Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 16/41/04. The contractual start date was in March 2018. The final report began editorial review in March 2021 and was accepted for publication in June 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Edwardson et al. This work was produced by Edwardson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Edwardson et al.
Chapter 1 Introduction and background
Sedentary behaviour and health
Sections of this report have been reproduced with permission from Edwardson et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Epidemiological evidence
Sedentary behaviour is defined as ‘any waking behaviour characterised by an energy expenditure ≤ 1.5 metabolic equivalents, while in a sitting, reclining or lying posture’. 2 The health implications of sedentary behaviour have received an increasing amount of attention over the last two decades, and there is now a wealth of epidemiological evidence linking high levels of sedentary behaviour to morbidity and mortality. Systematic reviews and meta-analyses present strong evidence that a greater amount of time spent sedentary is associated with higher all-cause and cardiovascular disease mortality rates,3–6 and a higher risk of type 2 diabetes3,4,7 and incident cardiovascular disease. 3,4,8 Moderate evidence exists for a higher risk of total cancer incidence, with incident endometrial, colon and lung cancers being associated with high levels of sedentary time. 4,9,10 Furthermore, for all-cause mortality,6,7,11 cardiovascular disease mortality12 and incident cardiovascular disease,8 there is evidence of a dose–response relationship with sedentary time.
The reported thresholds of sedentary time associated with adverse health outcomes vary depending on the health outcome of interest and sedentary behaviour assessment. Patterson et al. 13 concluded that for adults the risk of all-cause and cardiovascular disease mortality starts to increase at around 6–8 hours of sitting per day, when sitting time is self-reported. However, another meta-analysis14 with accelerometer-assessed sedentary time suggested that the threshold is slightly higher. Ekelund et al. 14 found that the dose–response relationship between sedentary time and all-cause mortality increased gradually from 7.5 hours of sedentary time per day to 9.5 hours per day, but increased sharply after this. For example, 10 hours and 12 hours of sedentary time were associated with a 1.48 and 2.92 higher risk of death, respectively, compared with 7.5 hours of sedentary time per day. For cardiovascular disease, an increased risk was observed for ≥ 10 hours of self-reported sedentary time per day. 8 It is important to note, however, that emerging evidence suggests that associations with all-cause and cardiovascular disease mortality are most pronounced in people who have lower levels of physical activity [i.e. people not achieving the recommended guidelines of at least 150 minutes of moderate or vigorous physical activity (MVPA) per week]. 12,15
In addition to physiological health outcomes, high levels of sedentary time have also been associated with cognitive function16 and mental health (e.g. anxiety,17,18 depression16,19,20 and a lower quality of life16,21). Although limited, in the workplace context there is some evidence to suggest that people with lower levels of sitting have higher work vigour/vitality (i.e. a subscale of work engagement),22,23 higher job performance22 and lower presenteeism. 24
Acute experimental evidence
Acute experimental research consistently shows that breaking up prolonged sitting with short (e.g. 2–5 minutes) but frequent (e.g. every 20–30 minutes) bouts of light-intensity physical activity (e.g. standing, walking, body weight exercises) over the course of a 6- to 8-hour time period reduces postprandial glucose, insulin, triacylglycerol and blood pressure, compared with prolonged sitting with no breaks. 25–28 However, the extent of the attenuation in these risk biomarkers has been shown to be dependent on weight, glycaemic and blood pressure status, sex, ethnicity and fitness level. 25–27,29,30 Females and individuals with a higher body mass index (BMI), impaired glycaemic status, of South Asian ethnicity and a low fitness level experience a worse metabolic response to prolonged sitting compared with their counterparts; however, these individuals also show a greater beneficial glucose and insulin response to regular light activity breaks. 25–27,29,30 Furthermore, the impact of the types of light activity breaks also appears to be dependent on certain characteristics and health markers of interest. For example, breaking up sitting with standing breaks has been shown to reduce glucose and insulin in overweight/obese individuals and individuals with impaired glucose, but not in healthy, normal weight individuals. 25
Prevalence of sedentary behaviour
Data gathered from large studies using accelerometer-based devices show that adults spend approximately 60% (≈9–10 hours/day) of their waking hours sedentary, a figure consistently reported across different countries. 31–33 Over the past 50 years, there has been an increase in sedentary occupations and a decrease in occupations involving MVPA. 34 Coupled with the fact that half of waking hours are spent at work, it is not surprising that working-age adults spend a large proportion of their waking hours and workday sedentary. For example, studies have shown that working-age adults spend between 60% and 70% of their waking day sedentary. 35,36 Likewise, while at work, studies have shown that adults spend around 60–70% of the workday sitting. 35,36 Furthermore, workdays tend to be more sedentary than non-workdays. 37–39
Evidence has also highlighted the key occupational groups that are more sedentary than others, and one such group is office workers. A recent systematic review and meta-analysis, including 132 studies, showed that office workers spend a higher proportion of their day sitting than workers in other occupations, both at work (office workers, 72.5%; other occupations, 49.7%) and during their waking time (office workers, 66.1%; other occupations, 55.9%). 35 Office workers have been shown to spend as much as 70–85% of their time at work sitting,36,40,41 and accumulate a large proportion (40–50%) of this time in prolonged, unbroken bouts. 40,41 These studies identify office workers as an important group for intervention.
Guidelines on sedentary behaviour
The increasing evidence base on the health implications of high levels of sedentary time, along with the now ubiquitous nature of sedentary behaviour, highlights the potential population health impact of this behaviour. This evidence has resulted in physical activity position statements and guidelines now including recommendations on reducing and/or regularly breaking up sedentary time. Examples of these statements and guidelines include the World Health Organization’s (WHO’s) WHO Guidelines on Physical Activity and Sedentary Behaviour,42 the US Physical Activity Guidelines Advisory Committee Scientific Report,7 UK’s Physical Activity Guidelines,43 The 2017 Dutch Physical Activity Guidelines,44 the Australian Government’s Physical Activity and Exercise Guidelines for all Australians45 and the Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. 46 Although the sedentary behaviour recommendation statements in these guidelines vary slightly by country, the general message is the same, that is to sit less and minimise prolonged sitting. Furthermore, in 2015, the first expert statement on sitting and standing in the workplace was published and recommended that workers should aim to spend 50% of their workday sitting and 50% upright. 47
Interventions targeting sitting in the workplace
In 2018, an updated systematic review was published, summarising the effectiveness of workplace interventions for reducing sitting time at work. 48 The interventions included physical workplace changes, such as providing height-adjustable desks to enable sitting or standing at work, pedalling workstations and treadmill desks, policy changes, information provision, counselling and computer prompts. Providing height-adjustable desks was the most frequently implemented intervention and was reported as the most promising for reducing sitting time at work, leading to reductions of 100 minutes per workday in the short term (up to 3 months) and 57 minutes per workday in the medium term (3–12 months). Although positive findings were observed, the quality of the evidence was deemed to be very low to low because of a lack of non-biased cluster randomised controlled trials (RCTs), small sample sizes (the majority had 20–50 participants) and a lack of longer-term follow-up. The review by Shrestha et al. 48 highlighted the need for larger cluster RCTs with long-term follow-up.
Our previous intervention: Stand More AT Work
To tackle the high levels of sitting exhibited by office workers, our group developed the Stand More AT Work (SMArT Work) intervention. To address the limitations of previous evaluations, we tested effectiveness of the SMArT Work intervention through a cluster RCT, with follow-up at 3, 6 and 12 months.
The SMArT Work intervention was developed following 12 months of development work, involving focus groups with office workers and managers. 49 The intervention consisted of a brief (≈30 minutes) group-based face-to-face education session, delivered by a member of the research team, which covered evidence on the health consequences of high levels of sitting and prolonged sitting, as well as the health benefits of regular breaks in sitting. At the end of the session, attendees received objective feedback on their own sitting time [collected from an activPAL device (PAL Technologies Ltd, Glasgow, UK) at baseline], which they used to set an action plan and goals to reduce and break up their sitting at work. Attendees were also given an educational leaflet that summarised the key health messages of the group education session, as well as tips for reducing sitting at work. Following the education session, participants received a height-adjustable desk or desk platform (they had the choice within a certain budget of a desk/platform that best suited their office space), with a demonstration from a researcher on how to use it and information on the correct sitting and standing postures while working. This education session was reinforced with a leaflet, which also presented the expert recommendations on how often to change posture (i.e. from sitting to standing and vice versa) during a working day. The recommendations were based on recommendations published by members of our group. 47 Participants were also provided with a Darma smart cushion (Darma Inc., California, USA). The Darma smart cushion was placed on the office chair to track sitting time and to provide feedback on sitting time and prolonged sitting (i.e. bouts ≥ 30 minutes), via a mobile phone application (app). Within the app, participants could (via a user-defined setting) also set the cushion to vibrate following a prolonged sitting bout. The Darma smart cushion provided the participants with an objective self-monitoring device with a participant-determined prompt. Participants were also given posters with messages that were designed to act as a motivator to reduce sitting (and these posters were developed during focus groups). New posters were provided to participants every 3 months. Following each follow-up measurement session, intervention participants were provided with feedback on their sitting time from the activPAL device, which displayed how this time compared with baseline. Every 3 months, participants also received a brief coaching session with a member of the research team, either face-to-face or over the telephone, to discuss progress and barriers and to review goals and action plans.
In the cluster RCT of the SMArT Work intervention,50 at 12-month follow-up, we found that participants who received the SMArT Work intervention sat for 83 minutes less per day during work hours than participants in the control group. 41 The intervention appeared to have many benefits, which included job performance, work engagement, occupational fatigue, sickness presenteeism and quality of life. Despite this success, the process evaluation and results indicated that multiple improvements could be made to maximise both behaviour change and benefits, and this led to the creation of the SMART Work & Life (SWAL) programme, which is an adapted and extended version of the SMArT Work intervention.
Adaptation of the SMArT Work intervention into SMART Work & Life
Based on the RCT results of the SMArT Work intervention, the process evaluation and stakeholder input, we decided on the following adaptations to the SMArT Work intervention for the creation of SWAL:
-
The sitting results from the activPAL device indicated that although participants significantly reduced sitting time at work, the sitting reductions observed for overall daily sitting time suggested that these reductions were driven solely by changes at work and not at home (i.e. no changes were made outside work). These results, therefore, indicated that a whole-day approach to encourage reductions in sitting time was needed, rather than focusing solely on workplace sitting. To reflect this, the SMArT Work intervention was renamed the ‘SMART Work & Life’ intervention and the intervention targeted siting at work and in leisure time.
-
The intervention strategies in the SMArT Work intervention were delivered by a researcher. To enhance sustainability within the workplace, and the scalability of the intervention, workplace champions were trained to facilitate the delivery of the SWAL intervention to participants.
-
In the SMArT Work intervention, participants ranked the brief group-based education session highly in terms of usefulness, increasing awareness and motivating behaviour change, but felt that the session should be longer to cover topics in more detail and allow more time for discussion and sharing. For the SWAL intervention, the initial education session was extended to include possible sitting reduction strategies, barriers faced and overcoming barriers. Furthermore, follow-up group sessions were included to revisit key messages, discuss progress, brainstorm strategies, share what was working and discuss barriers and solutions. Following stakeholder engagement, it was felt that workplace champions would not feel comfortable delivering the initial, more detailed, education session and so this was adapted to an online interactive education session, with the workplace champion facilitating the face-to-face group follow-up sessions, which were less formal.
-
In the SMArT Work intervention, participants felt that the goal-setting and action-planning booklet was too structured and time-consuming. Goal-setting and action-planning was, therefore, revised into a one-page leaflet for the SWAL intervention.
-
Although some participants found the Darma cushion helpful, many struggled with setting up the device on their mobile phones and regular charging was also seen as a barrier. Furthermore, the cushion assisted with only workplace sitting and not overall sitting. In addition, the cushions were also expensive. In the SWAL intervention, the self-monitoring and prompt tools recommended were freely available mobile phone apps, timers and computer software, and this reduced costs and offered participants a choice of options. The online education session in the SWAL intervention included a section on the importance of self-monitoring and prompt tools, and provided step-by-step guides for each of the tools suggested.
-
Participants felt that social support and competitions should be encouraged and facilitated more within the SMArT Work intervention and, therefore, regular sit less and move more challenges were incorporated and facilitated by the workplace champions in the SWAL intervention.
-
Participants valued having progress sessions in the SMArT Work intervention and suggested more ongoing contact and support throughout the programme. As well as the face-to-face group follow-up sessions that were incorporated into the SWAL intervention, the workplace champions also sent out monthly e-mails.
-
There was a lack of management buy-in during the SMArT Work intervention and it was felt that separate educational information was needed for managers.
More details about the SWAL programme can be found in the methods chapter (see Chapter 2).
Building on existing research
The SWAL intervention and its evaluation will advance the current evidence by:
-
being fully powered to detect differences between groups in sitting time (i.e. addresses limitations identified by Shrestha et al. 48)
-
having a robust cluster randomised controlled design (i.e. addresses limitations identified by Shrestha et al. 48)
-
emphasising a ‘whole-day’ preventative approach rather than just focusing on workplace sitting (to address no/limited behaviour change observed outside work hours) and having daily sitting time as the primary outcome
-
incorporating behaviour change maintenance strategies (to prevent the decline in positive behaviour change over the longer term)
-
improving scalability of the intervention by training workplace champions to facilitate intervention delivery, supplemented with online education and freely available self-monitoring and prompt tools
-
including two intervention arms to investigate how important providing a simple, but fairly expensive, environmental change (i.e. height-adjustable workstation) is for reductions in sitting
-
including a cost-effectiveness analysis.
Aims and objectives
The main aim of the study was to evaluate the effectiveness and cost-effectiveness of the SWAL intervention (provided with and without a height-adjustable workstation) in a sample of desk-based workers. If both interventions were shown to be effective in comparison with the control group, then a secondary aim would be to determine if one intervention were more effective and cost-effective than the other.
Primary objective
-
To investigate the impact of the SWAL intervention, delivered with and without a height-adjustable workstation, on device-assessed daily sitting time compared with usual practice at 12 months’ follow-up.
Secondary objectives
-
To investigate the impact of the SWAL intervention, delivered with and without a height-adjustable workstation, over the short term (assessed at 3 months) and longer term (assessed at 12 months) on:
-
daily sitting time across any valid day (3 months) and on workdays and non-workdays
-
sitting time during work hours
-
daily time spent standing and in light physical activity and MVPA across any valid day, during work hours and on workdays and non-workdays
-
daily time spent stepping and number of steps across any valid day, during work hours and on workdays and non-workdays
-
markers of adiposity (i.e. BMI, per cent body fat, waist circumference)
-
blood pressure
-
blood biomarkers [i.e. fasting glucose, cholesterol, triglycerides, glycated haemoglobin (HbA1c)]
-
musculoskeletal health
-
psychosocial health (i.e. fatigue, stress, anxiety and depression, well-being and quality of life)
-
work-related health and performance (i.e. work engagement, job performance and satisfaction, occupational fatigue, presenteeism, sickness absence)
-
sleep duration and quality.
-
-
To undertake a full economic analysis of the SWAL programme.
-
To conduct a mixed-methods process evaluation throughout the intervention implementation period (using qualitative and quantitative measures) with participants and workplace champions and to provide insights into the ways in which, and the extent to which, the intervention was implemented, as well as participant experiences of the intervention.
Chapter 2 Methodology
Study design
Shrestha et al. 48 published an updated systematic review on workplace interventions for reducing sitting time at work. The provision of height-adjustable desks was the most frequently used physical change to the workplace from the included studies, and also reported the highest reductions in sitting time at work. However, this systematic review highlighted the lack of non-biased RCTs and studies with larger sample sizes with long-term follow-up. This SWAL trial was a three-arm cluster RCT with a cost-effectiveness analysis and a process evaluation. The SWAL trial was registered with the International Standard Randomised Controlled Trial Number registry prior to recruitment (URL: www.isrctn.com/ISRCTNISRCTN11618007; accessed 6 October 2020). The trial protocol was published in September 2018,1 and the protocol revisions can be accessed via the NIHR Journals Library (URL: www.journalslibrary.nihr.ac.uk/programmes/phr/164104/#/; accessed 6 October 2020). A summary of the amendments to the protocol are listed in Table 1. A more detailed statistical analysis plan was subsequently signed off before the data analyst had access to the data (see Appendix 1).
| Amendment number | Date approved | Change to protocol |
|---|---|---|
| SA1 | 21 February 2018 | Blood tests to be completed in fasting state |
| SA2 | 9 April 2018 | Additional questionnaires added Clarification of inclusion criteria (0.6 FTE) Clarified job descriptive data to be collected Different point-of-care devices used for blood testing |
| SA3 | 15 June 2018 | Addition of Liverpool City Council Support and strategies for sitting less to be collected at baseline for both intervention and control groups Group catch-up sessions to be voice recorded rather than observed face to face |
| SA4 | 19 March 2019 | Change to recording of adverse events to record only those adverse events that are related to or may impact on the study intervention/outcomes |
| SA5 | 4 September 2019 | The size and number of clusters recruited was different from the anticipated number, therefore, the sample size was updated to reflect this. Dropout rate/non-compliance with activPAL device was increased to 40% |
| SA6 | 28 October 2020 | Owing to the COVID-19 pandemic, 24-month data collection was removed, as it was no longer viable to conduct. Therefore, 12-month data were to be used as the primary end point instead |
Local councils in Leicester, Leicestershire, Greater Manchester and Liverpool, UK, were the target organisations, with defined offices/departments/teams as the clusters and randomised to one of the following three conditions: (1) SWAL only, (2) the SWAL intervention with the addition of a height-adjustable workstation (i.e. SWAL plus desk) or (3) the control group, which continued with usual practice. Outcome measures were assessed at baseline, with follow-up assessments at 3 and 12 months. The study had originally planned to carry out assessments at 24-month follow-up; however, owing to the COVID-19 pandemic, we were unable to complete these assessments. Therefore, the primary end point was revised to 12 months and 12-month data collection was completed by the end of February 2020. The study methods are reported in accordance with the CONSORT (Consolidated Standards of Reporting Trials) statement for cluster RCTs.
Ethics approval and research governance
Ethics approval was obtained from the University of Leicester’s College of Life Sciences representatives and the University of Salford’s Research Enterprise and Engagement Ethics Approval Panel before the commencement of the study. The University of Leicester sponsored the study. All staff and students working on the study completed Good Clinical Practice training. An independent Data Monitoring and Ethics Committee (DMEC) and Trial Steering Committee (TSC) were appointed and met every 6 months during the study. The DMEC included an independent chairperson, one independent academic and a statistician. The TSC included the principal investigator, an independent chairperson, three independent academics (including a statistician) and two council representatives.
Council and participant recruitment
Council recruitment
To recruit councils, we approached contacts at local councils in Leicester, Leicestershire, Greater Manchester and Liverpool to introduce the study. These contacts were from the public health or physical activity and sports departments within each council. After initial meetings and discussions, the study was presented to the respective senior management teams in each council for approval (see Appendix 2 for specific contact and approval details for each participating council).
Participant recruitment
Participants were recruited from the following participating councils: Leicester City Council, Leicestershire County Council, Salford City Council, Bolton Council, Trafford Council and Liverpool City Council. Research teams were based at two study sites in Leicester and Salford. The Leicester research team was responsible for recruitment and data collection at Leicester City Council and Leicestershire County Council, and the Salford research team was responsible for recruitment and data collection at the Greater Manchester councils (i.e. Salford City Council, Bolton Council and Trafford Council) and Liverpool City Council.
Councils were provided with recruitment material to advertise the study (e.g. posters to display on employee noticeboards and wording to include in council communications); however, recruitment strategies were informed by the individual councils themselves (see Appendix 3). All study-related communications disseminated by the councils (e.g. via staff e-mails, staff intranet and weekly newsletters) stipulated that the study sought to recruit office-based employees who spent most of their day sitting. In three of the councils (i.e. Leicester City Council, Salford City Council and Bolton Council), participants were also invited to a briefing event led by a member of the research team. At each briefing event, potential participants were given a participant information sheet and received a detailed presentation about the study, the data collection procedures and the requirement of being involved in the study. At the end of each briefing event, employees were asked to complete an information form and a reply form, which were used to assess eligibility and to identify potential clusters. Participants were grouped into clusters either by a shared office space (could be made up of different teams/departments) or if they were members of the same team but split into different office spaces. To aid cluster development, in the initial stages of recruitment, interested individuals were also encouraged to promote the study within their team to ensure the cluster met the minimum quota of four or more participants prior to randomisation.
To be eligible, each cluster was also required to have at least one participant willing to undertake the role of workplace champion for the cluster if they were to be allocated to one of the intervention arms. Participants were asked to indicate whether or not they would be interested in becoming a workplace champion on the reply form and were, therefore, self-selecting.
Cluster and participant eligibility
Visits to all councils were conducted during the study set up and prior to data collection to understand the different buildings, office locations and set ups, and to inform the definition of a cluster and assist with grouping participants into clusters.
Cluster inclusion criteria
A cluster was required to have four or more participants, including one or more participants who had volunteered to act as the workplace champion. There was no maximum number of participants.
Participant inclusion criteria
Participants were required to meet the following inclusion criteria:
-
office based, aged ≥ 18 years and employed by one of the participating councils
-
spend the majority of their day sitting (self-reported)
-
work for the council at least 60% full-time equivalent
-
willing and able to give informed consent to take part in the study
-
able to walk without the use of an assistive device or requiring assistance form another person.
Participant exclusion criteria
Participants were not able to enter the study if any of the following criteria applied:
-
currently pregnant
-
already using a height-adjustable workstation at their primary work location
-
unable to communicate in English
-
unable to provide written informed consent.
Informed consent
All participants received a copy of the participant information sheet no less than 24 hours before attending a baseline data collection session. At the baseline session, the study details were verbally reiterated, including full details of study procedures, expectations and right to withdraw, and this was carried out by a member of the research team who was suitably qualified and who was authorised to do so by the principal investigator. Written informed consent was obtained prior to any measures being taken.
Allocation arms
Intervention arms
Intervention description
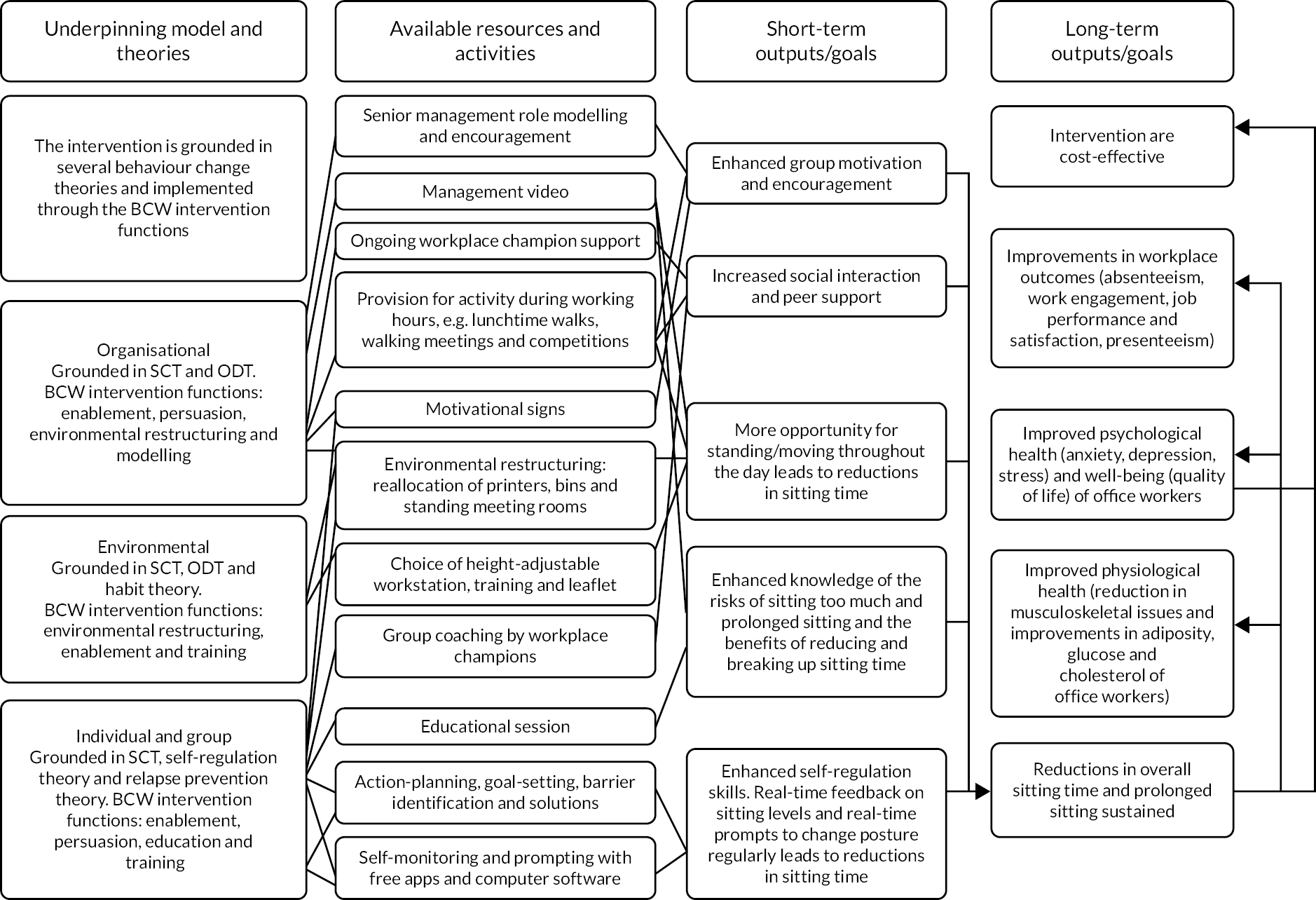
The SWAL intervention is a multicomponent intervention that aims to reduce daily sitting time in office workers. The SWAL intervention is grounded in several behaviour change theories, including social cognitive theory,51 organisational development theory,52 habit theory,53 self-regulation theory54 and relapse prevention theory. 55 The SWAL intervention promotes positive behaviour change through a range of multifaceted strategies (e.g. organisational, environmental, and individual and group). Each of the intervention strategies draws on the principles of the Behaviour Change Wheel and the associated COM-B (Capability, Opportunity, Motivation, Behaviour) approach,56 specifically behaviour guided by the provision of ‘capability’, ‘opportunity’ and ‘motivation’. The logic model summarises the underpinning model, theories and Behaviour Change Wheel intervention functions of the SWAL intervention (Figure 1).
FIGURE 1.
The SWAL intervention logic model. BCW, Behaviour Change Wheel; ODT, organisational development theory; SCT, social cognitive theory.
Organisational strategies
During the study set-up phase, management buy-in at each of the councils was sought. Support of senior leaders was secured through a series of business case documents and videos, which articulated the importance of reducing employee sitting behaviours, the positive impact this may have on workplace culture and how this may be achieved without disrupting performance and productivity. The programme was also delivered within each cluster in the intervention arms via workplace champions. Workplace champions were all council employees who were enrolled as participants in the study. Workplace champions were invited to attend a 3-hour training session before undertaking the role. The training session was designed to equip workplace champions with the skills and knowledge to implement the intervention. The training programme was designed and delivered by an experienced behaviour change education team and comprised the following eight sessions:
-
Introduction, housekeeping, expectations and concerns
-
SWAL study overview
-
SWAL champions roles and responsibilities
-
Group facilitation – opportunity to practice
-
Intervention fidelity
-
Assessing confidence to be a SWAL champion
-
Next steps
-
Revisiting expectations and concerns.
Following attendance at the training, workplace champions were provided with an electronic folder containing intervention resources, as described in the following sections, and a timeline of implementation (see Appendix 4). (Note that the programme was designed to be delivered over a 24-month period, but was cut short because of the COVID-19 pandemic.)
Environmental strategies
The intervention promoted the small-scale restructuring of the office environment (e.g. relocation of printers, wastepaper bins) to encourage more frequent movement around the office. Participants were also encouraged to think about their home environment. Motivational reminders were embedded into the office environment in the form of visual posters, as well as in a range of computer-based apps (for use both in the office and at home). Behavioural modelling, in the form of the internally based workplace champions, served to demonstrate positive examples within the context of the working environment. The workplace champions circulated monthly e-mails to participating colleagues, the contents of which varied between motivational prompts, hints and tips, and educational material.
Clusters in the second intervention arm also received a height-adjustable workstation that would allow them to transition between sitting and standing postures while working. Participants were able to select their preferred workstation from the following four models: Deskrite 100 (Posturite Ltd, Berwick, UK), Yo-Yo Desk Mini (Sit-Stand Trading Ltd, Swindon, UK), Yo-Yo Desk 90 (Sit-Stand Trading Ltd) and Yo-Yo Desk Go 1 (Sit-Stand Trading Ltd). In addition, participants could choose which colour they preferred (i.e. black or white). All height-adjustable workstations were designed to sit on top of the existing workstation. The desks were delivered to the councils and the facilities team within the councils and/or the study team installed the workstations. Participants were provided with instructions on how to use the equipment appropriately when in the sitting and standing positions.
Individual and group strategies
The intervention included an initial interactive online education session that emphasised the adverse health consequences of excessive sitting and reinforced the benefits of breaking up sitting time and reducing overall sitting time. The session also encouraged participants to estimate their own sitting time at work and at home, encouraged participants to think about strategies to reduce and break up sitting time at work and at home, provided a range of ideas to reduce and break up sitting time at work and at home, and covered barrier identification, goal-setting and the importance of self-monitoring and prompts for behaviour change. Participants were encouraged to download the suggested free smartphone-enabled apps and computer software/extensions and were provided with downloadable ‘how to’ guides. At the end of the education session, participants could download a range of resources, including posters, top tips and an action plan and goal-setting sheet. The workplace champions were responsible for providing participants with a link to the online education session, sending out monthly e-mails (templates were provided), setting sitting less challenges and organising and facilitating group catch-up sessions. Group catch-up sessions were an opportunity for participants to collectively review key messages, brainstorm ideas, discuss any barriers to and facilitators of reducing sitting time, and develop new goals and action plans (an agenda was provided to workplace champions). A copy of the agendas for each session can be found in Appendix 5.
Control arm
Participants in the control arm carried on with their usual working practices. Participants were provided with their results from the baseline and follow-up visits in terms of their anthropometrics, blood pressure and blood biomarkers, and this was the same as the participants in the two intervention arms.
Randomisation
Eligible clusters were randomised to a study arm once all members of the office group had completed the baseline measurements. Randomisation was conducted by a statistician from the Leicester Clinical Trials Unit using a pre-generated list. The statistician was blinded to any identifiable cluster features, with all clusters represented by a unique cluster ID. Randomisation was stratified by area (Leicester: Leicester City Council and Leicestershire County Council; Salford: Salford City Council, Bolton Council, and Trafford Council; Liverpool) and cluster size [small (< 10 people); large (≥ 10 people)]. The study team was responsible for coordinating the deployment of the intervention to workplace champions and were, therefore, unable to be blinded to allocation arm. Likewise, owing to the nature of the intervention, participants were unable to be blinded to the assigned intervention arm.
Sample size
Original sample size
Initial power calculations showed that with a total sample size of 420 participants and 10 clusters per intervention arm the study would have over 90% power to detect a 60-minute difference in average daily sitting time with a two-tailed significance level of 5%. The calculations assumed a standard deviation (SD) of 90 minutes,57 a conservative intraclass correlation coefficient (ICC) of 0.05,58 a coefficient of variation to allow for variation in cluster size of 0.54 (cluster size range of 15–45) and an average cluster size of 20 participants (based on data from councils that were interested in taking part). The trial was designed to test two intervention arms independently with the control arm, and so to keep an overall significance level of 5% the number of clusters was inflated by a factor of 1.23. 59 The sample size was also inflated by 30% to allow for potential individual loss to follow-up and non-compliance with wearing the activPAL (i.e. the device to assess the primary outcome). A further inflation was applied to allow for one whole cluster drop out per intervention arm. Therefore, the total proposed sample size was 660 participants to be recruited from 11 clusters per intervention arm (i.e. 33 clusters in total). The sensitivity of power was assessed against alternative ICC values of 0.021 and 0.10. 57,58 Adequate power for RCTs is accepted as 80%, and with these ICCs the power was above the required level at 98% and 81%, respectively. In addition, the calculations were based on a similar trial that used an ICC of 0.021 for daily sitting,57 although we chose a more conservative ICC of 0.05.
Re-estimated sample size
At the start of recruitment, the observed average cluster size and variability of cluster sizes were different from those assumed in the original sample size calculation. With the DMEC’s guidance, the sample size was recalculated to ensure that the study was adequately powered. Changing the average cluster size from 20 to 10, the variability in cluster size from 0.54 to 1.42 (cluster size range of 4–38) and the inflation for loss to follow-up and non-compliance with wearing the activPAL device from 30% to 40%, while keeping all other assumptions the same, required 690 participants from 72 clusters.
Study outcome measures
This section defines the primary and secondary study outcomes, and each of the study outcome measures, and when they were assessed, are listed in Appendix 6. The process evaluation methods are detailed in the subsequent section (see Process evaluation methods), and a summary of the sequence and timing of the outcome and the process evaluation measures is shown in Table 2 using a PaT plot. 60 Study measurements were taken at the participants’ place of work by trained researchers. The questionnaire booklet was provided to participants during the face-to-face measurement session; however, participants could take the booklet away with them to complete it in the week following the measurement session, and return the completed booklet at the same time as the activPAL and Axivity (Axivity Ltd, Newcastle upon Tyne, UK) devices.
| Timeline | Study arm | ||
|---|---|---|---|
| Control | SWAL only | SWAL plus desk | |
| Baseline | a , b , c | a , b , c | a , b , c |
| Randomisation | |||
| 3 months | a , b , c , e , f | a , b , c , e , f , g | a , b , c , e , f , g |
| 9 months | g | g | |
| 12 months | a , b , c , f , h | a , b , c , e , f , h , i | a , b , c , e , f , h , i |
| 15 months | g | g | |
Primary outcome
The primary outcome was average daily sitting time across any valid day, measured using the activPAL device, at 12-month follow-up (the primary end point was originally 24 months; however, this was changed to 12 months because of the COVID-19 pandemic).
Accelerometer-measured daily sitting time
The activPAL3 micro device (PAL Technologies Ltd, Glasgow, UK) was used to assess the primary outcome. The activPAL device is capable of distinguishing between sitting/lying, static standing, stepping time and transitions between sitting and standing. 61 At each assessment point, participants were asked to wear the device continuously (i.e. 24 hours/day) for 8 days (i.e. 7 full days plus the assessment day). Using the default manufacturer settings, the activPAL was initialised to record at a sampling frequency of 20 Hz. The device was waterproofed with a nitrile sleeve and applied (by the participant) to the midline anterior aspect of the thigh using a Hypafix transparent dressing (BSN Medical, Germany). Participants were asked to complete a log of the times they got into bed, went to sleep, woke up and got out of bed, as well as indicating which days were workdays and which days were non-workdays, and the start and finish times of each workday during the activPAL wear period. Participants were also asked to indicate whether or not each day was a typical day and if it was not a typical day to the reason why this was the case. In addition, participants were asked to note any times that they removed the device and why. Following completion of the wear period, the devices were collected by the research team, downloaded and visually checked for adequate wear. Where valid data were not obtained, participants were asked to repeat the wear period. Participants who provided an adequate number of valid days received £10 voucher at the end of each data collection time point.
Secondary outcomes
If both interventions were shown to result in a lower daily sitting time than the control arm (i.e. the primary objective), then a secondary objective was to determine if one intervention was more clinically effective and cost-effective than the other. In addition, other secondary objectives were to investigate whether the SWAL intervention with or without a height-adjustable desk (assessed at both 3 and 12 months) led to differences in a range of secondary outcomes, as detailed in the next section.
Secondary activPAL variables
Variables were derived by calculating the average across the number of valid days. The below variables were analysed for the following four different time periods: (1) daily variables (i.e. all waking hours) on any valid day, (2) variables during work hours, (3) daily variables on workdays and (4) daily variables on non-workdays:
-
average sitting time (minutes): total accumulated (3 months) and in prolonged bouts lasting ≥ 30 minutes
-
average standing time (minutes): total accumulated
-
average stepping time (minutes): total accumulated, as well as at a step cadence threshold of 100 steps per minute (in bouts lasting ≥ 1 minute)
-
average number of steps
-
average number of transitions from sitting to an upright posture.
The below variables were also summarised descriptively at each time point and time period:
-
average number of valid days
-
average waking wear time (minutes)
-
average percentage of the day spent sitting
-
average percentage of the day spent standing
-
average percentage of the day spent stepping
-
average percentage of total sitting time spent in prolonged sitting time.
Axivity
Participants were also asked to wear a wrist-worn accelerometer (Axivity AX3; Axivity Ltd) on their non-dominant wrist for 24 hours a day for same 8 days as the activPAL device so that different intensities of physical activity, as well as sleep duration and efficiency, could be calculated. Axivity monitors were initialised with a sampling frequency of 100 Hz, and a dynamic range of ±8 g. Participants were asked to note any time they removed the device on the same log used for the activPAL device.
Anthropometrics and blood pressure
Participants were asked to remove shoes, socks and any outer clothing prior to anthropometrics being taken. Height was measured using a portable stadiometer (Seca Ltd, Birmingham, UK) and recorded to the nearest millimetre. Body weight (kg) and body composition was assessed using the Marsden MBF-6000 Scales (Marsden Weighing Machine Group Ltd, Rotherham, UK) and included measures of weight, BMI and fat percentage. A clothing allowance of 1.5 kg was entered into the scales, along with the participants’ age, gender and height. Waist circumference (cm) was recorded to one decimal place using a standard anthropometric measuring tape (Seca Ltd). Blood pressure was taken using an Omron M3 automated blood pressure monitor (Omron Healthcare Inc., Kyoto, Japan). The participants sat quietly for 5 minutes before three measures of blood pressure were taken, with 1-minute intervals between each measure. The final two measures were used to form an average.
Biochemical measures
Point-of-care testing included measures of HbA1c, cholesterol [i.e. high-density lipoprotein (HDL), low-density lipoprotein (LDL) and total], triglycerides and fasting blood glucose. Capillary blood samples were collected via the finger-prick method while in a fasted state (fasted for 10 hours). A Quo-Test HbA1c analyser (EKF Diagnostics, Cardiff, UK) was used to measure levels of HbA1c and CardioChek Plus (PTS Diagnostics, Indianapolis, IN, USA) for cholesterol triglycerides and glucose.
Self-reported sitting behaviours
Self-reported sedentary behaviours were assessed using an adapted version of the Occupational Sitting and Physical Activity Questionnaire. 62 Participants were asked to estimate the hours that they spent sitting and breaking up sitting during the workday,63 and the percentage of time they spent in the office and what percentage they were based at their desk during the workday. The Past Recall of Sedentary Time questionnaire was used to assess time spent in sedentary behaviours outside work hours in different contexts. 39
Musculoskeletal health
The Standardised Nordic Questionnaire (SNQ), a self-reported measure of musculoskeletal pain, was used to measure musculoskeletal symptoms. 64
Self-report sleep
The Pittsburgh Sleep Quality Index65 was used to assess sleep duration and sleep quality. The Pittsburgh Sleep Quality Index65 consists of four questions relating to sleep duration, plus a further seven questions, measured on a four-point Likert scale, relating to sleep quality.
Mental health, well-being and quality of life
A range of measures were used to assess mental health. Anxiety and depression symptoms were assessed using the Hospital Anxiety and Depression Scale,66 which is a 14-item questionnaire, with seven items relating to anxiety and seven items relating to depression. Responses were scored on a scale of 0–3, with maximum scores of 21 for anxiety and for depression. Participants were also asked to rate their responses to the Perceived Stress Scale (PSS). 67 Measured on a five-point Likert scale, the scores from the PSS were obtained by reverse scoring the four positively stated items (items 4, 5, 7 and 8) and them summing across all scale items. Higher scores on the PSS indicate higher levels of stress. Emotion was assessed via the Positive and Negative Affect Schedule. 68 The Positive and Negative Affect Schedule is a 20-item questionnaire, with 10 items relating to positive emotions and a further 10 items relating to negative emotions. All items were measured on a five-point Likert scale, with separately summed scores for both positive and negative emotions.
The WHO-5 Wellbeing Index was used to measure psychological well-being. 69 The WHO-5 Wellbeing Index consists of five statements (e.g. ‘I have felt calm and relaxed’), with responses marked on a six-point scale. Responses were summed (range of 0–25) and scores were converted to a well-being index (0–100) by multiplying the summed total by four. Higher scores on the WHO-5 Wellbeing Index indicate greater well-being. Health-related quality of life (HRQoL) was measured using The EuroQol-5 Dimensions, five-level version (EQ-5D-5L). 70,71 The EQ-5D-5L is a two-part questionnaire. The first part generates a ‘health state’, based on participant responses to each of five health dimensions (i.e. mobility, self-care, usual activities, pain/discomfort, anxiety/depression). The ‘health state’ score ranges from 1 to –0.285, where ‘1’ signifies perfect health, ‘0’ death, and negative values have been described as ‘states worse than death’. 72,73 The second part, which asks participants to rate their overall health on a visual analogue scale, is scored between 0 and 100, where higher scores represent greater overall health.
Physical and mental fatigue
The Fatigue Scale,74 an 11-item scale, was used to assess both mental and physical fatigue. The Fatigue Scale is measured on a four-point Likert scale, with total scores ranging between 0 and 33. Higher scores on the Fatigue Scale indicate greater fatigue.
Work-related health and performance
A range of measures were used to assess work-related health. Both job performance75 and job satisfaction76 were assessed using single-item scales. (i.e. How satisfied are you with your job in general?/How well do you think you have performed in your job recently?) Each question was scored on a seven-point Likert scale where higher scores indicated greater performance/satisfaction. The Utrecht Work Engagement Scale (UWES)77 was used to measure work engagement, which consists of nine items. Each item was scored on a seven-point scale and responses were summed to provide an overall score. Higher scores represent higher work-related engagement. Occupational fatigue was measured using the Need for Recovery Scale. 78 Using the Need for Recovery Scale, participants indicated yes or no to 11-item statements (e.g. ‘I find it hard to relax at the end of a working day’).
The Work Limitations Questionnaire was used to measure sickness presenteeism. 79 The Work Limitations Questionnaire comprises eight self-rated questions, measured on a Likert scale. Two items (physical demands) were reversed scored. Responses were converted to percentages (where 0 = limited none of the time and 100 = limited all the time). The demands, control and support scales from the Health and Safety Executive Management Standards Indicator Tool80 were used to establish participants’ perceptions of workload and relations. Sickness absence information was collated via self-report at each assessment point. Absenteeism data were also collected directly from the employer, including duration and frequency of sickness absence 12 months prior to the study, as well as the 12-month study duration.
Social norms, cohesion and support for sitting less
Organisation social norms (e.g. ‘My workplace is committed to supporting staff choices to stand or move more at work’) were assessed via an eight-item questionnaire,57 rated on a five-point Likert scale (from ‘strongly disagree’ to ‘strongly agree’). The ‘social community’ subscale of the Copenhagen Psychosocial Questionnaire-II,81 a three-item questionnaire, using six-point Likert scales, was also used to assess organisational cohesion and support.
Dietary behaviours and alcohol consumption
Questions from the Whitehall II Study82 were used to gather data on dietary behaviours, including snack frequency, frequency of soft drink consumption, fruit and vegetable consumption and alcohol intake.
Health-related resource use
Data on the use of health-related resources were gathered at each assessment point. Participants were asked to provide information on quantity and duration of general practitioner (GP) and nurse practitioner visits, inpatient and outpatient appointments, and visits with other relevant health professionals.
Strategies used to sit less and move more often
Participants were asked to report the frequency of strategies used to reduce sitting behaviours and move more often. 83
Workplace champion characteristics
Workplace champions were asked to complete a questionnaire to collect data on their gender, date of birth, ethnicity, highest level of education, if they supervise staff, how long they have worked at the council, hours worked per week and whether or not they had been a workplace champion at the council previously.
Workplace audit
A cluster representative or a workplace champion was asked to complete an audit of their work environment. Questions related to if the participant’s building had open or closed plan offices or both, hot desking and what the physical environment (e.g. gym access, communal and meeting space with high tables to stand, centrally located bins, information on sitting less displayed) and cultural/policy environment (e.g. written policies on supporting staff to be active, support walking meetings) included.
Accelerometer data processing
activPAL data processing
activPAL data were processed by the principal investigator (blinded). Data were cleaned and processed using a freely available software app called Processing PAL version 1.3 [University of Leicester, Leicester, UK; URL: https://github.com/UOL-COLS/ProcessingPAL (accessed 6 December 2022)]. The validated algorithm in this app separates valid waking wear data from everything else (e.g. time in bed, prolonged non-wear and invalid data). 84 Once data were processed, heat maps were created of the valid waking wear data and invalid data and visually checked for any occasions where the algorithm had misclassified waking wear data, and vice versa. On any such occasion (e.g. early wake time on one day vs. the rest, or early or late sleep time on one day vs. the rest), the self-reported wake and sleep times were compared with the processed data and if this confirmed misclassification then data were corrected. Self-reported logs were also checked for scenarios where data should be removed, for example if the participants removed the device for swimming or it was not a typical day (e.g. some council employees reported working on election days where they had to stand and walk all day). Once this process was completed, summary variables were calculated. A valid activPAL wear day was defined as having ≥ 10 hours wear time per day,85 ≥ 1000 steps per day and < 95% of the day spent in any one behaviour. The first day of data collection was excluded.
To generate data during work hours only, the self-reported start and end of work times for each workday were entered into an excel sheet and uploaded to the Processing PAL app. The Processing PAL app automatically calculated the variables of interest during these specific dates and times. Short (≤ 5 hours) wear time during work hours and long (≥ 12 hours) wear time during work hours were checked against the self-reported logs. A work hours data set was considered valid if it had ≥ 3.5 hours.
Axivity data processing
Axivity data were downloaded in.cwa format using OmGui software (OmGui version 1.0.0.43, Open Movement, Newcastle upon Tyne, UK). All data files were processed through R package GGIR version 1.9-0,86 using R version 4.0.2 (The R Foundation for Statistical Computing, Vienna, Austria). The initial processing of the raw data in GGIR corrects for gravity, periods of non-wear and calculates the vector magnitude of acceleration (Euclidean Norm minus 1 g), using local gravity as a reference and averaged over 5-second epochs. 87 A valid day of daily data was defined as >16-hour detected wear within a 24-hour window, or where there was detected wear for each 15-minute period over a 24-hour cycle. 88 A workday data set was considered valid if it had ≥ 3.5 hours. To generate outcome variables based on a complete 24-hour cycle, the default non-wear setting in GGIR was used. Briefly, invalid data were replaced with mean acceleration values for similar time points from different days for each participant. 88 Acceleration thresholds for light physical activity and MVPA were 40–100 mg and >100 mg (where 80% of a 60-second window exceeded 100 mg). 89
Sleep metrics were derived using an estimated sleep period time window based on sustained inactivity bouts. Estimated arm angles were averaged over 5-second epochs and treated as sustained inactivity/potential sleep periods if the angle change was < 5° over a rolling 5-minute window. 88 The first and last night were removed because of the recording period starting and ending at midnight, likely meaning only part of the sleep window would have been captured. Visual reports were generated and compared for accuracy against participant diaries. Obvious inaccuracies in the predicted sleep window based on viewing the data resulted in the removal of the window altogether. 88
The variables below were derived by calculating the average across the number of valid days. The variables were analysed in the following four different time periods unless specified: (1) daily variables on any valid day, (2) variables during work hours, (3) daily variables on workdays and (4) daily variables on non-workdays. The variables were as follows:
-
average time spent in light physical activity (minutes)
-
average time spent in MVPA (minutes) in 1-minute bouts
-
average sleep duration (minutes) calculated daily for workdays and non-workdays
-
sleep efficiency (%), defined as the ratio of time an individual is asleep to the total time the individual has spent in bed, calculated daily for workdays and non-workdays.
