1.88 (1.05 to 2.71) | –2.0 (–2.9 to –1.0) |
| SMI (none) | |||
| SMI | 0.28 (–0.85 to 1.42) | 0.21 (–0.69 to 1.11) | –1.4 (–2.4 to –0.3) |
| Previous inpatient (none) | |||
| Previous inpatient | 0.07 (–0.99 to 1.13) | –0.08 (–0.92 to 0.75) | 0.0 (–1.0 to 0.9) |
| SWEMWBS score, baseline | – | 0.49 (0.41 to 0.58) | – |
| CES-D-10 score, baseline | – | – | 0.5 (0.4 to 0.6) |
Acute day unit participants also showed statistically significantly higher levels of well-being at the 8- to 12-week follow-up point than CRT participants. ADU participants had, on average, and taking into account the same covariates as above, a SWEMWBS score 1.38 (95% CI 0.58 to 2.17) points higher than that of CRT participants (p = 0.001).
Acute day unit participants also had statistically significantly lower levels of depression at the 8- to 12-week follow-up point than CRT participants (see Table 16). ADU participants had, on average, and taking into account the same covariates as above, CES-D-10 depression scores –1.7 (95% CI –2.6 to –0.7) points lower than those of CRT participants (p < 0.001).
Discussion: cohort study
Summary of results
This WP aimed to compare the outcomes, in terms of re-admission to acute mental health care, satisfaction and well-being, in two cohorts: those using ADUs and those using CRTs. Having recruited 431 ADU participants and 312 CRT participants (n = 744), we found important sociodemographic and clinical differences between the groups. ADU participants were more likely to be unemployed, have an SMI diagnosis and have previously been admitted to an inpatient ward and have higher HoNOS scores (indicating more severe symptoms and poorer social functioning). These findings suggest that those served by ADUs are more unwell than those using CRTs.
Even taking into account these differences between the groups, there was no significant difference between them in terms of re-admission (HR 0.94, 95% CI 0.67 to 1.32). At 8–12 weeks, after accounting for baseline differences in participant characteristics, ADU participants had significantly higher satisfaction [CSQ score: 26.66 (SD 5.04) vs. 24.37 (SD 6.57)], with better well-being [SWEMWBS score: 20.51 (SD 4.96) vs. 19.02 (SD 5.03)] and lower depression [CES-D-10 14.4 (SD 6.0) vs. 16.6 (SD 5.7)] than CRT participants. These results indicate that, despite serving a more unwell client group, ADUs produce comparable outcomes in terms of re-admission, and better satisfaction, depression and well-being results than CRTs. The effect sizes for the difference in satisfaction appeared clinically meaningful, as did the differences in depression and well-being scores, even adjusting for baseline difference between ADU and CRT participants (see Tables 14 and 16).
Previous research
Although no previous research has directly compared the outcomes for ADU and CRT participants, there is evidence comparing ADUs with inpatient wards, and evidence about satisfaction and re-admissions in CRTs. In a randomised controlled trial comparing day hospitals with inpatient care, Priebe et al. 13 measured satisfaction using the Client’s Assessment of Treatment Scale (CAT)27 instead of the CSQ, but, similar to this study, they found significantly higher satisfaction among the day-hospital group than among inpatients at discharge and at 3 months (although no difference was found at 12 months). The CSQ has been used in several other studies of acute mental health services; for example, in a cohort study of people using standard acute inpatient wards compared with those using alternative residential crisis services (e.g. crisis houses), those using alternative services had significantly higher satisfaction scores [26.4 (SD 4.9) vs. 23.19 (SD 6.6)]. 28 These scores are comparable to those found in the current study, with greater satisfaction among those using ADUs and crisis houses than among those using CRTs and inpatient wards.
In terms of re-admission, the most recent meta-analysis of research on ADUs12 found no difference in re-admission rates between ADU and inpatient services. However, this meta-analysis did find some evidence (albeit of low quality) that those using ADUs had better outcomes than inpatients in terms of subsequent employment. This is particularly interesting given our finding that ADU participants in this cohort had lower rates of employment than CRT participants. Werbeloff et al. 29 investigated the re-admission of CRT service users over 1 year and found that having a psychotic disorder increased the risk of re-admission. This study found HoNOS scores in two CRT cohorts that were similar to the scores of our CRT participants [13.3 (SD 6.4) vs. 11.8 (SD 5.5)].
Strengths and limitations
This cohort study has four key strengths: (1) the direct comparison of those using ADUs and CRTs, which to our knowledge has not been undertaken previously; (2) the relatively large sample size; (3) the range of geographic locations of the participating services; and (4) the high follow-up rates. As discussed above, there is a lack of evidence about ADUs, the majority of work having been carried out some time ago and on services that were substantially different from those available currently. This study provides a comprehensive overview of the sociodemographic and clinical characteristics of those using ADUs and CRTs, and offers insights into the comparative benefits of each type of service in terms of outcomes. To our knowledge, this is the largest cohort study of ADU participants to date, which lends weight to these results. The participating services were in areas serving urban, suburban and rural communities, with high and low deprivation levels. We were able to follow up 99.99% of participants via their EHRs at the 6-month time point, which included our primary outcome of service use during the 6 months, and 76% of participants at the 8- to 12-week time point, which included the secondary outcomes of satisfaction, well-being and depression.
The study has three main limitations: (1) recruitment bias, (2) lack of randomisation of participants and (3) EHR data quality. As is typical in cohort studies of this nature, we were reliant on people who were attending participating services being willing and able to take part. The nature and severity of some service users’ illness excluded them from the study, and as a result our findings may not be applicable to the most unwell users of these services. However, the sample who were recruited from both ADUs and CRTs included those with a variety of diagnoses and people who had previously been admitted, and in both groups substantial use of mental health services was reported at follow-up. Furthermore, many participants were single and unemployed and had diagnoses that included psychosis and personality disorder. This indicates that our sample were indeed people who had complex mental health needs.
We recruited just under 750 people to the study, having originally aimed for a target of 800, which would have given 90% statistical power. It seems unlikely that this slight under-recruitment would have affected our main findings. The adjusted HR for re-admissions was 0.78 (95% CI 0.54 to 1.14), which is not suggestive of any difference between ADU users and CRT users, even if a larger sample had been recruited. The differences in satisfaction, well-being and depression, each of which was in favour of ADUs, were all statistically significant, with convincing effect sizes.
The fact that participants were not randomised could be seen as a limitation; however, we were able to recruit a larger sample size than would have been possible in a randomised controlled trial, and in the analysis we adjusted for baseline differences between the two groups, including history of admission. We collected a large number of data from routinely entered EHRs, and so we were reliant on these records being accurate and up to date. Missing data were evident for most variables, and a number of errors were identified in the data provided to us.
These cohort results are discussed further in the context of findings from other WPs in Chapter 10.
Chapter 7 Work package 2.1: health economics from cohort study
Methods: health economics analysis
General principles of the economics analysis
This analysis adopts a health-care perspective, focusing on acute mental health care. To examine the costs associated with acute mental health care for those accessing ADUs (the ADU group) compared with the costs for those not accessing ADUs (the CRT group), it was necessary to collect information on acute mental health care resource use and mental health outcomes. The time horizon was 6 months and, consequently, the discounting of costs and outcomes was not necessary. This analysis uses the price year of 2017 and adopts an intention-to-treat principle, whereby the groups at baseline were analysed regardless of whether or not they transferred between groups during the 6 months. In this analysis, statistical significance is determined by a p-value of < 0.05.
Identifying resource use and costs
The first step in the analysis of acute mental health costs was to identify the different types of mental health care that were of interest. As in the primary statistical analysis, these were refined to:
-
acute mental health ward
-
ADU
-
CRT
-
crisis house.
To examine the costs to the two groups, it was necessary to capture the number of days in contact with each of the aforementioned services. To do this, the details of acute mental health contacts were collected from EHRs for the 6 months from baseline. To calculate the costs of acute mental health care, resource use data were combined with unit cost data. The unit costs for acute mental health wards and CRTs were collected from Personal Social Services Research Unit data,30,31 and the unit costs for crisis houses were estimated from published case studies. 32,33 Given that no existing unit costs were found in the literature for ADUs, it was necessary to estimate a unit cost. To do this, participating ADUs were contacted and information on the annual budget for running the ADUs was requested and combined with information on average caseloads from the WP 1 mapping study. This information was used to calculate a cost per day while in contact with ADU services. Information on acute service resource use was then combined with the unit cost data to calculate the total cost of acute mental health care over the 6-month period. Given the lack of established unit cost data for ADUs and crisis houses, sensitivity analyses were required to examine the impact of changes in unit costs.
Analysis of cost
The analysis first examines the resource use data descriptively. Differences in resource use were examined using standard statistical tests (t-tests for continuous variables and chi-squared test for categorical variables). The total cost end point was then analysed using a series of increasingly complex models, as discussed below, to estimate the differences in costs. In all models, CIs were calculated using non-parametric bootstrapping methods:
-
Model 1 – adjustment for clustering. This regression model examined the difference in costs between the two groups including provider trust as a fixed effect.
-
Model 2 – partially adjusted model. This model builds on model 1 by including variables that were statistically significantly different at baseline as covariates in addition to provider trust.
-
Model 3 – fully adjusted model. This model builds on model 2 by including all the prespecified covariates, which included age, sex, SMI, employment, baseline HoNOS score, trust and previous inpatient admission.
Analysis of outcomes
The HoNOS was used as the primary outcome measure in the cost-effectiveness analysis. The HoNOS is collected routinely within mental health services and is reverse scored, so that the lower the score, the better the mental health state of the individual. The most recently measured HoNOS score in EHRs was recorded at both baseline and 6 months. The differences in HoNOS scores recorded at baseline and follow-up are first presented descriptively, with t-tests used to examine the difference between the two cohorts.
To examine the mental health outcomes for the two groups and to account for baseline differences, changes in HoNOS scores were calculated (HoNOS score at 6 months minus HoNOS score at baseline). Three models were used to examine the impact of the cohort on the change in HoNOS score during the follow-up period. As above, CIs were calculated using non-parametric bootstrapping. The models included were:
-
Model 1 – adjustment for clustering. This regression model examined the difference in HoNOS change between the two groups including provider trust as a fixed effect.
-
Model 2 – partially adjusted model. This model built on model 1 by including variables that were statistically significantly different at baseline as covariates in addition to provider trust.
-
Model 3 – fully adjusted model. This model built on model 2 by including all of the prespecified covariates, which included age, sex, SMI, employment, baseline HoNOS, trust and previous inpatient admission.
Exploratory cost-effectiveness analysis
To assess cost-effectiveness, methods that account for clustering, baseline differences and correlation between costs and outcomes were required. To do this, seemingly unrelated regressions were used to jointly model costs and HoNOS score change while accounting for baseline differences between the two groups by including the covariates from model 3 in the joint regression. Had costs and outcomes fallen into the north-east cost-effectiveness quadrant (i.e. more costly, more effective), the cost per HoNOS point associated with the ADU group would have been calculated and presented. To examine the probability of cost-effectiveness and to characterise uncertainty, a net-benefit regression framework was used to generate cost-effectiveness acceptability curves (CEACs). These were used to examine the probability that ADUs were more cost-effective than CRTs.
Given the lack of preference-based measures in this study, it was possible to conduct only a cost-effectiveness analysis and not a cost–utility analysis. Had ADUs been more effective but more costly than CRTs, we had planned to examine the number of quality-adjusted life-years that the ADU group would need to gain to achieve cost-effectiveness using the upper National Institute for Health and Care Excellence threshold of £30,000 per QALY. 34 The changes in HoNOS score were used to inform the likely qualitative direction of the quality-adjusted life-years gained and the plausibility of this cost-effectiveness interpretation.
Sensitivity analyses
In addition to the unadjusted and partially adjusted models of cost and outcomes, several further sensitivity analyses were performed to examine the sensitivity of results to changes in assumptions:
-
Sensitivity analysis 1 – given the lack of established unit costs for ADUs and for crisis houses, it was necessary to examine the impact of significant changes to the unit costs for these two services. Therefore, in the first sensitivity analysis, the cost of both services is increased by 25% so that the sensitivity of the results to these increases in cost can be examined.
-
Sensitivity analysis 2 – the second sensitivity analysis replicates the first analysis; however, in this instance the unit costs for ADUs and crisis houses are reduced by 25%.
-
Sensitivity analysis 3 – a number of participants in the CRT group went on to access ADU services. The primary analysis adopts an intention-to-treat principle. This sensitivity analysis excludes those who crossed over from CRT to ADU service use.
-
Sensitivity analysis 4 – multiple imputation to partially address concerns with follow-up HoNOS data. When it was not clear that a participant’s follow-up HoNOS score data had been updated in their medical records (i.e. the HoNOS data in the medical records were recorded as the same at baseline and at follow-up), these follow-up data points were treated as missing in this sensitivity analysis. Multiple imputation using chained equations with predictive mean matching for continuous variables and logit for binary variables was used to impute missing data. Primary analysis covariates were included as covariates in the imputation, and 35 imputation sets were created. The main cost-effectiveness analysis was then repeated, using multiple imputation estimation procedures in Stata® 16 (StataCorp, College Station, TX, USA).
Results: health economics analysis
Service use
The unadjusted acute mental health care service use data for both groups during the 6-month follow-up period are shown in Table 17. During the follow-up period, the ADU group used slightly more acute mental health ward services (mean 3.78 vs. 2.53 ward days) than the CRT group; this difference was not statistically significant. Unsurprisingly, the CRT group had statistically significantly more days in contact with CRT services than the ADU group (7.15 vs. 3.84 days in contact). There was no significant difference in days in contact with ADU services or crisis house services. The mean ADU use was marginally higher in the CRT group, driven in part by a few heavy users of ADUs. The fact that the heaviest user of ADU services was a participant from the CRT group demonstrates that there was significant contamination between the two groups, highlighting the need to carry out a sensitivity analysis excluding these individuals.
| Service use | Observed | Mean | SE | 95% CI | Minimum | Maximum | Test for differencea |
|---|---|---|---|---|---|---|---|
| Ward days | |||||||
| CRT | 312 | 2.53 | 0.85 | 0.85 to 4.20 | 0.00 | 170.00 | |
| ADU | 432 | 3.78 | 1.03 | 1.76 to 5.79 | 0.00 | 177.00 | p = 0.38 |
| CRT days | |||||||
| CRT | 312 | 7.15 | 1.11 | 4.98 to 9.32 | 0.00 | 138.00 | |
| ADU | 432 | 3.84 | 0.59 | 2.67 to 5.00 | 0.00 | 131.00 | p = 0.005 |
| ADU days | |||||||
| CRT | 312 | 1.58 | 0.72 | 0.16 to 3.00 | 0.00 | 153.00 | |
| ADU | 432 | 1.10 | 0.31 | 0.48 to 1.72 | 0.00 | 65.00 | p = 0.50 |
| Crisis house days | |||||||
| CRT | 312 | 0.80 | 0.32 | 0.18 to 1.42 | 0.00 | 71.00 | |
| ADU | 432 | 1.21 | 0.37 | 0.49 to 1.92 | 0.00 | 121.00 | p = 0.42 |
Table 18 presents the same service use information in terms of cost. Across both groups the highest costs were associated with acute mental health ward use (over £1000 per service user in both groups). The ADU group experienced higher acute mental health ward costs over the 6-month period than the CRT group (£1526 vs. £1021). The next highest costs were related to CRT days, with the CRT group accruing statistically significantly higher costs than the ADU group (£851 vs. £457). Crisis houses were the next most costly component of acute mental health care, with the ADU group costing slightly more than the CRT group (£400 vs. £265). Finally, ADU stays were the least costly, with both groups having a relatively low ADU cost per service user.
| Service use | Observed | Mean | SE | SD | 95% CI | Test for differencea |
|---|---|---|---|---|---|---|
| Ward costs | ||||||
| CRT | 312 | 1021.65 | 344.75 | 6089.49 | 343.32 to 1699.99 | |
| ADU | 432 | 1526.22 | 414.69 | 8619.23 | 711.15 to 2341.29 | p = 0.38 |
| CRT days | ||||||
| CRT | 312 | 850.54 | 131.57 | 2323.99 | 591.67 to 1109.42 | |
| ADU | 432 | 456.72 | 70.54 | 1466.24 | 318.06 to 595.37 | p = 0.005 |
| ADU days | ||||||
| CRT | 312 | 106.86 | 48.76 | 861.28 | 10.92 to 202.81 | |
| ADU | 432 | 74.52 | 21.27 | 442.05 | 32.72 to 116.32 | p = 0.5 |
| CH days | ||||||
| CRT | 312 | 264.96 | 104.85 | 1852.07 | 58.65 to 471.27 | |
| ADU | 432 | 400.40 | 121.31 | 2521.28 | 161.98 to 638.82 | p = 0.42 |
Analysis of acute mental health costs
The results of the analysis of acute mental health costs are shown in Table 19.
| Total cost | Coefficient | SE | z | p > z | 95% CI |
|---|---|---|---|---|---|
| Model 1 (cluster adjusted) | |||||
| ADU | 332.60 | 593.74 | 0.56 | 0.575 | –831.10 to 1496.31 |
| Trust | |||||
| Trust 2 | –652.09 | 933.11 | –0.7 | 0.485 | –2480.96 to 1176.78 |
| Trust 3 | –903.45 | 1046.55 | –0.86 | 0.388 | –2954.65 to 1147.74 |
| Trust 4 | –2549.56 | 798.37 | –3.19 | 0.001 | –4114.33 to –984.79 |
| _cons | 3248.43 | 879.42 | 3.69 | 0 | 1524.79 to 4972.06 |
| Model 2 (partially adjusted) | |||||
| ADU | –103.03 | 592.93 | –0.17 | 0.862 | –1265.16 to 1059.09 |
| Employed | –196.49 | 638.20 | –0.31 | 0.758 | –1447.34 to 1054.36 |
| Baseline HoNOS score | –35.78 | 48.30 | –0.74 | 0.459 | –130.453 to 58.89 |
| Trust | |||||
| Trust 2 | –200.62 | 832.21 | –0.24 | 0.81 | –1831.72 to 1430.48 |
| Trust 3 | 342.87 | 1087.88 | 0.32 | 0.753 | –1789.32 to 2475.07 |
| Trust 4 | –1699.51 | 681.00 | –2.5 | 0.013 | –3034.25 to –364.78 |
| Previous inpatient: yes | 2908.56 | 699.32 | 4.16 | 0.000 | 1537.93 to 4279.20 |
| _cons | 1936.02 | 1025.76 | 1.89 | 0.059 | –74.43 to 3946.47 |
| Model 3 (fully adjusted) | |||||
| ADU | –37.17 | 662.65 | –0.06 | 0.955 | –1335.94 to 1261.61 |
| Age | 6.51 | 24.92 | 0.26 | 0.794 | –42.3287 to 55.36 |
| Sex: women | 909.31 | 676.84 | 1.34 | 0.179 | –417.273 to 2235.89 |
| SMI: yes | 1560.04 | 799.34 | 1.95 | 0.051 | –6.64337 to 3126.72 |
| Employed: yes | 145.96 | 717.92 | 0.20 | 0.839 | –1261.14 to 1553.06 |
| Baseline HoNOS score | –15.51 | 55.73 | –0.28 | 0.781 | –124.741 to 93.72 |
| Trust | |||||
| Trust 2 | 45.57 | 863.85 | 0.05 | 0.958 | –1647.54 to 1738.68 |
| Trust 3 | 498.94 | 1154.20 | 0.43 | 0.666 | –1763.26 to 2761.14 |
| Trust 4 | –1709.33 | 687.41 | –2.49 | 0.013 | –3056.62 to –362.04 |
| Previous inpatient: yes | 2619.76 | 706.62 | 3.71 | 0 | 1234.81 to 4004.72 |
| _cons | 382.34 | 1710.67 | 0.22 | 0.823 | –2970.50 to 3735.19 |
The final fully adjusted model 3 further reduces the cost difference between the two groups to a negligible amount (the mean cost is £37 lower in the ADU group than in the CRT group). Again, whether or not the individual has had a previous inpatient admission is the largest predictor of cost and is highly significant. Those who have SMI have higher costs than those who do not, but this is not statistically significant at the 5% level (p = 0.051). Trust 4 is again associated with lower costs than trust 1 at a statistically significant level. Following adjustment for baseline imbalances, there is no significant difference in the costs accrued by the two groups.
In model 1, NHS trust is included in the linear regression as a fixed effect. In this model, the ADU group is associated with increased costs (£332) compared with the CRT group. As demonstrated by the wide CIs, considerable uncertainty surrounds this mean cost difference. Of note, trust 4 had significantly lower costs than the comparator, trust 1.
Given the extensive baseline imbalance, model 2 adjusts for statistically significant baseline differences. When this is done, the cost difference between the ADU group and CRT group largely disappears, with the ADU group associated with marginally lower costs than the CRT group. The significant imbalance at baseline between the groups in terms of ‘previous inpatient admission’ appears to be particularly important. In model 2 this is the largest and most significant predictor of mental health costs, with those who have previously had an inpatient admission accruing significantly more costs than those who have not. The difference between trusts 1 and 4 remains significant; however, the cost difference is reduced following adjustment.
The final fully adjusted model 3 further reduces the cost difference between the two groups to a negligible amount (the ADU group is a mean of £37 cheaper than the CRT group). Again, whether or not the individual has had a previous inpatient admission is the largest predictor of cost and is highly significant. Those who have SMI have higher costs than those who do not, but the difference is not statistically significant at the 5% level (p = 0.051). Trust 4 is again associated with lower costs than trust 1 at a statistically significant level. Following adjustment for baseline imbalances, there is no significant difference between the costs accrued by the two groups. The full results can be seen in Table 19.
Analysis of Health of the Nation Outcome Scales scores
The raw unadjusted HoNOS scores are given in Table 20 for the groups at both baseline and 6-month follow-up. Both groups saw improvements between baseline and follow-up. The HoNOS scores in the CRT group improved from 12.43 to 11.91 and those in the ADU group improved from 14.11 to 13.26.
| Time point | Observed | Meana | SE | SD | 95% CI |
|---|---|---|---|---|---|
| Baseline | |||||
| CRT | 288 | 12.43 | 0.36 | 6.18 | 11.72 to 13.15 |
| ADU | 394 | 14.11 | 0.31 | 6.09 | 13.51 to 14.71 |
| Follow-up | |||||
| CRT | 292 | 11.91 | 0.35 | 5.97 | 11.22 to 12.60 |
| ADU | 400 | 13.26 | 0.32 | 6.34 | 12.64 to 13.89 |
The analysis of the change from baseline in HoNOS scores is shown in Table 21. When adjusted solely for clustering, model 1 suggests that the ADU group improved slightly (not statistically significantly) more than the CRT group, with a larger fall in HoNOS score between baseline and follow-up.
| HoNOS score change | Coefficienta | SE | z | p > z | 95% CI |
|---|---|---|---|---|---|
| Model 1 HoNOS (cluster adjusted) | |||||
| ADU | –0.27 | 0.39 | –0.69 | 0.493 | –1.03 to 0.50 |
| Trust | |||||
| Trust 2 | 1.04 | 0.58 | 1.77 | 0.076 | –0.11 to 2.18 |
| Trust 3 | –0.10 | 0.56 | –0.18 | 0.86 | –1.19 to 0.99 |
| Trust 4 | –0.48 | 0.63 | –0.77 | 0.444 | –1.72 to 0.76 |
| _cons | –0.74 | 0.48 | –1.53 | 0.126 | –1.68 to 0.21 |
| Model 2 HoNOS (partially adjusted) | |||||
| ADU | 0.39 | 0.38 | 1.01 | 0.310 | –0.36 to 1.14 |
| Employed | –0.84 | 0.37 | –2.28 | 0.023 | –1.56 to –0.12 |
| Baseline HoNOS | –0.36 | 0.05 | –7.89 | 0.000 | –0.45 to –0.27 |
| Trust | |||||
| Trust 2 | –0.17 | 0.54 | –0.31 | 0.757 | –1.23 to 0.90 |
| Trust 3 | –1.45 | 0.51 | –2.85 | 0.004 | –2.45 to –0.45 |
| Trust 4 | –1.06 | 0.59 | –1.80 | 0.071 | –2.21 to 0.09 |
| Previous inpatient: yes | –0.80 | 0.38 | –2.07 | 0.039 | –1.55 to –0.04 |
| _cons | 5.33 | 0.83 | 6.41 | 0.000 | 3.70 to 6.96 |
| Model 3 HoNOS (fully adjusted) | |||||
| ADU | 0.24 | 0.38 | 0.62 | 0.533 | –0.51 to 0.98 |
| Age | –0.01 | 0.01 | –0.35 | 0.730 | –0.03 to 0.02 |
| Sex: women | –0.06 | 0.37 | –0.17 | 0.862 | –0.79 to 0.66 |
| SMI: yes | –0.89 | 0.46 | –1.92 | 0.054 | –1.79 to 0.02 |
| Employed: yes | –1.18 | 0.40 | –2.93 | 0.003 | –1.97 to –0.39 |
| Baseline HoNOS score | –0.35 | 0.04 | –9.49 | 0.000 | –0.42 to –0.27 |
| Trust | |||||
| Trust 2 | –0.28 | 0.59 | –0.47 | 0.637 | –1.43 to 0.87 |
| Trust 3 | –1.52 | 0.56 | –2.71 | 0.007 | –2.62 to –0.42 |
| Trust 4 | –0.95 | 0.57 | –1.66 | 0.097 | –2.07 to 0.17 |
| Previous inpatient: yes | –0.69 | 0.41 | –1.68 | 0.093 | –1.51 to 0.12 |
| _cons | 5.72 | 1.08 | 5.31 | 0.000 | 3.61 to 7.83 |
When model 2 is partially adjusted by adding the statistically significant baseline variables, this difference disappears, with the CRT group experiencing a larger fall in HoNOS score than the ADU group. In this model, both baseline HoNOS score and previous inpatient admission are significant predictors of larger falls in HoNOS score. This suggests that the baseline differences in groups may be responsible for the majority of the difference between the two groups in model 1. Employment is also a significant predictor of a decrease in HoNOS score, with the suggestion that those in employment improved more than those who were unemployed over the 6-month period. Additionally, both trust 3 and trust 4 saw statistically significant improvements in HoNOS score compared with trust 1 (the comparator).
The implications of the final fully adjusted model 3 are similar to those of model 2. Again, the CRT group improves more than the ADU group, with baseline HoNOS score the most significant predictor of improvement. Employment status remains a statistically significant predictor of improvement from baseline. Trust 3 sees greater improvements than the comparator trust 1. Although it maintains the same direction, previous inpatient attendance is no longer statistically significant in this model. Given the strong and significant associations between baseline HoNOS score and HoNOS score change in models 2 and 3, this suggests that the larger change from baseline for the ADU group seen in model 1 is likely to be regression to the mean, with those in a worse initial health state having more potential to improve. This is reflected in the reversal of direction for the treatment group variable once covariate imbalances are included.
Cost-effectiveness analysis
The results of the fully adjusted joint analysis of costs and HoNOS score change are shown in Table 22.
| Seemingly unrelated regression | Coefficient | SE | z | p > z | 95% CI |
|---|---|---|---|---|---|
| Cost | –39.39 | 697.75 | –0.06 | 0.96 | –1406.96 to 1328.17 |
| HoNOS score change | 0.24 | 0.39 | 0.60 | 0.55 | –0.54 to 1.01 |
When costs and outcomes are analysed jointly, a marginal cost saving is associated with the ADU group compared with the CRT group. However, in terms of HoNOS score change, the ADU group performed less well than the CRT group. As demonstrated by the large CIs surrounding the estimates, there is a great deal of uncertainty around these results. To examine this uncertainty and the corresponding probability of cost-effectiveness, a CEAC was created, which is shown in Figure 4.
FIGURE 4.
Cost-effectiveness acceptability curve: probability of cost-effectiveness.
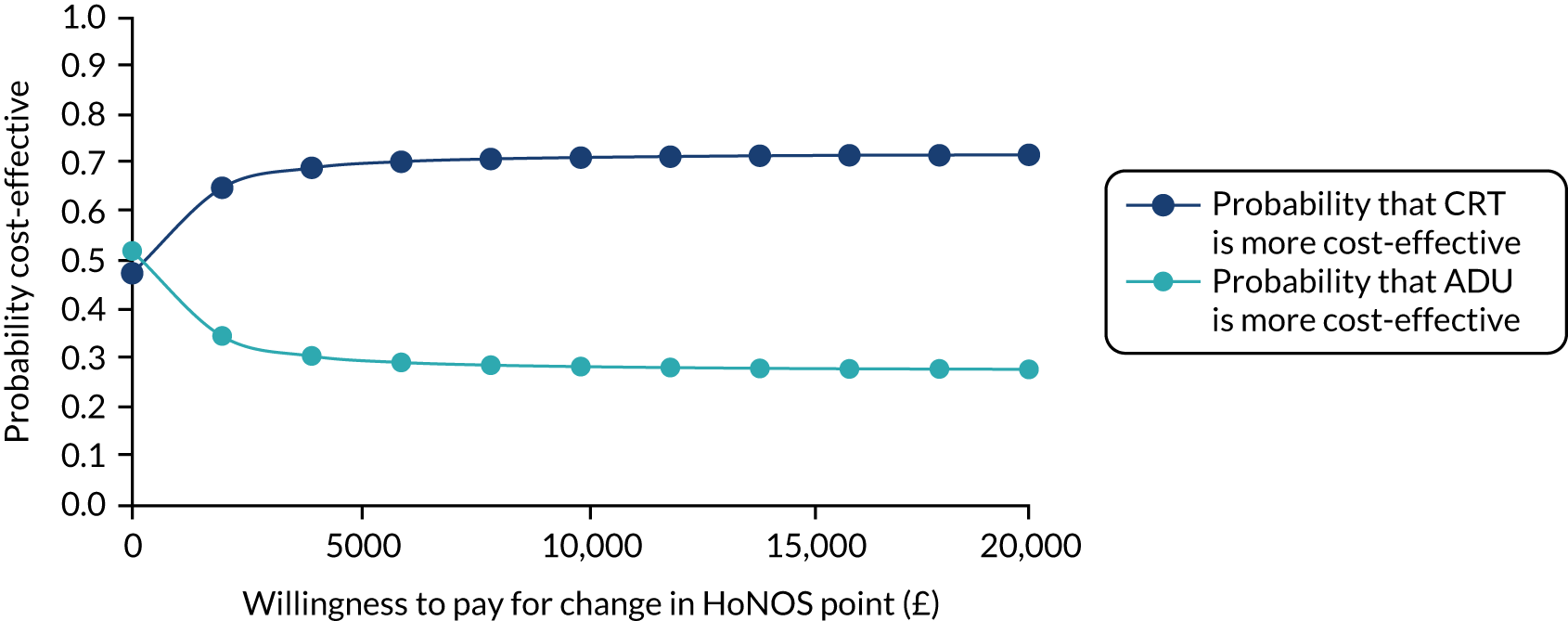
If we do not value benefits (i.e. no willingness to pay for HoNOS improvements), then there is a 52% probability that the ADU group is the more cost-effective option. As the willingness to pay for HoNOS improvements increases, the CRT group becomes the superior choice, with a 65% probability of being the more cost-effective option at a willingness to pay of £2000 per HoNOS point decrease before levelling off at 70% at a willingness to pay of £6000 per HoNOS point. Given the lack of difference in costs, this change is driven largely by the fact that, after baseline adjustment, the CRT group was associated with greater improvements than the ADU group.
The results of the four sensitivity analyses are shown in Table 23.
| Seemingly unrelated regression | Coefficient | SE | z | p > z | 95% CI |
|---|---|---|---|---|---|
| 1. Inflated crisis house and ADU costs | |||||
| Cost | 7.63 | 719.81 | 0.01 | 0.992 | –1403.16 to 1418.43 |
| HoNOS score change | 0.24 | 0.39 | 0.60 | 0.548 | –0.54 to 1.01 |
| 2. Deflated crisis house and ADU costs | |||||
| Cost | –86.42 | 679.11 | –0.13 | 0.899 | –1417.46 to 1244.61 |
| HoNOS score change | 0.24 | 0.39 | 0.60 | 0.548 | –0.54 to 1.01 |
| 3. Excluding those who crossed from CRT to ADU | |||||
| Cost | 124.41 | 710.26 | 0.18 | 0.861 | –1267.67 to 1516.50 |
| HoNOS score change | 0.23 | 0.40 | 0.56 | 0.575 | –0.56 to 1.02 |
| 4. Multiply imputed data | |||||
| Cost | –185.70 | 657.46 | –0.28 | 0.78 | –1474.30 to 1102.89 |
| HoNOS score change | 0.65 | 0.63 | 1.03 | 0.30 | –0.59 to 1.89 |
In the first two sensitivity analyses, the costs associated with care are altered. In terms of the joint analysis of costs, this has relatively little impact on the overall findings. In this first instance, the costs associated with the ADU are marginally higher than those associated with CRT, but this difference is negligible. Likewise, in sensitivity analysis 2, the cost savings associated with the ADU group increase compared with those associated with the CRT group. However, in the context of the uncertainty around the cost estimates, this has very little impact on the overall picture, as demonstrated in Figures 5 and 6, which show that, once any willingness to pay for benefits is considered, the CRT becomes more likely to be the cost-effective option. Sensitivity analysis 3 explores the impact of excluding those who crossed from the CRT group to the ADU group. In this analysis the ADU group is associated with higher costs than the CRT group. This cost difference is, again, relatively small when the uncertainty around the estimates is considered. The impact of this change is shown in Figure 7, which shows that CRT is the more cost-effective option at all levels of willingness to pay for benefits. In the final sensitivity analysis, which imputes for missing data, the ADU group is associated with lower costs than the CRT group; however, again there is substantial uncertainty around this estimate. The CRT group performs better than the ADU group in this analysis, with a slightly larger coefficient than in the primary analysis. This has relatively little impact on the overall interpretation, as shown in Figure 8. If outcomes are ignored, there is a 60% chance that ADU is the more cost-effective option; however, once outcomes are valued, CRT becomes the more cost-effective option.
FIGURE 5.
Sensitivity analysis 1: CEAC for inflated ADU/crisis house costs.
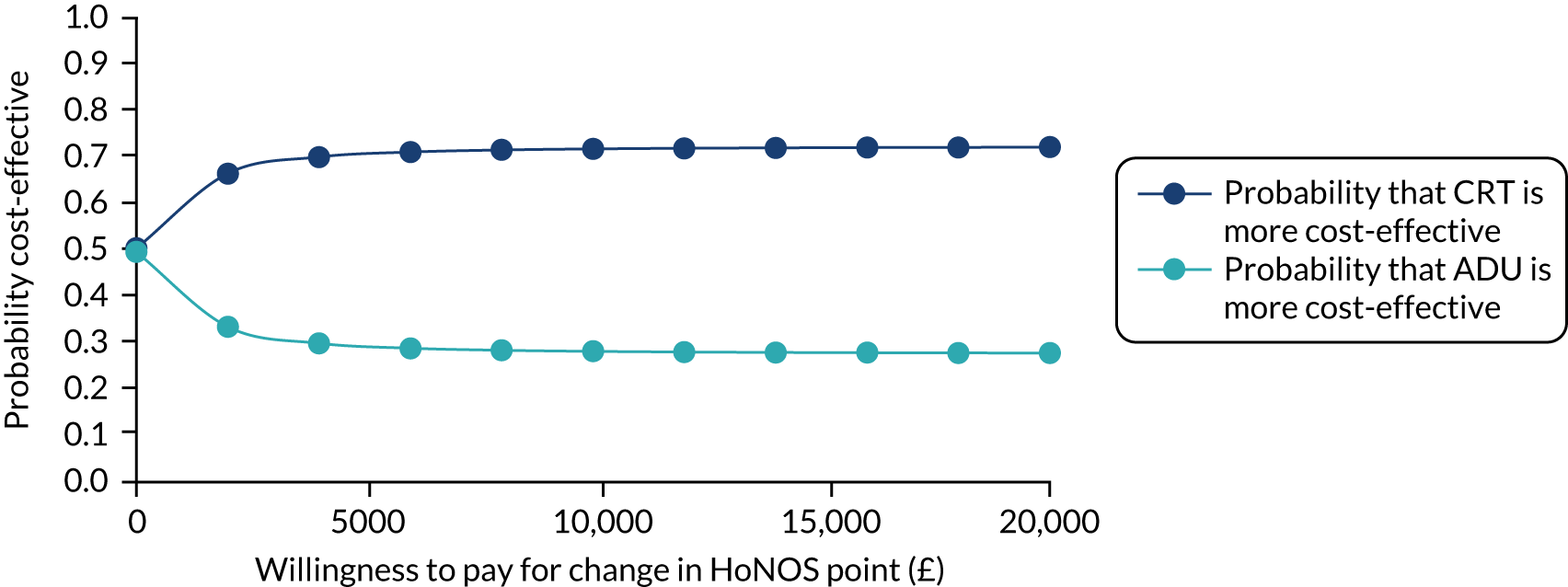
FIGURE 6.
Sensitivity analysis 2: CEAC for deflated ADU/crisis house costs.
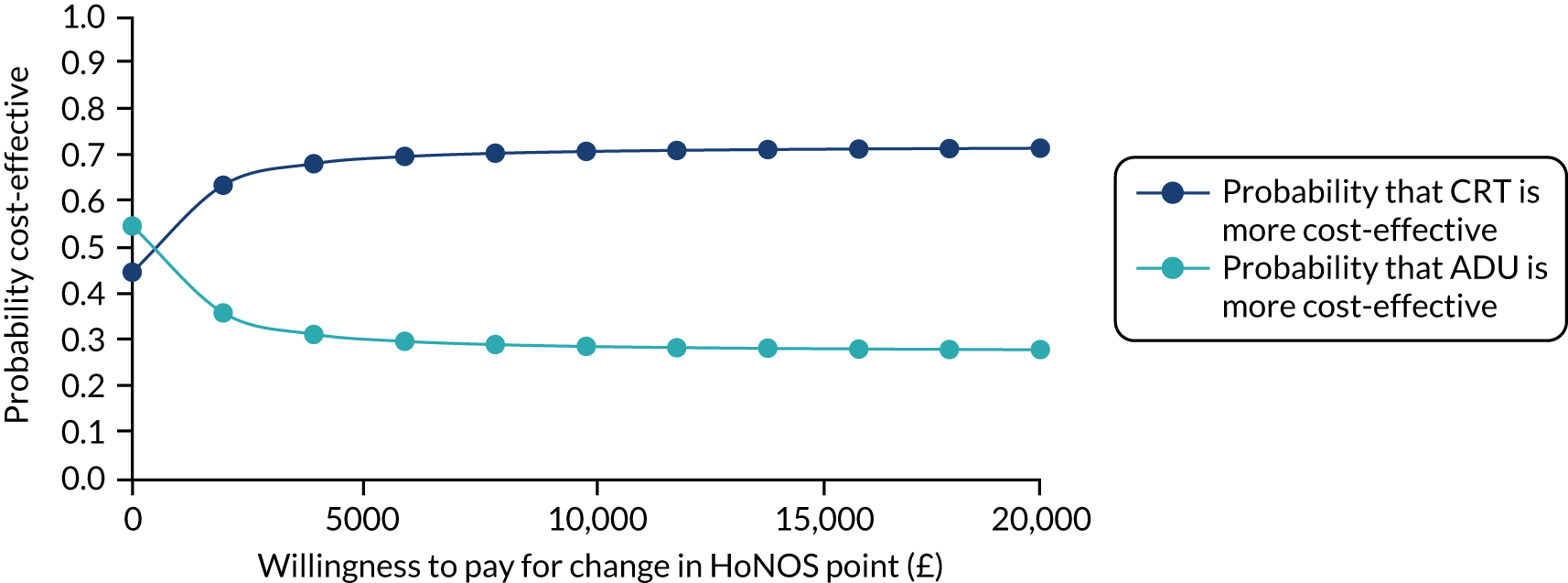
FIGURE 7.
Sensitivity analysis 3: excluding those who crossed over from CRT to ADU.
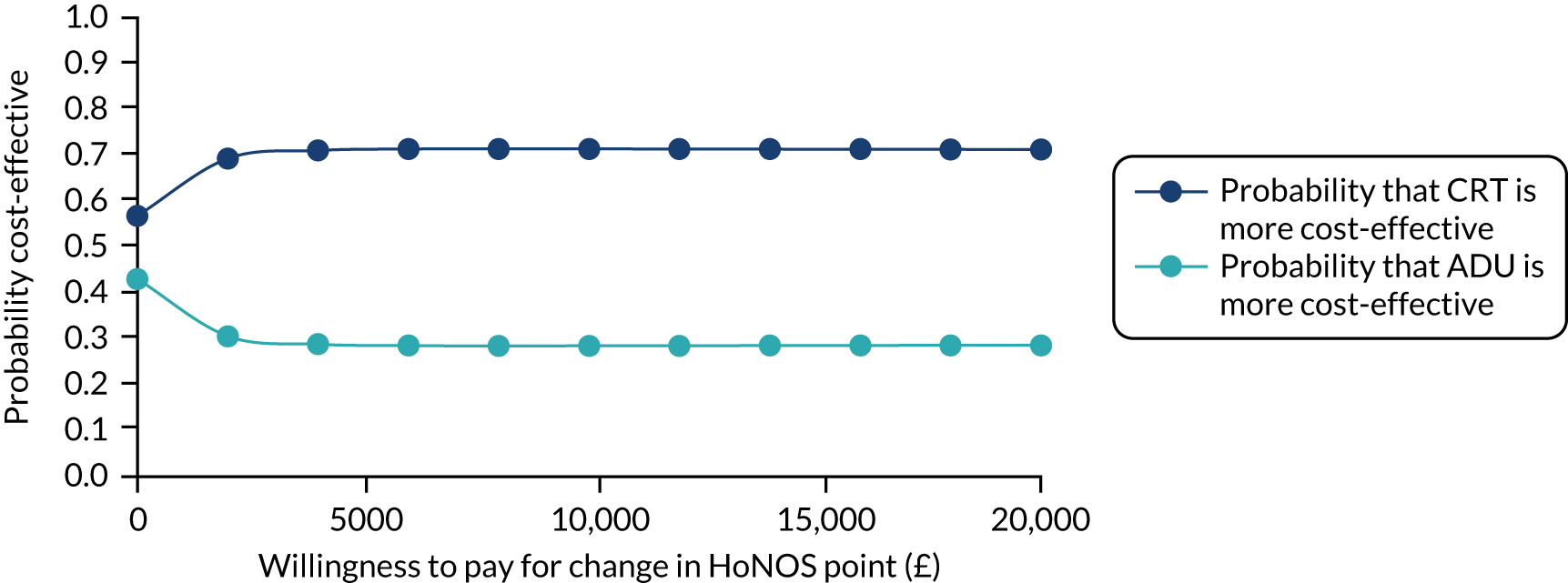
FIGURE 8.
Sensitivity analysis 4: multiple imputation.
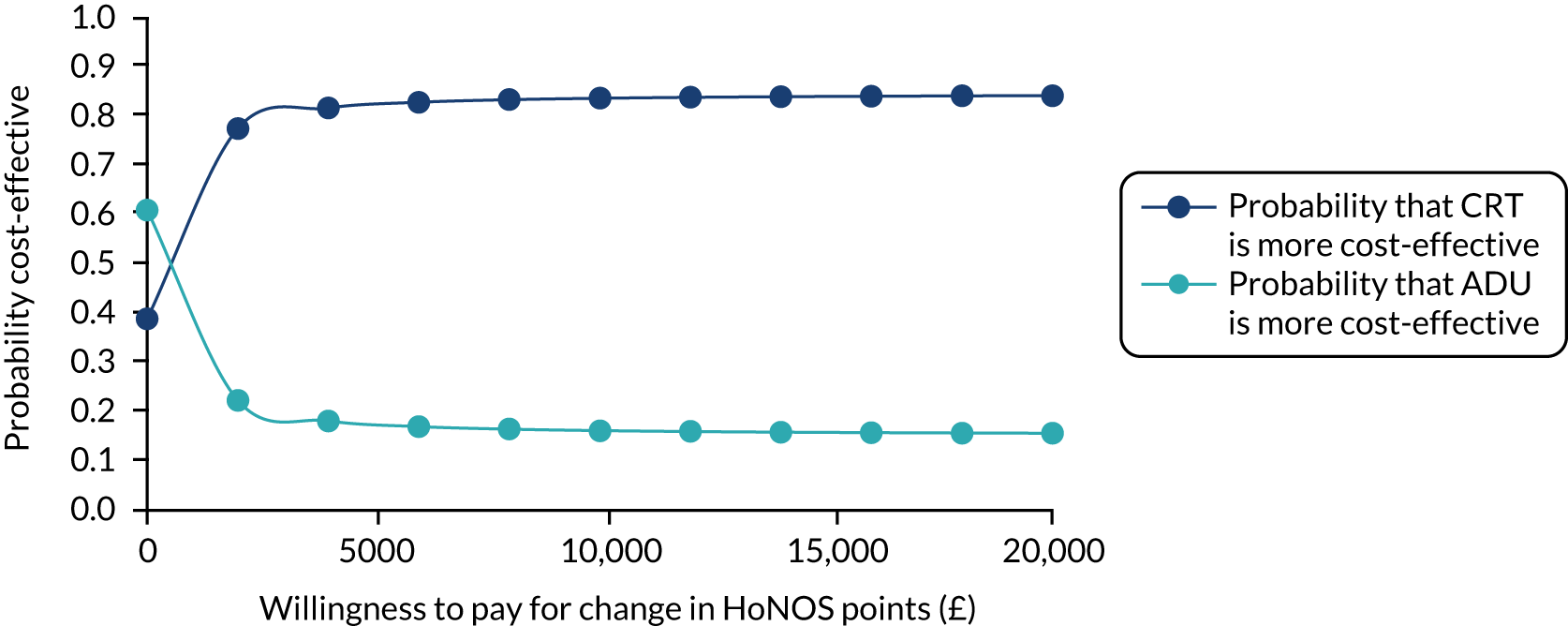
Discussion: health economics analysis
Given the context of scarce resources within mental health care,35 it is necessary to consider the costs and impacts of different models of care. ADUs have been suggested as an alternative type of care to high-cost acute inpatient wards, offering the possibility to both reduce costs and improve mental health outcomes. There is scarce evidence in the literature comparing costs and outcomes of service users with access to ADUs with those of service users who use other models of acute care. In this chapter we have conducted an economic evaluation of the costs and outcomes associated with those in areas with ADUs compared with those in areas without ADUs from an acute mental health care perspective.
In terms of acute mental health care use, there was no evidence that the presence of an ADU diverted people from subsequently using acute mental health wards, with those in the ADU group having slightly more acute mental health ward use. This was reflected when examining acute mental health care in terms of cost, of which acute mental health wards were the largest driver. However, it should be noted that there were notable baseline imbalances between the groups; the ADU group comprised a population who had worse baseline mental health scores and more previous inpatient admissions. After adjusting for baseline imbalances, there was no difference in acute mental health costs between the ADU and CRT groups. These baseline differences are reflected in the unadjusted reporting of baseline and follow-up HoNOS scores. Without adjustment for baseline mental health, the HoNOS score change between the two groups favoured the ADU group. However, once baseline adjustments were considered, this change disappeared, and the CRT group was associated with a greater improvement in mental health from baseline to follow-up.
Despite the limitations of the 6-month HoNOS data, these were used as the outcome in a cost-effectiveness framework. No explicit threshold of cost-per-HoNOS-point cost-effectiveness exists, so the cost-effectiveness results were presented using CEACs to examine the probability of cost-effectiveness at a range of willingness-to-pay values. When costs and outcomes were considered jointly in a cost-effectiveness framework, the cost-effectiveness assessment favoured CRT if HoNOS improvement was positively valued; this was driven by the greater improvement in HoNOS score from baseline in the CRT group than in the ADU group. However, a great deal of uncertainty surrounded the cost-effectiveness assessments, and, even at a high threshold of willingness to pay per HoNOS point decrease, the probability that CRT was more cost-effective than ADU did not surpass 75%. No preference-based measure was included in the study and, therefore, a cost–utility analysis could not be conducted. There was a very small but uncertain cost saving for the ADU group (–£39) in the primary fully adjusted joint analysis. Given this, any improvement in quality-adjusted life-years would lead to favourable cost-effectiveness conclusions for the ADU group. The results of the HoNOS score analysis suggest that this is unlikely to be the case; however, when considered with the significant weaknesses related to the HoNOS data (described below) and the short-term benefits at 8–12 weeks for the ADU group (see Chapter 6, Secondary outcomes), this remains uncertain and cannot be ruled out.
Many of the strengths and weaknesses of the economic evaluation reflect those of the main statistical findings. This evaluation is novel in that, to the authors’ knowledge, it is the first to examine the cost-effectiveness of ADUs compared with other models of care. Users of acute mental health services are a challenging population to engage in research; this study succeeded in including more than 700 service users, who had a diverse set of acute mental health illnesses.
However, this analysis had a number of limitations. The largest of these related to the HoNOS scores used in this analysis. As no other outcome measure was reported at 6 months, we relied on HoNOS scores collected in clinical records for outcome measurement in the cost-effectiveness analysis. HoNOS is collected routinely at points of contact with mental health services, including at the beginning and the end of all episodes of care, and every 6 months for long-term users. The HoNOS scores used at baseline and follow-up were the last recorded scores from service users’ clinical records at those time points; for many at follow-up, a considerable period of time might have passed since this information was last recorded, for example, at their last contact with services. A sensitivity analysis to examine this was conducted that imputed follow-up values that had not changed since baseline, but this did not meaningfully change the results. However, given the favourable results in terms of other outcome measures recorded at 8–12 weeks for the ADU group, this should be a reason to interpret this cost-effectiveness analysis with caution. The second key limitation related to the pragmatic cohort study design to form the two groups being assessed. A risk of such a study design, compared with a randomised controlled trial, is the likelihood of imbalance between the two groups being assessed. This was the case in this study, as the ADU group appeared to experience worse mental health at baseline. We attempted to accommodate for this by adjusting for baseline imbalances through multiple regression. Although a regression framework can help adjust for imbalances, it may be that we are dealing with different types of people in each group and so comparisons of costs and outcomes may be biased. Another limitation relates to the perspective taken for the economic evaluation. Previous research in acute mental health36 has shown that mental health inpatient costs are by far the biggest driver of costs in mental health care. Given this, we focused on the impacts on acute care pathways and acute mental health costs; consequently, there may have been other sources of costs [e.g. general practitioner (GPs) appointments] from both a wider health-care and a societal perspective that differed between the two groups and which were not captured. This analysis considered only a 6-month window, and there may be potential for longer-term impacts that were not captured in this analysis, and longer-term decision modelling could be considered for extending the time horizon. Finally, no preference-based health-related quality-of-life measure was included in the study and so a cost–utility analysis could not be conducted. The preference-based measure may have captured nuances in the strength of preference for given health domains that non-preference measures do not capture.
Chapter 8 Work package 2.2: qualitative study
Parts of this chapter have been reproduced with permission from Morant et al. 39 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
Methods: qualitative study
Design
This used a qualitative study design, involving a series of interviews conducted by a peer researcher with staff and service users of ADUs.
Objectives
-
Explore the views of service users, carers and practitioners regarding the strengths and weaknesses of ADUs and their component interventions.
-
Explore service user, carer and practitioner views concerning the role of ADUs in the acute care pathway.
-
Integrate these findings with those from WP 2.1 to generate theory around how outcomes are achieved.
-
Develop a set of recommendations outlining best practice in this field.
-
Explore the reflections of the study team on ADUs.
Setting
Data were collected from people working in and using ADUs in four NHS mental health trusts in England.
Participants
We aimed to use convenience sampling to collect data from five service users, three carers and three staff members at each study site ADU. We anticipated that the total sample numbers of 20 service users, 12 carers and 12 staff members would enable us to capture a diversity of views within the funding limitations of the study. 37 To ensure that we included people who broadly reflected the range of ADU service users, we aimed to recruit people who varied in terms of age, sex, ethnicity and diagnosis. For the staff sample, we aimed to include a range of professional disciplines to reflect the make-up of ADU staff teams identified in our earlier mapping of ADUs in England. 1
Measures
Semistructured interview schedules were developed for each stakeholder group (staff, carers and service users). These were reviewed and revised by the study’s PPI group (see Report Supplementary Material 23). Some interview questions were broad to allow discussions to be guided by participants’ unique experiences (inviting descriptions of what the interviewee’s experience of the service was like, and how the service helped people); other questions had a more specific focus (particularly concerning comparisons with other acute services, ADU staff and service users, ADU environments, and safety). Scope was allowed for exploring other topics as these arose.
Procedure
Service users were recruited by local researchers as part of our larger study. The eligibility requirements remained the same for WP 2.2 as for WP 2.1 (aged ≥ 18 years; used the ADU for at least 1 week; understood English sufficiently to participate in an interview; had capacity to provide informed consent; and did not pose a high risk to others or to themselves). Interested participants were given a study information sheet and provided with further information during a telephone call with a study researcher. For staff interviews, researchers approached ADU managers to ask about their own participation, and, using a snowballing sampling approach, asked them to identify two more members of staff from the ADU team. For carer recruitment, study researchers asked staff to identify carers from their caseload, and local researchers asked all participants in our larger cohort study if they had family members or friends who might be interested in participating. Written informed consent was provided by all participants.
Interviews took place on site at the relevant ADU. All interviews with service users and carers took place during the period of service users’ treatment, between 11 and 90 days after service users’ first attendance at the unit. All interviews were conducted by two peer researchers (MD and JW) who have lived experience of using acute mental health services as well as experience of qualitative research. The researchers disclosed their peer status to service user participants during the call to explain the study.
Interviews took place between May 2017 and May 2018 in private rooms that the researchers booked at each of the ADU sites. The interviews were audio-recorded and transcribed.
Analysis
Interview data were analysed using thematic analysis38 in NVivo (QSR International, Warrington, UK) software. A primarily inductive approach was adopted, but researchers also sought answers to the initial research questions about the strengths and weaknesses of ADUs and their component interventions, and the role of ADUs in the acute care pathway. Data were analysed primarily by the two peer researchers who collected data, with collaborative input from all other authors. A small subsample of data was initially explored to develop a preliminary coding framework. This was subsequently revised and refined through a cyclical process of reading, coding, reflecting on the data, and collaborative discussion. As part of this, the study’s PPI group met twice during the course of the analysis and provided guidance and input from the perspective of those with lived experience.
Results: qualitative study of service users and staff views in four acute day units
Sample characteristics
Individual interviews were carried out with 21 service users (four at ADU 1, seven at ADU 2, and five at ADU 3 and ADU 4), and 12 staff members (three at each site). We were able to recruit only three carers from sites: one each from ADU 1, ADU 3 and ADU 4. Sample characteristics of service users and carers are shown in Table 24; sample characteristics of staff are shown in Table 25.
| Characteristic | Service users | n (N = 21) | Carers | n (N = 3) |
|---|---|---|---|---|
| Sex | Male | 10 | Male | 0 |
| Female | 1 | Female | 3 | |
| Age group (years) | 16–24 | 4 | 16–24 | 0 |
| 25–34 | 5 | 25–34 | 2 | |
| 35–44 | 3 | 35–44 | 0 | |
| 45–54 | 4 | 45–54 | 0 | |
| 55–64 | 4 | 55–64 | 1 | |
| ≥ 65 | 1 | ≥ 65 | 0 | |
| Mean age (years) | 41 | Mean age (years) | 41 | |
| Ethnicity | White British | 17 | White British | 3 |
| White Irish | 1 | White Irish | 0 | |
| White other | 2 | White other | 0 | |
| Black British | 1 | Black British | 0 | |
| Asian British | 0 | Asian British | 0 | |
| Mixed ethnicity | 0 | Mixed ethnicity | 0 | |
| Other ethnic group | 0 | Other ethnic group | 0 | |
| Days of attendance at point of interview, mean (range) | 30 (11–90) | N/A | N/A | |
| Days of attendance per week, mean (range) | 4 (2–5) | N/A | N/A | |
| Hours of attendance per day, mean (range) | 4.5 (1.5–6) | N/A | N/A | |
| Characteristic | Subgroup | n (N = 12) |
|---|---|---|
| Role | Manager/nurse | 4 |
| Nurse | 2 | |
| Occupational therapist | 3 | |
| Support worker | 3 | |
| Sex | Male | 4 |
| Female | 8 | |
| Age group (years) | 16–24 | 0 |
| 25–34 | 3 | |
| 35–44 | 2 | |
| 45–54 | 4 | |
| 55–64 | 3 | |
| Mean age (years) | 45 | |
| Ethnicity | White British | 9 |
| White Irish | 2 | |
| Asian British | 1 | |
| Years worked in NHS, mean (range) | 14 (3.5–28) | |
| Years at current service, mean (range) | 6.6 (0.25–26) | |
Findings
Eight broad areas were identified as being represented strongly in the data across all stakeholder groups. These were organised into two larger domains related to the two research questions with which this work is concerned: (1) day-to-day functioning of ADUs (covering group therapy, one-to-one support, environment and safety, structure and purpose, and suggested improvements) and (2) the wider picture (covering ADUs in relation to other treatment options, the role of ADUs in the acute care pathway and the wider picture).