The average number of valid days and wear time (minutes) were also summarised descriptively at each time point and time period.
Process evaluation methods
A full process evaluation was carried out to provide insight into the observed outcomes and to contribute towards the understanding of the mechanisms of the SWAL intervention components. More specifically, the main areas to assess were recruitment, intervention implementation and participation, intervention sustainability, intervention contamination and unexpected events arising from the intervention and study. Methods comprised a range of questionnaires, focus groups, interviews and observations. The process evaluation plan can be found in Appendix 7.
Intervention fidelity
The fidelity of the intervention was monitored through several methods. First, via a questionnaire to individual participants at the 3- and 12-month time points, which asked about engagement with each intervention activity. Second, via an intervention timeline submitted by the workplace champions at the 3-, 9- and 15-month time points (note that this was collected earlier than 15 months in some councils once we knew that the study was going to use the 12-month follow-up as the primary outcome because of the COVID-19 pandemic; however, some councils had passed the 15-month stage and had, therefore, already submitted the documents). Workplace champions were required to indicate the date each task had been completed from a list of intervention activities. Third, the group catch-up meetings, led by the workplace champions, were audio-recorded. All recordings returned by champions were assessed to ensure that the content delivered was representative of the group catch-up agenda issued.
Group catch-up session fidelity
Group catch-up sessions were evaluated using an assessment tool designed specifically for this study. A copy of the tool is provided in Appendix 8. The aim of the assessment tool was to address each element as specified in the group catch-up session agenda (see Appendix 5). The assessment tool consisted of nine components in total (five components for catch-up session 1 and four components for catch-up session 2) (Table 3).
| Section | Group catch-up session | |
|---|---|---|
| 1 | 2 | |
| 1 | Introduction An outline of the catch-up session |
Introduction An outline of the catch-up session |
| 2 | Your story Opportunity to share what’s been going well and what’s not going well Share strategies or tips and any benefits experienced Identify solutions for barriers |
Your story Opportunity to share what’s been going well, what’s not going well – at work and outside work Set a group plan to help continue reducing sitting time at work |
| 3 | Refresher of key messages Revisit key messages from the online education session Discuss ideas to do at work as a group to reduce sitting time Discuss ideas to do outside work and how to get family and friends involved Remind group to visit resources available on the e-learning platform |
Slip-ups and relapse Information about slip-ups and relapse, definitions and their role in behaviour change Explore situations that could increase the risk of slip-ups or relapse and identify strategies Reflect and make a plan for any possible future slip-ups or relapse |
| 4 | Goal-setting/action-planning Reflect on past goals Revisit importance of setting goals and a reminder to set new ones |
Next steps Information on next session |
| 5 | Next steps Information on next session |
|
Workplace champions verbal behaviours
The workplace champions received training on the content of the group sessions and also on how to use interactive techniques derived from the motivational interviewing approach. 90 These skills included techniques such as Open-ended questions, Affirmations, Reflections, and Summaries (OARS). 91 In addition to the content components, it was important to assess the core micro-skills and, therefore, a component on OARS was also added to the assessment tool (see Appendix 8). Each component in the assessment tool was rated as ‘present’ (i.e. the behaviour was observed more than once), ‘absent’ (i.e. the behaviour was not observed) or ‘attempted’ (i.e. the behaviour was observed only once). Duration of the group catch-up sessions was also noted.
Inter-rater reliability of audio-recordings
To assess inter-rater reliability (IRR), 11 (20%) audio-recordings totalling 233 hours were tested by two coders. A third coder was involved in discussions to ensure that discrepancies were addressed and the tool was refined.
Data analysis
Inter-rater reliability was analysed using SPSS (version 25.0; IBM Corporation, Armonk, NY, USA) to generate Kappa scores within the cross-tabulation function. Kappa levels range from –1 to 1, with a Kappa level >0.60 indicating adequate agreement among raters. A percentage agreement level of ≥ 80% was used as the minimum acceptable inter-rater agreement.
The assessment tool data were analysed using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) to calculate the number of ‘present’, ‘attempted’ and ‘absent’ scores across different components. Data were also analysed to compare intervention arms (i.e. the SWAL-only and SWAL plus desk arms). Levels of adherence for specific components were categorised as high, moderate and low fidelity if they fell within the 80–100%, 51–79% and 0–50% ranges, respectively.
A chi-squared test was carried out to determine if there were differences in scoring between the two study intervention arms (SWAL only vs. SWAL plus desk) at the two catch-up sessions. Duration of the group catch-up sessions was analysed using Microsoft Excel and was based on the time reported by the two raters and then categorised as within time or over time.
Workplace champion feedback
The perceptions of intervention delivery by workplace champions were assessed with a questionnaire at 12 months. This contained open-ended questions exploring what elements of the programme the workplace champions felt had or had not worked well. Workplace champions were also invited to take part in a telephone interview to further explore their experiences of being a workplace champion. Telephone interviews were audio-recorded and later transcribed verbatim.
Office observations
Office observations were conducted in a sample of intervention and control clusters. Clusters were split into groups based on the council, the cluster size [small (< 10 people) or large (≥ 10 people)] and randomisation arm. One cluster was randomly selected to be observed in each group at the 3- to 6-month and 12- to 15-month time points. The observation period was approximately 2 hours long and sought to identify the integration of behaviours based on the normalisation process theory framework. 92 The observer recorded written notes on the use of height-adjustable workstations (for participants in the SWAL plus desk group), sitting and standing time, engagement with colleagues, office structure, and patterns of office-based encounters. Control group clusters were observed in the same manner to maintain consistency.
Evaluation questionnaire
All participants were issued with a process evaluation questionnaire at the 3- and 12-month time points. The questionnaire included a combination of scaled and open responses. The sections of the questionnaire were as follows:
-
online education feedback
-
workstation feedback
-
apps/computer software feedback
-
alternative support
-
group catch-up session feedback
-
sitting less challenges/competitions feedback
-
strategies to sit less
-
barriers to sitting
-
other lifestyle changes
-
health assessments.
Control group participants also received a questionnaire that enquired about any lifestyle changes that may have influenced their sitting time, and the impact that attending the study health assessments may have had on their behaviour.
Focus groups
Participants were invited to take part in focus groups at the 12-month time point. Separate focus groups were held for each intervention arm and the control group. Discussion was facilitated using a semistructured topic guide, covering the following themes: reasons for taking part, impact of measurement sessions on behaviour, views on intervention components, and benefits of and barriers to sitting less. Participants allocated to the SWAL plus desk arm were also asked about their experiences of their height-adjustable workstation use. Discussion for control participants was focused on reasons for taking part, organisational support for study activities, impact of measurement sessions on behaviour, lifestyle changes and any contact they may have had with intervention participants. Focus groups were audio-recorded and later transcribed verbatim.
Analysis of process evaluation questionnaire, focus groups and interviews
Analysis of the focus groups and interviews was informed by principles of the constant comparative approach. 93 Briefly, a sample of transcripts were read and re-read to begin the process of identifying initial themes and the relationship between themes (in an inductive manner), and this was translated into an initial coding framework. Transcripts were then uploaded to NVivo (QSR International, Warrington, UK) to facilitate the process of systematic coding of transcripts. The coding framework was refined and expanded throughout the coding process, adding new codes, refining the names of codes and amending relationships between codes. Free-text responses from the process evaluation questionnaire were uploaded to the same NVivo file to enable coding with the same framework. After a phase of open coding, a set of questions (derived from the aims of the process evaluation) informed the addition of further codes, and further coding of the transcripts (bringing in a more deductive element). Data coded to each relevant code were retrieved and re-read to identify patterns and ‘weight’ of findings to enable summaries to be produced.
Cost-effectiveness
Full details of the methods for the cost-effectiveness analysis are presented in Chapter 5. In brief, the economic evaluation assessed whether or not the SWAL intervention, with and without a height-adjustable workstation, was cost-effective compared with usual practice. To address the question of cost-effectiveness, the economic analysis of each SWAL intervention comprised the following:
-
a descriptive assessment of resource use, costs and outcomes
-
a cost-effectiveness analysis with costs and outcomes estimated within the trial period and extrapolated into the longer term
-
a series of sensitivity, scenario and threshold analyses considering the impacts of key uncertainties on base-case findings
-
a secondary cost-effectiveness analysis based on observed differences between secondary outcomes within the trial period.
Outcomes included quality-adjusted life-years (QALYs), in line with current UK guidance for economic evaluations. 94 Secondary outcomes included other measures of health, well-being and productivity. The analysis was performed initially from a public sector perspective, with an employer’s perspective subsequently considered. The base-case cost-effectiveness analysis extrapolated differences observed in the trial period into the longer term. Results over the trial’s time horizon (i.e. 12 months) are presented for comparison. Cost-effectiveness results are expressed in terms of incremental cost-effectiveness ratios (ICERs), showing the incremental cost per additional QALY compared with the other strategy, incremental net health benefits (INHBs) to show the difference between the health generated with a strategy and the health that could be generated elsewhere in the health-care system using the same resources, and incremental net monetary benefits (INMBs) to present the monetary value of the additional health generated, at thresholds of £15,000, £20,000 and £30,000 per QALY. 94 Scenario, sensitivity and threshold analyses were conducted across a variety of domains (participant characteristics, intervention costs, methodological approaches, model assumptions, etc.) to explore the uncertainty around the economic findings.
The COVID-19 pandemic
In March 2020, the COVID-19 pandemic led to the UK Government issuing guidelines on social distancing and restrictions on non-essential travel. As part of these measures, employees were encouraged to work at home, where possible. 95,96
COVID-19 Work Transport and Health Behaviours Questionnaire
In the light of the COVID-19 pandemic, and the UK Government-imposed restrictions that occurred in March 2020, SWAL participants were invited to complete an additional optional short online survey to identify any changes in peoples’ daily lifestyle behaviours relating to working practices, sitting and physical activity behaviour, and health, as a result of the COVID-19 pandemic.
The online survey was created on the Jisc online surveys platform (Jisc, Bristol, UK), which is a General Data Protection Regulation (GDPR)-compliant online survey tool designed for academic research, education and public sector organisations. A participant information sheet and a consent statement were included on the opening page of the survey. Ethics approval was gained from University of Leicester’s College of Life Sciences representatives and the University of Salford’s Research, Enterprise and Engagement Ethical Approval Panel.
The link to the questionnaire was issued to participants via e-mail at the beginning of May 2020. The following measures were included in the questionnaire:
-
geographic location, gender, age group and ethnicity
-
household composition and number of dependents
-
details of any caring and home-schooling responsibilities
-
changes in working situation (working from home/furloughed, etc.)
-
changes in ways of working (use of virtual meetings, etc.)
-
changes in time spent sitting, standing, moving and in physical activity
-
types of physical activity engaged in pre- and post-COVID-19 restrictions
-
musculoskeletal problems (measured using the SNQ)
-
sleep duration (measured using a short version of the Pittsburgh Sleep Quality Index).
Lifestyle behaviour questions were adapted slightly in wording to ask about lifestyle behaviour prior to the COVID-19 restrictions and since/during the COVID-19 restrictions.
Analysis of the COVID-19 questionnaire
Data were downloaded from the Jisc platform and imported into Stata (Stata Corp LP, College Station, TX, USA), where all data cleaning, reduction and analysis was carried out. Wilcoxon signed-rank tests and paired t-tests were carried out to compare the physical and lifestyle behaviours before and during COVID-19 restrictions.
Statistical analysis
Cluster- and participant-level baseline characteristics were summarised by randomisation group and for all participants (total). We also carried out a descriptive comparison of baseline data between completers (i.e. participants who provided valid activPAL data at baseline and at 12 months) and non-completers, within randomisation groups and overall.
Analysis of the primary outcome
The primary analysis was performed using a linear multilevel model. Analysis of covariance was used with each participant’s sitting time at 12-month follow-up as the outcome variable, adjusting for sitting time at baseline and for the average waking wear time across baseline and 12-month follow-up. The model also included a categorical variable for randomisation group (control group as reference) and terms for the stratification factors (i.e. area and cluster size). Office clusters were included as a random effect to model worker heterogeneity within office sites. The structure of the variance–covariance matrix for the random effect was assumed to be identity and the models were estimated using restricted maximum likelihood.
For the primary analysis, missing data were not replaced (complete-case analysis) and participants were included in the intervention group in which their cluster was randomised, irrespective of the intervention that was actually received.
For both comparisons (i.e. SWAL-only group vs. control group; SWAL plus desk group vs. control group), the estimate of the difference between intervention group and the control group for average daily sitting time at 12 months and the corresponding 97.5% confidence intervals (CIs) (to adjust for multiple testing – two-treatment arm comparisons) and p-values are presented. Statistical tests were two sided. Furthermore, the ICC and 95% CI were estimated to assess the strength of the clustering effect.
Secondary analyses
A secondary analysis was carried out to evaluate if one intervention was more effective than the other. The secondary analysis used similar methodology to the primary analysis; however, there was no formal adjustment for multiple significance testing, as this was an unpowered analysis. Estimates are presented with 95% CIs and p-values. Statistical tests were two sided.
Secondary outcomes
A restricted set of key secondary outcomes (i.e. sitting time, prolonged sitting time, standing time and stepping time – daily and on workdays and during work hours calculated from the activPAL data) were analysed using similar methodology as the primary outcome analysis; however, no corrections were made for multiple testing.
Given the number of secondary outcomes, all of the other secondary outcomes were summarised descriptively by intervention group.
Sensitivity analyses
The sensitivity analyses were conducted using similar methodology as the primary analysis of the primary outcome; however, there was no formal adjustment for multiple significance testing. The sensitivity and subgroup analyses were conducted for daily average sitting time at 12 months and average sitting during work hours at 12 months only. All tests and reported p-values were two sided. Estimates are presented with 95% CIs, with the exception of the primary analysis of the primary outcome, which is presented with 97.5% CIs.
Per-protocol analysis
The effect size was also estimated using a per-protocol analysis. The per-protocol analysis excluded the following participants:
-
participants who did not provide valid activPAL primary outcome data at baseline or at 12-month follow-up
-
control group participants with access to a standing desk at 12 months
-
participants in clusters belonging to the intervention arms who did not have a workplace champion assigned or the champion left their role within the first 3 months
-
participants who were out of their window for 12-month follow-up in terms of their activPAL data (± 2 months)
-
participants who did not spend the majority (>50%) of their day sitting at baseline as measured by activPAL.
Intention-to-treat analysis
A sensitivity analysis using multilevel multiple imputation was performed to evaluate the impact of missing outcome data on the results obtained and to account for uncertainty associated with imputing data [i.e. full intention-to-treat (ITT) analysis]. The sensitivity analysis was implemented using the jomo package in R,86 using the following steps:
-
The imputation model registered imputation of daily sitting time at the baseline and 3- and 12-month time points. The imputation model contained auxiliary variables as outcomes if they had missing data, or as covariates if they did not have any missing data. The auxiliary variables were BMI at baseline, BMI at 3 months, gender, ethnicity, age, cluster size category [small (< 10 people); large (≥ 10 people)] and area (Leicester; Salford; Liverpool). The model also included average waking wear time across baseline and 12 months as an outcome as it was adjusted for in the model for the primary analysis.
-
The multiple imputation was multilevel with cluster ID as the cluster-level variable.
-
The multilevel multiple imputation analysis was carried out in the jomo package in R, using a joint modelling approach, meaning that, in addition to the covariates specified, each of the outcome variables in the imputation model also informed the imputation of the other outcomes if that information was available.
-
The multilevel multiple imputation used 20 imputations, 10,000 burn-in iterations and 10,000 between-imputation iterations. The imputations were carried out separately by intervention arm. A seed was set to make the results reproducible.
-
Once the imputations were carried out, the same model as the primary analysis of the primary outcome was estimated using the lmer command in R. The model was fitted for each of the 20 imputed data sets and the estimates were combined using Rubin’s rules. 97
Effect on number of valid activPAL days
We carried out additional sensitivity analyses by assessing the effect of the number and type of valid activPAL days. The sensitivity analyses were performed by including participants who wore the activPAL for the following criteria:
-
≥ 4 valid days at both baseline and 12 months
-
≥ 1 valid day of workdays at both baseline and 12 months
-
≥ 3 valid days of workdays at both baseline and 12 months.
Standardising occupational/waking hours
To assess the impact of variation in occupational or waking hours between participants, time spent sitting was normalised to an 8-hour workday for sitting during work hours and a 16-hour waking day for daily sitting.
Subgroup analyses
Similar methods to those used in the primary analysis of the primary outcome were used to estimate the intervention effect in different subgroups. For each subgroup being assessed, an indicator variable for subgroup assignment was included in the model. An interaction term between intervention arm and subgroup was included to assess the level of heterogeneity in treatment effect between the subgroups. An estimate of the treatment effect (i.e. difference between subgroups) and 95% CI are presented for each subgroup, alongside the p-value for the interaction term. We investigated the intervention effect for the following subgroups:
-
area [Leicester (Leicester City Council and Leicestershire County Council), Liverpool, Salford (Salford City Council, Bolton Council, and Trafford Council)]
-
small compared with large clusters (< 10 people, ≥ 10 people)
-
type of worker (i.e. part time, full time)
-
sex (male, female)
-
age (< median, ≥ median)
-
BMI [normal, overweight/obese (≥ 25 kg/m2)].
Patient and public involvement
Council employees were involved in the study design during the grant application process and the study delivery phase. During the grant development phase, the study purpose, design and proposed intervention strategies were presented to two large groups of council employees. As a result, finger prick blood tests (rather than venous blood samples), participants receiving feedback on health measures and incentives for attending follow-up were included in the design. During the study set up and delivery, a council employee advisory group met several times and provided advice on intervention delivery, recruitment processes and workstation installation. Two council employees were also part of the TSC, which met twice per year during the study.
Chapter 3 Quantitative results
Number of clusters and participants
Between May 2018 and February 2019, 797 participants were recruited and consented into the study, with 756 participants across 78 clusters being randomised. Figure 2 shows the flow of participants through the study. There were 26 clusters (267 participants) randomised to the control arm, 27 clusters (249 participants) to the SWAL-only arm and 25 clusters (240 participants) to the SWAL plus desk arm. All clusters in all study arms were assessed at 3- and 12-month follow-up, with 87.7% of participants seen at 3 months (control group, 84.6%; SWAL only, 87.6%; SWAL plus desk, 91.3%) and 77.8% of participants seen at 12 months (control group, 74.2%; SWAL only, 75.5%; SWAL plus desk, 84.2%).
FIGURE 2.
A CONSORT figure of participant flow through the study. AE, adverse event.

Baseline characteristics
Table 4 presents the characteristics of the clusters and the participants within these clusters. The median cluster size was eight participants, with an interquartile range (IQR) of 6–11 participants. Approximately 54% of clusters and 60% of the participants were from councils in Leicester and Leicestershire (Leicester City Council, 31 clusters, 335 participants; Leicestershire County Council, 11 clusters, 122 participants; Salford City Council, 11 clusters, 94 participants; Bolton Council, six clusters, 57 participants; Trafford Council, four clusters, 47 participants; Liverpool Council, 15 clusters, 101 participants).
| Characteristic | Study arm | Total | ||
|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | ||
| Cluster level | ||||
| Number of clusters | 26 | 27 | 25 | 78 |
| Cluster size, n (%) | ||||
| Small (< 10 people) | 17 (65.4) | 17 (63.0) | 16 (64.0) | 50 (64.1) |
| Large (≥ 10 people) | 9 (34.6) | 10 (37.0) | 9 (36.0) | 28 (35.9) |
| Median (IQR) | 7 (5–12) | 8 (6–11) | 8 (6–10) | 8 (6–11) |
| Area, n (%) | ||||
| Leicester | 14 (53.9) | 15 (55.6) | 13 (52.0) | 42 (53.9) |
| Liverpool | 4 (15.4) | 5 (18.5) | 6 (24.0) | 15 (19.2) |
| Salford | 8 (30.8) | 7 (25.9) | 6 (24.0) | 21 (26.9) |
| Individual level | ||||
| Number of participants | 267 | 249 | 240 | 756 |
| Cluster size, n (%) | ||||
| Small (< 10 people) | 106 (39.7) | 108 (43.4) | 104 (43.3) | 318 (42.1) |
| Large (≥ 10 people) | 161 (60.3) | 141 (56.6) | 136 (56.7) | 438 (57.9) |
| Area, n (%) | ||||
| Leicester | 179 (67.0) | 141 (56.6) | 137 (57.1) | 457 (60.4) |
| Liverpool | 22 (8.2) | 35 (14.1) | 44 (18.3) | 101 (13.4) |
| Salford | 66 (24.7) | 73 (29.3) | 59 (24.6) | 198 (26.2) |
| Demographic measurements | ||||
| Age (years), mean (SD) | 44.5 (11.2) | 43.8 (9.9) | 45.9 (10.1) | 44.7 (10.5) |
| Gender, n (%) | ||||
| Male | 71 (26.6) | 64 (25.7) | 74 (30.8) | 209 (27.6) |
| Female | 196 (73.4) | 185 (74.3) | 166 (69.2) | 547 (72.4) |
| Ethnicity, n (%) | ||||
| White British | 180 (67.4) | 175 (70.3) | 172 (71.7) | 527 (69.7) |
| Other | 87 (32.6) | 74 (29.7) | 68 (28.3) | 229 (30.3) |
| Level of education, n (%) | ||||
| Degree or above | 152 (57.1) | 170 (68.3) | 134 (55.8) | 456 (60.5) |
| Marital status, n (%) | ||||
| Married/living with someone | 189 (71.0) | 178 (71.4) | 183 (76.2) | 550 (72.8) |
| Smoking status, n (%) | ||||
| Current smoker | 10 (3.8) | 15 (6.0) | 9 (3.8) | 34 (4.5) |
| Number of people in household | ||||
| Mean (SD) | 2.94 (1.27) | 2.96 (1.33) | 2.96 (1.25) | 2.95 (1.28) |
| Median (IQR) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) |
| Number of children in household | ||||
| Mean (SD) | 0.64 (0.97) | 0.73 (0.96) | 0.63 (0.93) | 0.67 (0.96) |
| Median (IQR) | 0 (0–1) | 0 (0–1) | 0 (0–1) | 0 (0–1) |
| Working characteristics | ||||
| Working pattern, n (%) | ||||
| Full time (≥ 35 hours/week) | 229 (85.8) | 205 (83.0) | 206 (86.2) | 640 (85.0) |
| Number who manage/supervise staff, n (%) | 85 (32.0) | 87 (35.4) | 90 (37.5) | 262 (34.8) |
| Duration (years) working at council, mean (SD) | 12.6 (9.87) | 11.6 (8.78) | 13.1 (9.59) | 12.4 (9.44) |
| Duration (years) in current role, mean (SD) | 5.50 (6.35) | 5.34 (4.59) | 5.48 (4.89) | 5.44 (5.36) |
| Contracted hours per week, mean (SD) | 35.3 (3.65) | 35.3 (3.60) | 35.4 (3.48) | 35.4 (3.57) |
| Number of people in office, mean (SD) | 68.7 (71.5) | 61.2 (66.2) | 47.2 (36.6) | 59.4 (61.1) |
| Biometric measurements | ||||
| Weight (kg), mean (SD) | 71.6 (17.1) | 75.1 (18.1) | 73.8 (17.6) | 73.4 (17.6) |
| BMI (kg/m2), mean (SD) | 25.8 (5.60) | 27.3 (6.42) | 26.4 (5.68) | 26.5 (5.93) |
| Per cent body fat, mean (SD) | 32.4 (9.26) | 33.7 (9.44) | 32.3 (9.27) | 32.8 (9.33) |
| Waist circumference (cm), mean (SD) | 86.6 (13.7) | 89.0 (15.0) | 89.2 (14.4) | 88.2 (14.4) |
| Systolic blood pressure (mmHg), mean (SD) | 116.9 (14.5) | 119.0 (17.3) | 119.2 (16.6) | 118.3 (16.2) |
| Diastolic blood pressure (mmHg), median (IQR) | 78.1 (9.46) | 79.4 (10.7) | 79.9 (11.1) | 79.1 (10.4) |
| Fasting glucose (mmol/l), median (IQR) | 5.30 (4.90–5.70) | 5.40 (5.00–5.80) | 5.40 (5.00–5.80) | 5.30 (5.00–5.75) |
| HbA1c (mmol/l), median (IQR) | 32.7 (30.5–35.1) | 33.3 (31.3–35.6) | 33.9 (31.1–36.2) | 33.3 (30.9–35.7) |
| HbA1c (%), median (IQR) | 5.14 (4.94–5.36) | 5.20 (5.01–5.41) | 5.25 (5.00–5.46) | 5.20 (4.98–5.42) |
| Triglycerides (mmol/l), median (IQR) | 1.04 (0.80–1.38) | 1.05 (0.83–1.38) | 1.05 (0.82–1.41) | 1.05 (0.82–1.39) |
| HDL cholesterol (mmol/l), mean (SD) | 1.46 (0.38) | 1.41 (0.42) | 1.42 (0.39) | 1.43 (0.40) |
| LDL cholesterol (mmol/l), mean (SD) | 2.52 (0.96) | 2.65 (1.26) | 2.56 (1.00) | 2.58 (1.08) |
| Total cholesterol (mmol/l), mean (SD) | 4.64 (1.04) | 4.71 (1.07) | 4.67 (1.06) | 4.67 (1.06) |
| activPAL variables | ||||
| Daily values | ||||
| Sitting (minutes/day), mean (SD) | 601.6 (83.7) | 605.2 (84.3) | 609.4 (78.5) | 605.2 (82.2) |
| Prolonged (≥ 30 minutes) sitting (minutes/day), mean (SD) | 316.6 (100.2) | 313.8 (97.6) | 324.2 (102.7) | 318.1 (100.1) |
| Standing (minutes/day), mean (SD) | 230.8 (66.5) | 226.4 (70.5) | 231.9 (70.1) | 229.7 (68.9) |
| Stepping (minutes/day), mean (SD) | 109.3 (33.5) | 108.7 (31.3) | 109.2 (33.3) | 109.1 (32.7) |
| Number of steps (steps/day), mean (SD) | 9291.0 (3209.1) | 9286.4 (3121.3) | 9230.9 (3228.7) | 9270.5 (3182.6) |
| MVPA stepping time (minutes/day), median (IQR) | 23.3 (14.0–36.4) | 23.1 (14.3–34.7) | 23.2 (13.6–36.0) | 23.2 (14.0–35.9) |
| Number of sit-to-upright transitions (transitions/day), mean (SD) | 53.7 (13.8) | 53.6 (13.5) | 52.3 (14.1) | 53.2 (13.8) |
| Wear time (minutes/day), mean (SD) | 941.7 (53.0) | 940.4 (56.3) | 950.4 (55.2) | 944.0 (54.7) |
| Number of valid days, mean (SD) | 7.39 (1.25) | 7.26 (1.33) | 7.25 (1.49) | 7.30 (1.36) |
| Work hours values | ||||
| Sitting (minutes/day), mean (SD) | 358.8 (65.3) | 356.4 (71.1) | 358.1 (67.6) | 357.8 (67.9) |
| Prolonged (≥ 30 minutes) sitting (minutes/day), mean (SD) | 193.7 (86.3) | 183.2 (92.5) | 194.4 (85.2) | 190.5 (88.1) |
| Standing (minutes/day), median (IQR) | 69.9 (52.1–98.5) | 73.4 (53.6–100.3) | 73.5 (50.7–100.1) | 71.7 (51.5–99.1) |
| Stepping (minutes/day), mean (SD) | 40.2 (14.5) | 41.3 (14.4) | 40.6 (17.1) | 40.7 (15.3) |
| Number of steps (steps/day), mean (SD) | 3822.7 (1452.2) | 3885.7 (1434.3) | 3835.3 (1686.2) | 3847.4 (1522.7) |
| MVPA stepping time (minutes/day), median (IQR) | 11.3 (7.0–17.1) | 10.8 (6.2–17.1) | 11.3 (5.7–17.8) | 11.2 (6.3–17.6) |
| Number of sit-to-upright transitions (transitions/day), mean (SD) | 27.5 (10.4) | 28.2 (11.0) | 25.8 (9.48) | 27.2 (10.4) |
| Wear time (minutes/day), mean (SD) | 482.5 (45.3) | 484.7 (52.4) | 482.4 (52.6) | 483.2 (50.0) |
| Number of valid days, mean (SD) | 4.82 (1.32) | 4.76 (1.30) | 4.81 (1.37) | 4.79 (1.33) |
On average, participants were aged (SD) 44.7 ± 10.5 years and had a BMI of 26.5 ± 5.9 kg/m2. The majority of participants were of white European ethnicity (69.7%), female (72.4%) and worked full time (85.0%). The percentage of time spent sitting, standing and stepping was 64.2% ± 8.3%, 24.3% ± 7.0% and 11.5% ± 3.3% of daily wear time, and 74.3% ± 11.7%, 17.5% ± 10.7% and 8.5% ± 3.2% of daily work time. Over half of the sitting time was accrued in prolonged bouts, with this value similar for daily sitting time (51.9% ± 12.1%) and work sitting time (51.5% ± 19.0%). There were no significant differences between participants with available primary outcome data at both baseline and 12 months (i.e. completers) and participants without (i.e. non-completers) for the characteristics reported in Table 4, except for age (as participants who were older were more likely to have available data: 41.6 ± 11.3 vs. 45.8 ± 10.0 years of age; p < 0.001).
Daily sitting time
12 months (primary outcome)
A significant difference between groups was found in daily sitting time in favour of the SWAL-only group (–22.22 minutes/day, 97.5% CI –38.8 to –5.7 minutes/day; p = 0.003) and the SWAL plus desk group (–63.73 minutes/day, –80.0 to –47.4 minutes/day; p < 0.001), compared with the control group in the complete-case analysis (Table 5). Participants in the SWAL plus desk group sat for 42 minutes less per day (95% CI –56.3 to –27.0 minutes/day; p < 0.001) than participants in the SWAL-only group. Similar results were seen in the ITT and per-protocol analyses.
| Number of clusters (participants) | Mean (SD) change from baseline to 12-month follow-up | Adjusted mean difference at follow-up (95% CI); p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | SWAL only vs. controla | SWAL plus desk vs. control | SWAL plus desk vs. SWAL only | |
| Primary analysis (complete case)b,c | 26 (183) | 27 (177) | 25 (187) | 15.6 (75.0) | –9.37 (80.5) | –53.7 (79.1) | –22.2 (–38.8 to –5.7); 0.003c | –63.7 (–80.1 to –47.4); < 0.001c | –41.7 (–56.3 to –27.0); < 0.001 |
| ITTb | 26 (267) | 27 (249) | 25 (240) | 13.3 (74.8) | –10.1 (82.8) | –53.1 (81.6) | –20.2 (–35.8 to –4.5); 0.012 | –63.1 (–78.4 to –47.7); < 0.001 | –42.9 (–58.5 to –27.3); < 0.001 |
| Per protocolb | 26 (164) | 22 (158) | 25 (167) | 11.4 (73.5) | –12.9 (81.4) | –56.3 (77.0) | –20.8 (–36.3 to –5.4); 0.008 | –61.2 (–76.5 to –45.9); < 0.001 | –41.0 (–57.2 to –24.8); < 0.001 |
| Standardised to waking day (16 hours)d | 26 (183) | 27 (177) | 25 (187) | 9.59 (46.2) | –1.73 (53.8) | –30.2 (55.4) | –10.3 (–20.4 to –0.26); 0.044 | –38.6 (–48.5 to –28.6); < 0.001 | –28.3 (–39.0 to –17.6); < 0.001 |
| Effect of number of valid activPAL days (complete case) | |||||||||
| ≥ 4 dayse | 26 (174) | 27 (169) | 25 (168) | 15.1 (71.9) | –10.9 (80.2) | –50.6 (78.7) | –22.1 (–37.0 to –7.1); 0.004 | –60.6 (–75.6 to –45.6); < 0.001 | –38.8 (–54.1 to –23.5); < 0.001 |
| ≥ 1 workdaye | 26 (176) | 26 (165) | 25 (177) | 15.0 (75.3) | –11.4 (79.8) | –54.2 (79.1) | –22.4 (–37.3 to –7.5); 0.003 | –63.2 (–77.8 to 48.6); < 0.001 | –40.8 (–55.9 to –25.8); < 0.001 |
| ≥ 3 workdayse | 26 (156) | 26 (144) | 25 (143) | 16.5 (72.9) | –8.9 (79.7) | –54.7 (79.0) | –21.5 (–37.4 to –5.5); 0.008 | –65.1 (–81.1 to –49.2); < 0.001 | –43.9 (–60.6 to –27.2); < 0.001 |
Sensitivity analyses
Sensitivity analyses showed similar results to the primary analysis, with significant differences observed in daily sitting time between groups at 12 months when standardising the data to a 16-hour waking day, and when ≥ 4 valid days, ≥ 1 valid workday or ≥ 3 valid workdays of activPAL data were used.
Subgroup analyses
The results of the subgroup analyses are displayed in Figures 3 and 4. For all subgroups, there were no significant interaction effects for either intervention group.
FIGURE 3.
Adjusted difference in average daily sitting time (minutes/day) at 12 months for SWAL-only group.
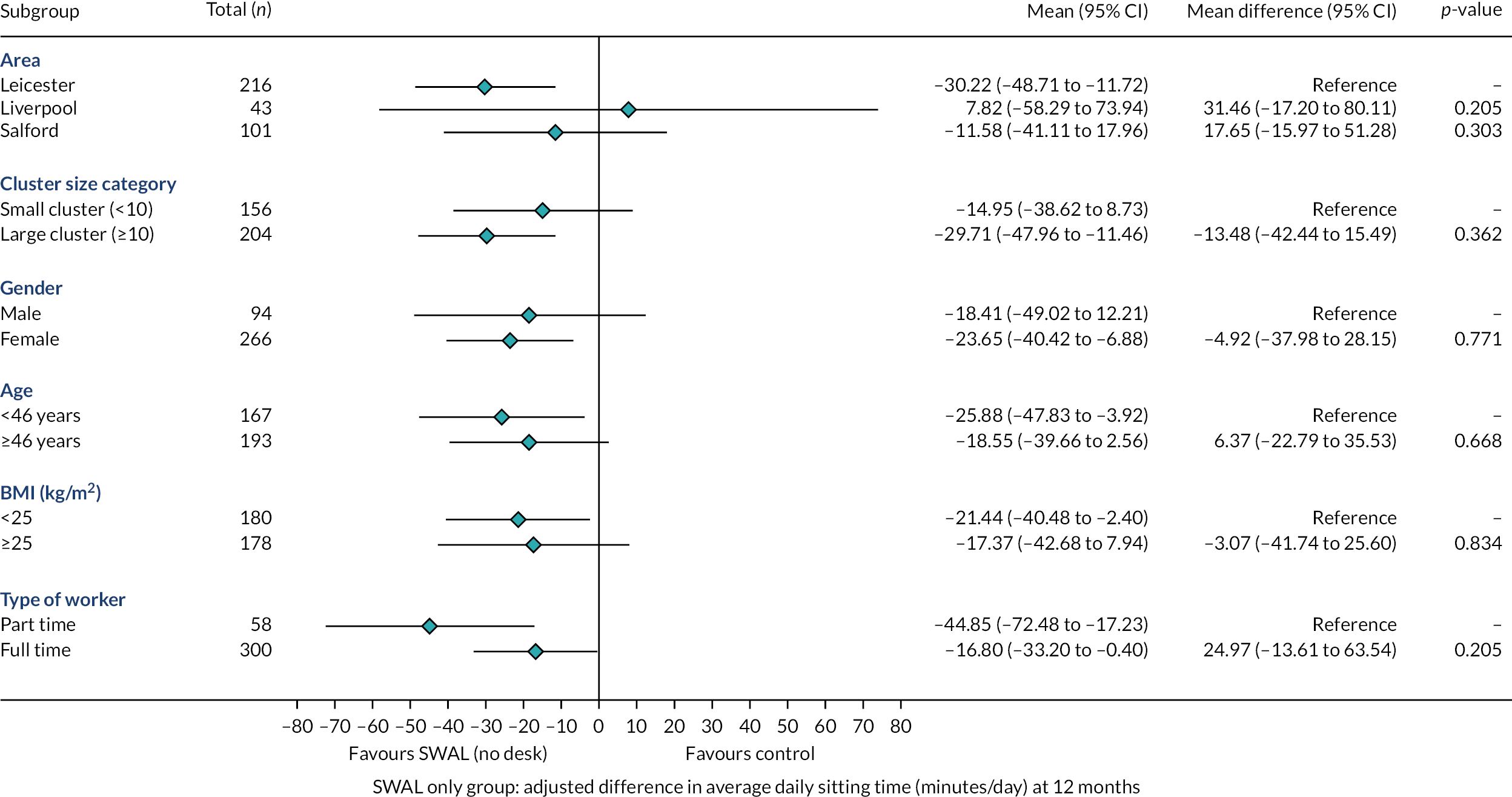
FIGURE 4.
Adjusted difference in average daily sitting time (minutes/day) at 12 months for SWAL plus desk group.
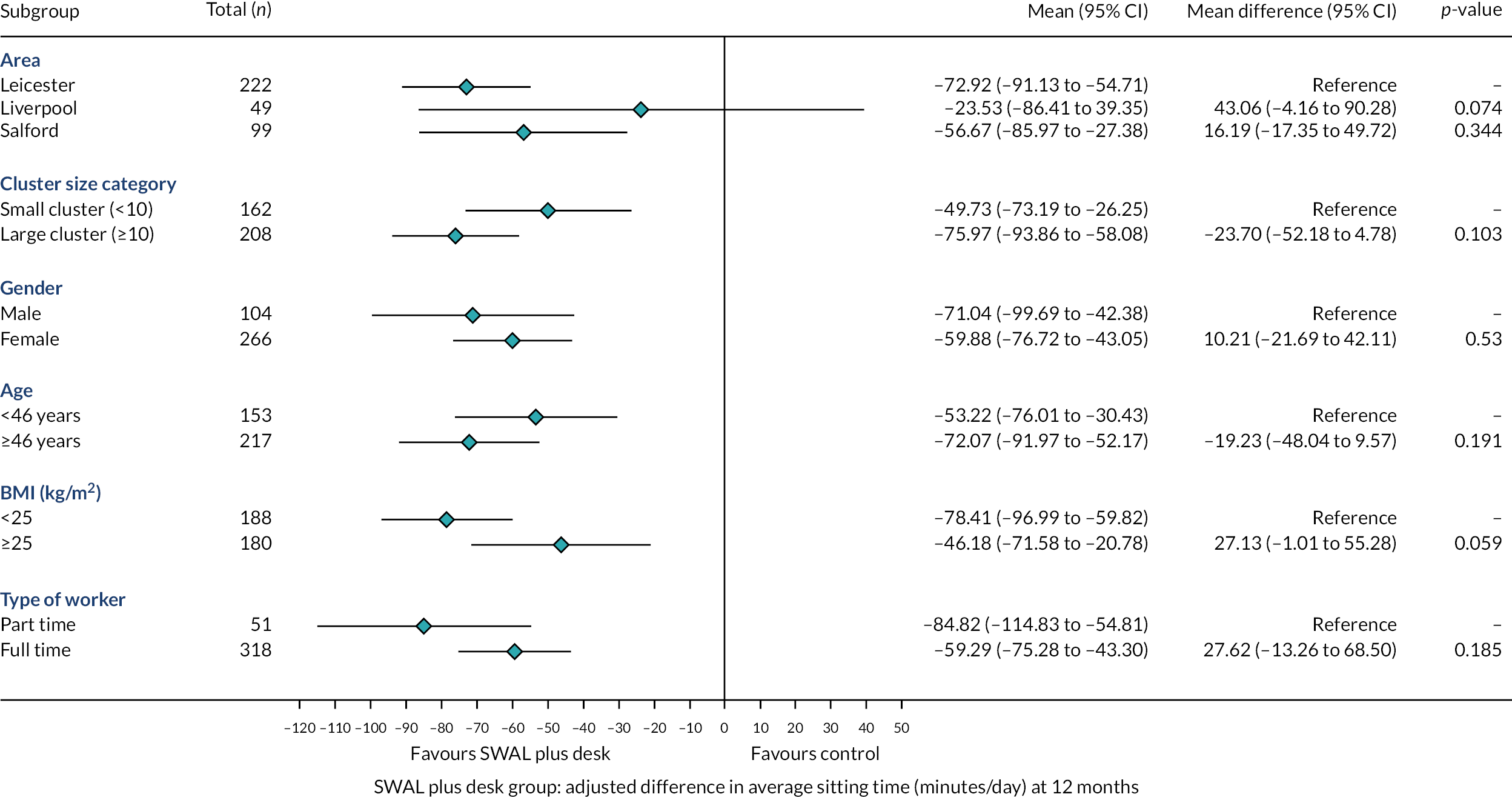
Secondary outcomes
Key activPAL assessed secondary outcomes
Differences in sitting time during work hours at 12 months
A significant difference between groups was found in sitting time during work hours in favour of the SWAL plus desk group (–57.89 minutes/day) compared with the control group in the complete-case analysis (Table 6). Similar results were seen in the ITT and per-protocol analyses, and in the analysis when ≥ 3 valid workdays of activPAL data were used.
| Number of clusters (participants) | Mean (SD) change from baseline to 12-month follow-up | Adjusted mean difference at follow-up (95% CI); p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk Did the measurements prompt GP visits? | SWAL only vs. control | SWAL plus desk vs. control | SWAL plus desk vs. SWAL only | |
| Primary analysis (complete case)a | 26 (176) | 26 (167) | 25 (177) | 2.19 (61.1) |
–12.8 (71.0) | –56.4 (85.5) | –13.4 (–29.0 to 2.17); 0.092 | –57.9 (–73.3 to –42.5); < 0.001 | N/A |
| ITTa | 26 (267) | 27 (249) | 25 (240) | –0.33 (60.9) | –10.3 (73.6) | –53.4 (85.4) | –11.5 (–26.5 to 3.49); 0.132 | –54.0 (–69.0 to –39.0); < 0.001 | N/A |
| Per protocola | 26 (157) | 22 (149) | 25 (157) | –0.09 (58.2) |
–14.5 (71.3) | –59.5 (83.5) | –12.5 (–28.4 to 3.47); 0.125 | –57.7 (–73.3 to –42.1); < 0.001 | N/A |
| Standardised to working day (8 hours)b | 26 (176) | 26 (167) | 25 (177) | 3.27 (53.1) | –12.4 (59.8 | –59.9 (73.4) | –14.9 (–28.6 to –1.24); 0.033 | –61.4 (–74.9 to –47.9); < 0.001 | –46.6 (–61.0 to –32.1); < 0.001 |
| Effect of number of valid activPAL days (complete case) | |||||||||
| ≥ 3 days during work hoursc | 26 (156) | 26 (144) | 25 (143) | 2.61 (61.7) |
–10.6 (69.4) | –59.8 (85.3) | –12.5 (–28.6 to 3.6); 0.127 | –60.3 (–76.3 to –44.2); < 0.001 | N/A |
In the analysis standardising sitting time to an 8-hour workday, significant differences in sitting time during work hours were observed between both intervention groups and the control group in changes in sitting time during work hours. Participants in the SWAL plus desk group sat for 47 minutes less per day than participants in the SWAL-only group.
For all subgroups, there were no significant interaction effects for either intervention groups, with the exception of age for the SWAL plus desk group. The intervention had a greater effect for participants aged ≥ 46 years (median age) (Figures 5 and 6).
FIGURE 5.
Adjusted difference in average sitting time during work hours (minutes/day) at 12 months for SWAL-only group.

FIGURE 6.
Adjusted difference in average sitting time during work hours (minutes/day) at 12 months for SWAL plus desk group.