Day-to-day functioning of acute day units
The overall picture from these results was highly positive. Staff and service users highly valued the model of care provided by ADUs, highlighting as particular strengths the high levels of contact time and the continuity of staffing, which led to strong therapeutic relationships; the flexible and personalised one-to-one and group-based support, as well as help and signposting for practical issues and peer support between service users; and the provision of structure and purpose as tools for recovery. Suggested improvements were focused largely on expanding existing services in a number of ways, such as having longer treatment times, higher staffing levels and more space; other suggestions included formalising service user and carer involvement, and making changes to the content of the group programmes.
Structure and purpose
The structure and routine of the ADU were frequently cited as things that participants found most helpful: the ‘daily-ness’ of having to get up and be somewhere. In addition, it seemed that the activities and group work helped to provide meaningful activities that had purpose and real benefits, enabling service users to gain some useful skills and not just fill time. As highlighted in the theme of comparison with other services, this meaningful activity was seen as different from other experiences that some participants had had:
. . . so, what it gave me was a structure that I’d been missing for a while. So, routine but also in many ways practical activities that focused on, you know, positive things like recovery and techniques for, you know, dealing with my situation.
ADU 4, service user 5
I think at a fundamental level it’s, sort of, you know, it provides a kind of structure for people’s day. You know, I think the people with, sort of, you know, a lot of mental health problems, you know, benefit from having a routine of structured activity. That’s aside from all the specific kind of things that we do here.
ADU 2, staff 2
For some, this was an important aspect of what the ADU provided for them: a reason to get out of bed and meaningful activities that did not overwhelm them:
So, it’s given me life skills, also it’s given me a purpose, and it’s given me structure, and those one, two, three elements have all contributed to me feeling much better.
Interviewer: Excellent, that’s really good to hear. What aspect of this service would you say has been most helpful for you?
I’d probably say the structure and the activities. The coming here each day, having a purpose that’s not too intense, but is engaging enough to kind of stimulate your mind, and having that routine. Because by being at home, you kind of completely fall out of your routine, and you kind of completely fall out of feeling part of society.
Whereas coming here, you kind of, you know, it’s almost like going to work. You get up, you come in here, you do your activities, you talk, but it’s that routine. And what you’re doing as well, it’s enjoyable, and it’s nourishing for the self, which is important. So, I’d probably say the structure and the purpose.
ADU 2, service user 2
However, one service user experienced the ADU as too busy, with people ‘coming and going all the time’, which may suggest that the benefits of the programme may depend on an individual’s circumstances and how they may be feeling at any one time:
For me it’s too busy because people are, well, coming in and out all the time. I like, sometimes when I’m not well, a bit of, you know, quiet like everyone does.
ADU 4, service user 4
The routine and structure seemed to be part of the recovery process for some; the predictable programme with a combination of helpful groups added value to their experience of attending the ADU:
With the ward, as I said before, there’s not really many groups to help you get back on track, and so you’re just left to your own devices. You can sleep or whatever. If you want to sleep all day, you can. There’s no get-up-and-go motivation. There’s no plan ahead of you. There’s no daily plan for you get up and do.
So at [ADU] it was nice to come in. There’s a plan written up on the board, so you know what you’re doing at what times, and the groups that they run are helpful. They’re useful. They’re not unnecessary, if that makes sense.
ADU 4, service user 2
Group therapy
There was a sense that the group programme was central to the work of all the ADUs. The groups seemed to serve a variety of functions, giving the main structure to the day at the units, with other activities fitted in around them, and offering shape and meaning to the time service users spend there. In most ADUs, the day was made up of free time, during which people had the chance to make individual contact with staff and/or peers; service users were expected to attend formal groups, but could opt in to or out of more informal groups. The daily programme was clearly defined in all ADUs, with local variations in the way that this was timetabled:
Yes, so, we do let them choose if they want to go into that. Because, you know, you can’t show everybody . . . we do like people to go in the morning groups, but if they’ve got a reason not to go in them, we will listen to that and say, well, yes, OK, you know, won’t argue with that.
ADU 3, staff 1
We, I think my previous colleagues mentioned that. We ran at least three groups a day, sometimes four groups a day. So, there’s quite a lot for people to do. And the morning groups tend to be more skills-based. So, things around care planning, anxiety management, recovery, vocational [unclear] groups. The afternoon groups are more fun groups, in terms like creative groups, quiz groups, games groups, interactive groups, which are all designed to get people to talk to each other. And talk to us, of course. So, and we always, and we run relaxation every lunchtime. So, yes, the groups are a really integral part of our service.
ADU 4, staff 2
Overall, the groups seemed to be a valued part of what was offered at the ADUs, especially when compared with the experience of being on a ward:
It’s helped me with joining groups as well. Groups, because I’m not really . . . I don’t really get involved too much with other people. I do know a lot of people and I do get involved, but I don’t get too involved – so it’s good that we do things in groups here.
And it’s nothing to be afraid of. And it’s good.
ADU 1, service user 3
Well it’s helped me tremendously. Like I mentioned earlier; sharing with the other service users. The groups are fantastic. It gives you something to focus on on your day.
ADU 4, service user 1
And it actually helps you, but on the ward they’ll do, like, colouring or maybe, like, making something crafty, where here it’s actually helping you, like, with your recovery. I find that they’re giving you, like, recovery sessions and care planning and anxiety management and things like that, and relaxation. And I think it’s all helpful.
ADU 4, service user 2
However, some service users found attending groups a struggle, and for a minority the group aspect was experienced as a negative part of attending the ADU. One person explained how it was only in retrospect that they could see the benefit of attending the groups:
The groups, I didn’t find particularly . . . Like, they made me come out and do something – which was a positive, in retrospect. I didn’t find them particularly helpful at the time, though looking back I do. And once I was in a better place with the meds, I started appreciating the activity and the occupation of the mind.
ADU 2, service user 6
Some service users found the groups too difficult to manage:
For me, it’s been actually very difficult using the service because actually mixing with other service users I find really difficult. So to do groups has been a real challenge, [unclear] done four groups in under 10 days.
ADU 4, service user 4
There was no standardised programme of groups across the ADUs; instead, the groups seemed to be designed around the needs of the service users and the skill set of those in the staff team, and appeared to offer flexibility within a basic framework. Service users appreciated this flexibility:
We have depression on a weekly basis, we have anxiety on a weekly basis, and then during the group discussions the tutors will listen to any other concerns we’ve got. That might not relate to anxiety or depression, but they’re always there as a listener to any other concerns we have as well, which is, which I find is good, because we’re not sticking to an agenda.
And most mental health people can’t stick to an agenda anyway. You wonder sometimes if that’s part of the illness, and you have to accommodate that sometimes, haven’t you?
ADU 3, service user 2
Well, I think it’s, because there are, there’s such a variety of different groups, I think, well hopefully we can tap into something that would be an interest to somebody. And then on every Friday we do a weekly community meeting and we would ask people is there anything you want to do. And they might just say, oh yes, I really fancy doing, I don’t know . . . Pottery or whatever, I just phone up. So we will consider oh right, how do we manage, yes.
ADU 4, staff 3
The main themes of the groups could be roughly categorised into the three areas of practical (life skills, e.g. cooking), psycho-educational/therapeutic and creative, although, arguably, all of the groups by their nature could be seen as therapeutic, with peer support a predominant feature:
Well, especially talking to people in groups. We can go to, like, a [unclear] I mentioned earlier on, or psychology, and we can all just get in there, and we can just talk about different things, different aspects basically of our own mental health . . .
ADU 2, service user 4
Practical groups could include life skills groups (e.g. cooking and gardening), but they also included care planning groups and ‘moving on’ groups, which some services users seemed to experience as enabling:
I’ve enjoyed the cooking on a Friday morning with staff. Because I’d lost all my confidence in cooking. So like I’ve learnt a few different things. I’d never made a lasagne until last week, so I was quite chuffed about that; made a cheese sauce from scratch . . .
ADU 3, service user 1
Yes, I like the groups that they run. I like the individual sessions you can have with staff. I like the help that they do, like cooking. They have people come from the outside, like a gardener, coming in and help you. They’re, like, fun things I do [?] like gardening. Things that you do at home, like daily living things. They just help you get back on track with that.
ADU 4, service user 2
Definitely the groups, the morning groups. They start at 11 because they’re the main ones. Like, as I’ve said so many times, the anxiety management and relapse prevention, well-being, care planning, all of those sort of groups I find really helpful for my recovery.
Like, it helped me, like, be involved in my care plan. So instead of someone writing the care plan for you, you’re involved in what goals you actually want to achieve, and you sit down with someone and you do it with them. Instead of them just giving you a care plan and saying, ‘Get on with it, there’s your goals’, you actually get to be involved.
ADU 4, service user 2
Psycho-educational groups were often cited as the most valuable, giving service users an opportunity to learn more about common mental health problems such as anxiety and depression. An important aspect for many was developing new coping strategies for managing their difficulties, something service users seemed to appreciate. These groups ventured into more specific therapeutic spaces to varying degrees. For example, at ADU 2 there was a commitment to providing psychodynamic groups as well as more skills-based groups:
Yes, I’ve found the big long sequence anxiety management [?] so that’s been very good. I really enjoy the mindfulness, I’ve been doing some mindful meditation and I have some one to one in a small group as well as larger group activities. So, that’s something a very flexible way of working and encouragement to continue this at home.
ADU 4, service user 5
Also, the groups that they’ve been also putting on, which I touched on, like the sleep deprivation, depression, anxiety, mindfulness, they just sort of teach you different little skills that you can put in. I’ve done the Moving Forward group, which was 2 weeks, where we look at the REP [?] plan.
ADU 3, service user 1
Most of the sites in the study had some groups that provided a space for exploring creativity. The groups offered were based around the skills of those in the staff team. For example, at ADU 3, a staff member had a particular skill for creating bonsai trees out of low-cost recycled materials. The process of service users creating these became therapeutic, as it offered an opportunity for service users to talk to staff and build connections with other service users, and everyone was really proud of the work they had created:
We do different artwork, which someone will show you later. And you can assess so many skills. We make bonsai trees, and there’s so much you can assess from a person making this bonsai tree, all the way through the process, and you can actually see them getting better. Because, when they see what they are going to make, they’ll say, I can’t do that. But when you see them through the weeks, it’s amazing, and they get a lot more confident.
ADU 3, staff 1
Yes because well, they’re all therapeutic, music, arts, yoga because I have a physical health problem as well, so yoga and some . . . They have dance and they just help you concentrate on something else instead of your mind turning around on your problems. And the auricular acupuncture relaxes me.
ADU 2, service user 2
This reflects the flexibility and often innovative culture in the ADUs; service users were able to develop new skills and try new things or even reconnect with past hobbies and interests, and staff were able to use their individual skills and interests to contribute to the programme of groups:
So, we’ve kind of brought in a dance movement therapy, one of the nurses Amin is running right now, so he’s self-trained, so he’s maintained that kind of energy. So, you know, we wouldn’t have had those, sort of groups, running say 10 years ago.
ADU 2, staff 1
It may not be everything on the timetable that’s meaningful for them, but there could be something new for them to explore or something that they can revisit.
ADU 2, staff 3
I think starting I expected it to be more talking therapies, and I was surprised at how beneficial the creative activities are in just helping you to engage in the moment and helping you find your own interests again. So it’s moved me a lot away from the feeling of depression and found the things that I really enjoy doing and enjoying music and expressing myself more. And people have said that I’m not the same person. I’m a more creative person, and it’s kind of encouraged that process with me, which is very healing.
ADU 2, service user 3
And what aspects of the service have been most helpful for you, do you think?
I’d say just sitting in the groups and just talking to the other clients, really.
ADU 3, service user 3
The groups offered service users the opportunity to reconnect with previous skills and interests or to learn new things. The following quotation illustrates the power of reconnecting with pleasurable activities:
So, for example, I used to dance quite a lot. I haven’t danced in a long time, but when I came here I did dance therapy and I started dancing again, and obviously that’s beautiful to start dancing again, and I remembered I loved it. And then, like now, in the mornings, when I wake up, I put on some music and I try and dance, and that relaxes me.
ADU 2, service user 2
The groups also seemed to offer a safe place to start reconnecting with other people in a meaningful way. Arguably, all of the groups provided a therapeutic space by nature of their composition and the dynamics this afforded, being made up of skilled staff facilitators and service users with a variety of demographic characteristics and life experience. The range of groups offered at all the ADUs was something that most service users valued:
Yes, that’s been good. I’ve been offered Pilates, it’s on today and it’s lovely. I’ve never done Pilates before and it’s really gentle and it’s not very advanced. But it’s a . . . I think it’s a lovely offering that they give, so, yes. And, yes, the other stuff on motivation, planning and, you know, goal-setting have also been good to work on stuff that I . . . not been there and I’d been avoiding. So, it got me to bring my focus back onto the, you know, pathways to recovery and solutions, so.
ADU 4, service user 5
One-to-one support
Central to the work of the ADU is the programme of therapeutic groups described in the preceding sections, but, in addition, the one-to-one work threads throughout the whole programme were a vital and highly valued element:
They’re just always there. If they see you’re on a bit of a low day or a little bit anxious . . . or need someone to talk to, they’ll take you into this quiet room, have a chat . . . they’re always there to have a chat with you if you need to.
I did have a couple of tearful days last week and [staff name] was there for me.
ADU 4, service user 2
All of the units in the study provided a named key worker. Other scaffolding for enabling one-to-one care included, at one ADU, providing out-of-hours telephone support, and at another providing a ‘one-stop-shop’ session each morning for service users to ask for individualised guidance and support.
Support often focused on, for example, mental health problems and symptom management, but also, importantly, practical issues (in the form of signposting, but also direct help from ADU staff).
One-to-one support was also provided on a more ad hoc basis, and this was particularly valued by service users; a combination of formalised key working and ad hoc individual support seems to be optimal.
Another key and valued factor in providing effective support was being flexible, individualised and responsive:
[Your key worker] will do a support plan with you – not as soon as you get here, but when it’s a convenient time; she asked me when is a convenient time for me to do that support plan. It’s like, you being here, I felt comfortable coming here to talk to you today, because I feel like I can talk to you today. If you came to my home, I wouldn’t be able to talk to you, because I’m not in the same mode as I am now. I would be so depressed at home, but I come out of that mode once I get here . . .
Because the environment’s more adaptable to me here. And that’s what the staff do here, they only do things with your permission, or consult with you first. It’s absolutely brilliant.
ADU 3, service user 2
Staff identified that having relatively small caseloads was essential to their ability to provide this kind of support:
And, I think it’s good here that, because of our caseloads being quite small compared with other services, we actually have the time to listen to people and support.
ADU 2, staff 2
In addition to the support provided by staff, peer support is an integral part of the ADU model.
All study ADUs provided a key worker, who was primarily responsible for a service user’s care during their stay, and with whom the service user would meet on a weekly basis.
Key working relationships are especially valued when a meaningful personal connection is established between service user and staff member, and a good rapport is established:
In particular, my key worker, [name], she was just amazing. The first time I came here, she was like, right, we’ll have a little chat. We just had such a laugh, we got on so well, and it was really good.
Because I don’t really get that with a lot of people. It’s difficult for me to get on with people. So when I met [name] it was like, yeah, she’s amazing.
ADU 1, service user 1
Conversely, one service user suggested that key working was less useful when it was restricted to formalised weekly appointments, which felt medicalised and lacking in personal connection:
Like, the staff are really nice, but sometimes it feels like . . . You know, when you go and see a GP and you have a conversation with your GP, and they just sit and they type, and they don’t look at you or make any eye contact, and it’s, like, they’re just typing away. Sometimes I do feel like . . . Like, in a one-to-one, it’s, like, do you really need to be typing down everything I say? Can’t you just look at me, and can’t we just talk, and can’t you do notes afterwards? Like, I find that really difficult.
ADU 2, service user 5
However, the same interviewee acknowledged the value of key working in principle as a way to have one member of staff as a single main point of contact:
. . . it’s helpful to have the same person and for that person to be your point of contact. Once when I was upset in the group, they told my one-to-one person. So that kind of thing is helpful, but I think it would just be more helpful to actually, like, have a conversation and be listened to instead of the, kind of, really medical approach.
ADU 2, service user 5
This was also mentioned as being useful from a staff perspective:
I wouldn’t say that I know all 10 people here really well. But that’s why we key-work. So, everyone’s got key workers . . . and if you want to know how the client is doing you can ask their key worker and usually they’ve got reams of information. So, that’s good.
ADU 1, staff 2
As well as the more formalised forms of one-to-one support available, particular value was placed on the importance of flexible, ad hoc support. Service users felt that it was useful to be able to seek one-on-one support whenever they needed it; staff considered it a privilege to be sufficiently resourced to be able to provide it.
Ad hoc support was described as useful for service users both as a means of seeking additional care when needed and as a way of removing oneself temporarily from the group environment:
And having someone to talk to. Like, if you’re struggling, you don’t actually have to sit with everyone in the lounge. They’ll say, ‘Do you want to go to a quiet room?’ and, ‘Do you want a member of staff to come sit and talk to you?’ I find that very helpful because, if you’re having a bit of a bad day, you don’t really want to be around other people, sort of thing. You just want to go to one side and speak to a member of staff or just sit on your own for a little while, and they facilitate that.
ADU 4, service user 2
The impetus for this can come from staff as well as from service users, and this is facilitated by staff members’ ability to better identify service users’ needs as a result of key working and greater general contact time:
But I think we manage patients well, and we get to know them so well that you can see if someone’s having a day where they’re not quite themselves. And we can say to them actually are you OK today, you know do you need to chat.
ADU 3, staff 3
There was one day in particular where I wasn’t feeling myself and had . . . my mood had dipped. And, the staff had noticed this and had a private chat with me about what I was going through at that time. And I was just really appreciative that, A, that they had noticed it, but also they were here to notice it. And that I had that support and we were able to just kind of tailor things for where I was at that time, and just help me further with my recovery.
ADU 4, service user 3
Ad hoc support was also provided out of hours over the telephone at one of the study ADUs, and this was seen as particularly valuable. Another offered a ‘one-stop-shop’ session every morning, to which service users could bring whatever current issues they had to members of staff.
As well as the therapeutic, empathetic support centred on symptom management described above, support with practical problems was emphasised by staff and service users at all study ADUs. Several members of staff acknowledged the likelihood that service users would experience practical problems (e.g. related to housing, benefits, legal issues) and the importance of addressing these as well as symptoms:
Yes, because if someone’s most anxious about something, you can try and work on a sleep diary or rhythm, you can try and do and set goals, but actually they’re very anxious and can’t work because of something else that’s happening, either at their home or they’re homeless or whatever it is, you’re going to try and help as much as possible, or signpost on, which can involve a lot of letter writing and things. You’re going to do that so that you can then work . . .
ADU 2, staff 3
Help with practical problems was often provided in the form of signposting tailored to the individual’s needs and interests. Signposting is an important part of all mental health services, particularly those such as ADUs that operate on a relatively short-term basis and need to facilitate continuity of support:
They also have guided me towards other services – [XXXX] for coping with alcoholism because I was on the bottle when I was depressed.
They’ve pointed me towards ways that I can get myself back into structured study. Like, starting with maybe the [college] or things like that. Small steps I can take, so I can get back to meaningful life.
ADU 2, service user 6
Perhaps if someone likes yoga, we can then know about the exercise and prescription in the community that there’s 12 weeks free if you’re unemployed. And that’s for physical health and mental health.
So we try . . . So each session has its own importance and also relevance towards signposting in the community because if someone enjoys it, why stop? Why not carry on? And so I do try and source as much low-cost or free things that reflect timetable in the community.
So if someone enjoys my pottery session, then I know . . . And if they’re unemployed I know then it’s free and it’s at [college], it’s in their area. And so it’s nice to be able to [unclear] when they say I really enjoy the session, it’s nice to be able to say, well actually this is . . . You can actually access it for free. And that’s a really nice feeling when people then come up and say look I’ve signed on for it, as they will do, and it can all help towards the discharge planning.
ADU 2, staff 3
This type of signposting helped people build links in their local community that were unrelated to formal mental health services, which may help prevent social isolation in the future:
One lady has been with us for about 4 weeks and she really enjoyed knitting on the unit. So, we said oh, why don’t you do a knitting group in the community? And she’s quite isolated – quite socially isolated. So, we were able to find three different knitting/crochet groups that she could do within [the area].
ADU 1, staff 2
In addition to conventional signposting work, at all of the ADU study sites there was evidence of staff really going above and beyond in terms of practical support, and offering their own help ‘in-house’ rather than referring on to social services, and so on, and service users valued this very highly:
[I had an] employment tribunal preliminary hearing . . . He said he could come along with me, which is absolutely brilliant. It was, like, just a couple of hours meeting with our preliminary with the judge and the respondents and the like. And so my key worker came along with me, which is absolutely a massive help, big time, because I felt reassured and, yes, to have somebody there . . . and he obviously knew what I was going through, and so it was really helpful. And even the judge commended it and said, thank you for being there, yes.
ADU 2, service user 4
They come in and just we’ll go 110%, whatever. Because I think on the wards, sometimes, it’s just like, well you need to talk to your care co-ordinator if it’s about benefits. Or you need to talk to someone if it’s about housing. We’re like, we’ll do it. What do you want us to do? We’ll bring you to the council, we’ll bring you to the benefits office, we’ll sit for 2 hours and do your paper application. There are no, this is us and that’s them.
ADU 4, staff 1
Only one ADU in the study, ADU 1, had formalised peer support worker roles: two volunteers attended the unit twice per week. Staff at the unit valued the perspective that the volunteers brought, and said that this work was beneficial to the peer support workers themselves as well as to ADU service users:
I think it gets to show that actually they can . . . people can recover, and then they can give back to the services, or give back to mental health as a whole, really. And show that people do become well and are able to function properly.
And also, I think it grounds the peer support workers to kind of realise that actually, you know, we need to make sure that they take care of their mental health and make sure that they don’t, sort of, relapse themselves or get themselves in a position where they’re more vulnerable.
And I think that . . . and it shows how far they’ve come in themselves from where maybe they were before. So I think they’re invaluable.
ADU 1, staff 3
At ADU 4, a former user of the service was employed there as a support worker; ADU 2 and ADU 3 did not employ peer support workers in any capacity. At all units, however, service users and staff emphasised the importance of informal peer support between service users as an aid to recovery:
So, at home I tend to sort of burrow into myself and ruminate, whereas here you get to do the classes, but you also get to speak to the other patients, and that itself is quite therapeutic, just talking and just sharing experiences.
Whereas here, you can be like, how are you? And someone will say, you know what, it was terrible. And you can just have that authentic conversation. And then doing so, they might say something, and you might say something, and you learn from each other. And you might pick up information about other places, or services, or stuff, just because you’re talking authentically.
ADU 2, service user 2
Peer support took place in a structured way during groups, but also during the ‘downtime’ between these, which staff pointed to as one of the reasons for having periods of the day without scheduled activities.
Three of the four ADU sites in the study (ADU 1, ADU 2 and ADU 3) provided clozapine titration in conjunction with the rest of the programme of treatments. Two sites (ADU 2 and ADU 3) had 1 day per week for clozapine titration sessions, which were separate from their usual remit and were for service users who did not otherwise attend the ADU. This was seen as in some ways as a hindrance; some service users perceived the influx of ‘outsiders’ as intimidating:
Like, the day I came here was when they had the clozapine clinical, and so when I walked in it was really busy in the waiting area, and people were really unwell, and I felt really, like, intimidated because it’s basically men as well, and I was, like, quite scared to come here because of that.
ADU 2, service user 5
Staff, on the other hand, perceived it as a logistical problem with regard to staffing and safety:
We have a clinic day every Tuesday for that . . . and we average about 150 a month of people coming through. So . . . on that, we have to have three members of staff on a Tuesday. And we’ve hardly got any. So Tuesday here is desperate.
ADU 3, staff 1
By contrast, however, ADU 1 did not run a separate outpatient clinic for clozapine; instead, clozapine titration was within the scope of the unit. Being able to provide clozapine restarts for people who had come off the medication was an important part of the team’s goal of preventing admissions to hospital, and service users who were being titrated back on to clozapine would also attend the full ADU programme. This was highlighted as a success of the unit by two of the three staff members interviewed:
We’ve got clozapine, we’ve got a clinic, we’ve got a nurse prescriber, we’ve got a consultant. So, we’ve been able to do three clozapine restarts here – so that’s been really good. Because if somebody needs to take that medication and they’ve been on that for a long time, being off it for weeks while you’re waiting for a hospital bed and then having to go into hospital while you don’t really want to – just because you’ve missed a medication dose – it’s just . . . So, that’s been really good.
ADU 1, staff 2
Environment and safety
Safety and environment seemed to mean different things to our interviewees, and we received a wide range of responses. There were also some differences in the way in which safety was spoken about. Service users spoke more about the ‘feel’ of the physical environment and relational dynamics, while staff from an acute care background focused more on ‘risk’ in terms of the potential for service users to harm themselves (e.g. being ligature free). Quite often when interviewees were asked about environment, issues of safety would come to the fore, and there did seem to be an interaction between the two:
. . . you’d have people coming from an inpatient perspective and wanted to spend a lot of money making it all ligature free. Then you had people coming from a community perspective where, you know, we met people in their homes – their homes aren’t ligature free. And we’re going there’s trees outside – they’re not ligature free. People are going home at night . . . so I think your threshold does go up a little bit . . .
ADU 1, staff 2
You know you don’t really have people rushing around and kind of creating anxiety, it’s very much the opposite of that. And just very welcoming.
ADU 4, service use 3
Important themes about safety were the security measures that were embedded in the ADU; for example, everyone who came into the ADU had to sign in, and the entrance doors used a fob system, so reception acted as a gateway. This was frequently mentioned as helping service users to ‘feel’ safe, but what was also often cited as contributing to the feeling of safety was the absence of ‘security wardens’ and the freedom for service users to come and go as they wanted. This was seen as very different from the wards and something that was appreciated by those attending the ADU. Staff also spoke about the fact that ADUs had a voluntary ethos, which contributed to safety and the lack of aggressive or violent incidents:
. . . on the ward, because they’re locked up against their will, they’re under section against their will and on medication against their will – so they’re fighting against it. Whereas, I think the voluntary aspect here and the fact that people ask us to go out – we never say no, we always let people out. It might be that they go out with somebody if we’re really concerned, or if we’re giving them a time frame to be back by, but at least it’s voluntary.
. . . I think it’s supportive staff. I think it’s the ability to have an open environment, and a warm and welcoming environment, where people can flourish therapeutically, and not have as much boundaries as they would do on the ward. I think that, in a sense, creates more safety, because they’re still in the community, but they just feel more supported, especially when they’re feel quite vulnerable in their mental health.
ADU 1, staff 2
The availability of staff was often mentioned and, combined with them being trusted to understand and deal with conflict, was seen as an important contributor to ‘feeling safe’. Greater staff retention, along with a predictable programme rather than shifts, as would be the case on a ward, was seen as helpful. One carer described the importance of continuity of care. Knowing who would be there and what would happen at the ADU appeared to contribute to service users experiencing the dynamics in the ADU as safe:
Some people are going to go off on one [?], but staff are pretty quick to respond and to kind of know how to, you know, what to say and to do. And I feel that they know what to do and say as a patient or a service user if someone else is kicking off. But it rarely happens, but I trust the staff that it will be dealt with and respecting the rest of the people but not taking away the dignity of the person who’s kicked off either. I always felt safe, and I still feel safe now.
ADU 2, service user 1
If we’ve noticed that people are clashing a bit, we will deliberately attach them to different groups. We’ll sometimes just be mindful of strong personality clashes. But generally, everyone’s getting on quite well. And because there’s not been any violence or aggression . . .
ADU 1, staff 2
But also there with the crisis team you don’t know who you’re going to see. She makes . . . This was the problem with the crisis team. She makes a connection with one person, and then on the following week it’s somebody completely different, and it’s having to discuss it all over again.
But here, she walks in the door, they know . . . She sees the same faces every day, and that’s the best thing for her, because she was struggling with seeing different people.