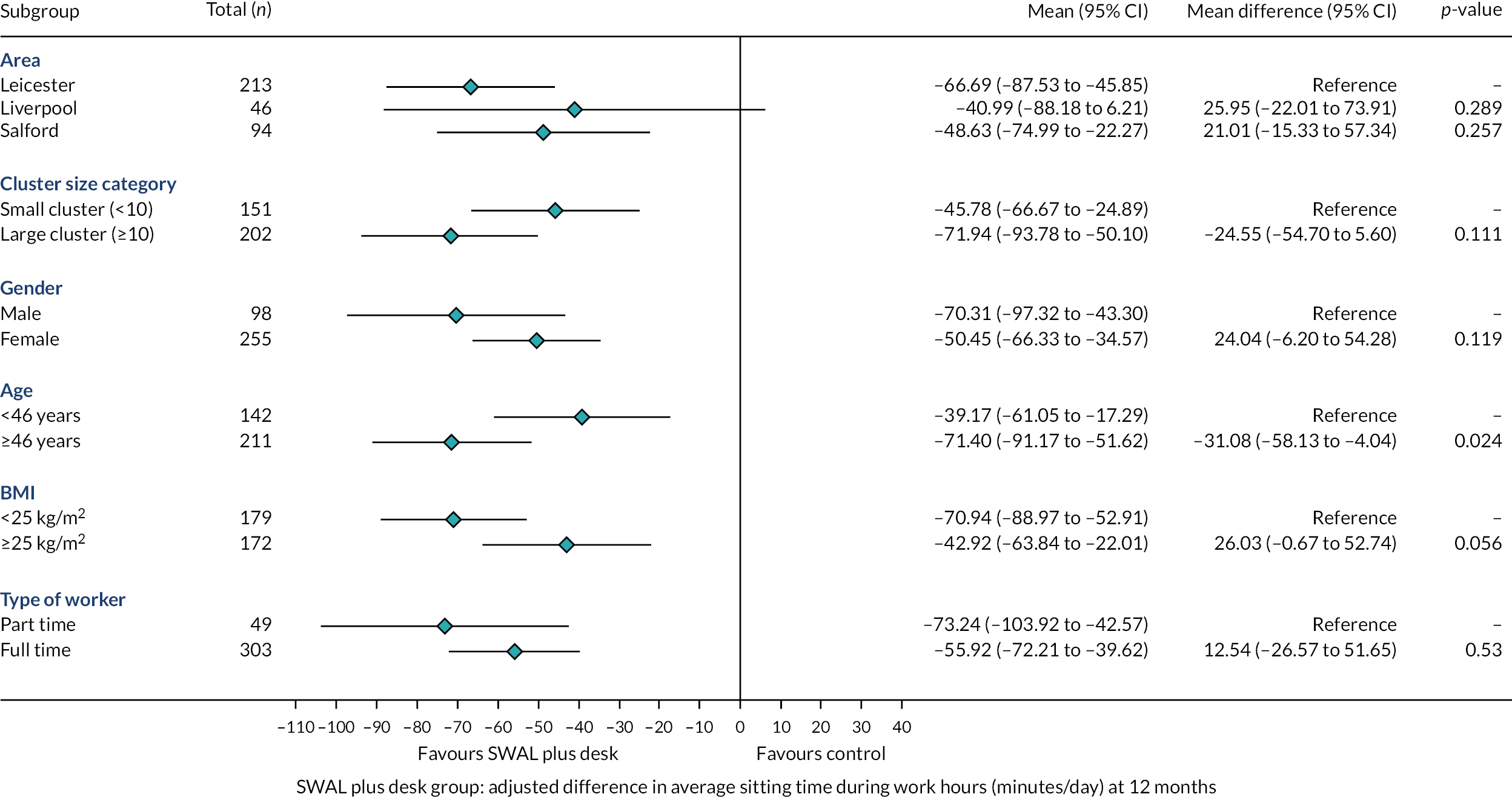
Other key activPAL-assessed outcomes: sitting, prolonged sitting, standing and stepping
In favour of the SWAL-only group, there were differences in comparison with the control group in daily sitting time at 3 months and sitting time during workdays at 3 and 12 months, as well as prolonged sitting time for daily, work hours and workdays at 3 and 12 months, and stepping time on workdays at 3 months (Table 7).
| Variable | Number of clusters (participants) | Mean (SD) change from baseline to follow-up | Adjusted mean difference at follow-up (95% CI); p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | SWAL only vs. control | SWAL plus desk vs. control | SWAL plus desk vs. SWAL only | |
| Daily variables (minutes/day) | |||||||||
| Sitting time | |||||||||
| 3-month follow-upa | 26 (210) | 27 (200) | 25 (202) | –3.54 (75.9) | –27.5 (87.2) | –68.5 (78.1) | –20.0 (–34.9 to –5.03); 0.009 | –62.7 (–77.6 to –47.8); < 0.001 | –43.4 (–60.4 to –26.3); < 0.001 |
| Prolonged sitting | |||||||||
| 3-month follow-upa | 26 (210) | 27 (200) | 25 (202) | 8.66 (81.0) | –25.7 (85.4) | –41.9 (83.6) | –32.1 (–47.8 to –16.4); < 0.001 | –47.4 (–63.0 to –31.8); < 0.001 | –15.9 (–32.9 to 1.1); 0.066 |
| 12-month follow-upb | 26 (183) | 27 (177) | 25 (187) | 24.9 (74.8) | –5.47 (82.7) | –29.2 (77.8) | –30.5 (–45.3 to –15.7); < 0.001 | –50.3 (–64.9 to –35.7); < 0.001 | –19.9 (–35.1 to –4.67); 0.010 |
| Standing time | |||||||||
| 3-month follow-upa | 26 (210) | 27 (200) | 25 (202) | 2.82 (51.3) | 9.52 (57.7) | 51.1 (64.6) | 5.47 (–7.46 to 18.4); 0.407 | 47.2 (34.3 to 60.2); < 0.001 | N/A |
| 12-month follow-upb | 26 (183) | 27 (177) | 25 (187) | –5.55 (50.7) | 0.08 (60.8) | 32.8 (65.6) | 5.98 (–6.42 to 18.4); 0.344 | 39.0 (26.8 to 51.3); < 0.001 | N/A |
| Stepping time | |||||||||
| 3-month follow-upa | 26 (210) | 27 (200) | 25 (202) | –3.47 (22.1) | 0.54 (26.6) | –1.54 (24.2) | 4.65 (–0.45 to 9.76); 0.074 | 3.01 (–2.11 to 8.12); 0.249 | N/A |
| 12-month follow-upb | 26 (183) | 27 (177) | 25 (187) | –4.65 (20.9) | –0.98 (26.1) | –1.03 (26.9) | 4.62 (–0.38 to 9.61); 0.070 | 4.14 (–0.81 to 9.08); 0.101 | N/A |
| Work hours variables (minutes/day) | |||||||||
| Sitting time | |||||||||
| 3-month follow-upc | 26 (186) | 26 (175) | 25 (176) | –7.13 (62.45) | –24.76 (62.06) | –82.55 (77.94) | –13.0 (–29.5 to 3.6); 0.125 | –74.3 (–90.8 to –57.7); < 0.001 | N/A |
| Prolonged sitting | |||||||||
| 3-month follow-upc | 26 (186) | 26 (175) | 25 (176) | –5.26 (68.2) | –28.1 (69.8) | –60.1 (72.6) | –20.5 (–34.6 to –6.41); 0.004 | –53.4 (–67.5 to –39.3); < 0.001 | –33.3 (–48.1 to –18.4); < 0.001 |
| 12-month follow-upd | 26 (176) | 26 (167) | 25 (177) | 8.71 (68.9) | –13.8 (78.0) | –42.0 (69.4) | –21.64 (–35.7 to –7.59); 0.003 | –47.7 (–61.6 to –33.8); < 0.001 | –25.5 (–39.0 to –12.0); < 0.001 |
| Standing time | |||||||||
| 3-month follow-upc | 26 (186) | 26 (175) | 25 (176) | 6.06 (52.1) | 12.3 (49.0) | 82.9 (71.4) | 4.72 (–10.9 to 20.3); 0.553 | 74.4 (58.7 to 89.9); < 0.001 | N/A |
| 12-month follow-upd | 26 (176) | 26 (167) | 25 (177) | –3.16 (50.3) | 11.1 (60.9) | 58.5 (76.5) | 13.0 (–0.87 to 26.8); 0.066 | 58.8 (45.1 to 72.5); < 0.001 | N/A |
| Stepping time | |||||||||
| 3-month follow-upc | 26 (186) | 26 (175) | 25 (176) | 0.05 (14.9) | 2.03 (15.5) | 2.53 (15.8) | 2.39 (–1.09 to 5.89); 0.179 | 2.79 (–0.72 to 6.29); 0.119 | N/A |
| 12-month follow-upd | 26 (176) | 26 (167) | 25 (177) | –1.04 (14.0) | 2.26 (15.0) | 4.64 (19.9) | 3.44 (–0.19 to 7.06); 0.063 | 5.39 (1.81 to 8.98); 0.003 | N/A |
| Workday variables (minutes/day) | |||||||||
| Sitting time | |||||||||
| 3-month follow-upe | 26 (187) | 26 (175) | 25 (176) | –5.47 (83.0) | –31.0 (85.4) | –92.4 (84.2) | –20.4 (–39.5 to –1.31); 0.036 | –85.8 (–104.9 to –66.7); < 0.001 | –65.2 (–86.1 to –44.2); < 0.001 |
| 12-month follow-upf | 26 (176) | 26 (165) | 25 (177) | 6.96 (83.2) | –15.9 (88.0) | –67.5 (95.3) | –19.6 (–36.8 to –2.51); 0.025 | –71.1 (–87.9 to –54.3); < 0.001 | –51.4 (–69.1 to –33.8); < 0.001 |
| Prolonged sitting | |||||||||
| 3-month follow-upe | 26 (187) | 26 (175) | 25 (176) | 5.15 (94.8) | –34.0 (93.0) | –64.0 (93.2) | –34.4 (–52.9 to –16.0); < 0.001 | –67.3 (–85.8 to –48.9); < 0.001 | –33.7 (–53.0 to –14.4); 0.001 |
| 12-month follow-upf | 26 (176) | 26 (165) | 25 (177) | 18.6 (86.8) | –11.9 (96.7) | –41.6 (85.3) | –26.9 (–44.1 to –9.59); 0.002 | –54.6 (–71.5 to –37.7); < 0.001 | –27.6 (–44.6 to –10.6); 0.001 |
| Standing time | |||||||||
| 3-month follow-upe | 26 (187) | 26 (175) | 25 (176) | –4.39 (61.0) | 2.01 (59.3) | 50.3 (84.5) | 7.56 (–8.73 to 23.9); 0.363 | 72.5 (56.2 to 88.8); < 0.001 | N/A |
| 12-month follow-upf | 26 (176) | 26 (165) | 25 (177) | –2.24 (61.5) | 4.96 (68.8) | 50.0 (81.3) | 6.99 (–8.11 to 22.1); 0.364 | 53.0 (38.1 to 67.8); < 0.001 | N/A |
| Stepping time | |||||||||
| 3-month follow-upe | 26 (187) | 26 (175) | 25 (176) | –4.00 (20.7) | 1.82 (24.3) | –0.97 (24.0) | 5.97 (1.54 to 10.4); 0.008 | 3.58 (–0.85 to 8.00); 0.113 | N/A |
| 12-month follow-upf | 26 (176) | 26 (165) | 25 (177) | –3.53 (21.3) | 0.47 (25.5) | 0.11 (28.6) | 3.63 (–1.98 to 9.24); 0.204 | 3.27 (–2.25 to 8.78); 0.245 | N/A |
| Non-workday variables (minutes/day) | |||||||||
| Sitting time | |||||||||
| 3-month follow-upg | 26 (170) | 26 (166) | 25 (162) | –4.94 (103.6) | –2.69 (111.2) | –21.2 (116.7) | 6.9 (–13.3 to 27.2); 0.502 | –12.33 (–32.8 to 8.12); 0.237 | N/A |
| 12-month follow-uph | 26 (160) | 26 (152) | 25 (156) | 16.6 (114.4) | 1.80 (110.6) | –11.4 (106.9) | –4.66 (–26.4 to –17.1); 0.675 | –19.8 (–41.3 to 1.83); 0.073 | N/A |
| Prolonged sitting | |||||||||
| 3-month follow-upg | 26 (170) | 26 (166) | 25 (162) | 6.45 (113.3) | –2.71 (117.9) | –6.54 (120.6) | –3.06 (–25.5 to 19.4); 0.789 | –5.79 (–28.4 to 16.8); 0.615 | N/A |
| 12-month follow-uph | 26 (160) | 26 (152) | 25 (156) | 27.3 (126.6) | –4.19 (122.7) | 1.20 (122.3) | –21.8 (–48.9 to 5.29); 0.115 | 15.6 (–42.5 to 11.2); 0.254 | N/A |
| Standing time | |||||||||
| 3-month follow-upg | 26 (170) | 26 (166) | 25 (162) | 4.56 (66.7) | 3.44 (74.6) | 8.34 (75.4) | –4.54 (–19.2 to 10.2); 0.545 | 4.85 (–9.93 to 19.6); 0.520 | N/A |
| 12-month follow-uph | 26 (160) | 26 (152) | 25 (156) | –5.25 (74.5) | –6.57 (79.4) | –2.13 (79.4) | –3.85 (–19.3 to 11.6); 0.625 | 4.87 (–10.4 to 20.2); 0.533 | N/A |
| Stepping time | |||||||||
| 3-month follow-upg | 26 (170) | 26 (166) | 25 (162) | 0.32 (39.5) | –2.61 (48.9) | –0.15 (45.7) | –0.61 (–9.94 to 8.69); 0.896 | –1.61 (–11.0 to 7.76); 0.736 | N/A |
| 12-month follow-uph | 26 (160) | 26 (152) | 25 (156) | –2.81 (40.2) | –4.10 (52.6) | –0.56 (43.4) | 1.39 (–6.99 to 9.78); 0.744 | 1.52 (–6.82 to 9.85); 0.721 | N/A |
In favour of the SWAL plus desk group, there were differences in comparison with the control group in daily sitting time and sitting time during work hours at 3 months, sitting time during workdays at 3 and 12 months, prolonged sitting time and standing time for daily, work hours and workdays at 3 and 12 months, as well as stepping time during work hours at 12 months.
Other key activPAL-assessed outcomes: moderate or vigorous physical activity, number of steps and number of sit-to-upright transitions
For daily variables, all groups showed a small reduction in the number of steps per day, time spent in MVPA stepping and number of sit-to-upright transitions at 3 and 12 months (Table 8). During work hours, there were small favourable changes for both intervention groups for the number of steps per day and time spent in MVPA, in comparison with the control group, at 3 and 12 months. The pattern of results for each variable was less consistent on workdays and non-workdays.
| Variable | Baseline value | 3 months | 12 months | Change at 3 months | Change at 12 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | |
| Daily, n | 257 | 237 | 229 | 213 | 206 | 207 | 184 | 182 | 193 | 210 | 200 | 202 | 183 | 177 | 187 |
| MVPA stepping (minute/day) | 27.1 (17.4) | 27.0 (18.8) | 26.5 (17.5) | 25.9 (16.3) | 27.4 (18.9) | 25.9 (17.6) | 26.8 (17.1) | 28.1 (20.0) | 27.4 (18.8) | –1.75 (12.9) | –0.45 (14.5) | –1.04 (12.6) | –2.23 (12.8) | –0.77 (14.5) | –0.22 (15.0) |
| Number of steps (steps/day) | 9291.0 (3209.1) | 9286.4 (3121.3) | 9230.9 (3228.7) | 8993.1 (2853.6) | 9356.2 (3082.4) | 9175.5 (3206.2) | 9158.8 (2975.4) | 9480.6 (3299.6) | 9328.6 (3253.0) | –375.2 (2114.7) | –8.62 (2516.3) | –189.8 (2241.8) | –481.9 (2013.4) | –118.9 (2650.6) | –124.4 (2608.9) |
| Number of sit-to-upright transition (number/day) | 53.7 (13.8) |
53.6 (13.5) | 52.3 (14.1) | 53.0 (13.5) | 53.0 (14.6) | 48.7 (13.8) | 53.0 (13.8) | 52.9 (12.8) | 48.9 (12.1) | –0.94 (9.02) | –0.35 (10.2) | –3.64 (9.92) | –0.86 (9.37) | –0.55 (9.95) | –3.43 (8.60) |
| Work hours, n | 243 | 226 | 218 | 195 | 184 | 187 | 183 | 177 | 190 | 186 | 175 | 176 | 176 | 167 | 177 |
| MVPA stepping (minute/day) | 13.0 (8.24) | 12.5 (8.42) | 12.8 (9.51) | 12.9 (8.80) | 13.1 (9.46) | 13.4 (9.98) | 12.9 (10.9) | 13.5 (9.66) | 14.6 (13.4) | –0.20 (7.68) | 0.68 (8.40) | 0.01 (8.61) | –0.54 (11.8) | 0.36 (8.86) | 1.43 (14.8) |
| Number of steps (steps/day) | 3822.7 (1452.2) | 3885.7 (1434.3) | 3835.3 (1686.2) | 3803.6 (1590.0) | 4076.4 (1719.7) | 4069.1 (1634.4) | 3772.5 (1396.9) | 4157.3 (1622.4) | 4181.4 (1919.5) | –11.3 (1421.0) | 194.9 (1501.2) | 157.0 (1508.7) | –123.7 (1415.1) | 202.3 (1448.3) | 308.6 (1879.9) |
| Number of sit-to-upright transition (number/day) | 27.5 (10.4) | 28.2 (11.0) | 25.8 (9.48) | 28.2 (11.2) | 28.3 (9.8) | 23.9 (8.7) | 26.9 (10.3) | 28.0 (11.0) | 24.7 (9.69) | 0.27 (8.19) | 0.57 (7.94) | –2.41 (8.37) | –1.60 (8.27) | 0.26 (9.40) | –1.29 (9.45) |
| Workdays, n | 244 | 226 | 218 | 196 | 184 | 187 | 183 | 175 | 190 | 187 | 175 | 176 | 176 | 165 | 177 |
| MVPA stepping (minute/day) | 30.2 (19.0) | 28.9 (20.8) | 29.2 (20.0) | 29.1 (18.6) | 29.6 (19.9) | 28.9 (18.2) | 29.9 (20.0) | 30.8 (22.4) | 30.2 (21.7) | –1.62 (13.0) | 0.26 (14.7) | –0.50 (13.9) | –2.03 (15.5) | 0.22 (16.0) | 0.01 (17.6) |
| Number of steps (steps/day) | 9359.2 (3241.9) | 9202.8 (3133.4) | 9293.4 (3453.9) | 8902.4 (3081.0) | 9393.4 (3248.4) | 9343.9 (3262.7) | 9196.2 (3166.5) | 9498.0 (3377.1) | 9485.9 (3586.7) | –411.9 (2042.7) | 130.0 (2391.2) | –136.7 (2385.4) | –410.2 (2228.7) | 52.1 (2645.1) | –35.7 (2886.6) |
| Number of sit-to-upright transition (number/day) | 55.8 (14.4) | 55.2 (14.9) | 53.3 (14.3) | 55.1 (15.6) | 55.8 (15.1) | 50.0 (13.7) | 55.0 (14.0) | 54.4 (14.3) | 50.3 (13.3) | –0.62 (9.50) | 1.19 (10.8) | –4.09 (11.5) | –1.24 (9.82) | –0.02 (12.1) | –3.43 (10.5) |
| Non-workdays, n | 236 | 219 | 203 | 182 | 178 | 183 | 170 | 163 | 178 | 170 | 166 | 162 | 160 | 152 | 156 |
| MVPA stepping (minute/day) | 20.1 (21.2) | 23.8 (24.4) | 20.4 (22.4) | 22.6 (22.8) | 22.3 (26.1) | 20.0 (28.7) | 20.7 (21.1) | 22.8 (24.1) | 22.8 (23.4) | 0.72 (24.3) | –1.91 (26.9) | –0.09 (25.2) | –1.48 (22.5) | –2.57 (26.1) | 1.84 (23.1) |
| Number of steps (steps/day) | 9051.8 (4150.4) | 9467.5 (4979.4) | 8941.5 (4166.9) | 9333.3 (3978.0) | 9127.1 (4157.8) | 8869.9 (5339.7) | 9108.7 (4008.0) | 9256.3 (4503.5) | 9166.1 (4063.1) | –17.0 (3939.0) | –407.9 (4982.4) | –51.4 (4419.1) | –343.8 (3813.8) | –482.9 (5269.2) | 78.5 (4046.5) |
| Number of sit-to-upright transition (number/day) | 51.8 (16.8) | 50.8 (15.8) | 50.3 (17.2) | 52.3 (35.9) | 52.2 (33.4) | 54.3 (58.6) | 49.8 (18.6) | 50.1 (14.4) | 47.2 (13.9) | 1.52 (36.1) | 1.70 (34.1) | 4.48 (62.1) | –0.62 (13.9) | –0.32 (13.4) | –2.36 (13.2) |
Axivity-assessed variables: light and moderate or vigorous physical activity, sleep duration and sleep efficiency
For daily and workday variables, there were no consistent pattern of results or noticeable changes in behaviour between groups (Table 9). During work hours, there were small favourable changes in light physical activity for the SWAL plus desk group compared with the control group at 12-month follow-up. On non-workdays, there were small unfavourable changes in light physical activity for the SWAL plus desk group compared with the control group at 3 and 12 months. There were no noticeable changes in sleep duration and efficiency between groups.
| Variable | Baseline value | 3 months | 12 months | Change at 3 months | Change at 12 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | |
| Daily, n | 255 | 235 | 228 | 207 | 205 | 208 | 185 | 178 | 191 | 203 | 197 | 202 | 182 | 170 | 184 |
| Light activity (minutes/day) | 182.8 (42.8) | 179.7 (49.2) | 186.4 (58.9) | 189.5 (58.8) | 181.8 (50.6) | 182.9 (51.8) | 185.1 (59.8) | 181.0 (54.9) | 186.5 (55.3) | 4.35 (46.0) | 1.60 (51.0) | –2.99 (57.5) | 1.73 (60.0) | –0.23 (53.9) | 0.73 (63.7) |
| MVPA (minutes/day) | 44.9 (24.3) | 42.6 (24.5) | 43.3 (23.9) | 45.8 (25.9) | 46.3 (29.0) | 44.1 (25.7) | 48.1 (36.6) | 48.0 (31.8) | 44.8 (26.0) | 0.22 (18.6) | 2.52 (24.8) | –0.02 (18.3) | 1.62 (30.9) | 2.41 (26.4) | 1.05 (20.1) |
| Sleep duration (minutes/day) | 456.8 (54.7) | 457.5 (55.8) | 448.0 (54.2) | 459.0 (58.4) | 461.7 (50.8) | 456.2 (57.0) | 454.1 (51.8) | 458.2 (50.0) | 455.3 (57.3) | 8.54 (53.5) | –1.17 (49.7) | 8.28 (53.7) | 1.64 (51.6) | –3.56 (48.9) | 9.50 (55.7) |
| Sleep efficiency (per day)a | 0.89 (0.05) | 0.88 (0.05) | 0.89 (0.05) | 0.89 (0.05) | 0.89 (0.05) | 0.88 (0.08) | 0.89 (0.04) | 0.89 (0.05) | 0.89 (0.07) | –0.00 (0.05) | 0.00 (0.04) | –0.01 (0.08) | 0.00 (0.04) | 0.00 (0.04) | –0.00 (0.05) |
| Work hours, n | 239 | 224 | 213 | 192 | 180 | 188 | 174 | 155 | 177 | 181 | 173 | 171 | 162 | 146 | 159 |
| Light activity (minutes/day) | 65.9 (20.8) | 68.7 (26.2) | 64.0 (26.6) | 70.0 (29.1) | 69.1 (23.3) | 66.6 (23.2) | 66.9 (23.0) | 70.5 (27.1) | 70.0 (28.0) | 2.73 (27.6) | 0.55 (21.5) | 3.76 (24.5) | 1.22 (23.8) | 3.23 (24.9) | 7.23 (28.7) |
| MVPA (minutes/day) | 17.7 (11.0) | 16.7 (9.6) | 17.8 (11.4) | 18.7 (11.9) | 19.9 (12.2) | 18.4 (11.1) | 17.7 (11.9) | 19.5 (12.1) | 18.7 (12.1) | 0.80 (9.61) | 3.01 (10.1) | 0.30 (9.69) | –0.12 (10.2) | 2.10 (9.63) | 1.12 (12.0) |
| Workdays, n | 240 | 226 | 213 | 192 | 187 | 188 | 182 | 171 | 188 | 182 | 179 | 171 | 171 | 160 | 170 |
| Light activity (minutes/day) | 174.8 (41.6) | 173.0 (48.7) | 174.2 (57.5) | 177.6 (57.5) | 175.7 (49.1) | 170.7 (41.9) | 178.0 (56.7) | 174.4 (56.9) | 179.4 (53.9) | 0.95 (44.5) | 1.91 (49.8) | –3.88 (50.0) | 2.80 (58.4) | 0.03 (58.0) | 4.77 (64.6) |
| MVPA (minutes/day) | 47.3 (25.0) | 44.0 (24.1) | 46.1 (25.7) | 48.2 (27.5) | 49.2 (29.1) | 46.7 (25.7) | 49.6 (34.6) | 50.0 (32.8) | 47.2 (27.5) | 0.15 (17.8) | 3.88 (23.6) | –0.16 (19.0) | 0.87 (28.9) | 3.91 (25.7) | 0.65 (22.0) |
| Sleep duration (minutes/day) | 452.5 (65.9) | 457.8 (68.1) | 445.6 (65.7) | 440.9 (56.5) | 446.3 (60.2) | 437.3 (56.9) | 437.6 (55.8) | 451.3 (58.3) | 436.9 (59.8) | –7.85 (69.7) | –11.7 (64.8) | –2.43 (71.4) | –8.46 (61.1) | –10.8 (65.2) | –5.01 (66.1) |
| Sleep efficiency (per day)a | 0.89 (0.05) | 0.88 (0.06) | 0.89 (0.05) | 0.89 (0.05) | 0.89 (0.05) | 0.88 (0.08) | 0.89 (0.05) | 0.89 (0.06) | 0.89 (0.06) | –0.00 (0.04) | 0.01 (0.05) | –0.01 (0.07) | 0.00 (0.04) | 0.00 (0.05) | 0.00 (0.05) |
| Non-workdays, n | 253 | 225 | 221 | 195 | 194 | 200 | 176 | 170 | 175 | 189 | 180 | 189 | 171 | 159 | 167 |
| Light activity (minutes/day) | 197.7 (55.9) | 188.7 (55.3) | 204.3 (64.9) | 201.1 (54.3) | 186.9 (54.3) | 199.6 (60.5) | 202.3 (74.1) | 190.9 (60.6) | 196.0 (62.0) | 1.24 (53.5) | 0.44 (48.8) | –7.60 (65.5) | 3.85 (74.2) | 0.43 (51.6) | –10.44 (64.7) |
| MVPA (minutes/day) | 39.4 (31.4) | 40.6 (36.8) | 38.2 (29.2) | 41.7 (32.8) | 40.8 (35.8) | 38.6 (37.3) | 44.8 (49.8) | 43.9 (38.2) | 39.8 (30.1) | 0.89 (34.0) | –1.13 (39.7) | 0.31 (32.8) | 3.38 (48.4) | 0.99 (41.9) | –0.22 (26.3) |
| Light activity (minutes/day) | 462.6 (66.3) | 462.5 (70.2) | 456.6 (65.3) | 484.3 (78.9) | 485.3 (69.4) | 479.6 (75.8) | 479.9 (71.9) | 479.5 (72.6) | 482.8 (82.4) | 26.1 (78.0) | 10.4 (78.5) | 21.2 (84.9) | 20.6 (81.6) | 9.3 (82.2) | 28.5 (90.4) |
| MVPA (minutes/day) | 0.88 (0.05) | 0.88 (0.06) | 0.89 (0.04) | 0.89 (0.06) | 0.88 (0.05) | 0.88 (0.05) | 0.89 (0.05) | 0.89 (0.05) | 0.88 (0.07) | 0.00 (0.06) | –0.01 (0.05) | –0.00 (0.05) | 0.01 (0.05) | 0.00 (0.05) | 0.00 (0.07) |
Self-reported lifestyle behaviours: sleep, self-reported sitting and physical activity, dietary behaviours and alcohol intake
The self-reported sitting and physical activity variables appear to follow a similar pattern to the activPAL-assessed sitting and physical activity variables, with favourable changes in the percentage of time sitting, prolonged sitting and standing for both intervention groups at 3- and 12-month follow-up in comparison with the control group (Table 10). There were no noticeable changes in other variables between groups.
| Variable | Baseline value | 3 months | 12 months | Change at 3 months | Change at 12 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | |
| Sleep quality (self reported)a | 6.76 (3.25) | 6.79 (3.32) | 6.95 (3.15) | 6.23 (3.14) | 6.48 (3.25) | 6.28 (3.08) | 6.64 (3.30) | 6.55 (3.25) | 6.62 (3.12) | –0.43 (2.16) | –0.24 (2.42) | –0.46 (2.85) | –0.03 (2.55) | –0.23 (2.74) | –0.17 (2.70) |
| Typical working week | |||||||||||||||
| Number of workdays | 4.83 (0.54) | 4.84 (0.70) | 4.81 (0.60) | 4.86 (0.51) | 4.83 (0.71) | 4.90 (0.54) | 4.83 (0.59) | 4.86 (0.66) | 4.90 (0.58) | 0.07 (0.54) | –0.02 (0.56) | 0.09 (0.61) | 0.01 (0.40) | 0.04 (0.62) | 0.08 (0.63) |
| Number of hours worked per day | 7.53 (0.57) | 7.62 (0.76) | 7.59 (0.74) | 7.50 (0.66) | 7.55 (0.73) | 7.59 (0.71) | 7.52 (0.66) | 7.60 (0.78) | 7.53 (0.65) | –0.05 (0.51) | –0.04 (0.45) | –0.00 (0.59) | –0.03 (0.54) | 0.01 (0.69) | –0.05 (0.68) |
| Per cent of day spent in office | 88.1 (15.2) | 84.1 (16.6) | 88.3 (13.5) | 88.3 (15.1) | 82.4 (17.7) | 87.0 (15.4) | 86.3 (16.7) | 83.4 (17.7) | 85.2 (15.8) | –0.73 (15.7) | –1.48 (16.7) | –1.71 (16.8) | –1.76 (13.6) | –1.64 (16.0) | –4.24 (15.1) |
| Per cent of day spent at desk | 81.3 (15.7) | 76.1 (18.7) | 81.0 (15.7) | 81.1 (16.6) | 74.9 (18.7) | 80.2 (15.1) | 79.4 (17.7) | 74.7 (19.2) | 78.2 (18.6) | –1.21 (14.7) | –1.09 (15.8) | –1.10 (14.3) | –1.69 (15.2) | –0.98 (16.8) | –2.55 (16.9) |
| Self-reported behaviours | |||||||||||||||
| Workday sitting (%) | 81.1 (11.2) | 78.5 (13.4) | 82.0 (12.2) | 79.9 (13.1) | 73.2 (14.4) | 58.7 (17.9) | 80.4 (11.7) | 73.3 (16.4) | 62.1 (18.2) | –1.99 (11.8) | –5.10 (12.6) | –23.8 (20.5) | –1.34 (11.9) | –5.13 (14.7) | –19.9 (21.2) |
| Workday standing (%) | 6.76 (5.87) | 7.64 (6.17) | 6.29 (5.70) | 7.70 (8.30) | 10.5 (7.75) | 28.4 (16.7) | 7.14 (6.81) | 10.7 (10.4) | 23.1 (17.1) | 1.29 (7.45) | 2.79 (7.72) | 22.7 (17.9) | 0.63 (7.42) | 2.92 (10.7) | 16.9 (18.9) |
| Workday walking (%) | 12.3 (7.50) | 14.0 (9.67) | 11.7 (8.19) | 12.6 (8.04) | 16.3 (9.96) | 12.9 (7.57) | 12.5 (7.55) | 16.2 (10.9) | 15.4 (9.71) | 0.85 (8.27) | 2.30 (9.64) | 0.94 (8.78) | 0.67 (8.57) | 2.33 (9.42) | 3.45 (10.5) |
| Workday prolonged sitting (%) | 68.2 (24.7) | 67.9 (24.3) | 71.8 (23.4) | 67.2 (22.6) | 62.8 (23.6) | 54.3 (26.0) | 66.8 (22.4) | 62.9 (23.2) | 60.9 (25.9) | –1.34 (23.3) | –6.49 (26.6) | –17.5 (28.9) | –2.07 (23.3) | –5.90 (26.7) | –11.5 (28.6) |
| Sitting while working (minutes/week) | 369.8 (175.8) | 358.9 (161.2) | 363.7 (170.2) | 350.6 (118.1) | 330.2 (156.4) | 294.0 (110.7) | 365.9 (118.7) | 324.4 (173.3) | 280.9 (121.3) | –35.0 (206.3) | –28.3 (229.8) | –70.8 (207.7) | –9.96 (169.7) | –38.1 (226.2) | –62.9 (149.6) |
| Number sitting breaks per hour | 1.64 (1.18) | 2.01 (1.50) | 1.72 (1.39) | 1.95 (1.38) | 2.15 (1.42) | 2.09 (–1.32) | 1.88 (1.32) | 2.01 (1.37) | 2.18 (1.39) | 0.37 (1.43) | 0.16 (1.63) | 0.34 (1.55) | 0.31 (1.52) | 0.08 (1.84) | 0.43 (1.58) |
| Weekdays (hours/weekday) | |||||||||||||||
| Sitting for transport | 0.93 (0.67) | 1.08 (0.76) | 0.93 (0.68) | 0.93 (0.86) | 1.03 (0.75) | 1.00 (1.46) | 0.84 (0.62) | 0.98 (0.87) | 0.97 (1.38) | 0.00 (0.87) | –0.04 (0.73) | 0.01 (0.65) | –0.04 (0.55) | 0.03 (0.85) | 0.10 (1.42) |
| Sitting for TV viewing | 1.82 (1.33) | 1.70 (1.22) | 1.74 (1.17) | 1.64 (1.11) | 1.61 (1.16) | 1.71 (1.22) | 1.59 (0.94) | 1.65 (1.09) | 1.64 (1.21) | –0.13 (1.11) | –0.10 (1.02) | –0.04 (1.00) | –0.25 (1.17) | –0.12 (1.13) | –0.07 (1.11) |
| Sitting for computer use | 1.16 (1.95) | 1.03 (1.40) | 1.07 (1.61) | 1.02 (1.39) | 1.26 (1.76) | 1.13 (1.81) | 1.06 (1.77) | 1.10 (1.74) | 1.22 (1.72) | –0.13 (1.70) | 0.11 (1.46) | 0.03 (2.05) | –0.01 (2.29) | 0.14 (2.00) | 0.22 (2.14) |
| Sitting other activities | 0.65 (0.93) | 0.72 (0.87) | 0.78 (1.48) | 0.55 (0.71) | 0.46 (0.81) | 0.54 (0.88) | 0.79 (1.42) | 0.56 (0.80) | 0.73 (1.73) | –0.08 (1.03) | –0.38 (1.15) | –0.24 (1.41) | 0.07 (1.35) | –0.44 (0.96) | –0.03 (1.67) |
| All sitting | 4.63 (2.42) | 4.30 (2.50) | 4.60 (3.19) | 3.86 (1.88) | 4.28 (2.63) | 4.13 (2.72) | 4.27 (2.82) | 4.26 (2.52) | 4.42 (3.55) | –0.55 (1.68) | –0.41 (2.63) | –0.67 (3.69) | –0.37 (2.63) | –0.63 (2.48) | 0.24 (4.16) |
| Weekends (hours/weekend day) | |||||||||||||||
| Sitting for transport | 0.90 (0.75) | 1.07 (1.14) | 1.10 (1.24) | 1.22 (2.15) | 0.94 (0.85) | 0.96 (0.82) | 0.93 (0.67) | 1.19 (1.63) | 0.91 (0.92) | 0.39 (2.34) | –0.06 (1.05) | –0.20 (1.30) | 0.15 (0.86) | 0.21 (2.07) | –0.22 (1.31) |
| Sitting for TV viewing | 2.79 (1.82) | 2.74 (1.90) | 2.74 (1.98) | 2.80 (2.12) | 2.61 (1.84) | 2.78 (1.94) | 2.72 (1.52) | 2.62 (1.64) | 2.98 (2.34) | 0.13 (1.71) | –0.19 (2.02) | 0.12 (2.10) | –0.15 (1.77) | –0.03 (1.51) | 0.14 (2.34) |
| Sitting for computer use | 1.38 (1.50) | 1.34 (1.30) | 1.28 (1.43) | 1.35 (1.60) | 1.41 (1.75) | 1.43 (1.83) | 1.26 (1.23) | 1.32 (1.38) | 1.54 (2.04) | 0.18 (1.28) | 0.07 (1.72) | 0.12 (1.92) | 0.09 (1.38) | 0.08 (1.48) | 0.15 (1.47) |
| Sitting other activities | 1.26 (1.40) | 1.52 (2.01) | 1.61 (2.33) | 1.45 (1.92) | 1.06 (1.76) | 1.55 (2.81) | 1.36 (2.03) | 0.88 (1.29) | 1.73 (3.34) | 0.11 (2.08) | –0.65 (2.18) | 0.03 (3.66) | –0.31 (2.16) | –1.20 (2.18) | –0.20 (2.48) |
| All sitting | 6.40 (2.88) | 6.31 (3.46) | 6.74 (3.98) | 6.40 (3.07) | 5.73 (3.50) | 6.36 (4.21) | 6.28 (3.03) | 6.00 (2.98) | 6.31 (3.81) | 0.32 (3.03) | –0.44 (4.00) | –0.92 (4.15) | –0.22 (3.25) | –0.81 (4.06) | –0.06 (3.95) |
| Weekly (hour/day) | |||||||||||||||
| Sitting for transport | 0.92 (0.57) | 1.07 (0.68) | 0.98 (0.70) | 1.01 (0.88) | 1.03 (0.65) | 0.98 (1.10) | 0.86 (0.53) | 1.05 (0.82) | 0.98 (1.10) | 0.11 (0.92) | –0.03 (0.55) | –0.07 (0.62) | 0.02 (0.50) | 0.06 (0.77) | 0.02 (1.16) |
| Sitting for TV viewing | 2.08 (1.31) | 1.97 (1.27) | 2.04 (1.22) | 1.98 (1.34) | 1.92 (1.21) | 1.99 (1.23) | 1.92 (0.99) | 1.93 (1.13) | 2.04 (1.35) | –0.04 (1.14) | –0.12 (1.08) | –0.01 (1.09) | –0.20 (1.21) | –0.07 (1.04) | –0.03 (1.19) |
| Sitting for computer use | 1.26 (1.63) | 1.09 (1.16) | 1.11 (1.32) | 1.11 (1.22) | 1.32 (1.47) | 1.22 (1.63) | 1.11 (1.44) | 1.18 (1.44) | 1.33 (1.51) | –0.03 (1.34) | 0.12 (1.31) | 0.10 (1.66) | –0.03 (1.83) | 0.16 (1.59) | 0.22 (1.73) |
| Sitting other activities | 0.79 (0.96) | 0.93 (1.11) | 1.01 (1.67) | 0.80 (0.99) | 0.64 (1.02) | 0.84 (1.29) | 0.94 (1.57) | 0.65 (0.90) | 0.99 (1.94) | –0.02 (1.25) | –0.44 (1.34) | –0.16 (1.96) | –0.03 (1.53) | –0.69 (1.24) | –0.13 (1.75) |
| All sitting | 5.09 (2.13) | 4.74 (2.30) | 5.18 (3.12) | 4.62 (1.82) | 4.69 (2.42) | 4.76 (2.89) | 4.83 (2.72) | 4.79 (2.24) | 5.02 (3.36) | –0.35 (1.85) | –0.38 (2.35) | –0.73 (3.36) | –0.39 (2.56) | –0.69 (2.25) | 0.35 (3.62) |
| Self-reported dietary behaviours (≥ 1/day), % (n) | |||||||||||||||
| Snack frequency | 28.3 (70) | 33.3 (77) | 31.5 (70) | 30.5 (54) | 33.3 (65) | 26.2 (50) | 29.1 (50) | 34.0 (55) | 26.2 (48) | 2.2 | 0.0 | –5.3 | 0.8 | 0.7 | –5.3 |
| Soft drink consumption | 11.3 (28) | 18.3 (42) | 18.7 (42) | 11.9 (21) | 12.2 (24) | 11.0 (23) | 9.1 (16) | 19.8 (32) | 14.1 (26) | 0.6 | –6.1 | –6.8 | –2.2 | 1.5 | –4.6 |
| Fruit consumption | 70.8 (177) | 69.6 (160) | 68.2 (152) | 67.2 (119) | 73.6 (145) | 73.8 (141) | 73.7 (129) | 64.2 (104) | 74.3 (136) | –3.6 | 4.0 | 5.6 | 2.9 | –5.4 | 6.1 |
| Vegetable consumption | 80.8 (202) | 72.9 (167) | 75.3 (168) | 79.1 (140) | 80.7 (159) | 74.7 (142) | 79.9 (139) | 79.0 (128) | 78.7 (144) | –1.7 | 7.8 | –0.6 | –0.9 | 6.1 | 3.4 |
| Alcohol intake | |||||||||||||||
| Total units/week | 8.70 (8.09) | 9.91 (8.58) | 9.84 (8.98) | 8.40 (8.31) | 11.1 (13.0) | 8.56 (8.47) | 8.39 (8.81) | 9.83 (8.29) | 8.26 (7.02) | 0.31 (5.27) | 0.84 (10.2) | –0.78 (7.43) | –0.43 (4.89) | –0.68 (5.75) | –1.63 (7.07) |
Physical and psychological health
Cardiometabolic health
For cardiometabolic health, there were no between-group differences in the mean changes for any variables at follow-up (Table 11).
| Variable | Baseline value | 3 months | 12 months | Change at 3 months | Change at 12 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | |
| Adiposity | |||||||||||||||
| Weight (kgs) | 71.6 (17.1) | 75.1 (18.1) | 73.8 (17.6) | 71.9 (16.4) | 74.2 (17.7) | 73.4 (16.9) | 71.3 (17.1) | 74.8 (16.8) | 73.9 (17.1) | –0.01 (2.16) | –0.17 (2.87) | –0.03 (2.91) | 0.05 (3.25) | 0.24 (4.15) | 0.31 (4.30) |
| Waist circumference (cm) | 86.6 (13.7) | 89.0 (15.0) | 89.2 (14.4) | 86.1 (13.3) | 88.6 (14.5) | 87.7 (13.1) | 85.4 (14.2) | 88.4 (14.1) | 87.3 (13.7) | –0.64 (4.85) | –0.03 (5.44) | –1.25 (5.47) | –0.94 (5.92) | –0.61 (6.67) | –1.58 (6.80) |
| Body fat (%) | 32.4 (9.36) | 33.7 (9.44) | 32.3 (9.27) | 32.6 (8.59) | 33.3 (9.22) | 32.5 (9.49) | 33.0 (8.42) | 33.4 (9.19) | 32.6 (9.53) | 0.49 (3.74) | 0.01 (3.58) | 0.46 (3.33) | –0.07 (4.27) | 0.46 (2.91) | 0.53 (3.37) |
| BMI (kg/m2) | 25.8 (5.60) | 27.3 (6.42) | 26.4 (5.68) | 25.6 (5.45) | 27.0 (6.38) | 26.2 (5.30) | 25.7 (5.61) | 27.1 (5.67) | 26.4 (5.50) | –0.01 (0.78) | –0.07 (1.08) | –0.02 (1.09) | 0.01 (1.20) | 0.09 (1.53) | 0.10 (1.55) |
| Blood pressure | |||||||||||||||
| Systolic blood pressure (mmHg) | 116.9 (14.5) | 119.0 (17.3) | 119.2 (16.6) | 116.5 (15.9) | 117.0 (14.6) | 116.9 (16.7) | 16.3 (15.1) | 116.5 (15.2) | 117.1 (16.0) | –1.96 (9.99) | –1.04 (9.93) | –2.09 (11.3) | –1.44 (10.8) | –1.78 (10.4) | –2.08 (11.8) |
| Diastolic blood pressure (mmHg) | 78.1 (9.46) | 79.4 (10.7) | 79.9 (11.1) | 77.6 (9.68) | 78.9 (10.4) | 77.7 (10.49) | 78.8 (9.51) | 79.2 (10.4) | 78.7 (9.73) | –1.16 (6.75) | –0.28 (6.29) | –1.96 (7.42) | 0.18 (6.91) | 0.08 (7.12) | –1.07 (7.85) |
| Biochemical | |||||||||||||||
| HbA1c (mmol/mol) | 33.5 (5.77) | 33.8 (4.99) | 34.5 (5.41) | 35.0 (7.31) | 34.3 (5.08) | 35.6 (2.92) | 36.2 (6.16) | 35.7 (5.27) | 36.6 (5.92) | 1.11 (4.06) | 0.40 (2.94) | 0.86 (3.38) | 2.42 (3.73) | 1.67 (3.10) | 1.84 (4.10) |
| HbA1c (%) | 5.22 (0.53) | 5.24 (0.46) | 5.31 (0.50) | 5.35 (0.67) | 5.28 (0.46) | 5.41 (0.54) | 5.46 (0.56) | 5.42 (0.48) | 5.50 (0.54) | 0.10 (0.37) | 0.04 (0.27) | 0.08 (0.31) | 0.22 (0.34) | 0.15 (0.28) | 0.17 (0.37) |
| Total cholesterol (mmol/l) | 4.64 (1.04) | 4.71 (1.07) | 4.67 (1.06) | 4.46 (1.01) | 4.68 (1.00) | 4.58 (1.04) | 4.38 (0.92) | 4.48 (0.85) | 4.35 (0.93) | –0.19 (0.80) | –0.05 (0.79) | –0.09 (0.79) | –0.28 (0.88) | –0.29 (0.89) | –0.34 (0.81) |
| HDL cholesterol (mmol/mol) | 1.46 (0.38) | 1.41 (0.42) | 1.42 (0.39) | 1.45 (0.35) | 1.43 (0.37) | 1.45 (0.37) | 1.43 (0.31) | 1.39 (0.34) | 1.40 (0.35) | –0.01 (0.26) | 0.01 (0.29) | 0.02 (0.20) | –0.05 (0.29) | –0.02 (0.29) | –0.03 (0.23) |
| LDL cholesterol (mmol/mol) | 2.52 (0.96) | 2.65 (1.26) | 2.56 (1.00) | 2.30 (0.84) | 2.49 (0.92) | 2.34 (0.97) | 2.35 (0.85) | 2.51 (0.80) | 2.30 (0.87) | –0.19 (0.75) | –0.19 (1.15) | –0.21 (0.93) | –0.15 (0.93) | –0.29 (1.28) | –0.29 (0.89) |
| Triglycerides (mmol/l) | 1.19 (0.62) | 1.22 (0.59) | 1.24 (0.64) | 1.21 (0.70) | 1.29 (0.71) | 1.24 (0.67) | 1.13 (0.52) | 1.23 (0.73) | 1.18 (0.66) | 0.01 (0.80) | 0.07 (0.61) | 0.03 (0.64) | –0.06 (0.72) | 0.01 (0.60) | –0.04 (0.58) |
| Fasting glucose (mmol/l) | 5.44 (1.07) | 5.44 (0.76) | 5.58 (1.04) | 5.61 (1.10) | 5.48 (0.92) | 5.57 (0.91) | 5.29 (1.12) | 5.32 (0.96) | 5.42 (1.10) | 0.14 (0.82) | 0.02 (0.71) | –0.01 (0.76) | –0.18 (0.83) | –0.15 (0.83) | –0.24 (1.12) |
| Cluster metabolic risk score | –0.08 (0.61) | 0.01 (0.67) | 0.07 (0.67) | –0.04 (0.64) | 0.02 (0.67) | 0.00 (0.62) | –0.06 (0.64) | 0.05 (0.69) | 0.03 (0.66) | 0.02 (0.33) | 0.02 (0.35) | –0.05 (0.33) | 0.01 (0.36) | 0.02 (0.41) | –0.04 (0.36) |
| Fatigue a | |||||||||||||||
| Physical | 8.78 (3.50) | 8.83 (3.80) | 8.76 (3.35) | 8.39 (3.40) | 8.32 (3.36) | 7.88 (3.57) | 8.46 (3.46) | 8.70 (3.94) | 8.32 (3.35) | –0.22 (3.42) | –0.42 (3.67) | –0.77 (3.66) | –0.12 (3.63) | 0.06 (4.35) | –0.25 (3.64) |
| Mental | 5.02 (2.12) | 4.99 (2.20) | 4.83 (2.03) | 3.76 (2.23) | 4.16 (2.12) | 3.99 (2.08) | 3.91 (2.36) | 3.83 (2.43) | 3.98 (2.04) | –1.27 (2.25) | –0.83 (2.04) | –0.82 (1.92) | –1.14 (2.31) | –1.15 (2.32) | –0.84 (2.15) |
| Global | 13.8 (5.08) | 13.8 (5.50) | 13.6 (4.98) | 9.61 (6.77) | 11.0 (6.18) | 10.6 (6.08) | 9.83 (6.93) | 9.83 (7.33) | 10.7 (6.15) | –4.27 (7.36) | –2.90 (6.90) | –3.04 (6.44) | –4.06 (7.62) | –3.98 (8.08) | –2.90 (7.02) |
| Musculoskeletal issues in the last 3 months, % ( n ) | |||||||||||||||
| Neck | 55.6 (134) | 54.8 (126) | 54.1 (119) | 43.7 (76) | 40.0 (77) | 40.6 (78) | 47.2 (83) | 41.4 (65) | 36.3 (65) | –9.8 | –12.8 | –15.9 | –6.6 | –9.2 | –15.8 |
| Lower back | 61.6 (151) | 58.1 (133) | 52.5 (115) | 46.3 (81) | 43.3 (84) | 40.8 (78) | 48.9 (85) | 44.9 (70) | 42.9 (76) | –10.9 | –13.4 | –8.9 | –11.5 | –10.7 | –8.2 |
| Upper extremity | 72.9 (180) | 72.3 (167) | 69.1 (154) | 53.3 (99) | 60.0 (117) | 57.1 (109) | 62.5 (110) | 55.6 (90) | 56.3 (103) | –14.3 | –9.1 | –10.9 | –8.2 | –16.7 | –11.8 |
| Lower extremity | 65.3 (160) | 70.4 (162) |
68.2 (150) | 47.4 (83) | 47.9 (93) | 56.3 (108) | 58.5 (103) | 54.7 (88) | 56.6 (103) | –16.9 | –18.9 | –12.6 | –4.1 | –12.8 | –11.3 |
| Any part | 88.8 (221) | 92.2 (214) | 89.4 (202) | 77.4 (137) | 80.1 (157) | 82.9 (160) | 82.5 (146) | 79.1 (129) | 82.7 (153) | –9.4 | –9.5 | –6.9 | –5.2 | –11.4 | –7.2 |
| Musculoskeletal pain in the last 3 months b | |||||||||||||||
| Neck | 1.82 (2.26) | 1.63 (2.09) | 1.58 (1.93) | 1.35 (2.01) | 1.30 (2.05) | 1.19 (1.91) | 1.47 (2.02) | 1.37 (2.03) | 1.16 (1.86) | –0.44 (1.86) | –0.25 (1.92) | –0.53 (1.95) | –0.29 (1.83) | –0.13 (1.97) | –0.39 (1.90) |
| Lower back | 2.42 (2.57) | 2.32 (2.60) | 2.10 (2.50) | 1.61 (2.17) | 1.41 (2.14) | 1.40 (2.16) | 1.79 (2.24) | 1.72 (2.41) | 1.51 (2.12) | –0.52 (2.50) | –0.77 (2.47) | –0.55 (2.13) | –0.44 (2.44) | –0.50 (2.44) | –0.43 (2.69) |
| Upper extremity | 2.33 (2.11) | 2.26 (2.04) | 2.27 (2.15) | 1.76 (2.02) | 2.03 (2.21) | 1.70 (1.97) | 1.85 (1.92) | 1.79 (2.11) | 1.75 (1.98) | –0.39 (1.97) | –0.14 (2.36) | –0.43 (2.20) | –0.24 (1.82) | –0.50 (2.38) | –0.37 (2.21) |
| Lower extremity | 2.18 (2.37) | 2.50 (2.42) | 2.45 (2.23) | 1.68 (2.21) | 1.81 (2.37) | 1.86 (2.12) | 2.00 (2.27) | 2.11 (2.46) | 1.86 (2.15) | –0.30 (2.12) | –0.45 (2.59) | –0.50 (2.39) | 0.07 (2.35) | –0.13 (2.56) | –0.47 (2.53) |
| Any part | 2.95 (1.93) | 3.14 (1.87) | 3.08 (1.86) | 2.50 (1.94) | 2.74 (2.09) | 2.68 (2.03) | 2.64 (1.85) | 2.79 (2.09) | 2.69 (1.93) | –0.26 (1.81) | –0.24 (2.32) | –0.27 (2.21) | –0.12 (1.77) | –0.29 (2.32) | –0.24 (2.42) |
Fatigue
For fatigue, there were no between-group differences in the mean changes for any variables at follow-up (see Table 11).