ADU 3, carer 1
What some service users found less conducive to feeling safe was service users from other services coming into the unit. For example, service users from another service joined ADU 2 at lunchtime and were able to join groups. This was experienced as unsettling and also created an issue around increasing the numbers in group activities. One person explained that they could not always access a group because there was no space left, which was a unique experience and not something that service users at other ADUs mentioned:
And there was a massive row. A member of staff came in, and I’m, like . . . Yes, so I did actually mention it in the business meeting. I said, you know, that there is some frictions that I’ve noticed. I said, like one of the groups that I personally wanted to attend, they were sat here a quarter of an hour before it started. You know, I wouldn’t think to be quarter of an hour early. I was 3 or 4 minutes early.
And you weren’t able to attend because they were full up?
And then . . . Yes, because there were eight people allocated, you know, and there’s six people over there, and they all were here. So [ADU 2] didn’t get [unclear], and I’m, like, there seems to be a bit of a them-and-us situation going on here. So now I know that [ADU 2] was, like, the 6-week thing, I just thought it was, you know, just [ADU 2] clients, you know, and all of a sudden you’ve got these . . . you know. And I’m not saying these people don’t need their own thing to be getting on with . . . Yes, it’s a bit strange.
ADU 2, service user 1
Staff saw it as important that service users were able to take responsibility for their own safety, in terms of self-harm, and service users appreciated staff being available and checking in with them on particularly bad days as a way of supporting them with this:
I think the availability of staff to talk to, being treated as an adult, being asked to take ownership of your own well-being, acknowledging we’re not scared of having those really risky conversations.
ADU 4, staff 1
What makes me feel safe? I think it’s the fact that the staff are open and approachable and understanding. It helps create a reassuring environment. And they can be quite blunt at times but, you know, it’s things that need to be said at times and they need to assess how you are and if you’re a danger to yourself or others, so.
ADU 4, service user 3
This sense of safety extended beyond the start and finish times, and, for some, beyond the walls of the ADU. Transport was often cited as a factor in safety; those who had real difficulty going out on their own appreciated this being provided. The following quotation shows how service-provided transport seemed to protect the interviewee from experiencing negative stigma:
And also, there’s transport laid on if it’s required, so that really makes you even safer, because you don’t have to go on the bus if you don’t want to, you don’t have to confront people when you’re feeling unwell.
Which are things that can make people a bit upset.
So, you don’t put yourself on show when you’re unwell sometimes, which can be a trigger for some other people, because I’ve had times with people saying, what are you staring at? So, having the transport laid on for those people who need it, that’s fine.
ADU 3, service user 2
Suggested improvements
Overall, the picture that emerged from these interviews was that respondents were generally highly positive about ADUs and their experience of working in or using them. The interview schedule specifically asked about improvements that respondents would like to see made to the service, and responses to this question were consistent with this generally positive view.
Five service user respondents could not think of any improvements they would like to make, and the majority of the improvements that were suggested were not radical. These could broadly be categorised as requesting ‘more of the same’ across a number of different domains: longer treatment times, larger numbers of groups and staff, and more physical space.
Other suggested changes that came up less frequently but were more substantive were altering the content of the programmes of groups, and instituting better formalised service user and carer involvement.
Finally, some service users found that ADU treatment was just not for them, and staff also had some opinions about who might not benefit from ADU care.
By far the most frequently mentioned suggested change (29 references across 12 out of 33 interviewees), from both service users and staff members, was lengthening the maximum length of time for which service users could use the ADU (at all study sites, the maximum was between 6 and 8 weeks).
In a minority of these cases, service users who had used day hospitals in the past, when such upper time limits did not exist, or staff members who had worked in these expressed a preference for the previous model:
Yes, that’s my thoughts on, well, you know, them taking away funding to the extent that this is 6 weeks, and I should feel grateful that it’s still open. Yes, I’d be devastated if it completely closed, but, to be frank, it needs to be open longer and have more staff here. That’s how I feel after 3 weeks, and if I feel like that after 3 weeks, God knows what I’ll be saying after another 3 weeks’ time.
ADU 2, service user 1
Most respondents advocated a slightly longer period of time – an extension of 2–4 weeks – on the grounds that it can take a while for people to be ‘weaned’ on and off medication, or to adjust in other ways to being able to benefit from the treatment:
I think it could take at least 4 weeks to settle in and to get used to the routine and the structure. And once you get settled then it’s time to go. So it’s like, at the point it starts to become helpful is the point where you’ve only got a few weeks left, and you’re being discharged.
ADU 2, service user 5
Sometimes I feel a bit frustrated by the length of stay that perhaps that people have here, you know, because it used to be 12 weeks but then it got cut to 8 weeks . . . For some people that’s enough but others, you’re looking at the 6 weeks, into the sixth week and you’re only really just reaching them, and they’re only just then beginning to come out of their shell, so to speak and figure out . . . So I understand that there has to be a limited time but I always thought the 12-week worked better than the 8.
ADU 3, staff 2
Suggestions for improvements to groups from both staff and service users were generally concerned with increasing either the quantity or the type of groups available. Service users at some study sites commented that they felt there were not enough groups to fill the day, or that there was not enough to do while they were not in a group:
I think it’s just the waiting times between the groups, where you’re just kind of left in the community area and you just sit and think because there’s nothing else to do. It’s not like they get games out for us to do, or anything like that. I’d say that’s the only issue, that there is quite a lot of waiting for groups. I think there needs to be a bit more structure in those waiting times.
ADU 3, service user 1
Staff respondents, however, did emphasise the importance of leaving some periods of the day unstructured, with the aim of fostering peer support and friendships between service users, and to give staff opportunities to provide one-on-one support where needed (both of these topics are discussed elsewhere in this chapter).
The type of groups emphasised varied between the sites involved in the study. Some sites opted for a programme mostly based around art, drama and music-based occupational therapy; others emphasised more psycho-educational or psychological groups; and yet others provided more activity-based groups that were not overtly therapeutic in nature.
As different types of groups appeal to different service users and staff, naturally a lot of suggestions for improvements were based around changing the balance of the groups provided by the ADU:
I guess, you know, some more practical activities, maybe some music and I am not musical but, maybe sometimes doing something even simple like the bongos, hitting some bongos or something might be quite good. A few people had mentioned that before and, you know, some musical thing would be, might be a nice thing to add.
ADU 4, service user 5
And I think there’s a need for more talking therapy groups and if anything, probably back in the day there was more of the talking therapies than there is now. So, I think that’s an area that I think would be, you know, identified as patients are asking more of, yes.
ADU 2, staff 1
When compared with other acute services, on paper the ratio of staff to service users in ADUs is relatively high; however, because the level of intervention offered is higher, and places a greater demand on staff time, at all of the study ADUs understaffing was raised repeatedly as an issue. This was represented in the data very strongly, particularly from staff interviews (8 out of 12 staff interviewed raised staffing levels as a problem):
Challenging. Again, staff, I would say. It’s certainly not the clients, you know? Staffing’s a massive issue. Yes, because I feel we could, we could develop a lot . . . not develop a lot more, but offer a lot more if we had, if we had the correct amount of staffing.
ADU 3, staff 1
Service users also recognised staff numbers as an ongoing issue that had a direct and obvious impact on the care that they received:
Well, I’ve noticed this week, for example, we’ve got someone on annual leave from last week. So that’s one staff down, and we’ve got someone who’s sick for this whole week, and they’re involved in two or three groups. So in the business meeting on Monday, it was, like, yes, these groups are not happening, but we’re having to improvise.
ADU 2, service user 1
Staff also cited lack of physical space as an issue. Staff felt that to work effectively they needed large rooms for group work as well as numerous smaller rooms for one-to-one work; at all sites, the group room space was not an issue, but there was a feeling that not enough small rooms were available.
Provisions for both service user and carer involvement varied between the ADUs involved in the study, but overall they were relatively limited. One site had regular carers’ groups, which were sparsely attended, and would meet separately with carers to provide support for them:
Everyone’s been very welcoming. I kind of feel there’s a really good support for him, but also for me, and the fact that I’ve been allowed in to meeting with the doctors, and they’re taking the time . . . But they’ve actually just spoken to me, so [service user’s name]’s gone out of the room.
ADU 4, carer 1
The other study sites, however, had no formalised carer involvement beyond allowing carers to sit in meetings with clinicians when requested, or signposting carers to external sources of support.
Reasons for the small number of carer interviews undertaken, and the possible explanations for limited carer engagement in general, will be explored in Discussion: qualitative study.
In one study, ADU peer support workers volunteered on a regular basis, whereas another had a former service user working as a support worker and the others had no formalised service user involvement.
At ADU 1, where the peer support volunteers worked, the other staff gave very positive feedback about the value of peer support:
. . . they come in and support the service users and they get something from it and so do the service users. And they seem to be really liking it, really . . . I think it goes to show that . . . people can recover, and then they can give back to the services, or give back to mental health as a whole, really. And show that people do become well and are able to function properly.
And also, I think it grounds the peer support workers to kind of realise that actually, you know, we need to make sure that they take care of their mental health and make sure that they don’t, sort of, relapse themselves or get themselves in a position where they’re more vulnerable . . . and it shows how far they’ve come in themselves from where maybe they were before. So I think they’re invaluable.
ADU 1, staff 3
A few service user respondents mentioned the need for better service user involvement:
So, we need more service users to get involved, and go to committee meetings, and meet with other guest speakers, and learn how to talk at meetings, and learn how to express yourself, and then you get more confidence. That is the thing, is when you’ve got mental illness sometimes you lose your confidence, and you need to build that back up again, and the only way you’ve got to do it is through service user involvement.
ADU 3, service user 2
Staff in all ADUs enumerated reasons why service users might not be suitable to attend the ADU. Most of these reasons were to be expected as exclusion criteria because of the nature of the service provided by an ADU (history of violence, risk to self, substance abuse, etc.).
One staff member recommended that ADUs be voluntary only, as the service did not work well for sectioned service users who were coerced into attending:
I don’t like people coming here on section who don’t want to be here. It ain’t going to work. Basically, we like people to . . . if they’re on section and they’re happy to come here, then I’m happy for them to be here. If they’re on section and they don’t want to be here, it’s just not going to work . . . You’re going to get people, they’re told, oh, well, why don’t you come to the acute day treatment unit? It’s a means for you to get off your section. It’s not necessarily going to work.
ADU 4, staff 2
Three staff members suggested that the service should consider whether or not it risks creating dependency in some service users:
If you’re somebody who is really struggling emotionally but also quite isolated, then actually if people only come here every day for 4 weeks and then they want to come, and they don’t want to leave. We don’t want to set people up to become dependent on something and then take it away because it might create more attachment difficulties.
So, I think we have to be really clear for everybody that comes here that, obviously, this is a short-term option.
ADU 1, staff 2
One service user also reported feeling that the service ‘wasn’t for them’ (although she said that she could appreciate its utility for other people), because her social anxiety did not work well with the largely group-based work:
For me, it’s been actually very difficult using the service because actually mixing with other service users I find really difficult. So to do groups has been a real challenge . . . even just going in and, you know, making a drink has been challenging, depending on how many people have been in the room . . . I’m suffering now because I pushed myself, you know, that far to attend a group. Staff tried to support me in there, but it was because . . . yes, it was just being with the other service users. It was just too much.
ADU 4, service user 4
The wider context
Role of the acute day unit in the acute care pathway
Staff and service users viewed ADUs as a crisis service and as an alternative to treatment by CRTs or on the ward:
. . . when we do inductions, I explain to people, 70, 80, 90% of the people here would be inpatients in a ward. That high . . . yes. That percentage. At least, at least 75% of the people here would be inpatients on a ward if we didn’t exist.
ADU 4, staff 2
Acute day units were perceived as serving a critical dual purpose in the acute care pathway of preventing crisis and providing a ‘step down’ post admission:
. . . there’s lots of different pathways that we’re amalgamating into one service. I think we do an inpatient step-down service and we do a crisis relapse prevention service, as well.
ADU 1, staff 1
. . . we’re a step up from the community or a step down from the ward.
ADU 4, staff 2
Acute day units significantly alleviate pressure on other local acute services – particularly CRTs, which have a similar remit – and reduce admissions to hospital.
Respondents raised concerns about a lack of plans or community service provision in place for service users post discharge from ADUs, and that ADUs might be overlooked as a treatment option by staff in other mental health services.
Levels of integration with CRTs varied across the case study sites; in one case the ADU and CRT were fully integrated, while in two others the CRT acted as sole gatekeepers for the ADU caseload, but staff and resources were not shared.
Respondents highlighted the ADU’s role as providing a ‘step down’ from ward care as being a primary source of referrals. Discharge from an inpatient ward can often feel like a very severe drop-off in support, which ADUs can help soften:
People can’t leave hospital and just go straight out into the community. They can’t go straight out to a recovery college. You know, some of them can’t even go straight out and deal with their medication. They need a little help in managing and learning to manage their medication from [ADU 2].
ADU 2, service user 1
It seems to be the case that . . . I’ve had a lot of that from people who have come from the wards, that they felt . . . They felt like they needed more intensive support. It was felt like they couldn’t just be discharged. They said it’s really helped them.
ADU 1, staff 1
Referral to ADU could also feel like a ‘step down’ from CRT care:
I’m just very grateful that there is a place like this and I think I would have been in a bit of a problem if I’d just been discharged by the crisis team and had nothing else to go on to. It’s difficult in everyday life to create a structure and this place has helped me create a structure so that I can have, you know, things to work towards and . . . But I do feel that it could be a longer stay.
ADU 2, service user 7
Another important purpose of ADUs is to facilitate early discharge from hospital:
. . . you get discharged quicker as well. Like, if you got [ADU 4] in place, you’re allowed to be back in the community sooner than what you would if [ADU] wasn’t here because you’ve got [ADU] as, like, the day hospital, and you can come during the day. Then you’re out in your own environment at night time. Whereas if [ADU] wasn’t here, you would have just been in the hospital all the time. You wouldn’t have a chance to come out during the day and go back at night time.
ADU 4, service user 2
However, this could sometimes prove difficult:
. . . sometimes when I look on the bed trackers, I see people on there and I just think, why are they in hospital? We could manage this. We could manage that risk. I know this person. But, once they get on to that ward, the ward tends to hold on to them and you can’t get them off again . . . we really struggle getting people off the ward early. We really struggle.
ADU 4, staff 1
Staff at ADUs reported that they had to be relatively selective about who they took on to their caseload, ‘making sure we don’t unsettle the status quo of the unit and their therapeutic environment’ (ADU 1, staff 3). In particular, those prone to aggression were generally not considered suitable for treatment in an ADU.
One suggested improvement was to provide follow-on care after discharge, or for leaving plans to be made more robust. Respondents linked this issue to the time-limited nature of ADU care, discussed above, but also to the lack of provision of other services after discharge:
I would like to have something like a staying well group. So when people were discharged there was a touch-base period . . . most people, not all people, but the majority of people have good experience here and being discharged to nothing could be, can be . . . That’s where I think it all starts to break down because the community services, there’s not enough care resources. I would like, but I don’t know whether I would like, yes, something like a staying well group or if they were struggling that there was a service that you could say, oh you know, you could just be that person on the phone.
ADU 4, service user 3
In one example, a service user’s community team had told her that they were unable to support her for some months after she had been discharged from the ADU (because of staffing issues at the community team, rather than lack of need):
I think that the main thing is there really needs to be safe leaving plans, and what worries me is that the people who come here are so unwell when they come here, and to not have a safe leaving plan I think is literally putting people’s lives in danger. You can’t go from an acute day unit to nothing because there’s no logic in that.
And I’m sure I’m not the only person who is going from an acute day unit to nothing because of just how the NHS is and how long waiting lists are.
ADU 2, service user 5
A number of service users reported feeling anxious about being discharged from the ADU, and were concerned that they did not feel it was clear what would be happening post discharge; better communication and clarity from staff would help with this.
One suggestion to help smooth the transition after discharge from ADU was a ‘buddy service’ of peer support workers to keep up regular contact for some weeks after discharge (ADU 3, service user 2).
There was a consensus from staff respondents that the ADU is too often overlooked as an option by staff working in other acute and community services; people who might be suitable for ADU treatment are not considered for it, often instead being admitted straight to hospital; and people are left as inpatients for too long without ADU being considered as a facilitator of early discharge. This was voiced as an issue by staff at all study ADUs, but appears to have been particularly problematic at ADU 4, where all three staff respondents raised similar concerns:
I think at the very beginning there was a lot of people didn’t know what this unit was about, and I still believe that now. I think you still get new doctors in the wards that still don’t know what this service is about and you feel that you’re banging your head against a brick wall. Because there’s only so many times you can go and do presentation.
So that’s the really frustrating part because we believe that we can provide a really good service but there’s almost this resistance from the wards to discharge early.
ADU 4, staff 3
So, when I look and I see so-and-so has been admitted, I’m just like, why are we here? Why are you admitting this person when you have this? Why would you not try us?
ADU 4, staff 2
I think there’s a genuine misunderstanding amongst my peers in other services, as to what actually we’re here to do.
ADU 4, staff 1
Another theme strongly represented in the data was reducing the use of other acute services, particularly inpatient care. Staff and service users agreed that, in the absence of any ADU provision, the impact on other acute and community services would be significant:
[ADU not being there would lead to] a larger bed waiting list . . . more cost, obviously, for the NHS . . . and then hospital admissions that can be quite lengthy but unnecessary. We’ve definitely prevented a lot of hospital admissions, I think that’s been the main thing. It’s that people have been able to come here instead of hospital as an alternative.
ADU 1, staff 2
If it didn’t exist, I’d be in hospital a lot more, definitely, and I wouldn’t be getting the support I needed in the community. So I’d be inpatient more, and there wouldn’t be the groups run like there is here, no . . . Yes, I’d just be an inpatient more.
ADU 4, service user 2
The extent to which study ADUs were integrated with other services was variable across the sites.
ADU 1 was fully integrated with a local CRT. All people using the ADU were also on the CRT caseload, and they would often be treated simultaneously by both teams (e.g. the CRT might visit in the evening to do a medication drop, after the service user had spent the day at the ADU). This was seen as an advantage:
It’s quite useful that we work jointly with the crisis team. So, whilst anybody is on our caseload here, they’re also on the crisis team caseload. And then weekends, when we’re closed, crisis team can visit if needed. If it’s late evening and we need somebody to go out and monitor a client’s medication, we can ask the crisis team to go out – just to make sure . . .
ADU 1, staff 2
ADU 2 and ADU 3 accepted referrals from only the CRT, which acted as ‘gatekeepers’ of all acute services. ADU 4 accepted referrals from multiple sources (but, as mentioned above, often struggled to be recognised as an option by community teams).
Acute day units in relation to other acute treatment options
Two of the most common difficulties service users have with CRT treatment are a lack of consistency (different staff members visiting each time) and limited contact time (staff visiting for only 10 minutes to 1 hour per day). 17 Two of the most common difficulties service users have with ward treatment are feeling that the environment is chaotic and unsafe (because of potentially aggressive service users, and the widespread use of restraint techniques by staff), and feeling that there is a lack of meaningful engagement from staff (because of low ratios of staff to service users, staff burnout and a high administrative burden). 40
There was a strong consensus among staff and service user respondents that the ADU model of treatment provides a solution to all four of these problems. The same staff are present each day, and service users have several hours of contact time with staff and other service users. ADU environments feel safer and less chaotic, and staff have higher job satisfaction and much more time to spend in therapeutic engagement with service users.
Acute day units are positioned as a part of the acute care pathway, and so are an alternative to admission to an inpatient ward, treatment from a CRT or staying at a crisis house. Staff and service users in interviews frequently gave less favourable opinions on CRTs than ADUs (to a lesser extent, this was also true of crisis houses, which were available in only two of our four sites, and were utilised much less frequently):
I think it is basically a good service, yes, and definitely far more positive than being on the wards and far more positive than using the crisis team.
ADU 2, service user 5
Acute day units were seen as providing service users with a stronger and more consistent level of support, while allowing them to retain their independence, agency, rights and integration into the community:
I feel it helps because it’s less restrictive than hospitals. I think the voluntary aspect is really important to the service because you get so many people – and they, you know, get unwell in the community and they just get sectioned into hospital. And they don’t want to be in hospital, they don’t want to be sectioned – they lose a lot of their rights, they lose a lot of ability to make a lot of choices over the medication they’re taking, the activities they engage in. You know, being taken away from the home environment.
Whereas here, you’re still with somebody for 6 hours a day. So, you can still monitor them, you can see symptoms, you can still treat somebody. They still get to go home in the evening and sleep in their own bed, have their own home comforts. So, I think that’s really important and I think we’re definitely missing a service like this.
In the community, obviously you can go . . . I worked in a crisis team for years, and you can obviously go out and see people at home and monitor them at home. And it’s nice to see people in the home environment. But realistically, you get about half an hour, 40 minutes with somebody – and then they’ve got 23 hours on their own at home. And then you don’t know what’s going on and you can’t monitor them.
ADU 1, staff 2
Staff felt that they were able to get to know service users better than was possible in other teams, and that, as a result, they could develop more meaningful and personalised interactions and treatments. One contributing factor was better ratios of staff to service users, which allowed for more one-to-one work and greater personalisation:
I’ve been a nurse on the wards, and you’re firefighting all of the time. So, it’s very rare you have the time to sit down with clients and do activities with them. The only thing you can do with them is one-to-ones. So, here, it’s . . . not too intense, but it’s a full-on programme. So, all, day, they are doing something. Whereas, on the ward, they get bored. To me, they get better quicker here.
ADU 3, staff 1
Another positive factor repeatedly mentioned was the lack of a shift system, which was also seen as ‘an advantage in terms of consistency’ (ADU 2, staff 2); having the same staff team providing treatment each day helped build rapport and establish therapeutic relationships.
Staff also reported that they were able to take more detailed notes as a result of deeper, more regular contact with service users (ADU 4, staff 1) and because they had more time to devote to each service user they were able to ‘provide a bit more basic care – make sure somebody washes and eats, has clean clothes to put on, that kind of thing’ (ADU 2, staff 2).
Generally, the mix of professions in ADUs was very similar to that found in a CRT or on a ward, being predominantly composed of nurses, support workers and occupational therapists, with variable support from psychologists; one unit (ADU 2) also employed dedicated art, dance and music therapists.
Acute day units were also seen as proponents of the recovery model of mental health or, more broadly, as less clinical in approach than ward and CRT treatments:
Far more recovery focused, the groups, the goal-setting, the triggers . . . even the fun groups where people can forget about being unwell and you can sit and have a bit of a laugh doing a quiz or something like that . . . Whereas I don’t think you’d get that so much on a ward. I think it would be probably more medical model than what we are here. Because it’s not just about a tablet, it’s a lot more than the taking of tablet. So a bit of both here.
ADU 3, staff 3
The most frequently mentioned difference between CRT and ADU treatment was contact time: service users attend ADUs for up to 6 hours every day, whereas CRT treatment is much less regular. Peer support, or, more generally, the social aspect of group treatment, was also mentioned as an important factor that was not available from CRT:
. . . the crisis team, like I said to you, they can only give 10, 15 minutes at a time. Whereas here, you’ve got 5, 6 hours a day, Monday to Friday.
ADU 1, service user 4
From the crisis team, they get a quick visit, maybe every couple of days. Once a day if they’re very acutely unwell. Here we can have them all week. We have that longitudinal assessment of somebody so that we can keep an eye on them all day. So that helps you make a very good assessment of somebody . . . crisis team could go out to someone every morning and they could be absolutely fine, but family are really struggling with them at different points during the day. So we get to see that kind of longitudinal assessment . . .
And with crisis team it’s maybe not intense enough. You don’t always have the time to spend with people, and they don’t get that peer support either at crisis team. So I think we’re a halfway house between the two, and I think we almost take the best of both. So keep them at home, but give them more support than just an hour’s visit.
ADU 3, staff 3
The lack of consistency mentioned above was the most frequently cited issue with CRT treatment:
This was the problem with the crisis team. She makes a connection with one person, and then on the following week it’s somebody completely different, and it’s having to discuss it all over again. But here, she walks in the door, they know . . . She sees the same faces every day, and that’s the best thing for her, because she was struggling with seeing different people.
ADU 3, carer 1
Consistency was also perceived as useful from a staff perspective as a way of increasing team coherence and bonding:
. . . it’s the best team I’ve ever worked with here, because it’s gelled. Because it’s consistent, it’s 9 to 5 Monday to Friday, so it’s not having to cover those shifts. So you’re on shift with the same staff each day, so the dynamic is constant and everyone, you can play people to their strengths. Whereas when I’ve worked at crisis team, because it’s shifts, each time you go on it’s a different balance of staff, which creates a bit of a different dynamic, which can be positive or negative in terms of patient care and in terms of your own stress levels of that particular day. Whereas here it’s constant, and I, absolutely the best team I’ve worked with for that. And I think that’s the reason why.
ADU 3, staff 3
Acute day units were seen as providing a more efficient use of staff time, as CRT work often involves driving long distances to service users’ homes:
If it’s a patient from [another town in the catchment area, ≈ 20 miles away] and crisis team are based in [the same town as the ADU], you know so it’s taking a lot of their workload off them.
ADU 3, staff 3
Almost all service user respondents who had been on inpatient wards preferred using an ADU. The ADU was described as more ‘relaxed’ and ‘chilled out’ (ADU 1, service user 1) and ‘safer’ and ‘less chaotic’ (ADU 1, service user 2), and staff on wards were described, in comparison with ADU staff, as ‘patronising’ (ADU 2, service user 1), careless and lacking in engagement: ‘abrupt . . . forgot my meds . . . we were just numbers’ (ADU 4, service user 1).
While acknowledging that ADU treatment was not suitable for everyone, and that in some cases ward treatment was necessary, in general both staff and service users saw ADUs as environments much more conducive than inpatient treatment to recovery:
. . . my experience on the ward was just, I may as well have been in prison. It was horrific. The staff don’t talk to you. People are very unwell. It’s very noisy. It’s very violent, and there’s nothing therapeutic about it. I don’t think there’s anything helpful about being on the wards, whereas something like this . . . I know that for some people they’re too unwell to be able to manage to come to a place each day, but if they can, I think it’s a preference definitely to being on the ward.
ADU 2, service user 5
In some cases, ward treatment was seen as potentially doing more harm than good:
[When people are treated on the ward] you’ve imposed restrictions on somebody and took them away from some other functioning that they’re able to do. Because obviously, people can still maintain functioning while being unwell, and to what level of functioning depends on their illness and what they’re able to keep up with. So I think sometimes with inpatient you take away the functioning altogether and that can add to the illness almost.
ADU 3, staff 3
Perhaps the most obvious advantage of ADU treatment over a ward was the ability to retain a feeling of independence by remaining based at home and sleeping there at night:
You’ve got [ADU 4] as, like, the day hospital, and you can come during the day. Then you’re out in your own environment at night time. Whereas if [the ADU] wasn’t here, you would have just been in the hospital all the time. You wouldn’t have a chance to come out during the day and go back at night time.
ADU 4, service user 2
All staff who had also worked on a ward preferred working in an ADU. Staff felt that an ADU provided a ‘less traumatic’ (ADU 3, staff 3) environment that felt safer for both staff and service users, helped by the absence of panic alarms and lack of use of control and restraint techniques (ADU 2, staff 1); and provided an opportunity to engage more productively with service users because of the higher staff-to-service user ratio, which in one case was approximately double:
I would say that we would do similar what the ward would do, but just more intensively, because we haven’t got 20-plus service users. We’ve only got 10, with four clinical staff, which on a normal ward, you’re only going to get four to five people with 19 service users.
ADU 1, staff 3
A further potentially important advantage for trusts of ADU treatment over ward stays is cost. A staff member at ADU 4 quoted figures that suggested a saving of around 50% when comparing costs per day directly:
. . . these figures I’m going to give you are 2 or 3 years old, but it gives you an approximation. It was about £139 a day, stroke night, for someone to be on a ward. It was about £65, £70 for them to come here. So, financially, it costs in as well.
ADU 4, staff 2
Only a couple of service user interviewees had used a crisis house, and in most of the participating trusts these services did not exist. However, those who had used a crisis house commented that periods of care there could be briefer than desired:
My issue with [crisis house] is that the stay is so short that you almost don’t get any therapeutic benefits. You come in there, and as soon as you’re in there they try and get you out, so you don’t actually get time to land and to settle, and to really kind of, consolidate the improvement you’ve made.
ADU 2, service user 2
The wider picture
This study took place against a wider backdrop of NHS mental health services under pressure and facing closure. The AD-CARE follow-up survey of ADUs nationally found that, of 22 originally identified, five NHS ADU services had closed down (three in one NHS trust and the others in two different trusts), and one had been redesigned to provide a pared-down model of ADU care to reduce costs.