Musculoskeletal issues
Prevalence of musculoskeletal issues was lower in all areas in all groups at both follow-up time points (see Table 11). There appeared to be small positive changes in the pain experienced in the lower extremity in the SWAL plus desk group compared with the control group at 12 months.
Psychological health
The descriptive statistics for psychological health are presented in Table 12. There appeared to be small improvement in stress and well-being in both intervention groups in comparison with the control group at 3 and 12 months. For other outcomes, there were no noticeable between-group differences.
| Variable | Baseline value | 3 months | 12 months | Change at 3 months | Change at 12 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | |
| Anxietya | 7.44 (4.05) | 7.36 (4.14) | 6.99 (3.90) | 7.24 (4.05) | 6.70 (3.95) | 6.44 (3.85) | 7.03 (391) | 7.06 (4.06) | 6.42 (4.04) | 0.11 (2.69) | –0.47 (3.17) | –0.38 (2.78) | –0.16 (2.91) | –0.24 (3.10) | –0.45 (3.13) |
| Depressiona | 4.28 (3.44) | 3.98 (3.43) | 3.94 (3.17) | 3.91 (3.44) | 3.84 (3.28) | 3.56 (3.17) | 3.90 (3.32) | 3.94 (3.32) | 3.53 (3.19) | –0.09 (2.16) | –0.04 (2.72) | –0.20 (2.90) | –0.15 (2.68) | –0.20 (3.04) | –0.31 (2.73) |
| Stressb | 15.9 (6.52) | 16.4 (7.02) | 16.1 (6.67) | 16.0 (6.69) | 16.1 (6.55) | 15.3 (6.83) | 16.1 (6.54) | 16.3 (6.61) | 15.6 (7.16) | 0.43 (5.10) | –0.26 (5.41) | –0.58 (5.64) | 0.44 (5.16) | –0.12 (5.55) | –0.24 (5.57) |
| Well-beingc | 54.7 (20.1) | 54.0 (20.3) | 55.4 (19.6) | 56.2 (20.6) | 57.0 (21.5) | 58.9 (20.0) | 55.6 (20.6) | 55.5 (20.6) | 57.8 (20.1) | 0.05 (13.9) | 2.46 (16.3) | 2.37 (17.0) | 0.69 (14.5) | 2.06 (19.7) | 2.12 (15.8) |
| Positive affectd | 30.3 (8.41) | 29.7 (8.46) | 30.3 (7.88) | 30.3 (8.30) | 30.2 (8.49) | 30.6 (7.94) | 30.2 (8.64) | 29.8 (8.49) | 30.2 (8.44) | –0.30 (6.61) | 0.66 (6.59) | 0.05 (6.93) | –0.26 (6.91) | 0.46 (7.38) | –0.21 (6.76) |
| Negative affecte | 16.8 (6.87) | 16.6 (7.04) | 16.1 (6.19) | 15.9 (6.47) | 16.7 (7.12) | 15.8 (6.19) | 16.6 (6.89) | 16.8 (6.94) | 15.5 (6.33) | –0.45 (5.32) | 0.34 (6.24) | 0.03 (5.89) | 0.17 (6.56) | 0.24 (6.97) | –0.45 (5.99) |
| Quality of life | |||||||||||||||
| Health utility scoref | 0.90 (0.10) | 0.88 (0.13) | 0.89 (0.10) | 0.90 (0.10) | 0.90 (0.10) | 0.90 (0.10) | 0.89 (0.11) | 0.89 (0.12) | 0.90 (0.11) | –0.01 (0.09) | 0.00 (0.09) | 0.01 (0.09) | –0.01 (0.09) | 0.00 (0.12) | 0.00 (0.10) |
| Health state scoreg | 74.8 (15.8) | 72.9 (16.3) | 74.6 (16.0) | 76.7 (15.6) | 74.4 (14.5) | 77.8 (15.8) | 77.0 (15.8) | 75.3 (15.5) | 77.1 (15.0) | 1.02 (13.8) | 0.87 (12.4) | 1.69 (14.6) | 2.30 (15.7) | 2.24 (14.3) | 1.79 (13.9) |
Work-related outcomes
The descriptive statistics for work-related outcomes are presented in Table 13. There appeared to be small favourable changes in vigour in both intervention groups in comparison with the control group at 12 months. There appeared to be favourable changes in organisational social norms and all support avenues in the SWAL plus desk group at 3- and 12-month follow-up compared with the control group, and for output demands at 12 months. There were no between-group differences in the mean changes in job performance and satisfaction, occupational fatigue recovery, workload and relations, social and for output demands at 12 months. There were no between-group differences in the mean changes in job performance and satisfaction, occupational fatigue recovery, workload and relations, social community, work limitations and absenteeism episodes. For absenteeism duration, there appeared to be unfavourable changes in the SWAL plus desk group during the 12-month study.
| Variable | Baseline value | 3 months | 12 months | Change at 3 months | Change at 12 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | Control | SWAL only | SWAL plus desk | |
| Work engagementa | |||||||||||||||
| Vigour | 3.31 (1.33) | 3.42 (1.27) | 3.30 (1.25) | 3.38 (1.34) | 3.52 (1.19) | 3.50 (1.19) | 3.35 (1.29) | 3.59 (1.14) | 3.46 (1.17) | 0.09 (0.86) | 0.10 (0.95) | 0.16 (0.87) | 0.05 (0.96) | 0.17 (0.93) | 0.16 (0.98) |
| Dedication | 4.13 (1.22) | 4.23 (1.23) | 4.09 (1.16) | 4.04 (1.14) | 4.11 (1.17) | 4.10 (1.04) | 4.00 (1.18) | 4.22 (1.16) | 4.06 (1.08) | –0.09 (0.75) | –0.10 (0.77) | 0.02 (0.75) | –0.11 (0.85) | –0.05 (0.84) | –0.02 (0.94) |
| Absorption | 4.14 (1.13) | 4.22 (1.11) | 4.16 (1.06) | 4.11 (1.01) | 4.15 (0.99) | 4.24 (1.01) | 4.11 (1.04) | 4.21 (1.06) | 4.26 (1.06) | 0.02 (0.90) | –0.07 (0.82) | 0.05 (0.80) | 0.06 (0.87) | –0.08 (0.93) | 0.08 (0.94) |
| Overall | 3.86 (1.10) | 3.96 (1.08) | 3.85 (1.01) | 3.84 (1.05) | 3.93 (1.02) | 3.94 (0.97) | 3.82 (1.04) | 4.00 (1.01) | 3.93 (1.00) | 0.00 (0.66) | –0.03 (0.67) | 0.08 (0.61) | –0.00 (0.73) | 0.01 (0.71) | 0.07 (0.78) |
| Job performanceb | 5.52 (1.01) | 5.54 (1.05) | 5.53 (0.93) | 5.45 (1.00) | 5.47 (1.02) | 5.44 (0.99) | 5.35 (0.99) | 5.45 (1.08) | 5.46 (0.98) | 0.06 (0.82) | –0.02 (0.96) | –0.11 (0.99) | –0.12 (0.94) | –0.10 (1.03) | –0.06 (1.10) |
| Job satisfactionc | 4.80 (1.38) | 4.97 (1.29) | 4.89 (1.24) | 4.79 (1.41) | 4.98 (1.30) | 4.76 (1.30) | 4.69 (1.40) | 5.01 (1.33) | 4.74 (1.29) | –0.02 (0.98) | 0.04 (0.94) | –0.10 (1.04) | –0.07 (1.17) | 0.01 (1.17) | –0.14 (1.27) |
| Occupational fatigue recoveryd | 0.45 (0.28) | 0.46 (0.29) | 0.44 (0.28) | 0.42 (0.29) | 0.45 (0.29) | 0.42 (0.28) | 0.45 (0.30) | 0.46 (0.28) | 0.40 (0.29) | 0.01 (0.21) | 0.00 (0.22) | –0.00 (0.23) | 0.01 (0.23) | 0.00 (0.25) | –0.03 (0.25) |
| Workload and relationse | |||||||||||||||
| Demands | 2.70 (0.75) | 2.70 (0.66) | 2.81 (0.74) | 2.75 (0.77) | 2.69 (0.67) | 2.75 (0.74) | 2.77 (0.78) | 2.75 (0.71) | 2.74 (0.75) | 0.04 (0.52) | 0.01 (0.52) | –0.06 (0.51) | 0.04 (0.63) | 0.09 (0.58) | –0.04 (0.52) |
| Control | 3.82 (0.71) | 3.87 (0.67) | 3.81 (0.63) | 3.82 (0.71) | 3.83 (0.67) | 3.87 (0.63) | 3.86 (0.72) | 3.85 (0.80) | 3.98 (0.65) | –0.05 (0.59) | –0.04 (0.53) | –0.00 (0.50) | 0.03 (0.53) | –0.06 (0.56) | 0.03 (0.57) |
| Support | 3.83 (0.69) | 3.87 (0.80) | 3.68 (0.83) | 3.72 (0.83) | 3.80 (0.79) | 3.70 (0.77) | 3.75 (0.82) | 3.81 (0.81) | 3.62 (0.77) | –0.11 (0.51) | –0.08 (0.62) | –0.01 (0.57) | –0.05 (0.68) | –0.06 (0.65) | –0.08 (0.70) |
| Organisational social normsf | 3.84 (0.57) | 3.93 (0.54) | 3.84 (0.54) | 3.82 (0.57) | 3.93 (0.56) | 4.09 (0.52) | 3.81 (0.59) | 3.95 (0.62) | 4.06 (0.57) | –0.01 (0.41) | –0.02 (0.47) | 0.25 (0.45) | –0.03 (0.54) | 0.00 (0.55) | 0.20 (0.63) |
| Social communityg | 1.81 (0.73) | 1.87 (0.75) | 1.96 (0.73) | 1.92 (0.78) | 1.84 (0.75) | 1.91 (0.71) | 1.96 (0.81) | 1.86 (0.80) | 2.00 (0.75) | 0.14 (0.64) | –0.05 (0.61) | –0.05 (0.58) | 0.13 (0.70) | –0.04 (0.73) | 0.07 (0.74) |
| Supporth | |||||||||||||||
| Organisation | 2.91 (1.16) | 3.05 (1.17) | 2.95 (1.13) | 2.80 (1.19) | 3.11 (1.17) | 3.56 (1.13) | 2.86 (1.20) | 3.21 (1.17) | 3.52 (1.09) | –0.05 (1.31) | –0.01 (1.27) | 0.61 (1.17) | –0.04 (1.28) | 0.01 (1.32) | 0.55 (1.33) |
| Manager | 3.11 (1.24) | 3.24 (1.23) | 3.09 (1.16) | 2.90 (1.18) | 3.23 (1.20) | 3.69 (1.08) | 3.01 (1.22) | 3.41 (1.20) | 3.46 (1.20) | –0.12 (1.21) | –0.10 (1.34) | 0.55 (1.19) | –0.12 (1.28) | 0.10 (1.34) | 0.32 (1.51) |
| Colleagues | 3.25 (1.15) | 3.27 (1.18) | 3.24 (1.20) | 3.02 (1.14) | 3.39 (1.15) | 3.94 (0.97) | 3.10 (1.16) | 3.44 (1.16) | 3.78 (1.01) | –0.18 (1.30) | 0.08 (1.32) | 0.63 (1.29) | –0.08 (1.31) | 0.20 (1.31) | 0.48 (1.37) |
| Family | 3.40 (1.23) | 3.44 (1.21) | 3.39 (1.18) | 3.32 (1.18) | 3.24 (1.23) | 3.63 (1.05) | 3.18 (1.17) | 3.46 (1.12) | 3.60 (1.07) | 0.00 (1.37) | –0.18 (1.38) | 0.18 (1.24) | –0.16 (1.37) | 0.08 (1.47) | 0.15 (1.35) |
| Work limitationsi | |||||||||||||||
| Time management | 1.71 (0.84) | 1.75 (0.82) | 1.63 (0.79) | 1.60 (0.73) | 1.76 (0.84) | 1.60 (0.77) | 1.68 (0.82) | 1.82 (0.84) | 1.66 (0.77) | –0.06 (0.76) | 0.02 (0.80) | 0.03 (0.78) | 0.02 (0.79) | 0.09 (0.92) | 0.07 (0.81) |
| Physical demands | 1.68 (0.87) | 1.72 (0.93) | 1.63 (0.85) | 1.70 (0.98) | 1.68 (0.86) | 1.66 (0.85) | 1.61 (0.89) | 1.82 (1.01) | 1.68 (0.94) | 0.01 (1.07) | 0.03 (1.08) | –0.03 (0.83) | 0.03 (1.00) | 0.18 (1.06) | 0.01 (1.03) |
| Mental-interpersonal demands | 1.55 (0.65) | 1.65 (0.73) | 1.61 (0.74) | 1.56 (0.64) | 1.61 (0.75) | 1.55 (0.71) | 1.54 (0.73) | 1.65 (0.72) | 1.56 (0.74) | 0.06 (0.58) | –0.01 (0.78) | –0.02 (0.83) | –0.01 (0.68) | 0.04 (0.83) | –0.04 (0.84) |
| Output demands | 1.59 (0.78) | 1.69 (0.88) | 1.70 (0.94) | 1.65 (0.85) | 1.61 (0.88) | 1.60 (0.88) | 1.66 (0.91) | 1.72 (0.85) | 1.62 (0.84) | 0.09 (0.81) | –0.06 (0.90) | –0.08 (0.96) | 0.06 (0.88) | 0.04 (0.99) | –0.07 (0.94) |
| Overall | 1.58 (0.54) | 1.63 (0.62) | 1.60 (0.62) | 1.58 (0.60) | 1.61 (0.64) | 1.56 (0.60) | 1.57 (0.60) | 1.71 (0.63) | 1.57 (0.63) | 0.04 (0.53) | –0.00 (0.62) | –0.02 (0.58) | 0.01 (0.53) | 0.10 (0.68) | –0.00 (0.61) |
| Absenteeism (self-report) | 1.57 (4.58) | 0.95 (3.71) | 0.82 (2.38) | N/A | N/A | N/A | 0.97 (3.14) | 1.22 (5.32) | 1.66 (7.27) | N/A | N/A | N/A | –0.57 (4.90) | 0.37 (6.73) | 0.86 (7.77) |
| Absenteeism (records) | |||||||||||||||
| Episodes | 0.80 (1.14) | 0.89 (1.47) | 0.75 (0.96) | N/A | N/A | N/A | 0.79 (1.28) | 0.83 (1.09) | 0.74 (1.04) | N/A | N/A | N/A | –0.01 (1.37) | –0.06 (1.20) | –0.01 (1.14) |
| Duration | 4.93 (14.2) | 4.22 (9.88) | 3.86 (7.89) | N/A | N/A | N/A | 4.59 (15.8) | 5.08 (11.9) | 6.02 (15.4) | N/A | N/A | N/A | –0.34 (20.8) | 0.87 (14.0) | 2.16 (14.4) |
Strategies to sit less and move more often
There were 28 strategies listed to sit less and move more at work and outside work (Table 14). In the control group, there was very little change in strategies to sit less and move more often over the time points. Overall, in the SWAL-only and the SWAL plus desk groups, 12 of 28 and 16 of 28 strategies increased by ≥ 5% at 3-month follow-up, respectively, and 18 of 28 and 17 of 28 strategies increased by ≥ 5% at 12-month follow-up, respectively.
| Strategy | Control, % (n) | SWAL only, % (n) | SWAL plus desk, % (n) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 12 months | Baseline | 3 months | 12 months | Baseline | 3 months | 12 months | |
| Stood up during a meeting | 0.4 (1) | 0.0 (0) | 0.0 (0) | 0.5 (1) | 3.5 (6) | 4.9 (7) | 0.0 (0) | 5.1 (9) | 4.1 (7) |
| Stood up when talking on the telephone at work | 5.6 (13) | 6.1 (10) | 9.2 (16) | 5.4 (12) | 16.4 (32) | 17.6 (28) | 4.2 (9) | 34.4 (65) | 30.4 (56) |
| Stood up when talking on the telephone at home | 48.5 (114) | 48.8 (80) | 44.0 (77) | 46.7 (105) | 50.0 (96) | 56.5 (91) | 45.3 (97) | 53.2 (100) | 54.1 (99) |
| Walked to talk to a colleague rather than sending them an e-mail or telephoning | 56.4 (133) | 52.1 (86) | 59.9 (106) | 46.5 (105) | 58.3 (113) | 57.2 (91) | 41.2 (89) | 59.0 (112) | 64.9 (120) |
| Walked to the printer that is further away from my office | 20.0 (47) | 24.7 (40) | 24.3 (43) | 23.5 (53) | 26.3 (51) | 33.1 (53) | 15.8 (34) | 25.7 (48) | 27.7 (51) |
| Walked to the bathroom that is further away from my office | 23.0 (54) | 24.4 (40) | 27.2 (48) | 29.2 (66) | 31.6 (62) | 38.8 (62) | 29.2 (63) | 42.3 (80) | 44.3 (81) |
| Walked to a centrally located bin instead of using my own bin | 54.3 (127) | 43.6 (72) | 46.6 (81) | 51.8 (116) | 52.1 (101) | 60.3 (94) | 49.3 (106) | 60.3 (114) | 58.5 (107) |
| Walked to places rather than drive | 37.5 (87) | 30.1 (50) | 36.8 (63) | 37.5 (84) | 41.5 (80) | 46.2 (73) | 38.7 (82) | 38.1 (72) | 42.5 (77) |
| Parked car further away from destination | 20.4 (46) | 18.5 (30) | 25.9 (44) | 23.9 (52) | 24.3 (45) | 32.9 (49) | 23.9 (49) | 29.7 (54) | 34.9 (61) |
| Attended a meeting where the chairperson indicated that it was acceptable to stand | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 2.1 (4) | 2.1 (4) | 0.6 (1) | 3.1 (5) | 3.3 (6) |
| Noticed signage around the office to encourage standing up, sitting less and moving more | 3.0 (7) | 1.8 (3) | 3.4 (6) | 1.3 (3) | 29.1 (57) | 31.3 (50) | 2.3 (5) | 38.1 (72) | 31.0 (57) |
| Used prompts at my desk (e.g. postcards and stickers) to remind me to stand up regularly | 0.4 (1) | 0.6 (1) | 2.3 (4) | 0.9 (2) | 13.3 (26) | 7.6 (12) | 1.9 (4) | 17.5 (33) | 13.0 (24) |
| Used computer break software or computer prompts to remind me to stand up regularly | 1.3 (3) | 1.8 (3) | 4.5 (8) | 1.3 (3) | 24.0 (47) | 15.6 (25) | 1..9 (4) | 20.5 (39) | 14.1 (26) |
| Used a mobile phone app to remind me to stand up regularly | 4.2 (10) | 6.7 (11) | 6.3 (11) | 7.1 (16) | 11.2 (22) | 15.0 (24) | 5.6 (12) | 10.0 (19) | 7.1 (13) |
| Used a mobile phone app to track your sitting time | 1.7 (4) | 4.2 (7) | 5.7 (10) | 4.0 (9) | 6.7 (13) | 6.9 (11) | 4.7 (10) | 7.5 (14) | 4.4 (8) |
| Stood up to do certain tasks at work rather than sit | 5.1 (12) | 3.7 (6) | 6.8 (12) | 4.5 (10) | 15.0 (29) | 19.0 (30) | 5.1 (11) | 54.5 (103) | 44.3 (81) |
| Eaten my lunch away from my desk | 18.7 (44) | 24.6 (54) | 21.5 (46) | 20.1 (33) | 26.6 (51) | 27.4 (51) | 18.4 (32) | 35.3 (55) | 32.8 (58) |
| Used the stairs instead of taking the lift | 69.8 (164) | 67.2 (111) | 72.2 (127) | 61.6 (138) | 68.4 (134) | 64.8 (103) | 61.6 (133) | 71.6 (136) | 73.9 (136) |
| Cycled to work | 9.8 (23) | 7.5 (12) | 9.6 (17) | 10.0 (22) | 9.3 (18) | 8.4 (13) | 8.5 (18) | 6.4 (12) | 9.3 (17) |
| Walked to work | 23.0 (54) | 20.6 (34) | 21.4 (37) | 15.6 (35) | 18.1 (35) | 17.2 (27) | 19.6 (41) | 18.5 (35) | 21.7 (39) |
| Walked during lunch break | 47.4 (111) | 43.0 (71) | 48.3 (84) | 45.0 (98) | 47.6 (91) | 56.0 (89) | 50.0 (105) | 48.7 (90) | 50.6 (89) |
| Had a walking meeting | 0.0 (0) | 1.2 (2) | 2.3 (4) | 1.4 (3) | 1.6 (3) | 4.6 (7) | 1.95 (4) | 1.6 (3) | 4.1 (7) |
| Walked laps of office | 6.8 (16) | 4.3 (7) | 5.1 (9) | 6.3 (14) | 13.9 (27) | 11.5 (18) | 5.1 (11) | 7.0 (13) | 11.0 (22) |
| Group physical activity sessions during work hours | 5.5 (13) | 6.1 (10) | 6.8 (12) | 3.6 (8) | 8.8 (17) | 13.3 (21) | 4.2 (9) | 9.6 (18) | 12.0 (22) |
| Got up during TV adverts | 28.2 (64) | 33.1 (54) | 34.3 (60) | 26.7 (59) | 36.5 (70) | 37.6 (59) | 30.0 (63) | 35.5 (65) | 32.2 (57) |
| Stood for some household chores rather than sit | 42.4 (100) | 39.6 (65) | 38.3 (67) | 42.6 (95) | 43.1 (84) | 41.7 (65) | 43.0 (92) | 44.2 (84) | 53.3 (97) |
| Used laptop/tablet at home while standing | 7.6 (18) | 9.1 (15) | 6.8 (12) | 6.8 (15) | 8.9 (17) | 13.5 (21) | 5.6 (12) | 6.9 (13) | 12.4 (23) |
| Talked to SWAL champion for encouragement | 0.8 (4) | 1.9 (3) | 1.8 (3) | 1.5 (3) | 16.3 (30) | 11.0 (17) | 0.5 (1) | 10.0 (18) | 8.0 (14) |
Online survey during the COVID-19 pandemic
Out of the 600 participants who were still enrolled in the study in May 2020, 317 (52.8%) also completed an online survey to examine time spent sitting and lifestyle behaviours during the pandemic. The survey was completed during ‘lockdown 1’. Participants were distributed across the three arms [control, n = 116 (38.4%); SWAL only, n = 87 (28.8%); SWAL plus desk, n = 99 (32.8%); and 15 respondents did not provide their SWAL participant number]. Respondents were more likely to be female (76.7%), aged ≥ 45 years old (63.9%) and white (76.7%).
The majority of survey participants (n = 300, 94.6%) had either ‘mostly’ or ‘all of the time’ worked at the workplace before the COVID-19 restrictions; however, during the COVID-19 restrictions, 96.5% (n = 305) were either ‘completely’ or ‘mostly’ working from home.
Survey participants were asked about their sitting, standing and walking times as a percentage of a typical weekday, and for their work hours. There was a significant increase in sitting time during COVID-19 restrictions compared with before restrictions. Both standing and walking times significantly decreased (Table 15). When data were split by group, only the SWAL plus desk group showed any significant differences. For example, sitting time increased from 55.9% to 68.6% for weekdays and from 59.0% to 74.0% for work hours. However, sitting time was still lower for participants in the SWAL plus desk group than for participants in the control group during COVID-19 restrictions (68.6 vs. 71.5% for weekdays; 74.0 vs. 77.8% for work hours). Significant decreases in standing time were seen from before to during the COVID-19 restrictions, and these decreases were driven by a reduction in standing time for those in the SWAL plus desk group from 24.3% to 13.9%; however, higher standing times were seen for both intervention groups than for the control group during the restrictions.
| Variable | Total (n = 317) | Study arm | ||
|---|---|---|---|---|
| Control (n = 116) | SWAL only (n = 87) | SWAL plus desk (n = 99) | ||
| Physical behaviour variables | ||||
| Sitting (weekday, %) | ||||
| Before | 63.4 (0.9) | 69.9 (1.2) | 63.8 (1.5) | 55.9 (1.8) |
| During | 68.6 (1.2) | 71.5 (1.4) | 64.0 (2.2) | 68.6 (1.8) |
| Standing (weekday, %) | ||||
| Before | 15.8 (0.7) | 10.4 (0.7) | 13.5 (0.9) | 24.3 (1.5) |
| During | 12.8 (0.8) | 10.2 (0.8) | 15.9 (1.8) | 13.9 (1.5) |
| Walking/moving (weekday, %) | ||||
| Before | 20.7 (0.6) | 19.7 (0.8) | 22.7 (1.2) | 19.8 (0.9) |
| During | 18.6 (0.6) | 18.3 (0.9) | 20.1 (1.3) | 17.5 (1.0 |
| Sitting (work hours, %) | ||||
| Before | 69.0 (1.0) | 76.4 (1.2) | 70.5 (1.5) | 59.0 (2.1) |
| During | 73.9 (1.2) | 77.8 (1.5) | 68.3 (2.6) | 74.0 (2.1) |
| Standing (work hours, %) | ||||
| Before | 14.4 (0.8) | 8.1 (0.8) | 11.2 (0.9) | 25.3 (1.8) |
| During | 11.7 (0.9) | 8.8 (1.0) | 15.3 (2.2) | 12.5 (1.8) |
| Walking/moving (work hours, %) | ||||
| Before | 16.6 (0.5) | 15.5 (0.8) | 18.3 (1.1) | 15.7 (0.9) |
| During | 14.4 (0.6) | 13.3 (0.9) | 16.4 (1.4) | 13.3 (0.9) |
| MVPA (minutes)a | ||||
| Before | 49.5 (1.9) | 47.6 (2.7) | 48.3 (3.4) | 49.9 (3.6) |
| During | 46.6 (1.9) | 43.3 (2.6) | 50.5 (4.4) | 46.5 (3.0) |
| Sleep duration (mean, SD) | ||||
| Sleep efficiency (%) | ||||
| Before | 87.1 (0.7) | 87.2 (0.9) | 87.0 (1.5) | 86.9 (1.4) |
| During | 85.4 (0.7) | 83.8 (1.0) | 86.4 (1.4) | 87.3 (1.3) |
When participants were asked about the time they spent in MVPA each day, there were no significant differences in the mean minutes per day before the COVID-19 restrictions (i.e. 49.5 minutes) and during the COVID-19 restrictions (i.e. 46.6 minutes), and this was similar for each intervention arm. There was a significant decrease in sleep efficiency from before to during the COVID-19 restrictions for all responders (from 87.1% to 85.4%) and for participants in the control group (from 87.2% to 83.8%).
Survey participants reported significantly higher rates of musculoskeletal issues during COVID-19 restrictions than before COVID-19 restrictions (Figure 7), for example neck and shoulder pain increased from 39% to 50% and from 43% to 49%, respectively. The highest percentage differences were seen in upper and lower back pain, with percentage increases of 57.4% (18.9–29.7%) and 42.9% (38.0–54.4%), respectively.
FIGURE 7.
Percentage of participants reporting musculoskeletal issues before and during the COVID-19 restrictions.
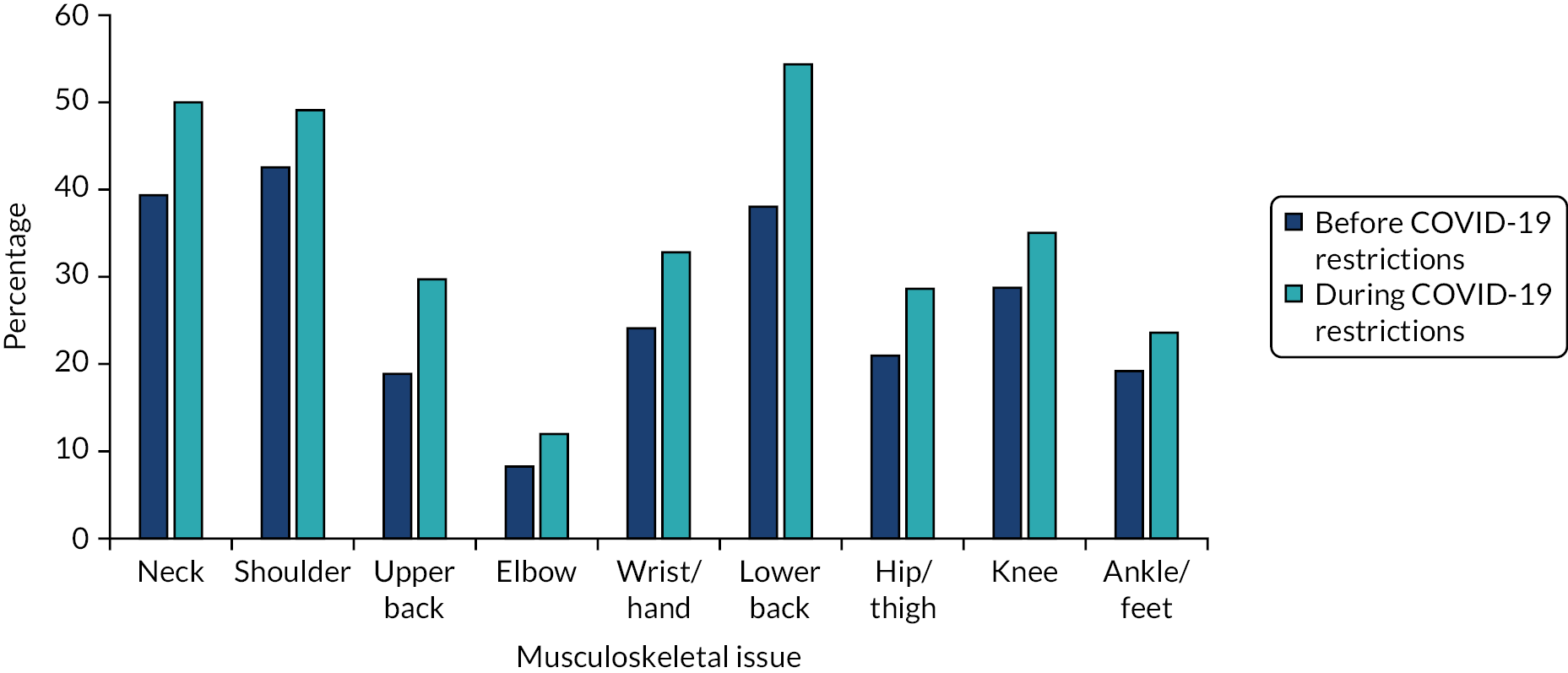
Chapter 4 Process evaluation results
Table 16 provides a summary of data collected for the process evaluation methods.
| Type of data | Collected from | Timing | Number of participants |
|---|---|---|---|
| Workplace champion training attendance | Workplace champions | At the training session | 56 workplace champions from 51 clusters |
| Questionnaire to assess workplace champion feedback on training | Workplace champions | The end of training | 56 workplace champions from 51 clusters |
| Questionnaire on intervention and study components | All intervention participants | 3 and 12 months | 3 months: SWAL only, 180 (78%); SWAL plus desk, 191 (85%) 12 months: SWAL only, 162 (73%); SWAL plus desk, 178 (80%) |
| Questionnaire on study assessments and lifestyle changes | All control participants | 3 and 12 months | 195 at 3 months (82%) and 187 at 12 months (77%) |
| Focus groups | >20% random sample from each study arm | 12 months | 36 focus groups (control, n = 11; SWAL only, n = 14; SWAL plus desk, n = 11) |
| Workplace champion questionnaire | Workplace champions | 12 months | 27 workplace champions |
| Interviews | Workplace champions | 12 months | 16 workplace champions representing 14 clusters |
| Observations | Representative subsample of office clusters | 3 and 12 months | 3 months: 18 clusters 12 months: 17 clusters |
| Workplace champion implementation records | Workplace champions | Submitted at 3, 9 and 15 monthsa | 48 clusters |
| Researcher records | Participants and workplace champions | Throughout | All participants |
Focus groups were conducted on a representative sample from each intervention arm within each local authority, apart from in Bolton Council (because of a change in senior management at the council and the need for re-approval for study activities and, therefore, focus group were not completed in time). Excluding Bolton Council, a mean of 30%, 27% and 34% of participants attended a focus group across all councils in the control, SWAL-only and SWAL plus desk groups, respectively. At least 50% of clusters were represented by one or more participants per cluster, with one-third of focus groups fully representing the intervention arm within each local authority (Table 17).
| Council | Control | SWAL only | SWAL plus desk | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Participant, n | % of arm | Clusters represented, % | Participant, n | % of arm | Clusters represented, % | Participant, n | % of arm | Clusters represented, % | |
| Leicester City | 26 | 28 | 90 | 20 | 23 | 82 | 27 | 28 | 80 |
| Leicester County | 12 | 26 | 100 | 8 | 32 | 75 | 5 | 23 | 67 |
| Salford City | 11 | 40 | 100 | 10 | 33 | 75 | 11 | 48 | 100 |
| Liverpool City | 3 | 21 | 50 | 6 | 20 | 60 | 5 | 13 | 50 |
| Trafford | 5 | 36 | 50 | 5 | 25 | 100 | 3 | 60 | 100 |
| Bolton | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 57 | 27 | 49 | 25 | 51 | 24 | |||
Recruitment and enrolment
Number of possible participants at each worksite and office group
On average, across all councils, we recruited 20.8% of the possible participants. The number of possible participants within viable clusters for the study are broken down in Appendix 9.
Number of worksites and office groups invited to participate, and number agreeing
Six local authorities that were within close proximity to the two research teams (i.e. Leicester and Salford) were approached across two study sites [Leicester (two local authorities: Leicester City Council and Leicestershire Council) and Salford (four local authorities: Salford City Council, Bolton Council, Trafford Council and Liverpool City Council)]. The study was initially advertised using each local authorities’ intranet and staff mailing systems. Additional recruitment strategies were incorporated for some local authorities, as detailed in the methods (see Chapter 2 and Appendix 3).
Leicester City Council
Fifteen study briefing events were held at Leicester City Council, with a mean attendance of 28 (range 10–50) participants per event, and 417 participants attended in total. Reply forms were received from 535 individuals either at the briefing event or directly via e-mail in response to an advertisement on the local authority intranet. Of the participants who responded, 336 (63% of those who expressed an interested) attended and consented at a baseline measurement session.
Leicestershire County Council
No briefing events were held at Leicester County Council. A quick turnaround was needed on recruitment, as this was an additional council that was recruited to account for lower-than-expected recruitment rates from the Greater Manchester and Liverpool councils. Reply forms were received from 248 individuals, and 123 individuals (50% of those who expressed an interested) attended and consented at a baseline measurement session.
Salford City Council
Sixteen briefing events were held, with a mean attendance of seven (range 1–18) participants. In total, 117 individuals attended, with 166 reply forms received after the briefing event or via e-mail in response to advertisements about the study. Of the participants who responded, 126 consented (76% of those who expressed an interest).
Bolton Council
Seven briefing events were held, with a mean of 13 (range 5–22) participants. In total, 90 people attended the briefing events, and 108 reply forms were received in person at the briefing events or via e-mail to the study team. Of the participants who responded, 63 consented (58% who expressed an interest) and formed six clusters.
Liverpool City Council
The advertisement remained on the intranet for a limited amount of time, as only approximately 100 participants were needed, and the advertisement was removed once enough interest in participation had been received. A total of 115 participants replied to the advertisement with a reply form, of whom 101 consented (88% who expressed an interest), forming 15 clusters.
Trafford Council
Participants were recruited via an advertisement through the council’s intranet, which signposted participants to the information sheet and reply form, and this resulted in 76 reply forms being sent to the study team. Of the participants who responded, 48 consented (63% of those who expressed an interest), forming four clusters.
Reasons for enrolment
At 3 months, participants were asked whether or not the offer of a health assessment had encouraged them to participate in the study. The proportion of participants who agreed or strongly agreed was 76.8%, 77.8% and 77.5% for the control, SWAL-only and SWAL plus desk arms, respectively, indicating that this was a motivator for taking part.
When asked about their reasons in the focus groups (at 12 months), desire for the standing desk was mentioned in every focus group (although not by every participant), with nearly all of the control and SWAL-only arm focus groups mentioning disappointment at not receiving a desk.
The second most common reason for taking part in the study was for the expected health benefits that could be gained from changing behaviours. For a large number of participants, this was explained fairly broadly as benefits to (non-specific) ‘health’ or the desire to maintain health as they became older. Other participants related health benefits to pre-existing health issues, such as ‘back ache’ or recognition of being at increased risk for health issues (e.g. diagnosis of type 2 diabetes or high cholesterol). Echoing the survey findings, many participants were keen to receive a free health check – and that this would be regularly repeated over the study period – which some participants saw as ‘less hassle’ than getting similar monitoring through their general practice.
Participants typically gave several reasons for enrolment, for example a combination of those above, as illustrated here:
I wanted the health data. I did want an uppy downy desk and I was gutted when I didn’t get one. But it was principally the health data and my body fat ratio.
FG10; control; P2
I would say the same, the health and the potential of getting a standing desk.
FG10; control; P3
Many participants described being ‘interested’, ‘intrigued’ or ‘curious’ in the research and its concepts, and a keenness to contribute to the evidence base for the benefits to themselves and others:
There’s potentially a wider benefit to other people not just to ourselves. I think that’s a good motivator for taking part. It’s why I wanted to take part in it, it’s not just for my own health but because it might actually influence policy further down the line.
FG6; SWAL plus desk; P1
Many participants expressed a strong desire to learn the results at the end of the study. Indeed, quite a few of the participants had hoped that the results would show sufficient significant benefits of the desk to persuade their organisation to install them (several participants from the control and the SWAL-only arms gave this view as reasons for their continued commitment to the study):
I thought, it was just something that I could take back to my manager. If the studies show that there is something beneficial, then it can be pushed out.
FG2; control; P1
The influence of colleagues underpinned many of the discussions in the focus groups, including as an influence on enrolling initially. A few participants, who had been more reluctant to initially take part in the study, mentioned having been ‘volunteered’ by colleagues, whereas more participants described a gentler influence, suggestions from colleagues or a collective decision as a team. Some participants described feeling a responsibility to set an example for others.
Several participants acknowledged that the £10 voucher had influenced them, whereas other participants referred to the voucher simply as a nice bonus or unnecessary.
Number of participants opting out, dropping out and non-compliance to the activPAL
There were a number of individuals (451/1248) who expressed an interest in the study but were ultimately not enrolled as a participant (see previous section) (see Figure 2). The majority of these individuals were not enrolled because of there being an insufficient number of individuals interested within their cluster. Other reasons for non-enrolment onto the study were the inability to make time to attend a baseline session because of work demands and no longer being interested in taking part.
The number of participants withdrawing prior to follow-up sessions, and the number of participants enrolled who did not provide valid activPAL data at 3- and 12-month follow-up, are presented in Table 18. The control and SWAL-only groups had similar drop-out and non-compliance rates at 12 months. There were a smaller number of withdrawals from the SWAL plus desk group, and this may have been influenced by participants having to return their height-adjustable workstation if they withdrew from the study prior to the final follow-up.
| Participants randomised, dropped out and non-compliant with primary outcome | Study arm, n (%) | ||
|---|---|---|---|
| Control | SWAL only | SWAL plus desk | |
| Randomised | 267 | 249 | 240 |
| Drop-out rate by 3-month follow-up | 26 (9.7) | 22 (8.8) | 15 (6.3) |
| Non-compliance to 3-month activPAL assessment | 19 (7.1) | 21 (8.4) | 18 (7.5) |
| Drop-out rate by 12-month follow-up | 32 (12) | 30 (12) | 13 (5.4) |
| Non-compliance to 12-month activPAL assessment (primary outcome) | 19 (7.1) | 12 (4.8) | 13 (5.4) |
Intervention acceptability and fidelity: participation and implementation
Workplace champion training
Participants who had volunteered to be a workplace champion and resided in clusters randomised to one of the two intervention arms were invited to a 3-hour group training session that took place at their workplace during work hours. Participants who were trained had the following mean characteristics: aged 44.0 (SD 11.5) years, 76% female, 90% white British, 58% educated to at least degree level and had been working at their respective councils for 12.2 (SD 9.6) years. This was representative of the characteristics of all participants. The training session was designed to equip workplace champions with the skills and knowledge to implement the SWAL intervention. The training programme was delivered by an experienced behaviour change education team and consisted of eight separate sessions, as detailed in Chapter 2.
Some clusters would train two workplace champions for the same cluster if it was felt that the workplace champions would need assistance in dividing the time-commitment of the role. In total, 12 training sessions across all councils were held to train 56 workplace champions, representing 51 clusters. Only one cluster did not have a workplace champion trained because the workplace champion became too busy to attend the training and no other participants within the cluster were willing to perform the role.
Workplace champions who attended the training completed an evaluation form at the end of the session. Overall ratings for each session were collected using a six-point Likert scale, with descriptors anchoring each end [from ‘not useful at all’ (1) to ‘very useful’ (6)]. Mean scores across all sessions ranged from 5.3 to 5.7 (out of a possible total of 6) (Figure 8), suggesting that the training was well received and the participants felt prepared for their role as SWAL champion.
FIGURE 8.
Workplace champion training feedback. Values are mean ± SD.
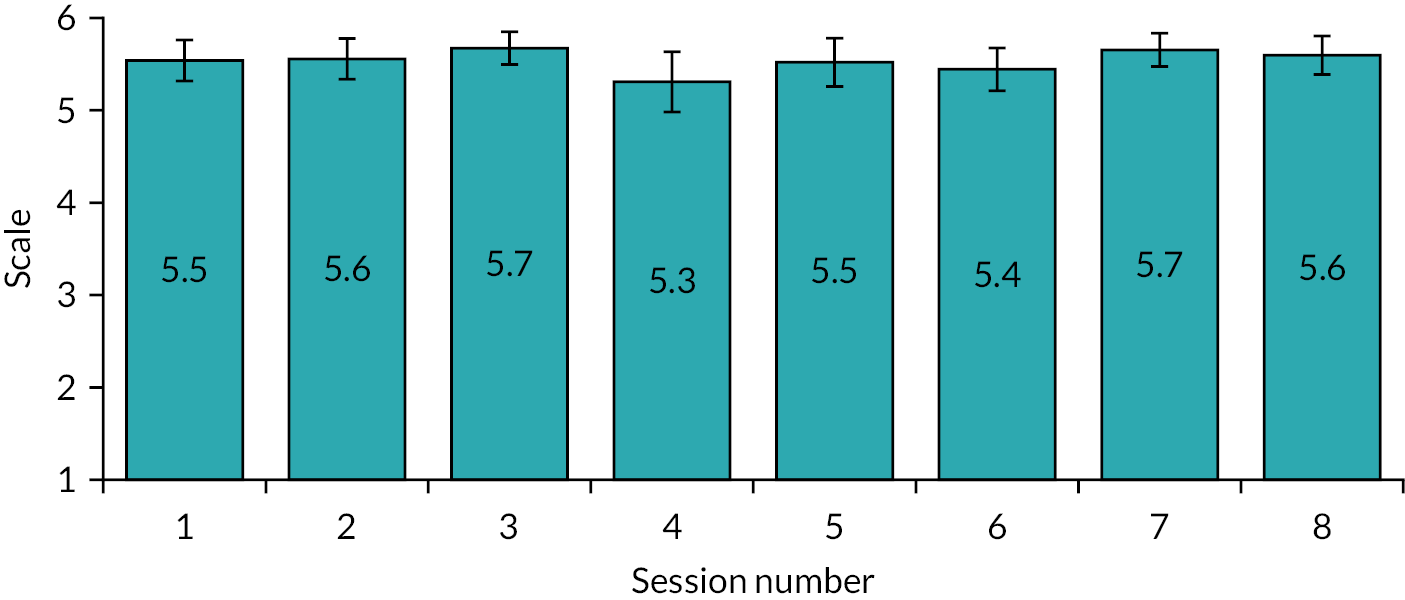
In an open comments section, attendees were asked to provide any positive comments or suggestions for improvement regarding the overall training experience.
Participants valued the clarity of the roles and responsibilities expected of them. Being provided with a full study timeline, indicating when each task was to be completed, was also appreciated, in addition to meeting other workplace champions and being able to share ideas in small groups:
Very thoroughly thought-out training. Executed and carried out well – good resource materials to take away.
Leicester WPC
Really enjoyed training. Received very helpful information and guidance.
Salford WPC
An area of improvement mentioned by multiple champions was that they would have valued being able to practice a group catch-up session while under the trainers’ guidance to improve their confidence and execution when facilitating it themselves:
Role play of group catch-up session using open questions, reflections, etc.
Leicester WPC
Workplace champion dropout
Workplace champions were trained for 51 of the 52 clusters in the two intervention arms. One cluster did not have a participant trained as a workplace champion (see above). Four of the workplace champions, who were trained, withdrew from the role within the first 3 months of the study. The study team attempted to find a replacement workplace champion, but were unsuccessful. By the end of the study, a further six clusters had no active workplace champion (i.e. 21% dropout). For two clusters, the workplace champions had left their employment at the council and other workplace champions cited a lack of time to perform the role under an increasing workload.
Workplace champion experiences of intervention implementation
Workplace champions completed a questionnaire at 12 months. The questionnaire assessed the workplace champions’ experiences in delivering the SWAL intervention, and 16 workplace champions were interviewed about their experiences.
The questionnaire indicated that the overall experience of being a workplace champion was mostly positive. Common aspects of what workplace champions thought went well was having a group whom they mostly knew or recognised and other group members actively engaging in the intervention, which made their role easier to perform and more enjoyable:
The positive from this has been that the majority of the team has really got on board with it and have implemented things to reduce sitting time and have been really positive and encouraging of me and my role as champion.
Questionnaire; WPC
The team we have are excellent and providing feedback, taking part and providing suggestions during the group catch ups, etc.
Questionnaire; WPC
Further positive impacts that came out of the interviews included growth in workplace champions’ self-confidence, an increased sense of ‘being a team’ and mutual support among cluster participants.
In terms of which aspects of workplace champions’ delivery had worked and not worked within their cluster, the questionnaire indicated that most workplace champions reported that the group catch-up sessions were well received:
The [catch-up session] worked well in terms of peer support, sharing ideas and motivating each other.
Questionnaire; WPC
Positive attributes mentioned in interviews included how the sessions sometimes acted as a ‘group confessional’, enhanced moral support and sharing of ideas, and triggered participants to re-focus and reinvigorate motivation; however, a few workplace champions found the catch-up sessions difficult to organise because of work demands and the difficulty of getting the cluster to agree on a convenient date/time often led to delays:
Can be hard to get everybody together for the group catch ups at the correct time as we are all in different teams. Sometimes it is delayed for several weeks.
Questionnaire; WPC
Some of the interviewed workplace champions who had small and/or high intracluster familiarity commented that the sessions were unnecessary, as they motivated each other regardless.
Workplace champions described the e-mail schedule as less burdensome than delivering the sessions, with many workplace champions reporting it easy to fit into their ‘day job’ if they were organised and planned it; however, other workplace champions fell behind in the schedule because of work pressures. A few workplace champions described how they adapted the e-mails to make them more substantial, motivating and impactful, even adding in humour. In this focus group, two champions discussed with their colleagues how they had adapted the e-mails:
Just on the e-mails and I can see it from both sides in terms of I’m a workplace champion, so I don’t think just black and white text they’re very inspiring at all...
FG20; P1
I colour mine up. I put smiley faces.
FG20; P3
One of our participants basically said, totally uninspiring. I think that was the phrase. So, the two or three I’ve done since then, I have added images.
FG20; P1
I noticed that actually.
FG20; P4
Just simple things like it’s OK to stand, it’s OK to sit, and an emoji or something like that which just feels like if I can add that in, and it stands out a bit more.
FG20; P1
Yes. I make my own random hashtags and I write #teamstanding.
FG20; P3
Interviewed workplace champions had mixed views on organising challenges in their clusters. Typically, workplace champions described challenges organised earlier on in the study fun and well received, but difficulty when thinking of new ideas and keeping colleagues engaged as time progressed. A difficulty mentioned by several champions, when reflecting on all elements of their delivery, was keeping both their own and their cluster’s motivation up over time:
We’ve tried to introduce a number of things that might keep people on the right track. The thing is having something new, though, every time, do you know what I mean? Because every time we meet, a lot of the things that I feel that we go over, we’ve been over before.
SWAL only
Although not related to the intervention itself, a final barrier for workplace champions was finding the time to complete the evaluation paperwork in addition to their normal workload.
Workplace champions were asked in the questionnaire to make suggestions on how things could be improved if they were to undertake the same role again. Several workplace champions mentioned that having more manager or senior leadership involvement would have helped so that their attempts to change behaviour at work was more ‘accepted’.
Among many workplace champions, a prevailing theme from free-text answers in the questionnaire was that the changes to workplace behaviour needed to be part of a wider change within the whole authority, not just a small proportion of it. Finally, some workplace champions felt that at least one meeting where all the workplace champions met together could have been timetabled to share experiences of what had worked well and how others had overcome challenges while performing their role.
Time spent on intervention delivery by workplace champions
Timesheets sent to the study team were used to calculate the amount of time workplace champions had facilitating the intervention. The mean (±SD) time spent by champions was 623 (±441) and 527 (±357) minutes in the SWAL-only and SWAL plus desk groups, respectively. The variability between workplace champions was in line with the amount of the intervention that was implemented.
Workplace champions were asked to rate on a scale of 1–10 (1 = not at all time-consuming, 10 = extremely time-consuming) the time burden of performing their role. Workplace champions reported a mean of 4.7, suggesting that the amount of time required was not overburdening and was manageable for most.
There were mixed experiences of time burden in those interviewed, which helps to explain the mean of 4.7. Some workplace champions talked about the role being easy to accommodate within their everyday work, noting good planning and organisation as key skills for being a workplace champion:
I’ve been able to fit it in. So, when I first got the timeline, I literally went onto the calendar and put in a reminder on all of the dates that I’ve had to send an email or the... group catch up.
SWAL only
Others workplace champions described difficulties with time and capacity during busy periods and increasing workload in their day job. Having more than one workplace champion in a cluster had, in most cases, helped share the workload and meant that someone else was available as a ‘back-up’.
Overall summary of intervention implementation
Appendix 10 provides a breakdown of the extent to which the components of the intervention were implemented within each cluster. The implementation of each intervention component will be discussed in more detail within this chapter.
Responses to questions on the different intervention components were split by gender to examine any potential differences between males and females; however, no meaningful differences in questionnaire responses were observed between male and female participants. Subsequently, responses in the following sections are summarised by intervention arm and time point only.
Online education
Participants were provided with a link to an online education session in the first e-mail they received from their workplace champion. If participants had not completed the online education training at 3-month follow-up, as indicated on their process evaluation questionnaire, then they were sent another e-mail as a reminder and then asked again at 12 months if this had now been completed. At 12-month follow-up, of the participants who were still enrolled in the study and returned a process evaluation questionnaire, 90% and 93% had completed the online education section for the SWAL-only and SWAL plus desk groups, respectively. Table 19 provides a breakdown of responses from participants who completed the online education.
| Response | Study arm, n (%) | Total, n (%) | |
|---|---|---|---|
| SWAL only | SWAL plus desk | ||
| Total | 198 (79.5) | 204 (85.0) | 402 (82.2) |
| Yes, all | 129 (65.2) | 145 (71.1) | 274 (68.2) |
| Yes, partially | 26 (13.1) | 18 (8.8) | 44 (10.9) |
| No | 43 (21.7) | 41 (20.1) | 84 (20.9) |
Participants who had not completed the online education were asked to explain the reason why. The following four key themes emerged from the responses received:
-
lack of time
-
forgot to do it
-
not aware of the online education
-
technical issues (e.g. no sound in the office to listen to the video excerpts).
Lack of time was the most prevalent reason why participants had not completed the online education. ‘Haven’t had time to do it, but I intend to’ (SWAL-only participant; 3-month follow-up) and ‘not got round to it yet’ (SWAL plus desk participant; 12-month follow-up) were common responses at both time points in both intervention arms. There were some participants who were not aware of the online education at 3-month follow-up. The link to the online education was included in the first welcome e-mail and so it is possible that some participants may not have read the e-mail fully. Technical issues were cited by a small proportion of participants who had not completed all of the online education session:
The link didn’t work for me and I forgot to let the team know.
SWAL plus desk participant; 3-month follow-up
Could not hear the sound on the video as the volume is disabled on computers in my office.
SWAL-only participant; 3-month follow-up
Participants who did fully complete the online education were asked to provide feedback on how useful found the online education, using a five-point Likert scale (1 = not useful at all, 5 = extremely useful) (Table 20). The top tips of ways to reduce sitting time was deemed the most useful component, with 66.2% of participants finding it useful or extremely useful between both intervention arms. The animations were also positively received, with 54.1% and 57.6% of participants finding animations useful or extremely useful within the SWAL-only and SWAL plus desk groups, respectively. There were also some case studies of previous participants provided, which were found to be useful or highly useful in 55.7% and 53.4% of participants within the SWAL-only and SWAL plus desk groups, respectively.
| Component | SWAL-only arm, % | SWAL plus desk arm, % | ||
|---|---|---|---|---|
| Useful | Extremely useful | Useful | Extremely useful | |
| Worksheet to calculate sitting time (%) | 38.8 | 7.8 | 42.7 | 9.9 |
| Goal setting sheet (%) | 5.8 | 35.7 | 7.7 | 33.1 |
| Top tips to reduce sitting time (%) | 48.0 | 16.2 | 44.4 | 23.8 |
| Animations (%) | 45.1 | 9.0 | 44.6 | 12.9 |
| Case studies from previous participants (%) | 48.4 | 7.4 | 38.2 | 15.3 |
Overall, the online education appeared to be very well received by both intervention groups (Table 21). The mean proportion of participants who agreed or strongly agreed across all statements was 81.6% and 83.9% for the SWAL-only and SWAL plus desk arms, respectively. The majority of participants from both intervention groups agreed or strongly agreed that the session increased their awareness of the health consequences of too much sitting, with 90.7% and 88.2% of participants in agreement within the SWAL-only and SWAL plus desk arms, respectively. Importantly, this increased awareness also resulted in 77.5% of participants in the SWAL-only arm and 85.7% of participants in the SWAL plus desk arm reporting that the session motivated them to make a change to the amount of time they spent sitting.
| Statement | SWAL-only arm, % | SWAL plus desk arm, % | ||
|---|---|---|---|---|
| Agree | Strongly agree | Agree | Strongly agree | |
| The level of the session was appropriate | 67.7 | 19.3 | 64.6 | 21.1 |
| The length of the session was appropriate | 62.7 | 12.4 | 62.1 | 18.0 |
| The session increased my awareness of the health consequences of too much sitting | 70.2 | 20.5 | 55.9 | 32.3 |
| The health consequences covered in the session motivated me to make a change to the time that I spend sitting | 61.5 | 19.3 | 54.7 | 24.8 |
| The health benefits of reducing and breaking up sitting motivated me to make a change to the time that I spend sitting | 60.2 | 18.0 | 55.3 | 28.6 |
| Overall, the session motivated me to make a change to the time that I spend sitting | 60.0 | 17.5 | 59.0 | 26.7 |
In addition to the process evaluation questionnaire, participants who attended the focus groups were asked to discuss their experiences of the online education. Focus group participants typically had vague memories of having completed the online education (it was approximately 12 months after they were asked to complete it), but recalled the online education as motivating and useful.
Participants who had positive memories of the online education tended to recall the content as interesting and surprising, in terms of facts and statistics about sitting and standing, and the impact that small changes can have:
I thought the little online training thing that we did right at the start, most of the details of which I’ve forgotten, but the message was quite clear, and I thought that was actually really good, really well done, well presented. And a little bit of an eye-opener in terms of the potential health risks. So, that was quite a motivator to get me going on it.
FG17; P3
Yes, because you don’t realise, I think, the implication of being sat down.
FG17; P2
Some participants recalled relishing the scientific content, whereas other participants ‘weren’t bothered about the science’ and preferred simple messages. When asked about key messages they could recall, participants tended to refer to the motivation they remember the programme triggering in them, as well as the overall health benefits of standing more:
Stand up more sit down less, it was about what I can remember from it.
FG20; P2
Two participants thought that the online education was so useful that they shared it with a wider group of colleagues, with one participant suggesting that it should be included as mandatory training:
Well, that’s what I predominantly used for my Lunch and Learn session. And I think it’s fab... We’ve got an online learning portfolio. And it should be part of the induction. Or a tailored version because it’s really interesting. And it’s really professional, informative.
FG34; P1
A small number of participants had revisited the online education, and many suggested that the link to the online education should be re-sent to jog their memories. Other participants said that they would prefer updated content and/or content in ‘bite-size’ chunks:
I mean, content updated, refresh the content and keep sending the links, and say look, this is something new.
FG1; P1
Yes, but do you know something, because we’ve done it once before, and because we’re so busy, I don’t think we would do it again, regardless.
FG1; P2
No, but if the content changed, new stories came up, then people would click and see what’s going on.
FG1; P1
Could you break it down into smaller chunks?
FG1; P3
Yes, rather than all at once.
FG1; P4
Because we may not have the time to review the whole thing again. I think I went in and had a couple of looks at certain little bits... But I think to go through the whole thing feels a bit too much.
FG1; P3
Some participants admitted being sceptical of online education as a format and associated the training with mandatory training for work, admitting that ‘another e-learning course certainly doesn’t get me excited’ (FG26) or noting how gamification allows completion without engagement:
You’re not rewarding me for reading what’s on the screen. You’re rewarding me for clicking next.
FG28
Other participants said that they struggled to absorb messages from e-learning, instead expressing a preference for in-person training with a chance to ask questions, which they felt would have been more memorable.
Participants were also asked to list what they thought the key messages of the online education were. Similar patterns were evident in the responses from both intervention groups. The most common response was to mention, in general terms, either the detrimental effects to health from sitting too much or the beneficial effects of reducing sitting. Typically, accompanying this was a message of standing more, moving more and/or sitting less, with some participants mentioning all three and some focusing on two:
The health consequences. How to move, sit less. The health benefits.
SWAL only
The benefits for your health and well-being by standing more at your desk and moving about. Sit less.
SWAL plus desk
Many health benefits to standing more and sitting less.
SWAL plus desk
A few participants were more specific, mentioning the benefits for reducing fatigue and improving alertness, improving the metabolism or blood sugar, musculoskeletal impacts, mood or well-being; however, it was more typical to refer to general health benefits.
Another common response was the importance of breaking up sitting by taking regular breaks, with some participants noting their comparative benefit:
Regular shorter breaks better than fewer longer breaks.
SWAL only
A common response was regarding having developed an awareness of the impact of sitting or realisation of the amount of time they spent sitting:
Awareness around health consequence of too much sitting.
SWAL only
Raised my awareness of how much I am sitting.
SWAL plus desk
Monthly e-mails
Workplace champions were provided with a folder of e-mail templates to send out monthly. Thirty three of 52 (63.5%) clusters reported sending ≥ 75% of the monthly e-mails over the 12-month period (see Appendix 10). Owing to the low burden of these e-mails, this was the most highly adhered-to task that workplace champions implemented.
In focus groups, there was a very mixed reception to e-mails. For participants who appreciated the e-mails, some commented that the e-mail content was not so important, rather that they served as a useful prompt and reminder:
What it does do is it reminds you. It does act as a reminder. I’ve never done any of the things and the e-mail could just say, ‘Stand!’ And that would probably do as much good for me as everything that’s in it because that’s the only thing it’s doing. It’s just giving me a prompt to remind me.
FG34; P2
Other participants emphasised the need for different content to enhance interest:
I think the e-mail is good. But more from your point of view, making sure you’ve got a suite of a different kind of tasks or things, so it doesn’t become repetitive.
FG29; P1
Some participants appreciated the effort of their workplace champion in preparing, sending and, in some cases, personalising the e-mails; however, many participants talked of ever-increasing e-mail traffic and overflowing inboxes with their everyday work, resulting in ‘e-mail blindness’ and SWAL e-mails just ‘get lost’ (FG28):
The e-mail prompts, I mean, a lot of people, most people get a lot of e-mails I’m guessing every day. So, they probably read it and go, oh okay and then onto the next thing.
FG20; P3
I don’t read any of them, and no offence because my workplace champion is sitting here!
FG20; P4
Alternative suggestions to e-mails included screensaver messages and pop-up messages a few times a week [e.g. information technology (IT) messages] on Yammer (Microsoft Corporation, Redmond, WA, USA) or Microsoft Teams (Microsoft Corporation; note that this was pre-COVID-19 when Microsoft Teams use was less common).
Sitting less challenges
There were three sitting less challenges that workplace champions were encouraged to initiate within their clusters over the 12-month period. Twenty eight of 52 (53.8%) clusters delivered all three challenges, with 45 (86.5%) clusters initiating at least one challenge. However, assessment of individual responses to the engagement with sitting less challenges showed that 34.2% and 26.6% of participants who answered the question in the SWAL-only and SWAL plus desk arms, respectively, reported taking part in a workplace challenge.
Participants who did take part in at least one challenge provided their feedback on the challenge(s) using a five-point Likert scale at 12-month follow-up (Table 22). A total of 64.5% and 53.2% participants in the SWAL-only and SWAL plus desk arms, respectively, agreed or strongly agreed that the challenges increased their motivation to sit less. A slightly smaller proportion of participants felt that the challenges had consequently reduced their sitting time (with 59.7% and 54.1% of participants in the SWAL-only and SWAL plus desk arms, respectively, at least agreeing). It also appeared that participants in the SWAL-only group found the challenges more enjoyable, with 64.5% of participants in agreement that they had enjoyed the challenges, compared with 48.4% of participants in the SWAL plus desk group.
| Statement | SWAL-only arm, % | SWAL plus desk arm, % | ||
|---|---|---|---|---|
| Agree | Strongly agree | Agree | Strongly agree | |
| The challenges increased my motivation me to sit less | 50.0 | 14.5 | 41.9 | 11.3 |
| The challenges reduced my sitting time | 46.8 | 12.9 | 45.9 | 8.2 |
| I enjoyed the challenges | 53.2 | 11.3 | 41.9 | 6.5 |
When asked of their experiences with the challenges in focus groups, the competitive element of intra or interteam challenges was enjoyed by many participants:
We did a contest... with some other teams... this step thing. Our team had the most steps compared to the two teams that we were pitted against that competition, which was nice.
FG9; SWAL only
Some workplace champions referred to competition as a good way to ‘get people energised’, with one workplace champion reflecting on how competition worked well for colleagues who knew each other well:
When we’ve done the competitive stuff... there’s been quite a bit of fun, banter and you know, that’s quite nice... A lot of us have worked together for a long time, and... you can have a more light-hearted approach to it,... So when we did the competitive element, and you know, ‘oh gosh, so and so... You’re last in terms of the competition... You have to know people well to take it to that level really so that’s been good.
SWAL only
Some participants in the SWAL plus desk group suggested that the challenges may be more useful for participants when not in the office:
I think all the challenges do as well is they acknowledge that you can do this over the weekend as well or stuff like that whereas we’ve been concentrating mainly on work.
FG26; SWAL plus desk; P2
A particular difficulty, in both intervention arms, was maintaining engagement in the challenges over time, as the novelty wore off or work took priority:
I think perhaps though, the challenges, probably we’re like, ‘yes we’ll do a challenge’. And then you get back into your work routines, and then work takes over.
FG27; SWAL only; P2
Workplace champions reflected on this difficulty and gave examples of efforts to increase interest, for example adding in a charity donation element as an incentive or adapting the challenges to make them more suitable or relevant:
It’s a talking point as well half the time... we’ve done the Land’s End to John O’Groats challenge which actually swiftly got changed to Land’s End to Liverpool, because... We’d still be doing that till way past the end of the project. So exactly, that’s been quite good... we did an update from Google Maps [Google Inc., Mountain View, CA, USA] and put who is where on the map, in terms of walking to try and generate a bit more competition.
SWAL only
A few participants reflected that their lack of engagement with the challenges was not lack of engagement in the study, rather that they preferred to reduce sitting and increase activity in their own way:
I think I was just more interested in, more naturally interested in just getting on with it myself, making myself do it... I did intend to actually record it and join in the challenges, but it petered out.
FG30; SWAL only; P1
Some participants and workplace champions felt that the challenges relied on having an activity monitor to track steps:
Unless you’ve got a device to monitor your steps, people aren’t going to do it because they haven’t got the devices to do it, and it’s very time-consuming.
FG7; SWAL plus desk; P2
Many others already had devices, but some put an app on their phone specifically for a challenge. One participant described how the combination of challenge and loading the app was a ‘wake-up call’:
And I think of myself as pretty active but the walking app that I’ve put on my phone which took me a while to get but once I’ve done it, told me I wasn’t. So, it really showed me how inactive I was in terms of walking when I thought I was more active. And it also showed how the smaller things can get your steps up that you don’t really think about but are pretty easy to incorporate.
FG26; SWAL plus desk; P1
Group face-to-face catch-up sessions
The intervention implementation timeline provided to workplace champions indicated that catch-up sessions should be held at 3 and 9 months. Twenty nine of 52 (56%) clusters had both catch-up sessions, 13 clusters reported running one session and 10 clusters did not have a catch-up session, meaning that 82% of clusters held at least one catch-up session.
At 12 months, participants were asked about their experiences of the catch-up sessions in the questionnaire. Of the participants who answered, 68.8% reported that they had attended a catch-up session. Of the participants who had not attended a catch-up session, 53% and 51% of participants in the SWAL-only and SWAL plus desk groups, respectively, said that they planned on attending future sessions. Participants reported their experiences of the catch-up sessions using a five-point Likert scale (Table 23). Participant responses were similar between both intervention arms. The majority of participants agreed that the group meetings were more worthwhile than a one-to-one meeting with the workplace champion, and that the meetings had helped to motivate them to sit less, although there was slightly lower agreement that the sessions had helped them to find solutions to the barriers they had experienced.
| Statement | SWAL-only arm, % | SWAL plus desk arm, % | ||
|---|---|---|---|---|
| Agree | Strongly agree | Agree | Strongly agree | |
| These sessions helped me formulate plans to sit less | 64.5 | 6.4 | 58.4 | 9.7 |
| These sessions helped me stay on track with my plans to sit less | 55.5 | 6.4 | 58.8 | 6.1 |
| These sessions motivated me to sit less | 66.4 | 8.2 | 61.4 | 9.6 |
| These sessions helped me find solutions to barriers I have experienced | 46.7 | 6.5 | 43.8 | 5.4 |
| Meeting as a group (rather than individually with the workplace champion) was worthwhile | 66.4 | 10.3 | 58.9 | 17.0 |
During focus groups, participants were asked if they had attended a group catch-up session and, if so, were asked for their feedback on the session. The views and experiences of participants were mixed, with some participants describing the sessions as ‘wonderful’ and others stating that they did not find the sessions helpful.
Participants who found the sessions useful and motivating said that they did so because of the long gaps between being measured, with the sessions refreshing interest and providing opportunities to hear tips from others:
Definitely useful. Like e-mails, as I said, if you keep refreshing, it’s motivating. Sometimes people lose track... so you help people to get back on trak...
FG4; SWAL plus desk; P1
It’s just good to hear other people’s techniques about what they do and get their ideas about how they move and carry out their day and things, so that was useful.
FG4; SWAL plus desk; P4
The encouragement as well, when you hear other people and what they’ve done as well. And it can motivate you again as well to think, oh I have to stand up a bit, because actually I could do that.
FG7; SWAL plus desk; P1
Other participants mentioned that the sessions provided dedicated time to reflect on their progress and an opportunity to consider barriers and gain peer support in addressing these:
It was good to think about and talk about it. And have a space to just come away from your work and consider how, actually, you can start making it a part of your routine, a bit more. Because [we’re] just into our habits and we don’t really have a chance to reflect...
FG34; SWAL only; P2
It was amazing. It was like a TED Talk [TED Conferences, LLC, New York, NY, USA]... If nothing else, it’s good for those who are brave enough to come along and ’fess up about how they’ve been doing or haven’t been doing. I think it’s a good reminder of why you’re part of it. Getting that information... and some coaching to help you think through what the barriers might have been.
FG34; SWAL only; P1
Furthermore, some participants talked about how sessions created a sense of being a team, which had an impact over and above supporting behaviour change:
And also encourage others so it’s like, you’re not alone, we’re in it together.
FG6; SWAL plus desk; P4
It has given us an element of solidarity really which is quite nice... it’s almost like the ten or 12 of us have got something in common that’s just for us.
FG6; SWAL plus desk; P2
In addition, as there were a lot of participants in the same office space taking part in the intervention, some participants felt that they regularly shared ideas outside the group catch-up sessions.
Several participants argued that the sessions worked better if group members knew each other well already and some participants described experiences of less enjoyable sessions when group member were less well known to each other and/or less forthcoming:
I think the characteristics of the team and the teams on this level could be quite different from other teams. So, a lot of the people we work with are maybe quite introverted so not as outspoken, so you don’t get the same openness to discuss... our catch-ups, the conversation are very stilted and we just kept to the agenda. Whereas in the office it’ll just flow.
FG26; SWAL plus desk; P1
The participants who spoke less favourably about the catch-up sessions, had typically not found the content useful, particularly in the later sessions:
Because it just didn’t seem very pointful. I did go to one meeting and there just didn’t seem any substance to it.
FG25; SWAL plus desk; P1
I didn’t find it useful, no. It felt like we need to meet. But do we really want to meet? And can we come up with anything? And nobody could really come up with anything. And we all just went away again.
FG30; SWAL only; P1
I think the first one was okay. I think the second one there was just a lot of repetitive group discussion.
FG26; SWAL plus desk; P1
Some participants mentioned their surprise that catch-up sessions were not organised as ‘stand-up’ meetings, although acknowledged that any one of them could have changed this.
Similar to the e-mails and challenges, some participants reflected that ‘one size doesn’t fit all’, with different elements working for different people. One workplace champion (who also participated in a focus group) described her efforts to adapt her delivery in recognition of how her group would receive it:
The thing about the group catch-ups is, you get like a six-page script as a champion that you’re supposed to do... I’ve not got time to read six pages before I go into it... because our team, we’ve all been there years, and we’re very close. If I sat there with that script, they’d absolutely laugh me out of the room.
FG27; SWAL only; P3
Participants varied on the frequency of sessions, with some participants recognising the difficulty of getting the optimal balance:
But I wonder... whether it would be better to meet more frequently, just to remind everybody that it’s what you’re doing and that it’s... still important... It’s a hard balance, isn’t it, between being too much and not enough.
FG29; SWAL only; P1
Participants recognised the logistical difficulties for workplace champions in organising the sessions because of people’s workloads and their differing work schedules, patterns and commitments.
Group catch-up session fidelity
Inter-rater reliability of audio-recordings
The recordings were assessed for IRR, based on a total of 53 recordings (SWAL plus desk group, n = 27; SWAL-only group, n = 26). However, after IRR was conducted, we noticed that three audio-recordings were invalid (i.e. two audio files were corrupt and one audio file was of a different session). Therefore, a total of 50 recordings (SWAL plus desk group, n = 25; SWAL-only group, n = 25) were assessed for intervention fidelity. Thirty recordings were for catch-up session 1 and 20 recordings were for catch-up session 2.
Fidelity on content
Overall, 62.9% and 55.8% of the content was ‘present’ and delivered as intended, 9.3% and 8.8% of the content was ‘attempted’, and 27.8% and 35.4% of the content was ‘absent’ for catch-up sessions 1 and 2, respectively.
The component ‘your story’ scored the highest (83.6%) in catch-up session 1 and the ‘introduction’ section scored the highest (76.2%) in catch-up session 2. Table 24 provides a full breakdown for each component per catch-up session.
| Component | Present, % | Attempted, % | Absent, % |
|---|---|---|---|
| Catch-up session 1 | |||
| Session introduction | 54.8 | 22.6 | 22.6 |
| Your story | 83.6 | 8.2 | 8.2 |
| Refresher of key messages | 62.5 | 7.1 | 30.3 |
| Goal-setting | 59.7 | 13.4 | 26.9 |
| OARS | 53.3 | 3.3 | 43.3 |
| Next steps | 63.3 | 1.1 | 35.6 |
| Overall scores | 62.9 | 9.3 | 27.8 |
| Catch-up session 2 | |||
| Introduction | 76.2 | 14.3 | 9.5 |
| Your story | 58.9 | 13.1 | 28.0 |
| Slip-ups and relapse | 49.6 | 7.8 | 42.6 |
| OARS | 51.2 | 4.8 | 44.0 |
| Next steps | 43.0 | 4.0 | 53.0 |
| Overall scores | 55.8 | 8.8 | 35.4 |
Fidelity on workplace champions’ verbal behaviours
The OARS component, consisting of four rows, was used to assess workplace champion verbal behaviours. The overall scores for catch-up sessions 1 and 2 were 53.3% and 51.2%, 3.3% and 4.8%, and 43.3% and 44% for ‘present’, ‘attempted’ and ‘absent’, respectively. Looking at each of the OARS techniques separately, findings showed that the use of an open-ended question technique was the most used skill for both sessions, with 90% and 90.5% ‘present’ for catch-up sessions 1 and 2, respectively. The scores for the rest of the OARS components rated as ‘present’ were 19.4% and 23.8% for affirmations, 56.7% and 52.4% for reflections, and 48.3% and 38.1% for summaries for catch-up sessions 1 and 2, respectively. A further breakdown of each OARS component is provided in Table 25, including ‘attempted’ and ‘absent’ scores.
| OARS component | Catch-up session 1, % | Catch-up session 2, % | ||||
|---|---|---|---|---|---|---|
| Present | Attempted | Absent | Present | Attempted | Absent | |
| Open-ended questions | 90.0 | 3.3 | 6.7 | 90.5 | 4.8 | 4.8 |
| Affirmations | 19.4 | 3.2 | 77.4 | 23.8 | 0 | 76.2 |
| Reflections | 56.7 | 0 | 43.3 | 52.4 | 9.5 | 38.1 |
| Summaries | 48.3 | 6.9 | 44.8 | 38.1 | 4.8 | 57.1 |
Duration
The overall time allocations for catch-up sessions 1 and 2 were 32 and 30 minutes, respectively. The analysis reported a mean delivery time of 32.52 minutes for session 1 and a mean delivery time of 37.45 minutes for session 2.
SWAL plus desk compared with SWAL only
The analysis showed a higher ‘present’ score for overall content and workplace champion’s verbal behaviours for the SWAL plus desk group (69.4% and 54.5%) than for the SWAL-only group (61.2% and 50.8%) for both catch-up sessions 1 and 2. The results showed that participants in the SWAL plus desk group were significantly more likely to score ‘present’ and significantly less likely to score ‘absent’ in catch-up session 1 (χ2 = 7.8, p = 0.020) than the SWAL only goup. There were no differences between intervention arms during catch-up session 2 (χ2 = 0.76, p = 0.684). The breakdown for the SWAL plus desk group were 8.1% and 9.1% for ‘attempted’ and 22.5% and 36.4% for ‘absent’ for catch-up sessions 1 and 2, respectively. For the SWAL only group, the scores were 7.2% and 8% for ‘attempted’ and 31.6% and 41.2% for ‘absent’ for catch-up sessions 1 and 2, respectively.
Self-monitoring
As part of the online education, participants were signposted to several computer- and phone-based software apps that are designed to assist in monitoring sitting time and/or to provide prompts to regularly break up sitting. Owing to the network security of the local authorities’ IT systems, some of the computer software and apps suggested required approval from the council IT teams to install them onto the work computers, and this presented a barrier for some participants.
Other self-monitoring tools included phone apps such as Rise & Recharge (Baker Heart and Diabetes Institute, Melbourne, VIC, Australia), MyHealthAvatar (URL: myhealthavatar.org) and Sitting Timer (Felno Jyrkänkatu, Lahti, Finland), as well as a Google Chrome extension [URL: outstandingapp.github.io (accessed 12 December 2022)]. Within the process evaluation questionnaire, participants were asked about their use of these self-monitoring tools at 3 and 12 months. There was a trend for participants to mention additional self-monitoring tools not included in the list of self-monitoring tools, such as wrist-worn activity trackers [Fitbits (Fitbit, San Francisco, CA, USA), Apple watches (Apple Inc., Cupertino, CA, USA), Mi Band (Xiaomi, Beijing, China), etc.], regular alarms on mobile telephones or alternative third-party mobile phone apps not suggested as part of the SWAL intervention. Table 26 presents the percentage of participants who reported using either our suggested tools or their own.
| Response | 3 months, % | 12 months, % | ||
|---|---|---|---|---|
| SWAL only | SWAL plus desk | SWAL only | SWAL plus desk | |
| Yes | 30.2 | 31.2 | 32.2 | 22.2 |
| No | 69.8 | 68.8 | 67.8 | 77.8 |
| No, but intend to try them | 44.0 | 45.8 | 31.0 | 26.2 |
The use of self-monitoring and prompt tools was low at 3 and 12 months, with less than one-third (31%) of responders reporting that they were using the tools.
The most popular self-monitoring tool among responders was Workrave, with 71% and 50.8% of participants who reported using a self-monitoring tool within the SWAL-only and SWAL plus desk groups, respectively, using Workrave at 12-month follow-up. The Google Chrome extension Outstanding was the second most used tool by participants in both intervention groups at 3 months (SWAL-only group, 31.2%; SWAL plus desk group, 44.6%). However, the percentage of participants using Outstanding dropped in both the SWAL-only and SWAL plus desk groups to 11.1% and 22.8%, respectively, by 12 months. Other self-monitoring tools used by participants were wrist-worn physical activity trackers that contained prompt functions when prolonged bouts of inactivity were detected. In addition to the type of self-monitoring tool used, participants were asked at 12-month follow-up whether they used the suggested self-monitoring tools at work or home. The majority of self-monitoring tools were used while at work only, with 100% and 96.8% of participants in the SWAL-only and SWAL plus desk groups, respectively, using the tools while at work. At home, use was much lower, with 14.8% and 12.9% of participants in the SWAL-only and SWAL plus desk groups, respectively, using a self-monitoring tool at home.
Participants were asked in the questionnaires and during focus groups to discuss their use of self-monitoring tools. Participants who reported using self-monitoring tools reported that the tools were useful in reminding them to take a break and raising awareness of the length of time between breaks:
I notice I really didn’t take any breaks, so it does prove as a good prompt. Even if you only take a break [for] a percentage of the prompts it’s still useful.
Questionnaire; SWAL plus desk
I think it has, it makes you aware. You know, you’re sat – you’re doing a piece of work and you think you’re only there for 5, 10 minutes. And then the thing goes off to say actually you’ve been sat for 30 minutes. So, it does give you that sort of prompt to get up and move around.
FG11; SWAL only; P1
Other participants reported that, despite being prompted at inconvenient times, they could see the value of having the tools as a tool for behaviour change:
At one point I got frustrated about being interrupted... when I had a deadline to achieve. I was quickly reminded of the shooting pains I used to get across my shoulders when I had worked all day – I have kept the app on ever since.
Questionnaire; SWAL only
Focus group participants typically described installing and trying out different prompt software and apps. Participants reported finding prompts helpful initially; however, over time, some participants turned the prompts off, as the novelty wore off or because of workload increases, and other participants reported that the prompts became increasingly intrusive:
... those things tend to work very short term for me and I forget about them or ignore them.
FG25; SWAL plus desk; P1
I found the Workrave thing that was installed on my laptop, it was just too... If I was working on a report where I might need to be sat at it for an hour, I just found it too intrusive, and once it broke my concentration, I couldn’t get back into it.
FG27; SWAL only; P1
I’ve got the Workrave thing, and when I first had it, I did tend to do some of the exercises and things... Partly I think it’s because my workloads just got more intense recently, but now when it pops up, I shut it down. It’s just become a thing that, it’s just a distraction really.
FG4; SWAL plus desk; P2
Some participants had managed to address one or more of these issues by changing the settings of apps/tools to suit their preferences:
Important to set the prompts at a sensible frequency otherwise it ends up being more irritating than useful and you then just turn it off!
Questionnaire; SWAL only
Many participants talked about using Fitbits or apps, both within and outside work. For some participants, this meant not using any of the software/apps on their work computer:
I haven’t really used any of them because I’m not someone who uses loads and loads of apps. But I’ve got a Fitbit, and I’ve had a Fitbit for probably a year and a half, 2 years maybe. So... I don’t really have room for another thing.
FG35; SWAL only; P1
Some participants admitted that having a smart watch that vibrated was even easier, as the smart watch did not require the participant to be carrying or looking at their phone or computer:
I prefer having my watch and then it just vibrates. And then that’s an automatic reminder.
FG34; SWAL only; P2
Height-adjustable workstation
All participants in the SWAL plus desk group received a height-adjustable workstation. Research teams initially aimed to get all workstations delivered within 1 month of randomisation; however, there was an unanticipated delay in getting workstations to some offices because of the process of purchasing the desks taking longer than expected, as the monetary value of the orders required additional checks from the university finance teams. There were also slight delays once the workstations had been delivered to the councils, as the workstations needed to be delivered and installed by facilities staff. Therefore, the average time between a participant being randomised and receiving their workstation was 65 days. Accordingly, the 3-month follow-up was pushed back slightly to ensure that participants had use of the workstation for at least 1 month prior to the 3-month follow-up assessment. A breakdown of which workstations participants chose is shown in Appendix 11.
In the first month of receiving the height-adjustable workstation, 77.7% of participants reported that they used the workstation every day, 17.5% reported using the workstation a few times a week, with only a small percentage of participants reporting using the workstation less frequently (Table 27). The proportion of participants using their workstation at 3 and 12 months was 98.9% and 94.3%, respectively. There was a decrease in the frequency of use between the 3- and 12-month follow-up, with a reduction of 27.6% of participants using the workstation every day. However, 82.9% of participants at 12-month follow-up were still using their workstation at least a few times a week, suggesting that they were still engaging with this aspect of the intervention.
| Response | Time point, % | ||
|---|---|---|---|
| First month | 3 months | 12 months | |
| Everyday | 77.7 | 80.1 | 52.5 |
| A few times a week | 17.5 | 16.0 | 30.4 |
| Once a week | 1.5 | 2.2 | 5.7 |
| Infrequently | 3.4 | 1.7 | 11.4 |
As noted earlier in this chapter, getting a workstation was the main incentive for participating in the study for many participants, and participants were keen to know whether or not they could keep the workstation after the study period, noting that they could not imagine being without it:
Yes, they’re really good. I can’t see myself working without the desk now...
FG4; SWAL plus desk; P3
I do like my desk, and I can’t imagine being without it now. Please don’t take it away.
FG4; SWAL plus desk; P1
I think you’d have to fight us!
FG4; SWAL plus desk; P4
Typically, participants with desks regarded the desks as key for changing their behaviour:
If we didn’t have the desks, then I don’t think it would have made any difference to me [in changing habits], to be honest with you. I think having the desk made a huge difference to me.
FG7; SWAL plus desk; P1
Participants provided many explanations for how the height-adjustable workstation worked for them as an enabling tool for changing their behaviour to working while standing and as a prompt in itself:
It helps me stand up a lot more than I usually would.
Questionnaire; SWAL plus desk
Having the desk and so the option to stand, it also acts as a prompt and has become a normal part of the office environment.
Questionnaire; SWAL plus desk
Means I can stand and continue to work uninterrupted, rather than try and find excuses to stand away from my desk.
Questionnaire; SWAL plus desk
Carry on working, I have an intensive/demanding job so I’m reluctant to take lots of breaks so being able to stand and take breaks every so often has been beneficial to me/my pattern of working.
Questionnaire; SWAL plus desk
Many focus group participants described developing routines and habits when they used their desk, but other participants admitted that their initial enthusiastic use of the desk had waned over time. Some participants explained this is terms of the novelty wearing off:
I think at the start I was a lot more yo-yo going up and down using the desk. That plateaued a little bit and I’ve been a bit sitty-downy. I have started to use it again. I know my colleague [name] he stands pretty much the whole day I think. He only sits down for his lunch or if he’s... I think when he’s reading stuff his desk’s always up. So yes, he must use it constant. But that suits him and his way of working whereas I chop and change. Which is fine, it works for me. But I don’t think I use it as much as I probably should.
FG16; SWAL plus desk; P4
I’m kind of like you, straight out of the blocks 12 months ago stood up as much as possible then all of a sudden... It’s easy to slip and slide into things isn’t it?
FG16; SWAL plus desk; P2
A key theme running throughout discussions of workstation use was the influence of other colleagues, both other users and others not in the study. Associated with the novelty of the workstations early on was talk of a ‘meerkat’ or ‘domino’ effect, whereby one person standing up to use the desk would impact on others:
I think overall people have taken to it, but I think in the last 6 months the meerkat effect has stopped. People are actually finding their desk a little bit clunky, a bit space consuming for other stuff... actually doing other things on your desk is quite limiting with these Yo-Yo desks. Trying to write something, I have to move and I’m interfering on the person next to me.
FG26; SWAL plus desk; P1
Some participants talked of their use dropping off because of issues with space on the desk, wires getting tangled and how having papers spread out on the workstation prevented regular use:
I don’t use it as much as I first did or as much as I thought I would use it. And partly, as someone mentioned before, it’s about having bits of paper and other things that you need when you’re standing up, it doesn’t work very well with that. And my desk was, until yesterday, an absolute tip. So, it’s a bit awkward because you get some stuff stuck underneath it.
FG25; SWAL plus desk; P1
Other participants described how physical difficulties moving the desk up and down had put them off using it over time:
I’ve had to stop using it as you know because I find... I don’t know if it’s because I’m petite or small, lifting it was straining my back. I have upper back problems anyway and then I found that aggravated it a bit.
FG16; SWAL plus desk; P5
A few participants admitted that, despite trying, standing just did not suit how they worked (which relates to the next section):
I just find myself sitting the same as I did 12 months ago, if I’m completely honest. That’s because I don’t get along with the standing desk. I stand and I find it hard to concentrate whilst standing as opposed to just sitting. I do a lot of data crunching, so I think to be... I like to have my face in the screen, and I don’t feel I can do that with my standing desk.
FG6; SWAL plus desk; P4
Participants reported the type of factors that influenced their desk use (Table 28). There was a higher tendency for desk use to be influenced by time-based and intrinsic factors, rather than prompt- or task-based factors, suggesting that participants were more likely to use their desk at certain times in the day or in response to listening to their body, than specifically using the desk when working on particular tasks, and this remained similar across time points.
| Factor | 3 months, % | 12 months, % | ||
|---|---|---|---|---|
| Often | Very often | Often | Very often | |
| Task-based factors (e.g. reading e-mails) | 23.2 | 7.7 | 21.8 | 6.4 |
| Time-based factors (e.g. in the afternoon, every hour for a certain length of time) | 36.3 | 21.4 | 31.3 | 15.6 |
| Prompt-based factors (e.g. when the telephone rings, when someone comes to see you) | 11.0 | 6.6 | 13.5 | 2.6 |
| Intrinsic factors (e.g. when your body tells you it’s time to stand up/sit down) | 48.3 | 24.2 | 37.9 | 25.5 |
A common example of a routine of workstation use was using it in the morning, but lowering it later when tired, achy or needing to do work that was easier when sitting:
I’ve just changed my routine now. I have a 30- to 40-minute drive in... so I don’t even sit down when I come in. I make a drink, put the stand up and my first least hour in the day is stood up, unless I feel tired.
FG20; SWAL plus desk; P1
I tend to start standing, and I stand for maybe an hour and a few minutes, and then sit. After lunch I tend to sit more.
FG4; SWAL plus desk; P3
Several participants described a tip for enabling routine as leaving their workstation up when they left work so that it would be ready for using first thing, as explained by this participant who had developed a regular routine:
When I leave work, I make sure I’ve left it up, so when I come in, it’s up, so then, yes, I’ll stand for as long as I... We usually have a meeting around either 8.45 or at 10.00, so I try and stand up until that meeting. I’ll sit down for the meeting but leave the desk up. I’ll stand up for as long as I can. I sit down for lunch and then try and get back up again as soon as I can.
FG17; SWAL plus desk; P1
Many participants talked about sitting for lunch, and although some participants preferred to stay sitting after lunch, others stood again to combat the post-lunch sluggishness or to aid digestion:
Yes, I’m normally straight after lunch. Helps me digest.
FG15; SWAL plus desk; P1
It’s very good for when you reach that afternoon lull. After lunch when you start getting that post-prandial feeling you think, I should stand up now, that would help.
FG16; SWAL plus desk; P4
Focus group participants commonly talked about different types of work that suited standing, both with and without the raised workstation, and other types of work that they preferred to do while sitting down, and this was very much an individual preference.
Many participants talked about e-mails and telephone calls being a suitable task to do standing, although some participants found difficulties with typing e-mails while standing:
It’s easier with e-mails. It’s harder for writing a report or doing any real written work. If I have to write a lot of reports, I find it’s difficult to do that.
FG17; SWAL plus desk; P2
Some participants preferred to do tasks that required concentration while sitting, whereas other participants commented on how standing helped them to concentrate on certain task:
I can work a bit better sitting down, being able to really get into a piece of work as opposed to standing up. I’ve not been able to find the sweet spot when standing. I can find myself, when I am standing, focusing more on trying to be comfortable while standing than actually on my piece of work. So, I immediately go, well I’m not concentrating on my work, let’s get back to the sitting down again.
FG6; SWAL plus desk; P4
I think when we first started, if I had something I had to concentrate on, I thought I had to be sat down and hunkered over it. Whereas actually I’m better, now concentrating on those tasks while I’m stood up and it’s just a little bit of a mindset change. I don’t have to be hunkered over the desk and, you know, like that. I can do that stood up. I can work through the complicated stuff whilst standing just as well as I can while sitting.
FG7; SWAL plus desk; P2
Strategies to sit less and move more
When participants were asked about strategies to sit less and move more in the process evaluation questionnaire, there were similarities and differences between the two intervention groups.
Starting with the main difference, the most common responses from participants in the SWAL plus desk arm related to their adjustable workstation and the associated strategies they used to facilitate using the workstation, for example using different reminder systems (Workrave software, apps, timers, etc.) to prompt raising the workstation at regular intervals or for a set duration:
Stand for 15 minutes at the top of every hour.
Questionnaire; SWAL plus desk
I stand for at least 3 hours, first thing in the morning, then 2 p.m.
Questionnaire; SWAL plus desk
Stand for at least 1 hour every afternoon. Stand for half an hour every morning.
Questionnaire; SWAL plus desk
Participants also reported strategies that aided developing a routine:
Keep the desk up in the evening so encourages you to stand first thing in morning.
Questionnaire; SWAL plus desk
Participants also talked about the influence of other colleagues raising their workstations or providing verbal reminders to stand.
Participants in the SWAL-only group mentioned efforts to stand, take breaks and move at regular intervals using reminders (e.g. Workrave, apps and alarms); however, there were far more mentions of this in the SWAL plus desk group.
Participants from both intervention arms mentioned task-based strategies for standing and moving. The two most popular task-based strategies included walking to speak to colleagues instead of e-mailing, or standing up when talking on the telephone or to a colleague in person:
Standing when taking calls going to speak to colleagues instead of e-mails.
Questionnaire; SWAL only
Making effort to see colleagues rather than emailing/phoning them standing up when colleagues come over to see me.
Questionnaire; SWAL plus desk
Again, these task-based strategies were echoed in the focus groups:
I do try, in any given hour... I try and get up and do something. I’ll save the e-mail and go and see the person. Or I’ll do a walk through the building. So, I do make it more of a priority to get up every hour whereas, previously, I wouldn’t have thought of getting up every hour.
FG34; SWAL only; P1
There were several mentions of standing in meetings and trying out a ‘walking meeting’, particularly for one-to-one meetings, but these strategies were not mentioned by many participants.
Popular strategies listed by participants in both intervention arms related to using different facilities in the office, including using toilets on different floor; making more frequent trips to the photocopier, printer or waste bin (as opposed to combining in one trip), and using those further away; making more frequent trips to the water cooler and using a smaller bottle to trigger this; making more hot drinks or collecting one’s own hot drink instead of relying on a colleague collecting it; and generally using the stairs more:
Picking up own letters from printer. Walk to furthest kitchen/toilet. Making own cup of tea.
Questionnaire; SWAL plus desk
Get fresh drink every hour – walk and hydrate.
Questionnaire; SWAL only
Making tea more often more toilet breaks.
Questionnaire; SWAL plus desk
These strategies were echoed and reflected on in the focus groups:
We use the toilets on the ground floor. We’re on the third floor so just little things like that.
FG16; SWAL plus desk; P2
A popular strategy mentioned by participants from both intervention arms was doing a regular lunchtime walk, either alone or with others:
Walk with work colleagues around block.
Questionnaire; SWAL only
Lunch time walk around local park.
Questionnaire; SWAL only
Go out more at lunch instead of working things.
Questionnaire; SWAL plus desk
In the focus groups, participants elaborated on how workload and habit meant that, more often than not, people tended to eat lunch at their desk. Many participants talked about the intervention triggering them to make a concerted effort to go for a lunchtime walk and how beneficial they thought this was:
If I get a phone call on my mobile, I stand up and go out now. I go for a walk at lunchtime every day, even if it just might just be around the gardens, which is a 10-minute walk, but I get outside and just move... Because [before] I was a proper ‘sit down with my lunch’... But now I get out the building and just move, really, so that’s a behaviour change.
FG29; SWAL only; P2
Other lunchtime activities featured in focus group discussions too, with participants mentioning running, cycling and yoga. Workplace champions, who had an awareness of their group’s collective activities, talked about the activities.
Walks tended to be subject to fewer barriers:
There’s been a running group that’s started as well... Three of the participants from the five are in the running group, all of the five are in the walking group and we’ve just started the cycle group, which is two of us are in that. So that’s me and [name] are actually starting to cycle as well on one day.
WPC; SWAL only
A strategy that featured in the questionnaire responses was adapting one’s commute and other travel to a more active mode, including parking one’s car further away from work/shops, getting off the bus at an earlier stop, standing while waiting of train/bus, and replacing driving with walking when shopping, running errands or dropping children off.