One of these closing ADUs was in the same trust as ADU 2. The manager of ADU 3 reported that ADU 3 was the fourth incarnation of an ADU in the trust:
They have opened . . . I think we’re the fourth, actually, in this area. And they’ve closed down at some point, but then opened another one. So that, obviously, there is a need for them, you know?
ADU 3, staff 1
In the interviews there was a background picture of wider frustration with and concern for the NHS, and for mental health services in particular, which was voiced very strongly by service users and staff alike (e.g. suspicion of ‘payment by results’, the idea of wilful misinterpretation of the recovery model for cost saving – and this being an additional constraint on the capabilities and remit of ADUs).
Discussion: qualitative study
Given that there has been little recent research, and no qualitative research, on modern ADUs as defined in this study, it is difficult to make useful direct comparisons with the existing corpus of research, much of which is significantly dated and/or focused on non-acute day hospital models. However, reviews and recent studies of other acute care options have shown high levels of user dissatisfaction with acute inpatient care40,41 and a mixed picture for CRTs. 17
Our data suggest a ringing endorsement of the ADU model from both staff and service users; with the exception of only one service user respondent (who acknowledged that ADUs seemed to be very useful for others, if not for her), all 36 people interviewed gave a broadly positive or very positive account of their experience of using or working in an ADU. It seems clear that there is a strong consensus about the strengths of ADUs, and that these are viewed in some trusts as a valuable part of the acute care pathway, providing better experiences for service users in a crisis than other available acute treatment options.
Strengths and limitations
To our knowledge, this is the first study to explore, in depth, the strengths and weaknesses of ADUs, and their role in the acute care pathway, across a range of contexts and from the multiple perspectives of relevant stakeholders, particularly service users and staff members. The size of the data corpus – drawing on 36 individual interviews – and the range of respondent characteristics gives some cause for confidence that the findings are representative of the views of these two stakeholder groups.
The target number of carer interviews, however, was not reached; only 3 of 12 intended interviews took place, and they produced data that were far less rich than those for the other stakeholder groups, with interviews with carers averaging 11 minutes, compared with an average of 30 minutes for the other groups. Two of the three interviewees did not report being particularly engaged with the ADU, and the third was also a mental health professional and so had an unusually high level of knowledge and engagement with the staff team. Carer interviewees were sought both through study clinical studies officers asking participants in the cohort study and by asking staff to identify carers. Possible reasons for this include the following: all of the ADUs in the study seemed to take a passive approach to carer engagement, or, in the case of ADU 4, attempts at carer outreach were met with limited success; service users who attend ADUs may be more likely to be lacking in social support (and indeed this may be one reason for their referral to ADU treatment rather than to home treatment from a CRT); and carers have historically proved a difficult group to access for qualitative research.
Although the sample was well balanced in terms of age and sex, 81% of service user respondents were white British. This is broadly in line with the national picture; the area where ADU 2 is located is very ethnically diverse, and four of the seven respondents from that area were white British. Previous qualitative research has shown that ethnic minority groups face significant barriers to help-seeking for mental illness,42 and to have only one ethnic minority respondent in the sample may be cause for concern that ethnic minority voices are not adequately represented in this work.
A limitation of the study was that interviews were carried out in a small number of trusts, and those trusts were self-selecting in agreeing to participate in the study. It may be that only those ADUs that were highly functioning, and therefore had generally satisfied service users, were willing to take part in the study, thus biasing our sample. This self-selection bias is, of course, inherent in all research where participants are required to opt in, although we attempted to minimise this issue by inviting all ADUs in the country to participate.
This study placed strong emphasis on service user involvement: both of the peer researchers who were responsible for gathering data and analysing results have lived experience of mental health problems and using acute mental health services. In addition, the UCL team was partnered with the McPin Foundation, which provided a Lived Experience Advisory Panel who were consulted repeatedly throughout the process. This has ensured authentic service user involvement at the three key levels of consultation, collaboration and control,43 which helped ensure that service user voices were represented appropriately throughout the study.
The results presented here are primarily descriptive, with more in-depth analysis being carried out for future publications.
Research implications
This paper forms part of the wider AD-CARE study, part of the purpose of which is to determine the efficacy of ADUs as a method of acute crisis care. The findings of this study should be considered again in context with the results of the other parts of the study, particularly the comparative cohort study which has as its focus the same four ADUs, and seeks to assess their effectiveness at preventing re-admission and satisfaction with services provided. This is discussed in Chapter 10.
One question that has not been adequately addressed is the cost of ADU treatment compared with other forms of acute crisis care. A 2006 study suggested that the cost per day of ADU treatment was 70% that of inpatient care,13 but the ADU model has been developed significantly since then. Anecdotal evidence from this study suggests that the cost per day is closer to 50% that of inpatient care, which is a significant difference worth exploring further; cost-effectiveness is likely to be a major factor influencing policy regarding ADUs.
Clinical implications
Only around 30% of NHS trusts in England currently have ADUs, and the closure of several ADUs during the study period, including in two of the trusts involved in this study, implies that the trend is towards this proportion decreasing. If the results of this study are representative of the national opinion about ADUs, there is a case to be made that this trend should be reversed, given the value that service users and staff place on ADUs and their model of care.
Given the well-documented pressure on mental health acute wards and reduction in available hospital beds,4 acute care options need to be reviewed urgently. ADUs provide a model that this study shows is highly popular, and may also be more effective and less expensive than crisis care alternatives.
Chapter 9 Work package 3: re-admission for acute treatment following discharge from acute mental health care – national cohort study
Parts of this chapter have been reproduced with permission from Osborn et al. 46 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
Methods: Mental Health Minimum Data Set study
Design
This study was a multilevel secondary analysis of routinely collected annual administrative data from providers of secondary mental health care services in England during 2013–15.
Aims
-
To assess whether or not acute re-admission rates are reduced in areas/trusts with a more enhanced crisis care pathway, defined as having an ADU in the pathway, determined from WP 1.
-
To assess whether or not in trusts with ADUs, individuals who access NHS-funded ADUs have different outcomes from similar (propensity score matched) people who have had an acute episode but do not access ADUs.
After data availability in the MHMDS was examined, a change was made to the protocol and we excluded aim 2 from our study [see Why acute day units were (not) identifiable in the Mental Health Minimum Data Set].
Objectives
-
To determine the re-admission rate to the acute care pathway in a national sample.
-
To determine the characteristics (predictors) associated with re-admission.
-
To determine whether or not trusts with an ADU differed in terms of re-admission rates to the acute pathway.
-
To explore the use of MHA in re-admissions.
-
To explore access to emergency services and use of the MHA after discharge from index admission (supplementary analyses).
Data source
-
The MHMDS: a national data set containing anonymised individual-level data about adults using secondary adult mental health services for the financial years 2013/14, 2014/15 and 2014/15 (incomplete, up to November 2015).
-
For supplementary analyses we used Hospital Episode Statistics (HES) data sets, which include administrative data for inpatient admissions to NHS acute hospitals (the Admitted Patient Care data set) and attendance at NHS A&E departments (A&E data set) in England. The linkage service was provided by the NHS Digital and was at the (pseudo/anonymised) individual level.
Study period
-
Cohort entry: index admission starting between 1 April 2013 and 31 May 2015.
-
Cohort exit: 6 months after discharge from index admission discharge or re-admission to acute care pathway if earlier than 6 months.
Study population
The population was individuals who were discharged from the acute care pathway in England during our study period and reported to the MHMDS who met the following inclusion criteria:
-
aged ≥ 16 years
-
not living with dementia or learning disabilities
-
receiving mental health care provided by a single NHS trust (thus excluding non-NHS trusts and acute trusts and care provided by multiple NHS trusts).
Main study outcome
The main outcome was re-admission to the acute care pathway within 6 months of index admission discharge.
Supplementary study outcomes
-
Re-admission to inpatient ward.
-
Re-admission under the MHA.
-
Attendance at A&E.
-
Attendance at A&E for self-harm.
-
Admission to acute hospital.
Predictors of re-admission selected a priori
-
Age.
-
Sex.
-
Marital status.
-
Ethnicity.
-
Payment by Results (PbR) care cluster.
-
IMD.
-
Type of index admission (CRT or inpatient ward).
-
Length of stay at index admission.
-
ADU trust (vs. non-ADU trust).
Definitions
-
ADUs: non-residential services offering daytime treatment and care to adults experiencing a mental health crisis who would otherwise be considered for acute psychiatric hospital admission, or other alternatives to admission including services provided by the CRT. Trusts with ADUs were identified in the initial mapping exercise conducted in 2016 (see Chapter 4) and further revised for this study’s period (2013–15).
-
Index admission to the acute care pathway: the first admission to an inpatient ward and/or CRT.
-
Re-admission to the acute care pathway: the first re-admission occurring in the first 6 months following discharge from index admission. Note that throughout this study we refer to admission and re-admission as admission and re-admission for treatment in the acute care pathway respectively (unless otherwise stated).
-
Main outcome: re-admission to the acute care pathway within 6 mon.hs after discharge from index admission, meaning a new episode of inpatient or CRT treatment.
-
Re-admission to inpatient care (ward): re-admission to the acute care pathway as an inpatient; if an individual was also admitted to CRT at some point during the same episode, the admission was still considered as re-admission to inpatient care.
-
Attendance at A&E: the first attendance to A&E during the 6-month period following discharge from index admission or before/at re-admission to the acute care pathway.
-
Admission at an acute general hospital: the first admission to an acute general hospital (mental health hospitals excluded) during the 6-month period following discharge from index admission or before/at re-admission to the acute care pathway.
-
Index admission under the MHA: an admission during which an individual was formally detained under any section of the MHA 1983 or other acts at any time during the index admission period.
-
Re-admission under the MHA: an admission during which an individual was formally detained under any section of the MHA 1983 or other acts within the first 7 days after the re-admission start date.
Information governance
As outlined above, this study was granted ethics approval (references 16/LO/2160 and 17/CAG/0101).
The data in this study contained confidential service user-level information, and the statistician (GF) and the chief investigator of the study (DO) were granted access to anonymised data by the NHS Digital Data Access and Advisory Group. All data analyses took place through the UCL Data Safe Heaven.
Data Safe Heaven is built using a walled-garden approach, whereby the data are stored, processed and managed within the security of the system, avoiding the complexity of assured end-point encryption. Data Safe Haven has been certified to the ISO27001 information security standard44 and conforms to NHS Digital’s Data Security and Protection Toolkit.
Identifying and cleaning the data
The MHMDS is a national, person-based, individual-level data set describing mental health service users and the care they receive. The MHMDS includes anonymised record-level (i.e. individual service user-level) data about adults (predominantly adults aged ≥ 18 years) using secondary adult mental health services. A small number of individuals aged < 18 years who are receiving treatment in a specialist secondary adult mental health service are also included in the provider trust returns.
Data are collated and released annually and are based on quarterly (or more frequent) returns from providers. Annual data sets include information about inpatient, day treatment, outpatient and community-based secondary mental health care. MHMDS data describe spells of care for each individual from initial referral to final discharge, including the start and end dates of each type of care received. All service user contacts should be reported, including contacts with CRTs. MHMDS also includes geographic identifiers: services provider trust, services commissioners, GP practice and census lower-layer super output area (LSOA). The LSOA is based on the postcode of the service user’s residence, allowing linkage to the local census and deprivation data (see below).
Before 2016, the MHMDS was collated and analysed by the former NHS Health and Social Care Information Centre (www.hscic.gov.uk), now named NHS Digital. Although renamed the Mental Health and Learning Disabilities Data Set in 2014 and the Mental Health Services Data Set in 2015, we shall refer to the data set as the MHMDS.
The structure of the Mental Health Minimum Data Set
For each financial year there are the following data files:
-
The Records data file includes an individual’s demographic data, LSOA and the provider and commissioner of the mental health services. From this file we extracted data on age, sex, ethnicity, marital status, LSOA and mental health service provider.
-
The Episodes data file includes data on care delivered over extended periods of time, and these periods can overlap. From this file we extracted data on admission to ward, admission to mental health team and PbR care cluster assignment.
-
The Events data file includes data on care delivered at specific moments in time, e.g. diagnosis and outpatient contact with a health-care professional. From this file we extracted data on primary and secondary diagnosis (and HoNOS).
Each individual in contact with mental health services reported to the MHMDS has a personal identifier, which does not change across the years and is linked with records, episodes and events. We used the personal identifier to link the annual data sets and the data fields of interest. Each episode and each event also have a personal identifier. We were warned that the same episode (or event) may have more than one identifier across the years or within the same year, creating a considerable number of identical episodes (or event) when merging the yearly data sets. Exploratory analysis confirmed this and, as part of the data management, a large amount of time was spent identifying and removing duplicate entries.
For details on data fields, we referred to the document ‘MHMDS specification.xlsm’ version 4, available on the NHS Digital website. 45
How the acute care pathway was identified in the Mental Health Minimum Data Set
Based on our definition of acute care pathway, we identified the following admissions:
-
admissions to CRT
-
admissions to inpatient ward.
Admissions to the CRT were extracted from the data field ‘TEAMEP’ in the data file ‘Episode’. The ‘TEAMEP’ data field is defined as ‘a continuous period of care for a patient under the responsibility of one or more mental health teams’ and contains a record for every time an individual was under the care of a mental health team and the type of team. We chose code = A02 for the CRT. In the TEAMEP table we also found a further code for CRT ( = A03) and home treatment ( = A04), but when this was compared with the NHS Dictionary we found some discrepancies in the coding. We contacted NHS Digital for clarification and also investigated the length of admissions by team coding (A02 vs. A03 vs. A04), as we expected CRT admissions to be the shortest (see Report Supplementary Material 5). NHS Digital reassured us that crisis resolution and home treatment team was coded A02 in the MHMDS.
Admissions to inpatient ward were extracted from the data field ‘PROVSPELL’ in the data file ‘Episode’. The ‘PROVSPELL’ is defined as ‘a continuous period of inpatient care under a single Hospital Provider, starting with hospital admission and ending with discharge from hospital’ and contains a record of every time an individual was a ward inpatient.
For details on how we defined admissions and extracted variables from MHMDS, see Report Supplementary Material 5.
How the study population was identified in the Mental Health Minimum Data Set
First, we identified individuals who did not meet the inclusion criteria:
-
Those aged < 16 years, from the data file Records.
-
Those whose care was provided by a non-NHS trust or an acute trust or those whose care was provided by more than one trust, from the data file Records.
-
Those with dementia or learning disabilities, from the data files Events and Episodes, using the following exclusion criteria:
-
Having a primary or secondary diagnosis of F70–F79, F00–F09 or G30–G32 (from the data fields PRIMDIAG and SECDIAG of the data file Events).
-
Having been assigned an organic PbR care cluster (18–21 or organic superclass care cluster) (from the data field CLUSTER of the data file Episodes).
-
Ever being admitted to the following mental health teams: organic, young-onset dementia, memory services/clinic, forensic learning disability service, learning disability services or community team for learning disabilities.
-
Second, we identified people who had been admitted to the acute care pathway (i.e. admitted to hospital and/or crisis team; see Chapter 6, Methods: cohort study) at least once during the study period, and excluded those who had not been admitted. For details, see How admissions to the acute care pathway were identified.
Last, we excluded people whose discharge date was unknown and those who were discharged after 31 May 2015 to ensure that 6 months of follow-up data were available for the analysis.
The remaining data set comprised 231,998 persons in 56 NHS trusts. For a visual summary, see the flow chart in Figure 9.
FIGURE 9.
Flow chart of how persons admitted to the acute care pathway between April 2013 and May 2015 reported to the MHMDS were identified for analysis. Adapted with permission from Osborn et al. 46 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
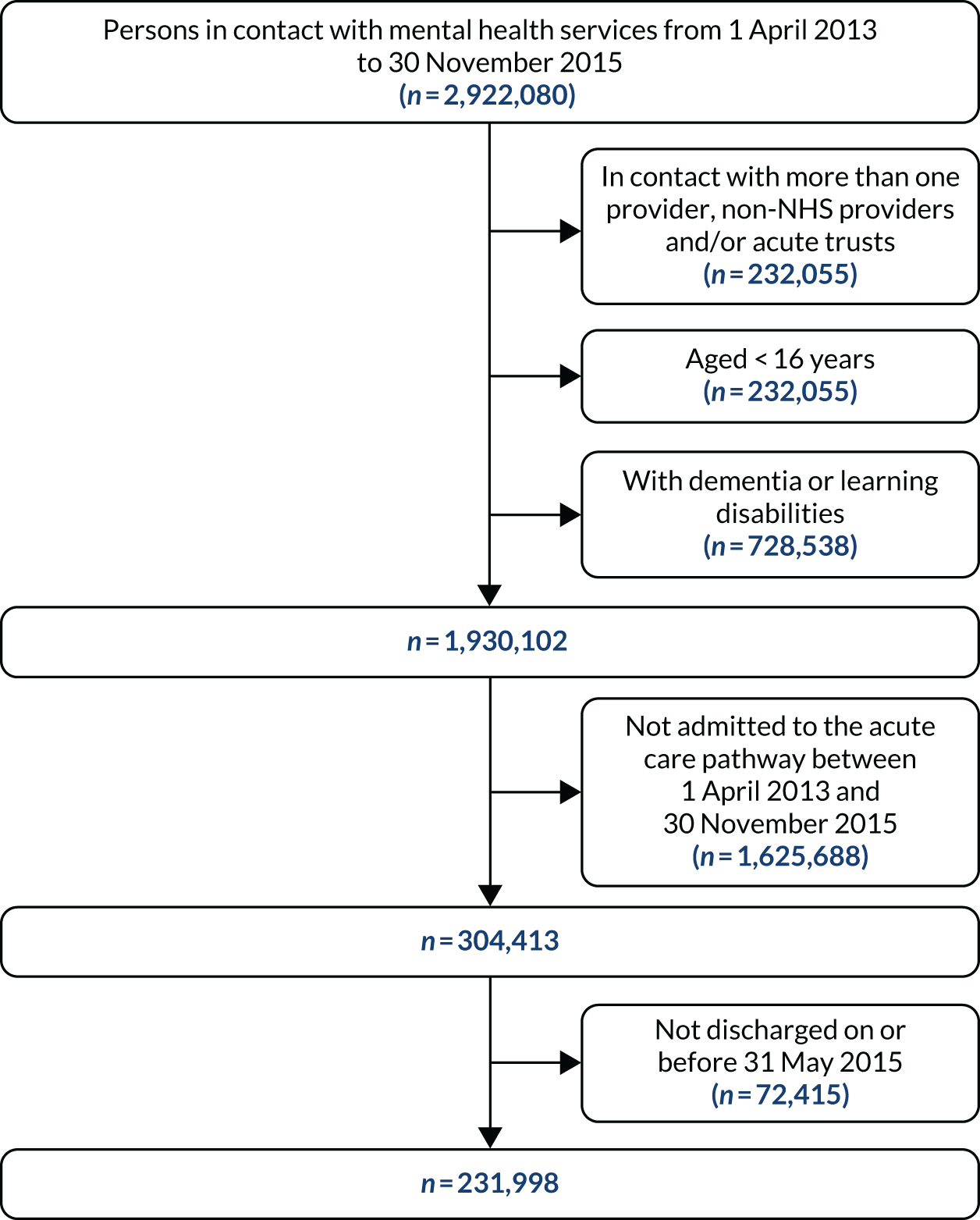
How admissions to the acute care pathway were identified
Exploratory analysis identified a large proportion of persons who had duplicate admissions (more than one admission starting and ending on the same date) but had different identifiers. The proportion of duplicate/identical admissions varied largely by NHS trust.
We noticed that even for the same person there were also admissions with overlapping dates, for example more than one admission starting on the same day but ending at different days or admissions starting and ending within the date range of another admission. We assumed that these admissions were all part of one single admission or episode as long as there was not a gap of more than 1 day between the end date of one and the start date of the next.
We developed an algorithm to identify and merge these identical entries (see Flow chart for decision-making in Report Supplementary Material 6–9). We proceeded as follows:
-
First, we applied this algorithm to clean the hospital admissions. We removed duplicate and merged admissions into one single admission if dates were overlapping. If an admission started on the same day that or the day after the previous admission ended, we considered these two admissions as one single admission episode (see Report Supplementary Material 7).
-
We used the same approach to identify, remove and/or merge admissions to CRTs. We noticed that some admissions to CRTs lasted longer than 180 days. We assumed that this was a data entry error as the duration of an admission to a CRT is much shorter than this (see Report Supplementary Material 8).
-
Finally, we created a variable for ‘admission to acute care pathway’ by merging admissions to hospital and admissions to CRTs into one single admission or acute care episode (see Report Supplementary Material 9).
-
To prepare the data set for analysis, we also excluded people whose date of discharge from their index admission was later than 31 May 2015 (see Report Supplementary Material 10).
Table 26 summarises the number of people identified at each stage and the final number of people of our study population for analysis.
| Admissions | Admissions (n) | Persons (n) |
|---|---|---|
| Admissions to hospital in the MHMDS | ||
| Starting on or after 1 April 2013 to 30 November 2015 | 189,319 | 113,047 |
| After cleaning admission dates | 159,616 | 113,047 |
| Admissions to CRT in the MHMDS | ||
| Starting on or after 1 April 2013 to 30 November 2015 and lasting ≤ 180 days | 500,131 | 261,000 |
| After cleaning admission dates | 420,484 | 260,996 |
| Admissions to acute care pathway (i.e. hospital and/or CRT) | ||
| All hospital and CRT admissions | 577,593 | 304,413 |
| After merging into one admission if dates are overlapping | 470,058 | 304,413 |
| Index admissions to acute care pathway | 304,413 | 304,413 |
| With a discharge date during the study period | 282,580 | 282,580 |
| With a discharge date on or before 31 May 2015 | 231,998 | 231,998 |
| Data set for main analysis | ||
| Number of index admissions (1 April 2013–31 May 2015): 231,998 | Number of persons: 231,998 | |
How predictors of acute re-admission were identified
The following predictors were included:
-
age at the time of index admission, extracted from the Records file
-
sex, extracted from the Records file
-
marital status at the time of index admission, extracted from the Records file
-
ethnicity, extracted from the Records file
-
PbR care cluster, extracted from the Episodes file
-
IMD (see Index of Multiple Deprivation)
-
being admitted in a trust with an ADU compared with being admitted in a trust with no ADU, from AD-CARE WP 1.
Payment by Results care clusters
In the NHS, PbR care clusters are a method of payment (‘currency’) from the health commissioner to the health services provider; each service of care has a fixed tariff based on the clinical characteristics of ‘service users’ (care cluster) as agreed locally with the health commissioners (as in 2015). If there was more than one cluster per person, we chose the one whose date was the closest to the discharge date from the index acute admission. Clusters were grouped into three main groups, indicative of non-psychosis (clusters 0–9), less severe psychosis (clusters 10, 11, 14 and 15) and severe psychosis (clusters 12, 13, 16 and 17).
There were multiple data entries for care clusters within the same person. They shared the same starting date and cluster type but had different identifiers and different ending dates. We removed the repeats and kept only the cluster with the latest ending date. If there was more than one (different) cluster per person we chose the one closest to the discharge date from the index admission (see Report Supplementary Material 11).
Index of Multiple Deprivation
We linked the LSOA of the person’s home address recorded in the MHMDS with the 2010 IMD published by the Office for National Statistics. LSOAs are a set of stable UK geographical areas developed to facilitate the estimation and dissemination of neighbourhood statistics, and they are also used for the reporting of census data. On average, LSOAs include over 600 households and over 1500 residents. The IMD is the official measure of relative deprivation for small areas in England, combining seven transformed domain scores, using the following weights:
-
income (22.5%)
-
employment (22.5%)
-
health and disability (13.5%)
-
education, skills and training (13.5%)
-
barriers to housing and services (9.3%)
-
crime (9.3%)
-
living environment (9.3%).
For further details on how each score is calculated, see the English Indices of Multiple Deprivation 2010. 18
We used the IMD for the year 2010, which is based on the 2010 census, because we could match all of the LSOA provided in the MHMDS with the IMD 2010. We tried to do the same with the IMD for the year 2015 (as it is closer to our study period), but we could not find a match for more than 11,500 (3.7%) LSOAs. The LSOA boundaries, and consequently the codes, changed after 2010. Around 1.8% of our cases did not have a LSOA, and IMD was replaced with a missing value. Of note, a very small number of persons lived in a LSOA of a UK region other than England (i.e. Wales, Scotland, Northern Ireland, Channel Islands) but, coincidentally, none of these persons was represented in our study population.
Acute day unit trusts
To identify the trusts that had access to an ADU service, we revisited the list of the NHS trusts with an ADU as identified in WP 1, because the study census period did not match the MHMDS cohort precisely (2016 for WP 1 and 2013–15 for WP 3). We re-contacted the NHS trusts for information about when their ADUs opened. Among the 56 NHS trusts in the MHMDS for the period between 2013 and 2015, 14 had had access to an ADU service at some point during the MHMDS study period. For brevity, we call these 14 trusts ‘ADU trusts’ and the remaining 42 trusts (out of the 56 identified in the MHMDS for the same study period) ‘non-ADU trusts’ (for lists of trusts, see Report Supplementary Material 12 and 13).
How individuals detained under the Mental Health Act were identified
First, we identified all episodes during which an individual was detained under the MHA between April 2013 and November 2015. We excluded MHA sections starting before 1 January 1990, those ending before the index admission start and those starting after 6 months from discharge. To explore whether or not a re-admission occurred under the MHA, we excluded sections that started later than 7 days from the date of re-admission. Sections of the MHA under which an individual was detained using the same code and starting on same date but ending on different dates were considered as one single episode under the MHA and the section with the most recent date was retained. For details of data cleaning for MHA definitions, see Report Supplementary Material 21.
How individuals attending accident and emergency and admitted to acute hospitals were identified
To obtain information on those in our study population who attended an A&E department or were admitted to an acute hospital within 6 months from discharge or before re-admission to acute care, we used the HES data sets, namely the Accident & Emergency (A&E) data set and the Admitted Patient Care data set. NHS Digital provided a bridge file that linked the two main data sets (MHMDS for the years 2013–16 and HES) at the individual level. After excluding people who were not in the acute care pathway during our study period and those who were admitted to a mental health hospital (and recorded in the Admitted Patient Care data set), we identified 29,298 people who attended A&E and 16,877 people who were admitted to an acute hospital and met our criteria (see flow chart in Report Supplementary Material 22). For details on how we extracted variables from HES, see Report Supplementary Material 5.
Why acute day units were (not) identifiable in the Mental Health Minimum Data Set
We were unable to find a reliable code for using an ADU in the MHMDS to address our second aim in Methods: Mental Health Minimum Data Set study, Aims, regarding individual ADU use.
This section provides some detail regarding the steps we took to attempt to overcome this problem. An initial search in the MHMDS dictionary showed that there was no field or category within a field indicative of an episode of ADU care. As data are entered in the MHMDS for the purpose of reimbursing the services provided by the NHS trusts, we expected that ADU services could be identified. We explored several fields and categories that could be used as proxies for ADU.
We hypothesised that if one of these fields was indeed a proxy for ADU then we would expect virtually zero individuals accessing this ‘proxy’ service in trusts that had been identified as not having an ADU in the WP 1 mapping survey.
Second, we explored the following fields that might be suggestive of ADU:
-
HPCONT – an event that describes the location where a day contact with a health-care professional (HPCONT) took place. It includes outpatient clinic, day hospital or day centre, which potentially could be used as alternative wording for ‘ADU’.
-
DAYATT – an event that describes an attendance at an NHS day-care facility, a term that potentially could be used as alternative wording for ‘ADU’.
-
DAYEP – an episode that describes a continuous period of care for a service user receiving NHS day-care services, which potentially could be used as alternative wording for continuous access to ‘ADU’.
Finally, we compared the number and percentage of individuals accessing the services above in trusts with and trusts without ADUs from the mapping exercise (WP 1). The percentage of individuals with these codes is based on the total number of individuals in the acute care pathway as identified in WP 3 in ADU and non-ADU trusts.