Focus groups participants elaborated on such changes:
I suppose also with work travel rather than driving places, whereas in the past I’d just think I’ll drive because it’s convenient door to door,... but more reflecting now when I’ve got a meeting, ‘Can I get the tram?!’... If I’ve got a meeting where I’m going somewhere train and tram, I can actually walk from home 10 minutes to the train, get on the train for 10 minutes and then get a tram.
FG35; SWAL only; P1
I walk to and from work, but I look for a slightly longer route than I would normally.
FG6; SWAL plus desk; P1
Participants were asked about the strategies they used to sit less and move more outside work. The most common responses related to reducing time spent sitting while watching television (TV), with many participants reporting using the advert breaks or the end of TV programmes as a trigger to stand up, stretch, move or walk to the kitchen to make a cup of tea. Many participants also mentioned standing/moving (e.g. walking on the spot, standing up to iron) for periods of TV-watching and for other screen-based activities (e.g. looking at social media or gaming) or reading. A similarly popular method was standing or pacing while on telephone calls:
I think it’s not just at work. I think even at home I’m consciously now, if I’m talking to somebody [on the telephone] in the past, I would sit for half an hour, but now I’m actually walking, I’m pacing up and down, whilst I’m doing that. Or, sometimes, even if I’m watching TV, I’ll just stand and watch a little bit. It’s not just at work, I think it’s made an impact on my whole day... I think I’ve changed my whole routine, not just at work, even at home.
FG4; SWAL plus desk; P2
Also common in the process evaluation questionnaire were strategies associated with household ‘chores’ (e.g. cooking and washing-up), with participants making a concerted effort to increase time spent doing chores and, therefore, being on one’s feet, or simply ensuring that one stayed standing while doing the chores. More kitchen-based standing was in the form of standing while eating breakfast or having a drink. Outside work, participants with children or caring responsibilities typically described being ‘on their feet’ a lot at home anyway, which was echoed in focus groups.
Many questionnaires featured reports of having increased walking as an activity, with reports mentioning more weekday evening and weekend walks, adding more dog-walks, some walking groups and using self-monitoring tools to count steps. Other participants reported starting, continuing or increasing running, gym work or gym classes; however, quite a few participants talked about being less active at home than at work, often because of being tired in the evenings or simply wanting to relax:
I think I probably sit down too much at home in some ways. Sometimes, but the time I’m home it’s getting later on anyway, and I’m ready for a rest by then. It’s been a long day.
FG4; SWAL plus desk; P1
Benefits of sitting less
Participants reported various benefits of sitting less in the questionnaire and most of the themes also featured in focus groups where participants elaborated further. Participants reported several psychosocial benefits, such as feeling more energetic and being more productive and focused during work:
Increased focus on reading, bit more energy, feeling like I must be doing something positive for my health.
Questionnaire; SWAL plus desk
It helps me to focus more on a task. I felt less fatigued at the end of the day. I feel more alert and productive.
Questionnaire; SWAL only
Several participants explained how the intervention, and the positive impact of feeling more energised, helped them to change their mindset and feel more justified in taking a break:
I think going out at lunchtime for our walks has definitely... It makes the afternoon easier. I feel a bit more motivated and a bit more energised in the afternoon on the days you go for a walk. I also feel less guilty about taking breaks from me desk now.
FG21; SWAL only; P1
The simple act of changing posture to stand or go for a short walk to break up sitting was welcomed as a nice change physically and mentally:
Psychologically positive as I feel I’m doing something to improve my health.
Questionnaire; SWAL only
Another common theme was the feeling that sitting less had helped participants to avoid the sluggish feeling they often experienced later in the afternoon:
By getting up and standing at regular intervals your body is fired back up and helps you to feel more alert.
Questionnaire; SWAL only
Good for back and when feeling sleepy after lunch.
Questionnaire; SWAL plus desk
There were several comments that reducing sitting had helped to attenuate participants’ previous musculoskeletal problems, relieve general ‘achiness’ or improve one’s posture:
Previous aches in neck and hips reduced; more comfortable standing.
Questionnaire; SWAL plus desk
Spend at least half day standing – more energy, don’t have the aches and pains after day of work.
Questionnaire; SWAL plus desk
I think it was helpful for the back from sitting. I used to get loads of just achiness and back problems from just sitting all day long, you know, at your desk, so positive from moving around... The aches and pains have gone away.
FG7; SWAL plus desk; P2
Barriers to sitting less
In the process evaluation questionnaire, common responses about barriers to sitting less or moving more could be grouped into the following categories: work related, physical office environment (including lack of height-adjustable workstation for those in the SWAL-only group), interpersonal, personal attributes and physical (e.g. tiredness and aches). These categories also all featured, and were explained in more detail, in focus group discussions.
The most common work-related barriers included workload, work and time pressure, and concentration, and all were typically being experienced as easier while sitting:
Need to concentrate for long periods in my job makes regular standing difficult.
Questionnaire; SWAL only
Business of work – we have been overwhelmed and understaffed.
Questionnaire; SWAL only
Feeling tired/stressed/too much on and no band width to think of the standing bit!
Questionnaire; SWAL plus desk
I think I’d got to a point where I was standing a lot. But I noticed that when things changed for me in terms of work... So, at the moment we’ve got a huge project that we’re trying to get over the line, quite stringent deadlines, really overwhelming with a lot of work. I’m not standing at all... I’m just sitting all the time. And I do miss the standing.
FG6; SWAL plus desk; P2
I think you’re right, I think it’s connected. When you’ve got so much on, you forget to stand up. You just, it just goes out your head.
FG6; SWAL plus desk; P5
Just goes out your head, yes.
FG6; SWAL plus desk; P2
And then, when you’ve got a bit of time then you suddenly think, I’ve not stood.
FG6; SWAL plus desk; P5
Yes, and work isn’t quite as pressurised, then you think, ‘I’ll stand today’.
FG6; SWAL plus desk; P2
Many participants in the SWAL-only arm mentioned lack of a height-adjustable workstation as a key barrier:
Not having anywhere to position my laptop to be able to work standing up.
Questionnaire; SWAL only
It’s not practical to stand when working at a regular desk.
Questionnaire; SWAL only
Interpersonal factors that featured included both perceived and/or experienced impact on others on one’s standing/moving more and the influence of others on these. Some participants expressed the feeling that not being sat at their desk meant that colleagues deemed them not to be working:
I do feel conscious if I keep getting up as it may give an impression that I am not working.
Questionnaire; SWAL only
In the SWAL plus desk group, feeling self-conscious while standing when surrounded by people sitting or in presence of senior management, as well as lacking peer support, had a detrimental effect for some participants:
Feeling self-conscious – during certain meetings involving senior management. I am less comfortable standing. I am ok with this during ordinary team meeting.
Questionnaire; SWAL plus desk
I’d also look a bit of a lemon because there’s nobody else standing around me. If I answer the phone with the headset on and I’m chatting away, I’m above everybody else.
FG11; SWAL only; P3
This self-consciousness of participants and need for peers translated to meetings too:
Awkwardness of standing in meetings when everyone sitting.
Questionnaire; SWAL only
In addition, participants mentioned many types of meetings where they perceived it to be impossible, inappropriate and/or not encouraged by the organisational culture to stand:
Too many meetings where it isn’t always appropriate to stand.
Questionnaire; SWAL only
Lack of support in the organisation i.e., not encouraged to do standing meetings.
Questionnaire; SWAL only
Participants also admitted to many personal attributes that they thought contributed to not standing or moving more, with the most common being ‘laziness’, forgetting and habits being too ingrained:
My own laziness!
Questionnaire; SWAL plus desk
Just forgetting to move sometimes.
Questionnaire; SWAL plus desk
I don’t know [why] I’m not using the desk as much. I can’t –
FG26; SWAL plus desk; P1
No, I don’t. I don’t know why,...
FG26; SWAL plus desk; P2
I can’t figure it out.
FG26; SWAL plus desk; P1
Because it’s comfortable when I do [use] it.
FG26; SWAL plus desk; P2
Some kind of ingrained, just laziness. I’ll be sat down, and I just think just get up and I just go ah, carry on.
FG26; SWAL plus desk; P1
A few participants in the SWAL-only group reported that they had tried to reduce sitting by standing at their desk without having the use of a height-adjustable workstation, resulting in neck, back or foot ache. In addition, some participants in the SWAL plus desk group initially reported aches in the first few weeks of sitting less; however, this often seemed to attenuate when other strategies were incorporated or over time as they got used to sitting less:
Feet ached initially, but wearing trainers while standing.
Questionnaire; SWAL plus desk
Feet got tired, it can be tiring, desk is heavy to lift up, slight back ache.
Questionnaire; SWAL plus desk
When I first started using it, it was quite tiring for legs and back [but I gradually got used to it].
Questionnaire; SWAL plus desk
Intervention sustainability
What proportion of the target group maintained any changes in their behaviours and were there any differences between males and females?
Owing to the COVID-19 pandemic, the originally planned 24-month follow-up did not take place and this was the time point where questions on maintaining behaviour change would have been addressed over the longer term. However, data from the questionnaire and focus groups indicated that engagement with some intervention strategies for some participants did wane over time, and there was some indication of this with workstation use and engagement with self-monitoring tools and challenges.
What proportion of the target group continued using/accessing intervention strategies across the study
There was a mixed level of sustained engagement with different intervention strategies over the duration of the study.
The proportion of participants using self-monitoring tools in the SWAL-only group increased slightly between the 3- and 12-month follow-ups, suggesting that participants in this group found the tools useful and continued using them throughout the study to help with behaviour change. Conversely, there was a ≈10% drop in the use of self-monitoring tools within the SWAL plus desk group. It is possible that participants in the SWAL plus desk group used the workstation as the main tool to change behaviour, and this is synonymous with the feedback that workstation use was initiated because of prompt-based factors in a small proportion of the group (3 months, 17.6%; 12 months, 16.1%).
The frequency of use of height-adjustable workstations was initially very high, with 96.1% of participants using the height-adjustable workstation at least a few times a week. By 12 months, use of height-adjustable workstations had decreased to 82.9%, which still represents a high level of sustained use, even after the novelty of using one had reduced. The factors prompting the use of the height-adjustable workstation did not change over time, suggesting that participants incorporated its use into their working pattern early on and this did not change throughout the study.
Are participants/workplace champions/the council going to continue with the intervention in some way and is there anything that needs to change with the intervention to assist with sustainability?
Owing to the COVID-19 pandemic, the originally planned 24-month follow-up did not take place, which was the time point where questions on sustainability were going to be explored, and we are, therefore, unable to answer this question.
Intervention contamination
Did movement of staff (e.g. participants, health and safety personnel) occur from intervention to control office groups?
During the study, there was one participant who moved office from an intervention cluster to a control cluster. In addition, there were two instances where a participant randomised to the SWAL plus desk group moved to an intervention-only cluster. In these instances, the participant moved with their desk (where applicable) to their new office location and continued receiving the other intervention components from their original workplace champion.
Did intervention participants interact with control participants?
Participants in the control group of the study were asked during focus groups if they had spoken with anyone from an intervention group or had been in any offices where the intervention was taking place, but most participants had not. Several participants had seen and walked through offices where there were standing desks, not necessarily always in use. A few participants had friends or colleagues in other groups who they had discussed the study with:
Yes, I’ve spoken to people that are in the middle group. They didn’t get the desk, but they got the other interventions. So, I’ve talked to them about that.
FG26; control; P3
Have you spoken about anything they’re doing, and has that influenced you in any way?
FG3; control; P3
No because the things that they’ve said to me are things that have irritated them! So, no, I don’t think so. Because obviously the interventions they’ve had are to try and encourage them to walk around a bit more, and stand up, and I’ve subconsciously trying to do that anyways.
FG3; control; P3
Do control office clusters engage in any strategies that may impact on their activity levels during work?
Within the process evaluation questionnaires, participants in the control group were asked about the wider impact of having health assessments as part of the study, and whether or not they had made any changes to their lifestyles in the preceding 3 months. Participants reported individual strategies to increase their physical activity and reduce sitting behaviour. Some participants reported that wanting to improve their health results from the baseline health assessment had resulted in them walking/cycling to work instead of taking public transport. During work, some participants reported that they were trying to use the stairs more often instead of the lift or were purchasing their lunch from a shop further away from their office to encourage additional walking. In relation to sitting behaviour at work, some participants reported that they had tried to change their behaviour, but this had been a struggle:
My work environment is NOT conjunctive to making changes – options for standing working are minimal and/or impractical – frustrating!
Questionnaire; control
I realise I should be standing up more as when I have been sitting for a long period of time, I feel stiff when I stand up. However, I get too caught up in my work to remember to stand.
Questionnaire; control
In the focus groups, a few control participants expressed a desire to change their behaviour because they were in the control group and were disappointed about not receiving the workstation or other intervention, disclosing that they wanted to prove that they could do it regardless:
There was a very tiny part of me that did think, I’ve not got the desk, but I shall still continue to walk upstairs and things and prove actually that having the riser desk doesn’t make any difference. But that was just a little bit of me thinking almost to disprove your study but then I just carried on obviously.
FG12; control; P3
Strategies that control participants mentioned included trying to stand more in meetings, arranging meetings in other buildings, using the stairs more, standing at regular intervals and walking to facilities that are further away:
So, I started to look for ways to improve my own health within the working environment. And I know the suggestions were to stand at your desk rather than sit, or you stand in a meeting rather than sit. Or you know, you set a meeting elsewhere where you have to walk to that meeting room rather than tell somebody to wheel over to your desk and stuff like that. So it did change my own attitude to how I was working in my own environment as well. It made me think about actually, if I make sure that at lunchtime I go for a walk. So, it’s all these little motivations to try to improve your own health and wellbeing.
FG1; control; P4
Yes, I think for me I get up every hour. I’ll just make sure I get up for a quick walk or get a coffee or do something.
FG14; control; P1
Actually, thinking about it I have changed. I do get up from my desk a lot more now than I did.
FG14; control; P2
Or to go a photocopier.
FG14; control; P3
Other participants talked about changing their commute or work travel to a more active mode (e.g. cycling or walking), whereas other participants focused more on dietary changes.
Unexpected events arising from the study
Did intervention and control participants modify their behaviours based on information provided at the baseline and follow-up measurements?
Participants in the control group were asked whether or not they thought being a part of the study, despite being in the control group, had changed their sitting behaviour at home or at work and 65 of 192 (34%) participants said yes at the 3-month follow-up and 53 of 185 (29%) participants said yes at the 12-month follow-up. Participants received results on their health assessments at baseline and at 3 and 12 months. At 3 months, a large proportion (77.0%) of control participants reported agreeing or strongly agreeing that the knowledge of receiving future health results motivated them to change their lifestyle; however, this had fallen to 47.9% of participants by the 12-month follow-up. A similar trend was observed when control participants were asked whether or not receiving follow-up health assessments had motivated them to change their sitting behaviour specifically, and at 3 months 69.3% of participants were in agreement or strong agreement, but this reduced to 29.0% by 12 months.
In the focus groups, control participants typically commented that receiving their test results had given them an increased awareness of the need to be more active and an impetus to make some behaviour changes. However, for some participants, this did not necessarily lead to a change in their results at the subsequent testing:
I think it gave me a bit of a kick-start back into exercise, because I’d given up the gym for a period of time so it made me think, yes, maybe your weight is not as great as what it should be... for me between the first and the second session, when I looked at my measurements, there wasn’t actually a really great deal of difference. And I think I was a bit disappointed in that, because I thought my weight might have gone down and things might have improved quite significantly, because I was exercising...
FG19; control; P1
I fortunately do a lunchtime exercise class at work, so it spurred me into going to that a bit more regularly. And making sure that I’m participating it, as [name] said. It was kind of a spur to do that more often when I can fit it into my working day.
FG19; control; P4
It just made me more conscious of what... Of my activity levels and it was like sometimes it’s quite easy to sit at your desk and then it’s 11 o’clock and you haven’t moved. And I make a conscious effort to move and to walk down the stairs and back up again.
FG19; control; P2
Participants in both intervention groups were more strongly motivated than participants in the control group to change their behaviour because of future health assessments, and 76% and 74% of participants in the SWAL-only and SWAL plus desk groups agreed or strongly agreed that knowing that they would receive follow-up health assessments had motivated them to change their lifestyle (see Appendix 12). This agreement also remained high (66% and 62%, respectively) at 12-month follow-up. A similar trend was seen when participants in intervention groups were asked whether or not knowing they would receive follow-up health assessments had motivated them to change their sitting behaviour, with 72% and 65% of participants agreeing or strongly agreeing within both intervention arms at 3 and 12 months, respectively.
Many intervention participants agreed that the measurements were motivating, although some more strongly than other participants. Some participants described a continued ‘back of the mind’ awareness of the upcoming tests as a continuous influence:
Well, you know in three months you’ll be checked again, so it was there in the back of your mind that you knew you’d have to do something if you wanted to see any effect.
FG4; SWAL plus desk; P2
Some participants talked more in terms of a driving focus:
That encouraged me to... That’s why I said initially I was standing up when all the prompts came and that. I feel like, right I know the next one is due in three/four months. Let’s see what real, what the reality is in terms of standing. Does it make a difference? So that did encourage me, yes. The baseline.
FG6; SWAL plus desk; P2
Yes, and me too, it was an incentive to try and get better scores. I appreciated there were issues around weight and cholesterol, so you know, I had to get those better.
FG6; SWAL plus desk; P1
For some groups, health assessments featured in discussions around the time of measurements:
I really looked forward to getting the results, so there was quite a lot of comparing going on in our office. All of us, I don’t know if you were the same on your side, but on our side, barring one we all came straight back out with them and ‘what did I get last time? What did I get last time?’ There was a bit of ‘have I improved on anything?’.
FG20; SWAL plus desk; P4
Many participants talked of disappointment when test results did not show a marked improvement, despite behaviour changes, and a few participants described this as demotivating:
Was what I found de-motivated me because I’m like, I’m working my socks off here. And I’ve come in here and you’re taking measurements and telling me I’m worse than I was before. So, what’s the [offensive word] point? I may as well just go back to what I was doing.
FG9; SWAL only
As noted earlier, measurements were an incentive to participate and remain in the study, and most participants appreciated them, regardless of whether or not they were happy with the results.
Did the measurements prompt general practitioner visits?
Several participants mentioned the results being less ‘healthy’ than they would hope, and most used this as motivation for engaging with the intervention components. For a small number of participants, the results had prompted them to book an appointment with their GP:
I think for me they did because I was borderline to high blood pressure, so I actually did go and visit my doctor and have that looked into for that. So, it was good to get an awareness of that from the study and then go and check if there was something that they wanted to take more action on.
FG19; control; P2
One workplace champion suggested improving the explanation and feedback given to participants about their results, emphasising the importance of seeking further advice about any test results that raised their concern.
Did participants experience any injuries/discomfort that may have been a result of a change in behaviour as a result of the intervention?
One participant reported that their back pain was exacerbated when using the height-adjustable workstation, despite seeing a chiropractor long term every month prior to the start of the study and being advised to try and change posture regularly. Similarly, a participant from different council reported experiencing pain in their back on using the workstation. The research team attended their office to assess their posture and an alternative workstation (i.e. Deskrite 100) was provided.
In the focus groups, some participants reported having experienced footache, backache or unspecified ‘achiness’, which they attributed to workstation use. However, in many cases, participants described having rectified this themselves, for example by changing footwear, making adjustments to their posture or adjusting the time spent standing accordingly:
I’m a bit asymmetrical because of arthritis and bunions and stuff, so I’ve bought some jelly in-soles, you know, just to even out my posture... I broke my left leg and left shoulder on separate snowboarding incidents. So, my left ankle has rotated forward a little. So, I was putting a bit more pressure on the heel on that side. The gel in-sole has made me, pushed me onto the balls of my feet a little bit more, taken the impact out. And since then, it’s been fine. But yes, but that only really happened after, as the time I was standing increased. Because I can stand for 4 hours and it’s not an issue, but I was standing for 6. That’s when it might start to nag a bit. You know? So, if people are standing 50% of the day, maybe they’re not hitting that issue, but yes, there are little injuries like that were starting to niggle. But then you adopt your posture around them, so you know, make small changes.
FG7; SWAL plus desk; P2
A few participants talked about difficulties of workstation use due to their height, being either taller or shorter than average and the standing desk height not being suitable, and some participants struggled with the strength required to move a desk between the up and down settings. For some participants, this affected workstation use, whereas other participants arranged a swap to a different type of workstation or sought assistance in adjusting it:
I changed mine. As soon as you told me that’s difficult to lift... And I’m actually glad, because I do think it’s a bit lighter. And [name]’s great because he’s adjusted the tensions on mine so it’s a bit lighter. Because when you’re quite small, and you know, it is hard and I’ve got two screens.
FG6; SWAL plus desk; P5
Did intervention participants change an existing activity-related behaviour for another as a result of participating in the study?
Sitting time was largely replaced by standing time, with little or no changes to stepping time. For example, from our results, it did not appear that participants in the SWAL plus desk group switched stepping for standing. No compensation effects were observed for sitting time during work hours to sitting time outside work hours, as participants reduced sitting time at work, but no opposite effect of an increase in siting time outside work was observed. Changes in daily behaviour were driven by changes during work hours on workdays.
Chapter 5 Cost-effectiveness analysis
Methodology
Overview
The aim of this economic analysis was to assess the cost-effectiveness of the SWAL intervention, with and without a height-adjustable workstation, compared with services as usual, using evidence from the SWAL RCT. Health outcomes were measured in QALYs, and other measures, including productivity, psychological health, satisfaction, work engagement and absenteeism, were considered. The National Institute for Health and Care Excellence (NICE) defines a QALY as ‘A measure of the state of health of a person or group in which the benefits, in terms of length of life, are adjusted to reflect the quality of life. One quality-adjusted life year (QALY) is equal to 1 year of life in perfect health’ (© NICE 2021 Glossary. Available from www.nice.org.uk/glossary. All rights reserved. Subject to Notice of rights NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication). 98 Costs were measured in GBP (2019–20) from a public sector perspective. Costs and QALYs were discounted at 3.5% per annum in line with UK guidelines. 94 ICERs are presented for secondary outcomes. Cost-effectiveness results using QALYs are presented as ICERs, INHBs and INMBs based on cost-effectiveness thresholds of £15,000, £20,000 and £30,000 per QALY. 99 Cost-effectiveness was considered from a public perspective, both over the trial period and over the lifetime of individuals. The cost-effectiveness from an employer’s perspective was also considered.
Within-trial costs and QALYs were estimated using econometric modelling to control for participant co-variables. Missing cost and QALY data were imputed using a multilevel approach. 100 These results were extrapolated over a lifetime horizon using a decision-analytic model to account for mortality benefits from reductions in sitting time. For the within-trial and lifetime results, probabilistic sensitivity analysis was used to reflect the uncertainty in input parameters and regression coefficients. Uncertainty surrounding base-case findings was explored using alternative assumptions through scenario, sensitivity and threshold analyses. Full details of the economic analysis are available in the health economic analysis plan (see Appendix 13).
Resource use and costs
Data on participant health-related resource use were collected using a service use questionnaire that recorded resource use within the 3 months prior to baseline and at 3- and 12-month follow-up. Participants’ resource use data between 3 and 9 months post baseline were taken as a linear interpolation between follow-up values (i.e. 3 month and 12 month). A micro-costing framework calculated the overall health-related costs for each trial participant by summating the number of resources consumed during the period multiplied by their respective unit costs. Health care unit costs in primary, secondary and community-led care were sourced from NHS reference costs and Personal Social Service Research Unit costs, and were measured in GBP 2019–20 (see Appendix 14). 101,102
Costs relating to the provision of each SWAL programme comprised (1) direct costs of providing training for workplace champions and general staff, (2) indirect staff time costs for receiving training; (3) managers correspondence time and office motivational materials and (4) the procurement and instillation of height-adjustable workstations (SWAL plus desk group only). The average programme costs per office worker were calculated on an ITT basis. It was assumed that SWAL programme costs would be incurred up-front (i.e. not annuitised) and that both SWAL interventions had no additional costs beyond the trial period. No programme-related costs were assumed in the control group.
Outcomes
The primary outcome used in the cost-effectiveness analysis was QALYs, which is a generic measure of health that combines longevity and morbidity (with 1 QALY equal to 1 year in perfect health). 99 The HRQoL weights for participants were collected using the EQ-5D-5L questionnaire at baseline and at 3- and 12-month follow-up. HRQoL refers to ‘a combination of a person’s physical, mental and social well-being; not merely the absence of disease’ (© NICE 2021 Glossary. Available from www.nice.org.uk/glossary. All rights reserved. Subject to Notice of rights NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication). 98 The EQ-5D-5L is a descriptive HRQoL instrument that requires individuals to rate their health in accordance to five levels of severity across five health dimensions (i.e. mobility, self-care, usual activity, pain/discomfort and anxiety/depression). 103 In line with NICE guidelines, base-case HRQoL weights were calculated from a published mapping of EQ-5D-5L responses onto HRQoL values calculated for the EuroQol-5 Dimensions, three-level version (EQ-5D-3L) instrument. 94,104 HRQoL weights using the EQ-5D-5L value set were considered as a scenario. Within-trial QALYs were estimated using an area under the curve approach using linear interpolation between time points. QALYs beyond the trial were calculated by the decision-analytic model (see Long-term cost-effectiveness model), which assumed that HRQoL beyond the trial was equal between arms and was equivalent to general population norms. 105
Secondary outcomes (see Chapter 2) were participants’ psychological well-being, work-related measures (e.g. performance, satisfaction, engagement) and absenteeism. Differences in the changes in outcomes between baseline and 12 months were compared with incremental costs for each intervention to inform secondary cost-effectiveness analyses.
Analysis
The cost-effectiveness of the SWAL plus desk, SWAL-only and the services as usual (control) groups was investigated according to the differences in estimated QALYs gained and costs incurred over the 12-month trial time horizon (i.e. within trial) and over the cohort’s lifespan (i.e. lifetime horizon). Differences in QALYs were compared with differences in costs measured from the public sector perspective and were presented as ICERs, INHBs and INMBs. 106 NICE defines ICERs as ‘the difference in the change in mean costs in the population of interest divided by the difference in the change in mean outcomes in the population of interest’ (© NICE 2021 Glossary. Available from www.nice.org.uk/glossary. All rights reserved. Subject to Notice of rights NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication). 98 ICERs represented the cost per additional QALY of a strategy compared with the next best alternative. INHB captures the health gain from a strategy compared with a comparator (i.e. service as usual) less the health that would have otherwise been generated elsewhere had the additional resources (again compared with service as usual) been allocated for alternative purposes (with this estimated based on a cost-effectiveness threshold). INMB captures the monetary value of the additional health generated. Three measures of health opportunity cost (cost-effectiveness threshold) were used: £15,000 per QALY, based on recent empirical estimates and the Department for Health and social Care’s chosen threshold,107,108 and at the £20,000 and £30,000 per QALY range used by NICE. 94 ICERs below the threshold are deemed cost-effective when compared with the next best relevant comparator. The INHB and INMB for the SWAL interventions were calculated and compared with service as usual. Positive values indicated cost-effectiveness compared with service as usual, with the highest positive value of the interventions compared indicating the most cost-effective intervention overall.
Within-trial analysis
Within-trial costs and QALYs were obtained from an adjusted analysis that used generalised linear regression models to estimate results according to treatment arm, while controlling for a set of relevant participant co-variables. All regression analyses controlled for age, gender, ethnicity (white, other), BMI, site area (Leicester, Salford, Liverpool) and cluster size (small, large). To account for differences in baseline HRQoL (see Report Supplementary Material 1), QALY regression analyses also controlled for baseline EuroQol-5 dimensions scores. 109 To account for the positive and right-skewed nature of the cost data, costing regressions used a log-link transformation and gamma family form. Linear ordinary least square regressions were applied for all QALY regression analyses. Linear multilevel regression models were considered in scenario analyses.
Missing data
To account for the hierarchical nature of the data (i.e. participants nested within sites), missing cost and QALYs were imputed using a multilevel multiple imputation approach. The imputation model controlled for all the covariates considered in the within-trial regression models and incorporated clusters as random effects (to account for heterogeneity between sites). The imputation was conducted using REALCOM-IMPUTE software and followed Carpenter et al. ’s. 164 recommended estimation settings for fitting multivariate response models to two-level data. Imputed costs were bounded to positive values and within-trial QALYs were bounded below 1.
Long-term cost-effectiveness model
The extrapolation of results beyond the trial was conducted using a two-state Markov model, where the cohort starts in an alive state and can either remain in that state or die and transition into an absorbing death state (see Appendix 15). Individuals in the alive state are assumed to incur no additional costs, regardless of treatment allocation, and experience HRQoL in line with age-adjusted English population norms. 105 Transitions to the death state in the control arm were directly informed by age- and sex-adjusted English general population mortality rates. 110 Transition probabilities for the SWAL-only and SWAL plus desk interventions were adjusted based on the change in their sedentary behaviour, according to the hazard ratios reported in Ekelund et al. ’s14 meta-analysis of the dose–response relationship between accelerometer-measured sedentary behaviour and all-cause mortality (see Appendix 16). An alternative scenario considered estimates from Patterson et al. ’s. 13 broader meta-analysis, which considered non-objective measures of sedentary behaviour on all-cause mortality. All-cause mortality hazard ratios, relative risks and their associated 95% CIs reported in the literature were interpolated using polynomial functions (see Appendix 16). Sedentary behaviour in the control arm was estimated using baseline values across arms and remained constant over time, In addition, SWAL-related differential sedentary behaviour time (see Table 4) would be reduced exponentially at a 50% decay rate per annum. Scenario analysis explored alternatively exponential decay rates and a linear decay rate of 20% per annum. 111 Treatment effects with respect to reductions in sitting time and associated mortality risk reductions were applied as common effects (i.e. irrespective of participant characteristics). An annual discount rate of 3.5% was applied to both costs and QALYs in accordance with NICE guidance. 112 An annual discount rate of 1.5% was applied as a scenario. 113 Please see Appendix 17 for a full list of parameters and assumptions applied in the long-term cost-effectiveness model.
Uncertainty
Overall decision uncertainty was estimated based on uncertainty in model inputs and regression estimates using Monte Carlo simulation, assuming normality around baseline participant sitting times and treatment effects (both the reduction in sitting time and associated all-cause mortality hazard ratios) and multivariate normality of regression coefficients (for within-trial costs and outcomes). 114 Levels of uncertainty were reported by 95% credible intervals around mean values (for costs, QALYs and INHB) and the probability of each comparator being the most costly, clinically effective and cost-effective. The probability of being cost-effective is presented for the three measures of health opportunity cost (i.e. the health that would have been generated elsewhere using the same resources) considered in this analysis (i.e. £15,000, £20,000 and £30,000 per QALY).
Key uncertainties explored as scenario analyses included the inclusion of participants’ expected lifetime costs,115 alternative exponential decay rates in treatment efficacy (i.e. 70%, 60%, 40%, 30%, 20%, 10% and 0%), different age (i.e. 30, 40, 50, 60 and 70 years) and gender (male and female) profiles, and a scenario that removes all estimated within-trial differences in costs and QALYs between arms. Deterministic univariate and bivariate sensitivity analyses were conducted to test how changes in the age, treatment decay rates and minute reductions in sitting times (i.e. treatment effect) affected the INMB of each SWAL intervention arm compared with the control. Threshold analyses sought to identify the specific age, decay rate, treatment effects (in minute reductions in sitting time) and incremental costs at which SWAL interventions are cost-effective for the range of threshold values considered.
Results
Health-care resource use questionnaires were completed by approximately 83.5% of participants at baseline, 67.3% of participants at 3-month follow-up and 61.8% of participants at 12-month follow-up. EQ-5D-5L data (and associated QALY estimates) were complete for 93.0%, 74.7% and 69.0% of trial participants at baseline and 3- and 12-month follow-up, respectively. Secondary job satisfaction/performance, work engagement and absenteeism outcomes had a comparable degree of missingness to the EQ-5D-5L (< 35%). Participant details are reported in Table 4.
At 12-month follow-up, individuals extrapolated after the first year were modelled with an average of 605, 583 and 542 minutes of sitting time spent per day in the control, SWAL-only (22.2 minutes difference) and SWAL plus desk (63.7 minutes difference) arms, respectively (see Table 5).
Resource use and costs
Intervention-level costs
Table 29 presents the total costs and the average per ITT participant costs of delivering the constituent elements provided by each intervention under investigation. The total costs of delivering the SWAL plus desk and SWAL-only interventions were £54,796 and £20,067, respectively, with average cost per ITT individual of £228.31 and £80.59, respectively. The SWAL plus desk intervention had broadly comparable non-desk-related costs as the SWAL-only intervention.
| Intervention | Cost (£) | Cost (£) per ITT individual |
|---|---|---|
| SWAL plus desk (n = 240) | ||
| Direct costs of providing workplace champion traininga | 1776.00 | 7.40 |
| Participant time to engage with components costsb | 13,076.91 | 54.49 |
| Workplace champions’ training time costs | 1419.84 | 5.92 |
| Workplace champions’ facilitation time costs | 3590.40 | 14.96 |
| Correspondence to managers | 145.19 | 0.60 |
| Desk purchases | 34,041.79 | 141.84 |
| Desk set-up labour costs | 720.00 | 3.00 |
| Motivational materials | 25.00 | 0.10 |
| Total | 54,795.13 | 228.31 |
| SWAL only (n = 249) | ||
| Direct costs of providing workplace champion training traininga | 1776.00 | 7.13 |
| Participant time to engage with components costsb | 12,377.61 | 49.71 |
| Workplace champions training time costs | 1321.92 | 5.31 |
| Workplace champions’ facilitation time costs | 4412.93 | 17.72 |
| Correspondence to managers | 151.03 | 0.61 |
| Motivational materials | 27 | 0.11 |
| Total | 20,066.49 | 80.59 |
Health-care resource use and non-intervention costs
Health-care resource use and associated costs were broadly balanced between the trial arms, with observed differences small in magnitude and inconsistent in direction of effect (i.e. interventions associated with more and less costs within and between health service categories, e.g. primary care, secondary care and mental health services) (see Report Supplementary Material 1–10). Overall, complete-case health-care costs were lowest for the SWAL plus desk intervention (£417.07) [vs. SWAL-only (£573.21) and control (£497.63)]. The SWAL plus desk intervention observed moderate cost savings in counsellor/therapy, general practice visits and NHS walk-in centre and urgent care centre visits, while concurrently associated with the highest mental health nurse- and outpatient hospital-related costs. When imputing missing values and controlling for participant covariates, non-intervention costs were found to be highest in the control arm, followed by the SWAL-only and SWAL plus desk arms. Report Supplementary Material 1 and 2 provide a complete-case analysis breakdown of resource use and costs by trial arm and resource category, respectively. Supplementary Material 3–10 report all estimated resource use and costings by follow-up period.
Outcomes
Outcomes in the SWAL plus desk and SWAL-only arms were similar to outcomes reported in the control arm. Complete-case EQ-5D-5L and mapped EQ-5D-3L scores rose between baseline and 3 months, and then declined below baseline values at final follow-up in each intervention arm (see Appendix 18). Lower HRQoL scores were observed, with the EQ-5D-3L reflecting differences between the EQ-5D-3L and EQ-5D-5L value sets. When imputing missing values, QALYs were broadly similar across arms for both the EQ-5D-5L and mapped EQ-5D-3L. Measures of job satisfaction, job performance and measures of work engagement collected at 3 and 12 months largely varied around baseline values observed in each treatment arm (see Table 13). The number of sick days reported by staff and employers were broadly similar across arms, albeit with changes from baseline values more favourable for the control group (i.e. reduction in sick days) relative to the SWAL-only and SWAL plus desk groups.
Effects on psychological well-being, absenteeism and work satisfaction, performance and engagement have been reported previously in Tables 12 and 13. Specific difference in differences of note between the SWAL plus desk and SWAL-only arms at baseline and 12 months, compared with the control arm, included 0.68 (1.43) and 0.56 (1.37) reductions in stress (and increases in well-being) (see Table 12), and an additional 0.80 (1.21) and 1.29 (2.50) self-reported (work recorded) days of leave [all Mean [SD)], respectively (see Table 13).
Cost-effectiveness analysis
Table 30 reports the adjusted within-trial and lifetime horizon base-case mean cost, QALY and cost-effectiveness estimates for each arm.
| Analysis | Cost (£) (95% CI) [probability (most costly)] | QALY (95% CI) [probability (most effective)] | ICER (£) | INHB (95% CI) (probability of being cost-effective) | ||
|---|---|---|---|---|---|---|
| £15,000 | £20,000 | £30,000 | ||||
| Within trial | ||||||
| Control | 642.06 (505.47 to 798.4) (0.085) | 0.84243 (0.82221 to 0.8642) (0.272) | (0.398) | (0.373) | (0.337) | |
| SWAL only | 691.19 (563.3 to 846.93) (0.216) | 0.84649 (0.8265 to 0.86585) (0.442) | 12,090.73 | 0.001 (–0.024 to 0.025) (0.423) | 0.002 (–0.022 to 0.025) (0.432) | 0.002 (–0.021 to 0.025) (0.435) |
| SWAL plus desk | 747.60 (641.42 to 871.14) (0.699) | 0.84187 (0.82246 to 0.86006) (0.286) | Dominated | –0.008 (–0.04 to 0.023) (0.179) | –0.007 (–0.038 to 0.024) (0.195) | –0.007 (–0.036 to 0.024) (0.228) |
| Lifetime horizon | ||||||
| Control | 642.06 (507.14 to 798.4) (0.085) | 17.79359 (17.77337 to 17.81535) (0.08) | (0.164) | (0.139) | (0.109) | |
| SWAL only | 691.19 (563.3 to 846.93) (0.216) | 17.80344 (17.78297 to 17.82346) (0.336) | 4984.86 | 0.007 (–0.019 to 0.032) (0.388) | 0.007 (–0.017 to 0.032) (0.376) | 0.008 (–0.015 to 0.032) (0.364) |
| SWAL plus desk | 747.60 (641.42 to 868.39) (0.699) | 17.80766 (17.78785 to 17.82522) (0.584) | 13,377.90 | 0.007 (–0.024 to 0.041) (0.448) | 0.009 (–0.023 to 0.042) (0.485) | 0.011 (–0.021 to 0.043) (0.527) |
For the within-trial analysis, the SWAL plus desk intervention was found to be the most costly and least effective, resulting in the SWAL plus desk intervention being dominated by the other arms over the trial period. The SWAL-only intervention was more costly and more effective than the control, resulting in an ICER of £12,091 per QALY. The SWAL-only intervention was cost-effective at the three cost-effectiveness thresholds considered. The SWAL-only intervention had INHBs, compared with control, of between 0.0011 and 0.0025, and a 42.3%, 43.2% and 43.5% probability of being cost-effective at the £15,000, £20,000 and £30,000 cost-effectiveness thresholds (per QALY), respectively.
In contrast, over a lifetime horizon, the SWAL plus desk intervention was found to be the most costly and most effective alternative, as a result of mortality benefits from reduced sitting time. The control was the least costly and least effective and the SWAL-only intervention had the second highest costs and effects. The ICER of the SWAL-only intervention compared with control was £4985 per QALY, and the ICER of the SWAL plus desk intervention compared with the SWAL-only intervention was £13,378 per QALY. The SWAL plus desk intervention was, therefore, cost-effective at the three thresholds considered. The SWAL plus desk intervention had a 44.8%, 48.5% and 52.7% probability of being the most cost-effective alternative at the £15,000, £20,000 and £30,000 cost-effectiveness thresholds (per QALY), respectively.
Table 30 reports the probability of each arm being the most costly and most effective. The 95% credible intervals for within-trial and lifetime costs and QALYs had considerable overlap between the three arms, suggesting a significant level of uncertainty in the incremental costs, outcomes and overall cost-effectiveness that SWAL, with or without a desk, may be expected to deliver. Report Supplementary Material 1–16 present each regression analysis used to inform the cost-effectiveness analysis, and Appendices 19 and 20 display the model inputs assigned to each treatment arm over the extrapolation period.
Scenario analyses
The mean cost and QALY estimates, and associated ICERs, for a series of scenario analyses can be seen in Report Supplementary Material 17. Report Supplementary Material 18–40 present a detailed assessment for each scenario, such as that presented for the base-case analysis (see Table 30).
Including lifetime costs results in higher costs in all arms, with the overall impact dependent on survival, and the SWAL plus desk intervention had the largest increase. For the SWAL-only intervention compared with control, the higher costs raised the ICER to £6706 per QALY. For the SWAL plus desk intervention compared with SWAL-only intervention, the higher costs raised the ICER to £18,956. The SWAL-only intervention was cost-effective at the lowest threshold of £15,000 per QALY, whereas the SWAL plus desk intervention was cost-effective at the higher thresholds.
Imposing a linear relationship on decay in the treatment effect in sedentary behaviour of the SWAL-only and SWAL plus desk interventions (i.e. 5 years of effect and 20% decline per annum) resulted in the SWAL arms having higher QALYs than the base case. The SWAL plus desk intervention remained cost-effective at all thresholds considered, with an ICER of £7674 per QALY compared with the SWAL-only intervention.
Alternative rates of efficacy decay (i.e. base case and 50% per annum) altered the survival benefits of the SWAL-only and SWAL plus desk arms. At higher rates of decay (i.e. 60% and 70%), the ICERs for both SWAL arms increased. The SWAL plus desk intervention was not cost-effective at a threshold of £20,000 per QALY and £30,000 per QALY at 60% and 70% decay rates, respectively. At lower rates of decay (i.e. ≤ 40%), the ICERs for both SWAL arms decreased, with the SWAL plus desk intervention being cost-effective at the thresholds considered. At very low rates of decay (i.e. 0% and 10%), the SWAL-only intervention was extendedly dominated (i.e. the SWAL-only intervention was dominated by the combination of the other two alternatives).
Using an alternative estimate of the impact of sedentary behaviour on all-cause mortality, based on non-objectively-measured sedentary behaviour,116 resulted in the SWAL plus desk intervention being dominated by the SWAL-only intervention. The SWAL-only intervention was also less effective and its ICER increased to £10,342 per QALY compared with control; however, the SWAL-only intervention was still the cost-effective option at the cost-effectiveness thresholds considered.
The application of multilevel regression analysis had a marked impact on within-trial cost-effectiveness results and affected the cost-effectiveness results markedly. For within-trial cost-effectiveness, the SWAL plus desk intervention remained dominated. The SWAL-only intervention had an ICER of £26,345 relative to control, suggesting that the SWAL-only intervention was cost-effective at only the highest cost-effectiveness threshold considered. Over a lifetime horizon, the SWAL-only intervention had an ICER of £8909 (relative to control) and the SWAL plus desk intervention had an ICER of £16,763 (relative to the SWAL-only intervention).
Using EQ-5D-5L preference weights to calculate within-trial QALYs resulted in higher QALY estimates in all arms. For the within-trial period, the use of EQ-5D-5L preference weights had minimal impact on cost-effectiveness results; however, for the lifetime horizon, the combined within-trial improvement in effectiveness of the SWAL plus desk intervention and the mortality benefits from reduced sitting time resulted in a lower ICER of £8164 per QALY.
Removing the within-trial differences in health-care costs and outcomes between trial arms (but incorporating intervention costs) resulted in the SWAL-only and SWAL plus desk interventions being less cost-effective than in the base case, and with higher ICERs. At a threshold of £15,000 per QALY, the SWAL-only intervention was the most cost-effective arm (with an ICER of £13,914), whereas at thresholds of £20,000 and £30,000 the SWAL plus desk intervention was the most cost-effective (with an ICER of £18,382).
Discounting at a rate of 1.5% per annum increased the lifetime discounted QALYs for all arms, and increased the estimated QALY differences between the arms. As a result, the SWAL plus desk intervention had a more favourable ICER of £6455, compared with the SWAL-only intervention, and was cost-effective at all cost-effectiveness thresholds (per QALY) considered.
The age at which an office worker receives an intervention affects the cost and QALY estimates for each alternative. Increased age is associated with higher mortality rates and, therefore, given a reduction in sitting time and associated relative risk of mortality, a greater absolute decrease in mortality. Therefore, reductions in sitting time are more beneficial for higher age groups. At lower ages, the SWAL interventions appear as less cost-effective; however, at higher ages, the SWAL interventions are more cost-effective.
Given that differential treatment effects were not considered in this analysis, gender did not have a marked affect on cost-effectiveness results.
Sensitivity and threshold analyses
The expected QALY gain and cost-effectiveness of the SWAL plus desk and SWAL-only interventions was highly sensitive to both the rate of decay in the treatment effect on sedentary behaviour over the extrapolation period (see Appendix 21) and the age at which office workers receive the SWAL intervention (see Appendix 22). The INMB for each SWAL intervention increased with reductions in the decay rate, ceteris paribus. The INMB of the SWAL plus desk intervention, compared with the control, SD in brackets, was equal to –£3 (£99) at a 90% decay rate, £0 at 88.4% and £110 (£325) at base case 50% decay, growing to £1293 (£2690) at a 10% decay rate and £6921 (£13,947) for 0% (i.e. a permanent lifetime reduction in sedentary behaviour) at a cost-effectiveness threshold of £15,000 (£30,000) per QALY (see Report Supplementary Material 41–44). The INMB for the SWAL plus desk intervention, compared with the control, was positive for all efficacy decay values examined (0–90%) at the upper £30,000 cost-effectiveness threshold, and exceeded that for the SWAL-only intervention at efficacy decay rates below 49.8% (61.0%) with a £15,000 (£30,000) cost-effectiveness threshold. The INMB for the SWAL plus desk intervention also increased with respect to increases in age at provision, ceteris paribus, with an INMB of –£12 (£62), £58 (£214), £202 (£514), £462 (£1046) and £855 (£1842) for ages 30, 40, 50, 60 and 70 years at a cost-effectiveness threshold of £15,000 (£30,000), respectively. Compared with the control, the INMB for the SWAL plus desk intervention was positive across all ages investigated (i.e. 23–80 years) at the upper £30,000 cost-effectiveness threshold and exceeded that for the SWAL-only intervention at ages ≥ 44 years (40 years) using a £15,000 (£30,000) cost-effectiveness threshold. Figure 9 presents the combined efficacy decay rates and age ranges in which ICER’s for the SWAL plus desk intervention compared with the SWAL-only intervention fall within the bounds of < £15,000, £15,000–20,000, £20,000–30,000 and >£30,000 (the remainder of other categories). The ICER values from the two-way sensitivity analysis can be found separately in Report Supplementary Material 45. ICERs above the £30,000 cost-effectiveness threshold were predominantly found to occur in younger cohorts (aged < 55 years) with moderate to high efficacy decay rates (>30%). All deterministic ICERs were below £15,000 per QALY when efficacy rates were below 24% (for ages 30–70 years) or for ages >62 years at intervention.
FIGURE 9.
Age and treatment efficacy decay ranges for which the ICER of the SWAL plus desk intervention (relative to the SWAL-only intervention) is below and within the range of £15,000–30,000 per QALY.
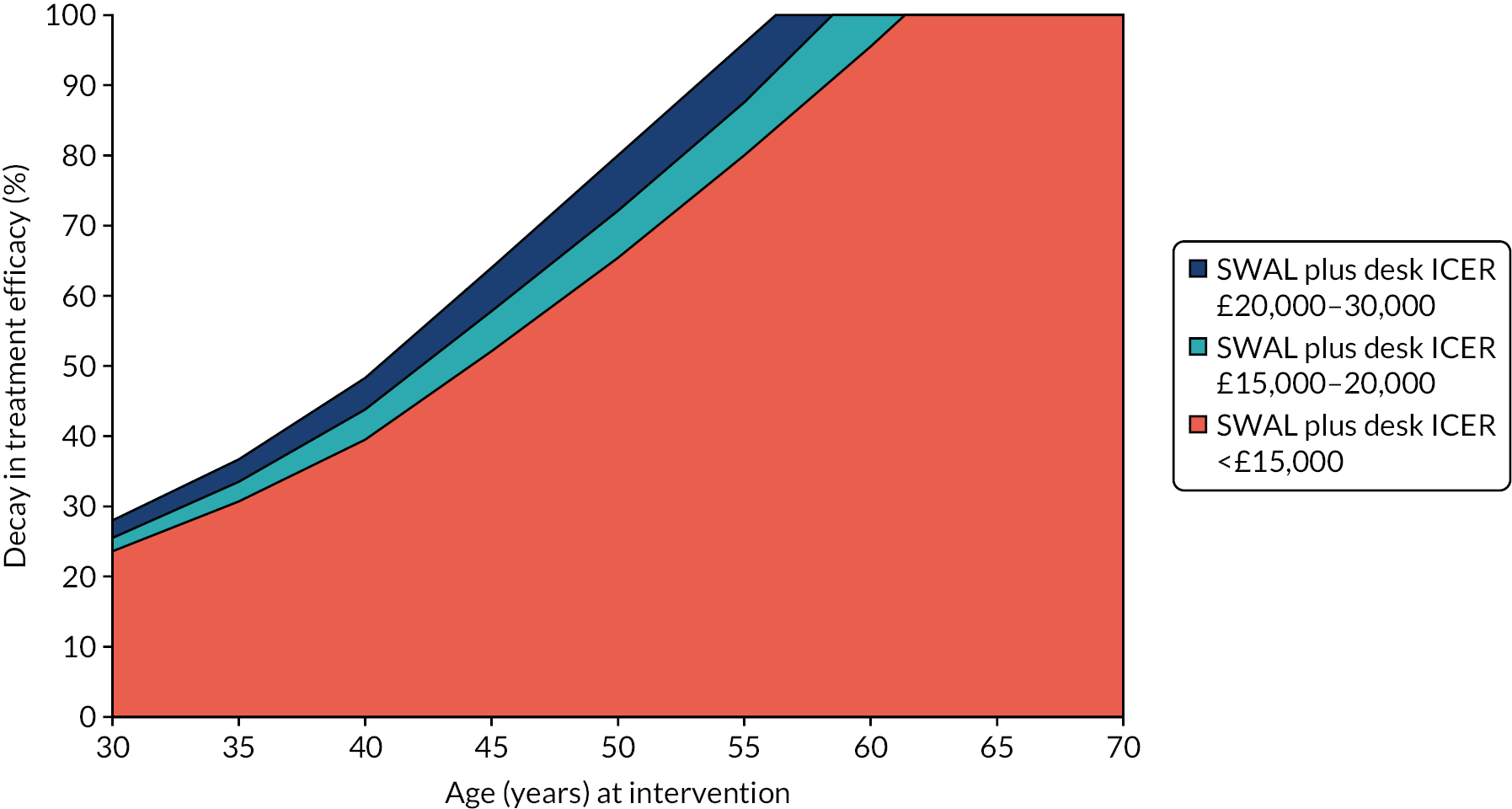
The cost-effectiveness for each SWAL arm was sensitive to intervention costs. The ICER for the SWAL-only intervention (compared with the control) remained below the thresholds of £15,000, £20,000 and £30,000 per QALY at programme costs of £191, £244 and £349 per employee, respectively. Removing estimated within-trial health-care cost differences brought the corresponding ITT participant programme cost thresholds down to £157, £210 and £315, respectively. The ICER for the SWAL plus desk intervention (compared with the SWAL-only intervention) remained below the thresholds of £15,000, £20,000 and £30,000 per QALY for incremental (desk-related) costs of £146, £165 and £202, and total programme costs of £227, £245 and £283, at base-case settings (i.e. at SWAL-only programme costs of £80.59), respectively. Removing all SWAL programme within-trial health-care cost differences brought the incremental (desk-related) costs required for the SWAL plus desk intervention to remain cost-effective down to £56, £75 and £113, and removing all within-trial cost and QALY differences gave incremental threshold values of £132, £176 and £265, at cost-effectiveness thresholds of £15,000, £20,000 and £30,000 per QALY, respectively.
The expected reduction in sitting time was the key driver of QALY gains for the SWAL plus desk intervention, as HRQoL outcomes were not improved over the trial time horizon. The INMB for the SWAL interventions increased at a positive but diminishing rate for larger reductions in sitting times (Figure 10). At a £15,000 cost-effectiveness threshold, the INMB for the SWAL plus desk intervention was positive at or above 29-minute reductions in sitting time. At a £30,000 cost-effectiveness threshold, the INMB for the SWAL plus desk intervention was positive at or above 15-minute reductions in sitting time. At a £15,000 cost-effectiveness threshold, the INMB for the SWAL plus desk intervention was positive at reductions at or above 59 minutes when removing estimated within-trial cost and QALY differences between arms. At a £30,000 cost-effectiveness threshold, the INMB for the SWAL plus desk intervention was positive at reductions at or above 24 minutes when removing estimated within-trial cost and QALY differences between arms. The SWAL-only intervention had a positive INMB across all reductions on account of modest positive within-trial gains in HRQoL; however, the INMB was positive only above 15 and 5 minutes, at £15,000 and £30,000 cost-effectiveness thresholds, when removing estimated within-trial cost and QALY differences between arms.
FIGURE 10.
The INHB of (a) the SWAL plus desk intervention; and (b) the SWAL-only intervention for alternative treatment efficacies in reductions in sitting time, relative to the control, with and without within-trial cost and HRQoL differentials (cost-effectiveness threshold = £15,000).
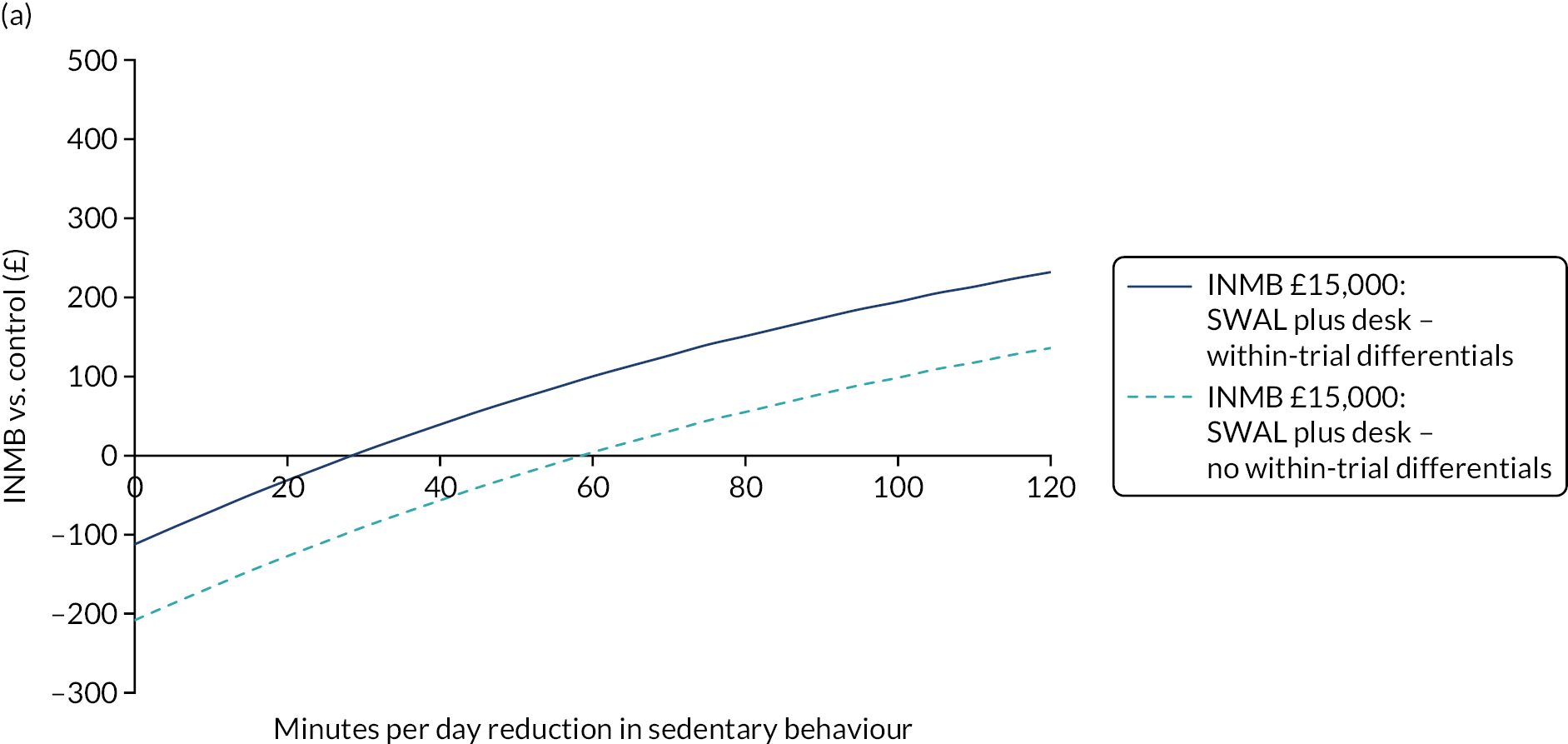
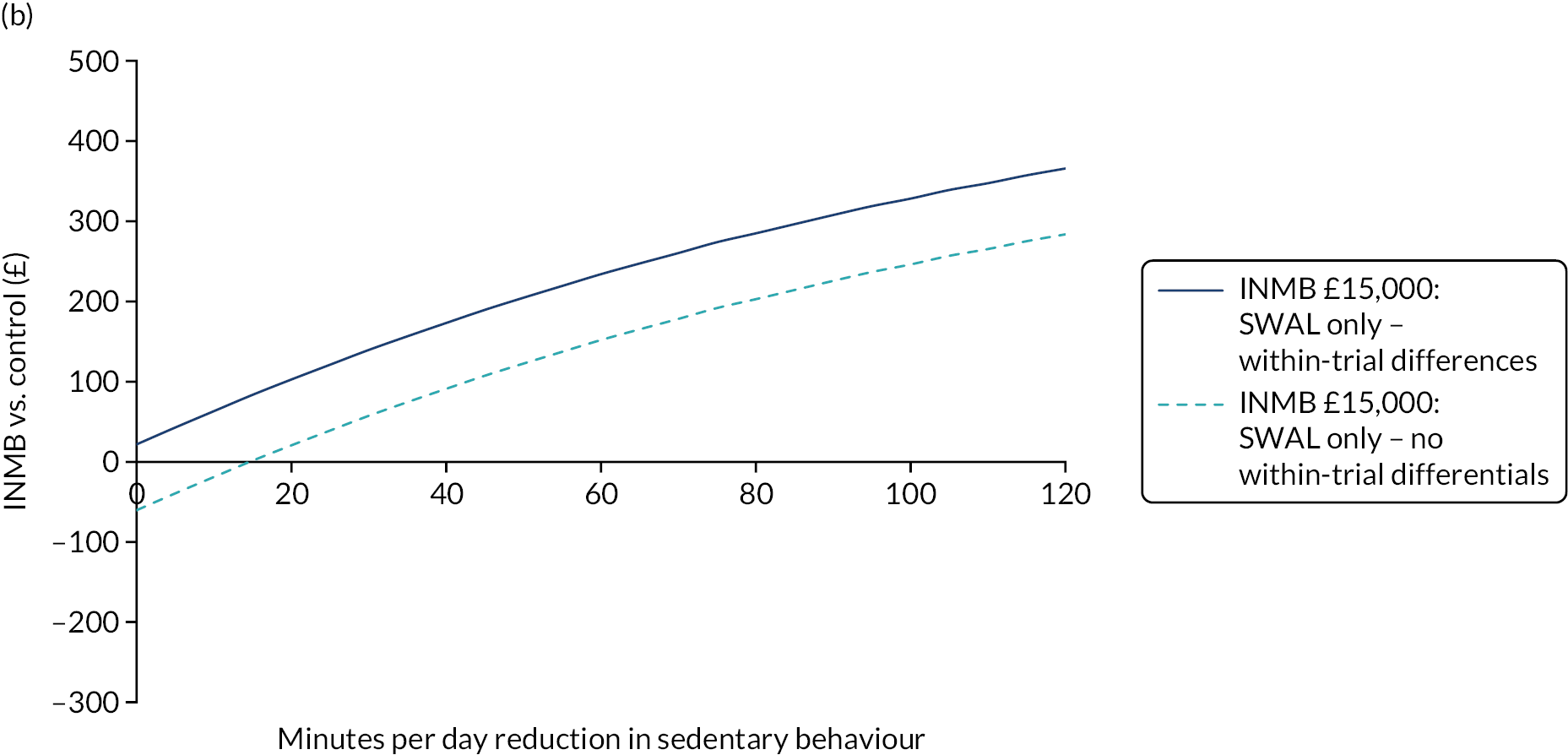
Secondary cost–consequence and cost-effectiveness analyses
The results of the secondary cost–consequence and cost-effectiveness analyses are presented in Appendix 23. The SWAL plus desk and SWAL-only interventions resulted in an average cost of £1.66 and £2.20 per adjusted minute reduction in sitting time, compared with the control, respectively. Considering only the direct costs of each intervention (i.e. no health-care cost savings) made for a £3.58 and £3.63 average cost per minute reduction in sitting time. The mean differences in physiological-related outcomes equated to a cost of £155.65 and £88.39 for a one-unit reduction in the PSS, and a cost of £73.75 and £35.78 for a one-unit reduction in the WHO-5 Wellbeing Index, of employees for the SWAL plus desk and SWAL-only interventions, respectively. Considering only the direct costs of each intervention raised the corresponding costs per unit to £336.72 and £114.98 for the PSS, and £159.55 and £58.39 the WHO-5 Wellbeing Index, respectively. Work-related measures had incremental costs of £1426.22 and £4492.02 per unit increase in engagement (UWES), and incremental costs of £1918.91 and £3509.29 per unit increase in performance, for the SWAL plus desk and SWAL-only interventions, respectively. The corresponding results considering the direct programme costs were £3085.27 and £4492.02 per unit change in engagement, and £4151.09 and £5,756.43 per unit change in performance, for the SWAL plus desk and SWAL-only interventions, respectively. Differences in work satisfaction were in favour of the control compared with the SWAL plus desk intervention. Differences between the SWAL-only intervention and control equated to an incremental cost per unit of £646.45 and £1060.39 when considering only direct intervention costs. In relation to absenteeism, SWAL programmes were dominated by the control (i.e. the SWAL programmes costed more and were associated with a larger number of days of leave than the control). Caution should be taken when interpreting the secondary cost–consequence and cost-effectiveness estimates given the small magnitude and large degrees of uncertainty surrounding the differential outcomes examined.
Chapter 6 Discussion and conclusion
Main findings of the randomised controlled trial
Primary outcome
The primary objective of this three-arm cluster RCT was to test the effect of the SWAL intervention, provided with and without a height-adjustable workstation, on daily sitting time in comparison with a control group at 12 months. The complete-case analysis found a significant difference in daily sitting time between both intervention groups and the control group, with the SWAL-only and the SWAL plus desk groups sitting for 22 and 64 less minutes per day, respectively, than the control group. The 64-minute difference between the SWAL plus desk group and the control group exceeds our minimum aim of achieving at least a 60-minute difference between groups at 12 months. The SWAL plus desk group was found to be more effective than the SWAL-only group by 42 minutes per day.
The results showed a similar pattern for the ITT, per-protocol and sensitivity analyses (i.e. effect of different activPAL days and standardising data to a 16-hour waking day), confirming the robustness of the primary analysis. Standardising data to a 16-hour waking day is one method of accounting for the variability in participants’ work hours and has been used in previous research. 117 In Australia, the Stand-Up Victoria intervention (a multicomponent intervention with the provision of a height-adjustable platform placed on top of existing workstation)117 was designed to reduce occupational sitting time in office workers. Some of Stand-Up Victoria the intervention components were delivered by the research team, whereas the SWAL components were delivered by a workplace champion. Although the Stand-Up Victoria intervention was delivered over 3 months (the height-adjustable platform was provided for the whole 12 months), the researchers evaluated its impact over a 12-month time period. When standardising the workday to a 16-hour day, the Stand-Up Victoria intervention observed a difference between groups of –36.3 minutes per day in daily sitting at 12 months, which is similar to the standardised results for the SWAL plus desk group (i.e. –38.6 minutes/day). 117
Recently, Pereira et al. 118 in a fully powered randomised trial, compared the Stand and Move at Work multicomponent intervention when provided with a height-adjustable desk (i.e. the STAND+ intervention) and without a height-adjustable desk (i.e. the MOVE+ intervention). Although most intervention strategies were the same across both intervention groups, the behaviour change messages were different. The MOVE+ group had a goal of an additional ≥ 30 minutes per workday of light-intensity physical activity, whereas the STAND+ group had a goal of increasing standing time to 50% of desk-based worktime, as well as the additional ≥ 30 minutes per workday of light-intensity physical activity. Pereira et al. 118 found that the group who received the intervention and desk (i.e. the STAND+ intervention) sat for 47.7 minutes less per 16-hour waking day than the MOVE+ group, an effect size similar to our study. However, in these previous studies, as well as in the current study, sitting reductions were replaced with changes in standing time and no or minimal changes were observed in stepping time.
The primary analysis was also conducted within a range of prespecified subgroups and the only significant interaction was for age in the SWAL plus desk group, with the intervention having a greater effect for participants aged ≥ 46 years. This finding corroborates the findings from our previous study (i.e. SMArT Work). 41 Although the data presented in this report do not provide a reason for this finding, it may be that as people age they become more concerned with their health status and are, therefore, more engaged in making a change.
Although not significant, there were some potentially meaningful differences (≥ 30 minutes/day) in how effective the intervention was by study area, although it is important to note that CIs were wide for Liverpool. For the SWAL-only groups, Liverpool clusters sat for 7.8 minutes per day more than the control group, whereas Salford (i.e. Salford City Council, Bolton Council and Trafford Council) and Leicester (i.e. Leicester City Council and Leicestershire Council) clusters sat for 11.6 and 30.2 minutes less per day, respectively, than the control group. The Leicester clusters sat for 31.5 minutes less per day than the Liverpool clusters. Similar results were seen for the SWAL plus desk group, whereby Liverpool participants sat for 23.5 minutes less per day than the control group, but Salford and Leicester participants sat for 56.7 and 72.9 minutes less per day, respectively, than the control group. The Leicester clusters sat for 43.1 minutes less per day than the Liverpool clusters. These results suggest that the intervention was more effective with Leicester-based participants than with Liverpool-based participants. These variations in the primary outcome by area may be due to the differences in the time workplace champions spent on intervention delivery, or variation between councils in the accessibility of apps to assist with monitoring sitting time. For example, fewer participants in Liverpool than in Leicester completed the online education session (69.1% vs. 85.4%). However, workplace variations may also be due to residual confounding from unmeasured characteristics between areas. 117
Secondary outcomes
One of our key activPAL-assessed secondary outcomes was occupational sitting time. The complete-case, ITT and per-protocol analyses found a significant difference between the SWAL plus desk group and control group, but there was not a significant difference for the SWAL-only group. The difference between the SWAL plus desk group and the control group was –57.9 minutes per day (complete-case analysis) in favour of the SWAL plus desk group. When occupational sitting time was standardised to an 8-hour workday, significant differences were also found for the SWAL-only group compared with the control group (–14.9 minutes/day), and the SWAL plus desk group effect size was similar to the complete-case analysis (–61.4 minutes/day). This effect size is larger than previous similar interventions at 12-month follow-up. For example, in the SMArT Work and Stand-Up Victoria interventions,41,117 the intervention group sat for 41.3 and 45.4 minutes less per standardised 8-hour workday, respectively, than the control groups.
For other key activPAL-assessed secondary outcomes, there are several points worth highlighting. First, behaviour change differences observed at 3 months were similar to those observed at 12 months, indicating that behaviour change was maintained over the longer time period, which was a focus of our intervention. Previous interventions, such as SMArT Work and Stand and Move,41,118 which included organisational, environmental and individual strategies over the full study period, also managed to maintain any behaviour changes over the longer term (i.e. 12 months). In contrast, interventions that do not include strategies, besides the height-adjustable workstation (environmental), beyond the initial intervention period see a reduction in the effect size between 3- and 12-month follow-up. 117 Therefore, when designing future interventions, researchers should take this into account. Second, our intervention messages were around reducing total time spent sitting, as well as breaking up prolonged sitting regularly, and our results indicate that participants received these messages, as we observed positive changes in both total sitting time and prolonged sitting time for both intervention groups in both the short (3 months) and long term (12 months). Third, although our intervention encouraged replacing sitting time with standing and moving more, our data showed that sitting time was largely replaced by standing time, rather than movement time, for both intervention groups (although did not reach significance in the SWAL-only group), with small but significant increases in stepping time seen in the SWAL plus desk group during work hours at 12 months. This is consistent with previous studies where sitting time was replaced mainly with standing time. 41,117,118 Although we observed differences in behaviour when examining activPAL-assessed variables on any valid day, when we examined results separately for workdays and non-workdays, behaviour change occurred on only workdays. Furthermore, effect sizes were similar during work hours and all waking hours (i.e. daily), indicating that behaviour change largely occurred during work hours and participants did not take the ‘whole-day’ preventative approach that we were promoting in our intervention. Although in the process evaluation some participants indicated strategies that they used to reduce their sitting time outside work, many participants also reported being less active at home than at work. Therefore, these results suggest that there is ‘more work to do’ to reduce sitting time within all domains across the whole day. 119
From the quantitative questionnaires and the physical measures, there was no obvious pattern for meaningful, beneficial changes for the intervention groups in physical or psychological and work-related outcomes, apart from stress, well-being, the vigour component of work engagement and pain in the lower extremity, for which small improvements were seen. The physical outcome results in terms of markers of cardiometabolic health are not surprising for several reasons. First, it is challenging to improve markers if they are already in the healthy range to begin with, and our population were, on average, in the healthy range for these markers. It is also known that cardiometabolic changes from sedentary interventions in general populations are small. 120 Second, sitting time was replaced by standing time, and experimental research in healthy adults has found no benefit of short standing breaks on physiological markers of health, such as glucose and insulin, but have for light walking (e.g. Bailey and Locke121 and Pulsford et al. 122), although recent studies in populations of overweight/obese individuals and individuals with impaired glucose regulation have. 123,124 Third, epidemiological research has indicated that larger health benefits may be achieved through substituting sitting with stepping, rather than standing. 125,126 Looking at changes in physical health in individuals with a higher BMI or glucose levels was not a prespecified objective of this study; however, this could be investigated in future analyses, providing that there are enough participants in these categories. Pereira et al. 118 recently investigated changes in physical health in their Stand and Move trial in an exploratory subgroup of 95 participants with prediabetes or diabetes, and found that the effect sizes were larger and clinically meaningful for blood glucose, triglycerides, systolic blood pressure, HbA1c, LDL cholesterol, body weight and body fat.
The small positive (beneficial) change in stress in this study is consistent with another cluster-randomised study that evaluated the effect of organisational-level strategies to reduce sitting time in a group of desk-based office workers, which found small changes in effects for stress at 12 months. 83 Across all treatment arms, SWAL participants scored, on average, in the lower end of the moderate stress category (i.e. 14–26 points). 127 Small positive changes were observed for stress in both intervention groups in comparison with the control group at both follow-ups, the average scores were still within the moderate stress category. Although it is recommended to include a measure of stress in workplace interventions for reducing sitting time at work,48 more recent large-scale RCTs have not used a valid measure of stress41,117,118 and, therefore, there is limited previous research to compare our findings with. Furthermore, a recent systematic review on associations between sedentary behaviour and indicators of stress concluded that associations are either inconsistent or null, and the evidence is limited in quality. 128 Similarly, there is limited research on sedentary behaviour and general well-being129 and, therefore, further research is needed to confirm our potential positive effect on well-being. It is possible that more meaningful changes in well-being may be seen in individuals who report poorer well-being at baseline. 130
Small effect sizes were seen for some musculoskeletal conditions,131 which is similar to our previous intervention (i.e. SMArT Work). 132 Favourable changes were seen in the pain experienced in the lower extremity in participants in the SWAL plus desk group, compared with participants in the control group, at 12 months. The small changes in the pain scale from the SNQ were similar to another intervention that aimed to reduce sitting time. 133 Previous literature is mixed on associations between sitting time and musculoskeletal conditions, with some studies reporting associations between sitting time and upper extremity symptoms, rather than lower extremity (as in the SWAL intervention),134,135 and other studies suggesting that it is jobs that are not desk-based that are more likely to be associated with low back pain. 136,137
At both 3 and 12 months, the small positive changes in the work engagement vigour subscale reported by participants in both intervention groups, in comparison with the control group, were also seen in desk-based workers from the SMArT Work randomised controlled study,41 and have been reported in studies that have looked at the effects of breaking up prolonged sitting bouts. 138,139 Weatherson et al. 140 have reasoned that interventions that reduce sitting in the workplace do not lead to negative outcomes related to work engagement and productivity. Vigour is characterised by high levels of personal energy (vitality),141 feelings of physical strength, emotional energy and cognitive liveliness. 142 At work, vigour is conceptually seen as a positive psychological response to one’s interaction with specific elements of the workplace, and high levels of vigour at work indicate optimal psychological and physical functioning. 142
For the SWAL plus desk group, positive changes were seen for organisational social norms, support from all sources and output demands, compared with the control group. At both 3 and 12 months, the SWAL plus desk group felt that their workplace, supervisors and colleagues were supportive and accepting of standing and moving more at work. Significant intervention effects for perceived organisational norms were observed at 3 months (but not significant at 12 months) in another multicomponent RCT that aimed to reduce workplace sitting. 143 The effect sizes for organisation norms from the Stand-Up Victoria study143 were similar to the changes for the SWAL plus desk intervention group at both 3 and 12 months. However, it is not clear why these findings were observed in the SWAL plus desk group and not in the SWAL-only group when the intervention they received was the same, aside from the workstation. In focus groups, participants in the SWAL-only group reported that if they moved from their desk to reduce and break up their sitting that colleagues/managers may deem this as not working and so this may be a potential explanation.
Main findings of the process evaluation
Identifying and training workplace champions within each cluster worked well. All clusters identified champions and only one cluster had a champion who was not trained. The training of workplace champions has been found to be an acceptable and effective approach for interventions to reduce workplace sitting. 144,145 The excellent feedback on the training demonstrates that this was well received. However, workplace champion retention was an issue over the 12 months, with 21% of clusters without a champion by the end of the 12-month period and this was due to workplace champions leaving their employment or withdrawing from the role because of increased workload. Managers agreed that workplace champions could to have 2 hours of protected time each month to carry out the role and champions reported, on average, spending 8.8 hours (SWAL plus desk) and 10.4 hours (SWAL only) on the intervention implementation and recording documents over the 12-month period. If SWAL was implemented outside a trial, then time would not need to be spent on the recording documents and so this would lessen the burden; however, organisations would need to ensure that workplace champions’ workload takes into consideration the time needed to implement health and well-being programmes like this one or employ alternative solutions to implementation (e.g. paying for an external partner to deliver).
Ideally, workplace champions would have delivered all intervention strategies and all participants would have engaged with all strategies; however, owing to work pressures and difficulty scheduling the group catch-up sessions, champions were unable to achieve this. Reasons for why participants did not engage in some strategies included not being aware of the strategies, not having time, IT issues or participants did not think that they would be of benefit. Of the participants who returned a process evaluation questionnaire (3 months, 85%; 12 months, 87%) and workplace champions who returned their recording documents (3 months, 92%), 79% completed or partially completed the online education. Sixty-nine per cent of clusters sent ≥ 75% of the monthly e-mails and 56% of clusters delivered both group catch-up sessions (although some had more ad hoc catch-ups). Furthermore, 54% of clusters delivered all three challenges and one-third of participants engaged in some form of self-monitoring of sitting/physical activity behaviours and prompts. For participants in the SWAL plus desk group, 100% received their height-adjustable workstation, with 80% and 53% using it every day at 3 and 12 months, respectively. Overall, there was quite large variation across clusters and participants in intervention delivery and engagement. Future research should explore ways in which to reduce the variation.
In SMArT Work, engagement with the online education session was slightly lower (79%) than engagement with the face-to-face education session (86%). 132 Feedback was similar between the interventions on increasing awareness, with 90% of SWAL participants agreeing or strongly agreeing that SWAL increased their awareness of the health consequences of sitting too much, compared with 93% of SMArT Work participants. Although the session’s ability to motivate a change was high, with ≈80% of participants agreeing or strongly agreeing that the session motivated them to make a change to the time they spent sitting, this was 15% lower than in SMArT Work. The change to make the education session online rather than face to face was taken as a result of stakeholder engagement at the start of the study. Although this change may have affected the potency of the session, the workplace champion and participant burden of having to organise and attend a face-to-face education session, as well as the increased training needed to deliver the session, is likely to have resulted in a lower engagement with the education session in this larger study.
It was clear from the other strategies (e.g. group catch-up sessions, challenges and self-monitoring) that many participants enjoyed the strategies and found them helpful towards reducing and breaking up their sitting time; however, there were also a number of participants who did not engage in the strategies or find them as useful, either because of time pressures or because they did not think that a particular strategy would work for them. Therefore, it appears that a ‘one size fits all’ approach does not work for this type of intervention, and that different strategies will work for different people. Identifying key elements that do need to be delivered and then offering a toolkit approach to additional strategies, whereby workplace champions and participants can both tailor and ‘dip in and out of’ strategies to suit them, seems appropriate. It is also worth noting that some participants in the SWAL plus desk group felt that some of the strategies (e.g. sitting less challenges) were not as applicable to them as they had the workstation to use. The workstation is only one strategy for enabling less sitting and more breaks in sitting, and it also does not promote more ambulation, which was also a focus in our intervention. Our intervention content included many options and top tips for reducing and breaking up sitting time without the use of the height-adjustable workstation, including strategies that involved more movement, but the data appears to suggest that some participants in the SWAL plus desk group did not think the strategies were needed if they had the workstation. Therefore, for future studies, we need to ensure that our messages and educational content emphasise that participants are asked to think beyond the use of the workstation when reducing and breaking up sitting time.
It was beyond the scope of the current analysis, but it would be informative to understand whether or not clusters that delivered more intervention strategies observed a larger change in behaviour, why some workplace champions managed to deliver more of the intervention than others and whether the characteristics of these champions differ, and if the participants who engaged more with the various strategies differ from participants who did not. These questions will help inform future implementation and maximise effectiveness of interventions.
Participants in both intervention groups identified many strategies that they adopted to reduce and break up their sitting time, including using toilets on a different floor; making more frequent trips to the photocopier, printer or waste bin, and using those further away; making more frequent trips to the water cooler and using a smaller bottle to trigger this; making more hot drinks or collecting one’s own hot drink instead of relying on a colleague collecting it; and, generally, using the stairs more. Many participants also reported more lunchtime activities, such as walking, running, yoga and cycling, and adapting their commute to incorporate more standing and walking. Despite the strategies being movement strategies, the activPAL data showed little or no differences in stepping time. Furthermore, although some participants reported trying to reduce sitting while at home by getting up during TV adverts or at the end of a programme, standing while engaging in screen-based activities or increasing time spent on chores, it was a challenge for many participants because of feelings of tiredness and wanting to relax. The activPAL data provided no indication that positive changes in sitting behaviour were made outside work. Although small changes were observed in the SWAL plus desk group, the changes were not enough to result in a significant difference.
Some of the qualitative results support our quantitative findings around well-being, stress and vigour. Participants reported feeling more energetic and alert, more focused and productive, felt that they were doing something positive for their health and felt more ‘psychologically positive’. In the process evaluation data, many participants were in attenuation of previous musculoskeletal issues and fewer aches and pains, and this complements the quantitative results, which showed small improvements in the pain experienced in the lower extremity. These benefits are consistent with the benefits reported from our previous intervention (i.e. SMArT Work). 132
Despite the SWAL intervention incorporating strategies to try and overcome the reported barriers from SMArT Work, participants still reported similar types of barriers to reducing and breaking up sitting, such as workload, work and time pressure, being concerned with what managers and colleagues thought about them being away from their desk or standing at their desk while others were sitting, and difficulty with standing in meetings and forgetting to get up. In addition, many participants admitted that laziness prevented them making changes to reduce their sitting time.
This was a cluster trial and participants were grouped into clusters either by a shared office space (although could be made up of different teams/departments) or if they were members of the same team but split into different office spaces. The process evaluation confirmed no evidence of contamination across the different intervention arms in the trial, demonstrating that our cluster grouping was effective.
Main findings of the cost-effectiveness analysis
Our cost-effectiveness analysis suggested that the reductions in sitting time achieved by the SWAL programme with a height-adjustable workstation translate into health gains that are cost-effective from a public payer perspective when a lifetime horizon is considered. Over the lifespan of the average worker, the SWAL plus desk intervention was expected to accrue an incremental 14.07 discounted QALYs per 1000 employees enrolled, at a public cost of £105,542, compared with control. For the SWAL-only intervention, the estimated within-trial gains in HRQoL combined with the longer-term impacts of reductions in sitting time amounted to the intervention being deemed cost-effective when compared with control over the trial period and beyond. Conclusions on cost-effectiveness were highly sensitive to a number of factors, including the modest and uncertain within-trial cost savings and HRQoL impacts, the recipients’ age at intervention, the persistence in the impact on sedentary behaviour (i.e. reduction in sitting time), the underlying risks associated with sedentary behaviour and the average cost of providing the intervention to office workers. All other methodological scenarios found both SWAL programmes to be cost-effective, compared with service as usual, at the maximum threshold recommended by NICE of £30,000 per QALY.
The strengths of this cost-effectiveness analysis include the relatively large sample size, prospective study design, accelerometer-measured changes in sitting time, the use of a validated HRQoL instrument, and the application of a robust and accelerometer-measured relationship between accelerometer-measured sitting time and all-cause mortality. Incorporating both a within-trial analysis and a long-term Markov model approach allowed the assessment of costs and outcomes to be conducted within the context of the trial and over the lifetime of participants, reflecting mortality impacts from improvements in workplace activity. However, several study limitations must also be acknowledged. First, our long-term model incorporated changes in all-cause mortality that result from changes in sitting times only, and, as such, consequences from differences in non-fatal events or HRQoL between arms was not incorporated into study findings. Second, the risk equations for all-cause mortality and the expected treatment effect (i.e. reduction in sitting time) was assumed to be generalisable across all office workers. Third, a cost-effectiveness analysis with a broader ‘societal’ perspective may have captured wider benefits of the intervention (e.g. on productivity, consumption). 111,146,147 Fourth, in the absence of any long-term evidence on the sustainability of treatment benefit, the decay rate (50%) was set to that used in other modelling studies, although the impact of this was considered as part of the scenario analysis. 148–152 Finally, the cost-effectiveness results were based on small and uncertain differences. Therefore, conclusions regarding the cost-effectiveness of the SWAL programmes must be interpreted with caution, given their contingency on uncertain within-trial cost and HRQoL differentials and the unknown sustainability of treatment effect.
A variety of factors may make SWAL interventions more cost-effective than our analysis suggests. Economies of scale, market factors (e.g. price reductions over time), modifications to the programme and specific workplace factors (e.g. shared desks) could all feasibly reduce SWAL programme costs now and in the future. Incorporating the potential cost and HRQoL impacts from non-fatal events avoided as a result of reductions in sitting time, including cardiovascular disease,3,153,154 type 2 diabetes155 and cancers,156 would likely further improve cost-effectiveness results in favour of SWAL programmes. In addition, health gains could be amplified by a more targeted approach whereby older staff, individuals with pre-existing conditions (who benefit from activity) and individuals undergoing the longest sitting times are prioritised. It should be noted, however, that future maintenance costs of equipment, training and staff work time (e.g. workplace champion support) and the potential for higher procurement costs than those observed in the trial may counteract or supersede aforementioned factors.
The conclusions of our analysis from an employer’s perspective are less clear. The trial reported largely inconsistent effects on worker performance and satisfaction, and although moderate gains in worker engagement and stress reduction were observed, there was also a rise in unplanned absences seen in SWAL arms compared with control (contradicting previous findings for similar interventions). 111,147 Therefore, whether or not SWAL programmes are a cost-effective investment from an employers’ perspective remains questionable. Employers may be interested in outcomes outside those monitored in this trial (e.g. positive work environment, job retention, company perception) and cost-sharing arrangements (e.g. subsidies) could strike a balance between sizeable public health gains and broader employer outcomes.
The results stress the importance of the persistence of impacts on sitting time and cost management, and emphasise prioritising individuals who stand to benefit the most from reductions in sitting time. Given trial evidence and recent estimates of all-cause mortality associated with sedentary behaviour, both SWAL interventions could be considered a cost-effective strategy for promoting the health of office workers in the UK.
Strengths and limitations
A major strength of this study was the implementation of the intervention through workplace champions within the target organisations, replicating a real-world delivery with no research team involvement. The evaluation of this intervention was conducted through a fully powered cluster RCT, where randomisation occurred at the office level (therefore, reducing contamination) after baseline assessments (therefore, reducing bias). The majority of previous studies evaluating sitting reduction interventions in the workplace have been pre–post and non-randomised studies. 48 Furthermore, our intervention was tested over a 12-month period, allowing for a longer-term evaluation of effectiveness, whereas previous interventions have mainly been tested over the short term, usually no more than 3 months. 48 No cluster drop out was encountered, and even although we experienced a 22% loss to follow-up of participants, which increases to 28% when considering loss to follow-up and participants who did not provide valid activPAL data for the primary outcome, our sample size was sufficiently large enough to account for this. This drop out/non-compliance rate was in line with two other 12-month evaluations of workplace interventions. 117,118
The use of an accelerometer-based device to assess the primary outcome was also a major strength. The activPAL has been shown to be nearly 100% accurate for detecting sitting behaviours and reductions in sitting. 61,157,158 Despite checking the data on return for adequate wear, requesting re-wears where necessary and offering a £10 gift voucher on the provision of complete outcome measures, compliance with wearing the activPAL still needs to be taken into account for sample size calculations. At each visit, ≈95% and ≈91% of participants seen provided at least 1 valid day and 4 valid days of activPAL data, respectively, which is similar to other workplace interventions that have aimed to reduce sitting time using the activPAL device. However, once you take into account that participants needed to have this number of valid data (valid days) at both baseline and the follow-up time point, compliance reduced again. For example, 93% of participants provided at least 1 valid activPAL day at both baseline and 12-month follow-up, but only 87% of participants provided ≥ 4 valid days at both time points. Researchers should also take this into account in their sample size calculations on top of accounting for drop out. To maximise our sample, for our main analysis we included all participants who provided at least 1 day of activPAL data. Owing to day-to-day variation, it is common practice to usually set minimum criteria of several days of valid data. 159 However, to test the robustness of our results, we performed a sensitivity analysis including only participants who provided more valid days of activPAL data, and our results remained largely unchanged to the main analysis.
We used a validated set of questionnaires commonly used to assess psychological health and important work-related outcomes, such as occupational recovery and work engagement, and this increases the robustness of the results and also allows comparison with previous research. We also collected absenteeism data directly from organisational records.
The SWAL intervention was a multicomponent intervention, and we included a detailed mixed-methods process evaluation that enabled us to understand the extent of cluster and participant engagement with each component, as well as workplace champions’ and participants’ experiences and perceptions of usefulness of each intervention component. In the qualitative component of the process evaluation, we ensured a good representation of clusters; however, we were unable to collect any qualitative data from participants at Bolton Council.
Although there were many strengths to this research, there are some limitations to be acknowledged. First, local government was the target for this intervention and study, and this may limit the generalisability of the intervention and findings to other types of organisations, although we did recruit six councils across different areas and regions of England, which adds to the representativeness of council desk-based workers. SWAL participants were similar to wider council employees in the UK in terms of age and median income, but were more likely to be female and of non-white ethnicity. Not all participants completed the process evaluation questionnaires and not all workplace champions returned the documentation that recorded how much of the intervention they had implemented and, therefore, engagement with, and feedback on, the different strategies may have been different, as we have reported on only returned responses.
Conclusions and future research
Our SWAL multicomponent intervention, provided with and without a height-adjustable workstation, was effective, with both SWAL groups sitting less than the control group in the short and longer term. However, the intervention with the height-adjustable workstation was found to be nearly three times more effective at changing sitting time than the intervention without a height-adjustable workstation. Behaviour change was maintained between 3 and 12 months, and largely occurred during work hours. Reductions in sitting were mirrored by increases in standing. From the quantitative questionnaires, there appeared to be small beneficial changes for stress, well-being, vigour and pain in the lower extremity for both intervention groups.
Our quantitative and qualitative process evaluation data showed that workplace champions and participants engaged with our intervention, but this did vary considerably across clusters and by intervention strategy. Workload and work pressure seemed to be barriers to engagement and behaviour change, as well as ‘laziness’, habits being too ingrained and organisation/work culture. Our intervention was seen in a positive light by the workplace champions and participants. Although, ideally, participants would have engaged in all intervention strategies, the SWAL intervention did enable participants to dip in and out of the strategies they deemed most useful for them, which seemed to vary across participants. A toolkit of strategies to reduce sitting seems like the best approach, rather than a one size fits all approach. As part of the process evaluation, participants in both intervention groups reported several benefits, such as feeling more energised, alert, focused and productive. Participants in the intervention plus desk group also reported improvements in musculoskeletal issues and general aches and pains.
The economic evaluation found that the SWAL-only and SWAL plus desk interventions are potentially cost-effective strategies for promoting the health of office workers in the UK. Conclusions are contingent on the persistence in sitting time reductions, participant age and intervention cost.
Based on the findings of the present study, we recommend that future research addresses the following:
-
There is a need to follow up over the longer term, such as 24 or 36 months, to investigate behaviour change maintenance. This may also be particularly important to see the impact on outcomes such as absenteeism, which may take longer to become evident.
-
The trends for better results in the Leicester area than in Liverpool highlights the need to recruit organisations in different areas of the UK, as well as in different countries, to investigate whether or not the intervention can be effective across different areas. Future research also needs to recruit different types of organisations. Where differences are found, research needs to investigate the reasons why.
-
Although our intervention encouraged replacing sitting time with standing and moving, sitting was replaced largely with standing, whereas time spent in more overt movement (e.g. stepping) remained more stable. More research is needed to determine how best we can support people to increase movement (i.e. light activity and MVPA).
-
There is a need to explore whether or not effects on physiological markers of health are evident in workers who have a poor health profile at baseline, using analysis techniques that do not assume that the relationship between the dependent and independent variables is the same at all levels.
-
Our intervention was focused on reducing sitting time both at work and outside work. However, most of the behaviour change occurred at work. More research is needed to determine how we can support people to make changes outside the work context.
-
To inform future intervention delivery, further qualitative understanding is needed on why some workplace champions managed to deliver more of the intervention than others, whether or not the characteristics of these champions differ and if the participants who engaged more with the various strategies differ from participants who did not.
The effect of COVID-19 on the ‘new normal’ for desk-based workers should be considered by prospective users of the SWAL intervention. We recommend that employees are involved in the implementation of the intervention with respect to the current working environment.
Acknowledgements
We thank all participants who took part in the study. We thank all of the project staff who are not named on this report but contributed to the study. We particularly thank Jill Clanchy (trial manager), members of the DMEC (Professor Trish Gorely, Professor Rob Copeland and Denise Howel) and members of the TSC (Professor John Buckley, Dr Daniel Bailey, Professor Charlie Foster, Dr Derrick Bennett, Paul Clark and Leesa Hellings-Lamb) for their advice and support over the course of the study.
Contributions of authors
Charlotte L Edwardson (https://orcid.org/0000-0001-6485-9330) (Associate Professor) had overall responsibility of the study as the chief investigator, led the study, led the study design and methods development, processed and cleaned the activPAL data (blinded), drafted the introduction, quantitative results and discussion chapters of the report, and obtained funds to complete the project.
Benjamin Maylor (https://orcid.org/0000-0002-4503-0479) (Research Assistant) conducted fieldwork, cleaned and processed Axivity data (blinded), analysed the quantitative process evaluation data and drafted the associated process evaluation chapter sections.
Stuart JH Biddle (https://orcid.org/0000-0002-7663-6895) (Professor) contributed to the study design and methods development, and obtained funds to complete the project.
Stacy A Clemes (https://orcid.org/0000-0001-5612-5898) (Reader) contributed to the study design and methods development, and obtained funds to complete the project.
Edward Cox (https://orcid.org/0000-0001-8981-0699) (Research Fellow) contributed to the health economic analysis plan, conducted the economic analysis and drafted the economic analysis sections of the report.
Melanie J Davies (https://orcid.org/0000-0002-9987-9371) (Professor) contributed to the study design and methods development, and obtained funds to complete the project.
David W Dunstan (https://orcid.org/0000-0003-2629-9568) (Professor) contributed to the study design and methods development, and obtained funds to complete the project.
Helen Eborall (https://orcid.org/0000-0002-6023-3661) (Lecturer) contributed to the study design and methods development, analysed the qualitative process evaluation data, drafted the associated process evaluation chapter sections and obtained funds to complete the project.
Malcolm H Granat (https://orcid.org/0000-0002-0722-2760) (Professor) acted as principal investigator for the Salford research site, contributed to the study design and methods development, and obtained funds to complete the project.
Laura J Gray (https://orcid.org/0000-0002-9284-9321) (Professor) contributed to the study design and methods development, and obtained funds to complete the project.
Michelle Hadjiconstantinou (https://orcid.org/0000-0003-2827-0988) (Research Associate) contributed to the intervention content and intervention fidelity methods.
Genevieve N Healy (https://orcid.org/0000-0001-7093-7892) (Associate Professor) contributed to the study design and methods development, and obtained funds to complete the project.
Nishal Bhupendra Jaicim (https://orcid.org/0000-0002-8584-0388) (Statistician) wrote the statistical analysis plan, cleaned and managed the data, and undertook the statistical analysis.
Sarah Lawton (https://orcid.org/0000-0001-5830-7521) (Research Assistant) conducted fieldwork and contributed to drafting the methods chapter.
Panna Mandalia (https://orcid.org/0000-0003-4445-3231) (Education and Research Facilitator) contributed to the intervention content and intervention fidelity methods, and conducted the intervention fidelity of the group catch-up sessions.
Fehmidah Munir (https://orcid.org/0000-0002-5585-0243) (Reader) contributed to the study design and methods development, and obtained funds to complete the project.
Gerry Richardson (https://orcid.org/0000-0002-2360-4566) (Professor of Health Economics) designed and oversaw the economic analysis, and obtained funds to complete the project.
Simon Walker (https://orcid.org/0000-0002-5750-3691) (Senior Research Fellow) contributed to the health economic analysis plan, conducted the economic analysis and drafted the economic analysis sections of the report.
Thomas Yates (https://orcid.org/0000-0002-5724-5178) (Professor) contributed to the study design and methods development, and obtained funds to complete the project.
Alexandra M Clarke-Cornwell (https://orcid.org/0000-0001-9510-7676) (Lecturer) had oversight of study co-ordination at the Salford research site, contributed to the study design and methods development, contributed to drafting the methods chapter and abstracts, edited the report and obtained funds to complete the project.
Publications
Edwardson CL, Biddle SJH, Clemes SA, Davies MJ, Dunstan DW, Eborall H, et al. Effectiveness of an intervention for reducing sitting time and improving health in office workers: three arm cluster randomised controlled trial. BMJ 2022;378:e069288.
Cox E, Walker S, Edwardson CL Biddle SJH, Clarke-Cornwell AM, Clemes SA, et al. The cost-effectiveness of the SMART work & Life intervention for reducing sitting time. Int J Environ Res Public Health 2022;19(22):14861.