All fields that we explored had been accessed by considerable numbers of individuals in both ADU and non-ADU trusts (Table 27). The proportion of individuals recorded in NHS day-care services (DAYEP), in outpatient clinics (HPCONT) and in NHS day-care facilities (DAYATT) was higher in trusts that had an ADU, suggesting that some trusts may use these fields to record ADU services within the scope of reimbursement. However, because some individuals were also using these services in trusts with no ADUs, we could not be confident in using any of these fields as a binary (yes/no) variable to identify individuals who definitely accessed an ADU service. We also concluded that these codes could be used for many other types of service, including longer-term day services, that are not part of the acute care pathway.
| Table | Field | Service users, n (%) | |
|---|---|---|---|
| ADU trusts (N = 61,450) | Non-ADU trusts (N = 170,548) | ||
| (1) HPCONT (event): health-care professional contact | Location where the contact happened | ||
| Code E01 outpatient clinic | 4761 (7.75) | 9837 (5.8) | |
| Code E03 day hospital | 463 (0.75) | 809 (0.5) | |
| Code H01 day centre | 377 (0.6) | 1202 (0.7) | |
| (2) DAYATT (event): a record for each separate attendance at an NHS day care facility | N/A | 4744 (7.7) | 9355 (5.5) |
| (1) DAYEP (episode): a continuous period of care for a service user receiving NHS day care services | N/A | 17,988 (29.3) | 11,419 (6.7) |
Exploring how an acute day unit is recorded in an example NHS trust
For completeness, we also contacted the information team manager and the data warehouse manager of one NHS trust that had an ADU to explore how that trust’s ADU was coded for NHS Digital. Mental health services data in this trust are stored in the recording system CareNotes, but, to send the data to NHS Digital (i.e. MHMDS), the data are mapped into a different system (compatible with the format required by NHS Digital). Currently, the data are mapped for the current version of MHMDS (the Mental Health Services Data set), and the information team manager was able to describe how ADU services are currently coded for this purpose (see Report Supplementary Material 14). However, they were unaware how ADU episodes were coded and reported to MHMDS historically, to cover our study period from 2013 to 2015.
Acute day unit services are currently (2019) coded in the table MHS201CareContact as Mental Health Services Data Set NATIONAL CODE = A01 (Day Care Service) and the trust’s identifier under Site_Code. The MHS201CareContact table replaces the old Table19HPCON. We were therefore unable to find a method for identifying ADUs in our historical national data. For details, see Report Supplementary Material 14. The flow chart of how individuals were identified in the acute care pathway is in Report Supplementary Material 15.
Summary
We concluded that there is no reliable field for ADU in our MHMDS cohort and there is no standardised way of entering ADU in the MHMDS nationally. Therefore, we cannot be certain about how the trusts coded ADU services during our study period. Some trusts may have used different codes for the same service, which makes it impossible to identify service users who were admitted to an ADU at an individual level in this data source.
As a consequence, we were unable to conduct a propensity score analysis of people in the acute care pathway who were admitted to ADU compared with those who were not admitted to an ADU, as originally planned and, therefore, we were unable to achieve aim 2 above (see Methods: Mental Health Minimum Data Set study, Aims), ‘To assess whether in trusts with ADUs individuals who access NHS-funded ADUs have different outcomes from similar (propensity score matched) people who have had an acute episode but do not access ADUs’.
This difficulty was reported to the funder in progress reports as the study went on.
Therefore, the next section will report on the statistical analysis and results of aim 1.
Analysis of re-admission to the acute care pathway
This section describes the statistical methods and the results of analyses details and how we dealt with missing records.
Aim (restricted to aim 1)
-
To assess whether or not acute re-admission rates are reduced in areas/trusts with a more enhanced crisis care pathway, defined as having an ADU in the pathway, determined from WP 1.
Objectives (restricted to aim 1)
-
To determine the re-admission rate to the acute care pathway in a national sample.
-
To determine the characteristics (predictors) associated with re-admission.
-
To determine the characteristics of people admitted in ADU trusts compared with those admitted in non-ADU trusts.
-
To determine whether or not trusts with an ADU differed from the acute pathway in terms of re-admission rates.
Supplementary objectives
-
To determine the individual characteristics associated with re-admissions to inpatient care.
-
To determine the individual characteristics associated with re-admissions under the MHA.
-
To determine the individual characteristics associated with attendance at A&E, attendance at A&E for self-harm and admission to acute hospital before or at cohort exit.
Method
Descriptive analysis of study population
First, we compared the characteristics of persons admitted in trusts with ADUs with the characteristics of those who were admitted in trusts without ADUs and tested whether or not the differences were statistically significant using chi-squared tests.
We included age as a six-category variable, as the association between age and re-admission was not linear. We grouped ethnicity into five categories (white, Asian/Asian British, black/black British, mixed and other), marital status into three categories (single, married/civil and other) and PbR care cluster into three groups (non-psychosis, non-severe psychosis and severe psychosis). IMD was divided into quintiles, with the lowest (the fifth) quintile representing the least deprived and the highest (the first) quintile representing the most deprived. We created a binary variable for trusts with ADU (yes) compared with trusts with no ADU (no) based from the revised list produced from AD-CARE WP 1. Fields coded as ‘unknown’ or undisclosed were treated as missing. For the list of codes used to identify the predictors, see Report Supplementary Material 5.
Data cleaning and statistical analyses were performed in Stata 15.1 (StataCorp, College Station, TX, USA).
Multivariable multilevel analysis
We investigated the predictors of re-admission by fitting a multilevel logistic regression, with service users (first level) nested in trusts (second level). These models account for possible service user clustering within trusts and allow for trust variation in the risk of re-admission (random effects), as well as an estimation of the strength of the associations between these outcomes and service user and trust characteristics (fixed effects), after accounting for trust-level variation.
First, we assessed the null model, which contains only an intercept and without any fixed part explanatory variables. We estimated the total variance in re-admission across trust, the overall mean re-admission (across trust) and the trust residuals (i.e. the distance of a trust mean from the mean of means trust) with the use of caterpillar plots and the variance partition coefficient, which explains the proportion of the ‘unexplained’ variation by trust. The variance partition coefficient was calculated following the convention that assumes that the binary outcome (re-admission) is defined by a continuous latent variable and service user-level variance is standardised to the logistic variance of π2/3 = 3.29.
The multivariable model included predictors that have been previously reported in the literature and are available in the MHMDS: sex, marital status at baseline, age at baseline, ethnicity, PbR care cluster (if there was more than one, we chose the one closest to the day of index admission discharge), IMD at baseline and whether or not the trust providing mental health care had an ADU in the local acute crisis pathway service (‘ADU trust’ vs. ‘non-ADU trust’).
Finally, we investigated the performance of the multilevel logistic analysis by assessing the residuals at trust level.
Missing data
As data were missing for the predictors of our model (25% for care cluster, 22% for marital status, 11% for ethnicity and 2% for IMD), multiple imputation with chained equation was used to handle missing data based on the assumption that the data were missing at random. We assumed that they were missing at random and imputed missing data for four covariates (care cluster, marital status, ethnicity and IMD) using financial year and age at discharge from index admission, trust, whether or not the person had been re-admitted (yes/no) and sex (for this purpose we dropped 319 persons with sex missing). We used the ‘augment’ command to avoid perfect prediction scenario, generated 10 imputed data sets and combined regression coefficients’ estimates across these using Rubin’s rules. 47 We tested whether missingness was completely at random rather than missing at random by examining differences in the pattern of missingness, and assessed the missing at random model performance by comparing the model estimates with the unadjusted analysis estimates. (For an explanation of multiple imputation with chained equation in lay terms, see Report Supplementary Material 18.)
Supplementary analyses
To explore the factors associated with re-admissions to inpatient care, re-admissions under the MHA, attendances at A&E and admissions to acute general hospital from the time of discharge from index admission to cohort exit, we used the same methodology as above, that is, a multilevel logistic regression analysis adjusted for same covariates as above and using the same imputed data set. For analysis on re-admission under MHA, we also adjusted for admission under MHA. We could not perform a multilevel multivariable analysis to examine the characteristics associated with self-harm because of the small proportion of people who attended A&E for self-harm.
Results: Mental Health Minimum Data Set study
Characteristics of the study population
We identified 231,998 individuals admitted to the acute care pathway between April 2014 and May 2015. The clinical and sociodemographic characteristics of the participants are described in Table 28. Briefly, they were mainly young/middle aged, of white ethnicity, single and living in more deprived areas. The majority had been admitted in a trust that had no ADU. In terms of clinical presentation, the most common care cluster group was non-psychosis. On average, the index admission lasted 10 days (median 10 days, IQR 1–30 days), and the most common index admission was admission to a CRT (156,968/231,998; 67.7%).
Over one-fifth (49,547/231,998; 21.4%) of individuals were re-admitted to the acute care pathway within 6 months of being discharged from their index admission, on average after 34 (median) days (IQR 10–88 days), and nearly half were admitted to inpatient care (23,290/49,547; 47.0%). Individuals who were re-admitted were more likely to be women, single, of mixed or black ethnicity, living in a more deprived area and to receive care for severe psychosis (see Table 28).
| Characteristic | Admitted, n (%) | Re-admitted, n re-admitted/total admitted within same category (%) |
|---|---|---|
| 213,998 (100.0) | 49,547/231,998 (21.4) | |
| Sex (n = 231,659) | ||
| Male | 115,075 (49.7) | 23,961/115,075 (20.8) |
| Female | 116,584 (50.3) | 25,559/116,584 (21.9) |
| Marital status (n = 181,578) | ||
| Single | 109,181 (60.1) | 26,417/109,181 (24.2) |
| Married/civil partnership | 44,126 (24.3) | 9699/44,126 (22.0) |
| Other | 28,271 (15.6) | 6752/28,271 (23.9) |
| Age at baseline (years) (n = 231,998) | ||
| 16–24 | 39,496 (17.0) | 7665/39,496 (19.4) |
| 25–34 | 50,128 (21.6) | 10,453/50,128 (20.9) |
| 35–44 | 49,170 (21.2) | 10,705/49,170 (21.8) |
| 45–54 | 47,844 (20.6) | 10,861/47,844 (22.7) |
| 55–64 | 24,338 (10.5) | 5625/24,338 (23.1) |
| > 64 | 21,022 (9.1) | 4238/21,022 (20.2) |
| Ethnic group (n = 206,309) | ||
| White | 174,983 (84.8) | 39,571/174,983 (22.6) |
| Mixed | 3487 (1.7) | 865/3487 (24.8) |
| Asian/Asian British | 10,864 (5.3) | 2227/10,864 (21.0) |
| Black/black British | 10,245 (5.0) | 2434/10,245 (23.8) |
| Other | 6,730 (3.3) | 1358/6,730 (20.2) |
| Cluster at discharge (n = 172,321) | ||
| No psychosis (0–9) | 109,053 (63.3) | 26,016/109,053 (23.9) |
| Psychosis (10, 11, 14, 15) | 33,349 (19.4) | 8921/33,349 (26.8) |
| Severe psychosis (12, 13, 16, 17) | 29,920 (17.4) | 8988/29,920 (30.0) |
| IMD quintile at baseline (n = 227,872) | ||
| First (most deprived) | 23,415 (10.3) | 4764/23,415 (20.4) |
| Second | 30,335 (13.3) | 6291/30,335 (20.8) |
| Third | 40,543 (17.8) | 8694/40,543 (21.4) |
| Fourth | 55,871 (24.5) | 12,360/55,871 (22.1) |
| Fifth (least deprived) | 77,708 (34.1) | 17,036/77,708 (21.9) |
Characteristics of people admitted and re-admitted to the acute care pathway in trusts with and trusts without acute day units
We identified 61,450 (26.5%) individuals whose care was provided by an ADU trust and 170,548 (73.5%) individuals whose care was provided by a non-ADU trust. There were differences between these two groups. Individuals admitted in an ADU trust were more likely to be single, younger and of non-white ethnicity; they were more likely to be admitted to hospital (rather than a CRT) (Figure 10) and to be in a care cluster for psychosis (moderate or severe) (Table 29). There were no differences in the proportions of people being re-admitted and in the characteristics of individuals being re-admitted to the acute care pathway within 6 months between ADU and non-ADU trusts (see Report Supplementary Material 16 and 17). The probabilities of not being re-admitted during the 6 months following discharge from index admission to acute care are shown in Figure 11 (survival curve).
FIGURE 10.
Venn diagrams showing the number of individuals in the acute care pathway included in the study by type of index admission: (a) ADU trusts (n = 61,450); and (b) non-ADU trusts (n = 170,548).
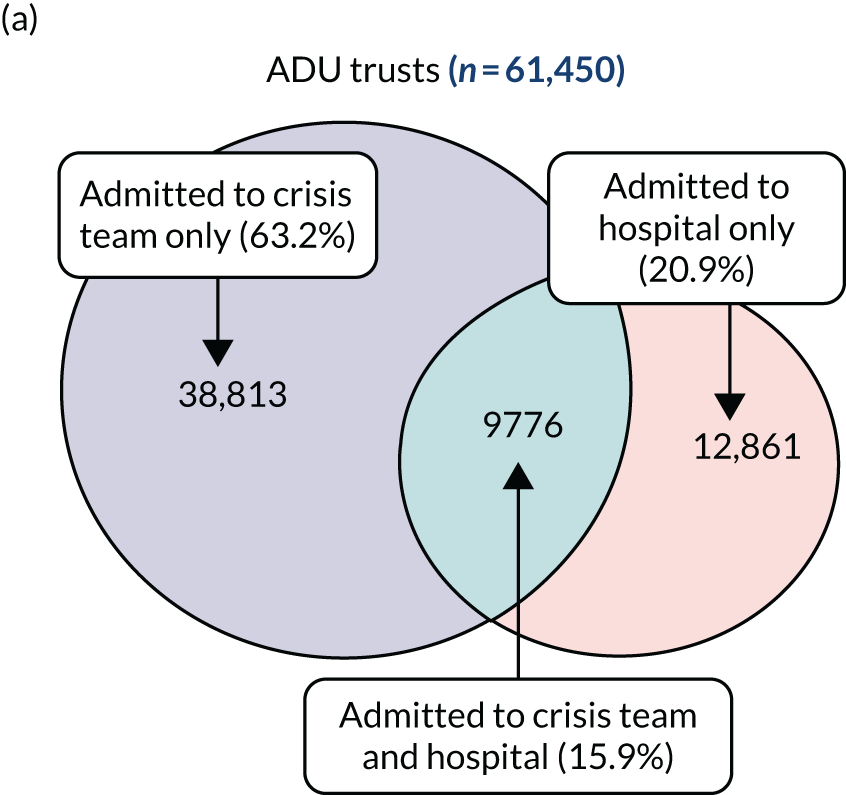

| Characteristic | NHS trusts, n (%) | |
|---|---|---|
| Without ADUsa (N = 170,548) | With ADUsa (N = 61,450) | |
| Sex (n = 231,659) | ||
| Male | 84,385 (49.6) | 30,690 (50.0) |
| Female | 85,843 (50.4) | 30,741 (50.0) |
| Marital status (n = 181,578) | ||
| Single | 80,392 (59.8) | 28,789 (61.1) |
| Married/civil partnership | 32,717 (24.3) | 11,409 (24.2) |
| Other | 21,317 (15.9) | 6954 (14.8) |
| Age at baseline (years) (n = 231,998) | ||
| 16–24 | 28,938 (17.0) | 10,558 (17.2) |
| 25–34 | 36,443 (21.4) | 13,685 (22.3) |
| 35–44 | 36,318 (21.3) | 12,852 (20.9) |
| 45–54 | 35,359 (20.7) | 12,485 (20.3) |
| 55–64 | 17,942 (10.5) | 6396 (10.4) |
| > 64 | 15,548 (9.1) | 5474 (8.9) |
| Ethnic group (n = 206,309) | ||
| White | 129,345 (85.6) | 45,638 (82.8) |
| Mixed | 2397 (1.6) | 1090 (2.0) |
| Asian/Asian British | 7248 (4.8) | 3616 (6.6) |
| Black/black British | 7138 (4.7) | 3107 (5.6) |
| Other | 5041 (3.3) | 1689 (3.1) |
| Cluster at discharge (n = 172,321) | ||
| No psychosis (0–9) | 82,307 (64.7) | 26,746 (59.3) |
| Psychosis (10, 11, 14, 15) | 24,068 (18.9) | 9281 (20.6) |
| Severe psychosis (12, 13, 16, 17) | 20,824 (16.4) | 9096 (20.2) |
| IMD quintile at baseline (n = 227,872) | ||
| First (most deprived) | 16,102 (9.6) | 7313 (12.1) |
| Second | 23,198 (13.9) | 7137 (11.8) |
| Third | 30,770 (18.4) | 9773 (16.2) |
| Fourth | 42,127 (25.2) | 13,744 (22.7) |
| Fifth (least deprived) | 55,208 (33.0) | 22,500 (37.2) |
FIGURE 11.
Survival curve showing the probabilities of not being re-admitted within 6 months following discharge from index admission to acute care (analysis time in number of days). Re-admission to acute care pathway by ADU and non-ADU trusts.
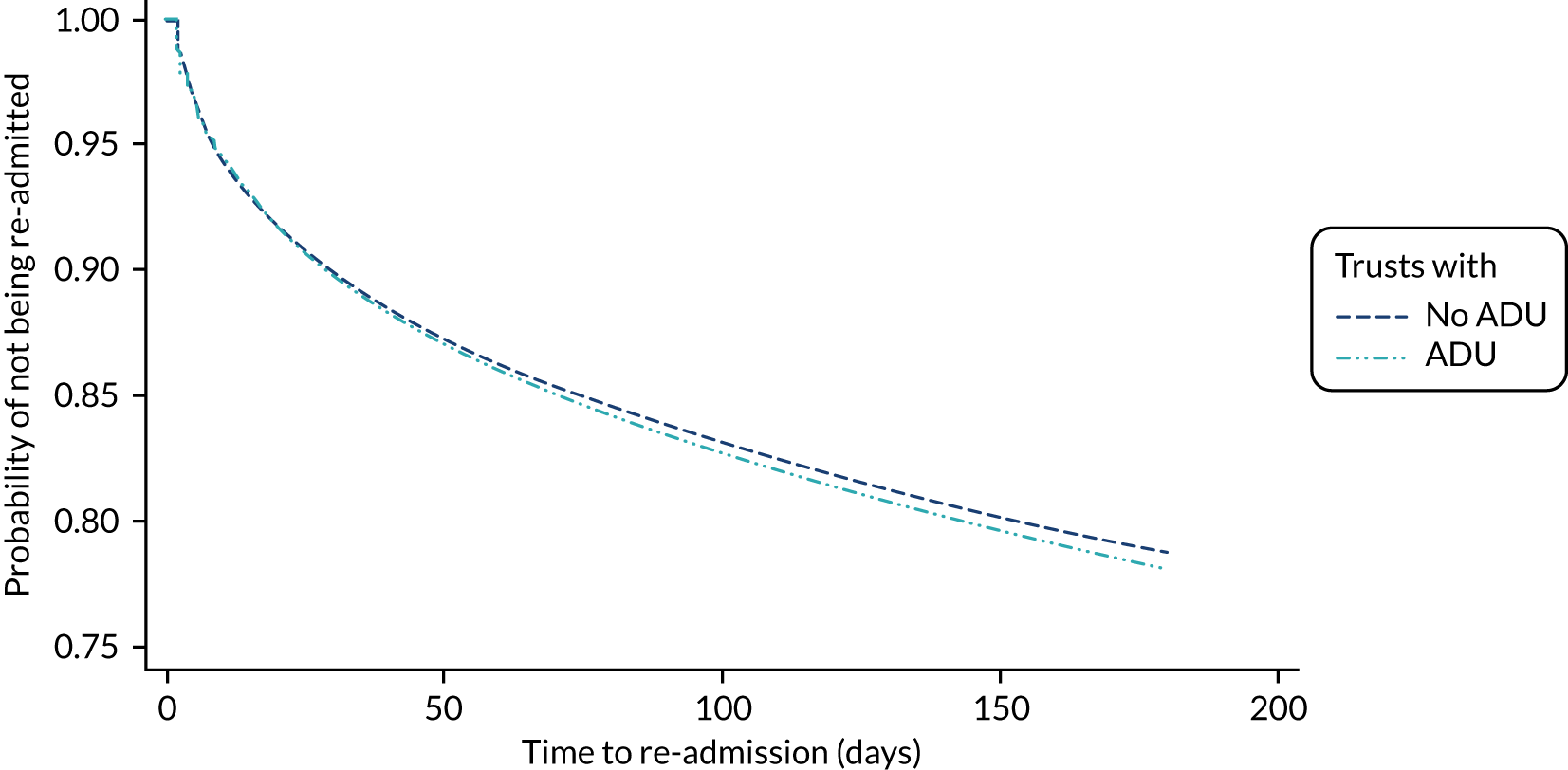
Variance across trusts and the null model
The null model suggested that the odds of being re-admitted in an ‘average’ trust were 0.25 (corresponding to a probability of 0.20) and that the 95% predicted odds of being re-admitted across trust ranged from 0.15 to 0.42 (from 0.13 to 0.30 in probabilities).
The caterpillar plot (Figure 12) shows that for a substantial number of trusts (irrespective of whether or not the trust had an ADU) the 95% CI did not overlap the horizontal line at zero, indicating that the odds of being re-admitted in these trusts were significantly above average (above zero line) or below average (below zero line) and that there was no substantial difference between ADU and non-ADU trusts.
FIGURE 12.
Caterpillar plot of the residuals by trust (null model).
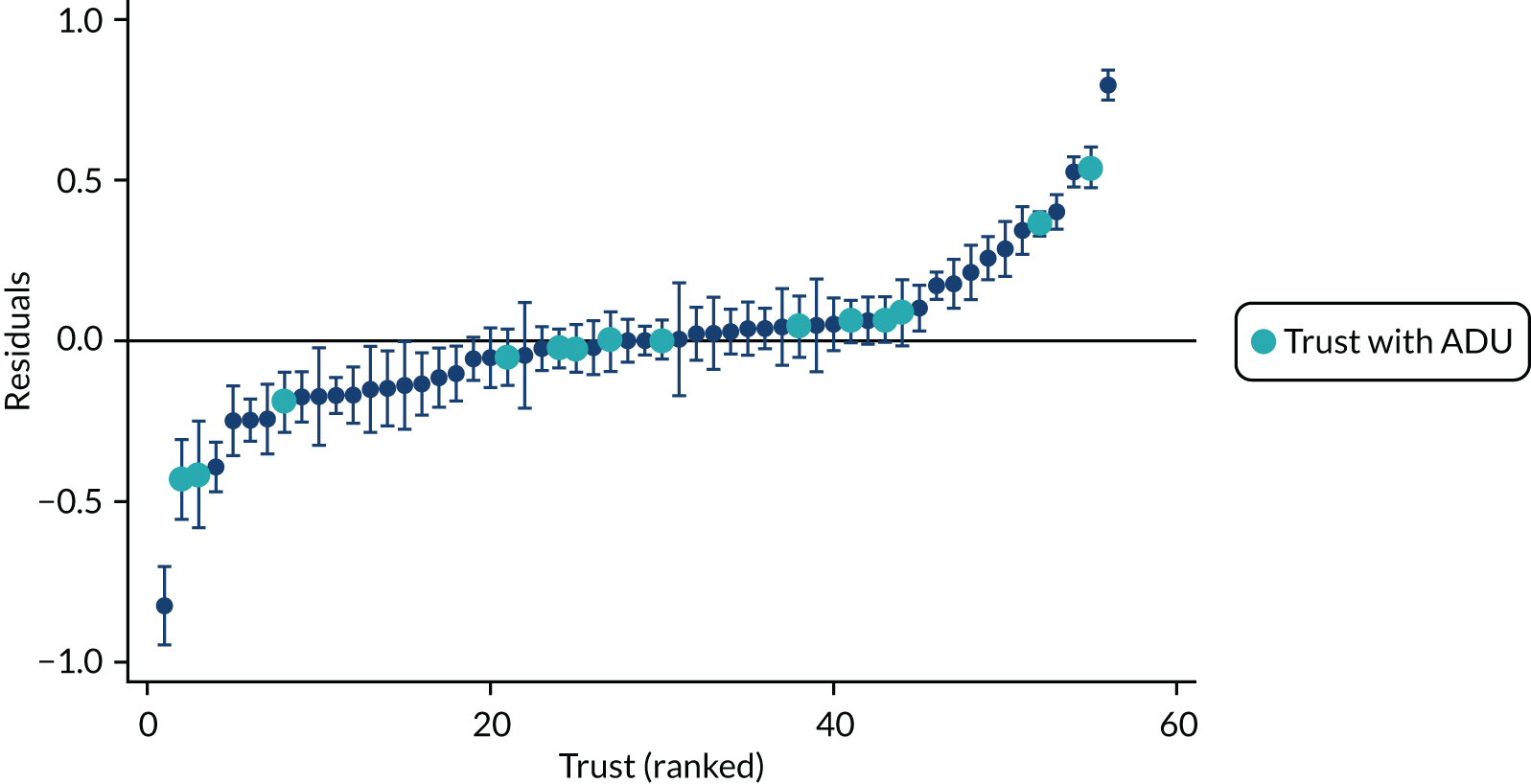
Missing data
Among the 231,998 people included in this study, 90,783 (39.1%) had at least one missing observation for sex, marital status, ethnicity, care cluster or IMD (Table 30). The variables with the largest proportion of missing observations were care cluster (with 25.7% missing observations) and marital status (with 21.7% missing observations).
| Variable | Missing, n (%) | In persons re-admitted (N = 53,456), n (%) | In persons not re-admitted (N = 178,542), n (%) |
|---|---|---|---|
| Cluster | 59,677 (25.7) | 5952 (11.1) | 53,725 (30.1) |
| Marital status | 50,419 (21.7) | 7131 (13.3) | 43,288 (24.3) |
| Ethnicity | 25,689 (11.1) | 3304 (6.2) | 22,385 (12.5) |
| IMD | 4126 (1.8) | 442 (0.8) | 3684 (2.1) |
| Sex | 339 (0.15) | 30 (0.1) | 309 (0.2) |
An investigation into the frequency of missingness by re-admission and age suggested that data were not missing completely at random and that there was strong evidence that re-admission and age were independently predictive of missingness in ethnicity, care cluster and marital status (see Report Supplementary Material 19–20). Therefore, a multivariable analysis using only complete cases (i.e. people with no missing data) would not be appropriate.