Maylor BD, Edwardson CL, Dempsey PC, Patterson MR, Plekhanova T, Yates T, et al. Stepping towards more intuitive physical activity metrics with wrist-worn accelerometry: validity of an open-source step-count algorithm. Sensors 2022;22(24):9984.
Dawkins NP, Yates T, Edwardson CL, Maylor B, Henson J, Hall AP, et al. Importance of overall activity and intensity of activity for cardiometabolic risk in those with and without a chronic disease. Medicine and Science in Sports and Exercise 2022;54(9):1582–90.
Edwardson CL, Biddle S, Clarke-Cornwell A, Clemes S, Davies M, Dunstan D, et al. A three-arm cluster randomised controlled trial to test the effectiveness and cost-effectiveness of the SMArT Work & Life intervention for reducing daily sitting time in office workers: study protocol. BMC Public Health 2018;18:1120.
Dawkins NP, Yates T, Edwardson CL, Maylor B, Dallosso H, Davies MJ, et al. Comparing 24 h physical activity profiles: office workers, women with a history of gestational diabetes and people with chronic disease condition(s). J Sports Sci 2020;39:219–26.
Rowlands A, Davies M, Dempsey P, Edwardson C, Razieh C, Yates T. Wrist-worn accelerometers: recommending ~1.0 m g as the minimum clinically important difference (MCID) in daily average acceleration for inactive adults. Br J Sports Med 2021;55:814–5.
Data-sharing statement
Requests for access to data from the study should be addressed to the corresponding author at ce95@le.ac.uk. The study protocol has been published. All proposals requesting data access will need to specify how it is planned to use the data, and all proposals will need approval of the trial co-investigator team before data release.
Funding
This project was funded by the National Institute for Health and Care Research (NIHR) Public Health Research programme and will be published in full in Public Health Research; Vol. 11, No. 6. See the NIHR Journals Library website for further project information. The study was also supported by the NIHR Leicester Biomedical Research Centre, which is a partnership between University Hospitals of Leicester NHS Trust, Loughborough University and the University of Leicester.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
Appendix 1 Detailed statistical analysis plan
Appendix 2 Contact and approval details for each participating council
| Council | Initial contact and approval process |
|---|---|
| Leicester City Council | A public health consultant was approached and several meetings were held to discuss the study in detail. The public health consultant discussed the study with the director of public health. The study was approved by the Corporate management team and also presented at a well-being group meeting |
| Leicestershire County Council | The director of public health was approached and a meeting was held with a public health consultant. A discussion was held with the assistant director of corporate services. The head of operational property and facilities management, communications manager, and health, safety and well-being manager were informed. The study was approved by the corporate management team |
| Salford City Council | A public health consultant and the corporate strategy and communications manager were approached, and a meeting was arranged to discuss the study. The public health consultant discussed the study with the director of public health who then presented the study to the corporate management team at Salford City Council. A letter of support was provided prior to commencement of the study from the consultant in public health |
| Bolton Council | The director of public health at Salford was covering the same role at Bolton Council. The study was presented to the executive management team at Bolton Council by the director of public health. A letter of support was provided prior to commencement of the study from the assistant director of public health |
| Trafford Council | The sport and physical activity relationship manager was approached. A discussion was held with the workplace well-being lead. The study was subsequently approved by Trafford Council directors |
| Liverpool City Council | The physical activity and sports specialist was approached, a meeting was held with this contact, the physical activity and sport development co-ordinator, the strategic physical activity and sports development manager and a communications manager. A workforce physical activity strategy document was developed specifically for this study. The study was subsequently approved by the chief executive team |
Appendix 3 Participant recruitment
| Council | Recruitment process |
|---|---|
| Leicester City Council | The study and the briefing events were advertised via:
|
| Leicestershire County Councila | The study was advertised via:
|
| Salford City Council | The study and the briefing events were advertised via:
|
| Bolton Council | The study and briefing events were advertised via:
|
| Trafford Councilb | The study was advertised via:
|
| Liverpool City Councila | The study was advertised via:
|
Appendix 4 Timeline of intervention activities provided to the workplace champions
| Time point | Date to be carried out by | Date completed | Activity |
|---|---|---|---|
| SWAL delivery starts | w/c |
|
|
| ≈1 month following after training date | Desk installation (for participants randomised to that group) | ||
| Week 1 | w/c | Send e-mail number 1b – details of the first challenge | |
| Month 1 | w/c | Send e-mail number 2 | |
| Month 2 | w/c | Send e-mail number 3 | |
| Month 3 (3-month follow-up measurements) | ≈[enter month] 2018 |
|
|
| w/c | First group catch-up session – ensure you arrange a date and time and book a room. Please remember to audio-record this | ||
| w/c | Send e-mail numbers 4a and 4b – details for second challenge | ||
| w/c | Arrange a mentorship telephone call – soon after group catch-up | ||
| w/c |
Send study team scanned copy of completed:
|
||
| Month 4 | w/c | Send e-mail number 5 | |
| Month 5 | w/c | Send e-mail number 6 | |
| Month 6 | w/c | Send e-mail number 7 | |
| Month 7 | w/c | Send e-mail number 8 | |
| Month 8 | w/c | Send e-mail number 9 | |
| Month 9 | w/c | Second group catch-up session – ensure that you arrange a date and time and book a room. Please remember to audio-record this | |
| w/c | Send e-mail number 10 – details for third challenge | ||
| w/c | Arrange a mentorship telephone call – soon after group catch-up | ||
| w/c | Send study team scanned copy of completed:
|
||
| Month 10 | w/c | Send e-mail number 11 | |
| Month 11 | w/c | Send e-mail number 12 | |
| Month 12 (12-month follow-up measurements) | ≈[enter month] 2019 |
|
|
| Send e-mail number 13 | |||
| Month 13 | Send e-mail number 14 | ||
| Month 14 | w/c | Send e-mail number 15 | |
| Month 15 | w/c | Third group catch-up session – ensure that you arrange a date and time and book a room. Please remember to audio-record this | |
| w/c | Send e-mail number 16 – details for fourth challenge | ||
| w/c | Arrange a mentorship telephone call – soon after group catch-up | ||
| w/c | Send study team scanned copy of completed:
|
||
| Month 16 | w/c | Send e-mail number 17 | |
| Month 17 | w/c | Send e-mail number 18 | |
| Month 18 | w/c | Send e-mail number 19 | |
| Month 19 | w/c | Send e-mail number 20 | |
| Month 20 | w/c | Send e-mail number 21 | |
| Month 21 | w/c | Fourth group catch-up session – ensure that you arrange a date and time and book a room. Please remember to audio-record this | |
| w/c | Send e-mail number 22 – details for fifth challenge | ||
| w/c | Arrange a mentorship telephone call – soon after group catch-up | ||
| w/c | Send study team scanned copy of completed:
|
||
| Month 22 | w/c | Send e-mail number 23 | |
| Month 23 | w/c | Send e-mail number 24 | |
| Month 24 (24-month follow-up measurement) | ≈[enter month] 2020 |
|
|
| w/c | Send e-mail number 25 | ||
| w/c | Send study team scanned copy of completed:
|
Appendix 5 Agendas for each group catch-up session
Appendix 6 Measurement schedule for outcome measures
| Measure | Time point | ||
|---|---|---|---|
| Baseline | 3 months | 12 months | |
| Device-assessed sitting, standing and physical activity | ✓ | ✓ | ✓ |
| Self-reported sitting and breaks | ✓ | ✓ | ✓ |
| Office/desk dwell time | ✓ | ✓ | ✓ |
| Job performance | ✓ | ✓ | ✓ |
| Job satisfaction | ✓ | ✓ | ✓ |
| Work engagement (UWES) | ✓ | ✓ | ✓ |
| Occupational fatigue (NFR) | ✓ | ✓ | ✓ |
| Fatigue (physical and mental) | ✓ | ✓ | ✓ |
| Musculoskeletal symptoms (SNQ) | ✓ | ✓ | ✓ |
| Presenteeism (WLQ) | ✓ | ✓ | ✓ |
| Work demands | ✓ | ✓ | ✓ |
| Social norms and cohesion | ✓ | ✓ | ✓ |
| Quality of life | ✓ | ✓ | ✓ |
| Sleep duration and quality (PSQI) | ✓ | ✓ | ✓ |
| Self-reported sickness absence | ✓ | ✓ | |
| Sickness absence via employee records | ✓ | ✓ | |
| Anthropometric and blood pressure | ✓ | ✓ | ✓ |
| Biochemical | ✓ | ✓ | ✓ |
| Diet, smoking and alcohol | ✓ | ✓ | ✓ |
| Mental health | ✓ | ✓ | ✓ |
| Medical history and medication | ✓ | ✓ | ✓ |
| Demographics | ✓ | ||
| Job description | ✓ | ✓ | ✓ |
| Client Service Receipt Inventory | ✓ | ✓ | ✓ |
| Strategies for sitting less and moving more often | ✓ | ✓ | ✓ |
| Workplace audit | ✓ | ||
| Workplace champion characteristics | ✓ | ||
| Support for sitting less and moving move | ✓ | ✓ | ✓ |
Appendix 7 Process evaluation plan
| Area to measure | Theory | General process question | Data source and data collection method | Total number and sampling strategy/timescales |
|---|---|---|---|---|
| Recruitment | Social cognitive theory, self-regulation theory and relapse prevention theory | Number of worksites and office groups invited to participate, and number agreeing | Project records, including the number of office workers within each worksite approached, number attending of briefing events, number of reply slips returned and number consenting | During recruitment phase |
| Number of possible participants at each worksite and office group | Council logs of staff numbers | During recruitment phase | ||
| Number of participants opting-out, dropping out and non-compliance to the primary outcome measure | Participant attendance records at measurement visits, and short questionnaires to explore reasons for non-participation, dropping out and non-compliance (non-compliance assessed by analysing activPAL data) | Ongoing throughout the project | ||
| Intervention acceptability and fidelity: implementation | Social cognitive theory and organisational development theory | Was the intervention implemented as planned? | Observations of education sessions and coaching sessions | All initial education sessions (in both intervention arms) will be observed and a random (≈30%) sample of fresher sessions at 6, 12 and 18 months will be observed. A random (20%) sample of coaching sessions will be audio-recorded at each 3-month period |
| Observations in intervention office clusters | A random (50%) sample of intervention offices in both intervention arms will be observed for 1 whole day at several different time points during the 24-month intervention period | |||
| Records of education and coaching sessions taking place | Attendance logs at each education and coaching session | |||
| How did workplace champions experience scheduling and conducting the education sessions and ongoing coaching support? | Interviews, using a flexible topic guide, with workplace champions who are trained as educators and implemented the workshops, coaching sessions and competitions | Interviews with all workplace champions at 12 and 24 months | ||
| What were the participants’ experiences of the intervention (education sessions, coaching sessions, self-monitoring, etc.)? | Participant questionnaires and focus groups for intervention participants | Short questionnaires administered after education sessions to participants and at each measurement session (3, 12 and 24 months) for the remaining intervention components Three to five (final sample depends on data saturation in accordance with research question) focus groups (each group having four to eight with individuals) in each intervention arm at 12 and 24 months |
||
| Time spent on intervention delivery by workplace champions | Log of time for workplace champion to complete | Ongoing throughout the project | ||
| Intervention acceptability: participation | Social cognitive theory, habit theory and self-regulation theory | What proportion of the target group participated in the intervention? | Attendance logs at education sessions and coaching sessions | All intervention participants will sign in for the education sessions and workplace champions will keep a record of coaching sessions |
| What components of the intervention were preferred, and did this differ between males and females? | Questionnaires and focus groups with intervention participants | Brief questionnaires about the intervention components administered to all intervention participants at 3, 12 and 24 months during measurement session Three to five (final sample depends on data saturation in accordance with research question) focus groups (each group having four to eight individuals) in each intervention arm at 12 and 24 months |
||
| What strategies were put in place by intervention participants to facilitate behaviour change? | Questionnaires and focus groups with intervention participants | Brief questionnaire administered to all intervention participants at 3, 12 and 24 months during measurement session Three to five (final sample depends on data saturation in accordance with research question) focus groups (each group having four to eight individuals) in each intervention arm at 12 and 24 months |
||
| Intervention sustainability | Social cognitive theory, organisational development theory, habit theory, self-regulation theory and relapse prevention theory | What proportion of the target group maintained any changes in their behaviours and were there any differences between males and females? | Quantitative data from the activPAL device | Data from activPAL at 3, 12 and 24 months |
| Focus groups with intervention participants | Three to five (final sample depends on data saturation in accordance with research question) focus groups (each group having four to eight individuals) in each intervention arm immediately following completion of the intervention | |||
| Questionnaires for intervention participants | Brief questionnaires administered to all intervention participants at 12 and 24 months during measurement session | |||
| What proportion continued using/accessing intervention strategies across the study? | Focus groups with intervention participants | Three to five (final sample depends on data saturation in accordance with research question) focus groups (each group having four to eight individuals) in each intervention arm immediately following completion of the intervention | ||
| Questionnaires for intervention participants | Brief questionnaires administered to all intervention participants at 3, 12 and 24 months during measurement session | |||
| Are the participants/workplace champions/council going to continue with the intervention in some way and is there anything that needs to change with the intervention to assist with sustainability? | Interviews with workplace champions | Interviews with all workplace champions at 24 months | ||
| Focus groups with intervention participants | Three to five (final sample depends on data saturation in accordance with research question) focus groups (each group having four to eight individuals) in each intervention arm immediately following completion of the intervention | |||
| Interviews or focus groups with health and safety personnel and managers | Interviews or focus groups with a small sample of managers and other relevant staff (final sample depends on data saturation in accordance with research question) at the end of the RCT measurement (i.e. 24 months) | |||
| Intervention contamination | None | Did movement of staff (e.g. participants, health and safety personnel) occur from intervention to control office groups? | Control office groups to keep a log of any staff changes | Logs collected on completion of the 12- and 24-month follow-up assessments |
| Did intervention participants interact with control participants? | Focus groups with intervention and control participants | Three to five (final sample depends on data saturation in accordance with research question) focus groups with intervention and control participants at 12 and 24 months | ||
| Do control office clusters engage in any strategies that may impact on their activity levels during work? | Observations in control office clusters | A random (50%) sample of control offices will be observed for 1 whole day at time points during the 24-month intervention period | ||
| Brief questionnaire | Brief questionnaires administered to all control participants at 3, 12 and 24 months during measurement session | |||
| Unexpected events arising from the study | Social cognitive theory, habit theory, self-regulation theory and relapse prevention theory | Did intervention and control participants modify their behaviours based on information provided at the baseline and follow-up measurements? | Focus groups and questionnaires to intervention and control participants | Short self-report question asked to intervention and control participants after all measurement sessions at 3, 12 and 24 months Three to five (final sample depends on data saturation in accordance with research question) focus groups with intervention and control participants at 12 and 24 months |
| Did the measurements prompt GP visits? | Brief health services use questionnaire | Brief questionnaire administered to all participants at 3, 12 and 24 months during measurement session | ||
| Did the participant experience any injuries/discomfort that may have been a result of a change in behaviour as a result of the intervention? | Questionnaire to intervention participants | Brief questionnaire administered to all intervention participants at 3, 12 and 24 months during measurement session | ||
| Did intervention participants change an existing activity-related behaviour for another as a result of participating in the study? | Focus groups and questionnaires to intervention participants | Short self-report question asked to intervention and control participants after all measurement sessions at 3, 12 and 24 months Three to five (final sample depends on data saturation in accordance with research question) focus groups (each group having four to eight individuals) in each intervention arm at 12 and 24 months |
Appendix 8 Group catch-up session assessment tool
Catch-up session 1
| Cluster ID | |||
|---|---|---|---|
| Section 1: session introduction; duration: 5 minutes | Outcome | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Champion outlines aim of session [e.g. to find out how everyone’s been getting on, to share tips and generate ideas, to have a discussion about the standing desk (if appropriate for the group), to revisit goal setting] | |||
| Section 2: your story; duration: 10 minutes | Present | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Record [flip chart, whiteboard, Post-it notes (3M, Bracknell, UK)] what’s been going well and what’s not been going well with reducing sitting time | |||
| Discussion around what helped/strategies used to help reduce sitting time | |||
| Discussion around any benefits experienced from reducing sitting | |||
| Acknowledges and identifies barriers/what’s not been going well | |||
| Discussion to identify solutions to overcome barriers | |||
| Champion reminds group about the online education programme | |||
| Section 3: refresher of key messages; duration: 10 minutes | Present | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Champion asked and covered time spent sitting: how much of the day should be spent sitting? | |||
| Champion asked and covered time spent sitting: how often to get up and move? | |||
| Champion asked and covered time spent sitting: how long to stand or move around for? | |||
| Champion informs the group about studies showing reduction in sitting time benefiting health and well-being | |||
| Discussion about things to do at work to reduce sitting time | |||
| Following discussion about things to do at work to reduce sitting time, champion encourages group to choose one or two ideas to try at work | |||
| Champion asks what people could do outside work to reduce sitting time | |||
| Champion asks how to get family and friends involved | |||
| Champion reminds group about the online education programme/phone apps/computer software/resources | |||
| Section 4: goal-setting; duration: 5 minutes | Present | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Champion provides goal-setting worksheet to each participant | |||
| Champion asks group questions to encourage them to reflect on previous goals they set themselves | |||
| Champion informs group why it’s important to write goals down | |||
| Champion encourages group to set a new goal and complete a new goal-setting sheet | |||
| OARS | |||
| Champion used open-ended questions | |||
| Champions used affirmations (e.g. highlighting positive attributes, strengths and efforts, moves away from focusing on problems to be fixed to positives that can be drawn on to help). Affirmations are different from praise or giving compliments | |||
| Champion used reflections (e.g. repeating or paraphrasing to further explore the statement and/or show you have listened to the participant) | |||
| Champion used summaries during the session | |||
| Section 5: next steps; duration: 2 minutes | Present | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Champion informs group when the next session will take place | |||
| Champion informs group they will continue to receive e-mails and challenges | |||
| Champion informs group who to contact with any study-related queries | |||
Catch-up session 2
| Cluster ID | |||
|---|---|---|---|
| Section 1: session introduction; duration: 2 minutes | Outcome | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Champion outlines aim of session (e.g. to find out how everyone’s been getting on, discussing slip-ups and relapse) | |||
| Section 2: your story; duration: 11 minutes | Present | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Champion reminds group about the first catch-up session (i.e. ideas generated for group activities/changes to office to help reduce sitting time, things done outside work) | |||
| Referring back to catch-up session 1 ideas: discussion around how they have been getting on with reducing sitting time | |||
| Champion provides a group action plan worksheet | |||
| Champion either runs through the plan/allows group some time to complete it together | |||
| Discussion around why doing something at work is helpful (generic benefits) | |||
| Discussion around how people have been getting on with reducing sitting time outside work (i.e. challenges, strategies, tips and advice) | |||
| Discussion around benefits experienced by people from reducing sitting time | |||
| Champion reminds group about the online education programme/phone apps/computer software/resources. | |||
| Section 3: slip-ups and relapse; duration: 15 minutes | Present | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Champion provides group with information about slip-ups and relapse | |||
| Discusses and elicits how slip-ups and relapse can help (i.e. to see what’s going wrong/challenges, opportunity to learn) | |||
| Champion explores situations where there may be an increased risk of slip-ups and relapse either using a pre-prepared flip chart (as outlined in manual) or examples from the group | |||
| Opportunity to identify strategies to overcome slip-ups or relapse that the group explored | |||
| Champion provides ‘preparing for slip-ups and relapse’ worksheet | |||
| Champion either runs through the ‘preparing for slip-ups and relapse’ worksheet or allows the group some time to complete it | |||
| Champion checks if anyone has any questions | |||
| OARS | |||
| Champion used open-ended questions | |||
| Champions used affirmations (e.g. highlighting positive attributes, strengths and efforts, moves away from focusing on problems to be fixed to positives that can be drawn on to help) | |||
| Affirmations are different from praise or giving compliments | |||
| Champion used reflections (e.g. repeating or paraphrasing) | |||
| Section 4: next steps; duration: 2 minutes | Present | If absent/attempted, why? | Comments: anything else you think is important or relevant |
| Start time: | |||
| End time: | |||
| Champion informs group when the next session will take place | |||
| Champion reminds group they will continue to receive e-mails and challenges | |||
| Champion informs group who to contact with any study-related queries | |||
| Champion hands out Post-it notes and asks participants to write down benefits they have experienced from reducing sitting time | |||
| Champion informs the group how information on Post-it notes will be used | |||
Appendix 9 Summary of possible participants within each local authority
| Local authority | Viable clusters, n | Possible participants, n | Participants enrolled, % |
|---|---|---|---|
| Leicester City | 31 | 1095 | 30.7 |
| Leicester County | 11 | 889 | 13.8 |
| Bolton | 6 | 269 | 23.4 |
| Salford City | 11 | 474 | 26.6 |
| Trafford | 4 | 249 | 19.3 |
| Liverpool City | 15 | 864 | 13.3 |
Appendix 10 Summary of intervention participation and implementation by cluster by 12-month follow-up data collection
| Cluster ID | Intervention arm | WPC trained | Per cent of cluster completing online education | Per cent of e-mails sent | Per cent of challenges delivered | Per cent of catch-up sessions held | Per cent using self-monitoring tools | Per cent using desk at least a few times a week |
|---|---|---|---|---|---|---|---|---|
| L01 | SWAL | Yes | 71.4 | 100.0 | 100.0 | 100.0 | 100.0 | N/A |
| L02 | SWAL | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 78.6 | N/A |
| L03 | Desk | Yes | 90.0 | 91.7 | 100.0 | 100.0 | 42.1 | 84.2 |
| L05 | SWAL | Yes | 77.8 | 100.0 | 100.0 | 100.0 | 62.5 | N/A |
| L08 | Desk | Yes | 80.0 | 18.2 | 0.0 | 0.0 | 40.0 | 80.0 |
| L10 | Desk | Yes | 85.7 | 100.0 | 100.0 | 100.0 | 80.0 | 100.0 |
| L12 | Desk | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 80.0 | 33.3 |
| L13 | SWAL | Yes | 100.0 | 70.0 | 66.7 | 50.0 | 80.0 | N/A |
| L14 | SWAL | Yes | 71.4 | 100.0 | 100.0 | 100.0 | 83.3 | N/A |
| L15 | Desk | Yes | 77.8 | 27.3 | 33.3 | 0.0 | 60.0 | 77.8 |
| L17 | Desk | Yes | 88.9 | 100.0 | 100.0 | 100.0 | 77.8 | 87.5 |
| L18 | Desk | Yes | 100.0 | 54.5 | 66.7 | 50.0 | 50.0 | 100.0 |
| L21 | SWAL | Yes | 80.0 | 36.4 | 66.7 | 50.0 | 50.0 | N/A |
| L22 | SWAL | Yes | 66.7 | 54.5 | 66.7 | 50.0 | 77.8 | N/A |
| L23 | SWAL | Yes | 100.0 | 27.3 | 33.3 | 100.0 | 100.0 | N/A |
| L24 | SWAL | Yes | 83.3 | 90.9 | 66.7 | 50.0 | 75.0 | N/A |
| L26 | SWAL | No | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | N/A |
| L28 | SWAL | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 80.0 | N/A |
| L30 | Desk | Yes | 75.0 | 36.4 | 33.3 | 0.0 | 87.5 | 75.0 |
| L32 | Desk | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 40.0 | 88.9 |
| L34 | Desk | Yes | 100.0 | 90.9 | 100.0 | 100.0 | 100.0 | 100.0 |
| L35 | SWAL | Yes | 50.0 | 0.0 | 0.0 | 0.0 | 0.0 | N/A |
| L36 | Desk | Yes | 100.0 | 90.0 | 66.7 | 0.0 | 60.0 | 60.0 |
| L39 | Desk | Yes | 100.0 | 40.0 | 66.7 | 50.0 | 33.3 | 66.7 |
| L40 | SWAL | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 33.3 | N/A |
| L41 | Desk | Yes | 93.3 | 100.0 | 100.0 | 100.0 | 46.7 | 85.71 |
| L42 | SWAL | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 62.5 | N/A |
| L45 | SWAL | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 55.6 | N/A |
| S02 | Desk | Yes | 70.6 | 100.0 | 100.0 | 100.0 | 35.7 | 66.67 |
| S03 | SWAL | Yes | 85.7 | 100.0 | 100.0 | 100.0 | 50.0 | N/A |
| S06 | SWAL | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 0.0 | N/A |
| S07 | Desk | Yes | 83.3 | 100.0 | 100.0 | 100.0 | 100.0 | 100.00 |
| S09 | SWAL | Yes | 100.0 | 80.0 | 66.7 | 0.0 | 50.0 | N/A |
| S10 | Desk | Yes | 60.0 | 90.0 | 66.7 | 50.0 | 40.0 | 60.00 |
| S11 | SWAL | Yes | 81.8 | 80.0 | 100.0 | 100.0 | 42.9 | N/A |
| S12 | Desk | Yes | 72.7 | 100.0 | 100.0 | 100.0 | 66.7 | 62.50 |
| S13 | SWAL | Yes | 50.0 | 0.0 | 0.0 | 0.0 | 20.0 | N/A |
| S15 | Desk | Yes | 66.7 | 30.0 | 33.3 | 50.0 | 75.0 | 100.00 |
| S16 | Desk | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 16.7 | 100.00 |
| S18 | SWAL | Yes | 100.0 | 100.0 | 100.0 | 100.0 | 60.0 | N/A |
| S19 | SWAL | Yes | 62.5 | 100.0 | 100.0 | 100.0 | 16.7 | N/A |
| S21 | Desk | Yes | 33.3 | 100.0 | 100.0 | 50.0 | 20.0 | 60.00 |
| S22 | Desk | Yes | 33.3 | 100.0 | 100.0 | 50.0 | 33.3 | 100.00 |
| S23 | SWAL | Yes | 84.2 | 100.0 | 100.0 | 100.0 | 56.3 | N/A |
| S24 | Desk | Yes | 40.0 | 100.0 | 100.0 | 100.0 | 60.0 | 75.00 |
| S27 | Desk | Yes | 80.0 | 50.0 | 100.0 | 100.0 | 40.0 | 100.00 |
| S29 | SWAL | Yes | 68.8 | 100.0 | 100.0 | 100.0 | 78.6 | N/A |
| S32 | SWAL | Yes | 77.8 | 70.0 | 66.7 | 100.0 | 66.7 | N/A |
| S33 | Desk | Yes | 75.0 | 100.0 | 100.0 | 100.0 | 50.0 | 100.00 |
| S34 | SWAL | Yes | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | N/A |
| S35 | SWAL | Yes | 60.0 | 50.0 | 50.0 | 100.0 | 66.7 | N/A |
| S37 | Desk | Yes | 61.5 | 0.0 | 0.0 | 100.0 | 33.3 | 63.64 |
Appendix 11 Summary of desks chosen by participants between study sites
| Desk model | Study site | |
|---|---|---|
| Leicester | Salford | |
| Deskrite 100 | 29 | 14 |
| Yo-Yo Mini | 17 | 47 |
| Yo-Yo 90 | 89 | 38 |
| Yo-Yo Go1 | 5 | 1 |
Appendix 12 Influence of health assessments on the motivation to change behaviour
| Statement | SWAL only, % | SWAL plus desk, % | ||
|---|---|---|---|---|
| 3 months: agree or strongly agree | 12 months: agree or strongly agree | 3 months: agree or strongly agree | 12 months: agree or strongly agree | |
| Knowing that I would receive a follow-up health assessment motivated me to want to change aspects of my lifestyle | 76.0 | 66.0 | 74.8 | 62.4 |
| Knowing that I would receive a follow-up health assessment motivated me to want to change how much time I spent sitting | 70.7 | 66.0 | 74.2 | 63.0 |
Appendix 13 Health economics analysis plan
Appendix 14 Health-care unit costs
| Resource | Unit cost (£) | Source |
|---|---|---|
| Primary care | ||
| GP: surgery visit | 33.00 | PSSRU 2019160 |
| GP: home visit | 107.07 | PSSRU 2010161 |
| GP: telephone call | 15.32 | PSSRU 2019160 |
| General practice nurse: surgery visit | 5.69 | PSSRU 2019160 |
| General practice nurse: home visit | 31.44 | PSSRU 2010161 |
| General practice nurse: telephone call | 6.00 | PSSRU 2019160 |
| NHS walk-in centre visit | 46.00 | NICE guideline 94162 |
| NHS urgent care centre visit | 67.00 | NICE guideline 94162 |
| Community services | ||
| Occupational health nurse | 39.42 | NHS reference costs 2017/18163 |
| Mental health care | ||
| Mental health nurse | 92.00 | PSSRU 2019160 |
| Other counsellor/therapist | 182.71 | NHS reference costs 2017/18163 (MHSTOTHPLA) |
| Secondary care | ||
| Accident and emergency visit | 112.41 | PSSRU 2010161 |
| Hospital outpatient appointments | 137.58 | NHS reference costs 2017/18163 (General Surgery) |
Appendix 15 Longer-term model schematic
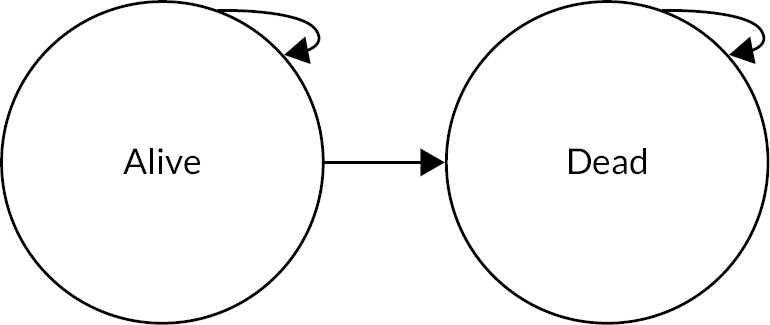
Appendix 16 Sedentary hazard ratios and interpolation between points
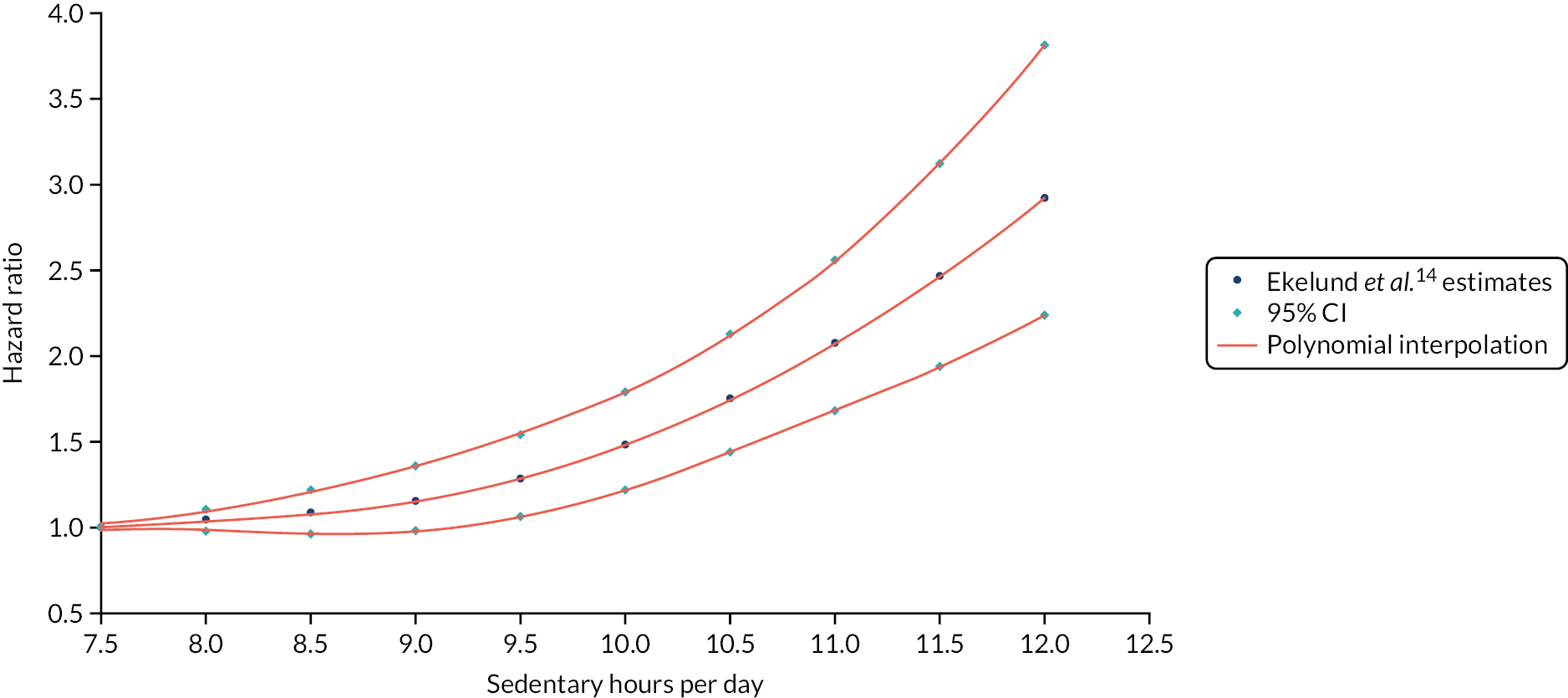
Appendix 17 Economic analysis inputs and key assumptions
| Input | Deterministic value | Probabilistic value | Description of inputs and relevant assumptions |
|---|---|---|---|
| Characteristics | |||
| Age (years) | 40 | N/A | Trial average characteristics: alternative age profiles explored in scenario analyses |
| Gender (male) | 28% | N/A | |
| Ethnicity (white British) | 69.7% | N/A | |
| Baseline BMI (kg/m2) | 26.47 | N/A | |
| Parameters | |||
| Sedentary behaviour | |||
| Baseline sedentary time (minutes/day) | 605.24 | SB ~N(605.24 to 6762) | Applied the average sedentary behaviour observed across all trial participants |
| Treatment effect | |||
| SWAL (plus desk) (minutes/day) | 63.73a | TESWAL_D ~N(63.73 to 69.63) | Treatment effects derived in primary trial analysis and assumed to follow a normal distribution |
| SWAL (no desk) (minutes/day) | 22.22a | TESWAL_D ~N(63.73 to 69.63) | |
| Decay rate | 50% per annum | N/A | Alternative rates and relationships explored in sensitivity and scenario analyses |
| Costs | |||
| Intervention costs (£) | |||
| SWAL (plus desk) | 228.31 | N/A | Alternative SWAL programme cost profiles explored in sensitivity analyses |
| SWAL (no desk) | 80.59 | N/A | |
| Control | 0 | N/A | |
| Within-trial costs (£) | |||
| SWAL (plus desk) | 602.86 | 95% CI 449.50 to 785.67 | Generalised linear model assuming multivariate normality with log-link and gamma family. Alternative regression methods and costings explored in scenario analyses. The mean and 95% credible intervals from 1000 draws are provided |
| SWAL (no desk) | 706.37 | 95% CI 524.00 to 906.12 | |
| Control | 749.14 | 95% CI 541.71 to 1003.22 | |
| Long-term costs | |||
| Lifetime costs | Age-adjusted average lifetime health-care costs in the English NHS reported by Asaria115 were explored as a scenario | ||
| HRQoL | |||
| Within-trial HRQoL | |||
| SWAL (plus desk) | 0.85222 | 95% CI 0.82478 to 0.87863 | Ordinary least squares estimation assuming multivariate normality. Alternative regression methods and preference weights (EQ-5D-5L) explored in scenario analyses. The mean and 95% credible intervals from 1000 draws are provided |
| SWAL (no desk) | 0.85727 | 95% CI 0.82894 to 0.88708 | |
| Control | 0.85257 | 95% CI 0.82187 to 0.88300 | |
| Longer-term HRQoL | 18–24 years: 0.929 | N/A | TTO UK general population age-adjusted HRQoL using the EQ-5D-3L – Janssen et al.105 It was assumed that individuals in each arm experienced the same UK general population HRQoL beyond the trial (i.e. within-trial differences were removed immediately after month 12) |
| 25–34 years: 0.919 | |||
| 35–44 years: 0.893 | |||
| 45–54 years: 0.855 | |||
| 55–64 years: 0.810 | |||
| 65–74 years: 0.773 | |||
| 75 years: 0.703 | |||
| Mortality risk | |||
| Baseline hazards | Assumed baseline mortality hazards of office workers in the UK were equal to ONS age- and gender-specific general population mortality rates | ||
| Sedentary hazard ratios | See Figure 2 | See Figure 2 | Dose–response relationship between sedentary behaviour and all-cause mortality derived from Ekelund et al.’s14 harmonised meta-analysis of accelerometer-measured physical activity and sedentary behaviour on all-cause mortality. Polynomial functions used to interpolate between points. Estimates, including non-accelerometer measures of sedentary behaviour, were explored in a scenario analysis (Patterson et al.13) |
| Discount rate | |||
| Costs | 3.5% | N/A | In line with NICE guidance, a 1.5% discount rate was explored as a scenario113 |
| QALYs | 3.5% | N/A | |
Appendix 18 Primary health economic trial outcomes
| Outcome | SWAL plus desk | SWAL only | Standard care | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Month 3 | Month 12 | Baseline | Month 3 | Month12 | Baseline | Month 3 | Month 12 | |
| EQ-5D-5L | 0.90031 | 0.90788 | 0.89748 | 0.89944 | 0.90484 | 0.89473 | 0.90333 | 0.90272 | 0.89956 |
| (Mapped) EQ-5D-3L | 0.84358 | 0.85060 | 0.83568 | 0.83693 | 0.84956 | 0.83969 | 0.84589 | 0.84893 | 0.84260 |
| QALYs (EQ-5D-5L)a | 0.89879 | 0.89520 | 0.89832 | ||||||
| QALYs (EQ-5D-3L)a,b | 0.84144 | 0.84113 | 0.84712 | ||||||
Appendix 19 Modelled sedentary time in each trial arm

Appendix 20 Modelled hazard ratios in each trial arm (relative to the control arm)

Appendix 21 Extrapolated discounted incremental quality-adjusted life-year gain for each intervention relative to the control arm by alternative decay rates
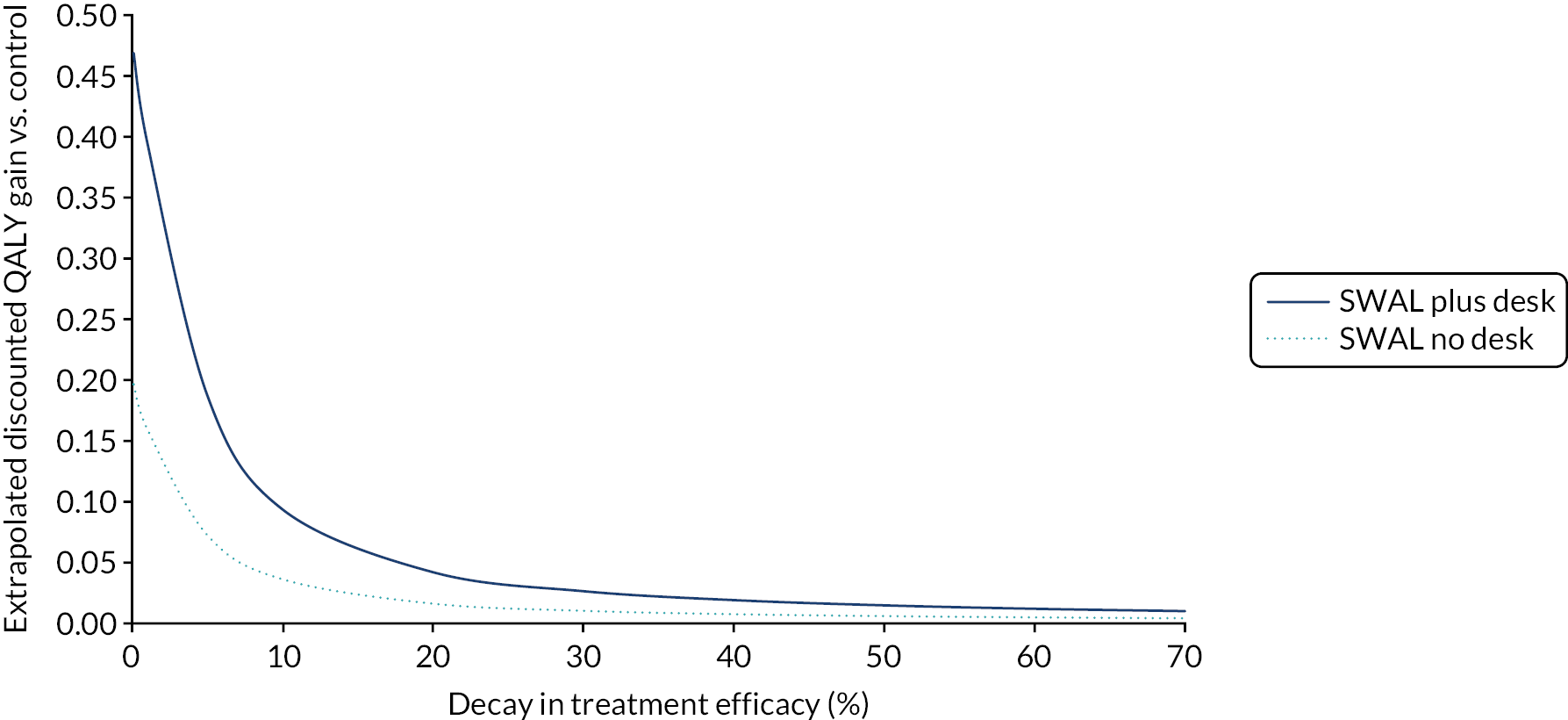
Appendix 22 Extrapolated discounted incremental quality-adjusted life-year gain for each intervention relative to the control arm by alternative ages at intervention

Appendix 23 Secondary cost-effectiveness analysis
| Secondary cost-effectiveness analysis | SWAL plus desk vs. control | SWAL only vs. control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline, mean differential | Month 12, mean differential | Difference in differencea | ICER | Baseline, mean differential | Month 12, mean differential | Difference in differencea | ICER | |||
| Direct cost (1) | Estimated cost (2) | Direct cost (1) | Estimated cost (2) | |||||||
| Costs | ||||||||||
| (1) Direct intervention costs | £228.31 | £228.31 | £80.59 | £80.59 | ||||||
| (2) Within-trial differences + (1)a | £228.31 | –£126.07 | £105.54 | £80.59 | –£34.14 | £49.13 | ||||
| Outcomes and cost-effectiveness | ||||||||||
| Sedentary minutes | ||||||||||
| Unadjusted | 7.8 | –61.5 | –69.3 | £3.29b | £1.52b | 3.6 | –21.4 | –25.0 | £3.22b | £1.97b |
| Adjusted§ | –63.7c | £3.58b | £1.66b | –22.2c | £3.63b | £2.20b | ||||
| PSS | 0.455 | –0.223 | –0.678 | £336.72b | £155.65b | 1.098 | 0.542 | –0.556 | £144.98b | £88.39b |
| WHO-5 Wellbeing Index | 0.053 | 1.484 | 1.431 | £159.55 | £73.75 | –2.014 | –0.640 | 1.373 | £58.69 | £35.78 |
| UWES: work engagement | 0.017 | 0.091 | 0.074 | £3085.27 | £1426.22 | 0.158 | 0.176 | 0.018 | £4492.02 | £2738.46 |
| Work satisfactiond | 0.0826 | 0.008 | –0.075 | Dominated | Dominated | 0.226 | 0.302 | 0.076 | £1060.39 | £646.45 |
| Work performancee | 0.063 | 0.118 | 0.055 | £4151.09 | £1918.91 | 0.076 | 0.090 | 0.014 | £5756.43 | £3509.29 |
| Sick days | –0.642 | 0.787 | 1.428 | Dominated | Dominated | –0.507 | 0.438 | 0.945 | Dominated | Dominated |
List of abbreviations
- app
- application
- BMI
- body mass index
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GP
- general practitioner
- HbA1c
- glycated haemoglobin
- HDL
- high-density lipoprotein
- HRQoL
- health-related quality of life
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- INHB
- incremental net health benefit
- INMB
- incremental net monetary benefit
- IQR
- interquartile range
- IRR
- inter-rater reliability
- IT
- information technology
- ITT
- intention to treat
- LDL
- low-density lipoprotein
- MVPA
- moderate to vigorous physical activity
- NICE
- National Institute for Health and Care Excellence
- OARS
- Open-ended questions, Affirmations, Reflections, and Summaries
- PSS
- Perceived Stress Scale
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SMArT Work
- Stand More AT Work
- SNQ
- Standardised Nordic Questionnaire
- SWAL
- SMART Work & Life
- TSC
- Trial Steering Committee
- TV
- television
- UWES
- Utrecht Work Engagement Scale
- WHO
- World Health Organization
Notes
-
Trial (non-intervention) total costs: complete-case analysis
-
Baseline trial resource use (3 months prior): complete-case analysis
-
Trial resource use (3–12 months assumed): complete-case analysis
-
Assumed costs (3–12 months’ follow-up): complete-case analysis
-
Base-case quality-adjusted life-year regression, using crosswalk EuroQol-5 Dimensions, three-level version, preference weights
-
Scenario quality-adjusted life-year regression, using EuroQol-5 Dimensions, five-level version, preference weights
-
Multilevel quality-adjusted life-year regression, using crosswalk EuroQol-5 Dimensions, three-level version, preference weights
-
Multilevel quality-adjusted life-year regression, using EuroQol-5 Dimensions, five-level version, preference weights
-
Cost-effectiveness scenario analysis: the inclusion of lifetime costs
-
Cost-effectiveness scenario analysis: linear efficacy decay (5-year effect; 20% decay per annum)
-
Cost-effectiveness scenario analysis: exponential 70% decay in efficacy per annum
-
Cost-effectiveness scenario analysis: exponential 60% decay in efficacy per annum
-
Cost-effectiveness scenario analysis: exponential 40% decay in efficacy per annum
-
Cost-effectiveness scenario analysis: exponential 30% decay in efficacy per annum
-
Cost-effectiveness scenario analysis: exponential 20% decay in efficacy per annum
-
Cost-effectiveness scenario analysis: exponential 10% decay in efficacy per annum
-
Cost-effectiveness scenario analysis: 0% decay in efficacy per annum
-
Cost-effectiveness scenario analysis: Patterson et al . 13 all-cause relative risk mortality estimates from sedentary behaviour
-
Cost-effectiveness scenario analysis: EuroQol-5 Dimensions, five-level version, preference values
-
Cost-effectiveness scenario analysis: EuroQol-5 Dimensions, five-level version, preference values within trial time horizon
-
Cost-effectiveness scenario analysis: no within-trial cost or quality-adjusted life-years differences between arms
-
Cost-effectiveness scenario analysis: 1.5% discounting of costs and quality-adjusted life-years
-
Within-trial cost-effectiveness scenario analysis: multilevel regression analysis of within-trial costs and quality-adjusted life-years
-
Cost-effectiveness scenario analysis: multilevel regression analysis of within-trial costs and quality-adjusted life-years
-
Sensitivity of net monetary benefit (k = £30,000) to the rate of treatment decay for SMART Work & Life plus desk and SMART Work & Life only, relative to control
-
Sensitivity of net monetary benefit (k = £30,000) to the age at provision for SMART Work & Life plus desk and SMART Work & Life only, relative to control
-
Sensitivity of net monetary benefit (k = £15,000) to the rate of treatment decay for SMART Work & Life plus desk and SMART Work & Life only, relative to control
-
Sensitivity of net monetary benefit (k = £15,000) to the age at provision for SMART Work & Life plus desk and SMART Work & Life only, relative to control
-
Two-way sensitivity analysis by age and efficacy decay of the incremental cost-effectiveness ratios of the SMART Work & Life plus desk intervention versus SMART Work & Life only: Ekelund et al . 14 estimates of all-cause mortality risks associated with sedentary behaviour
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/DNYC2141).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