Predictors to re-admission to the acute care pathway
Findings from the multivariable multilevel analysis (Table 31) suggest that severe and less severe psychosis (compared with non-psychosis), ageing (compared with aged ≤ 24 years), being female (compared with male), being single (compared with non-single), being of mixed ethnicity (compared with white ethnicity), living in most deprived areas (compared with living in least deprived areas) and being previously admitted to inpatient care are individual characteristics associated with an increased risk in re-admission to acute care. In contrast, being of Asian ethnicity (compared with white ethnicity) reduces the risk. Most (98%) variation was attributable to individual patient- rather than trust-level effects (2.0%). We did not observe any risk increase in trusts without ADUs compared with in those without ADUs (OR 0.96, 95% CI 0.80 to 1.15).
| Univariable model, crude OR (95% CI) | Complete-case model, adjusted OR (95% CI) | Imputed model, adjusted OR (95% CI) | |
|---|---|---|---|
| NHS trust (n = 231,998) | |||
| No ADU | 1.00 | 1.00 | 1.00 |
| ADU | 1.00 (0.86 to 1.17) | 0.95 (0.78 to 1.15) | 0.96 (0.80 to 1.15) |
| Age (years) (n = 231,998) | |||
| 16–24 years | 1.00 | 1.00 | 1.00 |
| 25–34 years | 1.11 (1.08 to 1.15) | 1.05 (1.01 to 1.10) | 1.09 (1.05 to 1.13) |
| 35–44 years | 1.18 (1.14 to 1.22) | 1.07 (1.02 to 1.11) | 1.14 (1.10 to 1.18) |
| 45–54 years | 1.24 (1.20 to 1.28) | 1.11 (1.06 to 1.16) | 1.20 (1.16 to 1.24) |
| 55–64 years | 1.27 (1.22 to 1.32) | 1.10 (1.04 to 1.15) | 1.23 (1.17 to 1.29) |
| > 64 years | 1.10 (1.05 to 1.15) | 0.95 (0.90 to 1.00) | 1.05 (1.00 to 1.10) |
| Sex (n = 231,659) | |||
| Male | 1.00 | 1.00 | 1.00 |
| Female | 1.07 (1.05 to 1.09) | 1.11 (1.08 to 1.14) | 1.14 (1.11 to 1.76) |
| Marital status (n = 181,578) | |||
| Single | 1.00 | 1.00 | 1.00 |
| Married/civil partnership | 0.87 (0.85 to 0.90) | 0.89 (0.86 to 0.92) | 0.88 (0.85 to 0.91) |
| Other | 0.98 (0.95 to 1.01) | 0.97 (0.93 to 1.01) | 0.96 (0.93 to 0.99) |
| Ethnic group (n = 206,309) | |||
| White | 1.00 | 1.00 | 1.00 |
| Mixed | 1.18 (1.09 to 1.28) | 1.08 (0.99 to 1.18) | 1.10 (1.02 to 1.19) |
| Asian/Asian British | 0.97 (0.93 to 1.0) | 0.92 (0.87 to 0.98) | 0.91 (0.87 to 0.96) |
| Black/black British | 1.16 (1.10 to 1.22) | 1.00 (0.94 to 1.06) | 0.98 (0.93 to 1.03) |
| Other | 0.86 (0.81 to 0.92) | 0.86 (0.80 to 0.92) | 0.87 (0.81 to 0.92) |
| IMD quintile (n = 227,872) | |||
| First (most deprived) | 1.00 | 1.00 | 1.00 |
| Second | 1.02 (0.97 to 1.06) | 1.02 (0.97 to 1.08) | 1.00 (0.96 to 1.04) |
| Third | 1.06 (1.02 to 1.10) | 1.04 (0.99 to 1.09) | 1.03 (0.99 to 1.07) |
| Fourth | 1.12 (1.08 to 1.17) | 1.08 (1.03 to 1.13) | 1.07 (1.03 to 1.11) |
| Fifth (least deprived) | 1.15 (1.10 to 1.19) | 1.08 (1.03 to 1.13) | 1.08 (1.04 to 1.12) |
| Care cluster (n = 172,321) | |||
| No psychosisa | 1.00 | 1.00 | 1.00 |
| Psychosisb | 1.25 (1.21 to 1.29) | 1.28 (1.24 to 1.32) | 1.21 (1.18 to 1.24) |
| Severe psychosisc | 1.50 (1.45 to 1.54) | 1.47 (1.42 to 1.52) | 1.76 (1.71 to 1.81) |
| Index admission (n = 231,998) | |||
| CRT | 1.00 | 1.00 | 1.00 |
| Inpatient ward | 1.33 (1.30 to 1.36) | 1.21 (1.17 to 1.25) | 1.35 (1.31 to 1.39) |
| Length of stay at index admission (days) (n = 231,998) | |||
| < 3 | 1.00 | 1.00 | 1.00 |
| 3–12 | 1.09 (1.06 to 1.12) | 0.81 (0.78 to 0.84) | 1.01 (0.98 to 1.04) |
| 13–31 | 1.03 (1.00 to 1.06) | 0.62 (0.59 to 0.64) | 0.89 (0.87 to 0.91) |
| > 31 | 0.99 (0.96 to 1.00) | 0.50 (0.48 to 0.52) | 0.74 (0.72 to 0.76) |
Re-admissions of inpatient care and re-admissions under the Mental Health Act
Nearly half (23,290/49,547, 47.0%) of re-admissions were to an inpatient ward. The risk of being re-admitted was 11% in an ‘average’ trust, and it was between 5% and 26% in 95% of trusts. Multivariable analysis (Figure 13) suggested similar associations between re-admission and individual characteristics to the main analysis, although some associations increased in effect size (psychosis, ageing, index admission at an inpatient ward, mixed ethnicity) or became statistically significant (being of black ethnicity increased the risk of re-admission to inpatient ward only) or became non-significant (e.g. IMD).
FIGURE 13.
Forest plots showing mutually adjusted ORs for re-admission inpatient care by predictors. Reproduced with permission from Osborn et al. 46 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The figure includes minor additions and formatting changes to the original figure.

Fourteen per cent (6814/49,547) of re-admissions were under the MHA. This percentage is quite similar to the proportion of index admissions that occurred under the MHA (16%; 36,454/231,998). The characteristics of individuals re-admitted under MHA are presented in Table 32. Multivariable analysis suggests that previous admissions under the MHA, severe and non-severe psychosis are strongly associated with re-admission under MHA, as, to a lesser extent, is being of black, mixed or Indian ethnicity and ageing (Figure 14).
| Characteristic | Re-admitted under the MHAa (N = 6814) | Admitted to acute general hospitalb (N = 16,877) | Attending A&Ec (N = 29,298) |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 3564 (52.3) | 7384 (43.8) | 14,082 (48.1) |
| Female | 3250 (47.7) | 9491 (56.2) | 15,210 (51.9) |
| Marital status, n (%) | |||
| Single | 4146 (66.1) | 7282 (54.2) | 14,628 (62.5) |
| Married/civil partnership | 1182 (18.9) | 3560 (26.5) | 5089 (21.8) |
| Other | 941 (15.0) | 2597 (19.3) | 3676 (15.7) |
| Age (years), n (%) | |||
| 16–24 | 919 (13.5) | 2509 (14.9) | 5987 (20.4) |
| 25–34 | 1489 (21.9) | 3089 (18.3) | 6488 (22.1) |
| 35–44 | 1447 (21.2) | 3258 (19.3) | 6015 (20.5) |
| 45–54 | 1487 (21.8) | 3512 (20.8) | 5655 (19.3) |
| 55–64 | 816 (12.0) | 2041 (12.1) | 2641 (9.0) |
| > 64 | 656 (9.6) | 2468 (14.6) | 2512 (8.6) |
| Ethnic group, n (%) | |||
| White | 5037 (76.2) | 13,709 (90.2) | 23,119 (87.5) |
| Mixed | 180 (2.7) | 179 (1.2) | 398 (1.5) |
| Asian/Asian British | 490 (7.4) | 551 (3.6) | 1154 (4.4) |
| Black/black British | 715 (10.8) | 453 (3.0) | 1064 (4.0) |
| Other | 189 (2.9) | 314 (2.1) | 700 (2.7) |
| Care cluster, n (%) | |||
| No psychosisd | 2200 (34.1) | 8952 (74.37) | 14,995 (71.6) |
| Psychosise | 2106 (32.7) | 1516 (12.6) | 2968 (14.2) |
| Severe psychosisf | 2144 (33.2) | 1579 (13.1) | 2976 (14.2) |
| IMD quintile, n (%) | |||
| First (most deprived) | 584 (8.7) | 1858 (11.1) | 2841 (9.8) |
| Second | 708 (10.6) | 2298 (13.7) | 3560 (12.3) |
| Third | 1108 (16.6) | 2978 (17.8) | 4913 (16.9) |
| Fourth | 1747 (26.1) | 4065 (24.3) | 7294 (25.1) |
| Fifth (least deprived) | 2549 (38.1) | 5555 (33.2) | 10,463 (36.0) |
| Index admission, n (%) | |||
| CRT | 3291 (48.3) | 11,885 (70.4) | 20,917 (71.4) |
| Inpatient ward | 3523 (51.7) | 4992 (30.0) | 8381 (28.6) |
| NHS trust, n (%) | |||
| No ADU | 4947 (72.6) | 12,038 (71.3) | 20,886 (71.3) |
| ADU | 1867 (27.4) | 4839 (28.7) | 8412 (28.7) |
| LoS in days, median (IQR) | 13 (2–35) | 7 (1–25) | 6 (1–23) |
| MHA at index admission, n (%) | 3182 (46.7) | 1903 (11.3) | 3453 (11.8) |
FIGURE 14.
Forest plot showing the adjusted ORs of being re-admitted under the MHA within 6 months of discharge from the index admission.
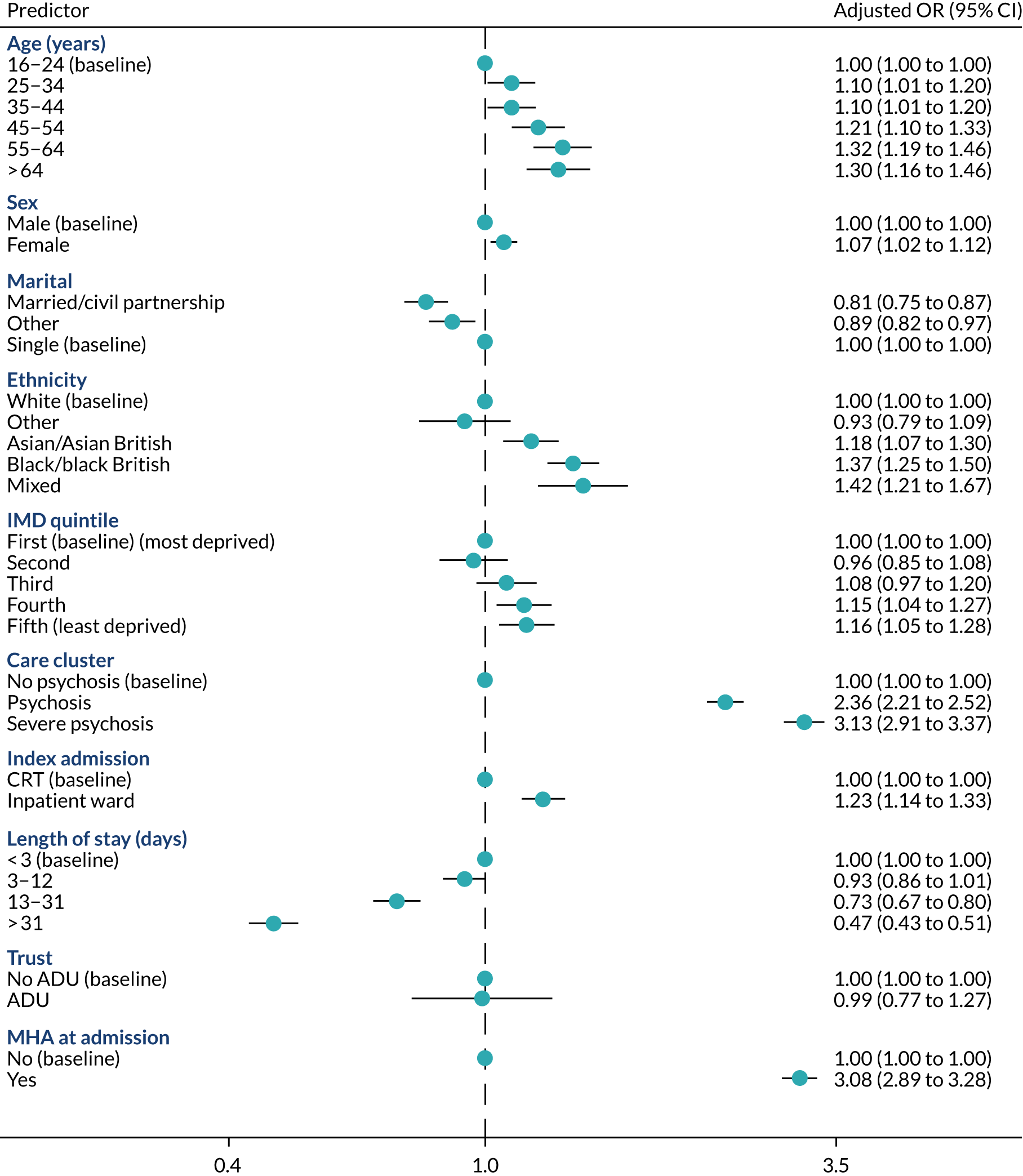
Attendances at accident and emergency and admissions to acute general hospital
Following discharge from index admission, 29,298 (12.6% of all cohort) people attended A&E and 16,877 (7.3%) were admitted to acute hospital. The first attendance at A&E occurred, on average, after 10 (IQR 1–52) days, and self-harm was the cause in 10% (2947/29,298) of these cases. The first admission to acute general hospital occurred, on average, after 44 (IQR 10–100) days, and the most frequent primary diagnosis (3679/16,877; 21.8%) was poisoning by drugs or medications (ICD-10 T36–T50), the most common (1206/16,887; 7.2%) being poisoning by non-opioid analgesics, antipyretics and antirheumatics (ICD-10 T39). The characteristics of individuals attending A&E and those admitted to acute general hospital are presented in Table 32. The results of the multilevel multivariable analyses are shown in Figures 15 and 16. For both outcomes (attendance at A&E and admission to general acute hospital), non-psychosis, being of white ethnicity, being female and staying in an inpatient ward at the index admission increased the risk. However, A&E was more likely to be attended by young people, whereas older people were more likely to be admitted to acute hospital. Living in a more deprived area increased the risk of attending A&E but not of being admitted to hospital.
FIGURE 15.
Forest plot showing the adjusted ORs of attending A&E within 6 months from index admission discharge.
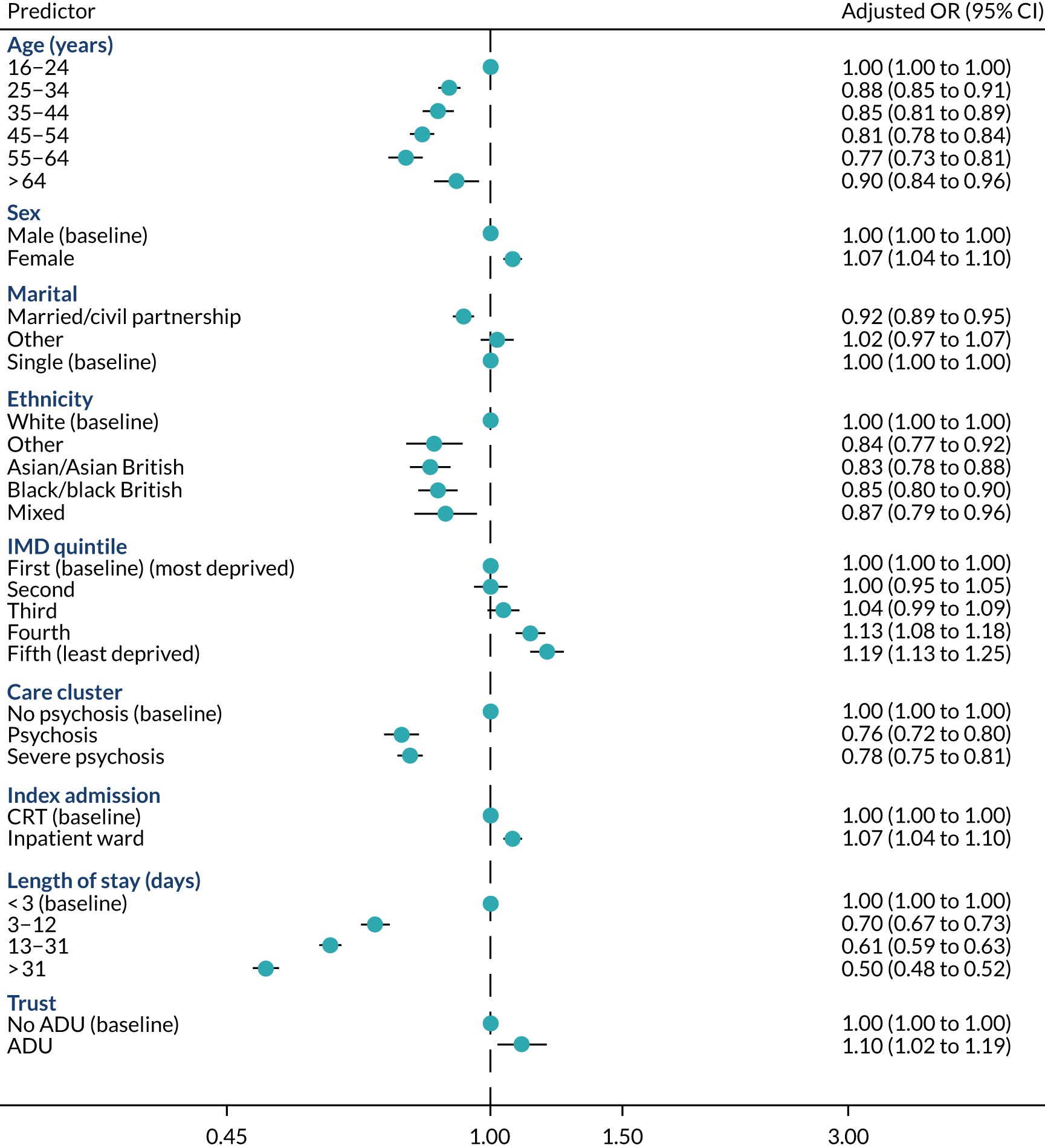
FIGURE 16.
Forest plot showing the adjusted ORs of being admitted to general acute hospital within 6 months from index admission discharge.
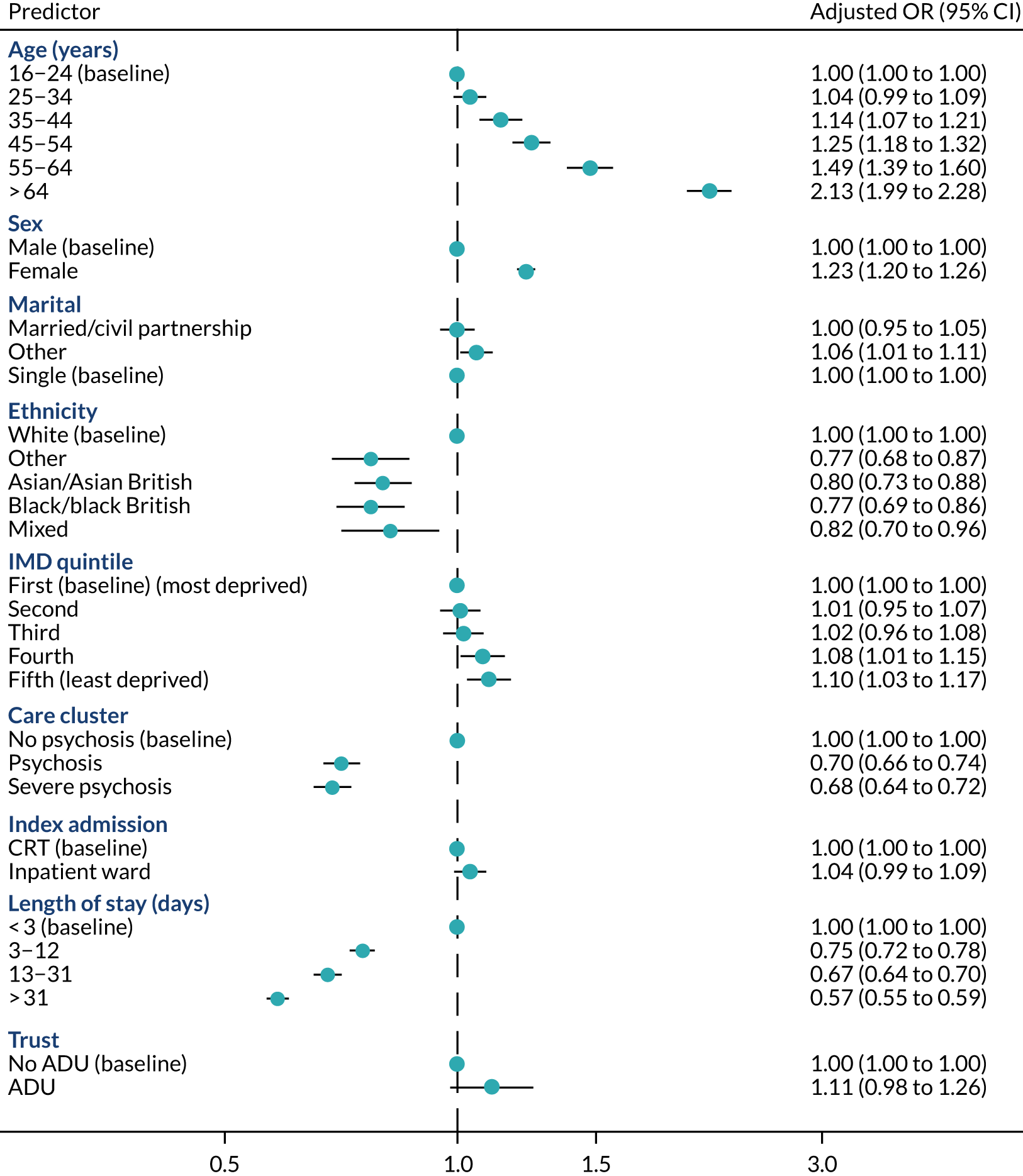
Discussion: Mental Health Minimum Data Set study
Summary of main findings
This study identified more than 230,000 individuals who were admitted and discharged from the acute care pathway in 56 NHS mental health trusts in England between 2013 and 2015. Over 20% of people were re-admitted to mental health acute care within 6 months, half of whom were admitted to an inpatient ward. The median time to re-admission was only 34 days after discharge. Analyses suggested no association between re-admission and the provision of an ADU within a trust’s catchment area. There was large variation in the proportion of acute re-admissions across trusts in England, but multilevel analysis suggests that most of these variations are explained at the level of the individuals who are admitted rather than by trust-level characteristics. The predictors of any acute re-admission identified by the analyses were psychosis, older age, being female, being single, being of mixed ethnicity, living in deprived areas, having shorter index admissions and being admitted to an inpatient ward at the index admission. The predictors of inpatient admission and admission under the MHA were broadly similar.
Almost 13% of the sample attended A&E after discharge from acute care, with a median time to attendance of 10 days. A&E attendees were more likely to be female, of white ethnicity and younger, and are less likely to have a psychosis care cluster. As with other outcomes, people discharged from inpatient stays were more likely to attend.
Strengths and limitations of study
The strength of our study is the size and comprehensive national coverage of the MHMDS, which allowed us to investigate the proportions and predictors of re-admissions to mental health acute care and inpatient wards. To our knowledge, this is the first study that has been able to address this question nationally. However, we were not able to identify access to ADUs at the individual level in the MHMDS data set and were able to answer only the first of our study aims by using a binary indicator at the trust level for ADUs.
The lack of differences between trusts with and trusts without ADUs may reflect the relatively small numbers of people who use ADUs compared with CRTs and psychiatric inpatient services.
The nature of administrative data collected for reimbursement purposes rather than research limited our analyses as we did not have information about (and thus we could not adjust for) important factors that may affect re-admission, such as social support, housing status previous mental health and medical history and employment status. Using the MHMDS is extremely time-consuming, requiring long periods of data cleaning to identify variables, to exclude erroneous and duplicate entries, and to create cohorts that span different years in the data set. Because of the time limitation of this project (18 months), we were unable to conduct further stratified analyses by factors such as psychosis (vs. non-psychosis), age and sex, although the factors associated with re-admission may affect these groups in a different manner.
The MHMDS comprises data submitted from trusts’ records, and the quality and precision of data entry may vary across trusts. For example, there were large variations in the coding of CRT admission, suggesting that coding as well as provision of CRT may vary across trusts. We identified a substantial number of repeated entries, which were dealt with a series of algorithms that allowed us to approach data cleaning in a standardised manner.
Recommendations for future research
Working with MHMDS demands a systematic approach to data cleaning but can still provide answers to research questions regarding mental health care at a national level. Future analysis on re-admission to mental health care should also consider stratifying analysis by mental health disorders groups (i.e. psychosis vs. non psychosis), age and sex. The MHMDS does not contain granular detail to allow a more accurate prediction of which individuals are at greater risk of re-admission.
The disparity between re-admission rates of white and ethnic minority patients is concerning and warrants further investigation. Our findings align with existing evidence about ethnic variations in involuntary admissions. 48
For future research it would be helpful if more accurate coding frameworks were developed to allow different service models in mental health services and the MHMDS to be identified, so that their effectiveness can be explored.
The re-admission rates following discharge are clearly of concern, and further research is needed to determine models of community care or support after discharge that might reduce these re-admission rates.
The overall findings regarding national re-admission rates after a period of acute care in England are discussed in the context of the AD-CARE programme in the following chapter.
Chapter 10 Discussion
Context of the AD-CARE programme: availability of acute day units in the acute care pathway in England
The AD-CARE programme was a mixed-methods study to explore and describe ADUs as part of the acute care system in England. We attempted to identify all NHS and non-NHS ADUs and to examine their key operational features and the types of care that they offer. We then performed more intensive quantitative and qualitative studies in four NHS ADUs to examine service user experience of and outcomes in these day units, and to compare quantitative data with those of people using only crisis teams. We also performed a large national analysis of people discharged from acute care in England to explore whether or not re-admission rates after discharge were different in trusts that offer access to ADUs.
We found that NHS ADUs (n = 27) are available in just under one-third of English NHS trusts. However, the geographical area and population covered by trusts differs substantially; some people have access to more than one ADU, but the majority have no access to ADUs. This is in contrast to inpatient acute care and crisis teams, which are available, in slightly different configurations, across all areas of England. The provision of ADUs is more similar to that of crisis houses, which are also available in only a limited number of areas of England. 49 We also found some voluntary sector or jointly provided ADUs (n = 17), which differed significantly from NHS ADUs in terms of their service model, and were generally located in similar geographical areas to the NHS ADUs available.
Although ADUs have often evolved from older models of care called day hospitals, it is clear that the modern NHS ADUs that we identified offer shorter-term care, with an average length of stay of 5 weeks. They offer daily care, including a range of clinical interventions, as well as opportunities for formal and informal peer support, psychological and social interventions. The day-care model is one that has historically been shown to be effective in reducing admissions and providing an alternative to other forms of acute care, with some evidence that it results in better outcomes. 12
From the mapping survey, we estimate that around 180 people per year are treated in each NHS day unit, which would mean that approximately 4860 people per year in England are treated in 27 units. This contrasts with the number of people discharged during our national MHMDS survey from 2013 to 2015, which was identified as 231,998 over 30 months, or approximately 93,000 people per year. This would roughly equate to just under 30,000 discharges from acute care in the trusts that have ADUs.
It was apparent from both the national mapping survey and our in-depth studies of ADUs that these ADUs have a precarious position in the acute mental health care pathway, despite relatively robust evidence supporting their use. Our study took place during a decade of austerity in England, with commissioning pressures in terms of cost savings and service cuts. When we followed up the initial mapping survey in 2017, five ADUs had already closed and one was being remodelled.
When we attempted to recruit five ADUs for the AD-CARE quantitative and qualitative studies, we had great difficulty identifying ADUs whose funding was stable enough that they could commit to a 2-year prospective research study. Reasons included planned imminent closure, major service reconfiguration and other uncertainty. Furthermore, we identified changes to some of the ADUs during the lifetime of the study. One of our recruitment sites was closed by commissioners in the early stages of participant recruitment and so had to be excluded. Another site was merged with a geographically adjacent ADU. Conversely, we were able to recruit a new site at which a new ADU had been opened to meet the needs of the local acute care system. This site remained open during the AD-CARE study, but was subsequently closed. Funding pressures and the fact that these services are not mandated seemed to explain the vulnerability of ADUs. It is noteworthy that ADUs were not even coded in the national MHMDS, suggesting that some service models in the English NHS are almost forgotten in the modern care pathway.
We were unable to conduct an in-depth study at the voluntary or jointly provided ADU sites for a number of reasons, mostly because the sites did not keep records of caseloads, but also because people did not attend frequently enough to recruit them, and because the ADUs did not keep the routine data we planned to collect, and which would allow us to collect the main variables necessary for our main research questions.
Content of care in NHS acute day units
Among the NHS ADUs we identified through the mapping, most reported that the purpose of their service was to prevent inpatient admissions or facilitate patient discharge from mental health wards. They were often co-located with other mental health services, and most frequently they received referrals from inpatient services, crisis teams and other secondary care services. Fewer received self-referrals and GP referrals.
We found that care was provided by a multidisciplinary team that often included nursing staff, occupational therapists, support workers, psychologists, psychiatrists and administrative staff. They generally opened during standard working hours on 5 days per week. A range of interventions were available, including one-to-one support, physical assessments, psychological work, peer support, medication reviews and support, daily living activities, and carer support or family work. The WP 1 chapter above discussed the fact that ADUs offer more interventions and greater contact time than crisis teams. There was a suggestion that their care model might further increase opportunities for peer support and peer involvement.
The cohort study explored content of care comparing 431 ADU services users with 312 CRT service users at the same site. The service users in the ADU were more likely to receive a physical assessment than CRT service users (80.38% vs. 34.19%), as well as psychological input (58.77% vs. 41.23%) and carer involvement (43.06% vs. 32.90%).
In the peer-researcher-led qualitative interviews, ADU participants positively described the structure of the day programme, the group activities available (and the variety of these), opportunities for psychoeducation and practical support. The key working and one-to-one work in ADUs were also valued by participants, as was the general flexible support that staff provided in the ADU. The PPI group reflected on how the units they visited had a clinical feel, contrasting to voluntary sector day services. This was observed in the physical environment of the units, including depot medication clinics or co-location with other clinical services, the staffing skill mix, and the range of activities offered in the weekly timetable.
Overall, we found that, in terms of content of care, ADUs play a distinctive role in the community acute care pathway. They provide physical, psychological and peer support, which is often lacking in crisis teams, as well as continuity of care, therapeutic relationships, activities and social support.
Service user population in acute day units
In the mapping survey of ADUs nationally, most ADUs reported providing services to adults with mental health problems, and they often had no exclusion criteria. Among those that did exclude people, the most common reasons for this were substance misuse, intoxication, dementia and high-risk psychosis.
The cohort study confirmed that the ADUs were providing care to people at risk of poorer mental health outcomes; most participants in ADUs were single (62%) and unemployed (71%). Compared with crisis team participants, more ADU participants had a recorded diagnosis of personality disorder, psychosis or SMI. They were also more likely to have previously received inpatient care (ADU, 57.5%; CRT, 37%). Two-fifths of participants in both groups were current smokers.
Service user outcomes and experience of acute day units
The peer-researcher-led qualitative study, in four ADUs, concluded that servicer users were extremely positive about their experience of care in the ADUs. They valued the continuity of care, therapeutic relationships with staff, peer support and the group programme (and variety of group content), as well as the structure of the daily care. The availability of one-to-one support and key working was also highlighted as positive.
Service users also described their experience of care at ADUs as far more positive than their experience of crisis teams or inpatient care. They spoke of the short amount of time that service users were offered by crisis teams and the lack of continuity in crisis team care due to shift patterns, which led to a different staff member visiting them at home each time. By contrast, ADUs were reported to provide continuity of staffing and much greater staff contact time, as well as peer support.
This positive experience of ADUs, in comparison with experience of crisis teams, was also confirmed by the cohort study. The mean satisfactions levels were significantly higher in ADUs on the client satisfaction questionnaire, after adjusting for baseline differences in participant characteristics.
Service user-reported clinical outcomes were also significantly better at 8–12 weeks in the ADU group than in the CRT group, with significantly lower depression scores on the CES-D-10 and significantly better well-being scores on the SWEMWBS. The effect sizes for these differences were clinically meaningful in terms of satisfaction, depression and well-being scores (see Tables 14 and 16).
Re-admissions to acute care after discharge
In our programme we examined re-admissions to the acute care pathway, following discharge from acute care at baseline, in a number of ways. Our national cohort study in England using the MHMDS confirmed that there is national variability of 13% and 30% (95 percentile range) among trusts in the proportions of people who return to crisis teams or inpatient services after they have been discharged from acute care. Overall, 49,547 (21.4%) out of 231,998 people were re-admitted to the acute care pathway 6 months after discharge. Worryingly, the median time to acute re-admission following discharge was only 34 days.
Little of this variation in re-admissions was explained at the trust level in multilevel modelling. In other words, the variation in outcomes is explained by variables associated with individuals in each trust population, such as psychosis, area-level deprivation, sex, ethnic group, previous inpatient care and age, rather than by trust-level variables. Only 2% of the variation in admission rates was attributable to trust-level characteristics, suggesting that variation in re-admission after discharge was not highly influenced by service configuration at a trust level during the time of our study. In line with this finding, there was no difference in re-admission rates between trusts with and trusts without access to ADUs in our national cohort study. Given the relatively small numbers of people who access ADUs, and the lack of influence of trust-level variables, we cannot conclude much about the impact of ADUs on re-admission rates from the cohort study finding.
In the qualitative study, ADU staff and service users felt that the ADU provided an alternative to inpatient admission. We certainly found that people using the ADUs in our cohort study were more likely to have previously used inpatient services and perhaps to have more complex mental health needs. The MHMDS study showed higher rates of re-admission among people who had previously received inpatient care. Therefore, it does appear that ADUs deliver a service for people with complex mental health needs.
The results from the cohort study in four ADUs revealed similar rates of re-admission over 6 months among people who had used ADUs and among people who had only used CRTs. There was no difference in admission rates after adjusting for baseline differences in the ADU and CRT groups, such as the fact that those in the ADU group had more previous admissions and were more likely to be unemployed. Across the four trusts we studied, there appeared to be variability in the comparisons of re-admission rates in ADU and CRT service users. In one trust re-admission rates were higher for ADU users than for CRT users, and in one trust rates were lower for ADU users. The other trusts had no statistically significantly different rates of re-admission for ADU and CRT users. The differences between trusts might be a chance finding, as numbers began to get small when we explored results in individual trusts and we did not plan our sample size for such analyses. Alternatively, these difference may be a finding worth further exploration in the future, perhaps including a comparison of the different ADU/CRT service models at the trusts, which is beyond the scope of the current report.
It is worth stating that re-admission is a rather crude outcome measure. It is a marker of relapse and of being then taken on for further acute care. It is also of interest to providers, and suggests that a crisis may not have abated fully or that insufficient care has been provided post crisis. However, re-admission is not a measure of ongoing quality of life or mental health per se, and some commentators would value the well-being and depression outcomes we report over and above a binary outcome of being re-admitted to acute mental health services.
Although the ADU participants did not show different re-admission rates or trajectories, they constitute a group of service users with demonstrable health needs who had better outcomes following a period of treatment in an ADU.
Costs
The health economic analysis explored service costs over 6 months and compared the ADU group with the CRT group within the cohort study. It appeared that there were few cost differences between the two groups during the follow-up period and this analysis accounted for the costs of providing the CRT or ADU services to participants. If anything, there was a negligible cost saving for the ADU group. When the costs of acute mental health care were compared, adjusting for baseline difference in the groups, there were no differences between ADUs and CRTs over 6 months. The cost-effectiveness of ADUs was explored through novel methods using clinical changes in HoNOS data, but the results were not consistent, depending on assumptions in the model. The cost-effectiveness models leaned towards favouring the CRT intervention over ADUs, but they did not achieve conclusive results, and the results for CRTs hinged on a greater improvement in HoNOS scores in the CRT group. This aligns with the findings from the clinical outcomes, which suggested similar re-admission rates but in the context of better depression and well-being outcomes for the ADU group.
Staff reports
The qualitative study explored the views of staff on the ADU, including their place in the acute pathway. Staff felt that the ADU provided positive care that avoided admission, and they valued working in the teams, which influenced staff retention. The value that service users placed on continuity of care was shared by staff, who valued working alongside long-standing colleagues who brought different skills and disciplines to the team. Similarly, both staff and service users valued the ability to build therapeutic relationships as a result of this staff continuity.
Future research
Overall, we found that the ADU care model is a highly acceptable service that should probably not be abandoned. In the future, it would be helpful to generate further evidence regarding the factors that make these models so hard to implement in a sustained way. Making comparisons internationally may help to determine whether or not they are better sustained in less financially constrained service systems. It would also be helpful to make comparisons between units in terms of referral pathways, content of care and service configuration. We were unable to study private or voluntary sector day units in our study for a variety of reasons pertaining to data availability and the stability of such services during the time frame of our study, but this would provide useful additional evidence in the future.
Given the very positive feelings about working in ADUs that staff expressed, it would be interesting to explore comparative rates of staff turnover, and any resulting impact on care, in various different acute care services (ADUs, CRTs, crisis houses, inpatient wards).
Our findings from the cohort work are the first analyses of our data, as final data collection and cleaning occurred in November and December 2019, with this report due on 17 January 2020.
Further analyses would be useful to explore predictors of outcomes within the cohort as well as other measures yet to be analysed, including loneliness and social connections. In particular, it would be interesting to investigate any differences in length of service use between ADUs and CRTs, and whether length of service use is related to teams discharging service users or to service users declining contact.
In summary, we recommend the following in terms of future research:
-
investigation of wider health and care system structures (including the voluntary sector) to determine how ADUs can best be integrated into post-discharge care pathways
-
development of a model of best practice for ADUs
-
inclusion of ADU as a category in data sets such as the MHMDS
-
investigation of staff turnover and well-being, and any impacts that these factors have on care
-
further analysis of our existing data set.
Implications for policy and practice
Our national work with routine NHS data demonstrates high levels of re-admission among people who are discharged from acute care across England. This is particularly marked for, but not restricted to, people with psychosis, women, some ethnic groups, and people who have previously received inpatient care. The time to re-admission is short.
Although re-admission might be the right option for some people who are in crisis, our findings suggest that people may be discharged early or may not receive timely or adequate support in the community. Length of baseline acute episode was inversely associated with risk of re-admission in the national data.
Acute day units are a component of the acute mental health pathway in around one-third of mental health trusts in England. They may not alter overall re-admission rates in their current form, partly because of their small number and partly because they provide care for people with complex mental health needs. However, previous evidence has shown that ADUs are effective as an alternative to inpatient care for some people,9,12 and previous commentaries have suggested that, of the ≈ 17,500 people receiving inpatient treatment at any one time,50 approximately 3130 could receive care in day settings as an alternative. 1,12
Our findings show that ADUs are a highly acceptable form of care for service users and staff, and that they improve well-being and satisfaction. However, they appear to be unstable parts of the mental health system that have been opened and closed. This instability is likely to affect the ability of ADUs to establish themselves within the health-care system. Without stability, they are unlikely to demonstrate their true effectiveness, as they will be unfamiliar to referrers, commissioners and service users. This might lead to underutilisation and make them vulnerable in the pathway, despite being valued by participants in our study.
Overall, our evidence suggests that ADUs probably do have a valuable place in the mental health service system, offering a different pathway from crisis teams and inpatient care, although far fewer people have the opportunity to use ADU services across the country and even within trusts that do provide access.
It is likely that the best way forward is to provide acute care pathways that offer a variety of elements to offer choice and to fit different patterns of service user needs.
A further benefit of ADUs is their ability to address existing problems with acute mental health care. There have been concerns regarding the service user experience of existing crisis care models,51 with many people rating their crisis care negatively. Our ADU findings are very different regarding the service user experience, which was very positive in both qualitative and quantitative assessments. Problems cited with CRT care include a lack of substantial therapeutic input, a lack of continuity of relationships, limited opportunities for social contact and a lack of peer support. ADUs seem to address some of these concerns, and may be particularly beneficial for those with SMI and more complex needs. Similarly, crisis houses have previously been shown to augment the acute pathway by meeting needs of people for whom the home environment is not suitable or home treatment is not possible, and show higher satisfaction. This demonstrates that flexibility in the acute system is preferential and delivering different models of care is likely to be beneficial. Given that costs and re-admissions do not seem to be higher with ADUs, it is probably justified to include this additional component within the acute mental health care pathway. Although the ADU model is sometimes regarded as outdated, our contemporary evidence suggests that ADUs fit with modern health service commitments to provide flexible, person-centred care in the system for people with different needs and preferences for care.
Our findings also show that ADUs provide more comprehensive care, including physical health care peer support, welfare and social interventions. This addresses the ambitions of the NHS long-term plan,52 for instance reducing the physical health comorbidities for people with mental health problems and delivering more integrated forms of community care. Our national findings regarding people discharged from acute care in England certainly suggest that different care models are required in the community to support service users. The need for more robust, holistic community care is in keeping with The Community Mental Health Framework for Adults and Older Adults,53 and ADUs appear to be a part of the modern mental health system that could contribute to this framework. They provide a multidimensional approach to community mental health care for people in a crisis or immediately post crisis. They are well positioned to make comprehensive assessments and to organise community aftercare plans that address the mental, social and physical needs of their service users.
Overall conclusions
Despite the relatively strong evidence base supporting ADUs, they do not form a major part of acute care systems in England. The positive findings from our study regarding clinical recovery and satisfaction with care support the continued provision of ADUs as a means of promoting choice and a range of crisis care options to meet service users’ individual needs.
Chapter 11 Dissemination
We intend to disseminate the results of each part of this programme of research as outlined below.
An infographic will be produced summarising the results of the study, and will be sent to all participants who asked to be kept informed of the study. This is expected to be circulated during the summer of 2021.
We intend to hold a dissemination event, aimed at informing ADU, CRT and other acute care staff, managers and commissioners, as well as service users, carers and policy-makers (e.g. Department of Health and Social Care, NHS England), and providing the opportunity to consider the place of ADUs in the crisis care system. Owing to the global COVID-19 pandemic, we have yet to determine an appropriate date for this event.
A paper has already been published outlining the results of the national mapping and survey work undertaken in WP 1. Lamb D, Davidson M, Lloyd-Evans B, Johnson S, Heinkel S, Steare T, et al. Adult mental health provision in England: a national survey of acute day units. BMC Health Serv Res 2019;19:866.
Individual papers giving the results of each study (WP 2.1, WP 2.2 and WP 3) were published in peer-reviewed journals during 2020–21.
Acknowledgements
We are very grateful to all the individuals who participated in our research: the staff, service users, and carers of the ADUs and CRTs in our study sites. We are also grateful to the NHS Research and Development and NIHR Clinical Research Networks (North Thames, West of England, Eastern, and West Midlands), especially the staff who facilitated and undertook data collection (special thanks to Lisa Carmody, Rose Tierney, Emily Benson, Anthony Wood, Tim Banks, Natalie Stonebank, Clare Davey, Ali Hodges and Jo Morris).
Thanks to our Study Steering Group members, who provided considered and helpful advice at key points in the project.
We wish to thank members of our PPI group, who provided thoughtful advice and discussion of findings, which helped us to better reflect service user perspectives in our work.
Contributions of authors
David Osborn (https://orcid.org/0000-0003-2519-1539) (Chief Investigator) conceived and designed the project, led work on all WPs and was the lead author of the final report.
Danielle Lamb (https://orcid.org/0000-0003-1526-9793) (Programme Manager) ran the project on a day-to-day basis, contributed to the design and management of each WP, collected and analysed quantitative and qualitative data, and contributed to writing the final report.
Alastair Canaway (https://orcid.org/0000-0002-4270-6808) (Health Economist) contributed to the conception and design of the project, led work on the health economics analysis and contributed to writing the final report.
Michael Davidson (https://orcid.org/0000-0002-0020-4578) (Peer Researcher) led work on the qualitative study, including data collection and analysis, and contributed to writing the final report.
Graziella Favarato (https://orcid.org/0000-0003-0694-9121) (Epidemiologist) led work on analysing the MHMDS for WP 3 and contributed to writing the final report.
Vanessa Pinfold (https://orcid.org/0000-0003-3007-8805) (PPI Lead) contributed to the conception and design of the project, led work on PPI and contributed to writing the final report.
Terry Harper (https://orcid.org/0000-0003-4644-7994) (PPI Group Member) contributed to the PPI group work and provided comments on the final report.
Sonia Johnson (https://orcid.org/0000-0002-2219-1384) (Study Group Member) contributed to the conception and design of the project, and provided material for and comments on the final report.
Hameed Khan (https://orcid.org/0000-0002-6185-4806) (PPI Group Member) contributed to the PPI group work and provided material for and comments on the final report.
James Kirkbride (https://orcid.org/0000-0003-3401-0824) (Study Group Member) contributed to the conception and design of the project, and provided material for and comments on the final report.
Brynmor Lloyd-Evans (https://orcid.org/0000-0001-9866-788X) (Study Group Member) contributed to the conception and design of the project, and provided material and comments on the final report.
Jason Madan (https://orcid.org/0000-0003-4316-1480) (Study Group Member) contributed to the conception and design of the project, and provided comments on the final report.
Farhana Mann (https://orcid.org/0000-0002-5890-0859) (Study Group Member) provided comments on the final report.
Louise Marston (https://orcid.org/0000-0002-9973-1131) (Study Group Member) contributed to the conception and design of the project, contributed to the analysis of WP 2.1 data, and provided comments on the final report.
Adele McKay (Study Group Member) provided comments on the final report.
Nicola Morant (https://orcid.org/0000-0003-4022-8133) (Study Group Member) contributed to the conception and design of the project, contributed to analysis and write-up of WP 2.2, and provided comments on the final report.
Debra Smith (https://orcid.org/0000-0002-5020-1228) (PPI Group Member) contributed to the PPI group work, and provided material for and comments on the final report.
Thomas Steare (https://orcid.org/0000-0002-3881-2018) (Research Assistant) collected and managed data for WP 2.1, contributed to the day-to-day running of the project, and provided comments on the final report.
Jane Wackett (https://orcid.org/0000-0001-9939-1002) (Peer Researcher) contributed to data collection, analysis and write-up of WP 2.2, and provided material for and comments on the final report.
Scott Weich (https://orcid.org/0000-0002-7552-7697) (Study Group Member) contributed to the conception and design of the project, and provided comments on the final report.
Publications
Lamb D, Davidson M, Lloyd-Evans B, Johnson S, Heinkel S, Steare T, et al. Adult mental health provision in England: a national survey of acute day units. BMC Health Serv Res 2019;19:866.
Lamb D, Steare T, Marston L, Canaway A, Johnson S, Kirkbride J, et al. A comparison of clinical outcomes, service satisfaction and well-being in people using acute day units and crisis resolution teams: cohort study in England. BJPsych Open 2021;7:E68.
Morant N, Davidson M, Wackett J, Lamb D, Pinfold V, Smith D, et al. Acute day units for mental health crises: a qualitative study of service user and staff views and experiences. BMC Psychiatry 2021;21:146.
Osborn D, Favarato G, Lamb D, Harper T, Johnson S, Lloyd-Evans B, et al. Readmission after discharge from acute mental healthcare among 231,988 people in England: cohort study exploring predictors of readmission including availability of acute day units in local areas. BJPsych Open 2021;7:E136.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Lamb D, Davidson M, Lloyd-Evans B, Johnson S, Heinkel S, Steare T, et al. Adult mental health provision in England: a national survey of acute day units. BMC Health Serv Res 2019;19. https://doi.org/10.1186/s12913-019-4687-8.
- British Medical Association . Breaking Down Barriers – The Challenge of Improving Mental Health Outcomes 2018. https://unitementalhealth.files.wordpress.com/2018/02/breaking-down-barriers-mental-health-briefing-apr2017.pdf (accessed 4 August 2020).
- Quirk A, Lelliott P. What do we know about life on acute psychiatric wards in the UK? A review of the research evidence. Soc Sci Med 2001;53:1565-74. https://doi.org/10.1016/S0277-9536(00)00457-3.
- Care Quality Commission . The State of Care in Mental Health Services 2014–17 2017. www.cqc.org.uk/sites/default/files/20170720_stateofmh_report.pdf (accessed 4 August 2020).
- Davies SC. Annual Report of the Chief Medical Officer 2013 Public Mental Health Priorities: Investing in the Evidence 2014.
- Crisis Care Concordat 2014. www.crisiscareconcordat.org.uk/ (accessed 7 May 2021).
- Crisp N, Smith G, Nicholson K. Old Problems, New Solutions – Improving Acute Psychiatric Care for Adults in England 2016. www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/policy/policy-old-problems-new-solutions-caapc-report-england.pdf?sfvrsn=7563102e_2 (accessed 4 August 2020).
- Lloyd-Evans B, Paterson B, Onyett S, Brown E, Istead H, Gray R, et al. National implementation of a mental health service model: a survey of crisis resolution teams in England. Int J Ment Health Nurs 2018;27:214-26. https://doi.org/10.1111/inm.12311.
- Kallert TW, Glöckner M, Priebe S, Briscoe J, Rymaszewska J, Adamowski T, et al. A comparison of psychiatric day hospitals in five European countries: implications of their diversity for day hospital research. Soc Psychiatry Psychiatr Epidemiol 2004;39:777-88. https://doi.org/10.1007/s00127-004-0813-x.
- Newbigging K, Mohan J, Rees J, Harlock J, Davis A. Contribution of the voluntary sector to mental health crisis care in England: protocol for a multimethod study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-019238.
- Shek E, Stein AT, Shansis FM, Marshall M, Crowther R, Tyrer P. Day hospital versus outpatient care for people with schizophrenia. Cochrane Database Syst Rev 2009;4. https://doi.org/10.1002/14651858.CD003240.pub2.
- Marshall M, Crowther R, Sledge WH, Rathbone J, Soares-Weiser K. Day hospital versus admission for acute psychiatric disorders. Cochrane Database Syst Rev 2011;12. https://doi.org/10.1002/14651858.CD004026.pub2.
- Priebe S, Jones G, McCabe R, Briscoe J, Wright D, Sleed M, et al. Effectiveness and costs of acute day hospital treatment compared with conventional in-patient care: randomised controlled trial. Br J Psychiatry 2006;188:243-9. https://doi.org/10.1192/bjp.188.3.243.
- NHS England . The Five Year Forward View for Mental Health 2016. www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf (accessed 4 August 2020).
- Department of Health and Social Care . The Mental Health Policy Implementation Guide 2001.
- Briscoe J, McCabe R, Priebe S, Kallert T. A national survey of psychiatric day hospitals. Psychiatr Bull 2004;28:160-3. https://doi.org/10.1192/pb.28.5.160.
- Morant N, Lloyd-Evans B, Lamb D, Fullarton K, Brown E, Paterson B, et al. Crisis resolution and home treatment: stakeholders’ views on critical ingredients and implementation in England. BMC Psychiatry 2017;17. https://doi.org/10.1186/s12888-017-1421-0.
- Ministry of Housing, Communities and Local Government . English Indices of Deprivation 2010 n.d. www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 4 April 2019).
- Lamb D, Steare T, Marston L, Canaway A, Johnson S, Kirkbride J, et al. A comparison of clinical outcomes, service satisfaction and well-being in people using acute day units and crisis resolution teams: cohort study in England. BJPsych Open 2021;7. https://doi.org/10.1192/bjo.2021.30.
- Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann 1982;5:233-7. https://doi.org/10.1016/0149-7189(82)90074-X.
- Haver A, Akerjordet K, Caputi P, Furunes T, Magee C. Measuring mental well-being: a validation of the Short Warwick–Edinburgh Mental Well-Being Scale in Norwegian and Swedish. Scand J Public Health 2015;43:721-7. https://doi.org/10.1177/1403494815588862.
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 1994;10:77-84. https://doi.org/10.1016/S0749-3797(18)30622-6.
- Hays RD, DiMatteo MR. A short-form measure of loneliness. J Pers Assess 1987;51:69-81. https://doi.org/10.1207/s15327752jpa5101_6.
- Lubben J, Blozik E, Gillmann G, Iliffe S, von Renteln Kruse W, Beck JC, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist 2006;46:503-13. https://doi.org/10.1093/geront/46.4.503.
- Health Education Authority . Health and Lifestyles: A Survey of the UK Population – Part 1 1995.
- Boyd JE, Otilingam PG, Deforge BR. Brief version of the Internalized Stigma of Mental Illness (ISMI) scale: psychometric properties and relationship to depression, self esteem, recovery orientation, empowerment, and perceived devaluation and discrimination. Psychiatr Rehabil J 2014;37:17-23. https://doi.org/10.1037/prj0000035.
- Priebe S, Gruyters T, Heinze M, Hoffmann C, Jäkel A. Subjective evaluation criteria in psychiatric care – methods of assessment for research and general practice. Psychiatr Prax 1995;22:140-4.
- Osborn DP, Lloyd-Evans B, Johnson S, Gilburt H, Byford S, Leese M, et al. Residential alternatives to acute in-patient care in England: satisfaction, ward atmosphere and service user experiences. Br J Psychiatry Suppl 2010;53:s41-5. https://doi.org/10.1192/bjp.bp.110.081109.
- Werbeloff N, Chang CK, Broadbent M, Hayes JF, Stewart R, Osborn DPJ. Admission to acute mental health services after contact with crisis resolution and home treatment teams: an investigation in two large mental health-care providers. Lancet Psychiatry 2017;4:49-56. https://doi.org/10.1016/S2215-0366(16)30416-3.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: Personal Social Services Research Unit, University of Kent; 2016.
- D’Agostino A, Swaby M. Crisis House and Crisis Café Report 2017.
- NHS Tees, Esk and Wear Valley . Recovery House in County Durham and Darlington 2018. www.tewv.nhs.uk/get-involved/what-you-can-do/recovery-house-in-county-durham-and-darlington/.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013 2013.
- The King’s Fund . Mental Health Under Pressure 2015. www.kingsfund.org.uk/publications/mental-health-under-pressure (accessed 4 August 2020).
- Burns T, Rugkåsa J, Yeeles K, Catty J. Coercion in mental health: a trial of the effectiveness of community treatment orders and an investigation of informal coercion in community mental health care. Programme Grants Appl Res 2016;4. https://doi.org/10.3310/pgfar04210.
- Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods 2006;18:59-82. https://doi.org/10.1177/1525822X05279903.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Morant N, Davidson M, Wackett J, Lamb D, Pinfold V, Smith D, et al. Acute day units for mental health crises: a qualitative study of service user and staff views and experiences. BMC Psychiatry 2021;21. https://doi.org/10.1186/s12888-021-03140-2.
- Gilburt H, Slade M, Rose D, Lloyd-Evans B, Johnson S, Osborn DPJ. Service users’ experiences of residential alternatives to standard acute wards: qualitative study of similarities and differences. Br J Psychiatry 2010;197:s26-31. https://doi.org/10.1192/bjp.bp.110.081075.
- Mind . Listening To Experience: An Independent Report into Acute and Crisis Mental Healthcare 2011.
- Mantovani N, Pizzolati M, Edge D. Exploring the relationship between stigma and help-seeking for mental illness in African-descended faith communities in the UK. Health Expect 2017;20:373-84. https://doi.org/10.1111/hex.12464.
- Syrett M. Service user involvement in mental health research: a user’s perspective. Adv Psychiatr Treat 2011;17:201-5. https://doi.org/10.1192/apt.bp.110.008003.
- International Organization for Standardization (ISO) . ISO/IEC/27001:2013./Information/Technology/—/Security/Techniques/—/Information/Security/Management/Systems/—/Requirements n.d. www.iso.org/isoiec-27001-information-security.html (accessed 18 May 2021).
- NHS Digital . Mental Health Services Data Set Archived Specification n.d. https://webarchive.nationalarchives.gov.uk/20171011052615/http://content.digital.nhs.uk/article/7439/Mental-Health-Services-Data-Set-Archived-Specification (accessed 25 March 2019).
- Osborn D, Favarato G, Lamb D, Harper T, Johnson S, Lloyd-Evans B, et al. Readmission after discharge from acute mental healthcare among 231,988 people in England: cohort study exploring predictors of readmission including availability of acute day units in local areas. BJPsych Open 2021;7.
- Rubin D. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons; 1987.
- Barnett P, Mackay E, Matthews H, Gate R, Greenwood H, Ariyo K, et al. Ethnic variations in compulsory detention under the Mental Health Act: a systematic review and meta-analysis of international data. Lancet Psychiatry 2019;6:305-17. https://doi.org/10.1016/S2215-0366(19)30027-6.
- Johnson S, Gilburt H, Lloyd-Evans B, Osborn DP, Boardman J, Leese M, et al. In-patient and residential alternatives to standard acute psychiatric wards in England. Br J Psychiatry 2009;194:456-63. https://doi.org/10.1192/bjp.bp.108.051698.
- NHS Digital . Statistics: Bed Availability and Occupancy Data – Overnight 2019. www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/bed-data-overnight/ (accessed 4 August 2020).
- Gibson S, Hamilton S, James K. Evaluation of the Crisis Care Concordat Implementation. London: McPin Foundation; 2016.
- NHS England . NHS Long Term Plan 2019. www.longtermplan.nhs.uk (accessed 4 August 2020).
- NHS England . The Community Mental Health Framework for Adults and Older Adults n.d. www.england.nhs.uk/publication/the-community-mental-health-framework-for-adults-and-older-adults/ (accessed 4 August 2020).
List of abbreviations
- A&E
- accident and emergency
- ADU
- acute day unit
- CEAC
- cost-effectiveness acceptability curve
- CES-D-10
- Center for Epidemiologic Studies Depression Scale-10
- CI
- confidence interval
- CORE
- CRT Optimisation and Relapse Prevention study
- CRT
- crisis resolution team
- CSQ
- Client Satisfaction Questionnaire
- EHR
- electronic health record
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- HoNOS
- Health of the Nation Outcome Scales
- HR
- hazard ratio
- ICD-10
- International Statistical Classification of Diseases, Tenth Revision
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- LSOA
- lower-layer super output area
- MHA
- Mental Health Act
- MHMDS
- Mental Health Minimum Data Set
- MHSDS
- Mental Health Services Data Set
- OR
- odds ratio
- PbR
- Payment by Results
- PPI
- patient and public involvement
- SD
- standard deviation
- SMI
- severe mental illness
- SWEMWBS
- Short Warwick–Edinburgh Mental Well-being Scale
- UCL
- University College London
- WP
- work package
Notes
-
Individual characteristics of those re-admitted in ADU and non-ADU trusts
-
Multiple imputation with chained equation (MICE) in lay terms
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr09180).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
